Prions: Protein Aggregation and Infectious Diseases - Physiological ...
Prions: Protein Aggregation and Infectious Diseases - Physiological ...
Prions: Protein Aggregation and Infectious Diseases - Physiological ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
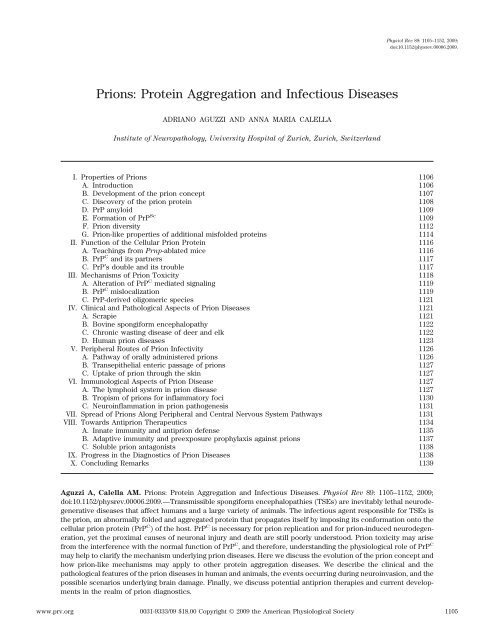
<strong>Prions</strong>: <strong>Protein</strong> <strong>Aggregation</strong> <strong>and</strong> <strong>Infectious</strong> <strong>Diseases</strong><br />
ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
Institute of Neuropathology, University Hospital of Zurich, Zurich, Switzerl<strong>and</strong><br />
I. Properties of <strong>Prions</strong> 1106<br />
A. Introduction 1106<br />
B. Development of the prion concept 1107<br />
C. Discovery of the prion protein 1108<br />
D. PrP amyloid 1109<br />
E. Formation of PrP Sc<br />
Physiol Rev 89: 1105–1152, 2009;<br />
doi:10.1152/physrev.00006.2009.<br />
F. Prion diversity 1112<br />
G. Prion-like properties of additional misfolded proteins 1114<br />
II. Function of the Cellular Prion <strong>Protein</strong> 1116<br />
A. Teachings from Prnp-ablated mice 1116<br />
B. PrP C <strong>and</strong> its partners 1117<br />
C. PrP’s double <strong>and</strong> its trouble 1117<br />
III. Mechanisms of Prion Toxicity 1118<br />
A. Alteration of PrP C mediated signaling 1119<br />
B. PrP C mislocalization 1119<br />
C. PrP-derived oligomeric species 1121<br />
IV. Clinical <strong>and</strong> Pathological Aspects of Prion <strong>Diseases</strong> 1121<br />
A. Scrapie 1121<br />
B. Bovine spongiform encephalopathy 1122<br />
C. Chronic wasting disease of deer <strong>and</strong> elk 1122<br />
D. Human prion diseases 1123<br />
V. Peripheral Routes of Prion Infectivity 1126<br />
A. Pathway of orally administered prions 1126<br />
B. Transepithelial enteric passage of prions 1127<br />
C. Uptake of prion through the skin 1127<br />
VI. Immunological Aspects of Prion Disease 1127<br />
A. The lymphoid system in prion disease 1127<br />
B. Tropism of prions for inflammatory foci 1130<br />
C. Neuroinflammation in prion pathogenesis 1131<br />
VII. Spread of <strong>Prions</strong> Along Peripheral <strong>and</strong> Central Nervous System Pathways 1131<br />
VIII. Towards Antiprion Therapeutics 1134<br />
A. Innate immunity <strong>and</strong> antiprion defense 1135<br />
B. Adaptive immunity <strong>and</strong> preexposure prophylaxis against prions 1137<br />
C. Soluble prion antagonists 1138<br />
IX. Progress in the Diagnostics of Prion <strong>Diseases</strong> 1138<br />
X. Concluding Remarks 1139<br />
Aguzzi A, Calella AM. <strong>Prions</strong>: <strong>Protein</strong> <strong>Aggregation</strong> <strong>and</strong> <strong>Infectious</strong> <strong>Diseases</strong>. Physiol Rev 89: 1105–1152, 2009;<br />
doi:10.1152/physrev.00006.2009.—Transmissible spongiform encephalopathies (TSEs) are inevitably lethal neurodegenerative<br />
diseases that affect humans <strong>and</strong> a large variety of animals. The infectious agent responsible for TSEs is<br />
the prion, an abnormally folded <strong>and</strong> aggregated protein that propagates itself by imposing its conformation onto the<br />
cellular prion protein (PrP C ) of the host. PrP C is necessary for prion replication <strong>and</strong> for prion-induced neurodegeneration,<br />
yet the proximal causes of neuronal injury <strong>and</strong> death are still poorly understood. Prion toxicity may arise<br />
from the interference with the normal function of PrP C , <strong>and</strong> therefore, underst<strong>and</strong>ing the physiological role of PrP C<br />
may help to clarify the mechanism underlying prion diseases. Here we discuss the evolution of the prion concept <strong>and</strong><br />
how prion-like mechanisms may apply to other protein aggregation diseases. We describe the clinical <strong>and</strong> the<br />
pathological features of the prion diseases in human <strong>and</strong> animals, the events occurring during neuroinvasion, <strong>and</strong> the<br />
possible scenarios underlying brain damage. Finally, we discuss potential antiprion therapies <strong>and</strong> current developments<br />
in the realm of prion diagnostics.<br />
www.prv.org 0031-9333/09 $18.00 Copyright © 2009 the American <strong>Physiological</strong> Society<br />
1105<br />
1109
1106 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
I. PROPERTIES OF PRIONS<br />
A. Introduction<br />
Prion diseases, also termed transmissible spongiform<br />
encephalopathies (TSEs), are inevitably fatal neurodegenerative<br />
conditions that affect humans <strong>and</strong> a wide variety<br />
of animals. Prion diseases may present with certain morphological<br />
<strong>and</strong> pathophysiological features that parallel<br />
other progressive encephalopathies, such as Alzheimer’s<br />
<strong>and</strong> Parkinson’s disease (12). However, prion diseases<br />
were considered unique in that they are transmissible. As<br />
it happens, the latter assertion may not be entirely correct.<br />
It has been reported that aggregates of amyloid-<br />
() peptide associated with Alzheimer’s disease behave<br />
like an infectious agent when injected into the brain of a<br />
mouse model of Alzheimer’s disease, showing a pattern of<br />
A deposition that depends on both the host <strong>and</strong> the<br />
agent (345). These findings suggest that what was considered<br />
to be a unique feature of prion disease may be a more<br />
general property of amyloids.<br />
The agent that causes TSEs was termed “prion” by<br />
Stanley B. Prusiner <strong>and</strong> is defined as “a small proteinaceous<br />
infectious particle that is resistant to inactivation<br />
by most procedures that modify nucleic acids” (403).<br />
<strong>Prions</strong> certainly differ from all other known infectious<br />
pathogens in several respects. First, prions do not appear<br />
to contain an informational nucleic acid genome longer<br />
than 50 bases that encodes for their progeny (423). Second,<br />
the only known component of the prion is a modified<br />
form of the cellular prion protein, PrP C , which is encoded<br />
by the gene Prnp. PrP C is a cell surface glycoprotein (481)<br />
of unknown function that has been identified in all mammals<br />
<strong>and</strong> birds examined to date, as well as in Xenopus<br />
laevis (482) <strong>and</strong> fish (425). Third, the central event in<br />
prion pathogenesis is the conformational conversion of<br />
PrP C into PrP Sc , an insoluble <strong>and</strong> partially protease-resistant<br />
isoform that propagates itself by imposing its abnormal<br />
conformation onto PrP C molecules.<br />
Numerous experiments have provided evidence that<br />
PrP C is a key player in prion replication as well as in<br />
prion-induced neurodegeneration. Mice lacking the prion<br />
gene are resistant to the disease (84), <strong>and</strong> PrP C expression<br />
is required for neurodegeneration in host neurons,<br />
because the presence of PrP Sc alone does not cause disease.<br />
For example, when neurografts propagating PrP Sc<br />
were implanted into Prnp knockout mice, no pathological<br />
changes were seen in PrP-deficient tissue, even in the<br />
immediate vicinity of the grafts (64). Additionally, transgenic<br />
mice expressing only a secreted form of PrP C lacking<br />
a glycosylphosphatidylinositol (GPI) anchor do not<br />
develop clinical signs of prion disease, although prion<br />
inoculation induces PrP Sc formation <strong>and</strong> aggregation of<br />
amyloid plaques (108). These findings suggest that expres-<br />
sion of membrane-anchored PrP C is necessary to initiate<br />
disease. Finally, neuron-specific ablation of PrP C in transgenic<br />
mice (321) or RNAi knockdown of PrP C expression<br />
in mice with established prion disease (519) rescues early<br />
neuronal dysfunction <strong>and</strong> prolongs the survival of mice<br />
despite the accumulation of extraneuronal PrP Sc .<br />
Attempts to identify posttranslational modifications<br />
that distinguish PrP Sc from PrP C have been mostly unsuccessful<br />
(480); however, increasing evidence indicates that<br />
they may exist (89, 122). Almost 45% of the PrP C protein<br />
is -helical with two very short stretches of -sheet (421).<br />
Conversion to PrP Sc results in a protein comprised of<br />
30% -helix <strong>and</strong> 45% -sheet. The mechanism by which<br />
PrP C is converted into PrP Sc is unknown, but PrP C appears<br />
to bind to PrP Sc , perhaps in combination with ancillary<br />
proteins, to form an intermediate complex during<br />
the formation of nascent PrP Sc (343). Transgenic mouse<br />
studies have provided genetic evidence that incoming<br />
prions in the inoculum interact preferentially with homotypic<br />
PrP C during the propagation of prions (412, 447).<br />
Prion disease is characterized by widespread neurodegeneration;<br />
therefore, affected individuals exhibit clinical<br />
symptoms of both cognitive <strong>and</strong> motor dysfunction.<br />
In addition, the disease is characterized by the propagation<br />
of infectious prions <strong>and</strong>, in many instances, the formation<br />
of amyloid plaques. The human prion diseases<br />
include Kuru, Creutzfeldt-Jakob disease (CJD), variant<br />
CJD (vCJD), Gerstmann-Sträussler-Scheinker (GSS) disease<br />
<strong>and</strong> fatal familial insomnia (FFI) (Table 1). The most<br />
common prion diseases of animals are scrapie, which<br />
affects sheep <strong>and</strong> goats, bovine spongiform encephalopathy<br />
(BSE) or “mad cow” disease, <strong>and</strong> chronic wasting<br />
disease (CWD), which affects deer <strong>and</strong> elk. Kuru was the<br />
first of the human prion diseases to be transmitted to<br />
experimental animals, <strong>and</strong> Gajdusek discovered that Kuru<br />
spread among the Fore people of Papua New Guinea<br />
through ritual cannibalism (172). The experimental <strong>and</strong><br />
presumed human-to-human transmission of Kuru led to<br />
the belief that prion diseases are infectious disorders<br />
caused by unusual viruses similar to those causing scrapie<br />
in sheep <strong>and</strong> goats. Yet autosomal dominant inheritance<br />
of CJD was first reported almost 90 years ago (260, 342),<br />
TABLE 1. Human prion diseases<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
Disease Etiology<br />
Kuru Infection<br />
Creutzfeldt-Jakob disease<br />
Iatrogenic Infection<br />
Sporadic Unknown<br />
Familial PRNP mutation<br />
Variant Presumed BSE infection<br />
Gerstmann-Sträussler-Scheinker disease PRNP mutation<br />
Fatal familial insomnia PRNP mutation<br />
BSE, bovine spongiform encephalopathy.
suggesting that CJD was also a genetic disease. The significance<br />
of familial CJD (fCJD) remained largely unappreciated<br />
until mutations were discovered in the protein<br />
coding region of the PRNP gene on the short arm of<br />
chromosome 20 (478). The earlier finding that brain extracts<br />
from patients who had died of familial prion diseases<br />
inoculated into experimental animals often transmit<br />
disease posed a conundrum that was resolved with the<br />
genetic linkage of these diseases to mutations of the<br />
PRNP gene that encodes PrP C (496). To date, all known<br />
cases of familial prion disease cosegregate with PRNP<br />
mutations.<br />
The most common form of prion disease in humans is<br />
“sporadic” CJD (sCJD) whose cause is unknown. Indeed,<br />
many attempts to show that the sporadic prion diseases<br />
are caused by infection have been unsuccessful (71, 125,<br />
324). The discovery that inherited prion diseases are<br />
caused by germ-line mutations in the PRNP gene raised<br />
the possibility that sporadic forms of these diseases might<br />
result from somatic mutations (402). Alternatively, since<br />
PrP Sc is derived from PrP C by a posttranslational process<br />
(58), sporadic prion diseases may result from the spontaneous<br />
conversion of PrP C into PrP Sc .<br />
The incidence of sCJD is low in all ethnicities <strong>and</strong> has<br />
been often said to affect one person in one million annually.<br />
However, in countries with active surveillance programs,<br />
the reported CJD incidence is often higher (13),<br />
<strong>and</strong> in Switzerl<strong>and</strong> it has reached 3.0/10 6 per year (187,<br />
429), suggesting that many cases may go undetected. Less<br />
than 1% of CJD cases arise from exposure to infected<br />
material, <strong>and</strong> most of these seem to be iatrogenic. Between<br />
5 <strong>and</strong> 15% of prion disease cases are inherited,<br />
whereas the remaining cases are sporadic. Kuru was once<br />
the most common cause of death among New Guinea<br />
women in the Fore region of the Highl<strong>and</strong>s (171, 173), but<br />
the incidence has since dissipated with the cessation of<br />
ritualistic cannibalism (341).<br />
In the past 20 years, more than 280,000 cattle suffering<br />
from BSE has provoked a major worldwide food crisis<br />
with thus far incomparable economic consequences for<br />
the European Union <strong>and</strong> other countries. In addition,<br />
transmission of BSE to humans is believed to have caused<br />
200 cases of variant CJD (vCJD). Direct experimental<br />
proof that vCJD is caused by the transmission of BSE<br />
prions to humans has not been demonstrated. However,<br />
epidemiological, biochemical, <strong>and</strong> neuropathological evidence,<br />
as well as transmission studies, strongly suggest<br />
that BSE has been transmitted to humans resulting in<br />
vCJD (106, 231, 523).<br />
In recent years, the United States has witnessed an<br />
enigmatic rise of CWD cases affecting elk <strong>and</strong> deer, <strong>and</strong><br />
there has been a recrudescence of scrapie outbreaks<br />
among European sheep flocks (e.g., Sweden, Austria, <strong>and</strong><br />
Sardinia). This resurgence of new cases might be linked<br />
to an increased sensitivity <strong>and</strong> frequency of the currently<br />
AGGREGATION AND INFECTIOUS DISEASE 1107<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
executed testing procedures. In any case, these findings<br />
have exposed our deficit in knowledge about prion epidemiology<br />
<strong>and</strong> possible transmission routes of prion diseases<br />
in humans <strong>and</strong> animals.<br />
B. Development of the Prion Concept<br />
Scrapie was originally hypothesized to be a muscle<br />
disease caused by parasites (310, 311). The transmissibility<br />
of scrapie was demonstrated in an early, seminal study<br />
(128) <strong>and</strong> led to the hypothesis that scrapie is caused by<br />
a “filterable” virus (527). The findings of Tikvah Alper <strong>and</strong><br />
colleagues (23, 24) that scrapie infectivity was resistant to<br />
inactivation by ultraviolet (UV) <strong>and</strong> ionizing irradiation<br />
resulted in a myriad of hypotheses on the chemical nature<br />
of the scrapie agent, including the clairvoyant conjecture<br />
by Griffith (197) that it may consist of a self-replicating<br />
protein.<br />
The experimental transmission of scrapie from sheep<br />
to mice (105) resulted in a much more convenient laboratory<br />
model, which yielded considerable information on<br />
the unusual infectious pathogen that causes scrapie (23–<br />
25, 182, 350, 383). Yet progress was, <strong>and</strong> in many instances<br />
continues to be, slow because quantification of<br />
infectivity in a single sample required holding many mice<br />
for at least 1 yr before accurate scoring could be accomplished<br />
(105).<br />
After scrapie incubation times were reported to be<br />
50% shorter in Syrian hamsters than in mice (329),<br />
studies were undertaken to determine whether the incubation<br />
times in hamsters could be related to the titer of<br />
the inoculated sample. There was an inverse correlation<br />
between the length of the incubation time <strong>and</strong> the logarithm<br />
of the dose of inoculated prions, which allowed for<br />
a more rapid <strong>and</strong> economical (albeit considerably less<br />
precise) bioassay (406, 408).<br />
The development of a quantitative, highly sensitive<br />
cell-based bioassay by Klohn <strong>and</strong> Weissmann was crucial<br />
for many practical purposes (270). In the scrapie cell<br />
assay (SCA), susceptible neuroblastoma cells (N2a) are<br />
exposed to prion-containing samples for 3 days, grown to<br />
confluence, passaged several times, <strong>and</strong> then the proportion<br />
of PrP Sc -containing cells is determined. In a log-log<br />
plot, the dose response is linear over two logs of prion<br />
concentrations. The SCA is about as sensitive as the<br />
mouse bioassay, 10 times faster, 2 orders of magnitude<br />
less expensive, <strong>and</strong> suitable for automation. SCA performed<br />
in a more time-consuming end point titration format<br />
(SCEPA) extends the sensitivity <strong>and</strong> shows that infectivity<br />
titers measured in tissue culture <strong>and</strong> in the<br />
mouse are similar.<br />
Once an effective protocol was developed for the<br />
preparation of partially purified fractions of scrapie agent<br />
from hamster brain, it became possible to demonstrate
1108 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
that the procedures that modify or hydrolyze proteins<br />
produce a diminution in scrapie infectivity (405, 406). At<br />
the same time, tests done in search of a scrapie-specific<br />
nucleic acid were unable to demonstrate any dependence<br />
of infectivity on a polynucleotide (403, 424), in agreement<br />
with earlier studies reporting the extreme resistance of<br />
infectivity to UV irradiation at 254 nm (23). On the basis of<br />
these findings, it seemed unlikely that the infectious<br />
pathogen capable of transmitting scrapie was a virus or a<br />
viroid. For this reason, the term prion was introduced by<br />
Prusiner to distinguish the proteinaceous infectious particles<br />
that cause scrapie, CJD, GSS, <strong>and</strong> Kuru from both<br />
viroids <strong>and</strong> viruses (403).<br />
A wealth of evidence has accumulated over the past<br />
decade supporting the protein-only hypothesis, which<br />
proposes that the main or perhaps only constituent of the<br />
infectious agent is the mammalian prion PrP Sc . Final<br />
proof of this hypothesis could be achieved if pure PrP C or,<br />
better yet, recombinant PrP produced in E. coli, could be<br />
converted into a form that elicits prion disease. A first,<br />
seminal step in this direction was the demonstration that<br />
radioactive PrP C incubated with unlabeled PrP Sc in a<br />
cell-free system generated radioactive PrP Sc , as characterized<br />
by its physical properties (97). However, an increase<br />
of infectivity was not demonstrated in these experiments<br />
(510). Another important advance was provided<br />
by the invention of protein misfolding cyclic<br />
amplification (PMCA), a technique by which PrP Sc is amplified<br />
by cycles of sonication followed by incubation<br />
with brain homogenate (433, 434). Soto <strong>and</strong> co-workers<br />
(94) showed that amplification of PrP Sc was accompanied<br />
by an amplification of infectivity. The use of purified PrP C<br />
instead of brain homogenate as a substrate for the in vitro<br />
PrP Sc generation decreased the efficiency of amplification,<br />
suggesting that additional cofactors may facilitate<br />
the conversion of PrP C to PrP Sc (134). In addition, initial<br />
attempts to use recombinant forms of PrP as a substrate<br />
in PMCA have failed. Caughey <strong>and</strong> co-workers (30) have<br />
since succeeded in carrying out PMCA using bacterially<br />
expressed hamster PrP as a substrate. While this represents<br />
a major advance in many ways, the sensitivity is not<br />
quite as high as with brain homogenate (5, 30).<br />
In an intriguing study, Supattapone <strong>and</strong> co-workers<br />
(135) identified the minimal components (PrP C , copurified<br />
lipids, <strong>and</strong> single-str<strong>and</strong>ed polyanionic molecules)<br />
required for the amplification of proteinase K-resistant<br />
PrP, <strong>and</strong> they convincingly showed that prion infectivity<br />
can be generated de novo in brain homogenates<br />
derived from healthy hamsters using PMCA. Inoculation<br />
of healthy hamsters with de novo formed prions<br />
caused prion disease (135), providing strong support<br />
for the prion hypothesis.<br />
Additional support for the prion hypothesis comes<br />
from the demonstration that infectious material can be<br />
generated in mice by altering the sequence of the prion<br />
protein (461). Moderate overexpression in transgenic<br />
mice of a mouse PrP with two point mutations (170N,<br />
174T) that subtly affect the structure of its globular domain<br />
causes a fully penetrant lethal spongiform encephalopathy<br />
with cerebral PrP plaques. This genetic disease<br />
was reproduced with 100% attack rate by intracerebral<br />
inoculation of brain homogenate to mice overexpressing<br />
wild-type PrP (154), <strong>and</strong> from the latter to wild-type mice,<br />
but not to PrP-deficient mice. This work provides an<br />
important step forward in elucidating the role of a specific<br />
domain of the prion protein in the generation of infectivity<br />
(471).<br />
C. Discovery of the Prion <strong>Protein</strong><br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
The dependence of prion infectivity on a protein<br />
intensified the search for a scrapie-specific protein. Although<br />
the insolubility of scrapie infectivity made purification<br />
problematic, this property, along with its relative<br />
resistance to degradation by proteases, was used by<br />
Prusiner to facilitate purification (409, 411). Radioiodination<br />
of partially purified brain fractions revealed a protein<br />
unique to preparations from scrapie-infected hamsters<br />
(55, 404), <strong>and</strong> in subcellular fractions of hamster brain<br />
enriched for scrapie infectivity, a protease-resistant<br />
polypeptide of 27–30 kDa (designated PrP 27–30 ) was identified<br />
(55, 337).<br />
Purification of PrP 27–30 to near-homogeneity allowed<br />
determination of its NH 2-terminal amino acid sequence,<br />
which permitted the synthesis of an isocoding mixture of<br />
oligonucleotides that was subsequently used to identify<br />
incomplete PrP cDNA clones from hamster (370) <strong>and</strong><br />
mouse (107). cDNA clones encoding the entire open reading<br />
frames (ORFs) of Syrian hamster <strong>and</strong> mouse PrP were<br />
subsequently isolated (39, 305). The above experiments<br />
established that PrP is encoded by a chromosomal gene,<br />
<strong>and</strong> not by a nucleic acid in the infectious scrapie prion<br />
particle (39, 370). Levels of PrP mRNA remain unchanged<br />
throughout the course of scrapie infection, an unexpected<br />
observation that led to the identification of the normal<br />
Prnp gene product, a protein of 33–35 kDa designated<br />
PrP C (39, 370). PrP C is protease sensitive <strong>and</strong> soluble in<br />
nondenaturing detergents, whereas PrP 27–30 is the protease-resistant<br />
core of a 33- to 35-kDa disease-specific<br />
protein, designated PrP Sc , which is insoluble in detergents<br />
(346).<br />
The entire ORF of all known mammalian <strong>and</strong> avian<br />
Prnp genes is contained within a single exon (39, 170, 230,<br />
515). This feature of the Prnp gene eliminates the possibility<br />
that PrP Sc arises from alternative RNA splicing (39,<br />
516), although mechanisms such as RNA editing, protein<br />
splicing, <strong>and</strong> alternative initiation of translation remain a<br />
possibility (54, 241, 246). The PRNP gene is located in the<br />
short arm of human chromosome 20 <strong>and</strong> in a homologous
egion in mouse chromosome 2 (479). Hybridization studies<br />
demonstrated 0.002 Prnp gene sequences per ID 50<br />
unit in purified prion fractions, strongly suggesting that a<br />
nucleic acid encoding PrP Sc cannot constitute a component<br />
of the infectious prion particle (370). This is a major<br />
feature that distinguishes prions from viruses, including<br />
retroviruses which carry cellular oncogenes <strong>and</strong> “satellite<br />
viruses” bearing coat proteins from viruses that had previously<br />
infected the host.<br />
D. PrP Amyloid<br />
The discovery of PrP 27–30 in fractions enriched for<br />
scrapie infectivity was accompanied by the identification<br />
of rod-shaped particles in the same fractions (404, 410).<br />
The fine structure of these particles, which had been<br />
originally described by Mertz as “scrapie-associated<br />
fibrils” (344), failed to reveal any regular substructure<br />
characteristic of most viruses (526). Conversely, prion<br />
rods are indistinguishable from many purified amyloids<br />
(114). This analogy was extended when the prion rods<br />
were found to display the tinctorial properties of amyloids<br />
(410). Small amyloidotropic dyes, such as derivatives of<br />
Congo red <strong>and</strong> thioflavins, bind with various degrees of<br />
selectivity to protein aggregates having an extensive cross<br />
-pleated sheet conformation <strong>and</strong> sufficient structural<br />
regularity <strong>and</strong> give rise to an enhanced fluorescence (thioflavins)<br />
or apple-green birefringence under cross-polarized<br />
light (Congo red) (47, 138). However, these dyes are<br />
not suitable for recognizing prefibrillary species <strong>and</strong> amyloid<br />
deposits of diverse morphological origin. Advancement<br />
in this direction has been provided by luminescent<br />
conjugated polymers (LCPs), a recently developed, novel<br />
class of amyloidotropic dyes (216, 366, 367).<br />
The amyloid plaques in the brains of humans <strong>and</strong><br />
other animals with prion disease contain PrP, as determined<br />
by immunoreactivity <strong>and</strong> amino acid sequencing<br />
(45, 132, 265, 426, 488). Solubilization of PrP 27–30 into<br />
liposomes with retention of infectivity (169) suggests that<br />
large PrP polymers are not required for infectivity, although<br />
it is certainly possible that PrP Sc oligomers may<br />
constitute nucleation centers pivotal to prion replication<br />
(238, 288). To systematically evaluate the relationship<br />
between infectivity, converting activity, <strong>and</strong> the size of<br />
various PrP Sc -containing aggregates, Caughey <strong>and</strong> coworkers<br />
(464) partially disaggregated PrP Sc . The resulting<br />
species were fractionated by size <strong>and</strong> analyzed by light<br />
scattering <strong>and</strong> nondenaturing gel electrophoresis. Intracerebral<br />
inoculation of the different fractions into hamsters<br />
revealed that with respect to PrP content, infectivity<br />
peaked markedly with 17–27 nm (300–600 kDa) particles.<br />
These results suggest that nonfibrillar particles, with<br />
masses equivalent to 14–28 PrP molecules, are the most<br />
efficient initiators of TSE disease (464). As with other<br />
AGGREGATION AND INFECTIOUS DISEASE 1109<br />
diseases characterized by protein aggregation, such as<br />
Alzheimer’s disease <strong>and</strong> other amyloidoses, the formation<br />
of large amyloid fibrils might be a protective process that<br />
sequesters the more dangerous subfibrillar oligomers of<br />
the amyloidogenic peptide or protein into relatively innocuous<br />
deposits.<br />
Prion-like amyloids also exist in lower eukaryotes<br />
such as yeast. Fungal prions are non-PrP related molecules<br />
that include HET-s, Ure2p, <strong>and</strong> Sup35 proteins,<br />
which can adopt both nonamyloid <strong>and</strong> self-perpetuating<br />
amyloid structures. In contrast to PrP Sc , the conversion of<br />
these proteins into their prion-like conformations has<br />
been shown to have important physiological functions in<br />
yeast. The conversion of Ure2p <strong>and</strong> Sup35 into their amyloid<br />
forms (URE3 <strong>and</strong> PSI, respectively) regulates the<br />
transcription <strong>and</strong> translation of specific yeast genes (237,<br />
492). Aggregated HET-s regulates heterokaryon incompatibility,<br />
a fungal self/non-self recognition phenomenon that<br />
prevents various forms of parasitism (509). So far there<br />
have been only a few reported instances of mammalian<br />
proteins that are functionally regulated in a nonpathological<br />
way by interconversion between nonamyloid <strong>and</strong> amyloid<br />
forms. A remarkable example is the synthesis of<br />
melanin, which involves the formation of amyloid structures<br />
(158). In addition, it has been proposed that proteins<br />
involved in establishing long-term memory might do so by<br />
converting reversibly to <strong>and</strong> from an amlyoid-like state<br />
(455, 457).<br />
E. Formation of PrP Sc<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
It remains to be established whether any form of<br />
PrP C can act as a substrate for PrP Sc formation, or<br />
whether a restricted subset of PrP molecules are precursors<br />
for PrP Sc (511). It is also unknown whether reactive<br />
transition states between the two exist. Several experimental<br />
results argue that PrP molecules destined to<br />
become PrP Sc exit to the cell surface prior to their conversion<br />
into PrP Sc (59, 99, 494). Similar to other GPIanchored<br />
proteins, PrP C appears to localize in cholesterolrich,<br />
nonacidic, detergent-insoluble membranes known as<br />
rafts (26, 195, 253, 456, 495). Within the raft compartment,<br />
GPI-anchored PrP C is apparently either converted into<br />
PrP Sc or partially degraded (343, 495). Chemical <strong>and</strong> enzymatic<br />
treatment of purified PrP 27–30 leads to the release<br />
of glycolipid components, suggesting that PrP Sc could be<br />
tethered to the membrane by a GPI anchor (481).<br />
The role of the GPI membrane anchor in the formation<br />
of PrP Sc in vivo has been addressed by Chesebro et<br />
al. (108), who have established a transgenic mouse model<br />
expressing anchorless, <strong>and</strong> hence secreted, PrP. When<br />
these transgenic mice were subsequently infected with<br />
protease-resistant PrP Sc , they developed significant amyloid<br />
plaque pathology in the brain, but clinical manifesta-
1110 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
tions were minimal. In contrast, combined expression of<br />
anchorless <strong>and</strong> wild-type PrP resulted in accelerated clinical<br />
scrapie (108).<br />
1. Structures of purified PrP C <strong>and</strong> PrP Sc<br />
Early low-resolution structural studies indicated that<br />
PrP C had a high -helix content (40% of the protein) <strong>and</strong><br />
relatively little -sheet (3% of the protein) (379). These<br />
findings were further refined by Wüthrich <strong>and</strong> colleagues<br />
who determined the fine structure of PrP C by nuclear<br />
magnetic resonance spectroscopy (Fig. 1A) (229, 421),<br />
<strong>and</strong> later also by crystallographic studies (271). The NH2 proximal half of the molecule is not structured at all,<br />
whereas the COOH-proximal half is arranged in three<br />
-helices corresponding, for the human PrP C , to the residues<br />
144–154, 173–194, <strong>and</strong> 200–228, interspersed with<br />
an antiparallel -pleated sheet formed by -str<strong>and</strong>s at<br />
residues 128–131 <strong>and</strong> 161–164. A single disulfide bond is<br />
found between cysteine residues 179 <strong>and</strong> 214 (421, 422,<br />
531). It is unlikely that the NH2 terminus is r<strong>and</strong>omly<br />
coiled in vivo, since functional studies in transgenic mice<br />
imply that the domain comprising amino acids 32–121<br />
carries out important physiological functions (453). It is<br />
possible that the flexible tail of PrP C acquires a defined<br />
structure when PrP C is present within membrane rafts<br />
(362).<br />
In contrast to PrP C , the -sheet content of PrP Sc<br />
comprises 40% of the protein, whereas -helices comprise<br />
30% of the protein as measured by Fourier-transform<br />
infrared (379) <strong>and</strong> CD spectroscopy (Fig. 1B) (436). No<br />
high-resolution structure is available for PrP Sc , although<br />
interesting models have been conjectured on the basis of<br />
electron crystallography studies (524). Prion rods of the<br />
NH2-terminally truncated form of PrP Sc derived by limited<br />
proteolysis, PrP 27–30 , exhibit green-gold birefringence after<br />
staining with Congo red, indicating that this isoform<br />
has a high -sheet content (410). Indeed, PrP 27–30 poly-<br />
FIG. 1. Structural features of PrP C <strong>and</strong> PrP Sc . A: NMR structure of<br />
the mouse prion protein domain (121–231). The ribbon diagram indicates<br />
the positions of the three helices (yellow) <strong>and</strong> the antiparallel<br />
two-str<strong>and</strong>ed -sheet (cyan). The connecting loops are displayed in<br />
green if their structure is well defined <strong>and</strong> in magenta otherwise. The<br />
disulfide bond between Cys-179 <strong>and</strong> Cys-214 is shown in white. The<br />
NH 2-terminal segment of residues 121–124 <strong>and</strong> the COOH-terminal segment<br />
220–231 are disordered <strong>and</strong> not displayed. (Figure kindly provided<br />
by S. Hornemann.) B: Fourier transform infrared spectroscopy of prion<br />
proteins. The amide I b<strong>and</strong> (1,700–1,600 cm 1 ) of transmission FTIR<br />
spectra of PrP C (black line), PrP Sc (gray line), <strong>and</strong> PrP 27–30 (dotted line).<br />
These proteins were suspended in a buffer in D 2O containing 0.15 M<br />
sodium chloride/10 mM sodium phosphate, pD 7.5 (uncorrected)/0.12%<br />
ZW. The spectra are scaled independently to be full scale on the ordinate<br />
axis (absorbance). [From Pan et al. (379).] C: electron micrographs of<br />
negatively stained <strong>and</strong> immunogold-labeled prion proteins. Each panel<br />
shows in following order PrP C , PrP Sc , <strong>and</strong> Prion rods, composed of<br />
PrP 27–30 , that were negatively stained with uranyl acetate. Bar, 100 nm.<br />
[From Pan et al. (379).]<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org
merized into rod-shaped particles with an ultrastructural<br />
appearance of amyloid (Fig. 1C) containing 50% -sheet<br />
<strong>and</strong> 20% -helix content (103, 176, 435). In contrast to<br />
PrP 27–30 , neither purified PrP C nor PrP Sc forms aggregates<br />
detectable by electron microscopy (338, 379).<br />
2. Models describing the replication of prions<br />
Transgenic mouse studies have provided genetic<br />
(412) <strong>and</strong> biochemical (343) evidence that the conversion<br />
of PrP C to PrP Sc occurs through the formation of a PrP C /<br />
PrP Sc complex. However, such a complex has never been<br />
isolated to purity. Consequently, it is unclear whether<br />
PrP C binds to one or more additional macromolecules<br />
during the process of PrP C to PrP Sc conversion. The formation<br />
of a PrP C /PrP Sc complex may be facilitated when<br />
the amino acid sequences of the two PrP isoforms are<br />
identical. For instance, hamster PrP differs from mouse<br />
PrP at 16 of 254 positions, perhaps explaining the strong<br />
species barrier between mice <strong>and</strong> hamsters. Differences<br />
in amino acid sequence delay the onset of prion disease<br />
by prolonging the incubation time (446). As the sequence<br />
specificity of PrP Sc formation is more important for the<br />
conversion to protease resistance than for the initial binding<br />
steps, additional intermolecular interactions between<br />
PrP C <strong>and</strong> PrP Sc may be required to complete the process<br />
of conversion to the protease-resistant state (228).<br />
The level of PrP C expression appears to be directly<br />
proportional to the rate of PrP Sc formation <strong>and</strong>, thus, inversely<br />
related to the length of the incubation time. Prnp o/o<br />
mice are resistant to prions <strong>and</strong> do not propagate scrapie<br />
infectivity (84, 407, 439). Mice hemizygous (Prnp /o ) for<br />
ablation of the Prnp gene have prolonged incubation times<br />
when inoculated with mouse prions (83, 326).<br />
According to the “protein only” hypothesis, there<br />
are two models to explain the conformational conversion<br />
of PrP C into PrP Sc . The “template-directed refolding”<br />
hypothesis predicates an instructionist role for<br />
PrP Sc on PrP C (Fig. 2A). Alternatively, the seeded nucleation<br />
hypothesis suggests that PrP Sc exists in equilibrium<br />
with PrP C . In a nondisease state, such an equilibrium<br />
would be heavily shifted toward the PrP C conformation,<br />
such that only minute amounts of PrP Sc<br />
would coexist with PrP C . If this were the case, PrP Sc<br />
could not possibly represent the infectious agent, since<br />
it would be ubiquitous. According to this “seeded nucleation”<br />
hypothesis (238), the infectious agent would<br />
consist of a highly ordered aggregate of PrP Sc molecules.<br />
The aggregated state would be an intrinsic property<br />
of infectivity. Monomeric PrP Sc would be harmless,<br />
but it might be prone to incorporation into nascent<br />
PrP Sc aggregates (Fig. 2B) (19).<br />
The recently developed PMCA (92, 93, 196, 432,<br />
434) is designed to mimic PrP Sc autocatalytic replication<br />
(Fig. 3). In the PMCA, PrP Sc is amplified in a cyclic<br />
AGGREGATION AND INFECTIOUS DISEASE 1111<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
FIG. 2. Models for the conformational conversion of PrP C into<br />
PrP Sc . A: the “refolding” or template assistance model postulates an<br />
interaction between exogenously introduced PrP Sc <strong>and</strong> endogenous<br />
PrP C , which is induced to transform itself into further PrP Sc . A highenergy<br />
barrier may prevent spontaneous conversion of PrP C into PrP Sc .<br />
B: the “seeding” or nucleation-polymerization model proposes that PrP C<br />
<strong>and</strong> PrP Sc are in a reversible thermodynamic equilibrium. Only if several<br />
monomeric PrP Sc molecules are mounted into a highly ordered seed, can<br />
further monomeric PrP Sc be recruited <strong>and</strong> eventually aggregate to amyloid.<br />
Fragmentation of PrP Sc aggregates increases the number of nuclei,<br />
which can recruit further PrP Sc <strong>and</strong> thus results in apparent replication<br />
of the agent.<br />
manner by incubating small amounts of PrP Sc -<br />
containing brain homogenate with uninfected, PrP C -<br />
containing brain homogenate, resulting in the conversion<br />
of PrP C to PrP Sc . The latter forms aggregates that<br />
are sonicated to generate multiple smaller units functioning<br />
as a seed for the continued formation of new<br />
PrP Sc aggregates.
