From FUS to Fibs: What's New in Frontotemporal ... - IOS Press
From FUS to Fibs: What's New in Frontotemporal ... - IOS Press
From FUS to Fibs: What's New in Frontotemporal ... - IOS Press
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Journal of Alzheimer’s Disease 21 (2010) 349–360 349<br />
DOI 10.3233/JAD-2010-091513<br />
<strong>IOS</strong> <strong>Press</strong><br />
Review<br />
<strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong><br />
Fron<strong>to</strong>temporal Dementia?<br />
James R. Burrell a,b and John R. Hodges a,∗<br />
a Pr<strong>in</strong>ce of Wales Medical Research Institute, University of <strong>New</strong> South Wales, Sydney, Australia<br />
b Pr<strong>in</strong>ce of Wales Cl<strong>in</strong>ical School, University of <strong>New</strong> South Wales, Sydney, Australia<br />
Accepted 1 February 2010<br />
Abstract. Fron<strong>to</strong>temporal dementia (FTD) is an important cause of non-Alzheimer’s dementia and is the second most common<br />
cause of young onset dementia. FTD presents with progressive changes <strong>in</strong> behavior and personality (behavioral variant FTD)<br />
or language deficits (also known as primary progressive aphasia), although both commonly coexist. Patients with progressive<br />
aphasia are subclassified accord<strong>in</strong>g <strong>to</strong> the pattern of language deficits <strong>in</strong><strong>to</strong> those with progressive non-fluent aphasia (PNFA)<br />
and semantic dementia (SD). FTD is pathologically heterogeneous, both macroscopically and on a molecular level, with tau<br />
positive, TDP-43 positive, and <strong>FUS</strong> positive <strong>in</strong>traneuronal <strong>in</strong>clusions recognized on immunohis<strong>to</strong>chemical analysis. TDP-43<br />
positive <strong>in</strong>clusions are also a feature of amyotrophic lateral sclerosis pathology, corroborat<strong>in</strong>g the observation of overlapp<strong>in</strong>g<br />
cl<strong>in</strong>ical features between the two conditions and reaffirm<strong>in</strong>g the FTD-ALS disease spectrum. Most FTD cases are sporadic, but an<br />
important m<strong>in</strong>ority is <strong>in</strong>herited <strong>in</strong> an au<strong>to</strong>somal dom<strong>in</strong>ant fashion, most commonly due <strong>to</strong> MAPT or progranul<strong>in</strong> gene mutations.<br />
Familial clusters of FTD and amyotrophic lateral sclerosis are also recognized but poorly unders<strong>to</strong>od. This paper reviews the<br />
cl<strong>in</strong>ical phenotypes, assessment and treatment of FTD <strong>in</strong> light of recent pathological and genetic discoveries.<br />
Keywords: Behavioral variant FTD, fron<strong>to</strong>temporal dementia, FTD-ALS, progressive non-fluent aphasia, semantic dementia, tau,<br />
TDP-43<br />
INTRODUCTION<br />
The recent demonstration of TAR-DNA b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong><br />
43 (TDP-43) as the constituent of ubiqu<strong>in</strong>tated<br />
<strong>in</strong>traneuronal <strong>in</strong>clusions <strong>in</strong> fron<strong>to</strong>temporal dementia<br />
(FTD) and amyotrophic lateral sclerosis (ALS) has<br />
stimulated a surge of cl<strong>in</strong>ical, pathological, and genetic<br />
research <strong>in</strong><strong>to</strong> these overlapp<strong>in</strong>g entities. FTD is the second<br />
most common cause of young onset dementia after<br />
Alzheimer’s disease [1,2], and three dist<strong>in</strong>ct cl<strong>in</strong>ical<br />
phenotypes of FTD are recognized, each with variable<br />
degrees of progressive behavior and language distur-<br />
∗ Correspondence <strong>to</strong>: Prof. John R. Hodges, Pr<strong>in</strong>ce of Wales<br />
Medical Research Institute, Cnr Barker St and Easy St, Randwick,<br />
Sydney, NSW 2031, Australia. Tel.: +61 2 9399 1132; Fax: +61 2<br />
9399 1005; E-mail: j.hodges@powmri.edu.au.<br />
ISSN 1387-2877/10/$27.50 © 2010 – <strong>IOS</strong> <strong>Press</strong> and the authors. All rights reserved<br />
bance. A proportion of patients with FTD also develop<br />
cl<strong>in</strong>ical and neurophysiological evidence of mo<strong>to</strong>r<br />
neuron dysfunction and many satisfy the El Escorial<br />
criteria for the diagnosis of ALS [3]. The pathology<br />
of FTD is heterogeneous with variable degrees of focal<br />
frontal and temporal atrophy [4]. Three <strong>in</strong>traneuronal<br />
<strong>in</strong>clusions types have been characterized immunohis<strong>to</strong>chemically<br />
as tau, TDP-43 or fused <strong>in</strong> sarcoma (<strong>FUS</strong>)<br />
positive [5–8]. TDP-43 positive <strong>in</strong>clusions are the most<br />
common type <strong>in</strong> FTD and are also identified <strong>in</strong> the<br />
majority of ALS cases [9,10].<br />
Until recently, FTD was considered a rare cause of<br />
dementia and cl<strong>in</strong>ical dist<strong>in</strong>ction from AD was considered<br />
very difficult [11,12]. Over time, the def<strong>in</strong><strong>in</strong>g<br />
cl<strong>in</strong>ical features of FTD have been elucidated and<br />
three cl<strong>in</strong>ical phenotypes are recognized (see Fig. 1).<br />
The behavioral variant of FTD (bvFTD) is character-
350 J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia?<br />
Fig. 1. Cl<strong>in</strong>ical Phenotypes of FTD. FTD is subclassified as behavioral variant (bvFTD) if behavior and personality changes predom<strong>in</strong>ate; Tau<br />
(green) and TDP-43 (blue) pathology are equally prevalent. Language variants <strong>in</strong>clude progressive non-fluent aphasia (PNFA), <strong>in</strong> which tau<br />
pathology is most prevalent and semantic dementia (SD), <strong>in</strong> which TDP-43 pathology is almost universal.<br />
Fig. 2. MRI appearances <strong>in</strong> FTD. T1 weighted, coronal MRI images reveal: A) bvFTD – dorsolateral and orbi<strong>to</strong>mesial, bifrontal atrophy, with<br />
dilatation of anterior horns of lateral ventricles (left > right); B) PNFA – moderate temporal atrophy (left > right) with subtle enlargement of<br />
the sylvian fissure due <strong>to</strong> <strong>in</strong>sula atrophy (s<strong>in</strong>gle arrow); C) SD – anterior temporal atrophy, severe on the left (double arrow) and moderate on the<br />
right with associated orbi<strong>to</strong>frontal atrophy.<br />
ized by marked changes <strong>in</strong> behavior and personality,<br />
with relatively preserved language function. Alternatively,<br />
patients with semantic dementia (SD) and progressive<br />
non-fluent aphasia (PNFA) develop progressive<br />
language deficits, with more subtle personality and<br />
behavior changes. FTD is a progressive neurodegenerative<br />
disorder and the median survival from symp<strong>to</strong>m<br />
onset is 6–8 years, but patients with FTD and ALS have<br />
an even worse prognosis [13,14].<br />
This review cannot cover every facet of this rapidly<br />
evolv<strong>in</strong>g field, but rather attempts <strong>to</strong> place the recent<br />
pathological and genetic discoveries with<strong>in</strong> the context<br />
of the cl<strong>in</strong>ical phenotypes of FTD and <strong>to</strong> outl<strong>in</strong>e an<br />
approach <strong>to</strong> cl<strong>in</strong>ical assessment and treatment.<br />
PATHOLOGY<br />
Focal frontal and temporal atrophy is identified <strong>in</strong><br />
patients with FTD on au<strong>to</strong>psy [4], but the pattern of<br />
atrophy varies significantly among the cl<strong>in</strong>ical phenotypes.<br />
Bilateral mesial and orbi<strong>to</strong>frontal and temporal<br />
atrophy is the characteristic f<strong>in</strong>d<strong>in</strong>g <strong>in</strong> patients with<br />
bvFTD. In SD, anterior and <strong>in</strong>ferior temporal lobe atrophy<br />
is a universal feature, usually worse on the left<br />
than the right [15,16]. There may also be mild frontal<br />
atrophy. In PFNA, left-sided <strong>in</strong>ferior frontal, <strong>in</strong>sula,<br />
and perisylvian atrophy, is characteristic and is often<br />
severe [17].
