C-Section Pre-Op Checklist - My Doctor Online The Permanente ...
C-Section Pre-Op Checklist - My Doctor Online The Permanente ...
C-Section Pre-Op Checklist - My Doctor Online The Permanente ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
kp.org<br />
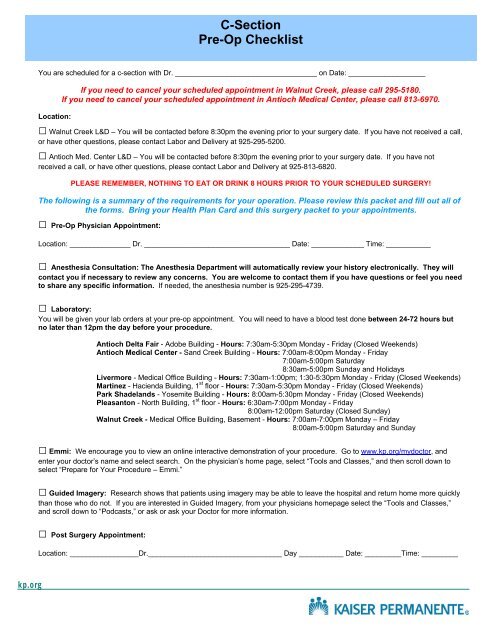
C-<strong>Section</strong><br />
<strong>Pre</strong>-<strong>Op</strong> <strong>Checklist</strong><br />
You are scheduled for a c-section with Dr. ___________________________________ on Date: ___________________<br />
If you need to cancel your scheduled appointment in Walnut Creek, please call 295-5180.<br />
If you need to cancel your scheduled appointment in Antioch Medical Center, please call 813-6970.<br />
Location:<br />
□ Walnut Creek L&D – You will be contacted before 8:30pm the evening prior to your surgery date. If you have not received a call,<br />
or have other questions, please contact Labor and Delivery at 925-295-5200.<br />
□ Antioch Med. Center L&D – You will be contacted before 8:30pm the evening prior to your surgery date. If you have not<br />
received a call, or have other questions, please contact Labor and Delivery at 925-813-6820.<br />
PLEASE REMEMBER, NOTHING TO EAT OR DRINK 8 HOURS PRIOR TO YOUR SCHEDULED SURGERY!<br />
<strong>The</strong> following is a summary of the requirements for your operation. Please review this packet and fill out all of<br />
the forms. Bring your Health Plan Card and this surgery packet to your appointments.<br />
□ <strong>Pre</strong>-<strong>Op</strong> Physician Appointment:<br />
Location: _______________ Dr. ____________________________________ Date: _____________ Time: ___________<br />
□ Anesthesia Consultation: <strong>The</strong> Anesthesia Department will automatically review your history electronically. <strong>The</strong>y will<br />
contact you if necessary to review any concerns. You are welcome to contact them if you have questions or feel you need<br />
to share any specific information. If needed, the anesthesia number is 925-295-4739.<br />
□ Laboratory:<br />
You will be given your lab orders at your pre-op appointment. You will need to have a blood test done between 24-72 hours but<br />
no later than 12pm the day before your procedure.<br />
Antioch Delta Fair - Adobe Building - Hours: 7:30am-5:30pm Monday - Friday (Closed Weekends)<br />
Antioch Medical Center - Sand Creek Building - Hours: 7:00am-8:00pm Monday - Friday<br />
7:00am-5:00pm Saturday<br />
8:30am-5:00pm Sunday and Holidays<br />
Livermore - Medical Office Building - Hours: 7:30am-1:00pm; 1:30-5:30pm Monday - Friday (Closed Weekends)<br />
Martinez - Hacienda Building, 1 st floor - Hours: 7:30am-5:30pm Monday - Friday (Closed Weekends)<br />
Park Shadelands - Yosemite Building - Hours: 8:00am-5:30pm Monday - Friday (Closed Weekends)<br />
Pleasanton - North Building, 1 st floor - Hours: 6:30am-7:00pm Monday - Friday<br />
8:00am-12:00pm Saturday (Closed Sunday)<br />
Walnut Creek - Medical Office Building, Basement - Hours: 7:00am-7:00pm Monday – Friday<br />
8:00am-5:00pm Saturday and Sunday<br />
□ Emmi: We encourage you to view an online interactive demonstration of your procedure. Go to www.kp.org/mydoctor, and<br />
enter your doctor’s name and select search. On the physician’s home page, select “Tools and Classes,” and then scroll down to<br />
select “<strong>Pre</strong>pare for Your Procedure – Emmi.”<br />
□ Guided Imagery: Research shows that patients using imagery may be able to leave the hospital and return home more quickly<br />
than those who do not. If you are interested in Guided Imagery, from your physicians homepage select the “Tools and Classes,”<br />
and scroll down to “Podcasts,” or ask or ask your <strong>Doctor</strong> for more information.<br />
□ Post Surgery Appointment:<br />
Location: _________________Dr._________________________________ Day ___________ Date: _________Time: _________
Medical Health History<br />
Name :______________________________________________________ Kaiser # _____________________________<br />
Reason for Surgery:<br />
OBGYN History:<br />
Number of pregnancies:_______ Number of Deliveries:_______ Last Menstrual Period (1 st day)_____________<br />
Post-menopausal: Yes/No Hysterectomy: Yes/No Birth Control Method_______________________<br />
Gynecologic problems:<br />
Abnormal Pap smear/Infections/Infertility Yes or No<br />
If yes, please explain:<br />
Other: Obstetrical (<strong>Pre</strong>gnancy-related) Problems: Yes or No<br />
Do you or have ever had any of the following conditions?<br />
(Family, friends and relatives may help to complete this section) Circle Yes or No Comments<br />
Heart: Heart attack or angina (chest pain), irregular heart beat) treadmill test Yes or No<br />
Rhythm (skipped beats, missed beats, very fast heart rate) Yes or No<br />
Heart failure (fluid on the lungs) Yes or No<br />
Other (murmur, shortage of breath when laying flat) Yes or No<br />
Circulation (high or low blood pressures, pain in legs with exercise) Yes or No<br />
Lungs: Asthma, bronchitis or emphysema Yes or No<br />
Shortage of breath or cough Yes or No<br />
Recent cold involving the lungs (within 2 weeks) Yes or No<br />
Nervous System (stroke, seizure, numbness, weakness, headache) Yes or No<br />
Disease of the brain or spine. Yes or No<br />
Liver (hepatitis, cirrhosis, jaundice, gallbladder disease or other problems) Yes or No<br />
Kidney disease (difficult urination, infection, etc.) Yes or No<br />
