Surgeons Offer New Procedures for Colon and Rectal Diseases
Surgeons Offer New Procedures for Colon and Rectal Diseases
Surgeons Offer New Procedures for Colon and Rectal Diseases
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Spring, 2006<br />
<strong>Surgeons</strong> <strong>Offer</strong> <strong>New</strong> <strong>Procedures</strong> <strong>for</strong><br />
<strong>Colon</strong> <strong>and</strong> <strong>Rectal</strong> <strong>Diseases</strong><br />
Minimally invasive techniques benefit patients<br />
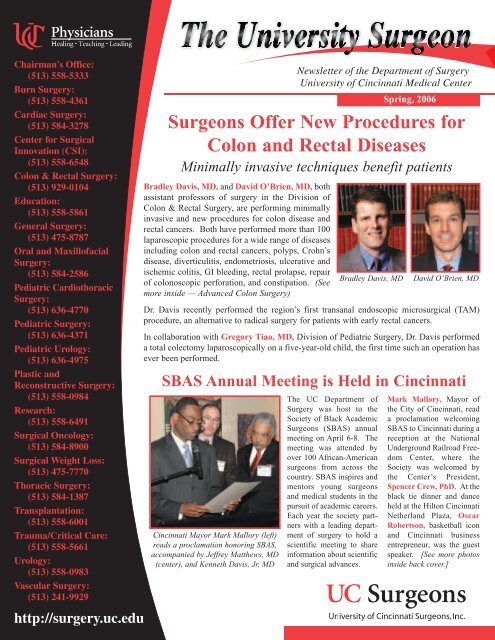
Bradley Davis, MD, <strong>and</strong> David O’Brien, MD, both<br />
assistant professors of surgery in the Division of<br />
<strong>Colon</strong> & <strong>Rectal</strong> Surgery, are per<strong>for</strong>ming minimally<br />
invasive <strong>and</strong> new procedures <strong>for</strong> colon disease <strong>and</strong><br />
rectal cancers. Both have per<strong>for</strong>med more than 100<br />
laparoscopic procedures <strong>for</strong> a wide range of diseases<br />
including colon <strong>and</strong> rectal cancers, polyps, Crohn’s<br />
disease, diverticulitis, endometriosis, ulcerative <strong>and</strong><br />
ischemic colitis, GI bleeding, rectal prolapse, repair<br />
of colonoscopic per<strong>for</strong>ation, <strong>and</strong> constipation. (See<br />
more inside — Advanced <strong>Colon</strong> Surgery)<br />
Dr. Davis recently per<strong>for</strong>med the region’s first transanal endoscopic microsurgical (TAM)<br />
procedure, an alternative to radical surgery <strong>for</strong> patients with early rectal cancers.<br />
In collaboration with Gregory Tiao, MD, Division of Pediatric Surgery, Dr. Davis per<strong>for</strong>med<br />
a total colectomy laparoscopically on a five-year-old child, the first time such an operation has<br />
ever been per<strong>for</strong>med.<br />
SBAS Annual Meeting is Held in Cincinnati<br />
Cincinnati Mayor Mark Mallory (left)<br />
reads a proclamation honoring SBAS,<br />
accompanied by Jeffrey Matthews, MD<br />
(center), <strong>and</strong> Kenneth Davis, Jr, MD<br />
Bradley Davis, MD<br />
The UC Department of<br />
Surgery was host to the<br />
Society of Black Academic<br />
<strong>Surgeons</strong> (SBAS) annual<br />
meeting on April 6-8. The<br />
meeting was attended by<br />
over 100 African-American<br />
surgeons from across the<br />
country. SBAS inspires <strong>and</strong><br />
mentors young surgeons<br />
<strong>and</strong> medical students in the<br />
pursuit of academic careers.<br />
Each year the society partners<br />
with a leading department<br />
of surgery to hold a<br />
scientific meeting to share<br />
in<strong>for</strong>mation about scientific<br />
<strong>and</strong> surgical advances.<br />
David O’Brien, MD<br />
Mark Mallory, Mayor of<br />
the City of Cincinnati, read<br />
a proclamation welcoming<br />
SBAS to Cincinnati during a<br />
reception at the National<br />
Underground Railroad Freedom<br />
Center, where the<br />
Society was welcomed by<br />
the Center’s President,<br />
Spencer Crew, PhD. At the<br />
black tie dinner <strong>and</strong> dance<br />
held at the Hilton Cincinnati<br />
Netherl<strong>and</strong> Plaza, Oscar<br />
Robertson, basketball icon<br />
<strong>and</strong> Cincinnati business<br />
entrepreneur, was the guest<br />
speaker. [See more photos<br />
inside back cover.]
Advances in <strong>Colon</strong> Surgery<br />
This year, in the United States, nearly 150,000 people will be<br />
diagnosed with colon cancer, which is the second leading cause<br />
of cancer-related deaths in the US. Fortunately, if detected <strong>and</strong><br />
treated early, colon cancer is one of the most curable cancers.<br />
The primary treatment <strong>for</strong> colon cancer is surgery. In the past,<br />
most patients underwent “open” surgery <strong>for</strong> colon cancer.<br />
However, the <strong>New</strong> Engl<strong>and</strong> Journal of Medicine recently published<br />
a l<strong>and</strong>mark National Institutes of Health (NIH) study, led<br />
by the Clinical Outcomes of Surgical Therapy (COST) Study<br />
Group that supports the use of laparoscopic-assisted colectomy<br />
<strong>for</strong> patients with colon cancer (N Engl J Med 2004; 350:2050-<br />
9). UC <strong>Surgeons</strong> Drs. Bradley Davis <strong>and</strong> David O’Brien are<br />
experts in this procedure, having each per<strong>for</strong>med more than 100<br />
laparoscopic procedures.<br />
As a result of this 10-year study, the American Society of <strong>Colon</strong><br />
<strong>and</strong> <strong>Rectal</strong> <strong>Surgeons</strong> released a supportive statement saying<br />
laparoscopic colectomy <strong>for</strong> curable cancer results in equivalent<br />
cancer-related survival to open colectomy when per<strong>for</strong>med by<br />
experienced surgeons. This surgical option now offers many of<br />
the same benefits of laparoscopic surgery over traditional open<br />
surgery, including quicker recovery time, less pain <strong>and</strong> scarring,<br />
shorter hospital stay, <strong>and</strong> improved cosmetic results. For patients<br />
whose cancer is operable, this alternative procedure is a great<br />
step <strong>for</strong>ward.<br />
During “minimally invasive” colon surgery, the surgeon makes<br />
a series of small incisions in the patient's abdomen. A small<br />
video camera (or “scope”) is placed in one of the incisions, providing<br />
a magnified view of the internal organs on a television<br />
monitor. Surgical instruments are placed in the other incisions,<br />
allowing the surgeon to work inside <strong>and</strong> remove portions of the<br />
colon. As with any surgical procedure, there are some risks. For<br />
more in<strong>for</strong>mation, log on to www.colonsurgeryinfo.com.<br />
______________<br />
In related news, Bradley Davis, MD, will be an instructor <strong>for</strong><br />
the laparoscopic colectomy course at the national meeting of the<br />
American Society of <strong>Colon</strong> <strong>and</strong> <strong>Rectal</strong> <strong>Surgeons</strong> (ASCRS), of<br />
which Janice Rafferty, MD, is program co-director. The meeting,<br />
to be held in June 2006 in Seattle, brings together more than<br />
1200 colon <strong>and</strong> rectal surgeons from around the country. This<br />
year the ASCRS will also be hosting the first allied health symposium<br />
in conjunction with the ASCRS meeting, dedicated to<br />
educating the allied health care professionals that work with<br />
members of the ASCRS. The fee <strong>for</strong> this program is $60 <strong>and</strong> registration<br />
is required. Allied Health Care professionals are welcome<br />
to attend the entire meeting. Further in<strong>for</strong>mation about the<br />
meeting is available at http://www.fascrs.org.<br />
Drs. Davis <strong>and</strong> Rafferty are presenting at the annual Crohn’s<br />
Colitis Foundation meeting of the local chapter in Cincinnati.<br />
Genetic Tests Can Help Determine<br />
Risk of <strong>Colon</strong> Cancer<br />
After two years of surgery <strong>and</strong> chemotherapy <strong>for</strong> her colon<br />
cancer, Judy Dusing’s doctors thought she might have a<br />
genetic predisposition <strong>for</strong> colon cancer. Concerned <strong>for</strong> her<br />
children, Judy decided to have genetic testing <strong>and</strong> consulted<br />
with Janice Rafferty, MD, Chief of the Division of <strong>Colon</strong><br />
<strong>and</strong> <strong>Rectal</strong> Surgery at UC. Dr. Rafferty states that published<br />
studies show “there are genes that can be detected in certain<br />
families that tend to have clusters of cancer.” While genetic<br />
testing is not practical <strong>for</strong> everyone, this simple blood test<br />
may be recommended <strong>for</strong> anyone who has had at least three<br />
relatives with colon cancer in the last two generations of their<br />
family. This is especially important if one of them is an<br />
immediate family member younger than 50 years old. Since<br />
colon cancer can be detected through precancerous polyps,<br />
anyone who tests positive should be carefully followed. “If<br />
we can find the polyps <strong>and</strong> remove them be<strong>for</strong>e the cancer<br />
develops, then we are in good shape,” said Dr. Rafferty. The<br />
amazing thing in all this <strong>for</strong> Judy Dusing was what the gene<br />
testing didn't find. “They discovered that all of my gene testing<br />
was negative.” That means she may not have passed on<br />
an additional cancer risk.<br />
Breast Cancer Trial Brings Good <strong>New</strong>s<br />
A study of almost 20,000 post-menopausal women found that<br />
the osteoporosis drug Raloxifene, also known as Evista, can<br />
help protect against breast cancer just as well as the leading<br />
breast cancer prevention drug, Tamoxifen.<br />
Elizabeth Shaughnessy, MD, PhD, Division of Surgical<br />
Oncology, directed the study section in Cincinnati. About<br />
12% of the Ohio patients were treated in Cincinnati.<br />
“I think it's very exciting because it opens up the possibilities<br />
<strong>for</strong> other women to take this medication. If one can't tolerate<br />
one drug, they can certainly switch to another.”<br />
According to Dr. Shaughnessy, the Tamoxifen appears to per<strong>for</strong>m<br />
better with invasive breast cancers, while Raloxifene<br />
poses a lower risk of uterine cancer, blood clots <strong>and</strong> cataracts.<br />
Dr. Elizabeth Shaughnessy (far left) leads a panel discussion on<br />
breast cancer at the Kingsgate Conference Center in Cincinnati
Burn Division’s Expertise is Featured<br />
Steven T. Boyce, PhD, Professor of Surgery, Division of<br />
Burn Surgery, was featured in an article in the Los Angeles<br />
