Cauda Equina Syndrome in a Pediatric Patient due to Lumbar Disc ...
Cauda Equina Syndrome in a Pediatric Patient due to Lumbar Disc ... Cauda Equina Syndrome in a Pediatric Patient due to Lumbar Disc ...
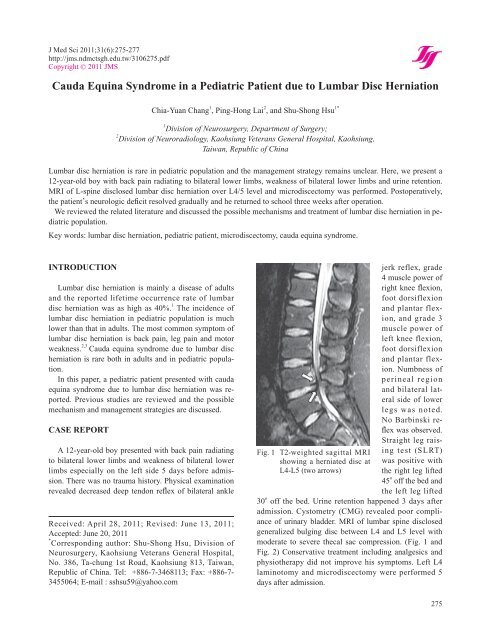
J Med Sci 2011;31(6):275-277 http://jms.ndmctsgh.edu.tw/3106275.pdf Copyright © 2011 JMS Received: April 28, 2011; Revised: June 13, 2011; Accepted: June 20, 2011 * Corresponding author: Shu-Shong Hsu, Division of Neurosurgery, Kaohsiung Veterans General Hospital, No. 386, Ta-chung 1st Road, Kaohsiung 813, Taiwan, Republic of China. Tel: +886-7-3468113; Fax: +886-7- 3455064; E-mail : sshsu59@yahoo.com Chia-Yuan Chang, et al. Cauda Equina Syndrome in a Pediatric Patient due to Lumbar Disc Herniation Chia-Yuan Chang 1 , Ping-Hong Lai 2 , and Shu-Shong Hsu 1* 1 Division of Neurosurgery, Department of Surgery; 2 Division of Neuroradiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, Republic of China Lumbar disc herniation is rare in pediatric population and the management strategy remains unclear. Here, we present a 12-year-old boy with back pain radiating to bilateral lower limbs, weakness of bilateral lower limbs and urine retention. MRI of L-spine disclosed lumbar disc herniation over L4/5 level and microdiscectomy was performed. Postoperatively, the patient’s neurologic defi cit resolved gradually and he returned to school three weeks after operation. We reviewed the related literature and discussed the possible mechanisms and treatment of lumbar disc herniation in pediatric population. Key words: lumbar disc herniation, pediatric patient, microdiscectomy, cauda equina syndrome. INTRODUCTION Lumbar disc herniation is mainly a disease of adults and the reported lifetime occurrence rate of lumbar disc herniation was as high as 40%. 1 The incidence of lumbar disc herniation in pediatric population is much lower than that in adults. The most common symptom of lumbar disc herniation is back pain, leg pain and motor weakness. 2,3 Cauda equina syndrome due to lumbar disc herniation is rare both in adults and in pediatric population. In this paper, a pediatric patient presented with cauda equina syndrome due to lumbar disc herniation was reported. Previous studies are reviewed and the possible mechanism and management strategies are discussed. CASE REPORT A 12-year-old boy presented with back pain radiating to bilateral lower limbs and weakness of bilateral lower limbs especially on the left side 5 days before admission. There was no trauma history. Physical examination revealed decreased deep tendon refl ex of bilateral ankle Fig. 1 T2-weighted sagittal MRI showing a herniated disc at L4-L5 (two arrows) jerk reflex, grade 4 muscle power of right knee fl exion, foot dorsiflexion and plantar flexion, and grade 3 muscle power of left knee flexion, foot dorsiflexion and plantar flexion. Numbness of perineal region and bilateral lateral side of lower legs was noted. No Barbinski refl ex was observed. Straight leg raising test (SLRT) was positive with the right leg lifted 45 o off the bed and the left leg lifted 30 o off the bed. Urine retention happened 3 days after admission. Cystometry (CMG) revealed poor compliance of urinary bladder. MRI of lumbar spine disclosed generalized bulging disc between L4 and L5 level with moderate to severe thecal sac compression. (Fig. 1 and Fig. 2) Conservative treatment including analgesics and physiotherapy did not improve his symptoms. Left L4 laminotomy and microdiscectomy were performed 5 days after admission. 275
