Serotonin Selective Reuptake Inhibitors - CME
Serotonin Selective Reuptake Inhibitors - CME
Serotonin Selective Reuptake Inhibitors - CME
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
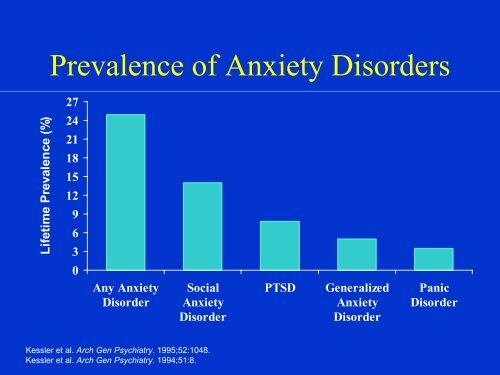
Lifetime Prevalence (%)<br />
Prevalence of Anxiety Disorders<br />
27<br />
24<br />
21<br />
18<br />
15<br />
12<br />
9<br />
6<br />
3<br />
0<br />
Any Anxiety<br />
Disorder<br />
Social<br />
Anxiety<br />
Disorder<br />
Kessler et al. Arch Gen Psychiatry. 1995;52:1048.<br />
Kessler et al. Arch Gen Psychiatry. 1994;51:8.<br />
PTSD Generalized<br />
Anxiety<br />
Disorder<br />
Panic<br />
Disorder
Outcome of Panic Disorder at<br />
Long-Term Follow-up<br />
Persistence of Rate (%) Range (%)<br />
Panic attacks 46 17-70<br />
Phobic avoidance 69 36-82<br />
Functional impairment 50 39-67<br />
Roy-Byrne & Cowley, 1995
Pharmacopoeia for Anxiety<br />
Disorders<br />
Antidepressants<br />
<strong>Serotonin</strong> <strong>Selective</strong> <strong>Reuptake</strong> <strong>Inhibitors</strong> (SSRIs)<br />
<strong>Serotonin</strong>-Norepinephrine <strong>Reuptake</strong> <strong>Inhibitors</strong> (SNRIs)<br />
Atypical Antidepressants<br />
Tricyclic Antidepressants (TCAs)<br />
Monoamine Oxidase <strong>Inhibitors</strong> (MAOIs)<br />
Benzodiazepines<br />
Other Agents<br />
Azaspirones<br />
Beta blockers<br />
Anticonvulsants<br />
Other strategies
<strong>Serotonin</strong> <strong>Selective</strong> <strong>Reuptake</strong> <strong>Inhibitors</strong><br />
• Fluoxetine (Prozac), 20-80 mg/d<br />
– Initiate with 5-10 mg/d<br />
• Sertraline (Zoloft), 50-200 mg/d<br />
– Initiate with 25-50 mg/d<br />
• Paroxetine (Paxil), 20-50 mg/d<br />
– Initiate with 10mg/d<br />
• Fluvoxamine (Luvox), 50-300 mg/d<br />
– Initiate with 25 mg/d<br />
• Citalopram (Celexa)<br />
- Initiate with 10-20 mg/d<br />
• Start low to minimize anxiety<br />
Adjunctive BZD, beta blocker
<strong>Serotonin</strong> <strong>Selective</strong> <strong>Reuptake</strong><br />
<strong>Inhibitors</strong> (cont)<br />
• Typical SSRI side effects:<br />
– GI distress, jitteriness, headaches, sleep<br />
disturbance, sexual disturbance<br />
• Clomipramine (Anafranil), 25-250 mg/d<br />
– Initiate with 25 mg/d<br />
• Efficacy: PDAG, PTSD, SP, OCD, GAD
IES<br />
score<br />
Sertraline In Comorbid PTSD<br />
60<br />
40<br />
20<br />
0<br />
Brady et al. J Clin Psychiatry. 1995;56:502.<br />
And Alcoholism<br />
Pre-treatment<br />
Pre treatment<br />
Post-treatment<br />
Post treatment<br />
IES Alcohol use<br />
140<br />
70<br />
0<br />
Standard<br />
drinks/week
Discontinuation of Treatment for<br />
Anxiety Disorders<br />
• Withdrawal/rebound more common with Bzd than<br />
other anxiolytic treatment<br />
• Relapse: a significant problem across treatments.<br />
Many patients require maintenance therapy<br />
• Bzd abuse is rare in non-predisposed individuals<br />
• Clinical decision: balance comfort/compliance/<br />
comorbidity during maintenance treatment with<br />
discontinuation-associated difficulties
Strategies for Anxiolytic<br />
• Slow taper<br />
Discontinuation<br />