Times on January 30, 2006. Dr. Boyce <strong>and</strong> his colleagues<br />
are world-renowned experts in creating artificial tissues to<br />
quickly <strong>and</strong> seamlessly patch burns <strong>and</strong> wounds.<br />
Dr. Boyce also received UC’s Established Entrepreneur<br />
Award at the Faculty Awards Celebration on May 8, 2006,<br />
sponsored by the Office of the President <strong>and</strong> Faculty<br />
Senate.<br />
Steven T. Boyce, PhD<br />
The recent construction of a new operating room at University<br />
Hospital allowed the opportunity to install videoconferencing<br />
technology that enhances patient care <strong>and</strong> resident training.<br />
The operating room (OR 20, the primary “trauma” OR), was<br />
fitted with a Stryker Communications Infinity system that is<br />
configured to connect to one of the Emergency Department<br />
(ED) bays via video through the Center <strong>for</strong> Surgical Innovation<br />
(CSI). The videoconferencing system allows the surgeon to<br />
actively see the patient's injury, request alternate views <strong>and</strong><br />
view vital signs. This enhances communication with the ED<br />
staff <strong>and</strong> provides better care <strong>for</strong> the patient.<br />
The system was successfully put into effect the week of April<br />
17. Dr. Jay Johannigman <strong>and</strong> Dr. Timothy Pritts (Division<br />
of Trauma <strong>and</strong> Critical Care) narrated two different cases: a<br />
gunshot wound <strong>and</strong> a splenectomy (the result of a car crash).<br />
W. Brian Gibler, MD, Chairman, Department of Emergency<br />
Medicine, <strong>and</strong> Jay Johannigman, MD, Director of the<br />
Division of Trauma <strong>and</strong> Critical Care, collaborated with Brett<br />
Harnett, Manager of Experimental IT <strong>for</strong> CSI, to develop the<br />
pilot system <strong>and</strong> clinical protocol, which could be fully imple-<br />
Richard J. Kagan, MD, Director of the Burn Division <strong>and</strong><br />
Chief of Staff at Shriners Hospital, in his capacity as representative<br />
<strong>for</strong> the American Burn Association developed 44 new<br />
CPT codes <strong>for</strong> application of skin grafts <strong>and</strong> skin substitutes.<br />
Kevin Yakuboff, MD, Chief of Plastic Surgery at Shriners<br />
Hospital, has begun a Brachial Plexus Clinic at the Cincinnati<br />
Children's Hospital.<br />
The staff of the Shriners Hospital-Cincinnati, which includes<br />
UC Department of Surgery faculty <strong>and</strong> residents, had 20<br />
abstracts accepted <strong>for</strong> presentation at the American Burn<br />
Association annual meeting held in Las Vegas, April 4-7, 2006.<br />
UC Burn Surgeon Treats Patient from Panama<br />
Kevin Bailey, MD (center) with<br />
members of the flight team.<br />
J. Kevin Bailey, MD, Division<br />
of Burn Surgery, traveled to<br />
Panama in February to bring a<br />
patient to Shriners <strong>for</strong> expert<br />
burn care. The 24-year-old<br />
Panamaniam was injured at<br />
work; his employer searched the<br />
U.S. to find a burn unit that<br />
would care <strong>for</strong> him without burdening<br />
the family <strong>and</strong> company<br />
with extensive medical bills.<br />
Shriners stepped in <strong>and</strong> accepted<br />
the patient, who was recently<br />
discharged home to Panama.<br />
University Hospital <strong>and</strong> CSI Exp<strong>and</strong> OR Videoconferencing Capabilities<br />
mented in the remaining ED bays by this summer.<br />
In addition to patient care advantages, video <strong>and</strong> audio footage<br />
can be stored <strong>and</strong> used <strong>for</strong> training purposes, while following<br />
all HIPAA regulations.<br />
The system is extremely af<strong>for</strong>dable <strong>and</strong> scalable. By using the<br />
Health Alliance's existing videoconferencing technology <strong>and</strong><br />
local area network (LAN) with inexpensive software <strong>and</strong> hardware,<br />
Harnett <strong>and</strong> CSI were able to design a system with many<br />
of the same advantages, but at a more reasonable cost.
Bower Memorial on June 21, 2006<br />
Please join us <strong>for</strong> Final Gr<strong>and</strong> Rounds on June 21st at 8:00 a.m. in the Surgical Amphitheater to celebrate the graduation of our<br />
general surgery chief residents <strong>and</strong> <strong>for</strong> the unveiling of the portrait of Dr. Robert H. Bower <strong>and</strong> dedication of the conference room.<br />
Dr. Bower’s portrait will be presented at Final Gr<strong>and</strong> Rounds with a ribbon cutting <strong>and</strong> inauguration of the Bower Memorial<br />
Conference Room to be held in the Chairman’s office immediately following Gr<strong>and</strong> Rounds. A reception in the Department of<br />
Surgery will follow. All faculty, alumni <strong>and</strong> community physicians are invited to attend.<br />
Cardiothoracic Surgery <strong>New</strong>s<br />
Walter H. Merrill, MD,<br />
Director of the Section of<br />
Cardiothoracic Surgery, played<br />
a major role at the annual<br />
meeting of the Society of<br />
Thoracic <strong>Surgeons</strong>. In addition<br />
to his two presentations<br />
(“Technique of intraoperative<br />
electrophysiologic mapping<br />
<strong>and</strong> identification of ganglionic<br />
plexi” <strong>and</strong> “Interim report of<br />
the Society of Thoracic<br />
Dr. Walter Merrill <strong>Surgeons</strong> Task Force on resident<br />
employment opportunities”), Dr. Merrill presided over<br />
the Thoracic Surgery Resident Luncheon panel entitled<br />
“Today’s Job Market: How to Look <strong>and</strong> What's in Dem<strong>and</strong>”<br />
<strong>and</strong> also moderated the “Adult Cardiac Case Presentation”<br />
Session.<br />
Dr. Flege Wins “Lifetime Hero” Award<br />
John B. Flege, Jr, MD,<br />
Professor of Surgery in the<br />
Division of Cardiac Surgery,<br />
was honored as a “Lifetime<br />
Hero” <strong>for</strong> his years of service<br />
to the community. Dr. Flege<br />
received the Cincinnati<br />
Dr. John B. Flege, Jr.<br />
Business Courier's Lifetime<br />
Health Care Hero award at the<br />
dinner on February 9. Dr.<br />
Flege is considered to be the<br />
“father of cardiac surgery” in<br />
the Cincinnati area. Dr. Flege<br />
gratefully acknowledged the<br />
support of the many nurses <strong>and</strong><br />
hospital staff who helped him build cardiac surgery programs<br />
at Jewish Hospital, Christ Hospital, University Hospital, <strong>and</strong><br />
St. Elizabeth Hospital in Northern Kentucky.<br />
R<strong>and</strong>all Wolf, MD, Professor of Surgery <strong>and</strong> Biomedical<br />
Engineering, <strong>and</strong> Director of the UC Center <strong>for</strong> Surgical<br />
Innovation (CSI), won the Innovator award. E. Steve<br />
Woodle, MD, Professor of Surgery <strong>and</strong> Director of the<br />
Division of Transplantation, was a nominee.<br />
Screening Chest CT Can Identify Early-Stage<br />
Lung Cancer in High-Risk Individuals<br />
Early results from the Lung Cancer Screening Study directed by<br />
John A. Howington, MD, Associate Professor of Surgery <strong>and</strong><br />
Chief of the Division of Thoracic Surgery, have shown that spiral<br />
CT (computed tomography) of high-risk individuals can identify<br />
early-stage lung cancer. The clinical implications are that early<br />
diagnosis allows surgical resection that is often curative.<br />
The study, from August 2001 through April 2005, included 131<br />
high-risk individuals over 50 years old with a minimum 20 packyear<br />
smoking history, but without symptomatic lung cancer at the<br />
time of screening or a history of cancer in the past five years. Fiftysix<br />
percent had at least one non-calcified nodule. Five subjects had<br />
nodules greater than 12 mm <strong>and</strong> four underwent biopsy. Three<br />
patients had stage IA non-small cell lung cancer (NSCLC) <strong>and</strong> one<br />
had stage IIIA NSCLC. All patients diagnosed with lung cancer<br />
underwent complete resections: 2 VATS lobectomies, 1 open lobectomy,<br />
<strong>and</strong> 1 open bilobectomy. There was no operative mortality.<br />
To date, no volunteer has undergone biopsy <strong>for</strong> a benign nodule.<br />
The study was conducted by Dr. Howington <strong>and</strong> Michael F. Reed,<br />
MD, Division of Thoracic Surgery; surgical residents Lynn (Chip)<br />
Huffman, MD, <strong>and</strong> Prakash K. P<strong>and</strong>alai, MD; thoracic nurse<br />
Jeffrey Neu; members of the Division of Pulmonary <strong>and</strong> Critical<br />
Care Medicine <strong>and</strong> Division of Hematology & Oncology,<br />
Department of Internal Medicine, <strong>and</strong> the Department of Radiology.<br />
Dr. Huffman won First Place <strong>for</strong> the abstract in the Cincinnati<br />
Surgical Society's 2005-2006 Resident Essay Competition.<br />
John Mehall, MD, cardiothoracic surgery<br />
resident, presented at the annual meeting of<br />
the Society of Thoracic <strong>Surgeons</strong>, <strong>and</strong> his<br />
comments on job opportunities <strong>for</strong> thoracic<br />
surgery residents were featured in the<br />
March/April issue of Thoracic Surgery<br />
<strong>New</strong>s. Dr. Mehall is President of the<br />
Thoracic Surgery Residents Association, as<br />
well as Program Director <strong>for</strong> the upcoming Dr. John Mehall<br />
Cardiothoracic Technology Symposium<br />
designed <strong>for</strong> thoracic surgery residents in accredited programs, to<br />
be held May 19-21, 2006, at the University of Cincinnati Center<br />
<strong>for</strong> Surgical Innovation (CSI) <strong>and</strong> Kingsgate Conference Center.<br />
For more in<strong>for</strong>mation, visit www.ctsymposium.org.