- Page 2 and 3: Cauda equina syndrome in a pediatri
J Med Sci 2011;31(6):275-277<br />
http://jms.ndmctsgh.edu.tw/3106275.pdf<br />
Copyright © 2011 JMS<br />
Received: April 28, 2011; Revised: June 13, 2011;<br />
Accepted: June 20, 2011<br />
* Correspond<strong>in</strong>g author: Shu-Shong Hsu, Division of<br />
Neurosurgery, Kaohsiung Veterans General Hospital,<br />
No. 386, Ta-chung 1st Road, Kaohsiung 813, Taiwan,<br />
Republic of Ch<strong>in</strong>a. Tel: +886-7-3468113; Fax: +886-7-<br />
3455064; E-mail : sshsu59@yahoo.com<br />
Chia-Yuan Chang, et al.<br />
<strong>Cauda</strong> <strong>Equ<strong>in</strong>a</strong> <strong>Syndrome</strong> <strong>in</strong> a <strong>Pediatric</strong> <strong>Patient</strong> <strong>due</strong> <strong>to</strong> <strong>Lumbar</strong> <strong>Disc</strong> Herniation<br />
Chia-Yuan Chang 1 , P<strong>in</strong>g-Hong Lai 2 , and Shu-Shong Hsu 1*<br />
1 Division of Neurosurgery, Department of Surgery;<br />
2 Division of Neuroradiology, Kaohsiung Veterans General Hospital, Kaohsiung,<br />
Taiwan, Republic of Ch<strong>in</strong>a<br />
<strong>Lumbar</strong> disc herniation is rare <strong>in</strong> pediatric population and the management strategy rema<strong>in</strong>s unclear. Here, we present a<br />
12-year-old boy with back pa<strong>in</strong> radiat<strong>in</strong>g <strong>to</strong> bilateral lower limbs, weakness of bilateral lower limbs and ur<strong>in</strong>e retention.<br />
MRI of L-sp<strong>in</strong>e disclosed lumbar disc herniation over L4/5 level and microdiscec<strong>to</strong>my was performed. Pos<strong>to</strong>peratively,<br />
the patient’s neurologic defi cit resolved gradually and he returned <strong>to</strong> school three weeks after operation.<br />
We reviewed the related literature and discussed the possible mechanisms and treatment of lumbar disc herniation <strong>in</strong> pediatric<br />
population.<br />
Key words: lumbar disc herniation, pediatric patient, microdiscec<strong>to</strong>my, cauda equ<strong>in</strong>a syndrome.<br />
INTRODUCTION<br />
<strong>Lumbar</strong> disc herniation is ma<strong>in</strong>ly a disease of adults<br />
and the reported lifetime occurrence rate of lumbar<br />
disc herniation was as high as 40%. 1 The <strong>in</strong>cidence of<br />
lumbar disc herniation <strong>in</strong> pediatric population is much<br />
lower than that <strong>in</strong> adults. The most common symp<strong>to</strong>m of<br />
lumbar disc herniation is back pa<strong>in</strong>, leg pa<strong>in</strong> and mo<strong>to</strong>r<br />
weakness. 2,3 <strong>Cauda</strong> equ<strong>in</strong>a syndrome <strong>due</strong> <strong>to</strong> lumbar disc<br />
herniation is rare both <strong>in</strong> adults and <strong>in</strong> pediatric population.<br />
In this paper, a pediatric patient presented with cauda<br />
equ<strong>in</strong>a syndrome <strong>due</strong> <strong>to</strong> lumbar disc herniation was reported.<br />
Previous studies are reviewed and the possible<br />
mechanism and management strategies are discussed.<br />
CASE REPORT<br />
A 12-year-old boy presented with back pa<strong>in</strong> radiat<strong>in</strong>g<br />
<strong>to</strong> bilateral lower limbs and weakness of bilateral lower<br />
limbs especially on the left side 5 days before admission.<br />
There was no trauma his<strong>to</strong>ry. Physical exam<strong>in</strong>ation<br />
