Download pdf version - Positively Aware
Download pdf version - Positively Aware
Download pdf version - Positively Aware
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
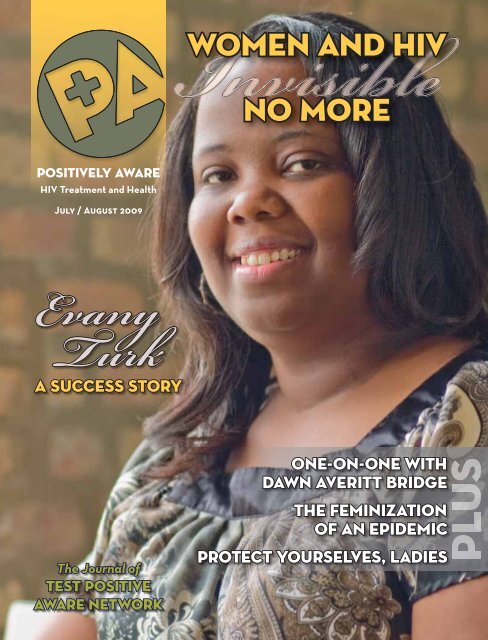
<strong>Positively</strong> <strong>Aware</strong><br />
HIV Treatment and Health<br />
July / August 2009<br />
Evany<br />
Turk<br />
A Success Story<br />
The Journal of<br />
Test Positive<br />
<strong>Aware</strong> Network<br />
Women and HIV<br />
No More<br />
One-on-One with<br />
Dawn Averitt Bridge<br />
The Feminization<br />
of an Epidemic<br />
Protect Yourselves, Ladies
Please read Important Safety Information below,<br />
and talk to your healthcare professional to learn<br />
more about PREZISTA.<br />
ABOUT PREZISTA<br />
PREZISTA ® (darunavir) is a prescription medicine.<br />
It is one treatment option in the class of HIV (human<br />
immunodefi ciency virus) medicines known as<br />
protease inhibitors.<br />
PREZISTA is always taken with and at the same time<br />
as ritonavir (Norvir ® ), in combination with other HIV<br />
medicines for the treatment of HIV infection in adults.<br />
PREZISTA should also be taken with food.<br />
• The use of other medicines active against HIV in<br />
combination with PREZISTA/ritonavir (Norvir ® ) may<br />
increase the likelihood of your overall treatment<br />
response. Your healthcare professional will work<br />
with you to fi nd the right combination of other<br />
HIV medicines<br />
• The long-term effects of PREZISTA therapy are<br />
unknown at this time. It is important that you remain<br />
under the care of your healthcare professional<br />
PREZISTA does not cure HIV infection or AIDS, and<br />
does not prevent passing HIV to others.<br />
IMPORTANT SAFETY INFORMATION<br />
• PREZISTA, together with Norvir ® (ritonavir), has<br />
rarely been observed to cause liver problems that<br />
may be life-threatening. It was not always clear<br />
if PREZISTA caused these liver problems because<br />
some patients had other illnesses or were taking<br />
other medicines. Your healthcare professional<br />
should do blood tests prior to initiating<br />
combination treatment including PREZISTA. If<br />
you have chronic hepatitis B or C infection, your<br />
healthcare professional should check your blood<br />
tests more often because you have an increased<br />
chance of developing liver problems<br />
Talk to your healthcare professional about the<br />
signs and symptoms of liver problems. These<br />
may include yellowing of your skin or whites of<br />
your eyes, dark (tea-colored) urine, pale-colored<br />
stools (bowel movements), nausea, vomiting,<br />
loss of appetite, or pain, aching or sensitivity on<br />
your right side below your ribs<br />
• Skin rashes have been reported in patients taking<br />
PREZISTA. Rarely, PREZISTA has been reported to<br />
cause a severe or life-threatening rash. Contact<br />
your healthcare professional if you develop a rash<br />
• Taking PREZISTA with certain medicines could<br />
cause serious and/or life-threatening side<br />
effects or may result in loss of its effectiveness.<br />
Do not take PREZISTA if you are taking the<br />
following medicines: dihydroergotamine (D.H.E.45 ® ,<br />
Migranal ® ), ergonovine, ergotamine (Wigraine ® ,<br />
Ergostat ® , Cafergot ® , Ergomar ® ), methylergonovine,<br />
cisapride (Propulsid ® ), pimozide (Orap ® ), oral<br />
midazolam, triazolam (Halcion ® ), rifampin (Rifadin ® ,<br />
Rifater ® , Rifamate ® ), indinavir (Crixivan ® ), lopinavir/<br />
ritonavir (Kaletra ® ), saquinavir (Invirase ® ), lovastatin<br />
(Mevacor ® ), pravastatin (Pravachol ® ), simvastatin<br />
(Zocor ® ), or products containing St. John’s wort<br />
• Before taking PREZISTA, tell your healthcare<br />
professional if you are taking sildenafi l (Viagra ® ),<br />
vardenafi l (Levitra ® ), tadalafi l (Cialis ® ), atorvastatin<br />
(Lipitor ® ), atorvastatin/amlodipine (Caduet ® ), or<br />
rosuvastatin (Crestor ® ). This is not a complete
Belief PREZISTA<br />
list of medicines. Be sure to tell your healthcare<br />
professional about all the medicines you are<br />
taking or plan to take, including prescription<br />
and nonprescription medicines, vitamins, and<br />
herbal supplements<br />
• Tell your healthcare professional if you are taking<br />
estrogen-based contraceptives (birth control).<br />
PREZISTA might reduce the effectiveness of estrogenbased<br />
contraceptives. You must take additional<br />
precautions for birth control, such as condoms<br />
• Before taking PREZISTA, tell your healthcare<br />
professional if you have any medical conditions,<br />
including allergy to sulfa medicines, diabetes, liver<br />
problems (including hepatitis B or C), or hemophilia<br />
• Tell your healthcare professional if you are pregnant<br />
or planning to become pregnant, or are breastfeeding<br />
– The effects of PREZISTA on pregnant women or<br />
their unborn babies are not known. You and your<br />
healthcare professional will need to decide if taking<br />
PREZISTA is right for you<br />
– Do not breastfeed if you are taking PREZISTA. You<br />
should not breastfeed if you have HIV because of the<br />
chance of passing HIV to your baby<br />
• High blood sugar, diabetes or worsening of diabetes,<br />
and increased bleeding in people with hemophilia have<br />
been reported in patients taking protease inhibitor<br />
medicines, including PREZISTA<br />
• Changes in body fat have been seen in some patients<br />
taking HIV medicines, including PREZISTA. The cause<br />
and long-term health effects of these conditions are<br />
not known at this time<br />
• As with other protease inhibitors, taking PREZISTA<br />
may strengthen the body’s immune response,<br />
enabling it to begin to fi ght infections that have been<br />
hidden. Patients may experience signs and symptoms<br />
of infl ammation that can include swelling, tenderness,<br />
or redness<br />
• The most common side effects related to taking<br />
PREZISTA include diarrhea, nausea, headache, and<br />
abdominal pain. Uncommon but severe side effects<br />
such as infl ammation of the pancreas and increased<br />
blood fat levels have also been rarely reported.<br />
This is not a complete list of all possible side effects.<br />
If you experience these or other symptoms, talk to<br />
your healthcare professional. Do not stop taking<br />
{<br />
in myself<br />
in my doctor<br />
in my care<br />
now offers ONCE-DAILY<br />
dosing for adults taking HIV meds for<br />
the fi rst time.<br />
PREZISTA must be taken with and at<br />
the same time as ritonavir (Norvir ® )<br />
and with food.<br />
PREZISTA must be taken in combination<br />
with other HIV meds.<br />
Talk to your doctor to see if PREZISTA is<br />
right for you.<br />
<br />
Please visit www.PREZISTA.com<br />
PREZISTA or any other medicines without fi rst talking to<br />
your healthcare professional<br />
• Please refer to the ritonavir (Norvir ® ) Product<br />
Information (PI and PPI) for additional information on<br />
precautionary measures<br />
For adults taking HIV meds for the fi rst time:<br />
PREZISTA 800 mg (two 400-mg tablets) must be<br />
taken at the same time with 100 mg Norvir ®<br />
once daily every day. y PREZISTA must be taken<br />
with food.<br />
You are encouraged to report negative side<br />
effects of prescription drugs to the FDA. Visit<br />
www.fda.gov/medwatch or call 1-800-FDA-1088.<br />
Please see Important Patient Information on<br />
the next page for more information, or visit<br />
www.PREZISTA.com.<br />
If you or someone you know needs help paying for<br />
medicine, call 1-888-4PPA-NOW (1-888-477-2669) or<br />
go to www.pparx.org.<br />
Distributed by: Tibotec Therapeutics/Division of Ortho Biotech Products, L.P.<br />
Bridgewater, New Jersey 08807-0914<br />
©2009 Tibotec Therapeutics 01/09 28PRZ0249A1 PREZIS2183R
FDA-Approved Patient Labeling<br />
PREZISTA ® (darunavir) Tablets<br />
Patient Information about<br />
PREZISTA (pre-ZIS-ta)<br />
for HIV (Human Immunodeficiency Virus) Infection<br />
Generic name: darunavir (da-ROO-nuh-veer)<br />
ALERT: Find out about medicines that should NOT be taken with PREZISTA. Please<br />
also read the section “Who should not take PREZISTA?”.<br />
Please read this information before you start taking PREZISTA. Also, read the<br />
leaflet each time you renew your prescription, just in case anything has changed.<br />
Remember, this leaflet does not take the place of careful discussions with your<br />
doctor. You and your doctor should discuss your treatment with PREZISTA prior to<br />
the first time you take your medicine and at regular checkups. You should remain<br />
under a doctor’s care when using PREZISTA and should not change or stop<br />
treatment without first talking with a doctor.<br />
WHAT IS THE MOST IMPORTANT INFORMATION I SHOULD<br />
KNOW ABOUT PREZISTA?<br />
PREZISTA, together with NORVIR ® (ritonavir), has rarely been observed to cause<br />
liver problems which may be life-threatening. It was not always clear if PREZISTA<br />
caused these liver problems because some patients had other illnesses or were<br />
taking other medicines. Your healthcare professional should do blood tests prior to<br />
initiating combination treatment including PREZISTA. If you have chronic hepatitis B<br />
or C infection, your healthcare professional should check your blood tests more often<br />
because you have an increased chance of developing liver problems. Please also<br />
read the section “What are the possible side effects of PREZISTA?”.<br />
Rarely, PREZISTA has been reported to cause a severe or life-threatening rash.<br />
Contact your healthcare provider if you develop a rash. Your healthcare provider<br />
will advise you whether your symptoms can be managed on therapy or whether<br />
PREZISTA should be stopped.<br />
WHAT IS PREZISTA?<br />
PREZISTA is an oral tablet used for the treatment of HIV (Human Immunodeficiency<br />
Virus) infection in adults. HIV is the virus that causes AIDS (Acquired Immune<br />
Deficiency Syndrome). PREZISTA is a type of anti-HIV medicine called a protease<br />
(PRO-tee-ase) inhibitor.<br />
HOW DOES PREZISTA WORK?<br />
PREZISTA blocks HIV protease, an enzyme which is needed for HIV to multiply.<br />
When used with other anti-HIV medicines, PREZISTA can help to reduce the<br />
amount of HIV in your blood (called “viral load”) and increase your CD4 (T) cell<br />
count. HIV infection destroys CD4 (T) cells, which are important to the immune<br />
system. The immune system helps fight infection. Reducing the amount of HIV and<br />
increasing the CD4 (T) cell count may improve your immune system and, thus,<br />
reduce the risk of death or infections that can happen when your immune system<br />
is weak (opportunistic infections).<br />
PREZISTA is always taken with and at the same time as ritonavir (NORVIR ® ), in<br />
combination with other anti-HIV medicines. PREZISTA should also be taken with food.<br />
DOES PREZISTA CURE HIV OR AIDS?<br />
PREZISTA does not cure HIV infection or AIDS. At present, there is no cure for HIV<br />
infection. People taking PREZISTA may still develop infections or other conditions<br />
associated with HIV infection. Because of this, it is very important for you to remain<br />
under the care of a doctor. Although PREZISTA is not a cure for HIV or AIDS, PREZISTA<br />
can help reduce your risks of getting illnesses associated with HIV infection (AIDS<br />
and opportunistic infection) and eventually dying from these conditions.<br />
DOES PREZISTA REDUCE THE RISK OF PASSING HIV<br />
TO OTHERS?<br />
PREZISTA does not reduce the risk of passing HIV to others through sexual contact,<br />
sharing needles, or being exposed to your blood. For your health and the health of<br />
others, it is important to always practice safer sex by using a latex or polyurethane<br />
condom or other barrier method to lower the chance of sexual contact with any body<br />
fluids such as semen, vaginal secretions, or blood. Never re-use or share needles.<br />
Ask your doctor if you have any questions on how to prevent passing HIV to other<br />
people.<br />
WHAT SHOULD I TELL MY DOCTOR BEFORE I TAKE PREZISTA?<br />
Tell your doctor about all of your medical conditions, including if you:<br />
• are allergic to sulfa medicines.<br />
• have diabetes. In general, anti-HIV medicines, such as PREZISTA, might increase<br />
sugar levels in the blood.<br />
• have liver problems, including hepatitis B and/or C.<br />
• have hemophilia. Anti-HIV medicines, such as PREZISTA, might increase the risk<br />
of bleeding.<br />
• are pregnant or planning to become pregnant. The effects of PREZISTA on<br />
pregnant women or their unborn babies are not known. You and your doctor will<br />
need to decide if taking PREZISTA is right for you. If you take PREZISTA while you<br />
are pregnant, talk to your doctor about how you can be included in the<br />
Antiretroviral Pregnancy Registry.<br />
• are breastfeeding. Do not breastfeed if you are taking PREZISTA. You should not<br />
breastfeed if you have HIV because of the chance of passing HIV to your baby.<br />
Talk with your doctor about the best way to feed your baby.<br />
IMPORTANT PATIENT INFORMATION<br />
WHO SHOULD NOT TAKE PREZISTA?**<br />
Together with your doctor, you need to decide whether taking PREZISTA is right<br />
for you.<br />
Do not take PREZISTA if you:<br />
• are allergic to darunavir or any of the other ingredients in PREZISTA<br />
• are allergic to ritonavir (NORVIR ® )<br />
• take any of the following types of medicines because you could experience<br />
serious side effects:<br />
Type of Drug Examples of Generic Names (Brand Names)<br />
Ergot Derivatives dihydroergotamine (D.H.E. 45 ® , Migranal ® )<br />
(to treat migraine and ergonovine<br />
headaches) ergotamine (Cafergot ® , Ergomar ® )<br />
methylergonovine<br />
Gastrointestinal Motility Agent cisapride<br />
(to treat some digestive conditions)<br />
Neuroleptic pimozide (Orap ® )<br />
(to treat psychiatric conditions)<br />
Sedative/hypnotics oral midazolam<br />
(to treat trouble with triazolam (Halcion ® )<br />
sleeping and/or anxiety)<br />
Herbal Product St. John’s wort (Hypericum perforatum)<br />
HMG-CoA Reductase nhibitors lovastatin (Mevacor ® , Altoprev ® , Advicor ® )<br />
(also known as statins) simvastatin (Zocor ® , Simcor ® , Vytorin ® )<br />
(to lower cholesterol levels)<br />
Antimycobacterial rifampin (Rifadin ® , Rifater ® , Rifamate ® ,<br />
(to treat tuberculosis or Rimactane ® )<br />
Mycobacterium avium complex)<br />
CAN PREZISTA BE TAKEN WITH OTHER MEDICATIONS?**<br />
Tell your doctor about all the medicines you take including prescription and<br />
nonprescription medicines, vitamins, and herbal supplements. PREZISTA and many<br />
other medicines can interact. Sometimes serious side effects will happen if PREZISTA<br />
is taken with certain other medicines (see “Who should not take PREZISTA?”).<br />
Tell your doctor if you are taking estrogen-based contraceptives (birth control).<br />
PREZISTA might reduce the effectiveness of estrogen-based contraceptives. You<br />
must take additional precautions for birth control such as a condom.<br />
Tell your doctor if you take other anti-HIV medicines. PREZISTA can be combined with<br />
some other anti-HIV medicines while other combinations are not recommended.<br />
Tell your doctor if you are taking any of the following medicines:<br />
Type of Drug Examples of Generic Names (Brand Names)<br />
Antiarrhythmics bepridil<br />
(to treat abnormal lidocaine (Lidoderm ® )<br />
heart rhythms) quinidine<br />
amiodarone (Cordarone ® )<br />
digoxin (Lanoxin ® )<br />
flecainide (Tambocor ® )<br />
propafenone (Rythmol ® )<br />
Anticoagulants warfarin (Coumadin ® )<br />
(to treat and prevent blood clots)<br />
Anticonvulsants carbamazepine (Tegretol ® , Carbatrol ® )<br />
(to treat epilepsy and phenobarbital<br />
prevent seizures) phenytoin (Dilantin ® , Phenytek ® )<br />
Antidepressants trazodone (Desyrel ® )<br />
(to treat depression) desipramine (Norpramin ® )<br />
Anti-infectives clarithromycin (Biaxin ® )<br />
(to treat bacterial infections)<br />
Antifungals ketoconazole (Nizoral ® )<br />
(to treat fungal infections) itraconazole (Sporanox ® )<br />
voriconazole (Vfend ® )<br />
Antimycobacterials rifabutin (Mycobutin ® )<br />
(to treat tuberculosis or<br />
Mycobacterium avium complex)<br />
ß-Blockers metoprolol (Lopressor ® , Toprol-XL ® )<br />
(to treat high blood pressure, timolol (Betimol ® , Combigan ® , Istalol ® ,<br />
heart attack, or heart failure or Cosopt ® , Timoptic ® )<br />
to lower pressure in the eye)<br />
Benzodiazepines midazolam administered by injection<br />
(to treat anxiety and/or<br />
trouble with sleeping)<br />
Calcium Channel Blockers felodipine (Plendil ® )<br />
(to treat heart disease) nifedipine (Adalat ® )<br />
nicardipine (Cardene ® )<br />
Corticosteroids dexamethasone<br />
(to treat inflammation or asthma) fluticasone propionate (Advair Diskus ® ,<br />
Cutivate ® , Flonase ® , Flovent Diskus ® )<br />
HMG-CoA Reductase atorvastatin (Lipitor ® )<br />
Inhibitors pravastatin (Pravachol ® )<br />
(also known as statins) rosuvastatin (Crestor ® )<br />
(to lower cholesterol levels)<br />
T<br />
I<br />
(<br />
r<br />
N<br />
(<br />
a<br />
N<br />
(<br />
b<br />
P<br />
(<br />
S<br />
I<br />
(<br />
o<br />
T<br />
p<br />
T<br />
t<br />
y<br />
m<br />
o<br />
P<br />
d<br />
H<br />
T<br />
t<br />
•<br />
•<br />
P<br />
d<br />
y<br />
T<br />
d<br />
C<br />
s<br />
t<br />
P<br />
y<br />
e<br />
P<br />
I<br />
a<br />
s<br />
1<br />
T<br />
s<br />
P<br />
I<br />
a<br />
s<br />
6<br />
T<br />
s<br />
Y<br />
I<br />
d<br />
(<br />
W<br />
L<br />
c<br />
o<br />
e<br />
P<br />
p<br />
t<br />
m<br />
c<br />
i<br />
b
t<br />
.<br />
Type of Drug Examples of Generic Names (Brand Names)<br />
(cont.)<br />
Immunosuppressants cyclosporine (Sandimmune ® , Neoral ® )<br />
(to prevent organ transplant tacrolimus (Prograf ® )<br />
rejection) sirolimus (Rapamune ® )<br />
Narcotic Analgesics methadone<br />
(to treat narcotic withdrawal<br />
and dependence)<br />
Neuroleptics risperidone (Risperdal ® , Risperdal ® Consta ® ,<br />
(to treat schizophrenia or Risperdal ® M-TAB ® )<br />
bipolar disorder) thioridazine<br />
PDE-5 Inhibitors sildenafil (Viagra ® )<br />
(to treat erectile dysfunction) vardenafil (Levitra ® )<br />
tadalafil (Cialis ® )<br />
Selective Serotonin Reuptake paroxetine (Paxil ® )<br />
Inhibitors (SSRIs) sertraline (Zoloft ® )<br />
(to treat depression, anxiety,<br />
or panic disorder)<br />
Tell your doctor if you are taking any medicines that you obtained without a<br />
prescription.<br />
This is not a complete list of medicines that you should tell your doctor that you are<br />
taking. Know and keep track of all the medicines you take and have a list of them with<br />
you. Show this list to all of your doctors and pharmacists any time you get a new<br />
medicine. Both your doctor and your pharmacist can tell you if you can take these<br />
other medicines with PREZISTA. Do not start any new medicines while you are taking<br />
PREZISTA without first talking with your doctor or pharmacist. You can ask your<br />
doctor or pharmacist for a list of medicines that can interact with PREZISTA.<br />
HOW SHOULD I TAKE PREZISTA?<br />
Take PREZISTA tablets every day exactly as prescribed by your doctor. You must<br />
take ritonavir (NORVIR ® ) at the same time as PREZISTA.<br />
• For adults who have never taken anti-HIV medicines, the usual dose is 800 mg<br />
(two 400 mg tablets) of PREZISTA, together with 100 mg (one 100 mg capsule) of<br />
ritonavir (NORVIR ® ), once daily every day.<br />
• For adults who have taken anti-HIV medicines in the past, the usual dose is<br />
600 mg (one 600 mg tablet or two 300 mg tablets) of PREZISTA, together with<br />
100 mg (one 100 mg capsule) of ritonavir (NORVIR ® ), twice daily every day. Do<br />
not take PREZISTA once daily if you have taken anti-HIV medicines in the past.<br />
PREZISTA and ritonavir (NORVIR ® ) should be taken together at the same time every<br />
day. If you have questions about when to take PREZISTA and ritonavir (NORVIR ® ),<br />
your doctor can help you decide which schedule works for you.<br />
Take PREZISTA and ritonavir (NORVIR ® ) with food. Swallow the whole tablets with a<br />
drink such as water or milk. Do not chew the tablets.<br />
Continue taking PREZISTA and ritonavir (NORVIR ® ) unless your doctor tells you to<br />
stop. Take the exact amount of PREZISTA and ritonavir (NORVIR ® ) that your doctor<br />
tells you to take, right from the very start. To help make sure you will benefit from<br />
PREZISTA and ritonavir (NORVIR ® ), you must not skip doses or interrupt therapy. If<br />
you don’t take PREZISTA and ritonavir (NORVIR ® ) as prescribed, the beneficial<br />
effects of PREZISTA and ritonavir (NORVIR ® ) may be reduced or even lost.<br />
Patients taking PREZISTA once daily<br />
If you miss a dose of PREZISTA or ritonavir (NORVIR ® ) by more than 12 hours, wait<br />
and then take the next dose of PREZISTA and ritonavir (NORVIR ® ) at the regularly<br />
scheduled time. If you miss a dose of PREZISTA or ritonavir (NORVIR ® ) by less than<br />
12 hours, take your missed dose of PREZISTA and ritonavir (NORVIR ® ) immediately.<br />
Then take your next dose of PREZISTA and ritonavir (NORVIR ® ) at the regularly<br />
scheduled time.<br />
Patients taking PREZISTA twice daily<br />
If you miss a dose of PREZISTA or ritonavir (NORVIR ® ) by more than 6 hours, wait<br />
and then take the next dose of PREZISTA and ritonavir (NORVIR ® ) at the regularly<br />
scheduled time. If you miss a dose of PREZISTA or ritonavir (NORVIR ® ) by less than<br />
6 hours, take your missed dose of PREZISTA and ritonavir (NORVIR ® ) immediately.<br />
Then take your next dose of PREZISTA and ritonavir (NORVIR ® ) at the regularly<br />
scheduled time.<br />
You should always take PREZISTA and ritonavir (NORVIR ® ) together with food.<br />
If a dose of PREZISTA or ritonavir (NORVIR ® ) is skipped, do not double the next<br />
dose. Do not take more or less than your prescribed dose of PREZISTA or ritonavir<br />
(NORVIR ® ) at any one time.<br />
WHAT ARE THE POSSIBLE SIDE EFFECTS OF PREZISTA?<br />
Like all prescription drugs, PREZISTA can cause side effects. The following is not a<br />
complete list of side effects reported with PREZISTA when taken either alone or with<br />
other anti-HIV medicines. Do not rely on this leaflet alone for information about side<br />
effects. Your doctor can discuss with you a more complete list of side effects.<br />
PREZISTA, together with NORVIR ® (ritonavir), has rarely been observed to cause liver<br />
problems which may be life-threatening. It was not always clear if PREZISTA caused<br />
these liver problems because some patients had other illnesses or were taking other<br />
medicines. Your healthcare professional should do blood tests prior to initiating<br />
combination treatment including PREZISTA. If you have chronic hepatitis B or C<br />
infection, your healthcare professional should check your blood tests more often<br />
because you have an increased chance of developing liver problems.<br />
IMPORTANT PATIENT INFORMATION<br />
Talk to your healthcare professional about the signs and symptoms of liver problems.<br />
These may include yellowing of your skin or whites of your eyes, dark (tea colored)<br />
urine, pale colored stools (bowel movements), nausea, vomiting, loss of appetite, or<br />
pain, aching or sensitivity on your right side below your ribs.<br />
Rash has been reported in 10.3% of subjects receiving PREZISTA. In some patients,<br />
PREZISTA has been reported to cause a severe or life-threatening rash. Contact<br />
your healthcare provider if you develop a rash. Your healthcare provider will advise<br />
you whether your symptoms can be managed on therapy or whether PREZISTA<br />
should be stopped.<br />
Other relevant severe side effects reported at an uncommon or rare frequency<br />
were inflammation of the liver or pancreas, increased blood fat levels, diabetes,<br />
and changes in body fat.<br />
Some side effects are typical for anti-HIV medicines in the same family as PREZISTA.<br />
These are:<br />
• high blood sugar (hyperglycemia) and diabetes. This can happen in patients<br />
taking PREZISTA or other protease inhibitor medicines. Some patients have<br />
diabetes before starting treatment with PREZISTA which gets worse. Some<br />
patients get diabetes during treatment with PREZISTA. Some patients will<br />
need changes in their diabetes medicine. Some patients may need new<br />
diabetes medicine.<br />
• increased bleeding in patients with hemophilia.<br />
• changes in body fat. These changes can happen in patients taking anti-HIV<br />
medicines, including PREZISTA. The changes may include an increased amount<br />
of fat in the upper back and neck, breast, and around the back, chest, and<br />
stomach area. Loss of fat from the legs, arms, and face may also happen. The<br />
exact cause and long-term health effects of these conditions are not known.<br />
• immune reconstitution syndrome. In some patients with advanced HIV infection<br />
(AIDS) and a history of opportunistic infection, signs and symptoms of<br />
inflammation from previous infections may occur soon after anti-HIV treatment,<br />
including PREZISTA, is started. It is believed that these symptoms are due to an<br />
improvement in the body’s immune response, enabling the body to fight infections<br />
that may have been present with no obvious symptoms.<br />
The most common side effects include diarrhea, nausea, headache, and abdominal<br />
pain.<br />
Tell your doctor promptly about these or any other unusual symptoms. If the condition<br />
persists or worsens, seek medical attention.<br />
WHAT DO PREZISTA TABLETS LOOK LIKE?<br />
PREZISTA 300 mg tablets are orange, oval-shaped, film-coated tablets mentioning<br />
“300” on one side and “TMC114” on the other side.<br />
PREZISTA 400 mg tablets are light orange, oval-shaped, film-coated tablets<br />
mentioning “400” on one side and “TMC” on the other side.<br />
PREZISTA 600 mg tablets are orange, oval-shaped, film-coated tablets mentioning<br />
“600” on one side and “TMC” on the other side.<br />
HOW SHOULD I STORE PREZISTA TABLETS?<br />
Store PREZISTA tablets at room temperature (77°F (25°C)). Short-term exposure to<br />
higher or lower temperatures [from 59°F (15°C) to 86°F (30°C)] is acceptable. Ask your<br />
doctor or pharmacist if you have any questions about storing your tablets.<br />
This medication is prescribed for your particular condition. Do not use it for any<br />
other condition or give it to anybody else. Keep PREZISTA and all of your medicines<br />
out of the reach of children. If you suspect that more than the prescribed dose of<br />
this medicine has been taken, contact your local poison control center or<br />
emergency room immediately.<br />
This is a brief summary of information about PREZISTA. If you have any questions or<br />
concerns about either PREZISTA or HIV, talk to your doctor.<br />
For additional information, you may also call Tibotec Therapeutics at 1-877-REACH-TT<br />
or 1-877-732-2488.<br />
**The brands listed are the registered trademarks of their respective owners and are<br />
not trademarks of Tibotec Pharmaceuticals, Ltd.<br />
Manufactured for Tibotec, Inc. by: JOLLC, Gurabo, Puerto Rico<br />
Distributed by:<br />
Tibotec Therapeutics<br />
Division of Ortho Biotech Products, L.P., Raritan NJ 08869<br />
Patent Numbers: 5,843,946; 6,248,775; 6,335,460 and other US patents pending<br />
NORVIR ® is a registered trademark of its respective owner.<br />
