Cognition and behaviour in motor neurone disease - ResearchGate
Cognition and behaviour in motor neurone disease - ResearchGate
Cognition and behaviour in motor neurone disease - ResearchGate
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Cognition</strong> <strong>and</strong> <strong>behaviour</strong> <strong>in</strong> <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong><br />
Patricia Lillo <strong>and</strong> John R. Hodges<br />
Neuroscience Research Australia, University of New<br />
South Wales, Sydney, New South of Wales, Australia<br />
Correspondence to Dr Patricia Lillo, Neuroscience<br />
Research Australia, Barker St, R<strong>and</strong>wick, NSW 2031,<br />
Australia<br />
Tel: +612 9399 1803; e-mail: p.lillo@neura.edu.au<br />
Current Op<strong>in</strong>ion <strong>in</strong> Neurology 2010, 23:638–642<br />
Introduction<br />
Motor <strong>neurone</strong> <strong>disease</strong> (MND) has long been considered<br />
a pure <strong>motor</strong> system <strong>disease</strong>, but recent evidence has led<br />
to its reconceptualization as a multisystem <strong>disease</strong> [1].<br />
Cl<strong>in</strong>ically, up to 50% of patients with MND have cognitive<br />
impairment. Furthermore, 10–15% fulfil criteria<br />
for frontotemporal dementia (FTD) which we have<br />
designated MND-FTD [2]. A similar proportion of<br />
patients with FTD develop MND (FTD-MND) [3].<br />
Pathological f<strong>in</strong>d<strong>in</strong>gs also support this overlap: MND<br />
patients <strong>and</strong> a subset of FTD cases have demonstrable<br />
TAR DNA b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong> 43 (TDP-43) <strong>in</strong>clusions [4].<br />
Here we review cognitive <strong>and</strong> <strong>behaviour</strong>al changes <strong>in</strong><br />
patients with MND <strong>in</strong> the context of recent pathological<br />
<strong>and</strong> genetic advances.<br />
Pathological overlap with frontotemporal<br />
dementia<br />
A major advance has been the f<strong>in</strong>d<strong>in</strong>g that TDP-43 is the<br />
pr<strong>in</strong>cipal component <strong>in</strong> frontotemporal lobar degeneration<br />
Purpose of review<br />
Motor <strong>neurone</strong> <strong>disease</strong> has traditionally been considered a pure <strong>motor</strong> syndrome which<br />
spares aspects of cognition <strong>and</strong> <strong>behaviour</strong>, although <strong>in</strong> recent years it has been<br />
suggested that up to 50% of patients with <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> may develop frontal<br />
dysfunction which, <strong>in</strong> some cases, is severe enough to reach criteria for frontotemporal<br />
dementia. We review the cognitive <strong>and</strong> <strong>behaviour</strong>al changes <strong>in</strong> <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong><br />
emphasiz<strong>in</strong>g the recent advances.<br />
Recent f<strong>in</strong>d<strong>in</strong>gs<br />
A major advance <strong>in</strong> pathology has been the recent discovery of TDP-43 <strong>and</strong> FUS<br />
<strong>in</strong>clusions as the key components <strong>in</strong> cases of <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong>, frontotemporal<br />
dementia–<strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> <strong>and</strong> some cases with pure frontotemporal dementia.<br />
In addition, mutations <strong>in</strong> TARDBP <strong>and</strong> FUS genes have been reported <strong>in</strong> recent years.<br />
Longitud<strong>in</strong>al studies showed that progression of cognitive impairment over the course<br />
of <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> appears to be mild <strong>and</strong> occurs only <strong>in</strong> a proportion of <strong>motor</strong><br />
<strong>neurone</strong> <strong>disease</strong> patients. The presence of cognitive impairment seems to be related to<br />
a faster <strong>disease</strong> <strong>and</strong> a shorter survival.<br />
Summary<br />
Motor <strong>neurone</strong> <strong>disease</strong> is a multi-system disorder which overlaps with frontotemporal<br />
dementia. Behavioural <strong>and</strong> cognitive changes appear to occur <strong>in</strong> a subset of patients<br />
with <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong>, but the cause of this variability rema<strong>in</strong>s unclear.<br />
Keywords<br />
amyotrophic lateral sclerosis, <strong>behaviour</strong>al changes, cognitive impairment,<br />
frontotemporal dementia, <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong><br />
Curr Op<strong>in</strong> Neurol 23:638–642<br />
ß 2010 Wolters Kluwer Health | Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s<br />
1350-7540<br />
with ubiquit<strong>in</strong>ated <strong>in</strong>clusions (FTLD-U), currently classified<br />
as FTLD-TDP. The condition is found <strong>in</strong> those<br />
patients who present with FTD but develop frank<br />
MND (FTD-MND), approximately a half of those with<br />
uncomplicated FTD <strong>and</strong> the majority of patients with<br />
both sporadic <strong>and</strong> familial MND. TDP-43 is a nuclear<br />
prote<strong>in</strong> of 43 kDa, which participates <strong>in</strong> various critical<br />
biological processes by b<strong>in</strong>d<strong>in</strong>g DNA <strong>and</strong> RNA. Normally,<br />
it is localized <strong>in</strong> nuclei of neurons <strong>and</strong> glial cells. Pathologically,<br />
normal nuclear TDP-43 sta<strong>in</strong><strong>in</strong>g is absent, <strong>and</strong><br />
cytoplasmic <strong>and</strong> nuclear TDP-43 <strong>in</strong>clusions are detectable<br />
[4]. Five patterns of TDP-43 aggregation are recognized.<br />
Pure MND, type 5, is characterized by cytoplasmic<br />
<strong>in</strong>clusions (ske<strong>in</strong>-like or dense granular), affect<strong>in</strong>g pr<strong>in</strong>cipally<br />
the <strong>motor</strong> cortex, the sp<strong>in</strong>al cord, basal ganglia <strong>and</strong><br />
thalamus. FTD-MND is usually associated with type 2,<br />
which is characterized by neuronal cytoplasmic <strong>in</strong>clusions<br />
<strong>in</strong> superficial <strong>and</strong> deep cortical layers <strong>in</strong>volv<strong>in</strong>g the<br />
temporal <strong>and</strong> frontal cortices, dentate gyrus, amygdala<br />
<strong>and</strong> subcortical white matter [5 ]. As expected, the degree<br />
of neuronal loss is more <strong>in</strong> FTD-MND than <strong>in</strong> pure MND<br />
<strong>and</strong> affects primarily the anterior c<strong>in</strong>gulate gyrus, substantia<br />
nigra <strong>and</strong> amygdala [6,7].<br />
1350-7540 ß 2010 Wolters Kluwer Health | Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s DOI:10.1097/WCO.0b013e3283400b41<br />
Copyright © Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohibited.
