Validation of Addenbrooke's cognitive examination for detecting ...
Validation of Addenbrooke's cognitive examination for detecting ...
Validation of Addenbrooke's cognitive examination for detecting ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
PSY-06255; No <strong>of</strong> Pages 4<br />
<strong>Validation</strong> <strong>of</strong> <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> <strong>for</strong> <strong>detecting</strong> early dementia in a<br />
Japanese population<br />
Hidenori Yoshida, Seishi Terada ⁎, Hajime Honda, Toshie Ata, Naoya Takeda, Yuki Kishimoto, Etsuko Oshima,<br />
Takeshi Ishihara, Shigetoshi Kuroda<br />
Department <strong>of</strong> Neuropsychiatry, Okayama University Graduate School <strong>of</strong> Medicine, Dentistry and Pharmaceutical Sciences, 2-5-1 Shikata-cho, Okayama 700-8558, Japan<br />
article info<br />
Article history:<br />
Received 15 January 2008<br />
Received in revised <strong>for</strong>m 16 May 2009<br />
Accepted 11 June 2009<br />
Available online xxxx<br />
Keywords:<br />
Addenbrooke<br />
ACE<br />
Dementia<br />
Cognitive evaluation<br />
Japanese<br />
1. Introduction<br />
abstract<br />
Early detection <strong>of</strong> dementia is an important challenge <strong>for</strong> the<br />
physician, especially since the introduction <strong>of</strong> disease-modifying<br />
treatments. Screening <strong>for</strong> early dementia requires a sensitive instrument<br />
<strong>for</strong> assessment <strong>of</strong> cognition. The Mini-Mental State Examination<br />
(MMSE) is a widely used cognition screening test in many parts <strong>of</strong> the<br />
world (Folstein et al., 1975). However, it has limitations in screening<br />
multiple <strong>cognitive</strong> domains and <strong>detecting</strong> early dementia (Teng et al.,<br />
1987; Naugle and Kawczak, 1989; Feher et al., 1992). <strong>Addenbrooke's</strong><br />
<strong>cognitive</strong> <strong>examination</strong> (ACE) has been proposed as a simple and<br />
effective instrument to detect dementia (Mathuranath et al., 2000).<br />
Besides, it has been validated in the following languages: Malayalam<br />
(Mathuranath et al., 2004), French (Bier et al., 2005), Spanish (García-<br />
Caballero et al., 2006), German (Alexopoulos et al., 2006), and Danish<br />
(Stokholm et al., 2009). Moreover, a revised version <strong>of</strong> ACE (ACE-R)<br />
has recently been made available (Mioshi et al., 2006). Here, we report<br />
our experience with this test and show that the Japanese ACE is<br />
effective in <strong>detecting</strong> dementia in a Japanese-speaking population.<br />
2. Methods<br />
2.1. The instrument<br />
The ACE was translated into Japanese with some adaptations concerning the nameand<br />
address-learning and delayed recall tests, verbal fluency test, word and sentence<br />
repetition tests, and reading tests (Table 1). In the tests <strong>of</strong> repetition, word reading and<br />
⁎ Corresponding author. Tel.: +81 86 235 7242; fax: +81 86 235 7246.<br />
E-mail address: terada@cc.okayama-u.ac.jp (S. Terada).<br />
0165-1781/$ – see front matter © 2009 Elsevier Ireland Ltd. All rights reserved.<br />
doi:10.1016/j.psychres.2009.06.012<br />
ARTICLE IN PRESS<br />
Psychiatry Research xxx (2009) xxx–xxx<br />
Contents lists available at ScienceDirect<br />
Psychiatry Research<br />
journal homepage: www.elsevier.com/locate/psychres<br />
There is a clear need <strong>for</strong> brief, but sensitive and specific, <strong>cognitive</strong> screening instruments <strong>for</strong> dementia. We<br />
assessed the diagnostic accuracy <strong>of</strong> the Japanese version <strong>of</strong> <strong>Addenbrooke's</strong> Cognitive Examination (ACE) in<br />
