A systematic review of the effectiveness of adalimumab
A systematic review of the effectiveness of adalimumab
A systematic review of the effectiveness of adalimumab
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
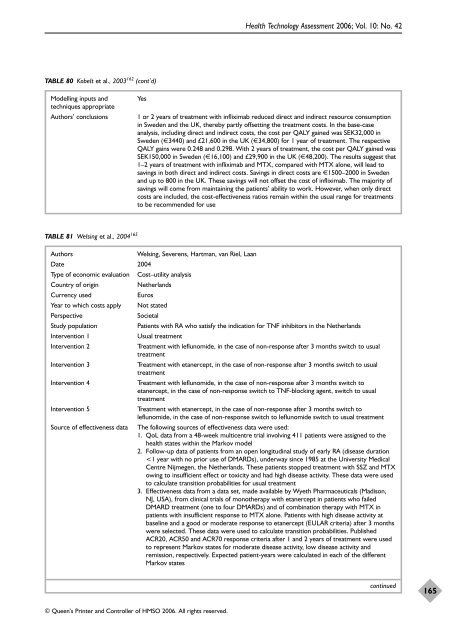
TABLE 80 Kobelt et al., 2003 162 (cont’d)<br />
© Queen’s Printer and Controller <strong>of</strong> HMSO 2006. All rights reserved.<br />
Health Technology Assessment 2006; Vol. 10: No. 42<br />
Modelling inputs and Yes<br />
techniques appropriate<br />
Authors’ conclusions 1 or 2 years <strong>of</strong> treatment with infliximab reduced direct and indirect resource consumption<br />
in Sweden and <strong>the</strong> UK, <strong>the</strong>reby partly <strong>of</strong>fsetting <strong>the</strong> treatment costs. In <strong>the</strong> base-case<br />
analysis, including direct and indirect costs, <strong>the</strong> cost per QALY gained was SEK32,000 in<br />
Sweden (€3440) and £21,600 in <strong>the</strong> UK (€34,800) for 1 year <strong>of</strong> treatment. The respective<br />
QALY gains were 0.248 and 0.298. With 2 years <strong>of</strong> treatment, <strong>the</strong> cost per QALY gained was<br />
SEK150,000 in Sweden (€16,100) and £29,900 in <strong>the</strong> UK (€48,200). The results suggest that<br />
1–2 years <strong>of</strong> treatment with infliximab and MTX, compared with MTX alone, will lead to<br />
savings in both direct and indirect costs. Savings in direct costs are €1500–2000 in Sweden<br />
and up to 800 in <strong>the</strong> UK. These savings will not <strong>of</strong>fset <strong>the</strong> cost <strong>of</strong> infliximab. The majority <strong>of</strong><br />
savings will come from maintaining <strong>the</strong> patients’ ability to work. However, when only direct<br />
costs are included, <strong>the</strong> cost-<strong>effectiveness</strong> ratios remain within <strong>the</strong> usual range for treatments<br />
to be recommended for use<br />
TABLE 81 Welsing et al., 2004 165<br />
Authors Welsing, Severens, Hartman, van Riel, Laan<br />
Date 2004<br />
Type <strong>of</strong> economic evaluation Cost–utility analysis<br />
Country <strong>of</strong> origin Ne<strong>the</strong>rlands<br />
Currency used Euros<br />
Year to which costs apply Not stated<br />
Perspective Societal<br />
Study population Patients with RA who satisfy <strong>the</strong> indication for TNF inhibitors in <strong>the</strong> Ne<strong>the</strong>rlands<br />
Intervention 1 Usual treatment<br />
Intervention 2 Treatment with leflunomide, in <strong>the</strong> case <strong>of</strong> non-response after 3 months switch to usual<br />
treatment<br />
Intervention 3 Treatment with etanercept, in <strong>the</strong> case <strong>of</strong> non-response after 3 months switch to usual<br />
treatment<br />
Intervention 4 Treatment with leflunomide, in <strong>the</strong> case <strong>of</strong> non-response after 3 months switch to<br />
etanercept, in <strong>the</strong> case <strong>of</strong> non-response switch to TNF-blocking agent, switch to usual<br />
treatment<br />
Intervention 5 Treatment with etanercept, in <strong>the</strong> case <strong>of</strong> non-response after 3 months switch to<br />
leflunomide, in <strong>the</strong> case <strong>of</strong> non-response switch to leflunomide switch to usual treatment<br />
Source <strong>of</strong> <strong>effectiveness</strong> data The following sources <strong>of</strong> <strong>effectiveness</strong> data were used:<br />
1. QoL data from a 48-week multicentre trial involving 411 patients were assigned to <strong>the</strong><br />
health states within <strong>the</strong> Markov model<br />
2. Follow-up data <strong>of</strong> patients from an open longitudinal study <strong>of</strong> early RA (disease duration<br />