1112 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
FIG. 3. Schematic representation of the protein misfolding cyclic amplification (PMCA) reaction. PrP C is recruited into growing aggregates of<br />
PrP Sc ; hence, it undergoes conformational conversion <strong>and</strong> becomes PrP Sc . During PMCA, the growing PrP Sc species are disrupted by repeated<br />
sonication in the presence of detergents. This treatment generates an exp<strong>and</strong>ed population of converting units for the continuous recruitment of<br />
PrP C . The whole procedure is repeated several times. PrP C is shown as light gray spheres. PrP Sc is shown as trapezium. The original seed is in dark<br />
gray, <strong>and</strong> the newly formed PrP Sc is in light gray.<br />
An important part of the prion replication process is<br />
the propagation of prions through the fragmentation of<br />
existing fibrils. This mechanism has been experimentally<br />
verified for yeast prions (62, 491). There are indications<br />
that similar processes govern the growth of mammalian<br />
prions (94, 295) as well as non-prion-related amyloid<br />
fibrils (139).<br />
Analysis of yeast prions has shown that the mechanical<br />
frangibility of formed prion fibrils plays a key role in<br />
fibril growth, complexity, <strong>and</strong> diversity (492). The fragility<br />
of yeast prions varies substantially between different<br />
classes of fibrils, but is relatively homogeneous within a<br />
single class (237, 492). Yeast prion classes with an aggressive<br />
tendency to multiply in vivo have been found to be<br />
composed of amyloid fibrils with the highest propensity to<br />
fragment. It is interesting to note that in terms of their<br />
mechanical rigidity, amyloid fibrils can be very heterogeneous<br />
(272), implying a substantial potential for intrinsic<br />
variability in their breakage rates. Although prion propagation<br />
in mammalian tissues is likely to be inherently<br />
more convoluted, recent observations indicate that the<br />
propagation of mammalian prion strains may be kinetically<br />
similar to fungal prions. Indeed, shorter fibrils,<br />
which may result from breakage of frangible structures,<br />
are more infectious than longer fibrils (464), an observation<br />
consistent with the fact that a larger number of free<br />
ends in a short fibril population leads to more rapid<br />
conversion of soluble cellular prion protein into misfolded<br />
fibrillar form <strong>and</strong> eventually overwhelming cellular<br />
clearance mechanisms.<br />
In agreement with this idea, an inverse correlation<br />
was recently found between the stability of prion aggregates<br />
<strong>and</strong> incubation times in vivo (296), a finding that is<br />
closely analogous to results obtained in yeast prions<br />
(499). Furthermore, in in vitro growth assays of many<br />
amyloid fibril systems, it has been noted that agitation<br />
significantly enhances the overall conversion rate of proteins<br />
into fibrillar forms (255, 371, 467), indicating that<br />
fibril breakage is an essential factor determining the rate<br />
of amyloid formation. In living systems, the rate constants<br />
for prion replication are clearly influenced not only by the<br />
intrinsic strength of PrP Sc aggregates, but also by other<br />
cellular components. Molecular chaperones in yeast, for<br />
instance, have been identified as important players in the<br />
rate of prion replication (454).<br />
F. Prion Diversity<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
One of the most puzzling phenomena in prion biology<br />
is the existence of prion strains. Prion strains are defined<br />
as infectious isolates that, when transmitted to identical
hosts, exhibit distinct prion-disease phenotypes. The phenotypic<br />
traits may include distinct patterns of protein<br />
aggregate deposition, incubation times, histopathological<br />
lesion profiles, <strong>and</strong> specific neuronal target areas. Most of<br />
these traits are relatively stable across serial passages.<br />
Often new distinct strains can be observed upon transmission<br />
of prions across an interspecies barrier or into<br />
animals of the same species expressing different polymorphisms<br />
of the prion gene, a phenomenon sometimes referred<br />
to as a “strain mutation” (76, 504).<br />
The diversity of scrapie prions was initially noted in<br />
goats inoculated with “hyper” <strong>and</strong> “drowsy” isolates (386).<br />
Scrapie isolates or “strains” from goats with a drowsy<br />
syndrome transmitted a similar syndrome to inoculated<br />
recipients, whereas those from goats with a “hyper” or<br />
ataxic syndrome transmitted an ataxic form of scrapie to<br />
recipient goats. Subsequent studies in mice have also<br />
demonstrated the existence of diverse scrapie strains that<br />
produce characteristic phenotypes in inoculated recipients<br />
(78, 136, 137) with respect to incubation times, the<br />
distribution of central nervous system (CNS), <strong>and</strong> the<br />
formation of amyloid plaques, although the clinical signs<br />
of scrapie tend to be similar.<br />
The identification of strains through the inoculation<br />
of mice is time-consuming, cumbersome, <strong>and</strong> prohibitively<br />
expensive. Moreover, the reliability of the resulting<br />
classification is based on mere correlative evidence. However,<br />
over time, a number of biochemical correlates for<br />
prion strains have been identified (Table 2) (9), <strong>and</strong> it is<br />
expected that these criteria will facilitate the study <strong>and</strong><br />
the diagnosis of prion strains.<br />
1. Prion strains <strong>and</strong> variations in patterns of disease<br />
Although defining of prion strains according to biochemical<br />
characteristics is useful in terms of nomenclature<br />
<strong>and</strong> classification of prion diseases, it certainly does<br />
not explain why strains display different organ tropisms.<br />
TABLE 2. Synopsis of currently used prion strain differentiation assays<br />
AGGREGATION AND INFECTIOUS DISEASE 1113<br />
For example, some prion strains preferentially propagate<br />
in the CNS <strong>and</strong> exhibit low abundance in secondary lymphoid<br />
organs. This neurotropic pattern of tissue distribution<br />
is observed in “classical” BSE in bovines. In other<br />
strains, PrP Sc <strong>and</strong>/or prion infectivity are detected not<br />
only in the CNS but also, to a large extent, in secondary<br />
lymphoid organs. These lymphotropic prion strains include<br />
vCJD, CWD (460), <strong>and</strong> many scrapie strains (20).<br />
However, these differences are not absolute. For example,<br />
in patients with sCJD, it was originally believed that<br />
prions were present in the CNS <strong>and</strong> other peripheral<br />
tissues, but not in secondary lymphoid organs (74). However,<br />
it is now acknowledged that PrP Sc can also be found<br />
in the spleen <strong>and</strong> skeletal muscle of patients with sCJD<br />
(183, 388).<br />
What defines the organ tropism of a given prion strain<br />
is still a completely open question. One might speculate<br />
that tropism is defined by the tertiary or (more probably)<br />
by the supramolecular structure of the prion agent, which<br />
influences its ability to bind to or interact with specific<br />
molecules (for example, receptors), <strong>and</strong> as a result affects<br />
specific cell types (9). The phenomenon of cellular prion<br />
tropism has been elegantly demonstrated by Charles<br />
Weissmann’s group in an array of cell lines which replicate<br />
different prion strains to varying degrees (319). The<br />
differential cell tropism of the various prion strains suggests<br />
the requirement for cell-specific cofactors, be they<br />
chaperones, specific uptake receptors, RNA species, a<br />
particular lipid environment, a specific posttranslationally<br />
modified PrP molecule, or a particular prion replicating<br />
subcellular environment. This hypothesis relies on the<br />
assumption that cofactors supporting the conversion of<br />
distinct prion strains exist in defined cell groups (16).<br />
2. Molecular basis of prion strains<br />
The mechanism by which isolate-specific information<br />
is carried by prions remains enigmatic. A dwindling num-<br />
Assay Principle Test Substrate Speed Cost Reference Nos.<br />
Incubation period in indicator mice Mice Years 164<br />
Histological lesion profile Mice Years 79, 163<br />
Histoblots Immunohistology Days 493<br />
Conformation-dependent immunoassay ELISA Days 437<br />
Conformational stability assay Western blot Days 390<br />
Conformation assay Infrared spectroscopy Days 101<br />
PK cleavage site Western blot Days 51<br />
Detection with NH 2-terminal antibodies Western blot Days 396<br />
Glycosylation profile Western blot Days 220<br />
Amyloid detection by thioflavin <strong>and</strong> Congo red stains Histochemistry Hours 460<br />
Luminescent-conjugated polymers Histochemistry Hours 462<br />
Cell panel assay Cell culture Weeks 319<br />
Most assays have high discriminatory power between few specific strains (e.g., glycosylation profiles for bovine spongiform encephalopathy<br />
<strong>and</strong> variant Creutzfeldt-Jakob disease) but may perform poorly with other strains. , Low; , high; , extremely high. Adapted<br />
from Aguzzi (9).<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org
1114 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
ber of investigators still contend that scrapie is caused by<br />
a viruslike particle containing a scrapie-specific nucleic<br />
acid that encodes the information expressed by each<br />
isolate (78). But to date, no such polynucleotide has been<br />
identified, despite the use of a wide variety of techniques,<br />
including the measurement of nucleic acids in purified<br />
preparations. An alternative hypothesis is that PrP Sc alone<br />
is capable of transmitting the disease <strong>and</strong> that the characteristics<br />
of PrP Sc are modified by a cellular nucleic acid<br />
(512). This accessory cellular polynucleotide is postulated<br />
to induce its own synthesis upon transmission from one<br />
host to another, but there is currently no experimental<br />
evidence to support its existence.<br />
In striking contrast, mice expressing Prnp transgenes<br />
have demonstrated that the level of PrP expression is<br />
inversely related to the incubation time (412). Taken together,<br />
these observations indicate that PrP Sc itself is the<br />
molecule in which prion “strain”-specific information is<br />
encrypted. Preliminary immunochemical evidence suggests<br />
that PrP Sc of different strains expose different<br />
epitopes (438) <strong>and</strong> display different degrees of stability to<br />
chaotropic salts (390). Infrared spectroscopy measurements<br />
have shown that types of PrP Sc associated with<br />
distinct hamster TSE strains can possess different conformations,<br />
even though they are derived from PrP with<br />
the same amino acid sequence (101). This could be interpreted<br />
as indirect evidence for conformational differences<br />
or could indicate that different PrP Sc strains associate<br />
with different molecules of proteinaceous or other<br />
nature.<br />
Both PrP C <strong>and</strong> PrP Sc exist in three main glycosylation<br />
states: unglycosylated, monoglycosylated, <strong>and</strong> diglycosylated.<br />
The relative ratios of these three forms of PrP Sc<br />
differ in various prion strains. In some cases, such differences<br />
are remarkably robust <strong>and</strong> are widely used for<br />
prion strain typing. On the basis of the fragment size <strong>and</strong><br />
the relative abundance of individual b<strong>and</strong>s identified by<br />
gel electrophoresis, three distinct patterns of PrP Sc (types<br />
1–3) have been identified for sporadic <strong>and</strong> iatrogenic CJD<br />
cases (118, 381). In contrast, all cases of vCJD display a<br />
novel pattern, designated type 4 by Collinge <strong>and</strong> type III<br />
by Parchi <strong>and</strong> Gambetti (Fig. 4). Interestingly, brain extracts<br />
from BSE-infected cattle as well as BSE-inoculated<br />
macaques exhibited a type 4 pattern. Even more intriguing,<br />
transmission of BSE or vCJD to mice produced<br />
mouse PrP Sc with a type 4 pattern indistinguishable from<br />
the original inoculum (219). These findings strongly support<br />
the hypothesis that vCJD is the result of BSE transmission<br />
to humans.<br />
It is clear that in some patients suffering from CJD,<br />
multiple distinct types of CJD-associated PrP Sc molecules<br />
coexist within the same patient (396). However,<br />
the molecular basis for these differences in glycosylation<br />
is poorly understood, <strong>and</strong> the mechanisms by<br />
which differences in PrP Sc glycosylation states affect<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
FIG. 4. Representation of the three glycosylated PrP Sc moieties<br />
(un-, mono-, <strong>and</strong> diglycosylated PrP Sc ) in immunoblots of brain extracts<br />
after digestion with proteinase K. Different inocula result in specific<br />
mobilities of the three PrP b<strong>and</strong>s as well as different predominance of<br />
certain b<strong>and</strong>s (top panel). These characteristic patterns can be retained,<br />
or changed to other predictable patterns after passage in wild-type mice<br />
(bottom panel). On the basis of the fragment size <strong>and</strong> the relative<br />
abundance of individual b<strong>and</strong>s, three distinct patterns (PrP Sc types 1–3)<br />
were defined for sCJD <strong>and</strong> iCJD cases. In contrast, all cases of vCJD <strong>and</strong><br />
of BSE displayed a novel pattern, designated as type 4 pattern.<br />
the disease remain unanswered. It has been proposed<br />
that the relative prevalence of distinct glycoforms may<br />
determine the structure of infectious PrP seeds <strong>and</strong><br />
thereby determine strain properties (116), although little<br />
physical evidence for this assertion existed until recently.<br />
This hypothesis is certainly compatible with the report<br />
that strains differ in their ability to infect hosts with<br />
restricted PrP glycosylation, <strong>and</strong> certain strains may only<br />
produce disease in hosts whose PrP C harbors specific<br />
carbohydrate side chains (501).<br />
G. Prion-like Properties of Additional<br />
Misfolded <strong>Protein</strong>s<br />
The “seeded nucleation” theory (238) described for<br />
PrP may also apply to amyloid formation in other protein<br />
misfolding disorders (PMDs). In fact, protein conformational<br />
changes associated with the pathogenesis of most<br />
PMDs result in the formation of abnormal proteins that<br />
are rich in -sheet structure, partially resistant to proteolysis,<br />
<strong>and</strong> have a high tendency to form larger-order<br />
aggregates, similar to PrP Sc . Amyloid formation depends<br />
on the slow interaction of misfolded protein monomers to<br />
form oligomeric nuclei, around which a faster phase of<br />
elongation takes place. The ability of oligomeric species<br />
to seed their own growth is analogous to the self-propagating<br />
activity of prions.<br />
These theoretical considerations are supported by<br />
extensive experimental data (474). In addition, it has been
eported that polyglutamine aggregates (420) <strong>and</strong> tau aggregates<br />
(167) can be internalized by mammalian cells in<br />
culture. These internalized fibrillar aggregates may then<br />
selectively recruit soluble cytoplasmic proteins <strong>and</strong> stimulate<br />
further misfolding of otherwise stable intracellular<br />
proteins. From a molecular st<strong>and</strong>point, all PMDs can be<br />
considered “infectious” in the sense that misfolded <strong>and</strong><br />
aggregated conformers act as a templates for the recruitment<br />
of native proteins. However, in no PMDs other than<br />
PrP Sc pathologies has bona fide “microbiological” infectivity<br />
been detected, <strong>and</strong> none of the non-PrP aggregation<br />
diseases has ever given rise to macroepidemics such as<br />
Kuru <strong>and</strong> BSE.<br />
Some experimental amyloidoses in mammals have<br />
shown evidence of being transmissible in the sense that<br />
amyloid taken from an amyloidotic individual can sometimes<br />
greatly accelerate amyloidosis in another individual.<br />
However, it is important to note that such “transmissions”<br />
have only been shown under experimental conditions<br />
in which the recipient animal is highly primed for<br />
susceptibility to amyloidosis <strong>and</strong> would be expected to<br />
spontaneously develop amyloidosis over time. Typical examples<br />
are AA amyloidosis <strong>and</strong> Alzheimer’s disease (AD).<br />
Most cases of AA amyloidosis in mammals appear to<br />
occur spontaneously due to chronic inflammation or genetic<br />
peculiarities that elevate blood levels of serum amyloid<br />
A (SAA) <strong>and</strong> predispose the organism to AA amyloid<br />
formation. AA amyloid is characterized by the accumulation<br />
of aggregated SAA NH 2-terminal-derived peptides in<br />
organs such as the kidney, liver, <strong>and</strong> spleen. Inoculation<br />
of unaffected mice with tissue extracts from amyloidotic<br />
mice can rapidly induce amyloidosis, as long as the recipients<br />
are “primed” for amyloidosis with proinflammatory<br />
treatments such as silver nitrate injections (261, 308).<br />
Given the “infectious” characteristics of AA amyloidosis,<br />
transmission between captive cheetahs may explain<br />
the high incidence of AA amyloidosis observed in this<br />
species. Acceleration of amyloidosis in mice upon oral<br />
administration of AA amyloid suggests a plausible fecaloral<br />
route for the natural transmission of AA amyloidosis<br />
in cheetahs. Indeed, amyloidotic cheetahs shed AA amyloid<br />
in the feces, <strong>and</strong> this fecal amyloid can accelerate AA<br />
amyloidosis when injected intravenously into silver nitrate-primed<br />
mice (533).<br />
However, unlike wild cheetahs, captive cheetahs exhibit<br />
chronic inflammation <strong>and</strong> high blood SAA levels<br />
(359). These factors could make them susceptible to<br />
spontaneous amyloidosis, as it is the case with silver<br />
nitrate-treated mice. Therefore, the high incidence of<br />
amyloidosis in captive cheetahs might also be due to<br />
spontaneous disease, rather than infection with amyloid<br />
from other animals. This raises the important question of<br />
whether, in the case of non-PrP Sc amyloids, inoculation<br />
with the amyloid actually initiates the disease, as is<br />
AGGREGATION AND INFECTIOUS DISEASE 1115<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
clearly the case with legitimate TSE prions, or merely<br />
enhances an already ongoing pathogenic process (96).<br />
Several attempts have been made to transmit AD to<br />
experimental animals, which have yielded intriguing, yet<br />
conflicting, results. An early report of buffy coat-borne AD<br />
transmission to hamsters (327) initially caused great consternation,<br />
but was later found to be irreproducible. Marmosets<br />
injected with brain homogenates from individuals<br />
with AD developed scattered deposits of the amyloid-<br />
protein (A) in the brain parenchyma <strong>and</strong> cerebral vasculature<br />
6–7 yr after inoculation (35). However, extensive<br />
studies by Gajdusek <strong>and</strong> colleagues (74) have failed to<br />
transmit AD <strong>and</strong> other dementias to primates.<br />
Jucker <strong>and</strong> co-workers (345) showed that the injection<br />
of the A peptide derived from human AD brains to<br />
transgenic mice overexpressing the A precursor protein<br />
APP induced cerebral -amyloidosis. The pathology in the<br />
APP transgenic mice was determined by both the host <strong>and</strong><br />
the inoculum (345). The authors postulated the existence<br />
of A strains that can initiate <strong>and</strong> accelerate aggregation<br />
<strong>and</strong> A pathology. It remains to be seen whether different<br />
A strains with distinct biochemical or neuropathological<br />
characteristics occur in humans. Once again, as was the<br />
case with the AA inoculation studies mentioned above, it<br />
is unclear whether inoculation with A amyloid causes<br />
amyloidosis or simply accelerates an ongoing pathogenic<br />
process, since transgenic recipients ultimately develop<br />
amyloid pathology in the brain, even without inoculation<br />
with A amyloid extracts.<br />
Another major unresolved issue is the extent to<br />
which the induced amyloidotic lesions can spread from<br />
localized sites of seeding by the inoculum to other sites<br />
within the host. Surprisingly, a recent study reported that<br />
healthy fetal tissue grafted into the brains of Parkinson’s<br />
disease patients acquired cytoplasmic -synuclein-rich<br />
Lewy bodies, suggesting that misfolded -synuclein<br />
spreads to healthy cells <strong>and</strong> acts as a template for the<br />
conversion of native -helices to pathogenic -sheets<br />
(299).<br />
Type 2 diabetes is yet another disease whose pathogenesis<br />
may involve ordered protein aggregation. Evidence<br />
for this was discovered early on (373) but was<br />
largely forgotten for almost a century. It is now evident<br />
that aggregation of islet amyloid polypeptide (IAPP) is an<br />
exceedingly frequent feature of type 2 diabetes. IAPP<br />
amyloid damages the insulin-producing -cells within<br />
pancreatic islets <strong>and</strong> may crucially contribute to the<br />
pathogenesis of diabetes (233). It is unknown, however,<br />
whether IAPP deposition simply accrues linearly with<br />
IAPP production, or whether it spreads in a prion-like<br />
fashion from one pancreatic islet to the next.<br />
In summary, the role of protein misfolding <strong>and</strong> aggregation<br />
in various human diseases has been clearly<br />
established in the past decade, yet an important challenge<br />
for the coming years will be to determine whether the
1116 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
prion mechanism of disease transmission might be operating<br />
in other human diseases, some of which are highly<br />
prevalent.<br />
II. FUNCTION OF THE CELLULAR PRION<br />
PROTEIN<br />
PrP C , following the cleavage of a 22-amino acid<br />
(aa) signal peptide, is exported to the cell surface as an<br />
N-glycosylated, GPI-anchored protein of 208–209 aa.<br />
PrP C contains a long NH 2-proximal flexible r<strong>and</strong>om-coil<br />
sequence, which is followed by a globular COOH-proximal<br />
domain. The structurally less-defined NH 2 proximal<br />
region consists of residues 23–124 <strong>and</strong> contains a<br />
stretch of several octapeptide repeats (OR), flanked by<br />
two positively charged clusters, CC1 (aa 23–27) <strong>and</strong><br />
CC2 (aa 95–110). These domains are linked by a hydrophobic<br />
stretch of amino acids known as the HC region<br />
(aa 111–134) (Fig. 5).<br />
The structure of the globular half of human PrP C is<br />
identical to many other mammals, as expected from the<br />
high degree of sequence identity (309). Interestingly, despite<br />
the low sequence identity between PrP C in chicken,<br />
turtle, or frog, <strong>and</strong> the mammalian isoforms, the major<br />
structural features of PrP C are remarkably preserved in<br />
nonmammalian species (88).<br />
Full-length PrP C is found in non-, mono-, or diglycosylated<br />
forms, corresponding to the variable occupancy of<br />
glycosyl groups on residues Asn-181 <strong>and</strong> Asn-197 in human<br />
<strong>and</strong> Asn-180 <strong>and</strong> Asn-196 in mice (201). A rather large<br />
variety of N-glycans are found attached to both full-length<br />
<strong>and</strong> truncated PrP C (380, 428), which may be differentially<br />
distributed in various areas of the central nervous system<br />
(49, 133). The physiological significance of PrP C glycosylation<br />
is unknown.<br />
Despite advances in the characterization of PrP C<br />
structure, the physiological function of PrP C is still unclear.<br />
An unrealistic plethora of possible functions have<br />
been ascribed to PrP. Therefore, there is a lingering suspicion<br />
that each of these reports represents a specific<br />
aspect of a more complex reality whose full picture is still<br />
not entirely understood. Importantly, it is not yet clear<br />
whether the physiological function of PrP C is actually<br />
linked to toxicity associated with prion diseases.<br />
A. Teachings From Prnp-Ablated Mice<br />
Obviously, the study of PrP knockout mice has thus<br />
far failed to elucidate the molecular function of the protein.<br />
This is particularly sobering when one considers the<br />
fact that independent lines of mice lacking PrP C have<br />
been generated by homologous recombination in embryonic<br />
stem cells in many laboratories. Mice with disruptive<br />
gene modifications restricted to the open reading frame<br />
are known as Prnp o/o (Zurich I) (85) <strong>and</strong> Prnp / (Edinburgh)<br />
(325). These mice were found to develop normally,<br />
although a number of subtle abnormalities have been<br />
described (120, 368, 498) whose molecular basis remains<br />
undefined. Among other functions, it has been suggested<br />
that PrP C may have a role in the synaptic machinery of the<br />
olfactory bulb (293). However, the reported involvement<br />
of PrP C in synaptic hippocampal activity has been the<br />
subject of intense controversy (301).<br />
The only molecularly well-defined phenotype of<br />
Prnp o/o mice is their resistance to prion inoculation<br />
(84). However, it seems rather unlikely that a protein as<br />
highly conserved among species as PrP C has evolved<br />
purely for the purpose of bestowing susceptibility to<br />
prion diseases upon organisms. If the function of PrP C<br />
were completely unrelated to prion disease pathogenesis,<br />
PrP C would be just one of many proteins whose<br />
function awaits clarification. Otherwise, the function of<br />
PrP C may reflect, in a subtle way, prion-induced damage.<br />
However, Prnp ablation does not elicit disease,<br />
even when induced postnatally (322). Therefore, prion<br />
pathology is unlikely to occur due to a simple loss of<br />
PrP C function. If PrP C possessed enzymatic activity or<br />
transduced a signal (similarly to many other GPI-linked<br />
proteins), one could hypothesize that conversion to<br />
PrP Sc alters PrP C substrate specificity or signal transduction<br />
strength, conferring as a result a toxic dominant<br />
function. Therefore, underst<strong>and</strong>ing the function of<br />
PrP C may be instrumental to deciphering prion pathol-<br />
FIG. 5. Outline of the primary structure of the cellular prion protein including posttranslational modifications. A secretory signal peptide resides<br />
at the extreme NH 2 terminus. CC 1 <strong>and</strong> CC 2 define the charged clusters. OR indicates the octapeptide repeat, <strong>and</strong> four are present. HC defines the<br />
hydrophobic core. MA denotes the membrane anchor region. S-S indicates the single disulfide bridge, <strong>and</strong> the glycosylation sites are designated as<br />
CHO. The numbers describe the position of the respective amino acids.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org
ogy, <strong>and</strong> perhaps even to devising therapeutic approaches.<br />
Glockshuber et al. (190) noted that PrP C had similarities<br />
to membrane-anchored signal peptidases, but<br />
their observation has not been substantiated by functional<br />
data. PrP C can bind copper (67, 505), but reports<br />
of increased copper content in neurons lacking PrP C<br />
have been called into question by contradictory findings<br />
(506). The idea that PrP C might be a superoxide<br />
dismutase (68, 69) was perceived as particularly attractive<br />
in view of its multiple copper-binding sites. However,<br />
PrP C does not provide any measurable contribution<br />
to dismutase activity in vivo (234, 506), although it<br />
has been suggested that NH 2-proximally-truncated PrP C<br />
may suppress endogenous dismutase activity (441).<br />
B. PrP C <strong>and</strong> Its Partners<br />
Perhaps PrP C <strong>and</strong> PrP Sc do not possess any intrinsic<br />
biological activity of their own, but modify the<br />
function of other proteins. GPI-anchored proteins must<br />
interact with transmembrane adaptors on the same cell<br />
or an adjacent cell to influence intracellular signal<br />
transduction pathway. This supposition has led to the<br />
search for PrP-interacting partners using methods such<br />
as yeast-two hybrid, cross-linking experiments, <strong>and</strong> coimmunoprecipitations.<br />
All known PrP C interaction partners<br />
have been summarized in a recent review (10).<br />
Putative PrP C interacting proteins include membrane<br />
proteins (receptors, enzymes, caveolin-1, Na -K -<br />
ATPase, <strong>and</strong> a potassium channel), cytoplasmic proteins<br />
(components of the cytoskeleton, heat-shock proteins,<br />
<strong>and</strong> adaptor proteins involved in signaling), <strong>and</strong><br />
even nuclear proteins. Recently, transgenic mice expressing<br />
functional tagged prion protein have been<br />
used to characterize the PrP C interactome (431). However,<br />
many studies used to identify such interactors are<br />
fraught with methodological issues. PrP C is exposed to<br />
the extracellular space, <strong>and</strong> therefore, it is questionable<br />
whether conventional yeast two-hybrid screens, which<br />
artificially expose PrP C to the cytosolic compartment,<br />
represent an appropriate method to investigate PrP C<br />
interaction partners. The same concerns may apply to<br />
chemical cross-linking experiments. Cross-linking<br />
fuses together any proteins that reside in the same<br />
microenvironment, even if they do not necessarily interact<br />
with each other. Furthermore, the choice of detergent<br />
conditions in coimmunoprecipitation experiments<br />
is also crucial, since it should allow for weak <strong>and</strong><br />
transient protein-protein interactions, but should destroy<br />
any potential artificial or postlysis nonspecific<br />
interactions. Ultimately, it would be desirable to validate<br />
reported interactions by physiological read-outs,<br />
yet this lofty goal has not been attained for most of the<br />
c<strong>and</strong>idates described thus far.<br />
AGGREGATION AND INFECTIOUS DISEASE 1117<br />
C. PrP’s Double <strong>and</strong> Its Trouble<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
After the original report by the Weissmann laboratory<br />
(85), several independent Prnp knockout mouse<br />
lines were generated, including Prnp / (Nagasaki),<br />
Rcm0, <strong>and</strong> Prnp / (Zurich II) (356, 427, 440). These<br />
endeavors have led to very surprising insights. All of the<br />
latter mice, but none of the Zurich I mice, developed<br />
ataxia <strong>and</strong> Purkinje cell loss later in life. The discrepancy<br />
among the different lines of PrP knockout mice was not<br />
resolved until a novel gene (Prnd), encoding a protein<br />
called Doppel (Dpl), was discovered. Prnd is localized 16<br />
kb downstream of Prnp. In all three lines of PrP C -deficient<br />
mice developing ataxia <strong>and</strong> Purkinje cell loss, a<br />
splice acceptor site to the third exon of Prnp was deleted.<br />
This placed Prnd under transcriptional control of the<br />
Prnp promoter, resulting in the formation of chimeric<br />
transcripts <strong>and</strong> overexpression of Dpl in the brain (513).<br />
The Prnd gene is evolutionarily conserved from humans<br />
to sheep <strong>and</strong> cattle <strong>and</strong> shares roughly 25% homology<br />
with the COOH-proximal two-thirds of PrP C ,<br />
but it lacks the PrP C octapeptide repeats <strong>and</strong> hydrophobic<br />
region. Structural studies indicate that Dpl contains<br />
three -helices, similar to PrP C , <strong>and</strong> two disulfide<br />
bridges between the second <strong>and</strong> third helix (307, 465). Dpl<br />
mRNA is expressed at high levels in testis <strong>and</strong> heart,<br />
moderately in spleen <strong>and</strong> some other organs <strong>and</strong>, notably,<br />
at very low levels in brain of adult wild-type mice. However,<br />
elevated Prnd mRNA transcripts have been detected<br />
during embryogenesis <strong>and</strong> in the brains of newborn mice,<br />
thus arguing for a possible function of Dpl in brain development<br />
(298). To probe the function of Dpl, the Prnd gene<br />
was inactivated in embryonic stem cells (43). Similarly to<br />
mice lacking PrP C , mice devoid of Dpl survive to adulthood<br />
<strong>and</strong> do not show obvious phenotypical alterations,<br />
suggesting that Dpl is dispensable for embryogenesis <strong>and</strong><br />
postnatal development (44). The similarities between<br />
PrP C <strong>and</strong> Dpl in primary amino acid sequence, in structure,<br />
<strong>and</strong> in subcellular localization suggest related biological<br />
functions (42). Therefore, a possible role of PrP C<br />
<strong>and</strong> Dpl during development may be masked by functional<br />
redundancy. To address this possibility, Prnp/Prnd<br />
double knockouts were generated using transallelic targeted<br />
meiotic recombination (177). Offspring carrying the<br />
double deletion exhibited no abnormalities, except for<br />
male sterility, <strong>and</strong> they did not develop ataxia, implicating<br />
a causal role for Dpl overexpression in the Zurich II<br />
phenotype. Furthermore, Dpl did not appear to compensate<br />
for the loss of any unrecognized function of PrP.<br />
Why the overexpression of Dpl is deleterious is still<br />
unclear. Neurodegeneration is not uniquely associated<br />
with overexpression of Dpl. Transgenic mice overexpressing<br />
partially deleted Prnp variants provoke spontaneous<br />
neurodegenerative disease, <strong>and</strong> some domains are<br />
also essential for restoring prion susceptibility (Table 3).
1118 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
TABLE 3. Summary of transgenic mutant for PrP<br />
PrP Deletion Mutants Phenotype Rescue by PrP (if applicable) Prion Propagation Reference Nos.<br />
PrP 1-22 231# Cerebellar disorder No No 314<br />
PrP 23-88 No Yes 360, 361<br />
PrP 23-88 C178A No No 360, 361<br />
PrP 23-88 95-107 No No 360, 361<br />
PrP 23-88 108-121 No No 360, 361<br />
PrP 23-88 122-140 Short-lived protein 360<br />
PrP 23-88 141-176 No Yes 360, 483<br />
PrP 23-88 141-221 Cerebellar disorder No No 484<br />
PrP 23-88 177-200 Storage disease No No 360<br />
PrP 23-88 201-217 Storage disease No No 360<br />
PrP 32-80 No Yes 153<br />
PrP 32-93 No Yes 154, 453<br />
PrP 32-106 No No 453*<br />
PrP 32-121 Cerebellar disorder Yes No 453<br />
PrP 32-134 Cerebellar disorder Yes No 453*<br />
PrP 94-134 Cerebellar disorder Yes Not done 40<br />
PrP 104-114 No Not done 204<br />
PrP 105-125 Cerebellar disorder Yes Not done 297<br />
PrP 114-121 No No 40, 225<br />
PrP 231# No Yes 108<br />
PrP 144# Short-lived protein 360<br />
PrP PG 14 Cerebellar disorder No Yes 109<br />
The left column denotes the individual mutants. The column named “phenotype” indicates presence or absence of phenotypic abnormalities<br />
in transgenic mice when expressed on a PrP-deficient genetic background; when the phenotype is rescued by endogenous PrP is indicated in the<br />
next column. The column named “prion propagation” describes the susceptibility of transgenic mice or transfected cell lines to prions. #Stop codon.<br />
*E. Flechsig, I. Hegyi, A. Aguzzi, <strong>and</strong> C. Weissman, unpublished results.<br />
Deletions of amino acids 32–121 or 32–134 (collectively<br />
termed PrP) confer strong neurotoxicity to PrP C in vivo,<br />
which indicates that PrP is a functional antagonist of<br />
PrP C (414, 453). Furthermore, a small deletion within the<br />
hydrophobic stretch (amino acids 94–134) is sufficient to<br />
produce a highly neurotoxic molecule (40). This pathology<br />
can be abrogated by the reintroduction of wild-type,<br />
full-length PrP C . Because the lack of PrP C itself does not<br />
induce an obvious phenotype, the latter pathologies imply<br />
the existence of pathways in which PrP C is functionally<br />
active. Hence, mice expressing PrP variants may allow for<br />
the identification of functionally relevant domains within<br />
PrP C (10).<br />
III. MECHANISMS OF PRION TOXICITY<br />
Despite considerable knowledge about the characteristics<br />
of the TSE infectious agent, its mechanism of replication,<br />
<strong>and</strong> the association of PrP Sc with neurodegeneration,<br />
the molecular pathways leading to cerebral<br />
damage are, for the most part, unknown. Depletion of<br />
PrP C is an unlikely cause, in view of the finding that<br />
abrogation of PrP does not cause scrapielike neuropathological<br />
changes (85), even when elicited postnatally (322).<br />
Moreover, it was observed that depletion of PrP C in mice<br />
with established prion infection reversed early spongiform<br />
degeneration <strong>and</strong> prevented neuronal loss <strong>and</strong> progression<br />
to clinical disease (321, 323). Importantly, this<br />
occurred despite the accumulation of extraneuronal<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
PrP Sc to levels similar to terminally ill, wild-type infected<br />
animals. These data suggest that PrP Sc might not be directly<br />
responsible for neurodegeneration; it is more likely<br />
that the toxicity of PrP Sc depends on some PrP C -dependent<br />
process culminating in neuronal dysfunction <strong>and</strong><br />
death (63, 64).<br />
The first experimental evidence in support of this<br />
hypothesis was provided when neural tissue overexpressing<br />
PrP C was grafted into the brains of PrP-deficient mice<br />
(153). Following scrapie inoculation, these mice remained<br />
free of symptoms for at least 70 wk, exceeding the survival<br />
time of scrapie-infected donor mice by at least sevenfold<br />
(64). Therefore, the presence of a continuous<br />
source of PrP Sc does not exert any clinically detectable<br />
adverse effects on a mouse devoid of PrP C . On the other<br />
h<strong>and</strong>, the grafted tissue developed characteristic histopathological<br />
features of scrapie after inoculation. The<br />
course of the disease in the graft was very similar to that<br />
observed in the brain of scrapie-inoculated wild-type mice<br />
(63). Since the grafts had extensive contact with the<br />
recipient brain, prions could navigate between the two<br />
compartments, as shown by the fact that inoculation of<br />
wild-type animals engrafted with PrP-expressing neuroectodermal<br />
tissue resulted in scrapie pathology in both graft<br />
<strong>and</strong> host tissue. Nonetheless, histopathological changes<br />
never extended into host tissue, even at the latest stages<br />
(450 days), although PrP Sc was detected in both grafts<br />
<strong>and</strong> recipient brain, <strong>and</strong> immunohistochemistry revealed<br />
PrP deposits in the hippocampus, <strong>and</strong> occasionally in the
parietal cortex, of all animals (64). The distribution of<br />
PrP Sc in the white matter tracts of the host brain suggests<br />
diffusion within the extracellular space (239) rather than<br />
axonal transport. Thus prions moved from the grafts to<br />
some regions of the PrP-deficient host brain without causing<br />
pathological changes or clinical disease.<br />
These findings suggest that the expression of PrP C by<br />
an infected cell, rather than the extracellular deposition<br />
of PrP Sc , is one of the critical prerequisites for the development<br />
of scrapie pathology. Furthermore, what is important<br />
is not only the expression of PrP, but also its<br />
location at the plasma membrane. Indeed, expression of a<br />
Prnp variant that lacks the peptide responsible for anchoring<br />
membrane GPI molecules resulted in transgenic<br />
mice that failed to develop disease after prion infection in<br />
spite of PrP Sc plaque formation in their brains (108). Also,<br />
the blood <strong>and</strong> hearts of GPI-negative transgenic mice<br />
contained both abnormal protease-resistant PrP as well<br />
as infectious prions (500). Evidently, removal of the GPI<br />
anchor abolishes the activation of downstream pathways<br />
<strong>and</strong> susceptibility to clinical disease while preserving the<br />
competence of soluble PrP C to support prion replication.<br />
This observation is consistent with a growing body of<br />
evidence that PrP C may function as a signaling molecule.<br />
However, it is still possible that abnormal topology or<br />
altered trafficking of PrP C might also underlie toxicity, or<br />
perhaps the formation of a toxic form of PrP termed PrP*<br />
by Charles Weissmann (511), other than PrP Sc is responsible<br />
for spongiosis, gliosis, <strong>and</strong> neuronal death. This<br />
theory could explain why in several instances (e.g., fatal<br />
familial insomnia) localized spongiform pathology is detectable<br />
although very little PrP Sc is present (21).<br />
A. Alteration of PrP C Mediated Signaling<br />
Although it is unlikely that the toxic activity of PrP Sc<br />
results primarily from loss of PrP C function, neurons<br />
derived from Prnp-deficient mice were originally reported<br />
to be more susceptible to the induction of apoptosis<br />
by serum deprivation. This effect could be rescued by<br />
expression of either B-cell lymphoma protein 2 (BCL2) or<br />
PrP C (286). Furthermore, it was shown that PrP C exerts<br />
its cytoprotective function by decreasing the rate of apoptosis<br />
induced by particular apoptotic stimuli such as Bax<br />
overexpression or tumor necrosis factor (TNF)-. Bax<br />
overexpression normally induces apoptosis in human<br />
neuronal cells, but coexpression of Bax with wild-type<br />
PrP C , but not of PrP lacking the octarepeats, could reverse<br />
this effect (60). Therefore, PrP C can be neuroprotective<br />
against various insults, suggesting that its conversion<br />
to PrP Sc could abrogate this function <strong>and</strong> induce<br />
neurodegeneration.<br />
A second possibility is that the binding of PrP Sc to<br />
PrP C triggers a signal transduction pathway leading to<br />
AGGREGATION AND INFECTIOUS DISEASE 1119<br />
neuronal damage. This hypothesis is supported by a report<br />
that injection of antibodies that recognize <strong>and</strong> crosslink<br />
PrP C in the mouse hippocampus results in rapid <strong>and</strong><br />
extensive neuronal apoptosis (469), although in the intervening<br />
5 years since this publication, no further insights<br />
have come forth to explain this phenomenon.<br />
B. PrP C Mislocalization<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
Abnormal topology or altered trafficking of PrP C has<br />
also been proposed to underlie PrP-related neuronal toxicity.<br />
After processing in the endoplasmic reticulum (ER)<br />
<strong>and</strong> Golgi apparatus, where it is glycosylated, mature<br />
PrP C is attached to the cell surface by its GPI anchor at its<br />
COOH terminus. PrP C can adopt at least two transmembrane<br />
topologies in the ER, Ctm PrP <strong>and</strong> Ntm PrP, which<br />
have either their COOH or NH 2 terminus in the ER<br />
lumen, respectively. It has been suggested that Ctm PrP<br />
<strong>and</strong> Ntm PrP normally comprise only a small portion of<br />
cellular PrP C , <strong>and</strong> an excess of Ctm PrP induces neurodegeneration<br />
(204, 205). Some PrP mutations favor<br />
Ctm PrP formation <strong>and</strong> are associated with a disease state<br />
characterized by low levels of PrP Sc accumulation. Thus<br />
the propensity for the formation of the Ctm PrP <strong>and</strong> Ntm PrP<br />
intermediates might lead to neurotoxicity in the absence<br />
of PrP Sc formation (Fig. 6).<br />
Another suggested mechanism of PrP-mediated neurotoxicity<br />
is aberrant PrP C trafficking resulting in the<br />