• Switch to longer-acting agent for taper<br />
• Cognitive-Behavioral therapy<br />
• Adjunctive<br />
– Antidepressant<br />
– Anticonvulsant<br />
– ?clonidine, ?beta blockers, ? buspirone
<strong>Serotonin</strong>-Norepinephrine<br />
<strong>Reuptake</strong> Inhibitor<br />
• Venlafaxine-XR (Effexor-XR) 75-300 mg/d<br />
– Initiate with 37.5 mg/d<br />
• Indicated for GAD; effective for panic<br />
disorder, social phobia, PTSD, OCD<br />
• Typical side effects<br />
– GI distress, jitteriness, headaches, sexual<br />
disturbance
Atypical Antidepressants<br />
• Nefazadone (300-500 mg/d)<br />
– 5-HT reuptake inhibitor<br />
– 5-HT2 antagonist<br />
– Initiate with 50 mg bid<br />
• Mirtazapine<br />
– Limited experience to date in anxiety disorders
Atypical Antidepressants (cont.)<br />
• Bupropion<br />
– Based on limited data, considered less effective<br />
for panic and other anxiety disorders, but<br />
reports suggestive of efficacy for<br />
• panic disorder<br />
• social anxiety disorder<br />
•PTSD<br />
• Trazodone<br />
– Based on limited data, considered less effective<br />
for panic and other anxiety disorders
Tricyclic Antidepressants<br />
• Imipramine (Tofranil)<br />
• Nortriptyline (Pamelor)<br />
• Desipramine (Norpramin)<br />
• Amitriptyline (Elavil)<br />
• Doxepin (Sinequan)<br />
• Effective in anxiety with or without comorbid depression<br />
• Recommended dosage 2.25 mg/kg/d Imipramine or its<br />
equivalent for panic<br />
• Initial anxiety worsening (Initiate with “test” dose, e.g.<br />
10 mg/d IMI)
Tricyclic Antidepressants (cont)<br />
• Typical TCA side effects<br />
– anticholinergic effects (dry mouth, blurred<br />
vision, constipation)<br />
– orthostatic hypotension<br />
– cardiac conduction disturbance<br />
– weight gain<br />
– sexual dysfunction<br />
• Lethal in overdose<br />
• Weight gain and sedation often become<br />
increasingly problematic over time<br />
• Efficacy: PDAG, GAD, PTSD
Monoamine Oxidase <strong>Inhibitors</strong><br />
• Phenelzine (Nardil) 45-90 mg/d<br />
• Tranylcypromine (Parnate) 30-60 mg/d<br />
• Isocarboxacid (Marplan) 10-30 mg/d<br />
• Initial worsening of anxiety is unusual<br />
• Side effects: light-headedness, neurological<br />
symptoms, weight gain, sexual dysfunction,<br />
edema<br />
• Dietary restrictions/Hypertensive crisis; “cheese<br />
reaction”<br />
• Risk of lethal overdose and toxicity<br />
• Generally reserved for refractory cases<br />
• Efficacy: PDAG, SP, OCD, PTSD
Benzodiazepines<br />
• Potency was considered critical determinant<br />
of anti-panic efficacy<br />
– Alprazolam (Xanax)<br />
– Clonazepam (Klonopin)<br />
– +/- Lorazepam (Ativan)<br />
• But comparable doses of diazepam as<br />
effective as alprazolam<br />
• All benzodiazepines effective for<br />
generalized anxiety
• Effective<br />
Potential Benefits of<br />
Benzodiazepine Therapy<br />
• Short latency of therapeutic onset<br />
• Well tolerated<br />
• Rapid dose adjustment feasible<br />
• Can be used “prn” for situational anxiety
Potential Drawbacks of<br />
Benzodiazepine Therapy<br />
• Initial sedation<br />
