Changing Concepts in Thyroid Pathology - Departments of ...
Changing Concepts in Thyroid Pathology - Departments of ...
Changing Concepts in Thyroid Pathology - Departments of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
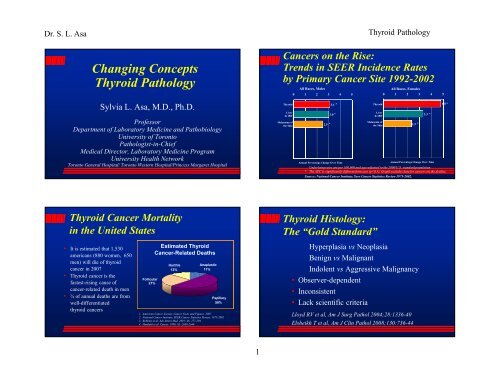
Dr. S. L. Asa<br />
<strong>Chang<strong>in</strong>g</strong> <strong>Concepts</strong><br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Sylvia L. Asa, M.D., Ph.D.<br />
Pr<strong>of</strong>essor<br />
Department <strong>of</strong> Laboratory Medic<strong>in</strong>e and Pathobiology<br />
University <strong>of</strong> Toronto<br />
Pathologist-<strong>in</strong>-Chief<br />
Medical Director, Laboratory Medic<strong>in</strong>e Program<br />
University Health Network<br />
Toronto General Hospital/ Toronto Western Hospital/Pr<strong>in</strong>cess Margaret Hospital<br />
<strong>Thyroid</strong> Cancer Mortality<br />
<strong>in</strong> the United States<br />
• It is estimated that 1,530<br />
americans (880 women, 650<br />
men) will die <strong>of</strong> thyroid<br />
cancer <strong>in</strong> 2007<br />
• <strong>Thyroid</strong> cancer is the<br />
fastest-ris<strong>in</strong>g cause <strong>of</strong><br />
cancer-related death <strong>in</strong> men<br />
• ¾ <strong>of</strong> annual deaths are from<br />
well-differentiated<br />
thyroid cancers<br />
Follicular<br />
27%<br />
Estimated <strong>Thyroid</strong><br />
Cancer-Related Deaths<br />
Hurthle<br />
12%<br />
Anaplastic<br />
11%<br />
Papillary<br />
50%<br />
1. American Cancer Society, Cancer Facts and Figures. 2007<br />
2. National Cancer Institute, SEER Cancer Statistics Review, 1975-2002<br />
3. Robb<strong>in</strong>s et al. Adv Intern Med. 2001; 46: 277-294<br />
4. Hundahl et al. Cancer. 1998; 83: 2638-2648<br />
1<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Cancers on the Rise:<br />
Trends <strong>in</strong> SEER Incidence Rates<br />
by Primary Cancer Site 1992-2002<br />
<strong>Thyroid</strong><br />
Liver<br />
& IBD<br />
Melanoma <strong>of</strong><br />
the Sk<strong>in</strong><br />
All Races, Males<br />
0 1 2 3 4 5<br />
2.5 *<br />
3.1 *<br />
3.0 *<br />
<strong>Thyroid</strong><br />
Liver<br />
& IBD<br />
Melanoma <strong>of</strong><br />
the Sk<strong>in</strong><br />
All Races, Females<br />
0 1 2 3 4 5<br />
2.3 *<br />
3.3 *<br />
4.8 *<br />
Annual Percentage Change Over Time<br />
Annual Percentage Change Over Time<br />
Underly<strong>in</strong>g rates are per 100,000 and age-adjusted to the 2000 U.S. standard population<br />
* The APC is significantly different from zero (p
Dr. S. L. Asa<br />
Question:<br />
1. Follicular Adenoma or<br />
2. Papillary Carc<strong>in</strong>oma?<br />
Sporadic Nodular Goiter<br />
• Mult<strong>in</strong>odular<br />
“colloid” goiter<br />
• Occasionally<br />
associated with<br />
hyperthyroidism<br />
» “Plummer’s<br />
disease”<br />
• Etiology and<br />
pathogenesis<br />
NOT understood<br />
78%<br />
22%<br />
1 2<br />
2<br />
The Answer:<br />
5 Years Later<br />
• Do we overcall many<br />
to catch this one?<br />
• Do we undercall many<br />
and miss this one?<br />
• Do we f<strong>in</strong>d scientific<br />
markers to predict<br />
behavior?<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Clonality Studies <strong>of</strong><br />
Sporadic Nodular Goiter<br />
• Dom<strong>in</strong>ant nodules <strong>of</strong>ten monoclonal<br />
• Nodules may show LOH or aberrant methylation<br />
• Multiple nodules from a s<strong>in</strong>gle goiter exhibit<br />
activation <strong>of</strong> the same allele<br />
?Diagnostic criteria<br />
Apel et al; Diagn. Mol. Pathol. 1995; 42:113-121
Dr. S. L. Asa<br />
Follicular Adenomas with<br />
Papillary Architecture<br />
