stage IIIA
stage IIIA
stage IIIA
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Corso Integrato di Clinica Medica<br />
ONCOLOGIA MEDICA<br />
AA 2010 - 2011<br />
LUNG CANCER. IV.<br />
THERAPY. I.<br />
NON SMALL CELL LUNG CANCER<br />
Prof. Alberto Riccardi
TREATMENT OF LUNG CARCINOMA<br />
* overall treatment approach to pts with LC<br />
formulated after:<br />
- histologic diagnosis, and<br />
- anatomic and physiologic staging;<br />
* pts encouraged to stop smoking (those<br />
who do fare better than those continuing to<br />
smoke)
SUMMARY<br />
OF TREATMENT APPROACH
NON SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach. I.<br />
Stages IA, IB, IIA, IIB and some <strong>IIIA</strong><br />
* Stages IA, IB, IIA, and IIB → surgical resection;<br />
- Stage IB: discussion of risk / benefits of adjuvant CT<br />
(not routinely given);<br />
- Stage II: adjuvant CT;<br />
- potential curative RT for "nonoperable" pts;<br />
* <strong>stage</strong> <strong>IIIA</strong> with "minimal N2 involvement” (discovered at<br />
thoracotomy or mediastinoscopy) → surgical resection<br />
with complete mediastinal lymph node dissection (also<br />
consideration of neoadjuvant CT) ;<br />
- postoperative RT for pts with N2 disease (if no<br />
neoadjuvant CT given)
NON SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach. II.<br />
Stage <strong>IIIA</strong> with selected types of <strong>stage</strong> T3<br />
* tumors with chest wall invasion (T3) = en bloc<br />
resection of tumor with involved chest wall (± post -<br />
operative RT);<br />
- superior sulcus (Pancoast's, T3) tumors = preoperative<br />
RT (30 - 45 Gy) → en bloc resection of involved lung and<br />
chest wall (± postoperative RT or intraoperative<br />
brachytherapy);<br />
* proximal airway involvement (< 2 cm from carina, T3)<br />
without mediastinal nodes = sleeve resection (preserving<br />
distal normal lung) or pneumonectomy
NON SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach. III.<br />
Stages <strong>IIIA</strong> "advanced, bulky, clinically evident<br />
N2" (discovered preoperatively)<br />
and IIIB disease includible in tolerable RT port<br />
* potential curative RT + CT (with reasonable good PS<br />
and general medical condition);<br />
- RT alone (if otherwise);<br />
* consider neoadjuvant CT and surgical resection for<br />
<strong>IIIA</strong> disease with advanced N2 involvement
NON SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach. IV.<br />
Stage IIIB with carinal invasion (T4) but no N2 involvement<br />
* consider pneumonectomy with tracheal sleeve<br />
resection with direct reanastomosis to contralateral<br />
mainstem bronchus
NON SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach. IV.<br />
Stage IIIB with carinal invasion (T4) but no N2 involvement<br />
* consider<br />
pneumonectomy<br />
with tracheal sleeve<br />
resection with direct<br />
reanastomosis to<br />
contralateral<br />
mainstem bronchus<br />
* carinal reconstruction with moderate amount of airway resected →<br />
trachea anastomosed end to end with either right or left mainstem<br />
bronchus, with the contralateral bronchus reimplanted into side of<br />
trachea (upper right diagram = more commonly used technique)
NON SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach. V.<br />
More advanced <strong>stage</strong> IIIB and <strong>stage</strong> IV disease<br />
* RT to symptomatic local sites;<br />
* CT for ambulatory pts (consider CT, cetuximab and<br />
bevacizumab for selected pts);<br />
* chest tube drainage of large malignant pleural<br />
effusions;<br />
* consider resection of primary tumor and isolated brain<br />
or adrenal metastases
* limited <strong>stage</strong> (good performance status) = combination<br />
CT + chest RT;<br />
* extensive <strong>stage</strong> (good performance status) =<br />
combination CT;<br />
- complete responders (all <strong>stage</strong>s): prophylactic cranial<br />
RT;<br />
* poor - performance - status pts (all <strong>stage</strong>s):<br />
- modified - dose combination CT;<br />
- palliative RT<br />
SMALL CELL LUNG CARCINOMA<br />
Summary of treatment approach
* palliative radiotherapy for brain metastases, spinal cord<br />
compression, weight - bearing lytic bony lesions,<br />
symptomatic local lesions (nerve paralyses, obstructed<br />
airway, hemoptysis not responding to CT);<br />
* appropriate diagnosis and treatment of other medical<br />
problems and supportive care;<br />
* encouragement to stop smoking;<br />
* entrance into clinical trial<br />
LUNG CARCINOMA<br />
All pts
TREATMENT BY STAGE<br />
OF NON SMALL CELL LUNG<br />
CARCINOMA
TREATMENT BY STAGE<br />
OF NON SMALL CELL LUNG<br />
CARCINOMA<br />
LOCALIZED<br />
OR LOCALLY ADVANCED DISEASE<br />
(STAGES I, II and nonbulky <strong>IIIA</strong>)
STAGES I - II
STAGE I
STAGE I (T1a - b, N0, M0)<br />
* T1 = ≤ 3 cm in greatest dimension, surrounded by lung or<br />
visceral pleura, without bronchoscopic evidence of<br />
invasion more proximal than lobar bronchus (i.e., not in<br />
main bronchus):<br />