Diabetes ( high or low blood sugar) Yes or No<br />
Thyroid disease Yes or No<br />
Stomach (ulcers, heartburn, diarrhea, constipation, bleeding with bowel) Yes or No<br />
Movements or abdominal pain Yes or No<br />
Bleeding disorders (excess bleeding with cuts or dental procedures) Yes or No<br />
Are you taking anticoagulants (blood thinners) Yes or No<br />
Musculoskeletal System (back or neck, injuries or arthritis) Yes or No<br />
Skin (psoriasis, abrasions, bruises or ulcerations Yes or No<br />
Cancer (ever received chemotherapy or radiation treatments) Yes or No<br />
Depression, Anxiety or other Mental Health problems Yes or No<br />
Other Medical Problems? Explain<br />
kp.org
kp.org<br />
C-<strong>Section</strong><br />
<strong>Pre</strong>-<strong>Op</strong> <strong>Checklist</strong><br />
You are scheduled for a c-section with Dr. ___________________________________ on Date: ___________________<br />
If you need to cancel your scheduled appointment in Walnut Creek, please call 295-5180.<br />
If you need to cancel your scheduled appointment in Antioch Medical Center, please call 813-6970.<br />
Location:<br />
□ Walnut Creek L&D – You will be contacted before 8:30pm the evening prior to your surgery date. If you have not received a call,<br />
or have other questions, please contact Labor and Delivery at 925-295-5200.<br />
□ Antioch Med. Center L&D – You will be contacted before 8:30pm the evening prior to your surgery date. If you have not<br />
received a call, or have other questions, please contact Labor and Delivery at 925-813-6820.<br />
PLEASE REMEMBER, NOTHING TO EAT OR DRINK 8 HOURS PRIOR TO YOUR SCHEDULED SURGERY!<br />
<strong>The</strong> following is a summary of the requirements for your operation. Please review this packet and fill out all of<br />
the forms. Bring your Health Plan Card and this surgery packet to your appointments.<br />
□ <strong>Pre</strong>-<strong>Op</strong> Physician Appointment:<br />
Location: _______________ Dr. ____________________________________ Date: _____________ Time: ___________<br />
□ Anesthesia Consultation: <strong>The</strong> Anesthesia Department will automatically review your history electronically. <strong>The</strong>y will<br />
contact you if necessary to review any concerns. You are welcome to contact them if you have questions or feel you need<br />
to share any specific information. If needed, the anesthesia number is 925-295-4739.<br />
□ Laboratory:<br />
You will be given your lab orders at your pre-op appointment. You will need to have a blood test done between 24-72 hours but<br />
no later than 12pm the day before your procedure.<br />
Antioch Delta Fair - Adobe Building - Hours: 7:30am-5:30pm Monday - Friday (Closed Weekends)<br />
Antioch Medical Center - Sand Creek Building - Hours: 7:00am-8:00pm Monday - Friday<br />
7:00am-5:00pm Saturday<br />
8:30am-5:00pm Sunday and Holidays<br />
Livermore - Medical Office Building - Hours: 7:30am-1:00pm; 1:30-5:30pm Monday - Friday (Closed Weekends)<br />
Martinez - Hacienda Building, 1 st floor - Hours: 7:30am-5:30pm Monday - Friday (Closed Weekends)<br />
Park Shadelands - Yosemite Building - Hours: 8:00am-5:30pm Monday - Friday (Closed Weekends)<br />
Pleasanton - North Building, 1 st floor - Hours: 6:30am-7:00pm Monday - Friday<br />
8:00am-12:00pm Saturday (Closed Sunday)<br />
Walnut Creek - Medical Office Building, Basement - Hours: 7:00am-7:00pm Monday – Friday<br />
8:00am-5:00pm Saturday and Sunday<br />
□ Emmi: We encourage you to view an online interactive demonstration of your procedure. Go to www.kp.org/mydoctor, and<br />
enter your doctor’s name and select search. On the physician’s home page, select “Tools and Classes,” and then scroll down to<br />
select “<strong>Pre</strong>pare for Your Procedure – Emmi.”<br />
□ Guided Imagery: Research shows that patients using imagery may be able to leave the hospital and return home more quickly<br />
than those who do not. If you are interested in Guided Imagery, from your physicians homepage select the “Tools and Classes,”<br />
and scroll down to “Podcasts,” or ask or ask your <strong>Doctor</strong> for more information.<br />
□ Post Surgery Appointment:<br />
Location: _________________Dr._________________________________ Day ___________ Date: _________Time: _________
011116-002 (4-10)<br />
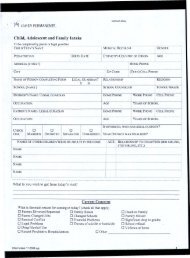
PRE-ADMIT FORM<br />
Admit Date: Medical Record Number:<br />
Dear Patient: To ensure accurate information, please complete this form in its entirety and return to<br />
the Admitting Department. As a Kaiser <strong>Permanente</strong> patient, you may have a hospital fee, deductible,<br />
copayment, or coinsurance which you are required to pay at the time of admission. If you would prefer<br />
to make a payment in advance of your admission, please call or visit the Admitting Department.<br />
Thank you.<br />
Emergency Contacts Patient Information<br />
Last Name First Name Middle Initial<br />
Date of Birth E-mail Address<br />
Address City State ZIP<br />
Home Phone Work Phone Cell Phone<br />
Ethnicity Marital Status ■ Registered Domestic Partner<br />
■ Hispanic/Latino—Other ■ Common Law ■ Single/Never Married<br />
■ Non-Hispanic/Non-Latino ■ Divorced ■ Separated<br />
■ Legally Separated ■ Widowed<br />
■ Married ■ Other<br />
During your admission, we have ■ Name ■ Religion Clergy visit?<br />
your permission to disclose ■ Condition ■ No Information/ ■ Yes<br />
(check all applicable boxes): ■ Location/Phone Confidential Admit ■ No<br />