toxic accumulation of PrP C in the cytoplasm (Fig. 6).<br />
Here, it is important to consider the mechanisms controlling<br />
protein synthesis <strong>and</strong> degradation. The fidelity of<br />
protein synthesis is ensured by quality control within the<br />
ER; misfolded proteins undergo retrograde transport to<br />
the cytosol, become polyubiquitinylated, <strong>and</strong> are degraded<br />
by the proteasome through a process called ERassociated<br />
degradation (ERAD). Both wild-type <strong>and</strong> misfolded<br />
forms of PrP C undergo ERAD (313, 529). It has<br />
been shown in vitro that the transfer of newly synthesized<br />
PrP C to the cytoplasm by ERAD, <strong>and</strong> its cytosolic accumulation<br />
through the pharmacological inhibition of the<br />
proteasome, leads to PrP Sc -like formation <strong>and</strong> neurotoxicity<br />
(312). Furthermore, the artificial expression of PrP in<br />
the cytosol in transgenic animals expressing a construct<br />
lacking ER-targeting <strong>and</strong> GPI-anchoring signals causes<br />
severe neurodegeneration (314).<br />
Recently, Rane et al. (417) have described a possible<br />
mechanism to explain the accumulation of cy(PrP) during<br />
TSE neurodegeneration. Chronic ER stress, produced by<br />
PrP Sc accumulation, leads to persistent activation of a<br />
“preemptive” quality control system (pQC) that aborts ER<br />
translocation of PrP, thereby facilitating proteasome-mediated<br />
degradation of PrP in the cytosol. This pathway<br />
constitutes a defense mechanism to prevent nascent protein<br />
entry into the ER lumen during conditions of com-
1120 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
FIG. 6. Toxicity mediated by abnormal topology or altered trafficking of PrP C . The normal cellular isoform of prion protein, PrP C (green coils),<br />
is synthesized, folded, <strong>and</strong> glycosylated in the endoplasmic reticulum (ER), where its glycosyl phosphatidylinositol (GPI) anchor is added, before<br />
further modification in the Golgi complex. Mature PrP C translocates to the outer leaflet of the plasma membrane. Instead, Ctm PrP <strong>and</strong> Ntm PrP are<br />
unusual transmembrane forms, generated in the ER, which have their COOH or NH 2 terminus in the ER lumen, respectively. It has been suggested<br />
that misfolded <strong>and</strong> aberrantly processed PrP (cyPrP <strong>and</strong> Ctm PrP, respectively) (orange coils), which would normally be degraded by the proteasomes<br />
through the ER-associated degradation (ERAD) pathway, aggregate in the cytoplasm <strong>and</strong> cause cell death. Putative proteasomal inhibition or<br />
malfunction during prion disease would contribute to this route of toxicity. Induction of ER stress by PrP Sc may lead to translocation of nascent<br />
PrP C molecules to the cytosol for proteasomal degradation as a way to alleviate the overloaded ER (pQC pathway). However, this mechanism of<br />
defense turns negative under chronic ER stress conditions, overwhelming the proteasome <strong>and</strong> leading to the cytosolic accumulation of potentially<br />
toxic PrP molecules (dashed lines).<br />
promised ER function. However, under chronic ER stress<br />
conditions, the proteasome may become overwhelmed,<br />
resulting in PrP accumulation in the cytosol. According to<br />
the study of Rane et al. (417), even a modest increase in<br />
PrP routing to pQC for prolonged periods of time causes<br />
clinical <strong>and</strong> histological neurodegenerative changes reminiscent,<br />
in some aspects, of those observed in prion<br />
diseases.<br />
Although ER stress in prion diseases is well documented<br />
(217), the relevance or even the existence of cy(PrP)<br />
continues to be rather controversial (142, 152). Furthermore,<br />
the transgenic mice with increased PrP translocation<br />
to the pQC pathway reported by Rane et al. (417) showed a<br />
relatively mild neurodegenerative phenotype that resembles<br />
only a subset of TSE pathology, <strong>and</strong> other cellular pathways<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
may also be contributing to prion-induced neurodegeneration<br />
(472). A role for dysfunction of the ubiquitin-proteasome<br />
system (UPS) in the pathogenesis of prion disease was<br />
also suggested: neuronal propagation of prions in the presence<br />
of mild proteasome impairment triggered a neurotoxic<br />
mechanism involving the intracellular formation of cytosolic<br />
PrP Sc aggresomes that, in turn, activated caspase-dependent<br />
neuronal apoptosis. A similar effect was also seen in vivo in<br />
brains of prion-infected mice (285). In a follow-up study, the<br />
same group reported that disease-associated prion protein<br />
specifically inhibited the proteolytic -subunits of the 26S<br />
proteasome. Upon challenge with recombinant prion <strong>and</strong><br />
other amyloidogenic proteins, only the prion protein in a<br />
nonnative -sheet conformation inhibited the 26S proteasome<br />
at stoichiometric concentrations. Furthermore, there
appears to be a direct relationship between prion neuropathology<br />
<strong>and</strong> impairment of the UPS in prion-infected UPSreporter<br />
mice (284). Together, these data suggest a possible<br />
mechanism of intracellular neurotoxicity mediated by misfolded<br />
prion protein.<br />
C. PrP-Derived Oligomeric Species<br />
The presence of highly organized <strong>and</strong> stable fibrillar<br />
deposits in the brain of patients <strong>and</strong> animals suffering<br />
from prion diseases initially led to the reasonable conjecture<br />
that this material is a causative agent of neurodegeneration.<br />
However, the most highly infective form of the<br />
mammalian prion protein is an oligomeric species of 20<br />
molecules, <strong>and</strong> such small aggregates are the most effective<br />
initiators of transmissible spongiform encephalopathies<br />
(464).<br />
More recent findings from other disorders associated<br />
with protein misfolding <strong>and</strong> aggregation, such as AD <strong>and</strong><br />
Parkinson’s disease, have raised the possibility that precursors<br />
to amyloid fibrils, particularly including low-molecular-weight<br />
oligomers <strong>and</strong>/or structured protofibrils,<br />
may represent the most toxic pathogenic species. In this<br />
respect, it is certainly plausible to speculate that the<br />
mechanism leading to neurotoxicity in prion disease<br />
could be similar to that of other disorders associated with<br />
protein misfolding.<br />
In AD, the severity of cognitive impairment correlates<br />
with the levels of low-molecular-weight species of<br />
A, rather than with the amyloid burden (202, 451). In<br />
addition, transgenic mice (290, 352), as well as Drosophila<br />
expressing A1–42 <strong>and</strong> A1–40 (127, 236), show deficits<br />
in synaptic plasticity before significant accumulation<br />
of amyloid. The existence of a toxic oligomeric intermediate<br />
is further supported by evidence that the aggressive<br />
“arctic” (E693G) mutation of the amyloid -precursor<br />
protein, associated with heritable early-onset manifestation<br />
of AD, has been found in vitro to enhance protofibril,<br />
but not fibril, formation (364).<br />
The toxicity of early aggregates has also been shown<br />
for Parkinson’s disease. In patients harboring mutations<br />
associated with juvenile Parkinson’s disease or early-onset<br />
forms of Parkinsonism, the loss of nigral <strong>and</strong> locus<br />
coeruleus neurons occurs in the absence of Lewy bodies<br />
(intracellular fibrillar deposits) (262). In transgenic fly or<br />
rat models of Parkinson’s disease, neuronal degeneration<br />
is not associated with the formation of detectable intracellular<br />
deposits (32, 304). Furthermore, transgenic mice<br />
exhibit substantial motor deficiencies <strong>and</strong> loss of dopaminergic<br />
neurons in the presence of nonfibrillar -synuclein<br />
deposits in various regions of the brain (330).<br />
Toxicity of smaller aggregates appears not to be restricted<br />
to the brain. For example, transthyretin (TTR) is<br />
an amyloidogenic protein implicated in systemic senile<br />
AGGREGATION AND INFECTIOUS DISEASE 1121<br />
amyloidosis (517) <strong>and</strong> familial amyloidotic polyneuropathy<br />
(124). The primary toxic species in TTR-associated<br />
diseases appear to be low-molecular-weight oligomers<br />
that do not stain with Congo red (470, 477).<br />
The toxicity of aggregated “preamyloid” proteins appears<br />
to be a fairly general phenomenon. For example, the<br />
prefibrillar forms of the non-disease-related HypF-N from<br />
E. coli, the SH3 domain from bovine phosphatidylinositol<br />
3-kinase, lysozyme from horse, <strong>and</strong> apomyoglobin from<br />
sperm whale are all highly toxic to cultured fibroblasts<br />
<strong>and</strong> neurons, whereas the monomeric native states <strong>and</strong><br />
the amyloid-like fibrils (formed in vitro) displayed very<br />
little, if any, toxicity (81, 320, 466). The finding that polyclonal<br />
antisera can bind to protofibrillar species from<br />
different sources, but not to their corresponding monomeric<br />
or fibrillar states, suggests that soluble amyloid<br />
oligomers have some important common structural elements<br />
(252).<br />
With the assumption that oligomeric intermediates of<br />
a particular structure are common initiators of neurotoxicity<br />
observed in prion disease <strong>and</strong> in other protein misfolding<br />
disorders, the crucial question remains why these<br />
protein species are toxic to cells. The conversion of a<br />
protein from its native state into an oligomeric form invariably<br />
generates a wide distribution of misfolded species<br />
which exposes an array of groups that are normally<br />
masked in globular proteins. The improper interactions<br />
between oligomers <strong>and</strong> cellular components, such as<br />
membranes, small metabolites, proteins, or other macromolecules,<br />
may conceivably lead to the malfunctioning of<br />
crucial aspects of the cellular machinery. Depending on<br />
the cell type involved, the result could be impairment of<br />
axonal transport, oxidative stress, sequestration of essential<br />
proteins, or a combination of disparate factors, ultimately<br />
leading to apoptosis or other forms of cell death.<br />
Small aggregates have a higher proportion of residues on<br />
their surfaces than larger aggregates, including mature<br />
amyloid fibrils, <strong>and</strong> therefore may be likely, in general, to<br />
have a higher relative toxicity (110).<br />
Elucidation of the mechanism of tissue damage by<br />
amyloid fibril proteins is undoubtedly an important issue<br />
in the development of therapeutic approaches, although<br />
the optimum strategy may be to prevent aggregation or<br />
even production of the amyloidogenic protein before it<br />
can generate any potentially damaging intermediates.<br />
IV. CLINICAL AND PATHOLOGICAL ASPECTS<br />
OF PRION DISEASES<br />
A. Scrapie<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
Even though scrapie was recognized as a distinct<br />
disorder of sheep with respect to its clinical manifestations<br />
as early as 1738, the disease remained an enigma,
1122 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
even with respect to its pathology, for more than two<br />
centuries (382). Some veterinarians thought that scrapie<br />
was a disease of muscle caused by parasites, whilst others<br />
thought that it was a dystrophic process (311). An investigation<br />
into the etiology of scrapie followed the vaccination<br />
of sheep for louping-ill virus with formalin-treated<br />
extracts of ovine lymphoid tissue unknowingly contaminated<br />
with scrapie prions (194). Two years later, more<br />
than 1,500 sheep developed scrapie from this vaccine.<br />
In 1998, aberrant cases of sheep scrapie were described<br />
in Norway, <strong>and</strong> the strain was newly classified as<br />
Nor98 (46). Active European Union surveillance later revealed<br />
additional cases of atypical scrapie in several other<br />
countries (87, 147); in fact, atypical scrapie appears to be<br />
the rule rather than the exception in some geographical<br />
areas.<br />
Scrapie of sheep <strong>and</strong> goats seems to be readily communicable<br />
within flocks, but the mechanism of the natural<br />
spread of scrapie among sheep is puzzling. The finding<br />
that chronic inflammation can alter the tropism of prion<br />
infectivity to organs hitherto believed prion free, like<br />
mammary gl<strong>and</strong>s, raised concerns about scrapie transmission<br />
through milk (210, 300).<br />
Polymorphisms at codons 136 <strong>and</strong> 171 of the Prnp<br />
gene in sheep that produce amino acid substitutions have<br />
been studied with respect to the occurrence of scrapie in<br />
sheep (113).<br />
B. Bovine Spongiform Encephalopathy<br />
In 1986, an epidemic of a previously unknown disease<br />
appeared in cattle in Great Britain (514): bovine<br />
spongiform encephalopathy (BSE) or “mad cow” disease.<br />
BSE was found to be a prion disease upon the<br />
discovery of protease-resistant PrP in the brains of ill<br />
cattle (226). On the basis mainly of epidemiological<br />
evidence, it has been proposed that BSE represents a<br />
massive common source epidemic that has caused<br />
more than 190,000 cases to date (http://www.oie.int/)<br />
(Fig. 7A). In Britain, cattle, particularly dairy cows,<br />
were routinely fed meat <strong>and</strong> bone meal as a nutritional<br />
supplement (521). Since 1988, the practice of using<br />
dietary protein supplements for domestic animals derived<br />
from rendered sheep or cattle offal has been<br />
forbidden in the United Kingdom.<br />
In 1992, the BSE epidemic reached a peak, with over<br />
35,000 cattle afflicted. In 1993, fewer than 32,000 cattle<br />
were diagnosed with BSE, <strong>and</strong> in 1994, the number was<br />
22,000. By 2003, BSE had become a rare disease in<br />
British <strong>and</strong> European cattle, but regrettably (<strong>and</strong> quite<br />
inexplicably) it still has not completely disappeared.<br />
Brain extracts from BSE cattle have transmitted disease<br />
to mice, cattle, sheep, <strong>and</strong> pigs after intracerebral<br />
inoculation (75, 130, 131, 165). Of particular importance to<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
the BSE epidemic is the transmission of BSE to the nonhuman<br />
primate marmoset after intracerebral inoculation<br />
followed by a prolonged incubation period (34).<br />
C. Chronic Wasting Disease of Deer <strong>and</strong> Elk<br />
Chronic wasting disease of deer <strong>and</strong> elk (CWD) was<br />
initially reported in 1980 as a TSE in captive research deer<br />
in Colorado <strong>and</strong> Wyoming. The disease origin still remains<br />
completely obscure (525). Since 1980, cases of CWD in<br />
free-ranging mule deer (Odocoileus hemionus), whitetailed<br />
deer (O. virginanus), <strong>and</strong> Rocky Mountain elk<br />
(Cervus elaphus nelsoni) have been detected in the same<br />
region of Colorado <strong>and</strong> Wyoming. Recently, increased<br />
surveillance efforts across the United States <strong>and</strong> Canada<br />
have startlingly revealed CWD in adjacent states (Nebraska,<br />
New Mexico, <strong>and</strong> Utah) but also distant (Wisconsin,<br />
Illinois, Canada) from this original endemic region.<br />
Thus far, CWD is only known to occur in North America<br />
<strong>and</strong> in South Korea. That said, international testing for<br />
CWD has been minimal with the exception of a CWD<br />
surveillance program in Germany (458).<br />
CWD is believed to be horizontally transmitted<br />
among cervids with high efficiency (348). Exposure<br />
through grazing in areas contaminated by prion-infected<br />
secretions, excretions (saliva, urine, feces), tissues (placenta),<br />
or decomposed carcasses is most likely the major<br />
source of spreading. Insightful experimental studies have<br />
recently revealed two key findings: 1) saliva from CWDinfected<br />
deer can transmit disease (332), <strong>and</strong> 2) CWDinfected<br />
carcasses allowed to decay naturally in confined<br />
pastures can lead to CWD infections in captive deer (349).<br />
Additionally, abundant CWD prion accumulation within<br />
lymphoid tissues may also lead to CWD prion buildup in<br />
nonlymphoid organs with lymphoid follicles, as was recently<br />
demonstrated in kidney, potentially shifting shedding<br />
routes (200). It is unknown whether other types of<br />
inflammation, such as the granulomatous inflammation in<br />
the intestine seen in Johne’s disease (Mycobacterium<br />
avium subsp. paratuberculosis; affects ruminants, including<br />
deer <strong>and</strong> elk) or parasitic inflammation could lead<br />
to or perhaps increase prion excretion by fecal routes.<br />
The potential for CWD transmission to other species<br />
is clearly an area of great concern. Wild predators <strong>and</strong><br />
scavengers are presumably feeding on CWD-infected carcasses.<br />
Skeletal muscle has been shown to harbor CWD<br />
prion infectivity (29), indicating that other species are<br />
almost certainly being exposed to CWD through feeding.<br />
However, CWD has not been successfully transmitted by<br />
oral inoculation to species outside of the cervid family,<br />
suggesting a strong species barrier for heterologous PrP<br />
conversion (458). Human susceptibility to CWD is still<br />
unclear, although we can be somewhat reassured in that<br />
there have been no large-scale outbreaks of human TSE
cases in Colorado <strong>and</strong> Wyoming, where CWD has existed<br />
for decades (334), <strong>and</strong> there is no doubt that people have<br />
been exposed to CWD through venison consumption, particularly<br />
in light of recent data showing CWD prion accumulation<br />
in muscle.<br />
Other indirect studies of human susceptibility to<br />
CWD also suggest that the risk is low. In biochemical<br />
conversion studies, the efficiency of CWD in converting<br />
recombinant human PrP into amyloid fibrils was low, yet<br />
similar to that of both BSE <strong>and</strong> scrapie (419). Accordingly,<br />
it has also been reported that human PrP-overexpressing<br />
mice were not susceptible to nine CWD isolates from<br />
mule deer, white-tailed deer, <strong>and</strong> elk (490), whereas the<br />
elk PrP expressing mice developed disease after only<br />
118–142 days postinoculation (275). However, mice have<br />
AGGREGATION AND INFECTIOUS DISEASE 1123<br />
FIG. 7. Bovine spongiform encephalopathy (BSE) <strong>and</strong> variant Creutzfeldt-Jakob disease (vCJD) cases reported worldwide. A: reported cases<br />
of BSE in the United Kingdom (UK) (black) <strong>and</strong> in countries excluding the UK (gray). Non-UK BSE cases include cases from countries both within<br />
<strong>and</strong> outside of the European Union. Data are as of December 2008 (http://www.oie.int). B: reported cases of vCJD in the UK (black) <strong>and</strong> in France<br />
(gray). In the table are reported vCJD cases worldwide. Data are as of January 2009. °Three cases are reported as secondary cases due to blood<br />
transfusion; #the third United States (US) patient was born <strong>and</strong> raised in Saudi Arabia <strong>and</strong> has lived permanently in the US since late 2005 <strong>and</strong>,<br />
according to the US case report, the patient was most likely infected as a child when living in Saudi Arabia; *the case from Japan had resided in<br />
the UK for 24 days in the period 1980–1996 [see the National Creutzfeldt-Jakob Disease Surveillance Unit Web site for vCJD data to December 2008<br />
(http://www.cjd.ed.ac. uk)].<br />
a limited life span, <strong>and</strong> further passages may be necessary<br />
to detect low levels of prion infectivity that may be<br />
present subclinically.<br />
D. Human Prion <strong>Diseases</strong><br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
Rapidly progressive dementia, myoclonus, visual or<br />
cerebellar impairment, pyramidal/extrapyramidal signs,<br />
<strong>and</strong> akinetic mutism clinically characterize fatal neurological<br />
diseases caused by prions. The human prion diseases<br />
are classified as infectious, inherited or sporadic disorders,<br />
depending on the clinical, genetic, <strong>and</strong> neuropathological<br />
findings.<br />
Prion disease, not only in inherited forms but also in<br />
iatrogenic <strong>and</strong> sporadic forms, is influenced by an amino
1124 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
acid polymorphism resulting in methionine (M)3valine<br />
(V) substitution at PrP codon 129 (375). The finding that<br />
homozygosity at codon 129 predisposes individuals to<br />
CJD supports the theory that protective polymorphisms in<br />
the human prion gene have been heavily selected for,<br />
possibly due to evolutionary pressure from cannibalismpropagated<br />
prions (341). However, several publications<br />
have pointed out that these conclusions may be incorrect<br />
(449, 468). It was recently described that incubation periods<br />
of Kuru could be as long as 56 years. PRNP analysis<br />
showed that most of those patients with Kuru were heterozygous<br />
at polymorphic codon 129, a genotype associated<br />
with extended incubation periods <strong>and</strong> resistance to<br />
prion disease (119).<br />
A second polymorphism resulting in glutamate<br />
(E)3lysine (K) substitution at codon 219 has been identified<br />
in the Japanese population, <strong>and</strong> it has also been<br />
reported to have an effect on the susceptibility of individuals<br />
to prion disease (264). Recently, additional c<strong>and</strong>idate<br />
loci have been identified by a genome-wide association<br />
study of the risk of vCJD (340) which justifies functional<br />
analyses of these biological pathways in prion disease.<br />
1. Iatrogenic prion diseases<br />
Iatrogenic CJD is accidentally transmitted during the<br />
course of medical or surgical procedures. The first documented<br />
case of iatrogenic prion transmission occurred in<br />
1974 <strong>and</strong> was caused by corneal transplantation of a graft<br />
derived from a patient suffering from sCJD (143). Iatrogenic<br />
CJD has also been transmitted by neurosurgery<br />
using contaminated EEG electrode implantations (50)<br />
<strong>and</strong> surgical operations using contaminated instruments<br />
or apparatuses (129, 331). Moreover, the transmission of<br />
CJD from contaminated human growth hormone (HGH)<br />
preparations derived from human pituitaries was discovered<br />
when fatal cerebellar disorders with dementia occurred<br />
in 80 patients ranging in age from 10 to over 60<br />
yr (73, 82, 160). Five cases of CJD have occurred in<br />
women receiving human pituitary gonadotropin (203). Although<br />
one case of spontaneous CJD in a 20-yr-old<br />
woman has been reported (377), CJD in people under 40<br />
yr of age is extremely rare.<br />
Molecular genetic studies have revealed that most<br />
patients developing iatrogenic CJD after receiving pituitary-derived<br />
HGH are homozygous for either Met or Val<br />
at codon 129 of the PRNP gene (72, 117).<br />
2. Inherited prion diseases<br />
Familial TSEs are associated with an autosomal dominant<br />
PRNP gene alteration. There is variability in the<br />
clinical <strong>and</strong> pathological findings, the age of onset, <strong>and</strong><br />
the duration depending on the particular PRNP mutation<br />
involved (Table 4). Familial TSEs account for 10–20% of<br />
all TSE cases in humans <strong>and</strong> include fCJD, GSS, <strong>and</strong> FFI.<br />
Clinically, fCJD is characterized by rapidly progressive<br />
dementia, with myoclonus <strong>and</strong> pseudoperiodic discharges<br />
on electroencephalogram; GSS by slow progression of<br />
ataxia followed by later onset dementia, <strong>and</strong> FFI from<br />
refractory insomnia, hallucinations, dysautonomia, <strong>and</strong><br />
motor signs. The clinical categories may be seen as phenotypic<br />
extremes of a continuum, because in reality the<br />
syndromes overlap considerably (339).<br />
fCJD have been associated with point mutations affecting<br />
the region between the second <strong>and</strong> the third helix<br />
of the COOH terminus, insertions in the octarepeat region<br />
in the NH2 terminus, <strong>and</strong> even a premature termination<br />
codon at position 145. The inheritance is, in all cases,<br />
autosomal dominant, often with very high penetrance. In<br />
TABLE 4. Synopsis of all PRNP mutations <strong>and</strong> polymorphisms <strong>and</strong> their association with inherited<br />
prion diseases<br />
Presentation Mutation in PRNP<br />
Creutzfeldt-Jakob phenotype D178N-129V, V180I, V180I-M232R, T183A, T188A, E196K, E200K, V203I, R208H,<br />
V210I, E211Q, M232R, 96 bpi, 120 bpi, 144 bpi, 168 bpi, 48 bpd<br />
Gerstmann-Sträussler-Scheinker phenotype P102L, P105L, A117V, G131V, F198S, D202N, Q212P, Q217R, M232T, 192 bpi<br />
Fatal familial insomnia phenotype D178N-129M<br />
Vascular amyloid depositions Y145STOP<br />
Proven but unclassified prion disease H187R, 216 bpi<br />
Neuropsychiatric disorder, no proven prion disease I138M, G142S, Q160S, T188K, T188R, M232R, P238S, 24 bpi, 48 bpi<br />
Polymorphisms, established influence on phenotype M129V<br />
Polymorphisms, suggested influence on phenotype N171S, E219K<br />
Silent polymorphisms P68P, A117A, G124G, V161V, N173N, H177H, T188T, D202D, Q212Q, R228R, S230S<br />
The wild-type human PRNP gene contains 5 octarepeats P(Q/H)GGG(G/–) WGQ from codons 51–91. Deletion of a single octarepeat at codon<br />
81 or 82 is not associated with prion disease (289, 413, 503); whether this deletion alters the phenotypic characteristics of a prion disease is unknown.<br />
There are common polymorphisms at codons 117 (Ala3Ala) <strong>and</strong> 129 (Met3Val); homozygosity for Met or Val at codon 129 seems to increase<br />
susceptibility to sporadic CJD (378). Octarepeat inserts of 16, 32, 40, 48, 56, 64, <strong>and</strong> 72 amino acids at codons 67, 75, or 83 are designated as bpi<br />
(base pair insertion); bpd indicates base pair deletion. Point mutations are designated by the wild-type amino acid preceding the codon number <strong>and</strong><br />
the mutant residue follows, e.g., P102L. These point mutations segregate with the inherited prion diseases, <strong>and</strong> significant genetic linkage has been<br />
demonstrated where sufficient specimens from family members are available. The single letter code for amino acids is as follows: A, Ala; D, Asp;<br />
E, Glu; F, Phe; I, Ile; K, Lys; L, Leu; M, Met; N, Asn; P, Pro; Q, Gln; R, Arg; S, Ser; T, Thr; V, Val; <strong>and</strong> Y, Tyr.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org
all fCJD, the clinicopathological disease phenotype varies<br />
depending on the actual mutation, as well as on polymorphisms<br />
at codon 129, <strong>and</strong> most likely on a plethora of yet<br />
unidentified modifiers <strong>and</strong> cofactors (280).<br />
The first reports of GSS originate from 1928 <strong>and</strong> 1936<br />
in an Austrian family (179, 199). GSS syndrome is a rare,<br />
inherited autosomal dominant disease that is associated<br />
with mutations in the PRNP gene (the most common are<br />
at codons 102 <strong>and</strong> 198). GSS syndrome is characterized by<br />
chronic progressive ataxia, terminal dementia, a long clinical<br />
duration (2–10 yr), <strong>and</strong> multicentric amyloid plaques<br />
that can be visualized by antibodies directed against the<br />
prion protein.<br />
FFI is characterized by sleep disturbances as well as<br />
vegetative <strong>and</strong> focal neurological signs as a result of<br />
thalamic lesions. The clinical phenotype depends on the<br />
D178N point mutation of the PRNP gene coupled with a<br />
methionine at codon 129 (175).<br />
3. Sporadic Creutzfeldt-Jakob disease<br />
Approximately 85% of all human prion diseases are<br />
sporadic forms of CJD. For sCJD, there is no association<br />
with a mutant PRNP allele, nor is there any epidemiological<br />
evidence for exposure to a TSE agent through contact<br />
with people or animals infected with TSEs.<br />
sCJD cases are currently subclassified according to<br />
the methionine/valine polymorphism at codon 129 of the<br />
PRNP gene <strong>and</strong> the size <strong>and</strong> glycoform ratio of proteaseresistant<br />
prion protein identified on western blot (type 1<br />
or type 2) (174). Heterozygosity (Met/Val) at PrP codon<br />
129 appears to be associated with a lower risk (378)<br />
<strong>and</strong>/or prolonged incubation time (119, 387).<br />
The lack of routine laboratory testing for preclinical<br />
diagnosis makes the search for agent sources <strong>and</strong> other<br />
risk factors extremely difficult. At present, the means of<br />
acquisition of a TSE agent in these patients remains a<br />
mystery. So far, there is no evidence for spontaneous<br />
PrP Sc formation in any animal or human TSE. In humans,<br />
the peak age incidence of sporadic CJD is 55–60 years.<br />
However, if spontaneous misfolding were the primary<br />
event, one might expect a continuously increasing incidence<br />
with age because more time would allow more<br />
opportunity for rare misfolding events.<br />
4. Variant Creutzfeldt-Jakob disease<br />
The most recently identified form of CJD in humans,<br />
new variant CJD (vCJD), was first described in 1996 <strong>and</strong><br />
has been linked to BSE (522).<br />
At the time of this writing, vCJD has killed 200<br />
individual victims worldwide (http://www.cjd.ed.<br />
ac.uk/). Most of the affected individuals lived in the<br />
United Kingdom <strong>and</strong> France. Fortunately, in the United<br />
Kingdom, the incidence appears to be decreasing since<br />
2001 to five diagnosed cases yearly in 2006 <strong>and</strong> 2007<br />
AGGREGATION AND INFECTIOUS DISEASE 1125<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
<strong>and</strong> one case in 2008. In contrast, in France, the number<br />
of probable <strong>and</strong> definite cases of vCJD increased from<br />
zero to three diagnosed cases per year in 1996–2004 to<br />
six per year in 2005 <strong>and</strong> 2006. In 2007, the number of<br />
cases was back to three again, <strong>and</strong> no cases were<br />
reported in 2008 (http://www.invs.sante.fr/publications/<br />
mcj/donnees_mcj.html) (Fig. 7B).<br />
vCJD represents a distinct clinicopathological entity<br />
that is characterized at onset by psychiatric abnormalities,<br />
sensory symptoms, <strong>and</strong> ataxia <strong>and</strong> eventually leads to dementia<br />
along with other features usually observed in sporadic<br />
CJD. What distinguishes vCJD from sporadic cases is<br />
that the age of patients is abnormally low (vCJD: 19–39 yr;<br />
sporadic CJD: 55–70 yr) <strong>and</strong> duration of the illness is rather<br />
long (vCJD: 7.5–22 mo; sporadic CJD: 2.5–6.5 mo). Moreover,<br />
vCJD displays a distinct pathology within the brain<br />
characterized by abundant “florid plaques,” decorated by a<br />
daisylike pattern of vacuolation. Florid plaques are spherical<br />
conglomerates of fibrillary birefringent material that stains<br />
positive with “amyloidotropic” dyes such as Congo red.<br />
What is the evidence that the agent causing vCJD may<br />
be identical to that of BSE when transmitted to humans?<br />
None of the arguments to date are conclusive. Considerable<br />
effort has been devoted to characterizing the “strain properties”<br />
of the agent that affects cows <strong>and</strong> humans. Since the<br />
molecular substrate underlying the phenomenon of prion<br />
strains is not known, strain-typing of prions must rely on<br />
surrogate markers.<br />
Two such markers have been particularly useful. One is<br />
the distribution of neuronal vacuoles in the brains of affected<br />
animals. BSE prions (extracted from the brains of<br />
affected cows) <strong>and</strong> vCJD prions derived from the brains of<br />
British patients produce the same lesion profile when transmitted<br />
to panels of susceptible mice (3, 22, 80). The second<br />
marker for strain typing of prions comes from analyzing the<br />
biochemical properties of disease-associated PrP recovered<br />
from the brains of cattle <strong>and</strong> humans. These traits were<br />
again found to be indistinguishable between BSE <strong>and</strong> human<br />
vCJD prions (118, 219). A third line of evidence linking<br />
BSE to human vCJD comes from the epidemiology of the<br />
disease. To date, the majority of vCJD cases have arisen in<br />
the United Kingdom, with relatively few cases in other countries<br />
including Irel<strong>and</strong>, France (106), <strong>and</strong> Italy. With the<br />
assumption that the quality of the epidemiological surveillance<br />
is similar in these countries <strong>and</strong> in the rest of Europe<br />
(which has not reported cases of vCJD), the unavoidable<br />
conclusion is that the incidence of vCJD correlates with the<br />
prevalence of BSE.<br />
Convincing as all of these arguments may seem, each<br />
is phenomenological rather than causal. Given that a large<br />
fraction of the European population may have been exposed<br />
to BSE prions, yet only a minute fraction actually<br />
developed vCJD, there can be hardly any doubt that additional<br />
genetic modifiers exist, other than PRNP polymorphisms.<br />
So what will the numbers of vCJD victims be
1126 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
in the future? Although many mathematical models have<br />
been generated (180, 181), the number of cases is still too<br />
small to predict future developments with any certainty. A<br />
30-yr mean incubation time of BSE/vCJD in humans is not<br />
entirely implausible, <strong>and</strong> therefore, some authors have<br />
predicted a multiphasic BSE endemic with a second increase<br />
in the incidence of vCJD affecting people heterozygous<br />
at codon 129 (119). Others, these authors included,<br />
regard the incidence of vCJD as subsiding (28). It is<br />
important to note, however, that the above considerations<br />
apply primarily to the epidemiology of primary transmission<br />
from cows to humans. Although by now a pool of<br />
preclinically infected humans may have been built, human-to-human<br />
transmission may present with characteristics<br />
very different from those of primary cow-to-human<br />
transmission, including enhanced virulence, shortened incubation<br />
times, disregard of allelic PRNP polymorphisms<br />
(129MM, MV or VV), <strong>and</strong> heterodox modes of infection<br />
including blood-borne transmission. If we account for the<br />
time it will take to eradicate these secondary transmissions<br />
in the population, vCJD is not likely to disappear<br />
entirely in the coming four decades. Four cases (three<br />
definite <strong>and</strong> one presumed) of vCJD transmission by<br />
blood transfusions have been reported in the United Kingdom<br />
(303, 387, 528) (see also http://www.cjd.ed.ac.uk/<br />
TMER/TMER.htm). Most worryingly, the Health Protection<br />
Agency of the United Kingdom has reported a case of<br />
a hemophilic patient who has most likely acquired vCJD<br />
prions through factor VIII preparation derived from<br />
plasma donated by a “preclinical” vCJD patient (http://<br />
www.hpa.org.uk).<br />
The fact that preclinical infected individuals can<br />
transmit vCJD underscores the important medical need<br />
for sensitive diagnostic tools, which could be used for<br />
screening blood units prior to transfusion.<br />
V. PERIPHERAL ROUTES OF PRION<br />
INFECTIVITY<br />
The fastest <strong>and</strong> most efficient method of inducing<br />
spongiform encephalopathy in the laboratory is intracerebral<br />
inoculation with brain homogenate. Inoculation of<br />
10 6 ID 50 infectious units (defined as the amount of infectivity<br />
that will induce TSE with 50% likelihood in a given<br />
host) will yield disease in approximately half a year; a<br />
remarkably strict inverse relationship can be observed<br />
between the logarithm of the inoculated dose <strong>and</strong> the<br />
incubation time (406).<br />
However, the above situation does not correspond to<br />
what typically happens in the field. There, acquisition of<br />
prion infectivity through any of several peripheral routes<br />
is the rule. Prion infections can be induced by oral challenge<br />
(159) <strong>and</strong> occur naturally as a result of food-borne<br />
contamination, as has been shown for Kuru, transmissible<br />
mink encephalopathy, BSE, <strong>and</strong> vCJD (27, 119, 222, 328).<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
However, prion diseases can also be initiated by<br />
intravenous <strong>and</strong> intraperitoneal injection (258) as well as<br />
from the eye by conjunctival instillation (445), corneal<br />
grafts (143), <strong>and</strong> intraocular injection (161). Two routes of<br />
infection have suggested for a long time that immune cells<br />
might be of importance for this phase of prion pathogenesis:<br />
oral challenge <strong>and</strong> administration by scarification<br />
(7). Therefore, these routes will be discussed in some<br />
detail in the following paragraphs.<br />
A. Pathway of Orally Administered <strong>Prions</strong><br />
After oral infection, an early increase in prion infectivity<br />
is observed in the distal ileum. Within 2 wk of prion<br />
ingestion, prions appear to enter peripheral nerves <strong>and</strong><br />
proceed by invasion of the dorsal motor nucleus of the<br />
vagus in the brain, as has been shown in mouse <strong>and</strong><br />
hamster scrapie studies (336). Gastrointestinal infections<br />
caused by viruses, bacteria, <strong>and</strong> parasites, as well as<br />
idiopathic inflammatory diseases, could alter the dynamics<br />
of prion entry <strong>and</strong> systemic spread. It has been recently<br />
reported that moderate colitis, caused by an attenuated<br />
Salmonella strain, more than doubles the susceptibility<br />
of mice to oral prion infection <strong>and</strong> modestly<br />
accelerates the development of disease after prion challenge<br />
(459).<br />
How do prions reach the peripheral nerves after having<br />
entered the gastrointestinal tract? Following exposure,<br />
many acquired TSE agents accumulate in lymphoid<br />
tissue, in the case of oral exposure, the gut-associated<br />
lymphatic tissue (GALT), which includes Peyer’s patches<br />
(PPs) <strong>and</strong> membranous epithelial cells (M cells), <strong>and</strong><br />
mesenteric lymph nodes. Following experimental intragastric<br />
or oral exposure of rodents to scrapie, or nonhuman<br />
primates <strong>and</strong> sheep to BSE, protease-resistant<br />
prion protein accumulates rapidly in the GALT, PPs, <strong>and</strong><br />
ganglia of the enteric nervous system (41, 57, 156, 259),<br />
long before they are detected in the CNS.<br />
Recruitment of activated B lymphocytes to PPs requires<br />
4 7 integrin as an essential homing receptor; PPs<br />
of mice that lack 7 integrin are normal in number, but<br />
are atrophic <strong>and</strong> almost entirely devoid of B cells (507).<br />
Therefore, it seemed interesting to investigate the susceptibility<br />
to orally administered prions of 7-deficient mice.<br />
Surprisingly, minimal infectious dose <strong>and</strong> disease incubation<br />
after oral exposure to logarithmic dilutions of prion<br />
inoculum were similar in 7-deficient <strong>and</strong> wild-type mice<br />
(399). Despite their atrophy, PPs of both 7-knockout <strong>and</strong><br />
wild-type mice contained 3–4 log LD 50/g prion infectivity<br />
at 125 or more days after challenge.<br />
Why does reduced mucosal lymphocyte trafficking<br />
not impair, as expected, the susceptibility to orally initiated<br />
prion disease? One possible reason may relate to the<br />
fact that, despite marked reduction of B cells, M cells
were still present in 7 / mice. In contrast, mice deficient<br />
in both TNF <strong>and</strong> lymphotoxin (LT)- (TNF- / <br />
LT / ) or in lymphocytes (RAG-1 / , MT), in which<br />
Peyer’s patches are reduced in number, were highly resistant<br />
to oral challenge, <strong>and</strong> their intestines were virtually<br />
devoid of prion infectivity at all times after challenge.<br />
Therefore, lymphoreticular requirements for enteric <strong>and</strong><br />
for intraperitoneal uptake of prions differ from each other<br />
in that susceptibility to prion infection following oral<br />
challenge correlates with the number of Peyer’s patches,<br />
but is independent of the number of intestinal mucosaassociated<br />
lymphocytes (189, 399).<br />
B. Transepithelial Enteric Passage of <strong>Prions</strong><br />
The requirements for transepithelial passage of prions<br />
are of obvious interest to prion pathogenesis. M cells<br />
are key sites of antigen sampling for the mucosal-associated<br />
lymphoid system (MALT) <strong>and</strong> have been recognized<br />
as major ports of entry for enteric pathogens in the gut via<br />
transepithelial transport (363).<br />
Interestingly, maturation of M cells is dependent on<br />
signals transmitted by intraepithelial B lymphocytes.<br />
Efficient in vitro systems have been developed, in<br />
which epithelial cells can be instructed to undergo differentiation<br />
to cells that resemble M cells, as judged by<br />
morphological <strong>and</strong> functional-physiological criteria (254).<br />
This led to the proposal that M cells could be a site of<br />
prion entry, a hypothesis that has been substantiated in<br />
coculture models (212). Although in vivo confirmation is<br />
required, M cells are plausible sites for the transepithelial<br />
transport of scrapie across the intestinal epithelium. However,<br />
the transport across the intestinal epithelium might<br />
not rely entirely on M-cell-mediated transcytosis: several<br />
reports have also indicated that prion transport may occur<br />
through enterocytes (372) <strong>and</strong> could be mediated by a<br />
ferritin-dependent mechanism (351) or via laminin-receptor<br />
binding <strong>and</strong> endocytosis (357).<br />
Dendritic cells (DCs), localized within the PPs beneath<br />
the M-cell intraepithelial pocket, are ideally situated<br />
to acquire antigens that have been transcytosed from the<br />
gut lumen <strong>and</strong> deliver them to peripheral nerves in lymphoid<br />
organs, thereby facilitating the process of neuroinvasion<br />
(232, 317). The contribution of CD11c DCs has<br />
been investigated in vivo using CD11c-diphtheria toxin<br />
receptor-transgenic mice in which CD11c DCs can be<br />
specifically <strong>and</strong> transiently depleted (418). With the use of<br />
two distinct scrapie agent strains (ME7 <strong>and</strong> 139A), depletion<br />
of CD11c DCs in the GALT <strong>and</strong> spleen before oral<br />
exposure blocked early prion accumulation in these tissues.<br />
These data suggest that migratory CD11c DCs play<br />
a role in the translocation of the scrapie agent from the<br />
gut lumen to the GALT, from which neuroinvasion proper<br />
may then ensue.<br />
AGGREGATION AND INFECTIOUS DISEASE 1127<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
C. Uptake of Prion Through the Skin<br />
Even less well understood, yet possibly much more<br />
efficient than oral administration of prions, is challenge<br />
by scarification. Removal of the most superficial layers of<br />
the skin, <strong>and</strong> subsequent administration of prions, has<br />
been known for long time to be a highly efficacious<br />
method of inducing prion disease (90, 497). It is conceivable<br />
that dendritic cells in the skin may become loaded<br />
with the infectious agent by this method, <strong>and</strong> in fact,<br />
dendritic cells have been implicated as potential vectors<br />
of prions in oral (232) <strong>and</strong> in hematogeneous spread (31)<br />