identifying early dementia in comparison with the conventional Mini-Mental State Examination (MMSE).<br />
Standard tests <strong>for</strong> evaluating dementia screening tests were applied. A total <strong>of</strong> 201 subjects (Alzheimer's<br />
disease (AD)=65, frontotemporal dementia (FTD)=24, vascular dementia=26, dementia with Lewy<br />
bodies =11, mild <strong>cognitive</strong> impairment (MCI)=13, and controls=62) participated in this study. The<br />
reliability <strong>of</strong> the ACE was very good (alpha coefficient=0.82). In our patient series, the sensitivity <strong>for</strong><br />
diagnosing dementia with an ACE score <strong>of</strong> ≤74 was 0.889 with a specificity <strong>of</strong> 0.987, and the sensitivity <strong>of</strong> an<br />
ACE score <strong>of</strong> ≤80 was 0.984 with a specificity <strong>of</strong> 0.867. The Japanese version <strong>of</strong> the ACE is a very accurate<br />
instrument <strong>for</strong> the detection <strong>of</strong> early dementia, and should be widely used in clinical practice.<br />
© 2009 Elsevier Ireland Ltd. All rights reserved.<br />
name and address recall, replacement with words <strong>of</strong> equivalent frequency and syllable<br />
length in Japanese were made. On verbal fluency test, words beginning with the<br />
letter ‘p’ were replaced by words beginning with the syllable ‘sa’ because the Japanese<br />
language is based on syllables rather than letters. Thereafter, a bilingual expert not<br />
familiar with the original ACE translated it back into English. The retranslated version<br />
was very similar to the original one.<br />
2.2. Subjects<br />
We administered the ACE to 126 consecutive patients who had been referred to the<br />
Memory Clinic <strong>of</strong> Okayama University Hospital and who had been diagnosed with<br />
Alzheimer's disease (AD), vascular dementia (VaD), frontotemporal dementia (FTD), or<br />
dementia with Lewy bodies (DLB) (Table 2). Sixty-two subjects who had no evidence <strong>of</strong><br />
organic dementing disorders or psychiatric diseases (30 men, 32 women; age range, 40–<br />
80 years; mean age, 66.7±10.1 years) and 13 subjects with a Clinical Dementia Rating<br />
(CDR) score <strong>of</strong> 0.5 without overt dementia who were recognized as having mild <strong>cognitive</strong><br />
impairment (MCI) (six men, seven women; age range, 43–83 years; mean age,<br />
62.7 ±12.3 years) (Table 2) wereusedasacontrolgroups.<br />
Sixty-five outpatients were diagnosed with AD (17 men, 48 women; age range,<br />
46–87 years; mean age, 74.1 ± 7.8 years), 24 with FTD (13 men, 11 women; age<br />
range, 48–77 years; mean age, 61.8 ± 9.1 years), 26 with VaD (18 men, eight<br />
women; age range, 57–87 years; mean age, 73.4 ± 9.8 years), and 11 patients with<br />
DLB (three men, eight women; age range, 67–87 years; mean age, 62.9 ± 8.1 years).<br />
All patients with dementia had a dementia severity <strong>of</strong> 0.5 (suspicious) or 1 (mild)<br />
based on the CDR (Hughes et al., 1982). All patients underwent general physical and<br />
neurological <strong>examination</strong>s and extensive laboratory testing, including thyroid function tests,<br />
serum vitamin B12, and syphilis serology, to exclude other potential causes <strong>of</strong> dementia. All<br />
individuals and/or the nearest relative <strong>of</strong> the patient gave in<strong>for</strong>med written consent.<br />
The pr<strong>of</strong>ile <strong>of</strong> each patient (age, sex, years <strong>of</strong> education, and years <strong>of</strong> disease<br />
duration) was recorded, and the CDR score was rated by the chief clinician.<br />
2.3. Diagnosis<br />