Race ■ Native American / Eskimo /Aleutian — Other<br />
■ Asian / Pacific Islander— Other Asian ■ White — Other White or European<br />
■ Asian / Pacific Islander— Other Pacific Islander ■ Other<br />
■ Black— Other Black ■ Unknown<br />
Religion <strong>Pre</strong>ferred Spoken Language <strong>Pre</strong>ferred Written Language<br />
Employer<br />
Address City State ZIP<br />
Phone Employment Status Occupation<br />
Primary Contact Name Relationship to Patient<br />
Home Phone Work Phone<br />
Address City State ZIP<br />
Secondary Contact Name Relationship to Patient<br />
Home Phone Work Phone<br />
Address City State ZIP
011116-002 (4-10) REVERSE<br />
PRE-ADMIT FORM<br />
Advance Directive Information<br />
Do you have an Advance Health Care Directive? ■ Yes ■ No<br />
If yes, please provide a copy to the Admitting Department.<br />
Subscriber Information<br />
Name Relationship to Patient<br />
Address City State ZIP<br />
■ Male<br />
■ Female<br />
Date of Birth Home Phone<br />
Employer Employment Status<br />
Employer Address City State ZIP<br />
Occupation Work Phone<br />
Other Insurance Information<br />
Subscriber Name Relationship to Patient<br />
Address City State ZIP<br />
■ Male<br />
■ Female<br />
Date of Birth Home Phone<br />
Subscriber Employer Employment Status<br />
Employer Address City State ZIP<br />
Occupation Work Phone<br />
Medicare Claim # Part A Effective Date Part B Effective Date<br />
Medi-Cal Benefits ID # Medi-Cal Issue Date<br />
Workers’ Compensation Claim # Date of Injury/Illness Workers’ Compensation Policy #<br />
Other Kaiser <strong>Permanente</strong> Region Coverage<br />
Other Insurance Company Group Number Insurance ID<br />
Insurance Company Address Street City State ZIP<br />
Insurance Phone Effective Date of Insurance Coverage
Type of surgery/procedure Type of Anesthesia Problems with anesthesia or<br />
procedures<br />
What is your occupation? _______________________________________________<br />
What is the name of your partner/spouse/significant other? _____________________________<br />
Have you filled out the Advanced Health Care Directive? Yes or No<br />
(please see Surgery Packet, and try to complete before your procedure)<br />
Who do you designate to make decisions regarding your health if you are unable to do so?<br />
Has any blood relative of yours had a serious reaction to anesthesia? Yes or No<br />
If yes, explain:<br />
Do you or have you ever smoked? Yes or No<br />
If so ______packs/day for ____years<br />
Do you drink alcohol? Yes or No<br />
If so ____ oz. a day /week/ month (circle one)<br />
Do you ever or have you ever used drugs? Yes or No<br />
(i.e. Marijuana, cocaine, intravenous drugs)<br />
Are you interested in a copy of our Guided Imagery CD to listen to before/during and after surgery to<br />
help with your preparation and recovery from surgery?<br />
Did you remember to fill out yellow Medication card with medications and allergies?<br />
Date: Patient Signature:<br />
kp.org<br />
List previous surgeries, including C-<strong>Section</strong>s<br />
Date
Women’s Health Center<br />
Tell your surgeon of all medications, including herbals and over the counter medications that you take.<br />
Some drugs cause bleeding when taken prior to surgery, especially blood thinners and antiinflammatories.<br />
If you are taking Coumadin of Warfarin you will need to contact the<br />
Anticoagulant Clinic as soon as possible at 925-372-1628. <strong>The</strong>y will instruct you about changing<br />
or discontinuing these medications prior to surgery. Stop taking the following drugs seven days<br />
prior to surgery. If you feel you cannot stop these medications due to your medical condition, discuss<br />
this with your surgeon as soon as possible. This list may not be totally inclusive – use it as a<br />
supplement to your discussion with your surgeon.<br />
Do not take medications from the list below for one week before the procedure. <strong>The</strong>se drugs can cause<br />
excessive bleeding if taken prior to surgery or biopsy. (NOTE: Tylenol is OK!)<br />
Advil Aspergum Carpon Double –A Fiorinal Magsal Neocylate Salatin Vanquish<br />
AlkaSeltzer Aspirin Cataflam Duoprin Flubiprofen Marnal Nuprin Saleto Vitamin E<br />
Aleve Asproject Clinoril Duradyne Garlic Major-cin Oxalid Sine-off Voltaren<br />
Anacin Axotal Cope Duragesic Gaysal –S Majoral PAC Solocol Warfarin<br />
Anaprox Bayer Coricidin Durasel Gemnisyn Measurin Pabalate Supac Zorpin<br />
Ansaid B C Tabs CP-2 Dynosal Ginko Maclomen Pabirin Synalgos<br />
Anturane Buf Tabs Cosprin Ecotrin Ginseng Micranin Panodynes Tandearil<br />
APSP Fort Buff A Coumadin Efficin Ibuprofen Midol Pepto-<br />
Bismal<br />
Tenstan<br />
Argesic Buffaprin Dasin Emgrin Indocin Mobidin Percodan Ticlid<br />
Athra – G Buffets II Dicifenac Empirin Isollyl Mobigesic Persantine Ticlopidine<br />
Artholate Buffinol Dipyridamole Encaprin Kaopectate Mementum Protension Tisma<br />
Arthropan Buflex Disalcid Equagesic Ketoralac Motrin Postel Tolectin<br />
Ascriptin Butal Comp Doans Pills Etodolac Lanorinal Nabumetone Relafen Toradol<br />
Asper Buf Butazolodin Dolcin Exederin Lodine Nalfon Rufen Trigesic<br />
Aspercin Cama Dolobid Feldene Magan Naprosyn Sal-Favne UracelS<br />
kp.org
Use this document to determine the most up-to-date hours of operation for the Laboratory, Pharmacy, and Radiology<br />
Department for the entire Diablo Service Area. Find the location you are interested in and click on the corresponding link<br />
