THE DILATED URETER - OU Medicine
THE DILATED URETER - OU Medicine
THE DILATED URETER - OU Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>THE</strong> <strong>DILATED</strong> <strong>URETER</strong><br />
FREE CME ONLINE<br />
FREE CME ONLINE<br />
To earn CME credit for this activity, participants should read<br />
the article and log onto www.contemporaryurology.com,<br />
where they must pass a post-test. After completing the test<br />
and online evaluation, a CME letter will be emailed to them.<br />
The release date for this activity is June 1, 2006. The<br />
expiration date is June 1, 2007.<br />
Accreditation<br />
This activity has been planned and implemented in<br />
accordance with the Essential Areas and policies of the<br />
Accreditation Council for Continuing Medical Education<br />
(ACCME) through the joint sponsorship of Thomson<br />
American Health Consultants (AHC) and Contemporary<br />
Urology. AHC is accredited by the ACCME to provide<br />
continuing medical education for physicians.<br />
AHC designates this educational activity for a maximum<br />
of 1 AMA PRA Category 1 Credit(s). Physicians should<br />
only claim credit commensurate with the extent of their<br />
participation in the activity.<br />
Target audience<br />
This activity is designated for urologists.<br />
Educational objectives<br />
After completing the following CME activity, the reader<br />
should be able to:<br />
• Outline the basic embryologic development of the ureter.<br />
• Classify the adult and pediatric patient with a megaureter<br />
based on the etiology of the condition.<br />
• Utilize imaging and clinical signs and symptoms to<br />
identify patients with primary obsructed megaureter who<br />
may be candidates for surveillance.<br />
• List 3 indications that should prompt consideration of<br />
repair of the primary obstructed megaureter.<br />
Faculty disclosures<br />
The authors (Stephen D. Confer, MD, Dominic Frimberger,<br />
MD, and Bradley P. Kropp, MD), reviewers of CME content<br />
(Culley C. Carson, MD and Stephen E. Strup, MD) and staff<br />
editors (Nancy Lucas, Editor and Beverly Lucas, Senior<br />
Editor) report no relationships with companies having ties to<br />
this field of study.<br />
44 CONTEMPORARY UROLOGY JUNE 2006<br />
By Stephen D. Confer, MD, Dominic Frimberger, MD, and Bradley P. Kropp, MD<br />
While dilated ureters are usually identified<br />
in adults when they present with symptomatic<br />
complaints, in children, identification<br />
is most likely due to aggressive screening<br />
with perinatal ultrasonography (US). Urologists who primarily<br />
treat adults should be familiar with the principles of evaluation<br />
and management options for adult, pediatric, and fetal populations<br />
as they may be asked to consult on a newborn or fetus with<br />
a dilated ureter. See “Embryology,” page 45, for a brief review of<br />
ureteral development.<br />
A variety of terms have been applied to ureters of abnormal<br />
caliber, including megaloureter, megaureter, dilatation of the<br />
ureter, and widened ureter. King has suggested the term megaureter<br />
to describe any ureter that is found to be dilated. 1 This<br />
broad term is defined further by 3 etiologic categories: obstructed<br />
megaureter, refluxing megaureter, and nonrefluxing nonobstructed<br />
megaureter (Table 1). Each category is further classified into<br />
primary and secondary subgroupings. This article focuses on diagnosis<br />
and management of primary obstructed megaureter.<br />
ETIOLOGY AND PRESENTATION<br />
Primary obstructed megaureter occurs in both pediatric and<br />
adult populations. 2 Rather than being caused by a lumenal obstruction,<br />
the condition is due to an intrinsic abnormality or an<br />
adynamic segment of the distal ureter that leads to a functional<br />
obstruction. In the past, the functional obstruction was thought<br />
to be similar to that seen in Hirschsprung’s disease of the colon.<br />
However, this has been disproven as excised samples demonstrated<br />
the presence of neural plexuses. 3,4<br />
Approximately two thirds of reported patients are males;<br />
however, 1 series displayed a female predominance. 5 The abnormality<br />
is unilateral in approximately two thirds of cases. 5 The<br />
Dr. Confer is a Resident in Urology; Dr. Frimberger is Assistant<br />
Professor, Section of Pediatric Urology; and Dr. Kropp is Professor<br />
and Chief of Pediatric Urology, Section of Urology, and Vice<br />
Chairman of the Department of Urology; University of Oklahoma<br />
Health Sciences Center, Oklahoma City.