• “Papillary adenomas”<br />
• Monoclonal benign neoplasms<br />
• Activat<strong>in</strong>g mutations <strong>of</strong><br />
TSH-receptor or Gsα<br />
• Plummer’s disease<br />
(Lyons et al, Science 249:635, 1990;<br />
van Sande et al,<br />
J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 80:2577, 1995)<br />
Def<strong>in</strong>itions: Capsular<br />
Invasion<br />
1. Nests, cords or cells <strong>in</strong><br />
capsule<br />
2. Islands <strong>in</strong> capsule<br />
associated with<br />
perpendicular rupture <strong>of</strong><br />
collagen<br />
3. In capsule beyond bulk<br />
<strong>of</strong> lesion<br />
4. Total thickness <strong>in</strong>to<br />
adjacent parenchyma<br />
12%<br />
12%<br />
30%<br />
47%<br />
1 2 3 4<br />
?? Artefactual trapp<strong>in</strong>g<br />
?? postFNA<br />
3<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Follicular Adenoma & Carc<strong>in</strong>oma<br />
What If There Is NO<br />
Tumor Capsule?<br />
• Capsular <strong>in</strong>vasion<br />
cannot be evaluated<br />
• Invasion must be<br />
assessed as<br />
<strong>in</strong>filtration <strong>in</strong>to<br />
surround<strong>in</strong>g<br />
parenchyma,<br />
per<strong>in</strong>eural or<br />
vascular <strong>in</strong>volvement<br />
• Encapsulated<br />
expansile growth<br />
• Malignant by<br />
capsular or<br />
vascular <strong>in</strong>vasion<br />
• Hematogenous<br />
spread
Dr. S. L. Asa<br />
Classification <strong>of</strong><br />
Follicular Carc<strong>in</strong>oma<br />
• M<strong>in</strong>imally <strong>in</strong>vasive carc<strong>in</strong>oma<br />
up to 100% 10 year survival<br />
• Widely <strong>in</strong>vasive carc<strong>in</strong>oma<br />
25-45% 10 year survival<br />
• Angio<strong>in</strong>vasive carc<strong>in</strong>oma<br />
controversial<br />
Identification <strong>of</strong> Vascular Invasion<br />
by Follicular Neoplasms<br />
• Rigid criteria<br />
predict high<br />
likelihood <strong>of</strong><br />
metastasis<br />
EVEN<br />
<strong>in</strong> differentiated<br />
thyroid carc<strong>in</strong>oma<br />
Mete and Asa, submitted<br />
4<br />
Vascular Invasion by<br />
Endocr<strong>in</strong>e Neoplasms<br />
1. Tumor cells bulg<strong>in</strong>g <strong>in</strong>to an<br />
endothelial-l<strong>in</strong>ed lumen<br />
2. Intravascular tumor nests<br />
covered with endothelium<br />
3. Tumor casts with<strong>in</strong> vessel lumen<br />
4. Thrombus adherent to <strong>in</strong>vasive<br />
tumor<br />
30%<br />
36%<br />
17% 17%<br />
1 2 3 4<br />
Papillary Carc<strong>in</strong>oma:<br />
A Cytologic Diagnosis<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
X<br />
? artificial<br />
implantation<br />
• Architecture irrelevant<br />
» Papillary, Follicular, Mixed, Solid , Cystic<br />
» Diffuse sclerosis variant is hard to recognize<br />
• Invasion not a criterion<br />
» Encapsulated variant<br />
• Nuclear features predict behavior
Dr. S. L. Asa<br />
Papillary Carc<strong>in</strong>oma<br />
Cytologic Features <strong>of</strong><br />
Papillary Carc<strong>in</strong>oma<br />
1. Enlarged, overlapp<strong>in</strong>g nuclei<br />
2. Pale vacuolated nucleoplasm with<br />
peripheral marg<strong>in</strong>ation <strong>of</strong> chromat<strong>in</strong><br />
3. Irregular nuclear membrane<br />
4. Nuclear grooves<br />
5. Nuclear pseudo<strong>in</strong>clusions<br />
14% 12%<br />
11%<br />
19%<br />
1 2 3 4 5<br />
• Often multifocal<br />
• Locally <strong>in</strong>filtrative<br />
• Lymphatic spread<br />
45%<br />
5<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Follicular Variant <strong>of</strong> Papillary Ca<br />
• Encapsulated<br />
expansile<br />
growth<br />
• Malignant by<br />