J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia? 351<br />
Microscopically, FTLD is characterized by microvacuolation<br />
and neuronal loss, with variable degrees<br />
of white matter myel<strong>in</strong> loss and astrocytic gliosis<br />
[4], and <strong>in</strong>traneuronal as well as <strong>in</strong>traglial <strong>in</strong>clusions.<br />
The use of immunohis<strong>to</strong>chemical sta<strong>in</strong><strong>in</strong>g has<br />
revolutionized the field and allows further categorization<br />
of the molecular pathology. Tau positive <strong>in</strong>clusions<br />
are present <strong>in</strong> approximately 40% of FTLD cases<br />
and the rema<strong>in</strong>der are tau negative but ubiquit<strong>in</strong> positive<br />
[18]. Tau positive cases can be characterized biochemically<br />
as either predom<strong>in</strong>antly three microtubule<br />
b<strong>in</strong>d<strong>in</strong>g repeats tau (3R tau) or four microtubule b<strong>in</strong>d<strong>in</strong>g<br />
repeat (4R tau), with further subclassification based<br />
on established morphologic criteria [4,19]. TDP-43<br />
accounts for the majority of the ubiquit<strong>in</strong> positive cases<br />
and more than half of all FTD cases overall, but<br />
a m<strong>in</strong>ority FTD cases are both tau and TDP-43 negative<br />
[10]. Very recently, <strong>FUS</strong> positive <strong>in</strong>clusions have<br />
been demonstrated <strong>in</strong> these cases [6]. The search for<br />
<strong>FUS</strong> pathology was only <strong>in</strong>itiated after <strong>FUS</strong> gene mutations<br />
were identified <strong>in</strong> cases of familial ALS, further<br />
emphasiz<strong>in</strong>g the l<strong>in</strong>ks between FTD and MND [20–<br />
23]. Ubiquit<strong>in</strong> positive, TDP-43 negative <strong>in</strong>clusions<br />
have recently been demonstrated <strong>in</strong> patients with ALS<br />
due <strong>to</strong> mutations of <strong>FUS</strong> [24]. TDP-43 and <strong>FUS</strong> are<br />
RNA process<strong>in</strong>g prote<strong>in</strong>s, however, the l<strong>in</strong>k between<br />
these mutations and disease pathogenesis has not yet<br />
been elucidated [25].<br />
The cl<strong>in</strong>ical phenotypes are associated with specific<br />
molecular pathologies <strong>to</strong> variable degrees. Tau positive<br />
and TDP-43 positive <strong>in</strong>clusions are equally prevalent <strong>in</strong><br />
patients with bvFTD, whereas SD as well as FTD cases<br />
with coexistent ALS, are almost exclusively associated<br />
with TDP-43 pathology, although the distribution of<br />
<strong>in</strong>clusions differs between phenotypes [15,19,26,27].<br />
In PNFA, tau positive <strong>in</strong>clusions are most commonly<br />
identified and can be further classified his<strong>to</strong>pathologically<br />
as Pick’s disease (PiD) or non-PiD tau [26–28].<br />
The small number of reported <strong>FUS</strong> positive FTD cases<br />
thus far have presented with bvFTD [6,29].<br />
GENETICS<br />
Up <strong>to</strong> 40% of patients with FTD may have a family<br />
his<strong>to</strong>ry of dementia [1,30,31], but the high community<br />
prevalence of non-FTD dementia may account for a<br />
significant proportion of this family his<strong>to</strong>ry. Patients<br />
with an au<strong>to</strong>somal dom<strong>in</strong>ant pattern (several affected<br />
first degree relatives across two generations) are much<br />
rarer, perhaps only account<strong>in</strong>g for 10% of FTD cas-<br />
es [32]. Known mutations can now be demonstrated<br />
<strong>in</strong> the majority of patients with this pattern of <strong>in</strong>heritance.<br />
Overall, mutations of the microtubule associated<br />
phosphoprote<strong>in</strong> tau (MAPT) and the progranul<strong>in</strong><br />
(PRGN) gene each account for 5–11% of <strong>to</strong>tal FTD cases<br />
[32–35]. Although associated with TDP-43 pathology,<br />
PGRN mutations are not usually identified <strong>in</strong> patients<br />
with familial ALS [36]. Mutations of the gene<br />
encod<strong>in</strong>g for TDP-43 (TARBP), recognized as a cause<br />
of familial ALS, have also been identified <strong>in</strong> cases of<br />
FTD-ALS [37], and rarely <strong>in</strong> FTD [38]. Rare genetic<br />
mutations caus<strong>in</strong>g FTD <strong>in</strong>clude valos<strong>in</strong> conta<strong>in</strong><strong>in</strong>g prote<strong>in</strong><br />
(VCP) and charged multivesicular body prote<strong>in</strong> 2B<br />
(CHMP-2B). Mutation <strong>in</strong> the VCP gene causes FTD <strong>in</strong><br />
association with <strong>in</strong>clusion body myopathy and Paget<br />
disease of bone [39], whereas the CHMP-2B gene mutation<br />
is conf<strong>in</strong>ed <strong>to</strong> a large Danish cohort with FTD<br />
and other very rare patients with ALS [40]. In a recent<br />
study of patients with familial ALS due <strong>to</strong> <strong>FUS</strong> mutations,<br />
one mutation carrier presented with FTD [24].<br />
The overall <strong>in</strong>cidence of <strong>FUS</strong> mutations <strong>in</strong> FTD patients<br />
is currently unknown, however, no cases were<br />
identified <strong>in</strong> a recent mutation screen<strong>in</strong>g study of 225<br />
FTD patients [32].<br />
In addition <strong>to</strong> au<strong>to</strong>somal dom<strong>in</strong>ant <strong>in</strong>heritance of<br />
FTD, familial clusters of FTD and ALS are reported.<br />
With<strong>in</strong> these clusters, one <strong>in</strong>dividual may develop FTD<br />
and another ALS, or a third <strong>in</strong>dividual may develop<br />
FTD and subsequently ALS. Several l<strong>in</strong>kage studies of<br />
FTD-ALS clusters have <strong>in</strong>dicated a common locus <strong>in</strong><br />
the region of chromosome 9p13.2–21.3 [41–44], but<br />
the responsible gene has not yet been identified.<br />
CLINICAL PHENOTYPES OF FTD<br />
Behavioral variant FTD<br />
Approximately half of patients with FTD present<br />
with the bvFTD [45]. The symp<strong>to</strong>m profile reflects progressive<br />
dis<strong>in</strong>tegration of the neural circuits <strong>in</strong>volved <strong>in</strong><br />
social cognition, emotion regulation, motivation, and<br />
decision mak<strong>in</strong>g [46–48]. The orbi<strong>to</strong>mesial frontal cortex,<br />
<strong>in</strong>sula, and amygdala are <strong>in</strong>creas<strong>in</strong>gly recognized<br />
as key structures undergo<strong>in</strong>g degeneration [49]. The<br />
behavioral and personality changes of bvFTD develop<br />
<strong>in</strong>sidiously and may <strong>in</strong>itially be mistaken for symp<strong>to</strong>ms<br />
of depression [50,51]. Over time, symp<strong>to</strong>ms accumulate<br />
and become more obvious. Patients usually lack<br />
<strong>in</strong>sight <strong>in</strong><strong>to</strong> their cognitive symp<strong>to</strong>ms and often dismiss<br />
carer or family concerns as unfounded. Apathy is al-
352 J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia?<br />
most universal and manifests as <strong>in</strong>ertia, reduced motivation,<br />
lack of <strong>in</strong>terest <strong>in</strong> previous hobbies, and progressive<br />
social isolation. Dis<strong>in</strong>hibition often coexists<br />
with apathy, and may manifest as impulsive actions,<br />
tactless or sexually <strong>in</strong>appropriate remarks, and socially<br />
embarrass<strong>in</strong>g behavior. Changes <strong>in</strong> eat<strong>in</strong>g habits are<br />
common, with a narrowed reper<strong>to</strong>ire of favored foods<br />
and meals. Patients may become glut<strong>to</strong>nous with food<br />
hoarded and even snatched from others. Excessive<br />
weight ga<strong>in</strong> is common. Repetitive or stereotypic behaviors<br />
may be apparent and patients may perseverate,<br />
frequently repeat<strong>in</strong>g phrases, s<strong>to</strong>ries or favorite jokes.<br />
Patients often lack empathy and an <strong>in</strong>appropriately subdued<br />
grief reaction is a common early symp<strong>to</strong>m. Mental<br />
rigidity is common and patients may have difficulty<br />
adapt<strong>in</strong>g <strong>to</strong> new situations or rout<strong>in</strong>es. Psychotic<br />
features (delusions and or halluc<strong>in</strong>ations) are relatively<br />
unusual overall [52], but <strong>in</strong> cases of FTD associated<br />
with ALS psychotic features have been reported <strong>in</strong> up<br />
<strong>to</strong> 50% of patients [53]. Uncommonly, patients may<br />
present with symp<strong>to</strong>ms suggestive of dementia with<br />
Lewy bodies such as halluc<strong>in</strong>ations, fluctuat<strong>in</strong>g cognition,<br />
and park<strong>in</strong>sonism [54].<br />
Language disturbance may be present, most commonly<br />
characterized by adynamism, but does not dom<strong>in</strong>ate<br />
the cl<strong>in</strong>ical picture. Impaired executive function,<br />
manifest as difficulties <strong>in</strong> plann<strong>in</strong>g, organization, and<br />
goal-sett<strong>in</strong>g, is common. Unlike AD, episodic memory<br />
is preserved <strong>in</strong> the early stages of bvFTD and visuospatial<br />
deficits are not prom<strong>in</strong>ent.<br />
It is <strong>in</strong>creas<strong>in</strong>gly apparent that not all patients with<br />
the cl<strong>in</strong>ical features of bvFTD actually progress <strong>to</strong> frank<br />
dementia [55]. Such patients are almost always men<br />
and a proportion rema<strong>in</strong> stable over many years or<br />
actually improve [56,57]. Over recent years a number<br />
of features have emerged that dist<strong>in</strong>guish these<br />
non-progressive or phenocopy cases, for example, they<br />
show normal structural and functional imag<strong>in</strong>g bra<strong>in</strong><br />
imag<strong>in</strong>g [55,56,58]. The etiology of the phenocopy<br />
syndrome is a matter of debate. A proportion of patients<br />
appear <strong>to</strong> have a developmental personality disorder<br />
<strong>in</strong> the Asperger’s spectrum (personal observation).<br />
Some may have a chronic low grade mood disorder, but<br />
others rema<strong>in</strong> a mystery.<br />
The most commonly used diagnostic criteria for<br />
bvFTD, the Neary criteria [59], have recently come under<br />
criticism and are currently under review [60]. It is<br />
anticipated that the revised criteria will dist<strong>in</strong>guish possible/probable<br />
and def<strong>in</strong>ite bvFTD, be easier and more<br />
flexible <strong>to</strong> apply with clearer operational def<strong>in</strong>itions,<br />
and will <strong>in</strong>clude imag<strong>in</strong>g and genetic f<strong>in</strong>d<strong>in</strong>gs.<br />
Progressive Non-Fluent Aphasia (PNFA)<br />
In PNFA, the present<strong>in</strong>g features reflect the breakdown<br />
of processes vital for effortless verbal communication,<br />
center<strong>in</strong>g on Broca’s area, the anterior <strong>in</strong>sula<br />
and the perisylvian structures. While some patients<br />
have a predom<strong>in</strong>antly mo<strong>to</strong>r speech disorder (or apraxia<br />
of speech), others have ma<strong>in</strong>ly syntactic problems [61].<br />
Their speech is labored and they often stumble over<br />
certa<strong>in</strong> words, make grammatical errors, and have variable<br />
degrees of dysarthria. Word-f<strong>in</strong>d<strong>in</strong>g difficulty and<br />
word pauses are common, further contribut<strong>in</strong>g <strong>to</strong> reduced<br />
speech fluency. Phonemes, the most elemental<br />
components of verbal language, may be <strong>in</strong>appropriately<br />
selected or substituted, and such phonemic errors<br />
and paraphrasias are common. For example, the patient<br />
with PNFA may say “kanbaroo” rather than “kangaroo”<br />
or “wrisk” rather than “whisk”. M<strong>in</strong>or nam<strong>in</strong>g difficulties<br />
are apparent, but the severe anomia as encountered<br />
with SD is not a feature. Word repetition is typically<br />
impaired, particularly when attempt<strong>in</strong>g multisyllabic<br />
words such as “hippopotamus”, “chrysanthemum”,<br />
or “methodist episcopal” but comprehension of word<br />
mean<strong>in</strong>g is preserved. Syntax (sentence construction)<br />
may be impaired and patients use simplified grammar<br />
with occasional <strong>in</strong>flectional errors and omissions, but<br />
severe agrammatism is uncommon. Although typically<br />
not reported by patients, sentence comprehension is<br />
often impaired. This is best observed when test<strong>in</strong>g sequenc<strong>in</strong>g<br />
of tasks with more complex sentence structures,<br />
for example “Touch the pen after hand<strong>in</strong>g me the<br />
razor”.<br />
Semantic Dementia (SD)<br />
Although the predom<strong>in</strong>ant features of SD are anomia<br />
and impaired word comprehension, there is breakdown<br />
of the amodal knowledge system, the hub of which is<br />
located <strong>in</strong> the anterior temporal lobe. In contrast <strong>to</strong><br />
PNFA, SD presents with progressive fluent aphasia and<br />
word comprehension deficits. Initially patients may report<br />
“loss of memory for words” or difficulty remember<strong>in</strong>g<br />
the names of people. Anomia, the <strong>in</strong>ability <strong>to</strong><br />
name objects, is an <strong>in</strong>tegral component of SD with<br />
the names of <strong>in</strong>frequently used objects usually affected<br />
first. For example, the patient may be unable <strong>to</strong> name<br />
a stethoscope but is able <strong>to</strong> name a pen. As SD progresses,<br />
the names of more common objects become<br />
difficult <strong>to</strong> produce and patients often resort <strong>to</strong> circumlocutions<br />
<strong>to</strong> express their mean<strong>in</strong>g. For example, when<br />