Center <strong>for</strong> Surgical Innovation (CSI) in the <strong>New</strong>s<br />
Advanced Center <strong>for</strong> Telemedicine <strong>and</strong> Surgical<br />
Innovation (ACTSI)<br />
The ACTSI was funded by the UC Congress through a grant<br />
with the US Army's Telemedicine <strong>and</strong> Advanced Technology<br />
Research Center (TATRC). Timothy Broderick, MD, is the<br />
Principal Investigator (PI) <strong>and</strong> Director of ACTSI. Mr. Charles<br />
Doarn serves as Co-PI <strong>and</strong> Deputy Director. The focus is on<br />
telesurgery <strong>and</strong> the tools <strong>and</strong> capabilities that enable advanced<br />
medical <strong>and</strong> surgical care on the battlefield. As ACTSI grows in<br />
stature <strong>and</strong> capability, the concept of “benchtop to battlefield to<br />
bedside” will be fully integrated across UC’s medical campus<br />
<strong>and</strong> academic campus through mutually beneficial collaborations<br />
between basic sciences, engineering <strong>and</strong> medical practices.<br />
ACTSI will utilize numerous assets, including the CSI.<br />
Atrial Fibrillation Innovation Center (AFIC)<br />
R<strong>and</strong>all K. Wolf, MD, <strong>and</strong> UC have teamed with the Clevel<strong>and</strong><br />
Clinic Foundation (CCF) to establish the Atrial Fibrillation<br />
Innovation Center (AFIC) through a three-year $22.8M grant<br />
from the State of Ohio. A Joint Use Agreement was established<br />
between UC <strong>and</strong> the CCF to implement the AFIC project. The<br />
CSI has a significant science component with Dr. Wolf serving<br />
as PI. His research will focus on minimally invasive surgical<br />
technologies <strong>for</strong> the treatment of atrial fibrillation, including<br />
robotic applications. Dr. Wolf will serve as a member of the<br />
AFIC Board of Directors.<br />
4th BME-Surgery Symposium - “Nanotechnology”<br />
On January 20, 2006, the Department of Surgery, the<br />
Department of Biomedical Engineering (BME), the Department<br />
of Electrical <strong>and</strong> Computer Engineering <strong>and</strong> Computer Science<br />
(ECECS), <strong>and</strong> the CSI hosted the fourth Surgery-BME seminar,<br />
“Clinical Applications of Biomedical Engineering in the<br />
Surgical Environment: Nanotechnology.” The focus on<br />
nanoscale science <strong>and</strong> technology in medicine provided a foundation<br />
<strong>for</strong> dynamic presentations from faculty of several interdisciplinary<br />
departments, including Chemistry, Pharmacology,<br />
Engineering, Surgery <strong>and</strong> Electrical Engineering from both UC<br />
<strong>and</strong> Cincinnati Children's Hospital Medical Center. Dr. Jennifer<br />
West from Rice University's Department of Biomedical<br />
Engineering was guest faculty <strong>and</strong> presented “Future Directions<br />
in Applied Nanoscience.” Dr. William Ball, Dr. Thomas Mantei,<br />
<strong>and</strong> Dr. R<strong>and</strong>all Wolf served as symposium chairs. More than<br />
70 people attended the seminar, including faculty <strong>and</strong> students<br />
from UC’s medical <strong>and</strong> academic campuses.<br />
Faculty Research Grant Awarded<br />
Brett Harnett, Manager of Experimental In<strong>for</strong>mation<br />
Technology, had his Faculty Research Grant approved by the<br />
University Research Council. His research focus is “A Mobile<br />
Neural Network <strong>for</strong> Real-Time Physiologic Monitoring.”<br />
NEEMO Educational Outreach <strong>Offer</strong>s Children <strong>and</strong><br />
Adults Opportunity to Speak with Underwater Crew<br />
A live event was held at the Cincinnati Museum Center on<br />
Monday, April 10, 2006, at which nearly 300 children were<br />
invited to speak directly with NASA’s Extreme Environment<br />
Mission Operations 9 (NEEMO 9) undersea crew, featuring<br />
Timothy J. Broderick, MD, NASA astronauts Ronald Garan<br />
<strong>and</strong> Nicole Stott; Canadian astronaut <strong>and</strong> mission comm<strong>and</strong>er,<br />
Dave Williams, MD, <strong>and</strong> habtechs Jim Buckley <strong>and</strong> Ross Hein,<br />
who were living <strong>for</strong> 18 days at 75 feet below the surface of the<br />
ocean near Key Largo, FL. Dr. Broderick served as crew chief<br />
<strong>and</strong> conducted robotic surgical research that will someday help<br />
treat astronauts on the Moon <strong>and</strong> Mars. In the short term, this<br />
technology is used everyday to take better care of patients.<br />
Live interaction with NEEMO 9 crew at the Cincinnati Museum Center<br />
3rd Advances in Laparoscopic Hepatic Surgery Course<br />
The CSI worked closely with Joseph Buell, MD, <strong>and</strong> the<br />
Division of Transplantation to conduct the third “Advances in<br />
Laparoscopic Hepatic Surgery” course, February 23-25, 2006.<br />
Attendees from the around the world participated in a two-<strong>and</strong>a-half-day<br />
course on issues <strong>and</strong> technologies <strong>for</strong> supporting<br />
laparoscopic hepatic surgery. The course involved both didactic<br />
lectures <strong>and</strong> h<strong>and</strong>s-on laboratory experience during which the<br />
participants tested <strong>and</strong> evaluated various technologies.<br />
Participants in the “Advances in Laparoscopic Hepatic Surgery” course
Vascular Surgeon Reports That Delayed<br />
Repair May Be Better <strong>for</strong> Aortic Injuries<br />
Patients who survive the first 24 hours of a blunt aortic trauma<br />
injury may have a better chance of long-term survival if repair to<br />
the damaged artery is delayed, according to vascular surgeons at<br />
the University of Cincinnati.<br />
The finding was reported by Amy B. Reed, MD, Assistant<br />
Professor of Surgery in the Division of Vascular Surgery, at the<br />
Midwestern Vascular Surgical Society in Chicago, September 15,<br />
2005, <strong>and</strong> recently published.in the April 2006 edition of the<br />
Journal of Vascular Surgery (volume 43, pp. 684-688).<br />
Dr. Amy B. Reed<br />
A severe blunt thoracic injury, often<br />
the result of sudden deceleration<br />
experienced in an auto accident, can<br />
jerk the aorta <strong>for</strong>ward <strong>and</strong> back again,<br />
causing it to crack. “The real problem<br />
is that most people die from blunt<br />
thoracic aortic trauma be<strong>for</strong>e ever<br />
reaching a hospital, <strong>and</strong> about 50% of<br />
those who do make it will die within<br />
a few hours,” Dr. Reed said.<br />
“Un<strong>for</strong>tunately, even if the aorta is repaired immediately, the<br />
patient almost always has other, equally life-threatening injuries<br />
that jeopardize their overall recovery <strong>and</strong> survival.”<br />
Dr. Reed <strong>and</strong> her colleagues analyzed 51 cases of blunt thoracic<br />
aortic trauma treated at University Hospital, including severity of<br />
accompanying injuries, time from trauma to repair, surgical<br />
method (open versus endovascular) <strong>and</strong> survival outcomes. Of<br />
the 24 patients who made it to the operating room, 13 (54%) were<br />
stabilized <strong>and</strong> then had successful delayed endovascular repair.<br />
Nine patients (38%) had immediate open repair, one of whom<br />
died during the procedure. Two patients (8%) had delayed open<br />
repair.<br />
“This data suggests that in some cases it is better to wait <strong>and</strong><br />
repair the thoracic aortic injury with the minimally invasive<br />
(endovascular) technique,” Dr. Reed said. “If surgeons can take<br />
care of other injuries (such as bleeding liver or serious head<br />
injury) first <strong>and</strong> then safely address the thoracic aortic trauma<br />
injury when the patient is stabilized, there will be a better chance<br />
of surviving.”<br />
Co-authors of the study include Charles (Chip) Crafton, Cindy<br />
Delvecchio, Dr. Joseph Giglia, <strong>and</strong> Dr. J. Keith Thompson.<br />
UC <strong>Surgeons</strong> at Cancer Education Day<br />