In addition, another prote<strong>in</strong> called FUS/TLS (fused <strong>in</strong><br />
sarcoma/translated <strong>in</strong>to liposarcoma), a 526-am<strong>in</strong>o-acid<br />
DNA/RNA b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong>, has been very recently<br />
identified <strong>in</strong> pathological cases of FTLD-U without<br />
TDP-43 <strong>in</strong>clusions [8]. The disorder is characterized<br />
by neuronal cytoplasmic <strong>and</strong> <strong>in</strong>tra-nuclear <strong>in</strong>clusions<br />
immunoreactive for FUS. This pattern has been also<br />
been found <strong>in</strong> cases with pure MND, MND-FTD <strong>and</strong><br />
cases of <strong>behaviour</strong>al variant FTD [9,10].<br />
Genetics<br />
There has been a recent explosion of knowledge <strong>in</strong> MND<br />
<strong>and</strong> FTD genetics, although the exact relationship<br />
between the identified genes <strong>and</strong> pathology rema<strong>in</strong>s<br />
unclear. A prom<strong>in</strong>ent family history is present <strong>in</strong> around<br />
5–10% of the patients with MND. It is <strong>in</strong>terest<strong>in</strong>g to<br />
note that the Cu–Zn superoxide dismutase 1 (SOD1)<br />
mutation, which accounts for 15–20% of autosomal dom<strong>in</strong>ant<br />
familial cases, is characterized by lack of TDP-43<br />
<strong>and</strong> FUS <strong>in</strong>clusions <strong>and</strong> an apparent absence of cognitive<br />
<strong>in</strong>volvement [9,11 ,12].<br />
A second gene now l<strong>in</strong>ked to both familial <strong>and</strong> sporadic<br />
MND is the TAR DNA b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong> (TARDBP) gene<br />
on chromosome 1p36.22, designated ALS10. It is present<br />
<strong>in</strong> 1–3% of MND cases, <strong>and</strong> over 30 mutations have been<br />
identified with an autosomal dom<strong>in</strong>ant pattern of <strong>in</strong>heritance.<br />
Two cases present<strong>in</strong>g with FTD-MND have been<br />
reported; one with language deficits <strong>and</strong> the other with<br />
<strong>behaviour</strong>al impairment. Only one sporadic case with<br />
pure FTD with a TARDBP mutation has, so far, been<br />
reported [11 ,13].<br />
The third group, classified as ALS6, have mutations <strong>in</strong><br />
the fused sarcoma/translocation <strong>in</strong> liposarcoma gene<br />
(FUS/TLS), on chromosome 16q12. Dom<strong>in</strong>ant <strong>and</strong> recessive<br />
mutations have been identified <strong>in</strong> familial <strong>and</strong><br />
sporadic MND cases, <strong>and</strong> one case of sporadic FTD<br />
[11 ,12,14].<br />
Other mutations l<strong>in</strong>ked to MND cases with FTD are<br />
missense mutations <strong>in</strong> angiogen<strong>in</strong> (ANG) gene <strong>and</strong><br />
mutations <strong>in</strong> the p150 subunit of dynact<strong>in</strong> 1 (DCTN1)<br />
gene. In addition, two mutations reported <strong>in</strong> FTD<br />
cases, affect<strong>in</strong>g chromat<strong>in</strong>-modify<strong>in</strong>g prote<strong>in</strong> 2B<br />
(CHMP2B) <strong>and</strong> progranul<strong>in</strong>e (PGRN) genes, although<br />
uncommon, have been found <strong>in</strong> cases with FTD <strong>and</strong><br />
MND [12].<br />
There are clearly more genes to be identified which are<br />
likely to be more common than some of the known<br />
mutations. A significant number of families <strong>in</strong> which<br />
some members have MND, FTD or both have been<br />
l<strong>in</strong>ked to chromosome 9, but the gene responsible<br />
rema<strong>in</strong>s elusive [15].<br />
