Hemoptysis during Sexual Intercourse* - CHEST Publications ...
Hemoptysis during Sexual Intercourse* - CHEST Publications ...
Hemoptysis during Sexual Intercourse* - CHEST Publications ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
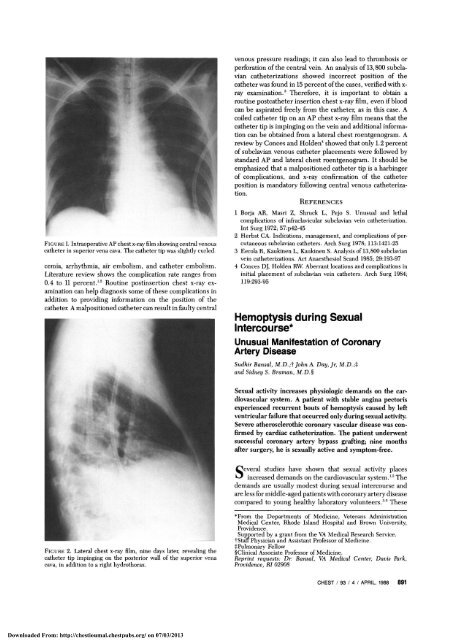
FIGURE 1. Intraoperative AP chest x-ray film showing central venous<br />
catheter in superior vena cava. The catheter tip was slightly curled<br />
cemia, arrhythmia, air embolism, and catheter embolism.<br />
Literature review shows the complication rate ranges from<br />
0.4 to 11 percent. 12 Routine postinsertion chest x-ray examination<br />
can help diagnosis some of these complications in<br />
addition to providing information on the position of the<br />
catheter. A malpositioned catheter can result in faulty central<br />
FIGURE 2. Lateral chest x-ray film, nine days later, revealing the<br />
catheter tip impinging on the posterior wall of the superior vena<br />
cava, in addition to a right hydrothorax.<br />
Downloaded From: http://chestioumal.chestpubs.org/ on 07/03/2013<br />
venous pressure readings; it can also lead to thrombosis or<br />
perforation of the central vein. An analysis of 13,800 subclavian<br />
catheterizations showed incorrect position of the<br />
catheter was found in 15 percent of the cases, verified with xray<br />
examination. 3 Therefore, it is important to obtain a<br />
routine postcatheter insertion chest x-ray film, even if blood<br />
can be aspirated freely from the catheter, as in this case. A<br />
coiled catheter tip on an AP chest x-ray film means that the<br />
catheter tip is impinging on the vein and additional information<br />
can be obtained from a lateral chest roentgenogram. A<br />
review by Conces and Holden 4 showed that only 1.2 percent<br />
of subclavian venous catheter placements were followed by<br />
standard AP and lateral chest roentgenogram. It should be<br />
emphasized that a malpositioned catheter tip is a harbinger<br />
of complications, and x-ray confirmation of the catheter<br />
position is mandatory following central venous catheterization.<br />
REFERENCES<br />
1 Borja AR, Masri Z, Shruck L, Pejo S. Unusual and lethal<br />
complications of infraclavicular subclavian vein catheterization.<br />
Int Surg 1972; 57:p42-45<br />
2 Herbst CA. Indications, management, and complications of percutaneous<br />
subclavian catheters. Arch Surg 1978; 113:1421-25<br />
3 Eerola R, Kaukinen L, Kaukinen S. Analysis of 13,800 subclavian<br />
vein catheterizations. Act Anaesthesiol Scand 1985; 29:193-97<br />
4 Conces DJ, Holden RW. Aberrant locations and complications in<br />
initial placement of subclavian vein catheters. Arch Surg 1984;<br />
119:293-95<br />
<strong>Hemoptysis</strong> <strong>during</strong> <strong>Sexual</strong><br />
<strong>Intercourse*</strong><br />
Unusual Manifestation of Coronary<br />
Artery Disease<br />
Sudhir Bansal, M.D.,t John A. Day, Jr, M.D.;t<br />
and Sidney S. Braman, M.D.I<br />
<strong>Sexual</strong> activity increases physiologic demands on the car<br />
diovascular system. A patient with stable angina pectoris<br />
experienced recurrent bouts of hemoptysis caused by left<br />
ventricular failure that occurred only <strong>during</strong> sexual activity.<br />
Severe atherosclerothic coronary vascular disease was con<br />
firmed by cardiac catheterization. The patient underwent<br />
successful coronary artery bypass grafting; nine months<br />
after surgery, he is sexually active and symptom-free.<br />
Several studies have shown that sexual activity places<br />
increased demands on the cardiovascular system. 1,2 The<br />
demands are usually modest <strong>during</strong> sexual intercourse and<br />
are less for middle-aged patients with coronary artery disease<br />
compared to young healthy laboratory volunteers. 35 These<br />
*From the Departments of Medicine, Veterans Administration<br />
Medical Center, Rhode Island Hospital and Brown University,<br />
Providence.<br />
Supported by a grant from the VA Medical Research Service.<br />
tStaff Physician and Assistant Professor of Medicine.<br />
^Pulmonary Fellow<br />
IClinical Associate Professor of Medicine.<br />