All patients with AD met the criteria <strong>for</strong> probable AD <strong>for</strong>mulated by the National<br />
Institute <strong>of</strong> Neurological and Communicative Disorders and Stroke and the Alzheimer's<br />
Please cite this article as: Yoshida, H., et al., <strong>Validation</strong> <strong>of</strong> <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> <strong>for</strong> <strong>detecting</strong> early dementia in a Japanese<br />
population, Psychiatry Res. (2009), doi:10.1016/j.psychres.2009.06.012
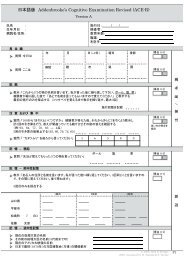
Table 1<br />
Comparison between the original and the adapted versions <strong>of</strong> the ACE.<br />
Item Original Adaptation<br />
Orientation Year, season, date, day, month Unchanged. appropriate japanese year accepted as correct response<br />
Country, county, town, hospital, floor Unchanged.<br />
Attention/calc. 100-7 up to five subtractions Unchanged<br />
saying “WORLD” backward Saying “fu-ji-no-ya-ma” backward<br />
Memory Lemon, key, ball Unchanged<br />
Seven-word address Seven-word address <strong>of</strong> local relevance<br />
Remote memory UK PM (current and previous) Japan (current and previous)<br />
UK (opposition leader), US (President) Japan (opposition leader), US (President)<br />
Verbal fluency Letter “p” and animal Letter “Sa” and animal<br />
Naming Pen, watch, giraffe, pig, crown, goat, camel, helicopter, kite,<br />
windmill, kangaroo, barrel<br />
Unchanged<br />
Language comprehension Read and obey and 1-stage, 3-stage and complex grammar Unchanged<br />
Repetition Brown, conversation, articulate Replaced with Japanese words <strong>of</strong> comparable frequency and length<br />
Phrases Replaced with Japanese phrase <strong>of</strong> comparable complexity and length<br />
Reading Regular words Replaced with “Kana” words <strong>of</strong> comparable frequency and word length<br />
Irregular words Replaced with “Kanji” words <strong>of</strong> comparable frequency and word length<br />
Visuospatial Overlapping pentagon, wire cube, clock-face drawing Unchanged<br />
Disease and Related Disorders Association (NINCDS-ADRDA) group (McKhann et al.,<br />
1984). All AD patients underwent head magnetic resonance imaging (MRI) and/or head<br />
computed tomography (CT). AD patients with evidence <strong>of</strong> stroke, as determined either by<br />
history or by imaging findings, were excluded. All patients with VaD met the criteria <strong>for</strong><br />
probable VaD <strong>for</strong>mulated by the National Institute <strong>of</strong> Neurological Disorders and Stroke<br />
and Association Internationale pour la Recherché et l'Enseignement en Neurosciences<br />
(NINDS-AIREN) group (Roman et al., 1993). All VaD subjects underwent head MRI and/or<br />
head CT, and had multiple lacunar infarcts <strong>of</strong> the basal gray matter and/or thalamus, in<br />
addition to periventricular and deep white matter lesions. FTD was diagnosed according to<br />
the international consensus criteria <strong>for</strong> frontotemporal lobar degeneration (FTLD) (Neary<br />
et al., 1998). No patient suited the criteria <strong>for</strong> semantic dementia or progressive nonfluent<br />
aphasia. All patients with DLB met the criteria <strong>for</strong> probable DLB <strong>for</strong>mulated by McKeith et<br />
al. (1996). All FTD and DLB patients underwent brain single-photon emission computed<br />
tomography (SPECT) as well as head CT and/or head MRI.<br />
2.4. Reliability<br />
Inter-rater reliability was then evaluated by intraclass correlation coefficient (ICC)<br />
on 20 consecutive patients admitted in our psychiatric department. Two investigators<br />