nuclear features<br />
• Often<br />
multifocal<br />
• Lymphatic<br />
spread<br />
Emer<strong>in</strong> Identifies Nuclear Features
Dr. S. L. Asa<br />
What Can Molecular <strong>Pathology</strong><br />
Teach Us<br />
About <strong>Thyroid</strong> Cancer?<br />
Markers <strong>of</strong> <strong>Thyroid</strong> Malignancy:<br />
Galect<strong>in</strong>-3<br />
• 31kD β-galactosideb<strong>in</strong>d<strong>in</strong>g<br />
lect<strong>in</strong><br />
• High percentage <strong>of</strong><br />
malignant thyroid<br />
tumors, not <strong>in</strong><br />
normal or benign<br />
lesions<br />
6<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Markers <strong>of</strong> <strong>Thyroid</strong> Malignancy:<br />
HBME-1<br />
• Monoclonal antibody<br />
• Unknown epitope<br />
• Unknown significance<br />
• Identified <strong>in</strong> 60% <strong>of</strong><br />
thyroid malignancies,<br />
not <strong>in</strong> normal or<br />
benign lesions<br />
Markers <strong>of</strong> Papillary Carc<strong>in</strong>oma:<br />
CK19<br />
• one <strong>of</strong> many kerat<strong>in</strong>s<br />
• identified diffusely <strong>in</strong> 60%<br />
<strong>of</strong> papillary carc<strong>in</strong>omas<br />
• also seen <strong>in</strong> reactive<br />
nontumorous thyroid<br />
Raphael et al, Mod Pathol. 1995;8(8):870-2
Dr. S. L. Asa<br />
Mechanisms <strong>of</strong> <strong>Thyroid</strong> Tumorigenesis<br />
TSH signal<strong>in</strong>g MAPK signal<strong>in</strong>g<br />
TSH GF<br />
TSH receptor<br />
Po<strong>in</strong>t mutation <strong>in</strong><br />
hyperfunction<strong>in</strong>g<br />
adenomas<br />
CREB<br />
Gsa<br />
PKA<br />
cAMP<br />
P<br />
CREB<br />
Adenylyl<br />
cyclase P<br />
RTK<br />
P<br />
ERK<br />
P<br />
P<br />
P<br />
ERK<br />
MEK<br />
GTP<br />
RAS<br />
BRAF<br />
Transcription<br />
Po<strong>in</strong>t mutations or<br />
rearrangement <strong>in</strong><br />
thyroid cancers<br />
Follicular cell<br />
Kondo, Ezzat and Asa, Nature Reviews Cancer 2006<br />
BRAF Mutations<br />
Cell differentiation<br />
Cell proliferation<br />
• Most common genetic event<br />
<strong>in</strong> thyroid cancer<br />
• Diagnostic marker <strong>of</strong> PTC<br />
• Genotype-phenotype correlations<br />
» BRAF V600E <strong>in</strong> classical variant PTC (common)<br />
» BRAF K601E <strong>in</strong> FVPTC (rare)<br />
» VK600-1E deletion (BRAF VK600-1E ) <strong>in</strong> solid variant<br />
(s<strong>in</strong>gle case)<br />
• Prognostic significance controversial<br />
7<br />
Follicular Adenomas with<br />
Papillary Architecture<br />
• “Papillary adenomas”<br />
• Monoclonal benign neoplasms<br />
• Activat<strong>in</strong>g mutations <strong>of</strong><br />
TSH-receptor or Gsα<br />
• Plummer’s disease<br />
Lyons et al, Science 249:635, 1990;<br />
van Sande et al,<br />
J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 80:2577, 1995<br />
Ret/PTC Rearrangements<br />
• Chromosomal rearrangement<br />
<strong>in</strong>volv<strong>in</strong>g chromosome 10 ret<br />
• Fusion <strong>of</strong> the ret tyros<strong>in</strong>e k<strong>in</strong>ase<br />
to :<br />
CCDC6 (H4) = ret/PTC1*<br />
R1α = ret/PTC2<br />
NcoA4 (ele) = ret/PTC3*<br />
» Chromosome 10 <strong>in</strong>versions<br />
most common<br />
At least 15 identified to date<br />
<strong>Thyroid</strong> <strong>Pathology</strong>
Dr. S. L. Asa<br />
Ret/PTC Rearrangements<br />
ret<br />
ret/PTC-1<br />
ret/PTC-2<br />
ret/PTC-3<br />
EC TM TK<br />
CCDC6 (H4)<br />
R1α<br />
NcoA4 (ele 1)<br />
These rearrangements result <strong>in</strong> cytoplasmic prote<strong>in</strong>;<br />
antibodies aga<strong>in</strong>st ret identify the C term<strong>in</strong>us that is conserved<br />