WHAT EVERY UROLOGIST SH<strong>OU</strong>LD KNOW<br />
The most important aspect in the management of the dilated ureter in adults and<br />
children is identification of patients who will need and benefit from surgical repair.<br />
presence of other anomalies, such as contralateral ureteropelvic<br />
junction (UPJ) obstruction, renal agenesis or ectopia, and<br />
ureteral duplication associated with primary obstructed megaureters,<br />
may be seen in up to 40% of affected patients. 5<br />
In adults, primary obstructed megaureter is usually detected<br />
when patients present with pain or other symptoms from urinary<br />
tract infection (UTI), calculi, or decreased renal function. 2<br />
In mild cases, however, patients are typically asymptomatic, and<br />
the condition is found during an unrelated workup.<br />
In the pediatric population, routine perinatal US has dramatically<br />
increased the likelihood of detection of the dilated<br />
ureter. 6 The megaureter can be dilated up to 3 cm and thus is<br />
easily identified on US as a hypoechoic cystic-appearing mass in<br />
the retroperitoneum that may extend from the UPJ to the<br />
ureterovesical junction (UVJ). 7 In a 5-year series in which US<br />
was performed on 3,856 fetuses after 28 weeks of gestation, the<br />
prevalence of primary megaureter at the level of the UVJ was<br />
approximately 1 in 2,000. 8<br />
GRADING<br />
Several different grading systems have been promulgated, but<br />
none is useful in predicting which patients will require surgery<br />
and which will benefit from observation. The earliest classification<br />
system, devised in 1978 by Pfister and Hendren, categorizes<br />
Embryology<br />
T<br />
he development of the ureter begins around the fifth<br />
week of gestation. A diverticulum arises from the<br />
posteriomedial aspect of the lower portion of the bilateral<br />
mesonephric ducts. It then elongates posteriorly to meet the<br />
metanephric blastema, thus inducing nephrogenesis. The tip<br />
of the ureteric bud dilates to form the collecting system from<br />
the ureterovesical junction (UVJ ) to the level of the<br />
collecting duct. During the sixth through the ninth weeks,<br />
the embryonic kidney ascends from its pelvic position.<br />
During the ascent of the kidneys, the ureters elongate.<br />
The lumen of the forming ureter develops from the<br />
midureter cranially and caudally until the eighth week.<br />
The urogenital sinus remains separated from the ureteric<br />
UROlogic<br />
➤ Primary obstructed megaureter is<br />
caused by an intrinsic abnormality<br />
or an adynamic segment of the<br />
distal ureter that leads to a<br />
functional obstruction.<br />
➤ While adults typically present with<br />
hematuria or symptomatic<br />
complaints from UTI or stone<br />
disease, most cases in children are<br />
detected antenatally.<br />
lumen by a membrane. This membrane, known as the<br />
Chwalle’s membrane, disappears by the middle of<br />
the eighth week. At approximately the ninth week of<br />
gestation, muscularization is induced by the passing of<br />
the first excreted urine. At 18 weeks, normal physiologic<br />
narrowing can be discerned at the ureteropelvic junction<br />
(UPJ) and the UVJ. It is at this time that dilation of the<br />
ureter may be observed. After 19 weeks, the ureter<br />
continues to grow; however, the normal ureteral<br />
diameter in the fetal population rarely exceeds 5 mm. 1<br />
REFERENCE<br />
1. Cussen LJ. The morphology of congenital dilatation of the ureter: intrinsic lesions.<br />
Aust NZ J Surg. 1971;441:185-194.<br />
JUNE 2006 CONTEMPORARY UROLOGY 45
PRIMARY OBSTRUCTED MEGA<strong>URETER</strong><br />
TABLE 1<br />
Differential diagnosis of megaureter<br />
OBSTRUCTED MEGA<strong>URETER</strong><br />
Primary: This condition is due to an intrinsic abnormality or an adynamic<br />
segment of the distal ureter that leads to a functional obstruction.<br />
Secondary: Any cause of ureteral obstruction not due to an adynamic<br />
segment. Etiologies include congenital lesions (ureteropelvic junction<br />
obstruction, ectopic ureterocele), inflammatory conditions (tuberculosis,<br />
schistosomiasis, Crohn’s disease, pelvic inflammatory disease, pelvic<br />