underneath.<br />
2/5/2011 1:03:00 PM<br />
Antioch<br />
Medical Center<br />
Antioch<br />
Delta Fair<br />
Livermore Martinez Park Shadelands<br />
Walnut Creek<br />
Pleasanton Walnut Creek<br />
Medical Center<br />
Laboratory Click Here Click Here Click Here Click Here Click Here Click Here Click Here<br />
Pharmacy Click Here Click Here Click Here Click Here Click Here Click Here Click Here<br />
Radiology Click Here Click Here Click Here Click Here Click Here Click Here Click Here
Information about your Hospitalization and Discharge<br />
It is very important while you are in our care that you get the information you need to care for<br />
yourself (or to be cared for) to return home. We encourage you and yours family to ask<br />
questions to improve the transition from hospital to home. Visiting hours are between 11am<br />
and 8pm.<br />
Your Nursing Care<br />
Your nurse will be your caregiver, teacher and advocate. He or she will be able to provide<br />
information and resources to help you prepare for your discharge from the hospital. While in<br />
the hospital, your nursing care will be provided by 3 shifts of nurses. You will be assigned a<br />
nurse to ensure your needs are met.<br />
Discharge<br />
Your physician will assess your condition daily to determine when you are well enough to leave<br />
the hospital. A typical hospital stay for c-section is two days. Our intention is to plan on<br />
discharging you before 11:00 am on your day of discharge. However, if for some reason other<br />
testing needs to be done or clinical monitoring is needed; you may be discharged later than<br />
11:00 am. Before you leave the hospital, your physician and nurses will give you information<br />
about your continuing recovery, medications and follow up appointments. If you have<br />
questions, there are resources available for you.<br />
Transportation Home<br />
Remember to check that arrangements for a ride home or to another health care setting are<br />
confirmed. Every intent will be made to have you ready for discharge by 11:00 am. Please<br />
arrange to have your family members available at this time to provide transportation. If you<br />
need help arranging transportation please let a Medical Social Worker or Continuing Care<br />
Coordinator know. Your provider will provide instructions when you will be able to drive upon<br />
discharge.<br />
Note: Please notify your nurse within 24 hours of admission of the name and phone number of<br />
the person who will provide your transportation by 11:00 am on the day of discharge.<br />
kp.org<br />
When to Call Your OB/GYN after Discharge:<br />
<strong>The</strong> nurses will review home care with you. Some symptoms occur with normal healing<br />
however please call your doctor if you experience the following:<br />
Two temperature readings of 100.4 taken 4 hours apart<br />
A single temperature reading of 101 or greater<br />
Unable to take fluids by mouth<br />
Vomiting after discharge from hospital<br />
No bowel movement within 4 days after discharge from hospital<br />
Separation of wound edges, drainage from wound, or large red hot expanding areas<br />
around the wound<br />
Heavy vaginal bleeding, filling 1 pad per hour for 4 or more hours
This is to alert you to the fact that you may have a fee for your<br />
surgical procedure, depending upon your coverage.<br />
We in the clinic do not have access to the actual charges a<br />
surgical procedure may incur. If you have any questions about<br />
these fees, please contact Member Services at:<br />
1-800-464-4000 (English) 1-800-757-7585 (Chinese Dialects)<br />
1-800-788-0616 (Spanish) 1-800-777-1370 (TTY)<br />
Questions regarding Kaiser <strong>Permanente</strong>’s financial assistance program, please call:<br />
1-866-399-7696<br />
kp.org<br />
CO–PAY ALERT<br />
Thank you
Women’s Health Center<br />
Abdominal Surgery Instructions<br />
If you’re having an incision on your abdomen (for example C/S, abdomen<br />
hysterectomy):<br />
Your cooperation is needed to ensure a successful outcome of your surgery. <strong>The</strong> purpose of<br />
the Hibiclens soap is to reduce the normal bacteria on your skin that may be a potential source<br />
of infection at the surgical site. Please follow these instructions carefully:<br />
1. Purchase 4 oz. container of Hibiclens from pharmacy (the cost will be approximately<br />
$5.00 to $6.00).<br />
2. Remove any body piercing jewelry prior to showering and leave out until after the<br />
surgery.<br />
3. Shower the night before surgery and the morning of the surgery, using ½ of the bottle for<br />
each shower.<br />
4. Hair may be shampooed with regular shampoo and rinsed thoroughly prior to use of the<br />
Hibiclens on the body.<br />
5. Use a clean washcloth to apply the Hibiclens.<br />
6. Wash your body from the neck down to your toes with Hibiclens.<br />
7. Be sure to clean the area well where the surgical incision will be.<br />
8. This is an effective cleaner, even though it doesn’t make suds well.<br />
9. Rinse thoroughly with running water. DO NOT use any other soap or body rinse on your<br />
skin.<br />
10. Pat dry with a clean absorbent towel.<br />
11. Do not use lotion, powder, deodorant or perfume/aftershave of any kind on the skin after<br />
bathing with Hibiclens.<br />
12.<br />
<strong>The</strong> admitting nurse will ask you if you have taken your pre-op antimicrobial showers.<br />
