Kevin King MD UT Southwestern Medical Center Division of ...
Kevin King MD UT Southwestern Medical Center Division of ...
Kevin King MD UT Southwestern Medical Center Division of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
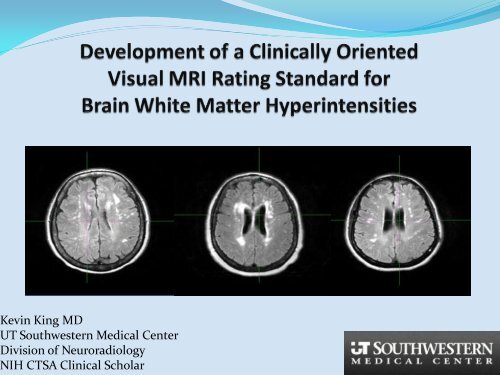
<strong>Kevin</strong> <strong>King</strong> <strong>MD</strong><br />
<strong>UT</strong> <strong>Southwestern</strong> <strong>Medical</strong> <strong>Center</strong><br />
<strong>Division</strong> <strong>of</strong> Neuroradiology<br />
NIH CTSA Clinical Scholar
Normal Impairment<br />
WMH
White Matter Hyperintensities are biomarkers <strong>of</strong><br />
preventable cerebral microvascular disease & predict risk<br />
for cognitive and motor impairment, stroke and death<br />
Debette S, Markus HS. The clinical importance <strong>of</strong> white matter hyperintensities on brain magnetic resonance<br />
imaging: Systematic review and meta-analysis. BMJ. 2010.341:c3666
Vascular pathology is likely involved in a majority <strong>of</strong><br />
clinically significant cases <strong>of</strong> dementia, lowering the<br />
threshold for development <strong>of</strong> Alzheimers Dementia<br />
Black, S., F. Gao, and J. Bilbao, Understanding white matter disease: imaging-pathological correlations in vascular<br />
cognitive impairment. Stroke, 2009. 40(3 Suppl): p. S48-52.
Normal Impairment
Without an accepted grading system, the near ubiquity <strong>of</strong><br />
WMH in older populations causes the finding to be<br />
ignored by most clinicians and is a source <strong>of</strong> unnecessary<br />
concern for many patients.
Fazekas<br />
An Ideal Clinical Screening Scale:<br />
Benefits:<br />
Simple: Easy to incorporate into practise<br />
Predictive <strong>of</strong> clinical outcomes<br />
Areas <strong>of</strong> concern:<br />
Rating <strong>of</strong> Deep vs. Periventricular<br />
Reproducibility
Original Fazekas WMH Scale<br />
Grade Descriptor Deep WMH Periventricular WMH<br />
0 Absent None None<br />
1 Mild Punctate Pencil Thin Lining<br />
2 Moderate Near Confluent Smooth Halo<br />
3 Severe Confluent Irregular band extending<br />
into the deep white matter<br />
Fazekas F, et al. MR signal abnormalities at 1.5 t in alzheimer's dementia and normal aging. Am. J. Roentgenol.<br />
1987;149:351-356
Fazekas outcome correlations<br />
equivalento to volumetry and<br />
more complex scales<br />
Scale Gait (SPPB) Cognition (MMSE)<br />
Fazekas- Gouw* -0.19 -0.13<br />
Scheltens -0.21 -0.13<br />
Volumetry -0.22 -0.10<br />
* included objective measurement criteria:<br />
mild 2cm.<br />
Gouw AA, et al. LADIS Study Group. Simple versus complex assessment <strong>of</strong> white matter hyperintensities in relation<br />
to physical performance and cognition: the LADIS study. J Neurol. 2006 Sep;253(9):1189-96. Sep 22.
Research insights on rating<br />
Periventricular Vs. Deep
Irregular Periventricular WMH<br />
demonstrated = pathologic changes<br />
as Severe Deep WMH<br />
Fazekas, et al. revision<br />
Grade Descriptor Deep WMH Periventricular WMH<br />
0 Absent Absent Absent<br />
1 Mild Punctate Pencil Thin Lining<br />
2 Moderate Near Confluent Smooth Halo<br />
3 Severe Confluent DWMH equivalent to Irregular PVWMH<br />
Fazekas F, et al. Pathologic correlates <strong>of</strong> incidental mri white matter signal hyperintensities. Neurology. 1993;43:1683-<br />
1689.
Periventricular & Deep WMH<br />
3D analysis by De Carli et al suggested identification <strong>of</strong><br />
periventricular vs. deep in 2D axial images is arbitrary-<br />
on sagittal and coronal ‘deep’ lesions <strong>of</strong>ten contact the<br />
ventricle<br />
C. DeCarli, et al. Anatomical Mapping <strong>of</strong> White Matter Hyperintensities (WMH): Exploring the Relationships<br />
Between Periventricular WMH, Deep WMH, and Total WMH Burden. Stroke, January 1, 2005; 36(1): 50 - 55.
Periventricular & Deep WMH<br />
Spatial analysis failed to identify distinct<br />
populations with Deep versus Periventricular<br />
disease.<br />
PVWMH and DWMH correlate highly with each<br />
other and with total WMH burden<br />
C. DeCarli, et al. Anatomical Mapping <strong>of</strong> White Matter Hyperintensities (WMH): Exploring the Relationships<br />
Between Periventricular WMH, Deep WMH, and Total WMH Burden. Stroke, January 1, 2005; 36(1): 50 - 55.