Different promoters drive transcript levels that modulate<br />
oncogenicity <strong>of</strong> RET/PTC oncoprote<strong>in</strong>s.<br />
Richardson et al: Cancer Res 2009;69:4861-4869.<br />
RAS Mutations Characterize<br />
Follicular Lesions<br />
• Follicular Variant PTC<br />
• Follicular Adenoma<br />
• Follicular Carc<strong>in</strong>oma<br />
• Poorly Differentiated Carc<strong>in</strong>oma<br />
8<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Methods <strong>of</strong> Ret/PTC Analysis<br />
• DNA<br />
» PCR analysis difficult due to variable break-po<strong>in</strong>t<br />
sites lead<strong>in</strong>g to heterogeneous tumor pr<strong>of</strong>iles<br />
• RNA<br />
» RT-PCR for ret/PTC mRNA is the “gold standard”<br />
» Variability <strong>of</strong> expression; not “all or none”<br />
• Prote<strong>in</strong><br />
» Immunohistochemistry us<strong>in</strong>g antisera to C term<strong>in</strong>us<br />
• FISH<br />
» Not widely available but promis<strong>in</strong>g<br />
Rhoden et al, JCEM 2006<br />
Pax 8-PPARγ 1 Fusion Oncogene<br />
• Identified <strong>in</strong> angio<strong>in</strong>vasive follicular ca<br />
Kroll TG et al, Science, 2000; 289:135<br />
• Diagnostically applicable by FISH and IHC for PPARγ<br />
• Also found <strong>in</strong> PTC Nikiforova et al: AJSP2002;26(8):1016-23
Dr. S. L. Asa<br />
CTNNB1 Mutations are Found <strong>in</strong><br />
Poorly Differentiated (Insular)<br />
<strong>Thyroid</strong> Carc<strong>in</strong>oma<br />
• Reduced membrane sta<strong>in</strong> for<br />
β-Caten<strong>in</strong> correlates with<br />
dedifferentiation<br />
• Nuclear translocation due to<br />
exon 3 mutation <strong>in</strong> 25% <strong>of</strong><br />
<strong>in</strong>sular carc<strong>in</strong>omas and 65%<br />
<strong>of</strong> anaplastic carc<strong>in</strong>omas<br />
Garcia-Rostan et al, Am J Pathol 2001;158:987<br />
p53 Alterations <strong>in</strong> <strong>Thyroid</strong> Carc<strong>in</strong>oma<br />
Mutations are common <strong>in</strong><br />
Anaplastic carc<strong>in</strong>oma ↓<br />
Immunolocalization correlates<br />
with extent <strong>of</strong> disease,<br />
extrathyroidal <strong>in</strong>volvement,<br />
recurrence and poor outcome <strong>in</strong><br />
differentiated carc<strong>in</strong>oma<br />
Hosal et al, Endocr Pathol 1997, 8:21-28<br />
9<br />
<strong>Thyroid</strong><br />
Follicular<br />
Cell<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
PIK3CA Mutations Predict<br />
Aggressive Behavior<br />
• Identified <strong>in</strong> anaplastic carc<strong>in</strong>oma<br />
» Garcia-Rostan et al, Cancer Res 2005;65:10199-207<br />
» Wang et al, JCEM 2007;92:2387-90<br />
• Accompanies other mutations <strong>in</strong> aggressive<br />
papillary carc<strong>in</strong>oma and metastases<br />
» Costa et al, Cl<strong>in</strong> Endocr<strong>in</strong>ol 2008;68:618-34<br />
» Ricate-Filho et al, Cancer Res 2009;69:4885-93<br />
Molecular Studies:<br />
Progression <strong>in</strong> <strong>Thyroid</strong> Cancer<br />
TSH-R<br />
Gs<br />
Hyperplasia<br />
BRAF<br />
RET/PTC<br />
TRK<br />
Ras<br />
Function<strong>in</strong>g<br />
Follicular<br />
Adenoma<br />
Follicular<br />
Adenoma<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
PPARγ<br />
Metastatic<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
Follicular<br />
Carc<strong>in</strong>oma<br />
Tall Cell<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
β-caten<strong>in</strong><br />
PIK3CA<br />
Insular<br />
Carc<strong>in</strong>oma<br />
β-caten<strong>in</strong><br />
PIK3CA<br />
p53<br />
Anaplastic<br />
Carc<strong>in</strong>oma
Dr. S. L. Asa<br />
What is the Cl<strong>in</strong>ical Significance <strong>of</strong><br />