<strong>Cognition</strong> <strong>and</strong> <strong>behaviour</strong> <strong>in</strong> <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> Lillo <strong>and</strong> Hodges 639<br />
Development of <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> <strong>in</strong><br />
patients with frontotemporal dementia<br />
Approximately, 15% of the patients with FTD develop<br />
frank MND <strong>in</strong> the course of the <strong>disease</strong> [3,16]. This<br />
cl<strong>in</strong>ical syndrome has a fairly consistent pattern <strong>in</strong> which<br />
rapidly evolv<strong>in</strong>g <strong>behaviour</strong>al <strong>and</strong> cognitive symptoms are<br />
followed after a period of 1–2 years later (sometimes up<br />
to 7 years) by bulbar <strong>and</strong> other signs of <strong>motor</strong> dysfunction<br />
[17,18 ]. The presentation may be with either <strong>behaviour</strong>al<br />
or language impairment, but usually both are<br />
present from the start.<br />
The <strong>behaviour</strong>al changes <strong>in</strong>clude poor <strong>in</strong>sight, lack of<br />
empathy, obsessions <strong>and</strong> tendency to eat sweet food <strong>and</strong><br />
hoard th<strong>in</strong>gs. Periods of apathy alternate with irritability<br />
<strong>and</strong> dis<strong>in</strong>hibition. The language impairment is characterized<br />
by a progressive nonfluent aphasia, lead<strong>in</strong>g to<br />
mutism [17]. A detailed case study of five patients with<br />
marked aphasia <strong>in</strong> association with MND documented a<br />
selective deficit <strong>in</strong> verb process<strong>in</strong>g <strong>in</strong>volv<strong>in</strong>g both production<br />
<strong>and</strong> comprehension. These patients were shown<br />
to have pathological <strong>in</strong>volvement of Broca’s area [19].<br />
Neuropsychological assessment often reveals prom<strong>in</strong>ent<br />
frontal/executive dysfunction. Although psychotic<br />
symptoms appear to be <strong>in</strong>frequent <strong>in</strong> FTD, remarkably,<br />
delusionshavebeenreported<strong>in</strong>upto50%ofpatients<br />
with the FTD-MND phenotype. Recent reports have<br />
focused attention on the presence of delusions <strong>in</strong> early<br />
stages of the <strong>disease</strong>, which have been described as<br />
persecutory type, phantom boarder syndrome, erotomania,<br />
bodily <strong>in</strong>vasion <strong>and</strong> delusional pregnancy [18 ,20 ].<br />
The course of the <strong>disease</strong>, with survival from diagnosis of<br />
2–3 years, is certa<strong>in</strong>ly shorter than <strong>in</strong> cases with pure<br />
FTD [18 ].<br />
Executive dysfunction<br />
The greatest body of literature on cognition <strong>in</strong> MND has<br />
related to executive function <strong>and</strong> by implication to prefrontal<br />
lobe abilities [2,21–24] (Table 1). Although estimates<br />
of the prevalence of such deficits range from 10 to<br />
70%, <strong>in</strong> the largest study to date subtle cognitive impairment<br />
was found <strong>in</strong> 50% of 279 patients with sporadic<br />
MND [2].<br />
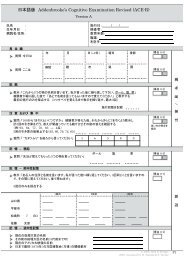
Table 1 Summary of cognitive <strong>and</strong> <strong>behaviour</strong>al changes <strong>in</strong><br />
patients with <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong><br />
Deficits caused by cognitive impairment Behavioural changes<br />
Attention Apathy<br />
Verbal fluency Irritability<br />
Work<strong>in</strong>g memory Lack of empathy<br />
Plann<strong>in</strong>g/organiz<strong>in</strong>g Dis<strong>in</strong>hibition<br />
Mental shift<strong>in</strong>g Compulsions<br />
Stereotyped <strong>behaviour</strong>s<br />
Data from [21–27,28 ].<br />
Copyright © Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohibited.