Several UC <strong>Surgeons</strong> provided expert commentary <strong>and</strong> the<br />
latest in<strong>for</strong>mation about preventing, detecting <strong>and</strong> treating all<br />
types of cancer at the 2nd Annual Community Cancer<br />
Education Day on March 25. Faculty spoke one-on-one with<br />
the public about cancer concerns <strong>and</strong> provided Q&A sessions<br />
<strong>and</strong> panel discussions. “The goal is to give people the in<strong>for</strong>mation<br />
they want <strong>and</strong> need in the fight against cancer,” said<br />
Elizabeth Shaughnessy, MD, PhD, Assistant Professor of<br />
Surgery in the Division of Surgical Oncology.<br />
Elizabeth Shaughnessy, MD, PhD, Division of Surgical Oncology,<br />
leads a panel discussion at UC’s Cancer Education Day<br />
S<strong>and</strong>ra Starnes, MD, Division of Thoracic Surgery,<br />
speaks with visitors at UC’s Cancer Education Day<br />
Surgeon Wins “Spirit of Caring” Award<br />
Kevin Yakuboff, MD, Chief of Plastic<br />
Surgery at Shriners Hospitals <strong>for</strong><br />
Children, was recently named 2006<br />
Spirit of Caring honoree. Dr. Yakuboff<br />
has been with the hospital since 1988.<br />
Dr. Yakuboff was recognized <strong>for</strong> “his<br />
Kevin Yakuboff, MD<br />
numerous contributions over the years<br />
to plastic surgery <strong>and</strong> burn patients <strong>and</strong><br />
his commitment to delivering outst<strong>and</strong>ing medical care to the<br />
patients in a caring <strong>and</strong> empathetic way.” Dr. Yakuboff was<br />
also recognized as a valuable resource in situations requiring<br />
his expertise in reconstructive <strong>and</strong> h<strong>and</strong> surgery as well as his<br />
ability to h<strong>and</strong>le difficult patient issues with compassion.<br />
The Spirit of Caring Award recognizes Shrine employees who<br />
demonstrate an exemplary level of caring <strong>and</strong> acknowledges<br />
outst<strong>and</strong>ing employee contributions towards fulfilling the<br />
mission of providing superior care at the Cincinnati hospital.
Dr. J. Wesley Alex<strong>and</strong>er<br />
Awards <strong>and</strong> Achievements<br />
J. Wesley Alex<strong>and</strong>er, MD, ScD, Professor of Surgery, Division of Transplantation, was a grant reviewer <strong>for</strong><br />
the National Institutes of Health <strong>for</strong> a Special Emphasis Panel/Scientific Review Group meeting in February.<br />
Ambikaipakan Balasubramaniam, PhD, Professor of Surgery <strong>and</strong> Director of the<br />
Peptide Laboratory, was a member of the organizing committee of the 8th<br />
International NPY meeting entitled “Neuropeptide Y <strong>and</strong> Cohorts in Human<br />
<strong>Diseases</strong>” held April 22-26, 2006, in St. Petersburg, FL. He chaired a session <strong>and</strong> presented<br />
a talk entitled “Peripherally active anorectic peptides based on NPY.” Dr.<br />
Balasubramaniam also is a member of the Editorial Board <strong>for</strong> the meeting proceedings<br />
to be published in a special issue of Peptides (Elsevier Press).<br />
Joseph S. Giglia, MD, Interim Director of the Division of Vascular Surgery, is the Dr. A. Balasubramaniam<br />
recipient of the 2006 Lifeline E.J. Wylie Memorial Traveling Fellowship from the<br />
American Vascular Association. Dr. Giglia will be presented with the award at the Annual Meeting of the<br />
Society <strong>for</strong> Vascular Surgery in June, 2006. The fellowship provides funds <strong>and</strong> opportunities to travel to<br />
other centers of excellence to learn new advances in vascular surgery.<br />
Alex B. Lentsch, PhD, Director of Research, is serving as a member of the National<br />
Institutes of Health Study Section, Hepatobiliary Pathophysiology. This study sec-<br />
Dr. Joseph Giglia tion reviews grant applications about the cell biology of liver cells; mechanisms of<br />
repair <strong>and</strong> regeneration; mechanisms of cell death <strong>and</strong> inflammation; cholesterol <strong>and</strong><br />
bile salt metabolism; fibrosis <strong>and</strong> cirrhosis; <strong>and</strong> viral hepatitis <strong>and</strong> liver transplantation. In May, 2006, Dr.<br />
Lentsch will be visiting professor at the Borgess Research Institute in Kalamazoo, Michigan, where he will<br />
present at the Trauma Services Gr<strong>and</strong> Rounds on the topic of ischemia/reperfusion injury.<br />
(L-R) Dr. M. Anthony Pogrel, Chair of Oral &<br />
Maxillofacial Surgery at UCSF, Dr. Robert D. Marciani,<br />
<strong>and</strong> Dr. William Ware following Dr. Marciani’s<br />
presentation of the William Ware Lecture<br />
Dr. Janice Rafferty<br />
Robert D. Marciani, DMD, Chief of the Division of Dr. Alex Lentsch<br />
Oral <strong>and</strong> Maxillofacial Surgery, was a visiting professor<br />
<strong>and</strong> the William Ware lecturer in January 2006 at the University of Cali<strong>for</strong>nia,<br />
San Francisco (UCSF).<br />
Michael S. Nussbaum, MD, FACS, Associate Professor<br />
of Surgery, Vice Chair <strong>for</strong> Clinical Affairs <strong>and</strong> Chief of<br />
Staff of The University Hospital, completed his four-year<br />
term on the Board of Directors of the American Board of<br />
Emergency Medicine (ABEM) on February 3, 2006.<br />
During his tenure on ABEM, Dr. Nussbaum served on the<br />
Assessment of Practice Per<strong>for</strong>mance, Test Development,<br />
<strong>and</strong> Credentials Committees. Dr. Nussbaum was recent-<br />
Dr. Michael Nussbaum<br />
ly elected Secretary of the Central Surgical Association<br />
<strong>for</strong> 2006-2009 <strong>and</strong> will serve as Local Program Director <strong>for</strong> the annual meeting<br />
to be held in Cincinnati in 2007.<br />
Janice Rafferty, MD, Chief of the Division of <strong>Colon</strong> <strong>and</strong> <strong>Rectal</strong> Surgery, is the program co-chair <strong>for</strong> the<br />
national meeting of American Society of <strong>Colon</strong> <strong>and</strong> <strong>Rectal</strong> <strong>Surgeons</strong> (ASCRS) to be held in June 2006 in<br />
Seattle. The meeting brings together more than 1,200 colon <strong>and</strong> rectal surgeons from around the country.<br />
Amy B. Reed, MD, Assistant Professor of Surgery <strong>and</strong> Director of the Vascular<br />
Surgery Fellowship Program, was named one of 15 “Businesswomen to Watch” by<br />
the Cincinnati Enquirer on January 29, 2006. Dr. Reed also was an invited speaker<br />
at the local program of the recent Society of Black Academic <strong>Surgeons</strong> meeting in<br />
Cincinnati, where she spoke on “Vascular Surgery Training in the 21st Century.”<br />
Dr. Amy Reed
Urology <strong>New</strong>s<br />
NEW UROLOGY FACULTY HAS EXPERTISE IN MICROSURGERY<br />
Dr. Ahmad Hamidinia<br />
Ahmad Hamidinia, MD, has joined UC <strong>Surgeons</strong> as Clinical Professor of Urology in the Division of<br />
Urology. Dr. Hamidinia specializes in urologic microsurgery <strong>and</strong> medical treatment of male reproductive<br />
evaluation as well as medical <strong>and</strong> surgical treatment (minimally invasive sling procedures <strong>and</strong> pelvic floor<br />
reconstructive procedures) <strong>for</strong> female incontinence.<br />
Dr. Hamidinia received his medical degree from the University of Mashhad School of Medicine in Mashhad,<br />
Iran. He served his general surgery residency at Bridgeport Hospital (affiliated with Yale University) in<br />
Bridgeport, CT. Dr. Hamidinia completed his urology residency at Southern Illinois University in<br />
Springfield, IL, where he served on faculty <strong>for</strong> nine years. He served as Chairman of the Section of Urology<br />
at Miami Valley Hospital <strong>and</strong> most recently was Clinical Associate Professor at Wright State University.<br />
Dr. Hamidinia has won several research <strong>and</strong> teaching awards. He is a member of the American Urology Association, American<br />
Fertility Society, American Association of Clinical Urologists, Ohio Urological Society, <strong>and</strong> a Fellow of the American College of<br />
