Behavioural-variant frontotemporal dementia: diagnosis, clinical ...
Behavioural-variant frontotemporal dementia: diagnosis, clinical ...
Behavioural-variant frontotemporal dementia: diagnosis, clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Review<br />
Lancet Neurol 2011; 10: 162–72<br />
Published Online<br />
December 13, 2010<br />
DOI:10.1016/S1474-<br />
4422(10)70299-4<br />
Neuroscience Research<br />
Australia, Randwick, NSW,<br />
Australia (O Piguet PhD,<br />
M Hornberger PhD,<br />
E Mioshi PhD,<br />
Prof J R Hodges FMedSci)<br />
Correspondence to:<br />
Prof John Hodges, Neuroscience<br />
Research Australia, Barker St,<br />
Randwick, NSW 2031, Australia<br />
j.hodges@neura.edu.au<br />
<strong>Behavioural</strong>-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>: <strong>diagnosis</strong>,<br />
<strong>clinical</strong> staging, and management<br />
Olivier Piguet, Michael Hornberger, Eneida Mioshi, John R Hodges<br />
Patients with behavioural-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong> (bvFTD) present with insidious changes in personality<br />
and interpersonal conduct that indicate progressive disintegration of the neural circuits involved in social cognition,<br />
emotion regulation, motivation, and decision making. The underlying pathological changes are heterogeneous and<br />
are characterised by various intraneuronal inclusions. Biomarkers to detect these histopathological changes in life are<br />
becoming increasingly important with the development of disease-modifying drugs. Gene mutations have been<br />
found that collectively account for around 10–20% of cases. Recently, criteria proposed for bvFTD defi ne three levels<br />
of diagnostic certainty: possible, probable, and defi nite. Detailed history taking from family members to elicit<br />
behavioural features underpins the diagnostic process, with support from neuropsychological testing designed to<br />
detect impairment in decision making, emotion processing, and social cognition. Brain imaging is important for<br />
increasing the level of diagnostic certainty. A recently developed staging instrument shows much promise for<br />
monitoring patients and evaluating therapies, which at present are aimed at symptom amelioration. Carer education<br />
and support remain of paramount importance.<br />
Introduction<br />
Frontotemporal <strong>dementia</strong> (FTD) is the <strong>clinical</strong> diagnostic<br />
term now preferred to describe patients with a range of<br />
progressive <strong>dementia</strong> syndromes associated with focal<br />
atrophy of the orbitomesial frontal and anterior temporal<br />
lobes. 1 Epidemiological studies suggest that FTD is the<br />
second most common cause of young-onset <strong>dementia</strong><br />
after Alzheimer’s disease (AD). 2,3 Two independent<br />
studies from the UK revealed a prevalence of around 15<br />
cases per 100 000 population aged 45–64 years (95% CI<br />
8–27 per 100 000). 2 Although thought to be a rare cause<br />
of <strong>dementia</strong> after age 65 years, FTD might be more<br />
common than assumed because older adults rarely<br />
undergo the types of investigation needed to establish a<br />
confi dent <strong>diagnosis</strong> in vivo and are not generally followed<br />
to autopsy.<br />
Unlike AD, both the <strong>clinical</strong> profi le and the underlying<br />
pathological changes are heterogeneous in FTD. Two<br />
broad presentations are recognised: progressive<br />
deterioration in social function and personality, known<br />
as behavioural-<strong>variant</strong> FTD (bvFTD), and insidious<br />
decline in language skills, known as primary progressive<br />
aphasia, which can, in turn, be subdivided according the<br />
predominant pattern of language breakdown into<br />
progressive non-fl uent aphasia and semantic <strong>dementia</strong>. 4–6<br />
The syndrome of FTD overlaps with motor neuron<br />
disease (MND) both <strong>clinical</strong>ly and pathologically, and<br />
with some of the extrapyramidal motor disorders. Around<br />
10% of patients with FTD develop <strong>clinical</strong> and<br />
neurophysiological evidence of MND, 7,8 and, similarly,<br />
patients with MND show behavioural and/or language<br />
changes that, in some instances, are severe enough to<br />
qualify for a <strong>diagnosis</strong> of FTD. 9 Of the extrapyramidal<br />
disorders, corticobasal degeneration and progressive<br />
supranuclear palsy show substantial overlap with FTD<br />
and share the fi nding of abnormal tau pathology. 10<br />
This is a broad and rapidly evolving fi eld; therefore, in<br />
this Review, we have focused on the <strong>clinical</strong> aspects of<br />
bvFTD because there have been recent authoritative<br />
reviews of the aphasic syndromes. 4,6 Our aim is to place<br />
advances in the <strong>diagnosis</strong>, staging, and management of<br />
bvFTD within the context of recent pathological and<br />
genetic discoveries. The assessment of any patient with<br />
suspected bvFTD should involve behavioural and<br />
neuropsychiatric tests, assessment of everyday abilities,<br />
cognitive testing, and neuroimaging. Various blood and<br />
CSF biomarkers are under development, but are not yet<br />
available for routine <strong>clinical</strong> application. Genetic testing<br />
is advised for those at high risk of a gene mutation<br />
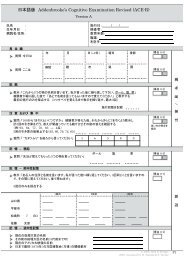
(fi gure 1). 11<br />
Pathology<br />
The subtypes of underlying pathological changes in<br />
patients with FTD are classifi ed on the basis of the<br />
pattern of protein accumulation, and are referred to<br />
collectively as <strong>frontotemporal</strong> lobar degeneration<br />
(FTLD). 12 At post mortem, cases share, by defi nition, the<br />
fi nding of bilateral <strong>frontotemporal</strong> atrophy with<br />
neuronal loss, microvacuolation, and a variable degree<br />
of astrocytic gliosis. The progression of this atrophy has<br />
been examined by mapping the pattern in patients with<br />
diff erent disease duration. 13 Initially, mesial and orbital<br />
frontal regions bear the brunt of the atrophy, followed<br />
by the temporal pole, hippocampal formation,<br />
dorsolateral frontal cortex, and the basal ganglia. This<br />
pattern of progression of atrophy has been shown to<br />
relate to the volume of cortical and subcortical regions,<br />
and to the underlying neuron loss. 14,15 Furthermore, it<br />
forms the basis of a useful and quick MRI rating scale<br />
described below.<br />
The use of immunohistochemical staining has<br />
revolutionised the fi eld of research in FTD. Inclusions of<br />
the microtubule-binding protein tau are present in<br />
approximately 40% of cases (FTLD-tau). 16 Tau-positive<br />
cases include the subset of patients with mutations in the<br />
microtubule-associated protein tau (MAPT) gene. Further<br />
162 www.thelancet.com/neurology Vol 10 February 2011
Possible phenocopy<br />
Possible bvFTD based on <strong>clinical</strong>, behavioural,<br />
cognitive, and ADL assessments*<br />
MRI<br />
Abnormal<br />
PET Probable bvFTD<br />
Normal<br />
Normal<br />
Abnormal<br />
Strong family history<br />
Figure 1: Possible investigations after the <strong>diagnosis</strong> of suspected bvFTD<br />
based on <strong>clinical</strong> assessment<br />
*Presence of neurodegenerative disease and at least three of six behavioural or<br />
cognitive core diagnostic criteria are required for <strong>diagnosis</strong> of the disease.<br />
bvFTD=behavioural-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>. ADL=activities of<br />
daily living.<br />
subclassifi cation is based on morphological criteria and<br />
the predominance of either tau with three microtubulebinding<br />
repeats (3R tau) or four microtubule-binding<br />
repeats (4R tau). 12 Most of the remaining cases are tau<br />
negative and ubiquitin positive, and have inclusions<br />
comprising the 43 kDa TAR DNA-binding protein (TDP-43;<br />
FTLD-TDP), but a minority (around 5–10%) are negative<br />
for both tau and TDP-43 proteins. 17 Recently, inclusions of<br />
the RNA-binding protein fused in sarcoma (FUS) have<br />
been found in many of these cases (FTLD-FUS). 16,18 The<br />
search for FUS pathology was initiated after FUS gene<br />
mutations were identifi ed in cases of familial MND. 19,20<br />
Both TDP-43 and FUS are RNA-processing proteins,<br />
although the mechanisms leading to TDP-43 and FUS<br />
accumulation and resulting neurodegeneration have not<br />
yet been elucidated. A small proportion of cases have<br />
either no inclusions or show ubiquitin-positive inclusions<br />
that are TDP-43 and FUS negative, suggesting that<br />
additional protein abnormalities will be found in FTLD. 16<br />
A major topic of investigation has been to establish the<br />
association between <strong>clinical</strong> phenotypes and molecular<br />
pathology. Unlike the progressive aphasic syndromes,<br />
which are generally associated more with one histological<br />
form of FTLD than another (progressive non-fl uent<br />
aphasia with FTLD-tau, semantic <strong>dementia</strong> with<br />
FTLD-TDP), in bvFTD any of the histological <strong>variant</strong>s<br />
can be found with an approximately 50:50 split between<br />
FTLD-tau and FTLD-TDP, 21–23 and a small proportion of<br />
FTLD-FUS cases. 24 With the advent of potential diseasemodifying<br />
therapies, ascertainment of a pathological<br />
<strong>diagnosis</strong> in vivo will be increasingly important. As yet,<br />