- T1a = ≤ 2 cm in greatest dimension;<br />
- T1b = > 2 - ≤ 3 cm in greatest dimension
STAGE I NON - SMALL CELL LUNG CANCER<br />
* <strong>stage</strong> IA = T ≤ 2 cm surrounded by lung or visceral pleura, without<br />
bronchoscopic evidence of invasion more proximal than lobar bronchus<br />
(i.e., not in main bronchus); N0; M0;<br />
* <strong>stage</strong> IB = - T > 2 - ≤ 3 cm + as for <strong>stage</strong> IA
STAGE II
STAGE IIA. I. T1a - T1b, N1, M0<br />
* T1a, N1, M0 : T1a = < 2 cm, surrounded by lung or<br />
visceral pleura, without bronchoscopic evidence of<br />
invasion more proximal than lobar bronchus (i.e., not in<br />
main bronchus); N1 (metastasis to ipsilateral peribronchial<br />
and / or ipsilateral hilar lymph nodes, and intrapulmonary<br />
nodes involved by direct extension of primary tumor); M0<br />
* T1b, N1, M0: T1b = > 2 - ≤ 3 cm + as above; N1; M0
STAGE IIA. II. (T2a, N1, M0; T2b, N0, M0)<br />
* T2a, N1, M0: T2a = > 3 - ≤ 5 cm or with any of following<br />
features: involves main bronchus ≥ 2 cm distal to carina;<br />
invades visceral pleura (PL1 or PL2); associated with<br />
atelectasis or obstructive pneumonitis extended to hilar<br />
region but not involving entire lung; N1 (metastasis to<br />
ipsilateral peribronchial and / or ipsilateral hilar lymph<br />
nodes, and intrapulmonary nodes involved by direct<br />
extension of primary tumor); M0<br />
* T2b, N0, M0: T2b = > 5 - ≤ 7 cm + as above; N0; M0
STAGE IIA (T1a - T1b, N1, M0; T2a, N1, M0; T2b, N0, M0)
STAGE IIB (T2b, N1, M0; T3, N0, M0)<br />
* T2b, N1, M0: T2b = > 5 - ≤ 7 cm or with any of following:<br />
involves main bronchus; ≥ 2 cm distal to carina; invades<br />
visceral pleura (PL1 or PL2); associated with atelectasis or<br />
obstructive pneumonitis not involving entire lung; N1<br />
(metastasis to ipsilateral peribronchial and / or ipsilateral<br />
hilar lymph nodes, and intrapulmonary nodes involved by<br />
direct extension of primary tumor); M0<br />
* T3, N0, M0: T3 = > 7 cm or directly invading any of following:<br />
parietal pleural (PL3), chest wall (including superior sulcus<br />
tumors), diaphragm, phrenic nerve, mediastinal pleura or<br />
parietal pericardium; tumor in main bronchus (< 2 cm from<br />
carina but without involvement of carina); associated<br />
atelectasis or obstructive pneumonitis of entire lung or<br />
separate tumor nodules in same lobe; N0; M0
STAGE IIB (T2b, N1, M0; T3, N0, M0)
STAGE II NON - SMALL CELL LUNG CANCER<br />
*e.g., <strong>stage</strong> IIA = T1b,<br />
N1, M0: T1b = > 2 - ≤ 3<br />
cm; N1 (metastasis to<br />
ipsilateral peribronchial<br />
and / or ipsilateral<br />
hilar lymph nodes);<br />
M0);<br />
* e.g., <strong>stage</strong> IIB = T3,<br />
N0, M0: T3 = > 7 cm or<br />
directly invading any of<br />
following: parietal<br />
pleural / chest wall (a),<br />
diaphragm (b), phrenic<br />
nerve, mediastinal<br />
pleura (c) or parietal<br />
pericardium (d); tumor<br />
in main bronchus (< 2<br />
cm from carina but<br />
without involvement of<br />
carina) (e);<br />
associated atelectasis or obstructive pneumonitis of<br />
entire lung or separate tumor nodules in same lobe; N0;<br />
M0
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. I. Surgery<br />
* pulmonary resection (pneunomectomy, lobectomy or<br />
segmental, wedge or sleeve resection) = treatment of<br />
choice for pts who can tolerate operation;<br />
- with complete resection possible, 5 - yr survival for N0<br />
disease ~ 60 - 80% (depending on size of tumor) and ~ 50%<br />
for N1 disease (hilar node involvement);<br />
* adjuvant chemotherapy after curative surgery for Stage II<br />
disease;<br />
- clinical trials of radiation therapy after curative surgery<br />
for Stage II disease
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. II. Surgery<br />
* extent of resection = surgical judgment based on<br />
findings at exploration;<br />
- in general, conservative resection encompassing<br />
all known tumor → survival = that obtained with more<br />
extensive procedures;<br />
- → lobectomy preferred to pneumonectomy [and to<br />
wedge resections and segmentectomies (↑ rate of<br />
local relapse)]
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. III. Surgery<br />
* pneumonectomy reserved for pts with tumors<br />
involving multiple lobes (T3A) or very central tumors and<br />
only be performed in pts with excellent pulmonary<br />
reserve;<br />
- in addition, pts undergoing right - sided<br />
pneumonectomy after induction chemotherapy and<br />
radiation therapy → high mortality rate = be carefully<br />
selected before surgery;<br />
- wedge resection and segmentectomy (potentially by<br />
video assisted thoracic surgery, VATS) reserved for pts<br />
with poor pulmonary reserve and small peripheral lesions
RIGHT PNEUMONECTOMY
RIGHT PNEUMONECTOMY
RIGHT LOBECTOMY
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. IV. Surgery<br />
Lobectomy vs limited resection<br />
* ↓ in local recurrence for pts treated with lobectomy compared with<br />
pts treated with limited excision<br />
