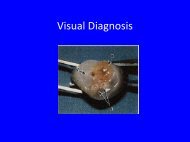
Visual Diagnosis
Visual Diagnosis
Visual Diagnosis
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Visual</strong> <strong>Diagnosis</strong>
Muscle Pain and<br />
Tea Colored Urine<br />
Kathleen Forcier
Presentation<br />
• 14 y/o previously healthy M presenting with<br />
b/l thigh pain and tea colored urine.<br />
• Pt is a wrestler and 3 d prior to admit had a<br />
particularly strenuous school practice. Since<br />
that time his thighs have been sore and<br />
maybe a little swollen. The night prior to<br />
admission he noticed his urine was coca‐cola<br />
colored.
More Questions?
Physical Exam<br />
• 63 kg T 36.9 HR 74 BP 144/90 RR 18<br />
• Gen: NAD<br />
• Chest: CTAB, no crackles<br />
• Cardiac: RRR, no murmurs<br />
• Abd: soft, NT, ND, no HSM<br />
• Ext: thighs firm (not tense) b/l, tender to<br />
palpation, 2+ femoral, popliteal and DP pulses,<br />
no erythema<br />
• Skin: no rashes<br />
• Neuro: 4/5 strength in legs, 5/5 in arms
www.toxinology.com<br />
LABS?
Labs<br />
• WBC 13.9 Hb 16.8 Plt 262<br />
• Chem Na 140 K 4.3 Cl 106 HCO3 30 BUN/Cr<br />
13/1.1 Ca 8.0 Phos 3.7<br />
• AST 3,602 ALT 438 Alk Phos 177<br />
• CK 236,905<br />
• UA: pH 7.5, 1.008, Ketone ‐, Glucose ‐, Nit ‐,<br />
LE ‐, Blood 3+ RBC 0‐3 WBC 0‐2
Rhabdomyolysis<br />
• Muscle injury causes extracellular Ca to leak<br />
into the intracellular space<br />
• Excess intracellular Ca causes muscle fiber<br />
necrosis<br />
• This releases K, Phos, Myoglobin, creatine<br />
kinase into the circulation
Causes<br />
• Most common causes:<br />
– Alcohol abuse<br />
– Muscle over exertion<br />
– Muscle compression<br />
– Illicit drugs
Meds that Causes Rhabdomyolysis<br />
Direct Myotoxicity Indirect muscle damage<br />
HMG‐CoA reductase inhibitors (statins) Alcohol ( predisposes to trauma, sz)<br />
Cyclosporine Cocaine<br />
Itraconazole Amphetamine<br />
Erythromycin Ecstasy<br />
Colchicine Neuromuscular blocking agents<br />
Corticosteriods<br />
Alcohol<br />
Sauret & Marinides. Rhabdomyolysis. American Family Physician. 2002: 65; 5; 907‐912
Traumatic/Exertional Causes<br />
Trauma Heat‐related causes Exertional Causes<br />
Lightning strike/electrical<br />
injury<br />
Heat stroke Marathon running<br />
immobilization Malignant hyperthermia overexertion<br />
3 rd degree burns Neuroleptic malignant<br />
syndrome<br />
Overexertion in sickle cell<br />
patient<br />
Crush injury Heat dissipation<br />
impairment<br />
Ischemic injury seizures<br />
Sauret & Marinides. Rhabdomyolysis. American Family Physician. 2002: 65; 5; 907‐912
Inflammatory/Metabolic Causes<br />
Infectious Inflammatory Metabolic/Endocrine<br />
Viruses: flu, paraflu, adeno,<br />
coxsackie, echovirus, CMV,<br />
EBV<br />
Bacteria: Strep, Staph,<br />
Salmonella, Legionella,<br />
Listeria<br />
Polymyositis Electrolyte imbalance<br />
(HypoNa, HypoK,<br />
HypoPhos, hypoCa)<br />
Dermatomyositis Hypothyroidism<br />
Snake bites Thyrotoxicosis<br />
Sauret & Marinides. Rhabdomyolysis. American Family Physician. 2002: 65; 5; 907‐912<br />
DKA
Genetic Causes<br />
Lipid Metabolism Carbohydrate Metabolism Purine Metabolism<br />
Carnitine<br />
palmitoyltransferase<br />
deficiency<br />
Carnitine deficiency Phosphofructokinase<br />
deficiency<br />
Acyl‐coenzyme A<br />
dehydrogenase deficiency<br />
McArdle’s disease Duchenne’s muscular<br />
dystrophy<br />
Phosphoglycerate mutase<br />
deficiency<br />
LDH deficiency (elevated<br />
CK, nl LDH)<br />
Myoadenylate deaminase<br />
deficiency<br />
Clues to genetic disorder: a) onset in childhood b) FHx c) mild baseline CK elevations d)<br />
muscle necrosis after minimal exertion e) recurrent attacks
Symptoms<br />
• Muscle pain/tenderness<br />