• Discontinuation difficulties<br />
• Potential for abuse in substance abusers<br />
• Not effective for comorbid depression
•Effective as AD in panic<br />
Alprazolam<br />
•Advantages: rapid onset of effect, lacks typical AD side effects<br />
•Disadvantages: short duration of effect (i.e., multiple dosing,<br />
interdose rebound), discontinuation syndromes, early relapse,<br />
abuse potential, disinhibition<br />
•Dosing: anticipate initial sedation (tachyphylaxis usually<br />
develops).<br />
•Range: 2-10 mg/d (4-6 mg/d usual) (QID dosing)
• Labeled as anticonvulsant<br />
Clonazepam<br />
• As effective as alprazolam for panic; issue of potency for antipanic<br />
efficacy<br />
• Advantages: Pharmacokinetic: longer duration of effect results<br />
in less frequent dosing, interdose symptoms, early relapse, or<br />
acute withdrawal symptoms. Slower onset of effect diminishes<br />
abuse potential<br />
• Disadvantages: Depression not more frequent than with other<br />
Bzd”s; disinhibition, headaches<br />
• Dosing: anticipate initial sedation (initiate at 0.25-0.5 mg qhs)<br />
• Range: 1-5 mg/d (BID dosing)
Combining Antidepressants<br />
with Benzodiazepines<br />
• Provides rapid anxiolysis during<br />
antidepressant lag<br />
• Decreases early anxiety associated with<br />
initiation of antidepressant<br />
• Treats residual anxiety wtih antidepressant<br />
treatment<br />
• Prevents and treats depression on<br />
benzodiazepines
Average PDSS scores<br />
2.5<br />
2<br />
1.5<br />
1<br />
0.5<br />
0<br />
End-Point (LVCF) Analysis of Panic Disorder Severity<br />
Scale Scores for Each Group<br />
Week<br />
00<br />
†<br />
*<br />
Week<br />
01<br />
*<br />
Week<br />
02<br />
Week<br />
03<br />
*<br />
Week<br />
04<br />
*<br />
Week<br />
05<br />
Clonazepam Taper<br />
Phase<br />
Week<br />
06<br />
Week<br />
07<br />
Week<br />
08<br />
* Together the Clonazepam groups differ from the Placebo group at p< .05<br />
† Clonazepam groups differ from each other at p
Buspirone<br />
• Non-benzodiazepine anxiolytic<br />
• Non-sedating, muscle relaxant, anticonvulsant<br />
• Effects on serotonin and dopamine receptors<br />
• Indicated for GAD; weak antidepressant<br />
effects<br />
• Useful as SSRI augmentation for panic, social<br />
phobia, depression, sexual dysfunction<br />
• Dosing: 30-60 mg/d
Beta Blockers<br />
• Decrease autonomic arousal<br />
• May be useful as adjunct for somatic<br />
symptoms of panic and GAD but not as<br />
primary treatment<br />
• Useful for non-generalized social phobia,<br />
performance anxiety subtype<br />
• Propranolol 10-60 mg/d; Atenolol 50-150<br />
mg/d
Anticonvulsants<br />
• Valproate and gabapentin effective for nonictal<br />
panic<br />
• Gabapentin effective for social phobia<br />
• Gabapentin (600-5400 mg/d) used as<br />
alternative to benzodiazepine<br />
• Valproate, Carbamazepine, Gabapentin,<br />
Topiramate and Lamotrigine for PTSD
Strategies for Refractory Anxiety<br />
• Maximize dose<br />
Disorder<br />
• Combine antidepressant and benzodiazepine<br />
• Administer cognitive-behavioral therapy<br />
• Attend to psychosocial issues<br />
.