Papillary Microcarc<strong>in</strong>oma?<br />
1. Potentially metastasiz<strong>in</strong>g<br />
2. Metastatic focus <strong>of</strong><br />
papillary carc<strong>in</strong>oma<br />
3. Cl<strong>in</strong>ically <strong>in</strong>significant<br />
24%<br />
11%<br />
66%<br />
1 2 3<br />
Implications <strong>of</strong> ret/PTC Data <strong>in</strong><br />
Multifocal Papillary Carc<strong>in</strong>oma<br />
• One major rationale for<br />
completion thyroidectomy<br />
<strong>in</strong> patients with “low risk”<br />
papillary carc<strong>in</strong>oma is<br />
unjustified<br />
F<strong>in</strong>k et al, Modern Pathol 1996; 9: 816-820<br />
10<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
ret/PTC <strong>in</strong><br />
Multifocal Papillary Carc<strong>in</strong>oma<br />
• ret/PTC expression is highly prevalent <strong>in</strong><br />
multifocal micropapillary thyroid cancer<br />
• Identical ret/PTC rearrangements are found <strong>in</strong> 32%<br />
<strong>of</strong> patients<br />
» possible spread <strong>of</strong> a s<strong>in</strong>gle tumor<br />
• Discordant ret/PTC patterns <strong>in</strong> 68%<br />
» discrete primary tumors<br />
Sugg et al, J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 83:4116-4122, 1998<br />
• Identical data us<strong>in</strong>g X-chromosome <strong>in</strong>activation<br />
Shattuck et al, N Engl J Med. 2005 Jun 9;352(23):2406-12<br />
Hürthle Cell Tumors<br />
• Hürthle cell adenoma,<br />
Hürthle cell carc<strong>in</strong>oma<br />
» dist<strong>in</strong>guished by<br />
<strong>in</strong>vasive behavior<br />
» controversial because <strong>of</strong><br />
unpredictable behavior<br />
• Hürthle cell PTC<br />
» def<strong>in</strong>ed by papillary<br />
architecture
Dr. S. L. Asa<br />
Molecular Basis <strong>of</strong> Hürthle Cell<br />
Papillary Carc<strong>in</strong>oma<br />
• ret/PTC identifies Hürthle cell tumors with lymph node mets<br />
» allows dist<strong>in</strong>ction from Hürthle cell adenoma<br />
» better prognosis than Hürthle cell carc<strong>in</strong>oma<br />
Cheung et al, J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 85: 878-882, 2000<br />
Molecular Diagnosis <strong>in</strong> <strong>Thyroid</strong><br />
Aspirates- Papillary Carc<strong>in</strong>oma<br />
• ret/PTC<br />
Cheung et al, J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 2001<br />
• BRAF<br />
Salvatore et al, J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 2004<br />
Improved diagnosis with comb<strong>in</strong>ed<br />
morphology and molecular test<strong>in</strong>g<br />
11<br />
mtDNA, GRIM19<br />
• Altered ATP synthesis<br />
Savagner et al, JCEM 2001;86:4920–4925<br />
• mtDNA somatic events<br />
Bonore et al, Cancer Res 2006; 66:6087–6096<br />
Gasparre et al, PNAS 2007: 104, 9001–9006<br />
• Mutations <strong>in</strong> non-neoplastic<br />
and neoplastic oncocytic cells<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
» Not specific to neoplastic transformation<br />
» Associated with BRAF, ret/PTC etc<br />
• GRIM19 (19p13.2) somatic and germl<strong>in</strong>e events<br />
Maximo et al, Virchows Arch 2000<br />
Sobr<strong>in</strong>ho-Simoes et al, Int J Surg Pathol 2005<br />
After “The Anatomy Lecture <strong>of</strong> Dr. Nicolaes Tulp” – Rembrandt, 1632<br />
(Courtesy <strong>of</strong> Dr. Carlos Cordón, New York, USA)
Dr. S. L. Asa<br />
BRAF K<strong>in</strong>ase Inhibition Arrests<br />
<strong>Thyroid</strong> Cancer Growth In Vivo<br />
Salvatore G et al, Cl<strong>in</strong> Cancer Res 2006;12:1623-9<br />
However ………<br />
Cl<strong>in</strong>ical trials have failed to show<br />
effectiveness <strong>of</strong> BRAF <strong>in</strong>hibitors<br />