of the agent.<br />
Following inoculation with scrapie by skin scarification,<br />
replication in the spleen <strong>and</strong> subsequent neuroinvasion<br />
is critically dependent on mature follicular dendritic<br />
cells (FDCs) (353). However, which lymphoid tissues are<br />
crucial for TSE pathogenesis following inoculation via the<br />
skin was not known until mice were created that lacked<br />
the draining inguinal lymph node (ILN), but had functional<br />
FDCs in remaining lymphoid tissues such as the<br />
spleen. In these mice, inoculated with the scrapie agent by<br />
skin scarification, the disease susceptibility was dramatically<br />
reduced demonstrating that, following inoculation<br />
by skin scarification, scrapie agent accumulation in FDCs<br />
in the draining lymph node is critical for the efficient<br />
transmission of disease to the brain (188).<br />
It is equally possible (<strong>and</strong> maybe more probable),<br />
however, that scarification induces direct neural entry of<br />
prions into skin nerve terminals. This latter hypothesis<br />
has not yet been experimentally tested, but it would help<br />
explain the remarkable speed with which CNS pathogenesis<br />
ensues following inoculation by this route: dermal<br />
inoculation of killed mice yields typical latency periods of<br />
the disease that are similar to those obtained by intracerebral<br />
inoculation.<br />
Rapid neuroinvasion was reported following intralingual<br />
inoculation <strong>and</strong> may also exploit a direct intraneural<br />
pathway (38).<br />
VI. IMMUNOLOGICAL ASPECTS OF PRION<br />
DISEASE<br />
In a discussion of the immunological aspects of prion<br />
diseases, it is important to distinguish between an early<br />
extraneural phase <strong>and</strong> a late CNS phase of pathogenesis.<br />
There is no doubt that components of the immune system<br />
participate in pathogenesis in both compartments, but<br />
their respective functional implications are strikingly different.<br />
A. The Lymphoid System in Prion Disease<br />
More than 40 years ago it was discovered using bioassays<br />
that lymphoreticular organs contain prion infectiv-
1128 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
ity (162, 385). For scrapie in sheep <strong>and</strong> goats, infectivity<br />
was assessed in a broad range of tissues using experimentally<br />
inoculated goats as donors <strong>and</strong> uninfected goats as<br />
recipients (384), <strong>and</strong> both spleen <strong>and</strong> lymph nodes were<br />
shown to transmit scrapie.<br />
In the decades following these discoveries, our underst<strong>and</strong>ing<br />
of the extraneural immune phase advanced<br />
considerably, <strong>and</strong> an impressive collection of data has<br />
accrued that provides clues about peripheral prion pathogenesis.<br />
The normal prion protein was found to be consistently<br />
expressed, albeit at moderate levels, in circulating<br />
lymphocytes (91). Subsequently it was clearly shown<br />
in a wealth of experimental paradigms that innate or<br />
acquired deficiency of lymphocytes would impair peripheral<br />
prion pathogenesis, whereas no aspects of pathogenesis<br />
were affected by the presence or absence of lymphocytes<br />
upon direct transmission of prions to the CNS (263,<br />
291). Klein <strong>and</strong> colleagues (4, 267) pinpointed the lymphocyte<br />
requirement to B cells. Interestingly, it was shown<br />
that only B cells within the secondary lymphoid organs<br />
accumulated prions in a PrP C -dependent fashion, while<br />
circulating lymphocytes contained no detectable infectivity<br />
(415). A series of bone marrow transfer experiments<br />
demonstrated that peripheral prion pathogenesis required<br />
the physical presence of B cells, but the expression of the<br />
cellular prion protein by these cells is dispensable for<br />
pathogenesis upon intraperitoneal infection in the mouse<br />
scrapie model (11). Adoptive transfer of Prnp / bone<br />
marrow to Prnp o/o -recipient mice did not suffice to restore<br />
infectibility of Prnp-expressing brain grafts, indicating<br />
that neuroinvasion was still defective (53), yet intraperitoneal<br />
infection occurred efficiently even in B-celldeficient<br />
hosts that had been engrafted with B cells from<br />
Prnp knockout mice (268, 354).<br />
Although the requirement for B cells appears to be<br />
very stringent in most instances investigated, it has<br />
emerged that not all strains of prions induce identical<br />
patterns of peripheral pathogenesis, even when propagated<br />
in the same, isogenic strain of host organism (452).<br />
Another interesting discrepancy that remains to be<br />
addressed concerns the actual nature of the cells that<br />
replicate <strong>and</strong> accumulate prions in lymphoid organs. In<br />
the RML paradigm, four series of rigorously controlled<br />
experiments over 5 years (18, 243, 269, 400) unambiguously<br />
reproduced the original observation by Blättler et<br />
al. (53) that transfer of Prnp / bone marrow cells (or<br />
fetal liver cells) to Prnp o/o mice restored accumulation<br />
<strong>and</strong> replication of prions in spleen. In contrast, Brown et<br />
al. (70) reported a diametrically opposite outcome of<br />
similar experiments when mice were inoculated with prions<br />
of the ME7 strain. This discrepancy may identify yet<br />
another significant difference in the cellular tropism of<br />
different prion strains.<br />
It is important to note that the results of the Blättler<br />
study do not necessarily indicate that lymphocytes are the<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
primary splenic repository of prions: in fact, other experiments<br />
suggest that this is quite unlikely. Instead, bone<br />
marrow transplantation may 1) transfer an ill-defined<br />
population with the capability to replenish splenic stroma<br />
<strong>and</strong> to replicate prions, or less probably, 2) donor-derived<br />
PrP C expressing hematopoietic cells may confer prion<br />
replication capability to recipient stroma by virtue of “GPI<br />
painting,” i.e., the posttranslational cell-to-cell transfer of<br />
glycophosphoinositol linked extracellular membrane proteins<br />
(277). Some evidence might be accrued for either<br />
possibility: stromal splenic follicular dendritic cells have<br />
been described by some authors to possibly derive from<br />
hematopoietic precursors, particularly when donors <strong>and</strong><br />
recipients were young (250, 486). Conversely, instances<br />
have been described in which transfer of GPI-linked proteins<br />
occurs in vivo with surprisingly high efficiency<br />
(278). GPI painting has been described specifically for the<br />
cellular prion protein (302).<br />
While it has been known for a long time that specific<br />
strains of prions may preferentially affect specific subsets<br />
of neurons, the Blättler/Brown paradox may uncover an<br />
analogous phenomenon in peripheral prion pathogenesis.<br />
The latter question may be much more important than it<br />
appears at face value, since the molecular <strong>and</strong> cellular<br />
basis of peripheral tropism of prion strains is likely to be<br />
directly linked to the potential danger of BSE in sheep<br />
(77, 185, 249), as well the potential presence of vCJD<br />
prions in human blood (6).<br />
1. Follicular dendritic cells <strong>and</strong> prion replication<br />
As mentioned above, prion infectivity rises very rapidly<br />
(in a matter of days) in the spleens of intraperitoneally<br />
infected mice. Although B lymphocytes are crucial for<br />
neuroinvasion, all evidence indicates that most splenic<br />
prion infectivity resides in a “stromal” fraction. Instead,<br />
the apparent requirement for B lymphocytes in peripheral<br />
pathogenesis is more likely to be derived, at least in part,<br />
from indirect effects, including the provision of chemokines<br />
or cytokines to cells that efficiently replicate prions<br />
in peripheral regions of the host body (14).<br />
Any potential profiteer from these B-lymphocyte-derived<br />
signals would be localized in close proximity to the<br />
B lymphocytes, be of stromal origin, <strong>and</strong> should also<br />
display PrP C on its cell surface. FDCs fulfill each of these<br />
criteria. FDCs support the formation <strong>and</strong> maintenance of<br />
the lymphoid microarchitecture by expressing homeostatic<br />
chemokines <strong>and</strong> have a role in antigen trapping <strong>and</strong><br />
capturing of immune complexes by Fc receptors. Identification<br />
of FDC-specific genes is extremely important<br />
<strong>and</strong> useful, to assess the contribution of FDCs to prion<br />
pathogenesis. Recently, the antigen FDC-M1 has been<br />
identified as Milk fat globule EGF factor 8 (Mfge8) (282).<br />
Gene deletion experiments in mice have shown that<br />
signaling by both TNF <strong>and</strong> lymphotoxins is required for
generation <strong>and</strong> maintenance of FDCs (145, 276). LTs belong<br />
to a family of structurally related cytokines, the TNF<br />
superfamily (306), <strong>and</strong> are expressed primarily by B lymphocytes<br />
<strong>and</strong> activated T lymphocytes. LT <strong>and</strong> LT are<br />
proinflammatory cytokines; ectopic expression of LTs in<br />
the liver, kidney, or pancreas leads to the generation of<br />
follicular structures resembling tertiary follicles (210,<br />
283), which are very similar to activated lymphoid follicles<br />
found in the spleen or lymph nodes.<br />
Membrane-bound LT-/ (LT- 1/ 2 or LT- 2/ 1) heterotrimers<br />
signal through the LT- receptor (LT-R)<br />
(508), thereby activating a signaling pathway required for<br />
the development <strong>and</strong> maintenance of secondary lymphoid<br />
organs (318, 333).<br />
A series of studies has been performed to define the<br />
effect of selective ablation of functional FDCs on the<br />
pathogenesis of scrapie in mice.<br />
FDCs accumulate PrP Sc following scrapie infection<br />
(263), <strong>and</strong> prion replication in the spleen was reported to<br />
depend on PrP C -expressing FDCs, at least in the ME7<br />
prion strain (70).<br />
Inhibiting the LTR pathway in mice <strong>and</strong> nonhuman<br />
primates, by treatment with LTR-Ig, results in the disappearance<br />
or dedifferentiation of mature, functional FDCs<br />
(191, 192). In addition, treatment with LTR-Ig was found<br />
to impair peripheral prion pathogenesis (316, 355). Treatment<br />
of mice with LTR-Ig for 1 wk before exposure to a<br />
relatively low dose (intraperitoneally) of prions, followed<br />
by further treatment for 2 wk postinoculation, resulted in<br />
the complete protection of the mice from disease (15).<br />
This suggests that B cell-deficient MT mice (266) may be<br />
resistant to intraperitoneal prion inoculation (267) because<br />
of impaired FDC maturation (268, 355).<br />
However, additional experimentation appears to indicate<br />
that PrP C -expressing hematopoietic cells are required<br />
in addition to FDCs for efficient lymphoreticular<br />
prion propagation (53, 243). This apparent discrepancy<br />
called for additional studies of the molecular requirements<br />
for prion replication competence in lymphoid<br />
stroma. Therefore, peripheral prion pathogenesis was<br />
studied in mice lacking TNF-, LTa/, or their receptors.<br />
After intracerebral inoculation, all treated mice developed<br />
clinical symptoms of scrapie with incubation times, attack<br />
rates, <strong>and</strong> histopathological characteristics similar to<br />
those of wild-type mice, indicating that TNF/LT signaling<br />
is not relevant to cerebral prion pathogenesis. Upon intraperitoneal<br />
prion challenge, mice defective in LT signaling<br />
(LT / , LT / , LTR / , or LT / TNF- / )<br />
proved virtually noninfectible with 5 log LD 50 scrapie<br />
infectivity, <strong>and</strong> establishment of subclinical disease (166)<br />
was prevented. In contrast, TNFR1 / mice were almost<br />
fully susceptible to all inoculum sizes, <strong>and</strong> TNF- / mice<br />
showed dose-dependent susceptibility. TNFR2 / mice<br />
had intact FDCs <strong>and</strong> germinal centers <strong>and</strong> were fully<br />
susceptible to scrapie. Unexpectedly, all examined lymph<br />
AGGREGATION AND INFECTIOUS DISEASE 1129<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
nodes of TNFR1 / <strong>and</strong> TNF- / mice had consistently<br />
high infectivity titers (400). Even inguinal lymph nodes,<br />
which are distant from the injection site <strong>and</strong> do not drain<br />
the peritoneum, contained infectivity titers equal to all<br />
other lymph nodes. Therefore, TNF deficiency prevents<br />
lymphoreticular prion accumulation in spleen but not in<br />
lymph nodes.<br />
Why is susceptibility to peripheral prion challenge<br />
preserved in the absence of TNFR1 or TNF- / , while<br />
deletion of LT signaling components confers high resistance<br />
to peripheral prion infection? After all, each of<br />
these defects (except TNFR2 / ) abolishes FDCs. For<br />
one thing, prion pathogenesis in the lymphoreticular system<br />
appears to be compartmentalized, with lymph nodes<br />
(rather than spleen) being important reservoirs of prion<br />
infectivity during disease. Second, prion replication appears<br />
to take place in lymph nodes even in the absence of<br />
mature FDCs; therefore, poorly defined immune cells or<br />
possibly stromal precursor cells (for example, for FDCs)<br />
might be capable of replicating the infectious agent.<br />
In an unexpected turn of events, it was found that<br />
lymphotoxin-dependent prion replication can occur in<br />
inflammatory stromal cells that are distinct from FDCs<br />
(208). Granulomas, a frequent feature of chronic inflammation,<br />
express PrP C <strong>and</strong> the LTR, even though they<br />
lacked FDCs <strong>and</strong> did not display lymphoneogenesis. After<br />
intraperitoneal prion inoculation, granulomas accumulated<br />
prion infectivity. Bone marrow transfers between<br />
Prnp / <strong>and</strong> Prnp o/o mice <strong>and</strong> administration of lymphotoxin<br />
signaling antagonists indicated that prion replication<br />
required radioresistant PrP C -expressing cells <strong>and</strong><br />
LTR signaling. The finding that a cell type other than<br />
mature FDCs is involved in prion replication <strong>and</strong> accumulation<br />
within lymph nodes may be relevant to the development<br />
of postexposure prophylaxis strategies.<br />
2. A role for the complement cascade in prion<br />
accumulation<br />
As FDCs interact with opsonized antigens through<br />
the CD21/CD35 complement receptors, a pertinent question<br />
is whether there is a role for the complement cascade<br />
in the pathology of prion diseases. Indeed, depletion of<br />
either one of the early complement factors (C1q, Bf/C2<br />
<strong>and</strong> C3) or the complement receptor (CD21/CD35) significantly<br />
delays the onset of disease symptoms in mice<br />
injected with limiting doses of the scrapie strains RML<br />
<strong>and</strong> ME7 (269, 315). The relative importance of CD21/35<br />
on hemopoietic <strong>and</strong> stromal cell types has been assessed<br />
through reciprocal reconstitution experiments by bone<br />
marrow transplantation. CD21/35 expression exclusively<br />
on FDCs in white pulp follicles resulted in prion titers,<br />
PrP Sc retention, <strong>and</strong> disease kinetics <strong>and</strong> severity similar<br />
to those of wild-type mice. CD21/35 expression on hemopoietic<br />
cells also significantly affected these parameters,
1130 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
but far less than FDC expression of CD21/35. Therefore,<br />
complement-mediated antigen trapping on FDCs is an<br />
important mechanism for lymphoid prion accumulation<br />
(530). The role of the classical complement cascade during<br />
peripheral prion infection certainly warrants further<br />
investigations, since complement is clearly an important<br />
determinant of pathogenesis yet its mechanics are not yet<br />
fully understood (14).<br />
B. Tropism of <strong>Prions</strong> for Inflammatory Foci<br />
Since proinflammatory cytokines <strong>and</strong> immune cells<br />
are involved in lymphoid prion replication, it is likely that<br />
chronic inflammatory conditions in nonlymphoid organs<br />
could affect the dynamics of prion distribution. Indeed,<br />
inclusion body myositis, an inflammatory disease of muscle,<br />
was reported to lead to the presence of large PrP Sc<br />
deposits in muscle (281). Many chronic inflammatory conditions,<br />
some of which are very common <strong>and</strong> include<br />
rheumatoid arthritis, type 1 diabetes, Crohn’s disease,<br />
Hashimoto’s disease <strong>and</strong> chronic obstructive pulmonary<br />
disease, result in organized inflammatory foci of B lymphocytes,<br />
FDCs, DCs, macrophages, <strong>and</strong> other immune<br />
cells associated with germinal centers (141, 224, 244, 489).<br />
In addition, tertiary follicles can be induced, <strong>and</strong> are<br />
surprisingly prevalent, in nonlymphoid organs by naturally<br />
occurring infections in ruminants (141, 502).<br />
Lymphoid follicles with prominent FDC networks<br />
can replicate prions in mice (210, 448), sheep (300), <strong>and</strong><br />
deer (200) (Fig. 8). In fact, in mice suffering from nephritis,<br />
hepatitis, or pancreatitis, prion accumulation occurs<br />
in otherwise prion-free organs (210). The presence of<br />
inflammatory foci consistently correlated with an upregulation<br />
of LTs <strong>and</strong> the ectopic induction of PrP C -expressing<br />
FDCs. Inflamed organs of mice lacking LT or LTR did<br />
not accumulate either PrP Sc or infectivity following prion<br />
inoculation. These data have raised concerns that analo-<br />
FIG. 8. Lymphoid follicles with prominent follicular dendritic cell<br />
(FDC) networks can replicate prions in mice, sheep, <strong>and</strong> deer. A: in<br />
prion-infected RIPLT-mouse, inflammatory foci in renal tissue overlap<br />
with PrP Sc deposition as shown by histoblot analysis of a renal cryosection<br />
blotted on a nitrocellulose membrane followed by proteinase K<br />
(PK) treatment <strong>and</strong> HE staininig. (Figure kindly provided by M. Heikenwalder.)<br />
B: in sheep infected with scrapie <strong>and</strong> presenting with mastitis,<br />
PrP Sc deposition in a mammary gl<strong>and</strong> coincides with tertiary follicles, as<br />
confirmed by petblot analysis of a paraffin section blotted on a nitrocellulose<br />
membrane, followed by PK treatment <strong>and</strong> HE staining. [Adapted<br />
from Ligios et al. (300).] C: in white-tailed deer experimentally inoculated<br />
with the agent of chronic wasting disease (CWD), PrP Sc is present<br />
in ectopic lymphoid tissue in the kidney. Note the presence of two<br />
lymphoid follicles subjacent to the uroepithelial layer <strong>and</strong> PrP Sc immunolabeling<br />
within the lymphoid follicles. (Figure kindly provided by<br />
A. N. Hamir.) HE, hematoxylin <strong>and</strong> eosin; IHC, immunohistochemistry;<br />
KM, medulla; RIPLT, transgenic mice expressing LT (lymphotoxin)<br />
under the control of the rat insulin promoter (RIP) in pancreatic -islet<br />
cells <strong>and</strong> renal proximal convoluted tubules.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
gous phenomena might occur in farm animals, since these<br />
are commonly in contact with inflammogenic pathogens.<br />
Indeed, PrP Sc has been observed in the inflamed mammary<br />
gl<strong>and</strong>s of sheep with mastitis <strong>and</strong> which are also<br />
infected with scrapie (300). These observations indicate<br />
that inflammatory conditions induce accumulation <strong>and</strong><br />
replication of prions in organs previously considered to<br />
be free from prion infection.<br />
In addition, inflammatory conditions could result in<br />
the shedding of the prion agent by excretory organs,
including the kidney. In fact, in various transgenic <strong>and</strong><br />
spontaneous mouse models of nephritis, prion infectivity<br />
was observed in the urine with both subclinical <strong>and</strong> terminal<br />
scrapie (448). Recently, consistent levels of infectivity<br />
have been detected in colostrum <strong>and</strong> milk from<br />
sheep incubating natural scrapie, several months prior to<br />
clinical onset. The presence of ectopic lymphoid follicles<br />
in ewes with lymphoproliferative mastitis could increase<br />
prion shedding in milk, although the prion infectivity was<br />
revealed in sheep with healthy mammary gl<strong>and</strong>s as well as<br />
those with chronic lymphoproliferative mastitis (287). If<br />
confirmed, these findings could have an impact on the risk<br />
assessment of dairy foodstuffs (for example, milk) <strong>and</strong><br />
could lead to a readjustment of current rules. It is possible<br />
that the horizontal spread of prions between hosts is<br />
mediated by secreted body fluids (for example, urine <strong>and</strong><br />
milk) that are derived from potentially infectious secretory<br />
organs (for example, kidney <strong>and</strong> mammary gl<strong>and</strong>s).<br />
However, chronic inflammation more commonly<br />
gives rise to granulomas whose cellular composition is<br />
different from that of lymphoid follicles. Granulomas occur,<br />
for example, in Crohn’s disease, sarcoidosis (235),<br />
<strong>and</strong> most mycobacterial (66, 146, 430), fungal, <strong>and</strong> parasitic<br />
infections, as well as in foreign body reactions. A<br />
recent study demonstrates that experimentally induced<br />
granulomas in mice enable prion replication after intraperitoneal<br />
inoculation (208). Because granulomas can occur<br />
at any site of the body, these results suggest that<br />
prions may colonize a broader spectrum of organs than<br />
previously anticipated. With respect to the relevance of<br />
the above findings for public health, it will be interesting<br />
to test whether prion replication in granulomas occurs in<br />
farm animals <strong>and</strong> in humans.<br />
C. Neuroinflammation in Prion Pathogenesis<br />
In the CNS, prion pathology involves large-scale activation<br />
<strong>and</strong> proliferation of microglia (215), the CNS<br />
equivalent of macrophages. The use of a prion organotypic<br />
slice culture assay (POSCA) (148) allowed pharmacogenetic<br />
ablation of microglia (Fig. 9A). In microgliadepleted<br />
slices, a 15-fold increase in prion titers <strong>and</strong> PrP Sc<br />
concentrations was observed. This suggests that the extensive<br />
microglia activation accompanying prion diseases<br />
represents an efficacious defensive reaction (Fig. 9, B–E)<br />
(149).<br />
In addition, it has been reported that T cells also<br />
infiltrate the CNS to some extent (52), which raises the<br />
possibility of atypical CNS inflammation, since the expression<br />
of both proinflammatory <strong>and</strong> effector cytokines<br />
are upregulated in prion infection (392). More importantly,<br />
intracerebral administration of prions has been<br />
shown to induce TSE in mice that have various immune<br />
deficiencies, including lack of B cells, T cells, interferon<br />
AGGREGATION AND INFECTIOUS DISEASE 1131<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
receptors, TNF, LTs or their receptors (267), receptors for<br />
IgG (FcRs), complement factors or their receptors (269),<br />
Toll-like receptors (398), or chemokine receptors (397).<br />
In all of these models, pathogenesis after intracerebral<br />
prion delivery proceeded with the same kinetics as in<br />
wild-type immunocompetent mice, <strong>and</strong> in terminally sick<br />
mice, intracerebral prion concentrations were unchanged<br />
(20). This evidence indicates that, after prions are present<br />
in the CNS, the disease course cannot be modified by<br />
manipulating immunological parameters.<br />
Furthermore, several studies have addressed the impact<br />
of the nuclear factor-B (NFB) pathway in prion<br />
pathogenesis. NFB is involved in a variety of physiological<br />
<strong>and</strong> pathological responses <strong>and</strong> plays an essential role<br />
in immune responses involving induction of inflammation,<br />
proliferation, <strong>and</strong> the regulation of apoptosis (56, 251). In<br />
acute <strong>and</strong> chronic neurodegenerative conditions such as<br />
AD, NFB is activated in neurons <strong>and</strong> glia, <strong>and</strong> it has been<br />
proposed that NFB might promote survival of neurons<br />
(245). Alternatively, NFB may contribute to neuronal<br />
degeneration through the production <strong>and</strong> release of inflammatory<br />
cytokines or of reactive oxygen molecules by<br />
microglia <strong>and</strong> astrocytes. In prion diseases, NFB activity<br />
was shown to be enhanced in parallel with the first neuronal<br />
pathological changes (256). Furthermore, the cytotoxic<br />
synthetic peptide PrP 106–126 activates NFB inmicroglia<br />
in vitro (33). Notably, it has been reported that<br />
NFB activity leads to mitochondrial apoptosis after<br />
prion infection (61). Despite these findings, it remains<br />
unclear whether NFB activation is protective or pathogenic<br />
in prion disease. However, when the impact of<br />
NFB signaling on prion disease was investigated in<br />
mouse models with a CNS-restricted elimination of IKK<br />
<strong>and</strong> in mice containing a nonphosphorylatable IKK subunit,<br />
no impairment of prion pathogenesis in the brain<br />
was observed (242).<br />
VII. SPREAD OF PRIONS ALONG PERIPHERAL<br />
AND CENTRAL NERVOUS SYSTEM<br />
PATHWAYS<br />
The process of prion infectivity transfer from the<br />
spleen to the CNS is termed “neuroinvasion.” In the last<br />
several years, a biphasic model has emerged to explain<br />
the process of prion. The first phase is characterized by<br />
widespread colonization of lymphoreticular organs, the<br />
details of which have been described in the previous<br />
section. The second phase has long been suspected to<br />
involve peripheral nerves. The innervation pattern of lymphoid<br />
organs is primarily sympathetic (150), <strong>and</strong> many<br />
studies suggest that is the way how the prion agent travels<br />
from lymphoid organs to the CNS (111, 115, 335). Not<br />
surprisingly, the sympathetic nervous system is affected<br />
in vCJD patients (198). The detection of PrP Sc in the
1132 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
FIG. 9. Role of microglia in prion disease. A: schematic representation for the conditional ablation of microglia in vitro <strong>and</strong> in vivo by using<br />
the cytotoxic prodrug ganciclovir (GCV) in CD11b-HSVTK mice (213). B: histoblot analysis of PrP Sc deposition in POSCA slices after 35 days in<br />
culture shows that PrP Sc accumulates predominantly in the molecular layer. Organotypic brain slices were prepared from 10-day-old tga20 TK (mice<br />
overexpressing PrP <strong>and</strong> carrying the CD11b-HSVTK transgene) <strong>and</strong> were inoculated with 100 g RML (R) or uninfected homogenate (Ø). PrP Sc was<br />
detected with anti-PrP antibody (POM1). C: accumulation of PrP Sc in slices was also shown by Western blot; tga20 TK <strong>and</strong> prnp o/o slices were<br />
cultured for 35 days, optionally digested with PK (g/ml), <strong>and</strong> probed with antibody POM1. D: microglia depletion in organotypic slices increases<br />
the amount of PK-resistant PrP. Organotypic slices from mice overexpressing PrP with the CD11b-HSVTK transgene (tga20 TK ) or without<br />
(tga20 TK ) were treated with GCV <strong>and</strong> inoculated with RML. Samples were PK-digested <strong>and</strong> PrP detected with POM1. E: microglia depletion in<br />
organotypic slices increases the infectivity as evaluated by SCEPA of homogenates of tga20 TK or prnp o/o/TK slices treated with GCV. Three<br />
independent biological replicas of tga20 TK <strong>and</strong> single replicas of prnp o/o/TK slices or RML were analyzed in 10-fold dilution steps using 6–12<br />
replica N2a-containing wells per dilution. Data are indicated as the number of infectious tissue culture units per gram of slice culture protein <strong>and</strong><br />
are the averages of biological replicas SD. Slices from the same animal (pairs of GCV <strong>and</strong> GCV samples) are represented by the same color.<br />
Sc, positive-control homogenate from brain of a mouse with scrapie; Inoc, inoculum. Left lane on all blots, molecular weight marker spiked with<br />
recombinant PrP C , yielding a PrP signal at 23 kDa with a cleavage product at 15 kDa. [B–E are adapted from Falsig et al. (149).]<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org
spleens of sCJD patients (183) indicates that the interface<br />
between cells of the immune <strong>and</strong> peripheral nervous systems<br />
might also be of relevance in sporadic prion diseases.<br />
Sympathectomy appears to delay the transport of<br />
prions from lymphatic organs to the thoracic spinal cord,<br />
which is the entry site of sympathetic nerves to the CNS.<br />
Denervation by injection of the drug 6-hydroxydopamine,<br />
as well as “immunosympathectomy” by injection of antibodies<br />
against nerve growth factor (NGF) leads to a<br />
rather dramatic decrease in the density of sympathetic<br />
innervation of lymphoid organs, <strong>and</strong> significantly delayed<br />
the development of scrapie (186). No alteration in lymphocyte<br />
subpopulations was detected in spleens at any<br />
time point investigated. In particular, no significant differences<br />
in the content of FDCs were detected between<br />
treated <strong>and</strong> untreated mice, which negate the possibility<br />
that the observed protection may be due to modulation of<br />
FDC microanatomy. Transgenic mice overexpressing<br />
NGF under control of the K14 promoter, whose spleens<br />
are hyperinnervated, developed scrapie significantly earlier<br />
than nontransgenic control mice.<br />
The distance between FDCs <strong>and</strong> splenic nerves influences<br />
the rate of neuroinvasion (397). FDC positioning<br />
was manipulated by ablation of the CXCR5 chemokine<br />
receptor, directing lymphocytes towards specific microcompartments<br />
(155). As such, the distance between germinal<br />
center-associated FDCs <strong>and</strong> nerve endings was reduced.<br />
This process resulted in an increased rate of prion<br />
entry into the CNS in CXCR5-deficient mice, probably<br />
owing to the repositioning of FDCs in juxtaposition with<br />
highly innervated, splenic arterioles.<br />
The cellular <strong>and</strong> molecular prerequisites for prion<br />
trafficking within the lymphoreticular system are not fully<br />
understood. Genetic or pharmacological ablation of germinal<br />
center B cells, located in close vicinity to FDCs, has<br />
shown no significant effects on splenic prion replication<br />
efficacy, PrP Sc distribution pattern, or latency to terminal<br />
disease (206), although in a previous report, the ablation<br />
of CD40L accelerated prion disease (86).<br />
The mechanism by which prions reach neurons <strong>and</strong><br />
take advantage of neuronal tracks to propagate from the<br />
periphery toward the CNS remains to be determined.<br />
Three different hypothesis could explain how prions enter<br />
neurons: 1) cell-cell contact, 2) vesicle transport, or<br />
3) “free-floating” prion infectivity.<br />
Convincing evidence for contact-mediated transmission<br />
of prion infectivity was presented in a study by<br />
Flechsig et al. (153a), where the inherent capacity of<br />
prions to strongly adhere to steel wires was used to study<br />
contact-mediated prion infection. Neuroblastoma cells<br />
adhering to such prion-coated steel wires become infected<br />
in tissue culture. Additionally, subsequent use of<br />
the identical steel wire mediates prion transmission efficiently<br />
to several PrP C -overexpressing indicator mice, in a<br />
AGGREGATION AND INFECTIOUS DISEASE 1133<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
short contact period of 30 min. Remarkably, this occurs<br />
without any reduction in prion infectivity. These data<br />
strongly suggest that contact-mediated transmission<br />
rather than an exchange of the infectious agent likely<br />
takes place. Consistent with these findings, cell-mediated<br />
infection was shown in a tissue-culture model (247). This<br />
study took advantage of genetically marked target cells in<br />
combination with scrapie mouse brain (SMB) cells chronically<br />
propagating PrP Sc (112). Several lines of evidence in<br />
this study, in particular efficient transmission after aldehyde<br />
fixation of the SMB cells, suggest that direct contact<br />
is responsible for the cell-to-cell transmission.<br />
A second possibility is neuronal prion transfer by<br />
vesicle-associated infectivity. Exosome-bound prion infectivity<br />
has been reported in two cell lines: Rov, a rabbit<br />
epithelial cell line, <strong>and</strong> Mov, a neuroglial cell line, which<br />
both express ovine PrP (151). This report of exosomes<br />
containing prions in vitro is in agreement with a study that<br />
suggests that retroviral infection robustly enhances the<br />
release of prion infectivity in cell culture (294). For example,<br />
prion infectivity within exosomes, which in turn<br />
may be released by prion-infected FDCs, may encounter<br />
peripheral nerves <strong>and</strong> contribute to neuroinvasion (15,<br />
397).<br />
The third potential source of prion infectivity may be<br />
cell-free, free-floating oligomeric or protofibrillar infectious<br />
particles (207). Several cell lines can be infected<br />
with brain homogenates or brain fractions treated in a<br />
way that renders the existence of intact cells or exosomes<br />
highly unlikely. However, this most likely does not exclude<br />
the possibility of prion infectivity encapsulated in<br />
micelles. One recent study that favors the latter hypothesis<br />
investigated the relationship between infectivity, converting<br />
activity, <strong>and</strong> the size of various PrP Sc -containing<br />
aggregates (464) <strong>and</strong> concluded that nonfibrillar particles,<br />
with masses equivalent to 14–28 PrP molecules, are the<br />
most efficient initiators of prion disease.<br />
All of these mechanisms shown in vitro potentially<br />
play a role in vivo. However, there is currently no convincing<br />
evidence that implies an exclusive role of any of<br />
the three possibilities in prion uptake by peripheral<br />
nerves in vivo. It remains plausible, therefore, that more<br />
than one of these pathways contributes to efficient prion<br />
uptake by peripheral nerves simultaneously.<br />
Although PrP C expression is known to modulate intranerval<br />
transport, it is unclear how prions are actually<br />
transported within peripheral nerves (184). Axonal <strong>and</strong><br />
nonaxonal transport mechanisms may be involved, <strong>and</strong><br />
nonneuronal cells (such as Schwann cells) may also play<br />
a role. Within the framework of the protein-only hypothesis,<br />
one may hypothesize a “domino” mechanism, by<br />
which infiltrating PrP Sc converts resident PrP C on the<br />
axolemmal surface, sequentially propagating the infection.<br />
While speculative, this model is attractive, since it<br />
may accommodate the finding that the velocity of neural
1134 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
prion spread is extremely slow (257) <strong>and</strong> may not follow<br />
the canonical mechanisms of fast axonal transport. The<br />
second hypothesis is that prion transport occurs within<br />
the axons of peripheral nerves similar to normal cargo<br />
proteins. This is known as the “streetcar” hypothesis (17).<br />
In the streetcar hypothesis, PrP Sc is taken up at nerve<br />
endings <strong>and</strong> then transported retrogradely, presumably by<br />
a microtubule-based mechanism, to the CNS.<br />
Despite evidence that neurons are the key mediators<br />
of prion propagation toward the CNS, low-efficiency alternatives<br />
such as transport via blood cannot be excluded<br />
completely: prion infectivity could directly invade the<br />
brain via the blood-brain barrier (BBB) (36). The cellular<br />
<strong>and</strong> molecular preconditions for such a process remain<br />
elusive. However, invasion of prion infectivity through the<br />
BBB could depend on the prion strain <strong>and</strong> the dose of<br />
administered prions (207).<br />
The existence of multiple prion strains is likely to<br />
make neuronal transport even more complex. It is conceivable<br />
that distinct strains use different mechanisms for<br />
uptake <strong>and</strong> transport (37). This may affect not only the<br />
mechanisms of prion uptake by different neuronal cell<br />
populations, <strong>and</strong> cell-to-cell transmissions, but may also<br />
alter the route of neuroinvasion, type of transport, lesion<br />
profile, or the incubation time of an infected host (8).<br />
The spread of prions within the central nervous system<br />
has been studied by ocular administration of prions.<br />
The retina is a part of the CNS, <strong>and</strong> intraocular injection<br />
does not induce direct physical trauma to the brain, which<br />
may disrupt the BBB <strong>and</strong> impair other aspects of brain<br />
physiology.<br />
Evidence that spread of prions occurs axonally relies<br />
mainly on the demonstration of diachronic spongiform<br />
changes along the retinal pathway after intraocular infection<br />
(161). Reports of iatrogenic prion transmissions in<br />
humans via cornea transplants are consistent with the<br />
idea that prions spread axonally, implying that prions<br />
propagate retrogradely toward the cornea <strong>and</strong> anterograde<br />
from the cornea to the brain (143).<br />
To investigate whether the spread of prions within<br />
the CNS is dependent on PrP C expression in the visual<br />
pathway, PrP-producing neural grafts have been used as<br />
sensitive indicators of the presence of prion infectivity in<br />
the brain of Prnp o/o hosts. After prion inoculation in the<br />
eyes of grafted Prnp o/o mice, none of the grafts showed<br />
signs of scrapie. It was concluded, therefore, that infectivity<br />
administered to the eye of PrP-deficient hosts cannot<br />
induce scrapie in a PrP-expressing brain graft (65).<br />
Engraftment of Prnp o/o mice with PrP C -producing<br />
tissue might lead to an immune response to PrP which<br />
neutralizes PrP Sc infectivity (214). To definitively rule out<br />
the possibility that prion transport was disabled by a<br />
neutralizing immune response, Prnp o/o mice were rendered<br />
tolerant by expressing PrP C under the control of the<br />
lck promoter. These mice overexpress PrP on T-lympho-<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
cytes but are resistant to scrapie <strong>and</strong> do not replicate<br />
prions in brain, spleen, <strong>and</strong> thymus after intraperitoneal<br />
inoculation with scrapie prions (416). Engraftment of<br />
these mice with PrP-overexpressing neuroectoderm did<br />
not lead to the development of antibodies to PrP after<br />
intracerebral or intraocular inoculation, presumably due<br />
to clonal deletion of PrP-immunoreactive T-lymphocytes.<br />
As before, intraocular inoculation with prions did not<br />
provoke scrapie in the graft, supporting the conclusion<br />
that lack of PrP C , rather than immune response to PrP,<br />
prevented prion spread (65). Therefore, PrP C appears to<br />
be necessary for the spread of prions along the retinal<br />
projections <strong>and</strong> within the CNS.<br />
These results indicate that intracerebral spread of<br />
prions is based on a PrP C -paved chain of cells, perhaps<br />
because they are capable of supporting prion replication.<br />
When such a chain is interrupted by interposed cells that<br />
lack PrP C , as in the case described here, no propagation<br />
of prions to the target tissue can occur. Perhaps prions<br />
require PrP C for propagation across synapses. PrP C is<br />
present in the synaptic region (157) <strong>and</strong> certain synaptic<br />
properties are altered in Prnp o/o mice (120, 520).<br />
Although a wealth of data has been acquired about<br />
the transport of PrP Sc from the periphery into the brain in<br />
recent years, the exact molecular mechanisms of neuronal<br />
prion transport are still unclear. It also is becoming<br />
clear that investigation of the precise molecular transport<br />
mechanisms within neurons is much more difficult than<br />
previously thought. It is not trivial to test the involvement<br />
of retrograde neuronal transport in prion pathogenesis<br />
because a complete block of this transport system is incompatible<br />
with long-term survival. Furthermore, mouse models<br />
with partially impaired transport mechanisms do not display<br />
altered prion pathogenesis, yet such negative results by no<br />
means disprove a role for axonal transport.<br />
One possible method of circumventing problems associated<br />
with in vivo studies may be to establish cell<br />
culture model systems of transport in vitro <strong>and</strong> ex vivo.<br />
Such systems may pave the way to a more precise molecular<br />
underst<strong>and</strong>ing of prion transport. Another advantage<br />
of in vitro systems may be the ability to pharmacologically<br />
manipulate specific neuronal transport pathways,<br />
which may be difficult to perform in vivo (207).<br />
VIII. TOWARDS ANTIPRION THERAPEUTICS<br />
The current therapeutic l<strong>and</strong>scape for prion diseases<br />
gives little reason to rejoice. An impressive wealth of<br />
molecules has been considered as potential antiprion lead<br />
compounds. However, none of these therapeutic leads<br />
has yet proven their usefulness in clinical settings, <strong>and</strong><br />
some have conspicuously failed. A startling variety of<br />
substances appears to possess prion-curing properties. A<br />
nonexhaustive list includes compounds as diverse as
Congo red (98), amphotericin B, anthracyclins (487), sulfated<br />
polyanions (100), porphyrins (104, 401), branched<br />
polyamines (485), “ sheet breakers” (475), the spice<br />
curcumin (102), <strong>and</strong> the single-str<strong>and</strong>ed phosphorothioated<br />
analogs of natural nucleic acids (273).<br />
In drug discovery generally, <strong>and</strong> in TSE therapeutics<br />
specifically, promising compounds are often initially<br />
screened using relatively high-throughput in vitro tests,<br />
prior to testing of the best c<strong>and</strong>idates in vivo. However,<br />
relatively few of the antiprion compounds that are active<br />
in vitro have shown any efficacy in vivo. Additional hurdles<br />
may lie in the identification of drugs that have sufficient<br />
in vivo efficacies, bioavailabilities, pharmacokinetics,<br />
<strong>and</strong> safety profiles to allow for applicability in the<br />
clinical phase of disease. Alternatively, one might conclude<br />
(<strong>and</strong> we lean towards this conclusion) that the<br />
initial cell culture screens are not very good at predicting<br />
in vivo antiprion activity.<br />
In our view, it is premature to treat patients with<br />
alleged antiprion drugs on the sole basis of antiprion<br />
efficacy in neuroblastoma cells. This shortcut was taken<br />
in the case of quinacrine, which cures scrapie-infected<br />
cultured cells with impressive efficacy (140), yet appears<br />
to be utterly ineffective in scrapie-infected mice (121) <strong>and</strong><br />
in CJD patients (123), besides being severely hepatotoxic<br />
(444). On the other h<strong>and</strong>, it is only fair to acknowledge<br />
that these are daunting tasks for any drug discovery<br />
project, even with great lead compounds in h<strong>and</strong>, <strong>and</strong> the<br />
lack of success thus far in identifying drugs that impact<br />
the course of prion disease in the clinical phase does not<br />