abscess), trauma, tumors, lower urinary tract conditions, neurogenic<br />
bladder, benign prostatic hypertrophy, pelvic lipomatosis, and urethral<br />
obstruction.<br />
REFLUXING MEGA<strong>URETER</strong><br />
Primary: This condition occurs most often in children and describes a wide<br />
ureter secondary to vesicoureteral reflux (VUR), when an abnormality of<br />
the ureteral orifice (or tunnel length) is the cause of the reflux.<br />
Secondary: Reflux due to high bladder pressures from a neurogenic<br />
bladder or bladder outlet obstruction.<br />
NONREFLUXING, NONOBSTRUCTED MEGA<strong>URETER</strong><br />
Primary: Dilation not due to obstruction or reflux (prune-belly syndrome.)<br />
Secondary: In this condition, ureters remain dilated after the correction of<br />
initial pathology.<br />
primary obstructive megaureter in children and adults<br />
according to the degree of dilatation of the proximal<br />
ureter. 5 In grade 1, the dilatation is limited to the distal<br />
ureteral segment. In grade 2, the dilation extends into<br />
the proximal ureter and there may be mild caliectasis.<br />
In grade 3, the entire ureter is dilated proximal to the<br />
adynamic segment and there is moderate to severe<br />
caliectasis. One drawback to Pfister and Hendren’s<br />
grading system is that excretory urography, which is<br />
rarely necessary today, is required.<br />
The most commonly used classification for neonates,<br />
which is now standard<br />
in adults, was<br />
UROlogic<br />
➤ While US is highly sensitive in<br />
detecting dilated ureters, it lacks<br />
specificity for diseases that require<br />
intervention. We recommend US<br />
and VCUG within 48 hours of birth<br />
in antenatally diagnosed infants.<br />
46 CONTEMPORARY UROLOGY JUNE 2006<br />
devised by the Society<br />
for Fetal Urology<br />
(SFU). It assigns a<br />
grade from 0 to 4<br />
based on the degree<br />
of upper urinary tract<br />
dilation. In grade 0,<br />
the central renal complex<br />
is intact. In grade<br />
1, there is mild split-<br />
ting of the renal complex. In grade 2,<br />
the pelvis is dilated but the calyces are<br />
not dilated. In grade 3, the pelvis is<br />
markedly split and the calyces are uniformly<br />
dilated but the renal parenchyma<br />
is normal. Grade 4 shares the characteristics<br />
of grade 3, but there is thinning<br />
of the renal parenchyma.<br />
EVALUATION OF PRENATALLY<br />
DIAGNOSED MEGA<strong>URETER</strong><br />
While US is highly sensitive for the detection<br />
of a dilated ureter, it lacks specificity<br />
for diseases that will actually require<br />
intervention. Classification of<br />
megaureters based on the etiology of<br />
the dilation allows the clinician to better<br />
inform patients about the treatment options<br />
and their risks and benefits. Thus,<br />
at our institution, we recommend that<br />
newborns with prenatally diagnosed<br />
megaureters undergo US and voiding<br />
cystourethrography (VCUG) within 48<br />
hours of birth. If reflux is ruled out on<br />
VCUG, we proceed to DTPA diuresis<br />
renography to better evaluate renal<br />
function and to determine the degree of<br />
ureteral obstruction (Figure 1).<br />
MANAGEMENT IN ADULTS<br />
Adults with primary obstructed megaureter typically<br />
present with pain, infection, or hematuria. Radiologic<br />
evaluation (Figure 1) usually reveals pathology in the<br />
distal ureter. Therefore, aggressive surgical management<br />
has been recommended for adults.<br />
Hemal and colleagues identified 53 of 55 adult primary<br />
obstructed megaureters on the basis of studies obtained<br />
to evaluate symptoms. 2 While the authors advocated<br />
surgical management in most instances, they<br />
found it unrewarding in patients with bilateral disease<br />
who have advanced renal failure. Of 5 patients with bilateral<br />
primary obstructed megaureter and uremia, 3<br />
underwent ureteral reimplantation. Of that group, only<br />
1 improved with adequate drainage, and the other 2 patients<br />
died. 2<br />
MANAGEMENT IN CHILDREN<br />
While surgery is the first-line therapy for primary obstructed<br />
megaureter in adults, the approach in children<br />