PREZISTA ® is a registered trademark of Tibotec Pharmaceuticals, Ltd.<br />
© Tibotec, Inc. 2006 Revised: December 2008 10101707 P
TPAN empowers people<br />
living with HIV through<br />
peer-led programming,<br />
support services, information<br />
dissemination, and advocacy.<br />
We also provide services to<br />
the broader community to<br />
increase HIV knowledge and<br />
sensitivity, and to reduce the<br />
risk of infection.<br />
5537 North Broadway<br />
Chicago, IL 60640<br />
phone: (773) 989–9400<br />
fax: (773) 989–9494<br />
e-mail: tpan@tpan.com<br />
www.tpan.com<br />
Editor<br />
Jeff Berry<br />
Associate Editors<br />
Keith R. Green<br />
Enid Vázquez<br />
Editorial Assistants<br />
Sue Saltmarsh<br />
Gregory Tate<br />
Contributing Writers<br />
Liz Highleyman, Laura Jones,<br />
Jim Pickett, Sue Saltmarsh, Matt Sharp<br />
Medical Advisory Board<br />
Daniel S. Berger, M.D., Patrick G. Clay, Pharm.D.,<br />
Rupali Jain, Pharm.D., and Ross M. Slotten, M.D.<br />
Art Direction<br />
Russell McGonagle<br />
Advertising Inquiries<br />
publications@tpan.com<br />
Distribution<br />
Joe Fierke<br />
distribution@tpan.com<br />
© 2009. <strong>Positively</strong> <strong>Aware</strong> (ISSN: 1523-2883) is published bi-monthly by<br />
Test Positive <strong>Aware</strong> Network (TPAN), 5537 N. Broadway, Chicago, IL 60640.<br />
<strong>Positively</strong> <strong>Aware</strong> is a registered trademark of TPAN. All rights reserved.<br />
Circulation: 85,000. For reprint permission, contact Sue Saltmarsh. Six issues<br />
mailed bulkrate for $30 donation; mailed free to TPAN members or those<br />
unable to contribute.<br />
TPAN is an Illinois not-for-profit corporation, providing information and<br />
support to anyone concerned with HIV and AIDS issues. A person’s HIV status<br />
should not be assumed based on his or her article or photograph in <strong>Positively</strong><br />
<strong>Aware</strong>, membership in TPAN, or contributions to this journal.<br />
We encourage contribution of articles covering medical or personal aspects<br />
of HIV/AIDS. We reserve the right to edit or decline submitted articles. When<br />
published, the articles become the property of TPAN and its assigns. You may<br />
use your actual name or a pseudonym for publication, but please include your<br />
name and phone number.<br />
Opinions expressed in <strong>Positively</strong> <strong>Aware</strong> are not necessarily those of staff<br />
or membership or TPAN, its supporters and sponsors, or distributing agencies.<br />
Information, resources, and advertising in <strong>Positively</strong> <strong>Aware</strong> do not constitute<br />
endorsement or recommendation of any medical treatment or product.<br />
TPAN recommends that all medical treatments or products be discussed<br />
thoroughly and frankly with a licensed and fully HIV-informed medical practitioner,<br />
preferably a personal physician.<br />
Although <strong>Positively</strong> <strong>Aware</strong> takes great care to ensure the accuracy of all<br />
the information that it presents, <strong>Positively</strong> <strong>Aware</strong> staff and volunteers, TPAN,<br />
or the institutions and personnel who provide us with information cannot be<br />
held responsible for any damages, direct or consequential, that arise from use<br />
of this material or due to errors contained herein.<br />
6 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
Departments<br />
9 Editor’s Note<br />
Table of Contents<br />
Designing for Women—Not<br />
Just a Fashion Statement<br />
Anymore<br />
14 Readers Forum<br />
16 Ask the HIV Specialist<br />
This issue’s specialists:<br />
Amy Sitapati, M.D., AAHIVS and<br />
Joseph Caperna, M.D., MPH,<br />
AAHIVS<br />
17 From TPAN<br />
Embracing “the Change”<br />
TPAN’s new Executive Director<br />
welcomes a new chapter<br />
by Bruce Weiss<br />
18 News Briefs<br />
by Enid Vázquez<br />
52 What’s Goin’ On?<br />
Prepping for a PrEP<br />
trial<br />
Critical observations<br />
before the study even<br />
begins<br />
by Keith R. Green<br />
54 PA Online<br />
July / August 2009 Volume 20 Number 4<br />
On the Cover:<br />
Evany Turk, see page 45.<br />
Photography by ©Russell McGonagle<br />
Distribution of <strong>Positively</strong> <strong>Aware</strong> is supported<br />
in part through an unrestricted grant from<br />
GlaxoSmithKline<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
24<br />
34<br />
Articles<br />
24 One-on-One with Dawn Averitt Bridge<br />
Wife, mother, and advocate for HIV-positive women<br />
Interview by Jeff Berry<br />
28 The Naked Truth:<br />
Young, Beautiful and HIV Positive<br />
The courageous tale of Marvelyn Brown<br />
A book review by Keith R. Green<br />
34 The Feminization of an<br />
Epidemic<br />
28Monica<br />
Gandhi, M.D., MPH<br />
Women and HIV in the United States<br />
by Saraswati Iobst, M.D. and<br />
40 Tiger Medicine<br />
A Native American woman’s story<br />
by Sue Saltmarsh<br />
42 Protect Yourselves, Ladies<br />
Young or old, black women continue to be at higher risk<br />
by Enid Vázquez<br />
40<br />
A model, photographer, or author’s HIV status should not be assumed based on<br />
their appearance in <strong>Positively</strong> <strong>Aware</strong>.<br />
You can view these (and other stories from previous issues) online at<br />
www.tpan.com and www.positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong><br />
7
Table of Contents<br />
July / August 2009 Volume 20 Number 4<br />
Articles continued<br />
45 45 Evany Turk<br />
43 Joyce Turner Keller<br />
A minister with AIDS lays reality on the line<br />
Interview by Enid Vázquez<br />
A success story<br />
Interview by Sue Saltmarsh<br />
48 Reaching Out to Our Sisters<br />
Chicago women’s conference off ers knowledge and support<br />
by Enid Vázquez<br />
48<br />
43<br />
49 Doctors Urge the Government to Keep Up<br />
with Medical Progress<br />
HIV policy and funding left in the dust of treatment<br />
success<br />
by Enid Vázquez<br />
49<br />
8 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
Photo © Russell McGonagle<br />
Designing for Women—Not Just a<br />
Fashion Statement Anymore<br />
Certain words and phrases come to mind when we think<br />
about women and HIV. Invisible. Stigma. Shame. Femalecontrolled<br />
prevention methods. Feminization of an epidemic.<br />
Half of the world’s infected population.<br />
Th e problem is, we don’t always think about women and HIV<br />
as much as we probably should.<br />
According to the U. S. Centers for Disease Control and Prevention’s<br />
(CDC) most recent data, HIV infection was “the leading cause<br />
of death for black women (including African American women)<br />
aged 25–34 years…[and] the 5th leading cause of death among all<br />
women aged 35–44 years. Th e only diseases causing more deaths of<br />
women were cancer and heart disease.”<br />
Interestingly, according to the CDC “high-risk heterosexual<br />
contact was the source of 80% of…newly diagnosed infections.” But<br />
sadly enough, a recent study showed that women were “slightly less<br />
likely than men to receive prescriptions for the most eff ective treatments<br />
for HIV infection.”<br />
Th is issue of <strong>Positively</strong> <strong>Aware</strong> poses a simple question to<br />
our readers: Why is this happening—and what can we do about<br />
it? Unfortunately, simple questions don’t always bring forth easy<br />
solutions.<br />
One of the solutions, however, and one which you’ll read about<br />
more in this issue, is simple—at least in theory. Studies designed<br />
with women in mind, and in which women and people of color are<br />
adequately represented. Th is should be easier to do now that the<br />
vast majority of studies concerning HIV medications are not using<br />
experimental drugs, but, rather, are comparing standard-of-care<br />
treatments. It can be done by not only recruiting these populations,<br />
but also by retaining them, or keeping them, in the study. It’s also<br />
important to select the appropriate study sites for any particular<br />
study, and to then off er the sites the support they need in order to<br />
be successful.<br />
I was recently invited to attend an investigators’ meeting for the<br />
GRACE study. GRACE, which stands for Gender, Race, and Clinical<br />
Experience, was the fi rst study of its kind, enrolling approximately<br />
70% women, the majority of whom were women of color. Th e study<br />
was conducted by Tibotec Th erapeutics, using their newly approved<br />
HIV protease inhibitor, Prezista (darunavir), and newly approved<br />
HIV NNRTI, Intelence (etravirine) and was designed to observe<br />
diff erences in viral load and CD4 response according to gender<br />
and race. Th e results of the study will be published and presented<br />
at upcoming conferences and in scientifi c journals in the coming<br />
months, but some of the real successes of GRACE were not only in<br />
the data, but in the stories and people behind the study itself.<br />
Halfway through the day’s meeting, the folks at Tibotec decided<br />
to mix it up between invited community representatives and<br />
clinical site investigators, and those of us from the community were<br />
able to hear fi rsthand some of the amazing stories behind GRACE.<br />
Editor’s Note<br />
We heard the story of one study participant who called a site<br />
investigator over the Christmas holidays and told her she had run<br />
out of her meds, and was confused about which medications to take,<br />
and what they were for. Th e investigator cancelled an appointment<br />
she had, went and got her the replacement meds, and brought them<br />
to the study participant at the housing project where she lived, and<br />
then sat down with her to explain the regimen.<br />
Tragically, another woman’s house burned down, and her meds<br />
were destroyed in the fi re. Th e investigator went to go fi nd her, and<br />
called Tibotec to get her replacement meds.<br />
One individual in the study travelled 40 miles to every visit.<br />
Her mother read her the informed consent form for the study,<br />
because she wasn’t able to read it herself. But she was able to do all<br />
this, and had the motivation to succeed, because she received support<br />
from her family and didn’t feel stigmatized.<br />
We heard that, “Some of this is just the way women’s lives are.<br />
We are the caretakers, the wives, the mothers.”<br />
Ultimately, it speaks to the need for studies to be more inclusive<br />
than exclusive. “Don’t not consider a patient because of their<br />
past,” said one investigator.<br />
Th e common thread woven through many of these patient success<br />
stories were that patients felt valued, and that they mattered.<br />
One investigator said that they just wouldn’t let the patients fail.<br />
Another key to the study’s successes seemed to lie in the fact<br />
that study sites were chosen where the community practitioners<br />
were, and the study also provided the background regimen of drugs<br />
to participants, free of charge. And it raises the question, “What is<br />
the role of the clinical trial beyond getting data?”<br />
Approximately 10% of these sites had never conducted or participated<br />
in a study before. And granted, this was their only study,<br />
whereas many sites typically have a dozen or more studies going on<br />
at any given time, spreading their resources thin.<br />
Th e important thing to remember is that the success of a study<br />
can be measured not only by the data that comes out of it, but also<br />
by the thought and planning that goes into it, the care that is provided<br />
during the course of the study, and the ongoing connection<br />
with patients that is made through direct contact and support. And<br />
sometimes success is achieved just by going that extra mile, which<br />
can make a world of diff erence to someone taking part in a study.<br />
Take care of yourself, and each other.<br />
Jeff Berry, Editor<br />
publications@tpan.com<br />
<strong>Positively</strong> <strong>Aware</strong><br />
PA • July / August 2009 • tpan.com • positivelyaware.com 9
IMPORTANT INFORMATION ABOUT REYATAZ® (atazanavir sulfate)<br />
INDICATION: REYATAZ is a prescription medicine used in combination with other<br />
medicines to treat people who are infected with the human immunodeficiency<br />
virus (HIV). REYATAZ has been studied in 48-week trials in both patients who have<br />
taken or have never taken anti-HIV medicines.<br />
REYATAZ does not cure HIV or help prevent passing HIV to others.<br />
IMPORTANT SAFETY INFORMATION:<br />
Do not take REYATAZ if you are allergic to REYATAZ or to any of its<br />
ingredients.<br />
Do not take REYATAZ if you are taking the following medicines:<br />
rifampin, Camptosar ® (irinotecan), Versed ® (midazolam) when taken<br />
by mouth, Halcion ® (triazolam), ergot medicines, Propulsid ® (cisapride),<br />
St. John’ s wort (Hypericum perforatum), Mevacor ® (lovastatin),<br />
Zocor ® (simvastatin), Orap ® (pimozide), Crixivan ® (indinavir),<br />
or Viramune ® (nevirapine).<br />
Speak with your healthcare provider before taking the following<br />
medicines if you are taking REYATAZ: hormonal contraceptives such<br />
as birth control pills or contraceptive patch, Viagra ® (sildenafil),<br />
Levitra ® (vardenafil), Cialis ® (tadalafil), Vfend ® (voriconazole),<br />
AcipHex ® (rabeprazole), Nexium ® (esomeprazole), Prevacid ® (lansoprazole),<br />
Prilosec ® (omeprazole), Protonix ® (pantoprazole), Axid ® (nizatidine),<br />
Pepcid AC ® (famotidine), Tagamet ® (cimetidine), or Zantac ® (ranitidine),<br />
Advair ® (fluticasone propionate and salmeterol inhalation powder),<br />
Flonase ® or Flovent ® (fluticasone propionate), or Sustiva ® (efavirenz).<br />
The above lists of medicines are not complete. Discuss all prescription<br />
and non-prescription medicines, vitamin and herbal supplements, or<br />
other health preparations you are taking or plan to take with your<br />
healthcare provider.<br />
Tell your healthcare provider right away if you have any side effects, symptoms,<br />
or conditions, including the following:<br />
• Mild rash (redness and itching) without other symptoms sometimes occurs<br />
in patients taking REYATAZ, most often in the first few weeks after the medicine is<br />
started, and usually goes away within two weeks with no change in treatment.<br />
• Severe rash has occurred in a small number of patients taking REYATAZ.This type<br />
of rash is associated with other symptoms which could be serious and potentially<br />
cause death. If you develop a rash with any of the following symptoms,<br />
stop using REYATAZ and call your healthcare provider right away:<br />
– Shortness of breath<br />
– General ill-feeling or<br />
“flu-like” symptoms<br />
– Fever<br />
– Muscle or joint aches<br />
– Conjunctivitis (red or inflamed<br />
eyes, like “pink-eye”)<br />
– Blisters<br />
– Mouth sores<br />
– Swelling of your face<br />
• Yellowing of the skin and/or eyes may occur due to increases in bilirubin<br />
levels in the blood (bilirubin is made by the liver).<br />
• A change in the way your heart beats may occur and could be a<br />
symptom of a heart problem.<br />
• Diabetes and high blood sugar may occur in patients taking protease<br />
inhibitor medicines like REYATAZ.<br />
• If you have liver disease, including hepatitis B or C, your liver disease<br />
may get worse when you take anti-HIV medicines like REYATAZ.<br />
• Kidney stones have been reported in patients taking REYATAZ. Signs or<br />
symptoms of kidney stones include pain in your side, blood in your urine,<br />
and pain when you urinate.<br />
• End stage kidney disease managed with hemodialysis.<br />
• Some patients with hemophilia have increased bleeding problems with<br />
protease inhibitor medicines like REYATAZ.<br />
• Changes in body fat have been seen in some patients taking anti-HIV<br />
medicines. The cause and long-term effects are not known at this time.<br />
Other side effects of REYATAZ taken with other anti-HIV medicines include:<br />
nausea, headache, stomach pain, vomiting, diarrhea, depression, fever, dizziness,<br />
trouble sleeping, numbness, and tingling or burning of hands or feet.<br />
You should take REYATAZ once daily with food (a meal or snack). You should take<br />
REYATAZ and your other anti-HIV medicines exactly as instructed by your<br />
healthcare provider.<br />
You are encouraged to report negative side effects of prescription drugs<br />
to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.<br />
On REYATAZ,<br />
Thursday<br />
5:30<br />
Choir<br />
practice<br />
Wednesday<br />
Mary’s<br />
birthday<br />
party<br />
Buy new<br />
shoes<br />
for Latisha<br />
Fight HIV your way.<br />
Please see Important Patient Information<br />
about REYATAZ on adjacent pages.
how you spen d your time is up to you.<br />
Once-daily REYATAZ can fit into your schedule and help fight your HIV.<br />
REYATAZ, a protease inhibitor (PI), in HIV combination therapy:<br />
◆ Can help lower your viral load and raise your T-cell (CD4+ cell) count<br />
◆ Has a low chance of diarrhea (shown in clinical trials) *<br />
◆ Is taken once a day with a snack or meal<br />
* REYATAZ in combination therapy had a 1%-3% rate of moderate-to-severe diarrhea.<br />
REYATAZ is one of several treatment options your doctor may consider.<br />
Ask your healthcare team about REYATAZ. www.REYATAZ.com<br />
Individual results may vary.<br />
REYATAZ does not cure HIV, a serious disease, and has not been shown to reduce the risk of passing HIV to others.<br />
REYATAZ is a registered trademark of Bristol-Myers Squibb Company.<br />
SUSTIVA is a registered trademark of Bristol-Myers Squibb Pharma<br />
Company. All other trademarks are the property of their respective<br />
owners and not of Bristol-Myers Squibb.<br />
© 2009 Bristol-Myers Squibb Company, Princeton, NJ 08543 U.S.A.<br />
687US09AB10103 04/09
687US09AB10103_8x10.5: 5/27/09 9:20 AM Page 3<br />
FDA-Approved Patient Labeling<br />
Patient Information<br />
REYATAZ ® (RAY-ah-taz)<br />
(generic name = atazanavir sulfate)<br />
Capsules<br />
ALERT: Find out about medicines that should NOT be taken with REYATAZ. Read<br />
the section “What important information should I know about taking REYATAZ with<br />
other medicines?”<br />
Read the Patient Information that comes with REYATAZ before you start using it and<br />
each time you get a refill. There may be new information. This leaflet provides a<br />
summary about REYATAZ and does not include everything there is to know about your<br />
medicine. This information does not take the place of talking with your healthcare<br />
provider about your medical condition or treatment.<br />
What is REYATAZ?<br />
REYATAZ is a prescription medicine used with other anti-HIV medicines to treat people<br />
who are infected with the human immunodeficiency virus (HIV). HIV is the virus that<br />
causes acquired immune deficiency syndrome (AIDS). REYATAZ is a type of anti-HIV<br />
medicine called a protease inhibitor. HIV infection destroys CD4+ (T) cells, which are<br />
important to the immune system. The immune system helps fight infection. After a<br />
large number of (T) cells are destroyed, AIDS develops. REYATAZ helps to block HIV<br />
protease, an enzyme that is needed for the HIV virus to multiply. REYATAZ may lower<br />
the amount of HIV in your blood, help your body keep its supply of CD4+ (T) cells, and<br />
reduce the risk of death and illness associated with HIV.<br />
Does REYATAZ cure HIV or AIDS?<br />
REYATAZ does not cure HIV infection or AIDS. At present there is no cure for<br />
HIV infection. People taking REYATAZ may still get opportunistic infections or other<br />
conditions that happen with HIV infection. Opportunistic infections are infections<br />
that develop because the immune system is weak. Some of these conditions are<br />
pneumonia, herpes virus infections, and Mycobacterium avium complex (MAC)<br />
infections. It is very important that you see your healthcare provider regularly<br />
while taking REYATAZ.<br />
REYATAZ does not lower your chance of passing HIV to other people through<br />
sexual contact, sharing needles, or being exposed to your blood. For your health<br />
and the health of others, it is important to always practice safer sex by using a latex<br />
or polyurethane condom or other barrier to lower the chance of sexual contact with<br />
semen, vaginal secretions, or blood. Never use or share dirty needles.<br />
Who should not take REYATAZ?<br />
Do not take REYATAZ if you:<br />
• are taking certain medicines. (See “What important information should I know<br />
about taking REYATAZ with other medicines?”) Serious life-threatening side<br />
effects or death may happen. Before you take REYATAZ, tell your healthcare<br />
provider about all medicines you are taking or planning to take. These<br />
include other prescription and nonprescription medicines, vitamins, and herbal<br />
supplements.<br />
• are allergic to REYATAZ or to any of its ingredients. The active ingredient is<br />
atazanavir sulfate. See the end of this leaflet for a complete list of ingredients<br />
in REYATAZ. Tell your healthcare provider if you think you have had an allergic<br />
reaction to any of these ingredients.<br />
What should I tell my healthcare provider before I take REYATAZ?<br />
Tell your healthcare provider:<br />
• If you are pregnant or planning to become pregnant. It is not known if<br />
REYATAZ can harm your unborn baby. Pregnant women have experienced<br />
serious side effects when taking REYATAZ with other HIV medicines called<br />
nucleoside analogues. You and your healthcare provider will need to decide if<br />
REYATAZ is right for you. If you use REYATAZ while you are pregnant, talk to<br />
your healthcare provider about the Antiretroviral Pregnancy Registry.<br />
• If you are breast-feeding. You should not breast-feed if you are HIV-positive<br />
because of the chance of passing HIV to your baby. Also, it is not known if<br />
REYATAZ can pass into your breast milk and if it can harm your baby. If you are<br />
a woman who has or will have a baby, talk with your healthcare provider about<br />
the best way to feed your baby.<br />
• If you have liver problems or are infected with the hepatitis B or C virus.<br />
See “What are the possible side effects of REYATAZ?”<br />
• If you have end stage kidney disease managed with hemodialysis.<br />
• If you have diabetes. See “What are the possible side effects of REYATAZ?”<br />
• If you have hemophilia. See “What are the possible side effects of<br />
REYATAZ?”<br />
• About all the medicines you take including prescription and nonprescription<br />
medicines, vitamins, and herbal supplements. Keep a list of your medicines<br />
with you to show your healthcare provider. For more information, see “What<br />
important information should I know about taking REYATAZ with other<br />
medicines?” and “Who should not take REYATAZ?” Some medicines can cause<br />
serious side effects if taken with REYATAZ.<br />
REYATAZ ® (atazanavir sulfate)<br />
How should I take REYATAZ?<br />
• Take REYATAZ once every day exactly as instructed by your healthcare<br />
provider. Your healthcare provider will prescribe the amount of REYATAZ that<br />
is right for you.<br />
• For adults who have never taken anti-HIV medicines before, the dose<br />
is 300 mg once daily with 100 mg of NORVIR ® (ritonavir) once daily<br />
taken with food. For adults who are unable to tolerate ritonavir, 400 mg<br />
(two 200-mg capsules) once daily (without NORVIR ® ) taken with food<br />
is recommended.<br />
• For adults who have taken anti-HIV medicines in the past, the usual dose is<br />
300 mg plus 100 mg of NORVIR ® (ritonavir) once daily taken with food.<br />
• Your dose will depend on your liver function and on the other anti-HIV medicines<br />
that you are taking. REYATAZ is always used with other anti-HIV medicines. If<br />
you are taking REYATAZ with SUSTIVA ® (efavirenz) or with VIREAD ® (tenofovir<br />
disoproxil fumarate), you should also be taking NORVIR ® (ritonavir).<br />
• Always take REYATAZ with food (a meal or snack) to help it work better.<br />
Swallow the capsules whole. Do not open the capsules. Take REYATAZ at the<br />
same time each day.<br />
• If you are taking antacids or didanosine (VIDEX ® or VIDEX ® EC), take<br />
REYATAZ 2 hours before or 1 hour after these medicines.<br />
• If you are taking medicines for indigestion, heartburn, or ulcers such<br />
as AXID ® (nizatidine), PEPCID AC ® (famotidine), TAGAMET ® (cimetidine),<br />
ZANTAC ® (ranitidine), AcipHex ® (rabeprazole), NEXIUM ® (esomeprazole),<br />
PREVACID ® (lansoprazole), PRILOSEC ® (omeprazole), or PROTONIX ®<br />
(pantoprazole), talk to your healthcare provider.<br />
• Do not change your dose or stop taking REYATAZ without first talking with<br />
your healthcare provider. It is important to stay under a healthcare provider’s<br />
care while taking REYATAZ.<br />
• When your supply of REYATAZ starts to run low, get more from your<br />
healthcare provider or pharmacy. It is important not to run out of REYATAZ. The<br />
amount of HIV in your blood may increase if the medicine is stopped for even a<br />
short time.<br />
• If you miss a dose of REYATAZ, take it as soon as possible and then take<br />
your next scheduled dose at its regular time. If, however, it is within 6 hours<br />
of your next dose, do not take the missed dose. Wait and take the next dose at<br />
the regular time. Do not double the next dose. It is important that you do not<br />
miss any doses of REYATAZ or your other anti-HIV medicines.<br />
• If you take more than the prescribed dose of REYATAZ, call your healthcare<br />
provider or poison control center right away.<br />
Can children take REYATAZ?<br />
Dosing recommendations are available for children 6 years of age and older for<br />
REYATAZ Capsules. Dosing recommendations are not available for children from<br />
3 months to less than 6 years of age. REYATAZ should not be used in babies under<br />
the age of 3 months.<br />
What are the possible side effects of REYATAZ?<br />
The following list of side effects is not complete. Report any new or continuing<br />
symptoms to your healthcare provider. If you have questions about side effects, ask<br />
your healthcare provider. Your healthcare provider may be able to help you manage<br />
these side effects.<br />
The following side effects have been reported with REYATAZ:<br />
• mild rash (redness and itching) without other symptoms sometimes occurs in<br />
patients taking REYATAZ, most often in the first few weeks after the medicine<br />
is started. Rashes usually go away within 2 weeks with no change in treatment.<br />
Tell your healthcare provider if rash occurs.<br />
• severe rash: In a small number of patients, a rash can develop that is associated<br />
with other symptoms which could be serious and potentially cause death.<br />
If you develop a rash with any of the following symptoms stop using<br />
REYATAZ and call your healthcare provider right away:<br />
• shortness of breath<br />
• general ill feeling or “flu-like” symptoms<br />
• fever<br />
• muscle or joint aches<br />
• conjunctivitis (red or inflamed eyes, like “pink eye”)<br />
• blisters<br />
• mouth sores<br />
• swelling of your face<br />
• yellowing of the skin or eyes. These effects may be due to increases in<br />
bilirubin levels in the blood (bilirubin is made by the liver). Call your healthcare<br />
provider if your skin or the white part of your eyes turn yellow. Although these<br />
effects may not be damaging to your liver, skin, or eyes, it is important to tell<br />
your healthcare provider promptly if they occur.