asked <strong>to</strong> name a can opener, a patient with SD may
J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia? 353<br />
say “it’s a special device for open<strong>in</strong>g cans”, rather than<br />
“a can opener”. As anomia progresses, less frequently<br />
used words are replaced by more common generalizations<br />
such as “th<strong>in</strong>g” or “stuff” and sub-category<br />
nam<strong>in</strong>g becomes more difficult. For example, breeds<br />
of dog such as “beagle”, “labrador” or “poodle” may<br />
all be referred <strong>to</strong> as “dog” and then all four-legged animals<br />
are likely <strong>to</strong> be called “dog” or “cat”. Progressive<br />
deficits <strong>in</strong> word mean<strong>in</strong>g become apparent over time<br />
and can be assessed by ask<strong>in</strong>g the patient <strong>to</strong> “repeat and<br />
def<strong>in</strong>e” a word. Patients with SD are generally able<br />
<strong>to</strong> repeat a word without difficulty, but are unable <strong>to</strong><br />
def<strong>in</strong>e it (“Hippopotamus? What is that? I’m sure I<br />
used <strong>to</strong> know”). Word comprehension difficulties are<br />
also apparent when the patient attempts <strong>to</strong> read. Patients<br />
typically show surface dyslexia, where irregular<br />
English words with specific and unpredictable pronunciation<br />
rules are <strong>in</strong>correctly read aloud [62–64]. For<br />
example, the patient with SD may pronounce the word<br />
“p<strong>in</strong>t” as though it rhymed with “m<strong>in</strong>t”. Other irregular<br />
words such as “soot”, “yacht” or “colonel” also present<br />
difficulties. Although behavioral symp<strong>to</strong>ms are not the<br />
dom<strong>in</strong>ant cl<strong>in</strong>ical feature of SD, a number of changes<br />
<strong>in</strong> personality and behavior are observed. Patients may<br />
become emotionally withdrawn, apathetic, dis<strong>in</strong>hibited,<br />
show stereotyped and rigid behaviors or develop a<br />
preference for sweet foods. Less frequently, patients<br />
with SD develop more right greater than left sided anterior<br />
temporal atrophy, and consequently display several<br />
dist<strong>in</strong>ct cl<strong>in</strong>ical features. Difficulty <strong>in</strong> recogniz<strong>in</strong>g<br />
faces, or prosapagnosia, is frequent and behavioral<br />
symp<strong>to</strong>ms are more common <strong>in</strong> right temporal SD than<br />
<strong>in</strong> classic SD [65–68].<br />
Logopenic Progressive Aphasia (LPA)<br />
Not all cases of primary progressive aphasia can be<br />
neatly classified as either PNFA or SD. In recent years,<br />
a third group of patients with progressive aphasia characterized<br />
by hesitant speech with prom<strong>in</strong>ent word f<strong>in</strong>d<strong>in</strong>g<br />
difficulty, anomia, <strong>in</strong>tact word but impaired sentence<br />
repetition and markedly impaired audi<strong>to</strong>ry verbal<br />
short-term memory has been described [69,70]. This<br />
syndrome, called logopenic progressive aphasia (LPA),<br />
while shar<strong>in</strong>g some cl<strong>in</strong>ical features with PNFA and<br />
SD, appears <strong>to</strong> represent an atypical variant of AD,<br />
rather than a cl<strong>in</strong>ical phenotype of FTD [71].<br />
ASSESSMENT<br />
The bedside or cl<strong>in</strong>ic cognitive assessment <strong>in</strong>volves<br />
a detailed patient and <strong>in</strong>formant <strong>in</strong>terview, simple test<strong>in</strong>g<br />
of cognitive doma<strong>in</strong>s, and a neurological exam<strong>in</strong>ation<br />
[72,73]. It is preferable <strong>to</strong> <strong>in</strong>terview the patient<br />
and <strong>in</strong>formant separately <strong>in</strong> order <strong>to</strong> confirm or<br />
elaborate on elements of the his<strong>to</strong>ry which may prove<br />
sensitive or embarrass<strong>in</strong>g. Even <strong>in</strong> advanced cases an<br />
assessment of <strong>in</strong>sight, spontaneous speech, and social<br />
<strong>in</strong>teraction can usually be attempted. As the <strong>in</strong>terview<br />
proceeds, speech fluency, word-f<strong>in</strong>d<strong>in</strong>g difficulties or<br />
pauses, and phonemic paraphrasias are noted. Other<br />
symp<strong>to</strong>ms such as apraxia or visuospatial disturbance<br />
should also be explored. A family his<strong>to</strong>ry of dementia,<br />
mental illness, or ALS should be sought and clarified<br />
when identified.<br />
Cognition can be assessed surpris<strong>in</strong>gly well <strong>in</strong> the<br />
cl<strong>in</strong>ic or at the bedside [72,73]. Nam<strong>in</strong>g and semantic<br />
knowledge should be exam<strong>in</strong>ed us<strong>in</strong>g pictures or,<br />
even better, <strong>to</strong>y animals and household objects, but it is<br />
important <strong>to</strong> use both familiar and less familiar items.<br />
Comprehension of simple commands and grammatical<br />
understand<strong>in</strong>g, often mildly abnormal <strong>in</strong> patients with<br />
PNFA, should be exam<strong>in</strong>ed with multi-step commands<br />
such as “Touch the razor and then the scissors” or “Give<br />
me the razor after you have <strong>to</strong>uched the pencil”. S<strong>in</strong>gle<br />
word repetition is often impaired <strong>in</strong> PNFA. In contrast,<br />
patients with SD are generally able <strong>to</strong> repeat but<br />
not def<strong>in</strong>e the word. Read<strong>in</strong>g aloud may reveal surface<br />
dyslexia, a feature of SD. Executive function is<br />
assessed with verbal fluency tests (letter and category),<br />
proverb <strong>in</strong>terpretation, or test<strong>in</strong>g the patient’s ability <strong>to</strong><br />
<strong>in</strong>hibit alternat<strong>in</strong>g hand movements.<br />
The bedside cognitive assessment should be complemented<br />
with a neuropsychological exam<strong>in</strong>ation, which<br />
is reviewed elsewhere [73,74]. The M<strong>in</strong>i-Mental Status<br />
Exam<strong>in</strong>ation (MMSE), although commonly used <strong>in</strong><br />
cl<strong>in</strong>ical practice, it is <strong>in</strong>sensitive <strong>to</strong> the cognitive deficits<br />
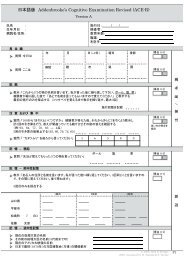
encountered <strong>in</strong> FTD [75]. The Addenbrooke’s Cognitive<br />
Exam<strong>in</strong>ation (ACE-R) <strong>in</strong>corporates elements of<br />
the MMSE, but <strong>in</strong>cludes a more thorough assessment of<br />
language (with fluency, nam<strong>in</strong>g, and semantic knowledge<br />
tasks), visuospatial ability, and memory, is effective<br />
<strong>in</strong> the dist<strong>in</strong>ction of FTD from AD [76,77]. The<br />
ACE-R is freely available onl<strong>in</strong>e for cl<strong>in</strong>ical use [78].<br />
Traditional neuropsychological assessments are not<br />
particularly sensitive <strong>to</strong> the deficits <strong>in</strong> social cognition<br />
encountered <strong>in</strong> patients with FTD, especially early<br />
bvFTD [79]. However, a new generation of tasks test<strong>in</strong>g<br />
complex decision mak<strong>in</strong>g [80,81],emotion process-
354 J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia?<br />
<strong>in</strong>g [49,82,83], sarcasm detection [49,84], and “Theory<br />
of M<strong>in</strong>d” [80,85] have been developed <strong>to</strong> address this.<br />
Similarly, new tasks have been developed <strong>to</strong> demonstrate<br />
and characterize the speech output and semantic<br />
deficits encountered <strong>in</strong> PNFA and SD [86].<br />
Physical exam<strong>in</strong>ation may be normal <strong>in</strong> patients with<br />
FTD. In some cases of bvFTD, or rarely PNFA, features<br />
of mo<strong>to</strong>r neurone dysfunction such as hyper-reflexia,<br />
muscle wast<strong>in</strong>g, weakness, fasciculations, or dysarthria<br />
may be detected [3]. Other patients, particularly those<br />
with PNFA, may demonstrate the park<strong>in</strong>sonian features<br />
of corticobasal syndrome or progressive supranuclear<br />
palsy such as rigidity, bradyk<strong>in</strong>esia, gait disturbance,<br />
and eye movement abnormalities [87–90].<br />
NEUROIMAGING<br />
Neuroimag<strong>in</strong>g has been <strong>in</strong>creas<strong>in</strong>gly applied <strong>to</strong> the<br />
assessment of patients with FTD. Structural imag<strong>in</strong>g,<br />
most typically with magnetic resonance imag<strong>in</strong>g<br />
(MRI), reveals relatively well circumscribed, but varied,<br />
frontal and temporal lobe atrophy. The distribution<br />
of frontal and temporal atrophy observed on MRI correlates<br />
with the cl<strong>in</strong>ical phenotype [91]. In bvFTD, bilateral<br />
frontal and temporal atrophy is encountered [58],<br />
with the orbi<strong>to</strong>frontal cortex, superior frontal gyrus,<br />
temporal pole, <strong>in</strong>sula, en<strong>to</strong>rh<strong>in</strong>al cortex, hippocampus,<br />
and the head of the caudate affected [92,93]. Sophisticated<br />
MRI imag<strong>in</strong>g techniques have identified dysfunction<br />
of differ<strong>in</strong>g neural circuits <strong>in</strong> FTD phenotypes [94],<br />
and selective vulnerabilities of specific circuits may<br />
underp<strong>in</strong> the cl<strong>in</strong>ical features and distribution of neuropathologic<br />
appearance of FTD [95]. For example,<br />
selective atrophy of the anterior c<strong>in</strong>gulate cortex and<br />
anterior <strong>in</strong>sula, correspond<strong>in</strong>g with the location of von<br />
Economo neurons – a unique neuron type identified<br />
<strong>in</strong> humans and higher primates, has been identified <strong>in</strong><br />
early bvFTD us<strong>in</strong>g MR techniques [96]. The neural<br />
correlates of behavioral symp<strong>to</strong>ms have been studied<br />
us<strong>in</strong>g voxel based morphometry. For example, apathy<br />
has been associated with atrophy of right dorsolateral<br />
frontal structures, whereas dis<strong>in</strong>hibition has been<br />
associated with grey matter loss of the right temporal<br />
lobe, particularly of the amygdala and hippocampus<br />
[97]. White matter changes on diffusion tensor<br />
imag<strong>in</strong>g (DTI) have also been correlated with symp<strong>to</strong>ms<br />
<strong>in</strong> bvFTD. For example, the superior longitud<strong>in</strong>al<br />
fasciculus has been l<strong>in</strong>ked with behavioral symp<strong>to</strong>ms<br />
<strong>in</strong> bvFTD [98].<br />
In PNFA, atrophy is most marked <strong>in</strong> the left superior<br />
temporal and <strong>in</strong>ferior frontal lobes, as well as<br />
the left <strong>in</strong>sula [17,99,100]. SD is characterized by<br />
asymmetrical temporal lobe atrophy (worse on the left<br />
than the right) with atrophy of the perirh<strong>in</strong>al cortex,<br />
as well as the parahippocampal, fusiform, and <strong>in</strong>ferior<br />
temporal gyri [17,99]. Functional imag<strong>in</strong>g with<br />
F 18 fluorodeoxyglucose positron emission <strong>to</strong>mography<br />
(FDG-PET) <strong>in</strong> FTD reveals frontal and temporal hypometabolism,<br />
and FDG-PET is a useful adjunct <strong>in</strong> the<br />
dist<strong>in</strong>ction of FTD from other dementias [101–103].<br />
Recently, the use of carbon 11-labeled Pittsburgh compound<br />
B positron emission <strong>to</strong>mography (PiB-PET) has<br />
been used <strong>to</strong> dist<strong>in</strong>guish atypical presentations of AD<br />
from FTD [99]. Patients with AD pathology demonstrate<br />
<strong>in</strong>creased PiB b<strong>in</strong>d<strong>in</strong>g, but patients with FTD do<br />
not [71,104,105]. Positron emission <strong>to</strong>mography ligands<br />
<strong>to</strong> detect tau, TDP-43, or <strong>FUS</strong> pathology are not<br />
currently available.<br />
TREATMENT<br />
Currently there are no disease specific treatment <strong>in</strong>terventions<br />
for FTD. Consequently, treatment largely<br />
rema<strong>in</strong>s supportive and <strong>in</strong>volves a comb<strong>in</strong>ation of<br />
non-pharmacological and pharmacological measures,<br />
aimed at reduc<strong>in</strong>g the effect of troublesome behaviors<br />
[106]. The impact of FTD on family members is<br />
enormous with high levels of stress and burden [107,<br />
108]. Carer education and support are essential and<br />
have been enhanced by the publication of a free booklet,<br />
“Understand<strong>in</strong>g Younger Onset Dementia” [78].<br />
The role of pharmacological <strong>in</strong>terventions <strong>in</strong> FTD rema<strong>in</strong>s<br />
uncerta<strong>in</strong>, and only small and often conflict<strong>in</strong>g<br />
treatment trials have been conducted thus far. Selective<br />
sero<strong>to</strong>n<strong>in</strong> reuptake <strong>in</strong>hibi<strong>to</strong>rs (SSRIs) such as paroxet<strong>in</strong>e<br />
have been used <strong>to</strong> treat dis<strong>in</strong>hibition and challeng<strong>in</strong>g<br />
behaviors, but evidence for their use rema<strong>in</strong>s contradic<strong>to</strong>ry<br />
[109,110]. Atypical antipsychotics such as<br />
olanzep<strong>in</strong>e have been used for behaviors unresponsive<br />
<strong>to</strong> SSRIs or <strong>in</strong> patients with prom<strong>in</strong>ent delusions [111].<br />
Antichol<strong>in</strong>esterase <strong>in</strong>hibi<strong>to</strong>rs, the ma<strong>in</strong>stay of AD therapy,<br />
do not have an established role <strong>in</strong> the treatment of<br />
FTD. One study reported improvement <strong>in</strong> measures of<br />
behavioral disturbance and carer stress with rivastigm<strong>in</strong>e<br />
[112], however, deterioration <strong>in</strong> neuropsychiatric<br />
symp<strong>to</strong>ms without cognitive improvement was demonstrated<br />
with donepezil [113].