but no significant difference in overall survival<br />
(Ginsberg RJ & Rubinstein LV Ann Thorac Surg 95)
* from Cochrane Collaboration<br />
group review, including 11<br />
randomized trials of 1.910 pts who<br />
underwent surgical interventions for<br />
early <strong>stage</strong> (I - <strong>IIIA</strong>) NSCLC, 4 - yr<br />
survival superior in pts with<br />
resectable <strong>stage</strong> I - <strong>IIIA</strong> who<br />
underwent resection and “Complete<br />
ipsilateral Mediastinal Lymph Node<br />
Dissection” (CMLND) compared with<br />
those who underwent resection and<br />
lymph node sampling (3 hilar + 3<br />
mediastinal nodes) (p = .005)<br />
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. V. Surgery<br />
Surgery for localized disease (<strong>stage</strong>s I - IIIa)<br />
* disease - free survival with lymph node sampling vs systematic<br />
sampling (CMLND) (Gajra A et al JCO 21; 1029, 2003)
WEDGE RESECTION OF LUNG CANCER<br />
* part of lung lobe containing cancer<br />
and small amount of healthy tissue around removed
WEDGE RESECTION OF<br />
LUNG CANCER<br />
* wedge resections and<br />
segmentectomies, potentially<br />
by VATS (Video - Assisted<br />
Thoracic Surgery via<br />
thoracoscopy, not usually<br />
used for curative LC resection)<br />
for pts with poor pulmonary<br />
reserve and small peripheral<br />
lesions
VIDEO - ASSISTED THORACIC SURGERY<br />
- video - assisted thoracic surgery (VATS) via<br />
thoracoscopy not usually used for curative lung cancer<br />
resection, but useful for peripheral lung nodules in pts<br />
with <strong>stage</strong> I disease and poor lung function;<br />
- VATS advocated to ↓ postoperative impairment of lung<br />
function, pain, length of hospital stay and recovery time<br />
(but randomized, controlled trials not confirm advantages)<br />
→ open thoracotomy still preferred surgical approach to<br />
curative resection of lung cancer
VIDEO - ASSISTED THORACIC SURGERY<br />
* for peripheral lung nodules in<br />
pts with <strong>stage</strong> I disease and poor<br />
lung function
VIDEO - ASSISTED THORACIC SURGERY<br />
* also used for diagnostic purposes<br />
to examine pleural surface and cavity<br />
and biopsy peripheral lung nodules or<br />
accessible mediastinal nodes (and to<br />
drain and treat large malignant<br />
effusions)
OVERALL OUTCOME OF SURGERY IN NSCLC. I.<br />
(STAGES I, II and nonbulky <strong>IIIA</strong>)<br />
* overall, complete pulmonary resection = treatment of<br />
choice in pts with:<br />
- <strong>stage</strong>s IA, IB, IIA and IIB (T1 - 2, N0 - 1) disease;<br />
- <strong>stage</strong> <strong>IIIA</strong> (T3, N0 - 1 + T1 - 3, N2) with favorable age,<br />
cardiopulmonary function and anatomy (from team<br />
approach, involving pulmonary medicine, thoracic surgery,<br />
medical and radiation oncology);<br />
[- neoadjuvant chemotherapy ± radiotherapy shrinks local<br />
tumor and treats micrometastases → surgical resection<br />
safer and more effective in “selected pts”]
OVERALL OUTCOME OF SURGERY IN NSCLC. II.<br />
(STAGES I, II and nonbulky <strong>IIIA</strong>)<br />
* 43% (43 / 100) of pts with NSCLC undergo<br />
thoracotomy:<br />
- 76% (= 33 / 43 pts): “curative resection”;<br />
- 12%: explored only for disease extent, and<br />
- 12%: palliative procedure with known disease left<br />
behind;<br />
* 30 - day hospital mortality = 3 and 6% for lobectomy<br />
and pneumonectomy, respectively
OVERALL OUTCOME OF SURGERY IN NSCLC. III.<br />
(STAGES I, II and nonbulky <strong>IIIA</strong>)<br />
* overall, ~ 30% of pts (~ 10 / 33 pts) treated with<br />
“curative resection” survive 5 yrs [~ 15% (5 pts)<br />
survive for 10 yrs];<br />
- most pts ultimately die of metastatic disease<br />
(usually within 5 yrs from surgery)
OVERALL OUTCOME OF SURGERY IN NSCLC. IV.<br />
(STAGES I, II and nonbulky <strong>IIIA</strong>)<br />
* for <strong>stage</strong> <strong>IIIA</strong>, 5 - yr survival for N1 and N2 disease = ~<br />
50% and 20%, respectively;<br />
* however, technically resectable only 20% of pts with N2<br />
disease (most pts discovered with N2 disease at<br />
thoracotomy)
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. VI.<br />
Radiotherapy with curative intent<br />
* pts with <strong>stage</strong> I or II disease refusing surgery or not<br />
candidates for pulmonary resection considered for<br />
radiation therapy with curative intent (based on extent of<br />
disease and volume of chest requiring irradiation);<br />
* pts with malignant pleural effusion or cardiac<br />
involvement not candidates for curative radiation<br />
treatment;<br />
- long - term survival for pts with all <strong>stage</strong>s of LC who<br />
receive radiation with curative intent ~ 20%
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. VII.<br />
Radiotherapy with curative intent<br />
* usually midplane doses of 55 - 60 mGy (5500 - 6000<br />
rad, either split course or continuous fraction<br />
radiotherapy);<br />
- major concern: amount of lung parenchyma and<br />
other thoracic organs (spinal cord, heart and<br />