REYATAZ ® (atazanavir sulfate) REYATAZ ® (atazanavir sulfate)<br />
• a change in the way your heart beats (heart rhythm change). Call your<br />
healthcare provider right away if you get dizzy or lightheaded. These could be<br />
symptoms of a heart problem.<br />
• diabetes and high blood sugar (hyperglycemia) sometimes happen in<br />
patients taking protease inhibitor medicines like REYATAZ. Some patients had<br />
diabetes before taking protease inhibitors while others did not. Some patients<br />
may need changes in their diabetes medicine.<br />
• if you have liver disease including hepatitis B or C, your liver disease may get<br />
worse when you take anti-HIV medicines like REYATAZ.<br />
• kidney stones have been reported in patients taking REYATAZ. If you develop<br />
signs or symptoms of kidney stones (pain in your side, blood in your urine, pain<br />
when you urinate) tell your healthcare provider promptly.<br />
• some patients with hemophilia have increased bleeding problems with<br />
protease inhibitors like REYATAZ.<br />
• changes in body fat. These changes may include an increased amount of fat in<br />
the upper back and neck (“buffalo hump”), breast, and around the trunk. Loss<br />
of fat from the legs, arms, and face may also happen. The cause and long-term<br />
health effects of these conditions are not known at this time.<br />
Other common side effects of REYATAZ taken with other anti-HIV medicines include<br />
nausea; headache; stomach pain; vomiting; diarrhea; depression; fever; dizziness;<br />
trouble sleeping; numbness, tingling, or burning of hands or feet; and muscle pain.<br />
Gallbladder disorders (which may include gallstones and gallbladder inflammation)<br />
have been reported in patients taking REYATAZ.<br />
What important information should I know about taking REYATAZ with other<br />
medicines?<br />
Do not take REYATAZ if you take the following medicines (not all brands may<br />
be listed; tell your healthcare provider about all the medicines you take).<br />
REYATAZ may cause serious, life-threatening side effects or death when used<br />
with these medicines.<br />
• Ergot medicines: dihydroergotamine, ergonovine, ergotamine, and<br />
methylergonovine such as CAFERGOT ® , MIGRANAL ® , D.H.E. 45 ® , ergotrate<br />
maleate, METHERGINE ® , and others (used for migraine headaches).<br />
• ORAP ® (pimozide, used for Tourette’s disorder).<br />
• PROPULSID ® (cisapride, used for certain stomach problems).<br />
• Triazolam, also known as HALCION ® (used for insomnia).<br />
• Midazolam, also known as VERSED ® (used for sedation), when taken by mouth.<br />
Do not take the following medicines with REYATAZ because of possible serious<br />
side effects:<br />
• CAMPTOSAR ® (irinotecan, used for cancer).<br />
• CRIXIVAN ® (indinavir, used for HIV infection). Both REYATAZ and CRIXIVAN<br />
sometimes cause increased levels of bilirubin in the blood.<br />
• Cholesterol-lowering medicines MEVACOR ® (lovastatin) or ZOCOR ®<br />
(simvastatin).<br />
Do not take the following medicines with REYATAZ because they may lower the<br />
amount of REYATAZ in your blood. This may lead to an increased HIV viral load.<br />
Resistance to REYATAZ or cross-resistance to other HIV medicines may develop:<br />
• Rifampin (also known as RIMACTANE ® , RIFADIN ® , RIFATER ® , or RIFAMATE ® ,<br />
used for tuberculosis).<br />
• St. John’s wort (Hypericum perforatum), an herbal product sold as a dietary<br />
supplement, or products containing St. John’s wort.<br />
• VIRAMUNE ® (nevirapine, used for HIV infection).<br />
Do not take the following medicine if you are taking REYATAZ and NORVIR ®<br />
together:<br />
• VFEND ® (voriconazole).<br />
The following medicines may require your healthcare provider to monitor your<br />
therapy more closely:<br />
• CIALIS ® (tadalafil), LEVITRA ® (vardenafil), or VIAGRA ® (sildenafil). REYATAZ<br />
may increase the chances of serious side effects that can happen with CIALIS,<br />
LEVITRA, or VIAGRA. Do not use CIALIS, LEVITRA, or VIAGRA while you are taking<br />
REYATAZ unless your healthcare provider tells you it is okay.<br />
• LIPITOR ® (atorvastatin) or CRESTOR ® (rosuvastatin). There is an increased<br />
chance of serious side effects if you take REYATAZ with this cholesterollowering<br />
medicine.<br />
• Medicines for abnormal heart rhythm: CORDARONE ® (amiodarone), lidocaine,<br />
quinidine (also known as CARDIOQUIN ® , QUINIDEX ® , and others).<br />
• VASCOR ® (bepridil, used for chest pain).<br />
• COUMADIN ® (warfarin).<br />
• Tricyclic antidepressants such as ELAVIL ® (amitriptyline), NORPRAMIN ®<br />
(desipramine), SINEQUAN ® (doxepin), SURMONTIL ® (trimipramine), TOFRANIL ®<br />
(imipramine), or VIVACTIL ® (protriptyline).<br />
• Medicines to prevent organ transplant rejection: SANDIMMUNE ® or NEORAL ®<br />
(cyclosporin), RAPAMUNE ® (sirolimus), or PROGRAF ® (tacrolimus).<br />
• The antidepressant trazodone (DESYREL ® and others).<br />
• Fluticasone propionate (ADVAIR ® , FLONASE ® , FLOVENT ® ), given by nose or<br />
inhaled to treat allergic symptoms or asthma. Your doctor may choose not to<br />
keep you on fluticasone, especially if you are also taking NORVIR ® .<br />
The following medicines may require a change in the dose or dose schedule of<br />
either REYATAZ or the other medicine:<br />
• INVIRASE ® (saquinavir).<br />
• NORVIR ® (ritonavir).<br />
• SUSTIVA ® (efavirenz).<br />
• Antacids or buffered medicines.<br />
• VIDEX ® (didanosine).<br />
• VIREAD ® (tenofovir disoproxil fumarate).<br />
• MYCOBUTIN ® (rifabutin).<br />
• Calcium channel blockers such as CARDIZEM ® or TIAZAC ® (diltiazem),<br />
COVERA-HS ® or ISOPTIN SR ® (verapamil) and others.<br />
• BIAXIN ® (clarithromycin).<br />
• Medicines for indigestion, heartburn, or ulcers such as AXID ® (nizatidine),<br />
PEPCID AC ® (famotidine), TAGAMET ® (cimetidine), or ZANTAC ® (ranitidine).<br />
Talk to your healthcare provider about choosing an effective method of<br />
contraception. REYATAZ may affect the safety and effectiveness of hormonal<br />
contraceptives such as birth control pills or the contraceptive patch. Hormonal<br />
contraceptives do not prevent the spread of HIV to others.<br />
Remember:<br />
1. Know all the medicines you take.<br />
2. Tell your healthcare provider about all the medicines you take.<br />
3. Do not start a new medicine without talking to your healthcare provider.<br />
How should I store REYATAZ?<br />
• Store REYATAZ Capsules at room temperature, 59° to 86° F (15° to 30° C).<br />
Do not store this medicine in a damp place such as a bathroom medicine<br />
cabinet or near the kitchen sink.<br />
• Keep your medicine in a tightly closed container.<br />
• Keep all medicines out of the reach of children and pets at all times. Do not<br />
keep medicine that is out of date or that you no longer need. Dispose of unused<br />
medicines through community take-back disposal programs when available or<br />
place REYATAZ in an unrecognizable, closed container in the household trash.<br />
General information about REYATAZ<br />
This medicine was prescribed for your particular condition. Do not use REYATAZ for<br />
another condition. Do not give REYATAZ to other people, even if they have the same<br />
symptoms you have. It may harm them. Keep REYATAZ and all medicines out of<br />
the reach of children and pets.<br />
This summary does not include everything there is to know about REYATAZ. Medicines<br />
are sometimes prescribed for conditions that are not mentioned in patient information<br />
leaflets. Remember no written summary can replace careful discussion with your<br />
healthcare provider. If you would like more information, talk with your healthcare<br />
provider or you can call 1-800-321-1335.<br />
What are the ingredients in REYATAZ?<br />
Active Ingredient: atazanavir sulfate<br />
Inactive Ingredients: Crospovidone, lactose monohydrate (milk sugar), magnesium<br />
stearate, gelatin, FD&C Blue #2, and titanium dioxide.<br />
VIDEX ® and REYATAZ ® are registered trademarks of Bristol-Myers Squibb Company.<br />
COUMADIN ® and SUSTIVA ® are registered trademarks of Bristol-Myers Squibb<br />
Pharma Company. DESYREL ® is a registered trademark of Mead Johnson and<br />
Company. Other brands listed are the trademarks of their respective owners and are<br />
not trademarks of Bristol-Myers Squibb Company.<br />
US Patent Nos: 5,849,911 and 6,087,383<br />
Princeton, NJ 08543 USA<br />
1246226A3 F1-B0001B-04-09 Rev April 2009
Readers Forum<br />
Ask the HIV Specialist<br />
Correction<br />
Last issue’s HIV Specialist’s credentials<br />
were mistakenly listed. Th e correct listing is<br />
Sharon Valenti, MSN, ACNP-BC, AAHIVS,<br />
AACRN, HIV/AIDS Nurse Practitioner, and<br />
her affi liation is with St. John Hospital and<br />
Medical Center in Detroit, Michigan. We<br />
apologize for the error!<br />
Thanks to “Dr. Z”<br />
Hi! My name is Patricia and I’ve been<br />
HIV-positive since May of 1996. Forgive me<br />
if this letter is a little crude, as I’m real nervous.<br />
I’ve never really reached out in this<br />
manner before.<br />
I was infected through IV drug use. As<br />
bad as this is, I made a conscious decision<br />
and I guess I must have thought I could<br />
“beat the odds.” Well, I didn’t. In all honesty,<br />
I’d been living in total disregard for my life,<br />
afraid if I slowed down long enough, that I<br />
would have to face my demons and I wasn’t<br />
going to do that, I was just too scared.<br />
One can only run for so long and it<br />
was my time to stop. I ended up in prison,<br />
with a whole new attitude and outlook on<br />
life. I was so glad when I got arrested. I<br />
know how that sounds, but it meant I could<br />
fi nally stop using and killing myself. And<br />
when I was arrested, I was sent to Cook<br />
County [Jail, Chicago], where I met the<br />
smartest and greatest doctor in the world,<br />
<strong>Positively</strong> <strong>Aware</strong> will treat all<br />
communications (letters, faxes, e-mail,<br />
etc.) as letters to the editor unless<br />
otherwise instructed. We reserve the<br />
right to edit for length, style, or clarity.<br />
Please advise if we can use your name<br />
and city.<br />
Write to: <strong>Positively</strong> <strong>Aware</strong>,<br />
5537 North Broadway<br />
Chicago, IL 60640<br />
Fax: (773) 989–9494<br />
E-mail: readersforum@tpan.com<br />
14<br />
Dr. [Chad] Zawitz! I truly thank God every<br />
day for him.<br />
I had been shooting heroin for years<br />
and I had a habit of sucking on the cotton<br />
that I used to draw up the heroin—<br />
long story short, I had been dealing with<br />
abscesses all over my body for three years<br />
straight. I’d seen doctor aft er doctor, had<br />
six surgeries and have scars, including one<br />
from my shoulder to my elbow because<br />
the muscle deteriorated so badly from the<br />
abscesses. Th ere wasn’t a doctor who could<br />
fi gure out why until I met “Dr. Z”—he was<br />
genius enough to ask if I sucked on the cottons<br />
and he saved my life.<br />
Now, here I am with a CD4 count of<br />
114 and a viral load that’s undetectable. I’m<br />
on Truvada and Kaletra and the only side<br />
eff ect I’ve had is diarrhea. I realize that I am<br />
a walking miracle. I’m still in prison, but<br />
I’m in the drug program here and I remain<br />
open and teachable. I’m in therapy for all<br />
my other issues and I’m working hard so<br />
I’ll never have to come back here or pick up<br />
another drug.<br />
I’ve been doing so well, in fact, that I’ve<br />
been asked to be an HIV peer educator and<br />
I’m starting a support group. I’m totally saddened<br />
by the way women here are so afraid<br />
to come to a support group that’s 100% confi<br />
dential. I’m in a prison with 500 women,<br />
most of whom have one or more risky<br />
behaviors and, so far, only two of us want to<br />
be open and honest about it. I understand—<br />
I’ve turned down the chance to speak at a<br />
couple of health seminars because it would<br />
mean “coming out of the closet,” and if the<br />
women here aren’t willing to be honest with<br />
themselves because of what might happen,<br />
what will they do to me?<br />
So I need some help as to how to handle<br />
“coming out” and I also want to be informed<br />
and armed with the best and latest information<br />
possible. Also, I’m to be released in<br />
about three months and I’m scared to death.<br />
Aft er all the hard work I’ve done, I’d hate to<br />
lose it because I didn’t have a proper plan<br />
in place. I would be happy and grateful for<br />
advice from anyone. Please help. Th ank you<br />
so much.<br />
Patricia Douglass R37503<br />
PO Box 3035 B-wing<br />
Decatur, IL 62524-3035<br />
<strong>Positively</strong> <strong>Aware</strong><br />
Enid Vázquez resp onds: Chad Zawitz<br />
was in New Orleans during Hurricane<br />
Katrina in the Fall of 2005 and is one of the<br />
doct ors who rushed to the aid of survivors.<br />
At the time, he was slated to provide the doctor’s<br />
comments to our 2006 HIV Drug Guide,<br />
and he kept his deadline a few weeks later<br />
desp ite the time taken for the emergency<br />
care. His presentations here at Test Positive<br />
<strong>Aware</strong> Network are always on the mark and<br />
well-received. We meet a lot of the best and<br />
brightest HIV sp ecialist s and we agree, Dr. Z.<br />
is one of them. We passed your letter on to<br />
him, and he was moved by your words. Good<br />
luck to you.<br />
Long-Term Survivor<br />
I want to let you know how much<br />
I appreciated your article “Th e Graying<br />
Epidemic” [Editor’s Note, May/June issue].<br />
Just when I start feeling like the only one<br />
concerned about what my future holds, and<br />
how much longer I have to live, I fi nd an<br />
article that gives me some hope.<br />
I have been HIV-positive for 21 years.<br />
I am 42. Without exaggeration, my closest<br />
friends from college who were gay are dead.<br />
I didn’t plan on living past 35. I worked so<br />
hard to be as successful as possible so that<br />
when I did die, my family wouldn’t be burdened<br />
with the cost of my medical issues or<br />
my death.<br />
I reached 35 and was not ready for<br />
the future. Aft er a 13-year relationship<br />
ended and I started with a new company, I<br />
couldn’t imagine what was next. I was now<br />
alone, except for my most faithful dog, and<br />
I was scared. What if I get sick, what if I get<br />
hurt? I felt like I was living in an old—I am<br />
talking 60ish—body.<br />
I got hurt last year and aft er two other<br />
surgeries, I had to have my left hip replaced,<br />
aft er a long fi ght with the insurance company.<br />
Aft er almost a year to date, AVN<br />
[avascular necrosis] has taken control of<br />
my right hip. I should get it replaced within<br />
a month.<br />
I can’t help but wonder if this is only<br />
the beginning of the end. I am now on disability<br />
and have to fi ght with the long-term<br />
disability company almost quarterly to<br />
prove that I am not able to work. I try to<br />
be positive about my situation, but I have<br />
never felt so worthless. Th at’s something I<br />
am working on.<br />
PA • July / August 2009 • tpan.com • positivelyaware.com
I am volunteering with YouthPride in<br />
Atlanta. I enjoy working with young people.<br />
I perform HIV testing and risk management,<br />
along with fundraising. I fi nd that<br />
rewarding.<br />
I could go on, but I think you understand<br />
where I am coming from. Who knew<br />
there would be a group of “long-term” survivors<br />
at all? I tell myself that I am one of<br />
the lucky ones.<br />
Th anks again for your article!<br />
Manuel Robles<br />
Via the Internet<br />
Missing Chicago<br />
Mr. Jeff Berry,<br />
When I read your articles you help me<br />
stay connected to Chicago and, of course,<br />
the latest of news to keep my health in order.<br />
You help me to think of all of our wild times<br />
at the Bistro and up and down Halsted St.<br />
Th ose were the good old days. We didn’t<br />
have a care in the world. I have been living<br />
in Florida for the last fi ve years, working in<br />
St. Pete but living in Naples. I only go home<br />
on my days off . It’s always on my mind to<br />
move back home, but until I do, thanks for<br />
making me feel like a part of Chicago.<br />
Marty<br />
Naples, Florida<br />
Comments to Nelson Vergel<br />
Dear Nelson,<br />
I just read your interview by <strong>Positively</strong><br />
<strong>Aware</strong> on Th e Body’s website and I have to<br />
say that you are an inspiration to me as a<br />
person living with AIDS.<br />
I was diagnosed at the age of 30 with<br />
zero T-cells and subsequently became very<br />
ill, fi nally losing my hearing, my eyesight,<br />
and my ability to walk from CMV myolitis.<br />
I was considered terminal and set to be<br />
sent off to hospice, but my parents took me<br />
home and nursed me back to health. I have<br />
regained my hearing and learned how to<br />
walk again, but I am still completely blind. I<br />
am now healthier in many ways than I ever<br />
was before, going to the gym every day, eating<br />
right, being pro-active about my health,<br />
and always looking for alternative solutions<br />
to my residual problems.<br />
I saw you speak to long-term survivors<br />
about six years ago in Ft. Lauderdale. I was<br />
there with my guide dog and a blind friend<br />
and his dog too. I was so proud and honored<br />
to meet you then and you were a great<br />
role model for me and my recovery. I am<br />
still inspired by you and wanted to let you<br />
know that I understand what you feel every<br />
day. Yes, it is hard, but please be comforted<br />
in knowing that you have changed lives<br />
and brought so much to so many. I hope<br />
that will sustain your mind and your body<br />
as well.<br />
I now speak to many diff erent groups<br />
about blindness and guide dogs and I am<br />
advocating for blind rights and accessibility<br />
in my community of Miami Beach, Florida.<br />
In many ways, this illness has been a gift ,<br />
enabling me to educate and help many others.<br />
I hope you feel the same way. Th ank you<br />
for being you.<br />
R. David New<br />
Miami Beach, Florida<br />
Hi, Nelson,<br />
Imagine my surprise when I opened<br />
my mail at Shanti and saw your picture on<br />
the cover of <strong>Positively</strong> <strong>Aware</strong>!<br />
I absolutely loved the article You’re<br />
Getting Older and Better.<br />
I love the title of your new book and<br />
am so looking forward to reading it when it<br />
hits the shelves.<br />
You look fabulous! Th ank you for your<br />
message, which profoundly aff ects so many<br />
people.<br />
Sarah Kasman<br />
Executive Director<br />
Shanti<br />
Dear Mr. Vergel,<br />
I recently read your profi le in the latest<br />
issue of <strong>Positively</strong> <strong>Aware</strong> and was impressed<br />
by the way you were able to frame the issue<br />
of aging with HIV. Our current work at<br />
ACRIA largely focuses on the psychosocial<br />
challenges of HIV and aging. If you haven’t<br />
seen it, please go to our website (www.acria.<br />
org) and you will fi nd a copy of the report<br />
“Research on Older Adults with HIV,” which<br />
is currently in press in an expanded form<br />
and should be available later this year. We<br />
also have a couple of booklets that address<br />
this issue from our HIV Health Literacy<br />
Program that are available at no cost.<br />
In addition to stigma, the two major<br />
issues we see facing adults aging with HIV<br />
are mental health (very high rates of depression)<br />
and the importance of social supports<br />
to meet the challenges of this condition now<br />
and in the future. In our New York City<br />
research, we are fi nding very high rates of<br />
health comorbidities, at approximately<br />
three times the rates found among older<br />
adults in general. We are currently working<br />
on interventions to address depression and<br />
social isolation.<br />
I noticed in the article that you are<br />
planning a conference to address this issue<br />
in the Houston area next year. If we could<br />
be of any assistance, please let us know.<br />
Mark Brennan, Ph.D.<br />
Senior Research Scientist<br />
Center on HIV and Aging<br />
AIDS Community Research Initiative of<br />
America (ACRIA)<br />
New York, New York e<br />
PA • July / August 2009 • tpan.com • positivelyaware.com 15<br />
<strong>Positively</strong> <strong>Aware</strong>
Ask the<br />
I am a 64-year-old male, diagnosed with HIV in 2006, and began<br />
taking Truvada and Kaletra (4 once daily). My viral load fell from<br />
362,000 to undetectable by early 2007 and remained undetectable<br />
until my last blood test in January this year. My doctor said it may be<br />
a blip, or the virus may have become resistant to the medication. I am<br />
scheduled for another blood test in early June, but the wait is making<br />
me very anxious. The last viral load reading was 108. My blood work<br />
for all other areas tested has been excellent, including cholesterol,<br />
PSA, liver and so on. My blood pressure is generally 115/72 or lower.<br />
I never miss my medication. If the virus has become resistant to the<br />
current medication, what are my options for other medication?<br />
Signed,<br />
Resistance or Blips?<br />
Dear ROB,<br />
We agree with your doctor. One does not know at this point<br />
[when the letter was received in February 2009] if this small increase<br />
in viral load was a “blip” or if the virus has become resistant.<br />
Is your provider an AAHIVM-credentialed HIV<br />
Specialist?<br />
If you are living with HIV, you have a lot of choices to<br />
make when seeking care and treatment. One of your most<br />
important choices is your health care practitioner—so why<br />
not choose someone who is knowledgeable about HIV and<br />
experienced in its treatment?<br />
The American Academy of HIV Medicine (AAHIVM)’s<br />
HIV Specialist credentialing program is the first and<br />
only clinical credentialing program offered domestically<br />
and internationally to physicians (MDs and DOs), nurse<br />
practioners, and physician assistants specializing in HIV<br />
care. HIV care providers become designated HIV Specialists<br />
after meeting experience and education requirements, and<br />
successfully completing a rigorous exam on HIV-specialized<br />
care. Look for the letters “AAHIVS” after their name.<br />
Locate an HIV Specialist<br />
Your search for an HIV Specialist is easy with AAHIVM’s<br />
online Find-A-Provider directory at www.aahivm.org. Just<br />
click on the “Find-A-Provider” window on the homepage, key<br />
in your location and click on the search button for a list of<br />
HIV Specialists near you.<br />
Due to space limitations, not all submitted questions can be<br />
answered in this column, but every effort is made to ensure<br />
you receive the information you have requested. For more<br />
information about AAHIVM, call 202-659-0699 or visit<br />
www.aahivm.org.<br />
<strong>Positively</strong> <strong>Aware</strong><br />
Submit your questions for Ask the HIV Specialist to AAHIVM@tpan.com<br />
This issue’s specialists:<br />
Amy Sitapati , M . D ., AAHIVS<br />
and Joseph Caperna , M . D ., MPH , AAHIVS<br />
If your virus has developed drug resistance, that is a topic for<br />
another column. We would need to see the results of a resistance test<br />
and the interpretation of resistance test results remains complicated.<br />
It is also important to know whether there is any new medical<br />
history, such as recent surgery, illness, or vaccination (these can<br />
increase viral load more than a blip, or greater than 200 copies/ml).<br />
A physician should assess you for new medications or herbs which<br />
might interact with the antivirals. Finally, we assume you are taking<br />
all doses of your medications. Intermittent “adherence” or not taking<br />
100% of the doses, can lead to blips.<br />
“Blips” are a common concern in the field of HIV. There are<br />
several ways to look at an increased viral load. Depending on which<br />
type of machine was used to measure the HIV viral load, the amount<br />
of virus used to classify undetectable will vary. A “blip” is a viral load<br />
increased to 200 (some authors use 400) copies/ml, slightly increased,<br />
but not completely undetectable.<br />
Historically, blips were discussed in 2000 or before, and at first<br />
were thought to predict future virologic failure, or that sometime in<br />
the future the viral load would increase dramatically. Using actual<br />
numbers, one example is a patient with less than 50 for years who<br />
has a new viral load of 188. It is uncertain whether or not this would<br />
mean the viral load might increase significantly (such as up to 3 logs<br />
or 188,000) in the near future. At the Durban International AIDS<br />
Conference in 2000, Dr. Diane Havlir presented a study of patients<br />
on indinavir [Crixivan] with prior long-term control of less than 50.<br />
Blips in this group did not predict future virologic failure. In contrast,<br />
Wensing et al, at the same conference, presented data on patients on<br />
different regimens. The Wensing study showed blips were associated<br />
with future greater increases in viral load.<br />
Again, a single blip does not mean virologic failure. In fact, the<br />
DHHS “Guidelines for the Use of Antiretroviral Agents in HIV-<br />
1-Infected Adults and Adolescents” (Nov. 2008) define virologic<br />
failure as “a confirmed HIV RNA level of greater than 400 copies/<br />
ml after 24 weeks, greater than 50 copies/ml after 48 weeks, or a<br />
repeated detectable HIV RNA level after prior suppression of viremia<br />
[viral load].”<br />
The definition of “blip” may change as newer assays (tests) are<br />
developed that detect down to incredible levels, such as less than 1<br />
copy/ml, and the new ability to see if patients with less than 50 have<br />
less than 1 or somewhere between 1–50, and what that might mean.<br />
We previously did not have this ability, and we are in transition with<br />
these more sensitive assays. Finally, as we look to the future, and the<br />
empowerment of patients, we hear of technology being developed<br />
that will allow patients to monitor their viral loads from home. Visit<br />
TheBody.com for excellent information on blips. e<br />
Amy Sitapati, M.D., AAHIVS<br />
Associate Director, Owen Clinic<br />
University of California, San Diego<br />
Joseph Caperna, M.D., MPH, AAHIVS<br />
Clinical Physician, Owen Clinic<br />
University of California, San Diego<br />
16 PA • July / August 2009 • tpan.com • positivelyaware.com
Photo © Russell McGonagle<br />
Embracing “the Change”<br />
TPAN’s new Executive Director welcomes a new chapter<br />
by Bruce Weiss<br />
I<br />
just made a complete change in my life. I packed up all my<br />
belongings, grabbed my dog, said goodbye to my friends, and<br />
left the city I had lived in for 15 years—Washington, D.C. I gave<br />
up far warmer weather and people I loved to make this move. But<br />
I took a wonderful opportunity to live in a great city like Chicago<br />
and to become part of an incredible organization called Test Positive<br />
<strong>Aware</strong> Network (TPAN).<br />
Well, not a complete change. I still work in the non-profi t sector,<br />
and continue my career in non-profi t management. Th is is the<br />
second Executive Director position I have held in my career. And<br />
TPAN is experiencing the same diffi cult economic times as almost<br />
every non-profi t in the current economy.<br />
I realize that you, the TPAN reader, might live anywhere in<br />
the country or the world, so I want to take a moment to tell you<br />
about TPAN. TPAN is an HIV care and prevention organization in<br />
Chicago with a staff of more than 30 very hard-working people and<br />
a volunteer base that really makes this organization possible. We<br />
pride ourselves on being “peer-led,” meaning that there are HIVpositive<br />
individuals throughout the organization, and that the voices<br />
of HIV-positive individuals aren’t just heard, but they continue<br />
to set the course of TPAN. We work hard to maintain, and even<br />
enhance, this culture and philosophy as we continue to grow.<br />
My focus for TPAN over the next year is nothing sexy or dramatic.<br />
While we hope to continue increasing the distribution of<br />
<strong>Positively</strong> <strong>Aware</strong>, our main focus in the next year will be internal.<br />
We will build our fi nancial stability in a challenging economic<br />
time, as well as improve the organization’s internal processes. As<br />
I said, nothing sexy, but absolutely vital to any non-profi t in 2009.<br />
Th is will involve change for TPAN—change you aren’t to likely see<br />
where you are, but change that will take place for staff and will<br />
hopefully improve the care and support we provide to clients. It is<br />
the kind of change that takes place underneath, where you might<br />
not notice it, until someone else mentions that they’ve noticed some<br />
changes and then it dawns on you that you have too.<br />
I recently had another life change that was more personal. And<br />
it makes it very clear to me why <strong>Positively</strong> <strong>Aware</strong> is so important for<br />
many HIV-positive people across the country. Soon aft er I moved to<br />
Chicago in April, I had a fi rst visit with my new doctor. He recommended<br />
a battery of tests, as doctors usually do, but he mentioned<br />
a few I didn’t recall ever having had before. Two weeks later, I went<br />
to see him and everything was great news, with a little surprise.<br />
He mentioned that I was in something called “andropause,” which<br />
means I had low testosterone. He told me the symptoms of andropause<br />
and it dawned on me, as he spoke, that I had all these symptoms.<br />
I had known that there was a pretty sudden change about four<br />
or fi ve years ago, when I started gaining weight, felt a lot less energy,<br />
a bit less “spark” in my life. Th at diminished spark meant both a<br />
decreased joy in my life, and a decreased desire for sex. All of this<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
From TPAN<br />
came rushing into my mind in about a minute as I began to discuss<br />
this with my doctor. It was an epiphany, to say the least.<br />
Th ere I was working in public health for years, running a<br />
health care clinic for part of that time, going to a doctor regularly,<br />
and I had never considered this as a possibility. It was right in front<br />
of me, but until a new doctor gave me the results and explained<br />
what the symptoms would look like, it had never crossed my mind.<br />
So I began using a testosterone gel about three weeks ago and the<br />
change has been pretty dramatic.<br />
Many people are not as fortunate as I am to have a doctor who<br />
is so thorough. Maybe if he had been my doctor a few years ago, I<br />
would have known this sooner, because I am guessing my decreasing<br />
testosterone didn’t happen suddenly or recently. Maybe not.<br />
But there are so many people living across this country who may<br />
have symptoms that have come on slowly over time, or even suddenly,<br />
but it never occurred to them to ask their doctor. Maybe their<br />
doctor doesn’t have as much awareness of important tests or they<br />
don’t screen their patients as thoroughly and don’t ask the right<br />
questions.<br />
“It was right in front of me,<br />
but until a new doctor gave<br />
me the results and explained<br />
what the symptoms would<br />
look like, it had never<br />
crossed my mind.”<br />
<strong>Positively</strong> <strong>Aware</strong> has a responsibility to provide information<br />
that might be that “aha” moment for you. <strong>Positively</strong> <strong>Aware</strong> can be,<br />
and is, the place to learn about health issues, to let you know about<br />
health information you might not have considered. Whether it is<br />
through an issue on aging and HIV, or this issue focused on women<br />
and HIV, <strong>Positively</strong> <strong>Aware</strong> is the source that makes you think about<br />
your own health, that helps you understand what your doctor<br />
should be asking, what you should be telling your doctor, what<br />
tests you might want to ask for. <strong>Positively</strong> <strong>Aware</strong> is your resource. If<br />
you’ve had your own “aha” moment, please let us know, if you think<br />
it’s something that should be discussed in this magazine. You can<br />
reach us at publications@tpan.com. You, our reader, are the reason<br />
we exist, you are our “peers,” and we need your ideas to inspire<br />
us. e<br />
<strong>Positively</strong> <strong>Aware</strong><br />
17
News Briefs<br />
by Enid Vázquez<br />
GSK and Pfizer announce joint company<br />
In April, GlaxoSmithKline (GSK) and Pfi zer announced that<br />
they will combine their HIV operations into one new company,<br />
which will account for nearly 20% of current HIV drug sales. Th is<br />
deal, the fi rst of its kind, is likely the result of lack of growth in the<br />
HIV drug arms of the two companies. Th e ever-evolving nature of<br />
the epidemic creates fi erce competition for pharmaceutical companies<br />
to develop newer compounds that are more tolerable and easier<br />
to take, as well as to counter issues associated with resistance.<br />
Relatively low returns on spending for research and development<br />
of these drugs, however, are forcing more and more pharmaceutical<br />
companies to explore ways to minimize their risks. Collaborative<br />
eff orts between HIV drug-makers are becoming increasingly<br />
common, as in the case of Bristol-Myers Squibb and Gilead<br />
Sciences working together to produce the multi-drug combo pill<br />
Atripla, currently leading the sale of HIV drugs.<br />
Though this type of shared business<br />
practice can oft en be rationalized<br />
with respect to bottom lines for pharma<br />
companies, advocates are concerned that<br />
drug companies may be moving away<br />
from HIV. “I hope we can get to a new<br />
generation of better and more tolerable<br />
drugs before progress in this fi eld halts,”<br />
said Bob Huff , editorial director and ARV<br />
project director of the New York–based<br />
Treatment Action Group.<br />
GSK chief executive offi cer Andrew<br />
Witty contends that one of the goals will<br />
be to develop new fi xed dose combination<br />
therapies, using existing and novel medicines.<br />
Witty cited benefi ts to both companies.<br />
GSK will now have access to the<br />
new medicines that Pfi zer has in clinical<br />
development while Pfi zer will gain GSK’s<br />
strong HIV marketing and distribution<br />
expertise.—Keith R. Green<br />
New AIDS awareness campaign<br />
From the U.S. Food and Drug Administration (FDA): “A new<br />
AIDS awareness campaign is being launched by FDA’s sister agency,<br />
the U.S. Centers for Disease Control and Prevention (CDC). HIV<br />
is still a signifi cant public health problem in the United States.<br />
Although HIV infection is preventable, every 9½ minutes, someone<br />
in the U.S. is infected with the virus.<br />
“Th e new Act Against AIDS campaign is designed to contribute<br />
to the goal of reducing HIV incidence in the United States. You can<br />
get the facts about the epidemic, learn how to prevent transmission<br />
18<br />
<strong>Positively</strong> <strong>Aware</strong><br />
of the virus, delay the onset of AIDS with proper treatment for HIV<br />
infection, and fi nd out ways to stem the tide of HIV infection in<br />
the United States by spreading the word about AIDS at a new CDC<br />
website Act Against AIDS, www.cdc.gov/nineandahalfminutes.”<br />
Th e following is from the website.<br />
As individuals:<br />
• We should know whether or not we are infected with HIV;<br />
• If we are infected, we should seek medical care and protect<br />
others from becoming infected;<br />
• We should protect ourselves and others from HIV;<br />
• We should educate ourselves and others about HIV.<br />
As communities:<br />
• We should mobilize to overcome the challenges and barriers<br />
to HIV prevention;<br />
• We should fi ght ignorance and complacency related to HIV;<br />
• We should increase the awareness about the severity of the<br />
epidemic and the continued impact that HIV is having on<br />
our communities;<br />
• We should make sure that HIV prevention services, HIV testing,<br />
medical care and treatment are<br />
available to all who need them;<br />
• We should work to prevent stigma<br />
and discrimination, and to increase<br />
support for people living with HIV.<br />
Free Gardasil for positive<br />
women<br />
Nurse Joan Swiatek of Rush University<br />
Medical Center in Chicago reminds<br />
everyone that a free series of Gardasil<br />
vaccine shots are still available for<br />
HIV-positive women through a clinical<br />
study. Th e vaccine protects against HPV<br />
(human papilloma virus), a common<br />
sexually transmitted infection that is<br />
particularly troublesome for women living<br />
with HIV. For more information on<br />
the ACTG study (AIDS Clinical Trials<br />
Group), e-mail Joan_A_Swiatek@rush.edu.<br />
Latest views of the epidemic<br />
In April, the Kaiser Family Foundation (KFF) released the<br />
results of a survey the organization took of perceptions and testing<br />
around HIV in the U.S. Th e following is from a KFF press release.<br />
“Less than a year aft er the Centers for Disease Control and Prevention<br />
(CDC) recalculated the size of the HIV/AIDS epidemic and<br />
announced that there were 40% more new HIV infections each year<br />
than previously believed, a new survey by the Kaiser Family Foundation<br />
fi nds that Americans’ sense of urgency about HIV/AIDS as<br />
a national health problem has fallen dramatically and their concern<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
Photo © Russell McGonagle
about HIV as a personal risk has also declined, even among some<br />
groups at higher risk.<br />
Key findings of the survey include:<br />
• Th e share of Americans naming HIV/AIDS as the most urgent<br />
health problem facing the nation dropped precipitously<br />
from 44% in 1995 to 17% in 2006 and to 6% now.<br />
• CDC estimates that HIV rates are<br />
seven times higher among African<br />
Americans and three times higher<br />
among Latinos compared to whites.<br />
While these groups are more likely<br />
than whites to see HIV/AIDS as<br />
an urgent problem, fewer say it is a<br />
“more urgent” problem for their community<br />
now than in 2006 (declining<br />
from 23% to 17% of all adults, 49% to<br />
40% of African Americans, and 46%<br />
to 35% of Latinos).<br />
• Th e share of those ages 18-29 who say<br />
they are personally very concerned<br />
about becoming infected with HIV<br />
declined from 30% in 1997 to 17%<br />
today; personal concern among<br />
young African Americans declined<br />
from 54% to 40% over the same time<br />
period.<br />
• More than half (53%) of non-elderly<br />
adults say they have been tested for HIV, including 19%<br />
who say they were tested in the past year. Testing is most<br />
common among adults under the age of 30, with three in<br />
ten young adults and nearly half (47%) of young African<br />
Americans reporting having been tested in the past year.<br />
However, reported testing rates for all these groups have not<br />
changed much in the past decade.<br />
“Many indicators of urgency and concern are moving in the<br />
wrong direction, including for higher risk groups,” said Kaiser<br />
President and CEO Drew Altman. “Th e survey underscores the<br />
need for a new focus on domestic HIV,” he added.<br />
Th e press released continued, “A signifi cant share of the public<br />
also harbors misconceptions about prevention and treatment<br />
of HIV/AIDS. Nearly one in fi ve (18%) do not know there is no<br />
cure for AIDS and about one-quarter (27%) believe or are unsure<br />
whether former professional basketball player Magic Johnson has<br />
been cured of AIDS. Additionally, a quarter (24%) believe or are<br />
unsure whether there is a vaccine available to prevent HIV infection.<br />
Many of these misconceptions are more common in the African<br />
American community, including that Magic Johnson has been<br />
cured (37% of African Americans think he has been cured or are<br />
unsure), that there is a vaccine available to prevent infection (36%),<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
and that there are drugs available that can cure HIV and AIDS<br />
(30%).” Visit www.kff .org.<br />
Pediatric warning on Testim and Androgel<br />
Th e FDA has added a boxed warning on the drug labels for Testim<br />
and Androgel aft er receiving reports of adverse eff ects in children<br />
who were inadvertently exposed to these testosterone products<br />
through contact with another person being treated with them.<br />
According to an FDA announcement,<br />
“Th e gels are approved for use in men who<br />
either no longer produce testosterone or<br />
produce it in very low amounts, and are<br />
oft en used by men living with HIV who<br />
have below normal testosterone levels.”<br />
Visit www.fda.gov/medwatch for more<br />
information.<br />
Women’s conference in<br />
Chicago<br />
Pharmaceutical Boehringer-<br />
Ingelheim (BI), maker of the HIV drugs<br />
Viramune (nevirapine) and Aptivus (tipranavir),<br />
is holding a free one-day women’s<br />
meeting on HIV here in Chicago.<br />
“Women Living <strong>Positively</strong>: It’s My Life,<br />
National Women’s Summit” is scheduled<br />
for Friday, July 17, from 9 a.m. to 2<br />
p.m. at New Zion Banquets, 1950 W. 13th<br />
Street (in the Illinois Medical District).<br />
Breakfast and lunch will be provided.<br />
Visit www.banquet.newzionmbc.com.<br />
Women interested in attending the summit should call toll-free at<br />
1–877–933–4310, extension 99512, as soon as possible to reserve a<br />
seat. BI videotaped one of its previous women’s summits, held in<br />
Florida. Judging from those speakers, the summit is an outstanding<br />
event. Visit www.vodium.com/goto/womenlivingpositive.asp.<br />
Due to issues of confi dentiality, question-and-answer sessions and<br />
breakout groups were not taped.<br />
Not taking it<br />
During International Women’s Month, in March, the Women’s<br />
Institute at GMHC (Gay Men’s Health Crisis) in New York City and<br />
Iris House re-launched its HIV prevention and testing campaign<br />
for women. According to a press release, the “We’re Not Taking It<br />
Lying Down campaign… continues to boldly celebrate and reclaim<br />
the sexuality, sexual health and strength of women of color. …Institutionalized<br />
racism, poverty, and violence create environments of<br />
risk.” It continued, “Both the Women’s Institute at GMHC and Iris<br />
House promote safer and satisfying sex that’s consensual and in<br />
one’s control. We subscribe to the idea that women don’t have to<br />
‘take it lying down.’ Testing regularly for HIV is but one way to take<br />
control.” Th e Women’s Institute provides community health education<br />
and advocacy for women and families. Iris House provides<br />
services to women, families, and communities aff ected by HIV,<br />
promoting prevention, education, and awareness. e<br />
<strong>Positively</strong> <strong>Aware</strong><br />
19
692US09AB02404_MeAd8x10.5:- 6/4/09 2:55 PM Page 1<br />
ONCE-DAILY SUSTIVA IN HIV COMBINATION THERAPY:<br />
• Can help keep viral loads undetectable* for a long time †<br />
• Helps improve your body’s immune system by raising your T -cell count<br />
*Undetectable is defined as a viral load of less than 400 copies/mL or less than 50 copies/mL (depending on the test used).<br />
†<br />
Up to 168 weeks.<br />
SUSTIVA does not cure HIV and has not been shown to prevent passing HIV to others.<br />
IMPORTANT INFORMATION ABOUT SUSTIVA ® (efavirenz)<br />
INDICATION: SUSTIVA ® (efavirenz) is a prescription medicine used<br />
in combination with other medicines to treat people who are<br />
infected with the human immunodeficiency virus type 1 (HIV-1).<br />
SUSTIVA does not cure HIV and has not been shown to<br />
prevent passing HIV to others.<br />
See your healthcare provider regularly.<br />
IMPORTANT SAFETY INFORMATION:<br />
Do not take SUSTIVA if you are taking the following medicines<br />
because serious and life-threatening side effects may occur<br />
when taken together: Vascor ® (bepridil), Propulsid ® (cisapride),<br />
Versed ® (midazolam), Orap ® (pimozide), Halcion ® (triazolam), or ergot<br />
medicines (for example, Wigraine ® and Cafergot ® ).<br />
In addition, SUSTIVA and Vfend ® (voriconazole) must not be<br />
taken together at standard doses. Some doses of voriconazole<br />
can be taken at the same time as a lower dose of SUSTIVA, but you<br />
must check with your healthcare provider first.<br />
AS PART OF<br />
HIV COMBINATION THERAPY:<br />
SUSTIVA<br />
&<br />
SUSTIVA should not be taken with ATRIPLA ® (efavirenz 600 mg/<br />
emtricitabine 200 mg/tenofovir disoproxil fumarate 300 mg)<br />
because it contains efavirenz, the active ingredient of SUSTIVA.<br />
Neither Fortovase ® (saquinavir) nor Invirase ® (saquinavir mesylate) should<br />
be used as the only protease inhibitor in combination with SUSTIVA.<br />
Taking SUSTIVA with St. John’s wort (Hypericum perforatum) is not<br />
recommended, as it may cause decreased levels of SUSTIVA,<br />
increased viral load, and possible resistance to SUSTIVA or crossresistance<br />
to other anti-HIV drugs.<br />
This list of medicines is not complete. Discuss with your<br />
healthcare provider all prescription and non-prescription<br />
medicines, vitamins, and herbal supplements you are taking<br />
or plan to take.<br />
Tell your healthcare provider right away if you have any side<br />
effects or conditions, including the following:<br />
• Severe depression, strange thoughts, or angry behavior<br />
have been reported by a small number of patients taking<br />
SUSTIVA. Some patients have had thoughts of suicide and a few<br />
have actually committed suicide. These problems may occur<br />
more often in patients who have had mental illness.