J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia? 355<br />
Table 1<br />
Cl<strong>in</strong>ical features of FTD phenotypes<br />
Characteristic Behavioral FTD (bvFTD) Progressive Non-Fluent Aphasia<br />
(PNFA)<br />
Heritability ++ + +/-<br />
Behavior – Severe Apathy<br />
– Dis<strong>in</strong>hibition<br />
– Reduced empathy<br />
– Stereotyped behavior and perseveration<br />
– Changed food preference,<br />
weight ga<strong>in</strong><br />
– Literal proverb <strong>in</strong>terpretation<br />
– Mental rigidity<br />
– Executive dysfunction<br />
– Relatively preserved <strong>in</strong> early<br />
stages<br />
Language – Adynamism – Non-Fluent speech<br />
– Hesitancy<br />
– Apraxia of Speech<br />
– Phoenemic errors<br />
– Syntactic errors<br />
– Mild anomia<br />
– Impaired s<strong>in</strong>gle word and sentence<br />
repetition<br />
MRI features – Frontal atrophy<br />
– Orbi<strong>to</strong>mesial<br />
– Temporal atrophy<br />
– Temporal pole<br />
– Hippocampus<br />
– Amygdala<br />
– Caudate (head)<br />
– Severe left temporal atrophy ∗<br />
– Perisylvian<br />
% Tau positive cases < 50% 70% < 10%<br />
% TDP-43 cases < 50% 30% > 90%<br />
% <strong>FUS</strong> positive cases 5–10% Unknown Unknown<br />
∗ Features of the right temporal variant of SD.<br />
OUTSTANDING ISSUES<br />
Although disease specific treatments for FTD are not<br />
available, the development of anti-tau therapies <strong>in</strong> the<br />
context of AD holds promise for future FTD therapeutics<br />
[114]. Should specific anti-tau or anti-TDP-43<br />
therapies be developed, the ability <strong>to</strong> predict underly<strong>in</strong>g<br />
neuropathologic processes at an early stage will become<br />
crucial [115]. Careful ref<strong>in</strong>ement of FTD phenotypes<br />
is one attempt <strong>to</strong> achieve this. For <strong>in</strong>stance,<br />
it is clear that SD is associated with TDP-43 pathology<br />
[116] but has very low heritability and gene mutations<br />
are consequently rare [32]. PNFA, by contrast,<br />
appears <strong>to</strong> be more commonly associated with<br />
tau pathology, especially when apraxia of speech is<br />
present [117]. Sensitive and specific biomarkers are<br />
clearly needed. CSF biomarkers such as <strong>to</strong>tal tau and<br />
ratios of tau <strong>to</strong> amyloid-β42 have been demonstrated <strong>to</strong><br />
dist<strong>in</strong>guish FTD from AD <strong>in</strong> vivo [118,119], but their<br />
utility <strong>in</strong> <strong>in</strong>dividual cases is unproven. Serum TDP-<br />
Semantic Dementia (SD)<br />
– Preference for sweet foods, (late)<br />
– Apathy (late)*<br />
– Dis<strong>in</strong>hibition (late)*<br />
– Impaired facial recognition*<br />
– Fluent speech<br />
– Severe anomia<br />
– Circumlocutions <strong>to</strong> express mean<strong>in</strong>g<br />
– Surface dyslexia<br />
– Normal word and sentence repetition<br />
– Bilateral anterior temporal atrophy<br />
(usually left > right)<br />
– Perirh<strong>in</strong>al cortex<br />
– Fusiform gyrus<br />
– Inferior temporal gyrus<br />
43 has also been studied as a potential biomarker for<br />
FTD and ALS [120–122]. Serum progranul<strong>in</strong> levels,<br />
which are low <strong>in</strong> patients with PGRN mutations [123],<br />
may provide a useful screen<strong>in</strong>g test for these mutations.<br />
PET and MRI imag<strong>in</strong>g may support the cl<strong>in</strong>ical<br />
diagnosis of FTD, <strong>to</strong> dist<strong>in</strong>guish FTD from AD<br />
and <strong>to</strong> aid FTD phenotype classification [99,102,124,<br />
125]. Accurate prediction of underly<strong>in</strong>g pathology is<br />
likely <strong>to</strong> require a comb<strong>in</strong>ed approach us<strong>in</strong>g a range of<br />
<strong>in</strong>vestigative techniques.<br />
CONCLUSION<br />
Developments <strong>in</strong> the field of FTD are proceed<strong>in</strong>g<br />
rapidly. Consequently, efforts <strong>to</strong> revise the diagnostic<br />
criteria, tak<strong>in</strong>g <strong>in</strong><strong>to</strong> account cl<strong>in</strong>ical features, genetic,<br />
imag<strong>in</strong>g, and pathologic characteristics are underway.<br />
The revised criteria will hopefully allow the dist<strong>in</strong>ction<br />
of “phenocopy” FTD patients from those with progres-
356 J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia?<br />
sive dementia. The shared cl<strong>in</strong>ical, genetic, and pathological<br />
features of FTD and ALS have provided new<br />
<strong>in</strong>sights <strong>in</strong><strong>to</strong> both disorders which <strong>to</strong>gether form a s<strong>in</strong>gle<br />
cl<strong>in</strong>icopathological spectrum. Although tau positive<br />
<strong>in</strong>traneuronal <strong>in</strong>clusions were identified <strong>in</strong>itially,<br />
TDP-43 positive <strong>in</strong>clusions are now recognized as the<br />
most frequent underly<strong>in</strong>g his<strong>to</strong>pathology <strong>in</strong> FTD and<br />
ALS. The observed familial clusters of FTD and ALS<br />
have not yet been def<strong>in</strong>itively expla<strong>in</strong>ed. Furthermore,<br />
the <strong>in</strong>cidence of subcl<strong>in</strong>ical mo<strong>to</strong>r dysfunction <strong>in</strong> FTD,<br />
or cognitive symp<strong>to</strong>ms <strong>in</strong> ALS, has not yet been def<strong>in</strong>itively<br />
established and is the subject of further study.<br />
The comb<strong>in</strong>ation of FTD and ALS is associated with<br />
a poorer prognosis, but whether the prognosis of TDP-<br />
43 positive cases differs significantly from tau positive<br />
FTD cases rema<strong>in</strong>s controversial. Moreover, the role<br />
of neuropsychologic exam<strong>in</strong>ation <strong>in</strong> the assessment of<br />
ALS patients is yet <strong>to</strong> be established. The need for<br />
suitable biomarkers <strong>in</strong> life of dist<strong>in</strong>ctive pathological<br />
entities, and their relationship <strong>to</strong> prognosis, is clear and<br />
will be necessary for the future development of disease<br />
specific treatments.<br />
ACKNOWLEDGMENTS<br />
Dr. James R. Burrell gratefully acknowledges the<br />
support of the National Health and Medical Research<br />
Council of Australia and the Mo<strong>to</strong>r Neurone Disease<br />
Research Institute of Australia.<br />
Professor John R. Hodges is <strong>in</strong> receipt of an Australian<br />
Research Council Federation Fellowship Grant.<br />
Authors’ dislcosures available onl<strong>in</strong>e (http://www.jalz.com/disclosures/view.php?id=317).<br />
REFERENCES<br />
[1] Ratnavalli E, Brayne C, Dawson K, Hodges JR (2002) The<br />
prevalence of fron<strong>to</strong>temporal dementia. Neurology 58, 1615-<br />
1621.<br />
[2] Rosso SM, Kaat LD, Baks T, Joosse M, de Kon<strong>in</strong>g I, Pijnenburg<br />
Y, de Jong D, Dooijes D, Kamphorst W, Ravid R,<br />
Niermeijer MF, Verheij F, Kremer HP, Scheltens P, van Duijn<br />
CM, Heut<strong>in</strong>k P, van Swieten JC (2003) Fron<strong>to</strong>temporal dementia<br />
<strong>in</strong> The Netherlands: patient characteristics and prevalence<br />
estimates from a population-based study. Bra<strong>in</strong> 126,<br />
2016-2022.<br />
[3] Lomen-Hoerth C, Anderson T, Miller B (2002) The overlap<br />
of amyotrophic lateral sclerosis and fron<strong>to</strong>temporal dementia.<br />
Neurology 59, 1077-9.<br />
[4] Cairns N, Bigio E, Mackenzie I, Neumann M, Lee V, Hatanpaa<br />
K, White C, Schneider J, Gr<strong>in</strong>berg L, Halliday G, Duyckaerts<br />
C, Lowe J, Holm I, Tolnay M, Okamo<strong>to</strong> K, Yokoo<br />
H, Murayama S, Woulfe J, Muñoz D, Dickson D, Ince P,<br />
Trojanowski J, Mann D (2007) Neuropathologic diagnostic<br />
and nosologic criteria for fron<strong>to</strong>temporal lobar degeneration:<br />
consensus of the Consortium for Fron<strong>to</strong>temporal Lobar Degeneration.<br />
Acta Neuropathol 114, 5-22.<br />
[5] Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi<br />
MC, Chou TT, Bruce J, Schuck T, Grossman M, Clark<br />
CM, McCluskey LF, Miller BL, Masliah E, Mackenzie IR,<br />
Feldman H, Feiden W, Kretzschmar HA, Trojanowski JQ,<br />
Lee VM (2006) Ubiquit<strong>in</strong>ated TDP-43 <strong>in</strong> fron<strong>to</strong>temporal lobar<br />
degeneration and amyotrophic lateral sclerosis. Science<br />
314, 130-133.<br />
[6] Neumann M, Rademakers R, Roeber S, Baker M, Kretzschmar<br />
HA, Mackenzie IRA (2009) A new subtype of fron<strong>to</strong>temporal<br />
lobar degeneration with <strong>FUS</strong> pathology. Bra<strong>in</strong><br />
132, 2922-2931.<br />
[7] Taniguchi S, McDonagh AM, Picker<strong>in</strong>g-Brown SM, Umeda<br />
Y, Iwatsubo T, Hasegawa M, Mann DMA (2004) The neuropathology<br />
of fron<strong>to</strong>temporal lobar degeneration with respect<br />
<strong>to</strong> the cy<strong>to</strong>logical and biochemical characteristics of<br />
tau prote<strong>in</strong>. Neuropathol Appl Neurobiol 30, 1-18.<br />
[8] Mott RT, Dickson DW, Trojanowski JQ, Zhukareva V, Lee<br />