esophagus) included in treatment plan;<br />
* deleterious effects of radiation on pulmonary<br />
function often hampers treatment in pts with major<br />
underlying pulmonary disease
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. VIII.<br />
Radiotherapy with curative intent: side effects<br />
Esophagitis<br />
* most common side<br />
effect of curative thoracic<br />
radiation = acute<br />
radiation esophagitis<br />
during treatment, usually<br />
self - limited
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. IX.<br />
Radiotherapy with curative intent: side effects<br />
* other side effects include fatigue, radiation myelitis<br />
(spinal cord injury may be permanent, but usually<br />
avoided by careful treatment planning) and radiation<br />
pneumonitis (sometimes progressing to pulmonary<br />
fibrosis)
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. X.<br />
Radiotherapy with curative intent: side effects<br />
Radiation pneumonitis<br />
* risk proportional to dose<br />
of radiation and volume of<br />
lung within radiation field;<br />
- full clinical syndrome<br />
(dyspnea, fever, and<br />
radiographic infiltrate<br />
corresponding to treatment<br />
port) in 5% of cases and<br />
treated with glucocorticoids
RADIATION PNEUMONITIS
RADIATION PNEUMONITIS<br />
* CT findings: a) homogeneous<br />
slight increase in attenuation (2 - 4<br />
mos after therapy); b) patchy<br />
consolidation (1 - 12 mos after<br />
therapy); c) non - uniform discrete<br />
consolidation (most common; 3 mos<br />
to 10 yrs after therapy)
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XI.<br />
Radiotherapy with curative intent<br />
* Continuous Hyperfractionated, Accelerated RT<br />
(CHART) = delivery of 36 treatments of 1.5 Gy 3 times /<br />
day for 12 consecutive days (total dose of 54 Gy);<br />
- 2 - yr survival rate > 20 - 30% (with more esophagites);<br />
* brachytherapy (local radiotherapy delivered by placing<br />
radioactive "seeds" in catheter into tumor bed) delivers ↑<br />
local dose with sparing surrounding normal tissue
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XII.<br />
Radiotherapy with curative intent<br />
* beside potentially curative, radiotherapy may<br />
control primary tumor and preventing symptoms<br />
related to local spreading and increase quality and<br />
length of life of non - cured pts
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XIII.<br />
* pts with resected <strong>stage</strong> IA NSCLC receive no other<br />
therapy but are at high risk of recurrence (~ 2 - 3% / yr) or<br />
developing second primary lung cancer → follow these pts<br />
with CT scans for first 5 yrs and consider entering onto<br />
early detection and chemoprevention studies
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XIV. Adjuvant chemotherapy. I.<br />
* meta - analysis of > 4300 pts → trend toward ↑ survival<br />
of ~ 5% at 5 yrs with cisplatin - based adjuvant therapy (p<br />
= .08);<br />
- however, from 3 subsequent randomized studies → no<br />
significant survival advantage despite addition of more<br />
"modern" postoperative adjuvant chemotherapy regimens;<br />
- still however, since then at least 5 additional randomized<br />
trials and two meta - analyses → survival benefit in<br />
response to postoperative adjuvant - based therapy<br />
→ adjuvant chemotherapy now routinely recommended in<br />
NSCLC pts with good performance status and <strong>stage</strong> IIA - B<br />
disease (though with modest beneficial effects)
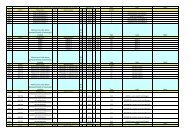
Randomized studies of adjuvant chemotherapy in NSCLC<br />
Study Treatment No. of pts 5-Year<br />
Survival<br />
(%)<br />
ECOG 3590<br />
(II–<strong>IIIA</strong>)<br />
ALPI<br />
(I–<strong>IIIA</strong>)<br />
Big Lung Trial<br />
(I–IIIB)<br />
IALT<br />
(IB–<strong>IIIA</strong>)<br />
UFT<br />
(IA–IB)<br />
Surgery RT<br />
vs. Surgery + post- op concurrent RT + cis / etoposide<br />
Surgery alone<br />
vs. Surgery + post- op mitomycin / vindesine / cisplatin<br />
Surgery alone<br />
vs. Surgery + post- op chemotherapy a<br />
Surgery alone<br />
vs. Surgery + post- op Cis + VP16 / vinca<br />
Surgery alone<br />
vs. Surgery + post- op UFT<br />
CALGB IB (ASCO 06) Surgery alone<br />
vs. Surgery + post- op carbo / paclitaxel<br />
NCI-C<br />
(IB–II)<br />
ANITA<br />
(IB, - <strong>IIIA</strong>)<br />
Surgery alone<br />
vs. Surgery + post- op Cis / vinorelbine<br />
Surgery alone<br />
vs. Surgery + post- op Cis / vinorelbine<br />
242<br />
246<br />
603<br />
606<br />
189<br />
192<br />
405<br />
361<br />
488<br />
469<br />
172<br />
172<br />
241<br />
241<br />
433<br />
407<br />
39%<br />
33%<br />
51%<br />
43%<br />
Median<br />
Survival<br />
39 mos vs.<br />
38 mos<br />
NR 33 mos<br />
34 mos<br />
40%<br />
44.5%<br />
85%<br />
88%<br />
57%<br />
59%<br />
54%<br />
69%<br />
43%<br />
51%<br />
p Value<br />
0.56<br />
NR 0.59<br />
0.90<br />
NR < 0.03<br />
NR 0.04<br />
78 mos<br />
95 mos<br />
73 mos<br />
94 mos<br />
44 mos<br />
66 mos<br />
0.10<br />
0.04<br />