evaluated patients at the same time but were blind to each other. Ten patients were<br />
actively evaluated by one <strong>of</strong> them while the other passively observed, and their roles<br />
were reversed <strong>for</strong> the other 10.<br />
The internal consistency reliability within the ACE was assessed using Cronbach's<br />
coefficient alpha (Cronbach and Meehl, 1955).<br />
2.5. Statistical analysis<br />
Statistical analysis was per<strong>for</strong>med using the SPSS 14.0 J s<strong>of</strong>tware program (SPSS<br />
Inc., Chicago, IL, USA). A value <strong>of</strong> Pb0.05 was accepted as significant.<br />
3. Results<br />
Table 2 summarizes the socio-demographic characteristics and<br />
scores on the ACE and MMSE <strong>for</strong> dementia and control groups in the<br />
complete sample.<br />
Inter-rater reliabilities <strong>of</strong> the ACE and MMSE were evaluated with<br />
ICC <strong>of</strong> 0.994 and 0.986, respectively. The reliability <strong>of</strong> the ACE was<br />
Table 2<br />
Epidemiological data<br />
n M/F Age Education CDR ACE MMSE<br />
0 0.5 1<br />
Normal 62 30/32 66.7±10.1 12.3±3.6 62 0 0 88.1±4.3 29.0 ±1.1<br />
MCI 13 6/7 62.7 ±12.3 11.2±1.7 0 13 0 82.6 ±6.9 27.2±2.1<br />
AD 65 17/48 74.1±7.8 10.1±2.4 0 25 40 63.3 ±7.8 21.7±2.9<br />
FTD 24 13/11 61.8±9.1 12.4±2.5 0 4 20 61.8±16.0 22.5 ±4.9<br />
DLB 11 3/8 75.5 ±5.0 9.8±2.4 0 3 8 62.9 ±8.1 22.8 ±2.8<br />
VaD 26 18/8 73.4 ±9.8 9.9±3.0 0 13 13 64.8±7.9 22.6 ±2.8<br />
M/F; male/female, age; years ±S.D., education; years±S.D., MMSE, ACE; mean score±<br />
S.D.<br />
MCI; mild <strong>cognitive</strong> impairment, AD; Alzheimer's disease, FTD; frontotemporal<br />
dementia.<br />
DLB; dementia with Lewy bodies, VaD; vascular dementia.<br />
ARTICLE IN PRESS<br />
2 H. Yoshida et al. / Psychiatry Research xxx (2009) xxx–xxx<br />
measured in terms <strong>of</strong> internal consistency, using Cronbach's alpha<br />
coefficient. The Cronbach's alpha <strong>for</strong> the ACE was 0.82.<br />
Two methods were used to calculate the norms <strong>for</strong> the composite<br />
score on the ACE. The first ACE cut<strong>of</strong>f score <strong>of</strong> 80/100 represented a<br />
value two standard deviations (S.D.s) below the mean composite<br />
score <strong>for</strong> the control group. The second cut<strong>of</strong>f was obtained by<br />
estimating the probability <strong>of</strong> diagnosing dementia in the 202 subjects<br />
in the clinic group. We estimated the sensitivity, specificity, and<br />
positive predictive values (PPVs) <strong>for</strong> diagnosing dementia at different<br />
prevalence rate (5, 19, 20, and 40%) <strong>for</strong> each ACE cut<strong>of</strong>f score from 70<br />
to 80. A broad range <strong>of</strong> prevalence rates was chosen to encompass the<br />
wide variation reported in various studies. A cut<strong>of</strong>f <strong>of</strong> 80 had high<br />
sensitivity (98%) at a specificity <strong>of</strong> 87% (Table 3). A cut<strong>of</strong>f score <strong>of</strong> 74<br />
had optimal sensitivity (89%) and specificity (99%), and maintained a<br />
reasonably high PPV at different prevalence rates. Table 3 also shows<br />
the sensitivity, specificity, and predictive values <strong>for</strong> diagnosing<br />
dementia using the MMSE with a conventional cut<strong>of</strong>f <strong>of</strong> 24 and a<br />
higher cut<strong>of</strong>f <strong>of</strong> 27 <strong>for</strong> the same sample population.<br />
DSM-IV was used to estimate the criterion validity <strong>of</strong> the ACE<br />
(composite score) in diagnosing dementia. The trade-<strong>of</strong>f between<br />
sensitivity and 1-specificity <strong>of</strong> the ACE and MMSE in diagnosing<br />
