?Who's the Boss is Not a Food!?
?Who's the Boss is Not a Food!?
?Who's the Boss is Not a Food!?
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
“Who Who’s s <strong>the</strong> <strong>Boss</strong>” <strong>Boss</strong> <strong>is</strong><br />
<strong>Not</strong> a <strong>Food</strong>!<br />
Kyle Lamphier<br />
Morning Report<br />
June 12, 2006
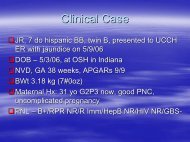
Case:<br />
11yo male comes to <strong>the</strong> ED with a chief<br />
complaint of “cough cough” x 3-4 3 4 days<br />
Evaluated in Triage:<br />
VS: 36.8 PMH—denies<br />
PMH denies<br />
96 24 106/68 96%O2<br />
Current meds—denies<br />
meds denies<br />
NKDA<br />
35kg<br />
Sent to Fast Track
HPI:<br />
Quality of cough? Productive?<br />
Varies with time of day?<br />
Any sick contacts?<br />
Fever?<br />
URI sx? sx<br />
H/o environmental allergies?<br />
Exacerbating/Alleviating factors?<br />
Seasonal component?
Past h<strong>is</strong>tory:<br />
PMH—uncomplicated PMH uncomplicated pregnancy/perinatal<br />
pregnancy/ perinatal<br />
course; denies previous admits<br />
IMM UTD (by report), NKDA, no PMD, has been<br />
taking OTC cough suppressant without effect<br />
FamHx—no<br />
FamHx no h/o cough, bronchit<strong>is</strong>, asthma,<br />
seasonal allergies, TB<br />
SocHx—LAHW SocHx LAHW mom, younger bro<strong>the</strong>r<br />
(healthy), no smoking at home, no pets, no<br />
dust/mice/cockroaches, 6 th grade, good<br />
student<br />
Anything else you can or should ask?
PEx<br />
VS—as VS as per Triage, RR still low 20’s 20<br />
GEN— GEN “Looks Looks good” good<br />
PULM— PULM<br />
WOB—no WOB no rtx, rtx,<br />
no heavy breathing, unable to count<br />
to 10 without taking breaths between numbers<br />
Auscultation—minimal Auscultation minimal to no air movement in all<br />
fields, more dimin<strong>is</strong>hed at <strong>the</strong> bases, occassional<br />
scattered wheezes throughout, coughs with deep<br />
breathing<br />
Rest—WNL Rest WNL (with one small exception that’s that s<br />
d<strong>is</strong>covered only later)
Now what?<br />
Send to OBS<br />
Put on monitor— monitor<br />
HR 120s, pulse-ox pulse ox 91%<br />
Nebs<br />
PIV<br />
What else might you do?
Fur<strong>the</strong>r H<strong>is</strong>tory:<br />
Upon more specific questioning, Mom<br />
says that he has a cough that comes on<br />
maybe 2x/year associated with URIs. URIs.<br />
It<br />
lasts about a week and <strong>the</strong>n goes away<br />
on its own<br />
SUMMARY:<br />
11yo male with apparently new onset<br />
cough/wheeze + and underlying h/o cough<br />
associated with URIs
DDx: DDx:<br />
many things can cause acute cough…. cough<br />
Pulm— Pulm<br />
Cough variant asthma<br />
Foreign body<br />
Post-nasal Post nasal drip<br />
Environmental allergies<br />
O<strong>the</strong>r— O<strong>the</strong>r<br />
Meds<br />
Psychogenic (acute on<br />
chronic)<br />
Chemical exposures<br />
ID— ID<br />
Bacterial Pneumonia<br />
URI<br />
Pertuss<strong>is</strong><br />
TB<br />
Viral pneumonit<strong>is</strong><br />
Atypical pneumonia<br />
Fungal/parasitic process<br />
GI— GI<br />
GERD<br />
Aspiration
Fur<strong>the</strong>r evaluation:<br />
CXR—increased<br />
CXR increased perihilar markings,<br />
hyperinflation, no focal opacities, no<br />
o<strong>the</strong>r abnormalities<br />
CBC—9.2/14.3/41.8/278 CBC 9.2/14.3/41.8/278 N35/B0/L51<br />
BMP—141/3.2/104/20/17/0.8/109/9.0<br />
BMP 141/3.2/104/20/17/0.8/109/9.0
Re-evaluation Re evaluation of <strong>the</strong> pt. after<br />
1 hour of continuous nebs:<br />
Auscultation—better Auscultation better air movement at apices,<br />
still dimin<strong>is</strong>hed at bases, more pronounced<br />
wheezing, still coughs with deep breathing<br />
