营养代谢疾病
营养代谢疾病
营养代谢疾病
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>营养代谢疾病</strong><br />
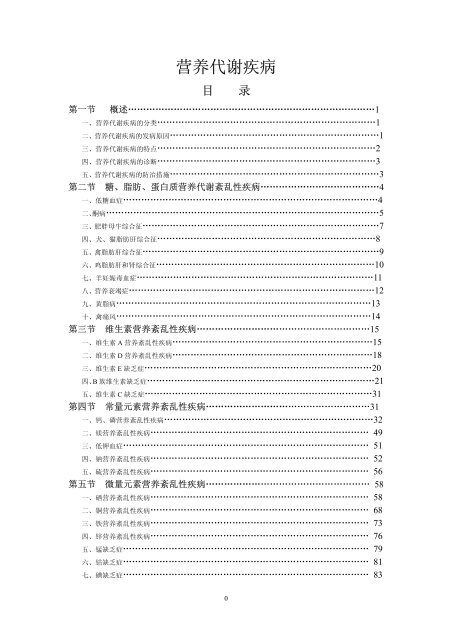
目 录<br />
第一节 概述………………………………………………………………………1<br />
一、<strong>营养代谢疾病</strong>的分类………………………………………………………………1<br />
二、<strong>营养代谢疾病</strong>的发病原因……………………………………………………………1<br />
三、<strong>营养代谢疾病</strong>的特点………………………………………………………………2<br />
四、<strong>营养代谢疾病</strong>的诊断………………………………………………………………3<br />
五、<strong>营养代谢疾病</strong>的防治措施……………………………………………………………3<br />
第二节 糖、脂肪、蛋白质营养代谢紊乱性疾病…………………………………4<br />
一、低糖血症…………………………………………………………………………4<br />
二、酮病………………………………………………………………………………5<br />
三、肥胖母牛综合征……………………………………………………………………7<br />
四、犬、猫脂肪肝综合征………………………………………………………………8<br />
五、禽脂肪肝综合征……………………………………………………………………9<br />
六、鸡脂肪肝和肾综合征………………………………………………………………10<br />
七、羊妊娠毒血症……………………………………………………………………11<br />
八、营养衰竭症………………………………………………………………………12<br />
九、黄脂病…………………………………………………………………………13<br />
十、禽痛风…………………………………………………………………………14<br />
第三节 维生素营养紊乱性疾病…………………………………………………15<br />
一、维生素 A 营养紊乱性疾病…………………………………………………………15<br />
二、维生素 D 营养紊乱性疾病…………………………………………………………18<br />
三、维生素 E 缺乏症…………………………………………………………………20<br />
四、B 族维生素缺乏症…………………………………………………………………21<br />
五、维生素 C 缺乏症…………………………………………………………………31<br />
第四节 常量元素营养紊乱性疾病………………………………………………31<br />
一、钙、磷营养紊乱性疾病……………………………………………………………32<br />
二、镁营养紊乱性疾病……………………………………………………………… 49<br />
三、低钾血症……………………………………………………………………… 51<br />
四、钠营养紊乱性疾病……………………………………………………………… 52<br />
五、硫营养紊乱性疾病……………………………………………………………… 56<br />
第五节 微量元素营养紊乱性疾病……………………………………………… 58<br />
一、硒营养紊乱性疾病……………………………………………………………… 58<br />
二、铜营养紊乱性疾病……………………………………………………………… 68<br />
三、铁营养紊乱性疾病……………………………………………………………… 73<br />
四、锌营养紊乱性疾病……………………………………………………………… 76<br />
五、锰缺乏症……………………………………………………………………… 79<br />
六、钴缺乏症……………………………………………………………………… 81<br />
七、碘缺乏症……………………………………………………………………… 83<br />
0
第二章 <strong>营养代谢疾病</strong><br />
第一节 概 述<br />
<strong>营养代谢疾病</strong>是营养紊乱和代谢紊乱疾病的总称。前者是因动物所需的某些营养物质的<br />
量供给不足或缺乏,或因某些营养物质过量而干扰了另一些营养物质的吸收和利用引起的疾<br />
病。后者是因体内一个或多个代谢过程异常改变导致内环境紊乱引起的疾病。<br />
现代生产中,人们从追求“高产出”目标出发,常常使动物的摄入不能完全满足体内代<br />
谢过程的需要,造成代谢失调。有人倾向于把它们称为生产病(productive disease)。<br />
一、<strong>营养代谢疾病</strong>的分类<br />
为了叙述方便,现在把<strong>营养代谢疾病</strong>分为:<br />
1.糖、脂肪、蛋白质代谢紊乱性疾病 例如乳牛的酮病、母畜妊娠毒血症、禽痛风、脂<br />
肪肝综合征、黄脂病、营养衰竭症等。<br />
2.维生素营养缺乏症 是因饲料中维生素供给不足,或因含有某些维生素拮抗剂,造成<br />
代谢过程中因维生素摄入不足,体内必需的辅酶生成不足而致代谢失调。如VA缺乏、VD缺<br />
乏、复合VB缺乏等等。<br />
3.矿物质营养缺乏症 矿物质不仅是机体硬组织的构成成分,而且是某些维生素和酶的<br />
构成成分。常见的矿物质营养缺乏症包括 7 种常量元素缺乏,如骨软症、低镁血症、低钾血<br />
症、低钠血症;15 种必需微量元素缺乏症,如铜缺乏症、硒缺乏症、锰缺乏症等。<br />
4.原因未定的<strong>营养代谢疾病</strong> 有些病不像是传染病,也不像是中毒或寄生虫病,它们符<br />
合营养代谢病的某些特点,但病因不明确。如肉用仔鸡腹水症、啄癖等。<br />
至于因遗传缺陷,引起内分泌失调造成的代谢紊乱,兽医学界把这类疾病列入动物遗传<br />
性疾病。水盐代谢紊乱性疾病,除了钾、钠缺乏症本书略有介绍外,多列入外科学或其它器<br />
官疾病中介绍。<br />
然而,营养与代谢,各种营养物质之间的关系又是互相影响、互相依存的。蛋白质是构<br />
成酶的基本成分,金属离子是许多酶的活性中心,维生素又是辅酶的主要构成成分,只有按<br />
动物需要,依一定比例供给,才能保证动物有最大生长速度和最佳的饲料报酬。<br />
二、<strong>营养代谢疾病</strong>的发病原因<br />
引起<strong>营养代谢疾病</strong>的原因主要有以下几方面。<br />
1.营养物质摄入不足 日粮不足,或日粮中缺乏某种营养物质。如缺硒地区的硒缺乏症,<br />
锰缺乏症、维生素 A 缺乏等。随着我国畜禽饲养方式改变,规模饲养和集约化经营逐步取<br />
代传统的庭院式饲养,各种高产、高周转速率、高饲料报酬品种被引进和饲养,基因工程技<br />
术发展,将培育出生长更快的动物,一旦在饲料供给、日粮配合中略有疏忽,就可造成某些<br />
营养物质摄入不足,产生疾病。<br />
2.营养物质消化、吸收不良,利用不充分 长期患某些慢性病、胃肠道、肝脏及胰腺等<br />
机能障碍,年老体弱,机能减退,不仅影响营养物质的消化吸收,而且影响营养物质在动物<br />
体内合成代谢。<br />
3.营养物质转化需求过多 近代畜牧业已把以生产人类食品为主要目标的动物,如乳<br />
牛、肉牛、羔羊、肉鸡、蛋鸡等生产纳入工业生产范畴(animal industry),它与工业生产一<br />
样,存在三个环节:原料供给(input),加工转化(throughput),产品投放(output)市场。<br />
为了追求高产出这一目标,育种学家培育出一代又一代高产优良品种,而这些品种对饲料配<br />
合的要求、对环境控制要求也更加严格,科学管理水平稍有疏忽,就很难使这三个环节以高<br />
效高速运转。有人曾作比较,1938~1939 年间,平均每头牛年产 2300L 乳。1966~1967 年间<br />
平均年产乳 3600L,1976 年平均年产 4550L,目前高产乳牛已达 6800~10000L。蛋白质转化<br />
率已从 27%增加至 38%以上,在这样高产出、高转化速率、高报酬的条件下,在饲料投入<br />
1
的量,各种营养成分的含量和比例,各项管理措施等,稍有疏忽或失误,就可引起营养代谢<br />
疾病。<br />
由此可见,在现代畜牧业中,产生<strong>营养代谢疾病</strong>的最主要原因是:在追求高产前提下,<br />
营养供给(input)与产出(output)之间平衡失调,或因管理方面失误,造成机体内、外环<br />
境平衡(throughout)失调,最终产生了代谢紊乱。<br />
三、<strong>营养代谢疾病</strong>的特点<br />
营养代谢性疾病种类繁多,发病机理复杂,但它们的发生、发展、临诊经过方面有一些<br />
共同特点:<br />
1.病的发生缓慢,病程一般较长 从病因作用到呈现临床症状一般都需数周、数月、甚<br />
至更长的时间,有的可能长期不出现明显临床症状而成为隐性型。如人为地减少饲料中钙的<br />
含量,1~2 月后能呈现骨软症早期轻微的临床症状,人工食饵造成鼠维生素缺乏症,64 天呈<br />
典型的临床症状,自然情况下发病可能更慢。<br />
2.发病率高,多为群发,经济损失严重 过去畜禽主要为散养、粗养,<strong>营养代谢疾病</strong>并<br />
不引起人们注意,随着畜牧生产高速发展和生产方式高度集约化,且一些传染病逐步得到控<br />
制,营养代谢性疾病已成为重要的群发病,遭受的损失愈发严重。如仔猪缺铁发生贫血、水<br />
肿病、幼畜白肌病等可在一个牧场或专业户内大群发病,生长发育受明显影响。严重者能造<br />
成畜禽大批死亡。<br />
3.生长速度快的畜禽、处于妊娠或泌乳阶段特别是乳产量高的家畜、幼畜禽容易发生,<br />
舍饲时容易发生。如猪的缺铁、缺硒均以幼龄阶段为多发,这主要由于此阶段抗病力相对较<br />
弱,同时正处于生长发育、代谢旺盛阶段,对营养物质的需求量相对增加,以致对某些特殊<br />
营养物质的缺乏尤为敏感。高产乳牛饲养管理不当易发生酮病。舍饲畜禽因光照不足易发生<br />
维生素 D 缺乏,继而致使钙磷代谢障碍出现的佝偻病等。<br />
4.多呈地方性流行 动物营养的来源主要是从植物性饲料及部分从动物饲料中所获得<br />
的,植物性饲料中微量元素的含量,与其所生长的土壤和水源中的含量有一定的关系,因此<br />
微量元素缺乏症或过多症的发生,往往与某些特定地区的土壤和水源中含量特别少(或多)<br />
有密切关系,常称这类疾病为生物地球化学性疾病,或称为地方病。据调查,我国约有 70<br />
%的县为低硒地区,从东北至西南形成一个低硒地带,沿海地区也严重缺硒,饲料中含硒量<br />
可低于 0.05mg/kg,缺硒可导致人的大骨节病、幼畜白肌病等。在土壤含氟量高的地区,<br />
或在炼铝厂、陶瓷厂附近,氟随烟尘散播于所在的农牧场或地面,可发生牛、羊的慢性氟中<br />
毒。江西赣南地区发生的所谓“牛白毛红皮病”,据研究认为是由于地区性钼过多,继发铜<br />
缺乏症所致。内地山区和沼泽地带,常发生地方性缺碘—甲状腺肿。<br />
5.临床症状虽然表现多样化,然而,病畜禽大多有舐癖、衰竭、贫血、生长发育停止、<br />
消化障碍、生殖机能扰乱等临床表现。多种矿物质如钠、钙、钴、铜、锰、铁、硫等的缺乏,<br />
某些维生素特别是 A 和 B 族(反刍兽除外)的缺乏,某些蛋白质和氨基酸的缺乏,均可能<br />
引起动物的异食癖;铁、铜、锰、钴等缺乏和铅、砷、镉等过多,都会引起贫血:锌、碘、<br />
锰、硒、钙和磷、钴、铜和钼,维生素 A、D、E、C 等的代谢状态都可影响生殖机能。<br />
6.无接触传染病史,一般体温变化不大,除个别情况及有继发或并发病的病例外,这类<br />
疾病时体温多在正常范围或偏低,畜禽之间不发生接触传染,这些是营养代谢性疾病与传染<br />
病的明显区别。<br />
病。<br />
7.通过饲料或土壤或水源检验和分析,一般可查明病因<br />
8.缺乏症时补充某一营养物质或元素,过多症时减少某一物质的供给,能预防或治疗该<br />
9.具有特征性器官和系统病理变化,有的还有血液生化指标的改变。例如仔猪低血糖症,<br />
呈现阵发性神经症状,血糖低于 2.24(5.04~5.6)mmol/L[40mg/100ml(正常为 90~100mg<br />
2
100ml)]。痛风发生尿酸血症,血中尿酸浓度由正常的 8.97~17.94mmol/L升至 89.7mmol<br />
/L(1.5~3mg/100ml升至 15mg/100m1)以上,致使关节囊、关节软骨周围组织,内脏器<br />
官中尿酸盐沉积。鸡锰缺乏发生骨粗短症。维生素A缺乏发生眼部病变。维生素D缺乏发生<br />
佝偻病。维生素B1缺乏发生多发性神经炎,呈现特殊的“观星”姿势。维生素B2缺乏呈现足<br />
趾向内蜷曲以跗关节着地等。<br />
四、<strong>营养代谢疾病</strong>的诊断<br />
群发性<strong>营养代谢疾病</strong>,尤其是地方流行的疾病诊断是极复杂的,不仅需要兽医临床工作<br />
者努力,还要营养学、临床化学、临床病理学、生物化学、地学、土壤学、医学等专家密切<br />
配合,共同努力,并按一定程序进行。<br />
1.首先要排除传染病、寄生虫病和中毒性疾病 由于许多<strong>营养代谢疾病</strong>呈群发、人兽共<br />
患和地方流行等特点。诊断时应利用一切现有手段排除病原微生物、寄生虫感染,亦测不出<br />
可疑毒物。抗菌药物,驱虫药物治疗,收效甚微,或仅对某些并发症有效。而使用针对性营<br />
养缺乏物质有良效时,可提示诊断。<br />
2.动物现症调查 在群养动物中长期存在生长迟缓、发育停滞、繁殖机能低下,屡配不<br />
孕,常有流产、死胎、畸胎生成、精子形态异常等;有不明原因的贫血、跛行、脱毛、异嗜<br />
等非典型的示病症状。越是高产(如产乳特别多、产蛋特别多)的越易出现各种临床症状者,<br />
可提示诊断。<br />
3.饲料调查 许多<strong>营养代谢疾病</strong>是因饲料中缺乏某些营养成分。应根据动物现症调查和<br />
初步治疗的体会,对可疑饲料中针对性营养成分如矿物质、维生素等测定,并和动物营养标<br />
准相比较。不仅要测当前饲料,可能的情况下要测病前所喂饲料,不仅测可疑物,还应测该<br />
物质的拮抗物。如测钼的同时测铜,测锌的同时测钙等。<br />
4.环境调查 放牧动物尤其应测土壤、植物、饮水中某些营养成分、施肥习惯、土壤 pH<br />
值、含水量、动物饮用水源是否受到污染及污染程度。我国江西耕牛钼中毒就是因矿山尾砂<br />
水污染,钼经稻草而进入牛,引起条件性缺铜所致。<br />
5.实验室诊断 实验室不仅要测定动物饲料、饮水中可疑成分及拮抗剂,而且对病畜血、<br />
肉尸、脏器等,特别是目标组织中可疑成分的含量,有关的酶活性测定,均有助于疾病诊断。<br />
6.动物回归试验及治疗 人工复制出与自然发生的疾病相同,用补充可疑营养成分可获<br />
得满意的效果,是诊断疾病的决定性依据。选择来自非病区健康动物,用可疑饲料或饮水喂<br />
养,并接受病区同样的管理,经一定时间饲喂试验,受试验动物产生的临床症状、血清成分、<br />
剖检及组织学变化与自然发生的病例完全一样,补充针对性营养成分,病情迅速好转,从而<br />
为建立诊断提供了可靠证据。<br />
有些动物试验,常需经过较长时间,会受到许多意想不到的因素的影响,甚至使试验归<br />
于失败。严格控制试验条件是保证实验结果可靠的关键步骤。<br />
综上所述,<strong>营养代谢疾病</strong>的病因诊断是困难的,有时需较长时间,耗费大量人力和经费,<br />
但一经诊断,则可迅速、大范围防治疾病。<br />
五、<strong>营养代谢疾病</strong>的防治措施<br />
防治群养动物<strong>营养代谢疾病</strong>的关键是要做到准确、均匀、经常、经济和方便。经过周<br />
密的调查和诊断,给动物日粮或饮水中准确地补充目标营养成分,使每头动物都有足够的机<br />
会获得所补充的物质,有时因某些物质在体内转换速度快,怎样使动物经常性地而又方便地<br />
获得补充物,是兽医工作者十分关注的,食草动物常采取草地喷洒某些微量元素(top<br />
dressing),或把某些微量元素制成铁丸、或用塑料胶囊罐装,投入瘤胃,沉入网胃,缓慢释<br />
放,达到补充目的,在日粮中掺入一定比例的目标营养成分,在饮水中加入补充物,也是常<br />
用的办法,但因动物采食量、饮水量不同,有时对防治效果有一定影响。在大规模饲养条件<br />
下,尤其要研究怎样补充目标营养物更经济、更方便、可节省人力是关键。合理改良土壤,<br />
3
添加微量营养物质到肥料中,并转入饲草或饲料中,在牧区也广为采用,但因其经济负担较<br />
大,如条件允许亦可试用。<br />
Introduction<br />
Amongst domestic farm animals the metabolic diseases achieve their greatest importance in dairy<br />
cows and pregnant ewes. In the other species these diseases occur only sporadically. The<br />
high-producing dairy cow always verges on abnormal homeostasis,and the breeding and feeding<br />
of dairy cattle for high milk yields is etiologically related to metabolic disease so common in these<br />
animals.<br />
Periparturient period<br />
In dairy cows,the incidence of metabolic diseases is highest in the period commencing at calving<br />
and extending until the peak of lactation is reached, and their susceptibility appears to be related to<br />
the extremely high turnover of fluids, salts and soluble organic materials during the early part of<br />
lactation. With this rapid rate of exchange of water, sodium, calcium, magnesium, chlorides and<br />
phosphates, a sudden variation in their excretion or secretion in the milk or by other routes, or a<br />
sudden variation in their intake because of changes in ingestion, digestion or absorption, may<br />
cause abrupt, damaging changes in the internal environment of the animal. It is the volume of the<br />
changes in intake and secretion and the rapidity with which they can occur that affects the<br />
metabolic stability of the cow. In addition, if the continued nutritional demands of pregnancy are<br />
exacerbated by an inadequate diet in the dry period, the incidence of metabolic disease will<br />
increase. The effect of pregnancy is particularly important in ewes, especially those carrying more<br />
than one lamb.<br />
Disease of lactation<br />
In the next phase of the production cycle, parturition is followed by the sudden onset of a profuse<br />
lactation which, if the nutrient reserves have already been seriously depleted, may further reduce<br />
them to below critical levels and clinical metabolic disease then occurs. The essential metabolite<br />
which is reduced below the critical level determines the clinical syndrome which will occur. Most<br />
attention has been paid to variations in balances of (1) calcium and inorganic phosphates relative<br />
to parturient paresis, (2) magnesium relative to lactation tetany, (3) blood sugar and ketones and<br />
hepatic glycogen relative to ketosis, and (4) potassium relative to hyperkalemia on cereal grazing,<br />
but it is probable that other imbalances are important in the production of as yet unidentified<br />
syndromes.<br />
During the succeeding period of lactation, particularly in cows on test schedules and under the<br />
strain of producing large quantities of milk, there is often a variable food intake, especially when<br />
pasture is the sole source of food, and instability of the internal environment inevitably follows.<br />
The period of early lactation is an unstable one in all species. Hormonal stimulation at this stage is<br />
so strong that nutritional deficiency often does not limit milk production and a serious drain on<br />
reserves of metabolites may occur.<br />
Breed susceptibility<br />
The fact that some dams are affected much more by these variations than others is probably<br />
explainable on the basis of variations in internal metabolism and degree of milk production<br />
between species and between individuals. Between groups of cows, variations in susceptibility<br />
appear to depend on either genetic or management factors. Certainly Jersey cows are more<br />
susceptible to parturient paresis than cows of other breeds, and Guernseys, in our experience,<br />
seem to be more susceptible to ketosis. Even within breeds considerable variation is evident in<br />
4
susceptibility between families. Under these circumstances it seems necessary to invoke genetic<br />
factors, at least as predisposing causes.<br />
Management practices<br />
Management practices of most importance are housing and nutrition. In those sections of North<br />
America where cattle are housed during the winter, and in poor pasture areas,ketosis is prevalent.<br />
In the Channel Islands, local cattle are unaffected by lactation tetany whereas the disease is<br />
prevalent in the United Kingdom. In New Zealand, metabolic diseases are complex and the<br />
incidence is high, both probably related to the practice of having the cows calve in late winter<br />
when feed is poor, to the practice of depending entirely on pasture for feed, and to the high<br />
proportion of Jerseys in the cattle population.<br />
A knowledge of these various factors is essential before any reasonable scheme of prevention<br />
can be undertaken. It should also indicate that although the more common disease entities are<br />
presented in this chapter, there is high probability that a disturbance of more than one of the<br />
metabolites mentioned may occur simultaneously in the one animal and give rise to complex<br />
syndromes which are not described here. The disease entities dealt with must be considered as<br />
arbitrary points in a long scale of metabolic disturbances.<br />
Occurrence and incidence<br />
Finally, only a knowledge of the etiological factors involved will help in understanding the<br />
incidence of the various syndromes. Largely because of variations in climate, the occurrence of<br />
metabolic disease varies from season to season and from year to year. In the same manner,<br />
variations in the types of disease occur. For example in some seasons most cases of parturient<br />
paresis will be tetanic; in others, most cases of ketosis will be complicated by hypocalcemia.<br />
Further, the incidence of metabolic disease and the incidence of the different syndromes will vary<br />
from region to region. Ketosis may be common in areas of low rainfall and on poor pasture.<br />
Lactation tetany may be common in colder areas and where natural shelter is poor. Recognition of<br />
these factors can make it possible to devise a means whereby the incidence of the diseases can be<br />
reduced.<br />
The metabolic diseases, because of high prevalence and high mortality rate, are of major<br />
importance in some countries, so much so that predictive systems are being set up. Rapid analysis<br />
of stored feed samples, pasture and soil is commonly used in Europe and North America but the<br />
interesting development has been the recognition of 'production diseases' and the consequent<br />
development of metabolic profile tests, particularly in the United Kingdom and in Europe.<br />
第二节 糖、脂肪、蛋白质营养代谢紊乱性疾病<br />
(Metabolic Disorder Caused by Carbohydrate,Lipid and Proteins)<br />
一、低糖血症(Hypoglycemia)<br />
动物,尤其是初生仔猪血糖浓度下降,临床上表现虚弱,平衡失调,体温下降,肌肉不<br />
自主运动,甚至惊厥死亡的现象称为低糖血症。本病又称为乳猪病(baby pig disease)或憔<br />
悴病(fading pig disease)。<br />
虽然,在酮病、妊娠毒血症、热射病时,成年动物血糖浓度亦会有明显降低,但本节着<br />
重介绍的是新生动物,尤其是生后一周内仔猪发生的因血糖浓度急剧降低而引起的惊厥和死<br />
亡。犊牛、羔羊理论上也会产生低糖血症,但自然发生本病的报道很少。<br />
【病因】 仔猪原发性低糖血症发生的主要原因是因吃乳量不足,这可能来自两方面①<br />
母猪泌乳量不足以供给全部吮乳仔猪的需要;②乳猪因各种原因无法吮吸足够的乳汁。母猪<br />
泌乳量不足甚至无乳可能由下列因素引起:乳房炎、传染性胃肠炎、子宫内膜炎、链球菌感<br />
5
染、母猪子宫炎-乳房炎-无乳综合征(MMA),麦角毒素中毒引起的无乳和乳头发炎坏死。<br />
母猪营养水平低,可明显影响泌乳和乳产量。<br />
初生仔猪,尤其是 1 周龄以内患有先天性肌阵挛、溶血症、脑室积水等可影响吃乳。<br />
由于母猪栏设计错误,要么把仔猪压伤不能行动而饿死,要么是仔猪无法接近母猪乳头<br />
而吃不到乳。猪舍保温条件差,仔猪抗寒能力弱可诱发本病。也有认为仔猪吮吸初乳后引起<br />
的过敏反应可引起低血糖症,仔猪胃肠内因缺乏乳酸杆菌,对乳汁消化障碍,亦可引发本病。<br />
遗传性低血糖症,常见于妊娠期过长,胎儿过大,肾上腺发育不良的新生仔畜,可见于<br />
犊牛、仔猪。<br />
本病最早发现于美国和英国,我国广东、江苏、湖南等省均有报道,在有些猪场本病发<br />
病率可达 30%~70%,甚至 100%,死亡率高达 50%~100%。有些仔猪发病后因太弱,懒动,<br />
而被母猪压死或被其它仔猪踩死。犊牛、羔羊生后丧母;又未及时人工哺乳者,亦可产生与<br />
乳猪低血糖症相似的症状。<br />
【病理】 新生仔猪肝内一般有良好的糖元贮备,肝糖元含量可达 100~140mg/kg,<br />
血糖浓度在生后 24h 内达 4.48~5.04mmol/L(80~90mg/100ml)。(不同窝次的猪可能有较<br />
大变动范围)。生后一周内尚无良好的生糖能力;这期间如吮乳受限制,糖贮备被迅速耗竭,<br />
血糖浓度迅速下降。因此,生后第一周常是本病发生的高峰期。据报道,发病快的于生后十<br />
数小时,大多于 2~3 天内发病死亡。血糖含量迅速降到 0.56~1.68mmol/L(10~30mg/<br />
100ml),甚至低至 0.1mmol/L(1.3mg/100ml),静脉注射胰岛素,使血糖浓度迅速降低,<br />
产生症状与自然发生的低血糖症相似,初产母猪所生仔猪更易发病。此期如人工哺乳,或给<br />
予葡萄糖水饮用,常可避免本病发生。<br />
【临床表现】 本病大多于生后 1~3 天内发生,开始有一头或数头不吃乳,四肢软弱<br />
无力,卧地不起,感觉迟钝或消失。有些猪虽能行走,但步态蹒跚,有的甚至呈犬坐姿势,<br />
呼吸加快,心跳次数减少至 80 次/min,可视黏膜苍白或变暗,体温下降至 36℃以下。卧<br />
地仔猪不时发出微弱的叫声,眼球移动缓慢,四肢伸直划动,肌肉震颤,抽搐,角弓反张。<br />
最后昏迷、瞳孔散大,数小时内迅速死亡。<br />
血糖浓度极度下降,有报道病死前血糖浓度为 0.3mmol/L(5.3mg/100ml)(1.3~11.2mg<br />
/l00ml)血中非蛋白氮、尿素氮浓度升高。<br />
剖检一般不显异常,少数猪胃内缺乏凝乳块,但许多病例胃内仍有部分食物,部分猪颈、<br />
胸、腹下有不同程度水肿。<br />
【诊断】 本病一般依血糖浓度明显下降,低体温,全身虚弱无力,对葡萄糖治疗反应<br />
迅速且良好而诊断。但应与新生仔猪其它疾病如细菌性败血症、病毒性脑炎、伪狂犬病、李<br />
氏杆菌病、链球菌感染等相区别。其中血糖浓度降低、体温下降两项,与上述疾病完全不同。<br />
【防治】 腹腔注射 5%~10%的葡萄糖 10~15ml,并配合Vc0.1ml,混合后作腹腔注射,<br />
4~6h一次,直至仔猪可以用人工哺乳或喝到寄母猪乳汁为止。应注意保暖和防寒,仔猪最适<br />
环境温度为 27~32℃。<br />
仔猪生后应精心照料,保暖防寒,必要时可行人工哺乳。妊娠后期应注意母猪的营养<br />
与保健,防止产后无乳或缺乳。<br />
NEONATAL HYPOGLYCEMIA<br />
Synopsis<br />
Etiology. Insufficient milk ingestion by newborn piglets in first few days of life or piglets affected<br />
with any disease which interferes with milk intake or that have enteropathy and are unable to<br />
digest milk.<br />
Epidemiology. Most common in piglets under 3 days of age. Sows have insufficient milk.<br />
Morbidity 30-70%, mortality 100%.<br />
6
Occurs in twin or triplet lambs exposed to hypothermia. Occurs rarely in calves with diarrhea.<br />
Occurs premature foals.<br />
Signs. Incoordination, shivering, dull, plaintive squeal, cold periphery, pale skin, weak, recumbent,<br />
terminal convulsions and death.<br />
Clinical pathology. Hypoglycemia.<br />
Lesions. No gross lesions. Stomach may be empty.<br />
Diagnostic confirmation. Response to treatment with glucose.<br />
Differential diagnosis list:<br />
Piglets<br />
•Coliform septicemia<br />
•Transmissible gastroenteritis (p. 1106)<br />
•Viral encephalomyelitis (pp. 1114, 1219)<br />
•Other septicemias.<br />
Lambs<br />
•Watery mouth disease (p. 1766)<br />
•Hypothermia (pp. 52, 129).<br />
Calves<br />
•Coliform septicemia (pp. 63, 789)<br />
•Bacterial meningitis (p. 538)<br />
•Dehydration and acidosis associatedwith enterotoxigenic colibacillosis(pp. 789, 791).<br />
Treatment. IV or IP glucose solutions.<br />
Control. Insure adequate colostrum and milk intake for newborn piglets, lambs and calves.<br />
ETIOLOGY<br />
An inadequate intake of milk is the primary cause of hypoglycemia in piglets. This may be due to<br />
failure of the sow's milk supply or to failure of the piglets to suck. Failure to suck may be due to<br />
such diseases as coliform septicemia, TGE, streptococcal infections, myoclonia congenita and<br />
hemolytic disease of the newborn (1). Piglets under 4 d of age rapidly develop hypoglycemia<br />
under fasting conditions; older pigs do not (2).<br />
In piglets affected with transmissible gastroenteritis (TGE), there is decreased digestion of<br />
lactose, reduced absorption of glucose following the severe and diffuse intestinal villous atrophy<br />
and, combined with the low-energy reserves of the newborn piglet, severe hypoglycemia can<br />
occur (3). Hypoglycemia may occur in newborn calves with acute severe diarrhea and when they<br />
are deprived of milk or a source of carbohydrates for more than a few days.<br />
Hypoglycemia occurs in twin or triplet lambs which become hypothermic after 12 h of age (4).<br />
EPIDEMIOLOGY<br />
Newborn pigs encounter several challenges to their survival during the initial hours of life. One is<br />
the inherent problem of glucose homeostasis with the first day of life being the most critical period.<br />
Liver glycogen is rapidly depleted postanatally (12-24 h) for the maintenance of blood glucose.<br />
Little insulation against heat loss is provided by the sparse hair coat and the 1-2% total body fat at<br />
birth. There is only a small amount of carcass fat and no brown fat, and consequently the piglet is<br />
dependent almost exclusively on carbohydrate metabolism for subsistence. Therefore,<br />
maintenance of the physiologically critical energy metabolite, glucose, depends on the ability of<br />
the neonatal pig to compete with its littermates for regular nourishment from its dam.<br />
Neonatal hypoglycemia in piglets occurs primarily during the first 3 d after birth. The disease<br />
7
has been recorded mainly from North America and the United Kingdom. Most affected piglets die<br />
if left untreated; the morbidity is usually 30-70% and may be as high as 100% in individual litters.<br />
Apart from deaths due to hypoglycemia, many piglets are too weak to avoid the sow and are killed<br />
by overlaying. Piglets which fail to ingest sufficient colostrum or milk because of a failure of the<br />
sow's milk supply or because of an inability of the piglet to suck normally are the most common<br />
primary circumstances. A secondary determinant occurs when piglets affected with an enteritis<br />
such as transmissible gastroenteritis are unable to properly digest the lactose in milk and absorb<br />
sufficient glucose.<br />
Hypoglycemia occurs in twin and triplet lambs which may be immature or undersized and are<br />
subjected to cold exposure and hypothermia (4). About 50% of the total lipid present in the<br />
newborn lambs is in the adipose tissue in the form of brown fat which is used by the lambs for<br />
non-shivering thermogenesis during the first 24 h following birth (5). However, the lipid content<br />
of newborn lambs can vary from 1.5-4.5% of birth weight and small lambs have low levels.<br />
Neonatal viability of lambs decreases as birth weight decreases, which may be related to their low<br />
lipid content in relation to body size (5). Additional factors include mismothering and complete<br />
absence of the ewe in lambs only a few days of age.<br />
Hypoglycemia in calves has been recorded as a concurrent disease with diarrhea (6, 7). The<br />
hypoglycemia may be secondary to the interference with absorption and digestion caused by the<br />
diarrhea. The signs are characteristic but the hypoglycemia docs not respond to glucose therapy as<br />
quickly, if at all, as in other species (6). However, hypoglycemia in diarrheic calves is not<br />
considered to be a significant problem if affected calves receive a supply of milk or milk replacer<br />
during the convalescent period.<br />
Hypoglycemia occurs in foals which are born premature and unable to suck the mare, those<br />
with septicemias, and those exposed to hypothermia.<br />
PATHOGENESIS<br />
The piglet is born with liver glycogen levels which may be as high as 200 mg/g WW, while<br />
muscle glycogen may reach 120 mg/g WW. The blood glucose level at birth is low at 30-60<br />
mg/dL (1.66-3.33 mmol/L) and increases rapidly after feeding on colostrum to 95 mg/dL (5.25<br />
mmol/L) (8). Satisfactory gluconeogenesis does not develop in piglets until the 7th day after birth,<br />
and during this period glycogen stores are likely to be rapidly exhausted if the intake of milk is<br />
restricted. The blood glucose level is then extremely unstable and dependent entirely upon dietary<br />
sources. The first week of life is thus the danger period (1). Deprivation of food after this produces<br />
only loss of weight and has no effect on blood glucose levels. This particular susceptibility to<br />
hypoglycemia in the early postnatal period seems to be characteristic of the pig and may play a<br />
major role in causing losses in piglets by contributing to the effects of various infectious and<br />
non-infectious agents.<br />
Signs appear first when blood glucose levels fall to about 50 mg/dL (2.775 mmol/L), although<br />
further depression to levels as low as 7 mg/dL (0.388 mmol/L) has been observed. Even in such<br />
extreme cases, complete recovery is possible after the administration of glucose (1). The<br />
hypoglycemic comatose state induced in piglets by fasting occurs as blood glucose values fall<br />
below 40 mg/dL (2.2 mmol/L) (3). Experimental hypoglycemia produced by the injection of<br />
insulin causes a clinical syndrome similar to that of the naturally occurring disease.<br />
In piglets with TGE, the blood glu¬cose levels decreased from a normal of 119 mg/dL (6.6<br />
mmol/L) to 36 mg/dL (2.0 mmol/L) (9). This hypoglycemia coincides with the onset of lethargy<br />
8
followed by a comatose state in a few hours.<br />
CLINICAL FINDINGS<br />
The disease is most characteristic in piglets under a few days of age. Incoordination is apparent<br />
first and the piglet has progressive difficulty in maintaining balance until recumbency becomes<br />
permanent. There is shivering, dullness and anorexia, and often a typical weak squeal. A<br />
characteristic feature is the subnormal rectal temperature and the cold, clammy skin which also<br />
evidences marked pallor and ruffling of the hair. The pallor is related to the failing circulation.<br />
The heart rate becomes increasingly feeble and slow and may fall as low as 80/min. In many cases<br />
there are few additional signs but convulsions are recorded as a common occurrence by some<br />
observers (1). These vary from aimless movements of the head and forelimbs to severe tetanic<br />
convulsions. In the latter there are violent galloping movements, particularly with the hindlegs,<br />
opisthotonos and champing of the jaws. Tortuous movements and rigidity of the neck and trunk<br />
also occur. Terminally, coma develops and death follows 24-36 h after the onset of signs. The<br />
clinical findings are similar in other species with weakness, incoordination, hypothermia, eventual<br />
recumbency and coma being characteristic. The nervous signs are most common in the piglet and<br />
not seen in the other species.<br />
CLINICAL PATHOLOGY<br />
Blood glucose levels of less than 50 mg/dL (2.8 mmol/L) in piglets are considered to indicate<br />
clinical hypoglycemia. The hypoglycemic comatose state induced in piglets by fasting occurs is<br />
blood glucose values below 40 mg/dL (2.2 mmol/L) (3). Significant rises in blood non-protein<br />
nitrogen and urea nitrogen are often observed but appear to be related to catabolism rather than to<br />
renal dysfunction (10).<br />
In calves with acute severe diarrhea, the blood glucose may tall to below 40 mg/dL (2.2 mmol/L)<br />
in 30-50% of cases (7).<br />
NECROPSY FINDINGS<br />
There are no visible lesions. Absence of curd in the stomach is good contributory evidence of lack<br />
of intake of milk but in many cases it will be obvious that some milk was consumed. Hepatic<br />
glycogen levels are usually negligible.<br />
DIFFERENTIAL DIAGNOSIS<br />
Unless blood glucose levels are estimated, the predominantly nervous signs may lead to an error in<br />
diagnosis. However, hypoglycemia and a good response to treatment with glucose may occur<br />
when the hypoglycemia is secondary to another disease. A definite diagnosis of neonatal<br />
hypoglycemia must depend on elimination of other diseases as primary causes.<br />
Piglets<br />
Coliform septicemia and enterotoxigenic<br />
colibacillosis are characterized by weakness, recumbency, collapse and dehydration.<br />
Viral encephalomyelitis and pseudorabies cause an almost identical clinical picture but are not<br />
restricted in occurrence to pigs less than 1 week old.<br />
Bacterial meningoencephalitis, including streptococcal septicemia and listeriosis, may also<br />
affect pigs of this age. Necropsy examination should make definition of viral and bacterial<br />
infections a relatively easy task.<br />
Lambs<br />
Watery mouth disease is characterized by weakness, drooling from the mouth,<br />
hypothermia, distended fluid abdomen and hypoglycemia.<br />
9
Foals<br />
Premature foals born several days before term, are weak and unable to stand and suck, and are<br />
hypoglycemic.<br />
Septicemias occur in foals born at term and are characterized by depression, failure to suck,<br />
inactivity, fever, dehydration, petechiation and death in several hours if not treated intensively.<br />
TREATMENT<br />
Piglets with primary hypoglycemia should be given glucose (15mL of 20% solution) IP, repeated<br />
even 4-6 h until the animal will suck a foster dam or drink an artificial diet. Protection from cold is<br />
important and an environmental temperature of 27-32℃(80-90℉) will improve the survival rate<br />
of piglets (10). The combined use of oral fluid therapy and the IP administration of 5% dextrose at<br />
a rate of 25 mL/kg BW to piglets affected with hypoglycemia associated with TGE did not correct<br />
the hypoglycemia (9). A newborn piglet weighing 1250 g requires 170 kcal (711 kj) per day when<br />
maintained at 30 ℃(88℉); 30 ml. of a 5% dextrose solution would provide approximately 1.5 g of<br />
glucose, which would yield only 5.6 kcal (23 kJ) per dose. It would be difficult to provide the<br />
energy requirements by parenteral administration of 5% dextrose because the amount of fluid<br />
injected per day should not exceed 8% of their body weight (9).<br />
Hypoglycemia and hypothermic lambs can be resuscitated by an IP injection of a 20% solution of<br />
glucose at a rate of 10 mL/kg BW followed by rewarming the air at 40(104) (11).<br />
CONTROL<br />
Avoidance of the causative factors described earlier constitutes prevention. Piglets should be<br />
carefully observed during the first week of life for early signs of any disease and treatment<br />
instituted promptly. Maintenance of a stable environmental temperature at 32 (90) may delay the<br />
onset of the disease, or in marginal circumstances prevent its occurrence.<br />
Lambs require between 180 and 210 ml. colostrum/kg BW during the first 18 h after birth in<br />
order to provide sufficient energy for heat production (12). The administration of colostrum at a<br />
rate of 30 mL/kg BW within a few minutes after birth, directly into the stomach using a catheter<br />
and syringe, is recommended to boost the energy supply of the small lamb (5). Ewes which are<br />
well fed during late pregnancy produce more colostrum than their lambs need, those with<br />
singletons have enough for a second lamb, but in most underfed ewes the lamb requirements for<br />
colostrum exceed the ewe's production. Colostrum can be readily obtained by milking those ewes<br />
with excess production. The effects of feeding ewe colostrum, cow colostrum, or ewe milk<br />
replacer, on plasma glucose in newborn lambs have been compared (13). Both ewe and cow<br />
colostrum resulted in a two-fold increase m plasma glucose within 1-3 h; the milk replacer caused<br />
marked hyperglycemia.<br />
REFERENCES<br />
(1)Goodwin, R F. W. (1955) lir. Vel.J.,Ill, 301.<br />
(2)Goodwin, R. F. W. (1957) Vet. Rec, 69,1290.<br />
(3)Drolet, R. et al. (1984) Can.J. Comp.Med., 48, 282.<br />
(4)Eales, F. A. ct al. (1982) Vet. Rec, I10,118.<br />
(5)Robinson, J. J. (1981) Livestock Prod. Sci.,8, 273.<br />
(6)Tennant, B. et al. (1968) Cornell Vet., 58,136.<br />
(7)Lewis, L, D. et al. (1975) Am.J. Vet. Rec,36, 413.<br />
(8)Mersmann, H.J. (1974) J. Aram. So., 38,1022.<br />
(9)Drolet, R. ct al. (1985) Can.), Comp.Med, 49, 357.<br />
10
(10)Momll, C. C. (1952) Am.J. Vet. Res., 13,164, 171, 322,325, 327.<br />
(11)Eales, F. A. et il. (1982) Vet. Rec, 110,121.<br />
(12)Mellow. D.J. & Murray, L. (1986) Vet.Rec, 118, 351.<br />
(13)Bales, F. A. et al. (1982) Vet. Rec, 111,451.<br />
二、酮病(Ketosis)<br />
动物因体内碳水化合物及挥发性脂肪酸代谢紊乱,致使血糖浓度下降,酮体生成增多,<br />
产生酮血症、酮尿症或酮乳症,称为酮病。反刍动物尤其是产后 6 周以内的乳牛发病最多,<br />
其次是乳山羊、绵羊、兔和豚鼠。狗、猫和人的糖尿病时,也可产生血中酮体增多,尿中酮<br />
体排泄增多,血糖浓度下降。临床上以昏睡或兴奋、产乳量下降、机体失水,偶尔发生运动<br />
失调为特征。<br />
【病因】 反刍动物血糖主要是由瘤胃中产生丙酸经糖异生途径转化为葡萄糖而维持<br />
的,凡是引起瘤胃内丙酸生成减少的因素,都可诱发乳牛酮病生成。如产前、产后采食量减<br />
少,各种原因引起产后消化机能下降,挥发性脂肪酸产生减少,饲料中碳水化合物供给不足,<br />
或精料过多,粗纤维不足均可导致酮病,成为本病的原发性原因。创伤性网胃炎、前胃弛缓、<br />
真胃溃疡、子宫内膜炎、胎衣滞留、产后瘫痪及饲料中毒等,导致消化机能减退,是酮病的<br />
继发性病因。<br />
丙酸需先转化为丙酰辅酶A,然后经糖异生合成葡萄糖。其中必须要有VB12参予,当动<br />
物缺乏钴时,直接影响瘤胃微生物的生长繁殖,不仅影响VB12的合成,也可影响前胃消化功<br />
能,导致酮病生成。<br />
体内糖消耗过多,耗糖速度过快,引起糖供给和糖消耗间不平衡。母牛分娩前后。血糖<br />
浓度常偏低,而分娩应激作用使初乳形成和分泌,如果母牛营养和代谢稍有不适,就可使已<br />
处于隐性酮病的牛,迅速产生临床症状。有人计算每天产 27L 乳的牛,体内将合成 1225g<br />
乳糖并转入乳汁中,一个乳糖需由二个单糖缩合而成。日产 34L 乳的母牛,几乎可将血中<br />
全部葡萄糖转化为乳糖。产后 40 天内即可达泌乳高峰期,泌乳峰期出现越快,产乳越多,<br />
越易患酮病。<br />
肝脏是反刍动物糖异生的主要场所,肝脏原发性或继发性疾病,都可能影响糖异生作用,<br />
如母牛脂肪肝综合征,可诱发酮病。<br />
通常情况下,体内可生成少量酮体,但它们可被肝外组织如骨骼肌、心肌所利用,亦可<br />
在皮下合成脂肪或在乳腺内生成乳脂,但如酮体生成过多,肝外组织不能及时清除它们,造<br />
成酮体蓄积。如有些青贮饲料中丁酸过多,加之体内草酰乙酸消耗太多,亦可产生酮病。<br />
当血糖浓度下降时,脂肪组织中脂肪分解速度大于合成速度,以利供给能量。脂肪分解<br />
所生成的甘油可作为生糖先质转化为糖,缓解血糖浓度下降速度,而脂肪酸则因脂肪组织中<br />
缺乏 α-磷酸甘油,不能重新合成脂肪。血液中游离脂肪酸含量增多,被运入肝脏以后,引<br />
起 β-氧化过程,生成过多的乙酰辅酶 A,因得不到足够的草酰乙酸经三羧酸循环途径而氧<br />
化放能,则经合成乙酰辅酶 A 途径,最终产生大量的酮体。另外,部分脂肪酸在肝内合成<br />
甘油三脂,因缺乏极低密度脂蛋白(VLDL)将其运出,蓄积在肝内引起脂肪肝生成,使糖<br />
异生障碍加剧,体内酮体蓄积更多,酿成酮病。<br />
在体脂分解的同时,体蛋白加速分解,其中生糖氨基酸可参加三羧酸循环而供能,生酮<br />
氨基酸则因没有足够的草酰乙酸,只能经丙酮酸氧化脱羧作用,生成乙酰辅酶 A,最后生成<br />
酮体。活体穿刺酮病牛肝组织证实,肝内草酰乙酸含量减少。注射胰岛素,人工降低血糖浓<br />
度,可诱发酮病,也从另一角度证实血糖浓度下降是产生酮病的起因,体内酮体生成增多,<br />
生成速度大于清除速度,造成酮体蓄积因而出现酮血症、酮尿症、酮乳症。<br />
激素调节在这一过程中起重要作用。血糖浓度下降,引起胰高血糖素分泌增多;胰岛素<br />
分泌减少,垂体内葡萄糖受体(glucoreceptors)兴奋,促使肾上腺髓质分泌肾上腺素。在三<br />
11
种激素共同作用下,肝糖元分解增多,脂肪水解为甘油和游离脂肪酸速度加快,酮体生成增<br />
多。激素还可刺激肌肉蛋白分解,其中生酮氨基酸在酮病生成中又起作用。此外,肾上腺皮<br />
质激素分泌不足,甲状腺功能低下等与酮病生成亦有密切关系。在催乳素作用下,把内源性<br />
和外源性生糖先质源源不断地转化为乳糖。在疾病初期,乳产量仍维持于高水平,但母牛食<br />
欲下降,体况迅速恶化、消瘦,消化功能降低,终使乳产量下降。<br />
酮体本身毒性作用较小,但高浓度的酮体对中枢神经有抑制作用,脑组织缺糖可使牛嗜<br />
眠。但当丙酮还原或 β-羟丁酸脱羧生成异丙醇,可使病牛兴奋不安。酮体本身还有利尿作<br />
用,病牛常常粪便干燥,机体失水,并迅速消瘦,消化不良以至拒食,使疾病迅速恶化。<br />