dementia is shown in the receiver operating characteristics (ROC)<br />
curve in Fig. 1. The area under the ROC curve (AUC) <strong>of</strong> the ACE was<br />
0.987 and <strong>of</strong> the MMSE was 0.963.<br />
Among the dementia group, the sensitivity and specificity <strong>for</strong><br />
diagnosing FTD with a Verbal-Language/Orientation Memory (VLOM)<br />
ratio b2.2 was 16.7% and 96.1%, and the sensitivity and specificity <strong>for</strong><br />
diagnosing AD with a VLOM ratio N3.2 was 84.6% and 60.7%.<br />
4. Discussion<br />
4.1. Japanese version <strong>of</strong> ACE<br />
This study was per<strong>for</strong>med to evaluate the Japanese version <strong>of</strong> the<br />
ACE in <strong>detecting</strong> early dementia. We compared the validity <strong>of</strong> the ACE<br />
Table 3<br />
Sensitivity and specificity <strong>of</strong> different ACE and MMSE cut<strong>of</strong>f scores <strong>for</strong> diagnosing<br />
dementia, with corresponding probabilities <strong>of</strong> dementia (PPV) at different rates <strong>of</strong><br />
prevalence.<br />
Test Cut<strong>of</strong>f Dementia PPV at different base rates<br />
score Sensitivity Specificity 5% 10% 20% 40%<br />
ACE 80/81 0.98 0.87 0.28 0.45 0.65 0.83<br />
74/75 0.89 0.99 0.78 0.88 0.94 0.98<br />
MMSE 27/28 0.95 0.83 0.22 0.38 0.58 0.79<br />
24/25 0.76 0.97 0.60 0.76 0.88 0.95<br />
Please cite this article as: Yoshida, H., et al., <strong>Validation</strong> <strong>of</strong> <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> <strong>for</strong> <strong>detecting</strong> early dementia in a Japanese<br />
population, Psychiatry Res. (2009), doi:10.1016/j.psychres.2009.06.012
Fig. 1. ACE and MMSE ROC curves <strong>for</strong> the detection <strong>of</strong> patients with dementia.<br />
with the validity <strong>of</strong> the MMSE, which is a short test with widespread<br />
international usage. We compared the diagnostic accuracy <strong>of</strong> the tests<br />
not only with regard to sensitivity and specificity, but also with regard<br />
to AUC. The AUC is independent <strong>of</strong> the decision criteria and less<br />
contaminated by the external factors that affect the response<br />
(Alexopoulos et al., 2006). Thus, the AUC provides a better measure<br />
<strong>of</strong> predictive accuracy than the measurement's sensitivity and<br />
specificity (Kim et al., 2005).<br />
According to our findings, the Japanese ACE has excellent accuracy in<br />
differentiating between patients with early dementia and <strong>cognitive</strong>ly<br />
healthy participants. The ACE has good sensitivity and specificity in<br />
<strong>detecting</strong> early dementia. The AUC value <strong>of</strong> the ACE <strong>for</strong> identifying early<br />
dementia was 0.987. This value indicates excellent accuracy.<br />
4.2. Difference between scores in the original ACE and Japanese ACE<br />
(Table 4)<br />
The two cut<strong>of</strong>f values <strong>for</strong> the original ACE were 88 and 83<br />
(Mathuranath et al., 2000), while those <strong>for</strong> the Japanese ACE<br />
composite were 80 and 74. Where does the difference come from?<br />
Table 4 summarizes the mean individual component and composite<br />
scores on the ACE <strong>for</strong> the <strong>cognitive</strong>ly normal groups <strong>of</strong> the original<br />
study and this study. Exact statistical analysis cannot be conducted,<br />
but the control group in this study had lower scores on memory and<br />
verbal components than the control group in the original study. Tests<br />
<strong>of</strong> both memory and verbal components include tests use language.<br />