ME<br />
Individual results may vary.<br />
. .. We’re in this together.<br />
• Dizziness, trouble sleeping or concentrating, drowsiness,<br />
unusual dreams, and/or hallucinations are common, and tend<br />
to go away after taking SUSTIVA for a few weeks. Symptoms<br />
were severe in a few patients, and some patients discontinued<br />
therapy. These symptoms may become more severe with the use<br />
of alcohol and/or mood-altering (street) drugs. If you are dizzy,<br />
have trouble concentrating, and/or are drowsy, avoid activities<br />
that may be dangerous, such as driving or operating machinery.<br />
• If you have ever had mental illness or are using drugs<br />
or alcohol.<br />
• Pregnancy: Women should not become pregnant while<br />
taking SUSTIVA and for 12 weeks after stopping SUSTIVA.<br />
Serious birth defects have been seen in children of women treated<br />
with SUSTIVA during pregnancy. Therefore, women must use a<br />
reliable form of barrier contraception, such as a condom or<br />
diaphragm, even if they also use other methods of birth control.<br />
• Breast-feeding: Women with HIV should not breast-feed<br />
because they can pass HIV through their milk to the baby. Also,<br />
SUSTIVA may pass through breast milk and cause serious harm<br />
to the baby.<br />
• Rash is a common side effect that usually goes away without any<br />
change in your medicines, but may be serious in a small number<br />
of patients. Rash may be a serious problem in some children.<br />
• If you have liver disease, your healthcare provider may want to<br />
do tests to check your liver.<br />
• Seizures have occurred in patients taking SUSTIVA, usually in<br />
those with a history of seizures. If you have ever had seizures or<br />
take medicines for seizures, your healthcare provider may want<br />
to switch you to another medicine or monitor you.<br />
SUSTIVA and the SUNRISE logo are registered trademarks of Bristol-Myers Squibb P harma Company.<br />
ATRIPLA is a trademark of Bristol-Myers Squibb & Gilead Sciences, LLC. All other trademarks are owned by third parties.<br />
© 2009 Bristol-Myers Squibb Company, Princeton, NJ 08543 U.S.A. 692US09AB02404 05/09<br />
Changes in body fat have been seen in some patients taking anti-HIV<br />
medicines. The cause and long-term health effects are not known.<br />
Other common side effects of SUSTIVA taken with other anti-HIV<br />
medicines include: tiredness, upset stomach, vomiting, and<br />
diarrhea. Some patients taking SUSTIVA have experienced increased<br />
levels of lipids (cholesterol and triglycerides) in the blood.<br />
You should take SUSTIVA on an empty stomach, preferably at<br />
bedtime, which may make some side effects less bothersome.<br />
SUSTIVA is one of several treatment options your doctor may<br />
consider.<br />
You are encouraged to report negative side<br />
effects of prescription drugs to the FDA. Visit<br />
www.fda.gov/medwatch or call 1-800-FDA-1088.<br />
Ask your doctor if SUSTIVA is right for you.<br />
Visit www.sustiva.com<br />
Please see Patient Information about SUSTIVA on the next page.
692US09AB02404_MeAd8x10.5:- 6/4/09 2:55 PM Page 3<br />
FDA-Approved Patient Labeling<br />
Patient Information<br />
SUSTIVA ® <br />
[efavirenz ]<br />
capsules and tablets<br />
ALERT: Find out about medicines that should NOT be taken with SUSTIVA.<br />
Please also read the section “MEDICINES YOU SHOULD NOT TAKE WITH<br />
SUSTIVA.”<br />
<br />
<br />
<br />
know about your medicine. This information is not meant to take the place of<br />
talking with your doctor.<br />
What is SUSTIVA (efavirenz)?<br />
SUSTIVA is a medicine used in combination with other medicines to help treat<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
under the care of your doctor.<br />
<br />
<br />
What are the possible side effects of SUSTIVA?<br />
Serious psychiatric problems. <br />
<br />
<br />
<br />
<br />
<br />
<br />
Common side effects. <br />
<br />
with SUSTIVA. These side effects may be reduced if you take SUSTIVA at<br />
<br />
<br />
<br />
<br />
right away if any of these side effects continue or if they bother you. It is possible<br />
<br />
<br />
<br />
<br />
<br />
<br />
call your doctor right away. Rash may be a serious problem in some<br />
children. Tell your child’s doctor right away if you notice rash or any other side<br />
effects while your child is taking SUSTIVA.<br />
<br />
<br />
<br />
Changes in body fat. <br />
<br />
<br />
<br />
<br />
<br />
taking SUSTIVA.<br />
SUSTIVA ® (efavirenz)<br />
Contact your doctor before stopping SUSTIVA because of side effects or for any<br />
other reason.<br />
This is not a complete list of side effects possible with SUSTIVA. Ask your doctor<br />
or pharmacist for a more complete list of side effects of SUSTIVA and all the<br />
medicines you will take.<br />
How should I take SUSTIVA?<br />
General Information<br />
<br />
<br />
<br />
which may increase the frequency of side effects.<br />
<br />
bothersome.<br />
<br />
<br />
<br />
<br />
<br />
<br />
doctor or pharmacist.<br />
<br />
<br />
to stop.<br />
<br />
contact your local Poison Control Center or emergency room right away.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Capsules<br />
<br />
<br />
children may be lower (see Can children take SUSTIVA?<br />
Tablets<br />
<br />
by mouth.<br />
Can children take SUSTIVA?<br />
<br />
be a serious problem in some children. Tell your child’s doctor right away if you<br />
notice rash or any other side effects while your child is taking SUSTIVA. The<br />
dose of SUSTIVA for children may be lower than the dose for adults. Capsules<br />
<br />
determine the right dose based on your child’s weight.<br />
Who should not take SUSTIVA?<br />
Do not take SUSTIVA if you are allergic <br />
<br />
<br />
What should I avoid while taking SUSTIVA?<br />
Women should not become pregnant while taking SUSTIVA and for<br />
12 weeks after stopping it. <br />
offspring of animals and women treated with SUSTIVA during pregnancy.<br />
It is not known whether SUSTIVA caused these defects. Tell your doctor<br />
right away if you are pregnant. Also talk with your doctor if you want to<br />
become pregnant.<br />
<br />
<br />
<br />
<br />
birth control. SUSTIVA may remain in your blood for a time after therapy
SUSTIVA ® (efavirenz)<br />
Do not breast-feed if you are taking SUSTIVA. <br />
<br />
<br />
SUSTIVA may pass through breast milk and cause serious harm to the<br />
<br />
<br />
<br />
<br />
<br />
These medicines include prescription and nonprescription medicines and<br />
(Hypericum perforatum).<br />
Before using SUSTIVA, tell your doctor if you<br />
have problems with your liver or have hepatitis. <br />
<br />
have ever had mental illness or are using drugs or alcohol.<br />
have ever had seizures or are taking medicine for seizures [for<br />
<br />
<br />
<br />
What important information should I know about taking other medicines<br />
with SUSTIVA?<br />
SUSTIVA may change the effect of other medicines, including ones for HIV,<br />
and cause serious side effects. <br />
<br />
it is very important to:<br />
<br />
<br />
<br />
<br />
<br />
<br />
doctor a complete picture of the medicines you use. Then he or she can decide<br />
the best approach for your situation.<br />
(Hypericum perforatum) <br />
<br />
recommended. Talk with your doctor if you are taking or are planning to take<br />
<br />
<br />
<br />
MEDICINES YOU SHOULD NOT TAKE WITH SUSTIVA<br />
<br />
<br />
taking SUSTIVA:<br />
<br />
<br />
<br />
<br />
<br />
<br />
The following medicine should not be taken with SUSTIVA since it contains<br />
<br />
<br />
SUSTIVA ® (efavirenz)<br />
The following medicines may need to be replaced with another medicine<br />
when taken with SUSTIVA:<br />
<br />
<br />
<br />
<br />
The following medicines may require a change in the dose of either<br />
SUSTIVA or the other medicine:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
These are not all the medicines that may cause problems if you take<br />
SUSTIVA. Be sure to tell your doctor about all medicines that you take.<br />
General advice about SUSTIVA:<br />
Medicines are sometimes prescribed for conditions that are not mentioned<br />
in patient information leaflets. Do not use SUSTIVA for a condition for<br />
which it was not prescribed. Do not give SUSTIVA to other people, even if<br />
they have the same symptoms you have. It may harm them.<br />
<br />
<br />
<br />
<br />
<br />
<br />
www.sustiva.com <br />
___________________________________________________________
Dawn Averitt Bridge, who turned 40 last December, was diagnosed with HIV in 1988<br />
when she was just 19 years old. Her doct or had never diagnosed another woman and had no<br />
idea what to expect , other than that an HIV diagnosis at the time meant a life expect ancy of<br />
about six months. Dawn’s fi rst goal was to make it to her 20th birthday. She is now happily<br />
married with two daughters, Madelyn Grace, 7, and Sophie, 5, both of whom are happy,<br />
healthy and HIV-negative.<br />
Dawn sat down with PA recently to talk about her family, her dreams, and her life’s<br />
work—educating and empowering other women with HIV, and letting them know that<br />
they are not alone.<br />
JEFF BERRY: Have you talked to<br />
your daughters about your status and having<br />
to take meds? Is it something you’ve discussed<br />
with them yet?<br />
DAWN AVERITT BRIDGE: I’ve<br />
never hidden it from them, but I also haven’t<br />
focused on it being extraordinarily unique—<br />
it’s their “normal.” About two years ago,<br />
Good Housekeeping did an article on my<br />
choice as an HIV-positive woman to have<br />
children, and I focused on my whole family<br />
in a way that I hadn’t let play out in the<br />
mainstream media very much. It was really<br />
24<br />
One-on-One wit h<br />
Dawn Averit t Bridge<br />
Wife, mother, and advocate for HIV-posit ive women<br />
<strong>Positively</strong> <strong>Aware</strong><br />
Interview by Jeff Berry<br />
a hard choice for me to make, because we’d<br />
just moved to this small, rural community<br />
in Virginia, and Maddy was all of four-anda-half,<br />
and I realized that, although I had<br />
made the choice to be a very public person<br />
long before they were ever around, having<br />
the kids really turned that on its ear. I had<br />
to do some serious soul-searching, figuring<br />
out what was important to me, and what<br />
was fair to them. I was [already] out [about<br />
my status], so perhaps the best thing I could<br />
do was reinforce for my children that there<br />
was nothing to be ashamed of. So, kind of<br />
take it head on, and deal with people’s fears,<br />
and unfortunately, at times, their anger, or<br />
dislike or bigotry, or whatever we want to<br />
call it.<br />
So I had to tell Maddy and Sophie—<br />
Sophie was only two-and-a-half, so this<br />
was a very short conversation with her—but<br />
I had to tell Maddy a little bit more about<br />
HIV. Maddy is this little redheaded, pixiefaced<br />
artist, an old soul, if you will. And<br />
she’s sitting in the back seat of the car, and<br />
I say, “Hey, Maddy, so you know how you<br />
see Mommy taking medicine?” And she<br />
said, “Nope.” [Laughs.] And I thought, oh,<br />
c’mon, your two-and-a-half year-old sister<br />
reminds me if I haven’t taken them. But<br />
of course, she wasn’t going to give me any<br />
room, so I thought, okay, I’m going to have<br />
to come at this from another angle.<br />
[Aft er they spoke, Dawn said it was<br />
a huge relief to have fi nally had “the talk”<br />
with Maddy, but she realized that it was just<br />
the beginning of an ongoing conversation<br />
that she would be having with her for the<br />
rest of Maddy’s life.]<br />
JB: So how did WISE and The Well Project<br />
come about?<br />
DAB: WISE was a completely separate<br />
entity from The Well Project [TWP]. Basically,<br />
when I was diagnosed my doctor said,<br />
“Don’t read anything, it’s too confusing, and<br />
don’t tell anyone, because it will ruin your<br />
family’s life.” And I took that advice for a<br />
number of years. I finished college, and<br />
went to D.C. and worked for a U.S. Senator,<br />
and it was there where I discovered what<br />
grassroots advocacy and activism truly was,<br />
and decided that I’d rather be on that side<br />
[laughs].<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
Photos provided by Dawn Averitt Bridge
It was actually during the whole gays<br />
in the military debacle that I was on the<br />
receiving end of ACT UP and Queer Nation,<br />
and all of these other advocacy groups. Of<br />
course, nobody knew that I was HIV-positive.<br />
I was also progressing fairly rapidly<br />
with the disease, and not tolerating treatment<br />
very well, and decided that I wanted<br />
to be back in Atlanta, closer to my family,<br />
and wanted to shift from government to<br />
working in community-based organizations.<br />
A friend of mine told me there was a<br />
position open at the Atlanta chapter of the<br />
National Association of People With AIDS<br />
[NAPWA], which became the AIDS Survival<br />
Project, and it would be really awesome<br />
to have a positive woman as the treatment<br />
resource specialist. Which was a complete<br />
joke—I knew about fi ve things about HIV. I<br />
knew I had it and I knew more T-cells were<br />
better than less T-cells. So I spent a weekend<br />
cramming and memorizing the whole<br />
Project Inform [PI] opportunistic infection<br />
chart, and I marched in there with my<br />
pumps and pantyhose, to this beleaguered<br />
set of queens who were sitting there looking<br />
at me like I’d just been sentenced to community<br />
service. And they said, “Why are<br />
you here?” And I had to say, “Well, I have<br />
HIV too,” and they were shocked. I quickly<br />
blurted out every infection; viral, parasitic,<br />
bacterial, and fungal, which of course was<br />
relatively useless information, but it meant<br />
that I was trainable. Remarkably, they hired<br />
me as Treatment Resource Specialist, and<br />
they didn’t even change the title. Th at was<br />
the early nineties, and the learning curve<br />
was extraordinarily steep. I found myself in<br />
a lot of places I probably had no business<br />
being, because I was a complete anomaly.<br />
I was a middle-class white girl from the<br />
South who was interested in the science.<br />
I found myself on everything from FDA<br />
advisory panels to NIH task forces and all<br />
kinds of things.<br />
Within about 12 months, I realized<br />
there was nothing out there for women,<br />
certainly nothing on treatment. I wrote my<br />
fi rst grant overnight, and it got funded. In<br />
1995, I launched WISE [Women’s Information<br />
Service and Exchange] and, to the best<br />
of my knowledge, we were one of the fi rst<br />
group to focus on treatment information<br />
and advocacy specifi cally for women.<br />
I merged WISE with Project Inform<br />
[in San Francisco] in 1997 and then, all of<br />
a sudden I was about to turn 30 and I’d<br />
lived with HIV for 10 years. So I decided<br />
to act out a childhood dream and hike the<br />
“I marched in<br />
there wit h my<br />
pumps and<br />
panty hose,<br />
to this<br />
beleaguered set<br />
of quee ns who<br />
were sit ting<br />
there looking<br />
at me like<br />
I’d just bee n<br />
sentenced to<br />
communit y<br />
service.”<br />
Appalachian Trail, from Maine all the way<br />
down to Georgia, which was a 2,200 mile<br />
journey, with my fi ve-drug combination in<br />
tow. On that journey I spent a lot of time<br />
thinking about what had worked and what<br />
hadn’t worked, in terms of reaching out to<br />
and mobilizing women and developing new<br />
treatment advocates. And what came out<br />
of it was a series of regional focus groups<br />
that ultimately gave me what I needed to<br />
develop a web portal that would service the<br />
whole spectrum of people involved in HIV<br />
disease management, so that people had<br />
tools for communicating about the challenging<br />
issues involved in living with HIV<br />
from a whole person perspective. What<br />
came out of that was Th e Well Project web<br />
portal, launched in 2003, and at the same<br />
time, we launched the Women and HIV<br />
Th ink Tank, which has now become the<br />
Women’s Research Initiative [WRI] on HIV/<br />
AIDS, a year-round initiative that has done<br />
some really amazing stuff , working with the<br />
FDA, and the companies, and research in<br />
general, and that’s all kind of fallen under<br />
the rubric of TWP.<br />
JB: I understand you just got back from<br />
a meeting of WRI—anything come out of<br />
that meeting that was exciting, that you’d<br />
want to share with our readers?<br />
DAB: Yeah, actually this year the WRI<br />
went back to where we started at our first<br />
meeting, looking at gaps and controversies<br />
in research, but in a much more refined way.<br />
Like how much do we really know about<br />
how women are infected with HIV? And<br />
how women can protect themselves, asking<br />
some very basic questions about what’s<br />
going on in a female body’s immune system.<br />
It was a fascinating meeting, and the group<br />
has a statement [with] a series of priorities<br />
around answering those questions. The goal<br />
of the WRI is more, better, faster research<br />
for women. And a lot of great things have<br />
come out of WRI. The validation that the<br />
GRACE study could be done and would<br />
work came out of the work of the WRI, as<br />
did the Women Living <strong>Positively</strong> Survey<br />
and some of the other things that you may<br />
be aware of.<br />
JB: So what are some of the issues that are<br />
important to women with HIV that you feel<br />
need more research or study?<br />
DAB: I think that there are a lot of issues<br />
that are really critically important. We<br />
are perpetually trying to understand better<br />
what happens, in relationship to pregnancy<br />
and fertility, in those women who<br />
choose to become biological mothers. It’s<br />
not just about whether the baby is going be<br />
infected with HIV, which we now know is<br />
way less likely to happen [especially when<br />
treated]. But we’re still struggling with how<br />
best to treat women during pregnancy and<br />
beyond, especially for women in the developing<br />
world. I think the microbicide issue<br />
is extraordinarily important, because it’s<br />
incredibly exciting, for both HIV-negative<br />
and positive women, and I think that there’s<br />
a lot of work still to be done on bringing the<br />
reproductive health community together<br />
to champion the microbicide research with<br />
those of us who’ve been working on women<br />
and HIV-related issues.<br />
I think I have a lot of basic science<br />
questions that are about the infl ammation<br />
process and what’s happening inside our<br />
bodies. I think that Bob Silicano’s talk at<br />
CROI [Conference on Retroviruses and<br />
Opportunistist Infections] this year was<br />
fascinating and the possibility that we don’t<br />
know everything we think we know is very<br />
real. We need to understand how to dose<br />
women appropriately; we need to under-<br />
PA • July / August 2009 • tpan.com • positivelyaware.com 25<br />
<strong>Positively</strong> <strong>Aware</strong>
stand how women process these drugs so<br />
that we know how to manage the toxicities<br />
and side eff ects over the long term. Th ere<br />
are a number of things for me that kind of<br />
stand out as big questions.<br />
JB: Why do you think that women have<br />
traditionally been underrepresented in<br />
clinical trials? What can be done to include<br />
more women in trials and why is that so<br />
important?<br />
DAB: Women have been underrepresented<br />
in clinical trials for a very long time, and<br />
not just in HIV, for a whole host of reasons.<br />
The biggest reason has been, of course, their<br />
ability to bear children, and the risk that if<br />
they become pregnant on an experimental<br />
therapy that they are going to cause significant<br />
damage to a fetus or even lose the baby.<br />
The FDA really came from the response to<br />
what happened when women were treated<br />
with thalidomide during pregnancy and<br />
we ended up with 10,000 or more thalidomide<br />
babies. The government said we’ve<br />
got to have a better grip on these things.<br />
Fortunately, there’s been significant progress<br />
made over the years, and increasingly,<br />
women are actively recruited to participate<br />
in clinical trials. There’s still a number of<br />
challenges—the sites where clinical trials<br />
are done are typically sites where many<br />
women are not being cared for, I’m speaking<br />
about HIV specifically now. The studies<br />
are not always designed with women’s<br />
issues or special circumstances in mind—<br />
how the studies are run, what questions<br />
are asked, or how the sites are prepared to<br />
manage the unique needs of women who<br />
are primary caretakers, and that type of<br />
thing. For years we’ve listed transportation<br />
and child care as the primary barriers for<br />
Dawn’s two daughters, Maddy (l) and Sophie (r) in April, 2009.<br />
women to clinical research, and I would<br />
say that, although child care and transportation<br />
are critical issues that should be<br />
addressed, they are not the primary drivers<br />
in preventing women from participating in<br />
clinical research.<br />
It’s important because we need to<br />
understand how these drugs work in<br />
women, and how this disease impacts<br />
women, specifi cally. I think it’s great news<br />
when we can actually power a study well<br />
enough to be able to say, look, we’ve had<br />
enough women in the study to actually tell<br />
you that there’s not a diff erence between<br />
men and women in terms of this aspect of<br />
this treatment. But there are a number of<br />
cases where, over time, as we’ve had more<br />
women on treatment, we’ve had unique<br />
issues, needs and circumstances that have<br />
arisen because we’ve fi nally had the drug in<br />
enough women. Th e obvious case is the differential<br />
prescribing structure for nevirapine<br />
[Viramune] for women versus men, and<br />
some of the side eff ects and toxicities that<br />
occur. Basically, we need women in clinical<br />
trials so that we can answer those questions<br />
and so we can know that when my doctor<br />
prescribes a drug for me, we know how it’s<br />
going to behave in my body.<br />
JB: So what are some of the challenges<br />
in designing trials for women, including<br />
the recruitment and retention? Could you<br />
talk in particular about the GRACE and<br />
SPRING studies?<br />
DAB: There are some significant challenges<br />
in designing trials for women, and I<br />
think GRACE has shown us that retention<br />
is also a challenge. How do we make it possible<br />
for women to participate over the long<br />
term in a study, and what are the things that<br />
threaten their ability to participate successfully?<br />
There are some great lessons that<br />
came out of the GRACE study, and for me,<br />
that makes it a huge success.<br />
From a protocol level, in the design of<br />
a clinical trial, you have to think about the<br />
questions you truly need answered. It’s really<br />
hard trying to fi gure out what information<br />
needs to be collected, anticipating what<br />
information you wish you had three years<br />
down the road. But we also have to consider<br />
what people are willing to do. How many<br />
visits do you really need? Do you have sites<br />
that have evening hours and fl exible schedules?<br />
Are treatments provided free of cost<br />
or do people have to pay for things, going<br />
through insurance to get them, just as they<br />
would if they had to go to their doctor’s<br />
offi ce? So what is their incentive to participate<br />
in the trial, other than to increase your<br />
hassle factor, despite the fact that you’re<br />
trying to be altruistic. Th en, of course, site<br />
selection is a very, very big issue. Th ere are<br />
a lot of wonderful people out there who<br />
care passionately about women’s issues, but<br />
whose sites just frankly are not positioned<br />
to enroll women eff ectively, just because<br />
women won’t go there, or feel like they<br />
don’t understand or trust the research that<br />
is happening. Th ere are a lot of myths in the<br />
community about clinical research overall,<br />
so the site selection is an essential piece to<br />
how we roll out clinical trials eff ectively.<br />
And then from there, what are you<br />
doing to provide support so the site understands<br />
how to meet the unique needs of the<br />
26 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
people, not just patients, who come through<br />
their door? A whole lot of what worked in<br />
GRACE was just about the sense of being<br />
a part of something bigger than yourself,<br />
being really valued, appreciated, and<br />
respected in an environment where, frankly,<br />
a lot of people are dealing with shame and<br />
stigma. Nothing that we’ve done in GRACE<br />
was rocket science, it was just a lot of basic,<br />
commonsense shift ing around and thinking<br />
about things a little bit diff erently, that<br />
yielded a great result, which was successfully<br />
enrolling so many women and specifi -<br />
cally women of color.<br />
In fairness, you can’t really compare<br />
the challenges with SPRING to GRACE,<br />
because they’re radically diff erent studies,<br />
diff erent patient populations. SPRING was<br />
more specifi cally for more advanced populations,<br />
it was run in eight countries, it was<br />
a very diff erent deal than GRACE, but I<br />
think there are a few things that could have<br />
been diff erent for SPRING. One was that<br />
we didn’t eff ectively communicate what the<br />
study was for, and why we were doing it, to<br />
the patient community or to people out in<br />
the mainstream. Th at makes it really hard,<br />
when you go to www.clinicaltrials.gov to<br />
sort out between the dozens and dozens of<br />
other studies that are out there. You need<br />
some way to identify a study so it surfaces,<br />
for the patient, the investigator, and the staff<br />
at the research site. Because they’re probably<br />
doing dozens of studies, and they need<br />
a study that’s kind of, “top of mind,” if you<br />
will. Th e branding around GRACE really<br />
seemed to work—it was easy to remember,<br />
it was colorful, and pretty. SPRING didn’t<br />
have any of that going for it. I think, frankly,<br />
that SPRING, on a conceptual level, was a<br />
fascinating study about using therapeutic<br />
drug monitoring [TDM] to do some individualization<br />
of care, a real step forward.<br />
JB: So what can women do to become<br />
more involved, as advocates for their own<br />
health care or for others?<br />
DAB: Well, lots of things. One of the<br />
things that keeps women from jumping<br />
into advocacy is that the term “advocacy” is<br />
a little daunting. I have to remind people<br />
that even though advocacy seems like something<br />
that only the fringe element might do,<br />
if you’ve ever been at the grocery store and<br />
the pickles were on sale for $1.25 and they<br />
charged you $2.50 for them, and you said,<br />
“Hey, wait a minute, that’s the wrong price,”<br />
you’ve been an advocate—we use advocacy<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
in all aspects of our lives. The first thing<br />
that women need to know is that advocacy<br />
begins with speaking up for yourself, and<br />
for people that you care about. You’re an<br />
advocate when you ask somebody to explain<br />
something you didn’t understand. You’re an<br />