640 Degenerative <strong>and</strong> cognitive <strong>disease</strong>s<br />
The most prom<strong>in</strong>ent deficit reported has been reduction<br />
<strong>in</strong> verbal fluency, which is evident <strong>in</strong> the letter fluency<br />
test [24,25]. This impairment has been associated with<br />
dysfunction of anterior c<strong>in</strong>gulate gyrus <strong>and</strong> middle <strong>and</strong><br />
<strong>in</strong>ferior frontal gyri as demonstrated by functional MRI<br />
[25]. Written rather verbal fluency has been exam<strong>in</strong>ed <strong>in</strong><br />
patients with significant dysarthria [24]. Attention (verbal<br />
series attention test <strong>and</strong> paced auditory serial addition<br />
test), work<strong>in</strong>g memory (reverse digit span test), plann<strong>in</strong>g<br />
(Tower of Hanoi) <strong>and</strong> cognitive flexibility (Wiscons<strong>in</strong><br />
card sort<strong>in</strong>g test) may also be impaired [21–24]. As<br />
impaired performance on neuropsychological assessment<br />
can be confounded by <strong>motor</strong> dysfunction, a recent study<br />
assessed executive function with a <strong>motor</strong>-free test. In this<br />
study, the performance of MND patients <strong>and</strong> controls<br />
was compared us<strong>in</strong>g the Medication Schedul<strong>in</strong>g Task,<br />
which <strong>in</strong>cludes plann<strong>in</strong>g, multitask<strong>in</strong>g, mental set shift<strong>in</strong>g<br />
<strong>and</strong> delay<strong>in</strong>g response components. The participants<br />
were asked to assemble a daily safe scheme for the<br />
adm<strong>in</strong>istration of the medication. Despite correction<br />
for <strong>motor</strong> disability, MND patients performed worse than<br />
the control group [26].<br />
Behavioural symptoms<br />
A range of <strong>behaviour</strong>al symptoms that parallel those<br />
found <strong>in</strong> FTD have been reported although, as with<br />
cognitive dysfunction, estimates of prevalence vary considerably.<br />
Apathy has been consistently found to be the<br />
most common feature. For <strong>in</strong>stance, one study reported<br />
apathy <strong>in</strong> 55% of MND patients, which correlated with<br />
deficits <strong>in</strong> verbal fluency but not with physical disability,<br />
mood disturbances or respiratory function [27]. A study<br />
on 225 MND patients, which used the Frontal Systems<br />
Behaviour Scale (FrSBe) designed to evaluate apathy,<br />
executive dysfunction <strong>and</strong> dis<strong>in</strong>hibition, showed an<br />
elevation <strong>in</strong> the total FrSBe score <strong>in</strong> a quarter of cases<br />
<strong>and</strong> over a third of cases had impairment <strong>in</strong> at least one<br />
<strong>behaviour</strong>al doma<strong>in</strong>. Patients with cognitive impairment<br />
had greater <strong>behaviour</strong>al changes, although the two<br />
doma<strong>in</strong>s were partially <strong>in</strong>dependent [28 ]. F<strong>in</strong>ally, two<br />
<strong>in</strong>formant-based <strong>behaviour</strong>al <strong>in</strong>terview surveys showed<br />
that patients with MND may also present <strong>in</strong>discrim<strong>in</strong>ate<br />
eat<strong>in</strong>g, gluttony, compulsions <strong>and</strong> <strong>behaviour</strong>al stereotypes<br />
[29,30] (see Table 1).<br />
Memory<br />
A majority of the studies assess<strong>in</strong>g memory have shown<br />
greater impairment of immediate recall than with recognition<br />
tasks, suggest<strong>in</strong>g a retrieval disturbance secondary<br />
to prefrontal dysfunction [21,31]. A recent meta-analysis<br />
of studies to date concluded that some aspects of memory<br />
are consistently impaired, notably immediate <strong>and</strong><br />
delayed visual memory <strong>and</strong> immediate verbal memory.<br />
The pattern is <strong>in</strong> keep<strong>in</strong>g with frontal lobe dysfunction,<br />
but <strong>in</strong>volvement of temporal lobe structures could not be<br />
discounted because of the effect size [32 ].<br />
Language<br />
Language assessment presents particular problems <strong>in</strong><br />
patients with dysarthria, but even allow<strong>in</strong>g for this it<br />
seems that significant aphasia occurs <strong>in</strong> a proportion of<br />
patients with MND <strong>and</strong> may be more common <strong>in</strong><br />
patients with bulbar onset <strong>disease</strong> [33]. The most commonly<br />
identified deficits have been reduced speech<br />
output <strong>and</strong> anomia [17,34]. Some patients develop significant<br />
aphasia designated progressive nonfluent aphasia<br />
with agrammatism <strong>in</strong> production <strong>and</strong> impaired syntactic<br />
comprehension. Interest<strong>in</strong>gly, a higher order disturbance<br />
of <strong>motor</strong> speech, apraxia of speech, has been reported <strong>in</strong><br />
patients with bulbar onset <strong>disease</strong>, frequently associated<br />
with spastic or mixed spastic–flaccid dysarthria [35].<br />
Emotional process<strong>in</strong>g<br />
The fact that emotion process<strong>in</strong>g is severely <strong>and</strong> consistently<br />
compromised <strong>in</strong> patients with FTD [36] has underst<strong>and</strong>ably<br />
led a number of <strong>in</strong>vestigators to study this<br />
aspect of social cognition <strong>in</strong> MND. Impaired recognition<br />
of emotional faces was found <strong>in</strong> a group of bulbar MND<br />
patients [37]. A selective deficit <strong>in</strong> the recognition of<br />
threat stimuli through faces has also been reported, which<br />
parallels that seen <strong>in</strong> patients with amygdala damage [38].<br />
Longitud<strong>in</strong>al studies<br />
A key question unanswered from cross-sectional studies<br />
is whether cognitive dysfunction rema<strong>in</strong>s conf<strong>in</strong>ed to a<br />
subset of patients with MND whose condition worsens<br />
over time or alternatively whether all patients with MND<br />
eventually develop cognitive or <strong>behaviour</strong>al changes.<br />
Longitud<strong>in</strong>al studies have found cognitive dysfunction<br />
early <strong>in</strong> the course of the <strong>disease</strong>, on the basis of verbal<br />
fluency deficits [39] particularly <strong>in</strong> those with bulbar<br />
onset <strong>disease</strong> [40], although this has not been a universal<br />
f<strong>in</strong>d<strong>in</strong>g [41,42 ].<br />
Progression of cognitive impairment over the course of<br />
MND appears to be mild. Older patients, <strong>and</strong> those with<br />
more rapidly progress<strong>in</strong>g <strong>disease</strong>, may be more predisposed<br />
to cognitive impairment, which, <strong>in</strong> turn, contributes<br />
to a shorter survival [42 ].<br />
Neuroimag<strong>in</strong>g<br />
The pr<strong>in</strong>cipal role of neuroimag<strong>in</strong>g <strong>in</strong> MND has been to<br />
exclude alternative diagnoses, although <strong>in</strong> more recent<br />
years new techniques have been used to assess the<br />
<strong>in</strong>tegrity of both the <strong>motor</strong> system <strong>and</strong> the extra <strong>motor</strong><br />
regions.<br />
Copyright © Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohibited.