Epigenetic Control: DNA Methylation<br />
N Engl J Med. 2007 Feb 15;356(7):731-3<br />
12<br />
<strong>Thyroid</strong><br />
Follicular<br />
Cell<br />
<strong>Thyroid</strong><br />
Follicular<br />
Cell<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Molecular Studies:<br />
Progression <strong>in</strong> <strong>Thyroid</strong> Cancer<br />
TSH-R<br />
Gs<br />
Hyperplasia<br />
BRAF<br />
RET/PTC<br />
TRK<br />
Ras<br />
Function<strong>in</strong>g<br />
Follicular<br />
Adenoma<br />
Follicular<br />
Adenoma<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
???????<br />
PPARγ<br />
Metastatic<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
Follicular<br />
Carc<strong>in</strong>oma<br />
Tall Cell<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
β-caten<strong>in</strong><br />
PIK3CA<br />
Insular<br />
Carc<strong>in</strong>oma<br />
β-caten<strong>in</strong><br />
PIK3CA<br />
Molecular Studies:<br />
Progression <strong>in</strong> <strong>Thyroid</strong> Cancer<br />
TSH-R<br />
Gs<br />
Hyperplasia<br />
RET/PTC<br />
BRAF<br />
TRK<br />
Function<strong>in</strong>g<br />
Follicular<br />
Adenoma<br />
Follicular<br />
Adenoma<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
PPARγ<br />
Metastatic<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
Epigenetic<br />
Dysregulation<br />
Follicular<br />
Carc<strong>in</strong>oma<br />
Tall Cell<br />
Papillary<br />
Carc<strong>in</strong>oma<br />
ras<br />
β-caten<strong>in</strong><br />
Insular<br />
Carc<strong>in</strong>oma<br />
ras<br />
β-caten<strong>in</strong><br />
p53<br />
p53<br />
Anaplastic<br />
Carc<strong>in</strong>oma<br />
Anaplastic<br />
Carc<strong>in</strong>oma
Dr. S. L. Asa<br />
Cycl<strong>in</strong> D1 and p27 Predict Metastasis<br />
<strong>in</strong> Papillary Carc<strong>in</strong>oma<br />
Khoo et al, J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 2002, 87:1814-8<br />
• CITED-1 (L)<br />
• Galect<strong>in</strong>-3<br />
• Fibronect<strong>in</strong> ( R)<br />
• HGF, MET<br />
• TPO<br />
• COX-2<br />
• CD44V6<br />
• CD57<br />
Prasad et al: Modern <strong>Pathology</strong> 2005;18:48-57<br />
13<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Vitam<strong>in</strong> D Targets p27 Degradation<br />
<strong>in</strong> <strong>Thyroid</strong> Cancer<br />
• VD/EB1089 <strong>in</strong>duce <strong>in</strong>tranuclear p27 accumulation by<br />
dim<strong>in</strong>ished degradation<br />
• VD/EB1089 hypophosphorylate p27 <strong>in</strong> a phosphatase<br />
dependent process that <strong>in</strong>volves the Akt pathway but<br />
may be PTEN <strong>in</strong>dependent<br />
Liu et al, Am J Pathol 2002;160:511-9<br />
• In an orthotopic model, <strong>in</strong> vivo VD adm<strong>in</strong>istration<br />
» decreases tumor volume<br />
» <strong>in</strong>creases p27 accumulation<br />
» enhances cellular differentiation<br />
» decreases lung metastases<br />
Dackiw et al, Endocr<strong>in</strong>ology 2004;145:5840-6<br />
Are There Other Targets <strong>of</strong> VD? Fibronect<strong>in</strong> is Upregulated <strong>in</strong><br />
Papillary <strong>Thyroid</strong> Carc<strong>in</strong>oma<br />
• Increased cDNA expression <strong>in</strong> microarray studies<br />
<strong>of</strong> papillary carc<strong>in</strong>oma cf normal<br />
• Dim<strong>in</strong>ished FN immunoreactivity reported at<br />
<strong>in</strong>vad<strong>in</strong>g edge <strong>of</strong> aggressive thyroid cancers<br />
• Negative <strong>in</strong> poorly-differentiated and anaplastic<br />
carc<strong>in</strong>omas<br />
• Function unclear<br />
» Increas<strong>in</strong>g <strong>in</strong>vasion?<br />
» Reactive upregulation?