Reprint requests: Dr. Bansal, VA Medical Center, Davis Park,<br />
Providence, RI 02908<br />
<strong>CHEST</strong> / 93 / 4 / APRIL, 1988 891
observations led Masters and Johnson to conclude that most<br />
middle-aged men with atherosclerotic heart disease who are<br />
not in congestive heart failure can safely engage in this<br />
activity. 6 We report the case of a middle-aged man with<br />
known stable angina pectoris who developed hemoptysis due<br />
to left ventricular dysfunction <strong>during</strong> sexual intercourse.<br />
Failure to recognize this unusual association caused some<br />
delay in appropriate diagnostic work-up and therapy.<br />
CASE REPORT<br />
A 65-year-old man with a six-year history of stable angina pectoris<br />
presented to the emergency room several times over a four-month<br />
period, complaining of "coughing up blood." He estimated the<br />
quantity to be a tablespoon each episode, this was always followed by<br />
blood streaking of the sputum which persisted for several hours.<br />
During his first few visits, he was quite vague about the circumstances<br />
of his illness, though all of his visits were in the early hours of<br />
the morning. Repeated chest roentgenograms and cytologic examinations<br />
of the sputum done <strong>during</strong> clinic follow-up visits were<br />
negative. On one of these visits, he reluctantly admitted that all of<br />
these episodes had been precipitated by sexual activity (intercourse<br />
or masturbation). The patient had had the same sexual partner for the<br />
past 50 years and had sex once a week. He suffered a total of six<br />
episodes. Each episode was accompanied by "coughing, hard<br />
breathing, and chest tightness." Relief came with no specific therapy.<br />
Despite these symptoms, the patient did not complain of decreased<br />
exercise tolerance, orthopnea, or an increased frequency of his usual<br />
angina, which was normally manifested by chest pain after physical<br />
exertion. The chest pain was normally relieved by one sublingual<br />
nitroglycerin tablet. He had no symptoms of chronic bronchitis<br />
despite a cigarette smoking history of two packs per day for 30 years<br />
until three years previously. His past medical history was significant<br />
for a schizoaffective disorder, osteoarthritis, and peptic ulcer<br />
disease.<br />
The patient was admitted to the hospital for an evaluation. At this<br />
time, his medications were propranolol, isosorbide dinitrite,<br />
cimetidine, chlordiazepoxide, and nitroglycerin. His physical examination<br />
was unremarkable. A resting ECG, echocardiogram, and<br />
chest roentgenogram were normal, as were a complete blood count,<br />
chemistry screen, and coagulation studies. After 314 minutes of a<br />
treadmill stress test, the patient developed chest tightness accompanied<br />
by global 3 mm ST segment depression at a heart rate of 134<br />
beats per minute. There were no blood pressure changes and no<br />
hemoptysis. His symptoms resolved five minutes after the administration<br />
of sublingual nitroglycerin. The ECG changes resolved after<br />
16 minutes. Cardiac catheterization revealed an ejection fraction of<br />
70 percent and a left ventricular end-diastolic pressure of 16 to 20<br />
mm Hg. Coronary angiography showed a 75 percent obstruction of<br />
the proximal left anterior descending with 99 percent obstructions of<br />
the first diagonal and obtuse marginal branches, and also a 99<br />
percent lesion of the right coronary artery.<br />
The patient underwent a saphenous vein bypass graft of these<br />
lesions with good results. Five months postoperatively, while managed<br />
on cimetidine and digoxin, the patient is completely<br />
asymptomatic with excellent exercise tolerance. He is currently<br />
having sex twice a week without any symptoms.<br />
DISCUSSION<br />
While lung diseases are the most common cause of<br />
hemoptysis, cardiovascular diseases must be considered in<br />
the appropriate clinical setting. We believe that our patient<br />
developed cardiac ischemia <strong>during</strong> sexual activity due to<br />
increased cardiovascular demands in the face of limited<br />
coronary blood supply. Transient left ventricular compromise<br />