0.017
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XV. Adjuvant chemotherapy. II.<br />
* role of adjuvant chemotherapy for <strong>stage</strong> IB disease<br />
undefined;<br />
- subset analysis of randomized studies → no benefit in<br />
pts with <strong>stage</strong> IB;<br />
- one trial focusing on IB disease and using carboplatin<br />
and paclitaxel (one of most commonly used regimens for<br />
advanced disease) → 20% ↓ in death (ns)<br />
→ pts with <strong>stage</strong> IB (T1b N0, M0) NSCLC not routinely<br />
given adjuvant therapy
Adjuvant chemotherapy<br />
Postoperative UFT (uracil - tegafur) in <strong>stage</strong> I adenocarcinoma<br />
Nakagawa M et al Ann Oncol 16; 75, 2005<br />
* post - operative UFT does not significantly ↑ survival of<br />
pathological <strong>stage</strong> I NSCLC [UFT ↑ survival of pT1 pts (T1a - b, N0,<br />
M0, p = .036), but not of pT2 pts]
Adjuvant chemotherapy. IIter.<br />
Postoperative UFT (uracil - tegafur) in<br />
<strong>stage</strong> I adenocarcinoma<br />
* 999 pts with completely resected T1 - 2<br />
N0M0 adenocarcinoma randomized (1994 -<br />
97) between oral UFT for 2 yrs and no CT;<br />
- 5 - yr OS ↑ in UFT with respect to<br />
control - arm due to greatly ↑ OS of pts<br />
with T2 disease (T2, N0, M0) in UFT arm<br />
(84.9 vs 73.5%) (p = .005) (no # among pts<br />
with T1 disease)<br />
Kato H et al NEJM 2004
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XVI. Neodjuvant chemotherapy<br />
* no evidence of # in overall survival with neo - adjuvant<br />
chemotherapy
TREATMENT BY STAGE. STAGE I - <strong>IIIA</strong> NSCLC. XVIbis.<br />
NEOADJUVANT CHEMOTHERAPY<br />
Preoperative chemotherapy in pts with resectable NSCLC: results of<br />
the MRC LU22 / NVALT 2 / EORTC 08012 multicentre randomised<br />
trial and update of systematic review (International Standard<br />
Randomised Controlled Trial, no. ISRCTN25582437). I.<br />
Gilligan D et al Lancet 2007; 369: 1929<br />
Background: although surgery is best chance of cure for pts with<br />
NSCLC, overall 5 - yr survival modest → improvements;<br />
- in 1990s, from small trials reporting striking results with neo -<br />
adjuvant chemotherapy → randomised trial designed to investigate<br />
whether, in pts with operable NSCLC of any <strong>stage</strong>, outcomes be ↑ by<br />
platinum - based chemotherapy before surgery<br />
Methods: pts randomised to surgery alone (S) or 3 cycles of<br />
platinum - based chemotherapy → surgery (CT - S);<br />
- primary outcome = overall survival, analysed on an intention - to -<br />
treat basis
idem. II.<br />
Gilligan D et al Lancet 2007; 369: 1929<br />
Results. I.: 519 pts randomised (S: 261, CT - S: 258) from 70 centres<br />
in UK, Netherlands, Germany and Belgium (61% = clinical <strong>stage</strong> I,<br />
31% = <strong>stage</strong> II and 7% = <strong>stage</strong> III);<br />
- neo - adjuvant chemotherapy feasible (75% of pts had all 3 cycles<br />
of chemotherapy), resulted in good response rate (49%) and downstaging<br />
in 31% of pts and did not alter type or completeness of<br />
surgery (lobectomy: S : 56%, CT - S: 60%, complete resection: S:<br />
80%, CT - S: 82%), with post - operative complications not ↑ in CT - S<br />
group and no impairment of quality of life
idem. III.<br />
Gilligan D et al Lancet 2007; 369: 1929<br />
- Results. II.: however, no benefit in<br />
overall survival (p = .86)<br />
- Interpretation: no evidence of # in<br />
overall survival with neo - adjuvant<br />
chemotherapy
TREATMENT BY STAGE<br />
STAGES I - II NSCLC. XVII. Adjuvant radiotherapy<br />
* after apparent complete resection, postoperative<br />
adjuvant radiation therapy → not ↑ survival (and actually<br />
detrimental to survival in N0 and N1 disease)
TREATMENT BY STAGE. XVIII.<br />
Superior sulcus or Pancoast tumors. I.<br />
* NSCLC of superior pulmonary sulcus (producing<br />
Pancoast's syndrome) behave # than LC at other sites and<br />
usually treated with combined radiotherapy and surgery
TREATMENT BY STAGE. XIX.<br />
Superior sulcus or Pancoast tumors. II.<br />
* usual preoperative staging procedures (including<br />
mediastinoscopy and CT and PET scans) for tumor extent<br />
and neurologic examination (and sometimes nerve<br />
conduction studies) to document involvement or<br />
impingement of nerves in region;<br />
- with mediastinoscopy negative → curative approaches<br />
be used in treating Pancoast's syndrome despite its<br />
apparent locally invasive nature
TREATMENT BY STAGE. XX.<br />
Superior sulcus or Pancoast tumors. III.<br />
* best results with employing concurrent preoperative<br />
irradiation [30 Gy in 10 treatments] and cisplatin and<br />
etoposide → en bloc resection of tumor and involved chest<br />
wall 3 - 6 wks later (65% of thoracotomy specimens →<br />
complete response or minimal residual microscopic<br />
disease on pathologic evaluation);<br />
- 2 - yr survival = 55% for all eligible pts and = 70% for pts<br />
with complete resection
TREATMENT BY STAGE. XXI.<br />
Superior sulcus or Pancoast tumors. IV.<br />