advocate when you ask somebody to work<br />
around a conflict so you can make something<br />
work. You’re advocating for yourself<br />
and for your own healthcare when you get<br />
that clarity and peace of mind. When you<br />
stand up for yourself and you figure out that<br />
you do have a voice, and it’s an important<br />
voice, there are all kinds of opportunities to<br />
get engaged. WORLD [Women Organized<br />
to Respond to Life Threatening Diseases],<br />
based out in Oakland, has been willing<br />
to parent the development of a new group<br />
called The Positive Women’s Network, and<br />
PWN is a coalition of HIV-positive women.<br />
I am a part of PWN, and many other women<br />
and organizations around the country are a<br />
part of PWN. It’s an exciting opportunity<br />
for positive women to find a place where<br />
they can, in a collective sisterhood with<br />
other positive women, find their voice, and<br />
figure out how they’re going to help themselves,<br />
their friends, or somebody on the<br />
local level, or for those who’re ready, to take<br />
the next step and do stuff on a regional or<br />
even national level. I find that incredibly<br />
exciting, because when I started in this,<br />
there wasn’t anything like that. There was<br />
a lot of desperation and a huge amount of<br />
need, and that certainly motivated many of<br />
us to find our ways into offices and rooms<br />
where we may not have been invited, to put<br />
in our two cents, to ask questions and get<br />
answers. It has paved the way for some real<br />
opportunities to have advocates at the table,<br />
leading the discussions, something that I<br />
think, in terms of other disease categories,<br />
people are trying to emulate. And it’s pretty<br />
exciting to be part of that.<br />
JB: What would be the first and foremost<br />
thing you would want to tell a woman who<br />
has just been diagnosed with HIV?<br />
DAB: You know, for the thousand times<br />
I’ve been asked that question, I wish I had<br />
that answer that I loved, and could spit out<br />
beautifully. The thing that automatically<br />
comes out of my mouth, and it comes out<br />
of many of the mouths of women I know is,<br />
“You’re not alone.” There is an enormous sis-<br />
“Basically, we nee d women in<br />
clinical trials so we can know that<br />
when my doct or prescribes a drug<br />
for me, we know how it ’s going to<br />
behave in my body.”<br />
terhood of women living with HIV, though,<br />
unfortunately, we are still largely invisible,<br />
especially to the mainstream. But there are<br />
all kinds of advances in our understanding<br />
of HIV, and people are living well, they’re<br />
living healthy, and they’re living out their<br />
dreams, whether that’s crazy, silly dreams<br />
like hiking Appalachian trails, or realistic<br />
“real people” dreams like having a family.<br />
And as devastating a blow as an HIV diagnosis<br />
can be, it is also your key, I believe, to<br />
staying well and taking care of yourself in a<br />
way that you may never have thought about<br />
doing before.<br />
JB: Anything else you’d like to tell us?<br />
DAB: No, except that I just feel incredibly<br />
grateful and privileged to do the work<br />
that I do. There are not many people in the<br />
world who feel they’re doing what they’re<br />
supposed to be doing, and I’m really thankful<br />
to have that. e<br />
Visit www.thewellproject .org.<br />
<strong>Positively</strong> <strong>Aware</strong><br />
27
The Naked Truth:<br />
Young, Beautiful<br />
and HIV Positive<br />
The courageous tale of<br />
Marvelyn Brown<br />
A book review by Keith R. Green<br />
If Magic Johnson going public about his HIV status served notice<br />
to African Americans that they were not exempt from the sting<br />
of HIV, Marvelyn Brown’s story is a clear indication that the<br />
younger generation did not get that memo.<br />
Marvelyn was a daddy’s girl from Nashville, Tennessee. Th ough<br />
she was oblivious to the ongoing drama between her parents, and<br />
far too young to comprehend the details related to it, her troubles<br />
in life can be traced to their separation.<br />
Her mother ruled their household with an iron fi st, which,<br />
from Marvelyn’s perspective, forced her father to leave when she<br />
was only fi ve years old. From then on, he’d only show up occasionally<br />
for birthdays or on holidays, leaving Marvelyn feeling rejected<br />
and yearning for the type of consistent and (arguably) healthy male<br />
aff ection that her father provided.<br />
What she didn’t know was that he suff ered from addiction to<br />
crack cocaine. Her mother had asked him to leave only aft er she’d<br />
had enough of covering for him and pulling the weight of their<br />
family on her own.<br />
With only half the story, Marvelyn blamed her mother’s strictness<br />
for her father’s departure, and, over time, developed a degree<br />
of resentment towards her that would tarnish their relationship for<br />
years to come.<br />
As she grew older, the harder her mother pushed, the more<br />
Marvelyn rebelled. School was never really her thing, but athletics<br />
kept her involved, barely. She excelled in both basketball and<br />
track, but allowed her insecurities to get the best of her, limiting<br />
28 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong><br />
Cover design by Mary Schuck • Cover photograph © Steve Azzara
her potential to succeed. She never really believed that she could be<br />
good enough to make her mother proud.<br />
From the long list of do’s and don’ts that her mother repeatedly<br />
held over her, the thing that stood out the most for Marvelyn was to<br />
not get pregnant. Neither HIV nor any other sexually transmissible<br />
infection, for that matter, was ever mentioned.<br />
Th ough she had learned a little about HIV in her high school<br />
health class, Marvelyn attributes the lack of understanding that she<br />
had about her own risks to the images in her textbook of sickly gay,<br />
white men and terribly thin people from Africa. For her, those were<br />
the faces of AIDS. And, because she was not having nearly as much<br />
sex as she had read Magic Johnson was having in his heyday, nor<br />
was anybody she knew, she was never able to recognize her connection<br />
to the virus even through his example.<br />
For the most part, though, she played it safe. Th ere were times,<br />
however, when her desire to fi ll the void that had been left by her<br />
father’s departure got the best of her. She tried, unsuccessfully, to<br />
get pregnant a couple of times, believing that carrying a man’s child<br />
would guarantee his love for her. Th e deprivation of a father’s love<br />
can lead to warped thinking within a child. Marvelyn’s search for<br />
love and acceptance from a man, however, eventually led her to<br />
place her trust in the wrong one.<br />
Her Prince Charming (as she aff ectionately dubbed him) came<br />
complete with all the trappings of perfection, and a little something<br />
extra to top it off . He was older, good looking, gainfully employed,<br />
had his own place and car, and treated Marvelyn like the princess<br />
that she knew deep down inside she was. Aft er several failed<br />
attempts at love, Marvelyn was convinced that this was the one.<br />
A couple of months into their relationship though, Marvelyn’s<br />
dream was shattered as quickly as it had come to life. In relatively<br />
great shape from her years as a high school athlete, Marvelyn was<br />
perplexed by her sudden onset of chronic fatigue and drastic weight<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
loss. She assumed at fi rst that it was simply a passing bug, until her<br />
symptoms became so severe that she literally passed out one morning<br />
while getting ready for work.<br />
She was not alone in her confusion with regards to her symptoms.<br />
Test aft er negative test, doctors at a local hospital were also<br />
baffl ed by what was going on with Marvelyn. One curious doctor<br />
decided to conduct an HIV test, the results of which would change<br />
Marvelyn’s life forever.<br />
Th is doctor was able to determine that Marvelyn’s infection<br />
was a recent one, but was amazed at the rate at which the virus<br />
had advanced (her symptoms were not those typically associated<br />
with HIV serocon<strong>version</strong>). Completely unaware of the stigma associated<br />
with HIV, Marvelyn began sharing her diagnosis with any<br />
and everyone, in hopes of gaining a better understanding about the<br />
virus that was ailing her. Why didn’t she know that she was at risk<br />
for HIV, she wondered? And if she didn’t know, how many other<br />
young, black women were also in the dark?<br />
Th us began Marvelyn’s miraculous journey from a dying<br />
young victim of the virus that causes AIDS to a world-renowned<br />
advocate whose story has been featured everywhere from BET to<br />
MTV to Th e Oprah Winfrey Show, and throughout the African<br />
diaspora. Her story is chronicled in her deeply moving and inspiring<br />
autobiography entitled Th e Naked Truth: Young, Beautiful and<br />
(HIV) Positive. Th is book is a must-read for us all, but especially<br />
for young African American women who, like Marvelyn, may be<br />
totally unaware of their own vulnerability to HIV. e<br />
The Naked Truth: Young, Beautiful, and (HIV) Positive (2008),<br />
by Marvelyn Brown with Courtney E. Martin is published by Amistad,<br />
an Imprint of HarperCollins Publishers; www.amist adbooks.<br />
com. Visit www.marvelynbrown.com.<br />
<strong>Positively</strong> <strong>Aware</strong><br />
29
697US09AB01702_DTC_LaunchAd_8x10.5_v3 2:- 4/6/09 3:49 PM Page 1<br />
Important Information<br />
INDICATION<br />
ATRIPLA ® (efavirenz 600 mg/emtricitabine 200 mg/<br />
tenofovir disoproxil fumarate [DF] 300 mg) is a<br />
prescription medication used alone as a complete<br />
regime n or with other medicines to treat HIV-1<br />
infection in adults.<br />
ATRIPLA does not cure HIV-1 and has not been<br />
shown to prevent passing HIV-1 to others.<br />
See your healthcare provider regularly.<br />
IMPORTANT SAFETY INFORMATION<br />
Contact your healthcare provider right away if<br />
you experience any of the following side effects<br />
or conditions associated with ATRIPLA:<br />
• Nausea, vomiting, unusual muscle pain, and/<br />
or weakness. These may be signs of a buildup<br />
of acid in the blood (lactic acidosis), which is<br />
a serious medical condition.<br />
• Light colored stools, dark colored urine, and/<br />
or if your skin or the whites of your eyes turn<br />
yellow. These may be signs of serious liver<br />
problems.<br />
• If you have HIV-1 and hepatitis B virus (HBV),<br />
your liver disease may suddenly get worse if<br />
you stop taking ATRIPLA. Do not stop taking<br />
ATRIPLA unless directed by your healthcare<br />
provider.<br />
Do not take ATRIPLA if you are taking the<br />
following medicines because serious and<br />
life-threatening side effects may occur when<br />
taken together:<br />
Vascor ® (bepridil), Propulsid ® (cisapride),<br />
Versed ® (midazolam), Orap ® (pimozide),<br />
Halcion ® (triazolam), or ergot medications (for<br />
example, Wigraine ® and Cafergot ® ).<br />
In addition, ATRIPLA should not be taken<br />
with: Combivir ® (lamivudine/zidovudine),<br />
EMTRIVA ® (emtricitabine),<br />
Epivir ® or Epivir-HBV ® (lamivudine),<br />
Epzicom ® (abacavir sulfate/lamivudine),<br />
SUSTIVA ® (efavirenz),<br />
Trizivir ® (abacavir sulfate/lamivudine/zidovudine),<br />
TRUVADA ® (emtricitabine/tenofovir DF),<br />
or VIREAD ® (tenofovir DF), because they contain<br />
the same or similar active ingredients as ATRIPLA.<br />
Vfend ® (voriconazole) or REYATAZ ® (atazanavir<br />
sulfate), with or without Norvir ® (ritonavir), should<br />
not be taken with ATRIPLA since they may lose their<br />
effect and may also increase the chance of having<br />
side effects from ATRIPLA. Fortovase ® or<br />
Invirase ® (saquinavir) should not be used as the<br />
only protease inhibitor in combination with ATRIPLA.<br />
Taking ATRIPLA with St. John’s wort or products<br />
containing St. John’s wort is not recommended as it<br />
may cause decreased levels of ATRIPLA, increased<br />
viral load, and possible resistance to ATRIPLA or<br />
cross-resistance to other anti-HIV drugs.<br />
This list of medicines is not complete. Discuss<br />
with your healthcare provider all prescription<br />
and nonprescription medicines, vitamins, or<br />
herbal supplements you are taking or plan<br />
to take.<br />
Contact your healthcare provider right away if you<br />
experience any of the following side effects or<br />
conditions:<br />
Please see Patient Information on the following pages.<br />
• Severe depression, strange thoughts, or angry<br />
behavior have been reported by a small number<br />
of patients. Some patients have had thoughts of<br />
suicide and a few have actually committed suicide.<br />
These problems may occur more often in patients<br />
who have had mental illness.<br />
• Dizziness, trouble sleeping or concentrating,<br />
drowsiness, unusual dreams, and/or<br />
hallucinations are common, and tend to go away<br />
after taking ATRIPLA (efavirenz 600 mg/<br />
emtricitabine 200 mg/tenofovir DF 300 mg) for<br />
a few weeks. Symptoms were severe in a few<br />
patients and some patients discontinued therapy.<br />
These symptoms may become more severe with<br />
the use of alcohol and/or mood-altering (street)<br />
drugs. If you are dizzy, have trouble concentrating,<br />
and/or are drowsy, avoid activities that may be<br />
dangerous, such as driving or operating machinery.<br />
• Kidney or liver problems. If you have had kidney<br />
or liver problems, including hepatitis infection or<br />
take other medicines that may cause kidney or<br />
liver problems, your healthcare provider should do<br />
regular blood tests.<br />
• Pregnancy: Women should not become<br />
pregnant while taking ATRIPLA and for<br />
12 weeks after stopping ATRIPLA. Serious birth<br />
defects have been seen in children of women<br />
treated during pregnancy with one of the<br />
medicines in ATRIPLA. Therefore, women must use<br />
a reliable form of barrier contraception, such as a<br />
condom or diaphragm, even if they also use other<br />
methods of birth control.<br />
• Breast-Feeding: Women with HIV-1 should not<br />
breast-feed because they can pass HIV-1 through<br />
their milk to the baby. Also, ATRIPLA may pass<br />
through breast milk and cause serious harm to the<br />
baby.<br />
• Rash is a common side effect that usually goes<br />
away without treatment, but may be serious in a<br />
small number of patients.<br />
• Seizures have occurred in patients taking a<br />
component of ATRIPLA, usually in those with<br />
a history of seizures. If you have ever had seizures,<br />
or take medicine for seizures, your healthcare<br />
provider may want to switch you to another<br />
medicine or monitor you.<br />
• Bone changes. If you have had bone problems in<br />
the past, your healthcare provider may want to<br />
check your bones.<br />
• If you have ever had mental illness or use illegal<br />
drugs or alcohol.<br />
Changes in body fat have been seen in some people<br />
taking anti-HIV-1 medicines. The cause and<br />
long-term health effects are not known.<br />
Other common side effects of ATRIPLA include<br />
tiredness, headache, upset stomach, vomiting, gas,<br />
and diarrhea. Skin discoloration (small spots or<br />
freckles) may also happen.<br />
You should take ATRIPLA once daily on an empty<br />
stomach. Taking ATRIPLA at bedtime may make<br />
some side effects less bothersome.<br />
ATRIPLA is one of several treatment options<br />
your doctor may consider.<br />
You are encouraged to report negative<br />
side effects of prescription drugs to the<br />
FDA. Visit www.fda.gov/medwatch or<br />
call 1-800-FDA-1088.<br />
Patient model.<br />
Individual results may vary.<br />
© 2009 Bristol-Myers Squibb &<br />
Gilead Sciences, LLC. All rights reserved.<br />
ATRIPLA is a trademark of Bristol-Myers<br />
Squibb & Gilead Sciences, LLC. EMTRIVA,<br />
VIREAD, and TRUVADA are trademarks of Gilead<br />
Sciences, Inc. SUSTIVA is a registered<br />
trademark of Bristol-Myers Squibb Pharma<br />
Company. REYATAZ is a registered trademark<br />
of Bristol-Myers Squibb Company. All other<br />
trademarks are owned by third parties.<br />
697US09AB01702/TR1495 03/09
Please see Important Safety Information, including information<br />
on lactic acidosis, serious liver problems, and flare-ups of<br />
hepatitis B virus (HBV) on adjacent page.<br />
*Synovate Healthcare Data; US HIV Monitor, Q3 2008.<br />
“ATRIPLA has all my HIV meds<br />
in one pill daily, and helps<br />
me take charge of my HIV.”<br />
ATRIPLA is the #1 prescribed HIV regimen. *<br />
• Only ATRIPLA combines 3 HIV medications in 1 pill daily.<br />
• Proven to lower viral load to undetectable † and help raise T-cell<br />
(CD4+) count to help control HIV through 3 years of a clinical study.<br />
Talk to your doctor to see if ATRIPLA is right for you.<br />
Your doctor may prescribe ATRIPLA alone or with other HIV medications.<br />
† Defined as a viral load of less than 400 copies/mL.<br />
Steven<br />
on ATRIPLA for 2 years<br />
To learn more, visit<br />
www.ATRIPLA.com
697US09AB01702_DTC_LaunchAd_8x10.5_v3 2: 4/6/09 3:49 PM Page 3<br />
FDA-Approved Patient Labeling<br />
Patient Information<br />
ATRIPLA ® (uh TRIP luh) Tablets<br />
ALERT: Find out about medicines that should NOT be taken with ATRIPLA.<br />
Please also read the section “MEDICINES YOU SHOULD NOT TAKE WITH ATRIPLA.”<br />
Generic name: efavirenz, emtricitabine and tenofovir disoproxil fumarate (eh FAH vih renz,<br />
em tri SIT uh bean and te NOE’ fo veer dye soe PROX il FYOU mar ate)<br />
Read the Patient Information that comes with ATRIPLA (efavirenz/emtricitabine/tenofovir<br />
disoproxil fumarate) before you start taking it and each time you get a refill since there may<br />
be new information. This information does not take the place of talking to your healthcare<br />
provider about your medical condition or treatment. You should stay under a healthcare<br />
provider’s care when taking ATRIPLA. Do not change or stop your medicine without first<br />
talking with your healthcare provider. Talk to your healthcare provider or pharmacist if you<br />
have any questions about ATRIPLA.<br />
What is the most important information I should know about ATRIPLA?<br />
• Some people who have taken medicine like ATRIPLA (which contains nucleoside<br />
analogs) have developed a serious condition called lactic acidosis (build up of an acid<br />
in the blood). Lactic acidosis can be a medical emergency and may need to be treated in<br />
the hospital. Call your healthcare provider right away if you get the following signs<br />
or symptoms of lactic acidosis:<br />
• You feel very weak or tired.<br />
• You have unusual (not normal) muscle pain.<br />
• You have trouble breathing.<br />
• You have stomach pain with nausea and vomiting.<br />
• You feel cold, especially in your arms and legs.<br />
• You feel dizzy or lightheaded.<br />
• You have a fast or irregular heartbeat.<br />
• Some people who have taken medicines like ATRIPLA have developed serious liver<br />
problems called hepatotoxicity, with liver enlargement (hepatomegaly) and fat in the<br />
liver (steatosis). Call your healthcare provider right away if you get the following<br />
signs or symptoms of liver problems:<br />
• Your skin or the white part of your eyes turns yellow (jaundice).<br />
• Your urine turns dark.<br />
• Your bowel movements (stools) turn light in color.<br />
• You don’t feel like eating food for several days or longer.<br />
• You feel sick to your stomach (nausea).<br />
• You have lower stomach area (abdominal) pain.<br />
• You may be more likely to get lactic acidosis or liver problems if you are female, very<br />
overweight (obese), or have been taking nucleoside analog-containing medicines, like<br />
ATRIPLA, for a long time.<br />
• If you also have hepatitis B virus (HBV) infection and you stop taking ATRIPLA, you<br />
may get a “flare-up” of your hepatitis. A “flare-up” is when the disease suddenly<br />
returns in a worse way than before. Patients with HBV who stop taking ATRIPLA need<br />
close medical follow-up for several months, including medical exams and blood tests to<br />
check for hepatitis that could be getting worse. ATRIPLA is not approved for the treatment<br />
of HBV, so you must discuss your HBV therapy with your healthcare provider.<br />
What is ATRIPLA?<br />
ATRIPLA contains 3 medicines, SUSTIVA ® (efavirenz), EMTRIVA ® (emtricitabine) and VIREAD ®<br />
(tenofovir disoproxil fumarate also called tenofovir DF) combined in one pill. EMTRIVA and<br />
VIREAD are HIV-1 (human immunodeficiency virus) nucleoside analog reverse transcriptase<br />
inhibitors (NRTIs) and SUSTIVA is an HIV-1 non-nucleoside analog reverse transcriptase<br />
inhibitor (NNRTI). VIREAD and EMTRIVA are the components of TRUVADA ® . ATRIPLA can be<br />
used alone as a complete regimen, or in combination with other anti-<br />
HIV-1 medicines to treat people with HIV-1 infection. ATRIPLA is for adults age 18 and over.<br />
ATRIPLA has not been studied in children under age 18 or adults over age 65.<br />
HIV infection destroys CD4 + T cells, which are important to the immune system. The immune<br />
system helps fight infection. After a large number of T cells are destroyed, acquired immune<br />
deficiency syndrome (AIDS) develops.<br />
ATRIPLA helps block HIV-1 reverse transcriptase, a viral chemical in your body (enzyme) that<br />
is needed for HIV-1 to multiply. ATRIPLA lowers the amount of HIV-1 in the blood (viral load).<br />
ATRIPLA may also help to increase the number of T cells (CD4 + cells), allowing your immune<br />
system to improve. Lowering the amount of HIV-1 in the blood lowers the chance of death or<br />
infections that happen when your immune system is weak (opportunistic infections).<br />
Does ATRIPLA cure HIV-1 or AIDS?<br />
ATRIPLA does not cure HIV-1 infection or AIDS. The long-term effects of ATRIPLA are not<br />
known at this time. People taking ATRIPLA may still get opportunistic infections or other<br />
conditions that happen with HIV-1 infection. Opportunistic infections are infections that<br />
develop because the immune system is weak. Some of these conditions are pneumonia,<br />
herpes virus infections, and Mycobacterium avium complex (MAC) infection. It is very<br />
important that you see your healthcare provider regularly while taking ATRIPLA.<br />
Does ATRIPLA (efavirenz/emtricitabine/tenofovir disoproxil fumarate) reduce the risk<br />
of passing HIV-1 to others?<br />
ATRIPLA has not been shown to lower your chance of passing HIV-1 to other people<br />
through sexual contact, sharing needles, or being exposed to your blood.<br />
• Do not share needles or other injection equipment.<br />
• Do not share personal items that can have blood or body fluids on them, like<br />
toothbrushes or razor blades.<br />
• Do not have any kind of sex without protection. Always practice safer sex by using a<br />
latex or polyurethane condom or other barrier to reduce the chance of sexual contact with<br />
semen, vaginal secretions, or blood.<br />
Who should not take ATRIPLA?<br />
Together with your healthcare provider, you need to decide whether ATRIPLA is right for you.<br />
Do not take ATRIPLA if you are allergic to ATRIPLA or any of its ingredients. The active<br />
ingredients of ATRIPLA are efavirenz, emtricitabine, and tenofovir DF. See the end of this<br />
leaflet for a complete list of ingredients.<br />
What should I tell my healthcare provider before taking ATRIPLA?<br />
Tell your healthcare provider if you:<br />
• Are pregnant or planning to become pregnant (see “What should I avoid while taking<br />
ATRIPLA?”).<br />
• Are breast-feeding (see “What should I avoid while taking ATRIPLA?”).<br />
• Have kidney problems or are undergoing kidney dialysis treatment.<br />
• Have bone problems.<br />
• Have liver problems, including hepatitis B virus infection. Your healthcare provider<br />
may want to do tests to check your liver while you take ATRIPLA.<br />
• Have ever had mental illness or are using drugs or alcohol.<br />
• Have ever had seizures or are taking medicine for seizures.<br />
What important information should I know about taking other medicines with<br />
ATRIPLA?<br />
ATRIPLA may change the effect of other medicines, including the ones for HIV-1, and<br />
may cause serious side effects. Your healthcare provider may change your other medicines<br />
or change their doses. Other medicines, including herbal products, may affect ATRIPLA. For<br />
this reason, it is very important to let all your healthcare providers and pharmacists know<br />
what medications, herbal supplements, or vitamins you are taking.<br />
MEDICINES YOU SHOULD NOT TAKE WITH ATRIPLA<br />
• The following medicines may cause serious and life-threatening side effects when taken<br />
with ATRIPLA. You should not take any of these medicines while taking ATRIPLA: Vascor<br />
(bepridil), Propulsid (cisapride), Versed (midazolam), Orap (pimozide), Halcion (triazolam),<br />
ergot medications (for example, Wigraine and Cafergot).<br />
• ATRIPLA also should not be used with Combivir (lamivudine/zidovudine), EMTRIVA, Epivir,<br />
Epivir-HBV (lamivudine), Epzicom (abacavir sulfate/lamivudine), Trizivir (abacavir<br />
sulfate/lamivudine/zidovudine), SUSTIVA, TRUVADA, or VIREAD.<br />
• Vfend (voriconazole) should not be taken with ATRIPLA since it may lose its effect or may<br />
increase the chance of having side effects from ATRIPLA.<br />
• Do not take St. John’s wort (Hypericum perforatum), or products containing<br />
St. John’s wort with ATRIPLA. St. John’s wort is an herbal product sold as a dietary<br />
supplement. Talk with your healthcare provider if you are taking or are planning to take<br />
St. John’s wort. Taking St. John’s wort may decrease ATRIPLA levels and lead to increased<br />
viral load and possible resistance to ATRIPLA or cross-resistance to other anti-HIV-1 drugs.<br />
It is also important to tell your healthcare provider if you are taking any of the following:<br />
• Fortovase, Invirase (saquinavir), Biaxin (clarithromycin); or Sporanox (itraconazole); these<br />
medicines may need to be replaced with another medicine when taken with<br />
ATRIPLA.<br />
• Calcium channel blockers such as Cardizem or Tiazac (diltiazem), Covera HS or Isoptin<br />
(verapamil) and others; Crixivan (indinavir); Methadone; Mycobutin (rifabutin); Rifampin;<br />
cholesterol-lowering medicines such as Lipitor (atorvastatin), Pravachol (pravastatin<br />
sodium), and Zocor (simvastatin); or Zoloft (sertraline); these medicines may need to<br />
have their dose changed when taken with ATRIPLA.<br />
• Videx, Videx EC (didanosine); tenofovir DF (a component of ATRIPLA) may increase<br />
the amount of didanosine in your blood, which could result in more side effects.<br />
You may need to be monitored more carefully if you are taking ATRIPLA<br />
(efavirenz/emtricitabine/tenofovir disoproxil fumarate) and didanosine together. Also, the<br />
dose of didanosine may need to be changed.<br />
• Reyataz (atazanavir sulfate) or Kaletra (lopinavir/ritonavir); these medicines may increase<br />
the amount of tenofovir DF (a component of ATRIPLA) in your blood, which could result in<br />
more side effects. Reyataz is not recommended with ATRIPLA. You may need to be<br />
monitored more carefully if you are taking ATRIPLA and Kaletra together. Also, the dose<br />
of Kaletra may need to be changed.<br />
• Medicine for seizures [for example, Dilantin (phenytoin), Tegretol (carbamazepine), or<br />
phenobarbital]; your healthcare provider may want to switch you to another medicine or<br />
check drug levels in your blood from time to time.