revealed decreased deep tendon refl ex of bilateral ankle<br />
Fig. 1 T2-weighted sagittal MRI<br />
show<strong>in</strong>g a herniated disc at<br />
L4-L5 (two arrows)<br />
jerk reflex, grade<br />
4 muscle power of<br />
right knee fl exion,<br />
foot dorsiflexion<br />
and plantar flexion,<br />
and grade 3<br />
muscle power of<br />
left knee flexion,<br />
foot dorsiflexion<br />
and plantar flexion.<br />
Numbness of<br />
per<strong>in</strong>eal region<br />
and bilateral lateral<br />
side of lower<br />
legs was noted.<br />
No Barb<strong>in</strong>ski refl<br />
ex was observed.<br />
Straight leg rais<strong>in</strong>g<br />
test (SLRT)<br />
was positive with<br />
the right leg lifted<br />
45 o off the bed and<br />
the left leg lifted<br />
30 o off the bed. Ur<strong>in</strong>e retention happened 3 days after<br />
admission. Cys<strong>to</strong>metry (CMG) revealed poor compliance<br />
of ur<strong>in</strong>ary bladder. MRI of lumbar sp<strong>in</strong>e disclosed<br />
generalized bulg<strong>in</strong>g disc between L4 and L5 level with<br />
moderate <strong>to</strong> severe thecal sac compression. (Fig. 1 and<br />
Fig. 2) Conservative treatment <strong>in</strong>clud<strong>in</strong>g analgesics and<br />
physiotherapy did not improve his symp<strong>to</strong>ms. Left L4<br />
lam<strong>in</strong>o<strong>to</strong>my and microdiscec<strong>to</strong>my were performed 5<br />
days after admission.<br />
275
<strong>Cauda</strong> equ<strong>in</strong>a syndrome <strong>in</strong> a pediatric patient <strong>due</strong> <strong>to</strong> lumbar disc herniation<br />
Fig. 2 Axial T1-weighted (left) and T2-weighted (right)<br />
MRI of the L4-L5 level show<strong>in</strong>g generalized bulg<strong>in</strong>g<br />
disc (arrow) with severe thecal sac compression.<br />
Pos<strong>to</strong>peratively, the patient’s pa<strong>in</strong> resolved and weakness<br />
of bilateral lower limbs improvement gradually.<br />
Ur<strong>in</strong>ary catheter was removed two weeks after operation.<br />
He returned <strong>to</strong> school 3 weeks after operation and recovered<br />
completely 6 months after operation. He rema<strong>in</strong>ed<br />
symp<strong>to</strong>m free at one-year follow-up (Low Back Outcome<br />
Score > 65).<br />
DISCUSSION<br />
<strong>Lumbar</strong> disc herniation is rare <strong>in</strong> pediatric population<br />
and may be missed <strong>due</strong> <strong>to</strong> the absence of classical symp<strong>to</strong>ms.<br />
It was reported the pediatric patients constitute<br />
only 0.5-6.8% of all patients hospitalized for lumbar disc<br />
herniation. 4,5 The <strong>in</strong>cidence of surgery for disc herniation<br />
<strong>in</strong> patients younger than 20 years ranges from 0.92% <strong>to</strong><br />
2.1% of all disc surgeries. 6 The symp<strong>to</strong>ms of pediatric<br />
lumbar disc herniation are generally similar <strong>to</strong> those observed<br />
<strong>in</strong> adults. They <strong>in</strong>cluded back pa<strong>in</strong>, radicular pa<strong>in</strong>,<br />
mo<strong>to</strong>r weakness, sensory impairment and cauda equ<strong>in</strong>a<br />
syndrome. Up <strong>to</strong> 90-95% of pediatric patients have a<br />
positive SLRT which can be expla<strong>in</strong>ed by their greater<br />
nerve root tension compared with that <strong>in</strong> adults. 2,7<br />
While chronic degenerative changes constitute the<br />