* as alternatives (as needed from pt conditions):<br />
- radiation therapy alone;<br />
- surgery alone (selected cases);<br />
- clinical trials of combined modality therapy
TREATMENT BY STAGE. XXII.<br />
NSCLC with T3, N0 Disease (Stage IIB)<br />
* subset of T3, N0 disease not presenting as Pancoast<br />
tumor (initially considered <strong>stage</strong> III disease, but with #<br />
natural history and treatment strategy than <strong>stage</strong> III N2<br />
disease) now considered as <strong>stage</strong> IIB;<br />
- pts with peripheral chest wall invasion → resection of<br />
involved ribs and underlying lung (chest wall defects then<br />
repaired with chest wall musculature or Marlex mesh and<br />
methylmethacrylate);<br />
- 5 - yr survival = 35 - 50% (adjuvant chemotherapy usually<br />
recommended)
STAGE III
TREATMENT BY STAGE. XXIII.<br />
STAGE III NSCLC. I.<br />
* treatment of still “locally advanced NSCLC” (with<br />
involvement of mediastinal lymph nodes, N2 - N3) = one of<br />
most controversial issues in management of LC;<br />
- treatment options include local therapy (surgery or<br />
radiation therapy) combined with systemic chemotherapy<br />
to control micrometastases
TREATMENT BY STAGE. XXIV.<br />
STAGE III NSCLC. II.<br />
* interpretation of results clouded by a no. of issues,<br />
including changing diagnostic techniques, variation of<br />
staging systems and # pt populations, with tumors ranging<br />
from “nonbulky <strong>stage</strong> <strong>IIIA</strong>” (clinical N1 nodes, with N2<br />
nodes discovered only at time of surgery, despite negative<br />
mediastinoscopy) to “bulky N2 <strong>stage</strong> <strong>IIIA</strong>” (enlarged<br />
adenopathy clearly visible on chest x - rays or multiple<br />
nodal level involvement) to clearly inoperable “<strong>stage</strong> IIIB<br />
disease”<br />
→ team approach involving pulmonary medicine, thoracic<br />
surgery and medical and radiation oncology essential for<br />
management of these pts
STAGE <strong>IIIA</strong>
STAGE <strong>IIIA</strong>. I. (T1a, N2, M0; T1b, N2, M0)<br />
* T1a, N2, M0: T1a = < 2 cm, surrounded by lung or visceral<br />
pleura, without bronchoscopic evidence of invasion more<br />
proximal than the lobar bronchus (i.e., not in main<br />
bronchus); N2 (metastasis to ipsilateral mediastinal and /<br />
or subcarinal lymph nodes); M0<br />
* T1b, N2, M0: T1b = > 2 - ≤ 3 cm + as above; N2; M0
STAGE <strong>IIIA</strong>. II. T3, N1, M0; T3, N2, M0<br />
* T3, N1, M0: T3 = > 7 cm or directly invading any of<br />
following: parietal pleural (PL3), chest wall (including<br />
superior sulcus tumors), diaphragm, phrenic nerve,<br />
mediastinal pleura or parietal pericardium; tumor in main<br />
bronchus < cm from carina but without involvement of<br />
carina); associated atelectasis or obstructive pneumonitis<br />
of entire lung or separate tumor nodule(s) in same lobe;<br />
N1 (metastasis to ipsilateral peribronchial and / or<br />
ipsilateral hilar lymph nodes, and intrapulmonary nodes<br />
involved by direct extension of primary tumor); M0<br />
* T3, N2, M0: T3 = as above; N2 (metastasis to ipsilateral<br />
mediastinal and / or subcarinal lymph nodes(s); M0
STAGE <strong>IIIA</strong>. IV. (T4, N0, M0; T4, N1, M0)<br />
* T4, N0, M0: T4 = any size invading any of following:<br />
mediastinum, heart, great vessels, trachea, recurrent<br />
laryngeal nerve, esophagus, vertebral body, carina or<br />
separate tumor nodule(s) in different ipsilateral lobe; N0;<br />
M0<br />
* T4, N1, M0: T4 = as above; N1 (metastasis to ipsilateral<br />
peribronchial and / or ipsilateral hilar lymph nodes, and<br />
intrapulmonary nodes involved by direct extension of<br />
primary tumor); M0
STAGE <strong>IIIA</strong><br />
(T1a - T1b, N2, M0; T3, N1 - N2 M0; T4, N0 - N1, M0)
STAGE <strong>IIIA</strong> NON - SMALL CELL LUNG CANCER<br />
* e.g., Stage III A: T3, N1, M0: T3<br />
= > 7 cm or directly invading any<br />
of following: tumor in main<br />
bronchus (< 2 cm from carina but<br />
without involvement of carina) (a);<br />
parietal pleura / chest wall (b);<br />
diaphragm (c); mediastinal pleura<br />
or parietal pericardium (e);<br />
phrenic nerve; associated<br />
atelectasis or obstructive<br />
pneumonitis of entire lung or<br />
separate tumor nodule(s) in same<br />
lobe; N1 (metastasis to ipsilateral<br />
peribronchial and / or ipsilateral<br />
hilar lymph nodes, and<br />
intrapulmonary nodes involved by<br />
direct extension of primary<br />
tumor); M0
TREATMENT BY STAGE. XXV.<br />
STAGE <strong>IIIA</strong> NSCLC. I.<br />
Options<br />
* options:<br />
- resection → postoperative radiation + chemotherapy for<br />
N2 disease;<br />
- neoadjuvant chemotherapy → resection, or<br />
- neoadjuvant chemo - radiotherapy → resection
TREATMENT BY STAGE. XXVI.<br />
Stage <strong>IIIA</strong> (N2 disease) NSCLC. II.<br />
Surgery<br />
* surgery for Stage <strong>IIIA</strong> (N2 disease) controversial;<br />
- for pts with N2 disease with "minimal<br />
disease" (involvement of only 1 node with microscopic foci,<br />