These are not all the medicines that may cause problems if you take<br />
ATRIPLA (efavirenz/emtricitabine/tenofovir disoproxil fumarate). Be sure to tell your<br />
healthcare provider about all medicines that you take.<br />
Keep a complete list of all the prescription and nonprescription medicines as well as any<br />
herbal remedies that you are taking, how much you take, and how often you take them.<br />
Make a new list when medicines or herbal remedies are added or stopped, or if the dose<br />
changes. Give copies of this list to all of your healthcare providers and pharmacists every<br />
time you visit your healthcare provider or fill a prescription. This will give your healthcare<br />
provider a complete picture of the medicines you use. Then he or she can decide the best<br />
approach for your situation.<br />
How should I take ATRIPLA?<br />
• Take the exact amount of ATRIPLA your healthcare provider prescribes. Never change<br />
the dose on your own. Do not stop this medicine unless your healthcare provider tells<br />
you to stop.<br />
• You should take ATRIPLA on an empty stomach.<br />
• Swallow ATRIPLA with water.<br />
• Taking ATRIPLA at bedtime may make some side effects less bothersome.<br />
• Do not miss a dose of ATRIPLA. If you forget to take ATRIPLA, take the missed dose right<br />
away, unless it is almost time for your next dose. Do not double the next dose. Carry on<br />
with your regular dosing schedule. If you need help in planning the best times to take your<br />
medicine, ask your healthcare provider or pharmacist.<br />
• If you believe you took more than the prescribed amount of ATRIPLA, contact your local<br />
poison control center or emergency room right away.<br />
• Tell your healthcare provider if you start any new medicine or change how you take old<br />
ones. Your doses may need adjustment.<br />
• When your ATRIPLA supply starts to run low, get more from your healthcare provider or<br />
pharmacy. This is very important because the amount of virus in your blood may increase<br />
if the medicine is stopped for even a short time. The virus may develop resistance to<br />
ATRIPLA and become harder to treat.<br />
• Your healthcare provider may want to do blood tests to check for certainside effects while<br />
you take ATRIPLA.<br />
What should I avoid while taking ATRIPLA?<br />
• Women should not become pregnant while taking ATRIPLA and for 12 weeks after<br />
stopping it. Serious birth defects have been seen in the babies of animals and women<br />
treated with efavirenz (a component of ATRIPLA) during pregnancy. It is not known whether<br />
efavirenz caused these defects. Tell your healthcare provider right away if youare<br />
pregnant. Also talk with your healthcare provider if you want to become pregnant.<br />
• Women should not rely only on hormone-based birth control, such as pills, injections, or<br />
implants, because ATRIPLA may make these contraceptives ineffective. Women must use<br />
a reliable form of barrier contraception, such as a condom or diaphragm, even if they also<br />
use other methods of birth control. Efavirenz, a component of ATRIPLA, may remain in your<br />
blood for a time after therapy is stopped. Therefore, you should continue to use<br />
contraceptive measures for 12 weeks after you stop taking ATRIPLA.<br />
• Do not breast-feed if you are taking ATRIPLA. The Centers for Disease Control and<br />
Prevention recommend that mothers with HIV not breast-feed because they can pass the<br />
HIV through theirmilk to the baby. Also, ATRIPLA may pass through breast milk and cause<br />
serious harm to the baby. Talk with your healthcare provider if you are breast-feeding. You<br />
should stop breast-feeding or may need to use a different medicine.<br />
• Taking ATRIPLA with alcohol or other medicines causing similar side effects as ATRIPLA,<br />
such as drowsiness, may increase those side effects.<br />
• Do not take any other medicines, including prescription and nonprescription medicines<br />
and herbal products, without checking with your healthcare provider.<br />
• Avoid doing things that can spread HIV-1 infection since ATRIPLA does not stop you<br />
from passing the HIV-1 infection to others.<br />
What are the possible side effects of ATRIPLA?<br />
ATRIPLA may cause the following serious side effects:<br />
• Lactic acidosis (buildup of an acid in the blood). Lactic acidosis can be a medical<br />
emergency and may need to be treated in the hospital. Call your healthcare provider<br />
right away if you get signs of lactic acidosis. (See “What is the most important<br />
information I should know about ATRIPLA?”)<br />
• Serious liver problems (hepatotoxicity), with liver enlargement (hepatomegaly) and fat<br />
in the liver (steatosis). Call your healthcare provider right away if you get any signs of liver<br />
problems. (See “What is the most important information I should know about ATRIPLA?”)<br />
• “Flare-ups” of hepatitisBvirus (HBV) infection, inwhich the disease suddenly returns<br />
in a worse way than before, can occur if you have HBV and you stop taking ATRIPLA. Your<br />
healthcare provider will monitor your condition for several months after stopping ATRIPLA<br />
if you have both HIV-1 and HBV infection and may recommend treatment for your HBV.<br />
• Serious psychiatric problems. A small number of patients may experience severe<br />
depression, strange thoughts, or angry behavior while taking ATRIPLA. Some patients have<br />
thoughts of suicide and a few have actually committed suicide. These problems may occur<br />
more often inpatients who have had mental illness. Contact your healthcare provider right<br />
away if you think you are having these psychiatric symptoms, so your healthcare provider<br />
can decide if you should continue to take ATRIPLA.<br />
• Kidney problems. If you have had kidney problems in the past or take other medicines<br />
that can cause kidney problems, your healthcare provider should do regular blood tests to<br />
check your kidneys.<br />
• Changes in bone mineral density (thinning bones). It is not known whether long-term<br />
use of ATRIPLA (efavirenz/emtricitabine/tenofovir disoproxil fumarate) will cause damage<br />
to your bones. If you have had bone problems in the past, your healthcare provider may<br />
need to do tests to check your bone mineral density or may prescribe medicines to help<br />
your bone mineral density.<br />
Common side effects:<br />
Patients may have dizziness, headache, trouble sleeping, drowsiness, trouble concentrating,<br />
and/or unusual dreams during treatment with ATRIPLA. These side effects may be reduced if<br />
you take ATRIPLA at bedtime on an empty stomach. They also tend to go away after you have<br />
taken the medicine for a few weeks. If you have these common side effects, such as<br />
dizziness, it does not mean that you will also have serious psychiatric problems, such as<br />
severe depression, strange thoughts, or angry behavior. Tell your healthcare provider right<br />
away if any of these side effects continue or if they bother you. It is possible that these<br />
symptoms may be more severe if ATRIPLA isusedwith alcohol or mood altering (street) drugs.<br />
If you are dizzy, have trouble concentrating, or are drowsy, avoid activities that may be<br />
dangerous, such as driving or operating machinery.<br />
Rash may be common. Rashes usually go away without any change in treatment. In a small<br />
number of patients, rash may be serious. If you develop a rash, call your healthcare provider<br />
right away.<br />
Other common side effects include tiredness, upset stomach, vomiting, gas, and diarrhea.<br />
Other possible side effects with ATRIPLA include:<br />
• Changes in body fat. Changes in body fat develop in some patients taking anti-HIV-1<br />
medicine. These changes may include an increased amount of fat in the upper back and<br />
neck (“buffalo hump”), in the breasts, and around the trunk. Loss of fat from the legs,<br />
arms, and face may also happen. The cause and long-term health effects of these fat<br />
changes are not known.<br />
• Skin discoloration (small spots or freckles) may also happen with ATRIPLA.<br />
Tell your healthcare provider or pharmacist if you notice any side effects while taking ATRIPLA.<br />
Contact your healthcare provider before stopping ATRIPLA because of side effects or for any<br />
other reason.<br />
This is not a complete list of side effects possible with ATRIPLA. Ask your healthcare<br />
provider or pharmacist for a more complete list of side effects of ATRIPLA and all the<br />
medicines you will take.<br />
How do I store ATRIPLA?<br />
• Keep ATRIPLA and all other medicines out of reach of children.<br />
• Store ATRIPLA at room temperature 77 °F (25 °C).<br />
• Keep ATRIPLA in its original container and keep the container tightly closed.<br />
• Do not keep medicine that is out of date or that you no longer need. If you throw any<br />
medicines away make sure that children will not find them.<br />
General information about ATRIPLA:<br />
Medicines are sometimes prescribed for conditions that are not mentioned in patient<br />
information leaflets. Do not use ATRIPLA for a condition for which it was not prescribed. Do<br />
not give ATRIPLA to other people, even if they have the same symptoms you have. It may<br />
harm them.<br />
This leaflet summarizes the most important information about ATRIPLA. If you would like more<br />
information, talk with your healthcare provider. You can ask your healthcare provider or<br />
pharmacist for information about ATRIPLA that is written for health professionals.<br />
Do not use ATRIPLA if the seal over bottle opening is broken or missing.<br />
What are the ingredients of ATRIPLA?<br />
Active Ingredients: efavirenz, emtricitabine, and tenofovir disoproxil fumarate<br />
Inactive Ingredients: croscarmellose sodium, hydroxypropyl cellulose, microcrystalline<br />
cellulose, magnesium stearate, sodium lauryl sulfate. The film coating contains black iron<br />
oxide, polyethylene glycol, polyvinyl alcohol, red iron oxide, talc, and titanium dioxide.<br />
September 2008<br />
ATRIPLA is a trademark of Bristol-Myers Squibb&Gilead Sciences, LLC. EMTRIVA, TRUVADA,<br />
and VIREAD are trademarks of Gilead Sciences, Inc. SUSTIVA is a trademark of Bristol-Myers<br />
Squibb Pharma Company. Reyataz and Videx are trademarks of Bristol-Myers Squibb<br />
Company. Pravachol is a trademark of ER Squibb & Sons, LLC. Other brands listed are the<br />
trademarks of their respective owners.<br />
SF-B0001B-10-08 21-937-GS-005 ST0064 Sept 2008
The<br />
Feminization<br />
of an Epidemic<br />
Women represent the fastest growing demographic of HIV<br />
infections worldwide. In order to work on reversing this<br />
trend, we must have a thorough understanding of the<br />
unique issues that aff ect women living with HIV infection. To date,<br />
the medical community has focused a large amount of its research<br />
eff orts on HIV/AIDS in men. 1, 2 However, both clinical experience<br />
and the observational data that we do have suggest that, despite the<br />
many similarities between HIV-positive men and women, there are<br />
some sex/gender-related diff erences with important HIV prevention<br />
and treatment implications. Th ese diff erences range from the<br />
interaction of HIV and the female immune system, to the social<br />
vulnerability that places women at higher risk for HIV and its complications.<br />
In order to design eff ective prevention and treatment<br />
strategies for HIV-positive women, we will need to understand and<br />
address any gender diff erences in the susceptibility to, and progression<br />
of, HIV infection. Th is article will review what we do know<br />
about women and HIV in terms of prevention and treatment, as<br />
well as highlighting areas that still require more research.<br />
The statistics<br />
Th e statistics serve as a potent reminder that specifi c HIV prevention<br />
strategies for girls and women are greatly needed. Women<br />
represent 46% of all people in the world infected with HIV. However,<br />
the rate of new infections among women is climbing, with<br />
50% of all new infections worldwide occurring in women (www.<br />
unaids.org). Th e United States has not escaped this global trend.<br />
Th e proportion of all AIDS cases in women has more than tripled<br />
in the past 15 years, from 7% in 1985 to 29% today. 3<br />
Women who are racial or ethnic minorities in this country are<br />
disproportionately at risk for HIV/AIDS. Th e Centers for Disease<br />
Control and Prevention (CDC) reports that, among HIV-positive<br />
women in the United States, over 80% are either African American<br />
or Hispanic. AIDS remains the leading cause of death in black<br />
women ages 25-34 in the U.S., while it represents the 10th leading<br />
cause of death in white women of the same age group.<br />
Th e threat of death from HIV/AIDS remains high in older<br />
African American women as well: AIDS is the 3rd and 4th leading<br />
causes of death in black women ages 35-44 and 45-54 years old,<br />
respectively. 4 Clearly, the rising rates of HIV infection in women<br />
Women and HIV in the United States<br />
by Saraswati Iobst, M.D. and Monica Gandhi, M.D., MPH<br />
and the disproportionate impact on women of color in this country<br />
require special attention.<br />
Women may be unaware of their risks for HIV<br />
infection<br />
In order to prevent new HIV infection in women, we must fi rst<br />
understand how women are being infected with HIV. According to<br />
many studies, approximately 40% of HIV-positive women report<br />
that they contracted HIV through sex with men. Th is number has<br />
not changed dramatically over the past two decades.<br />
What has changed, however, is an increasing number of<br />
women who do not know how they got HIV. In one large study<br />
of over 2,000 HIV-positive women, 48% of participants could not<br />
identify how they had contracted HIV. 5 Other studies have shown<br />
similar percentages of women not knowing how they contracted<br />
HIV, which likely indicates that women may not necessarily know<br />
the risk status of their male partners. 6<br />
A commonly-described phenomenon in the African American<br />
community, which may place black women at additional risk, is<br />
“down-low” behavior, where non-gay-identifi ed men have secretive<br />
sex with other men and then unprotected intercourse with female<br />
partners. 7 However, some analyses have shown that there is no real<br />
evidence that “down-low” behavior is fueling the epidemic among<br />
black women and that HIV prevention eff orts in the African American<br />
community should not be focused on a single risk behavior. 8<br />
Because the majority of women in the United States acquire<br />
HIV through sex with men, oft en without any knowledge that they<br />
are at risk, prevention eff orts in women must focus on increasing<br />
awareness of risk and routine diagnosis. Early diagnosis is critical<br />
to the prevention of HIV and AIDS.<br />
We know that identifying HIV in an individual decreases the<br />
risk of him or her infecting somebody else because of behavior<br />
modifi cation. 9 HIV treatment also decreases a person’s infectivity<br />
if he or she achieves undetectable viral loads. People who are diagnosed<br />
earlier also have a lower risk of progression to AIDS.<br />
Unfortunately, an estimated 24–27% of people living with<br />
HIV in the United States are unaware of their status. Furthermore,<br />
according to a National Health Interview Survey conducted in 2007,<br />
only 36% of adults reported ever being tested for HIV. 10<br />
34 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
In hopes of strengthening HIV prevention eff orts and maximizing<br />
the effi cacy of treatment for HIV-positive individuals, the<br />
CDC published new recommendations in September 2006 that all<br />
adults aged 13-64 should be tested at least once for HIV in a medical<br />
setting and that people at higher risk should be tested annually.<br />
11 Th e guidelines recommend opt-out screening, where a patient<br />
would be informed that he or she will be tested for HIV infection<br />
and given the opportunity to decline, instead of the previously<br />
instituted opt-in screening, where written consent was required for<br />
testing. Th e guidelines relaxed requirements on written consent<br />
and pre-testing counseling, which can be<br />
both time and labor intensive, in the hopes<br />
that this would decrease barriers for HIV<br />
screening for both patients and providers.<br />
These recommendations have not<br />
been fully implemented throughout the<br />
United States, since each state has needed to address the guidelines<br />
separately. California turned the CDC recommendations into law<br />
Table 1: Female-controlled methods of HIV prevention<br />
Method Current status<br />
Female condom Effective in reducing HIV<br />
transmission, but limitations<br />
include its expense, the fact<br />
that the female condom is not<br />
covert and the potential noise<br />
that the latex can make during<br />
intercourse.<br />
Microbicides Multiple trial failure; PRO2000<br />
(0.5%) in preliminary studies<br />
shows up to 30% reduced risk of<br />
transmission<br />
Diaphragms No evidence of efficacy in<br />
reducing infection rates to<br />
women<br />
Oral tenofovir-based<br />
prophylaxis<br />
In trials<br />
Partner treatment Reduces risk of transmission to<br />
serodiscordant partners<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
in 2007 with the passage of AB 682, which waives the need for written<br />
consent for HIV testing in this state. Widespread implementation<br />
of these recommendations would be especially benefi cial to<br />
women in this country, given the lack of perceived risk factors for<br />
HIV in this population. [Also see “Doctors Urge the Government<br />
to Keep up With Medical Progress” on page 49.]<br />
HIV prevention strategies in women<br />
Women are biologically and sociologically more vulnerable to<br />
HIV infection than men. Women are at greater risk of HIV infec-<br />
Prevention efforts<br />
need to focus on<br />
providing women with<br />
female-controlled<br />
prevention modalities.<br />
tion through heterosexual sex than are men simply by virtue of an<br />
unequal exchange of genital secretions. Th e risk of transmission of<br />
HIV from a man to a woman is approximately 1 in 1,000 for each<br />
sexual contact, whereas the risk of transmission from a woman to<br />
a man is much less (approximately one in 2,000). 12<br />
Women may also be at increased risk of infection during certain<br />
phases of their menstrual cycles (7-10 days following ovulation)<br />
because of hormonal interactions with the immune system, 13<br />
though further studies are needed on this topic.<br />
Women living in both resource-rich and resource-poor settings<br />
are vulnerable to HIV infection through sex for a variety of<br />
reasons, oft en arising from positions of dependence and an inability<br />
to insist upon the use of male condoms.<br />
Because women are more vulnerable to HIV through heterosexual<br />
sex, prevention eff orts need to focus on providing women<br />
with female-controlled prevention modalities. Currently, the male<br />
condom is the most eff ective form of HIV prevention for people<br />
engaging in sex, followed by male circumcision in terms of specifi<br />
c protection for the male partner. Obviously, women have much<br />
less control over the use of a male condom during a heterosexual<br />
encounter than men. Women-focused methods for HIV prevention<br />
are listed in Table 1. Although the female condom does have<br />
some effi cacy in reducing HIV transmission, it is not completely<br />
covert, as the outer ring or frame is visible outside the vagina. Further<br />
reducing its acceptability is the potential noise that the latex<br />
can make during intercourse. Additional hindrances to the use of<br />
the female condom include the fact that it is not readily available<br />
<strong>Positively</strong> <strong>Aware</strong><br />
35
in many countries, can be diffi cult to insert and remove, can be<br />
more expensive than male condoms and historically, can be used<br />
only once.<br />
Microbicides and diaphragms have received a lot of attention<br />
as they are relatively inexpensive and are completely female-centered<br />
modalities of prevention.<br />
Diaphragms were studied with lubricant gel in a large randomized<br />
open-label controlled trial of 4,948 HIV-negative Zambian and<br />
South African women and showed no effi cacy in protecting women<br />
against HIV transmission. 14<br />
Microbicides are biological or chemical substances that reduce<br />
transmission of HIV or other sexually transmitted diseases when<br />
applied to the vagina or rectum. Ideally a microbicide would be<br />
eff ective, safe with frequent use, widely available, easy to store and<br />
use, surreptitious, and acceptable to a variety of cultures. Most<br />
studies to date on diff erent microbicide products, starting with the<br />
failure of nonoxynol-9 to protect women against HIV infection<br />
(and the possibility of increased transmission rates), have shown<br />
disappointing results in terms of interrupting transmission.<br />
A recent study has provided some hope for the fi eld of microbicides<br />
and for the possibility of a female-controlled HIV prevention<br />
method at last. Th e interim safety and eff ectiveness results of<br />
a microbicide called PRO2000 (0.5%) were released at the 2009<br />
Conference of Retroviruses and Opportunistic Infections (CROI)<br />
in Montreal, Canada a few months ago. PRO2000 (0.5%) is a highly<br />
negatively-charged molecule (a polyanionic polymer) that is<br />
designed to interfere with HIV entry into target calls. Th e HPTN035<br />
We are starting to<br />
see a new trend of<br />
better outcomes<br />
in women compared<br />
to men.<br />
trial was also designed to study another microbicide product<br />
(Buff erGel) whose primary action is to lower vaginal pH levels. Th e<br />
trial enrolled 3,909 women from Malawi, South Africa, the United<br />
States, Zambia, and Zimbabwe, into four arms: the PRO2000 (0.5%)<br />
gel arm, the Buff erGel arm, a placebo gel arm, and a no gel arm. Th e<br />
trial followed participants for a mean of 20.4 months.<br />
Both microbicide products showed favorable safety profi les in<br />
the trial. While Buff erGel did not show a protective eff ect against<br />
HIV, the trial indicated that PRO2000 was at least 30% more eff ective<br />
than any other arm in the study in preventing new HIV infections.<br />
Th is preliminary trial was not designed to generate defi ni-<br />
tive data on PRO2000, although the data is highly suggestive of the<br />
potential effi cacy of this product. Th ese fi ndings were viewed with<br />
a great deal of enthusiasm in the microbicide and HIV prevention<br />
fi elds and other studies are underway. Studies that are looking at<br />
the effi cacy of a once-a-day pill (tenofovir or tenofovir/emtricitabine)<br />
for HIV-negative people to protect themselves against HIV<br />
infection (the pre-exposure prophylaxis or PrEP trials) are also<br />
underway. [Also see What’s Goin’ On on page 52.]<br />
Treatment issues for HIV-positive women<br />
HIV viral loads and CD4 counts in women versus men<br />
Th ere are clearly many unique issues that aff ect HIV prevention<br />
strategies for women, and the same is true for HIV treatment.<br />
Once a person is diagnosed with HIV, clinicians depend on viral<br />
loads and CD4 counts to determine when a patient should start<br />
treatment and to determine if their medications are working.<br />
It is generally assumed that a higher viral load means more<br />
viral activity in the body, and a higher CD4 count means a stronger<br />
immune system against HIV.<br />
We aim for undetectable viral loads and higher CD4 counts in<br />
the context of antiretroviral therapy. However, these assumptions<br />
and treatment guidelines were based mainly on studies on men. We<br />
are now learning that the immune system in women and HIV may<br />
interact diff erently than they do in men. Th ese fi ndings have led to<br />
some changes in treatment guidelines, as summarized below.<br />
Multiple studies have shown that<br />
women have lower levels of HIV (as measured<br />
by HIV RNA levels) in their blood<br />
than men do, even at the same CD4<br />
counts. 15 Th is means that at a certain CD4<br />
count (usually at higher CD4 counts), men<br />
will tend to have a higher viral load than<br />
women. Th is diff erence can be as much as<br />
two to six-fold for HIV viral levels.<br />
However, both men and women will<br />
progress to AIDS at the same rate. Another<br />
way to interpret this is that women are at<br />
increased risk of progression to AIDS when<br />
compared to men with the same viral loads,<br />
especially early on in infection. It is unclear<br />
why this phenomenon occurs, but these<br />
fi ndings have led to important treatment<br />
guideline changes.<br />
Prior guidelines recommended incorporating<br />
the HIV viral load to guide decisions<br />
regarding when to start treatment and<br />
when to modify therapy. However, that recommendation would<br />
mean that women would oft en get started on treatment much<br />
later than their male counterparts even though they had the same<br />
amount of immune suppression.<br />
Guidelines have now changed to refl ect that women oft en have<br />
viral loads that are much lower than men and the decision regarding<br />
when to start treatment is now made based on CD4 counts<br />
instead of viral loads.<br />
Women also tend to have higher CD4 cell counts than men, at<br />
least early on in infection. Th is does not necessarily mean that they<br />
have stronger immune systems, because we have found that women<br />
36 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
can develop AIDS at higher CD4 counts<br />
than men. Some authors have argued that,<br />
because women have higher CD4 counts<br />
when they develop AIDS, perhaps they<br />
should be started on highly active antiretroviral<br />
therapy (HAART) at higher CD4<br />
counts than men. More research is needed<br />
to determine how to use viral loads and<br />
CD4 counts in women to determine when<br />
to start antiretroviral (ARV) treatment.<br />
Efficacy of HAART in women versus men<br />
Despite the above diff erences in CD4 counts and viral loads<br />
between men and women, recent studies have shown that HAART<br />
is just as eff ective in women as it is in men. Early in the HIV epidemic,<br />
women with HIV seemed to progress faster to AIDS and<br />
death than men, 16 most likely because of decreased HIV testing,<br />
access to antiretrovirals (ARVs) and HIV care, lower rates of medication<br />
adherence in HIV-positive women, and higher rates of IV<br />
drug use among women with HIV.<br />
Disease progression to AIDS and death between men and<br />
women seemed to level out in the mid-1990s to early 2000s as more<br />
and more women were diagnosed with HIV and started on ARV<br />
treatment. 17 In the current era, we are starting to see a new trend of<br />
better outcomes in women compared to men. 18<br />
Th e reasons for this trend are multifactorial and all are not well<br />
understood, although increased access to HIV testing and ARVs<br />
have defi nitely contributed. Women also tend to have higher levels<br />
of ARV medications in their blood than men, which may lead to<br />
improved responses to treatment. Th e consequence of higher drug<br />
levels than men, however, can also be a higher number of adverse<br />
eff ects.<br />
Antiretroviral drug levels in women versus men<br />
Cross-sectional and small pharmacokinetic studies have<br />
shown that women tend to have higher levels of antiretrovirals in<br />
their blood than men. 19 Th is may partially explain the recent trend<br />
of improved outcomes among women as more and more women<br />
have access to medications.<br />
In addition, in the current era, it is possible that drug-experienced<br />
patients on antiretrovirals may have better outcomes when<br />
they have higher drug levels in their blood. Th ere are many variables<br />
that contribute to how people’s bodies process medications,<br />
many of which are aff ected by<br />
gender and hormones.<br />
For example, women generally<br />
weigh less and will therefore<br />
oft en have higher plasma levels<br />
of ARVs at a given dose. Estrogen<br />
aff ects protein production in the<br />
body, which will aff ect drug levels<br />
because proteins oft en attach<br />
to drugs in the blood and carry<br />
them around. Men seem to clear<br />
antiretroviral medications more<br />
rapidly than women due to differences<br />
in kidney and liver function.<br />
In general, there are a multitude<br />
of reasons why women may<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
have higher levels of HIV medications in their bloodstream and<br />
this fact may explain better treatment responses and higher rates<br />
of side eff ects.<br />
Rates of side effects on antiretrovirals are higher<br />
in women than men<br />
Higher levels of ARVs may also have detrimental eff ects for<br />
women. We have found that women experience more frequent and<br />
severe side eff ects from antiretrovirals compared to men. 20<br />
Th is remains an important issue to understand and address<br />
because side eff ects aff ect women’s quality of life, overall health,<br />
and place them at risk for stopping medications that they cannot<br />
tolerate, which could have devastating<br />
eff ects on their HIV treatment.<br />
Th ere are many diff erent side<br />
effects of antiretrovirals, but the<br />
most commonly reported side eff ects<br />
that seem to be worse in women are<br />
rashes, liver toxicity, and fat distribution<br />
changes.<br />
Women of child-bearing age<br />
represent an important category to<br />
consider because certain antiretrovirals<br />
can have negative eff ects on<br />
the fetus if a woman should become<br />
pregnant.<br />
Rash<br />
People commonly develop rashes<br />
as a side eff ect of antiretrovirals; most are mild, but some can<br />
lead to serious complications, including hospitalization and even<br />
death.<br />
Studies have shown that non-nucleoside reverse transcriptase<br />
inhibitor (NNRTI)-induced rashes are more common and tend to<br />
be more severe among women. 21<br />
A study of nevirapine (Viramune) showed that 15.8% of women<br />
compared to 8.4% of men developed rashes. Women were approximately<br />
seven times more likely than men to develop a severe rash,<br />
and 3.5 times more likely to discontinue nevirapine because of their<br />
rash. 22<br />
Another study confi rmed this fi nding and also reported a<br />
trend of increased risk of rash among patients with higher CD4<br />
counts. 23<br />
Studies of pregnant women have shown varied results, but<br />
most studies suggest that they have either the same or a reduced<br />
risk of NNRTI-induced rash than non-pregnant women.<br />
Another study of a new NNRTI, etravirine (Intelence), also<br />
showed that women had an increased risk of rash compared to men,<br />
34% versus 18%. 24<br />
Liver damage<br />
Women are also at increased risk of liver damage related to<br />
nevirapine compared to men. In fact, according to reports from<br />
post-marketing surveillance of this drug, women with CD4 counts<br />
higher than 250 cells/mm 3 had a 12-fold increased risk of developing<br />
clinically signifi cant liver damage compared to women with<br />
CD4 counts less than 250. Th is is in stark contrast to men who had<br />
a fi ve-fold increased risk of liver damage with higher CD4 counts<br />
(at greater than 400 cells/mm 3 ) compared to men with lower CD4<br />
<strong>Positively</strong> <strong>Aware</strong><br />
37
counts. 25 In a study from South Africa of HIV patients on nevirapine,<br />
20% of women compared to 12.8% of men had serious liver<br />
damage. Interestingly, 50% of the liver damage in the female group<br />
occurred in very thin women with body masses indices less than<br />
18.5. 26<br />
Fat redistribution<br />
Antiretroviral medications are well-known for their fat redistribution<br />
side eff ects, though this has been improving with more<br />
recent agents. However, women are uniquely aff ected by these side<br />
eff ects compared to men. Th is is likely due to a few reasons. First,<br />
women have more total body fat than men. And second, HIV-positive<br />
women tend to have more central obesity. However, women<br />
and men tend to have equal rates of fat loss from their extremities.<br />
Patients have described this fat pattern in women as resembling<br />
“beach balls on sticks.” [See “Lipodystrophy and Women,” May/<br />
June 2004 issue.] Further studies need to be done to understand the<br />
specifi c fat redistribution eff ects of ARVs in women, especially to<br />
determine if these changes could have detrimental eff ects on their<br />
overall health.<br />
Bone thinning<br />
Osteoporosis is defi ned as decreased bone mineral density and<br />
abnormal architecture of bone that increases the risk of serious<br />
fractures, which are in turn associated with a higher risk of death<br />
over 5 to 10 years.<br />
We already know that women in general are at increased risk<br />
of developing osteoporosis aft er menopause, but studies have also<br />
shown that HIV infection alone increases a person’s risk of losing<br />
bone mineral density. Th is places both men and women infected<br />
with HIV at increased risk of osteoporosis. 27<br />
HIV-positive women are at even higher risk, in fact approximately<br />
three times higher, for bone thinning than HIV-positive<br />
men. Other risk factors for HIV-positive individuals and bone loss<br />
include older age, lower body mass indices, higher viral loads, and<br />
lower CD4 counts. 28<br />
Th ere is some data to suggest that certain antiretrovirals may<br />
lead to bone mineral density loss. For example, two studies found<br />
that HIV-positive individuals on protease inhibitor (PI)-containing<br />
ARV regimens had higher rates of osteopenia and osteoporosis than<br />
HIV-positive individuals not on PI-containing regimens.<br />
Tenofovir (Viread) has been associated with bone thinning<br />
over time in randomized studies, possibly related to phosphate<br />
wasting on this drug. A large study that randomized patients to<br />
continuous therapy versus intermittent therapy (the SMART study)<br />
showed that patients in the continuous antiretroviral arm had<br />
higher rates of bone loss than those on intermittent ARVs.<br />
Most studies, however, show that HIV itself is a risk factor,<br />
whether or not antiretrovirals are implicated, and that higher viral<br />
loads, lower CD4 cell counts, and longer durations of HIV infection<br />
are associated with higher rates of bone mineral density loss, arguing<br />
that treatment of HIV infection is important in the prevention<br />
of osteoporosis. Many other studies have looked at standard osteoporosis<br />
treatments with bisphosphonates and calcium/vitamin D<br />
supplementation in HIV-positive patients on ARVs and have found<br />
these to be safe and eff ective treatments for osteoporosis. Most<br />
authors argue that vitamin D defi ciency should be ruled out in any<br />
HIV-positive patient with signifi cant osteoporosis to determine the<br />
need for extra supplementation.<br />
Th e bottom line here is that women with HIV need to be<br />
screened for osteoporosis regularly, and that both the treatment of<br />
their HIV and regular treatment for osteoporosis are warranted.<br />
HIV treatment considerations in pregnancy<br />
Women who could become pregnant require special consideration<br />
when deciding on the appropriate antiretroviral regimen<br />
because of the various eff ects of certain ARVs on pregnant women<br />
and the fetus.<br />
Efavirenz (Sustiva), which is a component of Atripla, is especially<br />
worrisome because this drug is known to cause serious neurologic<br />
consequences in the fetus and should be avoided in pregnancy.<br />
Women should be on birth control if they are sexually active<br />
while on efavirenz.<br />
Other ARVs that should be used with caution in pregnant<br />
women include didanosine [Videx] and stavudine [Zerit] together,<br />
which can lead to serious metabolic and liver conditions in<br />
women.<br />
Women with CD4 counts above 250 cells/mm 3 have been<br />
shown to be at higher risk of life-threatening liver toxicity and rash<br />
when starting nevirapine, as reviewed above, so this agent should<br />
also be used with caution in pregnant women.<br />
Important psychosocial considerations for HIVpositive<br />
women<br />
We have reviewed many of the biological and pharmacologic<br />
issues that are important in the treatment of HIV-positive women.<br />
However, many social and cultural issues, with special relevance<br />