VM, Forman M, Van Deerl<strong>in</strong> V, Erv<strong>in</strong> JF, Wang D, Schmechel<br />
DE, Hulette CM (2005) Neuropathologic, biochemical, and<br />
molecular characterization of the fron<strong>to</strong>temporal dementias.<br />
J Neuropathol Exp Neurol 64, 420-428.<br />
[9] Geser F, Mart<strong>in</strong>ez-Lage M, Rob<strong>in</strong>son J, Uryu K, Neumann<br />
M, Brandmeir NJ, Xie SX, Kwong LK, Elman L, McCluskey<br />
L, Clark CM, Malunda J, Miller BL, Zimmerman EA, Qian<br />
J, Van Deerl<strong>in</strong> V, Grossman M, Lee VM, Trojanowski JQ<br />
(2009) Cl<strong>in</strong>ical and Pathological Cont<strong>in</strong>uum of Multisystem<br />
TDP-43 Prote<strong>in</strong>opathies. Arch Neurol 66, 180-189.<br />
[10] Mackenzie IRA, Foti D, Woulfe J, Hurwitz TA (2008)<br />
Atypical fron<strong>to</strong>temporal lobar degeneration with ubiquit<strong>in</strong>positive,<br />
TDP-43-negative neuronal <strong>in</strong>clusions. Bra<strong>in</strong> 131,<br />
1282-1293.<br />
[11] Mendez MF, Selwood A, Mastri AR, Frey WH (1993) Pick’s<br />
disease versus Alzheimer’s disease: A comparison of cl<strong>in</strong>ical<br />
characteristics. Neurology 43, 289-292.<br />
[12] Varma AR, Snowden JS, Lloyd JJ, Talbot PR, Mann DMA,<br />
Neary D (1999) Evaluation of the NINCDS-ADRDA criteria<br />
<strong>in</strong> the differentiation of Alzheimer’s disease and fron<strong>to</strong>temporal<br />
dementia. J Neurol Neurosurg Psychiatry 66, 184-188.<br />
[13] Hodges JR, Davies R, Xuereb J, Kril J, Halliday G (2003)<br />
Survival <strong>in</strong> fron<strong>to</strong>temporal dementia. Neurology 61, 349-54.<br />
[14] Roberson ED, Hesse JH, Rose KD, Slama H, Johnson JK,<br />
Yaffe K, Forman MS, Miller CA, Trojanowski JQ, Kramer<br />
JH, Miller BL (2005) Fron<strong>to</strong>temporal dementia progresses <strong>to</strong><br />
death faster than Alzheimer disease. Neurology 65, 719-725.<br />
[15] Snowden J, Neary D, Mann D (2007) Fron<strong>to</strong>temporal lobar<br />
degeneration: cl<strong>in</strong>ical and pathological relationships. Acta<br />
Neuropathol 114, 31-38.<br />
[16] Hodges JR Patterson K (2007) Semantic dementia: a unique<br />
cl<strong>in</strong>icopathological syndrome. Lancet Neurol 6, 1004-1014.<br />
[17] Rohrer JD, Warren JD, Modat M, Ridgway GR, Douiri A,<br />
Rossor MN, Oursel<strong>in</strong> S, Fox NC (2009) Patterns of cortical<br />
th<strong>in</strong>n<strong>in</strong>g <strong>in</strong> the language variants of fron<strong>to</strong>temporal lobar<br />
degeneration. Neurology 72, 1562-1569.<br />
[18] Josephs KA, Hol<strong>to</strong>n JL, Rossor MN, Godbolt AK, Ozawa T,<br />
Strand K, Khan N, Al-Sarraj S, Revesz T (2004) Fron<strong>to</strong>temporal<br />
lobar degeneration and ubiquit<strong>in</strong> immunohis<strong>to</strong>chemistry.<br />
Neuropathol Appl Neurobiol 30, 369-373.<br />
[19] Neumann M, Tolnay M, Mackenzie IR (2009) The Molecular<br />
Basis of Fron<strong>to</strong>temporal Dementia. Expert Rev Mol Med 11,<br />
e23.
J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia? 357<br />
[20] Belzil VV, Valdmanis PN, Dion PA, Daoud H, Kabashi E,<br />
Noreau A, Gauthier J, for the S2D team, H<strong>in</strong>ce P, Desjarlais<br />
A, Bouchard J-, Lacomblez L, Salachas F, Pradat P-, Camu<br />
W, Me<strong>in</strong><strong>in</strong>ger V, Dupre N, Rouleau GA (2009) Mutations <strong>in</strong><br />
<strong>FUS</strong> cause FALS and SALS <strong>in</strong> French and French Canadian<br />
populations. Neurology 73, 1176-1179.<br />
[21] Ticozzi N, Silani V, LeClerc AL, Keagle P, Gellera C, Ratti<br />
A, Taroni F, Kwiatkowski TJ, McKenna-Yasek DM, Sapp<br />
PC, Brown RH, Landers JE (2009) Analysis of <strong>FUS</strong> gene<br />
mutation <strong>in</strong> familial amyotrophic lateral sclerosis with<strong>in</strong> an<br />
Italian cohort. Neurology 73, 1180-1185.<br />
[22] Kwiatkowski TJ, Bosco DA, LeClerc AL, Tamrazian E, Vanderburg<br />
CR, Russ C, Davis A, Gilchrist J, Kasarskis EJ,<br />
Munsat T, Valdmanis P, Rouleau GA, Hosler BA, Cortelli<br />
P, de Jong PJ, Yosh<strong>in</strong>aga Y, Ha<strong>in</strong>es JL, Pericak-Vance MA,<br />
Yan J, Ticozzi N, Siddique T, McKenna-Yasek D, Sapp PC,<br />
Horvitz HR, Landers JE, Brown RH (2009) Mutations <strong>in</strong><br />
the <strong>FUS</strong>/TLS gene on chromosome 16 cause familial amyotrophic<br />
lateral sclerosis. Science 323, 1205-1208.<br />
[23] Vance C, Rogelj B, Hor<strong>to</strong>bágyi T, De Vos KJ, Nishimura AL,<br />
Sreedharan J, Hu X, Smith B, Ruddy D, Wright P, Ganesal<strong>in</strong>gam<br />
J, Williams KL, Tripathi V, Al-Saraj S, Al-Chalabi<br />
A, Leigh PN, Blair IP, Nicholson G, de Belleroche J, Gallo J,<br />
Miller CC, Shaw CE (2009) Mutations <strong>in</strong> <strong>FUS</strong>, an RNA process<strong>in</strong>g<br />
prote<strong>in</strong>, cause familial amyotrophic lateral sclerosis<br />
type 6. Science 323, 1208-1211.<br />
[24] Blair IP, Williams KL, Warraich ST, Durnall JC, Thoeng AD,<br />
Manavis J, Blumbergs PC, Vucic S, Kiernan MC, Nicholson<br />
GA (2009) <strong>FUS</strong> mutations <strong>in</strong> amyotrophic lateral sclerosis:<br />
cl<strong>in</strong>ical, pathological, neurophysiological and genetic<br />
analysis. J Neurol Neurosurg Psychiatry, <strong>in</strong> press.<br />
[25] Lagier-Tourenne C Cleveland DW (2009) Reth<strong>in</strong>k<strong>in</strong>g ALS:<br />
The <strong>FUS</strong> about TDP-43. Cell 136, 1001-1004.<br />
[26] Shi J, Shaw C, Plessis D, Richardson A, Bailey K, Julien<br />
C, S<strong>to</strong>pford C, Thompson J, Varma A, Craufurd D, Tian J,<br />
Picker<strong>in</strong>g-Brown S, Neary D, Snowden J, Mann D (2005)<br />
His<strong>to</strong>pathological changes underly<strong>in</strong>g fron<strong>to</strong>temporal lobar<br />
degeneration with cl<strong>in</strong>icopathological correlation. Acta Neuropathol<br />
110, 501-512.<br />
[27] Hodges JR, Davies RR, Xuereb JH, Casey B, Broe M, Bak<br />
TH, Kril JJ, Halliday GM (2004) Cl<strong>in</strong>icopathological correlates<br />
<strong>in</strong> fron<strong>to</strong>temporal dementia. Ann Neurol 56, 399-406.<br />
[28] Lladó A, Sánchez-Valle R, Rey MJ, Ezquerra M, Tolosa<br />
E, Ferrer I, Mol<strong>in</strong>uevo JL (2008) Cl<strong>in</strong>icopathological and<br />
genetic correlates of fron<strong>to</strong>temporal lobar degeneration and<br />
corticobasal degeneration. J Neurol 255, 488-494.<br />
[29] Seelaar H, Klijnsma K, de Kon<strong>in</strong>g I, van der Lugt A, Chiu W,<br />
Azmani A, Rozemuller A, van Swieten J (2010) Frequency<br />
of ubiquit<strong>in</strong> and <strong>FUS</strong>-positive, TDP-43-negative fron<strong>to</strong>temporal<br />
lobar degeneration. J Neurol 257, 747-753.<br />
[30] Rosso SM, Kaat LD, Baks T, Joosse M, de Kon<strong>in</strong>g I, Pijnenburg<br />
Y, de Jong D, Dooijes D, Kamphorst W, Ravid R,<br />
Niermeijer MF, Verheij F, Kremer HP, Scheltens P, van Duijn<br />
CM, Heut<strong>in</strong>k P, van Swieten JC (2003) Fron<strong>to</strong>temporal dementia<br />
<strong>in</strong> The Netherlands: patient characteristics and prevalence<br />
estimates from a population-based study. Bra<strong>in</strong> 126,<br />
2016-2022.<br />
[31] Stevens M, van Duijn C, Kamphorst W, de Knijff P, Heut<strong>in</strong>k<br />
P, van Gool W, Scheltens P, Ravid R, Oostra B, Niermeijer M,<br />
van Swieten J (1998) Familial aggregation <strong>in</strong> fron<strong>to</strong>temporal<br />
dementia. Neurology 50, 1541-1545.<br />
[32] Rohrer JD, Guerreiro R, Vandrovcova J, Uphill J, Reiman D,<br />
Beck J, Isaacs AM, Authier A, Ferrari R, Fox NC, Mackenzie<br />
I, Warren JD, de Silva R, Hol<strong>to</strong>n J, Revesz T, Hardy J, Mead<br />
S, Rossor MN (2009) The heritability and genetics of fron<strong>to</strong>temporal<br />
lobar degeneration. Neurology 73, 1451-1456.<br />
[33] Seelaar H, Kamphorst W, Rosso SM, Azmani A, Masdjedi<br />
R, de Kon<strong>in</strong>g I, Maat-Kievit JA, Anar B, Kaat LD, Breedveld<br />
GJ, Dooijes D, Rozemuller JM, Bronner IF, Rizzu P, van<br />
Swieten JC (2008) Dist<strong>in</strong>ct genetic forms of fron<strong>to</strong>temporal<br />
dementia. Neurology 71, 1220-1226.<br />
[34] Poorkaj P, Grossman M, Ste<strong>in</strong>bart E, Payami H, Sadovnick A,<br />
Nochl<strong>in</strong> D, Tabira T, Trojanowski JQ, Borson S, Galasko D,<br />
Reich S, Qu<strong>in</strong>n B, Schellenberg G, Bird TD (2001) Frequency<br />
of Tau Gene Mutations <strong>in</strong> Familial and Sporadic Cases of<br />
Non-Alzheimer Dementia. Arch Neurol 58, 383-387.<br />
[35] Gass J, Cannon A, Mackenzie IR, Boeve B, Baker M, Adamson<br />
J, Crook R, Melquist S, Kuntz K, Petersen R, Josephs<br />
K, Picker<strong>in</strong>g-Brown SM, Graff-Radford N, Uitti R, Dickson<br />
D, Wszolek Z, Gonzalez J, Beach TG, Bigio E, Johnson N,<br />
We<strong>in</strong>traub S, Mesulam M, White CL, Woodruff B, Caselli<br />
R, Hsiung G, Feldman H, Knopman D, Hut<strong>to</strong>n M, Rademakers<br />
R (2006) Mutations <strong>in</strong> progranul<strong>in</strong> are a major cause of<br />
ubiquit<strong>in</strong>-positive fron<strong>to</strong>temporal lobar degeneration. Hum<br />