no reliable method for detecting these pathological<br />
changes in life exists. CSF biomarkers seem to be the<br />
most promising in distinguishing FTLD from AD: the<br />
ratio of tau to amyloid β 1–42 has been found to be lower in<br />
FTLD than in AD. 25 Increased concentrations of<br />
Yes<br />
Genetic screening<br />
CSF TDP-43 have also been reported in patients with<br />
MND and FTD, but without pathological confi rmation of<br />
the <strong>diagnosis</strong>. In addition, the substantial overlap<br />
between cases and controls limits the applicability of the<br />
assay in <strong>clinical</strong> practice. 26 Serum progranulin<br />
concentrations are exceptionally low in patients with<br />
mutations in the granulin gene (GRN), 27–29 and this assay<br />
seems to be a sensitive and specifi c method of screening<br />
for such cases, 30 with suggestions that plasma TDP-43<br />
concentrations could be related to brain pathology. 31<br />
Neuroimaging markers are discussed below.<br />
Genetics<br />
Up to 40% of patients with FTD have a family history<br />
of <strong>dementia</strong>, 3 but the high community prevalence of<br />
non-FTD <strong>dementia</strong> means that many of the elderly family<br />
members included in such estimates almost certainly<br />
have other causes of <strong>dementia</strong>. Patients with an autosomal<br />
dominant pattern (aff ected fi rst-degree relatives across<br />
two generations) account for only 10% of cases. 11 The<br />
strength of family history is highly predictive, in that<br />
mutations can now be shown in most patients with two<br />
or more fi rst-degree relatives with a <strong>dementia</strong> syndrome<br />
compatible with FTD. 11 Overall, patients with mutations<br />
in MAPT and GRN each account for 5–11% of total FTD<br />
cases. 11 Mutations in the gene that encodes TDP-43,<br />
TARDBP, and in FUS, recognised as a cause of familial<br />
amyotrophic lateral sclerosis (ALS), have also been<br />
identifi ed in a small number of cases of FTD-ALS, 32–35 but<br />
seem to be rare in uncomplicated FTD. 11 Rare genetic<br />
mutations causing FTD include those in the genes<br />
encoding valosin-containing protein (VCP) and charged<br />
multivesicular body protein 2B (CHMP2B; also known<br />
as chromatin-modifying protein 2B). Mutations in VCP<br />
cause FTD in association with inclusion body myopathy<br />
and Paget’s disease of bone, 36 whereas the CHMP2B gene<br />
mutation is mostly confi ned to a large Danish cohort<br />
with FTD. 37,38 Familial clusters of FTD and MND have<br />
been reported. A linkage study of FTD-MND clusters<br />
has indicated a common locus in the region of<br />
chromosome 9p13.2–21.3, 39 but the causative gene has<br />
not yet been identifi ed.<br />
From a practical perspective, a detailed family history<br />
should be taken for all patients with suspected FTD,<br />
bearing in mind the overlap between MND and FTD,<br />
that a <strong>diagnosis</strong> of FTD or Pick’s disease was rarely<br />
made in the past, and the phenotypic variability within<br />
families with gene mutations: one member might<br />
present with bvFTD, whereas others have a progressive<br />
aphasic syndrome or corticobasal syndrome. On the<br />
basis of a comprehensive analysis of the frequency of<br />
gene mutations according to strength of family history<br />
and <strong>clinical</strong> syndrome in a large <strong>clinical</strong> cohort, 31 we<br />
recommend that patients with one or more fi rst-degree<br />
relatives with a disease on the FTD spectrum should be<br />
screened for MAPT and GRN gene mutations after<br />
appropriate counselling in a <strong>clinical</strong> genetics setting.<br />
Review<br />
www.thelancet.com/neurology Vol 10 February 2011 163
Review<br />
Those with an informative family history that reveals no<br />
aff ected relatives can be confi dently reassured and need<br />
not undergo gene screening. 11 Of note, the age of onset<br />
in patients with MAPT mutations is almost always<br />
below 65 years, whereas those with GRN mutations are<br />
often older. 11<br />
<strong>Behavioural</strong> features<br />
Insidious changes in personality, interpersonal conduct,<br />
and emotional modulation characterise bvFTD and<br />
indicate progressive disintegration of the neural circuits<br />
involved in social cognition, emotion regulation,<br />
motivation, and decision making. 40–43 Onset is typically<br />
diffi cult to pinpoint. Since insight is limited, or absent, it<br />
is vital that close family members are interviewed alone,<br />
and sensitively, to elicit the nature of the early symptoms<br />
and their progression. Assessment and <strong>diagnosis</strong> have<br />
been greatly assisted by the development of carer-based<br />
questionnaires designed to document the range of<br />
symptoms found in the <strong>dementia</strong>, including the<br />
Neuropsychiatric Inventory, 44 Cambridge <strong>Behavioural</strong><br />
Inventory, 45 and Frontal <strong>Behavioural</strong> Inventory. 46 All of<br />
the features found in bvFTD can occur in other<br />
<strong>dementia</strong>s, but their predominance and early emergence<br />
typify bvFTD.<br />
Apathy is very common and manifests as inertia,<br />
reduced motivation, lack of interest in previous hobbies,<br />
and progressive social isolation. Disinhibition often<br />
coexists with apathy, and produces impulsive actions<br />
leading to overspending, tactless or sexually inappropriate<br />
remarks, and a range of socially embarrassing behaviour.<br />
New-onset pathological gambling or, more rarely, hyperreligiosity,<br />
can be the presenting feature. 47,48 Repetitive or<br />
stereotypic behaviours might be apparent with<br />
perseveration and a tendency to repeat phrases, stories,<br />
or jokes. Some carers describe excessive hoarding, which<br />
results in a state of squalor. Patients often lack empathy<br />
and an inappropriately subdued grief reaction is a<br />
common early symptom. Mental rigidity is common and<br />
patients can have diffi culty adapting to new situations or<br />
routines. A blunting of aff ect and reduction in range of<br />
emotional expression is frequent and some patients show<br />
elevation of mood resembling hypomania. Changes in<br />
eating behaviour, with impaired satiety, change in<br />
preferences towards sweet food, and dysregulation of<br />
food intake are common and seen across cultures. 49<br />
These alterations in eating have recently been found to<br />
be related to pathological changes in the hypothalamus,<br />
which is crucial for coordinating metabolic needs,<br />
including feeding. 50<br />
Psychotic symptoms such as delusions, paranoid<br />
ideation, and hallucinations are relatively rare in FTD,<br />
except in patients with combined MND and in patients<br />
with young-onset FTLD-FUS in whom such features are<br />
present in up to 50%. 7,51,52 Clinically, these patients seem<br />
to present with fl orid behavioural symptoms. In addition,<br />
their age of onset is often exceptionally young (≤40 years), 24<br />
and a positive family history seems rare in keeping with<br />
the absence of FUS gene mutations in this group. 24,52<br />
Patients destined to develop <strong>clinical</strong> MND who have<br />
FTLD-TDP also have a high rate of psychotic features<br />
and progress rapidly even before the onset of typically<br />
bulbar MND. 7<br />
Of the features listed above, social disinhibition,<br />
euphoria, stereotypical and aberrant motor behaviour,<br />
and changes in eating preference most clearly<br />
discriminate bvFTD from AD. 45,53 Variability in the<br />
symptom profi les reported across studies might have<br />
arisen from the aggregation of patients at diff erent stages<br />
of the disease. Increased behavioural changes have been<br />
associated with disease severity. 54 Agitation, disinhibition,<br />
and irritability also seem to be more frequent in the later<br />
stages, 55 whereas restlessness and hyperorality are<br />
present throughout the disease. 56 Another important<br />
variable is age of disease onset, with apathy being more<br />
prominent in late-onset bvFTD, 57 although this fi nding is<br />
not universal. 58<br />
In summary, behavioural assessment is at the core of<br />
assessment in patients with potential bvFTD and seems<br />
to be more sensitive in distinguishing bvFTD from AD<br />
than standard cognitive testing. Despite a substantial<br />
increase in our knowledge of the behavioural changes in<br />
bvFTD, which are at the root of so much carer distress<br />
(see below), much remains uncertain concerning their<br />
specifi city, neural basis, and their relation to the<br />
underlying pathology.<br />
bvFTD phenocopy syndrome: implications for<br />
diagnostic criteria<br />
The <strong>diagnosis</strong> of bvFTD is by no means an easy task in<br />
the early stages, and many of the symptoms overlap with<br />
those seen in psychiatric disorders and other <strong>dementia</strong>s. 51<br />
It is also increasingly apparent that a subset of patients<br />
who present with the <strong>clinical</strong> features of bvFTD do not<br />
progress to frank incapacitating <strong>dementia</strong>. 59 Such patients<br />
are almost always men and they either remain stable over<br />
many years or improve. 60,61 The symptom profi le as<br />
reported by family members is identical, except that<br />
activities of daily living (ADL) are less disrupted. 60,62<br />
Several features distinguish these non-progressor or<br />