Dr. S. L. Asa<br />
Down-regulation <strong>of</strong> FN Promotes<br />
Tumor Growth and Metastasis<br />
Control FN-siRNA<br />
Tumor volume (mm 3 )<br />
5000<br />
4500<br />
4000<br />
3500<br />
3000<br />
2500<br />
2000<br />
1500<br />
1000<br />
500<br />
0<br />
Control<br />
siRNA<br />
FN siRNA<br />
0 5 10 15 21 26<br />
Days after cancer cell <strong>in</strong>jection<br />
Mice n # <strong>of</strong> mice with mets # <strong>of</strong> lesions/mouse p<br />
Control 9 1 s<strong>in</strong>gle<br />
FN-siRNA 9 6 multiple
Dr. S. L. Asa<br />
CEACAM1 <strong>in</strong> <strong>Thyroid</strong> Cancer<br />
• CEACAM1 is expressed <strong>in</strong> a small thyroid malignancies<br />
with lymph node spread<br />
• CEACAM1 has a novel dual role <strong>in</strong> thyroid carc<strong>in</strong>oma:<br />
it suppresses thyroid cell proliferation, while promot<strong>in</strong>g<br />
<strong>in</strong>vasion and metastasis<br />
Liu et al, Oncogene 2007; 26:2747-58<br />
• VD <strong>in</strong>hibits CEACAM1 to promote <strong>in</strong>sul<strong>in</strong>/IGF-I receptor<br />
signal<strong>in</strong>g without compromis<strong>in</strong>g anti-proliferative action<br />
• CEACAM1 represents a target for VD therapy which may<br />
have potential therapeutic applications<br />
Liu et al, Lab Invest 2011 ;91(1):147-56<br />
FGFR2-IIIb Interrupts Signal<strong>in</strong>g<br />
Upstream <strong>of</strong> BRAF/MAPK<br />
Kondo et al,<br />
Cancer Res<br />
2007;67: 5461<br />
15<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
TMA Pr<strong>of</strong>il<strong>in</strong>g Shows Divergent<br />
Expression <strong>of</strong> FGFRs <strong>in</strong> the <strong>Thyroid</strong><br />
FGFR2, Normal thyroid<br />
FGFR2 is expressed<br />
exclusively <strong>in</strong> normal<br />
thyroid<br />
FGFR1, PTC<br />
FGFR1 is expressed <strong>in</strong><br />
hyperplastic and neoplastic<br />
lesions<br />
St Bernard et al, Endocr<strong>in</strong>ology 146:1145-1153, 2005<br />
FGFR2-IIIb Represses MAGE-A3/6<br />
MAGE subgroup I members , MAGE-A, B, C,<br />
are expressed <strong>in</strong> several tumors, but not <strong>in</strong><br />
normal tissues except testis and placenta<br />
“Cancer-testis antigens”<br />
Kondo et al, Cl<strong>in</strong> Cancer Res 2007;13(16):4713-20
Dr. S. L. Asa<br />
MAGE-A3 Control<br />
Time: 0 5 10 15 20 (hrs)<br />
Control<br />
MAGE-A3<br />
MAGE-A3 Promotes Migration & Invasion<br />
Control MAGE-A3<br />
Invasive Cells<br />
300%<br />
250%<br />
200%<br />
150%<br />
100%<br />
Liu et al, Cancer Res 2008;68:8104-8112<br />
50%<br />
0%<br />
C MAGE A3<br />
MAGE-A3 Promotes Metastasis<br />
Day 15 Day 20 Day 25<br />
Liu et al, Cancer Res 2008;68:8104-8112<br />
16<br />
Tumor volume (mm 3 )<br />
2500<br />
2250<br />
2000<br />
1750<br />
1500<br />
1250<br />
1000<br />
750<br />
500<br />
250<br />
0<br />
Control<br />
0 5 10 15 21<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
MAGE-A3 Enhances Tumor Growth<br />
Control MAGE-A3<br />
Tumor volume (mm 3 )<br />
6500<br />
6000<br />
5500<br />
5000<br />
4500<br />
4000<br />
3500<br />
3000<br />
2500<br />
2000<br />
1500<br />
1000<br />
500<br />
0<br />
MAGE A3<br />
*<br />
*<br />
Days after <strong>in</strong>jection<br />
*<br />
Control<br />
MAGE<br />
A3<br />
*<br />
*<br />
0 5 10 15 21 25<br />
MAGE <strong>in</strong> <strong>Thyroid</strong> Cancer<br />
*<br />
*<br />
Tumor weight (gram)<br />
Tumor weight (gram)<br />
2.5<br />
2<br />
1.5<br />
1<br />
0.5<br />
0<br />
6<br />
5.5<br />
5<br />
4.5<br />
4<br />
3.5<br />
3<br />
2.5<br />
2<br />
1.5<br />
1<br />
0.5<br />
0<br />
*<br />
N=20 N=20<br />
*<br />
N=20 N=17<br />
Control MAGE-A3<br />
• Downregulation or FN or FGFR2 <strong>in</strong>crease tumor<br />
growth and metastasis<br />
• Downregulation <strong>of</strong> FN or FGFR2 <strong>in</strong>duce expression <strong>of</strong><br />