Structural MRI has established that those with subtle<br />
cognitive or <strong>behaviour</strong>al impairment showed grey matter<br />
loss <strong>in</strong> frontal, parietal <strong>and</strong> limbic regions [43 ]. As<br />
expected, patients with MND-FTD have atrophy of<br />
frontotemporal lobes <strong>and</strong> hyper<strong>in</strong>tensity of subcortical<br />
white matter <strong>in</strong> medial anterior temporal lobe, similar to<br />
that seen <strong>in</strong> patients with pure FTD [44,45].<br />
A comparison of MND <strong>and</strong> MND-FTD patient groups<br />
us<strong>in</strong>g voxel-based morphometry showed a similar pattern<br />
of grey matter atrophy <strong>in</strong>volv<strong>in</strong>g bilateral <strong>motor</strong> <strong>and</strong><br />
pre<strong>motor</strong> cortices, superior, middle <strong>and</strong> <strong>in</strong>ferior frontal<br />
gyri, superior temporal gyri, temporal poles <strong>and</strong> left<br />
posterior thalamus that was, as predicted, greater <strong>in</strong><br />
the MND-FTD group [46].<br />
Functional MRI (fMRI) studies have shown reduced<br />
activation of the middle <strong>and</strong> <strong>in</strong>ferior frontal gyri <strong>and</strong><br />
anterior c<strong>in</strong>gulate gyrus <strong>in</strong> MND patients dur<strong>in</strong>g letter<br />
fluency tasks [29]. Deficits on word fluency <strong>and</strong> confrontation<br />
nam<strong>in</strong>g have been shown to correlate with<br />
impaired activation of the prefrontal region (Broca area),<br />
temporal, parietal <strong>and</strong> occipital lobes [29,43 ].<br />
A few recent studies have exam<strong>in</strong>ed the relationship<br />
between social process<strong>in</strong>g <strong>and</strong> regions of bra<strong>in</strong> activation<br />
us<strong>in</strong>g fMRI. One study demonstrated that patients with<br />
MND present<strong>in</strong>g altered sensitivity to social–emotional<br />
clues had an <strong>in</strong>creased response <strong>in</strong> the right supramarg<strong>in</strong>al<br />
area [47]. Another showed that impaired emotional<br />
process <strong>in</strong> ALS patients was related to right hemisphere<br />
dysfunction [48].<br />
Conclusion<br />
Recent advances <strong>in</strong> genetics <strong>and</strong> pathology have led to<br />
the concept of MND as a multisystem disorder which<br />
overlaps with frontotemporal dementia. The assessment<br />
of patients with MND is challeng<strong>in</strong>g, due to the <strong>motor</strong><br />
disability <strong>and</strong> the variability of the cl<strong>in</strong>ical phenotype. It<br />
appears that changes <strong>in</strong> <strong>behaviour</strong> <strong>and</strong> cognition, notably<br />
executive function, language <strong>and</strong> emotional process<strong>in</strong>g,<br />
occurs only <strong>in</strong> a subset of patients, but the cause of this<br />
variability <strong>in</strong> the cl<strong>in</strong>ical phenotype rema<strong>in</strong>s unclear.<br />
Acknowledgements<br />
The study was supported by the Australian Research Council<br />
Federation Fellowship, FF0776229 (Prof. Hodges) <strong>and</strong> CONICYT<br />
scholarship (Government of Chile) (Dr Lillo).<br />
J.R.H. serves on editorial boards of Aphasiology, Cognitive Neuropsychiatry,<br />
<strong>and</strong> Cognitive Neuropsychology; receives royalties from<br />
publication of Cognitive Assessment for Cl<strong>in</strong>icians (Oxford University<br />
Press, 2007) <strong>and</strong> Frontotemporal Dementia Syndromes (Cambridge<br />
University Press, 2007) <strong>and</strong> receives fellowship support from the<br />
Australian Research Council Federation.<br />
Thanks to Dr James Burrell, MBBS (Hons), for his assistance with<br />
proofread<strong>in</strong>g.<br />
<strong>Cognition</strong> <strong>and</strong> <strong>behaviour</strong> <strong>in</strong> <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> Lillo <strong>and</strong> Hodges 641<br />
References <strong>and</strong> recommended read<strong>in</strong>g<br />
Papers of particular <strong>in</strong>terest, published with<strong>in</strong> the annual period of review, have<br />