<strong>Surgeons</strong>. He has been invited to teach <strong>and</strong> per<strong>for</strong>m surgery in China the past four years. Dr. Hamidinia has published articles<br />
on microsurgical techniques <strong>and</strong> fertility disorders, in addition to several book chapters <strong>and</strong> videotape presentations.<br />
Dr. Hamidinia is certified by the American Board of Urology. He will see patients at the Medical Arts Building <strong>and</strong> at University<br />
Pointe. Dr. Hamidinia may be reached at (513) 475-8787.<br />
Inaugural Arthur T. Evans Visiting Professor<br />
The Division of Urology hosted the first annual Arthur T.<br />
Evans Visiting Professor in memory of Dr. Evans, a <strong>for</strong>mer<br />
director of the Division of Urology, on Wednesday, February<br />
15, 2006. Kevin T. McVary, MD, Professor of Urology at the<br />
Feinberg School of Medicine, Northwestern University, spoke<br />
at Surgical Gr<strong>and</strong> Rounds on “The Molecular Biology of<br />
Erectile Dysfunction: From Cavernous Nerve Injury to Sonic<br />
Hedgehog.” A memorial fund has also been established in Dr.<br />
Evans’ name to further the training of urology residents.<br />
<strong>New</strong> Research Awards<br />
Glendon Zinser, PhD,<br />
<strong>and</strong> Susan Waltz, PhD<br />
Urology residents <strong>and</strong> faculty with Kevin T. McVary, MD (fifth from left), the<br />
first Annual Arthur T. Evans Visiting Professor, at Surgical Gr<strong>and</strong> Rounds<br />
Glendon Zinser, PhD, post-doctoral fellow in the Division of Research, was awarded a Scholars<br />
Grant from UC's Building Interdisciplinary Research Careers in Women's Health (BIRCWH) program.<br />
Directed by Drs. Ken Clark <strong>and</strong> Leslie Myatt of the Department of Obstetrics <strong>and</strong> Gynecology,<br />
the BIRCWH program promotes the career development of independent junior researchers working<br />
on women's health issues by pairing scholars with senior investigators in a mentored, interdisciplinary<br />
scientific environment. Dr. Zinser, working under the mentorship of<br />
associate professor Susan Waltz, PhD, will focus on the cross-talk of nuclear<br />
hormone receptors <strong>and</strong> cell surface receptor tyrosine kinases in breast cancer.<br />
The BIRCWH program was enabled by a five-year, $2.5 million grant award<br />
to the Department of Obstetrics <strong>and</strong> Gynecology by the National Institutes of<br />
Health Office of Research on Women's Health.<br />
Karl Matlin, PhD, Director of Research, received a five-year R01 grant award fron the National Institutes<br />
of Health <strong>for</strong> his project “Cell-Matrix Interactions in Epithelial Polarization” to begin May 1, 2006.<br />
Karl Matlin, PhD
Ahmad SA, Wray C, Rilo HR, Choe KA, Gelrud A,<br />
Howington JA, Lowy AM, Matthews JB. Chronic pancreatitis:<br />
Recent advances <strong>and</strong> ongoing challenges. Current Problems<br />
in Surgery 43(3):124-238, 2006.<br />
In this invited monograph, faculty members from the UC<br />
Department of Surgery <strong>and</strong> the UC Pancreatic Disease Center<br />
provide an excellent reference to physicians <strong>and</strong> surgeons who<br />
wish to gain a more comprehensive underst<strong>and</strong>ing of chronic<br />
pancreatitis <strong>and</strong> its treatment. Subscribers can see the full text<br />
online at http://www.sciencedirect.com.<br />
Alex<strong>and</strong>er JH, Ferguson TB, Joseph DM, Mack MJ, Wolf RK,<br />
et al. The project of ex-vivo vein graft engineer via transfection<br />
IV (PREVENT IV) trial: study rationale, design, <strong>and</strong> baseline<br />
patient characteristics. Am Heart Journal 150:643-649, 2005.<br />
Alex<strong>and</strong>er JW, Goodman HR, Alloway RR, Woodle ES. Can<br />
immunonutrients reduce rejection rates in African-Americans?<br />
Exp Clin Transplant 3:349-350, 2005.<br />
Amlal H, Faroqui S, Balasubramaniam A, Sheriff S.<br />
Estrogen up-regulates neuropeptide Y Y1 receptor expression in<br />
a human breast cancer cell line. Cancer Research 66:3706-<br />
3714, 2006.<br />
The high incidence <strong>and</strong> activity of the Y1 receptor in human<br />
breast tumor cells suggests that it may play an important role in<br />
breast cancer.<br />
Chance WT, Dayal R, Friend LA, Sheriff S. Possible role of<br />
CRF peptides in burn-induced hypermetabolism. Life Sciences<br />
78:694-703, 2006.<br />
Davis BR, Matthews JB. Diverticular disease of the colon. In:<br />
Wolfe MM, Davis GL, Farraye FA, et al (eds), Therapy of<br />
Digestive Disorders, 2nd edition. Philadelphia: Elsevier, 2006;<br />
pp. 855-869.<br />
Doarn CR, Merrell RC. A look ahead [Editorial]. Telemed <strong>and</strong><br />
E Health 12:1, 2005.<br />
Doarn CR, Merrell RC. Telemedicine <strong>and</strong> e-health <strong>for</strong> international<br />
medical issues [Editorial]. Telemed <strong>and</strong> E Health 11:621-<br />
623, 2005.<br />
Doarn CR, Justis D, Chaudhri MS, Merrell RC. Integration of<br />
telemedicine practice into correctional medicine: An evolving<br />
st<strong>and</strong>ard. J Correctional Health Care 11:253-270, 2005.<br />
Doarn CR, Merrell RC. Changing of the guard [Editorial].<br />
Telemed <strong>and</strong> E Health 11:415-416, 2005.<br />
Doarn CR, Nicogossian AE, Merrell RC. Telematic support <strong>for</strong><br />
Recent Publications<br />
disaster situation. In: Istepanian RSH, Laxminarayan S,<br />
Pattichis CS (eds), M-Health: Emerging Mobile Health Systems.<br />
<strong>New</strong> York: Springer Science+Business Media, Inc., 2006; pp.<br />
549-559.<br />
Gillinov AM, Wolf RK. Surgical ablation of atrial fibrillation.<br />
Prog Cardiovasc Dis 48:169-177, 2006.<br />
Hanly EJ, Marohn MR, Schenkman NS, Miller BE, Moses GR,<br />
Marchessault R, Broderick TJ. Dynamics <strong>and</strong> organizations of<br />
telesurgery. European Surgery 37:274-278, 2005.<br />
Harnett BM. Telemedicine systems <strong>and</strong> telecommunications.<br />
J Telemedicine <strong>and</strong> Telecare 12:4-15, 2006.<br />
Husted TL, Broderick TJ. NASA <strong>and</strong> the emergence of new<br />
surgical technologies. J Surg Res 132:13-16, 2006.<br />
Merrell RC, Doarn CR. Disasters - How can telemedicine help?<br />
[Editorial] Telemed <strong>and</strong> E Health 11:511-512, 2005.<br />
Reed AB, Thompson JK, Crafton CJ, Delvecchio C, Giglia<br />
JS. Timing of endovascular repair of blunt traumatic thoracic<br />
aortic transections. J Vasc Surg 43:684-688, 2006.<br />
Shen H, Schuster R, Stringer KF, Waltz SE, Lentsch AB. The<br />
Duffy antigen/receptor <strong>for</strong> chemokines (DARC) regulates<br />
prostate tumor growth. FASEB Journal 20:59-64, 2006.<br />
This paper describes an important role <strong>for</strong> this receptor (the<br />
DARC) in controlling the development of prostate cancer. The<br />
majority of African-Americans lack this receptor, <strong>and</strong> this study<br />
suggests that the lack of the DARC may be an important contributing<br />
factor to the higher incidence <strong>and</strong> mortality of prostate<br />
cancer in African-American men.<br />
Thompson JK, Reed AB, Giglia JS. Novel endovascular treatment<br />
of blunt thoracic aortic trauma with a self-exp<strong>and</strong>ing stent<br />
lined with aortic extender cuffs. Ann Vasc Surg March 21, 2006<br />
[Epub ahead of print].<br />
The authors report successful treatment of blunt thoracic aortic<br />
trauma with a self-exp<strong>and</strong>ing stent lined with commercially<br />
available aortic extender cuffs. This technique could still have<br />
utility in emergency settings when approved thoracic endografts<br />
are available <strong>for</strong> this indication.<br />
Nicogossian AE, Lugg DJ, Doarn CR. Civilian telemedicine in<br />
remote <strong>and</strong> extreme environments. In: Istepanian RSH,<br />
Laxminarayan S, Pattichis CS (eds), M-Health: Emerging<br />
Mobile Health Systems. <strong>New</strong> York: Springer Science+ Business<br />
Media, Inc., 2006; pp. 517-529.<br />
Wolf RK. A perspicacious view. Innovations 1(1):1-2, 2005.