MAGE-A3 through histone methylation<br />
• MAGE- A3 mediates p21 down-regulation,<br />
accelerated cell cycle progression, <strong>in</strong>creased cell<br />
migration rate, <strong>in</strong>vasion and metastasis<br />
• MAGE-A3 is a functional <strong>in</strong>tegrator <strong>of</strong> diverse signals<br />
<strong>in</strong> mediat<strong>in</strong>g cancer progression<br />
Liu et al, Cancer Res 2008;68:8104-8112
Dr. S. L. Asa<br />
MAGE<br />
• Normal thyroid tissue exhibits weak cytoplasmic and<br />
strong nuclear MAGE reactivity.<br />
• Tumors exhibit an <strong>in</strong>crease <strong>in</strong> cytoplasmic MAGE scores<br />
that correlates with cl<strong>in</strong>ical behavior<br />
» larger tumors have higher MAGE scores<br />
» correlation between MAGE cytoplasmic score and<br />
number <strong>of</strong> lymph node metastases<br />
Cheng et al, Endocr<strong>in</strong>e Related Cancer 2009;16:455-466<br />
BRAF Mutations & Outcome<br />
410 PTCs<br />
Cheng et al, Cl<strong>in</strong> Cancer Res 2011:17(8):2385-94<br />
17<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
Proteomic Biomarkers <strong>in</strong> PTC<br />
• 410 PTCs with morphologic and cl<strong>in</strong>ical data<br />
• BRAF status known<br />
• TMA analysis <strong>of</strong>:<br />
• Histopathologic biomarkers <strong>of</strong> malignancy:<br />
Galect<strong>in</strong>-3, CK 19, HBME-1<br />
• Cell differentiation factors: NIS, CITED-1<br />
• Nuclear receptors: ERα, ERβ, and PPAR-γ<br />
• Adhesion molecules: CEACAM-1, Osteopont<strong>in</strong>,<br />
Fibronect<strong>in</strong>, E-Cadher<strong>in</strong><br />
• Cell cycle regulators: Cycl<strong>in</strong>-D1, p53, p27, p21<br />
PTC Proteome<br />
ETE:<br />
↑membranous CK19, HBME, Gal 3,OPN<br />
↓cytoplasmic HBME , CK19<br />
↑ nuclear ERβ, Gal3, p53<br />
LNM:<br />
↑ membranous HBME1, CK19, Gal3<br />
↓ cytoplasmic FBN and CK19<br />
↑ nuclear Gal3, Erβ<br />
VI:<br />
↑ membranous Gal3<br />
↓ cytoplasmic Gal3<br />
Cheng et al, Cl<strong>in</strong> Cancer<br />
Res 2011:17(8):2385-94
Dr. S. L. Asa<br />
Proteome <strong>of</strong><br />
Invasive PTC<br />
ETE:<br />
↑membranous CK19, HBME, Gal 3,OPN<br />
↓cytoplasmic HBME , CK19<br />
↑ nuclear ERβ, Gal3, p53<br />
LNM:<br />
↑ membranous HBME1, CK19, Gal3<br />
↓ cytoplasmic FBN and CK19<br />
↑ nuclear Gal3, Erβ<br />
VI:<br />
↑ membranous Gal3<br />
↓ cytoplasmic Gal3<br />
Cheng et al, Cl<strong>in</strong> Cancer Res<br />
2011 <strong>in</strong> press<br />
Conclusions Thanks To…….<br />
• The diagnosis <strong>of</strong> thyroid cancer is evolv<strong>in</strong>g as<br />
molecular data clarify the significance <strong>of</strong><br />
morphologic features and behaviors<br />
• Our data predict the need for target<strong>in</strong>g<br />
epigenetic factors along with <strong>in</strong>tragenic mutations<br />
<strong>in</strong> the control <strong>of</strong> thyroid cancer progression.<br />
18<br />
• Robyn Apel<br />
• Lei Zheng<br />
• Sonia Sugg<br />
• Mark Khoo<br />
• Carol Cheung<br />
• Wei Liu<br />
• P. Huang<br />
• Rosanne St. Bernard<br />
• Cather<strong>in</strong>e Wei<br />
• Daniel W<strong>in</strong>er<br />
• Tetsuo Kondo<br />
• Xuegong Zhu<br />
• Sonia Cheng<br />
<strong>Thyroid</strong> <strong>Pathology</strong><br />
PTC Proteome<br />
By Morphology<br />
FVPTC:<br />
ETE:<br />
↑ membranous CK19, HBME, Gal3, OPN<br />
↓cytoplasmic CK19<br />
↑nuclear Gal3<br />
LNM:<br />
↑membranous HBME1, CK19 and Gal3<br />
↓membranous E-Cadher<strong>in</strong><br />
↓cytoplasmic HBME1, CK19, FBN<br />
↑ nuclear Gal3<br />
↓nuclear PPARγ<br />
VI:<br />
↓ nuclear PPARγ<br />
Classic PTC<br />
ETE: ↑ ERβ<br />
LNM: ↑cycl<strong>in</strong> D1, ↓FBN<br />
VI: ↓ p27<br />
• Alan Dackiw<br />
• Lorne Rotste<strong>in</strong><br />
• Ana-Maria Bamberger<br />
• Christoph Bamberger<br />
• Christoph Wagener<br />
♥ Shereen Ezzat