is evolving. Several studies have compared surgical<br />
outcomes with conservative management, but all are<br />
retrospective and involve a considerable selection
ias. 7,9,10 Nevertheless, these studies<br />
document a shift from the traditional<br />
approach of surgical management to<br />
the current trend of surveillance.<br />
Between 1981 and 1987, Keating<br />
and colleagues assessed 44 renal units<br />
in 35 neonates with primary obstructed<br />
megaureter. 7 Infants with ureters<br />
dilated down to the UVJ with varying<br />
degrees of hydronephrosis were included<br />
in the study. Infants with secondary<br />
obstructed megaureters were<br />
eliminated from the analysis. Antenatal<br />
diagnosis was made by US in 23 of<br />
44 units. Of the 23 units, 87% were<br />
managed nonoperatively. Diagnoses<br />
for the remaining 21 units were made<br />
on the basis of symptomatic complaints<br />
due to UTI or the presence of a<br />
flank mass, or they were incidentally<br />
discovered. Only 12 of the 21 symptomatic<br />
units were managed conservatively.<br />
Subsequently, surgery was performed<br />
on 2 of the 12 conservatively<br />
managed units because of increased<br />
obstruction on DTPA diuresis renogram<br />
and increased dilation on US.<br />
The authors suggested that a decision<br />
to manage asymptomatic patients<br />
conservatively should be based on an<br />
estimate of absolute renal function as<br />
determined by diuresis renography. 7<br />
In 1994, Baskin and associates 9<br />
provided a long-term follow up of Keating and colleagues’<br />
7 carefully selected group and found that 10 of<br />
the original 35 neonates with 44 renal units ultimately<br />
underwent surgery. The remaining 25 were observed<br />
and managed with serial urinary tract imaging using<br />
DTPA diuresis renography, intravenous pyelography<br />
(IVP), and/or renal US. Seventeen of the 25 were diagnosed<br />
antenatally, 2 were identified due to infection,<br />
and 6 incidentally diagnosed. Mean follow-up was 7.3<br />
years for 24 patients. One patient was lost to follow-up<br />
after 1.5 years. The conservatively managed patients<br />
demonstrated no decline of renal function on DTPA<br />
diuresis renography during the observation period.<br />
The authors concluded that conservatively managed<br />
patients should be monitored closely as indications for<br />
surgical repair may arise. 9<br />
McLellan and co-workers evaluated the records of<br />
54 newborns who were prenatally diagnosed with primary<br />
obstructed megaureter from 1993 to 1998. 10 Me-<br />
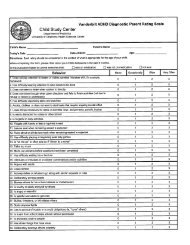
FIGURE 1<br />
Initial radiographic evaluation of suspected urologic<br />
abnormality<br />
Reflux<br />
Vesicoureteral<br />
reflux<br />
SUSPECTED UROLOGIC ABNORMALITY<br />
(prenatal US or symptoms)<br />
US shows dilation<br />
Perform VCUG<br />
Obstructed<br />
megaureter<br />
dian follow-up was 25.8 months. A total of 69 units<br />
were confirmed postnatally using various imaging<br />
modalities. Antibiotic prophylaxis was continued until<br />
the children were between the ages of 9 and 12 months,<br />
depending on physician’s preference. No child had a<br />
culture-documented UTI.<br />
Resolution, defined as a decrease in hydronephrosis to<br />
SFU grade 1 without hydroureter or minimal residual<br />
hydroureter, occurred in 39 (72%) patients. 10 Five patients<br />
(9%) had no resolution during the surveillance period,<br />
and 10 (19%)<br />
underwent surgery.<br />
The presenting grade<br />
of hydronephrosis appeared<br />
to be an important<br />
predictor of<br />
the resolution rate.<br />
SFU hydronephrosis<br />
grades 1 to 3 were<br />
No reflux<br />
Perform DTPA diuresis<br />
renography<br />
Obstruction No obstruction<br />
Nonobstructing,<br />
nonrefluxing<br />
megaureter<br />
UROlogic<br />
➤ Aggressive surgical management is<br />
recommended for most adults with<br />
primary obstructed megaureter.<br />
JUNE 2006 CONTEMPORARY UROLOGY 47
PRIMARY OBSTRUCTED MEGA<strong>URETER</strong><br />
“Parents of children with primary obstructed<br />
megaureter should be reassured that the<br />
condition is likely to resolve spontaneously.”<br />