Surgical Education <strong>New</strong>s<br />
Victim of Hurricane Katrina Finds a<br />
<strong>New</strong> Home in UC Surgical Residency<br />
Jerry Fortuna, MD, who was displaced by Hurricane Katrina from his<br />
surgical residency program at Keesler Air Force Base in Biloxi,<br />
Mississippi, was invited to continue his training in the UC Department<br />
of Surgery’s residency training program. This is his story:<br />
“A native of Columbia, South Carolina, I graduated from the US Air<br />
Force Academy in 1995. I attended the University of South Carolina<br />
School of Medicine, where I graduated in 1999 <strong>and</strong> completed my<br />
internship in 2000. I have spent the last 5 years as an active duty Flight<br />
Surgeon assigned to a combat coded F-15C fighter squadron. After<br />
multiple tours of duty in the Middle East, I re-entered residency training<br />
at Keesler AFB in Biloxi, MS. Very soon, however, Hurricane Katrina<br />
rendered the hospital non-operational <strong>and</strong> the residents were displaced<br />
to other programs across the country. Since my wife is from Louisville<br />
<strong>and</strong> is also an active duty physician, we looked <strong>for</strong> programs close to Air<br />
Force bases <strong>and</strong> close to home. Wright-Patterson AFB in Dayton <strong>and</strong><br />
the University of Cincinnati were a perfect fit. My younger brother is<br />
in his last year of residency in Radiology here at UC <strong>and</strong> the training<br />
programs here came highly recommended.”<br />
(L-R) Timothy Pritts, MD, PhD, Acting Director of Surgical Education, with<br />
surgical residents Tom Husted, MD, Jerry Fortuna, MD, <strong>and</strong> Jaime Lewis, MD<br />
“A veteran of several moves with the military, I can easily say that the<br />
UC Surgery Department has been absolutely outst<strong>and</strong>ing in welcoming<br />
me <strong>and</strong> my family into the program <strong>and</strong> the area. I am ecstatic about<br />
being in the program <strong>and</strong> have found my first two months here extremely<br />
challenging, fulfilling <strong>and</strong> utterly enjoyable. The staff here have put<br />
together an impressive group of residents <strong>and</strong> faculty, <strong>and</strong> I am honored<br />
to have been given an opportunity to train at such a reputable institution.<br />
I will remain on active duty during the duration of my training <strong>and</strong> will<br />
complete the remainder of my military commitment to the Air Force<br />
upon graduation. I am confident that I will have an outst<strong>and</strong>ing educational<br />
experience here at UC <strong>and</strong> we are excited to be so close to home<br />
<strong>and</strong> family! I look <strong>for</strong>ward to my years of training here at UC <strong>and</strong> we<br />
are very appreciative of all the help <strong>and</strong> support we have received from<br />
the Department of Surgery.”<br />
Jerry Fortuna, MD (on behalf of his wife, Sarah, <strong>and</strong> their children:<br />
Haleigh, Elizabeth, <strong>and</strong> Jerry III).<br />
Match Day 2006 Results<br />
Two UC College of Medicine students, Callisia Clarke <strong>and</strong><br />
Jonathan Thompson, matched with the UC Department of<br />
Surgery residency training program in general surgery.<br />
This year’s incoming interns in general surgery:<br />
Eric Campion, University of Michigan<br />
Callisia Clarke, University of Cincinnati<br />
Angela Ingraham, Loyola University<br />
Christopher Lundquist, V<strong>and</strong>erbilt University<br />
Charles Park, Brown Medical School<br />
Jonathan Thompson, University of Cincinnati<br />
Callisia Clarke opens the envelope, then shows her delight after<br />
matching with the UC Department of Surgery.<br />
Jonathan Thompson <strong>and</strong> his wife celebrate his matching with UC.<br />
“I am ecstatic about being in the program <strong>and</strong><br />
have found my first two months here extremely<br />
challenging, fulfilling <strong>and</strong> utterly enjoyable. I look<br />
<strong>for</strong>ward to my years of training here at UC <strong>and</strong> we<br />
are very appreciative of all the help <strong>and</strong> support<br />
we have received from the Department of<br />
Surgery.”<br />
Jerry Fortuna, MD
Andrew Knott, MD<br />
Kelly McLean, MD<br />
Surgical Education <strong>New</strong>s<br />
Andrew Knott, MD, <strong>and</strong> Kelly McLean,<br />
MD, were chosen by the American<br />
College of <strong>Surgeons</strong> <strong>and</strong> the Advisory<br />
Council <strong>for</strong> General Surgery to participate<br />
in GS08-Surgical Jeopardy during the<br />
2006 Spring Meeting at the Wyndham<br />
Anatole in Dallas, on April 23, 2006. The<br />
“Surgical Jeopardy” competition runs <strong>for</strong><br />
2.5 hours. Teams will compete in rounds<br />
of competition. The winning teams will<br />
advance to compete in a final round that<br />
will include a Jeopardy Round <strong>and</strong> a Final<br />
Jeopardy round, the winner of which will<br />
take all. The degree of difficulty will<br />
increase with each round of competition.<br />
Questions will be drawn from SESAP 12.<br />
Joshua M.V. Mammen, MD, served on a<br />
panel of key organizations (panelists<br />
including the heads of the American Board<br />
of Surgery, American College of <strong>Surgeons</strong><br />
Division of Education, <strong>and</strong> the Surgery<br />
Resident Review Committee) at the<br />
Association of Program Directors in<br />
Joshua Mammen, MD Surgery meeting in Tucson, as the representative<br />
of the Resident <strong>and</strong> Associate<br />
Society (RAS) of the American College of <strong>Surgeons</strong>. He serves<br />
as the Co-chair of the Education Committee <strong>and</strong> the Member-atlarge<br />
<strong>for</strong> General Surgery on the Executive Committee of RAS.<br />
Grady Alsabrook, MD<br />
Grady Alsabrook, MD, was one of six<br />
UC residents voted by UC College of<br />
Medicine students to receive a Gold<br />
Foundation Humanism <strong>and</strong> Excellence in<br />
Teaching Award. He will be presented<br />
with a certificate <strong>and</strong> cash award during<br />
the Student Clinician Ceremony on June<br />
30. Other finalists <strong>for</strong> the award included<br />
Drs. Kfir Ben-David, Jocelyn Logan-<br />
Collins, <strong>and</strong> Brian Pan.<br />
UC surgical residents took the top three places in the Cincinnati<br />
Surgical Society’s 2005-2006 Resident Essay Competition.<br />
Five-minute presentations were given by the winning residents<br />
at the meeting on May 2, 2006:<br />
1st Place: Lynn Huffman, MD: “Early Results from Lung<br />
Cancer Screening Using Spiral CT of High-Risk Individuals.”<br />
2nd Place: Bryon Boulton, MD: “APC Tumor Suppressor<br />
Regulates Mammary Epithelial Apoptosis <strong>and</strong> Proliferation.”<br />
3rd Place: Mubeen Jafri, MD: “Holangiocyte Injury Mediates<br />
Temporal Dependence of Experimental Biliary Atresia.”<br />
There were a total of 19 abstracts submitted <strong>and</strong> 6 judges.<br />
Richard Stevenson, MD, Director of the Student Clerkship in<br />
Surgery, won the Gold Apple Award winner as best teacher in<br />
the clinical years as voted by the UC Class of 2006.<br />
Department of Surgery Faculty Continue<br />
Key Roles in Prestigious Surgical Societies<br />
For the first time, the Society of University <strong>Surgeons</strong> (SUS)<br />
<strong>and</strong> the Association of Academic Surgery (AAS) held a joint<br />
meeting, referred to as the first annual Academic Surgical<br />
Congress. The February 2006 event in San Diego had recordbreaking<br />
attendance, <strong>and</strong> the UC Department of Surgery continues<br />
to play a key role in these organizations.<br />
Brad Warner, MD (pediatric surgery) <strong>and</strong> Jeffrey<br />
Matthews, MD (pancreatic/liver sugery) are past presidents<br />
of the SUS, serve on the SUS Foundation Exceutive<br />
Committee, <strong>and</strong> were on the task <strong>for</strong>ce that brought the two<br />
societies together <strong>for</strong> the joint meeting.<br />
Timothy Pritts, MD, PhD (trauma surgery/education) was<br />
elected to the AAS Education Committee. Michael Reed,<br />
MD (thoracic surgery) serves on the membership committee<br />
of the AAS. Andrew Lowy, MD (surgical oncology) <strong>and</strong><br />
Karyn Butler, MD (trauma surgery/cardiovascular research)<br />