phenocopy cases from those with true FTD, notably<br />
normal or marginal impairment on neuropsychological<br />
tests of executive function, preserved memory and social<br />
cognition, a lack of overt atrophy on MRI, and normal<br />
metabolic (PET) brain imaging. 59–61,63 The aetiology of the<br />
phenocopy syndrome is a matter of debate. A proportion<br />
of patients seem to have a developmental personality<br />
disorder on the Asperger’s spectrum with decompensation<br />
due to altered life circumstances (Hodges J, unpublished).<br />
Some might have a chronic low-grade mood disorder, but<br />
others remain a mystery.<br />
The phenocopy syndrome has major implications for<br />
the current <strong>clinical</strong> diagnostic criteria for FTD, 5 which<br />
require a profi le of symptoms compatible with the<br />
164 www.thelancet.com/neurology Vol 10 February 2011
<strong>diagnosis</strong> without imaging or other confi rmatory test<br />
results. These criteria also present diffi culties in their<br />
application due to under-specifi cation of some features<br />
and were derived by <strong>clinical</strong> consensus prior to the<br />
publication of quantitative studies comparing cohorts<br />
with pathologically verifi ed diagnoses. Recently proposed<br />
criteria developed by an international FTD research<br />
group (panel) 64 build on recent work with operationalised<br />
defi nitions that have three levels of diagnostic certainty:<br />
possible, probable, and defi nite bvFTD. Patients qualify<br />
for possible bvFTD on the basis of three core behavioural<br />
or cognitive features (including social disinhibition,<br />
apathy, loss of empathy, stereotypic behaviours or<br />
alterations in eating pattern, and neuropsychological<br />
defi cits indicative of frontal executive dysfunction). A<br />
probable <strong>diagnosis</strong> requires the same <strong>clinical</strong> features<br />
with evidence of progression and unequivocal neuroimaging<br />
abnormalities. The term “defi nite” is reserved<br />
for those with neuropathology or a pathogenic gene<br />
mutation. These new criteria (panel) are currently<br />
undergoing validation against neuropathological changes<br />
by an international consortium of researchers. 64<br />
Neuropsychology<br />
Cognition<br />
Early in the disease process, patients with bvFTD can<br />
perform relatively well on formal neuropsychological<br />
tests despite the presence of signifi cant personality and<br />
behavioural changes. 65 The mini mental state examination<br />
is insensitive, but the Addenbrooke’s cognitive<br />
examination seems to detect at least 90% of cases at<br />
presentation. 66 The prototypical cognitive profi le is one of<br />
relatively preserved language and visuospatial/<br />
constructive abilities. Whether patients with bvFTD show<br />
executive dysfunctions remains contentious, 67,68 and has<br />
been complicated by the inclusion of phenocopy cases.<br />
However, such defi cits constitute a central diagnostic<br />
feature of the newly proposed <strong>clinical</strong> diagnostic criteria. 64<br />
Recent evidence suggests that the combination of specifi c<br />
tests (eg, digit span backward task, Hayling test of<br />
response inhibition, and the short version of the executive<br />
and social cognition battery) might help diff erentiate<br />
these cases, because results are typically abnormal in<br />
patients with true bvFTD and normal in phenocopy<br />
cases. 68,69<br />
The presence of severe defi cits of episodic memory has<br />
been used as an exclusion criterion for a <strong>clinical</strong> <strong>diagnosis</strong><br />
of bvFTD, 5 although a proportion (10–15%) of patients<br />
with pathologically confi rmed FTLD present with severe<br />
amnesia. 21,70 A recent report has indicated that defi cits in<br />
episodic memory are more common than previously<br />
reported. 71 Carefully selected patients with bvFTD (ie,<br />
after excluding phenocopy cases) had similar memory<br />
impairments as seen in AD on tests of episodic memory,<br />
even after accounting for disease severity. 71 The criterion<br />
of relative sparing of episodic memory compared with<br />
executive functions proposed in the recent international<br />
consensus criteria for bvFTD might need to be revisited<br />
in the light of current research. 62<br />
The evidence reviewed thus far indicates that no specifi c<br />
cognitive profi le seems to be associated with bvFTD early<br />
in the disease, although careful cognitive assessment will<br />
reveal defi cits, generally in the domains of executive<br />
function and episodic memory. With disease progression,<br />
the atrophy evolves to involve the anterior temporal<br />
regions, and the pattern of defi cits becomes less distinct<br />
from other FTD subtypes, notably semantic <strong>dementia</strong>. 10<br />
Panel: International consensus criteria for bvFTD<br />
Review<br />
Neurodegenerative disease<br />
Must be present for any FTD <strong>clinical</strong> syndrome<br />
Shows progressive deterioration of behaviour and/or cognition by observation or history<br />
Possible bvFTD<br />
Three of the features (A–F) must be present; symptoms should occur repeatedly, not just<br />
as a single instance:<br />
A Early (3 years) behavioural disinhibition<br />
B Early (3 years) apathy or inertia<br />
C Early (3 years) loss of sympathy or empathy<br />
D Early (3 years) perseverative, stereotyped, or compulsive/ritualistic behaviour<br />
E Hyperorality and dietary changes<br />
F Neuropsychological profi le: executive function defi cits with relative sparing of<br />
memory and visuospatial functions<br />
Probable bvFTD<br />
All the following criteria must be present to meet <strong>diagnosis</strong>:<br />
A Meets criteria for possible bvFTD<br />
B Signifi cant functional decline<br />
C Imaging results consistent with bvFTD (frontal and/or anterior temporal atrophy on<br />
CT or MRI or frontal hypoperfusion or hypometabolism on SPECT or PET)<br />
Defi nite bvFTD<br />
Criteria A and either B or C must be present to meet <strong>diagnosis</strong>:<br />
A Meets criteria for possible or probable bvFTD<br />
B Histopathological evidence of FTLD on biopsy at post mortem<br />
C Presence of a known pathogenic mutation<br />
Exclusion criteria for bvFTD<br />
Criteria A and B must both be answered negatively; criterion C can be positive for possible<br />
bvFTD but must be negative for probable bvFTD:<br />
A Pattern of defi cits is better accounted for by other non-degenerative nervous system<br />
or medical disorders<br />
B <strong>Behavioural</strong> disturbance is better accounted for by a psychiatric <strong>diagnosis</strong><br />
C Biomarkers strongly indicative of Alzheimer’s disease or other neurodegenerative process<br />
Additional features<br />
A Presence of motor neuron fi ndings suggestive of motor neuron disease<br />
B Motor symptoms and signs similar to corticobasal degeneration and progressive<br />
supranuclear palsy<br />
C Impaired word and object knowledge<br />
D Motor speech defi cits<br />
E Substantial grammatical defi cits<br />
Criteria from Rascovsky et al. 64 bvFTD=behavioural-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>. FTD=<strong>frontotemporal</strong><br />
<strong>dementia</strong>. SPECT=single-photon emission computed tomography. FTLD=<strong>frontotemporal</strong> lobar degeneration.<br />
www.thelancet.com/neurology Vol 10 February 2011 165
Review<br />
Mild Moderate Severe<br />
Dorsolateral prefrontal and<br />
medial prefrontal cortices<br />
Orbitofrontal cortex<br />
Figure 2: Visual rating scale to estimate the severity of cortical atrophy in the dorsolateral, medial, and<br />
orbitofrontal cortices in suspected cases of bvFTD<br />
Modifi ed from Hornberger et al, 87 by permission of Karger AG, Basel. bvFTD=behavioural-<strong>variant</strong><br />
<strong>frontotemporal</strong> <strong>dementia</strong>.<br />
The diffi culty in identifying profi les of cognitive defi cits<br />
specifi c to bvFTD has led to an interest in aspects of social<br />
cognition (theory of mind), emotion recognition and<br />
complex problem solving, and the use of naturalistic tasks<br />
(ie, tasks indicating cognitive and non-cognitive demands<br />
more akin to daily activities). The orbitomesial frontal<br />
cortices are crucial for performance in these domains,<br />
and lesions within these brain regions have been shown<br />
to negatively aff ect tests measuring these cognitive<br />
constructs. 72 The Iowa gambling task of complex decision<br />
making requires individuals to inhibit responses that<br />
result in short-term high fi nancial gains but long-term<br />
losses in favour of responses resulting in small gains in<br />
the short term and reduced long-term losses. 73 This task<br />
was found to diff erentiate between patients with bvFTD,<br />
who consistently failed to inhibit the prepotent responses<br />
favouring short-term gains leading to long-term loss, and<br />
healthy controls. Interestingly, this defi cit is not related to<br />
performance on other cognitive tasks. 74<br />
Emotion recognition and social cognition<br />
A marked impairment in emotion detection and<br />
recognition is evident early in the course of bvFTD, 75,76<br />
and seems to be most pronounced for negative emotions<br />
(eg, fear, sadness, anger, and disgust). 76,77 Disorders of<br />
emotion detection and regulation are part of the <strong>clinical</strong><br />
diagnostic criteria for the disease (ie, early emotional<br />