Thank you for participating in your successful surgery.<br />
kp.org
BEFORE ANESTHESIA:<br />
Please follow these<br />
instructions carefully so that<br />
your surgery/procedure is not<br />
cancelled or delayed.<br />
Eating and Drinking<br />
After midnight: no food, mild,<br />
communion, or tobacco. Up to 4<br />
hours before surgery: clear liquids<br />
are okay (unless Anesthesia said<br />
no). <strong>The</strong> last 4 hours prior to<br />
surgery; nothing at all (including<br />
gum and mints).<br />
MEDICATIONS:<br />
Take only these medications (sip of<br />
water okay):<br />
• Stop aspirin 1 week before<br />
surgery<br />
• Stop Motrin (ibuprofen), Anaprox,<br />
Feldene 2 days before.<br />
CLOTHING /ACCESSORIES:<br />
Wear casual clothing, easy to<br />
kp.org<br />
ANESTHESIA DEPARTMENT<br />
INSTRUCTIONS FOR YOU SAFETY<br />
remove and replace. Remove eye<br />
makeup, artificial eyelashes, contact<br />
lenses, all jewelry, hairpieces,<br />
hairpins, and barrettes. Please<br />
bring your Kaiser <strong>Permanente</strong> Card.<br />
AFTER ANESTHESIA FOR<br />
OUTPATIENT SURGERY<br />
(Including local anesthesia):<br />
You must have a responsible adult<br />
• Drive you home (or ride in a taxi<br />
with you)<br />
• Help you for 8 hours after<br />
leaving the hospital<br />
QUESTIONS YOU MAY HAVE:<br />
Why can’t I eat or drink?<br />
Protective reflexes may be lost or<br />
decreased during anesthesia, even<br />
local or sedation. <strong>The</strong>refore, an<br />
empty stomach is essential because<br />
vomit could enter your lungs when<br />
protective reflexes are lost or<br />
diminished. If stomach contents<br />
enter the lungs, serious, possibly<br />
lethal, complications will result.<br />
What are Clear Liquids?<br />
Clear liquids have no residue (solid<br />
particles and fat) and digest quickly.<br />
<strong>The</strong>y include water, tea, black<br />
coffee, Kool-Aid, clear (flavored)<br />
Jell-O, fat free clear broth or bullion,<br />
apple juice, cranberry juice and<br />
grape juice. Sugar may be added to<br />
your beverage as it dissolves with<br />
no residue. Do not add milk, milk<br />
products, or non-dairy creamers to<br />
your beverages. MILK IS NOT A<br />
CLEAR LIQUID.<br />
Why stop Aspirin, Motrin, etc?<br />
<strong>The</strong>y decrease the blood’s ability to<br />
clot and may increase bleeding<br />
during surgery.<br />
Why do I need a responsible<br />
Adult?<br />
All anesthetics, even locals in large<br />
doses, produce drowsiness,<br />
impaired judgment, and poor<br />
coordination for several hours. It is<br />
essential for you to arrange in<br />
advance for assistance after leaving<br />
the hospital.
It takes your body about 24 hours to<br />
eliminate the drugs used.<br />
Until then, they interfere with normal<br />
judgment and response times. So,<br />
plan not to operate a vehicle or<br />
attempt to make responsible<br />
decisions for 24 hours. It is quite<br />
normal to feel tired and lacking in<br />
energy for 48 hours after minor<br />
surgery.<br />
Why can’t I wear Contact Lenses,<br />
Eye Makeup, and Artificial<br />
Eyelashes?<br />
<strong>The</strong>y can cause eye injury during<br />
anesthesia, plus contacts and<br />
eyelashes can be lost or damaged.<br />
Why can’t I wear my jewelry and<br />
hairpiece?<br />
<strong>The</strong>y may become pressure point<br />
areas while you are under<br />
anesthesia and can cause damage<br />
to your body. Rings should be<br />
removed as fingers my swell during<br />
surgery. And these items can be<br />
lost or damaged. Leave your<br />
valuables at home.<br />
kp.org<br />
ANESTHESIA DEPARTMENT<br />
INSTRUCTIONS FOR YOU SAFETY<br />
Can I wear my Dentures?<br />
Usually not in the operating room.<br />
Since dentures can be lost or<br />
broken. It is best to take them out at<br />
home or on the ward. You can ask<br />
to wear them until you enter the<br />
operating room, and then remove<br />
them.<br />
How soon will I leave the<br />
Hospital?<br />
As soon as your doctors consider it<br />
safe. This varies with different<br />
surgeries and anesthetics. With<br />
outpatient surgery the average time<br />
for leaving the hospital is between 6<br />
and 8 hours after you arrive at<br />
the hospital. <strong>The</strong> nurses will call the<br />
person driving you home if they<br />
don’t wish to wait.<br />
Do modern Anesthetics make you<br />
sick afterward?<br />
Not usually. Anesthetics seldom<br />
cause upset stomachs anymore.<br />
Pain relieving drugs often do<br />
though, and most operations require<br />
their use at least once, either<br />
before, during after surgery. Please<br />
tell the nurses if you become<br />
nauseated. <strong>The</strong>y have medications<br />
to treat nausea.<br />
After Outpatient Surgery, is<br />
there any chance I won’t be able<br />
to go home the same day?<br />
Yes. If any circumstances develop<br />
which require extended care, you<br />
will be admitted to the hospital. <strong>The</strong><br />
potential complications of surgery<br />
and anesthesia will be explained in<br />
advance by your doctors. For now,<br />
it is important for you and your<br />
family to understand that you might<br />
remain in the hospital overnight or<br />
longer.<br />
We look forward to caring for<br />
you. We want to give you the<br />
care that you need and<br />
deserve. Thank you for<br />
choosing Kaiser <strong>Permanente</strong>.