【临床表现】 临床型酮病常在产后几天至几周内出现,以消化紊乱和神经症状为主。<br />
患畜突然不愿吃精料,喜舔食垫草和污物,粪便干燥,表面被覆粘液,迅速消瘦,体况下降。<br />
精神沉郁、凝视,步样不稳并伴有轻瘫症状,大型乳牛场常呈群发。乳山羊酮病神经症状明<br />
显,常与脑炎或脊髓挫伤相混淆。产乳量迅速下降,乳脂含量升高,乳汁易形成泡沫,类似<br />
初乳状。尽管病牛不吃,但产乳仍持续进行,机体失水现象明显。临床综合征的严重程度与<br />
血中酮体含量成正比。病牛呼出气中也有明显的酮臭味,乳经加热酮臭更加明显。<br />
有些病牛嗜睡,常处于半昏睡状态。但也有少数病牛狂躁或激动,表现转圈、摇摆、感<br />
觉过敏,视力减弱,强迫运动,常无目的地吼叫,这些症状间断发生,每次持续 l~2h,间<br />
隔 8~12h 重又出现。尿色浅黄,易形成泡沫。呼吸减慢,心跳徐缓。乳产量急剧降低,常伴<br />
有子宫内膜炎,使休情期延长,繁殖机能减退。<br />
各种年龄牛均可发生,但有随胎次而增加的趋势。3 胎以上的牛隐性酮病发生率较高。<br />
产后一个月内最易发生。隐性酮病牛开始血糖浓度下降不明显,随之尿酮浓度升高,然后才<br />
有血酮浓度升高。<br />
【临床病理】病牛血糖浓度从正常时 2.8mmol/L 降至 1.12~2.24mmol/L,继发性酮病<br />
牛血糖浓度下降不明显。母牛血液中酮体浓度从 0~1720µmol/L 升高到 1720~17200µmol/<br />
L,继发性酮病牛血酮体浓度多在 8600µmol/L 以下。尿液酮体浓度因病牛饮水量而有较大<br />
波动,但多在 13760~223600µmol/L 之间,明显高于正常。乳酮浓度可从正常时 516µmol<br />
/L 升高到 6880µmol/L。肝糖元浓度下降,葡萄糖耐量曲线正常。瘤胃液中丁酸浓度大大<br />
升高。血中 β-羟丁酸浓度大大升高,血液 pH 从正常时的 7.43±0.01 降为 7.38±0.02,呈代<br />
谢性酸中毒。嗜酸性白细胞增多,淋巴细胞比例可达 60%~80%。嗜中性白细胞减少至 10<br />
%。有时,血清谷草或谷丙转氨酶活性升高。<br />
【诊断】 临床型酮病主要根据本病发生于围产期,低血糖、高血酮并伴有食欲骤减,<br />
乳产量急剧下降和神经症状等不难作出诊断。亚临床酮病诊断主要根据血、乳中酮体浓度升<br />
高,乳产量逐渐下降,多于产后 6 周内发生,并可持续 3 周,伴有体重下降现象而作出诊断。<br />
继发性酮病虽有血,尿中酮体浓度升高现象,但这些病多有其自身的特点,用高糖治疗仪有<br />
部分效果,只要原发病未根除,仍可反复出现血、尿、乳酮体浓度升高。<br />
原发性酮病除因脂肪肝生成恢复较慢外,一般预后良好,而继发性酮病在根治原发性疾<br />
病过程中,“酮症”可随之消失。<br />
【治疗】 许多治疗方法对大多数牛是有效的,但对有些牛效果不明显甚至无效。本病<br />
治疗的原则是补充体内糖的不足,提高酮体利用率。<br />
补糖法:用 50%葡萄糖静脉注射,多数患牛有显著疗效,但因维持时间较短,2h 后血<br />
糖又恢复到较低水平。这是因为静脉注射葡萄糖后,部分用于合成乳糖转入乳中,而且,短<br />
期内高血糖可引起尿糖排泄增多。以静脉滴注,或以 20%葡萄糖腹腔注射,可延长血糖保<br />
持在正常浓度的时间。口服丙酸钠,每天 250~500g,分 2 次给予,连用 10 天。它们在瘤胃<br />
中可不加改变地吸收,并在肝内转化为葡萄糖增加血糖浓度。蔗糖、麦芽糖灌服效果不理想,<br />
过量还可致酸中毒和食欲下降,甚至可致继发性酮病。用丙二醇(propanediol)治疗,效果<br />
12
亦较满意。饲料中拌和丙醇或甘油,一天 2 次,每日 225g,连用 2 天,随后日用量为 110g,<br />
每天 1 次,连用 2 天,口服或拌饲前静脉注射葡萄糖效果更明显。乳酸盐也是生糖物质,如<br />
乳酸钠、乳酸钙、首日用量 1kg/d,随后为 0.5kg/d 连用 7d,乳酸铵每天 200g,连用 5d,<br />
也有显著疗效。<br />
激素疗法:适用于体质较好的病牛,促肾上腺皮质激素 ACTH200~600 单位,肌肉注射,<br />
方便易行,不需预先给予生糖先质。糖皮质激素肌肉或静脉注射,可促进三羧酸循环,并可<br />
刺激糖异生作用,将氨基酸转化为糖,提高血糖浓度。糖皮质激素还可抑制泌乳作用,减少<br />
糖消耗,改善体内糖平衡。其缺点是,它可增加体脂分解,理论上它有使酮体生成增多的作<br />
用。许多糖皮质激素价格昂贵,而且对草酰乙酸的消耗增多,有人建议在补糖或使用 ACTH<br />
同时,注射胰岛素,但效果未必满意。<br />
其它疗法:水合氯醛口服,用作治疗牛的酮病已有很久,开始 30g,随后每天 7.0g,一<br />
天 2 次,连续数天,如剂量太大,可用胶囊罐装,或与蜜糖和水拌和后服用。水合氯醛有促<br />
进瘤胃中淀粉裂解,刺激葡萄糖生成和吸收作用,还可增加瘤胃内丙酸生成。硫酸钴每天<br />
100mg,放入水中或掺入饲料中口服。亦有建议用辅酶 A 先质半胱氨酸和延胡索酸钠治疗,<br />
据称开始时效果较好,但生产中尚难推广。5%的碳酸氢钠 300ml 静脉注射,可作为酮病治<br />
疗的辅助用药,用氯丙嗪、健胃剂等对症治疗,亦很有用。<br />
【预防】 为防止酮病,在妊娠期,尤其是妊娠后期增加能量供给,但又不致使母牛过<br />
胖。在催乳期间,或产前 4~5 周应逐步增加能量供绐,并维持到产犊和泌乳高峰期,这期间,<br />
不能轻易更换配方。随着乳产量增加,应逐渐供给生产性日粮,并保持粗料与精料有一定比<br />
例,其中蛋白质含量不超过 16%~18%,碳水化合物应供给碎玉米最好,这样可避开瘤胃的<br />
消化发酵和产酸过程,在真胃、肠内可供给葡萄糖。在达到产乳高峰期时,避免一切应激性<br />
因素的干扰,包括饲料组成、饲料来源的更换;同时要增加优质干草或青贮料供给,因为变<br />
质的青贮料中丁酸含量较高,可增加酮体生成。<br />
生。<br />
高产牛群还应经常监测,测定乳中酮体含量并及时采取补救措施,才能预防该病的发<br />
KETOSIS IN RUMINANTS (ACETONEMIA IN CATTLE, PREGNANCY TOXEMIA IN<br />
SHEEP)<br />
Synopsis<br />
Etiology. A multifactorial disorder of energy metabolism. Negative energy to hypoglycemia and<br />
ketonemia (the accumulation in blood of acetoacetate, beta-hydroxybutyrate and their<br />
decarboxylation products acetone and isopropanol). The diseases in cattle and sheep occur in<br />
different parts of the pregnancy-lactation cycle.<br />
Epidemiology. Primary ketosis occurs in well-conditioned cows with high lactation potential,<br />
principally in the first month of lactation with a higher prevalence in cows with a higher lactation<br />
number. Secondary ketosis occurs where other disease reduces feed intake.<br />
The disease in sheep is associated with a falling plane of nutrition, principally in the last month of<br />
pregnancy, in ewes bearing twins and triplets but can be induced by other stress at this time.<br />
Clinical findings. Cattle show wasting with decrease in appetite, fall in body condition and milk<br />
production. Some have short periods of bizarre neurological and behavioral abnormality.<br />
Response to treatment is good. Sheep have encephalopathy with blindness, muscle tremor,<br />
convulsions, metabolic acidosis and a clinical course of 2-8 d, usually terminating fatally unless<br />
treated early.<br />
Clinical pathology. Hypoglycemia, ketonemia, ketonuria or elevated ketones in milk.<br />
Necropsy findings. None specific. Twin lambs and fatty liver.<br />
13
Diagnostic confirmation. Ketonemia, ketonuria or elevated ketones in milk. Elevated<br />
beta-hydroxybutyrate (BHBA) in aqueous humor of dead sheep.<br />
Treatment. In cattle, parenteral glucose with corticosteroid and oral glucose precursors such as<br />
propylene glycol, occasionally insulin. Similar treatment in sheep, or oral glucose and electrolyte<br />
therapy. Cesarian section or induction of parturition in sheep. In cattle, the disease responds<br />
readily to treatment and is self-limiting, but in sheep the disease is highly fatal.<br />
Control. Correction of energy imbalance. Herd and flock biochemical monitoring coupled with<br />
condition scoring.<br />
ETIOLOGY<br />
Glucose metabolism in ruminants<br />
The maintenance of adequate concentrations of glucose in the blood is critical to the regulation of<br />
energy metabolism. The ruminant absorbs very little dietary carbohydrate as hexose sugar because<br />
dietary carbohydrates are fermented in the rumen to short chain fatty acids, principally acetate<br />
(70%), propionate (20%) and butyrate(10%).Consequentlyglucose needs in ruminants must<br />
largely be met by gluconeogenesis. Propionate and ainino acids are the major precursors for<br />
gluconeogenesis with glycerol and lactate of lesser importance (1).<br />
PROPIONATE is produced in the rumen from starch, fiber and proteins. It enters the portal<br />
circulation and is efficiently removed by the liver, which is the primary glucose-producing organ.<br />
Propionate is the most important glucose precursor; an increased availability can spare the hepatic<br />
utilization of other glucose precursors (2), and production of propionate is favored by a high grain<br />
inclusion in the diet (3).<br />
AMINO ACIDS The majority of amino acids are glucogenic and are also important precursors for<br />
gluconeogenesis. Dietary protein is the most important quantitative source but the labile pool of<br />
body protein is also an important source; together they contribute to energy synthesis and milk<br />
lactose synthesis as well as milk protein synthesis (1).<br />
DIETARY ACETATE is transported to peripheral tissues and to the mammary gland and<br />
metabolized to long chain fatty acids for storage as lipids or secretion as milk fat.<br />
Ketone formation<br />
Ketones arise from two major sources: butyrate in the rumen and mobilization of fat. A large<br />
proportion of butyrate produced by rumen fermentation of the diet is converted to<br />
beta-hydroxybutyrate (BHBA) in the rumen epithelium and is absorbed as such. Free fatty acids<br />
produced from the mobilization of fat are transported to the liver and oxidized to produce<br />
acetyl-CoA and NADH.<br />
Acetyl-CoA may be oxidized via the TCA cycle or metabolized to acetoacetyl-CoA. Its<br />
oxidation via the TCA cycle depends upon adequate supply of oxaloac-etate from the precursor<br />
propionate. If propionate, and consequently oxaloacetate, is deficient, oxidation of acetyl-CoA via<br />
the TCA cycle is limited and it is metabolized to acetoacetyl CoA and subsequently to<br />
acetoacetate and BHBA (1).<br />
The ketones BHBA and acetoacetate can be utilized as an energy source. They are normally<br />
present in blood and their concentration is a result of the balance between production in the liver<br />
and utilization by the peripheral tissues.<br />
Hepatic insufficiency in ketosis<br />
The uptake of fatty acids by the liver leads to a fatty liver. Hepatic insufficiency has been shown<br />
to occur in bovine (4) and ovine ketosis but it does not occur in all bovine cases (5).<br />
14
It has been suggested that hepatic insufficiency occurs in those cows predisposed to ketosis by<br />
overfeeding in the dry period (6).<br />
Since one of the reactions to hypoglycemia is mobilization of fat reserves and uptake of fat by<br />
the liver, some degree of hepatic insufficiency is to be expected as a secondary development of the<br />
disease.<br />
Role of insulin and glucagon<br />
The regulation of energy metabolism in ruminants is primarily governed by insulin and glucagon.<br />
Their counteracting effects play a central role in the homeostatic control of glucose. A low insulin:<br />
glucagon ratio stimulates lipolysis in adipose tissue and ketogenesis in the liver. Cows in early<br />
lactation have low insulin:glucagon ratios because of low blood insulin and are in a catabolic state<br />
(6). Elevated ketones may stimulate insulin production and may act as a negative feedback (7).<br />
Regulation is also indirectly governed by somatotropin, which is the most important determinant<br />
of milk yieldin cattle and is also lipolytic. Factors that decrease the energy supply to ruminants,<br />
that increase the demand for glucose, or that increase the utilization of body fat as an energy<br />
source are likely to increase ketone production and ketonemia. There is however considerable<br />
cow-to-cow and ewe-to-ewe variation in susceptibility to clinical ketosis.<br />
Energy balance<br />
In high-producing dairy cows there is often a negative energy balance in the first few weeks of<br />
lactation. The highest dry matter intake does not occur until 8-10 weeks after calving but peak<br />
milk production is at 4-6 weeks and energy intake may not keep up with demand. In response to a<br />
negative energy balance and low serum concentrations of glucose and insulin, cows will mobilize<br />
adipose tissue with consequent increases in serum concentrations of non-esterified fatty acids and<br />
BHBA. The hepatic mitochondrial metabolism ot fatty acids promotes both gluconeogenesis and<br />
ketogenesis.Cowspartition nutrients during pregnancy and lactation and are in a lipolytic stage in<br />
early lactation (8); cows arc at risk for ketosis during this period. Similarly the energy<br />
requirements in late pregnant twin-bearing ewes may place them in a lipolytic status.<br />
ETIOLOGY OF BOVINE KETOSIS<br />
It is not unreasonable to view clinical ketosis as the top end of a spectrum of a metabolic state that<br />
is common in heavily producing cows in the postcalving period. This is because high yielding<br />
cows in early lactation are in negative energy balance and are subclini-cally ketotic as a result.<br />
Ruminants are particularly vulnerable to ketosis because,although very little carbohydrate is<br />
absorbed as such, a direct supply of glucose is essential to tissue metabolism, particularly the<br />
formation of lactose. The utilization of volatile fatty-acids for energy purposes is also dependent<br />
upon a supply of available glucose. This vulnerability is further exacerbated, particularly in the<br />
cow, by the tremendous rate of turnover of glucose.<br />
In the period between calving and peak lactation the demand for glucose is increased and<br />
cannot be completely restrained. Cows will reduce milk production in response to a reduction of<br />
energy intake, but this does not follow automatically nor proportionately in early lactation because<br />
hormonal stimuli for milk production overcome the effects of reduced food intake. Under these<br />
circumstances lowered blood glucose levels result in a lowered blood insulin. Long chain fatty<br />
acids are released from fat stores under the influence of both a low blood insulin:glucagon ratio<br />
and the influence of high somatotropin concentration, and this leads to increased ketogenesis.<br />
Subclinical ketosis<br />
Elevated concentrations of blood ketones without clinical disease, subclinical ketosis, occur more<br />
15
commonly than clinical ketosis and have significant economic importance. Various studies have<br />
shown that subclinical ketosis is common in high-producing cows 2-7 weeks post-partum, with<br />
recorded prevalence ranging from 7-34% (2,9-11). It takes only a small additional nutritional or<br />
metabolic insult for these to develop clinical ketosis.<br />
Individual cow variation<br />
The rate of occurrence of negative energy status, and therefore the frequency of clinical cases, has<br />
undoubtedly increased sharply in the recent past because of the steep increase in the lactation<br />
potential of the modern dairy cow. Because of the mammary gland’s metabolic precedence in the<br />
partitioning of nutrients, especially glucose, milk production continues at a high rate, causing an<br />
energy drain. In many individual cows the need for energy is beyond their capacity for dry matter<br />
intake.<br />
Clinical ketosis has been produced in recently calved dairy cows by reducing the daily feed<br />
intake by 15-20% ad libitum and supplementing it with 1,3-butanediol, a ketogenic substrate. The<br />
biochemical characteristics of ketosis including depletion of hepatic glycogen and major increases<br />
in hepatic stores of triglycerides and ketone bodies were produced but ketosis was only produced<br />
in those cows that had a predisposition to the disease (12,13).<br />
Types of bovine ketosis<br />
There arc many theories on the cause, biochemical and hormonal pathogenesis of ketosis, and the<br />
importance of predisposing factors. Reviews of these studies are cited at the end of this disease<br />
section. In general, it can be stated that clinical ketosis occurs in ruminants when they are<br />
subjected to demands on their resources of glucose and glycogen that cannot be met by their<br />
digestive and metabolic activity.<br />
Recently Lean (1) has presented a classification of the disease based on its natural presentation<br />
in dairy herds, and one that accounts for the early lactational demand for glucose, a limited supply<br />
of propionate precursors and preformed ketones or mobilized lipids in the pathogenesis. Such a<br />
classification includes the following geneses of ketosis, which will be discussed in turn:<br />
1.Primary ketosis (production ketosis)<br />
2.Secondary ketosis<br />
3.Alimentary ketosis<br />
4.Starvation ketosis<br />
5.Ketosis due to specific nutritional deficiency.<br />
Primary ketosis (production ketosis)<br />
This is the ketosis of most herds, the socalled estate acetonemia. It occurs in cows in good to<br />
excessive body condition that have high lactation potential and are being fed good-quality rations.<br />
There is a tendency for the disease to recur in individual animals, winchis probably areflection of<br />
variation between cows in digestive capacity or metabolic efficiency. Thesecharacteristics appear<br />
not tobeinherited (14) and it is more probable thatthe rationsfed cause<br />
abnormalinternalmetabolism or ruminal function and leadto the development of ketosis.<br />
Secondary ketosis<br />
This occurs where other disease results in a decreased food intake. The cause of the reduction in<br />
food intake is commonly the result of abomasal displacement, traumatic reticulitis, metritis,<br />
mastitis or other diseases common to the postparturient period. A high incidence of ketosis has<br />
also been observed in herds affected with fluorosis. An unusual occurrence reported w as an<br />
outbreak of acetonemia in a dairy herd fed on a ration contaminated by a low level (9.5 ppm) of<br />
16
lincomycin, which caused ruminal microbial dysfunction (15). The proportion of cases of<br />
acetonemia which are secondary, and their diagnosis as such, are both matters of great interest as a<br />
significant proportion of cases of ketosis are secondary to other disease.<br />
Alimentary ketosis<br />
This form is due to excessive amounts of butyrate in silage and possibly also due<br />
to decreased food intake resulting from poor palatability of high butyrate silage. Silage made from<br />
succulent material may be more highly ketogenic than other types of ensilage because of its higher<br />
content of preformed butyric acid (16). Spoiled silage is also a cause and toxic bio-genic amines<br />
in silage, such as putresin, may also contribute (17). This type of ketosis is commonly subclinical<br />
but it may predispose to the development of production or primary ketosis.<br />
Starvation ketosis<br />
This occurs in cattle that are in poor body condition and that are fed poor-quality feedstuffs. There<br />
is a deficiency of propionate and protein from the diet and a limited capacity of gluconeogenesis<br />
from body reserves. Affected cattle recover with correct feeding.<br />
Ketosis due to specific nutritional deficiency<br />
Specific dietary deficiencies of cobalt and possibly phosphorus may also lead to a high incidence<br />
of ketosis. This may be due in part to a reduction in the intake of total digestible nutrients (TUN),<br />
but in cobalt deficiency the essential defect is a failure to metabolize propionic acid into the<br />
tricarboxylic acid (TCA) cycle. The problem is restricted to the cobalt deficient areas of the world,<br />
although the occurrence of cobalt deficiency in high-producing dairy cows in non-deficient areas<br />
has been described (18).<br />
ETIOLOGY OF OVINE KETOSIS<br />
Hypoglycemia and hyperketonemia are the primary metabolic disturbances in ovine ketosis as<br />
they are in the bovine disease. In sheep, the precipitating causes are the energy demands of the<br />
conceptus in the latter part of pregnancy. there are some biochemical differences between the two<br />
diseases, e.g. an elevation of plasma cortisol levels and significant hepatic dysfunction in<br />
pregnancy toxemia. Furthermore, in the terminal stages, the biochemical pathogenesis of the two<br />
diseases appears to be quite dissimilar.<br />
The most important etiological factor in pregnancy toxemia is a decline in the plane of nutrition<br />
during the last 2 months of pregnancy, particularly in ewes that are carrying twins or triplets, and<br />
in ewes that have been well fed in early and mid-pregnancy. There is a great deal of variation<br />
between sheep in the ease with which the disease can be produced experimentally, and in the<br />
variation in incidence of the naturally occurring disease in conditions which appear to be<br />
conducive to its development.<br />
It is probable that the difference between sheep depends upon the metabolic efficiency of the<br />
liver. Ewes that are predisposed to the disease have an ineffective gluconeogenic response to the<br />
continued, preferential demands for glucose by well-grown twin fetuses, resulting in<br />
hypoglycemia and the accumulation of ketone bodies and cortisol.<br />
The elevation of plasma cortisol levels, which is commonly encountered in ewes with<br />
pregnancy toxemia, has attracted attention because of its possible indication of adrenocortical<br />
involvement in causing the disease. It seems more likely that the observed increase is in response<br />
to environmental and nutritional stresses (19), and possibly to failure by the liver to metabolize the<br />
cortisol.<br />
According to the broad circumstances of occurrence, the disease in sheep can be divided as to<br />
17
cause as either 1. primary pregnancy toxemia, 2. Fat ewe pregnancy toxemia, 3. starvation<br />
pregnancy toxemia, or 4. secondary pregnancy toxemia.<br />
Primary pregnancy toxemia<br />
This is the most common manifestation and results in most flocks from a combination of a fall in<br />
the plane of nutrition during the latter half of pregnancy coupled with a short period of fast in<br />
conjunction with a management procedure in late pregnancy such as crutching, shearing and<br />
drenching. In some outbreaks the ewes have been moved on to better pasture during late<br />
pregnancy to prevent the occurrence of ketosis but it occurs because the ewes are unaccustomed to<br />
the type of feed and do not eat well, or because they are more exposed to bad weather and seek<br />
shelter rather than graze. Cold, inclement weather and an absence of shelter also appear to<br />
markedly increase the incidence. Another common occurrence is when ewes are bred too early<br />
and the pasture is not sufficiently advanced to provide a rising plane of nutrition m late pregnancy.<br />
Occasionally a stress alone will induce the condition such as: (1) transport in late pregnancy, (2)<br />
change in environment, or (3) the housing of late pregnant sheep not used to being housed.<br />
Fat ewe pregnancy toxemia<br />
This occurs without a stress induction in ewes that are very well fed and are in an overfat<br />
condition in late pregnancy. Fat ewes will experience a voluntary fall in food intake in late<br />
pregnancy due to the reduction of the rumen volume by the pressure of intra-abdominal fat and the<br />
developing fetus. Commonly there is concurrent hypocalcemia.<br />
Starvation pregnancy toxemia<br />
This occurs in ewes that are excessively thin. It is relatively uncommon but occurs in extensive<br />
grazing systems where there is prolonged drought and no alternative feed supply and can be seen<br />
in any production system where there is mismanagement.<br />
Secondary pregnancy toxemia<br />
This usually occurs as a sporadic disease as the result of the effect of an intercurrent disease such<br />
as foot rot, which affects food intake. Heavy worm infestation, e.g. with Haemonchus contortus,<br />
would add a similar drain on glucose metabolism and increase the chances of development of the<br />
disease.<br />
The disease occurs in goats during late pregnancy, where it is identical to ovine pregnancy<br />
toxemia and also in lactating does, where it resembles bovine ketosis. Goats exhibit greater<br />
dominant/submissive characteristics than sheep and this can result in lower food intake in<br />
submissive goats in groups that are hand fed.<br />
EPIDEMIOLOGY<br />
Ketosis in cattle<br />
Occurrence<br />
Ketosis is a disease of dairy cattle and is prevalent in most countries where intensive farming is<br />
practiced. It occurs mainly in animals housed during the winter and spring months and is rare in<br />
cows that calve on pasture.<br />
The occurrence of the disease is very much dependent upon management and nutrition and<br />
varies between herds. As might be expected, lactational incidence rates differ between studies but<br />
rates of 3.3% and 7.4% are reported from two Canadian studies (20, 21) and 6% from a Finnish<br />
study (22). Rates of sub-clinical ketosis are much higher, especially m undernourished herds, and<br />
can approach 34% (2,4, 9-11).<br />
18
Animal and management risk factors<br />
The disease occurs in the immediate post-parturient period with 90% of cases occurring in the first<br />
60 days of lactation (9-11, 23). Regardless of specific etiology it occurs most commonly during<br />
the first month of lactation, less commonly in the second month, and only occasionally in late<br />
pregnancy. In different studies the median time to onset following calving has varied from 10-28 d<br />
(20, 23). Cows of any age may be affected but the disease increases from a low prevalence at the<br />
first calving to a peak at the fourth. Clinical ketosis can also recur in the same lactation. There is<br />
little evidence for an heritable predisposition (11,19,23-25).<br />
In addition to those diseases that can produce secondary ketosis, there is a greater risk for the<br />
development of ketosis in cows that have an extended dry period, have a long dry period, are<br />
excessively fat at calving, and that develop milk fever, retained placenta, lameness or<br />
hypomagnesemia (20, 24, 25, 26-29). Overfeeding in late lactation predisposes ketosis in the next<br />
lactation. Cows with twins are also at risk for ketosis in the terminal stages of pregnancy (30, 31).<br />
Cows that have received bovine somatotrophin may be at less risk for ketosis in the subsequent<br />
lactation (29).<br />
Economic significance<br />
Clinical and subclinical ketosis is one of the major causes of loss to the dairy-farmer (32). In rare<br />
instances the disease is irreversible and the affected animal dies but the main economic loss is due<br />
to the loss of production while the disease is present and failure to return to full production after<br />
recovery (1). Both clinical and subclinical ketosis are accompanied by decreased milk yields and<br />
lower milk protein and milk lactose (1, 10, 29, 33) and increased risk for delayed estrus and lower<br />
first service conception rates, increased intercalving intervals (10, 34) and increased risk of cystic<br />
ovarian disease and mastitis (11, 35, 36).<br />
Sheep<br />
Occurrence<br />
Pregnancy toxemia occurs wherever sheep are raised but it is primarily a disease of intensive<br />
farming systems and is relatively rare in extensive grazing units unless there is drought or poor<br />
management.<br />
Animal and management risk factors<br />
The disease occurs only in ewes in the last 6 weeks of pregnancy, usually during the last month,<br />
and in ewes carrying triplet or twin lambs, although ewes bearing a single, large lamb may also be<br />
affected. The disease is uncommon in maiden ewes because of their low fecun¬dity and increases<br />
in prevalence up to parity three. In a study of sheep diseases in Canada, 19% of flocks were<br />
reported to have the disease (37).<br />
There is probably no breed difference in susceptibility and breed differences probably reflect<br />
differences in fecundity and differences in management systems. The British hill breeds arc<br />
possibly more resistant to the development of pregnancy toxemia in the face of nutritional<br />
deprivation of the ewe but resistance is achieved at the expense of lamb birth weight and has the<br />
penalty of higher neonatal mortality. There are however differences in the susceptibility of<br />
individual sheep that appear to be related to differences in rates of hepatic gluconeogenesis (38).<br />
The attack rate in a flock varies with the nature and severity of the nutritional deprivation and<br />
the proportion of the flock at risk. It can be very high in starvation pregnancy toxemia, whereas fat<br />
ewe pregnancy toxemia is generally of sporadic occurrence. In outbreaks that follow management<br />
procedures or other stressors, clinical disease is not manifest until 48 h afterwards and new cases<br />
19
will develop over several days. Intercurrent disease in late pregnant ewes, such as foot rot or foot<br />
abscess, may predispose pregnancy toxemia.<br />
Economic significance<br />
The economic effect of the disease is considerable. Without treatment, the case-fatality rate<br />
approaches 100% and in individual flocks the disease can reach a level of incidence sufficient to<br />
be classed as an outbreak. Flocks that experience pregnancy toxemia will also have a higher than<br />
normal mortality in neonatal lambs and usually a decrease in wool quality. Pregnancy toxemia<br />
predisposes to hypomagnesemia in sheep.<br />
PATHOGENESIS<br />
Bovine ketosis<br />
The principal metabolic disturbances observed,hypoglycemia and ketonemia, may both exert an<br />
effect on the clinical syndrome. However, in the experimental disease in cattle, it is not always<br />
clear what determines the development of the clinical signs in cases that convert from sub-clinical<br />
to clinical ketosis (39). In many cases, the severity of the clinical syndrome is proportional to the<br />
degree of hypoglycemia and this, together with the rapid response to parenterally administered<br />
glucose in cattle, suggests hypoglycemia as the predominant factor. This hypothesis is supported<br />
by the development of prolonged hypoglycemia and a similar clinical syndrome to that of ketosis,<br />
after the experimental, IV or SC injection of insulin (2 units/kg BW).<br />
However, in most field cases the severity of the clinical syndrome is also roughly proportional<br />
to the degree of ketonemia. This is an understandable relationship as ketone bodies are produced<br />
in larger quantities as the deficiency of glucose increases. However, the ketone bodies may exert<br />
an additional influence on the signs observed. Acetoacetic acid is known to be toxic and probably<br />
contributes to the terminal coma in diabetes mellitus in man.<br />
The nervous signs which occur in some cases of bovine ketosis are thought to be caused by the<br />
production of isopropyl alcohol, a breakdown product of acetoacetic acid in the rumen, although<br />
the requirement of nervous tissue for glucose to maintain normal function may also be a factor in<br />
these cases.<br />
Spontaneous ketosis in cattle is usually readily reversible by treatment;incomplete or temporary<br />
response is usually due to the existence of a primary disease with ketosis present only as a<br />
secondary development, although fatty degeneration of the liver in protracted cases may prolong<br />
the recovery period. Changes in ruminal flora after a long period of anorexia may also cause<br />
continued impairment of digestion.<br />
The higher susceptibility of postpartum cows to local and systemic infections may be related to<br />
impairment of the respiratory burst of neutrophils which occurs with elevated levels of BHBA (40).<br />
Pregnancy toxemia in sheep<br />
The disease in sheep is manifest with encephalopathy and is frequently not reversible unless<br />
treated in the early stages. The onset of clinical signs is always preceded by hypoglycemia and<br />
hyperketonemia. although the onset of signs is not related to minimum glucose or maximum<br />
ketone levels.<br />
The cause of the encephalopathy is not certain but it is probable that it is a hypoglycemic<br />
encephalopathy resulting from hypoglycemia in the early stages of the disease (41-43). In affected<br />
ewes, there is an abnormally high level of cortisol in plasma and both early and recent research<br />
has suggested that adrenal steroid diabetes contributes to the pathogenesis (44).<br />
Renal dysfunction is also apparent in the terminal stages of ovine ketosis, and may also<br />
20
contribute to the development of clinical signs and the fatal outcome. Those ewes which are<br />
carrying only one lamb and have been well fed prior to a short period of undernutrition may<br />
develop a subacute syndrome both clinically and biochemically.<br />
CLINICAL FINDINGS<br />
Bovine ketosis<br />
Two major forms of bovine ketosis arc described - wasting and nervous - but these are the two<br />
extremes of a range of syndromes in which wasting and nervous signs are present in varying<br />
degrees of prominence.<br />
THE WASTING FORM is the most common of the two and is manifest with a gradual but<br />
moderate decrease in appetite and milk yield over 2-4 d. In herds that feed components separately,<br />
the pattern of appetite loss is often unusual in that the cow first refuses to eat grain, then ensilage<br />
but may continue to eat hay. The appetite may also be depraved.<br />
Body weight is lost rapidly, usually at a greater rate than one would expect from the decrease in<br />
appetite. Farmers usually describe affected cows as having a “woody” appearance due to the<br />
apparent wasting and loss of cutaneous elasticity due presumably to disappearance of SC fat. The<br />
feces are firm and dry but serious constipation does not occur. The cow is moderately depressed<br />
and the hangdog appearance and disinclination to move and to eat may suggest the presence of<br />
mild abdominal pain.<br />
The temperature and the pulse and respiratory rates are normal and although the ruminal<br />
movements may be decreased in amplitude and number, they are within the normal range unless<br />
the course is of long duration when they may virtually disappear. A characteristic odor of ketones<br />
is detectable on the breath and often in the milk.<br />
Very few affected animals die, but without treatment the milk yield falls and although<br />
spontaneous recovery usually occurs over about a month, as equilibrium between the drain of<br />
lactation and food intake is established, the milk yield is never fully regained. The fall in milk<br />
yield may be as much as 25% and there is an accompanying sharp drop in the solids-not-fat<br />
content of the milk. In the wasting form, nervous signs may occur in a few cases but rarely<br />
comprise more than transient bouts of staggering and partial blindness.<br />
THE NERVOUS FORM Signs are usually bizarre and begin quite suddenly. The syndrome is<br />
suggestive of delirium rather than of frenzy and the characteristic signs include:<br />
• Walking in circles<br />
• Straddling or crossing of the legs<br />
• Head pushing or leaning into the stanchion<br />
• Apparent blindness<br />
• Aimless movements and wandering<br />
• Vigorous licking of the skin and inanimate objects<br />
• Depraved appetite<br />
• Chewing movements with salivation.<br />
Hyperesthesia may be evident, the animal bellowing on being pinched or stroked. Moderate<br />
tremor and tetany may be present and there is usually an incoordinate gait. The nervous signs<br />
usually occur in short episodes which last for 1 or 2 h and may recur at intervals of about 8-12 h.<br />
Affected cows may injure themselves during the nervous episodes.<br />
Subclinical bovine ketosis<br />
Many cows that are in negative energy balance in early pregnancy will have ketonuria without<br />
21
showing clinical signs, but will have diminished productivity including depression of milk yield<br />
and a reduction in fertility. Potential milk production is reduced by 1-9% (11,33). Surveys of large<br />
populations show a declining prevalence of ketosis-positive cows after a peak in the period<br />
immediately after calving, and a positive relationship between hyperketonemia and high milk<br />
yield (9,35). Infertility may appear as an ovarian abnormality, delayed onset of estrus or as<br />
endometritis resulting in an increase in calving to conception interval and reduced conception rate<br />
at first insemination. In Europe, endometritis itself is thought to be a sequel to a nutritional stress<br />
at this time, but much of the stress there is due to overfeeding in early lactation which increases<br />
the risk for both endometritis and acetonemia (45,46).<br />
Ovine ketosis<br />
The earliest signs of ovine ketosis are separation from the group, failure to come up for feeding,<br />
and apparent blindness which is manifested by an alert bearing but a disinclination to move. The<br />
ewe will stand still when approached by attendants or dogs and will turn and face them but make<br />
no attempt to escape. If it is forced to move, it blunders into objects and when an obstacle is<br />
encountered, presses against it with its head. Many affected ewes stand in water troughs all day<br />
and lap the water. Constipation is usual, the feces are dry and scanty and there is grinding of the<br />
teeth.<br />
In later stages, marked drowsiness develops and episodes of more severe nervous signs occur but<br />
they may be infrequent and are easily missed. In these episodes, tremors of the muscles of the<br />
head cause twitching of the lips, champing of the jaws and salivation, and these are accompanied<br />
by a cog-wheel type of clonic contraction of the cervical muscles causing dorsiflexion or lateral<br />
deviation of the head, followed by circling. The muscle tremor usually spreads to involve the<br />
whole body and the ewe falls with toniclonic convulsions. The ewe lies quietly after each<br />
convulsion and rises normally afterwards but is still blind.<br />
In the periods between convulsions there is marked drowsiness which may be accompanied by<br />
head pressing, the assumption of abnormal postures including unusual positions of the limbs and<br />
elevation of the chin - the“stargazing”posture - and incoordination and falling when attempting to<br />
walk. A smell of ketones may be detectable on the breath of the ewe.<br />
Affected ewes usually become recumbent in 3-4 d and remain in a state of profound depression<br />
or coma for a further 3-4 d, although the clinical course is shorter in fat ewes with pregnancy<br />
toxemia. Fetal death occurs commonly and is followed by transient recovery of the ewe, but the<br />
toxemia caused by the decomposing fetus soon causes a relapse.<br />
Affected ewes commonly have difficulty in lambing. Recovery may ensue if the ewe lambs or<br />
the lambs are removed by cesarean section in the early stages of the disease. In an affected flock<br />
the disease usually takes the form of a prolonged outbreak; a few ewes become affected each day<br />
over a period of several weeks. Recovered ewes may subsequently show a wool break.<br />
CLINICAL PATHOLOGY<br />
Hypoglycemia, ketonemia and ketonuria are characteristic of the disease<br />
Cattle<br />
BLOOD GLUCOSE levels are reduced from the normal of approximately 50 mg/dL to 20-40<br />
mg/dL in cattle and sheep. Ketosis secondary to other diseases is usually accompanied by blood<br />
glucose levels above 40 mg/dL and often above normal.<br />
Ketones<br />
BLOOD KETONE levels are elevated from a normal of up to 10 mg/dL to 10-100 mg/dL. The<br />
22
levels are high also in secondary ketosis but are rarely above 50 mg/dL. In Europe, serum<br />
beta-hydroxybutyrate measured in SI units is used for analysis of ketonemia. Normal cows have<br />
concentrations of less than 1.0 mmol/L and cows with ketosis have levels greater than 1.5 mmol/L<br />
and often in excess of 2.5 mmol/L.<br />
URINE KETONES Quantitative estimation of urinary ketones may be unsatisfactory because of<br />
the wide variations that occur depending upon the concentration of the urine. In clinically normal<br />
cattle, urinary ketones may be as high as 70 mg/dL, although they are usually lower than 10<br />
mg/dL. Levels of 80-1300 mg/dL indicate the presence of ketosis which may be primary or<br />
secondary.<br />
MilK KETONE levels are rather less variable, ranging from a normal of 3 mg/dL up to an average<br />
level of 40 mg/dL in cows with ketosis.<br />
COWSIDE TESTS are based on color reaction of ketone bodies and may be conducted on milk or<br />
urine. Milk is usually tested with sodium nitroprusside in the well of a porcelain plate.<br />
Commercial tablets or dip sticks are available for testing urine. The color change should be<br />
compared with a set of standard color references. There is some difference of opinion as to<br />
whether primary and secondary ketosis can be differentiated on the basis of the degree of color<br />
change in the reagent, but primary cases always give a strong reaction, whereas a moderate<br />
reaction is more common in secondary cases. Rough quantitative estimations of blood ketones can<br />
also be quickly made with some commercial reagents.<br />
Cowside tests have the advantage of being inexpensive, giving immediate results, and they can<br />
be used as frequently as necessary. A minor source of error is that the concentration of ketone<br />
bodies in these fluids will depend not only on the ketone level of the blood but also on the amount<br />
of urine excreted or on the milk yield. Milk is less variable, easier to collect and may give fewer<br />
false negatives with subclinical ketosis. A recent study reported that when subclinical ketosis was<br />
defined as a blood beta-hydroxybutyric acid concentration of 1.4 mmol/L or greater, the<br />
sensitivity of the milk test was 90% and the specificity 96%. The sensitivity of the urine test was<br />
100% but specificity was low (10). A dip stick test for semiquantitative measurement of<br />
beta-hydroxybutyric acid in milk is recently available in some countries and has good sensitivity<br />
(47).<br />
CLINICAL CHEMISTRY AND HEMATOLOGY<br />
White and differential cell counts are variable and not of diagnostic value for ketosis.<br />
There are usually elevations of liver enzymes but liver function tests are within the normal<br />
range. Liver biopsy is the only accurate method to determine the degree of liver damage (48).<br />
Liver glycogen levels are low and the glucose tolerance curve may be normal. Volatile fatty<br />
acid levels in blood and rumen are much higher in ketotic than in normal cows and the ruminal<br />
levels of butyric acid are markedly increased relative to acetic and propionic acids. There is a<br />
small but significant fall in serum calcium levels (down to about 9 mg/dL (2.25 mmol/L), due<br />
probably to increased loss of base in the urine to compensate for the acidosis.<br />
Sheep<br />
In sheep, the initial changes are similar to those found in cattle but the sequel is not.<br />
Hypoglycemia can be used as a diagnostic aid in the early stages of the disease but is of limited<br />
value later in the course as by the time that sheep become recumbent, blood glucose levels may be<br />
normal or grossly elevated. This may be the result of fetal death which has been shown to remove<br />
the suppressing effect of the fetus on hepatic neoglucogenesis (38).<br />
23
Ketonemia and ketonuria are constant and serum beta-hydroxybutyrate concentrations are in<br />
excess of 3.0 mmol/L (42).<br />
Sheep develop a severe metabolic acidosis, renal failure with a terminal uremia, and become<br />
dehydrated. In contrast to cattle, liver function tests are abnormal (49). Elevation of plasma<br />
cortisol occurs in pregnancy toxemia and concentrations above10 ng/ml are indicative of<br />
pregnancy toxemia (50), but pregnancy toxemia and clinical hypocalcemia can both cause<br />
sufficient stress to promote such an elevation.<br />
NECROPSY FINDINGS<br />
The disease is not usually fatal in cattle but fatty degeneration of the liver and secondary changes<br />
in the anterior pituitary gland and adrenal cortex may be present.<br />
Pregnancy toxemia in ewes is almost always fatal without treatment intervention. At necropsy<br />
there is severe fatty degeneration of the liver and there are usually twin lambs and evidence of<br />
constipation. Histopathologically there is also a poorly defined renal lesion and there may be<br />
evidence of neuronal necrosis (41). The lambs may be dead and in varying stages of<br />
decomposition. Hepatic glycogen levels are usually very low in both sheep and cattle.<br />
Concentrations of beta-hydroxybutyrate in the aqueous humor or the CSF greater than 2.5 or 0.5<br />
mmol/L, respectively, are supportive of a diagnosis of pregnancy toxemia (42).<br />
DIFFERENTIAL DIAGNOSIS<br />
Cattle<br />
The clinical picture is usually too indefinite, especially in cattle, to enable a diagnosis to be made<br />
solely on clinical grounds. General consideration of the history, with particular reference to the<br />
time of calving, the duration of pregnancy in ewes and the feeding program, and biochemical<br />
examination to detect the presence of hypoglycemia, ketonemia and ketonuria are necessary to<br />
establish a diagnosis.<br />
Wasting form<br />
• Abomasal displacement (pp.321,326)<br />
• Traumatic reticulitis (p.303)<br />
• Primary indigestion (p.280)<br />
• Cystitis and pyelonephritis (pp.491,492)<br />
• Diabetes mellitus (rare) (p.360).<br />
Nervous form<br />
• Rabies (p.1201)<br />
• Hypomagnesemia (pp.1442,1510)<br />
• Bovine spongiform encephalopathy (p.1233).<br />
Sheep<br />
Pregnancy toxemia is usually suspected in late pregnant ewes which show nervous signs and die<br />
within 2-7 d and there may be a history of exertion or sudden deprivation of food. Hypocalcemia<br />
can occur under similar circumstances but:<br />
1. The onset is within 12 h of the stress<br />
2. A considerable proportion of the flock will be affected at the same time<br />
3. The disease is manifest with myasthenia<br />
4. It has a much shorter course of 12-24 h<br />
5. Affected animals respond well to treatment with solutions of calcium salts.<br />
• Listeriosis<br />
24
• Cerebral abscess (p.533)<br />
• Rabies.<br />
TREATMENT<br />
In cattle, a number of effective treatments are available but in some affected animals the response<br />
is only transient; in rare cases the disease may persist and cause death or necessitate slaughter of<br />
the animals. Most of these cases are secondary and failure to respond satisfactorily to treatment is<br />
due to the primary disease.<br />
The rational treatment in ketosis is to relieve the need for glucose formation from tissues and<br />
allow ketone body utilization to continue normally. Theoretically the simplest means of doing this<br />
is by the administration of glucose replacement therapy. The effect of the administration of<br />
glucose is complex but it allows the reversal of ketogenesis and the establishment of normal<br />
patterns of energy metabolism (7).<br />
Replacement therapy<br />
Glucose (dextrose)<br />
The IV injection of 500 mL of a 50% solution of glucose results in transient hyperglycemia,<br />
increased insulin and decreased glucagon secretion, and reduced plasma concentration of<br />
non-esterified fatty acids. It effects a marked improvement in most cows but relapses occur<br />
commonly unless repeated treatments are used. This is probably due to the transience of the<br />
hyperglycemia or insufficient dosing - the dose required varies directly with the amount of lactose<br />
being lost in the milk. A significant proportion of the administered glucose is lost to urinary<br />
excretion. SC injections prolong the response but are not recommended as they cause discomfort,<br />
and large unsightly swellings, which often become infected may result. IP injections of 20%<br />
solution of dextrose may be used alternatively but are also accompanied by risk of infection.<br />
Other sugars<br />
Other sugars, especially fructose, either alone or as a mixture of glucose and fructose (invert<br />
sugar), and xylitol have been used in an effort to prolong the response but idiosyncrasies to some<br />
preparations, in the form of polypnea, muscle tremor,weakness and collapse, can occur while the<br />
injection is being given.<br />
Propylene glycol and glycerine<br />
To overcome the necessity for repeated injections, propylene glycol or glycerine (225 g twice<br />
daily for 2 d followed by 110 g daily for 2 d to cattle) can be administered as a drench. These<br />
solutions, or salts of propionic acid, can be administered in the feed and give excellent results.<br />
Administration in feed is preferred by some because this method avoids dangers of aspiration with<br />
drenching; however, cows not used to its inclusion in the feed may show feed refusal. It is<br />
recommended that for best results, dosing with these preparations be preceded by an IV injection<br />
of glucose.<br />
Parenteral infusions of glucose solutions and the feeding of glycerol depress the fat content of<br />
milk, and the net saving in energy may favorably influence response to these drugs. Glycerol and<br />
propylene glycol are not as efficient as glucose because conversion to glucose does utilize<br />
oxaloacetate. Propylene glycol is absorbed directly from the rumen and acts to reduce ketogenesis<br />
by increasing mitochondrial citrate concentrations; its metabolism to glucose occurs via<br />
conversion to pyruvate with subsequent production of oxaloacetate via pyruvate carboxylase (7).<br />
Other glucose precursors<br />
Because of its glucogenic effect, sodium propionatc is theoretically a suitable treatment but when<br />
25
administered in 110-225 g doses daily, the response in cattle is often very slow. Lactates are also<br />
highly glucogenic but both calcium and sodium lactate (1 kg initially, followed by 0.5 kg for 7 d)<br />
and sodium acetate (110-500 g/d) have given less satisfactory results than those obtained with<br />
sodium propionate. Ammonium lactate (200 g for 5 d) has however, been used extensively with<br />
reported good results. Sodium ethyl oxaloacetate given IV is effective in natural and experimental<br />
cases in ewes but is unlikely to be a practical form of treatment because of cost.<br />
Hormonal therapy<br />
GLUCOCORTICOIDS The efficiency of glucocorticoids in the treatment of bovine ketosis has<br />
been amply demonstrated in both experimental and field cases. Hyperglycemia occurs within 24 h<br />
of administration and appears to result from a repartitioning of glucose in the body rather than<br />
from gluconeogenesis (7). Historically, many preparations have been used successfully but current<br />
drugs are more potent, require lower dosage, and have fewer side-effects. A hyperglycemic state is<br />
produced for 4-6 d in ketotic cows given 10 mg of dexamethasone 21-isoni-cotinate and other<br />
preparations such as dexamethasone sodium phosphate (40 mg) and flumethasone (5 mg) are also<br />
used. Label regulations vary between countries and in general the recommendations of the<br />
manufacturer with regard to use and dosage should be followed. Profound hypokalemia with high<br />
case fatality is a potential sequel to prolonged repeated therapy of ketosis with isofluprednone<br />
acetate (51). Response of cows with primary ketosis to treatment with corticosteroids and IV<br />
glucose is superior, with fewer relapses, than therapy with corticosteroids or glucose alone (52).<br />
INSULIN facilitates cellular uptake of glucose, suppresses fatty acid metabolism and stimulates<br />
hepatic gluconeogenesis. It is administered in conjunction with either glucose or a glucocorticoid<br />
and may be of particular value in early-onset cases of ketosis that are unresponsive to glucose or<br />
corticosteroid therapy (7). The dose of protamine zinc insulin is 200-300 iu per animal<br />
administered SC every 24-48 h as required.<br />
ANABOLIC STEROIDS have also been used for treatment of lactational ketosis and ketosis in<br />
late pregnant cows that are overfat, stressed or have twin fetuses. Experimentally, 60 mg and 120<br />
mg of trenbolone acetate are effective as single injections but no extensive field trials are recorded<br />
and the drug is banned for use in food animals in most countries.<br />
MISCELLANEOUS TREATMENTS VitaminB12 and cobalt are indicated in regions where cobalt<br />
deficiency is a risk factor for ketosis. They are sometimes administered to cattle with ketosis in<br />
regions where cobalt deficiency does not occur but their therapeutic value is not proven.<br />
Cysteamine (a biological precursor of coenzyme A) and also sodium fumarate have been used to<br />
treat cases of the disease. Reported results were initially good but the treatment has not been<br />
generally adopted. The recommended dose rate of cysteamine is 750 mg IV for three doses at<br />
1-3-day intervals.<br />
There is some limited evidence that niacin given in the feed has a beneficial effect on the disease<br />
in cattle (1, 23) and on the glucogenic potential of diets in sheep. Niacin is antilipolytic and<br />
induces increases in blood glucose and insulin. It has been suggested that it should be<br />
supplemented from 2 weeks prior to parturition to 12 weeks postpartum (53).<br />
Treatment in sheep<br />
Sheep treated very early in the course of the disease generally respond favorably but response to<br />
therapy is poor once sheep have become recumbent and the IV administration of 50% dextrose at<br />
this time may hasten death. Therapy requires the correction of fluid, electrolyte and acid-base<br />
disturbances in addition to replacement therapy with glucose.<br />
26
PARENTERAL THERAPY Ideally, individual sheep should be examined biochemically and the<br />
corrective therapy based accordingly, with fluids, electrolytes and glucose given over a prolonged<br />
period of time. One recommendation for replacement therapy is the administration of 5-7 g of<br />
glucose IV 6-8 times a day in conjunction with 20-40 units of zinc protamine insulin given IM<br />
every other day for 3 d (54).<br />
In many sheep-raising areas intensive monitoring and therapy is not possible because of access,<br />
expense, or the number of sheep involved in an outbreak. In the absence of biochemical<br />
monitoring, therapy with glucose should be accompanied by the IV injection of isotonic sodium<br />
bicarbonate or lactated Ringer's solution and the administration of further fluids by a stomach tube.<br />
Less intensive therapy includes the use of propyiene glycol or glycerine (ll0g/d by mouth), which<br />
have given excellent results for some workers but poor results for others.<br />
Standard doses of corticosteroids have little therapeutic effect in sheep and therefore treatment<br />
with these drugs is not recommended. Very large doses are effective in ewes still able to stand but<br />
the success probably rests in the removal of the glucose drain by the induction of premature<br />
parturition.<br />
ORAL THERAPY Success in therapy is reported with the oral drenching, every 4-8 h, of 160 mL<br />
of a solution containing 45 g glucose, 8.5g sodium chloride.6.17g glycine and electrolytes, which<br />
is available commercially as a concentrated oral rehydration solution for calves with diarrhea. This<br />
therapy is now commonly used in the United Kingdom. Drenching of non-pregnant sheep with<br />
this solution is followed by higher blood concentrations of glucose than those achieved following<br />
drenching with glycerol or propylene glycol. Reported recovery rates in pregnancy toxemia are<br />
90% in early cases and 55% in advanced cases (55). Vasopressin has been used to induce closure<br />
of the esophageal groove in conunction with the oral administration of glucose.<br />
Treatment with recombinant bovine somatotrophin in conjunction with dextrose and<br />
electrolytes may improve ewe survival and result in a greater viability of lambs born (56).<br />
REMOVAL OF FETUS Cesarian section<br />
can be used as an alternate to replacement therapy. Provided ewes are in the early stages of the<br />
disease, removal of the lambs by cesarean section is probably the therapy that has the greatest<br />
success rate. Induction of parturition is another option. Either should only be attempted in the<br />
early stage of the disease as in the later stages the ewe’s condition is irreversible and the fetuses<br />
are often dead and decomposed. Induction with corticosteroids has been effected with<br />
dexamethasone 21-isonicotinate or the sodium phosphate at a dose rate of 16-25 mg per ewe but<br />
dexamethasone trimethylacetate appears to be ineffective. Lambs will be born 48-72 h after<br />
injection.<br />
When clinical cases occur, the rest of the flock should be examined daily for any evidence of<br />
ketosis and affected animals treated immediately with propylene glycol or glycerol.<br />
Supplementary feeding of the flock should be commenced immediately, with particular attention<br />
given to an increase in carbohydrate intake. With timid sheep, especially Merinos, the simple<br />
provision of feed may not be enough. It may be necessary to improve the palatability of the ration,<br />
and to get the sheep started by force feeding.<br />
CONTROL<br />
It is difficult to make general recommendations for the control of the disease because of the many<br />
conditions under which it occurs, its probable multiple etiology and feeding systems that vary<br />
27
from those that feed components separately to those that feed total mixed rations.<br />
Cattle<br />
Cows should neither have been starved nor be overfat at calving. One recommendation is that<br />
there should be a target of less than 10% of late lactation and dry cows with condition scores of 4<br />
on a 1-5 scale (57). An adequate caloric intake should be insured in the early part of lactation. In<br />
heavy-producing, heavily fed herds the big problem is to provide enough feed to avoid a deficient<br />
caloric intake, relative to utilization, but at the same time to avoid imbalance, ruminal acidosis on<br />
a too-high carbohydrate diet and acetonemia on a diet too high in protein. Too low a feeding<br />
frequency can lead to an increase in rates of ketosis (46). Careful estimation of diets by reference<br />
to feed value tables is recommended and detailed recommendations on diet and management have<br />
been provided (58,59).<br />
Points of general advice for herds in which feeding systems are not highly sophisticated are that<br />
cows should not be too fat nor too thin at the end of lactation, and that feeding in preparation for<br />
the next lactation should not begin until about 4 weeks prior to calving. At that time, the silage, or<br />
hay. or pasture being used as a maintenance ration should be supplemented with 1kg/d concentrate<br />
and this amount gradually increased to 5 kg daily at calving time. After calving the concentrate<br />
ration should be increased gradually as production increases, and be of the order of 3 kg/100 kg<br />
BW hay for maintenance (3 kg ensilage is equivalent to 1kg hay) and 1kg grain for each 3kg milk<br />
produced. In general, feeding should be at a slightly higher level than production actually warrants<br />
- lead feeding. The protein in the total ration should not exceed 16%, certainly not more than 18%,<br />
the carbohydrate should be readily digestible, and it oats or maize are used they should be crushed,<br />
and the hay or ensilage must be of good quality.<br />
In high-producing cows being fed stored feeds, poor quality roughage commonly leads to<br />
acetonemia. Wet ensilage containing much butyrate, and moldy or old and dusty hay, are the main<br />
offenders. In concentrates it is the change of source which creates off-feed effects and precipitates<br />
attacks of acetonemia.<br />
Cows that are housed should get some exercise each day and in herds where the disease is a<br />
particular problem during the stabling period, the cattle should be turned out to pasture as soon as<br />
possible in the spring.<br />
The ration should contain adequate amounts of cobalt, phosphorus, and iodine.<br />
If there is a high incidence in a herd receiving large quantities of ensilage, reduction of the<br />
amount fed for a trial period is indicated.<br />
The prophylactic feeding of sodium propionate may be considered in problem herds: 110 g/d<br />
for 6 weeks, commencing at calving, has given good results in reducing the incidence of clinical<br />
bovine ketosis and improving production. Propylene glycol (350 mL/d for 10 d after calving, or as<br />
6% of a concentrate ration for 8 weeks) has been similarly used with moderately good results.<br />
Theoretically, any procedure which increases the ratio of propionate to acetate production in the<br />
rumen would be of assistance in preventing ketosis. Monensin is a growth stimulant which acts in<br />
this way and the effective use of the compound in the prevention of ketosis in dairy cows has been<br />
reported (1, 23, 60) but it will also result in milk fat depression. The dose rate used was 25 mg/d<br />
monensin in a grain feed mix. Dose rates need to be monitored carefully because of the risks of<br />
toxicity which are described separately, Ionophores are not labelled for inclusion in lactating cow<br />
rations in some countries. Somatotropin also has considerable promise for the control of bovine<br />
ketosis (1).<br />
28
The control of clinical ketosis is integrally related to the adequate nutrition of the cow in the dry<br />
and lactating period. This encompasses details such as:<br />
•Dry matter intake<br />
•Fiber digestibility<br />
•Particle size distribution<br />
•Energy density<br />
•Fat incorporation in early lactation rations<br />
•Protein content<br />
•Feeding systems<br />
•Rumen size<br />
•Other factors better covered in texts on nutrition.<br />
These subjects have been visited from the point of view of clinical veterinary nutrition in a<br />
recent review series of articles (59). Experimental observations have tended to reduce the<br />
importance of heavy feeding of ensilage, failure to provide an adequate mineral mixture and<br />
failure to provide grain to stall-fed cows in late pregnancy. However, in view of the known<br />
multiple-factor etiology of this disease, these experiments do not prove that under particular sets<br />
of circumstances one or other of these factors may not be the precipitating cause.<br />
Sheep<br />
The same general recommendations apply in the prevention of ovine ketosis as in the prevention<br />
of ketosis in cattle. Insure that the plane of nutrition is rising in the second half of pregnancy, even<br />
if it means restricting the diet in the early stages.<br />
Ewes that are in condition score 2.5-3.0 on a 1.0-5.0 scale at 90 d of gestation and are in an<br />
ideal situation to respond to increased feeding in the latter part of gestation (19). If necessary,<br />
ewes with higher condition scores at the end of the first month of pregnancy can be fed to lose 0.5<br />
condition score during the period to the third month of pregnancy without any significant effect on<br />
the ewe or lamb size or viability. Many small farm sheep producers have sheep in too great a<br />
condition score early in pregnancy.<br />
The last 2 months are particularly important in the prevention of pregnancy toxemia as 70% of<br />
the lamb's birth weight is gamed during the last 6 weeks of pregnancy. During this period, the<br />
provision of a concentrate containing 10% protein at the rate of 0.25 kg/d, increasing to 1 kg/d in<br />
the last 2 weeks, has provided good protection. During this period the ewe should gain an increase<br />
of body weight of 10% for ewes with single lambs and 18% in ewes carrying twins. For the flock<br />
this represents a flock body condition score that maintains or gains to 3.0 3.5 during this period.<br />
Higher body condition scores can result in higher birth weight of lambs but other than in stud<br />
flocks these are not economic and the standard commercial flock runs the risk of fat ewe<br />
pregnancy toxemia with higher targeted body condition scores.<br />
An exception is the maiden ewe group which needs to be fed separately in order to provide for<br />
the requirement for growth in addition to the requirement for pregnancy, in fat ewes the only<br />
nutritional method of improving energy intake is to increase the energy density of the diet.<br />
There are managemental difficulties in any nutritional program for sheep because of the way<br />
they are husbanded. If there were a satisfactory way of easily determining the stage of pregnancy<br />
and whether there are one, two or three or no fetuses present, and if the sheep could then be<br />
divided into a number of subflocks so that the appropriate feeding regimen could be provided, it<br />
would be economical if separate paddocks and labor were available, to arrange a preventive<br />
29
feeding program. The use of ultrasound offers this selection and allows feeding to specific group<br />
requirements.<br />
Some account needs to be taken also of those ewes (and does) which are timid and for this and<br />
other reasons slow feeders. If supplementary feeding is practiced in a confined space, with<br />
insufficient trough space for all the flock to eat at one time, and if the feed fed is in small amounts<br />
and highly edible, a large proportion of ewes will get little or no feed. These difficulties add up to<br />
a formidable barrier in large flocks with minimum labor. It is necessary before embarking on a<br />
nutritional support program to estimate cost effectiveness. At the low level of prevalence that<br />
pregnancy toxemia usually achieves in well-managed flocks, it is often more profitable to do<br />
nothing and to let the disease occur in the very occasional sheep and treat it accordingly.<br />
Sudden changes in type of feed should be avoided and extra feed provided during bad weather.<br />
Shelter sheds should be available, and in purely pastoral areas lambing should not occur before the<br />
pasture is well grown. A high incidence is often encountered in small, well-fed flocks where the<br />
ewes get insufficient exercise. In such circumstances the ewes should be driven about for<br />
half-an-hour twice daily and, if pasture is available, only concentrate should be fed so that they<br />
will be encouraged to forage for themselves.<br />
General control<br />
HKRD MONITORING Biochemical monitoring of herds for subclinical ketosis and adequacy of<br />
periparturient feeding can be conducted using blood glucose estimations on a sample of cows in<br />
their 2nd week of lactation (53). Blood glucose levels of below 35 mg/dL (1.9mmol/L) suggest<br />
subclinical ketosis. For individual cows, blood glucose estimations should be done at about 14 d<br />
after calving. Regular tests for ketones in urine in the 2nd week after parturition has also been<br />
recommended for early detection of ketosis.<br />
Blood or milk BHBA levels or milk acetone levels are probably more accurate. Cut point levels<br />
vary with investigators but cow serum BHBA concentrations greater than 1.2-1.7 mmol/L<br />
(7-10mg/dL), milk BHBA concentrations greater than 100 mmol/L, or milk acetone<br />
concentrations greater than 0.70 mmol/L are indicative of subclinical ketosis (9,47). It has been<br />
suggested that milk acetone concentration should not exceed 0.05 mmol/L for maximal potential<br />
milk production (36).<br />
FLOCK MONITORING for latent pregnancy toxemia during the last 6 weeks of pregnancy can be<br />
conducted using blood BHBA as an indicator with concentrations of 0.8 mmol/L indicating<br />
adequate energy intake, 0.8-1.6 mmol/L inadequate energy intake and levels greater than 1.6<br />
mmol/L indicating severe undernourishment.<br />
REVIEW LITERATURE<br />
Brockman, R.I.(1979) Roles for insulin and glucagon in the development of ruminant ketosis.<br />
Can.Vet.J.,20,121.<br />
Littledike,E. T.,Young.J.W.& Beitz,D.C.(1981) Common metabolic diseases of cattle: ketosis.<br />
milk fever, grass tetany and downer cow complex.J.Dairy Sci.,64,1465-1482.<br />
Kronfield.D.S.(1982) Major metabolic determinants of milk volume, mammary efficiency, and<br />
spontaneous ketosis m dairy cows.J.Dairy Sci.,65. 2204-2212.<br />
Baird, G. D. (1982) Primary ketosis in the high-producing dairy cow: clinical and subclinical<br />
disorders,treatment,prevention and outlook.J.Dairy Sci.,65,1-10.<br />
Kelly, J. M. & Whitakcr. D. A. (1984) Subclinical ketosis and dairy cows. Vet.Ann., 24, 83-93.<br />
Brockman. R.P.& Loorveld, B(1986) Hormonal regulation of metabolism in ruminants; a<br />
30
eview. Livestock Prod. Sci.,14.313-334.<br />
Marteniuk. J. W. & Herdt, T.H.(1988)Pregnancy toxemia and ketosis of ewes and does. Vet. din.<br />
North Am.: Food Anim. Pract., 4(2), 307-315.<br />
Lean. I.J., Brass. M L.,Baldwin, R. L. & Trout, H. F. (1991) Bovine ketosis: a review. I.<br />
Epidemiology and pathogenesis. Vet. Bull., 61, 1209-1218.<br />
Herdt,T.H.& Emery,R. S. (1991) Therapy of diseases of ruminant intermediary metabolism.Vet.<br />
Clin.North Am.: Food AnimPract.,8(1).91-106.<br />
Lean,I.J.,Bruss,M.L.,Baldwin, R.L. & Trout, H. F.(1992) Bovine ketosis:a review II.<br />
Biochemistry and prevention.Vet. Hull., 62,1-13.<br />
REFERENCES<br />
(1)Lean, I. J. et al. (1992) Vet. Bull., 62, 1.<br />
(2)Brockman, R. P. & Laarveld, B. (1986)Livestock Prod. Sci., 74, 313.<br />
(3)Sutton.J. D. (1985)J Dairy Sci., 68, 3376.<br />
(4)Mills, S. E. et al. (1986)J. Dairy Sci., 69,362.<br />
(5)Steen, A. et al. (1997) J. Vet. Med. Assoc,44, 521.<br />
(6)Holtenuis, P. & Holtenuis, K. (1996) J.Vet. Med. Assoc, 43, 579.<br />
(7)Herdt, T. H. & Emery, R. S. (1992) Vet.Clin. North Am.: Food Anim. Pract., 8(1), 91.<br />
(8)McNamara, J. P. et al. (1986) J. Lipid Res.,27, 150.<br />
(9)Duffield, T. F. et al. (1997) Can. Vet.38, 713.<br />
(10)Nielen, M. et al. (1994) Can. Vet. J., 35,229.<br />
(11)Dohoo, I. R. &: Martin, S. W. (1984) Can.Comp. Med., 48, 1.<br />
(12)Mills, S. E. et al. (1986) J. Dairy Sci., 69,362.<br />
(13)Drackley.J. K. et al. (1992) J. Dairy Sri.,75, 1622.<br />
(14)Uribe, H. A. et al. (1995) J. Dairy Sci., 78,42I.<br />
(15)Rue, D. A. et al. (1983) Vet. Rec., 113. 495.<br />
(16)Andersson, L. & Lyndstrom, K. (1985)Zentralbl. Veterinarmed., 32, 15.<br />
(17)Tveil, B et al. (1992) J. Dairy Sci., 75,2421. 2433.<br />
(18)Sanders, D. E. (1989) Comp. Com. Educ.Pract. Vet., 11,757.<br />
(19)Russel, A. (1985) In Pract., 7(1), 23.<br />
(20)Bigras-Poulin, M. et al. (199?) Prev. Vet.Med., 10, 79.<br />
(21)Dohoo, I. R. et al. (1983) Prev. Vet. Med.,1,321.<br />
(22)Grohn, Y. T. et al. (1986) Acta Vet. Scand.,27, 182. 209.<br />
(23)Lean. I. J et al. (1991) Vet. Bull., 61, 1209.<br />
(24)Dohoo, I. R. et al. (1984) Prev. Vet. Med.,2.665. 671.<br />
(25)Eriksson, J. A. & Wretler, E. (1990) WorldRev. Anim. Prod., 25, 29.<br />
(26)Grohn, Y. T. et al. (1989) J. Dairy Sci., 72,1876.<br />
(27)Markusfcld. O. et al. (1997) Vet. Rec, 141,67.<br />
(28)Smith. T. R. et al. (1997)J Dairy Sci.. 80,1569.<br />
(29)Lean, I. j. et al. (1994) Rrs. Vet. Sci., 57,200.<br />
(30)Morris, C. A. et al. (1992) Prof. NZ. Sac.Anim. Prod.. 52, 21.<br />
(31)Tyler, J. W. et al. (1994) J. Am. Vet. Med.Assoc, 204, 1665.<br />
(32)Vagirholm, 1. et al. (1991) Prev. Vet. Med.,10. 195.<br />
(33) Miettmen, P. V. A. & Setala.J.J. (1993) Prev. Vet. Med., 17,1.<br />
(34)Hannan. J. L et al. (1996) Am.J. Vet.Res., 57, 640.<br />
31
(35)Anderson. L & Emanuelson, L. I. (1985)Prev. Vet. Med., 3. 449.<br />
(36)Miettmen, P. V. A. (1994)J Vet. Med.Assoc, 41, 102.<br />
(37)Dohoo, I R. et al. (1985) Can.J Comp.Med., 49, 239.<br />
(38)Wastney, M. E. et al. (1983) Aust.J. Biol.Sci., 36,271.<br />
(39)VcenhuizcnJ.J. et.il. (1991)J. Dairy Sci.,74, 4238.<br />
(40)Hoeben, D. et al. (1997) Vet. Immunol.Immunopath., 58, 165.<br />
(41)Jeffrey, M. tk Higgms, R. J. (1992) Vet.Rec, 301.<br />
(42)Scott, P. R. et a!. (1995) Br. Vet.J., 151,39, 459.<br />
(43)Sargison, N. D. et al. (1994) Br. Vel.J.,150, 271.<br />
(44)Sigurdsson, H. (1988) Ana. Vet. Scand., 29,407.<br />
(45)Markusfeld, O. (1985) Vet. Ree., 116, 489.<br />
(46)Gustafison, A. H. et al. (1995) Prev. Vet.Med., 237.<br />
(47)Dirksen, G. & Brenner, W. (1993) J. Vet.Med. Assoc, 40, 779.<br />
(48)Grohn, Y. et al. (1983)J Dairy Sci., 66,2320.<br />
(49)West, H J. (1996) Br. J. Nutr., 75, 593.<br />
(50)Ford, E.J. R. (1990) Br. Vet.J., 146, 539.<br />
(51)Sielman, E. S. et al. (1997) J. Am. Vet.Med. Assoc, 210, 240.<br />
(52)Shpigel, N. Y. (1996)J. Am. Vet. Med.ASSM., 208, 1702.<br />
(53)Hutjens, M. F. (1992) Vet. Clin. North Am.: Food Anim. Pract., 8(1), 525.<br />
(54)MartenuikJ.V.(1988) Vet.din.North Am.:Food Anim.Pract.,4(2),30.<br />
(53)Burwell.J. F:et al.(1986) Vet. Rec,118,208.<br />
(56)Scott,P.R.et al. (1998) Vet.J.,155,197.<br />
(57)Ferguson,J.D.et al.(1987) Comp.Com.Uduc.Pract.Vet., 9(5),F192.<br />
(58)Bair.l,G.D.et al.(1974) Br.Vet.J.,130,214.318.<br />
(59)Sniffen,C.J.& Herdt,I.H.(1992) Vet.Clin. North Am.: hood. Anim. Pract., 8(1),1.<br />
(60)Sauer,P.D.et al.(1989) J.Dairy Sci.,72,436.<br />
三、肥胖母牛综合征(Fatty Cow Syndrome)<br />
肥胖母牛综合征,又称牛的妊娠毒血症(pregnancy toxemia in cattle)或牛的脂肪肝病<br />
(fatty liver disease of cattle)。是因母牛怀孕期间过度肥胖,常于分娩前(肉用母牛)或分娩<br />
后(乳用母牛)发生以厌食、抑郁、虚弱为特征的疾病,死亡率很高与绵羊的妊娠毒血症类<br />
似。因主要发生于肥胖母牛,故称为肥胖母牛综合征。<br />
【病因】 饲养因素:在泌乳后期或干乳期,能量物质摄入过多,如饲料中谷物或青贮<br />
玉米太多,致使妊娠后期肥胖,加上分娩、泌乳等应激作用可诱发本病。用有毒羽扇豆类饲<br />
草饲喂,可加速本病发生。<br />
管理因素:妊娠后期母牛应与正在泌乳的牛群分开饲养,并喂给不同的日粮,否则可促<br />
使本病发生。妊娠后期对偏胖母牛饲料中能量物质逐渐减少,以便发挥其自身调节功能,并<br />
能耐过产犊应激,常可减少或避免疾病发生。<br />
怀双犊母牛,同时伴有缺钙,或受多量内寄生虫感染,可使发病增多。<br />
乳牛常在分娩后,泌乳高峰期发病,有些牛群发病率达 25%,死亡率达 80%,肉牛发<br />
病率较低,但死亡率很高。<br />
【病理】 分娩、泌乳等应激作用,使机体对能量需求剧增,如摄入不能满足这一需求,<br />
则可造成体脂动员,脂肪分解使游离脂肪酸大量增多,并引起肝细胞脂肪变性和脂肪沉着,<br />
妨碍肝脏其它功能(如合成糖元、合成蛋白质)的发挥,致使体脂分解更剧,呈恶性循环状<br />
32
态。<br />
有毒羽扇豆、四氯化碳、四环素等可损伤肝细胞,蛋氨酸、丝氨酸缺乏可影响脂蛋白合<br />
成,胆碱缺乏可影响脂肪从肝脏向脂肪组织运送,所有这些因素,都可诱发脂肪肝生成,而<br />
妊娠期间太胖、分娩前后体脂消耗过多,肝细胞变性是构成脂肪肝综合征的主要因素。<br />
【临床表现】 患畜异常肥胖,背脊展平,产后几天内呈现食欲下降,并逐渐停食。动<br />
物虚弱、躺卧、体内酮体增多、酮尿。按酮病治疗几乎无效。牛群中常有真胃扭转,前胃弛<br />
缓,胎衣不下,难产现象。部分牛还可出现神经症状,如举头,头颈部肌肉震颤,最后昏迷,<br />
心动过速。幸免一死的动物常有休情期延长,牛群中不孕症比例增高。肥胖肉母牛于产犊前<br />
表现不安,易激动,运步不协调、粘着步,粪少而干,心动过速,脂肪肝现象于产犊前 2<br />
个月发生时,患牛常有较长时期(10~14d)停食,精神抑郁,躺卧,粪稀少且臭,死亡率高,<br />
病程为 10~14d,最后昏迷并在安静中死亡。<br />
患病动物常有低钙血症(60~80mg/L),血清无机磷浓度升高达 6.46mmol/L(200mg<br />
/L)。开始时呈低糖血症,但后期呈高糖血症。血液中酮体、谷草转氨酶(GOT),鸟氨酰<br />
基转移酶(OCT)和山梨醇脱氢酶(SDH)活性升高,明显的酮尿和蛋白尿,白细胞总数升<br />
高。<br />
剖检可见肝脏轻度肿大,黄白色,脆而油嫩,肾小管上皮脂肪沉着,肾上腺扩大,色黄。<br />
真胃内常有寄生虫侵袭性炎症和霉菌性瘤胃炎及霉菌性灶性肺炎。<br />
【诊断】 奶牛常发生于产后,肉牛多发生于产前,患牛发病前膘情很好,多肥胖。常<br />
于产前或产后不久突然停食和躺卧者应怀疑为此病。诊断中应与真胃变位、酮病、胎衣滞留<br />
和生产瘫痪相区别,真胃左方变位在肋弓下呈明显的金属音调与本病相区别。生产瘫痪常在<br />
分娩后立即发生。对钙制剂、ACTH 及乳房送风等治疗效果较明显。本病与母牛卧倒不起综<br />
合征(downer cow syndrome)易混淆。它们都呈完全废食,明显酮尿等。但从病史看,肥<br />
胖母牛综合征是因妊娠后期饲喂大量谷物而过胖,卧倒不起综合征大多无过度肥胖现象。肥<br />
胖症与分娩综合征(parturition syndrome)十分类似,其实肥胖综合征也是围产期疾病之一。<br />
分娩综合征除包括肥胖症外,还有胎衣滞留、子宫内膜炎、卵巢功能不全、低钙血症、低镁<br />
血症、酮体增多性低血糖症,瘤胃运动减弱,乳房炎等症状,尤其是高产乳牛乳产量下降,<br />
尽管疾病呈慢性经过,用普通治疗方法效果甚差。<br />
肥胖母牛综合征于产前发生时应与真胃积食,迷走神经性消化不良和慢性腹膜炎等进行<br />
区别诊断。<br />
【防治】 该病死亡率高,经济损失大,较好的预防措施是,防止妊娠期间,特别是怀<br />
孕后 l/3 时期内摄入过多的能量型饲料,只要能满足胎儿生长和自身需要即可以了。但要<br />
做到这一点,又不引起过胖是很难的。建议对妊娠后期牛应分群饲养,并密切观察牛的体重<br />
变化。根据膘情给肥胖牛仅供给优质干草,少喂精料,补充钴化盐,增加运动,可防止牛过<br />
度肥胖。经常监测血液中葡萄糖及酮体浓度,有重要参考意义。当血中酮体浓度增加,葡萄<br />
糖浓度下降,除要作为酮病治疗外,应设法维持动物保持食欲,防止体脂过多动员。<br />
产后某些疾病如真胃变位,子宫内膜炎、酮病等应及时适当治疗。血糖不足,可用丙二<br />
醇促进生糖作用,对减少体脂溶解有一定意义。<br />
该病治疗前景不能令人满意,预后应慎重。如完全丧失食欲者,常归于死亡。尚能维<br />
持一定食欲者,应采取综合治疗措施。反复静脉注射葡萄糖、钙制剂,用ATCH糖皮质激素、<br />
VB12并配合钴盐,注射丙酸睾丸酮,促进同化作用,虽有一定改善作用,效果并非很满意。<br />
灌服健康牛瘤胃液 5~l0L,或喂给健康牛反刍食团,喂给丙二酸促进生糖作用,给予胰岛素<br />
鱼精蛋白锌 200~300IU皮下注射,一天两次,可促进糖向外周组织转移。多给优质干草和多<br />
饮水的同时,给予含钴盐砖,或用氯化胆碱,每 4h一次,每次 24g,口服或皮下注射,或用<br />
硒-VE制剂等,均有一定治疗作用,但效果均不能令人满意。<br />
33
四、犬、猫脂肪肝综合征(Dog and Cat Fatty Liver Syndrome)<br />
猫、狗脂肪肝综合征是多种疾病的共同病理现象,临床上以皮下脂肪蓄积过多,容易疲<br />
劳,消化不良为特点。<br />
猫、狗脂肪肝综合征,可因身体过度肥胖、糖尿病,或因长期摄入高脂肪、高能量、低<br />
蛋白饲料,突然减食,严重饥饿而引起。亦可因体内激素分泌障碍,或因糖尿病治疗不恰当<br />
所引起。也可因用药错误,如四环素、糖皮质激素或因某些毒素如内毒素的影响而发生该病。<br />
饥饿情况下,外周脂肪组织内脂肪水解为甘油和脂肪酸,游离脂肪酸在肝内或者被氧化、<br />
供能,或者与磷脂一起形成新的甘油三脂,当肝内脂肪生成速度大于运出速度,脂肪沉着在<br />
肝内。有些营养成分如胆碱、磷脂及其前体蛋氨酸、三甲基甘氨醛(betaine)、酪蛋白等缺<br />
乏可直接影响已合成的脂肪运出肝脏并形成脂肪肝。<br />
糖尿病前期的猫、狗大多较胖,因激素分泌障碍,可促使糖、脂肪、蛋白质的沉积。胰<br />
岛素分泌不足,可促使外周脂肪组织分解。而生长素、儿茶酚胺释放亦可促使外周脂肪分解,<br />
并进而加速脂肪在肝内积累。许多糖尿病狗血浆中甘油三酯和游离脂肪酸浓度升高,增加了<br />
脂肪肝生成的危险性。<br />
有些药物可以损伤肝细胞,干扰肝细胞对脂蛋白合成,如反复使用四环素、糖皮质激素、<br />
某些内毒素等,可导致脂肪肝生成,但停药后可以自动恢复。类固醇激素可增加外周脂肪分<br />
解,抑制肝内甘油三脂再脂化,两者共同的结果是肝内积脂过多,产生脂肪肝综合征。<br />
患病猫、狗外观营养佳良,体躯丰满,皮下脂肪丰富,因肥胖而导致易疲劳,消化不良<br />
易患糖尿病、血糖浓度升高,容易感染,并产生高糖血症,过度肥胖的动物心脏周围裸以脂<br />
肪,产生心搏障碍,呼吸困难和多种器官病理。<br />
饲以高蛋白,低脂肪、低碳水化合物,可有效地防止本病发生,一旦形成脂肪肝综合征,<br />
治疗效果不够理想。<br />
五、禽脂肪肝综合征(Pultry Fatty Liver syndrome)<br />
禽肝脏、腹腔及皮下为大量脂肪蓄积,产蛋量下降,常伴有小血管出血的疾病称为脂肪<br />
肝综合征,或称为脂肪肝出血综合征(falty Iiver hemorrhagic syndrome),常散发于产蛋母鸡,<br />
尤其是笼养鸡群。公鸡极少发生,填鸭、填鹅因食入大量能量饲料而产生的“肥肝”(fatty liver)<br />
实际上也呈现脂肪肝综合征。<br />
【病因】 禽日粮中能量物质,如小米、大麦、麦粉含量过多,运动不足,体重日渐增<br />
多,采食量始终处于高水平,那怕在夏季也不减食。重型鸡、鸭更易发生。饲料中脂肪含量<br />
过多甚至酸败,高温季节,通风不良,密度过大,热应激作用,或因突然更换饲料以后,饲<br />
喂次数过多等应激因素可促使本病发生。<br />
【病理】 家禽肝脏是合成体内脂肪的最重要器官,几乎全部体脂都在肝细胞内合成,<br />
由极低密度脂蛋白运送到脂肪组织贮藏。家禽肝脏的代谢活力很强,特别在产蛋期间,每年<br />
由肝脏合成的脂肪总量几乎等于家禽的体重。在脂肪从肝脏转移到脂肪组织过程中,胆碱起<br />
重要作用,缺乏胆碱,或者因肝脏合成的脂肪过多,都将蓄积在肝内,因而使肝脏呈淡黄色,<br />
或淡粉红色,有时在黄色背景下还有散在的小点样出血,并散在一些绿色的点或斑,这是因<br />
波及小胆管引起胆管破裂、胆汁外流的标志。能量摄入越多,体脂越丰富。在脂肪运输过程<br />
中需要脂蛋白,而蛋氨酸、丝氨酸及胆碱是合成磷酰脂胆碱的原料,也是合成脂蛋白的原料,<br />
当饲料中胆碱、蛋氨酸不足,脂肪贮积在肝内无法外运,遂产生脂肪肝。在脂肪肝形成过程<br />
中,病禽血浆甘油三脂浓度升高。<br />
【临床表现】 有的鸡群发病率较高,尤其是重型鸡。有报告称其病死率可达 31.4%<br />
~37.8%。病鸡在生前肥胖超过正常体重的 25%,貌似健康。产蛋率波动很大,可从 60%~75<br />
%下降为 30%~40%,甚至只有 10%。在下腹部可以摸到厚实的脂肪组织,病鸡冠及肉髯色<br />
淡,甚至发绀,继而变黄、萎缩。精神萎顿,多伏卧,少运动,有些病鸡食欲下降,鸡冠苍<br />
34
白,粪呈黄绿、水样,体温正常。当拥挤、驱赶、捕捉或抓提方法错误,引起强烈挣扎时,<br />
可突然死亡。病群中月死亡率超过 2%~4%。肝内脂肪过多,质脆易碎,在挣扎、拥挤时,<br />
常可因肝脏血管破裂、腹腔内出血引起急性死亡。病死禽腹腔内常有大块血凝块,呈油灰状,<br />
很脆。在皮下、腹腔、肠系膜、心包外、心冠状沟周围堆积了大量脂肪,呈淡黄色,几乎呈<br />
液状,有的厚达 5~7cm。组织学观察,仍可见到肝细胞,但视野内到处都是被零乱的脂肪泡<br />
干扰的内部结构,有些区域显示小血管破裂和继发性炎症、坏死和增生,大量脂肪增生可导<br />
致小血管破坏,引起出血症。<br />
【防治】 应控制日粮中高能物质的比例,严格按照蛋鸡饲养标准进行,必须保证饲粮<br />
中粗纤维和胆碱的供给。每吨饲料中供给 1kg氯化胆碱,多种维生素复合剂,或者在用胆碱<br />
的同时给予VE1 万单位,VB122mg,三周内喂完。<br />
中药“水飞蓟”(Silybum Marianum(L)Gaertn)是药用植物,有效成分为水飞蓟素,<br />
据报道,可降低血液中 41.9%的胆固醇,51.5%的甘油三脂,按饲料 1.5%的量加入可治疗<br />
鸡、兔脂肪肝综合征,其治疗率和显效率分别达 80.0%和 13.3%,无效率仅 6.7%。<br />
饲料中增加蛋白质、肌醇和硒的供给,有利于减少疾病发生。<br />
六、鸡脂肪肝和肾综合征(Fatty Liver and Kidney Syndrome)<br />
肉用仔鸡发生一种以肝、肾肿胀、肝苍白、肾呈各种色变,表现嗜睡、麻痹和内脏出血、<br />
突然死亡为特征的疾病,称为脂肪肝和肾综合征,主要发生于 10~30 日龄肉用仔鸡。<br />
【病因】 历史上对本病发生原因曾有不少争议,有人认为是白血病,但用含低脂肪、<br />
低蛋白的粉碎的小麦为基础的日粮,能复制出该病,而且死亡率很高,从而认为它属营养代<br />
谢病。日粮中增加蛋白质和脂肪,可减少死亡。如同时补充生物素,按 0.05~0.1mg/kg 体<br />
重,死亡率大大减少。<br />
某些应激因素,特别是当饲料中可利用生物素的含量处于临界水平时,突然中断饲料供<br />
给,捕捉、噪音干扰,温度过高或过低,光照不足,禽群转移和网上饲养等因素,可促使发<br />
病。<br />
【病理】 本病是否就是生物素缺乏症,或是两个不同的病尚待探讨。生物素缺乏对本<br />
病发生具有重要意义,但日粮中增加蛋白质和脂肪可减少发病。这可能与蛋白质饲料如大豆<br />
粉、鱼粉中生物素可利用率较高(100%),而小麦中生物素可利用率仅为 10%~20%有关。<br />
10~13 日龄以前的鸡不发病,与母源性生物素在雏鸡体内有一定贮存有关。30 日龄后发病少,<br />
与此更换饲料,玉米、豆饼中生物素含量较高,其中可利用生物素含量较高有关。然而,脂<br />
肪肝和肾综合征为何只发生于肉用仔鸡,其它品种禽和其它动物生物素缺乏时未见有类似的<br />
症状。应激因素是怎样促使疾病发生的,其机理尚难以解释。<br />
生物素是体内许多羧化酶(固定CO2)的辅酶,一个羧化酶分子内含 4 个生物素分子,<br />
4 个锰原子。在丙酮酸转为草酰乙酸,乙酰辅酶A转变为丙二酸单酰辅酶A等过程中起重要<br />
作用。脂肪肝和肾综合征的鸡有血糖浓度下降,血浆丙酮酸和游离脂肪酸浓度升高,肝脏中<br />
糖元浓度下降,说明糖元异生作用降低,导致脂肪在肝、肾蓄积。组织学观察证明,脂肪积<br />
累在小叶间及肝、肾细胞浆内,可产生肝、肾细胞脂肪变性。因脂蛋白酯酶受抑制,阻碍了<br />
脂肪从肝脏向外运输。低血糖和应激作用,增加了体脂的动员,最终造成脂肪在肝内蓄积。<br />
除心肌、骨骼肌及神经系统脂肪外,全身广泛脂肪浸润。<br />
【临床表现】 本病一般见于生长良好的鸡,年龄在 10~30 日龄之间。发病突然,表<br />
现嗜睡、麻痹,由胸部向颈部蔓延,几小时内死亡。死后头伸向前方,胸朝下趴伏,或躺卧<br />
将头弯向背侧,发病率、死亡率一般在 5%,有时可达 30%。有些病例死亡前可表现出生物<br />
素缺乏症的病症。如羽毛生长不良,干燥变脆,喙周围皮炎,足趾干裂,鸡群中其它鸡生长<br />
不受病鸡影响。<br />
剖检可见肝苍白、肿胀,在肝小叶外周表面有小的出血,有时出现被膜破裂,病禽突然<br />
35
死亡。肾肿胀,色各异,脂肪呈淡粉红色,这与脂肪内小血管充血有关。嗉囊、腺胃及十二<br />
指肠内含有黑色或棕色出血性液体,很臭。组织学检查发现肝、肾细胞内脂肪含量特别多,<br />
是正常鸡的 2~5 倍,主要是甘油三脂,这一特征具有诊断意义。心肌纤维亦有脂肪颗粒,其<br />
它组织的变化不明显。<br />
表 2-1 脂肪肝和肾综合征与包涵体肝炎、法氏囊病间区别诊断表<br />
包涵体肝炎 传染性法氏囊 脂肪肝和肾综合征<br />
发病日龄 28~45 >10 10~30<br />
鸡群状态 死亡前多数正常 不完全健康 死亡前正常<br />
死亡率(%) 0~8 0~25 0~10<br />
肝、肾变化 出血、色正常 肾小管肿胀<br />
肾色白,肾小管肿胀不及<br />
前两种鸡病明显<br />
法氏囊 退缩 出血或有脓 正常<br />
组织学变化<br />
肝包涵体变性及细胞广<br />
泛破裂<br />
— 过多脂质沉积,但无变性<br />
病鸡血清丙酮酸、乳酸、游离脂肪酸含量增加,丙酮酸羧基酶和脂蛋白酶活性下降。病<br />
禽肝内糖元含量极低,生物素含量
动,即使陌生人或狗走近时,他仅扭转身体而不敢移动,有时站在水中长时间不走或就地歇<br />
息。呼出气体内有明显的酮臭味,粪便干燥,常有便秘、磨牙、后期可发展为肌肉震颤,头<br />
不自主摇动,唇扭曲,流涎,空嚼,甚至产生角弓反张,头颈侧弯和转圈运动,肌震颤可扩<br />
散至全身,躺卧不起可保持 3~4 天甚至 1 周,最后躺卧产生痉挛,四肢作不随意运动,昏迷,<br />
死亡。幸存者常伴有难产,羔羊极度虚弱或生后不久死亡。<br />
血液检查表现为血糖浓度下降,从正常时的 3.33~4.99mmol/L 降至 0.14mmol/L 血清<br />
酮体浓度可从正常时的 5.85mmol/L 升高达 547mmol/L,β-羟丁酸从正常时的 0.47±<br />
0.06mmol/L 升高达 8.50mmol/L,游离脂肪酸和皮质醇浓度升高。尿液中酮体呈强阳性。<br />
【诊断】 根据怀孕后期有明显的神经症状,失明,呼出气中有酮臭,6~7 天内死亡,<br />
血液中糖浓度下降,酮体浓度升高等均可作出诊断。<br />
诊断中应与李氏杆菌病、伪狂犬病相区别,前者表现奇痒,而且发热,伪狂犬病呈现躁<br />
狂,瘫痪常是致死性的。脑脓肿,中耳炎发病是个别的。羊快疫(Louping-ill)仅在有传媒<br />
昆虫存在时才发生,并伴有发热。<br />
【治疗】 本病治疗原则是补糖、保肝、解毒。<br />
静脉注射及口服葡萄糖,20%葡萄糖 500ml,缓慢静注,并配合胰岛素,肌肉注射,同<br />
时口服 50g 糖加水 200ml,每日两次,连续 3d。有人主张口服丙酸钠 110g/天或丙二醇 20ml<br />
/天或甘油 20~30ml/天,其效果优于口服葡萄糖。为了纠正酸中毒,静脉注射重碳酸钠或<br />
乳酸钠。<br />
肌肉注射氢化泼尼松 75mg 和地塞咪松 25mg 或 ACTH20~60IU,静脉注射葡萄糖并注<br />
射钙、磷、镁制剂,其存活率可达 85%。<br />
如上述方法无效,可尽快施行剖腹产,或人工引产,当胎儿产出后症状迅速消失。<br />
【预防】<br />
1。加强营养,在怀孕最后两个月内,应喂给精料,从产前两个月起每日 125g,其中粗<br />
蛋白质含量为 10%,以后逐渐增加到每日 1kg。<br />
动。<br />
2。避免突然更换饲料,增加运动,遇到寒冷、恶劣气候时更应增加饲料供给,增加运<br />
FATTY LIVER IN CATTLE (FAT COW SYNDROME, PREGNANCY TOXEMIA IN<br />
CATTLE)<br />
Synopsis<br />
Etiology. Mobilization of excessive body fat to liver during periods of negative energy balance at<br />
time of parturition or in early lactation of dairy cows and late pregnancy of beef cows.<br />
Epidemiology. High-producing dairy cows overfed during dry period may develop fatty liver<br />
syndrome just before or after calving precipitated by any factor or disease which interferes with<br />
feed intake. Occurs in well-conditioned beef cattle in late pregnancy when energy intake suddenly<br />
decreased. Moderate and subclinical degrees of fatty infiltration may adversely affect reproductive<br />
performance of dairy cows.<br />
Signs. Inappetence to anorexia, ruminal atony, lethargic, inactive, ketonuria, fat body condition,<br />
weakness and recumbency if worsens. Recover if continue to eat and appetite improves.<br />
Clinical pathology. Increase in serum hepatic enzyme levels, increase in ketone bodies; increased<br />
fat in liver biopsy.<br />
Lesions. Fatty infiltration of liver.<br />
Diagnostic confirmation. Liver biopsy.<br />
Differential diagnosis list:<br />
•Left-sided displacement of abomasum<br />
37
(p. 321)<br />
•Right-sided displacement of abomasum (p. 326)<br />
•Milk fever (p. 1420)<br />
•Parturition syndrome<br />
•Abomasal impaction (p. 314)<br />
•Vagus indigestion (p. 311)<br />
•Peritonitis (p. 250).<br />
Treatment. Fluid and electrolyte therapy including glucose IV. Propylene glycol orally. Provision<br />
of palatable feed.<br />
Control. Avoid overfeeding during late lactation and dry period. Avoid situations which reduce<br />
feed intake at time of parturition.<br />
ETIOLOGY<br />
Fatty liver is caused by the mobilization of excessive quantities of fat from body depots to the<br />
liver. It occurs either because of a deprivation of feed in fat beef cattle, more severe in those<br />
bearing twins, or because of a sudden demand of energy in the immediate postpartum period in<br />
well-conditioned lactating dairy cows. The disease is an exaggeration of what is a common<br />
occurrence in high-producing dairy cows which are in a state of negative energy balance in early<br />
lactation (1). Body fat, especially SC fat, is mobilized and deposited primarily in liver but also<br />
muscle and kidney. Whether or not the cow is truly fat at parturition may not be important in<br />
determining the degree of fat mobilization, but the degree of negative energy balance in early<br />
lactation is critical.<br />
EPIDEMIOLOGY<br />
Fatty infiltration of the liver is common in high-producing dairy cattle from a few weeks before<br />
and after parturition and is associated with several periparturient diseases, and an increase in the<br />
calving-to-conception interval. A severe form of fatty infiltration of the liver immediately before<br />
or after parturition is known as the fatty liver or fat cow syndrome or pregnancy toxemia of<br />
cattle which can be highly fatal. In beef cattle, the disease occurs most commonly in late<br />
pregnancy when the nutrient intake is decreased in cattle which were previously well fed and in<br />
good body condition.<br />
Fatty infiltration of the liver is part of a generalized fat mobilization syndrome which occurs in<br />
early lactation, particularly in high-yielding dairy cows, as milk production outstrips appetite and<br />
body reserves are used to meet the energy deficit (2). The deficit occurs because dietary intake<br />
cannot meet the energy requirements for the high yield. Peak yields of milk are reached 4-7 weeks<br />
after calving, but the highest levels of volun¬tary feed intake are not reached until 8-10 weeks<br />
after calving. As a result of the energy deficit, the cow mobilizes body reserves for milk<br />
production and may lose a large amount of body weight.<br />
In about 30% of high-producing cows the infiltration is severe and is associated with reversible<br />
but significant effects on liver structure and function. In some populations of cows, the incidence<br />
of fatty liver is much lower and insignificant (3).<br />
In North America, the introduction of the system of challenge feeding of dairy cows was<br />
associated with an increased incidence of the disease. The overall effect of the system is to provide<br />
excess energy in the diet during late pregnancy or during the dry period generally. The diets fed<br />
may contain a high percentage of the cereal grains, corn ensilage, or brewer's grams. In this<br />
system, high-energy rations are fed beginning a few weeks before parturition. The total daily<br />
38
amount of feed is increased by regular increments to reach a high level at parturition and peak<br />
levels to coincide with the peak in the lactation curve several weeks after parturition. This resulted<br />
in some excessively fat cows at the time of parturition, when energy demands are high. The<br />
disease has also occurred in dairy cows which were fed excessive amounts of high-energy rations<br />
throughout the dry period. In dairy herds, the fatty liver syndrome has also been associated with an<br />
increase in the incidence of milk fever, ketosis and left-sided displacement of the abomasum, all of<br />
which are much more difficult to treat successfully because of the fatty liver.<br />
The body condition score at calving can have a direct effect on the health, milk yield and<br />
fertility of cows (4). It represents the cumulative effects of the dry period, the body condition<br />
score at drying off and the loss of body condition during the dry period. The risk of retained<br />
placenta may be greater for cows underconditioned at drying, whereas cows that lost more body<br />
condition during the dry period may be more affected by both retained placenta and metritis; the<br />
two effects are independent of each other. The risk of ketosis is increased in cows overconditioned<br />
at calving, which may be due to a long dry period. Cows calving in a higher body condition score<br />
produced more milk, fat and protein in the first 90 d of lactation and the effect was most<br />
pronounced on milk fat content (4). Cows with a higher body condition score at calving were less<br />
prone to anestrus but did not conceive more successfully to first service. A reduction of six open<br />
days in primiparous cows was estimated for each additional unit of body condition score at<br />
calving. Multiparous cows which lost more body condition during the dry period are more prone<br />
to inactive ovaries and are more likely to be open 150 d after calving in the next lactation.<br />
In a field study the percentage of cattle dying or being culled because of disease was affected by<br />
the amount of hepatic triglyceride -15%, 31% and 42% for cattle with mild, moderate and severe<br />
hepatic lipidosis, respectively (1).<br />
Cattle have been classified into three groups on the basis of liver fat content determined<br />
histologically 1 week after parturition (5). Less than 20% lipid corresponds to less than 50 mg/g<br />
liver by weight, 20-40% lipid, 50-100 mg/g liver, and greater than 40% represents more than 100<br />
mg/g liver (5). These concentrations correspond to mild, moderate and severe cases of fatty<br />
infiltration. Cows with less than 20% lipid in the liver at 1 week after calving are considered<br />
normal, and those with more than 20%, are considered to have a fatty liver. About 30% of<br />
high-yielding dairy cows m the United Kingdom are considered to have a fatty liver 1 week after<br />
calving. Clinical evidence of hepatic disease may not occur consistently until liver lipid<br />
concentrations are in the range of 35-45% or more.<br />
Outbreaks of the disease have occurred in dairy herds in which up to 25% of all cows were<br />
affected with a case-fatality rate of 90%. Dairy cows with abnormally long, dry periods also have<br />
a tendency to become obese and develop the fatty liver syndrome of parturition. The feeding of<br />
dairy cows in large groups as in loose housing systems has been associated with an increase in the<br />
incidence of the disease.<br />
In dairy cattle, there is a relationship between the occurrence of a subclinical fatty liver within<br />
the first few weeks after parturition and inferior reproductive performance due to a delay in the<br />
onset of normal estrus cycles and a reduction in the conception rate which results in an increase in<br />
the average days between calving and conception (6). There may be differences in reproductive<br />
performance between cows with mild and moderate fatty livers early after calving (7). However,<br />
an examination of the postpartum hormone profiles of cows with fatty liver did not reveal the<br />
pathogenetic mechanism of the reduced fertility (8). The fat cow syndrome may also be associated<br />
39
with an increased incidence of parturient paresis and unresponsive treatment for ketosis in early<br />
lactation.<br />
The disease can occur in non-lactating dairy cows by the imposition of a partial starvation diet<br />
in late pregnancy m an attempt to reduce the body weight of cows which are considered to be too<br />
fat (9). Changing the diet of pregnant beef cows from silage to straw in an attempt to reduce their<br />
body weight and the incidence of dystocia has resulted in outbreaks of the disease.<br />
In beef cattle in North America, the severe form of the disease, pregnancy toxemia, is seen most<br />
commonly in the last 6 weeks of pregnancy in cows which are fat and pregnant with twins. The<br />
affected cows are usually well fed until late pregnancy when an unexpected shortage of feed<br />
occurs, or the cows are too fat and cannot consume sufficient low-energy feed to meet the<br />
demands of pregnancy. Under usual circumstances the disease in beef cattle occurs sporadically:<br />
the morbidity is about 1% but the mortality is usually 100%.<br />
Pregnancy toxemia of cattle has occurred in pregnant beef cattle in Australia (10) and the<br />
United Kingdom. First-calf heifers were more commonly affected than older cows and most were<br />
in late pregnancy (7-9 months) or had just recently calved. Cows pregnant with twins are<br />
particularly susceptible.<br />
Cows exposed to toxic lupins may also develop the disease. In Australia, only beef cattle have<br />
been involved in pregnancy toxemia; the fat and the obese arc most commonly affected. The<br />
disease occurred most notably when there was a shift to autumn calving (February to April) when<br />
feed supplies were low because of low, late summer rainfall. The cows were in good to fat body<br />
condition because of lush pastures in the spring and early summer, but by autumn when the<br />
calving season approached, the feed supplies were low and the nutritive value of the pasture<br />
inadequate. The lack of feed combined with the expensive nature of supplementary feeding<br />
resulted in an inadequate level of nutrition during late pregnancy. Similarly the control of internal<br />
parasitism, especially ostertagiasis, is not intensively practiced. The morbidity is usually from<br />
1-3% but may be as high as 10% and the disease is usually fatal.<br />
PATHOGENESIS<br />
Under normal physiological conditions, the total amount of fat increases in the liver beginning a<br />
few weeks before calving, rises to an average of about 20% (of wet weight basis) 1 week after<br />
calving and declines slowly to the normal level of less than 5% by 26 weeks after calving.<br />
However, the levels vary from almost none to 70% among cows 1 week after calving. Fat<br />
mobilization begins about 2-3 weeks before calving and is probably induced by a changing<br />
hormonal environment prior to calving rather than an energy deficit. After calving there is a larger<br />
increase in fat accumulation. The changes in the liver in dairy cows are functional and reversible<br />
and related to the metabolic demands of late pregnancy and early lactation (11). The gradual<br />
increase in plasma non-ester-ified fatty1 acids (NE.FAs) during the final prepartum days may<br />
explain the gradual depression in dry matter intake and a contributing factor to triglyceride<br />
accumulation in the liver (12). During this period there is also an elevated level of plasma glucose<br />
and a lowered plasma betahydroxybutyrate (BHBA) concentration. The serum levels of lecithin:<br />
cholesterol acyltransferase activity in spontaneous cases of fatty liver in cows are also decreased,<br />
which may be associated with reproductive performance because cholesteryl esters are utilized for<br />
the synthesis of steroid hormones (13).<br />
The heavy demands for energy in the high-producing dairy cow immediately after parturition,<br />
or in the pregnant beef cow which may be bearing twins, result in an increased rate of<br />
40
mobilization of fat from body reserves, usually SC tat, to the blood which transports it to body<br />
tissues, particularly liver but also muscle and kidney. Any decrease in energy intake caused by a<br />
shortage of feed or an inability of the cow to consume an adequate amount of feed during the<br />
critical periods of late pregnancy or early lactation would result in the mobilization of an<br />
excessive amount of free fatty acids. This results in increased hepatic lipogenesis with<br />
accumulation of lipid in enlarged hepatocytes, depletion of liver glycogen and inadequate<br />
transport of lipoprotein from the liver (11). Most of the lipid infiltration of the liver in dairy cows<br />
after calving is in the form of triacylglycerols because of the increased uptake of NEFAs and a<br />
simultaneous increase in diacylglycerol acyltransferase; the activity of this enzyme is activated by<br />
fatty acids (6).<br />
Ruminants may be prone to fatty liver because their hepatic tissue has limited capacity to export<br />
very low density lipoprotein (8). Also, a prepartum surge of estrogen may contribute to the<br />
development of tatty liver in ruminants by increased tatty acid esterification along with limited<br />
export of triglyceride (14). The serum concentrations of triacylgly-cerol-rich lipoproteins are<br />
reduced m cattle with naturally occurring hepatic lipidosis.<br />
During fat mobilization, there is a concurrent loss of body condition and SC adipose tissue. The<br />
degree of mobilization will be dependent on the fatness of the cow and extent of the energy deficit.<br />
Fat and thin cows respond differently to the metabolic demands of early lactation (11). Fat cows<br />
appear less able to utilize mobilized tatty acids and as a result accumulate esterified tat in tissues.<br />
This can adversely influence susceptibility to disease and the response of the cow to that disease<br />
imposes further metabolic demands, particularly on muscle and protein metabolism.<br />
Both SC fat and skeletal muscle mass .are decreased after calving and fat cows lose 2.5 times<br />
more muscle fiber area than thin cows. Thus the loss of body condition is due to total tissue<br />
mobilization (protein and fat) rather than fat alone. There appears to be a higher rate of protein<br />
mobilization m tat cows than in thin cows.<br />
The severity of fatty liver has been arbitrarily classified into severe, moderate and mild, based<br />
on the amount of triglyceride present in the hepatocytes (5). Fatty infiltration of muscle also<br />
occurs and appears to be correlated with the degree of hepatic lipidosis (15); this condition may<br />
also be related to the weakness and recumbency seen in severe cases of cows with fatty liver<br />
syndrome. In severe hepatic lipidosis, the accumulation of triglyceride in the cytoplasm is<br />
accompanied by disturbances in hepatic structure and function which may result in hypoglycemia<br />
and ketonemia; these signs are manifested as anorexia and depression and there may be clinical<br />
evidence of nervous signs. Some severe cases appear to develop hepatic failure, do not respond to<br />
therapy, and become weak and recumbent and die. Terminally there is a marked hyperglycmia. A<br />
leukopenia has been observed in dairy cows with more than 20% liver fat in the 2nd week after<br />
calving (16). This may be related to the increased incidence of postparturient diseases such as<br />
mastitis and endometritis observed in cows with subclinical fatty liver. However, this is not<br />
necessarily a cause-and-effect relationship. The case-fatality rate in severe cases may reach 50%<br />
or more.<br />
Cows which are not fat initially do not develop fatty liver syndrome. Pregnant beef cows in thin<br />
body condition on pasture can become extremely emaciated and eventually recumbent and die of<br />
starvation, but they do not develop pregnancy toxemia.<br />
The pathogenesis of the relationship between reduced reproductive performance and mild or<br />
moderately severe fatty liver in dairy cows within the first 2 weeks after calving is unclear.<br />
41
CLINICAL FINDINGS<br />
In dairy cattle, fat cow syndrome occurs usually within the first few days following parturition and<br />
is commonly precipitated by any condition which interferes with the animal's appetite temporarily,<br />
such as:<br />
•Parturient hypocalcemia<br />
•Left-sided displacement of the abomasum<br />
•Indigestion<br />
•Retained fetal membranes<br />
•Dystocia.<br />
Affected cows are usually excessively fat with body condition scores of 5/5 or higher.<br />
Excessive quantities of SC fat arc-palpable over the flanks, the shoulder areas and around the tail<br />
head. The affected cow usually does not respond to treatment for some of these diseases and<br />
becomes anorexic. The temperature, heart rate and respirations are within normal ranges. Rumen<br />
contractions are weak or absent and the feces are usually scant. Periods of prolonged recumbency<br />
are common and affected cows may have difficulty in standing when they arc coaxed to stand. A<br />
severe ketosis which does not respond to the usual treatment may occur. There is marked<br />
ketonuria. Affected cows will not eat and gradually become weaker, totally recumbent and die in<br />
7-10 d. Some cattle exhibit nervous signs consisting of a staring gaze, holding the head high, and<br />
muscular tremors of the head and neck. Terminally there is coma and tachycardia.<br />
In cattle with moderately severe fatty liver, the clinical findings are much less severe and most<br />
will recover within several days if they continue to eat even small amounts of hay.<br />
In fat beef cattle shortly before calving, affected cows are aggressive, restless, excited and<br />
uncoordinated with a stumbling gait, and sometimes have difficulty m rising and they fall easily.<br />
The feces are scant and firm and there is tachycardia. When the disease occurs 2 months before<br />
calving, the cows are depressed for 1- 14 d and do not eat. Eventually they become sternally<br />
recumbent. The respirations are rapid, there may be an expiratory grunt, and the nasal discharge is<br />
clear but there may be flaking of the epithelium of the muzzle. The feces are usually scant but<br />
terminally, there is often a fetid yellow diarrhea. The disease is highly fatal; the course is 10-14 d<br />
and terminally there may be coma with cows dying quietly.<br />
Clinical pathology<br />
The changes will depend on the severity of the fatty liver, severe cases with hypoglycemia,<br />
ketonemia and ketonuria similar to a severe case of ketosis.<br />
Serum biochemistry<br />
The concentration of serum NEFAs is increased, there is an increase in DHBA, serum bilirubin<br />
and increases in the serum levels of liver enzymes which are released following liver cell injury<br />
(17). In addition there are decreases in cholesterol, albumin, magnesium and insulin.<br />
The biochemical changes associated with fatty liver syndrome in cows have been described<br />
based on blood and liver samples taken from cows at the abattoir immediately after slaughter (18).<br />
Serum liver enzymes<br />
Significant increases occur in the serum activities of isocitric dehydrogenase (ICDH),<br />
glucose-6-phosphate dehydrogenase (G6PDH), glutamic dehydrogenase (GLDH), lactic<br />
dehydrogenase (LDH), malic dehydrogenase (MDH), aspartate aminotransferase (AST), alkaline<br />
phosphatase (ALP) and acid phosphatase (ACP). Increased serum levels of AST are weakly<br />
associated with increased total liver lipid. AST is not exclusively a liver enzyme but is also present<br />
42
in muscle, kidney and small intestine and any increase may reflect injury to other tissues. The<br />
bromsulphalein (BSP) clearance test, γ-glutamyl transpeptidase (GGT) and sorbitol<br />
dehydrogenase (SDH) have also been used as liver function tests in cattle with hepatic lipidosis<br />
associated with displaced abomasa but are not considered diagnostic.<br />
Blood ketones<br />
In fatty infiltration of the liver in severely ketotic cows there is a positive correlation between<br />
blood ketone body concentrations and the degree of fatty liver (1). However, diurnal variations in<br />
the concentrations of plasma BHBA make their diagnostic interpretations difficult and unreliable<br />
as a diagnostic aid for fatty liver.<br />
Liver biopsy and analysis<br />
A liver biopsy can be used to determine the severity of the fatty liver and the concentration of<br />
triglyceride and is the most reliable method of accurately estimating the degree of fatty infiltration<br />
of the liver.<br />
The triglyceride concentration of liver in normal cows ranges from 10-15% on a wet weight<br />
(WW) basis (19). Estimation of the lipid content of bovine liver samples obtained by biopsy may<br />
be made by biochemical or histological methods (19). Both methods provide reasonable estimates<br />
of liver fat content over a wide range of values. The lipid content of bovine liver is highly<br />
correlated with its specific gravity and the submersion of needle biopsy specimens into water, and<br />
copper sulfate solutions with specific gravities of 1.025 and 1.055 can be used as a test to estimate<br />
lipid content (20). For routine clinical diagnosis, three solutions of specific gravities of 1, 1.025<br />
and 1.055 can be used. Liver samples which float in all three solutions contain greater than 34%<br />
lipid, those that sink in water but float in 1.025 and 1.055 specific gravity solutions contain less<br />
than 34% but greater than 25% lipid, whereas those that float only in 1.055 specific gravity<br />
solutions contain less than 25% but greater than 13% lipid. Samples which sink in all three<br />
solutions contain less than 13% lipid. Some limited evidence indicates that cows with liver lipid<br />
concentrations above 34% are severely affected and can be expected to have clinical<br />
manifestations of hepatic insufficiency. Those with liver lipid levels between 34% and 25% are<br />
moderately affected and might have-some clinical evidence of hepatic insufficiency. Those<br />
between 25% and 13% are mildly affected, which is the range of most postpartum dairy cows<br />
without any evidence of disease. Liver lipid concen¬trations below 13% are inconsequential (20).<br />
Ultrasonography of liver<br />
Digital analysis of hepatic ultrasonograms have been used to evaluate fatty infiltration in dairy<br />
cattle (21) and has the highest sensitivity, specificity, accuracy, and positive and negative<br />
predictive values, followed by ultrasonography compared to bipod and serum analysis (22).<br />
Hemogram<br />
In cattle with subclinical fatty liver there may be a leukopenia, neutropenia and lymphopenia (16).<br />
NECROPSY FINDINGS<br />
In severe fatal cases the liver is grossly enlarged, pale yellow, friable and greasy. Mild and<br />
moderate cases are usually not fatal unless accompanied by another fatal disease such as peracute<br />
mastitis. The degree of fatty infiltration in these is much less obvious. The histological changes<br />
include the occurrence of fatty cysts or lipogranulomas, enlarged hepatocytes, compression of<br />
hepatic sinusoids, a decreased volume of rough endoplasmic reticulum and evidence of<br />
mitochondria! damage (11). The latter two changes are reflected in reduced albumin levels and<br />
increased activities of liver enzymes m the blood.<br />
43
DIFFERENTIAL DIAGNOSIS<br />
In dairy cows, fatty liver must be differentiated from those diseases which occur commonly<br />
immediately following parturition. Left-sided displacement of the abomasum results in a<br />
secondary ketosis, inappetence, and pings over the left abdomen.<br />
Retained placenta and metritis may be accompanied by fever, inappetence to anorexia, rumina<br />
atony, and a foulsmelling vaginal discharge. A degree of fatty liver may occur in these cows,<br />
making it indistinguishable from the effects of the retained placenta and metritis.<br />
Primary ketosis may occur immediately after parturition or within several days rather than at<br />
the most common time, at 6-8 weeks of lactation. Inappetence. ruminal hypotonicity, marked<br />
ketonuria, and a good response to glucose and propylene glycol are characteristic.<br />
In beef cattle, pregnancy toxemia before parturition must be differentiated from abomasal<br />
impaction (p. 314), vagus indigestion (p. 311) and chronic peritonitis (p. 256).<br />
TREATMENT<br />
The prognosis for severe fatty liver is unfavorable and there is no specific therapy. In general,<br />
cows with fat cow syndrome which are totally anorexic for 3 d or more usually die m spite of<br />
intensive therapy. Those which continue to eat in increasing daily amounts will recover with<br />
supportive therapy and palatable feeds. Several different therapeutic approaches have been tried<br />
based on empirical experience.<br />
Intensive therapy directed at correcting the effects of the ketosis and the fatty liver is required.<br />
The recommended treatment includes continuous IV infusion of glucose and multiple electrolyte<br />
solutions, and the intraruminal administration of rumen juice (5-10 L) from normal cows in an<br />
attempt to stimulate the appetite of affected cows. Corticosteroids such as dexamethasone at a<br />
dose of 20 mg every second day until recovery have also been used (23). Recombinant bovine<br />
somatotrophin at a dose of 640 mg SC has been used and clinical impressions indicated that it<br />
was beneficial for the treatment of fat cow syndrome (24). There were no significant differences<br />
between the treated and untreated groups in the plasma concentrations of glucose, BHBA, albumin,<br />
total protein or calcium. However, plasma urea concentration was decreased in the precalving<br />
cows 7 and 10 d after treatment with somatotrophin, and in postcalving cows with fat cow<br />
syndrome (24). Propylene glycol given orally promotes gluconeogenesis and insulin (zinc<br />
protamine) at 200-300 SC twice daily promotes the peripheral utilization of glucose. Liberal<br />
quantities of highly palatable good quality hay and an ample supply of water should be provided.<br />
Water and multiple electrolytes (10 30 L) can be administered intraruminally. The use of choline<br />
chloride at a dose rate of 25 g every 4 h, SC or orally has been recommended for the treatment of<br />
severe cases. The use of anabolic steroids (Vebonol 300 mg or trenbolone acetate is recommended)<br />
provides some improvement but all treatments are less effective the longer their commencement is<br />
delayed. In mild and moderate cases therapy is usually not required.<br />
When outbreaks of fat cow syndrome occur in pregnant beet cattle, all remaining cows should<br />
be sorted into groups according to body conditions and fed accordingly. Excessively tat cows<br />
should be fed the best quality hay which is available with a supplement. Fat cows should be<br />
exercised by feeding them on the ground and forcing them to walk.<br />
CONTROL<br />
Because of the large economic losses associated with pregnancy toxemia in cattle, even, economic<br />
effort must be made to prevent the disease. The principal method of control is to prevent pregnant<br />
cattle from becoming fat during the last trimester of pregnancy, particularly during the dry period<br />
44
in dairy cattle. During pregnancy, mature cattle should receive sufficient feed to meet the needs for<br />
maintenance and pregnancy and the total daily nutrient intake must increase throughout the last<br />
trimester to meet the needs of the fetus. However, this increase is usually difficult to control<br />
without some cows getting fat and others losing weight. Sorting cows into groups on the basis of<br />
size and condition and feeding accordingly is recommended. Metabolic profiles may be used as a<br />
means of assessing energy status and correspondingly the likelihood of occurrence or otherwise of<br />
acetonemia or pregnancy toxemia. Both blood glucose and HHBA levels can be used.<br />
In dairy cattle, all of the common diseases which occur immediately after parturition must be<br />
treated promptly and every effort made to maintain a high energy intake in high-producing cows,<br />
particularly those which calve in a fat condition. Every effort must be made to maintain the<br />
appetite of these cows. The use of propylene glycol will promote gluconeogenesis and minimize<br />
the mobilization of depot fat. The daily oral administration of 1 L of propylene glycol beginning<br />
10 d prepartum reduces the triglyceride accumulation by 32% and 42% at 1 d and 21 d postpartum,<br />
respectively, and the NEFA and the BHBA concentrations are also reduced (25).<br />
Body condition scoring of dairy cows at strategic times can be used to monitor the nutritional<br />
status of the herd and minimize the incidence and severity of fatty liver syndrome (26). The<br />
scoring should be done throughout the production cycle as part of a herd health program. Scoring<br />
done at calving, at 21-40 d, and 90-110 d postpartum can be used to monitor the nutritional status<br />
of the herd. Scoring done at 100-60 d before drying off provides an opportunity for management<br />
to make appropriate adjustments in the feeding program so that optimal body condition goals are<br />
achieved. The optimum body condition score of a cow at calving which will result m the most<br />
economical amount of milk has not yet been determined. On a scale of 5, the suggested optimum<br />
score at calving has ranged from 3-4 (27). The optimum score will probably depend on the<br />
characteristics of the individual herd which include type of cow, type of feedstuffs available,<br />
season of the year, environmental temperature and the people doing the actual body condition<br />
scoring.<br />
REFERENCES<br />
(1)Gerloti, B.J. et al. (1986)J. Am. Vet. Med.Assoc., 188, 845.<br />
(2)Reid, I. M. & Roberts, C.J. (1983) Irish Vet.J, 37, 104.<br />
(3)Grohn, Y. et al. (1987) Ada Vet. Scant.,28, 143.<br />
(4) Markusfeld, O. et al. (1997) Vet. Rec, 141, 67.<br />
(5)Gaal, T. et al. (1983) Res. Vet. Sci., 34, 245.<br />
(6)Van Den Top, A. M. et al. (1995) J. DairySci., 78, 2208.<br />
(7)Heinonen, K. et al. (1987) Ada Vet.Scand., 28, 151.<br />
(8)Watson, E. D. & Williams, L. A. (1987)Amm. Prod., 45, 9.<br />
(9)Gcrloff, B.J. & Herdt, T.J. (1984) J. Am.Vet. Med. Assoc., 185, 223.<br />
(10)Caple, I. W. ct al. (1977) Aust. Vet.J, 53,289.<br />
(11)Reid, I. M. rt al. (1986) Amm. Prod., 43,7.<br />
(12)Vazquez-Anon, M. et al. (1994)}. DairySci., 77, 1521.<br />
(13)Nakagawa, H. et al. (1997) Vet. Res.Commun., 21. 1.<br />
(14)Grummen, R. R. et al. (1990)J Dairy Sci.,75, 1537.<br />
(15)Roberts, C.J. et al. (1983) Vet. Pathol, 20,23.<br />
(16)Reid, I. M. et al. (1984) Res. Vet. Sci., 57,63.<br />
(17)Avidar, Y. et al. (1986) IsraelJ. Vet. Med.,42, 318.<br />
45
(18)Bogin, E. et al. (1988)}. Comp. Pathol., 98,387.<br />
(19)Collins, R. A. et al. (1985)J. Comp.Pathol, 95, 437,<br />
(20)Herdt, T. H. et al. (1983)J. Am. Vet. Med.Assoc., 182, 953.<br />
(21)Acorda, J. A. et al. (1994) Vet. Radiol., 55,120.<br />
(22)Acorda.J. A. et al. (1995) Vet. Q., 17, 12.<br />
(23)Andrews, A. H. et al. (1991) Vet. Rec, 29,216.<br />
(24)Maisey, I. et al. (1993) Vet. Res., 155, 293.<br />
(25)Studer, V. A. et al. (1993)7. Dairy Sci., 76,2931.<br />
(26)Hady, P. J. ct al. (1994) J. Dairy Sci., 77,1543.<br />
(27)Braun, R. K. et al. (1987) Comp. ComEduc. Pract. Vet., 9, F62.<br />
八、营养衰竭症(Dietatic Exhaustion)<br />
动物因营养不良,过度消瘦,体况下降,临床上呈进行性消瘦,易疲劳,最终卧倒,体<br />
温下降,衰竭死亡的现象称为营养衰竭症,俗称为“低温病”。本病以牛、马发生较多,羊<br />
因缺钴,猪因缺磷所致瘦母猪综合症等也都呈明显消瘦。<br />
据江苏农学院 121 例牛衰竭症统计,本病一年四季都可发生,以冬天和早春发病较多。<br />
各种年龄动物均可发病,但以老年牛发生较多,劳役过重的牛亦多发生。近年来本病已几乎<br />
消失。<br />
【病因】 引起本病的原因不外乎营养供给不足、消化吸收障碍、能量损失过多,造成<br />
能量代谢负平衡。异化作用大于同化作用,造成体内糖元、蛋白质、脂肪被动员,因而全身<br />
日渐消瘦,体况日渐下降。<br />
1。营养物质供给不足 如饲料粗、老、干、硬,甚至霉烂变质,缺乏青绿饲料,地区性<br />
缺钴或缺锌,引起动物体内微生物区系发育紊乱和食欲下降,VB12合成不足,营养成分不足,<br />
是产生本病的主因。<br />
2。消化吸收障碍,能量利用率低 如老年动物因牙齿功能不好,咀嚼障碍或长期前胃弛<br />
缓,慢性腹泻。如肝片形吸虫引起的拉稀,肝胆疾病等,引起营养物质吸收障碍。<br />
3。能量损耗太大 长期处于重役状态,补饲不足,慢性消耗性疾病如锥虫病、肝片吸虫<br />
病、猪肺丝虫、猪瘟、仔猪白痢病、创伤性心包炎等,对能量消耗过多,补充不足就可致本<br />
病。<br />
【病理】 在损耗过多,摄入不足的情况下,唯一的补救是动员体内贮备,先动用糖元,<br />
接着动用体脂,然后体蛋白分解。病牛全身皮下脂肪消耗殆净,骨骼肌消瘦,骨骼显露,严<br />
重者全身脏器平滑肌也受动员,消化道菲薄。消化腺萎缩,使吸收更趋障碍。心脏肌菲薄,<br />
造成心力衰竭;肝脏受损,蛋白质合成减少,血浆蛋白质浓度下降,甚至某些酶活性下降,<br />
使全身代谢趋于恶性循环。<br />
由于血浆蛋白浓度下降,胶体渗透压降低,因而造成全身浮肿,血容量下降和脱水现象。<br />
因肌肉萎缩,负重困难,卧地不起,发展成褥疮。体温始终正常或略偏低,四肢下部、尾端、<br />
耳尖厥冷,心音亢进,甚至呈金属音调。呼吸平和,但稍作运动则喘息明显。食欲减少,但<br />
一直保持,甚至在濒死前还可吃草和饮水。排粪少而干,但无便秘。四肢、背部有轻度浮肿。<br />
病程多在 1 个月以上,最后衰竭、躺卧、于平静中死亡。<br />
【临床表现】 病牛表现全身消瘦、骨架显露、眼球下陷、步态蹒跚。体温大多在 37<br />
℃以下,饮欲、食欲、反刍、排粪、排尿、瘤胃蠕动始终维持。但动作显迟缓、蠕动无力。<br />
心跳为 30 次/min 左右,由于胸壁薄,心音响亮。后期,病牛基本卧地不起,甚至形成褥<br />
疮,体温 36℃以下(有的在 35℃以下),口、鼻、耳、尾、四肢下部皮温较低,甚至厥冷,<br />
机体极度脱水,皮肤失去弹性。饮食欲虽可保持,但采食量减少,胃肠蠕动缓慢,肛门括约<br />
46
肌松弛、排便无力。妊娠后期及分娩母牛常有阴道脱垂。大多归于死亡。<br />
本病宜及早诊治,如发展到卧地不起,褥疮生成者,预后不良。<br />
【防治】 针对病因,于秋季即开始补饲,不仅给予蛋白质丰富的饲料,而且还要给牛<br />
羊饲料中添加微量的钴和锌,治疗原发病。适当减轻劳役,加强和改善饲养、管理,可使病<br />
逐渐恢复。<br />
治疗以补充营养,提高能量代谢为原则,给予易消化的麸皮粥、豆浆,注射高糖、VC,<br />
纠正低血钾,给予苯丙酸诺龙等强壮剂。输血浆或或全血。<br />
九、黄脂病(Yellow Disease)<br />
黄脂病是因动物体内脂肪中有类蜡质(ceroid)沉着,使脂肪显黄色,多发生于猪,亦<br />
称为黄膘。貂、猫、狐狸、鼬鼠等均可发生。<br />
各种年龄的猪和水貂都可发生该病,但只有在宰杀、剥皮后才被发现。水貂多于 8~11<br />
月发病最多,幼龄貂发病率高于成年貂,雄貂死亡率高于雌貂。<br />
【病因】 引起黄脂的原因主要是饲料中不饱和脂肪酸含量过多,和/或VE缺乏所致。<br />
如饲料中掺入变质鱼粉,鱼加工下脚料及废弃物蚕蛹等易发生黄脂,麻油渣内含不饱和脂肪<br />
酸过多,尤其是用小磨麻油的油渣喂猪易诱发本病。水貂由变质鱼粉或含脂量过多的鱼,如<br />
鲱鱼、鲭、鳀、鲭占鱼、比目鱼、鲑鱼等饲喂最危险,这些鱼体内脂肪大多为不饱和脂肪。<br />
饲喂天然的含有黄色素饲料,有时亦可产生黄脂,如黄胡萝卜、南瓜、黄玉米等,因色<br />
素溶解在脂肪中亦可产生黄脂。<br />
遗传因素,有人曾作调查,凡产生黄脂的猪,其父本或母本也曾患有黄脂。<br />
鼬鼠用久经贮藏的冻肉或冰鱼饲喂之后,不仅有黄脂,还可伴发麻痹。<br />
【病理】 当VE缺乏或不足时,高不饱和脂肪酸在体内被氧化为过氧化脂质,随即与<br />
某些蛋白质结合,形成某些复合物,再被溶酶体酶分解之后被排出。如不能被分解,则形成<br />
棕色色素颗粒——类蜡质,它们或位于脂肪细胞外周,或存在于巨嗜细胞内,使脂肪呈现黄<br />
色。因类蜡质有刺激性,有腥气味,可引起脂肪发炎。鱼粉霉变后,鱼类加工下脚料变质后,<br />
VE大量破坏,加之不饱和脂肪酸过多,容易造成黄脂。用新鲜蚕蛹或干蚕蛹喂猪,不致发<br />
生黄脂,只有用腐败的未去油的蚕蛹饲喂才致病。猪、貂饲料中添加VE,可预防或减少疾<br />
病发生。<br />
【临床表现】 黄膘猪生前很难判断。常见的症状包括被毛粗糙、倦怠、衰弱和黏膜苍<br />
白,多数病猪食欲不良,增长缓慢,有的行走时颈背部硬,剖腹后可闻到一股腥臭味,加热<br />
或炼油时明显,腹腔脂肪显黄色,有的腹内脂肪萎缩,质硬。肝脏呈黄褐色,明显脂肪变性。<br />
【诊断】 根据尸体剖检、皮下和腹腔脂肪呈典型的黄色、黄褐色,肝脏呈土黄色,有<br />
的还有脂肪坏死者不难作出诊断。但必须区别黄脂、黄脂病和黄疸。黄脂仅皮下、网膜、肠<br />
系膜、腹部脂肪呈黄色。遇冷后褪色,水煮后又可恢复为淡黄色,一般无异味,或有点如煮<br />
玉米揭锅时的气味。黄脂病:与黄脂炎似,但一般都有鱼腥臭味,尤其是因吃鲜鱼或蚕蛹的<br />
猪肉,加热后更明显,镜检可见脂肪组织间有类蜡质黄色颗粒。黄疸:动物因受病原微生物<br />
侵袭或毒物中毒,大量出血或因胆汁排泄受阻所致,不仅脂肪显黄色,而且可视黏膜、多种<br />
组织、关节液等均呈黄色,加热后颜色减退,由橙色变为淡黄色,接触空气氧化以后颜色变<br />
深,如取脂肪少许用 50%酒精震荡抽提后,在滤液中加 10~20 滴浓硫酸,显绿色者为黄疸,<br />
继续加酸和加热,可显蓝色。<br />
【防治】 防治本病的原则是增加VE供给,减少食物中不饱和脂肪酸的含量,有条件<br />
的可先去油,后饲。<br />
每天给 500~700mg生育酚可防止猪的黄膘。水貂饲料中每天给 0.25mgVE,连续 100 天,<br />
同时给予VB1230~50mg,不仅可防止黄脂,还可提高受胎率和产仔率。<br />
十、禽痛风(Pultry Gout)<br />
47
痛风是指血液中蓄积过量尿酸盐,不能迅速排出体外,沉积在关节囊、关节软骨和软骨<br />
周围,或沉积在胸腹腔脏器表面和其它组织中,如肾小管和输尿管内,临床上表现为运动迟<br />
缓,腿、翅关节肿胀,厌食,衰弱及腹泻,因尿酸和尿酸盐增多,常引起肛周羽毛为白色尿<br />
酸盐沾附。<br />
痛风主要发生于鸡、火鸡、鹅、雉、鸽子,甚至丹顶鹤都可发生,在某些鸡群中本病发<br />
病率较高,有的甚至达 50%,但一般占 15%,近些年来本病发生有增多趋势。老年狗亦可<br />
患痛风。<br />
禽痛风分为内脏型和关节型两种,前者是指尿酸盐沉着在内脏表面,后者是指尿酸盐沉<br />
着在关节囊和关节软骨及其周围。<br />
【病因】 引起痛风的原因很多,但可归纳为:<br />
1。体内尿酸盐形成太多 饲料中蛋白质含量尤其是核蛋白含量太多,嘌呤喊含量太多。<br />
如用动物内脏、胸腺、肝、肾、头肉、肉屑、鱼粉或大豆粉、豌豆等作蛋白质源,而且掺入<br />
比例太高。当鱼粉用量超过 8%,或配合所用尿素超过 13%,粗蛋白含量超过 28%时,则<br />
因核酸和嘌呤代谢终产物尿酸生成过多,生成速率大于排泄速率,则可产生痛风。特殊情况<br />
下动物患慢性消耗性疾病,体蛋白分解,产生尿酸速度增加,如患白血病的鸡、蓝冠病等易<br />
患痛风。<br />
2.尿酸排泄障碍 引起尿酸排泄障碍多与肾功能状况有关,某传染因素如传染性支气管<br />
炎病毒,可引起肾炎,并产生痛风。此外,传染性法氏囊炎病毒、败血性霉形体、雏白痢、<br />
盲肠肝炎病毒等都可引起痛风。非传染性因素中如VA缺乏,食盐过多加上饮水不足,尿量<br />
减少,尿液浓缩,饲料中磷不足,钙太多、钙异位沉着,形成肾结石或积砂,排尿不畅。中<br />
毒性因素,某些重金属有嗜肾性,某些药物如磺胺类药物、丙酮等,菠菜、莴苣等草酸盐含<br />
量过多,棕色曲霉毒素等,可引起肾损伤,尿酸盐排泄不畅,可导致痛风。<br />
3。遗传因素 在某些品种鸡易发生痛风,特别是关节型痛风与高蛋白饲料和遗传因素关<br />
系密切,高蛋白饲料可促进这些鸡发生痛风。<br />
4,诱因 老年动物,纯系育种动物,运动不足,受凉、孵化时湿度太大,生活在卵内<br />
的雏就可能患内脏型痛风。<br />
【病理】 鸟类肝脏内缺乏精氨酸酶,蛋白质代谢终产物氨只能生成嘌呤,在黄嘌呤酶<br />
系作用下形成尿酸,经肾排出。饲料中蛋白质含量越高,产生尿酸越多,当尿酸盐生成速度<br />
大于排泄速度时,就造成尿酸盐蓄积。此外当泌尿器官本身疾病时,造成尿酸排泄障碍。尿<br />
酸盐沉积在胸膜腔、腹腔、关节腔。尿路通畅与否,对痛风形成至关重要。即使有肾小球性<br />
肾炎,间质性肾炎,不一定伴发痛风。但尿石症、堵塞了肾小管,则可能产生痛风。<br />
【临床表现】 两种类型痛风的发病率,临床表现有较大差异。生产中禽痛风以内脏型<br />
为多,关节型痛风较少见。<br />
内脏型痛风:可以是零星散发,也可成批发生,多因肾功能衰竭而死。一开始病禽消化<br />
扰乱和腹泻,在 6~9 天内鸡群中可完全展现。通常为慢性,鸡冠发白、贫血、脱羽,生长缓<br />
慢,粪呈白色,稀水样,少数可突然死亡。致病原因不一样,原发性症状也不一样。传染性<br />
气管炎有呼吸系统症状,VA缺乏伴有干眼、鼻孔易堵塞。高钙、低磷则可产生骨代谢障碍。<br />
关节型痛风:可表现腿翅关节软性肿胀、疼痛、运动迟缓、跛行、不能站立,切开关节<br />
腔有稠厚的白色、粘性液体流出。有时脊椎、甚至肉垂也形成结节性肿胀。<br />
剖检变化:内脏浆膜上覆盖着一层白色、石灰样尿酸盐沉淀,遍布整个脏器,肾肿大、<br />
色苍白、表面有雪花状花纹。肾实质中也可见到,输尿管增粗,内有尿酸盐结晶,因而又称<br />
为禽的尿石症。近年来剖检的鸡中,尿石症有增多的趋势。用含 2.5%的钙喂给 8~20 周龄小<br />
母鸡,可引起肾病、内脏痛风和尿酸钙沉着。关节型痛风主要变化在关节,切开关节囊,内<br />
有膏状白色尿酸盐沉着,因尿酸盐刺激常引起关节面溃疡及关节囊坏死。痛风石(tophus)<br />
48
是一种特殊的肉芽组织,由分散或成团的尿酸盐结晶沉积在坏死组织中,周围有炎性细咆、<br />
吞噬细胞、巨嗜细胞、成纤维细胞等构成。无论是内脏型还是关节型痛风,在肾脏和关节腔<br />
内及关节周围组织中都有痛风石形成。<br />
血液尿酸盐浓度升高,从正常时 0.09~0.18mmol/L(1.5~3.0mg/l00ml)升高到<br />
0.897mmol/L(15mg/l00ml)以上。血液中非蛋白氮(NPN)值也升高,因机体脱水,PCV<br />
值升高,血沉速率下降,尿钙浓度、尿液 pH 值升高。<br />
【诊断】 生前诊断根据跛行、跗关节、肩关节软性肿胀、粪色白而稀可作出诊断。确<br />
诊根据血液尿酸、尿酸盐浓度升高,内脏表面有尿酸盐沉着,关节腔内有白色混浊液体,有<br />
痛风石生成等特征作出诊断。但应与关节型结核,沙门氏菌和小球菌引起的传染性滑膜炎相<br />
区别。如关节液中有针状和禾束状晶体或放射形晶柱者则为痛风。<br />
【预防】 控制日粮中粗蛋自在 20%以下,限量用动物内脏及下脚料掺入日粮中,禁<br />
止用腺体(胸腺、甲状腺)和淋巴结组织饲喂。增加VA及VBl2的供给,鸡日粮中可掺入干牛<br />
粪饲喂,能防止痛风发生,严格控制各个生理阶段日粮中钙、磷供给量对防止该病有重要意<br />
义。<br />
本病治疗意义不大。对珍稀禽类可试用别嘌呤醇治疗。<br />
第三节 维生素营养紊乱性疾病<br />
(Nutritional Disorder of Vitamines)<br />
维生素是生命组织的重要营养成分之一,它不仅作为许多酶的辅酶参予生命活动,而且<br />
可直接或间接影响动物生长、器官和组织的发育。维生素缺乏可以引起一系列缺乏症<br />
(Vitamine deficiency)。反之,维生素供给过多亦可引起中毒症(vitamine toxicosis)。<br />
大多数动物、植物源性饲料中都含有丰富的维生素,有些维生素可由动物本身或寄生于<br />
消化道的细菌所合成,因而一般不易引起缺乏。但在饲料加工调制过程中,维生素本身及其<br />
前体被破坏,动物本身消化、吸收、转运机能受阻,或本身合成条件不具备,可造成某些维<br />
生素相对缺少;可因动物生理需要增加,又未及时获得补充时,亦可造成缺乏症。<br />
当动物处于某种维生素缺乏时,不适当地补充过多或长期饲以含某种维生素过多的食物<br />
则又可酿成中毒。<br />
缺乏等。<br />
兽医临床常见的维生素缺乏和中毒,包括两大类:<br />
1。脂溶性维生素缺乏和中毒,如VA缺乏和中毒,VD缺乏和中毒,VE缺乏症,VK缺乏症。<br />
2。水溶性维生素缺乏症,包括B族维生素缺乏症,胆碱、叶酸缺乏,生物素缺乏、Vc<br />
一、维生素 A 营养紊乱性疾病(Nutritional Discorder of Vitamine A)<br />
(一)维生素 A 缺乏症(Hypovitaminosis A)<br />
VA缺乏症是指动物体内VA含量不足而发生,临床上表现脑脊髓功能不全,晕厥,共济<br />
失调。表现夜盲,角膜干燥,干眼,成年动物繁殖机能下降,禽痛风发病率升高。有时甚至<br />
可出现仔畜或幼雏先天性缺陷。<br />
本病主要发生于犊牛、牛、猪、禽、兔、猫、犬也可发生。<br />
【病因】 目前所知,VA分为VA1和VA2,动物体内VA主要分布在肝脏,尤其是鲨鱼、<br />
比目鱼、鳕鱼等肝脏中含量丰富。植物组织中以胡萝卜、玉米黄素为VA的前体,胡萝卜、<br />
青草、南瓜、黄玉米中VA含量丰富,而谷类及其副产品如麸皮、米糠、粕类中VA含量较少。<br />
因此长期用配合日粮饲喂,未补充青绿饲料易产生缺乏症。饲料加工不当,贮存时间太长,<br />
可影响VA的含量。黄玉米贮存期超过 6 个月,约 60%VA可被破坏。粒料加工过程中可使β-<br />
胡萝卜素损失 32%以上。<br />
VA及胡萝卜素是脂溶性物质,它的消化吸收必须在胆汁酸参与下进行。因此,长期拉<br />
稀,肝胆疾病,十二指肠慢性炎症,可造成对VA吸收不充分,进入体内的VA及其前体随粪<br />
49
排出。长期食入过多的油脂,饲料中添加脂肪过多,可造成VA缺乏。<br />
VA不能通过胎盘,故初生仔畜容易患病。初乳中VA含量较高,是初生仔畜获得VA的唯<br />
一来源。动物分娩后死亡,或因各种原因吃不到初乳时,容易发生VA缺乏症。犊牛、仔猪 3<br />
周龄前,母乳中VA不足,或用代乳品饲喂,或断乳过早都可致VA缺乏。<br />
动物对VA需要量增多,可引起VA相对缺乏。妊娠、哺乳母畜,生长快速的幼畜,长期<br />
腹泻或患热性疾病的动物,对VA需要量增多。如不额外补充,则可酿成VA缺乏。<br />
有些因素可以影响VA的吸收利用,间接地产生VA缺乏症。如胆汁酸分泌不足,食物中<br />
脂肪含量过少等,可引起VA吸收利用不足;VE可促使VA的吸收,同时可作为抗氧化剂、防<br />
止VA在肠内被氧化;饲料中蛋白质含量减少,VA吸收率下降(可能与胰腺分泌胰脂肪酶数<br />
量不足有关),这些因素最终引起体内VA缺乏。<br />
【病理】 VA缺乏可产生机体器官和组织的一系列损伤:<br />
1.上皮组织角化 VA是维持上皮组织结构完整的重要营养成分。缺乏VA,可产生上皮<br />
组织干燥,过度角化及脱屑,其中以眼、呼吸道、消化道、泌尿道及生殖道黏膜受影响最严<br />
重。临床上出现干眼,咳嗽,消化不良,尿石生成,禽痛风生成,母畜流产或死胎等。公畜<br />
精子生成减少,胎儿先天性缺损或成形不全。<br />
2。生长发育迟滞 VA有促进生长发育,促使成骨细胞活性增高,导致骨皮质内钙沉着。<br />
当VA缺乏时,由于软骨内骨生成受阻或破坏,加之蛋白质合成减少,因而动物生长发育受<br />
影响。相反,VA过多时,则由于皮质内骨生成过度,骨间间隙减小,因而造成骨骼间活动<br />
受影响。如颈椎乃至全脊柱受影响。<br />
3。视力障碍 维生素A是合成视色素(视紫红质)的必需物质。在视网膜上有杆细胞和<br />
锥细胞,其中蛋白质可以分别与VA1和VA2结合,合成视紫质(牛)、视紫蓝质、视紫青质(禽<br />
类)等暗光感受物质。当爆光时,视色素分解为视黄醛和视蛋白,在光电子作用下构成不同<br />
的吸光谱,并产生这两种细胞上的电位差,分别感受强光和弱光,以辨周围环境。鸟类对强<br />
光反射敏感,对弱光反射弱,因而有“雀目”之称。当VA缺乏时,视黄醛合成减少,视紫<br />
红质合成受阻,导致对暗光适应能力减弱,发生夜盲症,严重时可完全丧失视力。<br />
4。骨塑形和骨精细构造受影响 VA可维持成骨细胞与破骨细胞功能的平衡,保持骨塑<br />
形良好,骨精细构造完好。当VA缺乏时,引起颅骨、椎骨、甚至长骨发育不匀称,骨腔狭<br />
小。临床上常可造成颅内压力增高,脑受挤压,甚至形成脑疝,小脑进入椎间大孔,脊索受<br />
挤而入椎间孔,引起中枢及外周机能障碍。如产生惊厥、平衡障碍,共济失调、视神经乳头<br />
水肿等。<br />
5。免疫防御机能下降 由于上皮组织完整性受损,抗微生物侵袭能力下降,VA缺乏后,<br />
白细胞吞噬活性减弱,抗体生成减少,防卫机能减弱,抗病力低下,极易感染疾病。<br />
【临床表现】 视力障碍,瞳孔对光反应迟钝。夜盲症(night blindness)是VA缺乏早<br />
期症状(猪除外)之一,在黎明、黄昏或月光下看不见物体。干眼病(xerophthaImia),狗<br />
和犊牛角膜上有厚的呈云雾状附属物,而其它品种角膜上有稀薄的浆液、粘液样分泌物,随<br />
后角膜呈角质化的云雾状,有时有角膜溃疡,甚至穿孔而失明。<br />
皮肤病变:皮肤干燥、脱屑、皮炎、被毛蓬乱无光泽,脱毛,秃毛,蹄、角生长不良,<br />
尤其是猪。蹄壳干燥有纵行皲裂,马最明显。<br />
神经症状:幼畜最明显,无目的地行走,转圈,有时前肢跪地后又举起,共济失调。有<br />
时出现假死和晕厥,常见于犊牛及仔猪。<br />
繁殖机能障碍:公畜精液品质不良;母畜发情扰乱,受胎率下降,胎儿发育不全、先天<br />
性缺陷、畸形或胎儿吸收,流产、早产、死产,所产仔畜生活力低下、体质孱弱、易死亡。<br />
尤其是新生仔猪常有唇裂、颚裂、无眼附耳等畸形,后肢变形,皮下囊肿,心脏缺陷,膈疝,<br />
脑室积水等。<br />
50
血浆中维生素 A 浓度从 250µg/L 降为 50µg/L,血浆胡萝卜素从 1500µg/L 以上至<br />
90µg/L 以下。<br />
抗病力低下:动物极易发生支气管炎、肺炎、胃肠炎等。<br />
由于种属、年龄和受损器官不同,患病动物除上述症状外尚有各自的症状。<br />
犊牛:病初呈夜盲症,后继发干眼病,甚至失明。同时并发唾液腺炎、副眼腺炎、角膜<br />
炎、脑脊液压力升高,共济失调,出现阵挛或强直性痉挛发作,或阵发性惊厥。视神经萎缩,<br />
亦有呈先天性脑病症状的犊牛。<br />
羔羊:缺乏VA时体质孱弱,视力障碍,易患支气管炎和肺炎;死亡率高,由于脑脊液压<br />
力升高,有时出现阵发性痉挛和共济失调,后躯瘫痪。<br />
仔猪:视力减弱,皮肤呈湿疹样炎症(脂溢性皮炎),脑脊液压力升高,呈现共济失调,<br />
后肢麻痹和惊厥。外周神经根损伤,致骨骼肌麻痹,有的仔猪出生后呈小眼畸形、颚裂、兔<br />
唇或后肢畸形,脑室积水等,很快死亡。存活仔猪生活力弱,腹泻,头偏向一侧,易继发肺<br />
炎、胃肠炎、佝偻病。<br />
禽:消瘦,鼻流水样或粘液状鼻液,眼睑粘着,有时被干酪样分泌物积聚。羞明流泪,<br />
严重时角膜软化,甚至穿孔失明。特征性变化是口、咽、硬腭、喉有白色伪膜状物附着,但<br />
易剥离。母鸡VA缺乏所产蛋,孵出的雏鸡经 5~7 天开始发病。多出现神经病状,知觉过敏,<br />
头颈扭转或呈向后退动作,共济失调,干眼或眼炎。<br />
【诊断】 初生仔畜突然出现神经症状、夜盲,母畜出现流产、死胎、胎儿畸形增多,<br />
可怀疑为VA缺乏。视神经乳头水肿,眼黏膜涂片检查,角化上皮细胞数量增多(健康牛一<br />
个视野中仅 3 个,病牛可达 11 个)。实验室测定血浆肝脏VA及胡萝卜素含量明显减少者,<br />
可提示诊断。剖检可见唾液腺、喉头、气管内有伪膜生成,可进一步肯定。<br />
鉴别诊断应与低镁血症、脑灰质软化症、魏氏梭菌毒素 D 中毒、伪狂犬病、散发性脑、<br />
脊髓炎等相区别。<br />
在猪,后肢麻痹现象更常见,但应与伪狂犬病、病毒性脑脊髓炎、食盐中毒、有机砷、<br />
有机汞中毒所引起的神经症状相区别。<br />
【防治】 用VA治疗效果明显,剂量是 133µg/kg(440IU/kg)体重,皮下注射。对<br />
猪、牛效果明显。鸡VA用量几乎是猪、牛的 3 倍,约 364µg/kg(1200IU/kg)体重,注射<br />
后脑脊髓液压力于 48 小时内恢复,眼疾恢复需时较长。<br />
在动物日粮中应添加VA,各种动物对VA的需要量的规律是妊娠、泌乳、催肥的动物是<br />
通常需要量的 1 倍。按需要量(µg/kg体重)计,牛,12~24;羊,9~24;猪,12~24;鸡,<br />
364~727;鸭、珍珠鸡、火鸡需要量比鸡另增加 20%左右。<br />
(二)维生素 A 过多症(Hyper vitaminosis A)<br />
当饲料中供给VA的含量是正常需要量的 100 倍以上,或者用动物肝脏饲喂猫,或用鱼<br />
内脏(去肠)制作猫食时,可引起VA过多症,又称VA中毒。狗可实验性产生VA中毒,犊牛<br />
和猪亦可引起VA中毒。<br />
猫中毒时,表现倦怠。牙龈充血、水肿,厌食,腹胀,跛行,颈部僵硬,椎脊突形成外<br />
生骨疣。中毒猫骨生长阻滞,成年动物的骨性骨疣十分明显。从第一颈椎至第二胸椎间,形<br />
成明显可见的关节桥。慢性病例椎体阴影模糊,骨干及关节周围也形成骨性增生。饲料中<br />
VA过多,对赘生骨骼中钙、磷的比例影响不大。VA对软骨正常生长、矿化及重溶都是很重<br />
要的,而VA过多可引起骨皮质内成骨过度,这是VA的主要毒性。另外VA过多还可使骨受伤<br />
时易破碎,年青动物生长阻滞。长期大量内服VA还可使猫的胎儿致畸。<br />
犊牛VA过多是因饲料中或治疗时给予VA不恰当引起的。患犊表现生长缓慢,跛行,行<br />
走不稳,瘫痪。第三指节骨形成外生骨疣,在X阴影上形成“第四”指节骨,骨节间软骨消<br />
失。长期供给大量VA还可造成角生长缓慢,脑脊液压力下降。剖检可见掌骨远端,近侧端<br />
51
和远侧端有薄薄的外生骨疣。<br />
仔猪用大量VA饲喂,可产生大面积出血和突然死亡。妊娠早期给予VA过多可引起胎儿<br />
增大,但实验性大量长期喂给VA过多,未发现对猪的胚胎的毒性作用和致畸作用。<br />
治疗VA中毒主要是更换饲料,部分VA中毒症状可得以克服,成年猫临床症状有所改善,<br />
但关节骨性增生常无法改观,血液VA含量几周内转为正常,但肝脏VA贮备几年内却能保持<br />
高水平。<br />
VITAMIN A DEFICIENCY (HYPOVITAMINOSIS-A)<br />
A deficiency of vitamin A may be caused by an insufficient supply of the vitamin in the ration or<br />
its defective absorption from the alimentary canal. In young animals, the manifestations of the<br />
deficiency are mainly those of compression of the brain and spinal cord. In adult animals, the<br />
syndrome is characterized by night blindness, corneal keratinization, pityriasis, defects in the<br />
hooves, loss of weight, and infertility.Congenital defects are common in the offspring of deficient<br />
dams. Vitamin A may also provide a protective effect against various infectious diseases and<br />
enhance many facets of the immune system.<br />
Synopsis<br />
Etiology.Dietary deficiency of vitamin A or its precursors.<br />
Epidemiology. Primary vitamin A deficiency in animals fed diet deficient in vitamin A or its<br />
precursors. Common in cattle grazing dry pastures for long periods. Occurs when diet of hand-fed<br />
animals is not supplemented with vitamin A.<br />
Signs Cattle: Night blindness. Loss of body weight. Convulsions followed by recovery.<br />
Episodes of syncope. Permanent blindness with dilated pupils and optic disc edema.<br />
Pigs: Convulsions, hindleg paralysis,congenital defects.<br />
Clinical pathology. Low levels plasma vitamin A.<br />
Lesions. Squamous metaplasia of interlobular ducts of parotid gland.<br />
Compression of optic nerve tracts and spinal nerve roots. Degeneration of testes.<br />
Diagnostic confirmation. Low levels of plasma vitamin A and squamous metaplasia of<br />
interlobular ducts of parotid glands.<br />
Differential diagnosis list:<br />
Cattle:<br />
• Polioencephalomalacia<br />
• Hypomagnesemic tetany<br />
• Lead poisoning<br />
• Rabies<br />
• Meningoencephalitis<br />
• Peripheral blindness due to bilateral<br />
ophthalmitis.<br />
Swine:<br />
• Salt poisoning<br />
• Pseudorabies<br />
• Viral encephalomyelitis<br />
• Spinal cord compression due to vertebral body abscess.<br />
Treatment. Vitamin A injections.<br />
Control. Feed diets with adequate carotene. Supplement diet with vitamin A. Parenteral injections<br />
of vitamin A at strategic times.<br />
52
ETIOLOGY<br />
Vitamin A deficiency may be primary disease, due to an absolute deficiency of vitamin A or its<br />
precursor carotene in the diet, or a secondary disease in which the dietary supply of the vitamin or<br />
its precursor is adequate, but their digestion, absorption or metabolism is interfered with to<br />
produce a deficiency at the tissue level.<br />
EPIDEMIOLOGY<br />
Primary vitamin A deficiency<br />
Primary vitamin A deficiency is of major economic importance in groups of animals on pasture or<br />
fed diets deficient in the vitamin or its precursors. Animals at pasture receive adequate supplies of<br />
the vitamin, except during prolonged droughts, but animals confined indoors and fed prepared<br />
diets may be deficient if not adequately supplemented. For example, a diet of dried sugar beet pulp,<br />
concentrates and poor quality hay can result in hypovitaminosis-A in confined beef cattle.<br />
Ruminants on pasture<br />
Primary vitamin A deficiency occurs in beef cattle and sheep on dry range pasture during periods<br />
of drought. Clinical vitamin A deficiency does not always occur under these conditions because<br />
hepatic storage is usually good and the period of deprivation not sufficiently long for these stores<br />
to reach a critically low level (1). Young sheep grazing natural, drought-stricken pasture can suffer<br />
serious depletion of reserves of the vitamin in 5-8 months, but normal growth is maintained for 1<br />
year at which time clinical signs develop. Adult sheep may be on a deficient diet for 18 months<br />
before hepatic-stores are depleted and the disease becomes evident. Cattle may subsist on<br />
naturally deficient diets for 5-18 months before clinical signs appear. However, during the annual<br />
dry season (October-June),herds of cattle, sheep, and goats in the Sahelian region of West Africa<br />
are managed on dry grasses and shrubby ligneous plants, which fail to provide maintenance levels<br />
of crude protein and vitamin A. These substandard conditions result in vitamin A deficiency<br />
characterized by night blindness, xerophthalmia, retarded growth rates, reproductive failures, and<br />
increased mortality (2). The pastoral herders associate the cure of night blindness with the<br />
consumption of green vegetation and will purposefully herd livestock into green vegetation areas<br />
when available. Certain ethnic groups of pastoral herders depend on ruminant milk as their<br />
principal source of vitamin A, and night blindness in lactating and pregnant women as well as in<br />
young children appears after the onset of night blindness in their cattle and sheep during the latter<br />
half of the dry season. Therefore, increasing vitamin A levels in the milk of cows may alleviate<br />
the clinical signs of vitamin A deficiency in herder families.<br />
Primary vitamin A deficiency is still relatively common in beef cattle that depend on pasture<br />
and roughage for the major portion of their diet. Beef calves coming off dry summer pastures at<br />
6-8 months of age are commonly marginally deficient.<br />
Maternal deficiency<br />
A maternal deficiency of vitamin A can result in herd outbreaks of congenital hypovitaminosis-A<br />
in calves (3). In one such occurrence, out of 240 heifers fed a vitamin A-deficient ration, 89 calves<br />
were born dead, 47 were born alive but blind and weak and died within 1-3 days after birth.<br />
Blindness with dilated pupils, nystagmus, weakness, and incoordination were characteristic. The<br />
status of the dam is reflected in that of the fetus only in certain circumstances, in that carotene, as<br />
it occurs in green feed, does not pass the placental barrier and a high intake of green pasture<br />
before parturition does not increase the hepatic stores of vitamin A in newborn calves, lambs or<br />
kids and only to a limited extent in pigs. However, vitamin A in the ester form, as it occurs in fish<br />
53
oils, will pass the placental barrier in cows. Feeding of these oils, or the parenteral administration<br />
of a vitamin A injectable preparation before parturition, will cause an increase in stores of the<br />
vitamin in fetal livers. Antepartum feeding of carotene and the alcohol form of the vitamin does,<br />
however, cause an increase in the vitamin A content of the colostrum. Young animals depend on<br />
the dam's colostrum for their early requirements of the vitamin which is always highest in<br />
colostrum and returns to normal levels within a few days of parturition. Pigs weaned very early at<br />
2-4 weeks may require special supplementation. Pregnant beef cows wintered on poor quality<br />
roughage commonly need supplementation with vitamin A throughout the winter months to insure<br />
normal development of the fetus and an adequate supply of the vitamin in the colostrum at<br />
parturition.<br />
Adequacy of supplements<br />
The addition of vitamin A supplements to diets may not always be sufficient to prevent deficiency.<br />
Carotene and vitamin A are readily oxidized, particularly in the presence of unsaturated fatty acids.<br />
Oily preparations are thus less satisfactory than dry or aqueous preparations, particularly if the<br />
feed is to be stored for any length of time. Pelleting of feed may also cause a serious loss up to<br />
32% of the vitamin A in the original feedstuff.<br />
Heat, light, and mineral mixes are known to increase the rate of destruction of vitamin A<br />
supplements in commercial rations. In one study, 47-92% of the vitamin A in several mineral<br />
supplements was destroyed after 1 week of exposure to the trace minerals, high relative humidity,<br />
sunlight, and warm temperatures (4).<br />
Feedlot cattle<br />
The disease still occurs in feedlot cattle in some parts of North America when feedlot cattle are<br />
fed rations low in carotene or vitamin A over a period of several months (5). The onset of clinical<br />
signs in growing feedlot cattle is typically seen 6-12 months after feeding a diet deficient in<br />
carotene or vitamin A. Small farm feedlots may feed their cattle a cereal grain such as barley, and<br />
barley straw with no vitamin supplementation (6) or inadequate supplementation (7). Grains, with<br />
exception of yellow corn, contain negligible amounts of carotene and cereal hay is often a poor<br />
source. Any hay cut late, leached by rain, bleached by sun, or stored for long periods loses much<br />
of its carotene content. The carotene content of yellow corn also deteriorates markedly with long<br />
storage. Moreover, under conditions not yet completely understood, the conversion by ruminants<br />
of carotene present in feeds such as silage may be much less complete than was formerly thought.<br />
In feedlot cattle, the disease is most common in steers fed the same ration as heifers which may<br />
remain clinically normal (4,5). It is suggested that sexual dimorphism may be due to the<br />
production of vitamin A by the corpus luteum of heifers (5).<br />
Swine<br />
Young pigs on a deficient diet may show signs after several months, but as in other animals, the<br />
length of time required before signs appear is governed to a large extent by the status before<br />
depletion commences. As a general rule it can be anticipated that signs will appear in pigs fed<br />
deficient rations for 4-5 months, variations from these periods probably being due to variations in<br />
the vitamin A status of the animal when the deficient diet is introduced. Congenital defects occur<br />
in litters from deficient sows, but the incidence is higher in gilts with the first litter than in older<br />
sows. It is presumed that the hepatic stores of vitamin A in older sows are not depleted as readily<br />
as in young pigs. Feeding white maize bran without supplementation can result in congenital<br />
defects in litters and paralysis in adult pigs (8).<br />
54
Horses<br />
Adult horses may remain clinically normal for as long as 3 years on a deficient diet.<br />
Secondary vitamin A deficiency<br />
Secondary vitamin A deficiency may occur in cases of chronic disease of the liver or intestines<br />
because much of the conversion of carotene to vitamin A occurs in the intestinal epithelium, and<br />
the liver is the main site of storage of the vitamin. Highly chlorinated naphthalenes interfere with<br />
the conversion of carotene to vitamin A and animals poisoned with these substances have a very<br />
low vitamin A status. The intake of inorganic phosphorus also affects vitamin A storage, low<br />
phosphate diets facilitating storage of the vitamin. This may have a sparing effect on vitamin A<br />
requirements during drought periods when phosphorus intake is low, and an exacerbating effect in<br />
stall-fed cattle on a good grain diet. However, phosphorus deficiency may lower the efficiency of<br />
carotene conversion. Vitamins C and E help to prevent loss of vitamin A in feedstuffs and during<br />
digestion. Additional factors which may increase the requirement of vitamin A include high<br />
environmental temperatures, a high nitrate content of the feed, which reduces the conversion of<br />
carotene to vitamin A, and rapid rate of gain. Both a low vitamin A status of the animal and high<br />
levels of carotene intake may decrease the biopotency of ingested carotene.<br />
The continued ingestion of mineral oil, which may occur when the oil is used as a preventive<br />
against bloat in cattle, may cause a depression of plasma carotene and vitamin A esters and the<br />
carotene levels in buffer fat. Deleterious effects on the cattle are unlikely under the conditions in<br />
which it is ordinarily used because of the short period for which the oil is administered and the<br />
high intake of vitamin A and carotene.<br />
PATHOGENFSIS<br />
Vitamin A is essential for the regeneration of the visual purple necessary for dim-light vision, for<br />
normal bone growth, and for maintenance of normal epithelial tissues. Deprivation of the vitamin<br />
produces effects largely attributable to disturbance of these functions. The same tissues are<br />
affected in all species. However, there is a difference in tissue and organ response in the different<br />
species and particular clinical signs may occur at different stages of development of the disease.<br />
The major pathophysiological effects of vitamin A deficiency are as follows.<br />
Night vision<br />
Ability to see in dim light is reduced because of interference with regeneration of visual purple.<br />
Cerebrospinal fluid pressure<br />
An increase in CSF pressure is one of the first abnormalities to occur in hypovitaminosis-A in<br />
calves. It is a more sensitive indicator than ocular changes and, in the calf, it occurs when the<br />
vitamin A intake is about twice that needed to prevent night blindness. The increase in CSF<br />
pressure is due to impaired absorption of the CSF due to reduced tissue permeability of the<br />
arachnoid villi and thickening of the connective tissue matrix of the cerebral dura mater. The<br />
increased CSF pressure is responsible for the syncope and convulsions, which occur in calves in<br />
the early stages of vitamin A deficiency. The syncope and convulsions may occur spontaneously<br />
or be precipitated by excitement and exercise. It is suggested that the CSF pressure is increased in<br />
calves with subclinical deficiency and that exercise further increases the CSF pressure to<br />
convulsive levels.<br />
Bone growth<br />
Vitamin A is necessary to maintain normal position and activity of osteoblasts and osteoclasts.<br />
When deficiency occurs there is no retardation of endochondral bone growth, but there is<br />
55
incoordination of bone growth in that shaping, especially the finer molding of bones, does not<br />
proceed normally. In most locations this has little effect but may cause serious damage to the<br />
nervous system. Overcrowding of the cranial cavity occurs with resulting distortion and<br />
herniations of the brain and an increase in CSF pressure up to four to six times normal. The<br />
characteristic nervous signs of vitamin A deficiency, including papilledema, incoordination and<br />
syncope, follow. Compression, twisting, and lengthening of cranial nerves and herniations of the<br />
cerebellum into the foramen magnum, causing weakness and ataxia, and of the spinal cord into<br />
intervertebral foraminae results in damage to nerve roots and localizing signs referable to<br />
individual peripheral nerves. Facial paralysis, and blindness due to constriction of the optic nerve,<br />
are typical examples of this latter phenomenon. The effect of excess vitamin A on bone<br />
development by its interference with vitamin D has been discussed elsewhere. Dwarfism in a<br />
group of pigs in a swine herd was suspected to be due to vitamin toxicosis (9).<br />
Epithelial tissues<br />
Vitamin A deficiency leads to atrophy of all epithelial cells, but the important effects are limited<br />
to those types of epithelial tissue with a secretory as well as a covering function. The secretory<br />
cells are without power to divide and develop from undifferentiated basal epithelium. In vitamin A<br />
deficiency these secretory cells are gradually replaced by the stratified, keratinizing epithelial cells<br />
common to non-secretory epithelial tissues. This replacement of secretory epithelium by<br />
keratinzed epithelium occurs chiefly in the salivary glands, the urogenital tract (including placenta<br />
but not ovaries or renal tubules) and the paraocular glands and teeth (disappearance of<br />
odontoblasts from the enamel organ). The secretion of thyroxine is markedly reduced. The mucosa<br />
of the stomach is not markedly affected. These changes in epithelium lead to the clinical signs of<br />
placental degeneration, xerophthalmia, and corneal changes.<br />
Experimental vitamin A deficiency in lambs results in changes in the epithelium of the small<br />
intestine characterized by vesicular microvillar degeneration and disruption of the capillary<br />
endothelium (10). Diarrhea did not occur.<br />
Embryological development<br />
Vitamin A is essential for organ formation during growth of the fetus. Multiple congenital defects<br />
occur in pigs and rats, and congenital hydrocephalus in rabbits on maternal diets deficient in<br />
vitamin A. In pigs, administration of the vitamin to depleted sows before the 17th day of gestation<br />
prevented the development of eye lesions but administration on the 18th day failed to do so. A<br />
maternal deficiency of vitamin A in cattle can result in congenital hypovitaminosis-A in the calves,<br />
characterized by blindness with dilated pupils, nystagmus, weakness, and incoordination.<br />
Constriction of the optic canal with thickening of the dura mater results in ischemic necrosis of the<br />
optic nerve and optic disc edema resulting in blindness. Retinal dysplasia also occurs. Thickening<br />
of the occipital and sphenoid bones and doming of the frontal and parietal bones with compression<br />
of the brain also occur. Dilated lateral ventricles may be present and associated with increased<br />
CSF pressure.<br />
Immune mechanisms<br />
The effects of vitamin A andβ-carotene on host defense mechanisms have been uncertain and<br />
controversial for many years (11). Some workers claim that the incidence and severity of bacterial,<br />
viral, ricketssial, and parasitic infections are higher in vitamin A-deficient animals (11). It is<br />
possible that vitamin A and β-carotene afford protection against infections by influencing both<br />
specific and non-specific host defense mechanisms. The protective effect of vitamin A may be<br />
56
mediated by enhanced polymorphonuclear neutrophil function but this effect is also influenced by<br />
the physiological status of the animal such as lactation status in dairy cattle (12). Experimentally,<br />
a severe vitamin A deficiency in lambs is associated with alterations in immune function, but the<br />
exact mechanism is unknown (13).<br />
CLINICAL FINDINGS<br />
In general, similar syndromes occur in all species, but because of species differences in tissue and<br />
organ response, some variations are observed. The major clinical findings are set out below.<br />
Night blindness<br />
Inability to see in dim light (twilight or moonlit night) is the earliest sign in all species, except in<br />
the pig in which it is not evident until plasma vitamin A levels are very low. This is an important<br />
diagnostic sign.<br />
Xerophthalmia<br />
True xerophthalmia, with thickening and clouding of the cornea, occurs only in the calf. In other<br />
species a thin, serous mucoid discharge from the eyes occurs,followed by corneal keratinization,<br />
clouding, and sometimes ulceration and photophobia.<br />
Changes in the skin<br />
A rough, dry coat with a shaggy appearance and splitting of the bristle tips in pigs is characteristic,<br />
but excessive keratinization, such as occurs in cattle poisoned with chlorinated naphthalenes, does<br />
not occur under natural conditions of vitamin A deficiency. Heavy deposits of branlike scales on<br />
the skin are seen in affected cattle. Dry, scaly hooves with multiple, vertical cracks are another<br />
manifestation of skin changes and are particularly noticeable in horses. A seborrheic dermatitis<br />
may also be observed in deficient pigs but is not specific to vitamin A deficiency.<br />
Body weight<br />
Under natural conditions a simple deficiency of vitamin A is unlikely to occur and the emaciation<br />
commonly attributed to vitamin A deficiency may be largely due to multiple deficiencies of<br />
protein and energy. Although inappetence, weakness, stunted growth, and emaciation occur under<br />
experimental conditions of severe deficiency, in field outbreaks, severe clinical signs of vitamin A<br />
deficiency are often seen in animals in good condition. Experimentally, sheep maintain their body<br />
weight under extreme deficiency conditions and with very low-plasma vitamin A levels.<br />
Reproductive effcyicien<br />
Loss of reproductive function is one of the major causes of loss in vitamin A deficiency. Both the<br />
male and female are affected. In the male, libido is retained but degeneration of the germinative<br />
epithelium of the seminiferous tubules causesreduction in the number of motile, normal<br />
spermatozoa produced. In young rams, the testicles may be visibly smaller than normal. In the<br />
female, conception is usually not interfered with, but placental degeneration leads to abortion and<br />
the birth of dead or weak young. Placental retention is common.<br />
Nervous system<br />
Signs related to damage of the nervous system include:<br />
Paralysis of skeletal muscles due to damage of peripheral nerve roots<br />
•Encephalopathy due to increased intracranial pressure<br />
•Blindness due to constriction of the optic nerve canal.<br />
These defects occur at any age but most commonly in young, growing animals and they have<br />
been observed in all species except horses.<br />
Paralysis<br />
57
The paralytic form is manifested by abnormalities of gait due to weakness and incoordination. The<br />
hindlegs are usually affected first and the forelimbs later. In pigs, there may be stiffness of the legs,<br />
initially with a stilted gait or flaccidity, knuckling of the fetlocks, and sagging of the hindquarters.<br />
Complete limb paralysis occurs terminally.<br />
Convulsions<br />
Encephalopathy, associated with an increase in CSF pressure, is manifested by convulsions, which<br />
are common in beef calves at 6-8 months, usually following removal from a dry summer pasture<br />
at weaning time. Spontaneously, or following exercise or handling, affected calves will collapse<br />
(syncope) and during lateral recumbency a clonic-toinc convulsion will occur, lasting for 10-30<br />
seconds. Death may occur during the convulsion or the animal will survive the convulsion and lie<br />
quietly for several minutes, as if paralyzed, before another convulsion may occur. Affected calves<br />
are usually not blind and the menace reflex may be slightly impaired or hyperactive. Some calves<br />
are hyperesthetic to touch and sound. During the convulsion there is usually ventroflexion of the<br />
head and neck, sometimes opisthotonos and, commonly, tetanic closure of the eyelids and<br />
retraction of the eyeballs. Outbreaks of this form of hypovitaminosis-A in calves have occurred<br />
and the case fatality rate may reach 25% (7). The prognosis is usually excellent; treatment will<br />
effect a cure in 48 hours but convulsions may continue for up to 48 hours following treatment.<br />
Seizures and acute death attributable to hypovitaminosis-A and hypovitaminosis-D have<br />
occurred in feeder pigs fed ground red wheat and whole milk and housed in a barn with no<br />
exposure to sunlight (14). Lethargy, inappetence, diarrhea and vomiting, and progression to<br />
convulsions were characteristic.<br />
Blindness<br />
The ocular form of hypovitaminosis-A occurs usually in yearling cattle (12-18 months old) and up<br />
to 2-3 years of age. These animals have usually been on marginally deficient rations for several<br />
months. Night blindness may or may not have been noticed by the owner. The cattle have usally<br />
been fed and housed for long periods in familiar surroundings, and the clinical signs of night<br />
blindness may have been subtle and not noticeable. The first sign of the ocular form of the disease<br />
is blindness in both eyes during daylight. Both pupils are widely dilated and fixed and will not<br />
respond to light. Optic disc edema may be prominent and there may be some loss of the usual<br />
brilliant color of the tapetum. Varying degrees of peripapillary retinal detachment, papillary and<br />
peripapillary retinal hemorrhages, and disruption of the retinal pigment epithelium may also be<br />
present (4). The menace reflex is usually totally absent, but the palpebral and corneal reflexes<br />
are present. The animal is aware of its surroundings and usually eats and drinks, unless placed in<br />
unfamiliar surroundings. The CSF pressure is increased in these animals, but not as high as in the<br />
calves described earlier. Convulsions may occur in these cattle if forced to walk, or if loaded onto<br />
a vehicle for transportation. The prognosis for the ocular form with blindness is unfavorable and<br />
treatment is ineffective because of the degeneration of the optic nerves. Exophthalmos and<br />
excessive lacrimation are present in some cases.<br />
Congenital defects<br />
These have been observed in piglets and calves. In calves, the defects are limited to congenital<br />
blindness due to optic nerve constriction and encephalopathy. In piglets, complete absence of the<br />
eyes (anophthalmos), or small eyes (microphthalmos), incomplete closure of the fetal optic<br />
fissure, degenerative changes in the lens and retina, and an abnormal proliferation of<br />
mesenchymal tissue in front of and behind the lens are some of the defects encountered. Other<br />
58
congenital defects attributed to vitamin A deficiency in pigs include cleft palate and harelip,<br />
accessory ears, malformed hindlegs, subcutaneous cysts, abnormally situated kidneys,<br />
cardiac ,defects, diaphragmatic hernia, aplasia of the genitalia, internal hydrocephalus, herniations<br />
of the spinal cord, and generalized edema.<br />
Affected pigs may be stillborn, or weak and unable to stand, or may be quite active. Weak pigs lie<br />
on their sides, make slow paddling movements with their legs and squawk plaintively.<br />
Other diseases<br />
Increased susceptibility to infection is often stated to result from vitamin A deficiency (7, 11). The<br />
efficacy of colostrum as a preventive against diarrhea in calves was originally attributed to its<br />
vitamin A content, but the high antibody content of colostrum is most important.<br />
CLINICAL PATHOLOGY<br />
Plasma vitamin A<br />
Vitamin A levels in the plasma are used extensively in diagnostic and experimental work. Plasma<br />
levels of 20 µg/dL are the minimal concentration for vitamin A adequacy (15). Papilledema is an<br />
early sign of vitamin A deficiency which develops before nyctalopia and at plasma levels below<br />
18µg/dL. Normal serum vitamin A concentrations in cattle range from 25 to 60 µg/dL. In pigs,<br />
levels of 11.0 µg/dL have been recorded in clinical cases, with normal levels being 23-29 µg/dL<br />
(14). In experimental vitamin A deficiency in lambs, serum levels declined to 6.8 µg/dL (normal<br />
lambs at 45.1 µg/dL) (10).<br />
The clinical signs may correlate with the scrum concentrations of vitamin A (6). In one<br />
outbreak, feedlot cattle with serum concentrations between 8.89 and 18.05 µg/dL had only lost<br />
body weight, those between 4.87 and 8.88 µg/dL had varying degrees of ataxia and blindness, and<br />
those below 4.88 µg/dL had convulsions and optic nerve constriction (6). Clinical signs can be<br />
expected when the levels fall to 5 µg/dL (7). For complete safety, optimum levels should be<br />
25µg/dL. or above.<br />
Plasma retinol<br />
Some information on the plasma retinol values in stabled Thoroughbred horses is available. The<br />
mean plasma level of retinol in 71 horses 2-3 years of age was 16.5µg/dL. The serum retinol<br />
levels in racing Trotters in Finland are lower than during the summer months, which is a reflection<br />
of the quality of the diets (16).<br />
Plasma carotene<br />
Plasma carotene levels vary largely with the diet. In cattle, levels of 150µg/dL are<br />
optimum and, in the absence of supplementary vitamin A in the ration, clinical signs appear when<br />
the levels fall to 9 µg/dL. In sheep, carotene is present in the blood in only very small amounts<br />
even when animals are on green pasture.<br />
Hepatic vitamin A<br />
A direct relationship between plasma and hepatic levels of vitamin A need not exist since plasma<br />
levels do not commence to fall until the hepatic stores are depleted. A temporary precipitate fall<br />
occurs at parturition and in acute infections in most animals. The secretion of large amounts of<br />
carotene and vitamin A in the colostrum of cows during the last 3 weeks of pregnancy may greatly<br />
reduce the level of vitamin A in the plasma.<br />
Hepatic levels of vitamin A and carotene can be estimated in the living animal from a biopsy<br />
specimen. Biopsy techniques have been shown to be safe and relatively easy, provided a proper<br />
instrument is used. Hepatic levels of vitamin A and carotene should be of the order of 60 and 4.0<br />
59
µg/g of liver, respectively. These levels are commonly as high as 200-800 µg/g. Critical levels at<br />
which signs are likely to appear are 2 and 0.5 µg/g for vitamin A and carotene, respectively.<br />
Cerebrospinal fluid<br />
CSF pressure is also used as a sensitive indicator of low vitamin A status. In calves, normal<br />
pressures of less than 100 mm of saline rise after depletion to more than 200 mm. In pigs, normal<br />
pressures of 80-145 mm rise to above 200 mm in vitamin A deficiency. An increase in pressure is<br />
observed at a blood level of about 7 µg vitamin A/dL plasma in this species. In sheep, normal<br />
pressures of 55-65 mm rise to 70-150 mm when depletion occurs. In the experimentally induced<br />
disease in cattle, there is a marked increase in the number of cornified epithelial cells in a<br />
conjunctival smear and distinctive bleaching of the tapetum lucidum as viewed by an<br />
ophthalmoscope. These features may have value as diagnostic aids in naturally occurring cases.<br />
NECROPSY FINDINGS<br />
Gross changes are rarely observed at necropsy. Careful dissection may reveal a decrease in the<br />
size of the cranial vault and of the vertebrae. Compression and injury of the cranial and spinal<br />
nerve roots, especially the optic nerve, may be visible. In outbreaks in which night blindness is the<br />
primary clinical sign, atrophy of the photoreceptor layer of the retina is evident histologically, but<br />
there are no gross lesions.<br />
Squamous metaplasia of the interlobular ducts of the parotid salivary gland is strongly<br />
suggestive of vitamin A deficiency in pigs, calves and lambs, but the change is transient and may<br />
have disappeared 2-4 weeks after the intake of vitamin A is increased. This microscopic change is<br />
most marked, and occurs first, at the oral end of the main parotid duct. Abnormal epithelial cell<br />
differentiation may also be observed histologically in a variety of other sites such as the tracheal,<br />
esophageal and ruminal mucosae, preputial lining, pancreatic ducts, and urinary epithelium.<br />
Hypovitaminosis-A has also been associated with an increased incidence of pituitary cysts in cattle.<br />
Secondary bacterial infections, including pneumonia and otitis media, are also common, due at<br />
least in part to the decreased barrier function of the lining epithelia.<br />
The abnormalities that occur in congenitally affected pigs have already been described.<br />
Samples for confirmation of diagnosis<br />
• Toxicology - 50 g liver, 500 g teed ASSAY (Vit A)<br />
• Histology - formalin-fixed parotid salivary gland (including duct), rumen, pituitary, pancreas,<br />
brain (including optic nerves), cervical spinal cord (including nerve roots); Bouin's-fixed eye<br />
(LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
When the characteristic clinical findings of vitamin A deficiency are observed a deficiency of the<br />
vitamin should be suspected if green feed or vitamin A supplements are not being provided. The<br />
detection of papilledema and testing for night blindness are the easiest methods of diagnosing<br />
early vitamin A deficiency in ruminants. Incoordination, paralysis, and convulsions are the early<br />
signs in pigs. Increase in CSF pressure is the earliest measurable change in both pigs and calves.<br />
Laboratory confirmation depends upon estimations of vitamin A in plasma and liver, the latter<br />
being most satisfactory. Unless the disease has been in existence for a considerable time, response<br />
to treatment is rapid. For confirmation at necropsy, histological examination of parotid salivary<br />
gland, and assay of vitamin A in the liver, are suggested.<br />
The salient features of the differential diagnosis of diseases of the nervous system of cattle are<br />
summarized in Table 88.<br />
60
Cattle<br />
Convulsive form of vitamin A deficiency in cattle must be differentiated from:<br />
• Polioencephalomalacia – characterized by sudden onset of blindness, head-pressing and<br />
tonic-clonic convulsions, usually in grain-fed animals but also in pastured animals ingesting an<br />
excess of sulfate in water and grass<br />
• Hypomagnesemic tetany - primarily in lactating dairy cattle on pasture during cool windy<br />
weather; characterized by hyperesthesia, champing tonic-clonic convulsions, normal eyesight, and<br />
tachycardia and loud heart sounds<br />
• Lead poisoning - in all age groups, but most commonly in pastured calves in the spring;<br />
characterized by blindness, tonic-clonic convulsions, champing of the jaw, head-pressing, and<br />
rapid death<br />
• Rabies - in all age groups; characterized by bizarre mental behavior, gradually progressive<br />
ascending paralysis with ataxia leading to recumbency, drooling saliva, inability to swallow,<br />
normal eyesight, and death in 4-7 days.<br />
Ocular form of vitamin A deficiency in cattle must be differentiated from those diseases of<br />
cattle characterized by central or peripheral blindness:<br />
• Central blindness:<br />
Polioencephalomalacia<br />
Lead poisoning<br />
Meningoencephalitis<br />
• Peripheral blindness:<br />
Bilateral ophthalmitis due to ocular disease.<br />
Loss of body condition in cattle, failure to grow and poor reproductive efficiency are general<br />
clinical findings not limited to vitamin A deficiency.<br />
Swine<br />
Convulsive form of vitamin A deficiency in pigs must be differentiated from:<br />
• Salt poisoning<br />
• Pseudorabies<br />
• Viral encephalomyelitis<br />
• Organic arsenic poisoning.<br />
Paralytic form of vitamin A deficiency in pigs must be differentiated from:<br />
• Spinal cord compression due to vertebral body abscess.<br />
Congenital defects similar to those caused by vitamin A deficiency may be caused by deficiencies<br />
of other essential nutrients, by inheritance or by viral infections in early pregnancy in all species.<br />
Maternal vitamin A deficiency is the most common cause of congenital defects in piglets. Final<br />
diagnosis depends upon the necropsy findings, analysis of feed, and serum vitamin A of the dams.<br />
TREATMENT<br />
Vitamin A<br />
Animals with curable vitamin A deficiency should be treated immediately with vitamin A at a dose<br />
rate equivalent to 10-20 times the daily maintenance requirement. As a rule, 440 IU/kg BW is the<br />
dose used. Parenteral injection of an aqueous rather than an oily solution is preferred. The<br />
response to treatment in severe cases is often rapid and complete, but the disease may be<br />
irreversible in chronic cases. Calves with the convulsive form due to increased CSF pressure will<br />
usually return to normal in 48 hours following treatment. Cattle with the ocular form of the<br />
61
deficiency and that are blind will not respond to treatment and should be slaughtered for salvage.<br />
Hypervitaminosis-A<br />
Daily heavy dosing (about 100 times normal) of calves causes reduced growth rate, lameness,<br />
ataxia, paresis, exostoses on the planter aspect of the third phalanx of the fourth digit of all feet,<br />
and disappearance of the epiphyseal cartilage. Persistent heavy dosing in calves causes lameness,<br />
retarded horn growth, and depressed CSF pressure. At necropsy, exostoses are present on the<br />
proximal metacarpal bones and the frontal bones are thin. Very high levels fed to young pigs may<br />
cause sudden death through massive internal hemorrhage, and excessive doses during early<br />
pregnancy are reputed to result in fetal anomalies. However, feeding vitamin A for prolonged<br />
periods at exceptionally high levels is unlikely to produce severe embryotoxic or teratogenic<br />
effects in pigs.<br />
CONTROL<br />
Dietary requirement<br />
The minimum daily requirement in all species is 40 IU of vitamin A/kg BW,<br />
<br />
Table 29.9 Daily dietary allowances of vitamin A<br />
Animal<br />
Cattle<br />
Growing calves<br />
Weaned beef calves at 6-8 months<br />
Calves 6 months to yearlings<br />
Maintenance and pregnancy<br />
Maintenance and lactation<br />
Feedlot cattle on high energy ration<br />
Sheep<br />
Growth and early pregnancy and fattening lambs<br />
Late pregnancy and lactation<br />
Pigs<br />
Growing pigs<br />
Pregnant gilts and sows<br />
Lactating gilts and sows<br />
Horses<br />
Working horse<br />
Growing horse<br />
Pregnant mare<br />
Lactating mare<br />
Vitamin A<br />
(IU/kg BW daily)<br />
40<br />
40<br />
40<br />
70-80<br />
80<br />
80<br />
30-40<br />
70-80<br />
40-50<br />
40-50<br />
70-80<br />
20-30<br />
which is a guideline for maintenance requirements. In the formulation of practical diets for all<br />
species, the daily allowances of vitamin A are commonly increased by 50-100% of the daily<br />
minimum requirements. During pregnancy, lactation, or rapid growth the allowances are usually<br />
increased by 50-75% of the requirements. The supplementation of diets to groups of animals is<br />
governed also by their previous intake of the vitamin and its probable level in the diet being fed.<br />
The rate of supplementation can vary from 0 to 110 IU/kg BW/d (1 IU of vitamin A is equivalent<br />
62<br />
40<br />
50<br />
50
in activity to 0.3 µg of retinol; 5-8 µg β-carotene has the same activity as 1 µg of retinol).<br />
The amounts of the vitamin to be added to the ration of each species to meet the requirements<br />
for all purposes should be obtained from published recommended nutrient requirements of<br />
domestic animals. Some examples of daily allowances of vitamin A for farm animals are set out in<br />
Table 29.9.<br />
Supplementation method<br />
The method of supplementation will vary depending on the class of livestock and the ease with<br />
which the vitamin can be given. In swine, the vitamin is incorporated directly into the complete<br />
ration, usually through the protein supplement. In feedlot and dairy cattle receiving complete<br />
feeds, the addition of vitamin A to the diet is simple. In beef cattle, which may be fed primarily<br />
on carotene-deficient roughage during pregnancy, it may not be possible to supplement the diet on<br />
a daily basis. However, it may be possible to provide a concentrated dietary source of vitamin A<br />
on a regular basis by feeding a protein supplement once weekly. The protein supplement will<br />
contain 10-15 times the daily allowance, which permits hepatic storage of the vitamin.<br />
Parenteral injection<br />
An alternative method to dietary supplementation is the IM injection of vitamin A at intervals of<br />
50-60 days at the rate of 3000-6000 IU/kg BW. Under most conditions, hepatic storage is good,<br />
and optimum plasma and hepatic levels of vitamin A are maintained for up to 50-60 days. In<br />
pregnant beef cattle the last injection should not be more than 40-50 days before parturition to<br />
insure adequate levels of vitamin A in the colostrum. Ideally, the last injection should be given 30<br />
days before parturition but this may not be practical under some management conditions. However,<br />
the most economical method of supplementing vitamin A is, in most cases, through the feed and<br />
when possible should be used.<br />
The use of injectable mixtures of vitamins A, D, and E is not always justifiable. The injection of<br />
a mixture of vitamins A, D, and E of feeder cattle in northern Australia prior to transport did not,<br />
contrary to anectodal evidence, reduce weight loss associated with transportation (17). Cattle in<br />
Queensland and north-western Australia have very high concentrations of hepatic vitamin A, and<br />
in fact, droughtstricken cattle in the terminal stages of malnutrition have also had high liver<br />
concentration. The indiscriminate use of vitamin A preparations in cattle is a public health concern<br />
because some bovine livers may contain high levels of vitamin A which are potentially teratogenic<br />
for pregnant women (18).<br />
Oral vitamin A<br />
The oral administration of a single bolus of vitamin A at a dose of 2.8 mg/kg BW to debilitated<br />
Sahelian cattle during the dry season was effective in raising the milk levels of vitamin A and was<br />
as effective as adding 10 g of the powder to the drinking water (2). Both the powder and bolus<br />
products provided high levels of vitamin A in milk within 3 days of treatment, and according to<br />
herder testimonials, night-blind people consuming milk from cattle previously treated with either<br />
oral vitamin A preparation were no longer affected with night blindness.<br />
REFERENCES<br />
(1)Molokwu, E. C. 1. (1978) Hr. Vet.J., 134,<br />
493.<br />
(2)Remillard, R L. et al. (1990) Prcv. Vet.<br />
Med., 9, 173.<br />
(3)van der Lugt.J.J. & Prozesky, L. (1989)<br />
63
Onderstepoorl.J. Vet. Res., 56, 99.<br />
(4)Divers, T.J. et al. (1986) J. Am. Vet. Med.<br />
Assoc, 189, 1579.<br />
(5)Paulson, M. E. et al. (1989) J. Am. Vet.<br />
Med. Assoc, 194, 933.<br />
(6)Booth, A. et al. (1987) J. Am. Vet. Med.<br />
Assoc, 190, 1305.<br />
(7)Sustronck, B. et al. (1993) V\aams Dietgen.<br />
Tijdschrifi. 62. 95.<br />
(8)Salum, M. R. & Njavike, S. M. (1993)<br />
Bull. Anim. Health. Prod. Africa, 41, 163.<br />
(9)Doige, C. E. & Schoonderwoerd, M.<br />
(1988) J. Am. Vet. Med. Assoc, 193, 691.<br />
(10)Holland, R. E. et al. (1993) Dig. Dis. Sci.,<br />
38, 333.<br />
(11)Chew, B. P. (1987) /. Dairy Sci., 70, 2732.<br />
(12)Tjoelker, L W. et al. (1988) J. Dairy Sci.,<br />
71, 3112,3120.<br />
(13)Bruns, N.J. & Webb, K. E.Jr. (1990) J.<br />
Anim. Sci., 68, 454.<br />
(14)LakntzJ. et al. (1993)J. Am. Vet. Med.<br />
Assoc, 202, 1276.<br />
(15)Chew, B P. et al. (1984) J. Dairy Sri., 67,<br />
1316.<br />
(16)Maepaa, P. H. et al. (1987) Equine Vet.J.,<br />
19, 237.<br />
(17)Jubb, T. H. et al. (1993) Aust. Vet.J., 70,<br />
171.<br />
(18)RutterJ. M. (1990) Vet. Rec, 127, 433.<br />
二、维生素 D 营养紊乱性疾病(Nutritional Disorder of Vitamine D)<br />
(一)维生素 D 缺乏症(Vitamin D deficiency)<br />
动物因长期关禁饲养缺乏阳光照射,或因饲料中缺乏VD,或因饲料中抗维生素D物质过<br />
多,引起动物VD缺乏症。临床上患病动物表现食欲下降,生长阻滞,严重时产生骨骼病变。<br />
幼年动物发生佝偻病,成年动物发生骨软症或骨纤维性营养不良。<br />
各种动物都可出现VD缺乏症,以幼年动物最易发生。<br />
【病因】 维生素D是固醇类衍生物,天然的VD有VD2、VD3。VD2主要来自植物,是植<br />
物中麦角固醇经紫外线照射后产生的,又称麦角钙化醇(ergocalciferol或vioerol)。商品VD2是<br />
用紫外线照射酵母菌而生产的。<br />
VD3是哺乳动物皮肤中 7-脱氢胆固醇经紫外线照射后而产生的,又称胆钙化醇<br />
(chole-calciferol)。<br />
VD4、VD5天然存在于某些鱼的脂肪中,作用不明。<br />
VD2、VD3实际上是前体维生素;它被吸收后需要在肝内先转化为 25-(OH)胆钙化醇<br />
(25-OHCC)后,与血液中α2-球蛋白结合,经血液运送到肾,在肾脏内转化为 1,25-(OH)<br />
2胆钙化醇(1,25-(OH)2CC)后,再与α2-球蛋白结合并运往靶组织,调节钙的吸收,转<br />
64
运与动员。<br />
因此当动物长期关禁饲养或冬天阳光不足,缺乏紫外线照射时,体内合成的VD3过少,<br />
则可能产生VD缺乏。长期以幼嫩饲料饲喂,牧草中VD2含量少,也可产生VD缺乏。<br />
VD在肠道吸收,在肝、肾内-羟化酶作用下才能转变为它的代谢活性产物 1,25-(OH)<br />
2CC。因此当长期拉稀,肝、肾功能衰竭,亦可造成VD缺乏。<br />
幼年动物对VD需要量较大,而且其主要来源于乳和皮肤内合成。因此,如母乳中VD含<br />
量不足或缺乏,或用代乳品饲喂,其中缺乏VD时,亦可造成VD缺乏。<br />
VD2的活性代谢产物 1,25-(OH)2麦角固醇的生物学活性仅为VD3的代谢物l,25-(OH)<br />
2CC的 1/5~1/10,因此雏禽饲料中,必须添加VD3,才能防止雏禽佝偻病。<br />
当饲料中Ca:P偏离正常比率(1:1~2:1)太远,对VD的需要量增加,如未能恰当补充VD亦<br />
可造成VD缺乏症。<br />
饲料中VA与VD是拮抗的,粗老植物中VD含量较高,幼嫩植物中VA含量较高,当VA或胡<br />
萝卜素含量太多,可干扰和阻碍VD的吸收,甚至酿成VD缺乏。<br />
【病理】 VD及其活性代谢产物与钙的吸收、定向运动和动员关系密切。有人认为它<br />
相当于一种激素,是和降钙素(calcitonin)、甲状旁腺素(parathyroidin)一样,作为第三种<br />
激素调节钙、磷代谢。在肾脏内完成其代谢活性产物转化后的 1,25-(OH)2CC与血浆α2球<br />
蛋白结合,转运到靶器官。如小肠、肾小管、骨骼,可能还有甲状旁腺,产蛋母鸡的生壳腺<br />
(shell gland),并发挥对钙、磷代谢的调节作用。VD对钙、磷代谢的调节作用表现在下述 3<br />
方面:<br />
1。促进小肠近端对钙的吸收,远端对磷的吸收 对钙吸收的促进作用首先表现在促进钙<br />
结合蛋白(CaBP)的合成,游离的 1,25-(OH)2CC可穿透肠黏膜靶细胞膜,结合到细胞<br />
浆的受体上,随后这种复合物转入细胞核,再结合到核染色质的特异性受体上,通过信使<br />
RNA合成,刺激基因表达并合成钙依赖性蛋白质CaBP和钙-ATP酶。肠黏膜细胞的纤毛上(刷<br />
状缘)含有大量的钙依耐性酶,例如Ca-ATP酶碱性磷酸酶,它们与CaBP一道有专性捕获肠<br />
腔中Ca 2+ 并使Ca 2+ 从低浓度的肠腔内向高浓度的细胞浆内转移,并在基底膜上与血浆中的钠<br />
离子交换以后入血,再与α球蛋白结合后使Ca 2+ 在血浆内运输,在肠黏膜细胞内,VD可促使<br />
钙只能从肠腔向肠黏膜基底部传递的定向运动。<br />
2。促进肾小管对钙的吸收 肾小管上皮细胞也可合成CaBP,可使原尿中Ca 2+ 重新吸收<br />
入血,这一作用是在 1,25-(OH)2CC作用下产生的。<br />
3。促进骨骼中Ca 2+ 的运动 骨细胞也是 1,25-(OH)2CC的靶细胞。近年来研究证实:<br />
在骨松质(spongiosa)和软骨生长板(cartilaginous growth plate)内也有VD依耐性CaBP,在<br />
年轻动物,其骨骼的有序生长和软骨生长板的矿化作用中需要 1,25-(OH)2CC。在缺乏<br />
VD时软骨生长板内的软骨细胞线粒体上的矿化质粒(mineral granules)上没有Ca 2+ 积聚,软<br />
骨基质中不产生矿化作用,因而骺端软骨肥大,无规则地增厚。而 25-(OH)CC;1,25-<br />
(OH)2CC可使这一现象重归有序化,并在骨表面形成钙化作用(calcification).<br />
对成年动物,VD又可使破骨细胞活跃,使钙从骨骼中重吸收。破骨细胞对甲状旁腺素<br />
的反应必须要有少量VD及其活性代谢产物参予。大剂量的VD及其代谢产物,可刺激破骨细<br />
胞增生,随之产生骨骼重吸收作用。1,25-(OH)2CC对刺激骨骼重吸收的强度是 25-(OH)<br />
CC的 100 倍。猫长期大量喂给鱼肝,其它动物补充VD过多可造成骨疏松和钙的异位沉着,<br />
如产生肾结石、胆结石等。<br />
由此可见,VD有促进钙磷吸收作用,保证血液中钙、磷浓度相对稳定,促进幼年动物<br />
钙、磷向骨骼中沉积作用。<br />
相反,VD缺乏则可引起肠道对钙、磷的吸收率下降,血浆钙磷浓度降低,促使甲状旁<br />
腺分泌,骨骼钙盐重溶,因而产生骨软症或纤维性骨营养不良;幼畜VD缺乏时,由于骨骼<br />
65
矿化不足,软骨肥大,骨变形。同时幼畜生长迟缓,产生佝偻病的各种症状。<br />
【临床表现】 幼年动物VD缺乏可产生佝偻病,症状详见佝偻病。最明显的表现是软<br />
骨肥大,骨变形,胸廓狭窄,肋骨与肋软骨处形成球状肿胀,呈串珠状排列,脊柱变形,四<br />
肢骨呈内弧或外弧状;禽胸骨脊呈S状弯曲。喙软,有橡皮喙之称。胫跗骨可微微弯曲,易<br />
折断。<br />
成年动物缺乏VD,可发生骨软症,或纤维性骨营养不良,成年鸡产薄壳蛋或软壳蛋,<br />
继则产蛋减少,蛋孵化率降低。<br />
VD缺乏时,早期血磷浓度降低,后期血钙浓度降低,AKP活性升高。<br />
【诊断】 本病根据常年舍饲,饲料中又未添加或添加的VD量不足,并配合骨骼变<br />
形,肋骨与肋软骨交界处呈串珠状增大,有条件的用X线摄影技术发现有肥大的软骨和蛾蚀<br />
状骨端,AKP活性升高,可作出诊断。<br />
【防治】 首先应在查明病因的基础上,调整日粮组成。在饲料中添加VD3,增加户外<br />
活动和晒太阳时间可防止该病。<br />
药物治疗,一般补充鱼肝油或鱼肝油丸(浓缩鱼肝油),剂量按 4~6ml/l00kg体重,口服。<br />
VA、VD复合注射液。猪、驹、犊牛 2~4ml,仔猪、羔羊 0.5~1.0ml,肌肉注射。或按 275µg/kg<br />
体重剂量一次性肌肉注射,可保持动物在 3~6 个月内不至于引起VD缺乏症,每天口服量为<br />
0.5~1.1µg/kg体重,一次大量口服 50mg,可保持 2 个月内不缺VD。禽舍中安装紫外灯;从<br />
10 日龄开始,每天照射 10min,亦可防止VD缺乏。<br />
注意饲料中钙、磷比例保持在 1:1~2:1 之间。<br />
动物对VD的需要量是:牛,7.5µg/kg(干物质计);猪,生长期 5µg/kg,繁殖期 7µg<br />
/kg日粮;羔羊,3.75µg/kg,繁殖期,6~7.5µg/kg(干物质计);马,0.15~0.2µgkg体重;<br />
肉鸡,VD3,100µg/kg日粮;种鸡,37.5µg/kg 日粮;产蛋期,种鸡,75µg/kg日粮;火<br />
鸡 100µg/kg日粮。<br />
VITAMIN D DEFICIENCY<br />
VitaminD deficiencys usually caused by insufficient solar irradiationof animals or their feed and<br />
is manifested by poor appetiteand growth, and in advanced cases by osteodystrophy.<br />
Synopsis<br />
Etiology. Lack of ultravioletsolar irradiation and/or deficiency of preformed vitamin D in diet.<br />
Epidemiology. Uncommon because diets are supplemente. Occurs in animals in countries with<br />
relative lack of UV irradiation especially in winter months; animals raised indoors for long periods.<br />
May occur in young grazinganimals in winter months. May be antivitamin D factor.<br />
Signs. Reduced productivity; poor weight gain; reduced reproductive performance. Rickets in<br />
young; osteomalacia in adults.<br />
Clinical pathology. Serumcalcium and phosphorus. Plasma vitamin D.<br />
Lesions. Lack of mineralization of bone.<br />
Diagnostic confirmation. Histology of bone<br />
lesions.<br />
Differential diagnosis list. See Rickets and<br />
osteomalacia.<br />
Treatment. Administervitamin D parenterally and oral calcium and phosphates.<br />
Control. Supplement diets with vitamin D.Injections of vitamin D when oral supplementation not<br />
possible.<br />
ETIOLOGY<br />
A lack of ultraviolet solar irradiation of the skin, coupled with a deficiency of preformed vitamin<br />
66
D complex in the diet, leads to a deficiency of vitamin D in tissues.<br />
EPIDEMIOLOGY<br />
Although the effects of clinically apparent vitamin D deficiency have been largely eliminated by<br />
improved nutrition, the subclinical effects have received little attention. For example, retarded<br />
growth in young sheep in New Zealand and southern Australia during winter months has been<br />
recognized for many years as responding to vitamin D administration.<br />
However, general realization of the importance of this subclinical vitamin D deficiency in<br />
limiting productivity of livestock has come only in recent years. This is partly due to the<br />
complexity of the relations between calcium, phosphorus and the vitamin, and their common<br />
association with protein and other deficiencies in the diet. Much work remains to be done before<br />
these individual dietary-essentials can be assessed in their correct economic perspective.<br />
Ultraviolet irradiation<br />
The lack of ultraviolet irradiation becomes important as distance from the equator increases and<br />
the sun's rays are filtered and refracted by an increasing depth of the earth's atmosphere. Cloudy,<br />
overcast skies, smoke-laden atmospheres, and winter months exacerbate the lack of irradiation.<br />
The effects of poor irradiation are felt first by animals with dark skin (particularly swine and some<br />
breeds of cattle) or heavy coats (particularly sheep), by rapidly growing animals, and by those that<br />
are housed indoors for long periods. The concentration of plasma vitamin D3 recorded in grazing<br />
sheep varies widely throughout the year. During the winter months in the United Kingdom the<br />
levels in sheep fall below what is considered optimal, while in the summer months the levels are<br />
more than adequate (1). There is a marked difference in vitamin D status between sheep with a<br />
long fleece and those that have been recently shorn, especially in periods of maximum sunlight.<br />
The higher blood levels of vitamin D in the latter group are probably due to their greater exposure<br />
to sunlight. Pigs reared under intensive farming conditions and animals being prepared for shows<br />
are small but important susceptible groups.<br />
Dietary vitamin D<br />
The importance of dietary sources of preformed vitamin D must not be underestimated. Irradiated<br />
plant sterols with anti-rachitic potency occur in the dead leaves of growing plants. Variation in the<br />
vitamin D content of hay can occur with different methods of curing. Exposure to irradiation by<br />
sunlight for long periods causes a marked increase in anti-rachitic potency of the cut fodder,<br />
whereas modern haymaking technique with its emphasis on rapid curing tends to keep vitamin D<br />
levels at a minimum. Grass ensilage also contains very little vitamin D<br />
Based on a survey of the concentrations of vitamin D in the serum of horses m the United<br />
Kingdom, the levels may be low (2). In the absence of a dietary supplement containing vitamin D,<br />
the concentration of 25-OH D2 and 25-OH D3 are, respectively, a reflection of the absorption of<br />
vitamin D2 from the diet and of biosynthesis of vitamin D3<br />
Information on the vitamin D requirements of housed dairy cattle is incomplete and<br />
contradictor)'. It appears, however, that m some instances natural feedstuffs provide less than<br />
adequate amounts of the vitamin for optimum reproductive performance in high-producing cows<br />
(3).<br />
Grazing animals<br />
The grazing of animals, especially in winter time, on lush green feed including cereal crops, leads<br />
to a high incidence of rickets in the young. An antivitamin D factor is suspected because calcium,<br />
phos¬phorus, and vitamin D intakes are usually normal, but the condition can be prevented by the<br />
67
administration of calciferol. Carotene, which is present in large quantities in this type of feed, has<br />
been shown to have antivitamin D potency but the existence of a further rachitogenic substance<br />
seems probable. The rachitogenic potency of this green feed varies widely according to the stage<br />
of growth and virtually disappears when flowering commences. Experimental overdosing with<br />
vitamin A causes a marked retardation of bone growth in calves. Such overdosing can occur when<br />
diets are supplemented with the vitamin, and may produce clinical effects (4).<br />
The importance of vitamin D to animals is now well-recognized and supplementation of the diet<br />
where necessary is usually performed by the livestock owner. Occasional outbreaks of vitamin D<br />
deficiency are experienced in intensive systems where animals are housed and in areas where<br />
specific local problems are encountered, e.g. rickets in sheep on green cereal pasture in New<br />
Zealand.<br />
PATHOGENESIS<br />
Vitamin D is a complex of substances with anti-rachitogenic activity. The important components<br />
are as follows:<br />
•Vitamin D3 (cholecalciferol) is produced from its precursor 7-dehydro-cholesterol in mammalian<br />
skin and by natural irradiation with ultraviolet light<br />
•Vitamin D2 is present in sun-cured hay and is produced by ultraviolet irradiation of plant sterols.<br />
Calciferol or viosterol is produced commercially by theirradiation of yeast. Ergosterol is<br />
the :provitamin<br />
•Vitamin D4 and D5 occur naturally in the oils of some fish.<br />
Vitamin D produced in the skin or ingested with the diet and absorbed by the small intestine is<br />
transported to the liver. In the liver, 25-hydroxycholecalcif-erol is produced, which is then trans<br />
ported to the kidney where at least two additional derivatives are formed by 1-Ct-hydroxylase (5).<br />
One is 1,25-dihydroxycholecalciferol (DHCC), and the other is 24,25-DHCC. Under conditions of<br />
calcium need or calcium deprivation the form predominantly produced by the kidney is<br />
1,25-DHCC. At present it seems likely that 1,25-DHCC is the metabolic form of vitamin D most<br />
active in eliciting intestinal calcium transport ; and absorption and is at least the closest known<br />
metabolite to the form of vitamin D functioning in bone mineralization. The metabolite also<br />
functions in regulat- ing the absorption and metabolism of the phosphate ion, and especially its<br />
loss from the kidney. A deficiency of the metabolite may occur in animals with renal disease,<br />
resulting in decreased absorption of calcium and phosphorus, decreased mineralization of bone,<br />
and excessive losses of the minerals through the kidney. A deficiency of vitamin D per se is<br />
governed in its importance by the calcium and phosphorus status of the animal.<br />
Because of the necessity for the conversion of vitamin D to the active metabolites, there is a lag<br />
period of 2- 4 days following the administration of the vitamin parenterally before a significant<br />
effect on calcium and phosphorus absorption can occur. The use of synthetic-analogs of the active<br />
metabolites such as 1-α-hydroxycholecalciferol (an analog of 1,25-DHCC) can increase the<br />
plasma concentration of calcium and phosphorus within 12 hours following administration (6) and<br />
has been recommended for the control of parturient paresis in cattle.<br />
Maternal status<br />
Maternal vitamin D status is important m determining neonatal plasma calcium concentration. I<br />
here is a significant correlation between maternal and neonatal calf plasma concentrations of<br />
25-OH D2, 25-OH D3, 24,25-(OH)2, D2, 24,25-(OH)2, D3 and 25,26-(OH)2 D3. This indicates<br />
that the vitamin D metabolite status of the neonate is primarily dependent on the 25-OH D status<br />
68
of the dam (7). The maternal serum concentrations of calcium, phosphorus, and magnesium do not<br />
determine concentrations of these minerals found in the newborn calf. The ability of the placenta<br />
to maintain elevated plasma calcium or phosphorus in the fetus is partially dependent on maternal<br />
1,25-(OH)2, D status. Parenteral cholecalciferol treatment of sows before parturition is an<br />
effective method of supplementing neonatal piglets with cholecalciferol via the sow's milk and its<br />
metabolite via placenta transport (6).<br />
Calcium:phosphorus ratio<br />
When the calcium:phosphorus ratio is wider than the optimum (1:1 to 2:1), vitamin D<br />
requirements for good calcium and phosphorus retention and bone mineralization are increased. A<br />
minor degree of vitamin D deficiency in an environment supplying an imbalance of calcium and<br />
phosphorus might well lead to disease, whereas the same degree of vitamin deficiency with a<br />
normal calcium and phosphorus intake could go unsus¬pected. For example, in growing pigs,<br />
vitamin D supplementation is not essential provided calcium and phosphorus intakes are rigidly<br />
controlled, but under practical circumstances this may not be possible.<br />
The minor functions of the vitamin include maintenance of efficiency of food utilization and a<br />
calorigenic action, the metabolic rate being depressed when the vitamin is deficient. These actions<br />
are probably the basis for the reduced growth rate and productivity in vitamin D deficiency. Some<br />
evidence suggests that vitamin D may have a role in the immune system (8). Local production of<br />
1,25-(OH)2 D by monocytes may be important in the immune function, particularly in the<br />
parturient dairy cow.<br />
CLINICAL FINDINGS<br />
The most important effect of lack of vitamin D in farm animals is reduced productivity. A<br />
decrease in appetite and efficiency of food utilization cause poor weight gains in growing stock<br />
and poor productivity in adults. Reproductive efficiency is also reduced and the overall effect on<br />
the animal economy may be severe.<br />
In the late stages lameness, which is most noticeable in the forelegs, is accompanied in young<br />
animals by bending of the long bones and enlargement of the joints. This latter stage of clinical<br />
rickets may occur simultaneously with cases of osteomalacia in adults. An adequate intake of<br />
vitaminD appears to be necessary for the maintenance of fertility in cattle, particularly if the<br />
phosphorus intake is low. In one study in dairy cattle, the first ovulation after parturition was<br />
advanced significantly in vitamin D supplemented cows (3).<br />
CLINICAL PATHOLOGY<br />
Serum calcium and phosphorus<br />
A pronounced hypophosphatemia occurs m the early stages and is followed some months later by<br />
a fall in serum calcium. Plasma alkaline phosphatase levels are usually elevated. The blood picture<br />
quickly returns to normal with treatment, often several months before the animal is clinically<br />
normal. Typical figures for beef cattle kept indoors are serum calcium 8.7 mg/dL (10.8 normal),<br />
2.2 mmol/L (2.7 normal); serum inorganic phosphate 4.3 mg/dL (6.3 normal), 1.1 mmol/L (1.6<br />
normal); and alkaline phosphatase 5.7 units (2.75 normal).<br />
Plasma vitamin D<br />
The normal ranges of plasma concentrations of vitamin D and its metabolites in the farm animal<br />
species are now available (9) and can be used to monitor the response of the administration of<br />
vitamin D parenterally or orally in sheep (10, 11). The serum concentrations of vitamin I) in the<br />
horse have been determined (2).<br />
69
NECROPSY FINDINGS<br />
The pathological changes in young animals arc those of rickets, while in older animals there is an<br />
osteomalacia. In all ages a variable amount of osteodystrophcia fibrosa may develop, and<br />
distinction of the origin of these osteodystrophies based on only gross and microscopic<br />
examination is impractical. A review of management factors and a nutritional analysis of the feed<br />
is essential. The samples for confirmation of the diagnosis at necropsy are as per calcium<br />
deficiency.<br />
DIFFERENTIAL DIAGNOSIS<br />
A diagnosis of vitamin D deficiency depends upon evidence of the probable occurrence of the<br />
deficiency and response of the animal when vitamin D is provided. Differentiation from clinically<br />
similar syndromes is discussed under the specific osteodystrophies.<br />
TREATMENT<br />
It is usual to administer vitamin D in the dose rates set out under control. Affected animals should<br />
also receive adequate calcium and phosphorus in the diet.<br />
CONTROL<br />
Supplementation<br />
The administration of supplementary vitamin D to animals by adding it to the diet or by injection<br />
is necessary only when exposure to sunlight or the provision of a natural ration containing<br />
adequate amounts of vitamin D is impractical.<br />
A total daily intake of 7-12 IU/kg BW is optimal. Sun-dried hay is a good source, but green<br />
fodders are generally deficient in vitamin D. Fish liver oils arc-high in vitamin D, but are subject<br />
to deterioration on storage, particularly with regard to vitamin A. They have the added<br />
disadvantage of losing their vitamin A and 1) content in premixed feed, of destroying vitamin E in<br />
these feeds when they become rancid, and of seriously reducing the butterfat content of milk.<br />
Stable water-soluble vitamin A and D preparations do not suffer from these disadvantages.<br />
Irradiated dry yeast is probably a simpler and cheaper method of supplying vitamin D in mixed<br />
grain feeds.<br />
Stable water-soluble preparations of vitamin D are now available and are commonly added to<br />
the rations of animals being fed concentrate rations. The classes of livestock that usually need<br />
dietary supplementation include:<br />
•Calves raised indoors on milk replacers<br />
•Pigs raised indoors on grain rations<br />
•Beef cattle receiving poor quality roughage during the winter months<br />
•Cattle raised indoors for prolonged periods and not receiving sun-cured forage containing<br />
adequate levels of vitamin D. These include calves raised as herd replacements, yearling cattle fed<br />
concentrate rations, bulls in artificial insemination centers, and purebred bulls maintained indoors<br />
on farms<br />
•Feedlot lambs fed grain rations during the winter months or under totally covered confinement<br />
•Young growing horses raised indoors or outdoors on rations that may not contain adequate<br />
concentrations of calcium and phosphorus. This may be a problem in rapidly growing,<br />
well-muscled horses receiving a high level of grain.<br />
Because there is limited storage of vitaminD in the body, compared to the storage of vitamin A,<br />
it is recommended that daily dietary supplementation be provided when possible for optimum<br />
effect.<br />
70
Injection<br />
In situations where dietary supplementa¬tion is not possible, the use of single IM injections of<br />
vitamin D2 (calciferol) in oil will protect ruminants for 3-6 months. A dose of 1 1 000 units/kg<br />
BW is recommended and should maintain an adequate vitamin D status for 3-6 months.<br />
In mature non-pregnant sheep weighing about 50 kg, a single IM injection of 6000 IU/kg body<br />
weight produced concentrations of 25-hydroxyvitamin D3 at adequate levels for 3 months (11).<br />
The parenteral administration of vitamin D,results in both higher tissue and plasma levels of<br />
vitamin D3 than does oral administration, and IV administration produces higher plasma levels<br />
than does the IM injection (12). The timing of the injection should be selected so that the vitamin<br />
D status of the ewe is adequate at the time of lambing (11). The vitamin D3 status of lambs can be<br />
increased by the parenteral administration of the vitamin to the pregnant ewe (13). Dosing<br />
pregnant ewes with 300000 IU of vitamin D3 in a rapidly available form, approximately 2 months<br />
before lambing, provides a safe means of increasing the vitamin D status of the ewe and the<br />
newborn lambs by preventing seasonally low concentrations of 25-hydroxyvitamin D3 (14). In<br />
adult sheep there is a wide margin of safety between the recommended requirement and the toxic<br />
oral dose, which provides ample scope for safe supplementation if such is desirable (10). In adult<br />
sheep given 20 times the recommended requirements for 16 weeks there was no evidence of<br />
pathological cification (10). Oral dosing with 30-45 units/kg BW is adequate, provided treatment<br />
can be given daily. Massive oral doses can also be used to give long-term effects, e.g. a single<br />
dose of 2 million units is an effective preventive for 2 months in lambs. Excessive doses may<br />
cause toxicity, with signs of drowsiness, muscle weakness, fragility of bones, and calcification in<br />
the walls of blood vessels. The latter finding has been recorded in cattle receiving 10 million units<br />
per day and in unthrifty lambs receiving a single dose of 1 million units, although larger doses are<br />
tolerated by healthy lambs.<br />
REVIEW LITERATURE<br />
Dobson, R. C. & Ward, G. (1974) Vitamin Dphysiology and its importance to dairy cattle:a<br />
review. J. Dairy Sci., 57, 985.<br />
Horst, R. L. & Reinhardt, T. A. (1983) Vitamin<br />
D metabolism in ruminants and its relevance<br />
to the periparturient cow.J. Dairy Sci., 66,<br />
661-678.<br />
Wasserman, R. H. (1975) Metabolism, function<br />
and clinical aspects of vitamin D. Cornell<br />
Vet., 65, 3.<br />
REFERENCES<br />
(1)Smith, B. S. W. & Wright, H. (1984) Vet..Rec, 115.537.<br />
(2)Smith, B. S. W. & Wright, H. (1984) Vet.Rec, 115. 579.<br />
(3)Ward, G. et al. (1971)J. Dairy Sci., 54, 204.<br />
(4)Grey, R. M. et al. (1965) Pathol. Vet., 2,446.<br />
(5)Engstrom, G. W. et al. (1987) J. Dairy Sci.,70, 2266.<br />
(6)Goff.J. P. (1984) J. Nutr., 114, 163.<br />
(7)Goff,J. P. ct al. (1982)J Nutr., 112, 1387.<br />
(8)Reinhardt, T. A. & Hustmyer, F. G.(1987) J. Dairy Sci., 70, 952.<br />
(9)Horst, R. L. et al. (1981) Anal. Biochem.,116, 189.<br />
71
(10)Smith, B. S. W. et al. (1985) Res. Vet. Sci.,38, 317.<br />
(11)Smith, B, S. W. & Wright, H. (1985) Res.Vet. Sci., 39, 59.<br />
(12)Hidiroglou, M. et al. (1984) Can.J. Anim.Sci., 64, 697.<br />
(13)Hidiroglou, M. & Knipfel.J. E. (1984)Can.J. Comp. Med., 48, 78.<br />
(14)Smith, B. S. W. et al. (1987) Vet. Rec,120, 199.<br />
(二)维生素 D 中毒病(Hypervitaminosis D)<br />
由于VD补充过多,亦可造成一些中毒表现。牛每天给予 250mg,羊给予 25mg,猪每天给<br />
予 1250~1750µg/kg体重,犬、猫给予大量猪肝或鱼肝油时,就可产生中毒,临床上表现为<br />
厌食、腹泻、漠然、呼吸困难,哑鸣,呕吐、消瘦甚至死亡。钙的异位沉着常可导致肾结石,<br />
动脉硬化。<br />
犬、猫用含VD较多的鱼肝饲喂,可出现血清钙浓度升高,血磷浓度正常或略有升高,<br />
骨骼脱钙。长期血钙浓度升高可造成多发性外周钙化现象,特别是肾脏的结石,骨骼疏松症<br />
等。<br />
VITAMIN D TOXICITY<br />
Vitamin D toxicity has occurred in cattle (1), horses (2), and swine (3) following the parenteral or<br />
oral administration of excessive quantities of the vitamin.<br />
n cattle, large parenteral doses of vitamin D, 15 17 million IU, results in prolonged<br />
hypercalcemia, hyperphosphatemia, and large increases in plasma concentrations of vitamin D,<br />
and its metabolites (1). Clinical signs of toxicity occur within 2-3 weeks and include marked<br />
anorexia, loss of body weight, dyspnea, tachycardia, loud heart sounds, weakness, recumbency,<br />
torticollis, fever, and a high case fatality rate (1). Pregnant cows 1 month before parturition are<br />
more susceptible than non-pregnant cows.<br />
Accidental vitamin D3 toxicity has occurred in horses fed a grain diet that supplied 12000-13<br />
000 IU/kg BW of vitamin D3 daily for 30 days (2), equivalent to about 1 million IU vitamin D,/kg<br />
of feed. Clinical findings included anorexia, stiffness, loss of body weight, polyuria, and<br />
polydipsia. There was also evidence of hyposthenuria, aciduria, soft-tissue mineralization, and<br />
fractures of the ribs (2). Calcification of the endocardium and the walls of large blood vessels are<br />
characteristic.<br />
Severe toxicity in pigs occurs at a daily oral dose of 50000-70000 IU/kg BW. Signs include a<br />
sudden onset of anorexia, vomiting, diarrhea, dyspnea, apathy, aphonia, emaciation, and death (2).<br />
Clinical signs arc commonly observed within 2 days after consumption of the feed containing<br />
excessive vitamin D. At necropsy, hemorrhagic gastritis and mild interstitial pneumonia are<br />
commonly present (3). Arteriosclerosis with calcification of the heart base vessels may also be<br />
visible macroscopically in poisoned cattle. Osteoporosis with multiple fractures has been observed<br />
in subacute to chronic hypervitaminosis D in swine. Histologically, there is widespread soft tissue<br />
mineralization, with a predilection for the lung and gastric mucosa, as well as elastinrich tissue,<br />
such as blood vessels. Changes in bone vary with the duration of exposure to toxic levels of the<br />
vitamin.<br />
Assay of the various metabolites of vitamin D in tissues is difficult. The diagnosis is therefore<br />
usually confirmed by correlating microscopic changes with a history of exposure to toxic levels of<br />
vitamin D.<br />
Samples for confirmation of diagnosis<br />
•Toxicology - 500 g of suspect feed(ASSAY (Vit D))<br />
72
•Histolog -formalin-fixed lung,stomach/abomasum, proximal aorta,lung, bone (LM).<br />
REFERENCES<br />
(1)Littledike. E. T. & 1 horst, R. L. (1982)J.Dairy Sci., 65. 749.<br />
(2)Harrington, D. D. & Page, E. H. (1983) J.Am. Vet. Med. Assoc, 182, 1358.<br />
(3)Long, G. C. (1984) J. Am. Vet. Med. Assoc,184, 164.<br />
三、维生素 E 缺乏症(Vitamine E Deficiency)<br />
VE又称生育酚,天然VE有 8 种,如α、β、γ、δ……,其中生育酚活性最强,由VE缺乏<br />
或VE与硒都缺乏在生产中可产生动物繁殖能力下降,幼畜肌肉营养不良,雏鸡产生小脑软<br />
化等营养性缺乏症,临床上常表现为幼畜的跛行,鸡平衡失调,母畜不孕、流产和胎衣不下<br />
等特征。<br />
各种动物均有发生,尤以幼年动物发病较多。而且VE缺乏常与硒缺乏合并发生,生产<br />
上难以区分,统称为硒-VE缺乏综合征。<br />
【病因】 维生素E广泛存在于动、植物性饲料中,尤其是胚芽中较多,通常情况下,<br />
不致于引起缺乏症,但VE是强的抗氧化剂,容易受曝晒、发酵、水浸、烘烤而失效,VE是<br />
脂溶性的,它随脂肪进入体内,必须在胆汁协助下,才能被吸收。因此当遇到下述情况之一,<br />
可产生VE缺乏症。<br />
长期用蒿杆类、根茎类植物喂饲,缺乏精料,或者用化学浸油法,使饼粕中VE残留太<br />
少,则可造成VE缺乏。<br />
谷物的种籽在收获过程中被曝晒、浸渍、发酵或霉烂时,其中VE损失过多,又未注意<br />
及时补充则可产生VE缺乏症。<br />
饲料中含不饱和脂肪酸过多(如亚麻油、花生油、豆油等),或其中含VE的拮抗成分,<br />
如鱼粉、鱼脂、鱼肝油等这些含不饱和脂肪酸较多的食物,可使体内VE消耗过多,亦可引<br />
起VE缺乏症。近年来采用丙酸等酸类物质处青贮料用作防霉,但VE缺乏症增多,因酸可降<br />
低植物中VE,增加植物中过氧化物。<br />
肝、胆疾病,因胆汁分泌不足或排泄受阻亦可产生VE缺乏。<br />
种籽湿度过大、贮仔 6 个月以上,其中VE含量大大降低,日粮中硒及含硫氨基酸缺乏,<br />
均可促进发病。<br />
VE缺乏时,主要引起体内不饱和脂肪酸含量较高的各种膜结构的氧化,体内过氧化氢<br />
及过氧化物被清除能力减弱,造成细胞膜、线粒体膜、微粒体膜损伤,因而产生渗出、出血<br />
和营养不良。<br />
VE与硒之间具有协同作用,但VE又不能完全代替硒,在缺硒的地区,尽管饲料中VE含<br />
量较高,但仍可出现硒缺乏。VE与硒之间协同作用机理见硒的缺乏症。<br />
【临床表现】 VE缺乏的许多表现与硒缺乏时的表现是类同的,例如产生营养性肌肉<br />
的坏死——白肌病、渗出性素质、桑葚心、营养性肝坏死等。硒-VE缺乏综合征的表现见硒<br />
缺乏症一节。<br />
有些疾病用补硒治疗几乎无效,如鸡的小脑软化症。有些病补硒后效果不明显,如黄脂<br />
病、繁殖机能障碍,而补VE效果显著。现分述如下:<br />
猪:有些猪因大量喂给鱼粉或变质的高脂肪类食物,如蚕蛹等缺乏VE,可致猪的黄脂病<br />
(见黄脂病)。<br />
禽:禽VE缺乏可产生小脑软化症及产蛋母鸡的蛋产量减少,孵化率下降。脑软化症多发<br />
生于 5 周龄,早期表现行走蹒跚如醉酒一样,常跌倒在地上翻转,并表现明显的运动不协调,<br />
痉挛和抽搐,进而瘫痪,颈部扭曲,沿身体纵轴旋转,并很快死亡。耐过的鸡常可留下终身<br />
不治的后遗症。头颈扭曲、跌倒,尤其在受惊吓时表现明显<br />
73
剖检表现脑部血管受损,脑广泛性出血,水肿,神经元坏死,变性,小脑有针尖样出血、<br />
水肿、大脑组织变性。<br />
成年公鸡VE缺乏还可产生睾丸肿大,精子生成障碍,精子活力下降,运动异常,甚至<br />
不产生精子。母鸡缺乏VE时,卵巢机能下降,性周期异常,不能受精或受精卵死亡,或胚<br />
胎发育不全,死亡率升高。<br />
意。<br />
小脑软化症,补充硒几乎无效,繁殖机能障碍补充硒效果不理想,唯用VE治疗效果满<br />
本病诊断常仅作出VE-Se缺乏综合征,采取的防治措施也一同考虑补充VE和Se。但应与<br />
传染性脑脊髓炎、中毒性脑病和肝病及单纯硒缺乏症相区别。<br />
【防治】 仔细查明原因,及时更换饲料,增加VE含量较高的大麦芽、绿豆芽的供给,<br />
或及时补充VE。夏季给予新鲜青绿饲料,冬季给予青草粉、苜蓿粉、松针粉和微量元素硒,<br />
使饲料中Se达 0.1~0.15mg/Kg。<br />
除去日粮中品质不好的脂肪、发霉、变质的鱼粉,酸败发酵的含脂丰富的饼粕等。在炎<br />
热季节(40~50℃),饲料中脂肪迅速变质,因而保存期不宜超过 3~5 天。<br />
一旦发现病禽,在饲料中添加浓缩VE,成年鸡 3~5mg/只,雏鸡 3mg/kg饲料,同时<br />
补充适量硒,防止Se和VE并发症。<br />
其它动物主要用VE制剂治疗。醋酸生育酚:牛、羊 5~20mg/kg体重,驹、犊 0.5~1.5g/<br />
头,仔猪 0.1~0.5g/头,皮下或肌肉注射。每天或隔日一次,连用 10~14 天,亦可用VE胶丸<br />
内服。<br />
对怀孕母畜,有人主张于分娩前 1~2 个月,待仔畜出生后一周内补充VE或亚硒酸钠,<br />
不仅可防止胎儿产后死亡,或胞衣不下,而且可使幼仔避免患白肌病。<br />
四、B 族维生素缺乏症(Water Soluble Vitamins Deficiency)<br />
水溶性维生素包括B族维生素、VC,这些维生素对食草动物一般不太重要,因为他们的<br />
消化道内的微生物可以合成。如B1、B2、烟酸、泛酸、吡啶、生物素、叶酸等。VC也可借<br />
其它途径合成。但对年青的犊牛、羔羊、马驹,当瘤胃或盲肠消化尚未健全时,非食草动物,<br />
容易引起B族维生素缺乏。VC也可在各种动物体内合成,在家畜中也不是很重要,但当有皮<br />
肤疾患时,亦可产生VC缺乏。<br />
Diseases caused by deficiencies of water-soluble vitamins<br />
Water-soluble vitamins, including vitamin C and the B complex, are of minor importance in<br />
herbivores animals (except for vitamin Bl2) because of their synthesis in the alimentary tract of<br />
these animals. Thiamin, nicotinic acid,riboflavin, pantothenic acid, pyridoxine B6, biotin, and<br />
folic acid are all synthesized by microbial activity; nicotinic acid and vitamin C are synthesized by<br />
other means. The young calf or lamb, in the period before rununal activity begins, is likely to<br />
receive inadequate supplies of these vitamins, and deficiency states can be produced<br />
experimentally. In the preruminant stage, colostrum and milk are good sources of the<br />
water-soluble vitamins, ewes' milk being much richer than cows' milk. The production of signs of<br />
deficiency of the B vitamins in horses by the feeding of deficient diets has raised some doubts as<br />
to the availability of the B vitamins synthesized in the large intestine in this species.<br />
Vitamin C is synthesized by all species and is not an important dietary essential in any of the<br />
domestic animals. Synthesis occurs in tissues and, although blood levels fall after birth, in the<br />
newborn calf they begin to rise again at about 3 weeks of age. However, a dermatosis of young<br />
calves has been associated with low levels of ascorbic acid in their plasma and responds to a<br />
single injection of 3 g of ascorbic acid. A heavy dandruff, followed<br />
by a waxy crust, alopecia, and dermatitis commences on the ears and spreads over the cheeks,<br />
74
down the crest of the neck, and over the shoulders. Some deaths have been recorded, but<br />
spontaneous recovery is more usual.<br />
There is some interest in the administration of high doses of ascorbic acid orally to horses to<br />