diminish the importance of prion drug discovery efforts<br />
that have been undertaken to date.<br />
For therapeutic or prophylactic purposes, it is possible<br />
to exploit the roles of the lymphoid system <strong>and</strong> immune<br />
cells in prion pathogenesis. At least four alternatives<br />
can be envisaged on the basis of the information that<br />
we have discussed: removal of functional FDCs <strong>and</strong> therefore<br />
ablation of lymphoid prion-replication sites; stimulation<br />
of the innate immune system; enhancement of elimination<br />
of PrP Sc using PrP-specific antibodies; or binding<br />
of available PrP C or PrP Sc so that they are unavailable for<br />
conversion (Fig. 10). All of these approaches, which include<br />
both suppression <strong>and</strong> stimulation of the immune<br />
system, are now being tested in suitable in vivo systems<br />
using mice experimentally infected with mouse-adapted<br />
scrapie. However, because the lymphoid system has been<br />
found to be involved in almost all forms of TSE, it is<br />
reasonable to presume that mouse-adapted scrapie provides<br />
a realistic generic model for TSE therapy.<br />
A. Innate Immunity <strong>and</strong> Antiprion Defense<br />
Antiprion treatment strategies focusing on immunosuppression<br />
consist of conditional dedifferentiation of<br />
AGGREGATION AND INFECTIOUS DISEASE 1135<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
FDCs with LTR-Ig, suppression of germinal centers, <strong>and</strong><br />
disruption of lymphoid microarchitecture. LTR-Ig treatment<br />
causes germinal center disruption due to the breakdown<br />
of FDC networks (Fig. 10A). The data from studies<br />
using LTR-Ig indicate that postexposure treatment of<br />
humans with LTR-Ig could only be considered for prophylaxis<br />
at well-defined, early time points in cases of<br />
known prion exposure. These cases might include recipients<br />
of blood transfusions from patients with CJD <strong>and</strong><br />
researchers, pathologists, neurologists, neurosurgeons,<br />
<strong>and</strong> technicians after accidental CJD injection. In these<br />
situations, we think that a case could be made for experimental<br />
use of postexposure prophylaxis with LTR-Ig,<br />
although it is not known how soon after exposure<br />
LTR-Ig would need to be administered. It should be<br />
considered that LTR-Ig will not offer any relief to patients<br />
with overt CJD, for whom neural entry has already<br />
taken place.<br />
Theoretically, LTR-Ig treatment might have unwanted<br />
effects on immune function. However, manipulation<br />
of the LT pathway has been carried out in<br />
macaques without apparent side effects. Primary antibody<br />
responses to keyhole limpet hemocyanin were<br />
found to be unaltered during a 20-day period (192).<br />
Moreover, LT-fusion proteins are already entering clinical<br />
trials as a treatment for rheumatoid arthritis. Hopefully,<br />
the results of such studies will become available<br />
in the foreseeable future (20).<br />
The ordered aggregate state of PrP Sc might render it<br />
recognizable as a pathogen-associated molecular pattern;<br />
therefore, the members of the Toll-like receptor (TLR)<br />
family might be involved in the recognition <strong>and</strong> subsequent<br />
degradation of prions.<br />
However, the kinetics of prion pathogenesis in<br />
MyD88 (myeloid differentiation primary-response protein<br />
88)-deficient mice inoculated with prions (by the<br />
intraperitoneal route) are identical to the kinetics observed<br />
in the wild-type control mice (398), suggesting<br />
that signaling by TLR1, -2, -6, <strong>and</strong> -9 (mediated by the<br />
adapter protein MyD88; Ref. 1) are probably not involved<br />
in prion recognition <strong>and</strong> signaling. Nevertheless,<br />
targeting TLR9 therapeutically might have other beneficial<br />
effects. TLR9 recognizes DNA sequences that are<br />
overrepresented in bacterial DNA. For example, unmethylated<br />
cytosine phosphate guanosine (CpG) motifs<br />
present in bacterial DNA can stimulate mouse <strong>and</strong> human<br />
immune responses through TLR9 (211) (Fig. 10B).<br />
Repetitive CpG motifs in synthetic oligodeoxynucleotides<br />
(CpG-ODN) simulate bacterial unmethylated nucleic<br />
acid sequences, <strong>and</strong> thereby stimulate the innate<br />
immune system through TLR9 expressed on various<br />
immune cells, including monocytes, macrophages, <strong>and</strong><br />
dendritic cells.<br />
CpG-ODN treatment has been discussed as a possible<br />
therapy to delay prion disease, primarily based on prom-
1136 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
FIG. 10. Immunotherapeutic strategies for prion disease. A: treatment with the lymphotoxin- receptor fusion protein (LTR)-Ig breaks up the FDC<br />
networks <strong>and</strong> disrupts lymphoid follicles. The best protection is achieved when the fusion protein is administered immediately after exposure to prions.<br />
B: ablation of mature follicular dendritic cells (FDCs) delays the development of prion disease in mice. However, treatment with multiple doses of<br />
CpG-containing oligodeoxynucleotides (CpG ODNs) produces severe unwanted side effects, including immunosuppression, liver necrosis, <strong>and</strong> thrombocytopenia.<br />
C: vaccination against a self-protein is difficult because of immune tolerance, <strong>and</strong> it has the potential to induce autoimmune disease. Transgenic<br />
expression of an immunoglobulin chain containing the epitope-interacting region of 6H4, a high-affinity anti-PrP monoclonal antibody, associated with<br />
endogenous <strong>and</strong> chains, leads to high anti-PrP C titers in Prnp o/o <strong>and</strong> Prnp / mice. It suffices to block prion pathogenesis upon intraperitoneal prion<br />
inoculation. After active immunization with full-length PrP in attenuated Salmonella vector, the mice develop high PrP specific antibody titers. D: treatment<br />
with dimeric full-length PrP fused to the Fc portion of human IgG1 (PrP-Fc 2) delays the development of prion disease in mice, most probably owing to<br />
its interaction with the disease-associated PrP (PrP Sc ). LT- 1 2, LT heterotrimer; TLR, Toll-like receptor.<br />
ising results in mouse scrapie (450). The delay in the<br />
development of prion disease in this model could be due<br />
to the destruction of the primary site of peripheral prion<br />
amplification, the lymphoid follicles (209). Alternatively,<br />
the massive expansion of macrophage <strong>and</strong> dendritic cells<br />
that is evident following repetitive CpG-ODN treatment<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
might lead to enhanced PrP Sc degradation or prion sequestration.<br />
Macrophages might conceivably function as prion<br />
transporters when exposed to high prion titers; on the<br />
other h<strong>and</strong>, they might also inhibit prion infectivity when<br />
confronted with manageable prion titers (48). However,
despite these promising results, CpG-ODNs are not likely<br />
to be a viable antiprion therapy owing to the severe toxic<br />
side effects associated with repeated administration. One<br />
might argue that severe side effects could be tolerable in<br />
the case of a disease that is invariably fatal. However, if<br />
the antiprion action of CpG ODNs is mediated by indiscriminate<br />
immune suppression, then there are alternative<br />
ways to achieve this goal that would at least not lead to<br />
hepatotoxicity.<br />
An interesting alternative approach might include<br />
phagocyte activation <strong>and</strong> targeted prion degradation without<br />
the reported adverse side effects associated with<br />
CpG-ODNs (20).<br />
B. Adaptive Immunity <strong>and</strong> Preexposure<br />
Prophylaxis Against <strong>Prions</strong><br />
For many conventional viral agents, vaccination is<br />
the most effective method of infection control. But is it at<br />
all possible to induce protective immunity in vivo against<br />
prions? <strong>Prions</strong> are extremely sturdy, <strong>and</strong> their resistance<br />
to sterilization is proverbial. Preincubation of PrP Sc inoculum<br />
with anti-PrP antisera was reported to reduce the<br />
prion titer of infectious hamster brain homogenates by up<br />
to 2 log units (168), <strong>and</strong> an anti-PrP antibody was found to<br />
inhibit formation of PrP Sc in a cell-free system (227). Also,<br />
antibodies (269) <strong>and</strong> F(ab) fragments raised against certain<br />
domains of PrP (144, 389) can suppress prion replication<br />
in cultured cells. However, it is difficult to induce<br />
humoral immune responses against PrP C <strong>and</strong> PrP Sc . This<br />
is most likely due to tolerance of the mammalian immune<br />
system to PrP C , which is an endogenous protein expressed<br />
rather ubiquitously. Ablation of the Prnp gene<br />
(85) renders mice highly susceptible to immunization<br />
with prions (65). Many of the best available monoclonal<br />
antibodies to the prion protein have been generated in<br />
Prnp o/o mice.<br />
However, Prnp o/o mice are unsuitable for testing vaccination<br />
regimens, since they do not support prion pathogenesis<br />
(84). Second, it was generally thought (with good<br />
reason) that antibodies specific for PrP C , if they could be<br />
elicited at all, might lead to severe systemic immunemediated<br />
diseases, because PrP is expressed by many cell<br />
types. Third, PrP-specific antibodies would be unlikely to<br />
cross the BBB in therapeutic concentrations.<br />
To test these various possibilities <strong>and</strong> circumvent the<br />
problem of PrP tolerance, genes encoding high-affinity<br />
anti-PrP antibodies (originally generated in Prnp o/o mice)<br />
were used to reprogram B-cell responses of prion-susceptible<br />
mice that express PrP C . In 2001, it was reported that<br />
mice transgenic for the -chain of a PrP-specific antibody<br />
were protected against prion disease after exposure by<br />
intraperitoneal inoculation (214) (Fig. 10C). A blatant autoimmune<br />
disease as a consequence of antiprion immu-<br />
AGGREGATION AND INFECTIOUS DISEASE 1137<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
nization was not observed, unless transgenic PrP C was<br />
artificially expressed at nonphysiological, extremely high<br />
levels.<br />
The strategy outlined above delivers proof-of-principle<br />
that a protective humoral response against prions can<br />
be mounted by the mammalian immune system <strong>and</strong> suggests<br />
that B cells are not intrinsically tolerant to PrP C . The<br />
challenges to practical antiprion immunization, however,<br />
are enormous. While providing an encouraging proof of<br />
principle, transgenic immunization cannot easily be reduced<br />
to practice. Furthermore, no protection was observed<br />
if treatment was started after the onset of clinical<br />
symptoms, suggesting that passive immunization might be<br />
a good c<strong>and</strong>idate for prophylaxis rather than therapy of<br />
TSEs. It was then found, in a follow-up study, that passive<br />
transfer of anti-PrP monoclonal antibodies can delay the<br />
onset of scrapie in prion-infected mice (518). Moreover,<br />
intracranial delivery of PrP C -specific antibodies (those<br />
having the epitope between aa 95–105 of the PrP sequence)<br />
has been shown to result in neuronal apoptosis in<br />
the cerebellum <strong>and</strong> hippocampus, most likely through<br />
clustering of PrP C , which is thought to trigger an abnormal<br />
signaling pathway (469). These results are alarming<br />
<strong>and</strong> certainly reinforce the concept that adequate in vivo<br />
safety studies must be carried out before prion immunoprophylaxis<br />
trials take place in humans. Active immunization,<br />
like in most antiviral vaccines, may be more effective,<br />
but is rendered exceedingly difficult by the stringent<br />
tolerance to PrP C (476). The laboratory of Thomas<br />
Wisnieswki was able to induce active immunization with<br />
recombinant prion protein <strong>and</strong> a delay in the onset of<br />
prion disease in wild-type mice was observed, although<br />
the therapeutic effect was relatively modest <strong>and</strong>, eventually,<br />
all the mice succumbed to the disease (463). This<br />
limited therapeutic effect may be explained by the observation<br />
that antibodies generated against prokaryotic PrP<br />
often do not have a high affinity towards PrP C (394).<br />
The possibility of producing protective immunity<br />
against prions has captured the imagination of a considerable<br />
number of scientists, <strong>and</strong> additional reports have<br />
since surfaced describing original methods of circumventing<br />
PrP tolerance <strong>and</strong> inducing an immune response in<br />
animals that express the normal prion protein, including<br />
mixing of the immunogenic moiety with bacterial chaperons<br />
(274). In a different study, tolerance was overcome by<br />
oral inoculation of the PrP protein expressed in an attenuated<br />
Salmonella vector. This mucosal vaccine induced<br />
gut anti-PrP immunoglobulins IgA <strong>and</strong> systemic anti-PrP<br />
IgG in 100% of mice with a high mucosal anti-PrP IgA titer<br />
<strong>and</strong> a high systemic IgG titer. Upon oral challenge with<br />
PrP Sc scrapie strain 139A, mice remained without symptoms<br />
of PrP infection at 400 days (193) (Fig. 10C). At<br />
present, it is unclear whether vaccination approaches will<br />
ultimately be translated to clinical practice. The predic-
1138 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
tive value of the different in vitro <strong>and</strong> in vivo experiments<br />
is limited, <strong>and</strong> further investigations will be required.<br />
C. Soluble Prion Antagonists<br />
In several paradigms, expression of two PrP C moieties<br />
with subtle differences antagonizes prion replication.<br />
The molecular basis for these effects is unknown.<br />
Perhaps the subtly modified PrP C acts as a decoy by<br />
binding incoming PrP Sc (or protein X) <strong>and</strong> sequestering it<br />
into a complex incapable of further replication.<br />
To test the latter hypothesis, a transgenic mouse<br />
was developed that expresses soluble full-length mouse<br />
PrP rendered dimeric by fusion with the Fc portion of<br />
human IgG1 (known as PrP-Fc 2) (Fig. 10D). After prion<br />
inoculation, these mice were surprisingly resistant to<br />
prion disease (343). The PrP-Fc 2 was not converted to<br />
a prion-disease-causing isoform. Moreover, when the<br />
transgenic mice expressing PrP-Fc 2 were back-crossed<br />
with wild-type mice <strong>and</strong> then inoculated with prions,<br />
they showed marked retardation in the development of<br />
prion disease, which was equivalent to a 10 5 -fold reduction<br />
in titer of the prion-infected inoculum. This antiprion<br />
effect occurred in two different lines of PrP-Fc 2expressing<br />
transgenic mice after either intracerebral or<br />
intraperitoneal infection with scrapie. Therefore, it<br />
seems that PrP-Fc 2 effectively antagonizes prion accumulation<br />
in the spleen <strong>and</strong> brain. Because PrP-Fc 2 cannot<br />
be converted to the protease-resistant, diseasecausing<br />
isoform, it might be effectively functioning as a<br />
“sink” for PrP Sc , by binding PrP Sc <strong>and</strong> preventing the<br />
binding <strong>and</strong> conversion of PrP C (20).<br />
Delivery of the soluble prion antagonist PrP-Fc 2 to<br />
the brains of mice by lentiviral gene transfer impaired<br />
replication of disease-associated PrP Sc <strong>and</strong> delayed disease<br />
progression (178). These results suggest that somatic<br />
gene transfer of prion antagonists may be effective for<br />
postexposure prophylaxis of prion diseases. In addition, it<br />
remains to be established whether the current form of<br />
PrP-Fc 2 has the strongest antiprion properties. For instance,<br />
the introduction of dominant-negative mutations<br />
analogous to those described for Prnp (374, 391) might<br />
considerably augment its efficacy. However, further research<br />
is needed to establish whether it may be effective<br />
as a biopharmaceutical.<br />
IX. PROGRESS IN THE DIAGNOSTICS OF<br />
PRION DISEASES<br />
As with any other disease, early diagnosis would<br />
significantly advance the chances of success of any possible<br />
intervention approaches. Unfortunately, prion diagnostics<br />
continue to be rather primitive. Presymptomatic<br />
diagnosis is virtually impossible, <strong>and</strong> the earliest possible<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
diagnosis is based on clinical signs <strong>and</strong> symptoms. Hence,<br />
prion infection is typically diagnosed after the disease has<br />
already progressed considerably.<br />
A significant advance in prion diagnostics was accomplished<br />
in 1997 by the discovery that proteaseresistant<br />
PrP Sc can be detected in tonsillar tissue of<br />
vCJD patients (221). It was hence proposed that tonsil<br />
biopsy may be the method of choice for diagnosis of<br />
vCJD (218). Furthermore, there have been reports of<br />
individual cases showing detectable amounts of PrP Sc<br />
at preclinical stages of the disease in the tonsil (443) as<br />
well as in the appendix (223), indicating that lymphoid<br />
tissue biopsy may represent a potential test for asymptomatic<br />
individuals. These observations triggered large<br />
screenings of human populations for subclinical vCJD<br />
prevalence, using appendectomy <strong>and</strong> tonsillectomy<br />
specimens (187). PrP Sc -positive lymphoid tissues were<br />
long considered to be a vCJD-specific feature that<br />
would not apply to any other forms of human prion<br />
diseases (218). However, a successive survey of peripheral<br />
tissues of patients with sporadic CJD has led to the<br />
identification of PrP Sc in as many as one-third of skeletal<br />
muscle <strong>and</strong> spleen samples (183). In addition, PrP Sc<br />
was found in the olfactory epithelium of patients suffering<br />
from sCJD (532). These unexpected findings<br />
raise the hope that minimally invasive diagnostic procedures<br />
may take the place of brain biopsy in intravital<br />
CJD diagnostics.<br />
For almost three decades, all gold st<strong>and</strong>ard methods<br />
for the molecular diagnosis of prion diseases have relied<br />
on the use of proteinase K (PK) to differentiate PrP C <strong>and</strong><br />
PrP Sc . Recently, the complementary use of the protease<br />
thermolysin has been introduced. This protease digests<br />
PrP C but, unlike PK, leaves PrP Sc intact without truncation<br />
of the NH 2 terminus (126, 376).<br />
The development of highly sensitive assays for biochemical<br />
detection of PrP Sc in tissues <strong>and</strong> body fluids is a<br />
top priority. One way to achieve this goal is to develop<br />
high-affinity immunoreagents that recognize PrP Sc . Examples<br />
include the “POM” series of antibodies that recognize<br />
various well-defined conformational epitopes in the structured<br />
COOH-terminal region of PrP C , <strong>and</strong> linear epitopes<br />
in the unstructured NH 2-terminal region (395). Because of<br />
the particular nature of the epitopes to which they are<br />
directed, some of these antibodies have affinities for the<br />
prion protein in the femtomolar range. Antibodies that<br />
specifically bind PrP Sc without binding PrP C have also<br />
been reported (279, 358), yet their affinity seems to be<br />
limited <strong>and</strong> their diagnostic value has awaited confirmation<br />
for more than one decade to no avail.<br />
Searching for PrP Sc binding reagents, Lau et al. (292)<br />
discovered PrP-derived peptides that bound PrP Sc . When<br />
coupled with a s<strong>and</strong>wich ELISA for detection, these peptide<br />
binding reagents create a sensitive assay that can detect<br />
PrP Sc nanoliter amounts of 10% (wt/vol) vCJD brain homog-
enate diluted in plasma, thereby yielding a powerful <strong>and</strong><br />
scalable assay that is very well suitable to blood testing.<br />
PMCA is also a promising method for the sensitive<br />
detection of the pathological prion protein (434, 473). It<br />
was recently shown to increase sensitivity 6,600-fold over<br />
st<strong>and</strong>ard detection methods (95). Amplifiable PrP Sc was<br />
detected in the blood of scrapie-infected hamsters by<br />
PMCA during most of the presymptomatic phase of disease<br />
(432).<br />
LCPs were recently developed as a novel class of<br />
amyloidotropic dyes (216, 366). These dyes contain a<br />
swiveling thiophene backbone, <strong>and</strong> the optical processes,<br />
e.g., the fluorescence from the dye, are highly<br />
sensitive to the geometry of the thiophene backbone.<br />
Hence, upon interaction with protein aggregates with a<br />
distinct morphology, the rotational freedom of the LCP<br />
backbone is restricted in a specific way <strong>and</strong> a unique<br />
optical fingerprint is obtained for a given protein conformation.<br />
Instead of measuring simply the total<br />
amount of aggregated protein, heterogeneous populations<br />
of specific protein aggregates can be differentiated<br />
by LCP staining. In a transgenic mouse model of<br />
AD pathology, LCPs identified a striking heterogeneity<br />
in amyloid plaques (365). LCPs also specifically bind<br />
prion deposits, even those which were negative for<br />
binding to other amyloidotropic dyes (Congo red <strong>and</strong><br />
ThT), <strong>and</strong> different prion strains could be discriminated<br />
via individual staining patterns of LCPs with distinct<br />
ionic side chains (462).<br />
Another exciting prospect may be the combination<br />
of PMCA with LCPs for PrP Sc detection. The unique<br />
photophysical properties of polythiophenes may pave<br />
the way for a “real-time PMCA,” where the buildup,<br />
lifetime, <strong>and</strong> conformational properties of prion aggregates<br />
may be visualized kinetically (9).<br />
The use of surrogate biomarkers represents a diagnostic<br />
strategy fundamentally different from those<br />
delineated above. Since they typically identify secondary<br />
host reactions, surrogate biomarkers of prion infection<br />
cannot aspire to match the specificity of PrP Sc<br />
detection. On the other h<strong>and</strong>, surrogate biomarkers<br />
may be useful for identifying subjects at risk <strong>and</strong> specifying<br />
acceptance or deferral of blood donations. In<br />
such cases, high sensitivity (i.e., the identification of all<br />
suspect individuals) is more important than absolute<br />
diagnostic specificity, as the latter can be supplied by<br />
confirmatory assays. Ideally, these surrogate markers<br />
should be detectable at preclinical stages of disease<br />
<strong>and</strong> differentially expressed in easily accessible body<br />
fluids such as blood or urine.<br />
S-100, neuron-specific enolase, <strong>and</strong> 14-3-3 protein<br />
have been reported to be elevated in cerebrospinal fluid<br />
(CSF) of sCJD patients (240, 442). These proteins may<br />
represent consequences of CNS damage <strong>and</strong> neuronal<br />
death. The cysteine proteinase inhibitor cystatin C was<br />
AGGREGATION AND INFECTIOUS DISEASE 1139<br />
also reported to be elevated in CSF of sCJD patients<br />
(393). Recently, urinary 1-antichymotrypsin has also<br />
been identified as a novel biomarker of prion infection<br />
(347).<br />
The gold st<strong>and</strong>ard of prion diagnostics is the ability<br />
to detect prion infectivity itself. Until recently, the<br />
animal bioassay was the only method available to<br />
screen for prion infectivity, for example, by using transgenic<br />
mice overexpressing PrP C (tga20) (154). Recently,<br />
the bank vole (Clethrionomys glareolus) has<br />
been suggested as a new <strong>and</strong> efficient model for bioassay<br />
of TSEs from different species, including human,<br />
sheep, goat, mouse, <strong>and</strong> hamster (2, 369). Additionally,<br />
the establishment of a human immune system in the mouse<br />
could be an efficient tool to test the potential human pathogenicity<br />
of various prion strains in vivo (14).<br />
However, these bioassays take 6–7 mo to complete<br />
<strong>and</strong> are very costly. More recently, the development of<br />
highly susceptible, cloned neural cell lines (PK1 N2a)<br />
have provided an assay that improves the precision,<br />
cost, <strong>and</strong> time required to do prion detection bioassays,<br />
<strong>and</strong> might lend itself to high-throughput automation<br />
(270). Although such assays have the potential to advance<br />
methodologies aimed at the diagnostic assessment<br />
of whether the prion agent is present, it should be<br />
noted that these cell lines are currently reported to be<br />
permissive only to murine prions. Future advances will<br />
hopefully provide a means by which the full range of<br />
prion strains <strong>and</strong> species can be assayed.<br />
X. CONCLUDING REMARKS<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
The study of prions has taken several unexpected<br />
turns over the years. The development <strong>and</strong> appropriate<br />
use of tools <strong>and</strong> technologies has enabled us to answer<br />
some long-st<strong>and</strong>ing key questions; however, many questions<br />
are still left unanswered. The physiological function<br />
of PrP C remains unknown. Although the Prnp gene<br />
encoding PrP C was identified in 1985 (39, 370) <strong>and</strong> the<br />
Prnp knockout mice were described in 1992 (85), the<br />
function of the protein is shrouded in mystery. Elucidation<br />
of the physiological function of PrP C has the<br />
potential to help researchers underst<strong>and</strong> the mechanisms<br />
involved in prion-induced pathogenesis.<br />
The molecular mechanisms of prion replication are<br />
not completely defined, <strong>and</strong> the possibility that other<br />
proteins assist the process cannot be excluded. We still<br />
do not underst<strong>and</strong> how strain information is maintained<br />
<strong>and</strong> transmitted, <strong>and</strong> we have no notion of the mechanisms<br />
that define the tropisms of prion strains. Finally, we<br />
do not underst<strong>and</strong> how neurotoxicity is induced by the<br />
prion agent, <strong>and</strong> why it is less toxic to cells of the immune<br />
system, where it also undergoes live replication. The ability<br />
to answer these questions in the future will rely mainly
1140 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
on the quality of the tools <strong>and</strong> technologies available to<br />
the prion field. These unresolved questions provide an<br />
opportunity for additional research which may have a<br />
significant impact on further protein misfolding disorders.<br />
ACKNOWLEDGMENTS<br />
This article honors the present <strong>and</strong> past members of the<br />
Aguzzi laboratory, whose enthusiastic commitment led to much<br />
of the work described here. Special thanks to Petra Schwarz for<br />
maintaining our prion-infected mouse colony in impeccable<br />
shape <strong>and</strong> to Rita Moos for excellent technical assistance.<br />
Mathias Heikenwälder, Christina Sigurdson, Jeppe Falsig, <strong>and</strong><br />
Mario Nuvolone provided crucial help with the section on “Immunological<br />
aspects of Prion disease” <strong>and</strong> Simone Hornemann<br />
with the section on “Structures of purified PrP C <strong>and</strong> PrP Sc .”<br />
Certain parts of the history of prion research were adapted from<br />
a previously published book chapter [A. Aguzzi. In: Topley &<br />
Wilson’s Microbiology <strong>and</strong> Microbial Infections (10 th ed.), 2005]<br />
whose previous edition had been published by Dr. Stanley B.<br />
Prusiner. We are grateful to Dr. Prusiner for giving us permission<br />
to utilize some of his material.<br />
Address for reprint requests <strong>and</strong> other correspondence: A.<br />
Aguzzi, Institute of Neuropathology, University Hospital Zürich,<br />
Schmelzbergstrasse 12, CH-8091 Zürich, Switzerl<strong>and</strong> (e-mail:<br />
adriano.aguzzi@usz.ch).<br />
GRANTS<br />
A. Aguzzi is supported by grants from the University of Zurich;<br />
the Swiss Federal Offices of Education, Science, <strong>and</strong> Health; the<br />
Swiss National Foundation; the National Center for Competence in<br />
Research on neural plasticity <strong>and</strong> repair; the United Kingdom Department<br />
for Environment, Food, <strong>and</strong> Rural Affairs; <strong>and</strong> the<br />
Stammbach Foundation. A. M. Calella was supported by the Roche<br />
Research Foundation <strong>and</strong> an EMBO fellowship.<br />
REFERENCES<br />
1. Adachi O, Kawai T, Takeda K, Matsumoto M, Tsutsui H,<br />
Sakagami M, Nakanishi K, Akira S. Targeted disruption of the<br />
MyD88 gene results in loss of IL-1- <strong>and</strong> IL- 18-mediated function.<br />
Immunity 9: 143–150, 1998.<br />
2. Agrimi U, Nonno R, Dell’Omo G, Di Bari MA, Conte M, Chiappini<br />
B, Esposito E, Di Guardo G, Windl O, Vaccari G, Lipp HP.<br />
Prion protein amino acid determinants of differential susceptibility<br />
<strong>and</strong> molecular feature of prion strains in mice <strong>and</strong> voles. PLoS<br />
Pathog 4: e1000113, 2008.<br />
3. Aguzzi A. Between cows <strong>and</strong> monkeys. Nature 381: 734, 1996.<br />
4. Aguzzi A. Neuro-immune connection in spread of prions in the<br />
body? Lancet 349: 742–743, 1997.<br />
5. Aguzzi A. Prion biology: the quest for the test. Nat Methods 4:<br />
614–616, 2007.<br />
6. Aguzzi A. Prion diseases, blood <strong>and</strong> the immune system: concerns<br />
<strong>and</strong> reality. Haematologica 85: 3–10, 2000.<br />
7. Aguzzi A. <strong>Prions</strong> <strong>and</strong> the immune system: a journey through gut,<br />
spleen, <strong>and</strong> nerves. Adv Immunol 81: 123–171, 2003.<br />
8. Aguzzi A. Underst<strong>and</strong>ing the diversity of prions. Nat Cell Biol 6:<br />
290–292, 2004.<br />
9. Aguzzi A. Unraveling prion strains with cell biology <strong>and</strong> organic<br />
chemistry. Proc Natl Acad Sci USA 105: 11–12, 2008.<br />
10. Aguzzi A, Baumann F, Bremer J. The Prion’s elusive reason for<br />
being. Annu Rev Neurosci 31: 439–477, 2008.<br />
11. Aguzzi A, Br<strong>and</strong>ner S, Fischer MB, Furukawa H, Glatzel M,<br />
Hawkins C, Heppner FL, Montrasio F, Navarro B, Parizek P,<br />
Pekarik V, Prinz M, Raeber AJ, Rockl C, Klein MA. Spongiform<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
encephalopathies: insights from transgenic models. Adv Virus Res<br />
56: 313–352, 2001.<br />
12. Aguzzi A, Haass C. Games played by rogue proteins in prion<br />
disorders <strong>and</strong> Alzheimer’s disease. Science 302: 814–818, 2003.<br />
13. Aguzzi A, Hegyi I, Peltola M, Glatzel M. Rapport des activitées 1996–<br />
1999. Hôpital universitaire de Zurich. Département de pathologie. Institut<br />
de neuropathologie. Centre nationale de référence pour les prionoses<br />
(NRPE): http://www.neuropathologie.usz.ch/documents/HealthProfes<br />
sionals/NationalesReferenzzentrumfuerPrionenerkrankungen/nrpe.pdf.<br />
14. Aguzzi A, Heikenwalder M. Pathogenesis of prion diseases: current<br />
status <strong>and</strong> future outlook. Nat Rev Microbiol 4: 765–775, 2006.<br />
15. Aguzzi A, Heikenwalder M. <strong>Prions</strong>, cytokines, <strong>and</strong> chemokines: a<br />
meeting in lymphoid organs. Immunity 22: 145–154, 2005.<br />
16. Aguzzi A, Heikenwalder M, Polymenidou M. Insights into<br />
prion strains <strong>and</strong> neurotoxicity. Nat Rev Mol Cell Biol 8: 552–<br />
561, 2007.<br />
17. Aguzzi A, Heppner FL, Heikenwalder M, Prinz M, Mertz K,<br />
Seeger H, Glatzel M. Immune system <strong>and</strong> peripheral nerves in<br />
propagation of prions to CNS. Br Med Bull 66: 141–159, 2003.<br />
18. Aguzzi A, Klein MA, Montrasio F, Pekarik V, Br<strong>and</strong>ner S,<br />
Furukawa H, Kaser P, Rockl C, Glatzel M. <strong>Prions</strong>: pathogenesis<br />
<strong>and</strong> reverse genetics. Ann NY Acad Sci 920: 140–157, 2000.<br />
19. Aguzzi A, Polymenidou M. Mammalian prion biology: one century<br />
of evolving concepts. Cell 116: 313–327, 2004.<br />
20. Aguzzi A, Sigurdson CJ. Antiprion immunotherapy: to suppress<br />
or to stimulate? Nat Rev Immunol 4: 725–736, 2004.<br />
21. Aguzzi A, Weissmann C. Prion research: the next frontiers. Nature<br />
389: 795–798, 1997.<br />
22. Aguzzi A, Weissmann C. Spongiform encephalopathies: a suspicious<br />
signature. Nature 383: 666–667, 1996.<br />
23. Alper T, Cramp WA, Haig DA, Clarke MC. Does the agent of<br />
scrapie replicate without nucleic acid? Nature 214: 764–766, 1967.<br />
24. Alper T, Haig DA, Clarke MC. The exceptionally small size of the<br />
scrapie agent. Biochem Biophys Res Commun 22: 278–284, 1966.<br />
25. Alper T, Haig DA, Clarke MC. The scrapie agent: evidence<br />
against its dependence for replication on intrinsic nucleic acid.<br />
J Gen Virol 41: 503–516, 1978.<br />
26. Anderson RGW. Caveolae: where incoming <strong>and</strong> outgoing messengers<br />
meet. Proc Natl Acad Sci USA 90: 10909–10913, 1993.<br />
27. Anderson RM, Donnelly CA, Ferguson NM, Woolhouse ME,<br />
Watt CJ, Udy HJ, MaWhinney S, Dunstan SP, Southwood TR,<br />
Wilesmith JW, Ryan JB, Hoinville LJ, Hillerton JE, Austin<br />
AR, Wells GA. Transmission dynamics <strong>and</strong> epidemiology of BSE<br />
in British cattle. Nature 382: 779–788, 1996.<br />
28. Andrews NJ, Farrington CP, Ward HJ, Cousens SN, Smith PG,<br />
Molesworth AM, Knight RS, Ironside JW, Will RG. Deaths from<br />
variant Creutzfeldt-Jakob disease in the UK. Lancet 361: 751–752,<br />
2003.<br />
29. Angers RC, Browning SR, Seward TS, Sigurdson CJ, Miller<br />
MW, Hoover EA, Telling GC. <strong>Prions</strong> in skeletal muscles of deer<br />
with chronic wasting disease. Science 311: 1117, 2006.<br />
30. Atarashi R, Moore RA, Sim VL, Hughson AG, Dorward DW,<br />
Onwubiko HA, Priola SA, Caughey B. Ultrasensitive detection of<br />
scrapie prion protein using seeded conversion of recombinant<br />
prion protein. Nat Methods 4: 645–650, 2007.<br />
31. Aucouturier P, Geissmann F, Damotte D, Saborio GP, Meeker<br />
HC, Kascsak R, Carp RI, Wisniewski T. Infected splenic dendritic<br />
cells are sufficient for prion transmission to the CNS in<br />
mouse scrapie. J Clin Invest 108: 703–708, 2001.<br />
32. Auluck PK, Chan HY, Trojanowski JQ, Lee VM, Bonini NM.<br />
Chaperone suppression of alpha-synuclein toxicity in a Drosophila<br />
model for Parkinson’s disease. Science 295: 865–868, 2002.<br />
33. Bacot SM, Lenz P, Frazier-Jessen MR, Feldman GM. Activation<br />
by prion peptide PrP106-126 induces a NF-kappaB-driven<br />
proinflammatory response in human monocyte-derived dendritic<br />
cells. J Leukoc Biol 74: 118–125, 2003.<br />
34. Baker HF, Ridley RM, Duchen LW, Crow TJ, Bruton CJ.<br />
Evidence for the experimental transmission of cerebral beta-amyloidosis<br />
to primates. Int J Exp Pathol 74: 441–454, 1993.<br />
35. Baker HF, Ridley RM, Duchen LW, Crow TJ, Bruton CJ.<br />
Induction of beta (A4)-amyloid in primates by injection of Alzheimer’s<br />
disease brain homogenate. Comparison with transmission of<br />
spongiform encephalopathy. Mol Neurobiol 8: 25–39, 1994.
36. Banks WA, Niehoff ML, Adessi C, Soto C. Passage of murine<br />
scrapie prion protein across the mouse vascular blood-brain barrier.<br />
Biochem Biophys Res Commun 318: 125–130, 2004.<br />
37. Bartz JC, Dejoia C, Tucker T, Kincaid AE, Bessen RA. Extraneural<br />
prion neuroinvasion without lymphoreticular system infection.<br />
J Virol 79: 11858–11863, 2005.<br />
38. Bartz JC, Kincaid AE, Bessen RA. Rapid prion neuroinvasion<br />
following tongue infection. J Virol 77: 583–591, 2003.<br />
39. Basler K, Oesch B, Scott M, Westaway D, Walchli M, Groth<br />
DF, McKinley MP, Prusiner SB, Weissmann C. Scrapie <strong>and</strong><br />
cellular PrP isoforms are encoded by the same chromosomal gene.<br />
Cell 46: 417–428, 1986.<br />
40. Baumann F, Tolnay M, Brabeck C, Pahnke J, Kloz U, Niemann<br />
HH, Heikenwalder M, Rulicke T, Burkle A, Aguzzi A. Lethal<br />
recessive myelin toxicity of prion protein lacking its central domain.<br />
EMBO J 26: 538–547, 2007.<br />
41. Beekes M, McBride PA, Baldauf E. Cerebral targeting indicates<br />
vagal spread of infection in hamsters fed with scrapie. J Gen Virol<br />
79: 601–607, 1998.<br />
42. Behrens A, Aguzzi A. Small is not beautiful: antagonizing functions<br />
for the prion protein PrP(C) <strong>and</strong> its homologue Dpl. Trends<br />
Neurosci 25: 150–154, 2002.<br />
43. Behrens A, Br<strong>and</strong>ner S, Genoud N, Aguzzi A. Normal neurogenesis<br />
<strong>and</strong> scrapie pathogenesis in neural grafts lacking the prion<br />
protein homologue Doppel. EMBO Rep 2: 347–352, 2001.<br />
44. Behrens A, Genoud N, Naumann H, Rulicke T, Janett F, Heppner<br />
FL, Ledermann B, Aguzzi A. Absence of the prion protein<br />
homologue Doppel causes male sterility. EMBO J 21: 3652–3658,<br />
2002.<br />
45. Bendheim PE, Barry RA, DeArmond SJ, Stites DP, Prusiner<br />
SB. Antibodies to a scrapie prion protein. Nature 310: 418–421,<br />
1984.<br />
46. Benestad SL, Sarradin P, Thu B, Schonheit J, Tranulis MA,<br />
Bratberg B. Cases of scrapie with unusual features in Norway <strong>and</strong><br />
designation of a new type, Nor98. Vet Rec 153: 202–208, 2003.<br />
47. Bennhold H. Eine specifische Amyloidfärbung mit Kongorot.<br />
Münchener Med Wochenschrift 44: 1537, 1922.<br />
48. Beringue V, Demoy M, Lasmezas CI, Gouritin B, Weingarten<br />
C, Deslys JP, Andreux JP, Couvreur P, Dormont D. Role of<br />
spleen macrophages in the clearance of scrapie agent early in<br />
pathogenesis. J Pathol 190: 495–502, 2000.<br />
49. Beringue V, Mallinson G, Kaisar M, Tayebi M, Sattar Z, Jackson<br />
G, Anstee D, Collinge J, Hawke S. Regional heterogeneity of<br />
cellular prion protein isoforms in the mouse brain. Brain 126:<br />
2065–2073, 2003.<br />
50. Bernoulli C, Siegfried J, Baumgartner G, Regli F, Rabinowicz<br />
T, Gajdusek DC, Gibbs CJ. Danger of accidental person-to-person<br />
transmission of Creutzfeldt-Jakob disease by surgery. Lancet 1:<br />
478–479, 1977.<br />
51. Bessen RA, Marsh RF. Distinct PrP properties suggest the molecular<br />
basis of strain variation in transmissible mink encephalopathy.<br />
J Virol 68: 7859–7868, 1994.<br />
52. Betmouni S, Perry VH, Gordon JL. Evidence for an early inflammatory<br />
response in the central nervous system of mice with<br />
scrapie. Neuroscience 74: 1–5, 1996.<br />
53. Blättler T, Br<strong>and</strong>ner S, Raeber AJ, Klein MA, Voigtländer T,<br />
Weissmann C, Aguzzi A. PrP-expressing tissue required for transfer<br />
of scrapie infectivity from spleen to brain. Nature 389: 69–73,<br />
1997.<br />
54. Blum B, Bakalara N, Simpson L. A model for RNA editing in<br />
kinetoplastid mitochondria: “guide” RNA molecules transcribed<br />
from maxicircle DNA provide the edited information. Cell 60: 189–<br />
198, 1990.<br />
55. Bolton DC, McKinley MP, Prusiner SB. Identification of a protein<br />
that purifies with the scrapie prion. Science 218: 1309–1311,<br />
1982.<br />
56. Bonizzi G, Bebien M, Otero DC, Johnson-Vroom KE, Cao Y,<br />
Vu D, Jegga AG, Aronow BJ, Ghosh G, Rickert RC, Karin M.<br />
Activation of IKKalpha target genes depends on recognition of<br />
specific kappaB binding sites by RelB:p52 dimers. EMBO J 23:<br />
4202–4210, 2004.<br />
57. Bons N, Mestre-Frances N, Belli P, Cathala F, Gajdusek DC,<br />
Brown P. Natural <strong>and</strong> experimental oral infection of nonhuman<br />
AGGREGATION AND INFECTIOUS DISEASE 1141<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
primates by bovine spongiform encephalopathy agents. Proc Natl<br />
Acad Sci USA 96: 4046–4051, 1999.<br />
58. Borchelt DR, Scott M, Taraboulos A, Stahl N, Prusiner SB.<br />
Scrapie <strong>and</strong> cellular prion proteins differ in their kinetics of synthesis<br />
<strong>and</strong> topology in cultured cells. J Cell Biol 110: 743–752, 1990.<br />
59. Borchelt DR, Taraboulos A, Prusiner SB. Evidence for synthesis<br />
of scrapie prion proteins in the endocytic pathway. J Biol Chem<br />
267: 16188–16199, 1992.<br />
60. Bounhar Y, Zhang Y, Goodyer CG, LeBlanc A. Prion protein<br />
protects human neurons against Bax-mediated apoptosis. J Biol<br />
Chem 276: 39145–39149, 2001.<br />
61. Bourteele S, Oesterle K, Weinzierl AO, Paxian S, Riemann M,<br />
Schmid RM, Planz O. Alteration of NF-kappaB activity leads to<br />
mitochondrial apoptosis after infection with pathological prion<br />
protein. Cell Microbiol 9: 2202–2217, 2007.<br />
62. Brachmann A, Baxa U, Wickner RB. Prion generation in vitro:<br />
amyloid of Ure2p is infectious. EMBO J 24: 3082–3092, 2005.<br />
63. Br<strong>and</strong>ner S, Isenmann S, Kuhne G, Aguzzi A. Identification of<br />
the end stage of scrapie using infected neural grafts. Brain Pathol<br />
8: 19–27, 1998.<br />
64. Br<strong>and</strong>ner S, Isenmann S, Raeber A, Fischer M, Sailer A,<br />
Kobayashi Y, Marino S, Weissmann C, Aguzzi A. Normal host<br />
prion protein necessary for scrapie-induced neurotoxicity. Nature<br />
379: 339–343, 1996.<br />
65. Br<strong>and</strong>ner S, Raeber A, Sailer A, Blattler T, Fischer M, Weissmann<br />
C, Aguzzi A. Normal host prion protein (PrPC) is required<br />
for scrapie spread within the central nervous system. Proc Natl<br />
Acad Sci USA 93: 13148–13151, 1996.<br />
66. Britton WJ, Lockwood DN. Leprosy. Lancet 363: 1209–1219,<br />
2004.<br />
67. Brown DR, Qin K, Herms JW, Madlung A, Manson J, Strome<br />
R, Fraser PE, Kruck T, von Bohlen A, Schulz-Schaeffer W,<br />
Giese A, Westaway D, Kretzschmar H. The cellular prion protein<br />
binds copper in vivo. Nature 390: 684–687, 1997.<br />
68. Brown DR, Schulz-Schaeffer WJ, Schmidt B, Kretzschmar HA.<br />
Prion protein-deficient cells show altered response to oxidative<br />
stress due to decreased SOD-1 activity. Exp Neurol 146: 104–112,<br />
1997.<br />
69. Brown DR, Wong BS, Hafiz F, Clive C, Haswell SJ, Jones IM.<br />
Normal prion protein has an activity like that of superoxide dismutase.<br />
Biochem J 344: 1–5, 1999.<br />
70. Brown KL, Stewart K, Ritchie DL, Mabbott NA, Williams A,<br />
Fraser H, Morrison WI, Bruce ME. Scrapie replication in lymphoid<br />
tissues depends on prion protein-expressing follicular dendritic<br />
cells. Nat Med 5: 1308–1312, 1999.<br />
71. Brown P, Cathala F, Raubertas RF, Gajdusek DC, Castaigne<br />
P. The epidemiology of Creutzfeldt-Jakob disease: conclusion of a<br />
15-year investigation in France <strong>and</strong> review of the world literature.<br />
Neurology 37: 895–904, 1987.<br />
72. Brown P, Cervenakova L, Goldfarb LG, McCombie WR,<br />
Rubenstein R, Will RG, Pocchiari M, Martinez Lage JF, Scalici<br />
C, Masullo C. Iatrogenic Creutzfeldt-Jakob disease: an example of<br />
the interplay between ancient genes <strong>and</strong> modern medicine. Neurology<br />
44: 291–293, 1994.<br />
73. Brown P, Gajdusek DC, Gibbs CJ Jr, Asher DM. Potential<br />
epidemic of Creutzfeldt-Jakob disease from human growth hormone<br />
therapy. N Engl J Med 313: 728–731, 1985.<br />
74. Brown P, Gibbs CJ Jr, Rodgers-Johnson P, Asher DM, Sulima<br />
MP, Bacote A, Goldfarb LG, Gajdusek DC. Human spongiform<br />
encephalopathy: the National Institutes of Health series of 300<br />
cases of experimentally transmitted disease. Ann Neurol 35: 513–<br />
529, 1994.<br />
75. Bruce M. Transmissions of BSE, scrapie <strong>and</strong> related diseases to<br />
mice. In: IXth International Congress of Virology Glasgow, Scotl<strong>and</strong>,<br />
1993, p.93.<br />
76. Bruce ME. Scrapie strain variation <strong>and</strong> mutation. Br Med Bull 49:<br />
822–838, 1993.<br />
77. Bruce ME, Boyle A, Cousens S, McConnell I, Foster J,<br />
Goldmann W, Fraser H. Strain characterization of natural<br />
sheep scrapie <strong>and</strong> comparison with BSE. J Gen Virol 83: 695–<br />
704, 2002.<br />
78. Bruce ME, Dickinson AG. Biological evidence that scrapie agent<br />
has an independent genome. J Gen Virol 68: 79–89, 1987.