Strategies for Refractory Anxiety<br />
• Augmentation<br />
– Anticonvulsants<br />
• Gabapentin<br />
• Valproate<br />
• Topiramate<br />
– Beta blocker<br />
– Buspirone<br />
– Clonidine/Guanfacine<br />
– Pindolol<br />
–Dopaminergic agonists<br />
(e.g., Ropinirole) for<br />
social phobia<br />
– Cyproheptadine<br />
Disorders<br />
• Combined SSRI/TCA<br />
• Alternative<br />
antidepressant<br />
– Clomipramine<br />
– MAOI<br />
• Other<br />
– Inositol<br />
–Kava-kava<br />
– Atypical neuroleptics
Cognitive-Behavioral Therapy<br />
for Anxiety Disorders<br />
• CBT useful alone or in combination with<br />
medication for<br />
– Refractory symptoms<br />
– Persistent cognitive factors, behavioral patterns and<br />
anxiety sensitivity<br />
– Comorbid conditions<br />
– Early intervention for PTSD prophylaxis<br />
• CBT may be provided by therapist or selfadministered<br />
(TherapyWorks manuals 800-228-<br />
0752///http://www.psychcorp.com)<br />
• CBT may facilitate medication discontinuation<br />
.
Continuation Phase Outcome with<br />
Sertraline Treatment of PTSD Based on<br />
Acute Phase Response Category<br />
Acute Phase<br />
Responder Status<br />
Acute Phase<br />
Responders<br />
Acute Phase<br />
Non-responders<br />
8%<br />
Sustained<br />
Response<br />
Continuation Phase<br />
Responder Status<br />
Lost response<br />
Converted to responder<br />
Continued non-response<br />
non response<br />
46%<br />
54%<br />
92%<br />
0% 20% 40% 60% 80% 100%<br />
Responder = > 30% decrease CAPS and CGI-S = 1 or 2<br />
Londborg et al. J Clin Psychiatry, in press.
Long-Term Treatment Of<br />
GAD<br />
• Need to treat long-term<br />
• Full relapse in approximately 25% of<br />
patients 1 month after stopping treatment<br />
• 60%-80% relapse within 1st year after<br />
stopping treatment<br />
Hales et al. J Clin Psychiatry. 1997;58(suppl 3):76.<br />
Rickels et al. J Clin Psychopharmacol. 1990;10(3 suppl):101S.
Change In<br />
Mean HAM-A<br />
Total Score<br />
Effect Of Venlafaxine On Total<br />
0<br />
-2<br />
-4<br />
-6<br />
-8<br />
-10<br />
-12<br />
-14<br />
-16<br />
-18<br />
HAM-A Scores<br />
Placebo (N=123)<br />
Venlafaxine XR (N=115)<br />
0 2 4 6 8 10 12 14 16 18 20 22 24 26 28<br />
Week Of Treatment<br />
P
Patients<br />
(%)<br />
Paroxetine Long-Term GAD Treatment<br />
% Remission<br />
Phase I: Single-Blind Phase II: Double-Blind<br />
80 Paroxetine 20-50 mg<br />
(N=599 responders)<br />
70<br />
Randomization<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
* P
Discontinuation of Treatment for<br />
Anxiety Disorders<br />
• Withdrawal/rebound more common with Bzd than<br />
other anxiolytic treatment<br />
• Relapse: a significant problem across treatments.<br />
Many patients require maintenance therapy<br />
• Bzd abuse is rare in non-predisposed individuals<br />
• Clinical decision: balance comfort/compliance/<br />
comorbidity during maintenance treatment with<br />
discontinuation-associated difficulties
Strategies for Anxiolytic<br />
• Slow taper<br />
Discontinuation<br />
• Switch to longer-acting agent for taper<br />
• Cognitive-Behavioral therapy<br />
• Adjunctive<br />
– Antidepressant<br />
– Anticonvulsant<br />
– ?clonidine, ?beta blockers, ? buspirone