blunting, early decline in social interpersonal conduct).<br />
However, such defi cits are not limited to this subtype of<br />
FTD and are also present in semantic <strong>dementia</strong>. 78<br />
Diffi culties in detecting and understanding emotions are<br />
observed with static (photos) or dynamic (fi lms) visual<br />
stimuli, voices, or even music. Importantly, physiological<br />
responses (eg, skin conductance) to some emotional<br />
stimuli are preserved. 79 Defi cits have also been observed<br />
in detecting more complex emotions, such as<br />
embarrassment. 80 These defi cits might be amenable to<br />
retraining to enhance their recognition and improve<br />
interpersonal relationships.<br />
Patients with bvFTD are also impaired on many aspects<br />
of social cognition. For example, the often reported<br />
feature of lack of empathy and coldness is confi rmed on<br />
formal testing. 81 Theory of mind is impaired in bvFTD,<br />
as exemplifi ed by defective ability to infer intention and<br />
mental states in others or to take someone else’s point of<br />
view, 74,75,82 and impaired detection of social faux pas, 82<br />
discrimination of sincere from sarcastic exchanges, 63<br />
and understanding of situations requiring moral<br />
judgment. 83 Whereas most of the tasks developed remain<br />
in the research arena, well validated tests of emotion and<br />
sarcasm detection exist, 84,85 which will hopefully become<br />
part of the standard cognitive assessment in suspected<br />
bvFTD.<br />
Neuroimaging<br />
By use of structural MRI, atrophy of the mesial frontal,<br />
orbitofrontal, and anterior insula cortices can be reliably<br />
observed on images acquired in the coronal plane<br />
(fi gure 2). 42,86,87 A combination of frontal and anterior<br />
temporal cortical and basal ganglia atrophy might also be<br />
seen at presentation in some patients. 88 This atrophy can<br />
be quickly and reliably estimated using relatively simple<br />
visual rating scales developed specifi cally for FTD. 89<br />
However, an apparently normal MRI on visual inspection<br />
does not completely exclude a <strong>diagnosis</strong> of bvFTD,<br />
because the changes can be subtle in the early stages.<br />
The development of automated quantitative methods,<br />
including voxel-based morphometry and cortical<br />
thickness mapping, has been important in revealing<br />
selective atrophy of the anterior cingulate and frontal<br />
insular cortices early in the course of bvFTD, 42,90,91 which<br />
is distinct from the pattern seen in other <strong>variant</strong>s of FTD<br />
and in AD. 92 The anterior cingulate-frontal insular<br />
complex contains a unique population of neurons, the<br />
von Economo cells, which are thought to be crucial in the<br />
development and maintenance of social cognition and<br />
have been shown to be depleted in patients with bvFTD<br />
at autopsy. 43,93 More recently, sophisticated MRI methods<br />
of exploring network connectivity have shown signifi cant<br />
changes in connectivity among the regions most sensitive<br />
to atrophy in bvFTD compared with healthy controls or<br />
patients with other <strong>dementia</strong> syndromes. 94,95<br />
Patterns of grey matter atrophy might be predictive of<br />
the underlying pathological process in bvFTD, with<br />
bilateral dorsolateral prefrontal atrophy being suggestive<br />
of Pick body inclusions (ie, Pick’s disease), and<br />
166 www.thelancet.com/neurology Vol 10 February 2011
asymmetric left and right temporal lobe atrophy being<br />
associated with FTLD-TDP and FTLD-tau, respectively. 96<br />
Marked atrophy of the caudate nucleus might also be<br />
predictive of FTLD-FUS. 24,97 However, patterns of atrophy<br />
seem to relate more closely to <strong>clinical</strong> features than to<br />
specifi c pathological changes. 98<br />
Brain changes in bvFTD are not limited to the cortex.<br />
Atrophy is also present in many subcortical brain regions,<br />
including the amygdala, hippocampus, caudate, striatum,<br />
putamen, thalamus, and hypothalamus, 50,99 accompanied<br />
by reduction in connectivity among subcortical structures. 95<br />
In addition, atrophy of the amygdala has been proven to be<br />
an effi cient discriminator between bvFTD and AD. 99<br />
By contrast with the well documented cortical grey<br />
matter changes, presence and severity of white matter<br />
changes in bvFTD have only recently been investigated. 100<br />
Frontal lobe white matter volume reduction largely<br />
parallels the atrophy in the adjacent grey matter in bvFTD,<br />
with diff erent subtypes of FTD showing specifi c patterns<br />
of white matter atrophy. 101 Using diff usion tensor imaging,<br />
an index of changes in the microstructural organisation of<br />
white matter, a study has successfully diff erentiated<br />
bvFTD from AD and other FTD subtypes. 102 Patients with<br />
bvFTD seem to show a selective reduction in some white<br />
matter tracts (superior longitudinal fasciculus, uncinate<br />
fasciculus, cingulum tracts, and genu and splenium of the<br />
corpus callosum), particularly those within frontal lobe<br />
(eg, genu of the corpus callosum) or those connecting<br />
frontal and temporal brain regions (eg, uncinate<br />
fasciculus). 102 Whether these white matter changes are<br />
reliable diagnostic markers for bvFTD remains unclear.<br />
Patients with the phenocopy syndrome who present with<br />
the <strong>clinical</strong> features of bvFTD show normal or marginal<br />
MRI changes. 61,89<br />
Serial MRIs show signifi cant atrophy over time in<br />
bvFTD. Annual rate of overall brain atrophy can reach 8%,<br />
almost twice as severe as that documented in AD, although<br />
some patients with bvFTD show atrophy rates similar to<br />
those seen in healthy controls (0·3% per year), which<br />
might be due to the inclusion of phenocopy cases. 103<br />
Functional neuroimaging techniques, such as [ 99m Tc]hexamethylpropyleneamine<br />
oxime single-photon emission<br />
computed tomography (SPECT) or [ 18 F]-fl uorodeoxyglucose<br />
(FDG)-PET are increasingly being used to help with the<br />
<strong>diagnosis</strong> of bvFTD. Frontal hypoperfusion is present on<br />
SPECT in bvFTD and diff ers from the pattern of<br />
hypoperfusion observed in AD, which is predominant in<br />
the temporoparietal and posterior cingulate cortices. 104<br />
Although SPECT seems to be more sensitive than<br />
structural MRI in detecting early pathological changes in<br />
bvFTD, quantifi cation and specifi city of these changes<br />
have not been established. Hypometabolism on FDG-PET<br />
is detected consistently and reliably in frontal brain regions<br />
in patients with bvFTD compared with those with AD, who<br />
show posterior cingulate hypometabolism early in the<br />
disease process. 105 These changes are detected before any<br />
changes are visible on structural MRI, making FDG-PET<br />
the most sensitive diagnostic tool currently available.<br />
FDG-PET is also particularly useful in helping to identify<br />
phenocopy cases as these will show preserved frontal<br />
metabolism. However, in patients showing clear brain<br />
atrophy on structural MRI, little additional diagnostic<br />
benefi t is gained by doing a PET scan, because focal<br />
atrophy is a positive predictive marker of FTD.<br />
A novel PET technique, which uses the amyloid-βdetecting<br />
[ 11 C]-Pittsburgh compound B, has shown<br />
promising results in discriminating AD and FTD<br />
cases, 106,107 particularly those presenting with language<br />
defi cits rather than behavioural changes. Its use as a<br />
routine test remains to be established, but its <strong>clinical</strong><br />
applicability is evident as therapeutic interventions are<br />
being developed that are likely to be pathology specifi c.<br />
In summary, neuroimaging investigations in the<br />
<strong>diagnosis</strong> of bvFTD are powerful tools, which can reliably<br />
diff erentiate bvFTD from other FTD subtypes and from<br />
other <strong>dementia</strong> syndromes, and can corroborate <strong>clinical</strong><br />
diagnostics based on neuropsychiatric symptoms.<br />
Functional abilities<br />
Disability in everyday life is more pronounced in bvFTD<br />
than in AD or in the language <strong>variant</strong>s of FTD, 65,108,109 even<br />
after controlling for length of symptoms or cognitive<br />
performance. 65,109 Compared with AD, a large proportion<br />
of patients with bvFTD are impaired in ADL, and show<br />
an early impairment in basic ADL at initial assessment. 110<br />
Marked changes in driving abilities occur and are<br />
associated with the degree of behavioural change, 111 which<br />
has clear practical implications. A 12-month follow-up<br />
study also identifi ed signifi cant changes in ADL, which<br />
were associated with general cognitive decline. 112 However,<br />
these changes were not present in phenocopy cases.<br />
Disease progression, functional staging, and<br />
survival<br />
Most studies, to date, have used the <strong>clinical</strong> <strong>dementia</strong><br />
rating (CDR) scale to measure <strong>dementia</strong> severity. 113 This<br />
instrument, which was originally developed for AD, is<br />
biased towards memory impairment and most likely<br />
underestimates the level of <strong>dementia</strong> severity in bvFTD. A<br />
version adapted for FTD includes language and behavioural<br />
domains (FTLD-CDR), 114 and the sum-of-boxes score seems<br />