usually discovered at thoracotomy or mediastinoscopy)<br />
and ? for more common pts with "advanced bulky<br />
disease” (preoperatively obvious on CT scan);<br />
[- pts with incidental finding of N2 disease at time of<br />
resection need adjuvant chemotherapy]
TREATMENT BY STAGE. XXVII.<br />
STAGE II - <strong>IIIA</strong> NSCLC. III.<br />
ADJUVANT CHEMOTHERAPY<br />
* overall, possible, modest ↑ survival with<br />
adjuvant chemotherapy after apparently complete<br />
resection
TREATMENT BY STAGE. XXVIII.<br />
STAGE I - <strong>IIIA</strong> NSCLC. IV. ADJUVANT THERAPY<br />
Cisplatin - based adjuvant CT in resected <strong>stage</strong> I - <strong>IIIA</strong> LC<br />
* 1867 radically operated pts (36%<br />
<strong>stage</strong> I, 25% <strong>stage</strong> II, 39% <strong>stage</strong> <strong>IIIA</strong>)<br />
randomized between receiving or not<br />
receiving adjuvant cisplatin - based<br />
CT;<br />
- 2 - and 5 - yr disease - free survival<br />
= 61 and 39% in CT arm vs 55 and<br />
34% in control arm, respectively (p< .<br />
003);<br />
- 2 - and 5 - yr survival = 70 and 45%<br />
in CT arm vs 67 and 40% in control<br />
arm, respectively (p < .03);<br />
- benefits more evident in <strong>stage</strong> III<br />
disease<br />
2004
TREATMENT BY STAGE. XXIX.<br />
STAGE I - <strong>IIIA</strong> NSCLC. V.<br />
ADJUVANT THERAPY<br />
Cisplatin - based adjuvant CT in resected<br />
<strong>stage</strong> I - <strong>IIIA</strong> LC<br />
Pignon JP et al JCO 28; 3552, 2008<br />
* from meta - analysis (5 large trials,<br />
4,584 pts) on cisplatin - based<br />
chemotherapy in pts with completely<br />
resected NSCLC (<strong>stage</strong>s IA = 8%, IB =<br />
30%; II = 35%; <strong>IIIA</strong> = 27%) → 5 - yr<br />
absolute benefit = 5.4%, mainly in <strong>stage</strong><br />
<strong>IIIA</strong> pts
Postoperative radio ± chemotherapy<br />
(cisplatin + etoposide) in resected <strong>stage</strong> II - <strong>IIIA</strong> NSCLC<br />
Keller S et al (for Eastern Cooperative Oncology Group) NEJM 343, 1217, 2000
TREATMENT BY STAGE. XXX.<br />
STAGE <strong>IIIA</strong> NSCLC. III. NEOADJUVANT CHEMO RADIOTHERAPY<br />
* no clear evidence suggests ↑ survival in pts with "bulky"<br />
multilevel ipsilateral mediastinal nodes (N2) with surgery and either<br />
pre - or post - operative chemotherapy compared with chemotherapy<br />
plus radiation therapy
NEOADJUVANT CHEMOTHERAPY IN STAGES IB - <strong>IIIA</strong><br />
* randomized trial of neoadjuvant<br />
CT (mitomycin, ifosfamide and<br />
cisplatin) vs surgery alone in 355<br />
pts with <strong>stage</strong>s IB (37%) - II (16%) -<br />
<strong>IIIA</strong> (47%) NSCLC;<br />
- responders received two<br />
postoperative cycles (and pT3 or<br />
pN2 pts RT too);<br />
* at a median follow up of 80<br />
mos, benefit of neoadjuvant<br />
therapy confined to pts with N0 -<br />
N1 disease<br />
Depierre A et al JCO 2002<br />
A = PCT = primary CT +<br />
surgery<br />
B = PRS = surgery alone<br />
p ns<br />
p = .02
TREATMENT BY STAGE. XXXI.<br />
STAGE <strong>IIIA</strong> NSCLC. IV. NEOADJUVANT CHEMO - RADIOTHERAPY<br />
Improved results of induction chemoradiation before surgical<br />
intervention for selected pts with <strong>stage</strong> <strong>IIIA</strong> - N2 NSCLC<br />
Karl L et al J Thorac Cardiovasc Surg 134; 188, 2007<br />
* Objective: optimal management of <strong>stage</strong> <strong>IIIA</strong> - N2 NSCLC<br />
controversial → chemoradiation before surgical intervention for<br />
selected pts with <strong>stage</strong> <strong>IIIA</strong> - N2 NSCLC → results after 7 yrs of<br />
reported<br />
Methods: retrospective study of 40 pts (25% T1, 62.5% T2, 7.5% T3,<br />
and 5% T4) with biopsy - proved T1-3 N2 M0 lung cancer and good<br />
performance status who underwent concurrent induction<br />
chemoradiation (radiation therapy + 2 cycles of cisplatin and<br />
etoposide) → lung resection → 2 further cycles of consolidation<br />
chemotherapy
TREATMENT BY STAGE. XXXIbis.<br />
STAGE <strong>IIIA</strong> NSCLC. IVbis. NEOADJUVANT CHEMO - RADIOTHERAPY<br />
Improved results of induction chemoradiation before surgical<br />
intervention for selected pts with <strong>stage</strong> <strong>IIIA</strong> - N2 NSCLC<br />
Karl L et al J Thorac Cardiovasc Surg 134; 188, 2007<br />
* Results: overall and disease - free<br />
median survivals = 40 and 37.1 mos,<br />
respectively (overall and disease - free<br />
3 - yr survivals = 51.7% and 52.3%,<br />
respectively)<br />
- trend for ↑ overall survival in pts with<br />
single node at mediastinoscopy;<br />
Conclusion: chemoradiation before<br />
pulmonary resection in carefully<br />
selected pts with surgically resectable<br />
<strong>stage</strong> <strong>IIIA</strong> (N2) NSCLC can lead to ↑<br />
overall survival
TREATMENT BY STAGE. XXXII.<br />
STAGE <strong>IIIA</strong> NSCLC. V. NEOADJUVANT CHEMO - RADIOTHERAPY<br />
Concurrent versus sequential chemoradiotherapy with cisplatin and<br />
vinorelbine in locally advanced NSCLC: a randomized study. I.<br />