Questioned Reproducibility<br />
Inter-rater reliability for Fazekas<br />
Variable among studies ranging from poor to excellent,<br />
kappa <strong>of</strong> .43 to .78<br />
May be higher in studies with more advanced WMH due<br />
to a ceiling effect<br />
? Increased by objective criteria such as in Gouw: not<br />
assessed for inter-rater reliability<br />
Scheltens, P., et al., White matter changes on CT and MRI: an overview <strong>of</strong> visual rating scales. European<br />
Task Force on Age-Related White Matter Changes. Eur Neurol, 1998. 39(2): p. 80-9.
Gouw Modification <strong>of</strong> Fazekas<br />
Gouw et al. revision<br />
Grade Descriptor Deep WMH Periventricular WMH<br />
0 Absent Absent Not explicitly described.<br />
1 Mild Single lesions < 10mm<br />
Grouped ≤ 20mm<br />
2 Moderate Single lesions 10-20mm<br />
Grouped >20mm<br />
3 Severe Single/ Confluent lesions<br />
>20mm<br />
Gouw AA, et al. Simple versus complex assessment <strong>of</strong> white matter hyperintensities in relation to physical<br />
performance and cognition: The ladis study. J Neurol. 2006;253:1189-1196
Proposed Clinical Scale<br />
Grade Descriptor Deep WMH Periventricular WMH*<br />
0 Absent All foci
Evaluation <strong>of</strong> New Method<br />
Subset <strong>of</strong> the Dallas Heart Study,<br />
a multi-ethnic community based study<br />
Age 50.7+9.7<br />
Hispanic 15%<br />
NonHisp Black 44%<br />
NonHisp<br />
White 38%<br />
Other Race 2%<br />
Female 52%
3T Images,<br />
Achieva Philips <strong>Medical</strong> Systems<br />
FLAIR<br />
3D MP RAGE
Initial Evaluation<br />
Test set <strong>of</strong> 52 studies demonstrating a range <strong>of</strong> WMH<br />
volumes independently read by two reviewers<br />
Evaluation <strong>of</strong> discordant reads demonstrated poor<br />
agreement in categorization <strong>of</strong> small hyperintense foci<br />
Revision<br />
Established 3mm size threshold, reviewed 40 random<br />
studies<br />
Agreement for grading <strong>of</strong> no versus mild disease was<br />
72.4% (kappa 0.44 SE 0.17) without the threshold<br />
compared with 89.2% with the rule (kappa 0.76 SE 0.11)<br />
with p= 0.055.
Overall Reproducibility<br />
For initial test group enriched for large WMH volumes<br />
Agreement <strong>of</strong> 67% (kappa=0.71) n=52<br />
For random community sample with overall small<br />
WMH volumes (with 3mm threshold)<br />
Agreement <strong>of</strong> 87.5% (kappa = 0.76) n=40
Comparison with WMH Volumes<br />
WMH scores from 559 participants showed<br />
significant correlation with automated<br />
volumes (spearman rho 0.57, p
Conclusion<br />
We report the development <strong>of</strong> a visual WMH scoring<br />
system suited for use in clinical practice.<br />
Grade<br />
0<br />
Descriptor<br />
Absent<br />
Deep WMH<br />
All foci
DHS Brain Study Group<br />
Ronald M. Peshock <strong>MD</strong> 1,2<br />
Keith M. Hulsey MS 1<br />
Lea Alhilali <strong>MD</strong> 3<br />
Roderick W. McColl PhD 1<br />
Myron Weiner 4<br />
Anthony R. Whittemore <strong>MD</strong> PhD 1<br />
Departments <strong>of</strong> 1 Radiology, 2 Internal Medicine, and 4 Neurology<br />
The University <strong>of</strong> Texas <strong>Southwestern</strong> <strong>Medical</strong> <strong>Center</strong><br />
Department <strong>of</strong> 3 Radiology<br />
University <strong>of</strong> Pittsburgh <strong>Medical</strong> <strong>Center</strong>
Regular progression <strong>of</strong> WMH<br />
Magnetic resonance abnormalities and cardiovascular disease in older adults. The Cardiovascular Health Study.<br />
Manolio TA, Bryan RN, et al. Stroke. 1994 Feb;25(2):318-27.
Age Related White Matter Changes<br />
Score: A variant <strong>of</strong> Fazekas<br />
Grade Descriptor<br />
0 No lesions (including symmetrical, well-defined caps or bands)<br />
1 Focal lesions, ≥5 mm<br />
2 Beginning confluence <strong>of</strong> lesions<br />
3 Diffuse involvement <strong>of</strong> the entire region<br />
• Frontal, Parieto-Occipital, Temporal, Infratentorial & Basal Ganglia scored<br />
separately for each hemisphere<br />
• Periventricular and Deep scored Jointly<br />
ARWMC Scale: A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke<br />
2001;32:1318–1322. Wahlund LO, Barkh<strong>of</strong> F, Fazekas F, Scheltens P. et al on behalf <strong>of</strong> the European Task Force on Age-<br />
Related White Matter Changes
Fazekas has good correlation with<br />
WMH volumetry<br />
Scale<br />
Agreement with<br />
Volumetry<br />
(Kendall W)<br />
Fazekas- Schmidt* 0.57<br />
Scheltens 0.48<br />
Manolio 0.37<br />
* included category for number <strong>of</strong> lesions with 0 for no lesions, 1 for 1 to 4<br />
lesions, 2 for 5 to 9 lesions, and 3 for >9 lesions.<br />
Kapeller Pet al. Visual rating <strong>of</strong> age-related white matter changes on magnetic resonance imaging: scale comparison,<br />
interrater agreement, and correlations with quantitative measurements. Stroke. 2003 Feb;34(2):441-5.
Among the Many Systems developed:<br />
Which to choose?<br />
Mäntylä R, et al.Variable agreement between visual rating scales for white matter hyperintensities on MRI. Stroke.<br />
1997 Aug;28(8):1614-23.