to be sensitive to change in most patients with FTD.<br />
Recently, the <strong>frontotemporal</strong> <strong>dementia</strong> rating<br />
scale (FRS) was developed specifi cally for FTD. 115 This<br />
staging tool incorporates changes in behaviour and ADL<br />
(table). On the FRS, patients with bvFTD tend to show<br />
greater disease severity and a faster progression through<br />
the <strong>clinical</strong> stages than patients with the language<br />
<strong>variant</strong>s of FTD, even after adjusting for length of<br />
symptoms. 115 Importantly, the FRS confi rmed that the<br />
CDR tends to underestimate <strong>dementia</strong> severity in bvFTD,<br />
with a great proportion of moderate and severe cases on<br />
the FRS being rated as “questionable <strong>dementia</strong>” or “mild”<br />
on CDR.<br />
Review<br />
www.thelancet.com/neurology Vol 10 February 2011 167
Review<br />
For the Mental Capacity Act<br />
see http://www.publicguardian.<br />
gov.uk<br />
Patients with bvFTD seem to progress faster than<br />
patients with AD, with median survival (from fi rst<br />
assessment) of about 3·0–4·5 years, 110,116,117 although this<br />
fi nding has not been universal. 118 Factors determining<br />
reduced survival are associated with MND or ALS and<br />
language impairment at <strong>diagnosis</strong>. 117 The eff ect of<br />
neuropathological subtype on survival remains<br />
contentious. 116,119<br />
Therapeutic intervention and caregiver stress<br />
Currently, no disease-specifi c treatment interventions for<br />
FTD exist. Consequently, treatment largely remains<br />
supportive and involves a combination of nonpharmacological<br />
and pharmacological measures aimed at<br />
reducing the eff ect of distressing symptoms. 120 The role of<br />
pharmacological interventions in FTD remains uncertain,<br />
and only small and often confl icting treatment trials have<br />
been done so far; these studies have not considered the<br />
eff ect on carer stress as a major outcome variable.<br />
Selective serotonin reuptake inhibitors have been used to<br />
treat disinhibition and challenging behaviours, but<br />
evidence for their use remains contradictory. 121,122 Atypical<br />
antipsychotics such as olanzapine have been used for<br />
patients with prominent agitation, aggressive behaviour,<br />
or psychosis. 123 Anticholinesterase inhibitors, the mainstay<br />
of AD therapy, do not have an established role in the<br />
treatment of FTD. One study reported improvement in<br />
measures of behavioural disturbance and carer stress<br />
with rivastigmine, 124 although deterioration in neuropsychiatric<br />
symptoms without cognitive improve ment<br />
was shown with donepezil. 125 Several drugs under<br />
development attempt to reduce aggregation of tau or<br />
TDP-43 and hence slow the fundamental pathological<br />
process in FTD. 120,126<br />
Behaviour Activities of daily living<br />
Caregiver intervention, which should be the most<br />
eff ective treatment within the context of <strong>dementia</strong>, has<br />
also not been trialled in FTD caregivers. A model for<br />
behavioural management has been proposed, whereby a<br />
focus on the antecedent–behaviour–consequence model<br />
could be applied to diff erent patient situations with<br />
recommendations for specifi c behaviours exhibited in<br />
bvFTD, 127 but research studies are needed to verify their<br />
benefi ts. This would be timely, because caregivers of<br />
patients with FTD present with high rates of burden and<br />
stress. Recent studies have shown that caregiver burden<br />
in FTD is much greater than in AD. 128–130 <strong>Behavioural</strong><br />
changes rather than level of disability seem to be<br />
correlated with caregiver distress and burden in bvFTD, 129<br />
although very few studies have been done. Evidence<br />
indicates that caregiver health is a major contributor to<br />
carer stress, with depression accounting for 58% of the<br />
variance of stress scores in FTD caregivers. 130 The key to<br />
reducing caregiver stress seems to lie in increasing their<br />
understanding of the symptoms and ways of dealing with<br />
challenging behaviours.<br />
Driving and other aspects of capacity in bvFTD are<br />
clearly of great practical importance, but have been<br />
subject to little systematic research. A single study of<br />
driving competence in bvFTD suggested signifi cant<br />
problems, even at an early stage of the disease. 111 On that<br />
basis, a driving assessment would seem to be<br />
recommended in all cases. In Australia, the UK, and<br />
many other countries, an established code of practice<br />
exists governing the issue of legal capacity associated<br />
with the relevant Mental Capacity Act. Its application is<br />
relatively straightforward in patients with advanced<br />
bvFTD, but establishing a lack of capacity could be<br />
complex in the early stages of the disease. Of note,<br />
Basic Instrumental<br />
Mild Lack of aff ection No changes Diffi culties in managing correspondence<br />
Diffi culties in planning of fi nances<br />
Moderate Confused in unusual places<br />
Agitated, restless<br />
“Sweet tooth”<br />
Uncooperative<br />
Confused with the date<br />
Eats the same foods<br />
Impulsive<br />
Inability to choose clothes adequate to the<br />
occasion<br />
Severe .. Lack of appropriate manners at mealtimes<br />
Lack of initiation to eat if not served<br />
Very severe .. Cannot stay at home alone<br />
Not using cutlery adequately<br />
Does not go to toilet in time (urine)<br />
Profound .. Bedridden ..<br />
Modifi ed from Mioshi et al, 115 by permission of Wolters Kluwer Health. bvFTD=behavioural-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Table: Characteristics of each severity stage in the disease progression of bvFTD<br />
Changes in driving ability<br />
Decline in standard of execution of household chores<br />
Diffi culties dialling telephone<br />
Lacks interest in fi nances<br />
Cannot plan meals as well as before<br />
Problems with shopping<br />
Needs supervision when preparing a meal<br />
Needs prompting to do household chores<br />
Needs prompting to prepare meal<br />
Needs prompting to take medications<br />
Needs prompting to do leisure activities<br />
Needs help with dosage of medications<br />
Diffi culties managing cash<br />
..<br />
168 www.thelancet.com/neurology Vol 10 February 2011
Search strategy and selection criteria<br />
References for this Review were identifi ed through searches<br />
of PubMed from 2000, until November, 2010, with the terms<br />
“<strong>frontotemporal</strong> <strong>dementia</strong>”, “<strong>frontotemporal</strong> lobar<br />
degeneration”, “behavioural-<strong>variant</strong> <strong>frontotemporal</strong><br />
<strong>dementia</strong>”, and “frontal-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>”.<br />
Articles were also identifi ed through searches of the authors’<br />
own fi les. Only papers published in English were reviewed.<br />
capacity is not a global phenomenon but is situation<br />
specifi c. Moreover, unlike in AD, in which capacity can<br />
be impaired by amnesia (which is easier to assess), in<br />
bvFTD, the key cognitive variables are insight and<br />
judgment, which are much harder to assess and quantify.<br />
Finally, many useful publications and DVDs are available<br />
for caregivers, which can be accessed through the<br />
Frontotemporal Dementia Research Group website or<br />
the Association for FTDs.<br />
Conclusions and future directions<br />
Knowledge of the <strong>clinical</strong> presentation of bvFTD and its<br />
pathological processes has improved substantially over<br />
the past 20 years. Clinicians have become more aware of<br />
this disabling neurodegenerative condition, which aff ects<br />
individuals who are often still in the workforce or have<br />
young children. Careful medical history and information<br />
from family members, combined with <strong>clinical</strong><br />
investigations, neuro psychological testing, and<br />
investigations of social cognition, have increased case<br />
identifi cation. Sensitivity has also improved with the use<br />
of advanced structural and functional neuroimaging<br />
techniques. However, the major challenge that remains is<br />
to improve the prediction of the underlying neuropathology<br />
in patients with bvFTD during life. Eff orts to identify<br />
potential disease biomarkers for the disease are promising<br />
but will require further investigations. This line of<br />
research will become particularly relevant as diseasemodifying<br />
agents are developed.<br />
Contributors<br />
All authors contributed equally to the conception, literature review, and<br />
writing of this Review.<br />
Confl icts of interest<br />
The authors declare that they have no confl icts of interest.<br />
Acknowledgments<br />
This project was supported in part by a National Health and Medical<br />
Research Council (NHMRC) of Australia project grant (#510106). OP is<br />
supported by an NHMRC <strong>clinical</strong> career development award<br />
fellowship (#510184). JRH is supported by an Australian Research<br />
Council Federation fellowship (#FF0776229) and was previously<br />
supported by the UK Medical Research Council.<br />
References<br />
1 Hodges JR. Overview of <strong>frontotemporal</strong> <strong>dementia</strong>. In: Hodges JR,<br />
ed. Frontotemporal <strong>dementia</strong> syndromes. Cambridge: Cambridge<br />