serve on the publications committee of the SUS, <strong>and</strong> were<br />
also appointed to the program committee of the SUS.<br />
<strong>New</strong> members admitted to the SUS include Timothy<br />
Broderick, MD (GI/endocrine surgery) <strong>and</strong> Joseph Buell,<br />
MD (transplant/liver surgery). Members-elect include<br />
Jeffrey Sussman, MD (surgical oncology), Thomas Inge,<br />
MD, PhD (pediatric surgery) <strong>and</strong> Jeffrey Pearl, MD (pediatric<br />
cardiac surgery).<br />
Drs. Karyn Butler, Andrew Lowy, Jeffrey Matthews, <strong>and</strong><br />
Brad Warner were session moderators. Surgery faculty<br />
made nine presentations at the meeting (see Presentations),<br />
including three by Timothy Crombleholme, MD (pediatric<br />
surgery) at the SUS Plenary Session.<br />
“It is exciting to see the UC Department of Surgery<br />
play such an important role in these two prestigious<br />
academic organizations. We are well represented<br />
across our divisions <strong>and</strong> specialties, <strong>and</strong> the success of<br />
our mission to train the future leaders of American<br />
Surgery is evident in the number of our rising stars who<br />
have become active in these prestigious organizations.”<br />
Jeffrey B. Matthews, MD<br />
Chairman, UC Department of Surgery
Trauma/Critical Care <strong>and</strong> CSTARS Faculty Are Honored<br />
John Heiser (left), President of the AARC, presents the Forrest<br />
M. Bird Lifetime Achievement Award to Richard Branson<br />
“Living Proof” Patient Revisits UC Trauma<br />
Center <strong>and</strong> Reveals Plan to Become a Doctor<br />
Rachael Swango, 18, who survived a life-threatening car accident in<br />
February, revisited the UC Trauma Center on April 17 to thank the<br />
surgeons <strong>and</strong> other trauma team members who helped save her life.<br />
She also revealed her plans to become a doctor. Ms. Swango was<br />
featured in University Hospital's “Living Proof” ad campaign, <strong>and</strong><br />
was presented with signed posters of the ad by the trauma team,<br />
including Timothy Pritts, MD, PhD.<br />
Dr. Pritts said that Ms. Swango suffered a severed vena cava, lacerated<br />
liver <strong>and</strong> collapsed lungs in the accident. Such an injury to the<br />
vena cava or other large veins has a mortality rate of approximately<br />
75 percent. According to Dr. Pritts, the exceptionally fast <strong>and</strong> efficient<br />
care offered by a Level I Trauma Center <strong>and</strong> its multidisciplinary<br />
team is best suited to treat multiple-trauma victims.<br />
Ms. Swango will graduate from Finneytown High School in June<br />
<strong>and</strong> plans to attend Concord University in West Virginia.<br />
Rachael Swango is presented with a signed poster of the “Living<br />
Proof” poster by Timothy Pritts, MD, PhD, <strong>and</strong> other members of<br />
the University Hospital’s Trauma Team who helped save her life.<br />
Branson Wins Lifetime Achievement Award<br />
Richard D. Branson, MS, RRT, MBA, FAARC, Associate<br />
Professor of Surgery in the Division of Trauma <strong>and</strong> Critical<br />
Care, received dual honors at the American Association <strong>for</strong><br />
Respiratory Care (AARC) International Respiratory Congress<br />
which was held in San Antonio, TX, in December 2005.<br />
Mr. Branson was named a Life Member of the AARC <strong>and</strong> also<br />
received the prestigious Forrest M. Bird Lifetime Achievement<br />
Award from the American Respiratory Care Foundation<br />
(ARCF). The Award was established in 1983 with a grant from<br />
Dr. Forrest M. Bird, founder of Bird Products Corporation, to<br />
acknowledge outst<strong>and</strong>ing individual scientific contributions in<br />
the area of respiratory care of cardiopulmonary disorders. The<br />
Life Membership Award is given annually to AARC members<br />
who have gone above <strong>and</strong> beyond the call of duty in advancing<br />
the respiratory care profession.<br />
Flight Surgeon in Afghanistan Expresses His<br />
Gratitude <strong>for</strong> CSTARS/CCATT Training at UC<br />
“I’d like to recognize the Cincinnati CSTARS [Center <strong>for</strong> Sustainment<br />
of Trauma <strong>and</strong> Readiness Skills] program <strong>for</strong> really helping to prepare<br />
me <strong>and</strong> my team <strong>for</strong> our recent deployment to Bagram, Afghanistan.<br />
Of all the Air Force training I’ve received over the last 7 years, I think<br />
CSTARS was some of the best <strong>and</strong> most practical. Specifically, the<br />
h<strong>and</strong>s-on equipment training <strong>and</strong> the simulated scenarios along with<br />
the flight exercise really paid off in the field. Our very first CCATT<br />
[Critical Care Air Transport Team] mission almost exactly mirrored the<br />
final ‘flight training’ scenario.<br />
CCATT Simulated C-17 Trainer as part of CSTARS training program at UC<br />
“The entire 36-hour mission will remain etched in my brain. Incredible<br />
stress, uncertainty, fatigue, <strong>and</strong> equipment problems! Fortunately, the<br />
CSTARS scenarios, equipment training <strong>and</strong> lectures really paid off <strong>for</strong><br />
our team. Specifically, Dr. Stephen Barnes ran us a scenario during our<br />
training flight at CSTARS that really helped. I was thanking Dr. Barnes<br />
<strong>and</strong> CSTARS the entire harrowing flight from Balad because I <strong>and</strong> my<br />
team felt confident <strong>and</strong> were able to get our patients to L<strong>and</strong>stuhl alive.<br />
We would have been lost <strong>and</strong> really in much bigger trouble <strong>and</strong> maybe<br />
lost a patient in flight without CSTARS.”<br />
Major Peter M. Harding, MD
UC Heart Program Celebrates 20 Years<br />
Heart transplant recipients at the 20-year celebration of University Hospital’s heart transplant program.<br />
The University Hospital celebrated its 20th anniversary of per<strong>for</strong>ming<br />
heart transplant surgeries during an event held on<br />
December 21, 2005, in the hospital's main lobby. Launched in<br />
December 1985, UC's heart transplant program has treated more<br />
than 348 patients.<br />
The first heart transplant locally was per<strong>for</strong>med by David<br />
Melvin, MD, PhD, on December 17, 1985. The University<br />
Hospital did one heart transplant in 1985 <strong>and</strong> 10 in 1989, as<br />
Cardiac faculty at University Hospital include (l-r) Lynne Wagoner, MD,<br />
David Melvin, MD, PhD, John Flege, Jr, MD, <strong>and</strong> Walter Merrill, MD<br />
cyclosporine dramatically changed the transplant l<strong>and</strong>scape.<br />
University Hospital did 12 of the 15 heart transplants per<strong>for</strong>med<br />
in Greater Cincinnati in 2004. The others were done at<br />
Children's Hospital Medical Center. They are the only two hospitals<br />
per<strong>for</strong>ming heart transplants in Greater Cincinnati.<br />
Nationally, there were 2,016 heart transplants in 2004.<br />
“As a team, we have to carefully evaluate patients be<strong>for</strong>e we put<br />
them on the list,” said Dr. Lynne Wagoner, medical director of<br />
the heart transplant program at the University of Cincinnati <strong>and</strong><br />
University Hospital. “Donor hearts are not sitting on a shelf<br />
waiting <strong>for</strong> us. We have to ensure the people who we put on the<br />
list are going to take care of the heart. We require them to stop<br />
smoking <strong>and</strong> insist on diet changes <strong>and</strong> exercising.”<br />
The prime organ donor c<strong>and</strong>idate is someone who suffers brain<br />
death, often from an accident or sudden medical crisis like an<br />
aneurysm. Fewer than 1% of deaths meet the criteria; thus,<br />
many more registered donors are needed. Nationally, 17 people<br />
die every day waiting <strong>for</strong> an organ transplant.<br />
As of January 20, 2006, approximately 3,000 patients in the<br />
nation were waiting <strong>for</strong> hearts. University Hospital has 20, <strong>and</strong><br />
there are 22 waiting throughout Greater Cincinnati.<br />
Oral & Maxillofacial Surgery Division To Welcome <strong>New</strong> Residents<br />
The Division of Oral <strong>and</strong> Maxillofacial Surgery had a very successful match<br />
with the following:<br />
Leslie A. Orzech, who will graduate in May from Case Western Reserve<br />
University School of Dental Medicine in Clevel<strong>and</strong>, Ohio.<br />