Zatloukal P et al Lung Cancer 46; 87, 2004<br />
* Purpose: relative merits of concurrent chemoradiotherapy (CRT)<br />
schedule vs sequential administration unclear;<br />
- Pts and methods: 102 previously untreated pts with locally<br />
advanced, <strong>stage</strong> <strong>IIIA</strong> (n = 15) or IIIB (n = 87) NSCLC randomized<br />
between concurrent (arm A) or sequential (arm B) CRT (cisplatin and<br />
vinorelbine + 60 Gy / 30 fractions for 6 wks)
TREATMENT BY STAGE. XXXIIbis<br />
STAGE <strong>IIIA</strong> NSCLC. Vbis. NEOADJUVANT CHEMO - RADIOTHERAPY<br />
Idem. II. Zatloukal P et al Lung Cancer 46; 87, 2004<br />
- Results: overall survival<br />
significantly longer in arm A vs<br />
B (median survival = 11.9 vs 8.5<br />
mos) (p = .024), as well as time<br />
to progression (TTP) (16.6 vs<br />
12.9 mos) and overall RR (80 vs<br />
47%, p = 0.001);<br />
- WHO G3 - 4 toxicity<br />
(leucopenia and nausea /<br />
vomiting) more frequent in arm<br />
A than in B;<br />
- Conclusion: concurrent CRT significantly benefits for response<br />
rate, overall survival and time to progression over sequential CRT;<br />
- concurrent CRT associated with higher toxicity
TREATMENT BY STAGE. XXXIII.<br />
STAGE <strong>IIIA</strong> NSCLC. VI. NEOADJUVANT CHEMO - RADIOTHERAPY<br />
Radiotherapy plus chemotherapy ± surgical resection for <strong>stage</strong> III<br />
NSCLC: a phase III randomised controlled trial. I.<br />
Albain KS et al Lancet 374; 379, 2009<br />
* Background: phase II studies in pts with <strong>stage</strong> <strong>IIIA</strong> NSCLC with<br />
ipsilateral mediastinal nodal metastases (N2) → feasibility of resection<br />
after concurrent chemotherapy and radiotherapy with promising rates of<br />
survival → phase III trial comparing concurrent chemotherapy and<br />
radiotherapy followed by resection with standard concurrent<br />
chemotherapy and definitive radiotherapy without resection<br />
- Methods: pts with <strong>stage</strong> T1 - 3pN2 M0 NSCLC randomly assigned to<br />
concurrent induction chemotherapy (2 cycles of cisplatin and etoposide<br />
+ radiotherapy;<br />
- with no progression, pts in “group 1 → resection” and pts in “group<br />
2 → continued radiotherapy”;<br />
- 2 additional cycles of cisplatin and etoposide given in both groups;<br />
- primary endpoint = overall survival (OS), on intention to treat<br />
(ClinicalTrials.gov, no. NCT00002550)
Idem. II<br />
Albain KS et al Lancet 374; 379, 2009<br />
* Findings: 202 pts (median age = 59 yrs)<br />
assigned to group 1 and 194 (median age<br />
= 61 yrs) to group 2;<br />
- median OS (below) = 23,6 vs 22,2 mos<br />
in groups 1 and 2 (p = .24), with pts alive<br />
at 5 yrs = 37 and 24% in group 1 and 2,<br />
respectively (p = .10);<br />
- with N0 status at thoracotomy, median<br />
OS = 34,4 mos;<br />
- progression - free survival (PFS)<br />
(above) better in group 1 (resection) than<br />
in 2 (continue radiotherapy) (median =<br />
12,8 vs 10,5 mos; p = .017, with pts<br />
without disease progression at 5 yrs = 32<br />
vs 13 %, respectively)
Idem. III.<br />
Albain KS et al Lancet 374; 379, 2009<br />
- G3 - 4 neutropenia and oesophagitis greater in group A than in B<br />
(38 and 10% and 41 and 23%, respectively, with treatment related<br />
deaths = 8 and 2%, respectively);<br />
- OS ↑ for pts on lobectomy, but not pneumonectomy, vs<br />
chemotherapy plus radiotherapy<br />
* Interpretation: chemotherapy + radiotherapy ± resection<br />
(preferably lobectomy: be considered, since treatment - related<br />
mortality greater in surgery arm (8 vs. 2%), with majority of deaths in<br />
pts undergoing pneumonectomy) options for pts with <strong>stage</strong> <strong>IIIA</strong> (N2)<br />
NSCLC
TREATMENT BY STAGE. XXXIV.<br />
STAGE <strong>IIIA</strong> NSCLC. VI. Bulky <strong>IIIA</strong>. I.<br />
* pts with persistent histologic N2 disease following<br />
neoadjuvant chemotherapy do particularly poorly, with<br />
some oncologists concluding that surgery for bulky <strong>IIIA</strong><br />
disease be conducted only in pts with clearing of<br />
mediastinal nodes following neoadjuvant therapy;<br />
- main role of neoadjuvant chemotherapy = to control<br />
micrometastatic disease;<br />
- if macroscopically mediastinal disease still evident =<br />
disease not sensitive to chemotherapy → unlikely that<br />
microscopic disease will be controlled → surgical removal<br />
of primary tumor after chemotherapy probably fruitless;<br />
[- likewise, neoadjuvant chemotherapy generally not be<br />
used to render inoperable disease operable]
TREATMENT BY STAGE. XXV.<br />
STAGE <strong>IIIA</strong> NSCLC. IV. Bulky <strong>IIIA</strong>. II.<br />
* exception to this approach = T4, N0 or T4, N1 (<strong>stage</strong> IIIB)<br />
disease for which preoperative chemotherapy provides<br />
enough tumor debulking to allow otherwise unresectable<br />
disease to be resected (chemotherapy may allow chest wall<br />
resection for direct extension of tumor, tracheal sleeve<br />
pneumonectomy and sleeve lobectomy for lesions near<br />
carina)