The Indo-European languages including English are written in letters,<br />
whereas the Japanese language is written in syllables. A “seven-word<br />
address” in the memory component <strong>of</strong> the Japanese version <strong>of</strong> the<br />
ACE might be more difficult than that in the original ACE. In the<br />
verbal fluency test also, the difference between letters and syllables<br />
Table 4<br />
Difference <strong>of</strong> scores between the original ACE and the Japanese ACE.<br />
might affect the results. In English, the alphabet consists <strong>of</strong> 26<br />
letters, whereas in Japanese, the “kana” writing system consists <strong>of</strong> 46<br />
syllables. The number <strong>of</strong> words beginning with letter “p” might be<br />
bigger than the number <strong>of</strong> words beginning with the syllable “sa”, and<br />
there<strong>for</strong>e, saying words beginning with the syllable “sa” might be a<br />
more difficult task than saying words beginning with the letter “p”.<br />
4.3. VLOM ratio (Table 5)<br />
We found that a VLOM ratio N3.2 indicated a better sensitivity in<br />
<strong>detecting</strong> AD than reported by Mathuranath et al. (84.6% versus 75%),<br />
but showed lower specificity (60.7% versus 84%) (Mathuranath et al.,<br />
2000) (Table 5).<br />
The major discordant finding in this study is the complete failure <strong>of</strong><br />
the ACE to detect FTD. In fact, only 16.7% <strong>of</strong> FTD cases had a VLOM ratio<br />
b2.2. Our result is in line with that <strong>of</strong> Bier et al. (2004). The VLOM ratio<br />
is the ratio between scores in language tasks and memory tasks. A<br />
lower VLOM ratio indicates a specificdeficit in language rather than in<br />
memory functions. In our dementia group, we had no case <strong>of</strong> primary<br />
progressive aphasia or semantic dementia among our FTD patients,<br />
who all presented with the pure frontal <strong>for</strong>m <strong>of</strong> the disease. We agree<br />
with the opinion <strong>of</strong> Bier et al. and think that a low (b2.2) VLOM ratio<br />
may be effective in diagnosing the <strong>for</strong>ms <strong>of</strong> FTLD with a selective<br />
language deficit.<br />
4.4. Limitations <strong>of</strong> this study<br />
Our study has several limitations. The participants were recruited<br />
at a university center. Thus, our results apply only to a clinic-based<br />
patient population. The applicability and reliability <strong>of</strong> the ACE in<br />
community samples require further investigation.<br />
We used the clinical diagnosis based on a comprehensive diagnostic<br />
workup and on international diagnostic criteria as the gold standard.<br />
Despite the high validity <strong>of</strong> the diagnostic criteria, clinical diagnoses are<br />
not always confirmed at autopsy. Thus, we should take into account the<br />
possibility <strong>of</strong> erroneous clinical assessments. There<strong>for</strong>e, the validity <strong>of</strong><br />
the ACE may be lower than our results suggest.<br />
5. Conclusion<br />
The Japanese version <strong>of</strong> the ACE is a very accurate instrument <strong>for</strong> the<br />
detection <strong>of</strong> early dementia, and should be widely used in clinical practice.<br />
n ACE MMSE Orientation Attention Memory Verbal Language Visuo⁎<br />
Mathuranath, et al. 127 93.8 ±3.5 29.1±0.8 9.8±0.3 7.8±0.4 32.6 ±1.9 11.0±2.2 27.8±0.5 4.6±0.5<br />
Yoshida, et al. 62 88.1±4.3 29.0 ±1.1 9.9±0.4 7.5±0.8 30.1±3.3 8.3 ±3.3 27.7±0.7 4.7±0.6<br />
Scores; mean ±S.D., visuo⁎; visuospatial.<br />
ARTICLE IN PRESS<br />
H. Yoshida et al. / Psychiatry Research xxx (2009) xxx–xxx<br />
Table 5<br />
VLOM ratio.<br />
n VLOM ratio<br />