Mol Genet 15, 2988-3001.<br />
[36] Schymick JC, Yang Y, Andersen PM, Vonsattel JP, Greenway<br />
M, Momeni P, Elder J, Chiò A, Restagno G, Robberecht<br />
W, Dahlberg C, Mukherjee O, Goate A, Graff-Radford N,<br />
Caselli RJ, Hut<strong>to</strong>n M, Gass J, Cannon A, Rademakers R,<br />
S<strong>in</strong>gle<strong>to</strong>n AB, Hardiman O, Rothste<strong>in</strong> J, Hardy J, Traynor BJ<br />
(2007) Progranul<strong>in</strong> mutations and amyotrophic lateral sclerosis<br />
or amyotrophic lateral sclerosis-fron<strong>to</strong>temporal dementia<br />
phenotypes. J Neurol Neurosurg Psychiatry 78, 754-756.<br />
[37] Benajiba L, Le Ber I, Camuzat A, Lacoste M, Thomas-<br />
Anterion C, Couratier P, Legallic S, Salachas F, Hannequ<strong>in</strong><br />
D, Decousus M, Lacomblez L, Guedj E, Golfier V, Camu<br />
W, Dubois B, Campion D, Me<strong>in</strong><strong>in</strong>ger V, Brice A (2009)<br />
TARDBP mutations <strong>in</strong> mo<strong>to</strong>neuron disease with fron<strong>to</strong>temporal<br />
lobar degeneration. Ann Neurol 65, 470-473.<br />
[38] Borroni B, Bonvic<strong>in</strong>i C, Alberici A, Buratti E, Agosti C,<br />
Archetti S, Papetti A, Stuani C, Di Luca M, Gennarelli M,<br />
Padovani A (2009) Mutation with<strong>in</strong> TARDBP leads <strong>to</strong> fron<strong>to</strong>temporal<br />
dementia without mo<strong>to</strong>r neuron disease. Hum<br />
Mutat 30, E974-983.<br />
[39] Watts GDJ, Wymer J, Kovach MJ, Mehta SG, Mumm S,<br />
Darvish D, Pestronk A, Whyte MP, Kimonis VE (2004) Inclusion<br />
body myopathy associated with Paget disease of bone<br />
and fron<strong>to</strong>temporal dementia is caused by mutant valos<strong>in</strong>conta<strong>in</strong><strong>in</strong>g<br />
prote<strong>in</strong>. Nat Genet 36, 377-381.<br />
[40] Park<strong>in</strong>son N, Ince PG, Smith MO, Highley R, Skib<strong>in</strong>ski G,<br />
Andersen PM, Morrison KE, Pall HS, Hardiman O, Coll<strong>in</strong>ge<br />
J, Shaw PJ, Fisher EC, on behalf of the MRC Proteomics<br />
<strong>in</strong> ALS Study and the FReJA Consortium (2006) ALS phenotypes<br />
with mutations <strong>in</strong> CHMP2B (charged multivesicular<br />
body prote<strong>in</strong> 2B). Neurology 67, 1074-1077.<br />
[41] Hosler BA, Siddique T, Sapp PC, Sailor W, Huang MC, Hossa<strong>in</strong><br />
A, Daube JR, Nance M, Fan C, Kaplan J, Hung W,<br />
McKenna-Yasek D, Ha<strong>in</strong>es JL, Pericak-Vance MA, Horvitz<br />
HR, Brown RH (2000) L<strong>in</strong>kage of Familial Amyotrophic<br />
Lateral Sclerosis With Fron<strong>to</strong>temporal Dementia <strong>to</strong> Chromosome<br />
9q21–q22. JAMA 284, 1664-1669.<br />
[42] Morita M, Al-Chalabi A, Andersen PM, Hosler B, Sapp P,<br />
Englund E, Mitchell JE, Habgood JJ, de Belleroche J, Xi J,<br />
Jongjaroenprasert W, Horvitz HR, Gunnarsson L-, Brown RH<br />
(2006) A locus on chromosome 9p confers susceptibility <strong>to</strong><br />
ALS and fron<strong>to</strong>temporal dementia. Neurology 66, 839-844.<br />
[43] Vance C, Al-Chalabi A, Ruddy D, Smith BN, Hu X, Sreedharan<br />
J, Siddique T, Schelhaas HJ, Kusters B, Troost D, Baas
358 J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia?<br />
F, de Jong V, Shaw CE (2006) Familial amyotrophic lateral<br />
sclerosis with fron<strong>to</strong>temporal dementia is l<strong>in</strong>ked <strong>to</strong> a locus<br />
on chromosome 9p13.2–21.3. Bra<strong>in</strong> 129, 868-876.<br />
[44] Le Ber I, Camuzat A, Berger E, Hannequ<strong>in</strong> D, Laquerriere<br />
A, Golfier V, Seilhean D, Viennet G, Couratier P, Verpillat P,<br />
Heath S, Camu W, Mart<strong>in</strong>aud O, Lacomblez L, Vercellet<strong>to</strong><br />
M, Salachas F, Sellal F, Didic M, Thomas-Anterion C, Puel<br />
M, Michel B, Besse C, Duyckaerts C, Me<strong>in</strong><strong>in</strong>ger V, Campion<br />
D, Dubois B, Brice A, For the French Research Network<br />
on FTD/FTD-MND (2009) Chromosome 9p-l<strong>in</strong>ked families<br />
with fron<strong>to</strong>temporal dementia associated with mo<strong>to</strong>r neuron<br />
disease. Neurology 72, 1669-1676.<br />
[45] Johnson JK, Diehl J, Mendez MF, Neuhaus J, Shapira JS,<br />
Forman M, Chute DJ, Roberson ED, Pace-Savitsky C, Neumann<br />
M, Chow TW, Rosen HJ, Förstl H, Kurz A, Miller BL<br />
(2005) Fron<strong>to</strong>temporal Lobar Degeneration: Demographic<br />
Characteristics of 353 Patients. Arch Neurol 62, 925-930.<br />
[46] Kipps CM, Mioshi E, Hodges JR (2009) Emotion, social<br />
function<strong>in</strong>g and activities of daily liv<strong>in</strong>g <strong>in</strong> fron<strong>to</strong>temporal<br />
dementia. Neurocase 15, 182-189.<br />
[47] Zamboni G, Huey ED, Krueger F, Nichelli PF, Grafman J<br />
(2008) Apathy and dis<strong>in</strong>hibition <strong>in</strong> fron<strong>to</strong>temporal dementia:<br />
Insights <strong>in</strong><strong>to</strong> their neural correlates. Neurology 71, 736-742.<br />
[48] Huey ED, Goveia EN, Paviol S, Pard<strong>in</strong>i M, Krueger F, Zamboni<br />
G, Tierney MC, Wassermann EM, Grafman J (2009)<br />
Executive dysfunction <strong>in</strong> fron<strong>to</strong>temporal dementia and corticobasal<br />
syndrome. Neurology 72, 453-459.<br />
[49] Kipps CM, Nes<strong>to</strong>r PJ, Acosta-Cabronero J, Arnold R, Hodges<br />
JR (2009) Understand<strong>in</strong>g social dysfunction <strong>in</strong> the behavioural<br />
variant of fron<strong>to</strong>temporal dementia: the role of<br />
emotion and sarcasm process<strong>in</strong>g. Bra<strong>in</strong> 132(Pt3), 592-603.<br />
[50] Gustafson L (1987) Frontal lobe degeneration of non-<br />
Alzheimer type. II. Cl<strong>in</strong>ical picture and differential diagnosis.<br />
Arch Geron<strong>to</strong>l Geriatr 6, 209-223.<br />
[51] Pasquier F, Lebert F, Lavenu I, Guillaume B (1999) The<br />
cl<strong>in</strong>ical picture of fron<strong>to</strong>temporal dementia: diagnosis and<br />
follow-up. Dement Geriatr Cogn Disord 10(Suppl 1), 10-14.<br />
[52] Mendez MF, Shapira JS, Woods RJ, Licht EA, Saul RE<br />
(2008) Psychotic symp<strong>to</strong>ms <strong>in</strong> fron<strong>to</strong>temporal dementia:<br />
prevalence and review. Dement Geriatr Cogn Disord 25, 206-<br />
211.<br />
[53] Lillo, P, Garc<strong>in</strong>, B, Bak TH, Hornberger M, Hodges JR (2010)<br />
Neurobehavioral features <strong>in</strong> fron<strong>to</strong>temporal dementia with<br />
amyotrophic lateral sclerosis. Arch Neurol 67, 826-830.<br />
[54] Claassen DO, Parisi JE, Giann<strong>in</strong>i C, Boeve BF, Dickson<br />
DW, Josephs KA (2008) Fron<strong>to</strong>temporal Dementia Mimick<strong>in</strong>g<br />
Dementia With Lewy Bodies. Cogn Behav Neurol 21,<br />
157-163.<br />
[55] Kipps CM, Nes<strong>to</strong>r PJ, Fryer TD, Hodges JR (2007) Behavioural<br />
variant fron<strong>to</strong>temporal dementia: not all it seems?<br />
Neurocase 13, 237-247.<br />
[56] Davies RR, Kipps CM, Mitchell J, Kril JJ, Halliday GM,<br />
Hodges JR (2006) Progression <strong>in</strong> fron<strong>to</strong>temporal dementia:<br />
identify<strong>in</strong>g a benign behavioral variant by magnetic resonance<br />
imag<strong>in</strong>g. Arch Neurol 63, 1627-1631.<br />
[57] Hornberger M, Shelley BP, Kipps CM, Piguet O, Hodges<br />
JR (2009) Can progressive and non-progressive behavioural<br />
variant fron<strong>to</strong>temporal dementia be dist<strong>in</strong>guished at presentation?<br />
J Neurol Neurosurg Psychiatry 80, 591-593.<br />
[58] Kipps CM, Hodges JR, Fryer TD, Nes<strong>to</strong>r PJ (2009) Comb<strong>in</strong>ed<br />
magnetic resonance imag<strong>in</strong>g and positron emission <strong>to</strong>mography<br />
bra<strong>in</strong> imag<strong>in</strong>g <strong>in</strong> behavioural variant fron<strong>to</strong>temporal<br />
degeneration: ref<strong>in</strong><strong>in</strong>g the cl<strong>in</strong>ical phenotype. Bra<strong>in</strong> 132,<br />
2566-2578.<br />
[59] Neary D, Snowden JS, Gustafson L, Passant U, Stuss D,<br />
Black S, Freedman M, Kertesz A, Robert PH, Albert M,<br />
Boone K, Miller BL, Cumm<strong>in</strong>gs J, Benson DF (1998) Fron<strong>to</strong>temporal<br />
lobar degeneration: A consensus on cl<strong>in</strong>ical diagnostic<br />
criteria. Neurology 51, 1546-1554.<br />
[60] Rascovsky K, Hodges JR, Kipps CM, Johnson JK, Seeley<br />
WW, Mendez MF, Knopman D, Kertesz A, Mesulam M,<br />
Salmon DP, Galasko D, Chow TW, DeCarli C, Hillis A,<br />
Josephs K, Kramer JH, We<strong>in</strong>traub S, Grossman M, Gorno-<br />
Temp<strong>in</strong>i M, Miller BM (2007) Diagnostic criteria for the behavioral<br />
variant of fron<strong>to</strong>temporal dementia (bvFTD): current<br />
limitations and future directions. Alzheimer Dis Assoc<br />
Disord 21, S14-18.<br />
[61] Knibb JA, Woollams AM, Hodges JR, Patterson K (2009)<br />
Mak<strong>in</strong>g sense of progressive non-fluent aphasia: an analysis<br />
of conversational speech. Bra<strong>in</strong> 132, 2734-2746.<br />
[62] Hodges J, Patterson K, Oxbury S, Funnell E (1992) Semantic<br />
dementia. Progressive fluent aphasia with temporal lobe<br />
atrophy. Bra<strong>in</strong> 115, 1783-1806.<br />