to women, aff ect HIV treatment considerations just as they aff ect<br />
HIV prevention.<br />
Only 60% of HIV-positive females who qualify for HAART in<br />
the U.S. are on this life-saving therapy, compared to 75% of HIVpositive<br />
men who qualify for therapy. Th e reasons for this gender<br />
disparity need to be further elucidated, but some of the reasons lie<br />
in community beliefs regarding HIV/AIDS.<br />
An interesting survey in 2005 interviewed 500 African Americans<br />
in the U.S. about their beliefs about HIV (65% were women).<br />
Of those surveyed, 53% believed that a cure for AIDS exists, but<br />
was being withheld from the poor; 44% felt that people taking new<br />
medications were “guinea pigs”; and 27% thought that AIDS was<br />
created in a government lab. 29<br />
Clearly, conspiracy beliefs and suspicions regarding the medical<br />
establishment in the African American community will aff ect<br />
HIV-positive women more than men, given the disproportionate<br />
percentage of minorities.<br />
Another reason that women are less likely to engage in HIV<br />
treatment or care lies in higher rates of physical and sexual abuse<br />
38 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
in women. A history of abuse has been shown to decrease the<br />
likelihood that a woman will start and stay on an antiretroviral<br />
regimen.<br />
In addition, women who suff er from substance abuse issues,<br />
such as cocaine addiction, are also at increased risk of not starting<br />
treatment for their HIV when relevant.<br />
And let’s not forget the overwhelming eff ect of stigma, which<br />
disproportionately effects women both internationally and<br />
domestically.<br />
A national survey performed by the American Foundation for<br />
AIDS Research (AMFAR) and released in 2008 revealed the following<br />
disturbing results regarding stigma against HIV-positive<br />
women: of almost 5,000 individuals polled, approximately 70%<br />
would not want an HIV-positive female dentist; 60% would not<br />
want an HIV-positive physician or childcare provider; and 50%<br />
would not want an HIV-positive food server. Only 14% of Americans<br />
polled felt that HIV-positive women should have children.<br />
Th is is less than the percentage of Americans who felt that women<br />
with schizophrenia or Down’s Syndrome should have children, at<br />
17% and 19% respectively.<br />
Strategies to improve HIV prevention and treatment in women<br />
need to address physical and sexual abuse, stigma, community<br />
beliefs, and substance abuse issues in order to be successful.<br />
Ending with a success story<br />
Th ere has been one major treatment success story in women<br />
in the U.S. that needs to be commended, which is in the domain<br />
of prevention of mother-to-child transmission (PMTCT). Th e<br />
risk of HIV-positive mothers giving birth to HIV-positive babies<br />
has decreased from approximately 25% in 1993 to less than 1%<br />
today due to appropriate treatment. Th is decline is secondary to<br />
increasing HIV testing rates during pre-natal visits, increasing<br />
use of HAART in HIV-positive women during their pregnancies<br />
to prevent transmission to the fetus, and an increase in elective<br />
Cesarean-section births by HIV-positive women with viral loads<br />
that are greater than 1,000 copies/ml.<br />
Worldwide, the number and percentage of women accessing<br />
PMTCT medications has also increased from approximately 10%<br />
in 2004 to almost 35% in 2007, although rates of such access are<br />
still woefully low.<br />
Th e current guidelines in the U.S. for PMTCT are to start<br />
HAART in the second trimester if the mother is not already on<br />
therapy and to give intravenous zidovudine (AZT) to the mother<br />
during delivery. At the time of delivery, the options for the delivery<br />
mode are determined by the mother’s HIV viral load.<br />
If the viral load is less than 1,000 copies/ml, vaginal delivery is<br />
as safe as C-section in terms of transmission rate to the baby. Th e<br />
baby receives six weeks of oral AZT aft er delivery. If no treatment<br />
is started prior to labor, the mother and infant should receive treatment<br />
at birth and the infant should receive post-exposure prophylaxis<br />
[HIV medications used to prevent infection].<br />
In summary, HIV infection rates are increasing disproportionately<br />
among women, especially in minority groups. Prevention of<br />
HIV in women needs to come from increased awareness of HIV<br />
through routine screening and through providing women with<br />
eff ective, safe, female-centered prevention methods. Of the little<br />
that is known regarding HIV treatment and women, we know that<br />
women will do as well, if not better, on ARVs compared to men.<br />
Th is may be in part due to higher levels of drugs found in women,<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
which may also explain the higher levels of side eff ects of these<br />
medications in HIV-positive women.<br />
Despite the improvement in HIV treatment outcomes in<br />
women, gender disparities, abuse, and stigma still remain signifi -<br />
cant barriers to HIV prevention and treatment.<br />
And fi nally, it is important to focus on PMTCT as a success<br />
story in the U.S. because this story shows that, when signifi cant<br />
research and program implementation eff orts are instituted, amazing<br />
progress in HIV prevention and treatment is possible. Th is<br />
should serve as an example for increasing research eff orts and special<br />
programs aimed at improving HIV prevention and treatment<br />
for women. e<br />
Strategies to improve<br />
HIV prevention and<br />
treatment in women<br />
need to address<br />
physical and sexual<br />
abuse, stigma,<br />
community beliefs,<br />
and substance abuse<br />
issues in order to be<br />
successful.<br />
Monica Gandhi, M.D., MPH, is an Assist ant Professor of Medicine<br />
in the Division of HIV/AIDS at the University of California, San<br />
Francisco (UCSF). She sp ecializes in the clinical care of HIV-infect ed<br />
women and direct s the HIV inpatient consult service at San Francisco<br />
General Hosp ital. Her research career is focused on examining<br />
treatment issues for HIV-infect ed women in the Women’s Interagency<br />
HIV Study (WIHS), a large prosp ect ive multicenter cohort st udy<br />
of HIV-infect ed women.<br />
Saraswati Iobst , M.D., is a second-year resident in the University<br />
of California Primary Care (UCPC) program at the University of<br />
California, San Francisco (UCSF). She graduated from the University<br />
of Pennsylvania, School of Medicine in 2007. Her career interest s<br />
include HIV, primary care, and international health.<br />
Referenced footnotes available online at www.positivelyaware.com.<br />
<strong>Positively</strong> <strong>Aware</strong><br />
39
Aft er searching unsuccessfully for<br />
an HIV-positive Native American<br />
woman to interview here in Chicago,<br />
the American Indian Community<br />
House in New York suggested Lisa Tiger.<br />
We spoke by phone; her honesty and willingness<br />
to share her experiences and wisdom<br />
were refreshing and inspirational.<br />
No shame<br />
A member of the Muscogee Nation and<br />
of Creek, Seminole, Cherokee, and Irish<br />
descent, Lisa Tiger has been one of the few<br />
public Native American faces of AIDS since<br />
1992 when she was fi rst diagnosed with HIV,<br />
advancing to AIDS in 1999.<br />
When asked how she became an advocate<br />
in the fi rst place, she explained, “It<br />
was something that just happened. Th ere’s<br />
something about me—things just don’t<br />
embarrass me. From the moment I found<br />
out I was positive, I told everybody. My<br />
mom thought I was crazy and my uncle told<br />
me not to go around telling everybody. But,<br />
even though at fi rst I was shocked to fi nd<br />
out I was positive, I wasn’t embarrassed or<br />
ashamed.”<br />
Wilma Mankiller, fi rst female chief of<br />
the Cherokee Nation, asked her to come<br />
to the reservation and share her story. She<br />
accepted the invitation because, she says,<br />
“Th ere is such a need for education. And<br />
people weren’t paying attention to the Red<br />
Cross coming in with their classes. Th ey<br />
needed to hear from one of their own.” She<br />
also believes that prevention eff orts must be<br />
made more authentically culturally-based<br />
in order to get the message out to Native<br />
American people.<br />
Hardship<br />
It was clear, hearing her story, that this<br />
is a woman who has dealt with more tragedy<br />
in her life than most of us can imagine.<br />
Starting with the death of her father when<br />
she was 2½, she has also lost her brother<br />
and an adopted daughter, both murdered,<br />
as well as an ex-fi ancé who “drank himself<br />
to death.” In addition to her losses, she is<br />
dealing with Parkinson’s disease as well as<br />
AIDS.<br />
As if all that wasn’t enough, she is currently<br />
in the midst of a divorce and custody<br />
battle over her fi ve-year-old daughter, who<br />
she conceived by self-administered artifi cial<br />
insemination. With a deep sense of perception<br />
and a touch of sadness, she told me, “My<br />
husband is a good guy,” remembering times<br />
when his support helped her face some of<br />
life’s diffi culties. As our phone conversation<br />
continued while she drove towards Santa Fe<br />
to fi nd her daughter, she stated hopefully<br />
that they would work things out.<br />
Forgiveness<br />
Her ability to look past anger and sadness<br />
is the result of several life lessons. She<br />
told me that when she was 40, she gave herself<br />
10 years to fi nally tell the truth about<br />
all the things she’d done in her life that she<br />
Tiger Medicine<br />
A Native American woman’s story<br />
by Sue Saltmarsh<br />
regretted or was ashamed of. In giving me<br />
some examples, I thought that if everyone<br />
were willing to be as honest about their<br />
human foibles as she was, we’d all be better<br />
off ! She found that once she started with her<br />
honesty campaign, it turned out to be not<br />
as daunting as she’d thought and she was<br />
able to get it all done way before the 10-year<br />
deadline.<br />
She also gave Oprah, and some of her<br />
guests, credit for inspiring her to make a<br />
conscious eff ort to “be a healthier person”<br />
in many ways. She found that once she forgave<br />
herself for the mistakes she’d made, she<br />
found forgiveness of others easier. “Th ere’s<br />
no hate, no anger. Anything’s forgivable.”<br />
She has even found a way to replace the<br />
anger she felt towards the killers of her<br />
brother and daughter with compassion and<br />
peace.<br />
Dedication<br />
Tiger credits tenacious dedication to<br />
exercise as one of her survival secrets. “I’ve<br />
done a mile every day for over two years<br />
now,” she proudly states. “It doesn’t matter<br />
if I walk, run, or do the stationary bike as<br />
long as I do a mile of something.” She found<br />
that even while at the hospital bedside of a<br />
dying friend, her commitment got her to<br />
the gym every day.<br />
Th at dedication shows up in other ways<br />
as well. In addition to the public presentations<br />
she does, she admits that she “always<br />
wants to be a good friend, the one people<br />
40 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong><br />
Photo © Gerald Woff ord
call when they need someone to talk to” and<br />
her generosity of heart is evident in everything<br />
from her 1996 adoption of four abandoned<br />
and abused children from the Pine<br />
Ridge Indian Reservation, to the opening of<br />
her home to her ex-fi ancé’s cousin. She even<br />
has a plan in case she wins the lottery—to<br />
build a fi tness center on the Pine Ridge Reservation<br />
in honor of her friend, Leo Black<br />
Feather.<br />
Native American factors<br />
When asked about some of the factors<br />
that are contributing to the increase in HIV<br />
infections among Native Americans (see<br />
sidebar), women in particular, Tiger cited<br />
poverty, self-esteem issues, and alcoholism,<br />
but added that those things, along with<br />
domestic violence, accidental death, and<br />
suicide are so common in Native American<br />
communities that HIV is not at the top of<br />
the list of diffi culties and dangers that tribal<br />
people must deal with. In fact, in a way, she<br />
feels that HIV has become, for her, a way out<br />
of a painful life—it has given her purpose<br />
and through the speaking she does, sharing<br />
the story about her life and HIV/AIDS, she<br />
has found emotional healing.<br />
When asked about her philosophy of<br />
life, Tiger noted that the Native American<br />
sense of humor had oft en gotten her<br />
through hard times. “Aft er all,” she laughed,<br />
“you gotta go through the manure to get to<br />
the magic.” e<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
There’s no hate, no anger.<br />
Anything’s forgiveable.<br />
Native Americans & HIV/AIDS<br />
According to the most current data available from the U.S. Department of Health<br />
and Human Services’ Offi ce of Minority Health and the Centers for Disease Control<br />
and Prevention (CDC) 2005 HIV/AIDS Surveillance Report, revised in August 2008,<br />
it has been determined that in the 33 states with long-term, confi dential, name-based<br />
HIV reporting, the rate per 100,000 persons with HIV/AIDS diagnoses was 10.4 for<br />
Native Americans, as compared to 71.3 for African Americans, 27.8 for Latinos, and<br />
8.8 for whites. It should be noted that the number for Native Americans may be skewed<br />
by racial misclassifi cation during data-gathering. For instance, according to the CDC,<br />
“In Los Angeles, 56% of American Indians and Alaska Natives with AIDS were racially<br />
misclassifi ed.” In addition to HIV infection rates being high, Native Americans also<br />
have the lowest AIDS survival rate of any group – only one in four lives longer than<br />
three years aft er an AIDS diagnosis. Th e Center for AIDS Prevention Studies at the<br />
University of California San Francisco cites factors such as poverty (32% of NA live<br />
below poverty level, as compared with 13% of the general population), high rates of<br />
alcohol and substance abuse, STDs, and mental health problems as all playing a part in<br />
the HIV infection rate.<br />
According to the CDC, in 2007, 201 new cases of HIV infection were reported<br />
among Native American men and 69 among women. Th is puts the rate of infection<br />
among women at almost 26%, a rate three times higher than the rate for white women.<br />
Violence, domestic and otherwise, may be an underlying cause. According to the U.S.<br />
Department of Justice (1999), “the rate of violent crimes against Native American<br />
women is highest among all ethnic categories.” A 2006 study published in the American<br />
Journal of Public Health reported that 48% of NA women reported being raped, 62%<br />
reported physical assault, and 40% reported multiple victimizations. Th e Department of<br />
Health and Human Services reports that “Native American and Alaska Native women<br />
experience the highest rate of intimate partner violence of any ethnic group.” With 68%<br />
of HIV infections in these women being attributed to heterosexual contact, domestic<br />
violence is obviously a signifi cant factor.<br />
In order to promote prevention and testing programs in Native communities, the<br />
CDC funds Capacity Building Assistance programs through such organizations as the<br />
National Native American AIDS Prevention Center and the Inter Tribal Council of<br />
Arizona. Mobilization eff orts like National Native American HIV/AIDS <strong>Aware</strong>ness Day<br />
(the second annual day occurred on March 20 of this year) help communities to plan<br />
events like talking circles, pow-wows, testing opportunities, and the presentations of<br />
speakers like Lisa Tiger that will hopefully continue to raise awareness and help develop<br />
sound strategies for Native Americans to lessen the toll the disease takes on their communities.<br />
Th anks to Felicia and Alice at the American Indian Health Service in Chicago for<br />
providing insight and information and for the work they’re doing to reach out to those<br />
at risk in the Native American community.—Sue Saltmarsh e<br />
Visit their website at www.natHIVeamericanawareness.org<br />
<strong>Positively</strong> <strong>Aware</strong><br />
41
When I started working here at Test Positive <strong>Aware</strong> Network<br />
(TPAN) more than a decade ago, I heard of women<br />
infected during the 1980s who thought they weren’t at<br />
risk because “it’s a gay disease.”<br />
Now, working on this issue, I’ve heard of recently infected<br />
women who didn’t think they were at risk because they thought<br />
that “it’s a gay disease.”<br />
Of special concern today is the fact that black women make up<br />
66% of all new infections among women in the U.S.<br />
“I thought he loved me”<br />
A former co-worker here at TPAN went to another organization<br />
and was astounded at the number of newly diagnosed young<br />
women he sees, including middle-class, black college students.<br />
He said that when he asks them about condoms, they tell<br />
him, “I thought he loved me” or “We’ve been seeing each other for<br />
a while.” “One girl told me, ‘I’ve been with this guy since I was 16.<br />
We’ve broken up once or twice, but he would never do<br />
anything to hurt me.’ One of the women had a<br />
partner who was recently in jail for drug possession.<br />
Most of them saw the HIV ads on<br />
Protect<br />
Yourselves, rselves, Lad Ladies<br />
the [Chicago public] trains, but didn’t<br />
think the message applied to them.”<br />
He explained their reasoning.<br />
“They weren’t sleeping around.<br />
Th ey weren’t prostituting. Some<br />
of them already have a kid<br />
with their partner. If they get<br />
with a guy close to their age,<br />
they expect him to be HIVnegative.<br />
Their life was so<br />
heterosexual and their man<br />
was straight and not on the<br />
down-low. Th ey didn’t think<br />
they were at risk at all. ‘How did<br />
it cross over to me?’<br />
“It crossed over with unfaithful<br />
men and not knowing what they’re<br />
doing and who they’re doing it with,” he<br />
said. “Th e black community still thinks it’s<br />
only the promiscuous and the drug users who<br />
get infected, but if you’re having sex, you’re at risk.”<br />
What he fi nds especially disturbing is the emotional<br />
manipulation he sees being used against the women. He has seen<br />
women test positive during pregnancy, and when getting the news,<br />
the male partner showed no emotion or seemed to be supportive<br />
(“this doesn’t mean we have to break up”). My friend interpreted<br />
this as an indication that the man wasn’t surprised to fi nd out<br />
she was positive, because he already knew he was. “Th e fact that<br />
the women are getting tested fi rst lets the guy off the hook,” he<br />
explained. “He lets her think that she infected him or he doesn’t<br />
get tested at all.”<br />
Grandmas<br />
He also sees newly infected senior citizens, both male and<br />
female. Th ey didn’t worry about sexually transmitted diseases<br />
because they weren’t worried about pregnancy. “Seniors defi nitely<br />
didn’t believe they would be positive this late in life. Remember,<br />
their generation didn’t test,” he said.<br />
Th e seniors tell him that they may have had sex “once, two<br />
years ago or twice, three years ago.” Although shocked, he says they<br />
repeat a common saying among African American churchgoers,<br />
“God didn’t put more on me than I can bear, so I will deal with it.”<br />
At a nearby clinic specializing in HIV, another service provider<br />
said so many seniors have been newly diagnosed, there was thought<br />
given to opening a special program.<br />
“Th e women are over 50, their children are grown, they’re starting<br />
to date, and coming up positive,” she said. “Th ey are 60, 70, 72.<br />
Th e numbers are really high, and they’re like, ‘I don’t believe it.’<br />
Th ey say, ‘I’m a grandmother. What am I doing with an STD?’ I met<br />
a lady today. She was 68 years old.”<br />
Blame game<br />
A long time ago, I heard a black gay man say that women are<br />
equally to blame for their infection for not insisting on condoms.<br />
Th is sounded so wrong to me. It made me realize that vulnerability<br />
is one thing, culpability is another.<br />
At the same time, I remember the words of<br />
community advocates who point out that<br />
there’s also something wrong when you<br />
don’t protect yourself.<br />
I struggled over my former<br />
co-worker’s comments about<br />
the young men who must have<br />
known they were positive when<br />
they got a woman pregnant and<br />
the idea that men like them<br />
shouldn’t be demonized.<br />
In the middle of my<br />
struggle, my co-associate editor,<br />
Keith Green, walked in,<br />
fresh from graduating with his<br />
masters degree in social work<br />
from the University of Wiscon-<br />
Young ng or old old, black wo women<br />
continue to be at higher risk<br />
sin-Madison.<br />
Keith has been a source of<br />
enlightenment, love, and understanding<br />
about HIV in the black community<br />
in his many years of working here at TPAN.<br />
He has become a powerful force at the national<br />
level. I asked him about what he’s learned and how<br />
he thinks I should proceed.<br />
“Th at’s your story,” he told me. “Everybody is to blame. How<br />
do you talk about these men? You balance it out. What they did is<br />
absolutely wrong, but you encourage the women to step up.<br />
“Mental health is needed on both sides,” Keith continued.<br />
“Something’s got to be wrong with you to knowingly infect someone.<br />
But something’s not quite right with you if you’re not protecting<br />
yourself. Th at opens up a big can of worms. Why do black people<br />
disproportionately need mental health? Maybe we don’t, but we just<br />
lack access to mental health services, or we lack trust in those services<br />
to help us and not harm us.<br />
“Th ere’s a segment of the gay community that’s trying to prove<br />
that women are not being infected by down-low men,” he said.<br />
“Th ere’s no data to prove this one way or another, but my impression<br />
is that many women are, especially black women. I keep getting<br />
into conversations about stigma and mental health. You have<br />
a recipe for disaster.” e<br />
by Enid Vázquez<br />
42 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
Joyce<br />
Turner<br />
Keller<br />
Joyce Turner Keller is the founder and CEO of Asp irations, a non-profi t organization<br />
in Louisiana. A minist er for 40 years, she founded Asp irations aft er learning of her HIV<br />
infect ion. Aft er so many decades of helping to empower others, she was able to disclose her<br />
infect ion to her family within hours of learning of it. She advocates for the elimination of<br />
st igma for all people living with HIV and for awareness of the risk of infect ion. She is on<br />
the board of the National Minority AIDS Council, based in Washington, D.C.<br />
Enid Vázquez: Tell me about<br />
yourself.<br />
Joyce Turner Keller: I<br />
am a 59-year-old HIV-positive woman living<br />
with AIDS. I contracted the disease<br />
through rape. I’m the mother of three and<br />
the grandmother of many.<br />
I work with people from all walks of<br />
life. I don’t judge people based on race, religion,<br />
creed, color, or any gender preferences.<br />
I thought it was necessary that people know<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
you don’t have to be gay or white, you don’t<br />
have to be using drugs, you don’t have to<br />
be a commercial sex worker, to be infected<br />
with HIV.<br />
Th e other thing I wanted to bring to<br />
the public is that it doesn’t matter how<br />
you become infected. When I say, “I’m a<br />
woman living with AIDS,” the eyebrows<br />
go up, because they can’t look at me and<br />
tell. Th ere are times when I get sympathy or<br />
empathy or people tend to change their tone<br />
once they fi nd out how I became infected.<br />
A minister<br />
with<br />
AIDS lays<br />
reality on<br />
the line<br />
Interview by<br />
Enid Vázquez<br />
People seem to be more accepting then and<br />
that sometimes infuriates me, because I<br />
don’t think there’s anybody in this world<br />
who says, “You know, I think I’ll get infected<br />
with HIV today.”<br />
Whether it was consensual, whether it<br />
was assault—whatever, the same side eff ects,<br />
the same discrimination, the same ills, the<br />
same woes, the same concerns are there<br />
for me just as they are for the woman who<br />
may have gotten high, the young man who<br />
may have had sex with another man, or the<br />
wife who didn’t know her husband was on<br />
the down-low, or the man who didn’t know<br />
his wife was on the down-low. It’s no different,<br />
and I thought it was necessary that<br />
I come out and talk about it so that we can<br />
erase some of the stigma, dispel some of<br />
the misconceptions of how this disease is<br />
transmitted.<br />
EV: How do you address the idea that<br />
someone could have protected themselves?<br />
JTK: Life happens to all of us. We know<br />
that in the heat of passion, nobody is trying<br />
to get infected with HIV or another STD,<br />
or hepatitis, and definitely not trying to<br />
get pregnant. What I do is talk about sex,<br />
because that’s one of the “s” words we have<br />
to deal with, even in church. I talk about<br />
that because we equate sex to sin, and sin<br />
to shame.<br />
But I talk about sex because it’s a normal<br />
bodily function. So I tell people we need<br />
<strong>Positively</strong> <strong>Aware</strong><br />
43
to be protected before we go into the water.<br />
Sex is good. Sex is real good. But there’s a<br />
way to do anything. I try not to be judgmental,<br />
because sometimes we fi nd ourselves in<br />
places dealing with things we had no idea<br />
that we were going to be dealing with. And<br />
there are times when people just become<br />
attracted to each other and we know that’s<br />
normal.<br />
Th at’s the message I try to get out. I<br />
tell people we need to be more cautious<br />
and more concerned and more open when<br />
talking about sex with our young people. It<br />
would be better if we told them how good it<br />
is and that it’s normal, that it’s not a shameful<br />
thing, and if we also tell young people<br />
that abstinence is the only way not to get<br />
infected with HIV, but if you choose not to<br />
abstain, then these are your other choic-<br />
es. We need to teach people how to make<br />
healthier choices. Just don’t judge.<br />
Th ey say they deserve it because they<br />
did this, that, and the other. Sometimes I<br />
have to remind some people in my family<br />
who are older to take a step back and<br />
remember that I know when they were<br />
younger, some of the choices they made<br />
were not the best.<br />
Th at’s the way it is with a lot of people.<br />
Ministers in the pulpit who frown on people<br />
living with AIDS and they’re infected as<br />
well. Ministers who have a tendency to talk<br />
about homosexuals and are very negative,<br />
and they themselves could defi nitely be gay<br />
or have someone in their family who is.<br />
We don’t have to participate in the<br />
behavior of others, but I think we could be<br />
a little bit more understanding. A whole lot<br />
more understanding.<br />
EV: I was just talking to someone who<br />
works at a clinic (see page 42) and it seems<br />
like women still don’t know they’re at risk.<br />
Do you see this?<br />
JTK: I do see it, even in my family. It’s<br />
this trust factor. “He said that he got tested,”<br />
or “he showed me a piece of paper.” Someone<br />
shows you a piece of paper showing that<br />
they tested negative today, but what if they<br />
“We need to to<br />
recognize<br />
this disease<br />
as a weapon<br />
of mass<br />
destruction<br />
in our<br />
community.”<br />
went out last night and had unprotected sex?<br />
Does that still mean that he’s not infected?<br />
Or there’s just the complacency, the<br />
idea that “it can’t happen to me.” People<br />
actually believe that there’s a house on fi re,<br />
but it’s not my house.<br />
I tell them, “You may know what you’re<br />
doing, but there are 24 hours in the day. I’m<br />
not trying to get you to distrust your man,<br />
but what I am trying to do is tell you to protect<br />
yourself.” I use the phrase “passion and<br />
protection go hand in hand.”<br />
I see a lot of women who still believe<br />
that the only way they can hold on to a man<br />
is to do what he wants, the way he wants<br />
it. And I think a lot of it goes back to selfesteem<br />
and women not valuing themselves<br />
enough.<br />
Another issue is the fact that women<br />
believe that there aren’t enough men to go<br />
around. But there are plenty of men around.<br />
Th ey just have to value themselves enough<br />
and let a good man fi nd them rather than<br />
picking up whatever they can have. It’s<br />
like going to the store and just shopping<br />
from the bargain basket when there may<br />
be things on the shelf that you could aff ord.<br />
You may get a better quality. You may be<br />
paying a little more, but it’s worth it. [Just<br />
a few days aft er this interview, a woman<br />
with HIV told me she was afraid to let go<br />
of her boyfriend because she didn’t think<br />
she could fi nd someone else, but when she<br />
released him, three other men showed up in<br />
her life trying to take his place.—EV.]<br />
I bared my soul to the world and<br />
it’s fi ne, because I want young people to<br />
understand that this is a disease of opportunity.<br />
I want the middle-aged to know that<br />
they’re just as much at risk as I am. And<br />
I want older people to know—the elderly,<br />
the grandmothers in their 70s—that just<br />
because you’re having sex with a man who’s<br />
70, 75, or 80 doesn’t mean that he’s safe.<br />
We need to recognize this disease as<br />
a weapon of mass destruction in our community.<br />
It’s out there every day and not just<br />
on days we raise awareness. If it means my<br />
disclosing to the world who I am and what<br />
I’m living with, fi ne. I want people to know<br />
that this is no walk in the park. Despite<br />
how good I look, I want young people to<br />
understand … I want everyone to understand.<br />
I say young people because many<br />
young people feel invincible, and I’m pretty<br />
sure I felt that same way when I was a<br />
teenager, when I was a young adult, when<br />
I was a young mother. I felt invincible, that<br />
the world was my oyster and I could eat it<br />
whenever I chose. I think many of us have<br />
that perception of life and we don’t see the<br />
dangers that await us.<br />
At the same time I guess my biggest<br />
message to the world is to let them know<br />
that this is not a diagnosis of death, that<br />
AIDS is something that you can live with.<br />
I wanted people to understand that just<br />
because you’re diagnosed positive does not<br />
demean who you are—if anything, AIDS<br />
has propelled me to another level. e<br />
44 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
Photo © Russell McGonagle<br />
Interview with<br />
Evany Turk<br />
Sue Saltmarsh: What’s the most important<br />
thing that women should know about HIV?<br />
Evany Turk: That it’s not a death sentence, that you<br />
can live pretty much a normal life with it.<br />
SS: Did you start on meds right away?<br />
ET: Yes, and that was a struggle. At that time, I was given like 16<br />
pills to take twice a day, so it was real hard for me to do it, but after<br />
some hard work and some therapy, I finally got it together.<br />
SS: What would you say your everyday food, exercise, and sleep<br />
formula is to stay healthy?<br />
ET: I try to have breakfast every morning, because they say that’s<br />
the most important meal. I try to go to bed every night at 9:00,<br />
because I need my proper rest. I try to drink plenty of water, plenty<br />
of green tea. I’ve eliminated sugars out of my diet completely and<br />
that’s because I learned that viruses feed off of sugar. As far as exercise,<br />
I walk as much as I can—I walk up stairs and to the store - and<br />
I dance a lot. I love to dance and that’s good exercise. I don’t do any<br />
drugs and I don’t smoke. I do drink socially, but I try to limit my<br />
drinks to two per weekend. In order to stay sane with seven kids, I<br />
have to have a social life! Oh, and stress! I try to eliminate as much<br />
stress as possible.<br />
Stigma<br />
by Sue Saltmarsh<br />
Evany Turk is an insp iration. Positive for eight years,<br />
Evany works as the Program Coordinator for the Positive<br />
Adherence Stable Housing Now program at Chicago<br />
House and Social Service Agency, as well as being a mother<br />
and fost er parent. On the day we met for this interview,<br />
Evany was fi ghting a cold, but her good energy and positive<br />
outlook on life, as well as her dedication to her work<br />
and family, were st rongly evident.<br />
SS: What’s been the most difficult thing about being positive?<br />
ET: The stigma. And dating. And the dating part is because of the<br />
stigma. When to tell, when not to tell, who to tell and how to tell—<br />
that’s been the most difficult part. It’s easier now that I’ve told most<br />
of the important people in my life. But it took me a while to do it. My<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
A success<br />
story<br />
family<br />
found<br />
out just by<br />
looking up<br />
my medication<br />
on the Internet, but<br />
I didn’t tell other people<br />
until three or four years ago.<br />
SS: Is there anything that you think can<br />
be done to reduce the stigma?<br />
ET: Yes. I think if we had bigger campaigns around HIV and the<br />
risks and how it’s really affecting individuals—I definitely think if<br />
there were more African American women, more women, period,<br />
out saying in public that they’re positive, it would give it a face that<br />
people could relate to.<br />
I know that people think, “Oh, it’s not going to aff ect me, I’m<br />
not close to that, I don’t know anybody who’s positive” and I’m fi nding<br />
more that when I tell individuals I’m positive, they say, “Wow!<br />
I never thought I’d know anybody who was HIV-positive.” It turns<br />
their attitude towards the whole thing around, just because they’ve<br />
never been close to anybody who’s positive before. It’s just not out<br />
<strong>Positively</strong> <strong>Aware</strong><br />
45
there like, say, a cancer campaign. I think<br />
it would really change things if individuals<br />
could start seeing people who are in their<br />
neighborhoods, in their social circles, who<br />
are talking about being positive.<br />
SS: Of the times that you’ve disclosed<br />
your status, have you found people to be<br />
sympathetic or judgmental?<br />
ET: For the most part, individuals I’ve<br />
disclosed to are sympathetic—they’re positive<br />
reactions, I should say. I’ve only had<br />
one bad reaction to it and it wasn’t horrible,<br />
more like, “Uh, I’ve never really dealt with<br />
that and I don’t want to deal with it.” And<br />
I was like, “Okay, that’s fine. If you ever<br />
want to talk about it, you can call me.” But<br />
for the most part, I’ve been lucky to have<br />
good people who want to learn more and<br />
I haven’t been rejected because of it. I was<br />
very surprised that they weren’t afraid and<br />
they just wanted to learn more and once<br />
they did, they were very accepting of it.<br />
Learn, Learn, Learn<br />
SS: What advice would you give to a woman who had just been<br />
diagnosed?<br />
ET: I would advise her to first learn about how healthy she is and<br />
what she needs to do to stay that way. I would definitely advise her<br />
to get a therapist immediately—even if she didn’t think she needed<br />
one. When you’re battling HIV, in my opinion, you automatically<br />
get a mental health diagnosis, because it’s such a life-changing<br />
thing. So I would advise her to get a therapist, work on her health,<br />
and just put her priorities in order as to what’s most important to<br />
her and what’s going to make her happy, now and in the future.<br />
When you’re positive, you have to stay as healthy as possible, which<br />
includes eliminating lots of stress and things in your life that don’t<br />
need to be there. I would advise her to learn as much as she could<br />
about the virus and the medications she’s taking, if she’s taking any,<br />
and go from there.<br />
SS: I know you’re a graduate of TEAM (Treatment, Education,<br />
Advocacy, Management, here at Test Positive <strong>Aware</strong> Network)—did<br />
you find that helpful in your own learning process?<br />