been highlighted as<br />
of special <strong>in</strong>terest<br />
of outst<strong>and</strong><strong>in</strong>g <strong>in</strong>terest<br />
Additional references related to this topic can also be found <strong>in</strong> the Current<br />
World Literature section <strong>in</strong> this issue (p. 708).<br />
1 Geser F, Br<strong>and</strong>meir NJ, Kwong LK, et al. Evidence of multisystem disorder <strong>in</strong><br />
whole-bra<strong>in</strong> map of pathological TDP-43 <strong>in</strong> amyotrophic lateral sclerosis. Arch<br />
Neurol 2008; 65:636–641.<br />
2 R<strong>in</strong>gholz GM, Appel SH, Bradshaw M, et al. Prevalence <strong>and</strong> patterns of<br />
cognitive impairment <strong>in</strong> sporadic ALS. Neurology 2005; 65:586–590.<br />
3 Lomen-Hoerth C, Anderson T, Miller B. The overlap of amyotrophic lateral<br />
sclerosis <strong>and</strong> frontotemporal dementia. Neurology 2002; 59:1077–1079.<br />
4 Neumann M, Sampathu DM, Kwong LK, et al. Ubiquit<strong>in</strong>ated TDP-43 <strong>in</strong><br />
frontotemporal lobar degeneration <strong>and</strong> amyotrophic lateral sclerosis. Science<br />
2006; 314:130–133.<br />
5 Geser F, Lee VMY, Trojanowski JQ. Amyotrophic lateral sclerosis <strong>and</strong><br />
frontotemporal lobar degeneration: a spectrum of TDP-43 prote<strong>in</strong>opathies.<br />
Neuropathology 2010; 30:103–112.<br />
A complete description of the pathology <strong>in</strong> MND with specific emphasis on the<br />
distribution of TDP-43 <strong>in</strong>clusions.<br />
6 Kersaitis C, Halliday GM, Xuereb JH, et al. Ubiquit<strong>in</strong>-positive <strong>in</strong>clusions <strong>and</strong><br />
progression of pathology <strong>in</strong> frontotemporal dementia <strong>and</strong> <strong>motor</strong> <strong>neurone</strong><br />
<strong>disease</strong> identifies a group with ma<strong>in</strong>ly early pathology. Neuropathol Appl<br />
Neurobiol 2006; 32:83–91.<br />
7 Geser F, Mart<strong>in</strong>ez-Lage M, Rob<strong>in</strong>son J, et al. Cl<strong>in</strong>ical <strong>and</strong> pathological<br />
cont<strong>in</strong>uum of multisystem TDP-43 prote<strong>in</strong>opathies. Arch Neurol 2009;<br />
66:180–189.<br />
8 Neumann M, Rademakers R, Roeber S, et al. A new subtype of frontotemporal<br />
lobar degeneration with FUS pathology. Bra<strong>in</strong> 2009; 132:2922–2931.<br />
9 Deng HX, Zhai H, Bigio EH, et al. FUS-immunoreactive <strong>in</strong>clusions are a<br />
common feature <strong>in</strong> sporadic <strong>and</strong> non-SOD1 familial amyotrophic lateral<br />
sclerosis. Ann Neurol 2010; 67:739–748.<br />
10 Urw<strong>in</strong> H, Josephs KA, Rohrer JD, et al. FUS pathology def<strong>in</strong>es the majority of<br />
tau- <strong>and</strong> TDP-43-negative frontotemporal lobar degeneration. Acta Neuropathol<br />
2010; 120:33–41.<br />
11 Dion PA, Daoud H, Rouleau GA. Genetics of <strong>motor</strong> neuron disorders: new<br />
<strong>in</strong>sights <strong>in</strong>to pathogenic mechanisms. Nat Rev Genet 2009; 10:769–782.<br />
An excellent update on the genetic f<strong>in</strong>d<strong>in</strong>gs across <strong>motor</strong> neuron <strong>disease</strong> with a<br />
brief <strong>and</strong> clear explanation of the pathogenic mechanism <strong>and</strong> cl<strong>in</strong>ical presentation.<br />
12 Millecamps S, Salachas F, Cazeneuve C, et al. SOD1, ANG, VAPB, TARDBP,<br />
<strong>and</strong> FUS mutations <strong>in</strong> familial amyotrophic lateral sclerosis: genotype–<br />
phenotype correlations. J Med Genet 2010; 47:554–560.<br />
13 Benajiba L, Le Ber I, Camuzat A, et al. TARDBP mutations <strong>in</strong> motoneuron<br />
<strong>disease</strong> with frontotemporal lobar degeneration. Ann Neurol 2009; 65:470–<br />
473.<br />
14 Van Langenhove T, van der Zee J, Sleegers K, et al. Genetic contribution of<br />
FUS to frontotemporal lobar degeneration. Neurology 2010; 74:366–371.<br />
15 Boxer AL, Mackenzie IR, Boeve BF, et al. Cl<strong>in</strong>ical, neuroimag<strong>in</strong>g <strong>and</strong> neuropathological<br />
features of a new chromosome 9p-l<strong>in</strong>ked FTD-ALS family.<br />