WOB—RR WOB RR 25, still with some difficulty counting<br />
to 10, o<strong>the</strong>rw<strong>is</strong>e “looks looks good” good<br />
Pulse ox—93% ox 93%<br />
RN—asks RN asks if he’s he s also a diabetic; she points out<br />
a strange odor on h<strong>is</strong> breath…<br />
breath
The The Family Family Guy Guy<br />
Lo<strong>is</strong>: Lo<strong>is</strong>:<br />
It's geat <strong>the</strong>y picked your<br />
<strong>the</strong>me, but <strong>is</strong>n't it a little esoteric?<br />
Peter: Peter:<br />
Esoteric?<br />
(Zoom in to <strong>the</strong> guys in Peter's<br />
brain)<br />
Guy1: Could it mean sexy?<br />
<br />
Guy2: I think it's a science term.<br />
Guy3: Guy3:<br />
Fellas, Fellas,<br />
fellas! fellas!<br />
Esoteric<br />
means delicious!<br />
(back to <strong>the</strong> real world)<br />
Peter: Peter:<br />
Lo<strong>is</strong>, "<strong>Who's</strong> <strong>the</strong> <strong>Boss</strong>" <strong>is</strong><br />
not a food.<br />
Brian (<strong>the</strong> dog): dog) : Swing and a<br />
m<strong>is</strong>s.
“Who Who’s s <strong>the</strong> <strong>Boss</strong>” <strong>Boss</strong> <strong>is</strong> not a<br />
food . . .<br />
. . . Something you might expect to hear from<br />
someone abusing chemical inhalants
Introduction<br />
Volatile substances—hydrocarbons,<br />
substances hydrocarbons,<br />
substituted hydrocarbons, nitrites—that<br />
nitrites that<br />
produce effects via direct inhalation<br />
Often <strong>the</strong> first drugs of abuse by children<br />
and adolescents because <strong>the</strong>y are<br />
inexpensive, hard to detect, and easily<br />
obtainable
Epidemiology<br />
Data from 2003 Youth R<strong>is</strong>k Behavior Surveillance<br />
Survey (YRBSS) shows that 12% of students have<br />
used inhalants during <strong>the</strong>ir lifetime, and that 4% were<br />
using <strong>the</strong>m currently (within <strong>the</strong> last 30 days)<br />
Data from Po<strong>is</strong>on Control Centers shows that ¾ of<br />
users were male<br />
O<strong>the</strong>r user character<strong>is</strong>tics: lower perceived self-worth, self worth,<br />
lower SES, comorbidities with conduct d<strong>is</strong>orders and<br />
drug/ETOH dependence
Techniques<br />
Sniffing—container<br />
Sniffing container<br />
with an inhalant held<br />
to nose<br />
Huffing—a Huffing a cloth<br />
saturated with an<br />
inhalant held over<br />
nose and mouth<br />
Bagging—a Bagging a bag<br />
containing an<br />
inhalant held to nose<br />
and mouth
Mechan<strong>is</strong>m of Action<br />
Enter blood stream through <strong>the</strong> lungs and<br />
diffuse throughout body; highly lipid soluble— soluble<br />
neurons very susceptible<br />
Effects take place within seconds and can last<br />
up to 45 minutes; intoxication maintained<br />
through repeated use<br />
Metabol<strong>is</strong>m—depending Metabol<strong>is</strong>m depending on <strong>the</strong> substance<br />
inhaled, can be excreted through <strong>the</strong> lungs,<br />
liver, and/or kidneys
Clinical manifestations<br />
Clues to use—chemical use chemical odors on breath,<br />
chemical stains on face or clothing,<br />
empty solvent containers, used bags or<br />
rags<br />
Euphoria—inhalants Euphoria inhalants are CNS<br />
depressants; depressants;<br />
initially cause intoxication<br />
similar to ETOH or marijuana followed by<br />
sleepiness, decreased RR and HR,<br />
impaired judgment and coordination
Systemic Effects<br />
Depends on <strong>the</strong> substance used . . .<br />
Pulmonary<br />
Hypoxia<br />
Asphyxia (if bagging) bagging<br />
Chemical pnuemonit<strong>is</strong><br />
Surfactant dysfunction<br />