ma<strong>in</strong> cause for lumbar disc herniation among adults, the<br />
etiology of lumbar disc herniation <strong>in</strong> pediatric patients<br />
is unclear. Genetic fac<strong>to</strong>rs lead<strong>in</strong>g <strong>to</strong> early degenerative<br />
changes have been considered. 8 Studies have shown that<br />
13%-57% of adolescents with lumbar disc herniation<br />
have a first-degree relative hav<strong>in</strong>g the same disorder.<br />
Various reports have also revealed strong predisposition<br />
of lumbar disc herniation by trauma while others have<br />
found little association. 9,10,11 Microtrauma which cannot<br />
be seen radiologically, may be a signifi cant contribut<strong>in</strong>g<br />
fac<strong>to</strong>r <strong>in</strong> these cases.<br />
It is diffi cult <strong>to</strong> decide on the management strategy for<br />
276<br />
lumbar disc herniation <strong>in</strong> pediatric population because<br />
the grow<strong>in</strong>g sp<strong>in</strong>e is more vulnerable <strong>to</strong> surgical trauma<br />
and iatrogenic deformities may develop after lam<strong>in</strong>ec<strong>to</strong>my.<br />
The <strong>in</strong>itial management of lumbar disc herniation<br />
<strong>in</strong> pediatric patients is the same as that <strong>in</strong> adults and<br />
<strong>in</strong>volves ma<strong>in</strong>ly conservative treatment which <strong>in</strong>cludes<br />
bed rest, analgesic, physical therapy and limitation of<br />
physical activities. Short-term <strong>to</strong> long-term success<br />
rate of conservative treatment for pediatric lumbar disc<br />
herniation without neurologic defi cits varies from 25 <strong>to</strong><br />
50%. 2,9,12 Several studies have compared the outcome<br />
between conservative treatment and discec<strong>to</strong>my. Kurth<br />
et al. found no signifi cant difference <strong>in</strong> outcome among<br />
33 pediatric patients (18 conservatively and 15 surgically<br />
treated cases) with a follow-up of 5.4 years. 13 Kev<strong>in</strong> et<br />
al. reported that among 44 new patients seek<strong>in</strong>g consultation<br />
for evaluation of lumbar disc herniation over a<br />
one-year period, only 13 underwent surgical treatment. 2<br />
Kurihara et al. reviewed 70 pediatric patients with disc<br />
herniation, only 40% of the patients responded <strong>to</strong> conservative<br />
treatment and the results after discec<strong>to</strong>my were <strong>in</strong><br />
general excellent. 9 DeLuca et al. found that over a 6-year<br />
follow-up, the rate of good results was only 25% <strong>in</strong> the<br />
nonoperative group managed with conservative treatment<br />
versus 91% <strong>in</strong> the operative group with discec<strong>to</strong>my performed.<br />
12 It has been widely agreed by most authors that<br />
pediatric patients may not respond as well <strong>to</strong> conservative<br />
treatment as adults. It may be because the herniated<br />
nucleus pulposus of children, as compared with adults,<br />
is less degenerated, more hydrated, soft and viscous. In<br />
addition, it does not dry up and resorb like a degenerated<br />
adult disc. 9,14<br />
Commonly agreed <strong>in</strong>dications for surgical <strong>in</strong>tervention<br />
on pediatric lumbar disc herniation <strong>in</strong>clude: (1)<br />
severe pa<strong>in</strong> refrac<strong>to</strong>ry <strong>to</strong> 4-6 weeks of conservative treatment,<br />