University Press, 2007: 1–24.<br />
2 Ratnavalli E, Brayne C, Dawson K, Hodges JR. The prevalence of<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2002; 58: 1615–21.<br />
3 Rosso SM, Donker Kaat L, Baks T, et al. Frontotemporal <strong>dementia</strong><br />
in The Netherlands: patient characteristics and prevalence<br />
estimates from a population-based study. Brain 2003;<br />
126: 2016–22.<br />
4 Hodges JR, Patterson K. Semantic <strong>dementia</strong>: a unique<br />
clinicopathological syndrome. Lancet Neurol 2007; 6: 1004–14.<br />
5 Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar<br />
degeneration: a consensus on <strong>clinical</strong> diagnostic criteria. Neurology<br />
1998; 51: 1546–54.<br />
6 Grossman M. Primary progressive aphasia: clinicopathological<br />
correlations. Nat Rev Neurol 2010; 6: 88–97.<br />
7 Lillo P, Garcin B, Hornberger M, Bak TH, Hodges JR.<br />
Neurobehavioral features in <strong>frontotemporal</strong> <strong>dementia</strong> with<br />
amyotrophic lateral sclerosis. Arch Neurol 2010; 67: 826–30.<br />
8 Lomen-Hoerth C, Anderson T, Miller B. The overlap of amyotrophic<br />
lateral sclerosis and <strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2002;<br />
59: 1077–79.<br />
9 Lillo P, Mioshi E, Zoing MC, Kiernan MC, Hodges JR. How<br />
common are behavioural changes in amyotrophic lateral sclerosis?<br />
Amyotroph Lateral Scler 2010; published online Sept 19.<br />
DOI: 10.3109/17482968.2010.520718.<br />
10 Kertesz A, McMonagle P, Blair M, Davidson W, Munoz DG. The<br />
evolution and pathology of <strong>frontotemporal</strong> <strong>dementia</strong>. Brain 2005;<br />
128: 1996–2005.<br />
11 Rohrer JD, Guerreiro R, Vandrovcova J, et al. The heritability and<br />
genetics of <strong>frontotemporal</strong> lobar degeneration. Neurology 2009;<br />
73: 1451–56.<br />
12 Cairns NJ, Bigio EH, Mackenzie IR, et al. Neuropathologic<br />
diagnostic and nosologic criteria for <strong>frontotemporal</strong> lobar<br />
degeneration: consensus of the Consortium for Frontotemporal<br />
Lobar Degeneration. Acta Neuropathol (Berl) 2007; 114: 5–22.<br />
13 Broe M, Hodges JR, Schofi eld E, Shepherd CE, Kril JJ,<br />
Halliday GM. Staging disease severity in pathologically confi rmed<br />
cases of <strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2003; 60: 1005–11.<br />
14 Kril JJ, Macdonald V, Patel S, Png F, Halliday GM. Distribution of<br />
brain atrophy in behavioral <strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
J Neurol Sci 2005; 232: 83–90.<br />
15 Kersaitis C, Halliday GM, Kril JJ. Regional and cellular pathology in<br />
<strong>frontotemporal</strong> <strong>dementia</strong>: relationship to stage of disease in cases<br />
with and without Pick bodies. Acta Neuropathol 2004; 108: 515–23.<br />
16 Mackenzie IR, Neumann M, Bigio EH, et al. Nomenclature and<br />
nosology for neuropathologic subtypes of <strong>frontotemporal</strong> lobar<br />
degeneration: an update. Acta Neuropathol 2010; 119: 1–4.<br />
17 Mackenzie IR, Foti D, Woulfe J, Hurwitz TA. Atypical<br />
<strong>frontotemporal</strong> lobar degeneration with ubiquitin-positive,<br />
TDP-43-negative neuronal inclusions. Brain 2008; 131: 1282–93.<br />
18 Neumann M, Rademakers R, Roeber S, Baker M, Kretzschmar HA,<br />
Mackenzie IR. A new subtype of <strong>frontotemporal</strong> lobar degeneration<br />
with FUS pathology. Brain 2009; 132: 2922–31.<br />
19 Kwiatkowski TJ Jr, Bosco DA, Leclerc AL, et al. Mutations in the<br />
FUS/TLS gene on chromosome 16 cause familial amyotrophic<br />
lateral sclerosis. Science 2009; 323: 1205–08.<br />
20 Vance C, Rogelj B, Hortobagyi T, et al. Mutations in FUS, an RNA<br />
processing protein, cause familial amyotrophic lateral sclerosis<br />
type 6. Science 2009; 323: 1208–11.<br />
21 Hodges JR, Davies RR, Xuereb JH, et al. Clinicopathological<br />
correlates in <strong>frontotemporal</strong> <strong>dementia</strong>. Ann Neurol 2004; 56: 399–406.<br />
22 Shi J, Shaw CL, Du Plessis D, et al. Histopathological changes<br />
underlying <strong>frontotemporal</strong> lobar degeneration with<br />
clinicopathological correlation. Acta Neuropathol 2005; 110: 501–12.<br />
23 Snowden J, Neary D, Mann D. Frontotemporal lobar degeneration:<br />
<strong>clinical</strong> and pathological relationships. Acta Neuropathol 2007;<br />
114: 31–38.<br />
24 Seelaar H, Klijnsma KY, de Koning I, et al. Frequency of ubiquitin<br />
and FUS-positive, TDP-43-negative <strong>frontotemporal</strong> lobar<br />
degeneration. J Neurol 2010; 257: 747–53.<br />
25 Bian H, Van Swieten JC, Leight S, et al. CSF biomarkers in<br />
<strong>frontotemporal</strong> lobar degeneration with known pathology. Neurology<br />
2008; 70: 1827–35.<br />
26 Steinacker P, Hendrich C, Sperfeld AD, et al. TDP-43 in<br />
cerebrospinal fl uid of patients with <strong>frontotemporal</strong> lobar<br />
degeneration and amyotrophic lateral sclerosis. Arch Neurol 2008;<br />
65: 1481–87.<br />
Review<br />
For the Frontotemporal<br />
Dementia Research Group see<br />
http://www.ftdrg.org<br />
For the Association for FTDs see<br />
http://www.ftd-picks.org<br />
www.thelancet.com/neurology Vol 10 February 2011 169
Review<br />
27 Sleegers K, Brouwers N, Van Damme P, et al. Serum biomarker for<br />
progranulin-associated <strong>frontotemporal</strong> lobar degeneration.<br />
Ann Neurol 2009; 65: 603–09.<br />
28 Finch N, Baker M, Crook R, et al. Plasma progranulin levels predict<br />
progranulin mutation status in <strong>frontotemporal</strong> <strong>dementia</strong> patients<br />
and asymptomatic family members. Brain 2009; 132: 583–91.<br />
29 Ghidoni R, Benussi L, Glionna M, Franzoni M, Binetti G. Low<br />
plasma progranulin levels predict progranulin mutations in<br />
<strong>frontotemporal</strong> lobar degeneration. Neurology 2008; 71: 1235–39.<br />
30 Schofi eld E, Halliday GM, Kwok JB, Loy C, Hodges JR. Low serum<br />
progranulin is diagnostic for progranulin mutations: a prospective<br />
study. J Alzheimers Dis 2010; published online Sept 21.<br />
DOI: 10.3233/JAD-2010-101032.<br />
31 Foulds PG, Davidson Y, Mishra M, et al. Plasma phosphorylated-<br />
TDP-43 protein levels correlate with brain pathology in<br />
<strong>frontotemporal</strong> lobar degeneration. Acta Neuropathol 2009;<br />
118: 647–58.<br />
32 Benajiba L, Le Ber I, Camuzat A, et al. TARDBP mutations in<br />
motoneuron disease with <strong>frontotemporal</strong> lobar degeneration.<br />
Ann Neurol 2009; 65: 470–73.<br />
33 Ticozzi N, Silani V, LeClerc AL, et al. Analysis of FUS gene<br />
mutation in familial amyotrophic lateral sclerosis within an Italian<br />
cohort. Neurology 2009; 73: 1180–85.<br />
34 Blair IP, Williams KL, Warraich ST, et al. FUS mutations in<br />
amyotrophic lateral sclerosis: <strong>clinical</strong>, pathological,<br />
neurophysiological and genetic analysis.<br />
J Neurol Neurosurg Psychiatry 2010; 81: 639–45.<br />
35 Kovacs GG, Murrell JR, Horvath S, et al. TARDBP variation<br />
associated with <strong>frontotemporal</strong> <strong>dementia</strong>, supranuclear gaze palsy,<br />
and chorea. Mov Disord 2009; 24: 1843–47.<br />
36 Watts GD, Wymer J, Kovach MJ, et al. Inclusion body myopathy<br />
associated with Paget disease of bone and <strong>frontotemporal</strong> <strong>dementia</strong><br />
is caused by mutant valosin-containing protein. Nat Genet 2004;<br />
36: 377–81.<br />
37 Parkinson N, Ince PG, Smith MO, et al. ALS phenotypes with<br />
mutations in CHMP2B (charged multivesicular body protein 2B).<br />
Neurology 2006; 67: 1074–77.<br />
38 van der Zee J, Urwin H, Engelborghs S, et al.<br />
CHMP2B C-truncating mutations in <strong>frontotemporal</strong> lobar<br />
degeneration are associated with an aberrant endosomal phenotype<br />
in vitro. Hum Mol Genet 2008; 17: 313–22.<br />
39 Vance C, Al-Chalabi A, Ruddy D, et al. Familial amyotrophic lateral<br />
sclerosis with <strong>frontotemporal</strong> <strong>dementia</strong> is linked to a locus on<br />
chromosome 9p13.2-21.3. Brain 2006; 129: 868–76.<br />
40 Kipps CM, Mioshi E, Hodges JR. Emotion, social functioning and<br />
activities of daily living in <strong>frontotemporal</strong> <strong>dementia</strong>. Neurocase 2009;<br />
15: 182–89.<br />
41 Huey ED, Goveia EN, Paviol S, et al. Executive dysfunction in<br />
<strong>frontotemporal</strong> <strong>dementia</strong> and corticobasal syndrome. Neurology<br />
2009; 72: 453–59.<br />
42 Seeley WW, Crawford R, Rascovsky K, et al. Frontal paralimbic<br />
network atrophy in very mild behavioral <strong>variant</strong> <strong>frontotemporal</strong><br />
<strong>dementia</strong>. Arch Neurol 2008; 65: 249–55.<br />
43 Seeley WW. Selective functional, regional, and neuronal vulnerability<br />
in <strong>frontotemporal</strong> <strong>dementia</strong>. Curr Opin Neurol 2008; 21: 701–07.<br />
44 Cummings JL, Mega M, Gray K, Rosenberg-Thompson S,<br />
Carusi DA, Gornbein J. The Neuropsychiatric Inventory:<br />
comprehensive assessment of psychopathology in <strong>dementia</strong>.<br />
Neurology 1994; 44: 2308–14.<br />
45 Bozeat S, Gregory CA, Ralph MA, Hodges JR. Which<br />
neuropsychiatric and behavioural features distinguish frontal and<br />
temporal <strong>variant</strong>s of <strong>frontotemporal</strong> <strong>dementia</strong> from Alzheimer’s<br />
disease? J Neurol Neurosurg Psychiatry 2000; 69: 178–86.<br />
46 Kertesz A, Davidson W, Fox H. Frontal behavioral inventory:<br />
diagnostic criteria for frontal lobe <strong>dementia</strong>. Can J Neurol Sci 1997;<br />