J Neurol Neurosurg Psychiatry 2010; Jun 10 [Epub ahead of pr<strong>in</strong>t].<br />
16 Lomen-Hoerth C. Characterization of amyotrophic lateral sclerosis <strong>and</strong> frontotemporal<br />
dementia. Dement Geriatr Cogn Disord 2004; 17:337–341.<br />
17 Bak TH, Hodges JR. Motor <strong>neurone</strong> <strong>disease</strong>, dementia <strong>and</strong> aphasia: co<strong>in</strong>cidence,<br />
co-occurrence or cont<strong>in</strong>uum? J Neurol 2001; 248:260–270.<br />
18 Lillo P, Garc<strong>in</strong> B, Hornberger M, et al. Neurobehavioral features <strong>in</strong> frontotemporal<br />
dementia with amyotrophic lateral sclerosis. Arch Neurol 2010;<br />
67:826–830.<br />
Provides <strong>in</strong>terest<strong>in</strong>g data compar<strong>in</strong>g the <strong>behaviour</strong>al symptoms of patients with<br />
FTD-MND vs. bvFTD <strong>and</strong> survival.<br />
19 Bak TH, O’Donovan DG, Xuereb JH, et al. Selective impairment of verb<br />
process<strong>in</strong>g associated with pathological changes <strong>in</strong> Brodmann areas 44 <strong>and</strong><br />
45 <strong>in</strong> the <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong>-dementia-aphasia syndrome. Bra<strong>in</strong> 2001;<br />
124:103–120.<br />
20 Loy CT, Kril JJ, Trollor JN, et al. The case of a 48 year-old woman with bizarre<br />
<strong>and</strong> complex delusions. Nat Rev Neurol 2010; 6:175–179.<br />
An unusual case with an excellent cl<strong>in</strong>ico-pathological correlation.<br />
21 Phukan J, Pender NP, Hardiman O. Cognitive impairment <strong>in</strong> amyotrophic<br />
lateral sclerosis. Lancet Neurol 2007; 6:994–1003.<br />
22 Woolley SC, Katz JS. Cognitive <strong>and</strong> behavioral impairment <strong>in</strong> amyotrophic<br />
lateral sclerosis. Phys Med Rehabil Cl<strong>in</strong> N Am 2008; 19:607–617.<br />
Copyright © Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohibited.
642 Degenerative <strong>and</strong> cognitive <strong>disease</strong>s<br />
23 Murphy JM, Henry RG, Langmore S, et al. Cont<strong>in</strong>uum of frontal lobe<br />
impairment <strong>in</strong> amyotrophic lateral sclerosis. Arch Neurol 2007; 64:530–<br />
534.<br />
24 Abrahams S, Leigh PN, Harvey A, et al. Verbal fluency <strong>and</strong> executive<br />
dysfunction <strong>in</strong> amyotrophic lateral sclerosis (ALS). Neuropsychologia<br />
25<br />
2000; 38:734–747.<br />
Abrahams S, Goldste<strong>in</strong> LH, Simmons A, et al. Word retrieval <strong>in</strong> amyotrophic<br />
lateral sclerosis: a functional magnetic resonance imag<strong>in</strong>g study. Bra<strong>in</strong> 2004;<br />
127:1507–1517.<br />
26 Stukovnik V, Zidar J, Podnar S, Repovs G. Amyotrophic lateral sclerosis<br />
patients show executive impairments on st<strong>and</strong>ard neuropsychological measures<br />
<strong>and</strong> an ecologically valid <strong>motor</strong>-free test of executive functions. J Cl<strong>in</strong><br />
Exp Neuropsychol 2010; 24:1–15.<br />
27 Grossman AB, Woolley-Lev<strong>in</strong>e S, Bradley WG, Miller RG. Detect<strong>in</strong>g neurobehavioral<br />
changes <strong>in</strong> amyotrophic lateral sclerosis. Amyotroph Lateral Scler<br />
2007; 8:56–61.<br />
28 Witgert M, Salamone AR, Strutt AM, et al. Frontal-lobe mediated behavioral<br />
dysfunction <strong>in</strong> amyotrophic lateral sclerosis. Eur J Neurol 2010; 17:103–<br />
110.<br />
The largest study of <strong>behaviour</strong>al changes <strong>in</strong> MND patients with neuropsychological<br />
correlation.<br />
29 Gibbons ZC, Richardson A, Neary D, Snowden JS. Behaviour <strong>in</strong> amyotrophic<br />
lateral sclerosis. Amyotroph Lateral Scler 2008; 9:67–74.<br />
30 Lillo P, Mioshi E, Zo<strong>in</strong>g MC, et al. How common are <strong>behaviour</strong>al changes <strong>in</strong><br />
amyotrophic lateral sclerosis? Amyotroph Lateral Scler 2010; Sep 19 [Epub<br />
ahead of pr<strong>in</strong>t].<br />
31 Mantovan MC, Baggio L, Dalla Barba G, et al. Memory deficits <strong>and</strong> retrieval<br />
processes <strong>in</strong> ALS. Eur J Neurol 2003; 10:221–227.<br />
32 Raaphorst J, de Visser M, L<strong>in</strong>ssen WH, et al. The cognitive profile of<br />