During recovery you should avoid movements<br />
that strain your abdominal muscles and incision.<br />
Protect your incision as well as your low back by<br />
using good body mechanics similar to those you<br />
used during pregnancy. As well, you can<br />
support your back during movement by<br />
tightening the pelvic floor (kegel) muscles and<br />
gently contracting the abdominal muscles.<br />
Body Mechanic Tips<br />
Breathe normally during movement; avoid breath<br />
holding.<br />
- To Get Into Bed: Sit at edge of bed, using your<br />
arms lower yourself to your side as you bring<br />
your legs onto the bed. Roll to your back with<br />
knees held hip width apart rather than separating<br />
legs.<br />
- To Get Out of Bed: roll to your side, lower legs<br />
over the edge of the bed and push with your<br />
bottom elbow and top hand against the bed to sit<br />
upright.<br />
- To Get Out of a Chair: come to the edge of the<br />
chair, keep your knees somewhat apart and<br />
squeeze buttocks as you stand up.<br />
- To Get in a Car: first sit down on the seat by<br />
backing in, keeping both knees together, pivot to get<br />
into car.<br />
- Bend your knees and hips when lifting. Avoid<br />
bending from the waist.<br />
- Avoid using one leg forcefully as this can put stress<br />
on abdominals and pelvic girdle i.e. do not use one<br />
leg to shove items on the floor; or stand on one leg<br />
kp.org<br />
Recovery After<br />
Cesarean <strong>Section</strong><br />
Page 1 of 2<br />
and put the other over a baby gate.<br />
- Hold a pillow against your abdomen if you<br />
should cough or sneeze to help decrease<br />
discomfort.<br />
-<br />
Regaining Abdominal Strength<br />
In the First 6 weeks:<br />
Many of the body/hormonal/postural<br />
changes that occur during pregnancy linger on<br />
several weeks after delivery. Because of this<br />
and the added fatigue of newborn care you<br />
need to gradually return to your regular<br />
exercise routine. To help your body transition<br />
use the same body mechanics you did when<br />
you were pregnant.<br />
Contract your pelvic floor and abdominal<br />
muscles when lifting to help protect your low<br />
back as well as to begin to re strengthen these<br />
areas. (Do this by gently tightening the vaginal<br />
and rectal muscles as if to hold in urine and<br />
gas while also pulling in abdominal muscles as<br />
if to zip up jeans. Breathe normally as you do<br />
this)<br />
Try to do 10 pelvic floor contractions<br />
(squeeze the vaginal rectal muscles as if to<br />
hold in urine and gas) holding 5-10 counts<br />
while feeding your baby. Pelvic floor exercise in<br />
the immediate postpartum period helps restrengthen<br />
these muscles, supports the<br />
spine/pelvic girdle and may help prevent<br />
urinary incontinence. (JOGC 517 June 2003)<br />
Resume walking in 15 minute<br />
increments and gradually transition to brisk<br />
walking as your energy level returns.<br />
Scar Mobilization: Massage gently along and<br />
across the length of the scar to promote<br />
mobility and uniform healing.
6-12 Weeks Post Partum<br />
At 6 weeks post partum you can start to<br />
resume your regular exercise routines.<br />
Because you are still recovering from<br />
delivery you should exercise for less time<br />
and at a lower intensity than pre-pregnancy<br />
and gradually increase to your regular<br />
routine. <strong>The</strong> following exercise will help you<br />
re-strengthen the lower abdominals:<br />
One Leg Heel Slide – Lay on back with<br />
knees bent. Contract pelvic floor and<br />
abdominal muscles as you slowly slide heel<br />
away from body and straighten leg. Relax.<br />
Contract muscles again as you slide heel<br />
back to start position. Begin with 10 on each<br />
side and work to 20-30.<br />
Single Leg Fall Out – Lay on back with knees<br />
bent, hip width apart and feet flat on floor.<br />
Breathe in, as you breathe out do a pelvic<br />
floor contraction and let one leg fall slowly<br />
out to the side. Relax. Do a pelvic floor<br />
contraction and bring leg back to starting<br />
position. Begin with 10 repetitions on each<br />
leg and work to 20 repetitions. When you<br />
can do 20 with each leg begin to do both legs<br />
together. Start with 10 and work to 20.<br />
Hands and Knees – On your bed get into a<br />
hands and knees position so that you are<br />
square: hands under shoulders and knees<br />
below hips. Allow back to relax into normal<br />
curve. Breathe in and as breathe out do a<br />
pelvic floor contraction and try to gentle pull<br />
abdominal muscles toward spine.<br />
kp.org<br />
Recovery After<br />
Cesarean <strong>Section</strong><br />
Page 2 of 2<br />
Begin with 10 repetitions, hold 5. Work to 2<br />
sets of 10 repetitions, hold 10.<br />
ACOG Committee <strong>Op</strong>inion No. 267: Exercise During<br />
<strong>Pre</strong>gnancy and the Postpartum period.<br />
It is important to continue with kegel exercise<br />
(pelvic floor contractions). A strong pelvic<br />
floor will help prevent urinary incontinence,<br />
organ prolapse and will contribute to sexual<br />
satisfaction.<br />
Continue to use good posture and body<br />
mechanics as this will prevent abdominal and<br />
low back strain as well as protect against<br />
organ prolapse. Be careful to support baby<br />
well during nursing. Bring baby to your breast<br />
as opposed to leaning forward as you nurse.<br />
Support your low back and abdominals by<br />
using good body mechanics when<br />
transferring baby in and out of car.<br />
Continue scar mobilization if your c-section<br />
scar is painful or stiff.<br />
Please note if you should become short of<br />
breathe or dizzy while lying on your back<br />
please stop the exercise immediately and let<br />
your provider know about your symptoms.