ET: Yes, it was very helpful. Actually, TEAM was the first class I<br />
took about the virus and it taught me so much and opened up a lot<br />
of avenues for me to research other stuff. It also showed me that I<br />
didn’t know as much as I thought I did! I thought that just by talking<br />
with my doctor, I knew everything there was to know, but once<br />
I went through TEAM, I was like, “Wow! I didn’t know about any<br />
of this stuff!” I wasn’t really communicating with other people who<br />
were HIV-positive and I didn’t know about a lot of the other stuff<br />
that comes along with being positive. So when I came to TEAM,<br />
and started hearing about everyone else’s experiences, it helped me<br />
see that my situation wasn’t so bad compared to what some people<br />
“No matter what<br />
a person looks<br />
like, acts like, or<br />
is doing, don’t<br />
judge them,<br />
because you<br />
never know what<br />
they’re going<br />
through.”<br />
went through. TEAM opened my eyes to a lot of new things, new<br />
information. It humbled me in the sense that I now know there will<br />
always be something new to learn about and it’s always changing.<br />
So TEAM was great for me.<br />
SS: How has being positive changed your life in a negative way?<br />
ET: That I have to take medications. Before I found out I was<br />
positive, I never took any kind of medication. I really never got<br />
sick! Now I have this extra thing that I have to do automatically, so<br />
that’s hard.<br />
SS: And how has it changed your life in a positive way?<br />
ET: It has made me very non-judgmental of pretty much everything.<br />
I have my own personal philosophy—no matter what a<br />
person looks like, acts like, or is doing, don’t judge them, because<br />
you never know what they’re going through. That has helped me<br />
become good at the work that I do—counseling people and helping<br />
them to figure out what they’re going through.<br />
It’s also helped me to see life in a diff erent way—no one’s guaranteed<br />
to be here tomorrow, so you might as well be happy today. I<br />
try my best not to stress out anymore and if I fi nd myself tensing<br />
up, I release it, because I know stress is not good for anybody. Every<br />
night when I go to bed, I refl ect back on my day to see what I’ve<br />
learned, because I want to learn something new every day. If I made<br />
a mistake, I want to learn from that mistake so I don’t make it again,<br />
because I really don’t have time to make mistakes that are going to<br />
stress me out. It’s helped me be happier and more productive and<br />
that’s refl ected by my children, which is a good thing. Something<br />
happens, we just roll with the punches. I try to teach them, “Don’t<br />
worry about it, we’ll get through it.” We try to have as much fun<br />
and laughter as we can, love each other as much as we can, because,<br />
again, you can be here today and gone tomorrow. So it just opened<br />
46 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
my eyes to the whole what-life-is-about thing and about what I<br />
should be doing while I’m here on earth.<br />
Parenting<br />
SS: You mentioned children and I can’t imagine what it would be<br />
like dealing with this illness and being a mother at the same time.<br />
I think a lot of women who are HIV-positive have struggled with<br />
that. Do you have any parenting secrets?<br />
ET: Again, it’s about making life as normal as possible. My secret<br />
is pretty much just trying to stay happy and deal with things as<br />
they come along and not stress about them, because once something<br />
happens, it’s just the process of how you deal with it, your<br />
outlook on it, as to how it turns out. And the kids—we sit down and<br />
talk about everything. As a matter of fact, I have two biological kids<br />
and five foster kids and five of the seven are teenagers. My mother<br />
says I’m crazy! It’s sort of fun, though—they keep me young, even<br />
though they make me grow grey hairs! And they all know—every<br />
time I get a foster kid, I make sure we sit down and have “the talk.”<br />
I explain to them about being positive. I explain to them, “You’re<br />
going to see me taking this medication every night, so I want you to<br />
know what I’m doing, why I’m taking it.” And it serves as a preventive<br />
for them—I have this, you could get it, please protect yourself.<br />
SS: That’s what I was going to ask next—do you think they have<br />
an awareness of applying your lesson to their own lives?<br />
ET: A few of them do and a few of them are still bumpin’ along,<br />
but we have open conversations. I tell them to be as honest as possible<br />
with me and that way, we can deal with whatever comes up<br />
and we can prevent a lot of things. I didn’t used to be that kind of<br />
mother before—but now, I know that if someone had talked to me<br />
when I was a teenager, if someone had sat down and let me be as<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
honest with them as I want my kids to be with me, I possibly would<br />
not have become HIV-positive. I didn’t have a hard childhood, but<br />
sex was never talked about, drugs were never talked about—those<br />
things were just not dealt with. I couldn’t bring it up because they<br />
wouldn’t want to talk about it. So applying that to my own parenting<br />
skills has allowed me to make it easier for the kids to come<br />
and talk to me—that way, if something is going on or they need<br />
some advice, I can give it to them and prevent them from getting<br />
on drugs or getting pregnant or getting somebody pregnant. My<br />
centerpiece on my dining room table is a big bucket of condoms!<br />
I know they all have sex, except the little ones, and I say, “I prefer<br />
you not to do it, but if you’re going to do it, at least protect yourself.”<br />
Because once the kids are out of the house, you can’t control<br />
what they do, so I would rather keep them protected than not. I tell<br />
them when I get sick, it’s because my immune system isn’t doing so<br />
well and I say, “I love to go to parties, but I can’t party like I used<br />
to because it’s stressful on my system. You don’t ever want to get<br />
something that’s going to compromise your immune system.” They<br />
ask me questions, they bring their friends over to talk to me—I<br />
don’t know how well their parents like that, but I’m just trying to<br />
keep the kids from getting something that they shouldn’t. And all<br />
that, the honesty and parenting skills, I wouldn’t have any of that<br />
if I hadn’t become HIV-positive, because I wouldn’t have known, I<br />
wouldn’t have learned about emotions and things like that. So all<br />
of those things have been beneficial for me.<br />
Ideas for Improvement<br />
SS: Is there anything about how this country is dealing with HIV/<br />
AIDS that you’d like to see change or improve?<br />
ET: I should first say that things could be worse—the services<br />
that positive individuals receive are exceptional services and there<br />
are a lot of services out there, at least in the city, that people can utilize.<br />
But if there was something the nation could do better, I’d say<br />
it would be to make it equal for all cities, all states. And of course,<br />
give more money to it. There are a lot of programs out here that<br />
work and if they had the money to expand, they would. I think the<br />
president and his administration should look at some of these programs<br />
and make them nationwide, because I think they would work<br />
for prevention and for treatment and care. A lot of HIV treatments<br />
and services are on the cutting edge of things that could work for<br />
individuals with other chronic illnesses. If they could make some of<br />
those programs universal, I think that would help a lot with health<br />
care.<br />
And, of course, if we could get rid of the stigma, make our messages<br />
more popular and get people, positive and negative, to talk<br />
about it more oft en on a regular basis, do more national education<br />
on it for everybody, I think those things would help a lot, and help<br />
it stop spreading.<br />
It remains to be seen how President Obama and Congress will<br />
change our health care syst em and the way HIV/AIDS is dealt with<br />
in this country. In the meantime, having people like Evany Turk willingly<br />
st anding in her truth; leading by example and act ively helping<br />
others who are HIV-positive; and raising her children to know that<br />
honest y is good and knowledge is power, may be one of the most eff ective<br />
ways we have of battling this disease. e<br />
<strong>Positively</strong> <strong>Aware</strong><br />
47
Reaching Out<br />
to Our Sisters<br />
Chicago women’s<br />
conference offers<br />
knowledge and support<br />
by Enid Vázquez<br />
As this issue geared up to go to press,<br />
the Chicago Women’s AIDS Project<br />
(CWAP) and one of the local<br />
branches of the national Women’s Interagency<br />
HIV Study (WIHS), located at the<br />
CORE Center, held their second annual<br />
conference for their clients and patients,<br />
called Reaching Out to Our Sisters. It was<br />
a chance for women to gather together in<br />
support and to learn more about HIV.<br />
The event included workshops on<br />
depression, living your best life, recovery,<br />
spirituality, aging, and supporting transgender<br />
women. Th e workshop “Writing<br />
Your Story” was conducted by the Chicagobased<br />
activist/literary duo AquaMoon (visit<br />
www.spokenexistence.com).<br />
Gathered together in the auditorium,<br />
the approximately 200 women in attendance<br />
listened (and told their own stories)<br />
as Dr. Mardge Cohen, principle investigator<br />
of the Chicago WIHS, discussed the<br />
powerful case for HIV medications, listed<br />
the negative statistics for women (especially<br />
black women), and addressed the need to<br />
“reach out to our sisters.”<br />
Dr. Cohen said that women made up<br />
8% of U.S. AIDS cases in the late 1980s, but<br />
today they make up 27%. 83% of women<br />
become infected through heterosexual sex<br />
and 16% through drug use; however, the<br />
sexual activity is sometimes with drugusing<br />
men, so drugs aren’t completely out of<br />
the picture, she noted. Black women make<br />
up 66% of all AIDS cases in women, but<br />
only 14% of the U.S. population.<br />
“So women are doing worse, and black<br />
women are doing worse,” said Dr. Cohen.<br />
“One of the ways we measure worse is mortality—people<br />
die.”<br />
According to June 2007 statistics from<br />
the U.S. Centers for Disease Control and<br />
Prevention (CDC), increases in persons<br />
dying of HIV/AIDS were seen in three different<br />
groups: women, black people, and<br />
individuals over the age of 45.<br />
Moreover, a black woman is 13 to 20<br />
times more likely to die of HIV/AIDS than<br />
a white woman. Black men are also more<br />
likely to die compared to white men. And<br />
older black women are 20 times more likely<br />
to die.<br />
Yet, there were places in the U.S. where<br />
the death rate was the same between races.<br />
“Why the diff erence?” asked Dr. Cohen.<br />
“Lack of insurance. Lack of trust—not<br />
treated equally.” She noted lack of treatment<br />
access in general. Th is has been called<br />
“poor HAART diff usion.” (HAART stands<br />
for “highly active antiretroviral therapy,” or<br />
HIV treatment.)<br />
“Th e data’s in… by and large, if you take<br />
HAART, you don’t progress to AIDS, you<br />
don’t die [of AIDS-related causes],” said Dr.<br />
Cohen. “It’s not negotiable. We want your<br />
T-cells to go up and your viral load to go<br />
down.”<br />
Now that newer HIV drugs are easier<br />
to take and therapy is more successful,<br />
other causes of death are taking on a greater<br />
importance in the U.S. epidemic.<br />
“People are dying of non-AIDS related<br />
things,” Dr. Cohen explained. “Th ere are<br />
other issues that are very important, like<br />
liver disease, heart disease, and cancers—<br />
smoking, which we could do something<br />
about. It’s very important to know your<br />
hepatitis status. Get your Pap test. Stop<br />
smoking.”<br />
Smoking doesn’t just lead to lung cancer,<br />
she said. “In spite of the emphysema,<br />
despite the dysfunction of the arteries that<br />
leads to heart disease, it also hurts your HIV.<br />
Your viral load doesn’t respond as well.”<br />
She pointed out the success story of<br />
pregnancy in HIV. Th anks to HIV testing<br />
and treatment during pregnancy, transmission<br />
from mother to child has virtually<br />
been eliminated in the United States. “We<br />
have to tell our daughters, there’s trust and<br />
there’s lack of trust, but we can take control<br />
of our health.”<br />
“HIV defi nes the fault lines that divide<br />
our society,” she concluded. “We need to<br />
make access totally decent and available<br />
to everyone. Tell other women. Reach out<br />
to your sisters—that’s the name and the<br />
message of the conference. HIV meds are<br />
important, so make the clinic work for you<br />
and make them work for everyone.” e<br />
48 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
Doctors Urge<br />
the Government<br />
to Keep Up with<br />
Medical Progress<br />
HIV policy and funding left in the dust<br />
of treatment success<br />
by Enid Vázquez<br />
What an era. Tolerable and easy-to-take medications can<br />
stop HIV in its tracks. Th is prevents AIDS. It prevents<br />
new infections. It saves mega-bucks.<br />
And so, say a group of medical providers, it’s time for this<br />
country to catch up with the reality of medical progress. It’s time<br />
for Medicaid and Medicare, as well as private insurers, to pay for<br />
HIV testing and thereby catch infections early. It’s time for earlier<br />
treatment, which is much less expensive than later treatment.<br />
Th is could not only save money and protect health, but also avoid<br />
spreading of the virus by those who don’t know they’re infected.<br />
Instead, what doctors see to this day is large numbers of<br />
patients come in suff ering from advanced infection when that could<br />
have been easily prevented. At this stage treatment is not only more<br />
expensive, but also less successful.<br />
Without coverage for HIV testing, poor people, and anyone<br />
else with fi nancial diffi culties, will not be able to aff ord the $60 or<br />
more it costs to pay for the test, and doctors can’t order it knowing<br />
that their clinic won’t be reimbursed.<br />
“Can the Red Ribbon survive red tape?” the doctors asked.<br />
And, they added, it’s time for the federal government to pay for<br />
proven prevention strategies like needle exchange, and stop wasting<br />
it on abstinence-only education, which has been proven to be<br />
ineff ective.<br />
Following are remarks made during a media teleconference by<br />
representatives of the two groups that issued the policy statement,<br />
the American College of Physicians (ACP) and the HIV Medicine<br />
Association (HIVMA), which is part of the Infectious Diseases<br />
Society of America (IDSA).<br />
Michael S. Saag, M.D.<br />
“Th e background of [our policy statement] is that there’s been<br />
incredible progress in the care of HIV patients. It was a disease<br />
that wasn’t known in 1980, fi rst described in 1981, had no therapies<br />
available at all until 1987, and was virtually a universal death<br />
sentence for almost everyone who was infected with HIV through<br />
the 1980s.<br />
“It emerged in the 1990s with a revolution in therapies, now up<br />
to 32 individual medications that are available and on the market<br />
for use and that, especially when used in combination, are able to<br />
halt the virus in its tracks—stop its replication.<br />
“What that translates into is an ability for people who are HIVpositive<br />
today to live near-normal lifespans based on these inter-<br />
<strong>Positively</strong> <strong>Aware</strong><br />
49
Early identifi cation is<br />
only going to come about<br />
through routine screening.<br />
ventions, and that type of progress was really unimaginable when<br />
most of us started working in this fi eld in the 1980s.<br />
“So what’s happened is that this progress has moved forward<br />
very rapidly, but a lot of the public policy that we’re using today to<br />
manage this epidemic in the United States were policies that were<br />
established in the late 1980s and early 1990s, and have not really<br />
been re-visited in a serious way since that time.<br />
“We know this virus is transmitted person-to-person, either<br />
through sexual activity, through sharing of blood through needles,<br />
or through pregnancy from mother to child. We basically<br />
stopped transmission from mother to child simply by doing prenatal<br />
screening of the mom to see if she’s HIV-positive while she’s<br />
being followed by her obstetrician. If she’s found to be HIV-positive<br />
through this universal opt-out testing, she gets treated, her virus<br />
goes to undetectable levels, and when she delivers, under those circumstances,<br />
there is no transmission of HIV from mother to child,<br />
whereas untreated that transmission rate would be about 25%, or<br />
one in four.<br />
“Th e problem today, though, is that that same concept needs to<br />
be applied to the entire population. Th e reason I say that is because…<br />
we are pretty much fi nding most of our patients when they’ve been<br />
infected for 10 to 12 years and they start getting sick due to the<br />
impact of the virus, and then they show up in our emergency room<br />
sick. We get them into care at that point, but the success of the<br />
therapy is diminished when people show up late.<br />
“And during that entire time while the virus was replicating<br />
in them, if they are having contact with somebody and exposing<br />
someone to the virus, it’s possible that that virus can be transmit-<br />
ted. Whereas if that person is on therapy,<br />
and their virus is reduced to undetectable<br />
levels, the risk of transmission from person<br />
to person is markedly reduced.<br />
“Briefl y, some data that can support this<br />
whole concept can be found at our clinic,<br />
where we follow, annually, the median<br />
of what’s called the CD4 count of people<br />
when they show up to clinic. CD4 count<br />
normally in an uninfected person is 500 to<br />
1,500. When somebody has advanced HIV<br />
it’s below 200.<br />
“The median CD4 count of people<br />
showing up at our clinic over the last<br />
decade is around 200, so that means half of<br />
our patients are showing up late.<br />
“Th e one exception to that is a group of<br />
patients who show up with a CD4 count of<br />
around 400 or so, and those are pregnant<br />
women. Why? Because of opt-out testing,<br />
being found when they have less advanced<br />
disease. Th ey get on treatment, they can live to a near-normal<br />
lifespan, take care of their child, not have a child who’s infected,<br />
everything’s better.<br />
“So what we need to do is implement a policy of opt-out testing<br />
that was recommended by the CDC two years ago, but to really<br />
make that happen, not just talk about it but implement it, so that the<br />
public health improves and the health of the individual improves.”<br />
Michael S. Saag, M.D., is a professor of medicine at the University<br />
of Alabama and chair of Infect ious Diseases at UAB. He is the<br />
HIVMA chair elect .<br />
Jeffrey Harris, M.D.<br />
“Last December the ACP and the HIVMA issued a guidance<br />
statement recommending that routine screening should begin. Th e<br />
CDC issued a similar recommendation, in September 2006. But<br />
federal funding and reimbursement lagged far behind.<br />
“It’s our understanding that the Centers for Medicaid and Medicare<br />
Services, the CMS, is now considering covering HIV testing,<br />
but limiting it to high-risk patients. What we would recommend<br />
to the CMS is that they expand this policy for routine screening<br />
to cover all Medicare benefi ciaries, that they also encourage the<br />
coverage and screening of the Medicaid population, and that they<br />
provide adequate funding. Th e screening could take place in community<br />
health centers, Federal Bureau of Prisons, and the Department<br />
of Veteran Aff airs.<br />
50 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
“We also believe that part of this evolving<br />
health reform debate should address<br />
the issue of expanding routine screening<br />
for HIV. Th is proposal is driven by the reality<br />
of funding. Th e cost of routine screening<br />
plus the cost of treating those who are<br />
detected earlier is simply less than the cost<br />
of treating those who present at a more<br />
advanced stage when they are immunecompromised.<br />
“Currently, it was suggested that about<br />
40% of those people who are turning out to<br />
be HIV-positive arrive at a time when they<br />
are already immune-compromised and<br />
thus much more ill. Th ere are data to suggest<br />
that when the CD4 cell count is greater<br />
than 350 when diagnosed, the cost of treating<br />
that individual is demonstrated to be<br />
$13,885.<br />
“In contrast, when a CD4 count is less<br />
than 50, the cost of treating that patient at<br />
that juncture is $36,533 annually.<br />
“Th us early identifi cation is only going to come about through<br />
routine screening. And this is only going to be possible if we can<br />
persuade federal programs and private insurers to embark upon a<br />
much broader screening program.”<br />
Jeff rey Harris, M.D., is president of the ACP.<br />
Kathleen E. Squires, M.D.<br />
“Th e ACP and the HIVMA has taken the position that it’s really<br />
time to support evidence-based prevention. We really do know what<br />
transmits HIV. So we do have evidence-based prevention strategies<br />
for the two major transmission factors, which are sexual activity<br />
as well as the use of intravenous drugs and things like exchanging<br />
needles and so forth.<br />
“Over the past several years, a major emphasis on the part of the<br />
federal government in terms of looking at prevention strategies is<br />
to fund abstinence-only education instead of supporting comprehensive<br />
sex education. Th is is despite the fact that there have been<br />
now numerous studies that really document that abstinence-only<br />
education is not eff ective.<br />
“If you look at federal spending on this issue since 1996, the<br />
federal government has spent more than 1.5 billion dollars on<br />
abstinence-only education. In the year 2009, Congress continues<br />
to spend about $99 million on abstinence-only education eff orts.<br />
[In the latest budget from President Obama, this $99 million has<br />
been cut from abstinence-only programs.]<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
The federal government<br />
really doesn’t support<br />
needle exchange programs<br />
despite numerous studies<br />
that demonstrate that<br />
these programs are very<br />
highly effective.<br />
“In terms of looking at the issue of intravenous drug use, the<br />
federal government really doesn’t support needle exchange programs<br />
despite numerous studies that demonstrate that these programs<br />
are very highly eff ective at reducing HIV and hepatitis C<br />
transmission, and do not increase drug use in the people who are<br />
participating in these exchange programs.<br />
“Th e other thing that we need to think about at the global level<br />
is that we are exporting ideological prevention strategies like the<br />
use of abstinence-only eff orts to other countries where it’s really<br />
important for us to employ all of the tools that have been proven to<br />
be eff ective at reducing transmission of HIV.<br />
“Now, this year and just last week [week of April 13th], the<br />
White House and the CDC announced a very important campaign,<br />
$45 million and a fi ve-year new communication campaign to<br />
raise awareness about the domestic HIV epidemic and specifi cally<br />
addressing the impact of HIV in African American people in this<br />
country. Th is campaign is one component of a broader HIV prevention<br />
strategy, but it’s really critical to increase funding across the<br />
range of tools that have been shown to be eff ective.”<br />
Kathleen E. Squires, M.D., is HIVMA vice-chair and direct or of<br />
infect ious disease at Jeff erson Medical College and associate professor<br />
of medicine at University Hosp ital in Philadelphia.<br />
“HIV Policy: Th e Path Forward” was published in the April 17<br />
Clinical Infect ious Diseases. Read the text and list of recommendations<br />
at www.hivma.org. e<br />
<strong>Positively</strong> <strong>Aware</strong><br />
51
What’s Goin’ On?<br />
I<br />
recently accepted a position as Project<br />
Director for a research study designed to<br />
assess the initial acceptability and feasibility<br />
of a pre-exposure prophylaxis (PrEP)<br />
trial among young men who have sex with<br />
men (YMSM) in Chicago.<br />
The concept of PrEP, in a nutshell,<br />
involves administering medications used in<br />
the treatment of HIV (particularly Viread<br />
or Truvada at this point) to “high risk” HIVnegative<br />
individuals, in hopes of preventing<br />
transmission of the virus. Several PrEP trials<br />
are currently underway across the globe,<br />
many of which will likely demonstrate the<br />
Prepping for a PrEP trial<br />
Critical observations before the study even begins<br />
by Keith R. Green<br />
effi cacy of both Viread and Truvada as biomedical<br />
interventions for the prevention of<br />
HIV.<br />
Th ough young men who have sex with<br />
men, particularly those of color, continue to<br />
contract HIV at alarming rates, these cur-<br />
I asked him how<br />
he addressed<br />
homosexuality<br />
during his church<br />
prevention work.<br />
His response made<br />
my head spin.<br />
52<br />
<strong>Positively</strong> <strong>Aware</strong><br />
rent trials ironically have very few young<br />
men enrolled in them. Th erefore, if in fact<br />
these studies are able to prove the eff ectiveness<br />
of PrEP, we will know very little about<br />
its implementation within the population<br />
that could benefi t most from this technology.<br />
Th e PrEP study that I am involved with<br />
seeks to provide some insight into this.<br />
For this study, we will attempt to<br />
recruit 99 YMSM between the ages of 18<br />
and 22, and to follow them over the course<br />
of two years.<br />
Th ere are three separate arms in the<br />
study. All participants will go through an<br />
intensive evidence-based behavioral intervention<br />
and then be randomized to one of<br />
three groups. One group will receive oncedaily<br />
Truvada, another group will receive<br />
a placebo (or sugar pill), and yet another<br />
group will receive nothing. Participants will<br />
be regularly monitored for HIV serocon<strong>version</strong>,<br />
behavioral disinhibition (getting buck<br />
wild sexually because they feel that they are<br />
protected by PrEP), and any adverse eff ects<br />
(among a host of other things).<br />
<strong>Aware</strong> of my search to hire research<br />
assistants who will largely be responsible<br />
for recruiting and retaining participants, a<br />
close friend recommended a friend of his for<br />
one of the positions. Trusting the judgment<br />
of my friend, I followed up on his recommendation<br />
and called his friend to arrange<br />
an interview.<br />
I didn’t expect him to be knowledgeable<br />
about PrEP. Th e average person wouldn’t<br />
be. His sexual orientation and racial identity<br />
were also of no concern to me. I simply<br />
needed him to be able to connect to<br />
the population that we have committed to<br />
engage in order to recruit and retain them<br />
in the study.<br />
I asked him what kind of experience<br />
he had with HIV prevention, and he mentioned<br />
that he had done some work within<br />
his church. Knowing that he was African<br />
American, and curious about the position<br />
that his church takes on homosexuality, I<br />
asked him how he addressed this when it<br />
came up during his prevention work there.<br />
His response made my head spin.<br />
He told me that he does not condone<br />
homosexuality, but that he doesn’t knock<br />
anybody for their choice. He said that<br />
everybody has to answer to God for their<br />
own sins, and that all he can do is help to<br />
steer people in the right direction.<br />
PA • July / August 2009 • tpan.com • positivelyaware.com<br />
Photo © Russell McGonagle
As taken aback as I was by this response,<br />
that wasn’t actually the part that did me<br />
in. Unfortunately, I’ve come to expect this<br />
type of mentality from people who make<br />
an eff ort to do HIV prevention work in the<br />
church (though I must point out that I have<br />
been pleasantly surprised at times). What<br />
got me was that while telling me about<br />
this friend of his who might be a good fi t<br />
for this position, my friend who’d recommended<br />
him inadvertently told me that he<br />
was somebody he “got down with every now<br />
and then.” Of course, I didn’t mention that<br />
during our conversation, but listening to<br />
him dissociate himself from his own sexual<br />
behaviors made me sick to my stomach.<br />
Th ere was no way in hell I could trust<br />
him with the potentially vulnerable members<br />
of the population that our study intends<br />
to enroll. To do so would be like throwing<br />
the whole “do no harm” clause of ethical<br />
research out the door. Th e young people<br />
Get<br />
<strong>Positively</strong><br />
<strong>Aware</strong>!<br />
J/A 2009<br />
Mail to:<br />
<strong>Positively</strong> <strong>Aware</strong><br />
5537 N. Broadway<br />
Chicago, IL 60640<br />
who choose to participate in this study<br />
deserve to have someone working with<br />
them who will support and encourage them<br />
to lead healthier lives—physically, mentally,<br />
and spiritually. I immediately thanked him<br />
for his interest, but assured him that he was<br />
not the man for this job. I then called my<br />
friend back and chewed him out for wasting<br />
my time by not screening this guy before<br />
giving me his number, but also to thank<br />
him for helping me to put some things into<br />
perspective.<br />
Could this mentality be partially to<br />
blame for why the existing PrEP studies<br />
(and many other types of studies related<br />
to HIV for that matter) lack participation<br />
from young people, and young people of<br />
color specifi cally? We continue to hear that<br />
people are more likely to become engaged<br />
in research and services if they feel that they<br />
have some connection to the researcher or<br />
service provider. But just because a provider<br />
❑ Subscribe: 1 year of <strong>Positively</strong> <strong>Aware</strong> for $30.*<br />
❑ Subscription renewal: My payment of $30 is enclosed.<br />
❑ Back issues: Please send me the following back issue(s) at $3 per copy:<br />
❍ Jan/Feb 2009 Qty. _____________❍ Mar/Apr 2009 Qty. _____________<br />
❍ May/Jun 2009 Qty. _____________❍ Jul/Aug 2008 Qty. _____________<br />
❍ Sep/Oct 2008 Qty. _____________❍ Nov/Dec 2008 Qty. _____________<br />
*Subscriptions are mailed free of charge to those who are HIV-positive.<br />
looks like you and may even engage in some<br />
of the same behaviors as you do, it doesn’t<br />
necessarily equate to a connection between<br />
the two of you. And, even if it does, there<br />
is no guarantee that such a connection will<br />
be a healthy one. Th at person’s negative or<br />
judgmental feelings about themselves and<br />
their own behaviors will most certainly<br />
have a negative impact on you, especially if<br />
you are already vulnerable.<br />
Th is observation is not one that will<br />
be included in the results of our study,<br />
because it deviates from the objectives that<br />
we have set out to measure. However, it has<br />
everything to do with the implementation<br />
of PrEP as an acceptable and feasible HIV<br />
prevention intervention among young men<br />
who have sex with men. We talk a lot about<br />
cultural sensitivity and inclusiveness within<br />
research and prevention, but self-awareness<br />
and radical acceptance are oft en careless<br />
whispers. e<br />
❑ Donation: *<br />
❑ $25 ❑ $50 ❑ $100<br />
❑ $250 ❑ $500 ❑ $__________<br />
Thank you for your donation. Your<br />
contribution helps to provide subscriptions<br />
to people who cannot<br />
afford them. All donations are<br />
tax-deductible to the full extent<br />
allowed by law.<br />
NAME: ____________________________________________________________________________________________________________________________________________________________________<br />
ADDRESS: ______________________________________________________________________________________________________________________________________________________________<br />
CITY: __________________________________________________________________ STATE: __________________________________________________ZIP: ____________________________<br />
PHONE: ______________________________________________________________ E-MAIL: _____________________________________________________________________________________<br />
CHARGE MY: ❑ VISA ❑ MASTERCARD ❑ AMERICAN EXPRESS TOTAL $ ________________________<br />
CARD NUMBER: ___________________________________________________________________________________ EXPIRES: _______________________________________________<br />
NAME ON CARD: __________________________________________________________SIGNATURE (REQUIRED): ____________________________________________<br />
Charges will appear on your credit card bill as TPA Network<br />
❑ Please send us bulk copies of <strong>Positively</strong> <strong>Aware</strong> at no charge (donation requested - U.S. and Canada only)<br />
_____________________________ Number of copies of each issue via U.P.S. (No P.O. Box)<br />
Test Positive <strong>Aware</strong> Network (TPAN) is a not-for-profit organization dedicated to providing support and information to all people impacted by HIV.<br />
PA • July / August 2009 • tpan.com • positivelyaware.com 53<br />
<strong>Positively</strong> <strong>Aware</strong>
PA Online<br />
This Issue’s Poll<br />
Stay Current with<br />
PA E-mail Updates<br />
Sign-up today for our <strong>Positively</strong> <strong>Aware</strong><br />
e-mail newsletter and receive regular<br />
updates on HIV treatment news and<br />
information.<br />
Visit www.tpan.com or www.positivelyaware.com<br />
and click on Subscribe.<br />
Once you receive a confi rmation e-mail,<br />
you can update your TPAN profi le to<br />
include “<strong>Positively</strong> <strong>Aware</strong> Updates.”<br />
join us on MySpace at<br />
www.myspace.com/positivelyaware<br />
Add us as your friend and<br />
check out our community partners.<br />
Join us in our online community forum<br />
The online community forum allows users to post and discuss topics, in a safe<br />
and non-judgmental environment with other individuals who share similar<br />
interests. It features several chat rooms, including The Women’s Forum, The<br />
Men’s Locker Room, SmartSex Talk, and the newly added Drug Guide section<br />
(where you can share your experience with diff erent drugs, side eff ects, and<br />
drug interactions).<br />
The staff of TPAN and PA regularly monitor the activity of the various chat<br />
rooms within the community forum, and are available to answer any specifi c<br />
questions users may have, as well as to provide technical support.<br />
You can also view exclusive online newsbriefs at www.positivelyaware.com, and<br />
stay in the know by subscribing to our bi-weekly PA E-mail Update.<br />
This Issue’s Question<br />
Since testing HIV positive,<br />
have you ever contracted another<br />
STI (sexually transmitted infection)?<br />
May/June 2009<br />
poll results<br />
What do you think is<br />
the most important<br />
issue for women<br />
regarding HIV?<br />
Vote at<br />
www.positivelyaware.com<br />
The 2008 PA index of articles<br />
is now available online at<br />
www.positivelyaware.com.<br />
Comments<br />
• Finding a mate<br />
• I just was diagnosed in 2007<br />
when I was expecting my fi rst<br />
baby. I wonder if I’ll have the<br />
chance to have more babies<br />
now that I am in this condition.<br />
• Reproductive issues<br />
• Emotional support<br />
54 PA • July / August 2009 • tpan.com • positivelyaware.com<br />
<strong>Positively</strong> <strong>Aware</strong>
AIDS Run & Walk Chicago 2009<br />
Saturday, October 3, 2009<br />
Grant Park, Chicago<br />
aidsrunwalk.org<br />
Top Fundraiser can win two round-trip<br />
tickets to Europe on American Airlines!<br />
Check out all of the fundraising incentives<br />
& sign up to run or walk at aidsrunwalk.org<br />
Photography by Mark Wiens
Abbott<br />
Ad<br />
Page<br />
Here