and resultant acute pulmonary congestion led to recurrent<br />
hemoptysis. We feel this is strongly supported by the<br />
absence of pulmonary disease, the fact that the hemoptysis<br />
was episodic and temporally related to sexual activity, and<br />
the fact that the patient returned to normal physical and<br />
sexual activity, without hemoptysis, following successful<br />
bypass surgery.<br />
<strong>Hemoptysis</strong> was a common symptom of mitral stenosis in<br />
the precardiac surgery era; it can result from acute pulmo<br />
nary congestion precipitated by sexual intercourse, physical<br />
exercise, and marked excitement. 7 Pulmonary congestion<br />
without the signs and symptoms of pulmonary edema is felt<br />
to cause blood streaking of sputum, as a result of rupture of<br />
pulmonary capillaries. 7 Our patient had repeatedly normal<br />
chest roentgenograms that were taken from two hours to<br />
three days after the episode of hemoptysis; presumably, the<br />
pulmonary congestion was quite transient and thus, missed<br />
by roentgenogram. Mitral stenosis was ruled out by both<br />
echocardiogram and catheterization.<br />
In our patient, ischemia-mediated ventricular dysfunction<br />
was believed to be the mechanism of acute pulmonary<br />
congestion. While this most often occurs in patients with<br />
impaired baseline ventricular function, patients with normal<br />
ventricular function are also subject to this complication." It<br />
has also been reported that sexual activity can precipitate<br />
dangerous arrhythmias in patients with ischemic heart dis<br />
ease; we doubt, however, that this was a factor in our case. 3<br />
In patients with recurrent hemoptysis associated with<br />
physical exertion, occult left ventricular dysfunction with<br />
resultant pulmonary congestion must be considered in the<br />
differential diagnosis. Our patient demonstrated that this<br />
may occur <strong>during</strong> the exertion of sexual intercourse in<br />
patients with ischemic heart disease.<br />
REFERENCES<br />
1 Bohlen JG, Held JP, Sandorson O, Patterson RE Heart rate, ratepressure<br />
product, and oxygen uptake <strong>during</strong> four sexual activities.<br />
Arch Intern Med 1984;114:1745-48<br />
2 Mann S, Craig Millar MW, Gould BA, Melville DI, Raferty EB.<br />
Coital blood pressure in hypertensives Gepalgia, syncope and the<br />
effects of beta-blockade. Br Heart J 1982; 47:84-89<br />
3 Nemec ED, Mansfield L, Kennedy JW. Heart rate and blood<br />
pressure responses <strong>during</strong> sexual activity in normal males. Am<br />
Heart J 1976; 92:274-77<br />
4 McNaughton M W. Heart rate and blood pressure response to stair<br />
cliimbing and sexual activity. Circulation 1978; 57:215<br />
5 Hellerstien HK, Friedman EH. <strong>Sexual</strong> activity and the post<br />
coronary patient. Arch Intern Med 1970; 125:987-99<br />
fi Masters WH, Johnson VE. Human sexual inadequacy. London:<br />
Churchill, 1970:998<br />
7 Hurst WB. The heart, 6th ed. New York: McGraw-Hill, 1986:<br />
118-19<br />
8 Clark LT, Garfien OB, Dwyer EM Jr. Acute pulmonary edema due<br />
to ischaemic heart disease without accompanying myocardial<br />
infarction: natural history and clinical profile. Am J Med 1983; 75:<br />
332-36<br />
9 Fletcher GF, Johnston BL, Cantwell JD. Dynamic electrocardiographic<br />
monitoring <strong>during</strong> coitus in patients post myocardial<br />
infarction and revascularization. Circulation 1978; 7:204<br />
892 <strong>Hemoptysis</strong> <strong>during</strong> <strong>Sexual</strong> Intercourse (Bansal, Day, Braman)<br />
Downloaded From: http://chestioumal.chestpubs.org/ on 07/03/2013
Delivers 40-140 more actuations<br />
than other oral steroid inhalers.<br />
Built-in barrel eliminates need<br />
and cost of spacers.<br />
Large barrel slows spray to<br />
a fine mist, not a jet spray that<br />
requires precise breathing<br />
coordination. Easily inhaled mist makes over<br />
90% of dose potentially available<br />
to airways.<br />
Inhalation made easy.<br />
(Plus low cost and portability)<br />
I Azmacort"<br />
^ (triamcinolone<br />
acetonide) a<br />
costs<br />
i<br />
less than other<br />