24: 29–36.<br />
47 Manes FF, Torralva T, Roca M, Gleichgerrcht E, Bekinschtein TA,<br />
Hodges JR. Frontotemporal <strong>dementia</strong> presenting as pathological<br />
gambling. Nat Rev Neurol 2010; 6: 347–52.<br />
48 Postiglione A, Milan G, Pappata S, et al. Fronto-temporal <strong>dementia</strong><br />
presenting as Geschwind’s syndrome. Neurocase 2008; 14: 264–70.<br />
49 Shinagawa S, Ikeda M, Nestor PJ, et al. Characteristics of abnormal<br />
eating behaviours in <strong>frontotemporal</strong> lobar degeneration: a crosscultural<br />
survey. J Neurol Neurosurg Psychiatry 2009; 80: 1413–14.<br />
50 Piguet O, Petersén Å, Lam BYK, et al. Eating and hypothalamus<br />
changes in behavioural-<strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Ann Neurol 2010; published online Nov 12.<br />
DOI: 10.1002/ana.22244.<br />
51 Loy CT, Kril JJ, Trollor JN, et al. The case of a 48 year-old woman<br />
with bizarre and complex delusions. Nat Rev Neurol 2010; 6: 175–79.<br />
52 Urwin H, Josephs KA, Rohrer JD, et al. FUS pathology defi nes the<br />
majority of tau- and TDP-43-negative <strong>frontotemporal</strong> lobar<br />
degeneration. Acta Neuropathol 2010; 120: 33–41.<br />
53 Liu W, Miller BL, Kramer JH, et al. Behavioral disorders in the<br />
frontal and temporal <strong>variant</strong>s of <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Neurology 2004; 62: 742–48.<br />
54 Diehl-Schmid J, Pohl C, Perneczky R, Forstl H, Kurz A. Behavioral<br />
disturbances in the course of <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Dement Geriatr Cogn Disord 2006; 22: 352–57.<br />
55 Srikanth S, Nagaraja AV, Ratnavalli E. Neuropsychiatric symptoms<br />
in <strong>dementia</strong>-frequency, relationship to <strong>dementia</strong> severity and<br />
comparison in Alzheimer’s disease, vascular <strong>dementia</strong> and<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. J Neurol Sci 2005; 236: 43–48.<br />
56 Pasquier F, Lebert F, Lavenu I, Guillaume B. The <strong>clinical</strong> picture of<br />
<strong>frontotemporal</strong> <strong>dementia</strong>: <strong>diagnosis</strong> and follow-up.<br />
Dement Geriatr Cogn Disord 1999; 10 (suppl 1): 10–14.<br />
57 Shinagawa S, Toyota Y, Ishikawa T, et al. Cognitive function and<br />
psychiatric symptoms in early- and late-onset <strong>frontotemporal</strong><br />
<strong>dementia</strong>. Dement Geriatr Cogn Disord 2008; 25: 439–44.<br />
58 Borroni B, Agosti C, Bellelli G, Padovani A. Is early-onset <strong>clinical</strong>ly<br />
diff erent from late-onset <strong>frontotemporal</strong> <strong>dementia</strong>? Eur J Neurol<br />
2008; 15: 1412–15.<br />
59 Kipps CM, Nestor PJ, Fryer TD, Hodges JR. <strong>Behavioural</strong> <strong>variant</strong><br />
<strong>frontotemporal</strong> <strong>dementia</strong>: not all it seems? Neurocase 2007;<br />
13: 237–47.<br />
60 Hornberger M, Shelley BP, Kipps CM, Piguet O, Hodges JR. Can<br />
progressive and non-progressive behavioral <strong>variant</strong> <strong>frontotemporal</strong><br />
<strong>dementia</strong> be distinguished at presentation?<br />
J Neurol Neurosurg Psychiatry 2009; 80: 591–93.<br />
61 Davies RR, Kipps CM, Mitchell J, Kril JJ, Halliday GM, Hodges JR.<br />
Progression in <strong>frontotemporal</strong> <strong>dementia</strong>: identifying a benign<br />
behavioral <strong>variant</strong> by magnetic resonance imaging. Arch Neurol<br />
2006; 63: 1627–31.<br />
62 Piguet O, Hornberger M, Shelley BP, Kipps CM, Hodges JR.<br />
Sensitivity of current criteria for the <strong>diagnosis</strong> of behavioral <strong>variant</strong><br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2009; 72: 732–37.<br />
63 Kipps CM, Hodges JR, Fryer TD, Nestor PJ. Combined magnetic<br />
resonance imaging and positron emission tomography brain<br />
imaging in behavioural <strong>variant</strong> <strong>frontotemporal</strong> degeneration:<br />
refi ning the <strong>clinical</strong> phenotype. Brain 2009; 132: 2566–78.<br />
64 Rascovsky K, Hodges JR, Kipps CM, et al. Diagnostic criteria for the<br />
behavioral <strong>variant</strong> of <strong>frontotemporal</strong> <strong>dementia</strong> (bvFTD): current<br />
limitations and future directions. Alzheimer Dis Assoc Disord 2007;<br />
21: S14–18.<br />
65 Mioshi E, Kipps CM, Dawson K, Mitchell J, Graham A, Hodges JR.<br />
Activities of daily living in <strong>frontotemporal</strong> <strong>dementia</strong> and Alzheimer<br />
disease. Neurology 2007; 68: 2077–84.<br />
66 Kipps CM, Nestor PJ, Dawson CE, Mitchell J, Hodges JR.<br />
Measuring progression in <strong>frontotemporal</strong> <strong>dementia</strong>: implications<br />
for therapeutic interventions. Neurology 2008; 70: 2046–52.<br />
67 Giovagnoli AR, Erbetta A, Reati F, Bugiani O. Diff erential<br />
neuropsychological patterns of frontal <strong>variant</strong> <strong>frontotemporal</strong><br />
<strong>dementia</strong> and Alzheimer’s disease in a study of diagnostic<br />
concordance. Neuropsychologia 2008; 46: 1495–504.<br />
68 Hornberger M, Piguet O, Kipps C, Hodges JR. Executive function<br />
in progressive and nonprogressive behavioral <strong>variant</strong><br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2008; 71: 1481–88.<br />
69 Gleichgerrcht E, Torralva T, Roca M, Manes F. Utility of an<br />
abbreviated version of the executive and social cognition battery in<br />
the detection of executive defi cits in early behavioral <strong>variant</strong><br />
<strong>frontotemporal</strong> <strong>dementia</strong> patients. J Int Neuropsychol Soc 2010;<br />
19: 1–8.<br />
70 Graham A, Davies R, Xuereb J, et al. Pathologically proven<br />
<strong>frontotemporal</strong> <strong>dementia</strong> presenting with severe amnesia. Brain<br />
2005; 128: 597–605.<br />
71 Hornberger M, Piguet O, Graham AJ, Nestor PJ, Hodges JR. How<br />
preserved is episodic memory in behavioral <strong>variant</strong> <strong>frontotemporal</strong><br />
<strong>dementia</strong>? Neurology 2010; 74: 472–79.<br />
170 www.thelancet.com/neurology Vol 10 February 2011
72 Fellows LK, Farah MJ. Ventromedial frontal cortex mediates<br />
aff ective shifting in humans: evidence from a reversal learning<br />
paradigm. Brain 2003; 126: 1830–37.<br />
73 Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to<br />
future consequences following damage to human prefrontal cortex.<br />
Cognition 1994; 50: 7–15.<br />
74 Torralva T, Roca M, Gleichgerrcht E, Bekinschtein T, Manes F. A<br />
neuropsychological battery to detect specifi c executive and social<br />
cognitive impairments in early <strong>frontotemporal</strong> <strong>dementia</strong>. Brain<br />
2009; 132: 1299–309.<br />
75 Lough S, Kipps CM, Treise C, Watson P, Blair JR, Hodges JR. Social<br />
reasoning, emotion and empathy in <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Neuropsychologia 2006; 44: 950–58.<br />
76 Snowden JS, Austin NA, Sembi S, Thompson JC, Craufurd D,<br />
Neary D. Emotion recognition in Huntington’s disease and<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Neuropsychologia 2008; 46: 2638–49.<br />
77 Fernandez-Duque D, Black SE. Impaired recognition of negative<br />
facial emotions in patients with <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Neuropsychologia 2005; 43: 1673–87.<br />
78 Rankin KP, Gorno-Tempini ML, Allison SC, et al. Structural<br />
anatomy of empathy in neurodegenerative disease. Brain 2006;<br />
129: 2945–56.<br />
79 Werner KH, Roberts NA, Rosen HJ, et al. Emotional reactivity and<br />
emotion recognition in <strong>frontotemporal</strong> lobar degeneration.<br />
Neurology 2007; 69: 148–55.<br />
80 Sturm VE, Rosen HJ, Allison S, Miller BL, Levenson RW. Selfconscious<br />
emotion defi cits in <strong>frontotemporal</strong> lobar degeneration.<br />
Brain 2006; 129: 2508–16.<br />
81 Fernandez-Duque D, Hodges SD, Baird JA, Black SE. Empathy in<br />
<strong>frontotemporal</strong> <strong>dementia</strong> and Alzheimer’s disease.<br />
J Clin Exp Neuropsychol 2010; 32: 289–98.<br />
82 Gregory C, Lough S, Stone V, et al. Theory of mind in patients<br />
with frontal <strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong> and Alzheimer’s<br />
disease: theoretical and practical implications. Brain 2002;<br />
125: 752–64.<br />
83 Mendez MF, Shapira JS. Altered emotional morality in<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Cogn Neuropsychiatry 2009; 14: 165–79.<br />
84 Kipps CM, Nestor PJ, Acosta-Cabronero J, Arnold R, Hodges JR.<br />
Understanding social dysfunction in the behavioural <strong>variant</strong> of<br />
<strong>frontotemporal</strong> <strong>dementia</strong>: the role of emotion and sarcasm<br />
processing. Brain 2009; 132: 592–603.<br />
85 McDonald S, Flanagan S, Rollins J, Kinch J. TASIT: a new <strong>clinical</strong><br />
tool for assessing social perception after traumatic brain injury.<br />
J Head Trauma Rehabil 2003; 18: 219–38.<br />
86 Davatzikos C, Resnick SM, Wu X, Parmpi P, Clark CM. Individual<br />
patient <strong>diagnosis</strong> of AD and FTD via high-dimensional pattern<br />
classifi cation of MRI. Neuroimage 2008; 41: 1220–27.<br />
87 Hornberger M, Savage S, Hsieh S, Mioshi E, Piguet O, Hodges JR.<br />
Orbitofrontal dysfunction discriminates behavioural <strong>variant</strong><br />
<strong>frontotemporal</strong> <strong>dementia</strong> from Alzheimer’s disease.<br />
Dement Geriatr Cogn Disord 2011 (in press).<br />
88 Whitwell JL, Przybelski SA, Weigand SD, et al. Distinct anatomical<br />