b2.2 2.2−3.2 3.2b<br />
Normal 62 23 36 3<br />
MCI 13 0 10 3<br />
AD 65 1 9 55<br />
FTD 24 4 10 10<br />
DLB 11 2 8 1<br />
VaD 26 1 12 13<br />
MCI; mild <strong>cognitive</strong> impairment.<br />
AD; Alzheimer's disease.<br />
FTD; frontotemporal dementia.<br />
DLB; dementia with Lewy bodies.<br />
VaD; vascular dementia.<br />
Please cite this article as: Yoshida, H., et al., <strong>Validation</strong> <strong>of</strong> <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> <strong>for</strong> <strong>detecting</strong> early dementia in a Japanese<br />
population, Psychiatry Res. (2009), doi:10.1016/j.psychres.2009.06.012<br />
3
Acknowledgements<br />
We thank Ms. Ido, Ms. Imai and Ms. Yabe <strong>for</strong> their skillful assistance<br />
<strong>of</strong> this study. This work was supported by grants from the Japanese<br />
Ministry <strong>of</strong> Education, Culture, Sports, Science and Technology, and<br />
the Zikei Institute <strong>of</strong> Psychiatry.<br />
References<br />
Alexopoulos, P., Greim, B., Nadler, K., Martens, U., Krecklow, B., Domes, G., Herpertz, S.,<br />
Kurz, A., 2006. <strong>Validation</strong> <strong>of</strong> the <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> <strong>for</strong> <strong>detecting</strong><br />
early Alzheimer's disease and mild vascular dementia in a German population.<br />
Dementia and Geriatric Cognitive Disorders 22, 385–391.<br />
Bier, J.C., Ventura, M., Donckels, V., Van Eyll, E., Claes, T., Slama, H., Fery, P., Vokaer, M.,<br />
Pandolfo, M., 2004. Is the <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> effective to detect<br />
frontotemporal dementia? Journal <strong>of</strong> Neurology 251, 428–431.<br />
Bier, J.C., Donckels, V., Van Eyll, E., Claes, T., Slama, H., Fery, P., Vokaer, M., 2005. The<br />
French <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> is effective in <strong>detecting</strong> dementia in a<br />
French-speaking population. Dementia and Geriatric Cognitive Disorders 19, 15–17.<br />
Cronbach, L., Meehl, P., 1955. Construct validity in psychological tests. Psychological<br />
Bulletin 52, 281–302.<br />
Feher, E.P., Mahurin, R.K., Doody, R.S., Cooke, N., Sims, J., Pirozzolo, F.J., 1992. Establishing<br />
the limits <strong>of</strong> the Mini-Mental State. Examination <strong>of</strong> ‘subtests’. Archieves <strong>of</strong><br />
Neurology 49, 87–92.<br />
Folstein, M.F., Folstein, S.E., McHugh, P.R., 1975. Mini-Mental State: a practical method<br />
<strong>for</strong> grading the <strong>cognitive</strong> state <strong>of</strong> patients <strong>for</strong> the clinician. Journal <strong>of</strong> Psychiatric<br />
Research 12, 189–198.<br />
García-Caballero, A., García-Lado, I., González-Hermida, J., Recimil, M., Area, R., Manes, F.,<br />
Lamas, S., Berrios, G., 2006. <strong>Validation</strong> <strong>of</strong> the Spanish version <strong>of</strong> the <strong>Addenbrooke's</strong><br />
Cognitive Examination in a rural community in Spain. International Journal <strong>of</strong><br />
Geriatric Psychiatry 21, 239–245.<br />
Hughes, C.P., Berg, L., Danziger, W.L., Coben, L.A., Martin, R.L., 1982. A new clinical scale<br />
<strong>for</strong> the staging <strong>of</strong> dementia. British Journal <strong>of</strong> Psychiatry 140, 566–572.<br />
Kim, K.W., Lee, D.Y., Jhoo, J.H., Youn, J.C., Suh, Y.J., Jun, Y.H., Seo, E.H., Woo, J.I., 2005.<br />
Diagnostic accuracy <strong>of</strong> Mini-Mental Status Examination and Revised Hasegawa<br />
Dementia Scale <strong>for</strong> Alzheimer's disease. Dementia and Geriatric Cognitive<br />
Disorders 19, 324–330.<br />
ARTICLE IN PRESS<br />
4 H. Yoshida et al. / Psychiatry Research xxx (2009) xxx–xxx<br />