amyotrophic lateral sclerosis: a meta-analysis. Amyotroph Lateral Scler<br />
2010; 11:27–37.<br />
First meta-analysis <strong>in</strong>clud<strong>in</strong>g a review of neuropsychological assessments.<br />
33 Abrahams S, Goldste<strong>in</strong> LH, AlChalabi A, et al. Relation between cognitive<br />
dysfunction <strong>and</strong> pseudobulbar palsy <strong>in</strong> amyotrophic lateral sclerosis. J Neurol<br />
Neurosurg Psychiatry 1997; 62:464–472.<br />
34 Bak TH, Hodges JR. The effects of <strong>motor</strong> <strong>neurone</strong> <strong>disease</strong> on language:<br />
further evidence. Bra<strong>in</strong> Lang 2004; 89:354–361.<br />
35 Duffy JR, Peach RK, Str<strong>and</strong> EA. Progressive apraxia of speech as a sign of<br />
<strong>motor</strong> neuron <strong>disease</strong>. Am J Speech Lang Pathol 2007; 16:198–208.<br />
36 Lough S, Kipps CM, Treise C, et al. Social reason<strong>in</strong>g, emotion <strong>and</strong> empathy <strong>in</strong><br />
frontotemporal dementia. Neuropsychologia 2006; 44:950–958.<br />
37 Zimmerman EK, Esl<strong>in</strong>ger PJ, Simmons Z, Barrett AM. Emotional perception<br />
deficits <strong>in</strong> amyotrophic lateral sclerosis. Cogn Behav Neurol 2007; 20:79–<br />
82.<br />
38 Schmolck H, Mosnik D, Schulz P. Rat<strong>in</strong>g the approachability of faces <strong>in</strong> ALS.<br />
Neurology 2007; 69:2232–2235.<br />
39 Abrahams S, Leigh PN, Goldste<strong>in</strong> LH. Cognitive change <strong>in</strong> ALS: a prospective<br />
study. Neurology 2005; 64:1222–1226.<br />
40 Schreiber H, Gaigalat T, Wiedemuth-Catr<strong>in</strong>escu U, et al. Cognitive function <strong>in</strong><br />
bulbar- <strong>and</strong> sp<strong>in</strong>al-onset amyotrophic lateral sclerosis: a longitud<strong>in</strong>al study <strong>in</strong><br />
52 patients. J Neurol 2005; 252:772–781.<br />
41 Rob<strong>in</strong>son KM, Lacey SC, Grugan P, et al. Cognitive function<strong>in</strong>g <strong>in</strong> sporadic<br />
amyotrophic lateral sclerosis: a six month longitud<strong>in</strong>al study. J Neurol Neurosurg<br />
Psychiatry 2006; 77:668–670.<br />
42 Gordon PH, Goetz RR, Rabk<strong>in</strong> JG, et al. A prospective cohort study of<br />
neuropsychological test performance <strong>in</strong> ALS. Amyotroph Lateral Scler 2010;<br />
11:312–320.<br />
Analyses the previous longitud<strong>in</strong>al studies <strong>and</strong> br<strong>in</strong>gs analysis on groups of risk for<br />
cognitive impairment <strong>and</strong> shorter survival.<br />
43 Agosta F, Chio A, Cosott<strong>in</strong>i M, et al. The present <strong>and</strong> the future of neuroimag<strong>in</strong>g<br />
<strong>in</strong> amyotrophic lateral sclerosis. AJNR Am J Neuroradiol 2010; Apr 1<br />
[Epub ahead of pr<strong>in</strong>t].<br />
A complete review of the neuroimag<strong>in</strong>g <strong>in</strong> <strong>motor</strong> <strong>and</strong> extra<strong>motor</strong> bra<strong>in</strong> areas.<br />
44 Mori H, Yagishita A, Takeda T, Mizutani T. Symmetric temporal abnormalities<br />
on MR imag<strong>in</strong>g <strong>in</strong> amyotrophic lateral sclerosis with dementia. AJNR Am J<br />
Neuroradiol 2007; 28:1511–1516.<br />
45 Mezzapesa DM, Ceccarelli A, Dicuonzo F, et al. Whole-bra<strong>in</strong> <strong>and</strong> regional<br />
bra<strong>in</strong> atrophy <strong>in</strong> amyotrophic lateral sclerosis. AJNR Am J Neuroradiol 2007;<br />
28:255–259.<br />
46 Chang JL, Lomen-Hoerth C, Murphy J, et al. A voxel-based morphometry study<br />
of patterns of bra<strong>in</strong> atrophy <strong>in</strong> ALS <strong>and</strong> ALS/FTLD. Neurology 2005; 65:75–<br />
80.<br />
47 Lule D, Diekmann V, Anders S, et al. Bra<strong>in</strong> responses to emotional stimuli <strong>in</strong><br />
patients with amyotrophic lateral sclerosis (ALS). J Neurol 2007; 254:519–<br />
527.<br />
48 Palmieri A, Naccarato M, Abrahams S, et al. Right hemisphere dysfunction<br />
<strong>and</strong> emotional process<strong>in</strong>g <strong>in</strong> ALS: an fMRI study. J Neurol 2010; Jul 1 [Epub<br />
ahead of pr<strong>in</strong>t].<br />
Copyright © Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohibited.