TRITACE COMP 1. DESCRIPTION 1.1 Active Moiety(ies) / Active ...
TRITACE COMP 1. DESCRIPTION 1.1 Active Moiety(ies) / Active ...
TRITACE COMP 1. DESCRIPTION 1.1 Active Moiety(ies) / Active ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>TRITACE</strong> <strong>COMP</strong><br />
<strong>1.</strong> <strong>DESCRIPTION</strong><br />
<strong>1.</strong>1 <strong>Active</strong> <strong>Moiety</strong>(<strong>ies</strong>) / <strong>Active</strong> Ingredients<br />
Ramipril Hydrochlorothiazide<br />
Ramiprilat, the active metabolite of ramipril, is an inhibitor of the enzyme<br />
dipeptidylcarboxypeptidase I (synonyms: angiotensin-converting enzyme [ACE],<br />
kininaseII). Hydrochlorothiazide is a thiazide diuretic.<br />
<strong>1.</strong>2 Therapeutic or Pharmacological Class<br />
ACE inhibitor plus diuretic. Antihypertensive.<br />
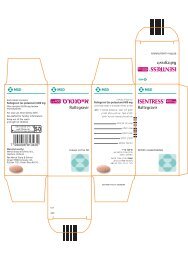
<strong>1.</strong>3 Pharmaceutical Form(s)<br />
Tablets.<br />
<strong>1.</strong>4 Composition<br />
<strong>Active</strong> ingredient<br />
Each tablet *TM 1/1* contains, as active ingredients, 5 mg ramipril and 25 mg<br />
hydrochlorothiazide.<br />
Each tablet *TM 1/2* contains, as active ingredients, 2.5 mg ramipril and 12.5 mg<br />
hydrochlorothiazide.<br />
Excipients<br />
See background documentation.<br />
<strong>1.</strong>5 Nature and Contents of Container<br />
See background documentation.<br />
2. INDICATIONS<br />
●<br />
To lower blood pressure in essential hypertension, when treatment with a combination<br />
preparation is indicated.<br />
*TM* is not suitable for the treatment of hypertension resulting from primary<br />
hyperaldosteronism.<br />
3. DOSAGE AND ADMINISTRATION
Dosage<br />
The dosage is based on the desired antihypertensive effect and on how the patient<br />
tolerates the drug.<br />
The following dosage appl<strong>ies</strong> in the absence of special circumstances defined below:<br />
Usual initial dosage: 2.5 mg ramipril / 12.5 mg hydrochlorothiazide (corresponding to 1<br />
tablet * TM 1/2 * or ½ tablet *TM 1/1 *) daily.<br />
If necessary, the dose may be increased at intervals of 2 to 3 weeks.<br />
Maximum permitted daily dose: 10 mg ramipril / 50 mg hydrochlorothiazide<br />
(corresponding to 4 tablets * TM 1/ 2* or 2 tablets *TM 1/1*).<br />
Generally, it is recommended that the daily dose be administered in the morning as a<br />
single dose.<br />
In most cases, blood pressure will fall sufficiently after 2.5 mg ramipril / 12.5 mg<br />
hydrochlorothiazide to 5 mg ramipril / 25 hydrochlorothiazide (corresponding to 1 to 2<br />
tablets *TM 1 /2 * or ½ to 1 tablet *TM 1/1 *) daily.<br />
Special circumstances<br />
●Dosage in patients pre-treated with diuretics<br />
In patients pre-treated with a diuretic, consideration must be given to discontinuing the<br />
diuretic at least 2 to 3 days or (depending on the duration of action of the diuretic) longer<br />
before starting treatment with * TM*, or at least to reducing the diuretic dose.<br />
Should discontinuation not be possible, it is recommended that treatment be initiated with<br />
the smallest possible dosage or ramipril (<strong>1.</strong>25 mg daily) in a free combination. It is<br />
recommended that, subsequently, a changeover be made to an initial daily dose of not<br />
more than 2.5 mg ramipril / 12.5 mg hydrochlorothiazide (corresponding to 1 tablet *TM<br />
1 /2 * or ½ tablet *TM 1/1*).<br />
●Dosage in patients with impaired renal function<br />
Creatinine clearance 60 to 30 ml/min per <strong>1.</strong>73 m 2 body surface area: Treatment is started<br />
with ramipril alone at a daily dose of <strong>1.</strong>25 mg. After gradually increasing the dose of<br />
ramipril, medication with the combination preparatiojn is started at a daily dose of 2.5 mg<br />
ramipril / 12,5 mg hydrochlorothiazide (corresponding to 1 tablet *TM 1 /2 * or ½ tablet<br />
*TM 1/1*).<br />
Maximum permitted daily dose: 5 mg ramipril / 25 mg hydroclorothiazide<br />
(corresponding to 2 tablets *TM 1 /2 * or 1 tablet *TM 1/1*).<br />
In patients with impaired liver function, the response to the treatment with Tritace Comp<br />
may be either increased or reduced. Treatment in these patients must therefore be
initiated only under close medical supervision. Maximum permitted daily dose in this<br />
case is Ramipril 2.5 mg.<br />
Administration<br />
*TM* tablets have to be swallowed whole with sufficient amounts of liquid (approx. ½<br />
glass). The tablets must not be chewed or crushed.<br />
*TM* may be taken before, during or after a meal.<br />
4. CONTRAINDICATIONS<br />
*TM* must not be used<br />
●In patients with hypersensitivity to ramipril, any other ACE inhibitor,<br />
hydrochlorothiazide, other thiazide diuretics, sulfonamides or any of the excipients of<br />
*TM*.<br />
●In patients with a history of angioneurotic oedema.<br />
●In patients with severe impairment of renal function with a creatinine clearance below<br />
30 ml/min per <strong>1.</strong>73 m 2 body surface area, and in dialysis patients.<br />
●In patients with haemodynamically relevant renal artery stenosis, bilateral or unilateral<br />
in the single kidney.<br />
●In patients with haemodynamically relevant left-ventricular inflow or outflow<br />
impediment (e.g., stenosis of the aortic or mitral valve).<br />
●In patients with clinically relevant electrolyte disturbances which may worsen<br />
following treatment with *TM* (e.g., hypokalaemia, hyponatraemia, or hypercalcaemia).<br />
●In patients with severe impairment of liver function.<br />
●During pregnancy.<br />
●In breast feeding women.<br />
Concomitant use of ACE inhibitors and extracorporeal treatments leading to contact of<br />
blood with negatively charged surfaces must be avoided, since such use may lead to<br />
severe anaphylactoid reactions. Such extracorporeal treatments include dialysis or<br />
haemofiltration with certain high-flux (e.g. polyacrylonitril) membranes and low-density<br />
lipoprotein apheresis with dextran sulfate.
5. WARNINGS<br />
Angioneurotic oedema occurring during treatment with an ACE inhibitor necessitates<br />
immediate discontinuation of the drug.<br />
Angioneurotic oedema may involve the tongue, glottis or larynx. Emergency treatment of<br />
life-threatening angioneurotic oedema includes immediate administration of epinephrine<br />
(subcutaneous or slow intravenous injection) accompanied by monitoring of ECG and<br />
blood pressure. Hospitalization of the patient is advisable with observation for at least 12<br />
to 24 hours and discharge only upon complete resolution of the symptoms.<br />
Insufficient experience has been gained concerning the use of *TM* in children.<br />
6. PRECAUTIONS<br />
Treatment with *TM* requires regular medical supervision.<br />
Patients with hyper-stimulated renin angiotensin system<br />
In the treatment of patients with a hyper-stimulated renin-angiotensin system, particular<br />
caution must be exercised (see also under "3. Dosage and administration"). Such patients<br />
are at risk of an acute pronounced fall in blood pressure and deterioration of renal<br />
function due to ACE inhibition, especially when an ACE inhibitor is given for the first<br />
time or for the first time at an increased dose. Initial doses or initial dose increases must<br />
be accompanied by close blood pressure monitoring until such time as no further acute<br />
reduction in blood pressure is to be anticipated.<br />
Significant activation of the renin angiotensin system is to be anticipated, for example:<br />
in patients with severe, and particularly with malignant hypertension.The initial phase of<br />
treatment requires special medical supervision.<br />
in patients with concomitant, and particularly with severe heart failure. If heart failure is<br />
severe, the initial phase of treatment requires special medical supervision.<br />
in patients with haemodynamically relevant left-ventricular inflow or outflow<br />
impediment (e.g., stenosis of the aortic or mitral valve). The initial phase of treatment<br />
requires special medical supervision.<br />
in patients with haemodynamically relevant renal artery stenosis. The initial phase of<br />
treatment requires special medical supervision. See also under ‘Monitoring of renal<br />
function’ below.<br />
in patients pre-treated with diuretics. Where discontinuing use or reducing the dose of the
diuretic is not possible, the initial phase of treatment requires special medical supervision.<br />
in patients in whom fluid or salt depletion exists or may develop (as a result of<br />
insufficient fluid or salt intake, or as a result of, for example, diarrhoea, vomiting or<br />
excessive sweating in cases where salt and fluid replacement is inadequate).<br />
Generally, it is recommended that dehydration, hypovolaemia or salt depletion be<br />
corrected before initiating treatment (in patients with heart failure, however, such<br />
corrective action must be carefully weighed against the risk of volume overload). When<br />
these conditions have become clinically relevant, treatment with *TM* must only be<br />
started or continued if appropriate steps are taken concurrently to prevent an excessive<br />
fall in blood pressure and deterioration of renal function.<br />
Patients at particular risk from a pronounced reduction in blood pressure<br />
In patients who would be at particular risk from an undesirably pronounced reduction in<br />
blood pressure (e.g. patients with haemodynamically relevant stenoses of the coronary<br />
arter<strong>ies</strong> or of the blood vessels supplying the brain), the initial phase of treatment requires<br />
special medical supervision.<br />
Elderly<br />
Some elderly patients may be particularly responsive to ACE inhibitors. Evaluation of<br />
renal function at the beginning of treatment is recommended.<br />
Monitoring of renal function<br />
It is recommended that renal function be monitored, particularly in the initial weeks of<br />
treatment. Particularly careful monitoring is required in patients with<br />
heart failure<br />
renovascular disease, including patients with haemodynamically relevant unilateral renal<br />
artery stenosis. In the latter patient group, even a small increase in serum creatinine may<br />
be indicative of unilateral loss of renal function.<br />
impairment of renal function<br />
kidney transplant patients.<br />
Electrolyte monitoring<br />
Treatment with *TM* requires regular monitoring of serum sodium, potassium, calcium,<br />
uric acid, and blood glucose. More frequent monitoring of serum potassium is necessary<br />
in patients with impaired renal function.<br />
Haematological monitoring<br />
It is recommended that the white blood cell count be monitored to permit detection of a<br />
possible leucopenia. More frequent monitoring is advised in the initial phase of treatment
and in patients with impaired renal function, those with concomitant collagen disease<br />
(e.g. lupus erythematosus or scleroderma) or those treated with other drugs that can cause<br />
changes in the blood picture. See also under "12. Adverse reactions".<br />
7. DRIVING A VEHICLE OR PERFORMING OTHER HAZARDOUS TASKS<br />
Some adverse effects (e.g. some symptoms of a reduction in blood pressure such as<br />
lightheadedness, dizziness) may impair the patient's ability to concentrate and react and,<br />
therefore, constitute a risk in situations where these abilit<strong>ies</strong> are of particular importance<br />
(e.g. operating a vehicle or machinery).<br />
8. INTERACTIONS<br />
8.1 Food<br />
Absorption or ramipril is not significantly affected by food.<br />
8.2 Drug interactions<br />
8.2.1 Contraindicated combinations<br />
Extracorporeal treatments leading to contact of blood with negatively charged surfaces<br />
such as dialysis or haemofiltration with certain high-flux membranes (e.g.<br />
polyacrylonitril membranes) and low-density lipoprotein apheresis with dextran sulfate:<br />
Risk of severe anaphylactoid reactions, see also under "4. Contraindications".<br />
8.2.2 Not recommended associations<br />
POTASSIUM SALTS POTASSIUM-RETAINING DIURETICS, HEPARIN: Rise in<br />
serum potassium concentration possible. Concomitant treatment with potassium-retaining<br />
diuretics (e.g. spironolactone) or with potassium salts requires close monitoring of serum<br />
potassium.<br />
8.2.3 Precautions for use<br />
ANTHYPERTENSIVE AGENTS AND OTHER SUBSTANCES WITH<br />
ANTIHYPERTENSIVE POTENTIAL (E.G., NITRATES, TRICYCLIC<br />
ANTIDEPRESSANTS, ANAESTHETICS):<br />
Potentiation of the anithypertensive effect is to be anticipated (concerning diuretics see<br />
also “6: Precautions”, 12. Adverse reactions” and “3 Dosage and administration”).<br />
Vasopressor sympathomimetics: These may reduce the antihypertensive effect of *TM*.<br />
Particularly close blood pressure monitoring is recommended. Furthermore, tThe effect<br />
of the vasopressor sympathomimetics may be attenuated by hydrochlorothiazide.
LITHIUM SALTS: Reduction of the excretion of lithium salts. This may lead to<br />
increased serum lithium levels and increased lithium toxicity. Lithium levels must,<br />
therefore, be monitored.<br />
ALLOPURINOL, IMMUNOSUPPRESSANTS, CORTICOSTEROIDS,<br />
PROCAINAMIDE, CYTOSTATICS AND OTHER SUBSTANCES THAT MAY<br />
CHANGE THE BLOOD PICTURE: Increased likelihood of haematological reactions<br />
( see also under “6: Precautions”).<br />
ANTIDIABETIC AGENT (E.G. INSULIN AND SULFONYLUREA DERIVATIVES):<br />
ACE inhibitors may reduce insulin resistance. In isolated cases, such reduction may lead<br />
to hypoglycaemic reactions in patients concomitantly treated with antidiabetics.<br />
Hydrochlorothiazide may attenuate the effect of antidiabetics. Particularly close blood<br />
glucose monitoring is, therefore, recommended in the initial phase of co-administration.<br />
8.2.4 Take into account<br />
SALT: Possible attenuation of the antihypertensive effect by increase dietary salt intake.<br />
NONSTEROIDAL ANTI-INFLAMMATORY DRUGS (e.g. INDOMETHACIN) and<br />
acetylsalicylic acid : Possible attenuation of the effect of *TM* as well<br />
as development of acute renal failure or an increase in serum potassium.<br />
PRESSOR AMINES (E.G. EPINEPHRINE): Possible attenuation of the effect of pressor<br />
amines.<br />
CORTICOSTEROIDS, CARBENOXOLONE, LARGE AMOUNTS OF LIQUORICE,<br />
LAXATIVES (IN CASE OF A PROLPNGED USE), AND OTHER KALIURETIC<br />
AGENTS: Promotion of the development of hypokalaemia.<br />
DIGITALIS PREPARATIONS: Possible intensification of digitalis toxicity as a result of<br />
changes in electrolyte concentrations (e.g. hypokalaemia, hypomagnesaemia).<br />
METHYLDOPA: Haemolysis possible.<br />
ENTERALLY ADMINISTERED ION EXCHANGERS SUCH AS<br />
COLESTYRAMINE: Reduced absorption of hydrochlorothiazide.<br />
CURARE-TYPE MUSCLE RELAXANTS: Possible intensification and prolongation of<br />
the muscular relaxing effect.<br />
ALCOHOL: Ramipril may lead to increased vasodilation and thus potentiate the effect<br />
of alcohol.
DESENSITIZATION THERAPY: The likelihood and severity of anaphylactic and<br />
anaphylactoid reactions to insect venoma is increased under ACE inhibition. It is<br />
assumed that this effect may also occur in connection with other allergens.<br />
8.2.4 Absence of pharmacokinetic drug interaction<br />
No information currently deemed necessary.<br />
9. INTERFERENCE WITH LABORATORY AND DIAGNOSTIC TEST<br />
TESTS FOR PARATHROID FUNCTION: Hydrochlorothiazide stimulates renal calcium<br />
reabsorption and may cause hypercalcaemia. This must be considered when carrying out<br />
tests for parathyroid function.<br />
10. PREGNANCY<br />
*TM* must not be taken during pregnancy. Therefore, pregnancy must be excluded<br />
before starting treatment.<br />
Pregnancy must be avoided in cases where changeover to a treatment regimen without<br />
ACE inhibitors and diuretics is not possible. Otherwise there is a risk of harm to the<br />
fetus.<br />
1<strong>1.</strong> LACTATION<br />
If treatment with *TM* is necessary during lactation, the patient must not breast feed in<br />
order to prevent the infant from ingesting small quantit<strong>ies</strong> of ramipril and<br />
hydrochlorothiazide with breast milk.<br />
12. ADVERSE REACTIONS<br />
As *TM* is an antihypertensive, many of its adverse reactions are effects secondary to its<br />
blood-pressure-lowering action which results in adrenergic counter-regulation or organ<br />
hypoperfusion. Numerous other effects (e.g. effects on electrolyte balance, certain<br />
anaphylactoid reactions or inflammatory reactions of the mucous membranes) are due to<br />
the ACE inhibition or to other pharmacologic actions of ramipril or hydrochlorothiazide.<br />
The following adverse effects have been observed during therapy with *TM*, its<br />
constituents ramipril and hydrochlorothiazide, other ACE inhibitors, or comparable<br />
diuretics, and may, therefore, occur.<br />
Blood pressure<br />
At the start of treatment in particular, symptoms such as lightheadedness – sometimes
accompanied by concentration disturbances – as well as impaired reactions, fatigue,<br />
weakness, and dizziness may occur as a result of vasodilatation, or as result of the<br />
lowering of raised blood pressure even to the desired level.<br />
Other symptoms including tachycardia ,palpitations ,disturbed orthostatic regulation,<br />
disorders of balance ,nausea ,sweating ,tinnitus ,disturbed hearing ,disturbed vision,<br />
headache , anxiety ,drowsiness and somnolence may supervene following an excessive<br />
reduction in blood pressure. Then syncope may also occur.<br />
In rare instances, cardiac arrhythmias may occur, they may be caused for example by an<br />
excessive reduction in blood pressure or by disturbances in electrolyte balance.<br />
An undesirably pronounced fall in blood pressure may occur particulary after the initial<br />
dose and after every first increased dose of *TM*.<br />
A pronounced fall in blood pressure, sometimes progressing to shock, may be more likely<br />
in patients with:<br />
●Severe and particularly with malignant hypertension.<br />
●Concomitant, and particularly with severe heart failure.<br />
●Previous diuretic therapy.<br />
●Fluid or salt depletion.<br />
●Haemodynamically relevant renal artery stenosis.<br />
Perfusin disturbances due to vascular stenoses may be exacerbated during treatment with<br />
*TM*. Mainly in patients with coronary heart disease or a haemodynamically relevant<br />
stenosis of blood vessels supplying the brain, myocardial ischaemia (e.g. with ensuing<br />
angina pectoris and myocardial infarction) or cerebral ischaemia (e.g. with ensuing<br />
transient ischaemic attack of stroke) may occur, particularly as a result of an excessive<br />
fall in blood pressure.<br />
Once an adequate blood pressure and fluid balance have been regained, treatment with<br />
*TM* can generally be continued.<br />
Kidney and electrolyte balance<br />
During treatment with *TM* , there may be a deterioration in renal function, under<br />
certain circumstances progressing to acute renal failure, particularly<br />
●In patients with renovascular disease (e.g. haemodynamically relevant renal artery<br />
stenosis).<br />
●In kidney transplant patients.<br />
●In conjunction with a more pronounced fall in blood pressure, mainly in patients with<br />
concomitant heart failure.
In isolated cases, interstitial nephritis may develop during therapy with<br />
hydrochlorothiazide.<br />
As signs of impaired renal function, serum creatinine and serum urea may increase.<br />
Pre-existing proteinuria may deteriorate (though ACE inhibitors usually reduce<br />
proteinuria). Particularly in patients with diabetics nephropathy, however, renal protein<br />
excretion may also be reduced.<br />
*TM* may cause, or contribute to a decline in serum sodium concentration, particularly<br />
in conjunction with restricted salt intake. Hydrochlorothiazide may contribute or lead to<br />
the development of hypochloraemia, hypomagnesaemia, as well as hypercalcaemia. In<br />
addition, *TM* may contribute to the development or aggravation of a metabolic<br />
alkalosis.<br />
Ramipril may cause, or contribute to an increase in the concentration of serum potassium,<br />
whereas hydrochlorothiazide may cause or contribute to a decrease in potassium<br />
concentration. Thus, during therapy with *TM*, both a decline and an increase in the<br />
concentration of serum potassium are possible, the latter effect being encountered mainly<br />
in patients with impaired renal function (e.g. due to diabetic nephropathy) or where<br />
potassium-retaining diuretics or potassium salts are administered concomitantly.<br />
General signs of disturbances in the electrolyte balance include tiredness, headache,<br />
drowsiness, sleepiness, confusion, apathy, muscle cramps, tetany, but also muscular<br />
weakness, gastrointestinal disturbances and intensified thirst.<br />
Particularly at the commencement of treatment, a transiently increased fluid excretion<br />
may occur. This may be the expression of the diuretic effect of hydrochlorothiazide, but<br />
also of cardiac recompensation. If fluid depletion develops – particularly in older<br />
patients – haemoconcentration or, in especially severe cases, thromboses may occur.<br />
Skin, blood vessels, anaphylactic and anaphylactoid reactions<br />
Angioneurotic oedema occur rarely during treatment with *TM*. They are due to the<br />
desired ACE inhibition, and necessitate immediate discontinuation of *TM* therapy;<br />
other ACE inhibition of similar combination preparations are also ruled out in such cases.<br />
Angioneurotic oedema, for example, of the tongue, throat of larynx may become lifethreatening<br />
and necessitate emergency measures.<br />
Milder non-angioneurotic oedema, e.g., involving the ankle, are also possible.<br />
Uncommonly, pharmacologically mediated mild angioneurotic oedema may occur (the<br />
incidence of ACE inhibitor angio-oedema seems to be increased in black, i.e. Afro-<br />
Caribbean, patients as compared with non-black patients). Serious reactions of this type<br />
and other, not pharmacologically mediated anaphylactic or anaphylactoid reactions to<br />
ramipril or any of the other ingredients are rare.
In addition, the following cutaneous of mucosal reactions may occur, e.g., as<br />
manifestations of an allergic reacton: reddening of skin areas with accompanying heat<br />
sensation, conjunctivitis, pruritus and urticaria; rarely, reactions such as maculopapular<br />
and lichenoid exanthema and enanthema, erythema multiform, Stevens-johnson<br />
syndrome,toxic epidermal necrolysis alopecia, hypersensitivity of the skin to light ,and<br />
precipitation or intensification of Raynaud’s phenomenon may also occur.<br />
With other ACE inhibitors, pemphigus,exacerbation of psoriasis, psoriasiform or<br />
pemphigoid exanthema and enanthema, and onycholysis have been observed.<br />
Anaphylactic reactions to hydrochlorothiazide are possible.<br />
In the event of pruritus with urticaria, the patient must inform a physician immediately.<br />
The likelihood and the severity of anaphylactic and anaphylactoid reaction to insect<br />
venoma is increased under the influence of ACE inhibitors. It is assumed that this effect<br />
may also occur in conection with other allergens.<br />
This must be considered when desensitization is performed.<br />
Respiratory Tract<br />
Due possibly to ACE inhibition, a dry (non-productive) tickling cough frequently occurs.<br />
This is often worse at night and when the patient is lying down and occurs more<br />
frequently in women and non-smokers. In some cases a changeover to another<br />
ACE inhibitor is successful. However, the cough may force patients to stop taking ACE<br />
inhibitors altogether.<br />
Also possibly due to ACE inhibition, nasal congestion, rhinitis, sinusitis, bronchitis and,<br />
especially in patients with tickling cough, bronchospasm and dyspnoea may occur.<br />
Administration of hydrochlorothiazide may include pneumonitis and pulmonary oedema,<br />
presumably due to an allergic reaction.<br />
In the event dyspnoea develops or worsens, the patient must inform a physician<br />
immediately.<br />
Digestive tract,liver<br />
Uncommonly, nausea, increases in serum levels of hepatic enzymes and/or bilirubin as<br />
well as cholestatic jaundice may occur. Rarely, dryness of the mouth, glossitis,<br />
inflammatory reactions of the oral cavity and gastrointestinal tract, abdominal discomfort,<br />
gastric pain (including gastritic-like gastric pain), digestive disturbances, constipation,<br />
diarrhoea, vomiting and increased levels of pancreatic enzymes may develop. In isolated<br />
cases, pancreatitis, or liver damage (including acute liver failure) may occur.
Blood picture<br />
The following blood picture changes may occur: a mild –severe reduction in the red<br />
blood cell count and haemoglobin content (in isolated instances also due to haemolytic<br />
anaemia) , blood platelet count and white blood cell count (even presenting as<br />
neutropenia), agranulocytosis, bone marrow depression and pancytopenia.<br />
Such changes of the blood picture are more likely to occur in patients with impaired<br />
renal function and in patients with concomitant collagen disease (e.g. lupus<br />
erythematosus or scleroderma) or in patients treated with other drugs that may cause<br />
changes of the blood picture. See also under “Interactions” and “Special warning and<br />
precautions”.<br />
In isolated cases, haemolytic anaemia may develop.<br />
Other adverse effects<br />
Peripheral oedema, flushing,disturbances of balance, visual disorders, headache,<br />
nervousness, restlessness, tremor, sleep disturbances, confusion, loss of appetite,<br />
depressed mood, feeling of anxiety, paraesthesiae, taste change (e.g. metallic taste), taste<br />
reduction and sometimes even loss of taste, smell disturbances, muscle cramps as well as<br />
erectile impotence and reduced libido may occur.<br />
The possibility of exacerbation of activation of systemic lupus erythmatosus has been<br />
reported.<br />
Vasculitis, myalgia, arthalgia, fever and eosinophilia may also occur. Raised titres of<br />
antinuclear antibod<strong>ies</strong> may occur . In temporal relationship with the administration of<br />
hydrochlorothiazide, the development of a lupus erythematosus has been described.<br />
During therapy with hydrochlorothiazide- and thus with *TM*- increased serum<br />
concentrations of uric acid may occur. This may lead to gout attacks, particularly in those<br />
patients whose uric acid levels are already elevated.<br />
Hydrochlorothiazide may lower tolerance to glucose. In patients with diabetes mellitus,<br />
this may lead to a deterioration of the metabolic control. A latent diabetes mellitus may<br />
become manifest for the first time.<br />
Hydrochlorothiazide may cause an increase in serum cholesterol and triglycerides.<br />
13. OVERDOSE<br />
Symptoms<br />
Possible signs and symptoms of overdose included: persistent diuresis excessive<br />
peripheral vasodilatation (with marked hypotension, shock), bradycardia, ,renal failure<br />
electrolyte disturbances, cardiac arrhythmias, impairment of consciousness up to and<br />
including coma, cerebral convulsions, pareses and paralytic ileus.
In patients with obstruction of urinary outflow (e.g. from prostatic hyperplasia), sudden<br />
diuresis may induce acute urinary retention with overdistension of the bladder.<br />
Management<br />
The treatment given depends on how and when the drug was taken and on the type and<br />
severity of symptoms.<br />
Steps must be taken to eliminate any *TM* which has not yet been absorbed (e.g. gastric<br />
lavage, administration of adsorbants, sodium sulfate, if possible during the first 30<br />
minutes). Vital and organ functions must be monitored under intensive care conditions,<br />
and safeguarded if necessary. Monitoring must also include frequent checks of water,<br />
electrolyte and acid -base balance. In the event of hypotension administration of<br />
α1-adrenergic agonists (e.g. norepinephrine, dopamine) and angiotensin II<br />
(angiotensinamide) must be considered in addition to volume and salt substitution.<br />
No experience is available concerning the efficacy of forced diuresis, altering urine pH,<br />
haemofiltration or dialysis in speeding up the elimination of ramipril or ramipirilat. If<br />
dialysis or haemofiltration is nevertheless contemplated, see also under<br />
“Contraindications”.<br />
Hydrochlorothiazide is dialyzable.<br />
14. ABUSE AND DEPENDENCE<br />
Not applicable.<br />
15. PHARMACODYNAMICS<br />
*TM* has antihypertensive and diuretic effects. Ramipiril and hydrochlorothiazide are<br />
used singly or together for antihypertensive therapy. The antihpertensive effects of both<br />
substances are complementary.<br />
The blood-pressure-lowering effects of both components are approximately additive.<br />
Whereas the loss of potassium which accompan<strong>ies</strong> the action of hydrochlorothiazide is<br />
attenuated through the use of ramipril.<br />
Mode of action<br />
Ramipril: Ramiprilat, the active metabolite of the prodrug ramipril, inhibits the enzyme<br />
dipepitdylcarboxypeptidase I (synonyms: angiotensin – converting enzyme, kininase II).<br />
In plasma and tissue this enzyme catalyses the conversion of angiotensin I to the active<br />
vasodilatator bradykinin.
Reduced angiotensin II formation and inhibition of bradykinin breakdown lead to<br />
vasodilatation.<br />
Since angiotensin II also stimulates the release of aldosterone, ramiprilat causes a<br />
reduction in aldosterone secretion. The increase in bradykinin activity probably<br />
contributes to the cardioprotective and endothelioprotective effects observed in animal<br />
experiments. It has not yet been established to what extent this is also responsible for<br />
certain unwanted effects (e.g. tickling cough).<br />
ACE inhibitors are effective even in patients with low-renin hypertension. The average<br />
response to ACE inhibitor monotherapy was lower in black (Afro-Caribbean)<br />
hypertensive patients (usually a low-renin hypertensive population) than in non-black<br />
patients.<br />
Hydrochlorothiazide: Hydrochlorothiazide is a thiazide diuretic. It inhibits the<br />
reabsorption of sodium and chloride in the distal tubule. The increase renal excretion of<br />
these ions is accompanied by increased urine output (due to osmotic binding of water).<br />
Potassium and magnesium excretion are increased, uric acid excretion is decrease. High<br />
doses lead to increased excretion of bicarbonates, and long-term treatment decreases the<br />
excretion of calcium.<br />
Possible mechanisms of the antihypertensive action of Hydrochlorothiazide could be: the<br />
modified sodium balance, the reduction in extracellular water and plasma volume, a<br />
change in renal vascular resistance as well as a reduced response to norepinephrine and<br />
angiotensin II.<br />
Pharmacodynamic characteristics<br />
Ramipril: administration of ramipiril causes a marked reduction in peripheral arterial<br />
resistance. Generally, these are no major changes in renal plasma flow and glomerular<br />
filtration rate.<br />
Administration of ramipril to patients with hypertension leads to a reduction in supine<br />
and standing blood pressure without a compensatory rise in heart rate.<br />
In most patients the onset of the antihypertensive effect of a single dose becomes<br />
apparent 1 to 2 hours after oral administration. The peak effect of a single dose is usually<br />
reached 3 to 6 hours after oral administration. The antihypertensive effect of a single dose<br />
usually lasts for 24 hours.<br />
The maximum antihypertensive effect of continued treatment with ramipril is generally<br />
apparent after 3 to 4 weeks. It has been shown that the antihypertensive effect is sustained<br />
under long term therapy lasting 2 years.<br />
Abrupt discontinuation of ramipril does not produce a rapid and excessive rebound<br />
increase in blood pressure.
Hydrochlorothiazide: Electrolyte and water excretion starts approx. 2 hours after<br />
administration, reaches its peak after 3 to 6 hours and lasts from 6 to 12 hours.<br />
The onest of the antihypertensive effect occurs after 3 to 4 days and can last up to one<br />
week after discontinuation of therapy.<br />
16. PHARMACOKINETICS<br />
Ramiprill: The prodrug ramipril undergoes an extensive hepatic first pass metabolisim,<br />
which is essential for the formation of the sole active metabolite ramiprilat (hydrolysis,<br />
which occurs principally in the liver). In addition to this activation into ramiprilat,<br />
ramipril is glucuronized and transformed into ramipril diketopiperazine (ester).<br />
Ramiprilat is glucuronized as well and transformed into ramiprilat diketopiperazine<br />
(acid).<br />
As a result of this activation/metabolization of the prodrug, approx 20% of orally<br />
administered ramipril is bioavailable.<br />
The bioavailability of ramiprilat after oral administration of 2.5 and 5mg. Ramipril is<br />
approx. 45% compared with its availability after intravenous administration of the same<br />
doses.<br />
Following oral administration of 10mg. Of radioactive labelled ramipiril, approx. 40% of<br />
total radioactivity is excreted in faeces and approx. 60% in urine. After intravenous<br />
administration of ramipril, approx. 50 to 60% of the doses have been detected in urine (as<br />
ramipril and metabolites); aprox. 50% were eliminated apparently by non-renal routes.<br />
Following intravenous administration of ramiprilat approx. 70% of the substance and its<br />
metabolites have been found in urine – indicating non-renal ramiprilat elimination of<br />
approx. 30% . After oral administration of 5mg ramipril in patients with drainage of the<br />
bile ducts, approx. the same amount of ramipril and its metabolites was excreted in urine<br />
and bile during the first 24 hours.<br />
Approx. 80 to 90% of the metabolites in urine and bile have been identified as ramiprilat<br />
of ramiprilat metabolites. Ramipril glucuronide and ramipril diketopiperazine represented<br />
approx. 10 to 20% of the total amount, whereas unmetabolized ramipril accounted for<br />
approx. 2%.<br />
Stud<strong>ies</strong> in lactating animals have shown that ramipril passes into the milk.<br />
Ramipril is rapidly absorbed after oral administration. As measured by the recovery of<br />
radioactivity in the urine, which represent only one of the elimination routes, absorption<br />
of ramipril is at least 56% .Administration of ramipril at the same time as food has no<br />
relevant effect on absorption.<br />
Peak plasma concentrations of ramipril are reached within 1 hour after oral<br />
administration. The elimination half-life of ramipril is approx. 1 hour. Peak plasma<br />
concentrations of ramipirilat are reached 2 to 4 hours after oral administration of ramipril.<br />
Plasma concentrations of ramiprilat decline in a polyphasic manner. The initial<br />
distribution and elimination phase has a half-life of approx. 3 hours. It is followed by an
intermediate phase (half-life approx. 15 hours) and a terminal phase with very low<br />
plasma ramiprilat concentrations and half-life of approx. 4 to 5 days.<br />
This terminal phase is due to the slow dissociation of ramiprilat from the close but<br />
saturable binding to ACE.<br />
Despite this long terminal phase, a single daily dose of 2.5mg. ramipril of more yields<br />
steady state plasma concentrations of ramiprilat after approx. 4 days. The “effective”<br />
half-life, which is relevant for dosage, is 13 to 17 hours under multiple-dose conditions.<br />
After intravenous administration the systematic distribution volume of ramipril is approx.<br />
90 liters, and the relative systemic distribution volume of ramiprilat is approx. 500 liters.<br />
In-vitro stud<strong>ies</strong> have shown an overall inhibitory constant of ramiprilat of 7 pmol/l and a<br />
dissociation half-life of ramiprilat from ACE of 10.7 hours, which indicates high potency.<br />
The protein-binding of ramipril and ramiprilat is approx. 73% and approx. 56%<br />
respectively.<br />
In healthy subjects aged between 65 and 76 years ramipril and ramiprilat kinetics are<br />
similar to those in healthy young Subjects.<br />
Renal excretion of ramiprilat is reduced in patients with impaired renal function, and<br />
renal ramiprilat clearance is proportionally related to creatinine clearance. This results in<br />
elevated plasma concentrations of ramiprilat, which decrease more slowly than in persons<br />
with normal renal function.<br />
When high doses (10mg.) of ramipril are administered, impairment of hepatic function<br />
retards the activation of ramipril into ramiprilat, resulting in increased ramipril plasma<br />
levels, and slows down the elimination of ramiprilat.<br />
As in healthy persons and patients with hypertension, there was also no relevant<br />
accumulation of ramipril and ramipirlat after oral administration of 5mg. ramipril once<br />
daily over two weeks in patients with congestive heart failure.<br />
Hydrochlorothiazide: Approx. 70% of hydrochlorothiazide is absorbed after oral<br />
administration; the bioavailability of hydrochlorothiazide after oral administration is<br />
approx. 70%<br />
Peak plasma concentrations of 70 ng/ml were reached <strong>1.</strong>5 to 4 hours after oral<br />
administration of 12.5mg. of hydrochlorothiazide, peak concentrations of 142 ng/ml 2 to<br />
5 hours after oral administration of 25mg. Hydrochlorothiazide, and peak concentrations<br />
of 260 ng/ml 2 to 4 hours after oral intake of 50mg.<br />
Hydrochlorothiazide. Approx. 40% hydrochlorothiazide is bound to plasma proteins.<br />
Hydrochlorothiazide is excreted almost quantitatively (more than 95%) by renal route
in unchanged form. After oral administration of a single dose, 50 to 70% is excreted<br />
within 24 hours. Detectable amounts of the substance appear in the urine as early as 60<br />
minutes after intake.<br />
The elimination half-life is 5 to 6 hours. In renal insufficiency excretion is reduced and<br />
the half-life prolonged. Renal clearance of hydrochlorothiazide correlates closely with<br />
creatinine clearance. In patients with glomerular filtration rates less than 10 ml/min only<br />
10% of the administered dose was found in the urine. More recent stud<strong>ies</strong> indicate that<br />
some of the drug is excreted via non-renal routes (bile).<br />
Hydrochlorothiazide passes into breast milk in small quantit<strong>ies</strong>.<br />
No relevant changes in the pharmacokinetics of hydrochlorothiazide have been noted in<br />
liver cirrhosis. Stud<strong>ies</strong> on pharmacokinetics in patients with heart failure are not<br />
available.<br />
Ramipril + hydrochlorothiazide: Concurrent administration of ramipril and<br />
hydrochlorothiazide has no influence on the bioavailability of the single components.<br />
The fixed dose combination tablet of 5mg. Ramipril and 25mg. Hydrochlorothiazide and<br />
the free combination of 5mg. Ramipril and 25 mg. Hydrochlorothiazide capsules may be<br />
considered bioequivalent.<br />
17. NON-CLINICAL SAFTEY DATA<br />
Acute toxicity:<br />
Ramipril: as it has an LD50 in excess of 10,000 mg/kg Body weight in mice and rats and<br />
above 1000 mg/kg body weight in beagle hounds, oral administration of ramipril has<br />
been found to be devoid of acute toxicity.<br />
Hydrochlorothiazide: In stud<strong>ies</strong> on acute toxicity in mice, the LD50 (after oral<br />
administration) was in excess of 10,000 mg/kg body weight and 884 mg/kg body weight<br />
after intravenous administration.<br />
In rats the acute LD50 oral administration was in excess of 10,000 mg/kg body weight,<br />
and after intraperitoneal administration it was 3130 mg/kg body weight.<br />
In rabbits the acute LD50 after intravenous administration was 461 mg/kg body weight<br />
and in dogs it was approx. 1000 mg/kg body weight. Dogs tolerated 2000 mg/kg body<br />
weight or more after oral administration without showing any signs of toxicity.<br />
Ramipril + Hydrochlorothiazide: The oral LD50 in rats and mice is in excess of 10,000<br />
m./kg body weight , i.e., the combination ramipril + Hydrochlorothiazide
(1:5) is totally devoid of acute toxicity. This is consistent with the results of acute<br />
toxicity. This is consistent with the results of acute toxicity testing of the single<br />
components.<br />
Chronic toxicity<br />
Ramipril: Stud<strong>ies</strong> involving chronic administration have been conducted in rats, dogs and<br />
monkeys. In rats, daily doses of the order of 40 mg/kg body weight lead to shifts in<br />
plasma electrolytes and to anaemia. At daily doses of 3.2 mg/kg body weight or higher<br />
there was some evidence of changes in renal morphology (distal tubular atrophy).<br />
However, these effects can be explained in pharmacodynamic terms and are characteristic<br />
of the substance class. Daily doses of 2 mg/kg body weight have been tolerated by rats<br />
without toxic effects. Tubular atrophy is encountered in rats, but not in dogs and<br />
monkeys.<br />
As an expression of the pharmacodynamic activity of ramipril (a sign of increased renin<br />
production as a reaction to reduced angiotensin II formation) ,pronounced enlargement of<br />
the juxtaglomerular apparatus has been noted in the dog and monkey – especially at daily<br />
doses of 250 mg/kg body weight or higher. Indication of plasma electrolyte shifts and<br />
changes in blood picture have also been found in the dog and monkey. Dogs and<br />
monkeys tolerated daily doses of 2.5 mg/kg body weight and 8 mg/kg body weight<br />
respectively without harmful effects.<br />
Hydrochlorothiazide: Subchronic (subacute) oral toxicity stud<strong>ies</strong> in rats with 500, 1000<br />
and 2000 mg/kg per body weight daily (five days a week over a total period of three<br />
weeks) yielded no signs of a toxic drug effect: such fatalit<strong>ies</strong> as occurred were attributed<br />
to pneumonia.<br />
In stud<strong>ies</strong> conducted in dogs receiving 250, 500 and 1000 mg/kg per body weight daily<br />
over a period of eight weeks, no serious effects of the drug were noted with the exception<br />
of an imbalance in electrolytes.<br />
Chronic toxicity stud<strong>ies</strong> in rats receiving oral doses of up to 2000 mg/kg per body weight<br />
daily five days a week over a period of 26 weeks revealed no signs of a toxic drug effect<br />
and no alterations attributable to the drug were noted during the drug were noted during<br />
the post-mortem investigations.<br />
Dogs received doses of 125,250 and 500 mg/kg per body weight daily over a period of 26<br />
weeks (in the 500 mg. group, however, the medication was interrupted after the 7 th .<br />
weeks for 11 weeks).<br />
A slight reduction in plasma potassium occurred. Further, in the course of the<br />
macroscopic investigation, small quantit<strong>ies</strong> of yellow crystalline precipitates were found<br />
in the bladders of 2 of the 12 dogs. Histomorphological investigations revealed no<br />
disturbances attributable to the drug.<br />
Ramipril + Hydrochlorothiazide: with the exception of disturbances in electrolyte<br />
balance, stud<strong>ies</strong> conducted in rats and monkeys yielded no conspicuous findings.
Reproduction toxicology<br />
Ramipril: Reproduction toxicology stud<strong>ies</strong> in the rat, rabbit and monkey did not disclose<br />
any teratogenic propert<strong>ies</strong>.<br />
Fertility was not impaired either in male or in female rats.<br />
The administration of ramipril to female rats during the fetal period and lactation<br />
produced irreversible renal damage (dilatation of the renal pelvis) in the offspring at<br />
doses of 50 mg/kg body weight or higher.<br />
When ACE inhibitors have been administered to women in the second and third trimester<br />
of pregnancy, there have been reports of harmful effects on the fetus and newborn child,<br />
including – sometimes in conjunction with oligohydramnios (presumably as an<br />
expression of impaired fetal renal function) – craniofacial deformit<strong>ies</strong>, pulmonary<br />
hypoplasias, fetal limb contractures, hypotension, anuria reversible and irreversible renal<br />
failure as well as death. Prematurity, intrauterine growth retardation and persistence of<br />
Botallo’s duct have also been reported in humans, although it is uncertain whether these<br />
phenomena are a consequence of exposure to ACE inhibitors.<br />
Hydrochlorothiazide: In animal stud<strong>ies</strong>, hydrochlorothiazide crosses the placenta.<br />
Stud<strong>ies</strong> conducted in mice, rats and rabbits yielede no indication of teratogenic effect.<br />
Experience is available in humans on the use of the drug in more than 7,500 pregnant<br />
women. Of these, 107 had taken hydrochlorothiazide during the first trimester.<br />
It is suspected that neonatal thrombopenia may develop following administration of<br />
Hydrochlorothiazide in the second half of pregnancy.<br />
It is possible that disturbances in electrolyte balance in pregnant women may effect the<br />
fetus.<br />
Ramipril + Hydrochlorothiazide: in stud<strong>ies</strong> on embryotoxicity, the combination was<br />
administered during the sensitive phase of organogenesis: to rats in daily doses of 1, 10,<br />
150, 600 or 2400 mg/kg body weight, and to rabbits in daily doses of 0.96, 2.40 or 6.00<br />
mg/kg body weight.<br />
Hydrochlorothiazide has been stud<strong>ies</strong> in a similar way alone at daily doses of 125,500 or<br />
2000 mg/kg body weight in rats, and at a daily dose of 2 mg/kg body weight in rabbits;<br />
these doses corresponded to the proportions of hydrochlorothiazide contained in the high<br />
doses of the combination.<br />
The stud<strong>ies</strong> in rats shows that dams tolerated the combination administered at dose levels<br />
of 1 mg/kg and 10mg/km body weight without complications. Doses of 150 mg/kg body
weight and above showed toxic effects on dams and led to reduced food intake and<br />
weight development. Heart and liver weights were reduced. Clinical symptoms of<br />
toxicity and deaths occurred at dose levels of 2400 mg/kg body weight.<br />
At dose levels of 150 mg/kg body weight and above, urine excretion increased and after<br />
2400 mg/kg body weight kidney weights were slightly increased. These effects are<br />
attributable to the pharmacodynamic action of hydrochlorothiazide.<br />
1 mg/kg body weight does not impair the development of the embryo. Doses of<br />
10 mg/kg body weight and above led to a slight retardation in development of the fetus,<br />
which manifested itself in delayed skeletal ossification and, at dose levels of<br />
150 mg/kg body weight and above, in reduced body weight and reduced body length.<br />
Placenta weight was also reduced.<br />
Morphological investigations conducted in fetuses revealed increased occurrences of<br />
dilatation of the renal pelvis and the ureter as well as waved thickened ribs at dose levels<br />
of 150 mg/kg body weight and above and, at levels of 600 mg/kg body weight and<br />
above, bent and shortened scapula and bones of the limbs.<br />
The stud<strong>ies</strong> with hydrochlorothiazide alone confirm that the retardation of fetal growth is<br />
attributable to the diuretic. The other findings point to a joint effect of the two single<br />
components in the combination.<br />
Administration of the combination in rabbits at dose levels of 0.96mg/kg body weight led<br />
to a slight reduction in food intake and stagnation in body weight. However , it had no<br />
adverse effect on the intrauterine development in the progeny.<br />
Following administration at dose levels of 2.40 and 6.00mg/kg body weight , the dams<br />
reduced their intake of food and water and lost weight; furthermore ,deaths and<br />
spontaneous abortions occurred at these dose levels and living fetuses showed slightly<br />
retarded growth at birth. No signs of external anomal<strong>ies</strong> or of anomal<strong>ies</strong> affecting internal<br />
organs and skeleton of the fetuses were detected which could be attributed to<br />
administration of the combination.<br />
Hydrochlorothiazide alone administered at daily doses of 2 mg/kg body weight was<br />
tolerated by the dams and their fetuses.<br />
The two stud<strong>ies</strong> in rats and rabbits revealed that the combination is somewhere more<br />
toxic than either of the single components, but none of the stud<strong>ies</strong> revealed any signs of a<br />
teratogenic effect of the combination or of hydrochlorothiazide.<br />
Stud<strong>ies</strong> were conducted in rats to determine the peri-and postanal toxicity of the<br />
combination doses of 10 and 60 mg/kg body weight daily were given orally during the<br />
last third of pregnancy and during the 3 weeks of lactation. At doses of<br />
10 mg/kg body weight, the drug neither had an adverse effect on the dams’general<br />
condition, the course of pregnancy of parturition , nor did it lead to a disturbance of<br />
intrauterine and postnatal development of the progeny.
After administration of 60 mg/kg body weight, the dams reduced food intake slightly, and<br />
the pups showed slightly reduced weights at birth and during the first week thereafter. In<br />
the subsequent period, the postnatal development of the pups turned up no conspicuous<br />
findings. The incidence of dilatation of the renal pelvis (such as has been noted following<br />
higher doses of ramipril) was not increased.<br />
Stud<strong>ies</strong> on possible impairment of fertility and reproductive capability were not<br />
conducted with the combination, since no toxic effect was to be excepted on the basis of<br />
results in the single components.<br />
Immunotoxicology<br />
Ramipril: toxicology stud<strong>ies</strong> have yielded no indication that ramipril possesses any<br />
immunotoxic effects.<br />
Mutagenicity<br />
Ramipril: Extensive mutagenicity testing using several test systems has yielded no<br />
indication that ramipril possesses mutagenic or genotoxic propert<strong>ies</strong>.<br />
Hydrochlorothiazide: there is limited evidence of genotoxicity of hydrochlorothiazide<br />
In virto. It may be deduced from in vivo data that the substance is not mutagenic.<br />
Ramipril + Hydrochlorothiazide: mutagenicity stud<strong>ies</strong> were not conducted with the<br />
combination since the results of tests with each component alone have shown no<br />
evidence of any such risk.<br />
Carcinogenicity:<br />
Ramipril: Long –term stud<strong>ies</strong> in rat and mouse have yielded to indication of any<br />
tumorigenic effect.<br />
Renal tubules with oxyphilic cells and tubules with oxyphilic cellular hyperplasia in rats<br />
are regarded as respone to functional alterations and morphological changes, and not as a<br />
neoplastic or pre-neoplastic respone.<br />
Hydrochlorothiazide: A carcinogenicity study with hydrochlorothiazide in mice yielded<br />
equivocal evidence of carcinogenic activity in male animals at high doses (in the form of<br />
an increased incidence of hepatocellular neoplasis). There was no evidence of<br />
carcinogenicity in female mice. A study with hydrochlorothiazide in male and female rats<br />
also yielded no evidence of carcinogenic potential.<br />
Summarizing these findings, it may be assumed that hydrochlorothiazide lacks any<br />
neoplastic potential.
Ramipril + hydrochlorothiazide: carcinogenicity stud<strong>ies</strong> were not conducted with the<br />
combination since the results of test with each component alone have shown no evidence<br />
of any such risk.<br />
Manufacturer: Aventis Pharma Germany.<br />
Importer: Aventis Pharma Ltd., P.O.B. 8090, Netanya 42170.