more likely to resolve within 12 to 36 months. Increasing<br />
or severe hydronephrosis, decreasing renal function,<br />
and/or retrovesical ureteral diameter greater than 1 cm<br />
seemed to correlate with the need for surgical repair.<br />
Multiple reports support conservative management<br />
for primary obstructed megaureter detected in asymptomatic<br />
neonates. 6,7,9,10 We follow these patients with<br />
serial US and DTPA diuresis renography if increased<br />
dilation is observed on US (Figure 2). Once vesicoureteral<br />
reflux has been excluded by VCUG, antibiotic<br />
prophylaxis can be discontinued.<br />
INDICATIONS FOR SURGERY<br />
The absolute indications for surgical intervention have<br />
yet to be determined. Indications for surgery suggested<br />
by Simoni and associates include significant impairment<br />
of urine flow on renal scan, worsening renal<br />
function during observation, and recurrent UTI in<br />
spite of adequate antibiotic prophylaxis. 11<br />
Stehr and colleagues proposed 3 indications for<br />
surgery using US, VCUG, IVP, and MAG-3 renal scan:<br />
initial impaired renal function with an obstructive pattern,<br />
normal function and at least an equivocal urinary<br />
drainage pattern with no improvement, or deterioration<br />
of the urinary drainage and/or function during follow-up.<br />
Using these criteria, only 5 (9.6%) of 42 patients<br />
were managed surgically. 12<br />
Liu and co-workers studied 67 units with pathology<br />
at the UVJ. 13 Eleven<br />
(17%) patients failed<br />
UROlogic<br />
➤ In most antenatally diagnosed<br />
children, the condition resolves<br />
spontaneously. Consequently,<br />
asymptomatic patients can be<br />
followed conservatively with US.<br />
If dilation increases on US, DTPA<br />
diuresis renography should be<br />
performed.<br />
48 CONTEMPORARY UROLOGY JUNE 2006<br />
conservative therapy<br />
and required surgical<br />
repair—3 due to<br />
breakthrough infections<br />
and 8 because<br />
of deteriorating function.<br />
8 The remaining<br />
56 (83%) patients<br />
were managed conservatively<br />
by periodic<br />
followup with US<br />
and DTPA diuresis<br />
renography.<br />
SURGICAL METHODS OF REPAIR<br />
In uncomplicated nondilated ureters, reported success<br />
rates for the various open reimplantation techniques<br />
are well over 95% in children 1 year of age or<br />
older. 14 However, for large dilated ureters requiring<br />
plication or tapering in addition to the usual intravesical<br />
reimplant, no conclusive data have been published.<br />
Glassberg and associates reported a 99% success<br />
rate with tapering using a transverse ureteral advancement<br />
technique of ureteroneocystostomy (Cohen<br />
reimplant) in 7 primary obstructed megaureters. 14<br />
They noted that megaureters measuring 8 to 12 mm in<br />
width, regardless of etiology, can be reimplanted successfully<br />
without tapering.<br />
Hospitalization following reimplantation usually<br />
only requires an overnight stay. A double-pigtail<br />
ureteral stent is routinely placed and is removed at<br />
1 month. Ureteral reimplantation in the neonatal period<br />
can be difficult due to the discrepancy in size between<br />
the megaureter and the small neonatal bladder.<br />
Should surgery become necessary in the neonatal<br />
period, we recommend that a cutaneous ureterostomy<br />
be performed. This procedure is followed in the first<br />
year of life by open intravesical reimplantation with or<br />
without the tapering. The need for surgery is based on<br />
initial poor renal function tests, a 10% reduction in serial<br />
renal function tests, worsening serial US findings,<br />
and/or the presence of breakthrough infections.<br />
CONCLUSION<br />
The most important aspect in the management of the<br />
dilated ureter is identification of patients who will need<br />
and benefit from surgical repair. Historically, patients<br />
with dilated ureters presented with symptomatic complaints,<br />
and diagnosis preceded surgical correction.<br />
Today, antenatal US screening identifies most cases in<br />
children. The antenatal diagnosis of a dilated ureter<br />
with or without hydronephrosis warrants postnatal<br />