Mathuranath, P.S., Nestor, P.J., Berrios, G.E., Rakowicz, W., Hodges, J.R., 2000. A brief<br />
<strong>cognitive</strong> test battery to differentiate Alzheimer's disease and frontotemporal<br />
dementia. Neurology 55, 1613–1620.<br />
Mathuranath, P.S., Hodges, J.R., Mathew, R., Cherian, P.J., George, A., Bak, T.H., 2004.<br />
Adaptation <strong>of</strong> the ACE <strong>for</strong> a Malayalam speaking population in southern India.<br />
International Journal <strong>of</strong> Geriatric Psychiatry 19, 1188–1194.<br />
McKeith, I.G., Galasko, D., Kosaka, K., Perry, E.K., Dickson, D.W., Hansen, L.A., Salmon, D.P.,<br />
Lowe, J., Mirra, S.S., Byrne, E.J., Lennox, G., Quinn, N.P., Edwardson, J.A., Ince, P.G.,<br />
Bergeron, C., Burns, A., Miller, B.L., Lovestone, S., Collerton, D., Jansen, E.N., Ballard, C.,<br />
de Vos, R.A., Wilcock, G.K., Jellinger, K.A., Perry, R.H., 1996. Consensus guidelines <strong>for</strong><br />
the clinical and pathological diagnosis <strong>of</strong> dementia with Lewy bodies (DLB). Report<br />
<strong>of</strong> the Consortium on DLB International Workshop. Neurology 47, 1113–1124.<br />
McKhann, G., Drachman, D., Folstein, M., Katzman, R., Price, D., Stadlan, E.M., 1984.<br />
Clinical diagnosis <strong>of</strong> Alzheimer's disease: report <strong>of</strong> the NINCDS-ADRDA Work Group<br />
under the auspices <strong>of</strong> Department <strong>of</strong> Health and Human Services Task Force on<br />
Alzheimer's disease. Neurology 34, 939–944.<br />
Mioshi, E., Dawson, K., Mitchell, J., Arnold, R., Hodges, J.R., 2006. The Addenbrooke_s<br />
Cognitive Examination Revised (ACE-R): a brief <strong>cognitive</strong> test battery <strong>for</strong> dementia<br />
screening. International Journal <strong>of</strong> Geriatric Psychiatry 21, 1078–1085.<br />
Naugle, R.I., Kawczak, K., 1989. Limitations <strong>of</strong> the Mini-Mental State Examination.<br />
Cleveland Clinical Journal <strong>of</strong> Medicine 56, 277–281.<br />
Neary, D., Snowden, J.S., Gustafson, L., Passant, U., Stuss, D., Black, S., Freedman, M.,<br />
Kertesz, A., Robert, P.H., Albert, M., Boone, K., Miller, B.L., Cummings, J., Benson, D.F.,<br />
1998. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria.<br />
Neurology 51, 1546–1554.<br />
Roman, G.C., Tatemichi, T.K., Erkinjuntti, T., Cummings, J.L., Masdeu, J.C., Garcia, J.H.,<br />
Amaducci, L., Orgogozo, J.M., Brun, A., H<strong>of</strong>man, A., Moody, D.M., O'Brien, M.D.,<br />
Yamaguchi, T., Grafman, J., Drayer, B.P., Bennett, D.A., Fisher, M., Ogata, J., Kokmen,<br />
E., Bermejo, F., Wolf, P.A., Gorelick, P.B., Bick, K.L., Pajeau, A.K., Bell, M.A., DeCarli, C.,<br />
Culebras, A., Korczyn, A.D., Bogousslavsky, J., Hartmann, A., Scheinberg, P., 1993.<br />
Vascular dementia: diagnostic criteria <strong>for</strong> research studies. Report on the NINDS–<br />
AIREN International Work Group. Neurology 43, 250–260.<br />
Stokholm, J., Vogel, A., Johannsen, P., Waldemar, G., 2009. <strong>Validation</strong> <strong>of</strong> the Danish<br />
<strong>Addenbrooke's</strong> Cognitive Examination as a screening test in a memory clinic.<br />
Dement and Geriatric Cognitive Disorders 27, 361–365.<br />
Teng, E.L., Chui, H.C., Teng, E.L., Chui, H.C., 1987. The Modified Mini-Mental State (3MS)<br />
Examination. Journal <strong>of</strong> Clinical Psychiatry 48, 314–318.<br />
Please cite this article as: Yoshida, H., et al., <strong>Validation</strong> <strong>of</strong> <strong>Addenbrooke's</strong> <strong>cognitive</strong> <strong>examination</strong> <strong>for</strong> <strong>detecting</strong> early dementia in a Japanese<br />
population, Psychiatry Res. (2009), doi:10.1016/j.psychres.2009.06.012