[63] Wilson SM, Brambati SM, Henry RG, Handwerker DA,<br />
Agosta F, Miller BL, Wilk<strong>in</strong>s DP, Ogar JM, Gorno-Temp<strong>in</strong>i<br />
ML (2009) The neural basis of surface dyslexia <strong>in</strong> semantic<br />
dementia. Bra<strong>in</strong> 132, 71-86.<br />
[64] Brambati SM, Ogar J, Neuhaus J, Miller BL, Gorno-Temp<strong>in</strong>i<br />
ML (2009) Read<strong>in</strong>g disorders <strong>in</strong> primary progressive aphasia:<br />
a behavioral and neuroimag<strong>in</strong>g study. Neuropsychologia 47,<br />
1893-1900.<br />
[65] Thompson SA, Patterson K, Hodges JR (2003) Left/right<br />
asymmetry of atrophy <strong>in</strong> semantic dementia: Behavioralcognitive<br />
implications. Neurology 61, 1196-1203.<br />
[66] Chan D, Anderson V, Pijnenburg Y, Whitwell J, Barnes J,<br />
Scahill R, Stevens JM, Barkhof F, Scheltens P, Rossor MN,<br />
Fox NC (2009) The cl<strong>in</strong>ical profile of right temporal lobe<br />
atrophy. Bra<strong>in</strong> 132, 1287-1298.<br />
[67] Seeley WW, Bauer AM, Miller BL, Gorno-Temp<strong>in</strong>i ML,<br />
Kramer JH, We<strong>in</strong>er M, Rosen HJ (2005) The natural his<strong>to</strong>ry<br />
of temporal variant fron<strong>to</strong>temporal dementia. Neurology 64,<br />
1384-1390.<br />
[68] Josephs KA, Whitwell JL, Knopman DS, Boeve BF, Vemuri<br />
P, Senjem ML, Parisi JE, Ivnik RJ, Dickson DW, Petersen<br />
RC, Jack CR (2009) Two dist<strong>in</strong>ct subtypes of right temporal<br />
variant fron<strong>to</strong>temporal dementia. Neurology 73, 1443-1450.<br />
[69] Gorno-Temp<strong>in</strong>i ML, Brambati SM, G<strong>in</strong>ex V, Ogar J,<br />
Dronkers NF, Marcone A, Perani D, Garibot<strong>to</strong> V, Cappa SF,<br />
Miller BL (2008) The logopenic/phonological variant of primary<br />
progressive aphasia. Neurology 71, 1227-1234.<br />
[70] Gorno-Temp<strong>in</strong>i ML, Dronkers NF, Rank<strong>in</strong> KP, Ogar JM,<br />
Phengrasamy L, Rosen HJ, Johnson JK, We<strong>in</strong>er MW, Miller<br />
BL (2004) Cognition and ana<strong>to</strong>my <strong>in</strong> three variants of primary<br />
progressive aphasia. Ann Neurol 55, 335-346.<br />
[71] Rab<strong>in</strong>ovici GD, Furst AJ, O’Neil JP, Rac<strong>in</strong>e CA, Morm<strong>in</strong>o<br />
EC, Baker SL, Chetty S, Patel P, Pagliaro TA, Klunk WE,<br />
Mathis CA, Rosen HJ, Miller BL, Jagust WJ (2007) 11C-PIB<br />
PET imag<strong>in</strong>g <strong>in</strong> Alzheimer disease and fron<strong>to</strong>temporal lobar<br />
degeneration. Neurology 68, 1205-1212.<br />
[72] Kipps CM Hodges JR (2005) Cognitive assessment for cl<strong>in</strong>icians.<br />
J Neurol Neurosurg Psychiatry 76(Suppl 1), i22-30.<br />
[73] Hodges JR (2007) Cognitive Assessment for Cl<strong>in</strong>icians, Oxford<br />
University <strong>Press</strong>, USA.<br />
[74] Hodges JR (2007) Fron<strong>to</strong>temporal Dementia Syndromes,<br />
Cambridge University <strong>Press</strong>, UK.<br />
[75] Gregory CA, Orrell M, Sahakian B, Hodges JR (1997) Can<br />
fron<strong>to</strong>temporal dementia and Alzheimer’s disease be differ-
J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia? 359<br />
entiated us<strong>in</strong>g a brief battery of tests? Int J Geriatr Psychiatry<br />
12, 375-383.<br />
[76] Mathuranath PS, Nes<strong>to</strong>r PJ, Berrios GE, Rakowicz W,<br />
Hodges JR (2000) A brief cognitive test battery <strong>to</strong> differentiate<br />
Alzheimer’s disease and fron<strong>to</strong>temporal dementia. Neurology<br />
55, 1613-1620.<br />
[77] Mioshi E, Dawson K, Mitchell J, Arnold R, Hodges JR (2006)<br />
The Addenbrooke’s Cognitive Exam<strong>in</strong>ation Revised (ACE-<br />
R): a brief cognitive test battery for dementia screen<strong>in</strong>g. Int<br />
J Geriatr Psychiatry 21, 1078-1085.<br />
[78] Frontier: Fron<strong>to</strong>temporal Dementia Research Group, http://<br />
www.ftdrg.org/, Accessed 10 March 2010.<br />
[79] Gregory CA, Serra-Mestres J, Hodges JR (1999) Early diagnosis<br />
of the frontal variant of fron<strong>to</strong>temporal dementia:<br />
how sensitive are standard neuroimag<strong>in</strong>g and neuropsychologic<br />
tests? Neuropsychiatry Neuropsychol Behav Neurol 12,<br />
128-135.<br />
[80] Torralva T, Kipps CM, Hodges JR, Clark L, Bek<strong>in</strong>schte<strong>in</strong><br />
T, Roca M, Calcagno ML, Manes F (2007) The relationship<br />
between affective decision-mak<strong>in</strong>g and theory of m<strong>in</strong>d <strong>in</strong> the<br />
frontal variant of fron<strong>to</strong>-temporal dementia. Neuropsychologia<br />
45, 342-349.<br />
[81] Torralva T, Roca M, Gleichgerrcht E, Bek<strong>in</strong>schte<strong>in</strong> T, Manes<br />
F (2009) A neuropsychological battery <strong>to</strong> detect specific executive<br />
and social cognitive impairments <strong>in</strong> early fron<strong>to</strong>temporal<br />
dementia. Bra<strong>in</strong> 132, 1299-1309.<br />
[82] Keane J, Calder AJ, Hodges JR, Young AW (2002) Face and<br />
emotion process<strong>in</strong>g <strong>in</strong> frontal variant fron<strong>to</strong>temporal dementia.<br />
Neuropsychologia 40, 655-665.<br />
[83] Rank<strong>in</strong> KP, Gorno-Temp<strong>in</strong>i ML, Allison SC, Stanley CM,<br />
Glenn S, We<strong>in</strong>er MW, Miller BL (2006) Structural ana<strong>to</strong>my<br />
of empathy <strong>in</strong> neurodegenerative disease. Bra<strong>in</strong> 129, 2945-<br />
2956.<br />
[84] Rank<strong>in</strong> KP, Salazar A, Gorno-Temp<strong>in</strong>i ML, Sollberger M,<br />
Wilson SM, Pavlic D, Stanley CM, Glenn S, We<strong>in</strong>er MW,<br />
Miller BL (2009) Detect<strong>in</strong>g sarcasm from paral<strong>in</strong>guistic<br />
cues: Ana<strong>to</strong>mic and cognitive correlates <strong>in</strong> neurodegenerative<br />
disease. NeuroImage 47, 2005-2015.<br />
[85] Gregory C, Lough S, S<strong>to</strong>ne V, Erz<strong>in</strong>clioglu S, Mart<strong>in</strong> L,<br />
Baron-Cohen S, Hodges JR (2002) Theory of m<strong>in</strong>d <strong>in</strong><br />
patients with frontal variant fron<strong>to</strong>temporal dementia and<br />
Alzheimer’s disease: theoretical and practical implications.<br />
Bra<strong>in</strong> 125, 752-764.<br />
[86] Hodges JR, Mart<strong>in</strong>os M, Woollams AM, Patterson K, Adlam<br />
AR (2008) Repeat and Po<strong>in</strong>t: differentiat<strong>in</strong>g semantic<br />
dementia from progressive non-fluent aphasia. Cortex 44,<br />
1265-1270.<br />
[87] Diehl-Schmid J, Schulte-Overberg J, Hartmann J, Förstl H,<br />
Kurz A, Häussermann P (2007) Extrapyramidal signs, primitive<br />
reflexes and <strong>in</strong>cont<strong>in</strong>ence <strong>in</strong> fron<strong>to</strong>-temporal dementia.<br />
Eur J Neurol 14, 860-864.<br />
[88] Padovani A, Agosti C, Premi E, Bellelli G, Borroni B<br />
(2007) Extrapyramidal symp<strong>to</strong>ms <strong>in</strong> Fron<strong>to</strong>temporal Dementia:<br />
Prevalence and cl<strong>in</strong>ical correlations. Neurosci Lett 422,<br />
39-42.<br />
[89] Garbutt S, Matl<strong>in</strong> A, Hellmuth J, Schenk AK, Johnson JK,<br />
Rosen H, Dean D, Kramer J, Neuhaus J, Miller BL, Lisberger<br />
SG, Boxer AL (2008) Oculomo<strong>to</strong>r function <strong>in</strong> fron<strong>to</strong>temporal<br />
lobar degeneration, related disorders and Alzheimer’s<br />
disease. Bra<strong>in</strong> 131, 1268-1281.<br />
[90] Meyniel C, Rivaud-Péchoux S, Damier P, Gaymard B (2005)<br />
Saccade impairments <strong>in</strong> patients with fron<strong>to</strong>-temporal dementia.<br />
J Neurol Neurosurg Psychiatry 76, 1581-1584.<br />
[91] Pereira J, Williams GB, Acosta-Cabronero J, Pengas G, Spi-<br />
llant<strong>in</strong>i MG, Xuereb JH, Hodges JR, Nes<strong>to</strong>r PJ (2009) Atrophy<br />
patterns <strong>in</strong> his<strong>to</strong>logic vs cl<strong>in</strong>ical group<strong>in</strong>gs of fron<strong>to</strong>temporal<br />
lobar degeneration. Neurology 72, 1653-1660.<br />
[92] Looi J, L<strong>in</strong>dberg O, Zandbelt B, Ostberg P, Andersen C,<br />
Botes L, Svensson L, Wahlund L (2008) Caudate nucleus<br />
volumes <strong>in</strong> fron<strong>to</strong>temporal lobar degeneration: differential<br />
atrophy <strong>in</strong> subtypes. AJNR Am J Neuroradiol 29, 1537-1543.<br />
[93] L<strong>in</strong>dberg O, Ostberg P, Zandbelt B, Oberg J, Zhang Y, Andersen<br />
C, Looi J, Bogdanovic N, Wahlund L (2009) Cortical<br />
morphometric subclassification of fron<strong>to</strong>temporal lobar<br />
degeneration. AJNR Am J Neuroradiol 30, 1233-1239.<br />
[94] Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD<br />
(2009) Neurodegenerative diseases target large-scale human<br />
bra<strong>in</strong> networks. Neuron 62, 42-52.<br />
[95] Seeley WW (2008) Selective functional, regional, and neuronal<br />
vulnerability <strong>in</strong> fron<strong>to</strong>temporal dementia. Curr Op<strong>in</strong><br />
Neurol 21, 701-707.<br />
[96] Seeley WW, Carl<strong>in</strong> DA, Allman JM, Macedo MN, Bush<br />
C, Miller BL, DeArmond SJ (2006) Early fron<strong>to</strong>temporal<br />