oral steroid<br />
inhalers.<br />
Downloaded From: http://chestioumal.chestpubs.org/ on 07/03/2013<br />
• •<br />
Very low<br />
incidence<br />
of oral<br />
candidiasis.<br />
Breathable, economical, portable—the<br />
unbeatable choice<br />
for asthma patients who must<br />
have steroid therapy.<br />
Azmacort<br />
(triamcinolone acetonide)<br />
From the makers of Slo-bid<br />
(THEOPHYLLINE ANHYDROUSL<br />
RORER PHARMACEUTICALS<br />
i n l a division of<br />
\mM RORER PHARMACEUTICAL CORPORATION<br />
\mM\ FORT WASHINGTON PA 19034<br />
PLEASE SEE NEXT PAGE FOR BRIEF SUMMARY OF PRESCRIBING INFORMATION.<br />
Inhaler telescopes into a<br />
compact unit that fits pocket<br />
or purse.<br />
FC#76<br />
892-A
892-B<br />
AzmaCOrt (triamcinolone acetonide) inhaler<br />
Brief Summary For Oral Inhalation Only<br />
INDICATIONS: Azmacort itriamcinolone acetoniclei inhaler is indicated only for patients<br />
who require chronic treatment with corticosteroids tor the control ol the symptoms<br />
ot bionchial asthma Such patients would include those already receiving systemic<br />
codicosleroids and selected patients who are inadequately controlled on a non-steroid<br />
regimen and in whom steroid therapy has been withheld because ot concern over<br />
potential adverse effects<br />
Azmacort" inhaler Is WO/" indicated: 1 For relief of asthma which can be controlled Oy<br />
bronchodilators and other non-steroid medications 2 In patients who require systemic<br />
corticosteroid treatment infrequently 3 In the treatment of non-asthmatic bronchitis<br />
CONTRAINDICATIONS: Azmacort inhaler is contraindicated in the pnmary treatment<br />
ol status asthmaticus or olher acute episodes of asthma where intensive measures<br />
are required<br />
Hypersensitivity to any ol the ingredients of this preparation contramrticates its use<br />
WARNINGS:<br />
Particular caie is needed in patients who are transferred from systemically active<br />
corticosteroids to Azmacort " inhaler because deaths due to adrenal insufficiency<br />
have occurred in asthmatic patients <strong>during</strong> and after Iransfer Irom systemic<br />
corticosteroids to aerosolized steroids in recommended doses After withdrawal<br />
Irom systemic corticosteroids, a number of months is usually required for recovery<br />
ol hypothalamic piimtaiy adicuai iHPA; function For some patients who have<br />
iccmvcd l.iii|i: dose:; of (u.il M-muds 1 nr lung pounds nl tuns; liiilcit' Ihi'iapy v.-111<br />
Azmacort inhaler is initiated recovery may be delayed for one year or longer<br />
During this period ol HPA suppression patients may exhibit signs and symptoms<br />
of adrenal insufficiency when exposed to trauma surgery or infections particularly<br />
gastroenteritis or other conditions with acute electrolyte loss Although Azmacort<br />
inhaler may provide control ol asthmatic symptoms <strong>during</strong> these episodes, in<br />
'ecommended doses n supplies only normal physiological amounts of corticosteroid<br />
systemically and does NOT provide the increased systemic steroid which is<br />
necessary for coping with these emergencies.<br />
During periods of stress or a severe asthmatic attach patients who have been<br />
recently withdiawrt from systemic coiticosteioids should be instructed lo resume<br />
systemic steroids (in large doses> immediately and to contact their physician<br />
lor further instruction These patients should also be instructed to carry<br />
a warning card indicating that they may need supplementary systemic steroids<br />
<strong>during</strong> periods of stress or a severe asthma attack<br />
Localized infections with Candida albicans have occurred infrequently in the mouth<br />
and pharynx these areas should be examined by the treating physician at each<br />
patient visit T he percentage ol positive mouih and thioat cultures for Candida<br />
albicans did not change dunng a yeai ol continuous therapy The incidence ol<br />
clinically apparent infection is low |2 5%!. These infections may disappear spontaneously<br />
oi may require treatment with appropriate antifungal therapy or discontinuance of<br />
treatment with Azmacort inhaler<br />
Azmacort inhaler is not to be regarded as a bronchodilator and is not mdicalec<br />