Dear Member,<br />
When you come in for your procedure, you will be asked if you have an Advance Directive. This is a<br />
written form where you write down two important things:<br />
1. Your wishes about life support and other treatments<br />
2. Who you want to speak for you if you become too ill to speak for yourself in making medical<br />
decisions.<br />
Why pay attention to this now? None of us knows when a medical crisis might happen and important<br />
decisions will need to be made. Going into the medical center is a good opportunity to think these<br />
things over and complete the Advance Directive, so that your right to make your medical decisions can<br />
be honored even if you can no longer speak for yourself.<br />
We can help. A form is enclosed in this packet. Call your nearest Kaiser <strong>Permanente</strong> Health Education<br />
Office to sign up for one of our two hour workshops to help your complete your Advance Directive.<br />
<strong>The</strong>se services are free and well worth doing for you and your loved one’s peace of mind.<br />
Kaiser <strong>Permanente</strong> Health Education Offices:<br />
Antioch 925-779-5147<br />
Martinez 925-372-1198<br />
Park Shadelands 925-906-2190<br />
Pleasanton 925-847-5172<br />
Walnut Creek 925-295-4410<br />
Deer Valley 925-813-3560<br />
Livermore 925-243-2920<br />
kp.org<br />
Advance Directives
CALIFORNIA ADVANCE HEALTH CARE DIRECTIVE<br />
Including Power of Attorney for Health Care<br />
Imprint / MRN<br />
NOTE: <strong>The</strong> document meets legal requirements for most Californians, but might not be<br />
appropriate in special circumstances. If you might have special needs, consult an attorney.<br />
PART 1: APPOINTING AN AGENT TO MAKE HEALTH CARE DECISIONS<br />
NOTE: You should discuss your wishes in detail with your designated agent(s)<br />
<strong>My</strong> name is:_____________________________________ Date of Birth:________________<br />
<strong>My</strong> address is:_______________________________________________________________<br />
In this document I appoint an agent. That agent will make health care decisions for me<br />
in the future, if and when I no longer have the mental capacity to make my own health<br />
care decisions.<br />
<strong>Op</strong>tional: I want my agent to make my health care decisions now, even though I currently<br />
have the mental capacity to make my own health care decisions. _______ (Do not initial<br />
here if you want to continue making your own health decisions for as long as you are able.)<br />
<strong>The</strong> following persons cannot be selected as your agent or alternate agent:<br />
• Your primary physician<br />
• An employee of the health care institution or residential care facility where you<br />
receive care (unless you are related to that person or you are co-workers).<br />
PRIMARY AGENT:<br />
Agent’s Name: ___________________________________________________<br />
Address:___________________________________________________________________<br />
____________________________________________________<br />
(Phone numbers – indicate home, work, pager, and cellular phone)<br />
1 st ALTERNATE AGENT (If Agent is not willing, able, or reasonably available to serve.)<br />
Name of first alternate agent: ____________________________________________________<br />
Address:___________________________________________________________<br />
____________________________________________________<br />
(Phone numbers – indicate home, work, pager, and cellular phone)<br />
2nd ALTERNATE AGENT (If Agent and 1 st Alternate are unavailable or unwilling to serve.)<br />
Name of second alternate agent: _______________________________________<br />
Address:___________________________________________________________<br />
____________________________________________________________<br />
(Phone numbers – indicate home, work, pager, and cellular phone)<br />
Page 1 of 4 www.codaalliance.org 7-25-04
WHAT MY AGENT MAY DO<br />
<strong>My</strong> agent will be allowed to make health care decisions for me just as I can presently make<br />
my own. For example, I give my agent my trust to make decisions (1) to accept or refuse<br />
treatment for me, including accepting or discontinuing food and fluid that is given through a<br />
tube into my stomach or into a vein; (2) to choose for me a particular physician or health care<br />
facility; and (3) to receive or review my medical information and records, or to permit release<br />
of my records for others’ review. _______(initial here)<br />
WHAT MY AGENT MUST DO<br />
<strong>My</strong> agent shall make health care decisions for me by considering what I have written here, and<br />
by considering my other wishes. <strong>My</strong> agent will try to find out as much as he/she can about my<br />
wishes. If my agent does not know my wishes, he/she shall consider my personal values as<br />
much as possible and make decisions that he/she thinks are in my best interest. I ask that when<br />
my agent is trying to consider my values and prior wishes, that he/she talk to other loved ones<br />
who know me and care about me. _______(initial here)<br />
<strong>The</strong> following individual(s) are to be EXCLUDED from any part of health care decisionmaking<br />
for me:<br />
No Exclusions ____________________________________________ _______(initial here)<br />
AFTER MY DEATH<br />
<strong>My</strong> agent will be able to authorize an autopsy, donate all or part of my body, and/or determine<br />
the disposition of my remains. If I have written a will or made funeral arrangements, my agent<br />
should follow those instructions on what happens to my body after my death or other<br />
arrangements I have made. If I want to make exceptions to this authority, I write them<br />
here or in an attachment to this form:<br />
No Exceptions ____________________________________________ _______(initial here)<br />
(Sign and date the attached pages when this document is witnessed.)<br />
PART 2: HEALTH CARE INSTRUCTIONS (Cross out the sections that do not apply)<br />
I have made additional written instructions to my agent and attached them. _______(initial here)<br />