• Weakness<br />
• Tea‐colored urine<br />
• Swelling<br />
• Fever<br />
• Nausea/vomiting<br />
• Anuria
Complications<br />
• Hyperkalemia cardiac arrhythmias<br />
• Hypocalcemia (because of hyperPhos, Ca<br />
deposition in damaged muscle)<br />
• Hepatic dysfunction in 25% of patients.<br />
Muscle proteases cause hepatic inflammation<br />
– Both AST and ALT are increased in muscle injury<br />
even without liver injury AST:ALT 3:1
• Acute Renal Failure<br />
Complications<br />
• Occurs in 15% of patients<br />
• Degree of serum enzyme elevation doesn’t<br />
always predict ARF<br />
• CK levels >16,000 associated with higher<br />
likelihood of renal failure
Heme Protein‐induced ARF<br />
• Renal vasoconstriction<br />
– Patients are volume depleted , heme proteins<br />
scavenge NO<br />
• Intraluminal cast formation<br />
– Depends on [myoglobin], urine acidity (more<br />
acidic the less soluble)<br />
• Direct heme‐protein toxicity<br />
– Heme Fe induced oxidative stress
Treatment/Prevention of ARF<br />
• Fluids, fluids, fluids,<br />
more fluids<br />
• Goal UOP in an adult is<br />
200 cc/hr to prevent<br />
cast formation<br />
• NaHCO3?<br />
• Mannitol?
• Advantages<br />
Alkalinizing the Urine<br />
• Incr. myoglobin solubility,<br />
thereby decreasing cast<br />
formation<br />
• Shift K into cells<br />
• Prevents release of free<br />
Fe from myoglobin<br />
• Disadvantages<br />
• No direct evidence shows<br />
NaHCO3 is better than NS<br />
• May worsen<br />
hypocalcemia (tetany, sz,<br />
arrhythmias)
• Advantages<br />
• Proximal diuretic and<br />
increases heme excretion<br />
• Radical scavenger (may<br />
lessen oxidative stress)<br />
Mannitol<br />
• Disadvantages<br />
• Can cause hyperosmolar<br />
state<br />
• Can lead to volume<br />
depletion<br />
• Pts who receive mannitol<br />
don’t have lower rates of<br />
ARF<br />
Brown et al. Showed BIC/MAN didn’t lower rates of RF, dialysis, mortality.
Hemodialysis<br />
• Myoglobin too big to be removed by HD<br />
• HD still used for<br />
– Hyperkalemia<br />
– Fluid overload<br />
– Acidemia<br />
– uremia
When to Stop Treatment<br />
• CK < 5‐10,000<br />
– CPK levels peak 24‐36 hours after injury then<br />
decline usu 40% q24h<br />
• Urine discoloration clears
Back to Our Patient<br />
• CK peaked at 312,535 now 46,978<br />
• 10/7 first heme negative urine<br />
• Cr peaked at 1.1, now is 0.9<br />
• DFA – negative<br />
• Viral culture – prelim negative<br />
• CMV IgM negative<br />
• Utox + only for opiates (morphine in ER)<br />
• Free T4 1.4 TSH 1.91
Take Home Points<br />
• Classic presentation of rhabdomyolysis<br />
includes myalgia, muscle weakness and dark<br />
urine<br />
• Rhabdomyolysis causes ARF by direct renal<br />
toxicity, renal vasoconstriction, renal tublar<br />
obstruction<br />
• Treatment of rhabdomyolysis is aggressive<br />
hydration
Words of Wisdom from<br />
Scott Sutherland, MD
Sources<br />
• Brown et al. Preventing renal failure in patients with<br />
rhabdomyolysis: do bicarbonate and mannitol make a difference.<br />
Journal of Trauma. 2004; 56: 1191‐1196.<br />
• Chopra. Patterns of plasma aspartate and alanine aminotransferase<br />
levels with and without liver disease. 2009. Uptodate.com.<br />
• Moghtader, Brady and Bonadio. Exertional rhabdomyolysis in an<br />
adolescent athlete. Pediatric Emergency Care. 1997; 13: 382‐385.<br />
• Rhabdomyolysis and myohemoglobinuric acute renal failure.<br />
Editoral Review. Kidney International. 1996; 49: 314‐326.<br />
• Rose. Clinical features and prevention of heme pigment‐induced<br />
acute tubular necrosis. 2009, Uptodate.com<br />
• Sauret & Marinides. Rhabdomyolysis. American Family Physician.<br />
2002; 65: 907‐912.