Karen K. Potaczek, who will graduate in May from Marquette University<br />
School of Dentistry in Milwaukee, Wisconsin.<br />
They will begin their Oral <strong>and</strong> Maxillofacial Surgery residency training on<br />
July 1, 2006.<br />
Leslie Orzech Karen Potaczek
Joseph F. Buell, MD (fourth from right),<br />
with faculty of McGill University<br />
Recent Presentations<br />
Joseph F. Buell, MD, Division of Transplant Surgery, was invited professor<br />
<strong>and</strong> spoke on “Laparoscopic Hepatic Resection” at the 2005 McGill<br />
Hepatopancreatobiliary & Liver Transplant Surgery conference at McGill<br />
University, Montreal, Quebec, Canada, November 7-9, 2005.<br />
Mr. Charles Doarn, Executive Director of the UC Center <strong>for</strong> Surgical<br />
Innovation (CSI), presented “Telesurgery” at the National Virtual<br />
Telemedicine Gr<strong>and</strong> Rounds via VTC (video teleconference), January 17,<br />
2006.<br />
Mr. Doarn also participated in the “Innovation Imperative” symposium in<br />
Cincinnati on March 3, 2006, comprising a group of international thought<br />
leaders in a day-long <strong>for</strong>um to discuss innovation <strong>and</strong> ways in which universities<br />
play a key role in the creative economy.<br />
Harnett BM. “Advanced Network Opportunities <strong>for</strong> Surgical Tele-<br />
Robotics.” Center <strong>for</strong> Computational Sciences, University of Kentucky, Lexington, KY, February, 2006.<br />
Pritts TA. “Good Medicine in Good Places.” Nursing Education <strong>and</strong> Professional Practice Group, University Hospital, Cincinnati, Ohio,<br />
January 18, 2006.<br />
Wolf RK. “Surgical Microdevices <strong>and</strong> Nanodevices.” BME (Biomedical Engineering) Seminar, University of Cincinnati, January 23,<br />
2006.<br />
John Howington MD, Associate Professor of Surgery <strong>and</strong> Director of the Division of Thoracic Surgery, <strong>and</strong> Ms. J. Rita McNeil, City<br />
Solicitor <strong>for</strong> the City of Cincinnati, spoke at the “Closing the Gap” conference on April 12, 2006, about the St. Vincent DePaul (SVDP)<br />
Charitable Pharmacy opening this summer at the Bank Street location. Patient counseling <strong>and</strong> advocacy are already taking place with volunteers<br />
assisting clients in enrollment <strong>for</strong> Medicare part D <strong>and</strong> Pharmaceutical Company Assistance programs. Dr. Howington <strong>and</strong> Ms.<br />
McNeil are alumni of the Leadership Cincinnati Class of 2003-2004. Ms. McNeil is President of the SVDP Charitable Pharmacy Board<br />
of Directors, on which Dr. Howington is a Board member along with several other Leadership Cincinnati classmates.<br />
For the first time, the Society of University <strong>Surgeons</strong> (SUS) <strong>and</strong> the Association of Academic Surgery (AAS) held a joint meeting,<br />
referred to as the First Annual Academic Surgical Congress, held February 7-11, 2006, in San Diego, CA. The following abstracts were<br />
presented at the meeting (faculty in red) <strong>and</strong> also published in Journal of Surgical Research 2006;130(2):160-338.<br />
Boulton BJ, Ebetino MB, Willson TA, Goss KH. “The APC tumor suppressor regulates apoptosis <strong>and</strong> proliferation in human breast cancer<br />
cells.”<br />
Huffman LC, Knight DD, Butler K. “Increased age is associated with reduced survival following trauma to the duodenum or pancreas.”<br />
Panait L, Merrell RC, Rafiq A, Dudrick SJ, Broderick TJ. “Virtual reality laparoscopic skill assessment in microgravity.”<br />
Pritts TA, Schuster RM, Chaiken M, Worrell R, Matlin K, Lentsch A, Matthews JB. “Thermal injury increases endotoxin susceptibility<br />
<strong>and</strong> intestinal TLR4 expression.”<br />
Reed MF, Zagorski WA, Dhamija A, Knudsen ES. “Inhibition of RB tumor suppressor activity increases chemosensitivity in lung cancer<br />
xenografts.”<br />
Sheng GS, Warner BW. “EGF receptor signaling induces proliferation of intestinal epithelial cells via MAPK-directed increase in P21<br />
expression.”<br />
In addition, three papers were presented at the SUS Plenary Session by pediatric surgeon Timothy Crombleholme, MD, <strong>and</strong> colleagues:<br />
Marwan A, Parvadia J Vaikunth S, Harkness U, Maldonado A, Kalinowska B, Alaee D, Uzvolgyi E, Crombleholme T.<br />
“Postpneumonecty compensatory lung growth occurs through an endothelial progenitor cell-mediated mechanism.”<br />
Parvadia J, Marwan A, Vaikunth S, Harkness U, Maldonado A, Alaee D, Kalinowska B, Ripberger M, Uzvolgyi E, Crombleholme T.<br />
“Liver regeneration is a salivary VEGF dependent phenomenon.”<br />
Vaikunth SS, Keswani SG, Parvadia JK, Marwan A, Harkness U, Maldonado A, Alaee D, Kalinowska B, Uzvolgyi E, Crombleholme T.<br />
“Exogenous endothelial precursor cells (EPCS) correct the wound healing deficit <strong>and</strong> enhance neovascularization in FVBN-MMP-9<br />
knock-out mice.”
SBAS Meeting Attracts Prominent <strong>Surgeons</strong> <strong>and</strong> Stars<br />
(L-R) Mr. Oscar Robertson with Drs.<br />
Jeffrey Matthews <strong>and</strong> Henri Ford<br />
James Kingsbury, Executive Director of<br />
University Hospital (left) with Kenneth<br />
Davis, Jr, MD, <strong>and</strong> Jane Henney, MD,<br />
Provost, UC Medical Center<br />
(L-R) Anthony Stallion, MD (UC alumnus),<br />
Kenneth Davis, Jr, MD, Mrs. Oscar (Yvonne)<br />
Robertson, <strong>and</strong> W. Lynn Weaver, MD<br />
Kenneth Davis, Jr, MD, introduces<br />
Karyn Butler, MD, at local program<br />
Michael Nussbaum, MD (center) introduces<br />
Callisia Clarke (recent UC Medical School<br />
graduate who matched to UC Department<br />
of Surgery) to Steven Stain, MD (far left)<br />
(L-R) Selwyn Vickers, MD, SBAS President,<br />
Mayor Mark Mallory, Jeffrey Matthews, MD,<br />
<strong>and</strong> Kenneth Davis, Jr, MD, after reading of<br />
proclamation by Mayor Mallory at SBAS<br />
Selwyn Vickers, MD, President of<br />
SBAS (left), presents Jeff Matthews,<br />
MD, with Asa Yancey Lecture plaque<br />
Mr. Oscar Robertson presents guest lecture<br />
(L-R) Jeff Matthews, MD, Selwyn Vickers, MD,<br />
Mayor Mark Mallory, <strong>and</strong> Ken Davis, Jr, MD<br />
Local SBAS program in Surgical Amphitheater<br />
UC surgery residents <strong>and</strong> other guests at SBAS<br />
(L-R) Eddie Hoover, MD, Walter Merrill, MD,<br />
<strong>and</strong> David Melvin, MD, PhD [Drs. Hoover <strong>and</strong><br />
Merrill were thoracic surgery residents together]
Surgical Gr<strong>and</strong> Rounds Schedule<br />
May 10, 2006 Joseph F. Buell, MD (Transplant Surgery): “Progress in Laparoscopic Liver Transplant Surgery”<br />
May 17, 2006 Guest Lecturer, Richard A. Hodin, MD, Associate Professor of Surgery, Harvard Medical<br />
School; Surgical Director, MGH Inflammatory Bowel Disease Center: “Advances in Surgery <strong>for</strong><br />
Inflammatory Bowel Disease”<br />
May 24, 2006 Guest Lecturer, Frederick Grover, MD, Chief of Surgery, Denver VA Medical Center; Professor<br />
<strong>and</strong> Head, Division of Cardiothoracic Surgery, University of Colorado Health Sciences Center:<br />
“Lung Transplantation: Past, Present, <strong>and</strong> Future”<br />
May 31, 2006 Joint Anesthesia/Surgery Gr<strong>and</strong> Rounds - Anesthesia Visiting Professor, Lee Fleisher, MD,<br />
Robert D. Dripps Professor <strong>and</strong> Chair, Department of Anesthesiology <strong>and</strong> Critical Care; Professor<br />
of Medicine, University of Pennsylvania: “Strategies to Reduce Cardiac Risk of Noncardiac<br />
Surgery” [Note time changed to 7:00 a.m.]<br />
June 7, 2006 Pediatric Surgery<br />
June 14, 2006 Hector R. Wong, MD (Research), Professor of Pediatrics; Director, Division of Critical Care<br />
Medicine, Cincinnati Children's Hospital: “Genome Wde Expression Patterns in Pediatric SIRS <strong>and</strong><br />
Septic Shock”<br />
June 21, 2006 Final Gr<strong>and</strong> Rounds [Gr<strong>and</strong> Rounds will resume in September]<br />
(l-r) Drs. Mubeen Jafri, Prakash P<strong>and</strong>alai, Lynn (Chip) Huffman, <strong>and</strong> Ryan Thomas<br />
are the four finalists in the Resident Research Competition. The winner will be<br />
announced at Final Gr<strong>and</strong> Rounds on June 21, 2006.<br />
University Surgeon is published September-October, quarterly by UC <strong>Surgeons</strong>, 2004 Inc.<br />
Written by Steve Wiesner, 558-4207, steve.wiesner@uc.edu<br />
Edited by Elizabeth Pierce, 558-1321, elizabeth.pierce@uc.edu<br />
Spring, 2006