1142 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
79. Bruce ME, McBride PA, Farquhar CF. Precise targeting of the<br />
pathology of the sialoglycoprotein, PrP, vacuolar degeneration in<br />
mouse scrapie. Neurosci Lett 102: 1–6, 1989.<br />
80. Bruce ME, Will RG, Ironside JW, McConnell I, Drummond D,<br />
Suttie A, McCardle L, Chree A, Hope J, Birkett C, Cousens S,<br />
Fraser H, Bostock CJ. Transmissions to mice indicate that “new<br />
variant” CJD is caused by the BSE agent. Nature 389: 498–501,<br />
1997.<br />
81. Bucciantini M, Giannoni E, Chiti F, Baroni F, Formigli L,<br />
Zurdo J, Taddei N, Ramponi G, Dobson CM, Stefani M. Inherent<br />
toxicity of aggregates implies a common mechanism for protein<br />
misfolding diseases. Nature 416: 507–511, 2002.<br />
82. Buchanan CR, Preece MA, Milner RD. Mortality, neoplasia, <strong>and</strong><br />
Creutzfeldt-Jakob disease in patients treated with human pituitary<br />
growth hormone in the United Kingdom. BMJ 302: 824–828, 1991.<br />
83. Büeler H, Raeber A, Sailer A, Fischer M, Aguzzi A, Weissmann<br />
C. High prion <strong>and</strong> PrPSc levels but delayed onset of disease<br />
in scrapie-inoculated mice heterozygous for a disrupted PrP gene.<br />
Mol Med 1: 19–30, 1994.<br />
84. Büeler HR, Aguzzi A, Sailer A, Greiner RA, Autenried P,<br />
Aguet M, Weissmann C. Mice devoid of PrP are resistant to<br />
scrapie. Cell 73: 1339–1347, 1993.<br />
85. Büeler HR, Fischer M, Lang Y, Bluethmann H, Lipp HP, De-<br />
Armond SJ, Prusiner SB, Aguet M, Weissmann C. Normal<br />
development <strong>and</strong> behaviour of mice lacking the neuronal cellsurface<br />
PrP protein. Nature 356: 577–582, 1992.<br />
86. Burwinkel M, Schwarz A, Riemer C, Schultz J, Van L<strong>and</strong>eghem<br />
F, Baier M. Rapid disease development in scrapie-infected<br />
mice deficient for CD40 lig<strong>and</strong>. EMBO Rep 5:527–531, 2004.<br />
87. Buschmann A, Biacabe AG, Ziegler U, Bencsik A, Madec JY,<br />
Erhardt G, Luhken G, Baron T, Groschup MH. Atypical scrapie<br />
cases in Germany <strong>and</strong> France are identified by discrepant reaction<br />
patterns in BSE rapid tests. J Virol Methods 117: 27–36, 2004.<br />
88. Calzolai L, Lysek DA, Perez DR, Guntert P, Wüthrich K. Prion<br />
protein NMR structures of chickens, turtles, <strong>and</strong> frogs. Proc Natl<br />
Acad Sci USA 102: 651–655, 2005.<br />
89. Canello T, Engelstein R, Moshel O, Xanthopoulos K, Juanes<br />
ME, Langeveld J, Sklaviadis T, Gasset M, Gabizon R. Methionine<br />
sulfoxides on PrPSc: a prion-specific covalent signature. Biochemistry<br />
47: 8866–8873, 2008.<br />
90. Carp RI. Transmission of scrapie by oral route: effect of gingival<br />
scarification. Lancet 1: 170–171, 1982.<br />
91. Cashman NR, Loertscher R, Nalbantoglu J, Shaw I, Kascsak<br />
RJ, Bolton DC, Bendheim PE. Cellular isoform of the scrapie<br />
agent protein participates in lymphocyte activation. Cell 61: 185–<br />
192, 1990.<br />
92. Castilla J, Gonzalez-Romero D, Saa P, Morales R, De Castro<br />
J, Soto C. Crossing the species barrier by PrP(Sc) replication in<br />
vitro generates unique infectious prions. Cell 134: 757–768, 2008.<br />
93. Castilla J, Morales R, Saa P, Barria M, Gambetti P, Soto C.<br />
Cell-free propagation of prion strains. EMBO J 27: 2557–2565, 2008.<br />
94. Castilla J, Saa P, Hetz C, Soto C. In vitro generation of infectious<br />
scrapie prions. Cell 121: 195–206, 2005.<br />
95. Castilla J, Saa P, Soto C. Detection of prions in blood. Nat Med<br />
11: 982–985, 2005.<br />
96. Caughey B, Baron GS, Chesebro B, Jeffrey M. Getting a grip on<br />
prions: oligomers, amyloids, <strong>and</strong> pathological membrane interactions.<br />
Annu Rev Biochem 78: 177–204, 2009.<br />
97. Caughey B, Horiuchi M, Demaimay R, Raymond GJ. Assays of<br />
protease-resistant prion protein <strong>and</strong> its formation. Methods Enzymol<br />
309: 122–133, 1999.<br />
98. Caughey B, Race RE. Potent inhibition of scrapie-associated PrP<br />
accumulation by congo red. J Neurochem 59: 768–771, 1992.<br />
99. Caughey B, Raymond GJ. The scrapie-associated form of PrP is<br />
made from a cell surface precursor that is both protease- <strong>and</strong><br />
phospholipase-sensitive. J Biol Chem 266: 18217–18223, 1991.<br />
100. Caughey B, Raymond GJ. Sulfated polyanion inhibition of<br />
scrapie-associated PrP accumulation in cultured cells. J Virol 67:<br />
643–650, 1993.<br />
101. Caughey B, Raymond GJ, Bessen RA. Strain-dependent differences<br />
in beta-sheet conformations of abnormal prion protein.<br />
J Biol Chem 273: 32230–32235, 1998.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
102. Caughey B, Raymond LD, Raymond GJ, Maxson L, Silveira J,<br />
Baron GS. Inhibition of protease-resistant prion protein accumulation<br />
in vitro by curcumin. J Virol 77: 5499–5502, 2003.<br />
103. Caughey BW, Dong A, Bhat KS, Ernst D, Hayes SF, Caughey<br />
WS. Secondary structure analysis of the scrapie-associated protein<br />
PrP 27–30 in water by infrared spectroscopy. Biochemistry 30: 7672–<br />
7680, 1991.<br />
104. Caughey WS, Raymond LD, Horiuchi M, Caughey B. Inhibition<br />
of protease-resistant prion protein formation by porphyrins <strong>and</strong><br />
phthalocyanines. Proc Natl Acad Sci USA 95: 12117–12122, 1998.<br />
105. Ch<strong>and</strong>ler RL. Encephalopathy in mice produced by inoculation<br />
with scrapie brain material. Lancet 1: 1378–1379, 1961.<br />
106. Chazot G, Broussolle E, Lapras C, Blättler T, Aguzzi A, Kopp<br />
N. New variant of Creutzfeldt-Jakob disease in a 26-year-old French<br />
man. Lancet 347: 1181, 1996.<br />
107. Chesebro B, Race R, Wehrly K, Nishio J, Bloom M, Lechner D,<br />
Bergstrom S, Robbins K, Mayer L, Keith JM. Identification of<br />
scrapie prion protein-specific mRNA in scrapie-infected <strong>and</strong> uninfected<br />
brain. Nature 315: 331–333, 1985.<br />
108. Chesebro B, Trifilo M, Race R, Meade-White K, Teng C,<br />
LaCasse R, Raymond L, Favara C, Baron G, Priola S, Caughey<br />
B, Masliah E, Oldstone M. Anchorless prion protein results in<br />
infectious amyloid disease without clinical scrapie. Science 308:<br />
1435–1439, 2005.<br />
109. Chiesa R, Piccardo P, Ghetti B, Harris DA. Neurological illness<br />
in transgenic mice expressing a prion protein with an insertional<br />
mutation. Neuron 21: 1339–1351, 1998.<br />
110. Chiti F, Dobson CM. <strong>Protein</strong> misfolding, functional amyloid, <strong>and</strong><br />
human disease. Annu Rev Biochem 75: 333–366, 2006.<br />
111. Clarke MC, Kimberlin RH. Pathogenesis of mouse scrapie: distribution<br />
of agent in the pulp <strong>and</strong> stroma of infected spleens. Vet<br />
Microbiol 9: 215–225, 1984.<br />
112. Clarke MC, Millson GC. Infection of a cell line of mouse L<br />
fibroblasts with scrapie agent. Nature 261: 144–145, 1976.<br />
113. Clouscard C, Beaudry P, Elsen JM, Milan D, Dussaucy M,<br />
Bounneau C, Schelcher F, Chatelain J, Launay JM, Laplanche<br />
JL. Different allelic effects of the codons 136 <strong>and</strong> 171 of the prion<br />
protein gene in sheep with natural scrapie. J Gen Virol 76: 2097–<br />
2101, 1995.<br />
114. Cohen AS, Shirahama T, Skinner M. Electron microscopy of<br />
amyloid. In: Electron Microscopy of <strong>Protein</strong>s, edited by Harris JR.<br />
New York: Academic, 1982, p. 165–206.<br />
115. Cole S, Kimberlin RH. Pathogenesis of mouse scrapie: dynamics<br />
of vacuolation in brain <strong>and</strong> spinal cord after intraperitoneal infection.<br />
Neuropathol Appl Neurobiol 11: 213–227, 1985.<br />
116. Collinge J. Molecular neurology of prion disease. J Neurol Neurosurg<br />
Psychiatry 76: 906–919, 2005.<br />
117. Collinge J, Palmer MS, Dryden AJ. Genetic predisposition to<br />
iatrogenic Creutzfeldt-Jakob disease. Lancet 337: 1441–1442, 1991.<br />
118. Collinge J, Sidle KC, Meads J, Ironside J, Hill AF. Molecular<br />
analysis of prion strain variation <strong>and</strong> the aetiology of “new variant”<br />
CJD. Nature 383: 685–690, 1996.<br />
119. Collinge J, Whitfield J, McKintosh E, Beck J, Mead S, Thomas<br />
DJ, Alpers MP. Kuru in the 21st century–an acquired human prion<br />
disease with very long incubation periods. Lancet 367: 2068–2074,<br />
2006.<br />
120. Collinge J, Whittington MA, Sidle KC, Smith CJ, Palmer MS,<br />
Clarke AR, Jefferys JG. Prion protein is necessary for normal<br />
synaptic function. Nature 370: 295–297, 1994.<br />
121. Collins SJ, Lewis V, Brazier M, Hill AF, Fletcher A, Masters<br />
CL. Quinacrine does not prolong survival in a murine Creutzfeldt-<br />
Jakob disease model. Ann Neurol 52: 503–506, 2002.<br />
122. Colombo G, Meli M, Morra G, Gabizon R, Gasset M. Methionine<br />
sulfoxides on prion protein Helix-3 switch on the alpha-fold<br />
destabilization required for conversion. PLoS ONE 4: e4296, 2009.<br />
123. Cooper E. Quinacrine in possible or probable CJD: it is blinded<br />
investigators, not patients, who must be in equipoise over treatment.<br />
BMJ 324: 239, 2002.<br />
124. Costa PP, Figueira AS, Bravo FR. Amyloid fibril protein related<br />
to prealbumin in familial amyloidotic polyneuropathy. Proc Natl<br />
Acad Sci USA 75: 4499–4503, 1978.<br />
125. Cousens SN, Harries Jones R, Knight R, Will RG, Smith PG,<br />
Matthews WB. Geographical distribution of cases of Creutzfeldt-
Jakob disease in Engl<strong>and</strong> <strong>and</strong> Wales 1970–84. J Neurol Neurosurg<br />
Psychiatry 53: 459–465, 1990.<br />
126. Cronier S, Gros N, Tattum MH, Jackson GS, Clarke AR,<br />
Collinge J, Wadsworth JD. Detection <strong>and</strong> characterization of<br />
proteinase K-sensitive disease-related prion protein with thermolysin.<br />
Biochem J 416: 297–305, 2008.<br />
127. Crowther DC, Kinghorn KJ, Mir<strong>and</strong>a E, Page R, Curry JA,<br />
Duthie FA, Gubb DC, Lomas DA. Intraneuronal Abeta, nonamyloid<br />
aggregates <strong>and</strong> neurodegeneration in a Drosophila model<br />
of Alzheimer’s disease. Neuroscience 132: 123–135, 2005.<br />
128. Cuille J, Chelle PL. Experimental transmission of trembling to<br />
the goat. C R Seances Acad Sci 208: 1058–1160, 1939.<br />
129. Davanipour Z, Goodman L, Alter M, Sobel E, Asher D, Gajdusek<br />
DC. Possible modes of transmission of Creutzfeldt-Jakob<br />
disease. N Engl J Med 311: 1582–1583, 1984.<br />
130. Dawson M, Wells GA, Parker BN. Preliminary evidence of the<br />
experimental transmissibility of bovine spongiform encephalopathy<br />
to cattle. Vet Rec 126: 112–113, 1990.<br />
131. Dawson M, Wells GA, Parker BN, Scott AC. Primary parenteral<br />
transmission of bovine spongiform encephalopathy to the pig. Vet<br />
Rec 127: 338, 1990.<br />
132. DeArmond SJ, McKinley MP, Barry RA, Braunfeld MB, Mc-<br />
Colloch JR, Prusiner SB. Identification of prion amyloid filaments<br />
in scrapie-infected brain. Cell 41: 221–235, 1985.<br />
133. DeArmond SJ, Qiu Y, Sanchez H, Spilman PR, Ninchak-Casey<br />
A, Alonso D, Daggett V. PrP C glycoform heterogeneity as a function<br />
of brain region: implications for selective targeting of neurons<br />
by prion strains. J Neuropathol Exp Neurol 58: 1000–1009, 1999.<br />
134. Deleault NR, Geoghegan JC, Nishina K, Kascsak R, Williamson<br />
RA, Supattapone S. Protease-resistant prion protein amplification<br />
reconstituted with partially purified substrates <strong>and</strong> synthetic<br />
polyanions. J Biol Chem 280: 26873–26879, 2005.<br />
135. Deleault NR, Harris BT, Rees JR, Supattapone S. Formation of<br />
native prions from minimal components in vitro. Proc Natl Acad<br />
Sci USA 104: 9741–9746, 2007.<br />
136. Dickinson AG, Fraser H. An assessment of the genetics of scrapie<br />
in sheep <strong>and</strong> mice. In: Slow Transmissible <strong>Diseases</strong> of the Nervous<br />
System, edited by Prusiner SB, Hadlow WJ. New York: Academic,<br />
1979, p. 367–386.<br />
137. Dickinson AG, Outram GW. Genetic aspects of unconventional<br />
virus infections: the basis of the virino hypothesis. Ciba Found<br />
Symp 135: 63–83, 1988.<br />
138. Divry P. Etude histochimique des plaques seniles. J Neurol Psychiatry<br />
27: 643, 1927.<br />
139. Dobson C. <strong>Protein</strong> folding <strong>and</strong> misfolding. Nature 426: 884–890,<br />
2003.<br />
140. Doh-Ura K, Iwaki T, Caughey B. Lysosomotropic agents <strong>and</strong><br />
cysteine protease inhibitors inhibit scrapie-associated prion protein<br />
accumulation. J Virol 74: 4894–4897, 2000.<br />
141. Drayton DL, Liao S, Mounzer RH, Ruddle NH. Lymphoid organ<br />
development: from ontogeny to neogenesis. Nat Immunol 7: 344–<br />
353, 2006.<br />
142. Drisaldi B, Stewart RS, Adles C, Stewart LR, Quaglio E,<br />
Biasini E, Fioriti L, Chiesa R, Harris DA. Mutant PrP is delayed<br />
in its exit from the endoplasmic reticulum, but neither wild-type<br />
nor mutant PrP undergoes retrotranslocation prior to proteasomal<br />
degradation. J Biol Chem 278: 21732–21743, 2003.<br />
143. Duffy P, Wolf J, Collins G, DeVoe AG, Streeten B, Cowen D.<br />
Possible person-to-person transmission of Creutzfeldt-Jakob disease.<br />
N Engl J Med 290: 692–693, 1974.<br />
144. Enari M, Flechsig E, Weissmann C. Scrapie prion protein accumulation<br />
by scrapie-infected neuroblastoma cells abrogated by<br />
exposure to a prion protein antibody. Proc Natl Acad Sci USA 98:<br />
9295–9299, 2001.<br />
145. Endres R, Alimzhanov MB, Plitz T, Futterer A, Kosco-Vilbois<br />
MH, Nedospasov SA, Rajewsky K, Pfeffer K. Mature follicular<br />
dendritic cell networks depend on expression of lymphotoxin beta<br />
receptor by radioresistant stromal cells <strong>and</strong> of lymphotoxin beta<br />
<strong>and</strong> tumor necrosis factor by B cells. J Exp Med 189: 159–168, 1999.<br />
146. Ernst JD, Trevejo-Nunez G, Banaiee N. Genomics <strong>and</strong> the<br />
evolution, pathogenesis, <strong>and</strong> diagnosis of tuberculosis. J Clin Invest<br />
117: 1738–1745, 2007.<br />
AGGREGATION AND INFECTIOUS DISEASE 1143<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
147. Everest SJ, Thorne L, Barnicle DA, Edwards JC, Elliott H,<br />
Jackman R, Hope J. Atypical prion protein in sheep brain collected<br />
during the British scrapie-surveillance programme. J Gen<br />
Virol 87: 471–477, 2006.<br />
148. Falsig J, Aguzzi A. The prion organotypic slice culture assay—<br />
POSCA. Nat Protoc 3: 555–562, 2008.<br />
149. Falsig J, Julius C, Margalith I, Schwarz P, Heppner FL,<br />
Aguzzi A. A versatile prion replication assay in organotypic brain<br />
slices. Nature Neurosci 11: 109–117, 2008.<br />
150. Felten SY, Felten DL, Bellinger DL, Carlson SL, Ackerman<br />
KD, Madden KS, Olschowka JA, Livnat S. Noradrenergic sympathetic<br />
innervation of lymphoid organs. Prog Allergy 43: 14–36,<br />
1988.<br />
151. Fevrier B, Vilette D, Archer F, Loew D, Faigle W, Vidal M,<br />
Laude H, Raposo G. Cells release prions in association with<br />
exosomes. Proc Natl Acad Sci USA 101: 9683–9688, 2004.<br />
152. Fioriti L, Dossena S, Stewart LR, Stewart RS, Harris DA,<br />
Forloni G, Chiesa R. Cytosolic prion protein (PrP) is not toxic in<br />
N2a cells <strong>and</strong> primary neurons expressing pathogenic PrP mutations.<br />
J Biol Chem 280: 11320–11328, 2005.<br />
153. Fischer M, Rülicke T, Raeber A, Sailer A, Moser M, Oesch B,<br />
Br<strong>and</strong>ner S, Aguzzi A, Weissmann C. Prion protein (PrP) with<br />
amino-proximal deletions restoring susceptibility of PrP knockout<br />
mice to scrapie. EMBO J 15: 1255–1264, 1996.<br />
153a.Flechsig E, Hegyi I, Enari M, Schwarz P, Collinge J, Weissmann<br />
C. Transmission of Scrapie by Steel-surface-bound <strong>Prions</strong>.<br />
Mol Med 7: 679–684, 2001.<br />
154. Flechsig E, Shmerling D, Hegyi I, Raeber AJ, Fischer M,<br />
Cozzio A, von Mering C, Aguzzi A, Weissmann C. Prion protein<br />
devoid of the octapeptide repeat region restores susceptibility to<br />
scrapie in PrP knockout mice. Neuron 27: 399–408, 2000.<br />
155. Forster R, Mattis AE, Kremmer E, Wolf E, Brem G, Lipp M. A<br />
putative chemokine receptor, BLR1, directs B cell migration to<br />
defined lymphoid organs <strong>and</strong> specific anatomic compartments of<br />
the spleen. Cell 87: 1037–1047., 1996.<br />
156. Foster JD, Parnham DW, Hunter N, Bruce M. Distribution of<br />
the prion protein in sheep terminally affected with BSE following<br />
experimental oral transmission. J Gen Virol 82: 2319–2326, 2001.<br />
157. Fournier JG, Escaig Haye F, Billette de Villemeur T, Robain<br />
O. Ultrastructural localization of cellular prion protein (PrP C )in<br />
synaptic boutons of normal hamster hippocampus. C R Acad Sci III<br />
318: 339–344, 1995.<br />
158. Fowler D, Koulov A, Balch W, Kelly J. Functional amyloid–from<br />
bacteria to humans. Trends Biochem Sci 32: 217–224, 2007.<br />
159. Fox KA, Jewell JE, Williams ES, Miller MW. Patterns of<br />
PrPCWD accumulation during the course of chronic wasting disease<br />
infection in orally inoculated mule deer (Odocoileus hemionus).<br />
J Gen Virol 87: 3451–3461, 2006.<br />
160. Fradkin JE, Schonberger LB, Mills JL, Gunn WJ, Piper JM,<br />
Wysowski DK, Thomson R, Durako S, Brown P. Creutzfeldt-<br />
Jakob disease in pituitary growth hormone recipients in the United<br />
States. JAMA 265: 880–884, 1991.<br />
161. Fraser H. Neuronal spread of scrapie agent <strong>and</strong> targeting of lesions<br />
within the retino-tectal pathway. Nature 295: 149–150, 1982.<br />
162. Fraser H, Dickinson AG. Pathogenesis of scrapie in the mouse:<br />
the role of the spleen. Nature 226: 462–463, 1970.<br />
163. Fraser H, Dickinson AG. Scrapie in mice. Agent-strain differences<br />
in the distribution <strong>and</strong> intensity of grey matter vacuolation.<br />
J Comp Pathol 83: 29–40, 1973.<br />
164. Fraser H, Dickinson AG. The sequential development of the brain<br />
lesion of scrapie in three strains of mice. J Comp Pathol 78:<br />
301–311, 1968.<br />
165. Fraser H, McConnell I, Wells GA, Dawson M. Transmission of<br />
bovine spongiform encephalopathy to mice. Vet Rec 123: 472, 1988.<br />
166. Frigg R, Klein MA, Hegyi I, Zinkernagel RM, Aguzzi A. Scrapie<br />
pathogenesis in subclinically infected B-cell-deficient mice. J Virol<br />
73: 9584–9588, 1999.<br />
167. Frost B, Jacks RL, Diamond MI. Propagation of tau misfolding<br />
from the outside to the inside of a cell. J Biol Chem 284: 12845–<br />
12852, 2009.<br />
168. Gabizon R, McKinley MP, Groth D, Prusiner SB. Immunoaffinity<br />
purification <strong>and</strong> neutralization of scrapie prion infectivity. Proc<br />
Natl Acad Sci USA 85: 6617–6621, 1988.
1144 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
169. Gabizon R, McKinley MP, Prusiner SB. Purified prion proteins<br />
<strong>and</strong> scrapie infectivity copartition into liposomes. Proc Natl Acad<br />
Sci USA 84: 4017–4021, 1987.<br />
170. Gabriel JM, Oesch B, Kretzschmar H, Scott M, Prusiner SB.<br />
Molecular cloning of a c<strong>and</strong>idate chicken prion protein. Proc Natl<br />
Acad Sci USA 89: 9097–9101, 1992.<br />
171. Gajdusek D, Zigas V. Clinical, pathological <strong>and</strong> epidemiological<br />
study of an acute progressive degenerative disease of the central<br />
nervous system among natives of the eastern higl<strong>and</strong>s of New<br />
Guinea. Am J Med 26: 442–469, 1959.<br />
172. Gajdusek DC. Unconventional viruses <strong>and</strong> the origin <strong>and</strong> disappearance<br />
of kuru. Science 197: 943–960, 1977.<br />
173. Gajdusek DC, Zigas V. Degenerative disease of the central nervous<br />
system in New Guinea: the endemic occurrence of “kuru” in<br />
the native population. N Engl J Med 257: 974–978, 1957.<br />
174. Gambetti P, Kong Q, Zou W, Parchi P, Chen SG. Sporadic <strong>and</strong><br />
familial CJD: classification <strong>and</strong> characterisation. Br Med Bull 66:<br />
213–239, 2003.<br />
175. Gambetti P, Parchi P, Petersen RB, Chen SG, Lugaresi E.<br />
Fatal familial insomnia <strong>and</strong> familial Creutzfeldt-Jakob disease: clinical,<br />
pathological <strong>and</strong> molecular features. Brain Pathol 5: 43–51,<br />
1995.<br />
176. Gasset M, Baldwin MA, Fletterick RJ, Prusiner SB. Perturbation<br />
of the secondary structure of the scrapie prion protein under<br />
conditions that alter infectivity. Proc Natl Acad Sci USA 90: 1–5,<br />
1993.<br />
177. Genoud N, Behrens A, Miele G, Robay D, Heppner FL,<br />
Freigang S, Aguzzi A. Disruption of Doppel prevents neurodegeneration<br />
in mice with extensive Prnp deletions. Proc Natl Acad<br />
Sci USA 101: 4198–4203, 2004.<br />
178. Genoud N, Ott D, Braun N, Prinz M, Schwarz P, Suter U,<br />
Trono D, Aguzzi A. Antiprion prophylaxis by gene transfer of a<br />
soluble prion antagonist. Am J Pathol 172: 1287–1296, 2008.<br />
179. Gerstmann J, Sträussler E, Scheinker I. über eine eigenartige<br />
hereditär-familiäre Erkrankung des Zentralnervensystems. Zugleich<br />
ein Beitrag zur Frage des vorzeitigen lokalen Alterns Z<br />
Neurol 154: 736–762, 1936.<br />
180. Ghani AC, Donnelly CA, Ferguson NM, Anderson RM. Assessment<br />
of the prevalence of vCJD through testing tonsils <strong>and</strong> appendices<br />
for abnormal prion protein. Proc Biol Sci 267: 23–29, 2000.<br />
181. Ghani AC, Ferguson NM, Donnelly CA, Hagenaars TJ, Anderson<br />
RM. Estimation of the number of people incubating variant<br />
CJD. Lancet 352: 1353–1354, 1998.<br />
182. Gibbons RA, Hunter GD. Nature of the scrapie agent. Nature 215:<br />
1041–1043, 1967.<br />
183. Glatzel M, Abela E, Maissen M, Aguzzi A. Extraneural pathologic<br />
prion protein in sporadic Creutzfeldt-Jakob disease. N Engl<br />
J Med 349: 1812–1820, 2003.<br />
184. Glatzel M, Aguzzi A. PrP(C) expression in the peripheral nervous<br />
system is a determinant of prion neuroinvasion. J Gen Virol 81:<br />
2813–2821, 2000.<br />
185. Glatzel M, Aguzzi A. The shifting biology of prions. Brain Res<br />
Brain Res Rev 36: 241–248, 2001.<br />
186. Glatzel M, Heppner FL, Albers KM, Aguzzi A. Sympathetic<br />
innervation of lymphoreticular organs is rate limiting for prion<br />
neuroinvasion. Neuron 31: 25–34, 2001.<br />
187. Glatzel M, Ott PM, Lindner T, Gebbers JO, Gmur A, Wuest W,<br />
Huber G, Moch H, Podvinec M, Stamm B, Aguzzi A. Human<br />
prion diseases: epidemiology <strong>and</strong> integrated risk assessment. Lancet<br />
Neurol 2: 757–763, 2003.<br />
188. Glaysher BR, Mabbott NA. Role of the draining lymph node in<br />
scrapie agent transmission from the skin. Immunol Lett 109: 64–71,<br />
2007.<br />
189. Glaysher BR, Mabbott NA. Role of the GALT in scrapie agent<br />
neuroinvasion from the intestine. J Immunol 178: 3757–3766, 2007.<br />
190. Glockshuber R, Hornemann S, Billeter M, Riek R, Wider G,<br />
Wuthrich K. Prion protein structural features indicate possible<br />
relations to signal peptidases. FEBS Lett 426: 291–296, 1998.<br />
191. Gommerman JL, Browning JL. Lymphotoxin/light, lymphoid microenvironments<br />
<strong>and</strong> autoimmune disease. Nat Rev Immunol 3:<br />
642–655, 2003.<br />
192. Gommerman JL, Mackay F, Donskoy E, Meier W, Martin P,<br />
Browning JL. Manipulation of lymphoid microenvironments in<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
nonhuman primates by an inhibitor of the lymphotoxin pathway.<br />
J Clin Invest 110: 1359–1369, 2002.<br />
193. Goni F, Prelli F, Schreiber F, Scholtzova H, Chung E, Kascsak<br />
R, Brown DR, Sigurdsson EM, Chabalgoity JA, Wisniewski T.<br />
High titers of mucosal <strong>and</strong> systemic anti-PrP antibodies abrogate<br />
oral prion infection in mucosal-vaccinated mice. Neuroscience 153:<br />
679–686, 2008.<br />
194. Gordon WS. Advances in veterinary research. Vet Res 58: 516–520,<br />
1946.<br />
195. Gorodinsky A, Harris DA. Glycolipid-anchored proteins in neuroblastoma<br />
cells form detergent-resistant complexes without<br />
caveolin. J Cell Biol 129: 619–627, 1995.<br />
196. Green KM, Castilla J, Seward TS, Napier DL, Jewell JE, Soto<br />
C, Telling GC. Accelerated high fidelity prion amplification within<br />
<strong>and</strong> across prion species barriers. PLoS Pathog 4: e1000139, 2008.<br />
197. Griffith JS. Self-replication <strong>and</strong> scrapie. Nature 215: 1043–1044,<br />
1967.<br />
198. Haik S, Faucheux BA, Sazdovitch V, Privat N, Kemeny JL,<br />
Perret-Liaudet A, Hauw JJ. The sympathetic nervous system is<br />
involved in variant Creutzfeldt-Jakob disease. Nat Med 9: 1121–<br />
1122, 2003.<br />
199. Hainfellner JA, Brantner Inthaler S, Cervenakova L, Brown<br />
P, Kitamoto T, Tateishi J, Diringer H, Liberski PP, Regele H,<br />
Feucht M. The original Gerstmann-Straussler-Scheinker family of<br />
Austria: divergent clinicopathological phenotypes but constant PrP<br />
genotype. Brain Pathol 5: 201–211, 1995.<br />
200. Hamir AN, Kunkle RA, Miller JM, Hall SM. Abnormal prion<br />
protein in ectopic lymphoid tissue in a kidney of an asymptomatic<br />
white-tailed deer experimentally inoculated with the agent of<br />
chronic wasting disease. Vet Pathol 43: 367–369, 2006.<br />
201. Haraguchi T, Fisher S, Olofsson S, Endo T, Groth D, Tarentino<br />
A, Borchelt DR, Teplow D, Hood L, Burlingame A.<br />
Asparagine-linked glycosylation of the scrapie <strong>and</strong> cellular prion<br />
proteins. Arch Biochem Biophys 274: 1–13, 1989.<br />
202. Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease:<br />
progress <strong>and</strong> problems on the road to therapeutics. Science<br />
297: 353–356, 2002.<br />
203. Healy DL, Evans J. Creutzfeldt-Jakob disease after pituitary gonadotrophins.<br />
BMJ 307: 517–518, 1993.<br />
204. Hegde RS, Mastrianni JA, Scott MR, DeFea KA, Tremblay P,<br />
Torchia M, DeArmond SJ, Prusiner SB, Lingappa VR. A transmembrane<br />
form of the prion protein in neurodegenerative disease.<br />
Science 279: 827–834, 1998.<br />
205. Hegde RS, Tremblay P, Groth D, DeArmond SJ, Prusiner SB,<br />
Lingappa VR. Transmissible <strong>and</strong> genetic prion diseases share a<br />
common pathway of neurodegeneration Nature 402: 822–826, 1999.<br />
206. Heikenwalder M, Federau C, von Boehmer L, Schwarz P,<br />
Wagner M, Zeller N, Haybaeck J, Prinz M, Becher B, Aguzzi A.<br />
Germinal center B cells are dispensable in prion transport <strong>and</strong><br />
neuroinvasion. J Neuroimmunol 192: 113–123, 2007.<br />
207. Heikenwalder M, Julius C, Aguzzi A. <strong>Prions</strong> <strong>and</strong> peripheral<br />
nerves: a deadly rendezvous. J Neurosci Res 85: 2714–2725, 2007.<br />
208. Heikenwalder M, Kurrer MO, Margalith I, Kranich J, Zeller N,<br />
Haybaeck J, Polymenidou M, Matter M, Bremer J, Jackson<br />
WS, Lindquist S, Sigurdson CJ, Aguzzi A. Lymphotoxin-dependent<br />
prion replication in inflammatory stromal cells of granulomas.<br />
Immunity 29: 998–1008, 2008.<br />
209. Heikenwalder M, Polymenidou M, Junt T, Sigurdson C, Wagner<br />
H, Akira S, Zinkernagel R, Aguzzi A. Lymphoid follicle<br />
destruction <strong>and</strong> immunosuppression after repeated CpG oligodeoxynucleotide<br />
administration. Nat Med 10: 187–192, 2004.<br />
210. Heikenwalder M, Zeller N, Seeger H, Prinz M, Klohn PC,<br />
Schwarz P, Ruddle NH, Weissmann C, Aguzzi A. Chronic lymphocytic<br />
inflammation specifies the organ tropism of prions. Science<br />
307: 1107–1110, 2005.<br />
211. Hemmi H, Takeuchi O, Kawai T, Kaisho T, Sato S, Sanjo H,<br />
Matsumoto M, Hoshino K, Wagner H, Takeda K, Akira S. A<br />
Toll-like receptor recognizes bacterial DNA. Nature 408: 740–745,<br />
2000.<br />
212. Heppner FL, Christ AD, Klein MA, Prinz M, Fried M, Kraehenbuhl<br />
JP, Aguzzi A. Transepithelial prion transport by M cells.<br />
Nat Med 7: 976–977, 2001.