dementia targets neurons unique <strong>to</strong> apes and humans. Ann<br />
Neurol 60, 660-667.<br />
[97] Zamboni G, Huey ED, Krueger F, Nichelli PF, Grafman J<br />
(2008) Apathy and dis<strong>in</strong>hibition <strong>in</strong> fron<strong>to</strong>temporal dementia:<br />
Insights <strong>in</strong><strong>to</strong> their neural correlates. Neurology 71, 736-742.<br />
[98] Borroni B, Brambati SM, Agosti C, Gipponi S, Bellelli G,<br />
Gasparotti R, Garibot<strong>to</strong> V, Di Luca M, Scifo P, Perani D,<br />
Padovani A (2007) Evidence of white matter changes on<br />
diffusion tensor imag<strong>in</strong>g <strong>in</strong> fron<strong>to</strong>temporal dementia. Arch<br />
Neurol 64, 246-251.<br />
[99] Gorno-Temp<strong>in</strong>i ML, Dronkers NF, Rank<strong>in</strong> KP, Ogar JM,<br />
Phengrasamy L, Rosen HJ, Johnson JK, We<strong>in</strong>er MW, Miller<br />
BL (2004) Cognition and ana<strong>to</strong>my <strong>in</strong> three variants of primary<br />
progressive aphasia. Ann Neurol 55, 335-346.<br />
[100] Nes<strong>to</strong>r PJ, Graham NL, Fryer TD, Williams GB, Patterson K,<br />
Hodges JR (2003) Progressive non-fluent aphasia is associated<br />
with hypometabolism centred on the left anterior <strong>in</strong>sula.<br />
Bra<strong>in</strong> 126, 2406-2418.<br />
[101] Herholz K (2003) PET studies <strong>in</strong> dementia. Ann Nucl Med<br />
17, 79-89.<br />
[102] Foster NL, Heidebr<strong>in</strong>k JL, Clark CM, Jagust WJ, Arnold SE,<br />
Barbas NR, DeCarli CS, Scott Turner R, Koeppe RA, Higdon<br />
R, M<strong>in</strong>oshima S (2007) FDG-PET improves accuracy<br />
<strong>in</strong> dist<strong>in</strong>guish<strong>in</strong>g fron<strong>to</strong>temporal dementia and Alzheimer’s<br />
disease. Bra<strong>in</strong> 130, 2616-2635.<br />
[103] Panegyres PK, Rogers JM, McCarthy M, Campbell A, Wu<br />
J (2009) Fluorodeoxyglucose-Positron Emission Tomography<br />
<strong>in</strong> the differential diagnosis of early-onset dementia: a<br />
prospective, community-based study. BMC Neurol 9, 41.<br />
[104] Wiley CA, Lopresti BJ, Venneti S, Price J, Klunk WE,<br />
DeKosky ST, Mathis CA (2009) Carbon 11-labeled Pittsburgh<br />
Compound B and Carbon 11-Labeled (R)-PK11195<br />
positron emission <strong>to</strong>mographic imag<strong>in</strong>g <strong>in</strong> Alzheimer disease.<br />
Arch Neurol 66, 60-67.<br />
[105] Ng SY, Villemagne VL, Masters CL, Rowe CC (2007) Evaluat<strong>in</strong>g<br />
atypical dementia syndromes us<strong>in</strong>g positron emission<br />
<strong>to</strong>mography with Carbon 11 labeled Pittsburgh Compound<br />
B. Arch Neurol 64, 1140-1144.<br />
[106] Boxer AL Boeve BF (2007) Fron<strong>to</strong>temporal dementia treatment:<br />
current symp<strong>to</strong>matic therapies and implications of<br />
recent genetic, biochemical, and neuroimag<strong>in</strong>g studies.<br />
Alzheimer Dis Assoc Disord 21, S79-S87.<br />
[107] Bris<strong>to</strong>w M, Cook R, Erz<strong>in</strong>clioglu S, Hodges J (2008) Stress,<br />
distress and mucosal immunity <strong>in</strong> carers of a partner with<br />
fron<strong>to</strong>-temporal dementia. Ag<strong>in</strong>g Ment Health 12, 595-604.
360 J.R. Burrell and J.R. Hodges / <strong>From</strong> <strong>FUS</strong> <strong>to</strong> <strong>Fibs</strong>: What’s <strong>New</strong> <strong>in</strong> Fron<strong>to</strong>temporal Dementia?<br />
[108] Mioshi E, Bris<strong>to</strong>w M, Cook R, Hodges JR (2009) Fac<strong>to</strong>rs<br />
underly<strong>in</strong>g caregiver stress <strong>in</strong> fron<strong>to</strong>temporal dementia and<br />
Alzheimer’s disease. Dement Geriatr Cogn Disord 27, 76-81.<br />
[109] Moretti R, Torre P, An<strong>to</strong>nello RM, Cazza<strong>to</strong> G, Bava A (2003)<br />
Fron<strong>to</strong>temporal dementia: paroxet<strong>in</strong>e as a possible treatment<br />
of behavior symp<strong>to</strong>ms. A randomized, controlled, open 14month<br />
study. Eur Neurol 49, 13-19.<br />
[110] Deak<strong>in</strong> J, Rahman S, Nes<strong>to</strong>r P, Hodges J, Sahakian B (2004)<br />
Paroxet<strong>in</strong>e does not improve symp<strong>to</strong>ms and impairs cognition<br />
<strong>in</strong> fron<strong>to</strong>temporal dementia: a double-bl<strong>in</strong>d randomized<br />
controlled trial. Psychopharmacology (Berl) 172, 400-408.<br />
[111] Moretti R, Torre P, An<strong>to</strong>nello RM, Cazza<strong>to</strong> G, Griggio S,<br />
Bava A (2003) Olanzap<strong>in</strong>e as a treatment of neuropsychiatric<br />
disorders of Alzheimer’s disease and other dementias: a 24month<br />
follow-up of 68 patients. Am J Alzheimers Dis Other<br />
Demen 18, 205-214.<br />
[112] Moretti R, Torre P, An<strong>to</strong>nello RM, Cattaruzza T, Cazza<strong>to</strong> G,<br />
Bava A (2004) Rivastigm<strong>in</strong>e <strong>in</strong> fron<strong>to</strong>temporal dementia: an<br />
open-label study. Drugs Ag<strong>in</strong>g 21, 931-937.<br />
[113] Mendez MF, Shapira JS, McMurtray A, Licht E (2007) Prelim<strong>in</strong>ary<br />
f<strong>in</strong>d<strong>in</strong>gs: behavioral worsen<strong>in</strong>g on donepezil <strong>in</strong> patients<br />
with fron<strong>to</strong>temporal dementia. Am J Geriatr Psychiatry<br />
15, 84-87.<br />
[114] Schneider A Mandelkow E (2008) Tau-Based Treatment<br />
Strategies <strong>in</strong> Neurodegenerative Diseases. Neurotherapeutics<br />
5, 443-457.<br />
[115] Sonnen JA, Mont<strong>in</strong>e KS, Qu<strong>in</strong>n JF, Kaye JA, Breitner JC,<br />
Mont<strong>in</strong>e TJ (2008) Biomarkers for cognitive impairment and<br />
dementia <strong>in</strong> elderly people. Lancet Neurol 7, 704-714.<br />
[116] Hodges JR, Mitchell J, Dawson K, Spillant<strong>in</strong>i MG, Xuereb<br />
JH, McMonagle P, Nes<strong>to</strong>r PJ, Patterson K (2009) Semantic<br />
dementia: demography, familial fac<strong>to</strong>rs and survival <strong>in</strong> a<br />
consecutive series of 100 cases. Bra<strong>in</strong> 133(Pt 1), 300-306.<br />
[117] Josephs KA, Duffy JR, Strand EA, Whitwell JL, Lay<strong>to</strong>n KF,<br />
Parisi JE, Hauser MF, Witte RJ, Boeve BF, Knopman DS,<br />
Dickson DW, Jack CR, Petersen RC (2006) Cl<strong>in</strong>icopathological<br />
and imag<strong>in</strong>g correlates of progressive aphasia and<br />
apraxia of speech. Bra<strong>in</strong> 129, 1385-1398.<br />
[118] Bian H, Van Swieten JC, Leight S, Massimo L, Wood E,<br />
Forman M, Moore P, de Kon<strong>in</strong>g I, Clark CM, Rosso S, Trojanowski<br />
J, Lee VM, Grossman M (2008) CSF biomarkers<br />
<strong>in</strong> fron<strong>to</strong>temporal lobar degeneration with known pathology.<br />
Neurology 70, 1827-1835.<br />
[119] Kapaki E, Paraskevas GP, Papageorgiou SG, Bonakis A,<br />
Kalfakis N, Zalonis I, Vassilopoulos D (2008) Diagnostic<br />
value of CSF biomarker profile <strong>in</strong> fron<strong>to</strong>temporal lobar degeneration.<br />
Alzheimer Dis Assoc Disord 22, 47-53.<br />
[120] Foulds P, McAuley E, Gibbons L, Davidson Y, Picker<strong>in</strong>g-<br />
Brown SM, Neary D, Snowden JS, Allsop D, Mann DMA<br />
(2008) TDP-43 prote<strong>in</strong> <strong>in</strong> plasma may <strong>in</strong>dex TDP-43 bra<strong>in</strong><br />
pathology <strong>in</strong> Alzheimer’s disease and fron<strong>to</strong>temporal lobar<br />
degeneration. Acta Neuropathol 116, 141-146.<br />
[121] Foulds P, Davidson Y, Mishra M, Hobson D, Humphreys<br />
K, Taylor M, Johnson N, We<strong>in</strong>traub S, Akiyama H, Arai T,<br />
Hasegawa M, Bigio E, Benson F, Allsop D, Mann D (2009)<br />
Plasma phosphorylated-TDP-43 prote<strong>in</strong> levels correlate with<br />
bra<strong>in</strong> pathology <strong>in</strong> fron<strong>to</strong>temporal lobar degeneration. Acta<br />
Neuropathol 118, 647-658.<br />
[122] Kasai T, Tokuda T, Ishigami N, Sasayama H, Foulds P,<br />
Mitchell DJ, Mann DMA, Allsop D, Nakagawa M (2009)<br />
Increased TDP-43 prote<strong>in</strong> <strong>in</strong> cerebrosp<strong>in</strong>al fluid of patients<br />
with amyotrophic lateral sclerosis. Acta Neuropathol 117,<br />
55-62.<br />
[123] F<strong>in</strong>ch N, Baker M, Crook R, Swanson K, Kuntz K, Surtees<br />
R, Bisceglio G, Rovelet-Lecrux A, Boeve B, Petersen RC,<br />
Dickson DW, Younk<strong>in</strong> SG, Deramecourt V, Crook J, Graff-<br />
Radford NR, Rademakers R (2009) Plasma progranul<strong>in</strong> levels<br />
predict progranul<strong>in</strong> mutation status <strong>in</strong> fron<strong>to</strong>temporal dementia<br />
patients and asymp<strong>to</strong>matic family members. Bra<strong>in</strong><br />
132, 583-591.<br />
[124] Krueger C, Dean D, Rosen H, Halabi C, We<strong>in</strong>er M, Miller B,<br />
Kramer J (2009) Longitud<strong>in</strong>al rates of lobar atrophy <strong>in</strong> fron<strong>to</strong>temporal<br />
dementia, semantic dementia, and Alzheimer’s<br />
disease. Alzheimer Dis Assoc Disord 24, 43-48.<br />
[125] Small GW, Bookheimer SY, Thompson PM, Cole GM,<br />
Huang S, Kepe V, Barrio JR (2008) Current and future uses<br />
of neuroimag<strong>in</strong>g for cognitively impaired patients. Lancet<br />
Neurol 7, 161-172.