subtypes of the behavioural <strong>variant</strong> of <strong>frontotemporal</strong> <strong>dementia</strong>: a<br />
cluster analysis study. Brain 2009; 132: 2932–46.<br />
89 Kipps CM, Davies RR, Mitchell J, Kril JJ, Halliday GM, Hodges JR.<br />
Clinical signifi cance of lobar atrophy in <strong>frontotemporal</strong> <strong>dementia</strong>:<br />
application of an MRI visual rating scale.<br />
Dement Geriatr Cogn Disord 2007; 23: 334–42.<br />
90 Boccardi M, Sabattoli F, Laakso MP, et al. Frontotemporal<br />
<strong>dementia</strong> as a neural system disease. Neurobiol Aging 2005;<br />
26: 37–44.<br />
91 Schroeter ML, Raczka K, Neumann J, Yves von Cramon D. Towards<br />
a nosology for <strong>frontotemporal</strong> lobar degenerations—a meta-analysis<br />
involving 267 subjects. NeuroImage 2007; 36: 497–510.<br />
92 Davies RR, Scahill VL, Graham A, Williams GB, Graham KS,<br />
Hodges JR. Development of an MRI rating scale for multiple brain<br />
regions: comparison with volumetrics and with voxel-based<br />
morphometry. Neuroradiology 2009; 51: 491–503.<br />
93 Seeley WW, Carlin DA, Allman JM, et al. Early <strong>frontotemporal</strong><br />
<strong>dementia</strong> targets neurons unique to apes and humans. Ann Neurol<br />
2006; 60: 660–67.<br />
94 Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD.<br />
Neurodegenerative diseases target large-scale human brain<br />
networks. Neuron 2009; 62: 42–52.<br />
95 Zhou J, Greicius MD, Gennatas ED, et al. Divergent network<br />
connectivity changes in behavioural <strong>variant</strong> <strong>frontotemporal</strong><br />
<strong>dementia</strong> and Alzheimer’s disease. Brain 2010; 133: 1352–67.<br />
96 Whitwell JL, Josephs KA, Rossor MN, et al. Magnetic resonance<br />
imaging signatures of tissue pathology in <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Arch Neurol 2005; 62: 1402–08.<br />
97 Josephs KA, Whitwell JL, Parisi JE, et al. Caudate atrophy on MRI is<br />
a characteristic feature of FTLD-FUS. Eur J Neurol 2010; 17: 969–75.<br />
98 Pereira JM, Williams GB, Acosta-Cabronero J, et al. Atrophy<br />
patterns in histologic vs <strong>clinical</strong> groupings of <strong>frontotemporal</strong> lobar<br />
degeneration. Neurology 2009; 72: 1653–60.<br />
99 Barnes J, Whitwell JL, Frost C, Josephs KA, Rossor M, Fox NC.<br />
Measurements of the amygdala and hippocampus in pathologically<br />
confi rmed Alzheimer disease and <strong>frontotemporal</strong> lobar<br />
degeneration. Arch Neurol 2006; 63: 1434–39.<br />
100 Cardenas VA, Boxer AL, Chao LL, et al. Deformation-based<br />
morphometry reveals brain atrophy in <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Arch Neurol 2007; 64: 873–77.<br />
101 Chao LL, Schuff N, Clevenger EM, et al. Patterns of white matter<br />
atrophy in <strong>frontotemporal</strong> lobar degeneration. Arch Neurol 2007;<br />
64: 1619–24.<br />
102 Zhang Y, Schuff N, Du AT, et al. White matter damage in<br />
<strong>frontotemporal</strong> <strong>dementia</strong> and Alzheimer’s disease measured by<br />
diff usion MRI. Brain 2009; 132: 2579–92.<br />
103 Chan D, Fox NC, Jenkins R, Scahill RI, Crum WR, Rossor MN.<br />
Rates of global and regional cerebral atrophy in AD and<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2001; 57: 1756–63.<br />
104 Varma AR, Adams W, Lloyd JJ, et al. Diagnostic patterns of regional<br />
atrophy on MRI and regional cerebral blood fl ow change on SPECT<br />
in young onset patients with Alzheimer’s disease, <strong>frontotemporal</strong><br />
<strong>dementia</strong> and vascular <strong>dementia</strong>. Acta Neurol Scand 2002;<br />
105: 261–69.<br />
105 Kanda T, Ishii K, Uemura T, et al. Comparison of grey matter and<br />
metabolic reductions in <strong>frontotemporal</strong> <strong>dementia</strong> using FDG-PET<br />
and voxel-based morphometric MR studies.<br />
Eur J Nucl Med Mol Imaging 2008; 35: 2227–34.<br />
106 Rowe CC, Ng S, Ackermann U, et al. Imaging beta-amyloid burden<br />
in aging and <strong>dementia</strong>. Neurology 2007; 68: 1718–25.<br />
107 Engler H, Santillo AF, Wang SX, et al. In vivo amyloid imaging with<br />
PET in <strong>frontotemporal</strong> <strong>dementia</strong>. Eur J Nucl Med Mol Imaging 2008;<br />
35: 100–06.<br />
108 Wicklund AH, Johnson N, Rademaker A, Weitner BB, Weintraub S.<br />
Profi les of decline in activities of daily living in non-Alzheimer<br />
<strong>dementia</strong>. Alzheimer Dis Assoc Disord 2007; 21: 8–13.<br />
109 Rosen HJ, Allison SC, Schauer GF, Gorno-Tempini ML,<br />
Weiner MW, Miller BL. Neuroanatomical correlates of behavioural<br />
disorders in <strong>dementia</strong>. Brain 2005; 128: 2612–25.<br />
110 Rascovsky K, Salmon DP, Lipton AM, et al. Rate of progression<br />
diff ers in <strong>frontotemporal</strong> <strong>dementia</strong> and Alzheimer disease.<br />
Neurology 2005; 65: 397–403.<br />
111 de Simone V, Kaplan L, Patronas N, Wassermann EM, Grafman J.<br />
Driving abilities in <strong>frontotemporal</strong> <strong>dementia</strong> patients.<br />
Dement Geriatr Cogn Disord 2007; 23: 1–7.<br />
112 Mioshi E, Hodges JR. Rate of change of functional abilities in<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Dement Geriatr Cogn Disord 2009;<br />
28: 419–26.<br />
113 Morris JC. Clinical <strong>dementia</strong> rating: a reliable and valid diagnostic<br />
and staging measure for <strong>dementia</strong> of the Alzheimer type.<br />
Int Psychogeriatr 1997; 9 (suppl 1): 173–78.<br />
114 Knopman DS, Kramer JH, Boeve BF, et al. Development of<br />
methodology for conducting <strong>clinical</strong> trials in <strong>frontotemporal</strong> lobar<br />
degeneration. Brain 2008; 131: 2957–68.<br />
115 Mioshi E, Hsieh S, Savage S, Hornberger M, Hodges JR. Clinical<br />
staging and disease progression in <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Neurology 2010; 74: 1591–97.<br />
116 Roberson ED, Hesse JH, Rose KD, et al. Frontotemporal <strong>dementia</strong><br />
progresses to death faster than Alzheimer disease. Neurology 2005;<br />
65: 719–25.<br />
117 Garcin B, Lillo P, Hornberger M, et al. Determinants of survival in<br />
behavioral <strong>variant</strong> <strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2009;<br />
73: 1656–61.<br />
118 Pasquier F, Richard F, Lebert F. Natural history of <strong>frontotemporal</strong><br />
<strong>dementia</strong>: comparison with Alzheimer’s disease.<br />
Dement Geriatr Cogn Disord 2004; 17: 253–57.<br />
Review<br />
www.thelancet.com/neurology Vol 10 February 2011 171
Review<br />
119 Hodges JR, Davies R, Xuereb J, Kril J, Halliday G. Survival in<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Neurology 2003; 61: 349–54.<br />
120 Boxer AL, Boeve BF. Frontotemporal <strong>dementia</strong> treatment: current<br />
symptomatic therapies and implications of recent genetic,<br />
biochemical, and neuroimaging studies. Alzheimer Dis Assoc Disord<br />
2007; 21: S79–87.<br />
121 Moretti R, Torre P, Antonello RM, Cazzato G, Bava A.<br />
Frontotemporal <strong>dementia</strong>: paroxetine as a possible treatment of<br />
behavior symptoms. A randomized, controlled, open 14-month<br />
study. Eur Neurol 2003; 49: 13–19.<br />
122 Deakin JB, Rahman S, Nestor PJ, Hodges JR, Sahakian BJ.<br />
Paroxetine does not improve symptoms and impairs cognition in<br />
<strong>frontotemporal</strong> <strong>dementia</strong>: a double-blind randomized controlled<br />
trial. Psychopharmacology (Berl) 2004; 172: 400–08.<br />
123 Moretti R, Torre P, Antonello RM, Cazzato G, Griggio S, Bava A.<br />
Olanzapine as a treatment of neuropsychiatric disorders of<br />
Alzheimer’s disease and other <strong>dementia</strong>s: a 24-month follow-up of<br />
68 patients. Am J Alzheimers Dis Other Demen 2003; 18: 205–14.<br />
124 Moretti R, Torre P, Antonello RM, Cattaruzza T, Cazzato G, Bava A.<br />
Rivastigmine in <strong>frontotemporal</strong> <strong>dementia</strong>: an open-label study.<br />
Drugs Aging 2004; 21: 931–97.<br />
125 Mendez MF, Shapira JS, McMurtray A, Licht E. Preliminary<br />
fi ndings: behavioral worsening on donepezil in patients with<br />
<strong>frontotemporal</strong> <strong>dementia</strong>. Am J Geriatr Psychiatry 2007; 15: 84–87.<br />
126 Mendez MF. Frontotemporal <strong>dementia</strong>: therapeutic interventions.<br />
Front Neurol Neurosci 2009; 24: 168–78.<br />
127 Merrilees J, Klapper J, Murphy J, Lomen-Hoerth C, Miller BL.<br />
Cognitive and behavioral challenges in caring for patients with<br />
<strong>frontotemporal</strong> <strong>dementia</strong> and amyotrophic lateral sclerosis.<br />
Amyotroph Lateral Scler 2010; 11: 298–302.<br />
128 Riedijk SR, De Vugt ME, Duivenvoorden HJ, et al. Caregiver<br />
burden, health-related quality of life and coping in <strong>dementia</strong><br />
caregivers: a comparison of <strong>frontotemporal</strong> <strong>dementia</strong> and<br />
Alzheimer’s disease. Dement Geriatr Cogn Disord 2006; 22: 405–12.<br />
129 Boutoleau-Bretonniere C, Vercelletto M, Volteau C, Renou P,<br />
Lamy E. Zarit burden inventory and activities of daily living in the<br />
behavioral <strong>variant</strong> of <strong>frontotemporal</strong> <strong>dementia</strong>.<br />
Dement Geriatr Cogn Disord 2008; 25: 272–77.<br />
130 Mioshi E, Bristow M, Cook R, Hodges JR. Factors underlying<br />
caregiver stress in <strong>frontotemporal</strong> <strong>dementia</strong> and Alzheimer’s<br />
disease. Dement Geriatr Cogn Disord 2009; 27: 76–81.<br />
172 www.thelancet.com/neurology Vol 10 February 2011