213. Heppner FL, Greter M, Marino D, Falsig J, Raivich G, Hovelmeyer<br />
N, Waisman A, Rulicke T, Prinz M, Priller J, Becher<br />
B, Aguzzi A. Experimental autoimmune encephalomyelitis repressed<br />
by microglial paralysis. Nat Med 11: 146–152, 2005.<br />
214. Heppner FL, Musahl C, Arrighi I, Klein MA, Rulicke T, Oesch<br />
B, Zinkernagel RM, Kalinke U, Aguzzi A. Prevention of scrapie<br />
pathogenesis by transgenic expression of anti-prion protein antibodies.<br />
Science 294: 178–182, 2001.<br />
215. Heppner FL, Prinz M, Aguzzi A. Pathogenesis of prion diseases:<br />
possible implications of microglial cells. Prog Brain Res 132: 737–<br />
750, 2001.<br />
216. Herl<strong>and</strong> A, Nilsson KP, Olsson JD, Hammarstrom P, Konradsson<br />
P, Inganas O. Synthesis of a regioregular zwitterionic conjugated<br />
oligoelectrolyte, usable as an optical probe for detection of<br />
amyloid fibril formation at acidic pH. J Am Chem Soc 127: 2317–<br />
2323, 2005.<br />
217. Hetz CA, Soto C. Stressing out the ER: a role of the unfolded<br />
protein response in prion-related disorders. Curr Mol Med 6: 37–43,<br />
2006.<br />
218. Hill AF, Butterworth RJ, Joiner S, Jackson G, Rossor MN,<br />
Thomas DJ, Frosh A, Tolley N, Bell JE, Spencer M, King A,<br />
Al-Sarraj S, Ironside JW, Lantos PL, Collinge J. Investigation<br />
of variant Creutzfeldt-Jakob disease <strong>and</strong> other human prion diseases<br />
with tonsil biopsy samples. Lancet 353: 183–189, 1999.<br />
219. Hill AF, Desbruslais M, Joiner S, Sidle KC, Gowl<strong>and</strong> I, Collinge<br />
J, Doey LJ, Lantos P. The same prion strain causes vCJD<br />
<strong>and</strong> BSE. Nature 389: 448–450, 1997.<br />
220. Hill AF, Joiner S, Beck JA, Campbell TA, Dickinson A,<br />
Poulter M, Wadsworth JD, Collinge J. Distinct glycoform ratios<br />
of protease resistant prion protein associated with PRNP point<br />
mutations. Brain 129: 676–685, 2006.<br />
221. Hill AF, Zeidler M, Ironside J, Collinge J. Diagnosis of new<br />
variant Creutzfeldt-Jakob disease by tonsil biopsy. Lancet 349: 99,<br />
1997.<br />
222. Hilton DA. Pathogenesis <strong>and</strong> prevalence of variant Creutzfeldt-<br />
Jakob disease. J Pathol 208: 134–141, 2006.<br />
223. Hilton DA, Fathers E, Edwards P, Ironside JW, Zajicek J.<br />
Prion immunoreactivity in appendix before clinical onset of variant<br />
Creutzfeldt-Jakob disease. Lancet 352: 703–704, 1998.<br />
224. Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu<br />
L, Cherniack RM, Rogers RM, Sciurba FC, Coxson HO, Pare<br />
PD. The nature of small-airway obstruction in chronic obstructive<br />
pulmonary disease. N Engl J Med 350: 2645–2653, 2004.<br />
225. Holscher C, Delius H, Burkle A. Overexpression of nonconvertible<br />
PrP C delta114-121 in scrapie-infected mouse neuroblastoma<br />
cells leads to trans-dominant inhibition of wild-type PrP(Sc) accumulation.<br />
J Virol 72: 1153–1159, 1998.<br />
226. Hope J, Reekie LJ, Hunter N, Multhaup G, Beyreuther K,<br />
White H, Scott AC, Stack MJ, Dawson M, Wells GA. Fibrils<br />
from brains of cows with new cattle disease contain scrapieassociated<br />
protein. Nature 336: 390–392, 1988.<br />
227. Horiuchi M, Caughey B. Specific binding of normal prion protein<br />
to the scrapie form via a localized domain initiates its conversion to<br />
the protease-resistant state. EMBO J 18: 3193–3203, 1999.<br />
228. Horiuchi M, Priola SA, Chabry J, Caughey B. Interactions between<br />
heterologous forms of prion protein: binding, inhibition of<br />
conversion, <strong>and</strong> species barriers. Proc Natl Acad Sci USA 97:<br />
5836–5841, 2000.<br />
229. Hornemann S, Korth C, Oesch B, Riek R, Wider G, Wuthrich<br />
K, Glockshuber R. Recombinant full-length murine prion protein,<br />
mPrP(23-231): purification <strong>and</strong> spectroscopic characterization.<br />
FEBS Lett 413: 277–281, 1997.<br />
230. Hsiao K, Baker HF, Crow TJ, Poulter M, Owen F, Terwilliger<br />
JD, Westaway D, Ott J, Prusiner SB. Linkage of a prion protein<br />
missense variant to Gerstmann-Sträussler syndrome. Nature 338:<br />
342–345, 1989.<br />
231. http://www.cjd.ed.ac.uk/figures.htm. Creutzfeldt-Jakob disease statistics<br />
in the United Kingdom.<br />
232. Huang FP, Farquhar CF, Mabbott NA, Bruce ME, MacPherson<br />
GG. Migrating intestinal dendritic cells transport PrP(Sc) from the<br />
gut. J Gen Virol 83: 267–271, 2002.<br />
AGGREGATION AND INFECTIOUS DISEASE 1145<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
233. Hull RL, Westermark GT, Westermark P, Kahn SE. Islet amyloid:<br />
a critical entity in the pathogenesis of type 2 diabetes. J Clin<br />
Endocrinol Metab 89: 3629–3643, 2004.<br />
234. Hutter G, Heppner FL, Aguzzi A. No superoxide dismutase<br />
activity of cellular prion protein in vivo. Biol Chem 384: 1279–1285,<br />
2003.<br />
235. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl<br />
J Med 357: 2153–2165, 2007.<br />
236. Iijima K, Liu HP, Chiang AS, Hearn SA, Konsolaki M, Zhong Y.<br />
Dissecting the pathological effects of human Abeta40 <strong>and</strong> Abeta42<br />
in Drosophila: a potential model for Alzheimer’s disease. Proc Natl<br />
Acad Sci USA 101: 6623–6628, 2004.<br />
237. Immel F, Jiang Y, Wang Y, Marchal C, Maillet L, Perrett S,<br />
Cullin C. In vitro analysis of SpUre2p, a prion-related protein,<br />
exemplifies the relationship between amyloid <strong>and</strong> prion. J Biol<br />
Chem 282: 7912–7920, 2007.<br />
238. Jarrett JT, Lansbury PT Jr. Seeding “one-dimensional crystallization”<br />
of amyloid: a pathogenic mechanism in Alzheimer’s disease<br />
<strong>and</strong> scrapie? Cell 73: 1055–1058, 1993.<br />
239. Jeffrey M, Goodsir CM, Bruce M, McBride PA, Scott JR,<br />
Halliday WG. Correlative light <strong>and</strong> electron microscopy studies of<br />
PrP localisation in 87V scrapie. Brain Res 656: 329–343, 1994.<br />
240. Jimi T, Wakayama Y, Shibuya S, Nakata H, Tomaru T, Takahashi<br />
Y, Kosaka K, Asano T, Kato K. High levels of nervous<br />
system-specific proteins in cerebrospinal fluid in patients with<br />
early stage Creutzfeldt-Jakob disease. Clin Chim Acta 211: 37–46,<br />
1992.<br />
241. Juanes ME, Elvira G, Garcia-Gr<strong>and</strong>e A, Calero M, Gasset M.<br />
Biosynthesis of prion protein nucleocytoplasmic isoforms by alternative<br />
initiation of translation. J Biol Chem 284: 2787–2794, 2009.<br />
242. Julius C, Heikenwalder M, Schwarz P, Marcel A, Karin M,<br />
Prinz M, Pasparakis M, Aguzzi A. Prion propagation in mice<br />
lacking central nervous system NF-kappaB signalling. J Gen Virol<br />
89: 1545–1550, 2008.<br />
243. Kaeser PS, Klein MA, Schwarz P, Aguzzi A. Efficient lymphoreticular<br />
prion propagation requires PrP(c) in stromal <strong>and</strong> hematopoietic<br />
cells. J Virol 75: 7097–7106, 2001.<br />
244. Kaiserling E. Newly-formed lymph nodes in the submucosa in<br />
chronic inflammatory bowel disease. Lymphology 34: 22–29, 2001.<br />
245. Kaltschmidt B, Uherek M, Wellmann H, Volk B, Kaltschmidt<br />
C. Inhibition of NF-kappaB potentiates amyloid beta-mediated neuronal<br />
apoptosis. Proc Natl Acad Sci USA 96: 9409–9414, 1999.<br />
246. Kane PM, Yamashiro CT, Wolczyk DF, Neff N, Goebl M,<br />
Stevens TH. <strong>Protein</strong> splicing converts the yeast TFP1 gene product<br />
to the 69-kD subunit of the vacuolar H -adenosine triphosphatase.<br />
Science 250: 651–657, 1990.<br />
247. Kanu N, Imokawa Y, Drechsel DN, Williamson RA, Birkett CR,<br />
Bostock CJ, Brockes JP. Transfer of scrapie prion infectivity by<br />
cell contact in culture. Curr Biol 12: 523–530, 2002.<br />
249. Kao RR, Gravenor MB, Baylis M, Bostock CJ, Chihota CM,<br />
Evans JC, Goldmann W, Smith AJ, McLean AR. The potential<br />
size <strong>and</strong> duration of an epidemic of bovine spongiform encephalopathy<br />
in British sheep. Science 295: 332–335, 2002.<br />
250. Kapasi ZF, Qin D, Kerr WG, Kosco-Vilbois MH, Shultz LD,<br />
Tew JG, Szakal AK. Follicular dendritic cell (FDC) precursors in<br />
primary lymphoid tissues. J Immunol 160: 1078–1084, 1998.<br />
251. Karin M. Nuclear factor-kappaB in cancer development <strong>and</strong> progression.<br />
Nature 441: 431–436, 2006.<br />
252. Kayed R, Head E, Thompson JL, McIntire TM, Milton SC,<br />
Cotman CW, Glabe CG. Common structure of soluble amyloid<br />
oligomers implies common mechanism of pathogenesis. Science<br />
300: 486–489, 2003.<br />
253. Keller GA, Siegel MW, Caras IW. Endocytosis of glycophospholipid-anchored<br />
<strong>and</strong> transmembrane forms of CD4 by different endocytic<br />
pathways. EMBO J 11: 863–874, 1992.<br />
254. Kerneis S, Bogdanova A, Kraehenbuhl JP, Pringault E. Conversion<br />
by Peyer’s patch lymphocytes of human enterocytes into M<br />
cells that transport bacteria. Science 277: 949–952, 1997.<br />
255. Kim H, Chatani E, Goto Y, Paik S. Seed-dependent accelerated<br />
fibrillation of alpha-synuclein induced by periodic ultrasonication<br />
treatment. J Microbiol Biotechnol 17: 2027–2032, 2007.<br />
256. Kim JI, Ju WK, Choi JH, Choi E, Carp RI, Wisniewski HM,<br />
Kim YS. Expression of cytokine genes <strong>and</strong> increased nuclear fac-
1146 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
tor-kappa B activity in the brains of scrapie-infected mice. Brain<br />
Res 73: 17–27, 1999.<br />
257. Kimberlin RH, Hall SM, Walker CA. Pathogenesis of mouse<br />
scrapie. Evidence for direct neural spread of infection to the CNS<br />
after injection of sciatic nerve. J Neurol Sci 61: 315–325, 1983.<br />
258. Kimberlin RH, Walker CA. Pathogenesis of mouse scrapie: effect<br />
of route of inoculation on infectivity titres <strong>and</strong> dose-response<br />
curves. J Comp Pathol 88: 39–47, 1978.<br />
259. Kimberlin RH, Walker CA. Pathogenesis of scrapie in mice after<br />
intragastric infection. Virus Res 12: 213–220, 1989.<br />
260. Kirschbaum WR. Zwei eigenartige Erkrankungen des Zentralnervensystems<br />
nach Art der spastischen Pseudosklerose (Jakob). Z<br />
Ges Neurol Psychiatr 92: 175–220, 1924.<br />
261. Kisilevsky R. Preparation <strong>and</strong> propagation of amyloid-enhancing<br />
factor. Methods Mol Biol 299: 237–241, 2005.<br />
262. Kitada T, Asakawa S, Hattori N, Matsumine H, Yamamura Y,<br />
Minoshima S, Yokochi M, Mizuno Y, Shimizu N. Mutations in<br />
the parkin gene cause autosomal recessive juvenile parkinsonism.<br />
Nature 392: 605–608, 1998.<br />
263. Kitamoto T, Muramoto T, Mohri S, Doh ura K, Tateishi J.<br />
Abnormal isoform of prion protein accumulates in follicular dendritic<br />
cells in mice with Creutzfeldt-Jakob disease. J Virol 65:<br />
6292–6295, 1991.<br />
264. Kitamoto T, Tateishi J. Human prion diseases with variant prion<br />
protein. Philos Trans R Soc Lond B Biol Sci 343: 391–398, 1994.<br />
265. Kitamoto T, Tateishi J, Tashima T, Takeshita I, Barry RA,<br />
DeArmond SJ, Prusiner SB. Amyloid plaques in Creutzfeldt-<br />
Jakob disease stain with prion protein antibodies. Ann Neurol 20:<br />
204–208, 1986.<br />
266. Kitamura D, Roes J, Kuhn R, Rajewsky K. A B cell-deficient<br />
mouse by targeted disruption of the membrane exon of the immunoglobulin<br />
mu chain gene. Nature 350: 423–426, 1991.<br />
267. Klein MA, Frigg R, Flechsig E, Raeber AJ, Kalinke U, Bluethmann<br />
H, Bootz F, Suter M, Zinkernagel RM, Aguzzi A. A<br />
crucial role for B cells in neuroinvasive scrapie. Nature 390: 687–<br />
690, 1997.<br />
268. Klein MA, Frigg R, Raeber AJ, Flechsig E, Hegyi I, Zinkernagel<br />
RM, Weissmann C, Aguzzi A. PrP expression in B lymphocytes<br />
is not required for prion neuroinvasion. Nat Med 4: 1429–<br />
1433, 1998.<br />
269. Klein MA, Kaeser PS, Schwarz P, Weyd H, Xenarios I, Zinkernagel<br />
RM, Carroll MC, Verbeek JS, Botto M, Walport MJ,<br />
Molina H, Kalinke U, Acha-Orbea H, Aguzzi A. Complement<br />
facilitates early prion pathogenesis. Nat Med 7: 488–492, 2001.<br />
270. Klohn PC, Stoltze L, Flechsig E, Enari M, Weissmann C. A<br />
quantitative, highly sensitive cell-based infectivity assay for mouse<br />
scrapie prions. Proc Natl Acad Sci USA 100: 11666–11671, 2003.<br />
271. Knaus KJ, Morillas M, Swietnicki W, Malone M, Surewicz WK,<br />
Yee VC. Crystal structure of the human prion protein reveals a<br />
mechanism for oligomerization. Nat Struct Biol 8: 770–774, 2001.<br />
272. Knowles T, Fitzpatrick A, Meehan S, Mott H, Vendruscolo M,<br />
Dobson C, Well<strong>and</strong> M. Role of intermolecular forces in defining<br />
material properties of protein nanofibrils. Science 318: 1900–1903,<br />
2007.<br />
273. Kocisko DA, Vaillant A, Lee KS, Arnold KM, Bertholet N,<br />
Race RE, Olsen EA, Juteau JM, Caughey B. Potent antiscrapie<br />
activities of degenerate phosphorothioate oligonucleotides. Antimicrob<br />
Agents Chemother 50: 1034–1044, 2006.<br />
274. Koller MF, Grau T, Christen P. Induction of antibodies against<br />
murine full-length prion protein in wild-type mice. J Neuroimmunol<br />
132: 113–116, 2002.<br />
275. Kong Q, Huang S, Zou W, Vanegas D, Wang M, Wu D, Yuan J,<br />
Zheng M, Bai H, Deng H, Chen K, Jenny AL, O’Rourke K,<br />
Belay ED, Schonberger LB, Petersen RB, Sy MS, Chen SG,<br />
Gambetti P. Chronic wasting disease of elk: transmissibility to<br />
humans examined by transgenic mouse models. J Neurosci 25:<br />
7944–7949, 2005.<br />
276. Koni PA, Sacca R, Lawton P, Browning JL, Ruddle NH, Flavell<br />
RA. Distinct roles in lymphoid organogenesis for lymphotoxins<br />
alpha <strong>and</strong> beta revealed in lymphotoxin beta-deficient mice. Immunity<br />
6: 491–500, 1997.<br />
277. Kooyman DL, Byrne GW, Logan JS. Glycosyl phosphatidylinositol<br />
anchor. Exp Nephrol 6: 148–151, 1998.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
278. Kooyman DL, Byrne GW, McClellan S, Nielsen D, Tone M,<br />
Waldmann H, Coffman TM, McCurry KR, Platt JL, Logan JS.<br />
In vivo transfer of GPI-linked complement restriction factors from<br />
erythrocytes to the endothelium. Science 269: 89–92, 1995.<br />
279. Korth C, Stierli B, Streit P, Moser M, Schaller O, Fischer R,<br />
Schulz-Schaeffer W, Kretzschmar H, Raeber A, Braun U, Ehrensperger<br />
F, Hornemann S, Glockshuber R, Riek R, Billeter<br />
M, Wuthrich K, Oesch B. Prion (PrPSc)-specific epitope defined<br />
by a monoclonal antibody. Nature 390: 74–77, 1997.<br />
280. Kovacs GG, Head MW, Bunn T, Laszlo L, Will RG, Ironside<br />
JW. Clinicopathological phenotype of codon 129 valine homozygote<br />
sporadic Creutzfeldt-Jakob disease. Neuropathol Appl Neurobiol<br />
26: 463–472, 2000.<br />
281. Kovacs GG, Lindeck-Pozza E, Chimelli L, Araujo AQ, Gabbai<br />
AA, Strobel T, Glatzel M, Aguzzi A, Budka H. Creutzfeldt-Jakob<br />
disease <strong>and</strong> inclusion body myositis: abundant disease-associated<br />
prion protein in muscle. Ann Neurol 55: 121–125, 2004.<br />
282. Kranich J, Krautler NJ, Heinen E, Polymenidou M, Bridel C,<br />
Schildknecht A, Huber C, Kosco-Vilbois MH, Zinkernagel R,<br />
Miele G, Aguzzi A. Follicular dendritic cells control engulfment of<br />
apoptotic bodies by secreting Mfge8. J Exp Med 205: 1293–1302,<br />
2008.<br />
283. Kratz A, Campos-Neto A, Hanson MS, Ruddle NH. Chronic<br />
inflammation caused by lymphotoxin is lymphoid neogenesis. J<br />
Exp Med 183: 1461–1472, 1996.<br />
284. Kristiansen M, Deriziotis P, Dimcheff DE, Jackson GS, Ovaa<br />
H, Naumann H, Clarke AR, van Leeuwen FW, Menendez-<br />
Benito V, Dantuma NP, Portis JL, Collinge J, Tabrizi SJ.<br />
Disease-associated prion protein oligomers inhibit the 26S proteasome.<br />
Mol Cell 26: 175–188, 2007.<br />
285. Kristiansen M, Messenger MJ, Klohn PC, Br<strong>and</strong>ner S, Wadsworth<br />
JD, Collinge J, Tabrizi SJ. Disease-related prion protein<br />
forms aggresomes in neuronal cells leading to caspase-activation<br />
<strong>and</strong> apoptosis. J Biol Chem 280: 38851–38861, 2005.<br />
286. Kuwahara C, Takeuchi AM, Nishimura T, Haraguchi K, Kubosaki<br />
A, Matsumoto Y, Saeki K, Matsumoto Y, Yokoyama T,<br />
Itohara S, Onodera T. <strong>Prions</strong> prevent neuronal cell-line death.<br />
Nature 400: 225–226, 1999.<br />
287. Lacroux C, Simon S, Benestad SL, Maillet S, Mathey J, Lugan<br />
S, Corbiere F, Cassard H, Costes P, Bergonier D, Weisbecker<br />
JL, Moldal T, Simmons H, Lantier F, Feraudet-Tarisse C,<br />
Morel N, Schelcher F, Grassi J, Andreoletti O. <strong>Prions</strong> in milk<br />
from ewes incubating natural scrapie. PLoS Pathog 4: e1000238,<br />
2008.<br />
288. Lansbury PT. Mechanism of scrapie replication. Science 265: 1510,<br />
1994.<br />
289. Laplanche JL, Chatelain J, Launay JM, Gazengel C, Vidaud M.<br />
Deletion in prion protein gene in a Moroccan family. Nucleic Acids<br />
Res 18: 6745, 1990.<br />
290. Larson J, Lynch G, Games D, Seubert P. Alterations in synaptic<br />
transmission <strong>and</strong> long-term potentiation in hippocampal slices<br />
from young <strong>and</strong> aged PDAPP mice. Brain Res 840: 23–35, 1999.<br />
291. Lasmezas CI, Cesbron JY, Deslys JP, Demaimay R, Adjou KT,<br />
Rioux R, Lemaire C, Locht C, Dormont D. Immune systemdependent<br />
<strong>and</strong> -independent replication of the scrapie agent. J Virol<br />
70: 1292–1295, 1996.<br />
292. Lau AL, Yam AY, Michelitsch MM, Wang X, Gao C, Goodson<br />
RJ, Shimizu R, Timoteo G, Hall J, Medina-Selby A, Coit D,<br />
McCoin C, Phelps B, Wu P, Hu C, Chien D, Peretz D. Characterization<br />
of prion protein (PrP)-derived peptides that discriminate<br />
full-length PrPSc from PrPC. Proc Natl Acad Sci USA 104: 11551–<br />
11556, 2007.<br />
293. Le Pichon CE, Valley MT, Polymenidou M, Chesler AT, Sagdullaev<br />
BT, Aguzzi A, Firestein S. Olfactory behavior <strong>and</strong> physiology<br />
are disrupted in prion protein knockout mice. Nat Neurosci<br />
12: 60–69, 2009.<br />
294. Leblanc P, Alais S, Porto-Carreiro I, Lehmann S, Grassi J,<br />
Raposo G, Darlix JL. Retrovirus infection strongly enhances<br />
scrapie infectivity release in cell culture. EMBO J 25: 2674–2685,<br />
2006.<br />
295. Legname G, Baskakov IV, Nguyen HO, Riesner D, Cohen FE,<br />
DeArmond SJ, Prusiner SB. Synthetic mammalian prions. Science<br />
305: 673–676, 2004.
296. Legname G, Nguyen HO, Peretz D, Cohen FE, DeArmond SJ,<br />
Prusiner SB. Continuum of prion protein structures enciphers a<br />
multitude of prion isolate-specified phenotypes. Proc Natl Acad Sci<br />
USA 103: 19105–19110, 2006.<br />
297. Li A, Christensen H, Stewart L, Roth K, Chiesa R, Harris D.<br />
Neonatal lethality in transgenic mice expressing prion protein with<br />
a deletion of residues 105–125. EMBO J 26: 548–558, 2007.<br />
298. Li A, Sakaguchi S, Shigematsu K, Atarashi R, Roy BC, Nakaoke<br />
R, Arima K, Okimura N, Kopacek J, Katamine S. <strong>Physiological</strong><br />
expression of the gene for PrP-like protein, PrPLP/Dpl, by<br />
brain endothelial cells <strong>and</strong> its ectopic expression in neurons of<br />
PrP-deficient mice ataxic due to Purkinje cell degeneration. Am J<br />
Pathol 157: 1447–1452, 2000.<br />
299. Li JY, Englund E, Holton JL, Soulet D, Hagell P, Lees AJ,<br />
Lashley T, Quinn NP, Rehncrona S, Bjorklund A, Widner H,<br />
Revesz T, Lindvall O, Brundin P. Lewy bodies in grafted neurons<br />
in subjects with Parkinson’s disease suggest host-to-graft disease<br />
propagation. Nat Med 14: 501–503, 2008.<br />
300. Ligios C, Sigurdson CJ, Santucciu C, Carcassola G, Manco G,<br />
Basagni M, Maestrale C, Cancedda MG, Madau L, Aguzzi A.<br />
PrPSc in mammary gl<strong>and</strong>s of sheep affected by scrapie <strong>and</strong> mastitis.<br />
Nat Med 11: 1137–1138, 2005.<br />
301. Linden R, Martins VR, Prado MA, Cammarota M, Izquierdo I,<br />
Brentani RR. Physiology of the prion protein. Physiol Rev 88:<br />
673–728, 2008.<br />
302. Liu T, Li R, Pan T, Liu D, Petersen RB, Wong BS, Gambetti P,<br />
Sy MS. Intercellular transfer of the cellular prion protein. J Biol<br />
Chem 277: 47671–47678, 2002.<br />
303. Llewelyn CA, Hewitt PE, Knight RS, Amar K, Cousens S,<br />
Mackenzie J, Will RG. Possible transmission of variant<br />
Creutzfeldt-Jakob disease by blood transfusion. Lancet 363: 417–<br />
421, 2004.<br />
304. Lo Bianco C, Ridet JL, Schneider BL, Deglon N, Aebischer P.<br />
alpha-Synucleinopathy <strong>and</strong> selective dopaminergic neuron loss in a<br />
rat lentiviral-based model of Parkinson’s disease. Proc Natl Acad<br />
Sci USA 99: 10813–10818, 2002.<br />
305. Locht C, Chesebro B, Race R, Keith JM. Molecular cloning <strong>and</strong><br />
complete sequence of prion protein cDNA from mouse brain infected<br />
with the scrapie agent. Proc Natl Acad Sci USA 83: 6372–<br />
6376, 1986.<br />
306. Locksley RM, Killeen N, Lenardo MJ. The TNF <strong>and</strong> TNF receptor<br />
superfamilies: integrating mammalian biology. Cell 104: 487–<br />
501, 2001.<br />
307. Lu K, Wang W, Xie Z, Wong BS, Li R, Petersen RB, Sy MS,<br />
Chen SG. Expression <strong>and</strong> structural characterization of the recombinant<br />
human doppel protein. Biochemistry 39: 13575–13583, 2000.<br />
308. Lundmark K, Westermark GT, Nystrom S, Murphy CL, Solomon<br />
A, Westermark P. Transmissibility of systemic amyloidosis<br />
by a prion-like mechanism. Proc Natl Acad Sci USA 99: 6979–<br />
6984, 2002.<br />
309. Lysek DA, Schorn C, Nivon LG, Esteve-Moya V, Christen B,<br />
Calzolai L, von Schroetter C, Fiorito F, Herrmann T, Güntert<br />
P, Wüthrich K. Prion protein NMR structures of cats, dogs, pigs,<br />
<strong>and</strong> sheep. Proc Natl Acad Sci USA 102: 640–645, 2005.<br />
310. M’Fadyean JM. Scrapie. J Comp Pathol 31: 102–131, 1918.<br />
311. M’Gowan JP. Investigation into the Disease of Sheep Called<br />
“Scrapie.” Edinburgh: William Blackwood, 1914.<br />
312. Ma J, Lindquist S. Conversion of PrP to a self-perpetuating<br />
PrPSc-like conformation in the cytosol. Science 298: 1785–1788,<br />
2002.<br />
313. Ma J, Lindquist S. Wild-type PrP <strong>and</strong> a mutant associated with<br />
prion disease are subject to retrograde transport <strong>and</strong> proteasome<br />
degradation. Proc Natl Acad Sci USA 98: 14955–14960, 2001.<br />
314. Ma J, Wollmann R, Lindquist S. Neurotoxicity <strong>and</strong> neurodegeneration<br />
when PrP accumulates in the cytosol. Science 298: 1781–<br />
1785, 2002.<br />
315. Mabbott NA, Bruce ME, Botto M, Walport MJ, Pepys MB.<br />
Temporary depletion of complement component C3 or genetic<br />
deficiency of C1q significantly delays onset of scrapie. Nat Med 7:<br />
485–487, 2001.<br />
316. Mabbott NA, Mackay F, Minns F, Bruce ME. Temporary inactivation<br />
of follicular dendritic cells delays neuroinvasion of scrapie.<br />
Nat Med 6: 719–720, 2000.<br />
AGGREGATION AND INFECTIOUS DISEASE 1147<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
317. Mabbott NA, MacPherson GG. <strong>Prions</strong> <strong>and</strong> their lethal journey to<br />
the brain. Nat Rev Microbiol 4: 201–211, 2006.<br />
318. Mackay F, Majeau GR, Lawton P, Hochman PS, Browning JL.<br />
Lymphotoxin but not tumor necrosis factor functions to maintain<br />
splenic architecture <strong>and</strong> humoral responsiveness in adult mice.<br />
Eur J Immunol 27: 2033–2042, 1997.<br />
319. Mahal SP, Baker CA, Demczyk CA, Smith EW, Julius C,<br />
Weissmann C. Prion strain discrimination in cell culture: the cell<br />
panel assay. Proc Natl Acad Sci USA 104: 20908–20913, 2007.<br />
320. Malisauskas M, Ostman J, Darinskas A, Zamotin V, Liutkevicius<br />
E, Lundgren E, Morozova-Roche LA. Does the cytotoxic<br />
effect of transient amyloid oligomers from common equine lysozyme<br />
in vitro imply innate amyloid toxicity? J Biol Chem 280:<br />
6269–6275, 2005.<br />
321. Mallucci G, Dickinson A, Linehan J, Klohn PC, Br<strong>and</strong>ner S,<br />
Collinge J. Depleting neuronal PrP in prion infection prevents<br />
disease <strong>and</strong> reverses spongiosis. Science 302: 871–874, 2003.<br />
322. Mallucci GR, Ratte S, Asante EA, Linehan J, Gowl<strong>and</strong> I,<br />
Jefferys JG, Collinge J. Post-natal knockout of prion protein<br />
alters hippocampal CA1 properties, but does not result in neurodegeneration.<br />
EMBO J 21: 202–210, 2002.<br />
323. Mallucci GRWM, Farmer M, Dickinson A, Khatun H, Powell<br />
AD, Br<strong>and</strong>ner S, Jefferys JG, Collinge J. Targeting cellular<br />
prion protein reverses early cognitive deficits <strong>and</strong> neurophysiological<br />
dysfunction in prion-infected mice. Neuron 53: 325–335, 2007.<br />
324. Malmgren R, Kurl<strong>and</strong> L, Mokri B, Kurtzke J. The epidemiology<br />
of Creutzfeldt-Jakob disease. In: Slow Transmissible <strong>Diseases</strong> of<br />
the Nervous System, edited by Prusiner SB, Hadlow WJ. New York:<br />
Academic, 1979, p. 93–112.<br />
325. Manson JC, Clarke AR, Hooper ML, Aitchison L, McConnell I,<br />
Hope J. 129/Ola mice carrying a null mutation in PrP that abolishes<br />
mRNA production are developmentally normal. Mol Neurobiol 8:<br />
121–127, 1994.<br />
326. Manson JC, Clarke AR, McBride PA, McConnell I, Hope J. PrP<br />
gene dosage determines the timing but not the final intensity or<br />
distribution of lesions in scrapie pathology. Neurodegeneration 3:<br />
331–340, 1994.<br />
327. Manuelidis EE, de Figueiredo JM, Kim JH, Fritch WW, Manuelidis<br />
L. Transmission studies from blood of Alzheimer disease<br />
patients <strong>and</strong> healthy relatives. Proc Natl Acad Sci USA 85: 4898–<br />
4901, 1988.<br />
328. Marsh RF, Hadlow WJ. Transmissible mink encephalopathy. Rev<br />
Sci Tech 11: 539–550, 1992.<br />
329. Marsh RF, Kimberlin RH. Comparison of scrapie <strong>and</strong> transmissible<br />
mink encephalopathy in hamsters. II. Clinical signs, pathology,<br />
<strong>and</strong> pathogenesis. J Infect Dis 131: 104–110, 1975.<br />
330. Masliah E, Rockenstein E, Veinbergs I, Mallory M, Hashimoto<br />
M, Takeda A, Sagara Y, Sisk A, Mucke L. Dopaminergic loss <strong>and</strong><br />
inclusion body formation in alpha-synuclein mice: implications for<br />
neurodegenerative disorders. Science 287: 1265–1269, 2000.<br />
331. Masters CL, Richardson EP. Subacute spongiform encephalopathy<br />
(Creutzfeldt-Jakob disease). The nature <strong>and</strong> progression of<br />
spongiform change. Brain 101: 333–344, 1978.<br />
332. Mathiason CK, Powers JG, Dahmes SJ, Osborn DA, Miller KV,<br />
Warren RJ, Mason GL, Hays SA, Hayes-Klug J, Seelig DM,<br />
Wild MA, Wolfe LL, Spraker TR, Miller MW, Sigurdson CJ,<br />
Telling GC, Hoover EA. <strong>Infectious</strong> prions in the saliva <strong>and</strong> blood<br />
of deer with chronic wasting disease. Science 314: 133–136, 2006.<br />
333. Matsumoto M, Fu YX, Molina H, Huang G, Kim J, Thomas DA,<br />
Nahm MH, Chaplin DD. Distinct roles of lymphotoxin alpha <strong>and</strong><br />
the type I tumor necrosis factor (TNF) receptor in the establishment<br />
of follicular dendritic cells from non-bone marrow-derived<br />
cells. J Exp Med 186: 1997–2004, 1997.<br />
334. Mawhinney S, Pape WJ, Forster JE, Anderson CA, Bosque P,<br />
Miller MW. Human prion disease <strong>and</strong> relative risk associated with<br />
chronic wasting disease. Emerg Infect Dis 12: 1527–1535, 2006.<br />
335. McBride PA, Beekes M. Pathological PrP is abundant in sympathetic<br />
<strong>and</strong> sensory ganglia of hamsters fed with scrapie. Neurosci<br />
Lett 265: 135–138, 1999.<br />
336. McBride PA, Schulz-Schaeffer WJ, Donaldson M, Bruce M,<br />
Diringer H, Kretzschmar HA, Beekes M. Early spread of scrapie<br />
from the gastrointestinal tract to the central nervous system in-
1148 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
volves autonomic fibers of the splanchnic <strong>and</strong> vagus nerves. J Virol<br />
75: 9320–9327, 2001.<br />
337. McKinley MP, Bolton DC, Prusiner SB. A protease-resistant<br />
protein is a structural component of the scrapie prion. Cell 35:<br />
57–62, 1983.<br />
338. McKinley MP, Meyer RK, Kenaga L, Rahbar F, Cotter R,<br />
Serban A, Prusiner SB. Scrapie prion rod formation in vitro<br />
requires both detergent extraction <strong>and</strong> limited proteolysis. J Virol<br />
65: 1340–1351, 1991.<br />
339. Mead S. Prion disease genetics. Eur J Hum Genet 14: 273–281,<br />
2006.<br />
340. Mead S, Poulter M, Uphill J, Beck J, Whitfield J, Webb TE,<br />
Campbell T, Adamson G, Deriziotis P, Tabrizi SJ, Hummerich<br />
H, Verzilli C, Alpers MP, Whittaker JC, Collinge J. Genetic risk<br />
factors for variant Creutzfeldt-Jakob disease: a genome-wide association<br />
study. Lancet Neurol 8: 57–66, 2009.<br />
341. Mead S, Stumpf MP, Whitfield J, Beck JA, Poulter M, Campbell<br />
T, Uphill JB, Goldstein D, Alpers M, Fisher EM, Collinge<br />
J. Balancing selection at the prion protein gene consistent with<br />
prehistoric kurulike epidemics. Science 300: 640–643, 2003.<br />
342. Meggendorfer F. Klinische und genealogische Beobachtungen bei<br />
einem Fall von spastischer Pseudosklerose Jakobs. Z Ges Neurol<br />
Psychiatr 128: 337–341, 1930.<br />
343. Meier P, Genoud N, Prinz M, Maissen M, Rulicke T, Zurbriggen<br />
A, Raeber AJ, Aguzzi A. Soluble dimeric prion protein binds<br />
PrP(Sc) in vivo <strong>and</strong> antagonizes prion disease. Cell 113: 49–60,<br />
2003.<br />
344. Merz PA, Somerville RA, Wisniewski HM, Manuelidis L, Manuelidis<br />
EE. Scrapie-associated fibrils in Creutzfeldt-Jakob disease.<br />
Nature 306: 474–476, 1983.<br />
345. Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S,<br />
Schaefer C, Kilger E, Neuenschw<strong>and</strong>er A, Abramowski D,<br />
Frey P, Jaton AL, Vigouret JM, Paganetti P, Walsh DM,<br />
Mathews PM, Ghiso J, Staufenbiel M, Walker LC, Jucker M.<br />
Exogenous induction of cerebral beta-amyloidogenesis is governed<br />
by agent <strong>and</strong> host. Science 313: 1781–1784, 2006.<br />
346. Meyer RK, McKinley MP, Bowman KA, Braunfeld MB, Barry<br />
RA, Prusiner SB. Separation <strong>and</strong> properties of cellular <strong>and</strong><br />
scrapie prion proteins. Proc Natl Acad Sci USA 83: 2310–2314,<br />
1986.<br />
347. Miele G, Seeger H, Marino D, Eberhard R, Heikenwalder M,<br />
Stoeck K, Basagni M, Knight R, Green A, Chianini F, Wuthrich<br />
RP, Hock C, Zerr I, Aguzzi A. Urinary alpha1-antichymotrypsin:<br />
a biomarker of prion infection. PLoS ONE 3: e3870, 2008.<br />
348. Miller MW, Williams ES. Prion disease: horizontal prion transmission<br />
in mule deer. Nature 425: 35–36, 2003.<br />
349. Miller MW, Williams ES, Hobbs NT, Wolfe LL. Environmental<br />
sources of prion transmission in mule deer. Emerg Infect Dis 10:<br />
1003–1006, 2004.<br />
350. Millson GC, Hunter GD, Kimberlin RH. An experimental examination<br />
of the scrapie agent in cell membrane mixtures. II. The<br />
association of scrapie activity with membrane fractions. J Comp<br />
Pathol 81: 255–265, 1971.<br />
351. Mishra RS, Basu S, Gu Y, Luo X, Zou WQ, Mishra R, Li R, Chen<br />
SG, Gambetti P, Fujioka H, Singh N. Protease-resistant human<br />
prion protein <strong>and</strong> ferritin are cotransported across Caco-2 epithelial<br />
cells: implications for species barrier in prion uptake from the<br />
intestine. J Neurosci 24: 11280–11290, 2004.<br />
352. Moechars D, Dewachter I, Lorent K, Reverse D, Baekel<strong>and</strong>t V,<br />
Naidu A, Tesseur I, Spittaels K, Haute CV, Checler F, Godaux<br />
E, Cordell B, Van Leuven F. Early phenotypic changes in transgenic<br />
mice that overexpress different mutants of amyloid precursor<br />
protein in brain. J Biol Chem 274: 6483–6492, 1999.<br />
353. Mohan J, Brown KL, Farquhar CF, Bruce ME, Mabbott NA.<br />
Scrapie transmission following exposure through the skin is dependent<br />
on follicular dendritic cells in lymphoid tissues. J Dermatol<br />
Sci 35: 101–111, 2004.<br />
354. Montrasio F, Cozzio A, Flechsig E, Rossi D, Klein MA, Rulicke<br />
T, Raeber AJ, Vosshenrich CA, Proft J, Aguzzi A, Weissmann<br />
C. B lymphocyte-restricted expression of prion protein does not<br />
enable prion replication in prion protein knockout mice. Proc Natl<br />
Acad Sci USA 98: 4034–4037, 2001.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
355. Montrasio F, Frigg R, Glatzel M, Klein MA, Mackay F, Aguzzi<br />
A, Weissmann C. Impaired prion replication in spleens of mice<br />
lacking functional follicular dendritic cells. Science 288: 1257–1259,<br />
2000.<br />
356. Moore RC, Lee IY, Silverman GL, Harrison PM, Strome R,<br />
Heinrich C, Karunaratne A, Pasternak SH, Chishti MA, Liang<br />
Y, Mastrangelo P, Wang K, Smit AF, Katamine S, Carlson GA,<br />
Cohen FE, Prusiner SB, Melton DW, Tremblay P, Hood LE,<br />
Westaway D. Ataxia in prion protein (PrP)-deficient mice is associated<br />
with upregulation of the novel PrP-like protein doppel. J Mol<br />
Biol 292: 797–817, 1999.<br />
357. Morel E, Andrieu T, Casagr<strong>and</strong>e F, Gauczynski S, Weiss S,<br />
Grassi J, Rousset M, Dormont D, Chambaz J. Bovine prion is<br />
endocytosed by human enterocytes via the 37 kDa/67 kDa laminin<br />
receptor. Am J Pathol 167: 1033–1042, 2005.<br />
358. Moroncini G, Mangieri M, Morbin M, Mazzoleni G, Ghetti B,<br />
Gabrielli A, Williamson RA, Giaccone G, Tagliavini F. Pathologic<br />
prion protein is specifically recognized in situ by a novel PrP<br />
conformational antibody. Neurobiol Dis 23: 717–724, 2006.<br />
359. Munson L, Terio KA, Worley M, Jago M, Bagot-Smith A,<br />
Marker L. Extrinsic factors significantly affect patterns of disease<br />
in free-ranging <strong>and</strong> captive cheetah (Acinonyx jubatus) populations.<br />
J Wildl Dis 41: 542–548, 2005.<br />
360. Muramoto T, DeArmond SJ, Scott M, Telling GC, Cohen FE,<br />
Prusiner SB. Heritable disorder resembling neuronal storage disease<br />
in mice expressing prion protein with deletion of an alphahelix.<br />
Nat Med 3: 750–755, 1997.<br />
361. Muramoto T, Scott M, Cohen FE, Prusiner SB. Recombinant<br />
Scrapie-like prion protein of 106 amino acids is soluble. Proc Natl<br />
Acad Sci USA 93: 15457–15462, 1996.<br />
362. Naslavsky N, Stein R, Yanai A, Friedl<strong>and</strong>er G, Taraboulos A.<br />
Characterization of detergent-insoluble complexes containing the<br />
cellular prion protein <strong>and</strong> its scrapie isoform. J Biol Chem 272:<br />
6324–6331, 1997.<br />
363. Neutra MR, Frey A, Kraehenbuhl JP. Epithelial M cells: gateways<br />
for mucosal infection <strong>and</strong> immunization. Cell 86: 345–348,<br />
1996.<br />
364. Nilsberth C, Westlind-Danielsson A, Eckman CB, Condron<br />
MM, Axelman K, Forsell C, Stenh C, Luthman J, Teplow DB,<br />
Younkin SG, Naslund J, Lannfelt L. The “Arctic” APP mutation<br />
(E693G) causes Alzheimer’s disease by enhanced Abeta protofibril<br />
formation. Nat Neurosci 4: 887–893, 2001.<br />
365. Nilsson KP, Aslund A, Berg I, Nystrom S, Konradsson P,<br />
Herl<strong>and</strong> A, Inganas O, Stabo-Eeg F, Lindgren M, Westermark<br />
GT, Lannfelt L, Nilsson LN, Hammarstrom P. Imaging distinct<br />
conformational states of amyloid-beta fibrils in Alzheimer’s disease<br />
using novel luminescent probes. ACS Chem Biol 2: 553–560, 2007.<br />
366. Nilsson KPR, Hammarstrom P, Ahlgren F, Herl<strong>and</strong> A, Schnell<br />
EA, Lindgren M, Westermark GT, Inganas O. Conjugated polyelectrolytes-conformation-sensitive<br />
optical probes for staining <strong>and</strong><br />
characterization of amyloid deposits. Chembiochem 7: 1096–1104,<br />
2006.<br />
367. Nilsson KPR, Herl<strong>and</strong> A, Hammarstrom P, Inganas O. Conjugated<br />
polyelectrolytes: conformation-sensitive optical probes for<br />
detection of amyloid fibril formation. Biochemistry 44: 3718–3724,<br />
2005.<br />
368. Nishida N, Tremblay P, Sugimoto T, Shigematsu K, Shirabe S,<br />
Petromilli C, Erpel SP, Nakaoke R, Atarashi R, Houtani T,<br />
Torchia M, Sakaguchi S, DeArmond SJ, Prusiner SB, Katamine<br />
S. A mouse prion protein transgene rescues mice deficient<br />
for the prion protein gene from Purkinje cell degeneration <strong>and</strong><br />
demyelination. Lab Invest 79: 689–697, 1999.<br />
369. Nonno R, Bari MA, Cardone F, Vaccari G, Fazzi P, Dell’omo G,<br />
Cartoni C, Ingrosso L, Boyle A, Galeno R, Sbriccoli M, Lipp<br />
HP, Bruce M, Pocchiari M, Agrimi U. Efficient transmission <strong>and</strong><br />
characterization of Creutzfeldt-Jakob disease strains in bank voles.<br />
PLoS Pathog 2: e12, 2006.<br />
370. Oesch B, Westaway D, Walchli M, McKinley MP, Kent SB,<br />
Aebersold R, Barry RA, Tempst P, Teplow DB, Hood LE,<br />
Weissmann C. A cellular gene encodes scrapie PrP 27–30 protein.<br />
Cell 40: 735–746, 1985.