lot rapid relief of bronchospasm<br />
Patients should be instructed to contact then physician immediately when episodes of<br />
asthma which aie not responsive to bronchodilators occur <strong>during</strong> the course of tieatment<br />
with Azmacort inhaler Dunng such episodes patients may require therapy with<br />
systemic corticosteroids.<br />
There is no evidence that control of asthma can De achieved by the administration<br />
of Azmacort"'' inhaler in amounts greater than the recommended doses which appear lo<br />
be the therapeutic equivalent ol approximately 10 mg/day of oral prednisone<br />
Theoretically, the use of inhaled corticosteroids with alternate day prednisone oral<br />
therapy should be accompanied by more HPA suppression than a therapeutically<br />
equivalent regimen of either alone<br />
Transfer of patients from systemic steroid therapy to Azmacort inhaler may unmask<br />
allergic conditions previously suppressed by the systemic steroid therapy, e.g.. rhinitis<br />
conjunctivitis and eczema<br />
PRECAUTIONS: During withdiawal from oral steroids some patients may experience<br />
symptoms of systemically active steroid withdrawal eg joint and or muscular pain<br />
lassitude and depression, despite maintenance or even improvement of respiratory<br />
(unction (See DOSAGE AND ADMINISTRATION lor delailsi Although steroid withdrawal<br />
effects are usually transient and not severe, severe and even fatal exacerbation<br />
of asthma can occui if Ihe previous daily oral conirostcmid requirement had significantly<br />
exceeded 10 mg day ol prednisone or equivalent<br />
In responsive patients inhaled corticosteroids will often permit control of asthmatic<br />
symptoms wiin less suppression of HPA function than therapeutically equivalent oral<br />
doses of prednisone Since triamcinolone acetonide is absorbed into the circulation aim<br />
can be systemically active, the beneficial effects of Azmacort inhaler in minimizing<br />
or preventing HPA dysfunction may be expected only when recommended dosages<br />
are not exceeded<br />
Suppression ol HPA function has been reported in volunteers who received 4000 meg<br />
daily ot triamcinolone acetonide In addition suppression ol HPA function has been<br />
reported in some patients who have leceived recommended doses lor as little as<br />
6-12 weeks Since the response ol HPA function to inhaled corticosteroids is highly<br />
individualized the physician should consider this information when treating patients<br />
Because of the possibility of systemic absorption of inhaled corticosteroids patients<br />
healed with these drugs should be observed carefully for any evidence of systemic<br />
corticosteroid elfects including suppression of growth in children Particular care<br />
should be taken in observing patients postoperatively oi <strong>during</strong> periods of stress lor<br />
evidence ol a decrease in adrenal lunciion<br />
The long-term effects of triamcinolone acetonide inhaler in human subjects are not<br />
completely known although patients have received Azmacort inhaler on a continuous<br />
basis for periods of two years or longer While there has been no cluneal evidence<br />
ol adverse experiences the local elfects of the agent on developmental or immunologic<br />
processes in the mouth, pharynx, trachea and lung are also unknown<br />
The potential elfects of Azmacort inhaler on acute recurrent or chronic pulmonary<br />
nfections including active or quiescent tubercu osi! an nol km ivn For this reason<br />
since systemic administration of corticosteroids may mask some signs of lungal<br />
bacterial or viral infection, the same caution should be observed when treating patients<br />
with Azmacort ' inhaler. The potential effects of long-term administration of Azmacort<br />
inhaler on lung or other tissues are unknown However pulmonary infiltrates with<br />
eosinophils have occurred in patients receiving olher inhaled corticosteroid's<br />
Pregnancy: Pregnancy Category D Azmacort triamcinolone acetonide' has been<br />
•• :• v/iitngc'iic n rats ;ind •abb ts .'.I'-en in doses aimpa'a:] e tc no<br />
highest dose recommended foi humanuse approximately 0 032 mg kq day Administration<br />