(2) disabl<strong>in</strong>g pa<strong>in</strong> affect<strong>in</strong>g one’s daily activities,<br />
(3) cauda equ<strong>in</strong>a syndrome, (4) progressive neurological<br />
defi cits, and (5) associat<strong>in</strong>g sp<strong>in</strong>al deformities. 7 As <strong>in</strong> the<br />
case of adults, surgical treatment for pediatric lumbar<br />
disc herniation comprises percutaneous endoscopic discec<strong>to</strong>my<br />
and microdiscec<strong>to</strong>my. Percutaneous endoscopic<br />
discec<strong>to</strong>my was associated with short-term success rate<br />
of 91.3 <strong>to</strong> 100% but no long-term follow-up had been<br />
reported. The short-term success rate of microdiscec<strong>to</strong>my<br />
ranged from 98 <strong>to</strong> 100% while the medium-term (5-10<br />
years) and long-term (> 10 years) success rate dropped <strong>to</strong><br />
92 and 85%, respectively. 9,12,14 How much disc material<br />
should be removed is a crucial question. A discec<strong>to</strong>my<br />
with <strong>in</strong>suffi cient nucleus removal is likely <strong>to</strong> fail while<br />
excessive nucleus removal can also lead <strong>to</strong> stenos<strong>in</strong>g
change at operated disc level and degenerative change<br />
at adjacent disc level. For pediatric patients, it is especially<br />
important <strong>to</strong> ma<strong>in</strong>ta<strong>in</strong> the <strong>in</strong>tegrity of the <strong>in</strong>ner<br />
part of the annulus where proteoglycan synthesis is the<br />
most active. 15 Serdar et al. reported 17 pediatric patients<br />
undergo<strong>in</strong>g microdiscec<strong>to</strong>my with none of them develop<strong>in</strong>g<br />
iatrogenic sp<strong>in</strong>al deformities dur<strong>in</strong>g a mean 60month<br />
follow-up. 4 It is reported that cases with long-term<br />
follow-up had higher re-operation rate than those with<br />
medium-term follow-up. Papagelopoulos et al. calculated<br />
the re-operation rate of 72 surgically treated cases us<strong>in</strong>g<br />
Survivorship Analysis and suggested that the probability<br />
that a patient would not need a re-operation was 80% at<br />
10 years and 74% at 20 years after the <strong>in</strong>itial operation. 14<br />
Sp<strong>in</strong>al fusion should not be performed rout<strong>in</strong>ely for pediatric<br />
patients unless the symp<strong>to</strong>ms contribute <strong>to</strong> <strong>in</strong>stability.<br />
Early post-operation complications <strong>in</strong>clude wound<br />
hema<strong>to</strong>ma, wound <strong>in</strong>fection and discitis which are rarely<br />
reported <strong>in</strong> pediatric patients.<br />
In conclusion, pediatric lumbar disc herniation is rare<br />
and conservative treatment should be the <strong>in</strong>itial management.<br />
For patients not respond<strong>in</strong>g <strong>to</strong> conservative<br />
treatment or hav<strong>in</strong>g neurologic deficit such as mo<strong>to</strong>r<br />
weakness or cauda equ<strong>in</strong>a syndrome, discec<strong>to</strong>my should<br />
be considered. With the operation performed by an experienced<br />
surgeon, the operat<strong>in</strong>g time of microdiscec<strong>to</strong>my<br />
can be m<strong>in</strong>imized with less blood loss and short hospital<br />
stay. Microdiscec<strong>to</strong>my is the appropriate treatment for<br />