Pulmonary edema<br />
RAD similar to asthma<br />
CV<br />
Dysrhythmias<br />
Myocardit<strong>is</strong><br />
MI<br />
Sensitization of myocardium to<br />
catecholamines<br />
Bradycardia<br />
Tachycardia<br />
Hypotension<br />
CNS<br />
Slurred speech<br />
Ataxia<br />
D<strong>is</strong>orientation<br />
Headache<br />
Hallucinations<br />
Agitation or aggresivness<br />
SZ<br />
Peripheral neuropathies<br />
Depression of respiratory centers<br />
of <strong>the</strong> brain causing respiratory<br />
arrest<br />
GI<br />
N/V<br />
Hepatotoxicity<br />
Renal<br />
Metabolic acidos<strong>is</strong> (K+ wasting)<br />
Calculi<br />
glomerulonephrit<strong>is</strong>
Potential Causes of Death<br />
Asphyxia from bagging<br />
Suffocation from bagging or from oxygen<br />
d<strong>is</strong>placement via inhaled substance<br />
Choking on vomitus<br />
Careless or dangerous behavior<br />
“Sudden Sudden sniffing death” death<br />
Thought to be caused by cardiac arrhythmia<br />
from myocardium overly sensitized to<br />
catecholamines
Evaluation<br />
Again, depends on <strong>the</strong> inhalant . . .<br />
EKG and cardiac monitoring<br />
Pulse oximetry<br />
Drug screen<br />
CBC, CMP, UA<br />
Me<strong>the</strong>moglobin levels if nitrites<br />
suspected<br />
BLL if gasoline suspected<br />
CXR
Management<br />
Largely supportive<br />
Acute illness<br />
Supplemental O2<br />
If arrythmias present, be careful of using catecholamines due<br />
to <strong>the</strong> sensitized myocardium<br />
If me<strong>the</strong>moglobin, me<strong>the</strong>moglobin,<br />
<strong>the</strong>n high dose O2 or IV methylene blue<br />
If lead toxicity, chelation <strong>the</strong>rapy<br />
Call Po<strong>is</strong>on Control!<br />
Clearance of <strong>the</strong> substance depends on its half-life half life and<br />
how it’s it s metabolized<br />
Chronic effects may be reversible once <strong>the</strong> pt.<br />
becomes drug free
Long Term Management<br />
Formal detoxification if indicated<br />
Possible referral to a treatment center<br />
No good data comparing which types of<br />
treatment programs may be effective
Back to our pt . . .<br />
It’s It s presumed that he may have had an underlying<br />
component of undiagnosed cough-variant cough variant asthma that<br />
in th<strong>is</strong> case was triggered by inhalant abuse<br />
Particular substance inhaled <strong>is</strong> unknown<br />
He was asked in private whe<strong>the</strong>r or not he was abusing<br />
inhalants, and he denied it<br />
He was admitted for respiratory d<strong>is</strong>tress and treated for<br />
h<strong>is</strong> apparent asthma exacerbation. Of note, he did<br />
appear to continue to respond to typical asthma<br />
management<br />
Social work was consulted, and he continued to deny<br />
using inhalants<br />
Upon d<strong>is</strong>charge he was given a PMD appointment, and<br />
it’s it s unknown whe<strong>the</strong>r or not he followed up
References<br />
Endom, Endom,<br />
EE., MD. Inhalant Abuse in Children and<br />
Adolescents. UpToDate, UpToDate,<br />
2006.<br />
Dinwiddie, SH. Abuse of inhalants: A review.<br />
Addiction 1994; 89:925.<br />
Kurtzman, Kurtzman,<br />
TL, Otsuka, Otsuka,<br />
KIN, Wahl, RA. Inhalant abuse<br />
by adolescents. J Adolesc Health. 2001; 28:170.<br />
Grunbaum, Grunbaum,<br />
JA, Kann, Kann,<br />
L, Kinchen, Kinchen,<br />
S. et al. Youth r<strong>is</strong>k<br />
behavior surveillance—United surveillance United States, 2003. MMWR<br />
Surveill Summ 2004; 53:1.<br />
Neumark, Neumark,<br />
YD,Delva, YD,Delva,<br />
J, Anthony, JC. The<br />
epidemiology of adolescent inhalant drug involvement.<br />
Arch Pediatr Adlosec Med 1998; 152:781.