371. Ohhashi Y, Kihara M, Naiki H, Goto Y. Ultrasonication-induced<br />
amyloid fibril formation of beta2-microglobulin. J Biol Chem 280:<br />
32843–32848, 2005.<br />
372. Okamoto M, Furuoka H, Horiuchi M, Noguchi T, Hagiwara K,<br />
Muramatsu Y, Tomonaga K, Tsuji M, Ishihara C, Ikuta K,<br />
Taniyama H. Experimental transmission of abnormal prion protein<br />
(PrPsc) in the small intestinal epithelial cells of neonatal mice.<br />
Vet Pathol 40: 723–727, 2003.<br />
373. Opie EL. The relation of diabetes mellitus to lesions of the pancreas:<br />
hyaline degeneration of the islets of Langerhans. J Exp Med<br />
5: 527–540, 1901.<br />
374. Ott D, Taraborrelli C, Aguzzi A. Novel dominant-negative prion<br />
protein mutants identified from a r<strong>and</strong>omized library. <strong>Protein</strong> Eng<br />
Des Sel 21: 623–629, 2008.<br />
375. Owen F, Poulter M, Collinge J, Crow TJ. Codon 129 changes in<br />
the prion protein gene in Caucasians. Am J Hum Genet 46: 1215–<br />
1216, 1990.<br />
376. Owen JP, Maddison BC, Whitelam GC, Gough KC. Use of<br />
thermolysin in the diagnosis of prion diseases. Mol Biotechnol 35:<br />
161–170, 2007.<br />
377. Packer RJ, Cornblath DR, Gonatas NK, Bruno LA, Asbury AK.<br />
Creutzfeldt-Jakob disease in a 20-year-old woman. Neurology 30:<br />
492–496, 1980.<br />
378. Palmer MS, Dryden AJ, Hughes JT, Collinge J. Homozygous<br />
prion protein genotype predisposes to sporadic Creutzfeldt-Jakob<br />
disease. Nature 352: 340–342, 1991.<br />
379. Pan KM, Baldwin M, Nguyen J, Gasset M, Serban A, Groth D,<br />
Mehlhorn I, Huang Z, Fletterick RJ, Cohen FE, et al. Conversion<br />
of alpha-helices into beta-sheets features in the formation of<br />
the scrapie prion proteins. Proc Natl Acad Sci USA 90: 10962–<br />
10966, 1993.<br />
380. Pan T, Li R, Wong BS, Liu T, Gambetti P, Sy MS. Heterogeneity<br />
of normal prion protein in two-dimensional immunoblot: presence<br />
of various glycosylated <strong>and</strong> truncated forms. J Neurochem 81:<br />
1092–1101, 2002.<br />
381. Parchi P, Giese A, Capellari S, Brown P, Schulz-Schaeffer W,<br />
Windl O, Zerr I, Budka H, Kopp N, Piccardo P, Poser S,<br />
Rojiani A, Streichemberger N, Julien J, Vital C, Ghetti B,<br />
Gambetti P, Kretzschmar H. Classification of sporadic<br />
Creutzfeldt-Jakob disease based on molecular <strong>and</strong> phenotypic analysis<br />
of 300 subjects. Ann Neurol 46: 224–233, 1999.<br />
382. Parry HB. Scrapie Disease in Sheep. New York: Academic, 1983.<br />
383. Pattison IH, Jones KM. The possible nature of the transmissible<br />
agent of scrapie. Vet Rec 80: 2–9, 1967.<br />
384. Pattison IH, Millson GC. Distribution of the scrapie agent in the<br />
tissues of experimentally inoculated goats. J Comp Pathol 72:<br />
233–244, 1962.<br />
385. Pattison IH, Millson GC. Further observations on the experimental<br />
production of scrapie in goats <strong>and</strong> sheep. J Comp Pathol 70:<br />
182–193, 1960.<br />
386. Pattison IH, Millson GC. Scrapie produced experimentally in<br />
goats with special reference to the clinical syndrome. J Comp<br />
Pathol 71: 101–108, 1961.<br />
387. Peden AH, Head MW, Ritchie DL, Bell JE, Ironside JW. Preclinical<br />
vCJD after blood transfusion in a PRNP codon 129 heterozygous<br />
patient. Lancet 364: 527–529, 2004.<br />
388. Peden AH, Ritchie DL, Head MW, Ironside JW. Detection <strong>and</strong><br />
localization of PrPSc in the skeletal muscle of patients with variant,<br />
iatrogenic, <strong>and</strong> sporadic forms of Creutzfeldt-Jakob disease. Am J<br />
Pathol 168: 927–935, 2006.<br />
389. Peretz D, Williamson RA, Kaneko K, Vergara J, Leclerc E,<br />
Schmitt-Ulms G, Mehlhorn IR, Legname G, Wormald MR,<br />
Rudd PM, Dwek RA, Burton DR, Prusiner SB. Antibodies inhibit<br />
prion propagation <strong>and</strong> clear cell cultures of prion infectivity. Nature<br />
412: 739–743, 2001.<br />
390. Peretz D, Williamson RA, Legname G, Matsunaga Y, Vergara<br />
J, Burton DR, DeArmond SJ, Prusiner SB, Scott MR. A change<br />
in the conformation of prions accompanies the emergence of a new<br />
prion strain. Neuron 34: 921–932, 2002.<br />
391. Perrier V, Kaneko K, Safar J, Vergara J, Tremblay P, De-<br />
Armond SJ, Cohen FE, Prusiner SB, Wallace AC. Dominantnegative<br />
inhibition of prion replication in transgenic mice. Proc<br />
Natl Acad Sci USA 99: 13079–13084, 2002.<br />
AGGREGATION AND INFECTIOUS DISEASE 1149<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
392. Perry VH, Cunningham C, Boche D. Atypical inflammation in the<br />
central nervous system in prion disease. Curr Opin Neurol 15:<br />
349–354, 2002.<br />
393. Piubelli C, Fiorini M, Zanusso G, Milli A, Fasoli E, Monaco S,<br />
Righetti PG. Searching for markers of Creutzfeldt-Jakob disease<br />
in cerebrospinal fluid by two-dimensional mapping. Proteomics 6<br />
Suppl 1: S256–S261, 2006.<br />
394. Polymenidou M, Heppner FL, Pellicioli EC, Urich E, Miele G,<br />
Braun N, Wopfner F, Schaetzl H, Becher B, Aguzzi A. Humoral<br />
immune response to native eukaryotic prion protein correlates<br />
with anti-prion protection. Proc Natl Acad Sci USA 101: 14670–<br />
14676, 2004.<br />
395. Polymenidou M, Moos R, Scott M, Sigurdson C, Shi YZ, Yajima<br />
B, Hafner-Bratkovic I, Jerala R, Hornemann S, Wuthrich K,<br />
Bellon A, Vey M, Garen G, James MN, Kav N, Aguzzi A. The<br />
POM monoclonals: a comprehensive set of antibodies to nonoverlapping<br />
prion protein epitopes. PLoS ONE 3: e3872, 2008.<br />
396. Polymenidou M, Stoeck K, Glatzel M, Vey M, Bellon A, Aguzzi<br />
A. Coexistence of multiple PrPSc types in individuals with<br />
Creutzfeldt-Jakob disease. Lancet Neurol 4: 805–814, 2005.<br />
397. Prinz M, Heikenwalder M, Junt T, Schwarz P, Glatzel M,<br />
Heppner FL, Fu YX, Lipp M, Aguzzi A. Positioning of follicular<br />
dendritic cells within the spleen controls prion neuroinvasion.<br />
Nature 425: 957–962, 2003.<br />
398. Prinz M, Heikenwalder M, Schwarz P, Takeda K, Akira S,<br />
Aguzzi A. Prion pathogenesis in the absence of Toll-like receptor<br />
signalling. EMBO Rep 4: 195–199, 2003.<br />
399. Prinz M, Huber G, Macpherson AJ, Heppner FL, Glatzel M,<br />
Eugster HP, Wagner N, Aguzzi A. Oral prion infection requires<br />
normal numbers of Peyer’s patches but not of enteric lymphocytes.<br />
Am J Pathol 162: 1103–1111, 2003.<br />
400. Prinz M, Montrasio F, Klein MA, Schwarz P, Priller J, Odermatt<br />
B, Pfeffer K, Aguzzi A. Lymph nodal prion replication <strong>and</strong><br />
neuroinvasion in mice devoid of follicular dendritic cells. Proc Natl<br />
Acad Sci USA 99: 919–924, 2002.<br />
401. Priola SA, Raines A, Caughey WS. Porphyrin <strong>and</strong> phthalocyanine<br />
antiscrapie compounds. Science 287: 1503–1506, 2000.<br />
402. Prusiner SB. Creutzfeldt-Jakob disease <strong>and</strong> scrapie prions. Alzheimer<br />
Dis Assoc Disord 3: 52–78, 1989.<br />
403. Prusiner SB. Novel proteinaceous infectious particles cause<br />
scrapie. Science 216: 136–144, 1982.<br />
404. Prusiner SB, Bolton DC, Groth DF, Bowman KA, Cochran SP,<br />
McKinley MP. Further purification <strong>and</strong> characterization of scrapie<br />
prions. Biochemistry 21: 6942–6950, 1982.<br />
405. Prusiner SB, Cochran SP, Downey DE, Groth DF. Determination<br />
of scrapie agent titer from incubation period measurements in<br />
hamsters. Adv Exp Med Biol 134: 385–399, 1981.<br />
406. Prusiner SB, Cochran SP, Groth DF, Downey DE, Bowman<br />
KA, Martinez HM. Measurement of the scrapie agent using an<br />
incubation time interval assay. Ann Neurol 11: 353–358, 1982.<br />
407. Prusiner SB, Groth D, Serban A, Koehler R, Foster D, Torchia<br />
M, Burton D, Yang SL, DeArmond SJ. Ablation of the prion<br />
protein (PrP) gene in mice prevents scrapie <strong>and</strong> facilitates production<br />
of anti-PrP antibodies. Proc Natl Acad Sci USA 90: 10608–<br />
10612, 1993.<br />
408. Prusiner SB, Groth DF, Cochran SP, Masiarz FR, McKinley<br />
MP, Martinez HM. Molecular properties, partial purification, <strong>and</strong><br />
assay by incubation period measurements of the hamster scrapie<br />
agent. Biochemistry 19: 4883–4891, 1980.<br />
409. Prusiner SB, Groth DF, Cochran SP, McKinley MP, Masiarz<br />
FR. Gel electrophoresis <strong>and</strong> glass permeation chromatography of<br />
the hamster scrapie agent after enzymatic digestion <strong>and</strong> detergent<br />
extraction. Biochemistry 19: 4892–4898, 1980.<br />
410. Prusiner SB, McKinley MP, Bowman KA, Bolton DC, Bendheim<br />
PE, Groth DF, Glenner GG. Scrapie prions aggregate to<br />
form amyloid-like birefringent rods. Cell 35: 349–358, 1983.<br />
411. Prusiner SB, McKinley MP, Groth DF, Bowman KA, Mock NI,<br />
Cochran SP, Masiarz FR. Scrapie agent contains a hydrophobic<br />
protein. Proc Natl Acad Sci USA 78: 6675–6679, 1981.<br />
412. Prusiner SB, Scott M, Foster D, Pan KM, Groth D, Mirenda C,<br />
Torchia M, Yang SL, Serban D, Carlson GA, Hoppe PC, Westaway<br />
D, De Armond SJ. Transgenetic studies implicate interac-
1150 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
tions between homologous PrP isoforms in scrapie prion replication.<br />
Cell 63: 673–686, 1990.<br />
413. Puckett C, Concannon P, Casey C, Hood L. Genomic structure<br />
of the human prion protein gene. Am J Hum Genet 49: 320–329,<br />
1991.<br />
414. Radovanovic I, Braun N, Giger OT, Mertz K, Miele G, Prinz M,<br />
Navarro B, Aguzzi A. Truncated prion protein <strong>and</strong> Doppel are<br />
myelinotoxic in the absence of oligodendrocytic PrPC. J Neurosci<br />
25: 4879–4888, 2005.<br />
415. Raeber AJ, Klein MA, Frigg R, Flechsig E, Aguzzi A, Weissmann<br />
C. PrP-dependent association of prions with splenic but not<br />
circulating lymphocytes of scrapie-infected mice. EMBO J 18:<br />
2702–2706, 1999.<br />
416. Raeber AJ, Sailer A, Hegyi I, Klein MA, Rülicke T, Fischer M,<br />
Br<strong>and</strong>ner S, Aguzzi A, Weissmann C. Ectopic expression of<br />
prion protein (PrP) in T lymphocytes or hepatocytes of PrP knockout<br />
mice is insufficient to sustain prion replication. Proc Natl Acad<br />
Sci USA 96: 3987–3992, 1999.<br />
417. Rane NS, Kang SW, Chakrabarti O, Feigenbaum L, Hegde RS.<br />
Reduced translocation of nascent prion protein during ER stress<br />
contributes to neurodegeneration. Dev Cell 15: 359–370, 2008.<br />
418. Raymond CR, Aucouturier P, Mabbott NA. In vivo depletion of<br />
CD11c cells impairs scrapie agent neuroinvasion from the intestine.<br />
J Immunol 179: 7758–7766, 2007.<br />
419. Raymond GJ, Bossers A, Raymond LD, O’Rourke KI, Mc-<br />
Holl<strong>and</strong> LE, Bryant PK, Miller MW, Williams ES, Smits M,<br />
Caughey B. Evidence of a molecular barrier limiting susceptibility<br />
of humans, cattle <strong>and</strong> sheep to chronic wasting disease. EMBO J<br />
19: 4425–4430, 2000.<br />
420. Ren PH, Lauckner JE, Kachirskaia I, Heuser JE, Melki R,<br />
Kopito RR. Cytoplasmic penetration <strong>and</strong> persistent infection of<br />
mammalian cells by polyglutamine aggregates. Nat Cell Biol 11:<br />
219–225, 2009.<br />
421. Riek R, Hornemann S, Wider G, Billeter M, Glockshuber R,<br />
Wüthrich K. NMR structure of the mouse prion protein domain<br />
PrP(121-231). Nature 382: 180–182, 1996.<br />
422. Riek R, Hornemann S, Wider G, Glockshuber R, Wüthrich K.<br />
NMR characterization of the full-length recombinant murine prion<br />
protein, mPrP(23-231). FEBS Lett 413: 282–288, 1997.<br />
423. Riesner D. Transmissible spongiform encephalopathies: the prion<br />
theory–background <strong>and</strong> basic information. Contrib Microbiol 11:<br />
1–13, 2004.<br />
424. Riesner D, Kellings K, Wiese U, Wulfert M, Mirenda C,<br />
Prusiner SB. <strong>Prions</strong> <strong>and</strong> nucleic acids: search for “residual” nucleic<br />
acids <strong>and</strong> screening for mutations in the PrP-gene. Dev Biol<br />
St<strong>and</strong> 80: 173–181, 1993.<br />
425. Rivera-Milla E, Stuermer CA, Malaga-Trillo E. An evolutionary<br />
basis for scrapie disease: identification of a fish prion mRNA.<br />
Trends Genet 19: 72–75, 2003.<br />
426. Roberts GW, Lofthouse R, Allsop D, L<strong>and</strong>on M, Kidd M,<br />
Prusiner SB, Crow TJ. CNS amyloid proteins in neurodegenerative<br />
diseases. Neurology 38: 1534–1540, 1988.<br />
427. Rossi D, Cozzio A, Flechsig E, Klein MA, Rulicke T, Aguzzi A,<br />
Weissmann C. Onset of ataxia <strong>and</strong> Purkinje cell loss in PrP null<br />
mice inversely correlated with Dpl level in brain. EMBO J 20:<br />
694–702, 2001.<br />
428. Rudd PM, Endo T, Colominas C, Groth D, Wheeler SF, Harvey<br />
DJ, Wormald MR, Serban H, Prusiner SB, Kobata A, Dwek RA.<br />
Glycosylation differences between the normal <strong>and</strong> pathogenic<br />
prion protein isoforms. Proc Natl Acad Sci USA 96: 13044–13049,<br />
1999.<br />
429. Ruegger J, Stoeck K, Amsler L, Blaettler T, Zwahlen M,<br />
Aguzzi A, Glatzel M, Hess K, Eckert T. A case-control study of<br />
sporadic Creutzfeldt-Jakob disease in Switzerl<strong>and</strong>: analysis of potential<br />
risk factors with regard to an increased CJD incidence in the<br />
years 2001–2004. BMC Public Health 9: 18, 2009.<br />
430. Russell DG. Who puts the tubercle in tuberculosis? Nat Rev Microbiol<br />
5: 39–47, 2007.<br />
431. Rutishauser D, Mertz KD, Moos R, Brunner E, Rulicke T,<br />
Calella AM, Aguzzi A. The comprehensive native interactome of<br />
a fully functional tagged prion protein. PLoS ONE 4: e4446, 2009.<br />
432. Saa P, Castilla J, Soto C. Presymptomatic detection of prions in<br />
blood. Science 313: 92–94, 2006.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
433. Saa P, Castilla J, Soto C. Ultra-efficient replication of infectious<br />
prions by automated protein misfolding cyclic amplification. J Biol<br />
Chem 281: 35245–35252, 2006.<br />
434. Saborio GP, Permanne B, Soto C. Sensitive detection of pathological<br />
prion protein by cyclic amplification of protein misfolding.<br />
Nature 411: 810–813, 2001.<br />
435. Safar J, Roller PP, Gajdusek DC, Gibbs CJ Jr. Conformational<br />
transitions, dissociation, unfolding of scrapie amyloid (prion) protein.<br />
J Biol Chem 268: 20276–20284, 1993.<br />
436. Safar J, Roller PP, Gajdusek DC, Gibbs CJ Jr. Thermal stability<br />
<strong>and</strong> conformational transitions of scrapie amyloid (prion) protein<br />
correlate with infectivity. <strong>Protein</strong> Sci 2: 2206–2216, 1993.<br />
437. Safar J, Wille H, Itri V, Groth D, Serban H, Torchia M, Cohen<br />
F, Prusiner S. Eight prion strains have PrP Sc molecules with<br />
different conformations. Nat Med 4: 1157–1165, 1998.<br />
438. Safar J, Wille H, Itri V, Groth D, Serban H, Torchia M, Cohen<br />
FE, Prusiner SB. Eight prion strains have PrP(Sc) molecules with<br />
different conformations. Nat Med 4: 1157–1165, 1998.<br />
439. Sailer A, Büeler H, Fischer M, Aguzzi A, Weissmann C. No<br />
propagation of prions in mice devoid of PrP. Cell 77: 967–968, 1994.<br />
440. Sakaguchi S, Katamine S, Nishida N, Moriuchi R, Shigematsu<br />
K, Sugimoto T, Nakatani A, Kataoka Y, Houtani T, Shirabe S,<br />
Okada H, Hasegawa S, Miyamoto T, Noda T. Loss of cerebellar<br />
Purkinje cells in aged mice homozygous for a disrupted PrP gene.<br />
Nature 380: 528–531, 1996.<br />
441. Sakudo A, Lee DC, Saeki K, Nakamura Y, Inoue K, Matsumoto<br />
Y, Itohara S, Onodera T. Impairment of superoxide dismutase<br />
activation by N-terminally truncated prion protein (PrP) in PrPdeficient<br />
neuronal cell line. Biochem Biophys Res Commun 308:<br />
660–667, 2003.<br />
442. Sanchez-Juan P, Green A, Ladogana A, Cuadrado-Corrales N,<br />
Sánchez-Valle R, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki<br />
J, Hess K, Bodemer M, Slivarichová D, Saiz A, Calero M,<br />
Ingrosso L, Knight R, Janssens ACJW, van Duijn C, Zerr I.<br />
CSF tests in the differential diagnosis of Creutzfeldt-Jakob disease.<br />
Neurology 67: 637–643, 2006.<br />
443. Schreuder BE, Vankeulen LJ, Vromans ME, Langeveld JP,<br />
Smits MA. Preclinical test for prion diseases. Nature 381: 563,<br />
1996.<br />
444. Scoazec JY, Krolak-Salmon P, Casez O, Besson G, Thobois S,<br />
Kopp N, Perret-Liaudet A, Streichenberger N. Quinacrine-induced<br />
cytolytic hepatitis in sporadic Creutzfeldt-Jakob disease.<br />
Ann Neurol 53: 546–547, 2003.<br />
445. Scott JR, Foster JD, Fraser H. Conjunctival instillation of<br />
scrapie in mice can produce disease. Vet Microbiol 34: 305–309,<br />
1993.<br />
446. Scott M, Foster D, Mirenda C, Serban D, Coufal F, Waelchli<br />
M, Torchia M, Groth D, Carlson G, DeArmond SJ, Westaway<br />
D, Prusiner SB. Transgenic mice expressing hamster prion protein<br />
produce species-specific scrapie infectivity <strong>and</strong> amyloid<br />
plaques. Cell 59: 847–857, 1989.<br />
447. Scott M, Groth D, Foster D, Torchia M, Yang SL, DeArmond<br />
SJ, Prusiner SB. Propagation of prions with artificial properties in<br />
transgenic mice expressing chimeric PrP genes. Cell 73: 979–988,<br />
1993.<br />
448. Seeger H, Heikenwalder M, Zeller N, Kranich J, Schwarz P,<br />
Gaspert A, Seifert B, Miele G, Aguzzi A. Coincident scrapie<br />
infection <strong>and</strong> nephritis lead to urinary prion excretion. Science 310:<br />
324–326, 2005.<br />
449. Sekercioglu CH. Prion diseases <strong>and</strong> a penchant for brains. Science<br />
305: 342–343, 2004.<br />
450. Sethi S, Lipford G, Wagner H, Kretzschmar H. Postexposure<br />
prophylaxis against prion disease with a stimulator of innate immunity.<br />
Lancet 360: 229–230, 2002.<br />
451. Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson<br />
NE, Smith I, Brett FM, Farrell MA, Rowan MJ, Lemere CA,<br />
Regan CM, Walsh DM, Sabatini BL, Selkoe DJ. Amyloid-beta<br />
protein dimers isolated directly from Alzheimer’s brains impair<br />
synaptic plasticity <strong>and</strong> memory. Nat Med 14: 837–842, 2008.<br />
452. Shlomchik MJ, Radebold K, Duclos N, Manuelidis L. Neuroinvasion<br />
by a Creutzfeldt-Jakob disease agent in the absence of B<br />
cells <strong>and</strong> follicular dendritic cells. Proc Natl Acad Sci USA 98:<br />
9289–9294, 2001.
453. Shmerling D, Hegyi I, Fischer M, Blattler T, Br<strong>and</strong>ner S, Gotz<br />
J, Rulicke T, Flechsig E, Cozzio A, von Mering C, Hangartner<br />
C, Aguzzi A, Weissmann C. Expression of amino-terminally truncated<br />
PrP in the mouse leading to ataxia <strong>and</strong> specific cerebellar<br />
lesions. Cell 93: 203–214, 1998.<br />
454. Shorter J, Lindquist S. Hsp104 catalyzes formation <strong>and</strong> elimination<br />
of self-replicating Sup35 prion conformers. Science 304: 1793–<br />
1797, 2004.<br />
455. Shorter J, Lindquist S. <strong>Prions</strong> as adaptive conduits of memory<br />
<strong>and</strong> inheritance. Nat Rev Genet 6: 435–450, 2005.<br />
456. Shyng SL, Heuser JE, Harris DA. A glycolipid-anchored prion<br />
protein is endocytosed via clathrin-coated pits. J Cell Biol 125:<br />
1239–1250, 1994.<br />
457. Si K, Lindquist S, K<strong>and</strong>el ER. A neuronal isoform of the Aplysia<br />
CPEB has prion-like properties. Cell 115: 879–891, 2003.<br />
458. Sigurdson CJ. A prion disease of cervids: chronic wasting disease.<br />
Vet Res 39: 41, 2008.<br />
459. Sigurdson CJ, Heikenwalder M, Manco G, Barthel M, Schwarz<br />
P, Stecher B, Krautler NJ, Hardt WD, Seifert B, Macpherson<br />
AJ, Corthesy I, Aguzzi A. Bacterial colitis increases susceptibility<br />
to oral prion disease. J Infect Dis 199: 243–252, 2008.<br />
460. Sigurdson CJ, Manco G, Schwarz P, Liberski P, Hoover EA,<br />
Hornemann S, Polymenidou M, Miller MW, Glatzel M, Aguzzi<br />
A. Strain fidelity of chronic wasting disease upon murine adaptation.<br />
J Virol 80: 12303–12311, 2006.<br />
461. Sigurdson CJ, Nilsson KP, Hornemann S, Heikenwalder M,<br />
Manco G, Schwarz P, Ott D, Rulicke T, Liberski PP, Julius C,<br />
Falsig J, Stitz L, Wuthrich K, Aguzzi A. De novo generation of<br />
a transmissible spongiform encephalopathy by mouse transgenesis.<br />
Proc Natl Acad Sci USA 106: 304–309, 2009.<br />
462. Sigurdson CJ, Nilsson KP, Hornemann S, Manco G, Polymenidou<br />
M, Schwarz P, Leclerc M, Hammarstrom P, Wuthrich<br />
K, Aguzzi A. Prion strain discrimination using luminescent conjugated<br />
polymers. Nat Methods 4: 1023–1030, 2007.<br />
463. Sigurdsson EM, Brown DR, Daniels M, Kascsak RJ, Kascsak<br />
R, Carp R, Meeker HC, Frangione B, Wisniewski T. Immunization<br />
delays the onset of prion disease in mice. Am J Pathol 161:<br />
13–17, 2002.<br />
464. Silveira JR, Raymond GJ, Hughson AG, Race RE, Sim VL,<br />
Hayes SF, Caughey B. The most infectious prion protein particles.<br />
Nature 437: 257–261, 2005.<br />
465. Silverman GL, Qin K, Moore RC, Yang Y, Mastrangelo P,<br />
Tremblay P, Prusiner SB, Cohen FE, Westaway D. Doppel is an<br />
N-glycosylated, glycosylphosphatidylinositol-anchored protein. Expression<br />
in testis <strong>and</strong> ectopic production in the brains of Prnp(0/0)<br />
mice predisposed to Purkinje cell loss. J Biol Chem 275: 26834–<br />
26841, 2000.<br />
466. Sirangelo I, Malmo C, Iannuzzi C, Mezzogiorno A, Bianco MR,<br />
Papa M, Irace G. Fibrillogenesis <strong>and</strong> cytotoxic activity of the<br />
amyloid-forming apomyoglobin mutant W7FW14F. J Biol Chem<br />
279: 13183–13189, 2004.<br />
467. Sluzky V, Tamada J, Klibanov A, Langer R. Kinetics of insulin<br />
aggregation in aqueous solutions upon agitation in the presence of<br />
hydrophobic surfaces. Proc Natl Acad Sci USA 88: 9377–9381, 1991.<br />
468. Soldevila M, Andres AM, Ramirez-Soriano A, Marques-Bonet<br />
T, Calafell F, Navarro A, Bertranpetit J. The prion protein gene<br />
in humans revisited: lessons from a worldwide resequencing study.<br />
Genome Res 16: 231–239, 2006.<br />
469. Solforosi L, Criado JR, McGavern DB, Wirz S, Sanchez-Alavez<br />
M, Sugama S, DeGiorgio LA, Volpe BT, Wiseman E, Abalos G,<br />
Masliah E, Gilden D, Oldstone MB, Conti B, Williamson RA.<br />
Cross-linking cellular prion protein triggers neuronal apoptosis in<br />
vivo. Science 303: 1514–1516, 2004.<br />
470. Sorgjerd K, Klingstedt T, Lindgren M, Kagedal K, Hammarstrom<br />
P. Prefibrillar transthyretin oligomers <strong>and</strong> cold stored<br />
native tetrameric transthyretin are cytotoxic in cell culture. Biochem<br />
Biophys Res Commun 377: 1072–1078, 2008.<br />
471. Soto C. Constraining the loop, releasing prion infectivity. Proc Natl<br />
Acad Sci USA 106: 10–11, 2009.<br />
472. Soto C. Endoplasmic reticulum stress, PrP trafficking, <strong>and</strong> neurodegeneration.<br />
Dev Cell 15: 339–341, 2008.<br />
473. Soto C, Anderes L, Suardi S, Cardone F, Castilla J, Frossard<br />
MJ, Peano S, Saa P, Limido L, Carbonatto M, Ironside J,<br />
AGGREGATION AND INFECTIOUS DISEASE 1151<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
Torres JM, Pocchiari M, Tagliavini F. Pre-symptomatic detection<br />
of prions by cyclic amplification of protein misfolding. FEBS<br />
Lett 579: 638–642, 2005.<br />
474. Soto C, Estrada L, Castilla J. Amyloids, prions <strong>and</strong> the inherent<br />
infectious nature of misfolded protein aggregates. Trends Biochem<br />
Sci 31: 150–155, 2006.<br />
475. Soto C, Kascsak RJ, Saborio GP, Aucouturier P, Wisniewski<br />
T, Prelli F, Kascsak R, Mendez E, Harris DA, Ironside J,<br />
Tagliavini F, Carp RI, Frangione B. Reversion of prion protein<br />
conformational changes by synthetic beta-sheet breaker peptides.<br />
Lancet 355: 192–197, 2000.<br />
476. Souan L, Tal Y, Felling Y, Cohen IR, Taraboulos A, Mor F.<br />
Modulation of proteinase-K resistant prion protein by prion peptide<br />
immunization. Eur J Immunol 31: 2338–2346, 2001.<br />
477. Sousa MM, Cardoso I, Fern<strong>and</strong>es R, Guimaraes A, Saraiva<br />
MJ. Deposition of transthyretin in early stages of familial amyloidotic<br />
polyneuropathy: evidence for toxicity of nonfibrillar aggregates.<br />
Am J Pathol 159: 1993–2000, 2001.<br />
478. Sparkes RS, Simon M, Cohn VH, Fournier RE, Lem J, Klisak<br />
I, Heinzmann C, Blatt C, Lucero M, Moh<strong>and</strong>as T. Assignment of<br />
the human <strong>and</strong> mouse prion protein genes to homologous chromosomes.<br />
Proc Natl Acad Sci USA 83: 7358–7362, 1986.<br />
479. Sparkes RS, Simon M, Cohn VH, Fournier RE, Lem J, Klisak<br />
I, Heinzmann C, Blatt C, Lucero M, Moh<strong>and</strong>as T. Assignment of<br />
the human <strong>and</strong> mouse prion protein genes to homologous chromosomes.<br />
Proc Natl Acad Sci USA 83: 7358–7362, 1986.<br />
480. Stahl N, Baldwin MA, Teplow DB, Hood L, Gibson BW, Burlingame<br />
AL, Prusiner SB. Structural studies of the scrapie prion<br />
protein using mass spectrometry <strong>and</strong> amino acid sequencing. Biochemistry<br />
32: 1991–2002, 1993.<br />
481. Stahl N, Borchelt DR, Hsiao K, Prusiner SB. Scrapie prion<br />
protein contains a phosphatidylinositol glycolipid. Cell 51: 229–240,<br />
1987.<br />
482. Strumbo B, Ronchi S, Bolis LC, Simonic T. Molecular cloning of<br />
the cDNA coding for Xenopus laevis prion protein. FEBS Lett 508:<br />
170–174, 2001.<br />
483. Supattapone S, Bosque P, Muramoto T, Wille H, Aagaard C,<br />
Peretz D, Nguyen HO, Heinrich C, Torchia M, Safar J, Cohen<br />
FE, DeArmond SJ, Prusiner SB, Scott M. Prion protein of 106<br />
residues creates an artifical transmission barrier for prion replication<br />
in transgenic mice. Cell 96: 869–878, 1999.<br />
484. Supattapone S, Bouzamondo E, Ball HL, Wille H, Nguyen HO,<br />
Cohen FE, DeArmond SJ, Prusiner SB, Scott M. A proteaseresistant<br />
61-residue prion peptide causes neurodegeneration in<br />
transgenic mice. Mol Cell Biol 21: 2608–2616, 2001.<br />
485. Supattapone S, Wille H, Uyechi L, Safar J, Tremblay P, Szoka<br />
FC, Cohen FE, Prusiner SB, Scott MR. Branched polyamines<br />
cure prion-infected neuroblastoma cells. J Virol 75: 3453–3461,<br />
2001.<br />
486. Szakal AK, Kapasi ZF, Haley ST, Tew JG. Multiple lines of<br />
evidence favoring a bone marrow derivation of follicular dendritic<br />
cells (FDCs). Adv Exp Med Biol 378: 267–272, 1995.<br />
487. Tagliavini F, McArthur RA, Canciani B, Giaccone G, Porro M,<br />
Bugiani M, Lievens PM, Bugiani O, Peri E, Dall’Ara P, Rocchi<br />
M, Poli G, Forloni G, B<strong>and</strong>iera T, Varasi M, Suarato A, Cassutti<br />
P, Cervini MA, Lansen J, Salmona M, Post C. Effectiveness<br />
of anthracycline against experimental prion disease in Syrian<br />
hamsters. Science 276: 1119–1122, 1997.<br />
488. Tagliavini F, Prelli F, Ghiso J, Bugiani O, Serban D, Prusiner<br />
SB, Farlow MR, Ghetti B, Frangione B. Amyloid protein of<br />
Gerstmann-Straussler-Scheinker disease (Indiana kindred) is an 11<br />
kd fragment of prion protein with an N-terminal glycine at codon<br />
58. EMBO J 10: 513–519, 1991.<br />
489. Takemura S, Braun A, Crowson C, Kurtin PJ, Cofield RH,<br />
O’Fallon WM, Goronzy JJ, Wey<strong>and</strong> CM. Lymphoid neogenesis<br />
in rheumatoid synovitis. J Immunol 167: 1072–1080, 2001.<br />
490. Tamguney G, Giles K, Bouzamondo-Bernstein E, Bosque PJ,<br />
Miller MW, Safar J, Dearmond SJ, Prusiner SB. Transmission<br />
of elk <strong>and</strong> deer prions to transgenic mice. J Virol 80: 9104–9114,<br />
2006.<br />
491. Tanaka M, Chien P, Naber N, Cooke R, Weissman JS. Conformational<br />
variations in an infectious protein determine prion strain<br />
differences. Nature 428: 323–328, 2004.
1152 ADRIANO AGUZZI AND ANNA MARIA CALELLA<br />
492. Tanaka M, Collins SR, Toyama BH, Weissman JS. The physical<br />
basis of how prion conformations determine strain phenotypes.<br />
Nature 442: 585–589, 2006.<br />
493. Taraboulos A, Jendroska K, Serban D, Yang SL, DeArmond<br />
SJ, Prusiner SB. Regional mapping of prion proteins in brain.<br />
Proc Natl Acad Sci USA 89: 7620–7624, 1992.<br />
494. Taraboulos A, Raeber AJ, Borchelt DR, Serban D, Prusiner<br />
SB. Synthesis <strong>and</strong> trafficking of prion proteins in cultured cells.<br />
Mol Biol Cell 3: 851–863, 1992.<br />
495. Taraboulos A, Scott M, Semenov A, Avraham D, Laszlo L,<br />
Prusiner SB. Cholesterol depletion <strong>and</strong> modification of COOHterminal<br />
targeting sequence of the prion protein inhibit formation<br />
of the scrapie isoform. J Cell Biol 129: 121–132, 1995.<br />
496. Tateishi J, Doh-ura K. Prion protein gene analysis <strong>and</strong> transmission<br />
studies of Creutzfeldt-Jakob disease. In: Prion <strong>Diseases</strong> of<br />
Humans <strong>and</strong> Animals, edited by Prusiner SB, Collinge J. London:<br />
Horwood, 1992, p. 129–134.<br />
497. Taylor DM, McConnell I, Fraser H. Scrapie infection can be<br />
established readily through skin scarification in immunocompetent<br />
but not immunodeficient mice. J Gen Virol 77 1595–1599, 1996.<br />
498. Tobler I, Gaus SE, Deboer T, Achermann P, Fischer M,<br />
Rülicke T, Moser M, Oesch B, McBride PA, Manson JC. Altered<br />
circadian activity rhythms <strong>and</strong> sleep in mice devoid of prion protein.<br />
Nature 380: 639–642, 1996.<br />
499. Toyama BH, Kelly MJ, Gross JD, Weissman JS. The structural<br />
basis of yeast prion strain variants. Nature 449: 233–237, 2007.<br />
500. Trifilo MJ, Yajima T, Gu Y, Dalton N, Peterson KL, Race RE,<br />
Meade-White K, Portis JL, Masliah E, Knowlton KU, Chesebro<br />
B, Oldstone MB. Prion-induced amyloid heart disease with<br />
high blood infectivity in transgenic mice. Science 313: 94–97, 2006.<br />
501. Tuzi NL, Cancellotti E, Baybutt H, Blackford L, Bradford B,<br />
Plinston C, Coghill A, Hart P, Piccardo P, Barron RM, Manson<br />
JC. Host PrP glycosylation: a major factor determining the outcome<br />
of prion infection. PLoS Biol 6: e100, 2008.<br />
502. Vernau W, Jacobs RM, Valli VE, Heeney JL. The immunophenotypic<br />
characterization of bovine lymphomas. Vet Pathol 34: 222–<br />
225, 1997.<br />
503. Vnencak Jones CL, Phillips JAD. Identification of heterogeneous<br />
PrP gene deletions in controls by detection of allele-specific<br />
heteroduplexes (DASH). Am J Hum Genet 50: 871–872, 1992.<br />
504. Wadsworth JD, Asante EA, Desbruslais M, Linehan JM,<br />
Joiner S, Gowl<strong>and</strong> I, Welch J, Stone L, Lloyd SE, Hill AF,<br />
Br<strong>and</strong>ner S, Collinge J. Human prion protein with valine 129<br />
prevents expression of variant CJD phenotype. Science 306: 1793–<br />
1796, 2004.<br />
505. Wadsworth JD, Hill AF, Joiner S, Jackson GS, Clarke AR,<br />
Collinge J. Strain-specific prion-protein conformation determined<br />
by metal ions. Nat Cell Biol 1: 55–59, 1999.<br />
506. Waggoner DJ, Drisaldi B, Bartnikas TB, Casareno RL, Prohaska<br />
JR, Gitlin JD, Harris DA. Brain copper content <strong>and</strong> cuproenzyme<br />
activity do not vary with prion protein expression level.<br />
J Biol Chem 275: 7455–7458, 2000.<br />
507. Wagner N, Lohler J, Kunkel EJ, Ley K, Leung E, Krissansen<br />
G, Rajewsky K, Muller W. Critical role for beta7 integrins in<br />
formation of the gut-associated lymphoid tissue. Nature 382: 366–<br />
370, 1996.<br />
508. Ware CF, VanArsdale TL, Crowe PD, Browning JL. The lig<strong>and</strong>s<br />
<strong>and</strong> receptors of the lymphotoxin system. Curr Top Microbiol<br />
Immunol 198: 175–218, 1995.<br />
509. Wasmer C, Lange A, Van Melckebeke H, Siemer A, Riek R,<br />
Meier B. Amyloid fibrils of the HET-s(218–289) prion form a beta<br />
solenoid with a triangular hydrophobic core. Science 319: 1523–<br />
1526., 2008.<br />
510. Weissmann C. Birth of a prion: spontaneous generation revisited.<br />
Cell 122: 165–168, 2005.<br />
511. Weissmann C. Spongiform encephalopathies. The prion’s<br />
progress. Nature 349: 569–571, 1991.<br />
512. Weissmann C. A “unified theory” of prion propagation. Nature<br />
352: 679–683, 1991.<br />
513. Weissmann C, Aguzzi A. Perspectives: neurobiology. PrP’s double<br />
causes trouble. Science 286: 914–915, 1999.<br />
Physiol Rev VOL 89 OCTOBER 2009 www.prv.org<br />
514. Wells GA, Scott AC, Johnson CT, Gunning RF, Hancock RD,<br />
Jeffrey M, Dawson M, Bradley R. A novel progressive spongiform<br />
encephalopathy in cattle. Vet Rec 121: 419–420, 1987.<br />
515. Westaway D, Goodman PA, Mirenda CA, McKinley MP, Carlson<br />
GA, Prusiner SB, et al. Distinct prion proteins in short <strong>and</strong><br />
long scrapie incubation period mice. Cell 51: 651–662, 1987.<br />
516. Westaway D, Mirenda CA, Foster D, Zebarjadian Y, Scott M,<br />
Torchia M, Yang SL, Serban H, DeArmond SJ, Ebeling C.<br />
Paradoxical shortening of scrapie incubation times by expression<br />
of prion protein transgenes derived from long incubation period<br />
mice. Neuron 7: 59–68, 1991.<br />
517. Westermark P, Sletten K, Johansson B, Cornwell GG 3rd.<br />
Fibril in senile systemic amyloidosis is derived from normal transthyretin.<br />
Proc Natl Acad Sci USA 87: 2843–2845, 1990.<br />
518. White AR, Enever P, Tayebi M, Mushens R, Linehan J, Br<strong>and</strong>ner<br />
S, Anstee D, Collinge J, Hawke S. Monoclonal antibodies<br />
inhibit prion replication <strong>and</strong> delay the development of prion disease.<br />
Nature 422: 80–83, 2003.<br />
519. White MD, Farmer M, Mirabile I, Br<strong>and</strong>ner S, Collinge J,<br />
Mallucci GR. Single treatment with RNAi against prion protein<br />
rescues early neuronal dysfunction <strong>and</strong> prolongs survival in mice<br />
with prion disease. Proc Natl Acad Sci USA 105: 10238–10243,<br />
2008.<br />
520. Whittington MA, Sidle KC, Gowl<strong>and</strong> I, Meads J, Hill AF,<br />
Palmer MS, Jefferys JG, Collinge J. Rescue of neurophysiological<br />
phenotype seen in PrP null mice by transgene encoding human<br />
prion protein. Nat Genet 9: 197–201, 1995.<br />
521. Wilesmith JW, Ryan JB, Hueston WD, Hoinville LJ. Bovine<br />
spongiform encephalopathy: epidemiological features 1985 to 1990.<br />
Vet Rec 130: 90–94, 1992.<br />
522. Will R, Zeidler M. Diagnosing Creutzfeldt-Jakob disease. BMJ 313:<br />
833–834, 1996.<br />
523. Will RG, Ironside JW, Zeidler M, Cousens SN, Estibeiro K,<br />
Alperovitch A, Poser S, Pocchiari M, Hofman A, Smith PG. A<br />
new variant of Creutzfeldt-Jakob disease in the UK. Lancet 347:<br />
921–925, 1996.<br />
524. Wille H, Michelitsch MD, Guenebaut V, Supattapone S, Serban<br />
A, Cohen FE, Agard DA, Prusiner SB. Structural studies of<br />
the scrapie prion protein by electron crystallography. Proc Natl<br />
Acad Sci USA 99: 3563–3568, 2002.<br />
525. Williams ES, Young S. Chronic wasting disease of captive mule<br />
deer: a spongiform encephalopathy. J Wildl Dis 16: 89–98, 1980.<br />
526. Williams RC. Electron microscopy of viruses. Adv Virus Res 2:<br />
183–239, 1954.<br />
527. Wilson DR, Anderson RD, Smith W. Studies in Scrapie. J Comp<br />
Pathol 60: 267–282, 1950.<br />
528. Wroe SJ, Pal S, Siddique D, Hyare H, Macfarlane R, Joiner S,<br />
Linehan JM, Br<strong>and</strong>ner S, Wadsworth JD, Hewitt P, Collinge<br />
J. Clinical presentation <strong>and</strong> pre-mortem diagnosis of variant<br />
Creutzfeldt-Jakob disease associated with blood transfusion: a case<br />
report. Lancet 368: 2061–2067, 2006.<br />
529. Yedidia Y, Horonchik L, Tzaban S, Yanai A, Taraboulos A.<br />
Proteasomes <strong>and</strong> ubiquitin are involved in the turnover of the<br />
wild-type prion protein. EMBO J 20: 5383–5391, 2001.<br />
530. Zabel MD, Heikenwalder M, Prinz M, Arrighi I, Schwarz P,<br />
Kranich J, von Teichman A, Haas KM, Zeller N, Tedder TF,<br />
Weis JH, Aguzzi A. Stromal complement receptor CD21/35 facilitates<br />
lymphoid prion colonization <strong>and</strong> pathogenesis. J Immunol<br />
179: 6144–6152, 2007.<br />
531. Zahn R, Liu A, Luhrs T, Riek R, von Schroetter C, Lopez<br />
Garcia F, Billeter M, Calzolai L, Wider G, Wuthrich K. NMR<br />
solution structure of the human prion protein. Proc Natl Acad Sci<br />
USA 97: 145–150, 2000.<br />
532. Zanusso G, Ferrari S, Cardone F, Zampieri P, Gelati M,<br />
Fiorini M, Farinazzo A, Gardiman M, Cavallaro T, Bentivoglio<br />
M, Righetti PG, Pocchiari M, Rizzuto N, Monaco S.<br />
Detection of pathologic prion protein in the olfactory epithelium<br />
in sporadic Creutzfeldt-Jakob disease. N Engl J Med 348: 711–<br />
719, 2003.<br />
533. Zhang B, Une Y, Fu X, Yan J, Ge F, Yao J, Sawashita J, Mori<br />
M, Tomozawa H, Kametani F, Higuchi K. Fecal transmission of<br />
AA amyloidosis in the cheetah contributes to high incidence of<br />
disease. Proc Natl Acad Sci USA 105: 7263–7268, 2008.