pediatric lumbar disc herniation. Long-term follow-up is<br />
required because recurrence may occur years after treatment.<br />
DISCLOSURE<br />
The authors declare that they have no confl ict of <strong>in</strong>terest.<br />
REFERENCES<br />
1. Frymoyer JW, Pope MH, Clements JH, Wilder DG,<br />
MacPherson B, Ashikaga T. Risk fac<strong>to</strong>rs <strong>in</strong> low-back<br />
pa<strong>in</strong>. An epidemiological survey. J Bone Jo<strong>in</strong>t Surg<br />
Am 1983;65:213-218.<br />
2. Kev<strong>in</strong> SC, Ian Dunn, Thorste<strong>in</strong>n G. <strong>Lumbar</strong> microdiscec<strong>to</strong>my<br />
<strong>in</strong> pediatric patients: a large s<strong>in</strong>gle –<strong>in</strong>stitution<br />
series. J. Neurosurg: sp<strong>in</strong>e 2010;12:165-170.<br />
Chia-Yuan Chang, et al.<br />
3. Raj K, V. Kumar, N.K. Das. Adolescent lumbar disc<br />
disease : f<strong>in</strong>d<strong>in</strong>gs and outcome. Childs Nerv syst<br />
2007;23:1295-1299.<br />
4. Serdar O, Deniz K, O. Zafer T, Adnan D, M.Memet O.<br />
<strong>Lumbar</strong> disc herniation <strong>in</strong> adolescence. Pediatr neurosurg<br />
2007;43:77-81.<br />
5. Garrido E, Humphreys RP, Hendrick EB, Hoffman<br />
HJ. <strong>Lumbar</strong> disc disease <strong>in</strong> children. Neurosurgery<br />
1978;2:22-26.<br />
6. Techakapuch S. Rupture of the lumbar cartilage plate<br />
<strong>in</strong><strong>to</strong> the sp<strong>in</strong>al canal <strong>in</strong> an adolescent. A case report. J<br />
Bone Jo<strong>in</strong>t Surg Am 1981;3:481-482.<br />
7. Lei D, Zhongjun L. A review of current treatment for<br />
lumbar disc herniation <strong>in</strong> children and adolescents.<br />
Eur Sp<strong>in</strong>e J 2010;19:205-214.<br />
8. Adams MA , Roughley PJ. What is <strong>in</strong>tervertebral disc<br />
degeneration and what cause is? Sp<strong>in</strong>e 2006;31:2151-<br />
2161.<br />
9. Kurihara A, Kataoka O. <strong>Lumbar</strong> disc herniation <strong>in</strong><br />
children and adolescents. A review of 70 operated<br />
cases and their m<strong>in</strong>imum 5-year follow-up studies.<br />
Sp<strong>in</strong>e 1980;5:443-451.<br />
10. Kumar R, Kumar V, Das NK, Behari S, Mahapatra<br />
AK. Adolescent lumbar disc disease: f<strong>in</strong>d<strong>in</strong>gs and<br />
outcome. Child Nerv Syst 2007;23:1295-1299.<br />
11. Raj KV, Kumar NK, Das SB, Behari AK. Adolescent<br />
lumbar disc disease. Childs Nerv Syst 2007;23:1295-<br />
1299.<br />
12. DeLuca PF, Mason DE, Weiand R, Howard R, Bassett<br />
GS. Excision of herniated nucleus pulposus <strong>in</strong> children<br />
and adolescents. J Pediatr Orthop 1994;14:318-<br />
322.<br />
13. Kurth AA, Rau S, Wang C, Schmitt E. Treatment of<br />
lumbar disc herniation <strong>in</strong> the second decade of life.<br />
Eur Sp<strong>in</strong>e J 1996;5:220-224.<br />
14. Papagelopoulos PJ ,Shaughnessy WJ, Ebersold MJ,<br />
Bianco AJ Jr, Quast LM. Long-term outcome of<br />
lumbar discec<strong>to</strong>my <strong>in</strong> children and adolescents sixteen<br />
years of age or younger. J Bone Jo<strong>in</strong>t Surg Am<br />
1998,80:689-698.<br />
15. Bayliss MT, Johns<strong>to</strong>ne B, O’Brien JP. Proteoglycan<br />
synthesis <strong>in</strong> the human <strong>in</strong>tervertebral disc Variation<br />
with age, region and pathology. Sp<strong>in</strong>e 1988;13:972-<br />
981.<br />
277