confirmation by US and institution of antibiotic prophylaxis.<br />
Ominous signs include bilaterally dilated systems,<br />
anuria, maternal oligohydramnios, or poor renal<br />
function, and necessitate more aggressive evaluation<br />
within the first 48 hours of life.<br />
Most patients with primary obstructed megaureter<br />
detected antenatally can be followed conservatively<br />
with US. DTPA diuresis renography may be performed<br />
after identification of increased dilation on US. Following<br />
antenatal diagnosis of primary obstructed megaureter,<br />
72% resolve spontaneously, 19% will need operative<br />
repair, and 9% will have persistent dilation on<br />
imaging without symptoms or deterioration of func-
FIGURE 2<br />
Management of primary megaureter<br />
tion. 13 Predictors for the need for surgical management<br />
include severe or worsening hydronephrosis, ureteral<br />
dilation greater than 1 cm in diameter, and worsening<br />
renal function. 10<br />
While aggressive surgical management is usually<br />
recommended for adults with primary obstructed<br />
megaureter, parents of children with the condition<br />
should be reassured that it is likely to resolve spontaneously.<br />
However, surgical management, when indicated,<br />
is usually successful.<br />
CU<br />
REFERENCES<br />
Improvement or<br />
no change<br />
Perform serial US<br />
imaging<br />
Resolution of<br />
obstruction<br />
No further<br />
imaging<br />
1. King LR. Megaloureter: definition, diagnosis and management. J Urol.<br />
1980;123(2):222-223.<br />
2. Hemal AK, Ansari MS, Doddamani D, et al. Symptomatic and complicated<br />
adult and adolescent primary obstructive megaureter—indications for surgery:<br />
analysis, outcome, and follow-up. Urology. 2003;61(4):703-707.<br />
3. Dunnick NR, McCallum RW, Sandler CM. Textbook of Uroradiology. 1st<br />
ed. Baltimore, Md: Williams & Wilkins; 1991.<br />
4. Leibowitz S, Bodian M. A study of the vesical ganglia in children and the<br />
relationship to the megaureter megacystis syndrome and Hirschsprung’s disease.<br />
J Clin Pathol. 1963;16:342-350.<br />
US, VCUG, and DTPA diuresis renography<br />
Primary megaureter<br />
Low- to mid-grade ureteral<br />
obstruction<br />
Worsening renal<br />
function<br />
Increased dilation<br />
DTPA diuresis<br />
renography<br />
Infection or pain<br />
High-grade ureteral<br />
obstruction<br />
Surgical repair<br />
Decreased function<br />
(>10%) or increased<br />
obstruction<br />
5. Pfister RC, Hendren WH. Primary megaureter in children and adults. Clinical<br />
and pathophysiologic features of 150 ureters. Urology. 1978;12(2):<br />
160-176.<br />
6. Manzoni C. Megaureter. Rays. 2002;27(2):83-85.<br />
7. Keating MA, Escala J, Snyder HM et al. Changing concepts in management<br />
of primary obstructive megaureter. J Urol. 1989;142(2 pt 2):636-640.<br />
8. Gunn TR, Mora JD, Pease P. Antenatal diagnosis of urinary tract abnormalities<br />
by ultrasonography after 28 weeks’ gestation: incidence and outcome.<br />
Am J Obstet Gynecol. 1995;172(2 pt 1):479-486.<br />
9. Baskin LS, Zderic SA, Snyder HM, et al. Primary dilated megaureter: long<br />
term followup. J Urol. 1994;152(2 pt 2):618-621.<br />
10. McLellan DL, Retik AB, Bauer SB, et al. Rate and predictors of spontaneous<br />
resolution of prenatally diagnosed primary nonrefluxing megaureter.<br />
J Urol. 2002;168(5):2177-2180.<br />
11. Simoni F, Vino L, Pizzini C, et al. Megaureter: classification, pathophysiology,<br />
and management. Pediatr Med Chir. 2000;22(1):15-24.<br />
12. Stehr M, Metzger R, Schuster T, et al. Management of the primary obstructed<br />
megaureter (POM) and indications for operative treatment. Eur J Pediatr<br />
Surg. 2002;12(1):32-37.<br />
13. Liu HY, Dhillon HK, Yeung CK, et al. Clinical outcome and management<br />
of prenatally diagnosed primary megaureters. J Urol. 1994;152(2 pt 2):614-<br />
617.<br />
14. Glassberg KI, Laungani G, Wasnick RJ, et al. Transverse ureteral advancement<br />
technique of ureteroneocystostomy (Cohen reimplant) and a modification<br />
for difficult case (experience with 121 ureters). J Urol. 1985; 134(2):<br />
304-307.<br />
JUNE 2006 CONTEMPORARY UROLOGY 49