of aeiosol inhalation to pregnant rats and rabbits produced emoryotoxic and<br />
fetotoxic effects which were comparable lo those produced by administration by<br />
other routes.<br />
Teratogenic elfects in both species included a low incidence of cleft palate and/or<br />
internal hydrocephaly and axial skeletal defects These findings lepiesenl known<br />
effects of glucocorticoids in laboratory animals<br />
There aie no well-controlled studies in pregnant women Experience with other dosage<br />
forms of triamcinolone acetonide does not include any positive evidence of adverse<br />
elfects on the fetus However, since such experience cannot exclude possibility of<br />
fetal damage, Azmacort"'' inhaler should be used <strong>during</strong> pregnancy only if the benefit<br />
clearly justifies the potential risk to Ihe fetus Infants born to mothers who have<br />
received substantial doses of corticosteroids <strong>during</strong> pregnancy should be carefully<br />
observed lor hypoartrenahsm<br />
Nursing mothers: It is not known whether this drug is excreted in human milk<br />
Because of the potential for tumorigenicity shown for triamcinolone acetonide in animal<br />
studies, a decision should be made whether to discontinue nursing or to discontinue<br />
the drug, taking info account Ihe importance of the drug to the mother<br />
ADVERSE REACTIONS: A few cases of oral candidiasis have been reported isee<br />
1 WARNINGS In addition, some patients receiving Azmacort inhaler have experienced<br />
hoarseness dry thioat irritated throal and dry mouth Increased wheezing and cough<br />
have been reported infrequently as has facial edema These adverse elfects have<br />
generally been mild and transient.<br />
RORER PHARMACEUTICALS<br />
KB RORERPHARMACEUTICAL CORPORATION<br />
HSI FORT WASHINGTON PA 19034<br />
Downloaded From: http://chestioumal.chestpubs.org/ on 07/03/2013<br />
AMERICAN<br />
COLLEGE OF<br />
<strong>CHEST</strong><br />
PHYSICIANS<br />
Postgraduate Courses<br />
54th ANNUAL<br />
SCIENTIFIC ASSEMBLY<br />
POSTGRADUATE COURSES<br />
Date:<br />
October 3,1988<br />
Location:<br />
Anaheim, California<br />
This year's Annual Scientific Assembly,<br />
to be held October 3-7, will feature a<br />
"track" focusing on "New/High<br />
Technology in Chest Medicine and<br />
Surgery". The following postgraduate<br />
courses will be held at the Meeting.<br />
• Perioperative Management of the<br />
Cardiothoracie Patient<br />
• Invasive and Noninvasive Diagnosis in<br />
Lung Cancer<br />
• The Pleural Space<br />
• Cardiac Disease in the ICU (Non-MI)<br />
• Chest Imaging<br />
• Overview of Pulmonary Infections<br />
Sponsor:<br />
American College of Chest Physicians<br />
For further information contact:<br />
Division of Education, ACCP<br />
911 Busse Highway<br />
Park Ridge, IL 60068-2375<br />
(312) 698-2200
m Tidal Volume, Air Flow<br />
• Paradoxical Breathing<br />
• Apnea Alarms—<br />
Obstructive/Central<br />
• Diaphragm Fatigue<br />
• Neonate—Pediatric—Adult<br />
• Ambulatory Capability<br />
The<br />
of all these patients are<br />
being monitored by<br />
®<br />
'"For complete information, fill out coupon<br />
and mail to:<br />
AMBULATORY MONITORING, INC.<br />
731 SAW MILL RIVER RD., ARDSLEY, NEW YORK 10502<br />
TELEPHONE: (914) 693-9240 TELEX: CALIB ARLY 131 423<br />
Name. Title<br />
Hospital/Institution<br />
Address<br />
City State Zip<br />
My need is urgent, please call at<br />
Downloaded From: http://chestioumal.chestpubs.org/ on 07/03/2013<br />
The non-invasive, long term pulmonary<br />
monitoring system jfe,'<br />
A Respiratory Inductive Plethysmograph (Respitrace®)<br />
offers quantitative tidal volumes and flow measurements<br />
while simultaneously describing diaphragm and chest<br />
wall muscle contributions breath by breath.. .eliminates<br />
measurement errors introduced by mouthpiece or mask.<br />
With calibration to ± 10% of spirometry, Respitrace can<br />
be worn comfortably for hours without losing accuracy.<br />
Compatible with existing DC recorders and computer<br />
systems for data storage.<br />
n SYSTEMS<br />
. J AN ESTABLISHED METHOD IN PULMONARY MEDICINE<br />
892-C