(Sign and date the attached pages when this document is witnessed.)<br />
TRUST IN AGENT: <strong>The</strong> instructions I give to my agent are guidelines to assist him/her in<br />
making the best medical decisions for me. <strong>The</strong> subject of unacceptable treatments is a complex<br />
one. Whether I would or would not want a particular medical intervention might depend on<br />
context. At some point there might be a conflict between treatment instructions I have given and<br />
what my agent thinks best in circumstances that I could not have predicted. I trust that my agent<br />
will honor my goals and values. _______(initial here)<br />
PERSONAL CARE DECISIONS: By my initials here I direct that my agent(s) named above<br />
authorize personal care on my behalf including, but not limited to, choice of residence, clothing,<br />
receipt of my mail, care for my personal belongings, care for my pet(s) if any, and all other<br />
decisions of a personal nature not included in the description of health care. _____(initial here)<br />
DNR ORDER: I have completed a <strong>Pre</strong>hospital Do Not Resuscitate Form. _______(initial here)<br />
Page 2 of 4 www.codaalliance.org 7-25-04
REVOCATION OF PREVIOUS DOCUMENTS: I revoke any previously-executed Power of<br />
Attorney for Health Care, Individual Health Care Instruction, or Natural Death Act Declaration.<br />
I have the right to revoke this directive at a future date by creating a new one.<br />
PART 3: SIGNATURE OF PERSON WHO IS MAKING THIS DIRECTIVE<br />
Sign the document in the presence of the witnesses or the Notary.<br />
Date: _______________ Signature: _____________________________________________<br />
If the person making this directive is unable to write, have the person make a mark,<br />
have a witness write the name of the person making this directive and sign next page.<br />
PART 4: THIS DOCUMENT MUST EITHER BE NOTARIZED OR SIGNED BY TWO<br />
WITNESSES ON THE NEXT PAGE.<br />
WITNESSES: Certain individuals cannot serve as witnesses. Those rules are set forth in the<br />
following witness statements:<br />
I DECLARE UNDER PENALTY OF PERJURY UNDER THE LAWS OF CALIFORNIA<br />
(1) That the individual who signed or acknowledged this Advance Health Care Directive is personally<br />
known to me, or that the individual’s identity was proven to me by convincing evidence.<br />
(2) That the individual signed or acknowledged this Advance Directive in my presence,<br />
(3) That the individual appears to be of sound mind and under no duress, fraud, or undue influence,<br />
(4) That I am not a person appointed as agent by this Advance Directive, and<br />
(5) That I am not the individual’s health care provider, an employee of the individual’s health care<br />
provider, the operator of a community care facility, an employee of an operator of a community<br />
care facility, the operator of a residential care facility for the elderly, nor an employee of an<br />
operator of a residential care facility for the elderly.<br />
First Witness: _________________________________ _________________________________<br />
Name (printed) Signature<br />
Date: __________________ Address: __________________________________________<br />
Second Witness: _______________________ __________________________<br />
Name (printed) Signature<br />
Date: __________________ Address: __________________________________________<br />
ONE OF THE PRECEDING WITNESSES ALSO MUST SIGN THE FOLLOWING DECLARATION:<br />
I further declare under penalty of perjury under the laws of California that I am not related to the<br />
individual executing this advance health care directive by blood, marriage, or adoption, and, to the<br />
best of my knowledge, I am not entitled to any part of the individual’s estate upon his or her death<br />
under a will now existing or by operations of law.<br />
Date: __________________ Signature: __________________________________________<br />
Page 3 of 4 www.codaalliance.org 7-25-04
Only if the person making this directive is unable to write, witnesses complete this section:<br />
_________________________________, being unable to write, made his/her mark in<br />
our presence and requested the first of the undersigned to write his/her name, which he/she did,<br />
and we now subscribe our names as witnesses thereto.<br />
____________________________ _____________________________<br />
Signature of Witness #1 Signature of Witness #2<br />
If the principal (the person appointing the agent) currently resides in a<br />
nursing facility, this document also must be witnessed by a representative of California’s<br />
Long-Term Care Ombudsman Program. If the two-witness method is chosen, the<br />
Ombudsman Program representative may serve as one of the two witnesses, or may serve as<br />
a third witness. If the notarization method is chosen, the Ombudsman Program<br />
representative serves as a separate witness.<br />
DECLARATION OF OMBUDSMAN PROGRAM REPRESENTATIVE<br />
(Required ONLY if person appointing the agent currently resides in a nursing facility.)<br />
I declare under penalty of perjury under the laws of California that I am an ombudsman<br />
designated by the California Department of Aging and that I am serving as a witness as required<br />
by <strong>Section</strong> 4675 of the California Probate Code.<br />
_________________________________ _________________________________ ____________________<br />
Name (printed) Signature Date<br />
CERTIFICATE OF ACKNOWLEDGEMENT OF NOTARY PUBLIC<br />
(Not required if two-witness method is followed)<br />
State of California, County of __________________________<br />
On this ____ day of __________________, ______, before me, the undersigned, a Notary Public in<br />
and for said State, personally appeared ______________________________________, personally<br />
known to me or proved to me on the basis of satisfactory evidence to be the person whose name is<br />
subscribed to the within instrument, and acknowledged to me that he/she executed it.<br />
WITNESS my hand and official seal.<br />
(seal) Signature _______________________________________<br />
Page 4 of 4 www.codaalliance.org 7-25-04