counteract the effects of stress and minimize the effects of infections. A single oral dose of 20 g of<br />
ascorbic acid does not result in any increase in plasma concentrations. However, daily<br />
administration of either 4.5 g or 20 g results in significant increases in plasma concentrations (1).<br />
REVIEW LITERA TURE<br />
Blair, R. & Newsome, F. (1985) Involvement of water-soluble vitamins in diseases of the<br />
swine. J. Anim. Sci., 60, 1508.<br />
REFERENCE<br />
(1) Snow, D. H. et al. (1987) Equine Vet.J., 19, 520.<br />
(一)硫胺素缺乏症(Thiamin deficiency)<br />
硫胺素即VB1,当鸡等非食草动物或幼年动物饲料中缺乏VB1或因VB1拮抗成分太多,可<br />
引起VB1缺乏症。临床上以神经机能障碍为特点。<br />
VB1广泛存在于各种植物性饲料中,稻麦类饲料中VB1存在于外胚层,胚体含量较高,米<br />
糠、麸皮中含量较高,饲料酵母中含量最高。反刍动物瘤胃及马族动物盲肠内微生物可合成<br />
它;因此晒干的牛粪、马粪中VB1含量丰富。动物性食物如乳、肉类、肝、心、肾中VB1含量<br />
也很高。通常条件下动物不致于产生VB1缺乏症。<br />
【病因】 原发性VB1缺乏,主要是饲料中VB1供给不足。VB1是水溶性的,不耐高温,<br />
因此用水浸泡,高温焖煮,可使其损失,引起VB1缺乏。<br />
继发性VB1缺乏病因有三种:①犬、猫饲料中供给太多的生鱼,因其中含硫胺素酶<br />
(thiaminase)可破坏硫胺素;②马族动物采食蕨类植物及马尾草(horsetail)引起神经症状,<br />
还有问荆木等这类植物中含硫胺素酶较多。猪亦可实验性饲喂蕨类植物而致病。马饲以大量<br />
芜菁,缺乏谷物时亦可引起VB1缺乏;③发酵饲料,其中蛋白质含量不足,糖类过剩时,可<br />
引起VB1缺乏。<br />
此外,动物胃肠机能紊乱,微生物区系破坏,长期慢性腹泻,长期大量使用抗菌素抑制<br />
正常共生菌生长,及使用抗球虫药氨丙嘧吡啶(amprolium)等,均可产生VB1缺乏症。幼龄<br />
动物主要是由于初乳或母乳以及代乳品中VB1含量不足引起VB1缺乏症。<br />
【病理】 硫胺素作为一种辅酶,与硫辛酸和辅酶I (NAD)一起,在丙酮酸的氧化脱<br />
羧中起重要作用。此外在磷酸己糖循环中,焦磷酸硫胺素是转酮反应的辅酶。当动物缺乏<br />
VB1,糖代谢不能顺利进行,大脑和神经系统对能量供给最敏感,当VB1缺乏时,过多的丙酮<br />
酸和乳酸分解受阻,在组织内蓄积,引起脑皮质坏死而呈现痉挛、抽搐、麻痹等神经症状,<br />
且心肌弛缓,心力衰竭。<br />
糖代谢紊乱进而影响脂代谢,导致中枢和外周神经鞘损伤,引起多发性神经炎。因VBl可<br />
促进乙酰胆碱合成。缺乏VB1时,胆碱能神经传导障碍,致胃肠蠕动缓慢,消化液分泌减少,<br />
消化不良。<br />
【临床表现】 犊牛:发病年龄为 30 天以内,平均 21 天发生,以神经症状为主,兴奋、<br />
痉挛发作、惊厥、四肢抽搐、坐地、倒地、眼球震颤甚至失明、牙关紧闭、角弓反张,有的<br />
犊牛呈现脑灰质软化(polio encephalo malacia)症,用VB1治疗收效明显。<br />
羔羊:呈转圈、无目的地奔跑,共济失调,倒地抽搐,昏迷死亡。<br />
禽:病初表现两腿无力,体重减轻,麻痹,消化不良,体温下降,雏鸡用缺乏VB1饲料喂<br />
饲两周后,开始出现症状。羽毛蓬松,脚无力,步态不稳,鸡冠发青、随病情发展个别肌群<br />
75
出现麻痹,在肌纤维中可见坏死灶,有特征性颈部回缩,后仰。鸡、鸽子最易患病,呈多发<br />
性神经炎,病鸡腿曲屈,坐地呈观星姿势。成年鸡发病缓慢,冠呈兰色,肌肉逐渐麻痹,开<br />
始发生于趾的伸肌,然后向上蔓延,波及到腿、翅和颈部的伸肌。小公鸡睾丸发育受抑制,<br />
母鸡卵巢萎缩。<br />
犬、猫硫胺素缺乏可引起对称性脑灰质软化症,小脑桥和大脑皮质损伤。猫对硫胺素的<br />
需要量比狗还多,猫主要因喂全鱼性食物,狗喂给熟肉而发生。表现为厌食,平衡失调,惊<br />
厥,呈现勾颈,头向腹侧弯,知觉过敏,瞳孔扩大,运动神经麻痹,四肢呈进行性瘫痪,惊<br />
厥,最后患畜半昏迷,四肢强直死亡。进行性脑灰质软化,从两侧性空泡生成到明显的坏死。<br />
原发性损伤位于脑干、尾丘(candal colliculi)、腹核,靠近第四脑室的小脑叶动眼神经核附<br />
近。<br />
猪:因食用生杂鱼或在海滩放牧引起VB1缺乏,50Kg重猪易发生呕吐,腹泻,后肢跛行,<br />
四肢肌肉病理造成步态不稳,痉挛、抽搐甚至瘫痪,间忽出现强直、痉挛,最后麻痹,直到<br />
死亡。<br />
马属动物蕨类植物中毒,可见咽麻痹,共济失调,阵挛或惊厥,昏迷死亡。<br />
临床病理学检查:血液丙酮酸浓度从 20~30µg/L 升高至 60~80µg/L;血浆硫胺素度从<br />
正常时 80~100µg/L 降至 25~30µg/L;脑脊液中细胞数量由正常时 0~3 个/ml 增到 25~100<br />
个/ml。<br />
【诊断】 根据饲料组成及曾否添加复合VB的生活史,临床上出现神经症状,禽出现<br />
进行性麻痹,颈前肌麻痹,呈观星姿势等而诊断。但应与雏鸡传染性脑脊髓炎相区别,该病<br />
有头颈震颤、晶状体震颤,仅发生于雏鸡,大鸡不发生是其特点。测定红细胞中转酮酶活动<br />
性(T。P。P效应),尿样中VB1含量与肌酐含量比值,有助于诊断。<br />
【防治】 立即更换饲料,提供充足的富含VB1的饲料如优质草粉、麸皮、米糠和饲料<br />
酵母,犬、猫应增加肝、乳、肉的供给,幼畜和雏鸡应补充VB1,按 5~10mg/kg饲料的计<br />
量,或按 30~60µg/kg体重计算。当饲料中含有磺胺或抗球虫药安丙嘧吡啶时,应多供给VB1,<br />
以防拮抗作用。目前普遍采用复合VB预防本病。<br />
药物治疗:用盐酸硫胺素注射液,按 0.25~0.5mg/kg体重的剂量,肌肉注射或静脉注射,<br />
但因VB1代谢较快,应每 3h一次,连用 3~4 天,可有显效。口服VB1,连用 10 天效果明显。<br />
犬给予 3mg/kg体重,猫给予 8mg/kg体重。大剂量使用VB1,可引起全身酥软,呼吸困<br />
难,进而昏迷等反应,曾有报告指出猫肌肉注射 50mgVB1,可出现上述反应,及早使用扑尔<br />
敏、安钠咖和糖盐水抢救,大多能治愈,久病体弱的小猫剂量为 1~2mg,肌肉注射。<br />
THIAMIN DEFICIENCY<br />
(HYPOTHIAMINOSIS)<br />
The disease caused by deficiency of thiamin in tissues is characterized chiefly by nervous signs.<br />
ETIOLOGY<br />
Thiamin deficiency may be primary, due to deficiency of the vitamin in the diet, or secondary,<br />
because of destruction of the vitamin in the diet by thiaminase. A primary deficiency is unlikely<br />
under natural conditions because most plants, especially seeds, yeast, and milk contain adequate<br />
amounts.<br />
Thiamin is normally synthesized in adequate quantities in the rumen of cattle and sheep on a<br />
well-balanced roughage diet. The degree of synthesis is governed to some extent by the<br />
composition of the ration, a sufficiency of readily fermentable carbohydrate causing an increase of<br />
synthesis of most vitamins of the B complex, and a high intake in the diet reducing synthesis. The<br />
etiology of polioencephalomalacia has been discussed in detail under that heading. Microbial<br />
synthesis of thiamin also occurs in the alimentary tract of monogastric animals, and in young<br />
76
calves and lambs, but not in sufficient quantities to avoid the necessity for a dietary supply, so that<br />
deficiency states can be readily induced in these animals with experimental diets. Thiamin is<br />
relatively unstable and easily destroyed by cooking.<br />
The coccidiostat amprolium is a thiamin antagonist and others are produced by certain plants,<br />
bacteria, fungi, and fish.<br />
EPIDEMIOLOGY<br />
One of the best examples of secondary thiamin deficiency is inclusion of excess raw fish in the<br />
diet of carnivores, resulting in destruction of thiamin because of the high content of thiaminase in<br />
the fish.<br />
Two major occurrences of secondary thiamin deficiency are recorded. In horses, the ingestion<br />
of excessive quantities of bracken fern (Pteridium aquilinum) and horsetail (Equisetum arvense)<br />
causes nervous signs because of the high concentration of thiaminase in these plants. The disease<br />
has been induced in a pig fed bracken rhizomes, and the possibility exists of it occurring under<br />
natural conditions. It has also been reported in horses fed large quantities of turnips (Beta vulgaris)<br />
without adequate grain. The second important occurrence of thiamin deficiency is in the etiology<br />
of polioencephalomalacia and is discussed under that heading.<br />
A thiaminase-induced subc.linical thiamin deficiency causing suboptimal growth rate of weaner<br />
lambs has been described (1). High levels of thiaminase activity were present in the feces and<br />
rumen contents of lambs with poor growth rate compared to normal lambs. Bacillus<br />
thiaminolyticus was isolated from the feces and ruminal fluids of affected lambs, and<br />
supplementation of thiami-nase-excreting lambs with IM injections of thiamine hydrochlonde was<br />
associated with significantly improved growth rate.(1)<br />
Thiamin deficiency occurs in sheep being subjected to live export from Australia to the Middle<br />
East (2). Sheep that died or were clinically ill and euthanized had significantly lower hepatic and<br />
ruminal thiaminase concentrations than clinically healthy control sheep. A high proportion had<br />
thiamin concentrations comparable to those found in sheep that die with polioencephalomalacia.<br />
The evidence indicates that the thiamin deficiency is a primary one associated with deprivation of<br />
feed during transportation to the pre-embarkation feedlots. The low feed intake and failure of the<br />
ruminal microbes to adapt, thrive, and synthesize a net surplus of thiamin during alterations in the<br />
ruminal environment are considered to be major contributing factors.<br />
PATHOGENESIS<br />
The only known function of thiamin is its activity as a cocarboxylase in the metabolism of fats,<br />
carbohydrates and proteins, and a deficiency of the vitamin leads to the accumulation of<br />
endogenous pyruvates. Although the brain is known to depend largely on carbohydrate as a source<br />
of energy, there is no obvious relationship between a deficiency of thiamin and the development of<br />
the nervous signs which characterize it. Polioencephalomalacia has been produced experimentally<br />
in prerununant lambs on a thiamin-free diet. There are other prodromal indications of deficiency<br />
disease. For example, there is a decrease in erythrocyte precursors and in erythrocyte transketolase.<br />
Additional clinical signs also in the circulatory and alimentary systems, but their pathogenesis<br />
cannot be clearly related to the known functions of thiamin. Subclinical thiamin deficiency due to<br />
thiaminases in the alimentary tract is associated with low erythrocyte transketolase activities and<br />
elevated thiamin pyrophosphate effects, which may explain the poor growth rate (1).<br />
CLINICAL FINDINGS<br />
Bracken fern (Pteridium aquilinum) and horsetail (Equisetum arvense,) poisoning in the<br />
77
horse<br />
Incoordination and falling, and bradycardia due to cardiac irregularity, are the cardinal clinical<br />
signs of bracken fern poisoning in the horse. These signs disappear after the parenteral<br />
administration of thiamin. Similar clinical effects occur with horsetail. Swaying from side to side<br />
occurs first, followed by pronounced incoordination, including crossing of the forelegs and wide<br />
action in the hindlegs. When standing, the legs are placed well apart, and crouching and arching of<br />
the back are evident. Muscle tremor develops and eventually the horse is unable to rise. Clonic<br />
convulsions and opisthotonos are the terminal stage. Appetite is good until late in the disease when<br />
somnolence prevents eating. Temperatures are normal and the heart rate slow until the terminal<br />
period when both rise to above normal levels. Some evidence has also been presented relating the<br />
occurrence of hemiplegia of the vocal cords in horses with a below normal thiamin status. Neither<br />
plant is palatable to horses and poisoning rarely occurs at pasture. The greatest danger is when the<br />
immature plants are cut and preserved in meadow hay.<br />
Experimental syndromes<br />
These syndromes have not been observed to occur naturally but are produced readily on<br />
experimental rations.<br />
In pigs, inappetence, emaciation, leg weakness, and a fall in body temperature, respiratory rate<br />
and heart rate occur. The electrocardiogram is abnormal and congestive heart failure follows.<br />
Death occurs in 5 weeks on a severely deficient diet. In calves, weakness, incoordination,<br />
convulsions and retraction of the head occur, and in some cases anorexia, severe scouring and<br />
dehydration.<br />
Lambs 1-3 days old placed on a thiamin-deficient diet show signs after 3 weeks. Somnolence,<br />
anorexia, and loss of condition occur first, followed by tetanic convulsions.<br />
Horses fed amprolium (400-800 mg/kg BW daily) developed clinical signs of thiamin<br />
deficiency after 37-58 days. Bradycardia with dropped heart beats, ataxia, muscle fasciculation,<br />
and periodic hypothermia of hooves, ears and muzzle were the common signs, with blindness,<br />
diarrhea and loss of body weight occurring inconstantly.<br />
CLINICAL PATHOLOGY<br />
Blood pyruvic acid levels in horses are raised from normal levels of 2-3µg/dL to 6-8 µg/dL. Blood<br />
thiamin levels are reduced from normal levels of 8-10 µg/dL to 2.5-3.0 µg/dL. Electrocardiograms<br />
show evidence of myocardial insufficiency. In pigs, blood pyruvate levels are elevated and there is<br />
a fall in blood transketolase activity. These changes occur very early in the disease. In sheep<br />
subjected to export, liver and rumen thiamin concentrations, and erythrocyte transketolase<br />
activities, were all below levels found in clinically normal sheep (2).<br />
NECROPSY FINDINGS<br />
No macroscopic lesions occur in thiamin deficiency other than non-specific congestive heart<br />
failure in horses. The myocardial lesions are those of interstitial edema and lesions are also present<br />
in the liver and intestine.<br />
In the experimental syndrome in pigs there are no degenerative lesions in the nervous system,<br />
but there is multiple focal necrosis of the atrial myocardium accompanied by macroscopic<br />
flabbiness and dilatation without hypertrophy of the heart.<br />
DIFFERENTIAL DIAGNOSIS<br />
Diagnosis of secondary thiamin deficiency in horses must be based on the signs of paralysis and<br />
known access to bracken fern or horsetail. A similar syndrome may occur with poisoning by:<br />
78
•Crotalaria spp.<br />
•Perennial rye-grass<br />
•Indigofera enneaphylla<br />
•Ragwort (Senecio jacobea).<br />
It is accompanied by hepatic necrosis and fibrosis. The encephalomyelitides are usually<br />
accompanied by signs of cerebral involvement, by fever and failure to respond to thiamin therapy.<br />
TREATMENT<br />
In clinical cases the injection of a solution of the vitamin produces dramatic results (5 mg/kg BW<br />
given every 3 hours). The initial dose is usually given IV followed by IM injections for 2-4 days.<br />
An oral source of thiamin should be given daily for 10 days and any dietary abnormalities<br />
corrected.<br />
CONTROL<br />
The daily requirement of thiamin for monogastric animals is, in general, 30-60µg/kg BW. The<br />
addition of yeast, cereals, grains, liver, and meat meal to the ration usually provides adequate<br />
thiamin.<br />
REFERENCES<br />
(1)Thomas, K. W. (1986) Vet. Res. Commun.,10, 125.<br />
(2)Thomas, K. W. ct al. (1990) Aust. Vet.].,67, 215.<br />
(二)核黄素缺乏症(Riboflavin Deficiency)<br />
核黄素又称VB2,饲料中VB2供给不足或缺乏,引起动物生长阻滞,皮炎,禽类脚爪卷缩,<br />
飞节着地而行的特征。<br />
本病主要发生于家禽、貂、猪等,幼年食草动物偶可发生。<br />
【病因】 核黄素广泛存在于植物组织、多叶蔬菜、鱼、肉等饲料中,许多动物自身及<br />
其体内微生物也可合成它。与VB1不同,它比较耐热,280℃开始熔化,分解,常温下热稳定。<br />
不受空气中氧的影响,但在碱性条件下,或在紫外光中暴晒则不稳定。自然条件下VB2缺乏<br />
不多见,但当饲料中缺乏青绿植物或因胃、肠、肝、胰疾病,使VB2消化吸收障碍,长期大<br />
量使用抗菌素或其它抑菌药物,致使体内微生物区系破坏。禽类几乎不能合成VB2(仅幼鸡<br />
盲肠内可合成少量VB2),而仅以稻谷饲喂时,更易引起VB2缺乏。<br />
妊娠、哺乳动物,生长快速的肉仔鸡、肉仔鸭等对VB2需要量较大,可引起VB2相对乏。<br />
【病理】 核黄素是黄素单核苷酸(FMN)和黄素腺瞟呤二核苷酸(FAD)—辅酶的<br />
组成成分,参予细胞呼吸,又称为黄素蛋白(flavoprotein)。有催化蛋白质、脂肪、糖代谢、<br />
氧化还原过程,因而可影响到体内多种组织的代谢,特别是神经血管机能,亦可影响上皮及<br />
黏膜的完整性。缺乏VB2,可引起上皮角质化生,在人,引起糙皮病和鹅口疮、口角炎;在<br />
动物,可引起角膜炎,皮肤增厚。<br />
【临床表现】 禽:用缺乏VB2的饲料喂 2~3 周的雏鸡,就可以发病。羽毛生长缓慢,眼<br />
充血,两腿软弱,脚向一个方向伸展,腿部肌肉萎缩,病鸡常蹲伏,因采食困难而生长阻滞、<br />
消瘦、死亡。<br />
母鸡(种母鸡、母鹅)因饲料单一,缺乏VB2时,本身症状不明显,但所产蛋孵化率降<br />
低,孵化至第 3、第 12~14 天及第 20 天,胚可达死亡高峰。即使不死,雏出壳时瘦小、水<br />
肿、脚爪弯曲。神经干变性,胚或雏鸡出生时羽不能破开毛鞘,形成棍棒状毛(clubbed down)。<br />
因羽在毛鞘内弯曲,形成小球节,尤其是黑羽鸡胚更明显,因为在黑色素形成中需要VB2。<br />
火鸡脚趾卷曲,脚、小腿、口角、眼睑等部位皮炎。雄火鸡生长缓慢,喙交叉,慢性者<br />
两肢发炎,腿关节水肿,有时皮下出血。母鸡产蛋减少,孵化率下降。小腿、口角、眼睑等<br />
79
部皮炎。<br />
犬、猫:VB2缺乏时,皮屑增多,胸部,后躯皮肤形成红癍,水肿,后肢肌肉虚弱,脑、<br />
脊髓神经变性,肌肉痛性痉挛(cramping),平衡失调,惊厥。<br />
猪VB2缺乏时,生长缓慢,经常腹泻,被毛粗乱无光,并有大量脂性渗出,鬃毛脱落,<br />
由于跛行,不愿走步,眼结膜损伤,眼睑肿胀,卡他性炎症,甚至晶体混浊,失明。母猪缺<br />
乏VB2,仔猪生后不久死亡。<br />
犊牛:厌食、生长不良、腹泻、流涎、流泪、掉毛、口角炎、口周炎。但眼疾不明显。<br />
【病理剖检】 病鸡主要表现坐骨神经及其分支的终板及肌肉本身变性,神经干肿胀,<br />
是正常鸡的 4~5 倍,色淡黄。神经鞘内有核原浆质块细胞(schwan cell)增生,经骨髓发育<br />
不良,有再生障碍性贫血倾向。皮肤角质肥厚,间以角化不全,棘层稍厚,表皮和真皮水肿,<br />
毛细,血管和淋巴管增多扩大,皮脂萎缩。<br />
【诊断】 鸡有特征性腿麻痹,爪卷曲,坐骨神经干肿大等现象,不难诊断。但应与神<br />
经型马立克氏病相区别。其它动物上皮变化应与VA缺乏相区别。红细胞内VB2下降,全血中<br />
VB2含量低于 0.0399µmol/L及测定任一尿样中VB2与肌酐含量的比值可作为诊断依据。其正<br />
常值为 80~270µgVB2/g肌酐。<br />
【防治】 调整日粮组成,增加含VB2丰富的饲料,如带叶蔬菜,酵母粉的供给。鱼粉、<br />
肉粉中VB2含量亦较高,三叶草粉或干燥的牛、马粪粉等均可预防VB2缺乏。必要时可补充复<br />
合VB制剂,作饲料添加剂。<br />
药物治疗,应用VB2混于饲料中,雏禽饲料中应含 4mg/kg,产蛋禽给予 5~6mg/kg,<br />
鹅、鸭、大鸡给予 6mg/kg(6g/T)。仔猪 5~6mg/头,犊牛 30~50mg/头,大猪 50~70mg<br />
/头,连用 8~15 天。亦可补充饲用酵母,仔猪 10~20g/头,育成猪 30~60g/头每日 2 次,<br />
连用 7~15 天。犬 5mg/kg 体重,猫 8mg/kg 体重。<br />
RIBOFLAVIN DEFICIENCY<br />
(HYPORIBOFLAVINOSIS)<br />
Although riboflavin is essential for cellular oxidative processes in all animals, the occurrence of<br />
deficiency under natural conditions is rare in domestic animals because actively growing green<br />
plants and animal protein are good sources, and some synthesis by alimentary tract microflora<br />
occurs in all species. Synthesis by microbial activity is sufficient for the needs of ruminants but a<br />
dietary source is required in these animals in the preruminant stage. Milk is a very good source.<br />
Daily requirements for pigs are 60-80µg/kg BW and 2-3 g/tonne of feed provides adequate<br />
supplementation. The trend towards confinement feeding of swine has increased the danger of<br />
naturally occurring cases in that species.<br />
On experimental diets the following syndromes have been observed.<br />
•Pigs -slow growth, frequent scouring, rough skin, and matting of the hair coat with heavy,<br />
sebaceous exudate are characteristic. There is a peculiar crippling of the legs with inability to walk<br />
and marked ocular lesions, including conjunctivitis, swollen eyelids, and cataract. The incidence<br />
of stillbirths may be high<br />
•Calves -anorexia, poor growth,scours, excessive salivation and lacrimation, and alopecia occur.<br />
Areas of hyperemia develop at the oral commissures, on the edges of the lips and around the navel.<br />
There are no ocular lesions.<br />
(三)泛酸缺乏(Pantothenic Acid Deficiency)<br />
泛酸又称为VB3,也是水溶性维生素,除反刍动物外,对各种动物均很重要。泛酸又称<br />
抗鸡皮炎因子。<br />
80
饲料中泛酸供给不足或缺乏,可引起泛酸缺乏症,临床上以皮炎,眼周围形成暗棕色渗<br />
出性炎症和斑块状脱毛,走路时呈高抬腿运动为特征。自然发生本病的有猪和鸡。<br />
泛酸广泛存在于动、植物组织中,如牛肉、猪肉、海鱼、蛋、牛奶、面粉、马铃薯、豌<br />
豆、水果等含量丰富,但玉米和蚕豆中含量较少。酵母中含量最丰富,为 200mg/kg。它溶<br />
于水、乙醇,对酸、碱、热均不稳定,饲喂纯玉米日粮、缺乏青绿饲料时可引起泛酸缺乏。<br />
体内微生物可以合成泛酸,但水杨酸、扁桃酸等与泛酸是拮抗的。动物中泛酸缺乏是不常见<br />
的。<br />
泛酸主要在组织内可转变为辅酶 A,存在于各种组织中,在物质代谢中作羧酸的载体,<br />
再与草酰乙酸相结合进入三羧酸循环。辅酶 A 与乙酸结合后作为胆固醇合成的前体,与许<br />
多固醇类激素合成关系密切;同时与脂肪的 β 氧化作用,辅酶 A 与乙酸结合后成为活性乙<br />
酸,与磺胺类药物在肝内乙酰化,使其失去抗菌作用。可见,泛酸是体内糖、脂肪代谢中重<br />
要辅酶。<br />
【临床表现】 猪有用全玉米日粮而自然产生泛酸缺乏症病例,典型特点呈后腿踏步动<br />
作或成正步走、高抬腿,鹅步(goose stepping),并常伴有眼,鼻周围痂状皮炎,斑块状秃<br />
毛,毛色素减褪呈灰色,严重者可发生皮肤溃疡,神经变性,并发生惊厥。渗出性鼻黏膜炎<br />
并发展到支气管肺炎,肝脂肪变性,腹泻,有时肠道有溃疡,结肠炎,恒伴有神经鞘变性。<br />
肾上腺有出血性坏死,并伴有虚脱及脱水,低色素性贫血,可能与琥珀酰辅酶 A 合成受阻,<br />
不能合成血红素有关。有些动物还出现胎儿吸收,畸形不育。<br />
禽:雏缺乏泛酸时,生长缓慢,羽毛发育障碍,衰弱,皮炎尤其是喙角皮肤发炎,眼睑<br />
炎症并有渗出液粘着,头部羽毛脱落,皮肤增厚结痂,鸡胚胎多在孵化第 12~14 天死亡,显<br />
有水肿,皮下出血,因孵化受阻,鸡出壳后,有呼吸衰竭,不能站立,病初几天内死亡。<br />
犬、猫:表现厌食,低糖血症,低氯血症和氮质血症,有时可出现惊厥、昏迷和死亡。<br />
远东低营养人群的足灼热症与泛酸缺乏可能有关。<br />
现象。<br />
诊断中应与烟酸缺乏和VB2缺乏相区别。VB2缺乏亦可引起皮炎,但VB2缺乏有脚趾挛缩<br />
本病常与生物素缺乏伴发,应注意区别。<br />
【防治】 饲料中添加含泛酸丰富的食物,如酵母、干草粉、贻糖浆、花生粉等。药物<br />
治疗采用泛酸钙:猪按 500µg/kg 体重,饲料中按 10~12g/t 添加;犬、猫按 50mg/kg 体重<br />
给予;家禽出壳后 l~6 天雏鸡饲料中应含 6~10mg/kg,雏火鸡 10.5mg/kg,雏鸭 11.0mg<br />
/kg,野鸡 10.0mg/kg,产蛋鸡 15.0mg/kg,肉仔鸡 6.5~8.0mg/kg,成年火鸡 16mg/kg。<br />
PANTOTHENIC ACID DEFICIENCY<br />
(HYPOPANTOTHENOSIS)<br />
Pantothenic acid is a dietary essential in all species other than ruminants, which synthesize it in<br />
the rumen. Deficiency under natural conditions has been recorded mainly in pigs on rations based<br />
on corn.<br />
In pigs, a decrease in weight gain due to anorexia and inefficient food utilization occurs first.<br />
Dermatitis develops with a dark brown exudate collecting about the eyes, and there is a patchy<br />
alopecia. Diarrhea and incoordination with a spastic, goose-stepping gait are characteristic. At<br />
necropsy a severe, sometimes ulcerative, colitis is observed constantly, together with degeneration<br />
of myelin.<br />
Calcium pantothenate (500µg/kg BW/d) is effective in treatment and prevention. As a feed<br />
additive, 10-12 g/tonne is adequate.<br />
Experimentally induced pantothenic acid deficiency in calves is manifested by rough hair coat,<br />
dermatitis under the lower jaw, excessive nasal mucus, anorexia, and reduced growth rate and is<br />
81
eventually fatal. At necropsy, there is usually a secondary pneumonia, demyelination in the spinal<br />
cord and peripheral nerves, and softening and congestion of the cerebrum.<br />
(四)胆碱缺乏症(Choline Deficieney)<br />
胆碱,又称为VB4、抗脂肪肝因子。胆碱缺乏症是因饲料内胆碱缺乏或不足所引起的,<br />
亦称胆碱缺少症(hypocholinosis)。临床上表现为发育受阻,肝、肾脂肪变性,消化不良,<br />
运动障碍,禽骨短粗症。<br />
胆碱缺乏症以仔猪和禽较为多发,犊牛也偶有发病,其它动物少见。<br />
【病因与病理】 胆碱是一个无色的结晶物,易吸湿,是强有机碱。以磷酸脂或乙酰胆<br />
碱的形式广泛分布于自然界,主要来源于鱼粉、肉粉、骨粉等和青绿植物以及饼粕等。谷物<br />
蔬菜中约含 1g/kg。<br />
胆碱可以在肝内合成。合成胆碱的原料为蛋氨酸、丝氨酸和甜菜碱。因此当饲料中缺乏<br />
蛋氨酸、丝氨酸时,胆碱合成不足。产蛋母鸡对胆碱需要量很多,每产一个蛋约需 500mg<br />
以上的胆碱,蛋黄中胆碱含量特别丰富,超过 17000mg/kg。产蛋母鸡若不供给胆碱,就可<br />
能因胆碱缺乏而产生脂肪肝综合征。<br />
日粮中烟酸过多,通常以甲基烟酰胺形式自体内排出,使机体缺少为合成胆碱和其它化<br />
合物所必需的甲基族,可导致胆碱缺乏。微量元素锰参予胆碱运送脂肪的过程,缺锰也可导<br />
致胆碱缺乏同样的症状。<br />
胆碱在体内主要生物学作用是参予将在肝内合成的脂肪运送到脂肪组织并贮藏。在脂肪<br />
运送中,脂蛋白作为脂肪的载体,脂蛋白分为低密度、极低密度脂蛋白等。脂蛋白是在肝内<br />
合成的,以多聚核蛋白和磷酰脂胆碱为原料,同时消耗 ATP。而某些损伤肝细胞因子,如四<br />
氯化碳、乳清酸等,及影响胆碱合成的因子蛋氨酸、丝氨酸等缺少,均可产生与胆碱缺乏一<br />
样的症状—肪肝生成。<br />
胆碱在体内乙酰化以后,形成乙酰胆碱。它是一种神经冲动传导介质,可引起胆碱能神<br />
经兴奋,引起胃肠道蠕动增强,分泌增多。<br />
胆碱还能促进肝糖元合成和储存。<br />
【临床表现】 胆碱是家禽、猪和幼龄犊牛必需的营养成分。缺乏时病畜呈现精神不振,<br />
食欲减退,生长发育缓慢,衰竭乏力。关节肿胀,屈曲不全,共济失调。皮肤黏膜苍白,消<br />
化不良等共同症状。<br />
猪:除乏力,关节肿胀、共济失调外,因肝脂肪变性引起消化不良,死亡率升高。仔猪<br />
生长发育缓慢,衰弱,被毛粗糙,腿关节曲屈不全,运动不协调,有的呈先天性八字形腿。<br />
禽:雏鸡可引起骨短粗症,跗关节肿大,转位,致胫跗关节变为平坦,严重时可与胫骨<br />
脱离,致双腿不能支撑体重。关节软骨移位,跟腱滑脱。即使饲料中有足量的生物素、叶酸<br />
和锰,缺乏胆碱也可引起骨短粗。病情发展呈渐进性,个体较大的发病尤多,肝脂肪变性和<br />
卵黄性腹膜炎。青年鸡极易发生脂肪肝,因肝破裂致急性内出血死亡。<br />
母鸡产蛋量减少,有时几乎不产蛋。蛋孵化率低下,即使出壳形成弱雏,关节韧带、肌<br />
腱往往发育不良。<br />
雏鸭用缺乏胆碱饲料饲喂,于 20 日龄出现共济失调,肌伸张无力,步履蹒跚、瘫痪,<br />
跗关节着地,关节肿胀,触之有痛感,骨短粗,关节周围有点状出血,肿胀肝有油腻感,病<br />
的发展呈渐进性,以生长迅速,个体肥大者为多见,发病前食欲旺盛,添加 0.16%的胆碱后<br />
迅速好转。<br />
犊牛,实验性用缺乏胆碱的合成饲料喂给 2 日龄犊牛,第 7 天出现食欲不振,衰弱乏力,<br />
不能站立,呼吸急促,消化不良,用胆碱治疗,很快康复。<br />
【诊断】 通常根据饲料中胆碱含量,剖检变化(肝、肾脂肪积累、腹脂过多,胫骨、<br />
82
跖骨发育不全)进行诊断。<br />
【防治】 首先查清病因后,立即供给胆碱丰富的全价饲料。胆碱在饲料中含量较多,<br />
一股占 0.1%。即 1t 饲料中含 1kg 胆碱。并供给含蛋氨酸、丝氨酸丰富的食物,如骨粉、肉<br />
粉、鱼粉、麦麸、油料、豆粕、豆类及酵母等。<br />
药物治疗:通常应用氯化胆碱,内服或拌入饲料中,按 1.5kg/t 的剂量。<br />
为防止鸡发生脂肪肝,可向每千克饲料中添加氯化胆碱 1g,肌醇 1g,VE10 单位,可获<br />
良好的预防效果。<br />
CHOLINE DEFICIENCY<br />
(HYPOCHOLINOSIS)<br />
Choline is a dietary essential for pigs and young calves. Calves fed on a synthetic<br />
choline-deficient diet from the second day of life develop an acute syndrome in about 7 days.<br />
There is marked weakness and inability to get up, labored or rapid breathing, and anorexia.<br />
Recovery follows treatment with choline. Older calves are not affected. On some rations the<br />
addition of choline increases daily gain in feedlot steers, particularly during the early<br />
part of the feeding period. In pigs, ataxia, fatty degeneration of the liver, and a high mortality rate<br />
occur. Enlarged and tender hocks have been observed in feeder pigs. For pigs, 1 kg/tonne of food<br />
is considered to supply sufficient choline (1).<br />
Congenital splayleg of piglets has been attributed to choline deficiency but adding choline to<br />
the ration of the sows does not always prevent the condition.<br />
REFERENCE<br />
(1) Simmins,P.H.& Brooks,P.H.(1983) Vet.Rec,112,415.<br />
(五)烟酸缺乏(Nicotinic Acid Deficiency)<br />
烟酸,又称烟酰胺。有人把它定名为VB5,或称为VPP、尼克酸(niacin)或抗癞皮病因<br />
子。动物饲料中因烟酸含量绝对或相对不足而致病。临床上以皮肤和黏膜代谢障碍,消化功<br />
能紊乱,被毛粗糙,皮屑增多和神经症状为特征。<br />
烟酸广泛存在于动物和植物类饲料中,肉、鱼、蛋、乳和乳酪中含量丰富,全麦粉,其<br />
它植物性饲料及水果、蔬菜中都含有丰富的烟酸。玉米中也含有烟酸,但量较少(与麦类相<br />
比),其前体色氨酸含量也比较低,酵母、米糠中烟酸含量较高。烟酸是水溶性维生素,它<br />
对热稳定,对光、空气、酸或碱也不敏感。<br />
反刍动物瘤胃微生物可以合成烟酸,即使犊牛,也不致产生烟酸缺乏,但自然发生的猪<br />
的烟酸缺乏,鸡烟酸缺乏已有报道。<br />
【病因与病理】 动物以玉米为食物时,可引起烟酸缺乏。仔猪、家禽易患烟酸缺乏症,<br />
因体内合成量很少。饲料中因色氨酸是烟酸的前体,色氨酸含量低,蛋白质供给不足,可促<br />
使发病。饲料中某些烟酸拮抗成分较多,如长期服用抗菌药物,干扰胃、肠内微生物区系的<br />
繁殖;3-吡啶磺酸、磺胺吡啶、吲哚-3-乙酸(玉米中含量较高)、三乙酸吡啶、亮氨酸等与<br />
烟酸是拮抗的,用石灰水处理玉米后,烟酸效应提高,患糙皮病相应减少。<br />
烟酸构成递氢辅酶 I (NAD)和辅酶 II (NADP),参予氢传递和细胞呼吸,在中间代<br />
谢中起重要作用。大多数脱氢酶需要 NAD 或 NADP 作为辅酶,所催化的反应对正常组织的<br />
完整性,特别是皮肤、黏膜代谢和神经功能作用是重要的。,此外烟酸还可以扩张末梢血管,<br />
降低血清胆固醇含量。因此缺乏烟酸时,由于可影响皮肤黏膜代谢,临床上可产生腹泻、皮<br />
肤角质化生(糙皮);影响神经功能,可表现痴呆。故号称三 D,即腹泻、糙皮和痴呆(Diarrhea,<br />
Dermatitis,Dementia)。<br />
【临床表现】 烟酸缺乏首先表现黏膜功能紊乱,出现减食、厌食,消化不良、腹泻、<br />
83
消化道黏膜发炎、大肠和盲肠发生坏死、溃疡以至出血,动物皮毛粗糙,并形成鳞屑。睾丸<br />
上皮退行性变化,神经变性,运动失调,反射紊乱,麻痹和癫痫。<br />
禽:烟酸缺乏除有上述消化道症状外,羽毛生长不良,跗关节增生、发炎,骨短粗、股<br />
骨弯曲,罗圈腿。鼻黏膜、喙角、眼睑、皮肤发炎明显。<br />
猪:因饲料中玉米成分过多而有自然缺乏的病例。但墨西哥人用石灰水处理玉米后则不<br />
发生此病。实验性诱导烟酸缺乏时,猪食欲下降,严重腹泻;皮屑增多性皮炎,呈污秽黄色;<br />
后肢瘫痪;胃、十二指肠出血,大肠溃疡,与沙门氏菌性肠炎类似;回肠、大结肠局部坏死,<br />
黏膜变性。用抗烟酰胺药产生的烟酸缺乏症,还有平衡失调,四肢麻痹,脊髓的脊突、腰段<br />
腹角扩大,灰质损伤,软化,尤其是灰质间区明显损伤。这些变化与自然发生的病例是一样<br />
的。<br />
犬、猫:烟酸缺乏以舌部变化明显,开始是红色,后是蓝色素沉着,俗称黑舌病。而且<br />
分泌出粘的有臭味的唾液。口腔溃疡、拉稀。睾丸曲精小管上皮退行性变,精子生成减少,<br />
精子活力下降。有神经症状、虚弱、惊厥、昏迷、神经组织广泛变性,尤其是脊髓的背角、<br />
腹角和腹侧脊神经根变性。严重者可引起脱水,酸中毒,骨髓再生不良,红细胞发育停滞于<br />
成红细胞阶段,本病常伴发贫血,因烟酸可影响卟啉代谢,卟啉沉着,因而皮肤发红,对光<br />
反射敏感。用烟酸治疗后,尿中卟啉排泄增多。<br />
【防治】 许多饲料、食品中含有烟酸。如麸皮、米糠、饲用酵母等,每千克麸皮叶中<br />
含 1.25~4g 烟酸,米糠中含 10g 左右,但因大多处于结合态,利用率不高,每千克肉中含 1~2g<br />
尼克酸。鸡对烟酸的需要量为 25~70mg/kg 饲料,猪生长期为 0.6~1mg/kg 体重,维持量<br />
为 0.1~0.4mg/kg 体重。犬 25mg/kg 体重;猫,60mg/kg 体重;兔,50mg/kg 体重;貂、<br />
狐,30mg/kg 体重。<br />
口服治疗量为:每吨饲料中添加 10~20g 烟酸。烟酸价格不贵,猪、禽日粮中应经常添加<br />
它,特别是以玉米为主食的动物。<br />
烟酸过多也是有毒的,特别是鼠类,急性中毒剂量中 4~5g/kg 体重,若为烟酸氨需加倍。<br />
烟酸对人和其它动物毒性作用较小,长期给鼠、鸡、狗以 2/kg 体重,连续 2 个月不见中毒,<br />
但烟酸过多可产生暂时性反应,如共济失调、紫绀。人用烟酸后可也现脸、颈发红。对热敏<br />
感、麻刺感和搔痒。头胀、眩晕、头疼、恶心、呕吐、短暂腹痛,甚至出现荨麻疹、心肌无<br />
力、心舒张增强,血管扩张等。<br />
NICOTINIC ACID DEFICIENCY<br />
(HYPONIACINOSIS)<br />
Nicotinic acid or niacin is essential for normal carbohydrate metabolism. Because of the high<br />
content in most natural animal feeds, deficiency states are rare in ordinary circumstances, except<br />
in pigs fed rations high in corn. Corn has both a low niacin content and a low content of<br />
tryptophan, a niacin precursor. A low protein intake exacerbates the effects of the deficiency, but a<br />
high protein intake is not fully protective.<br />
In ruminants, synthesis within the animal provides an adequate source. Even in young calves,<br />
signs of deficiency do not occur and because rumen microfloral activity is not yet of any<br />
magnitude, extraruminal synthesis appears probable.<br />
The oral supplementation of niacin in the diet of periparturient dairy cows may result in an<br />
increase in serum inorganic phosphorus and a decrease in serum potassium, calcium, and sodium<br />
concentrations. Niacin has been used to study the effects of artificially induced ketonemia and<br />
hypoglycemia in cattle.<br />
The daily requirements of niacin for mature pigs are 0.1-0.4µg/kg BW, but growing pigs appear<br />
to require rather more (0.6-1 mg/kg BW) for optimum growth.<br />
84
Experimentally induced nicotinic acid deficiency in pigs is characterized by inappetence, severe<br />
diarrhea, a dirty yellow skin with a severe scabby dermatitis, and alopecia. Posterior paralysis also<br />
occurs. At necropsy, hemorrhages in the gastric and duodenal walls, congestion and swelling of<br />
the small intestinal mucosa, and ulcers in the large intestine are characteristic and closely resemble<br />
those of necrotic enteritis caused by infection with Salmonella spp.<br />
Histologically, there is severe mucoid degeneration followed by local necrosis in the wall of the<br />
cecum and colon. Experimental production of the disease in pigs by the administration of an<br />
antimetabolite to nicotinamide causes ataxia or quadriplegia, accompanied by distinctive lesions in<br />
the gray matter of the cervical and lumbar enlargements of the ventral horn of the spinal cord. The<br />
lesions are malacic and occur in the intermediate zone of the gray matter. The identical lesions and<br />
clinical picture have been observed in naturally occurring disease.<br />
The oral therapeutic dose rate of nicotinic acid in pigs is 100-200mg; 10-20 µg/tonne of feed<br />
supplies sufficient nicotinic acid for pigs of all ages. Niacin is low in price and should always be<br />
added to swine rations based on corn.<br />
(六)吡哆醇缺乏(Pyridoxine Deficiency)<br />
吡哆醇、吡哆醛、吡哆胺合称维生素B6,以吡哆醇为代表。三者进入体内后均迅速变为<br />
辅酶—磷酸吡哆醛和磷酸吡哆胺而发挥生理作用。天然情况下未见有吡哆醇缺乏的报道,吡<br />
哆醇存在于植物组织中,在哺乳动物体内可转化为吡哆醛和吡哆胺,而后两者不能逆转为吡<br />
哆醇。<br />
吡哆醇广泛存在于各种植物性食物中,如马铃薯、菠菜、豌豆、蚕豆、胡萝卜、桔子等<br />
水果中及主食玉米、面粉中,动物性食品中亦有丰富的吡哆胺和吡哆醛,如牛奶、乳酪、蛋、<br />
肉类、鱼类等。胃肠道微生物还可合成VB6,尤其食草动物,通常情况下可产生VB6缺乏。<br />
VB6在体内因构成磷酸吡哆醛(胺),这一辅酶与体内转氨酶类、辅脱羧酶、脱氨酶、转硫酶<br />
等多种酶活性有关。<br />
实验性VB6缺乏症临床表现有:<br />
禽:小鸡、小鸭、火鸡缺乏VB6时,食欲下降,生长缓慢、皮炎、明显贫血和惊厥颤抖,<br />
不随意运动,病禽腰背塌陷,腿痉挛。<br />
肪浸润。<br />
猪:呈周期性癫痫样惊蹶,呈小细胞性贫血和泛在性含铁血黄素沉着,骨髓增生,肝脂<br />
人、猫:呈小细胞、低染性贫血,血液中铁浓度升高,含铁血黄素沉着,幼狗,幼猫有<br />
VB6缺乏症的记述,但尚缺乏必要的证据,如缺少体内VB6的测定结果等。<br />
犊:VB6缺乏表现厌食、生长不良,病态,被毛粗乱、掉毛,严重者呈不致死性癫痫作,<br />
异形红细胞增多(poikilocytosis)性贫血。<br />
各种动物对吡哆醇的需要量:雏鸡 6.2~8.2mg/kg 饲料,青年鸡 4.5mg/kg,育肥肉鸡<br />
4.5mg/kg,鸭 4.0mg/kg,鹅 3.0mg/kg 饲料,猪 1mg/kg 饲料或 0.1mg/kg 体重,犬、猫<br />
3~6mg/kg 体重,幼犬幼猫加倍量。<br />
PYRIDOXINE (VITAMIN B6)<br />
DEFICIENCY<br />
(HYPOPYRIDOXINOSIS)<br />
A deficiency of pyridoxine in the diet is not known to occur under natural conditions.<br />
Experimental deficiency in pigs is characterized by periodic epileptiform convulsions, and at<br />
necropsy by generalized hemosiderosis with a microcytic anemia, hyperplasia of the bone marrow,<br />
and fatty infiltration of the liver. The daily requirement of pyridoxine in the pig is of the order of<br />
85
100.µg/kg BW or 1 mg/kg of solid food, although higher levels have been recommended on<br />
occasions. Certain strains of chickens have a high requirement for pyridoxine and the same may<br />
be true of swine.<br />
Experimentally induced deficiency in calves is characterized by anorexia, poor growth, apathy,<br />
dull coat, and alopecia. Severe, fatal epileptiform seizures occur in some animals. Anemia with<br />
poikilocytosis is characteristic of this deficiency in cows and calves.<br />
(七)VB12缺乏症(Vitamin B12 Deficiency)<br />
VB12又称氰钴胺,是促红细胞生成因子,现定名钴胺素。VB12缺乏对食草动物而言,是<br />
因饲料中缺乏钴而引起的,对杂食动物是因饲料中缺乏VB12引起的,临床上表现厌食、消瘦、<br />
造血机能障碍等特征。<br />
猪、禽及其它鸟类容易发生VB12缺乏,牛、羊、马、兔常因地方性缺钴而呈地区性流行,<br />
其它动物VB12缺乏者很少。<br />
【病因】 VB12广泛存在于各种动物性饲料中,以肝脏中最丰富,其次是肾脏、心脏、<br />
鱼粉中,植物性饲料中几乎不含VB12。VB12可以由许多微生物合成,反刍动物瘤胃微生物,<br />
马、兔盲肠内微生物,其它动物肠道微生物都可以合成VB12,但禽及其它鸟类主要以植物性<br />
饲料为主,加之体内合成VB12能力很小,最易产生VB12缺乏。<br />
VB12合成过程中,需要有微量元素钴和蛋氨酸,因此饲料中如缺乏钴和蛋氨酸则因原料<br />
不足可产生VB12缺乏。钴缺乏症,常因土壤中缺钴或因其它的拮抗成分含量太多所致(详见<br />
钴缺乏症)。<br />
长期大量内服抗菌药,引起消化道微生物区系紊乱,亦可影响VB12合成。<br />
VB12在体内的生物学作用还决定于内源性因子(intrinsic factor)即胃粘蛋白。它存在于<br />
胃贲门和胃底,与VB12结合后进入回肠刷状缘,与特异性受体结合而吸收。因此,当胃溃疡、<br />
胃病理,内源因子分泌减少,亦可产生VB12 缺乏。此外胰腺机能不全、小肠炎症可影响VB12<br />
吸收。<br />
幼年动物VB12主要来源于母乳,如母乳不足或因母畜本身处于临界缺乏状态,乳汁中<br />
VB12含量不足,幼畜又无法接触粪便,亦可产生VB12缺乏。<br />
VB12经小肠的回肠段吸收进入肝脏后转化为具有高度生物学活性的代谢产物—甲基钴<br />
胺,而参予氨基酸、胆碱、核酸的生物合成。因此,当肝脏损伤、肝功能障碍时,亦可产生<br />
VB12缺乏样症状。<br />
【病理】 在钙离子作用下,胃的胃粘蛋白(IF)被激活,它有两个结合部位,一个与<br />
Ca 2+ 结合,另一个与VB12结合,结合后的复合物可不被小肠消化液破坏,运至回肠的刷状缘,<br />
B12与胃粘蛋白分离,再与特异性受体结合后而吸收,VB12在血浆中由运钴蛋白(I或II)运<br />
至肝脏或全身。其中一部分转化为肝肠循环。另一部分随粪便排出。<br />
VB12对反刍动物体内糖代谢有影响。丙酸酰化后生成丙酰辅酶A,它必须在VB12参予下<br />
才能转变为琥珀酰辅酶A(因VB12是丙二酸单酰辅酶A的辅酶),然后进入三羧酸循环。在VB12<br />
参予下,可使N5甲基四氢叶酸转变为有生物活性的四氢叶酸,然后重新甲基化后合成胸腺<br />
嘧啶。因此,缺乏VB12时,胸腺嘧啶核苷酸合成受阻,细胞分裂中止,导致巨幼红细胞或人<br />
红细胞血癌,同时动物消瘦。<br />
【临床表现】 患病动物一般出现食欲减退或反常,牛生长缓慢,发育不良,可视黏膜<br />
苍白,皮肤湿疹,神经兴奋性增高,触觉过敏,共济失调,易发肺炎和胃肠炎等疾病。<br />
禽:缺乏VB12时,产蛋量下降,肌胃糜烂,肾上腺扩大。种鸡缺乏VB12时,孵化率大幅度<br />
下降,鸡胚胎畸形,多在孵化第 17 天死亡。<br />
犬、猫:VB12缺乏引起贫血,厌食,幼仔脑水肿发生较多。在外周血液中可同时见到红<br />
86
细胞母细胞和髓母细胞,称为红白血病(erythro leukemia)和巨母红细胞(mega-loblast)血<br />
症。<br />
猪:VB12缺乏可有厌食、生长停滞神经性障碍,应激性增加,运动失凋,以及后腿软弱,<br />
皮肤粗糙,背部有湿疹样皮炎,偶有局部皮炎,胸腺、脾脏以及肾上腺萎缩,肝脏和舌头常<br />
呈肉芽瘤组织的增殖和肿大,并发生典型的小细胞性贫血(幼猪中偶有腹泻和呕吐)。成年<br />
猪繁殖机能紊乱,易发生流产、死胎、胎儿发育不全,畸形,产仔数减少,仔猪活力减弱,<br />
生后不久死亡。<br />
小牛:喂给不含VB12的牛乳时,生长停止和神经疾病,如纵向不等同运动,行走时摇摆<br />
不稳,运动失调。<br />
【诊断】 根据病史,饲料分析(用放射免疫技术测定钴),VB12含量低下,临床上贫<br />
血,巨红细胞血症,白细胞减少,骨髓内有巨母红细胞骨髓相,皮疹,消化不良,消瘦,黏<br />
膜苍白,尿中甲基丙二酸浓度增高而诊断,但应与泛酸、叶酸、钴缺乏等相区别。<br />
【防治】 在查明原因的基础上,调整日粮组成,给予富含VB12的饲料,如全乳,鱼粉,<br />
肉粉,大豆副产品,反刍动物亦可补充氯化钴等钴化物。<br />
药物方面通常用氰钴胺或羟钴胺治疗,猪日需要量为 20~40µg,治疗量 300~400µg。赛<br />
狗、赛马按 2µg/kg 体重,作为缓解寄生性和食物性贫血,不需天天用药,l 针可以维持 2~4<br />
周,雏鸡 15~27µg/kg 饲料,雏火鸡 2~10µg/kg,蛋鸡 7µg/kg,肉鸡 1~7µg/kg,火鸡 10µg<br />
/kg,鸭 10µg/kg 饲料。犬、猫 0.2~0.3mg/kg 体重。<br />
反刍动物不需补充VB12,只要口服硫酸钴就行,硫酸钴经肌肉或静脉注射效果不如口服<br />
明显。马、兔食物性贫血也只要在食物中添加钴即可。<br />
VITAMIN B12 DEFICIENCY<br />
(HYPOCYANOCOBALAMINOSIS)<br />
Vitamin B12 deficiency is unlikely to occur under natural conditions other than because of a<br />
primary dietary deficiency of cobalt, which is an important disease in many countries of the world.<br />
Although microbial synthesis of the vitamin occurs in the rumen in the presence of adequate<br />
cobalt, and in the intestines of other herbivores such as the horse, it is probably a dietary essential<br />
in the pig and young calf. Animal protein is a good source. A deficiency syndrome has been<br />
produced in young calves on a synthetic ration. Signs include anorexia, cessation of growth, loss<br />
of condition and muscular weakness. The daily requirement under these conditions is 20-40 µg of<br />
vitamin B12. Sows vary in their ability to absorb the vitamin and those with poor absorption<br />
ability, or on deficient diets, show poor reproductive performance.<br />
For pigs, 10-50 mg/tonne of feed is considered to be adequate (1).<br />
The vitamin is used empirically in racing dogs and horses to alleviate parasitic and dietetic<br />
anemias in these animals at a dose rate of 2µg/kg BW. Cyanocobalamin zinc tannate provides<br />
effective tissue levels of vitamin B12 for 2-4 weeks after one injection, and normal and abnormal<br />
blood levels have been established for all species. It is also used as a feed additive for fattening<br />
pigs, usually in the form of fish or meat meal or as ‘animal protein factor’. It is essential as a<br />
supplement if the diet contains no animal protein, and maximum results from the feeding of<br />
antibiotics to pigs are obtained only if the intake of vitamin B12 is adequate.<br />
REFERENCE<br />
(1) Simmins,P.H.& Brooks,P.H.(1983) Vet.Rec,112,415.<br />
(八)叶酸缺乏症(Folic Acid Deficiency)<br />
叶酸又称为VM,是抗猴(monkey)贫血因子,故称之。抗鸡贫血因子,称为VBC,两<br />
87
者其实是同一物质,因在菠菜中发现生长因子,与此物同,故又称为叶酸。其纯品定名为蝶<br />
酰单谷氨酸,但习惯上仍称作叶酸。动物饲料中因叶酸含量不足或缺乏,称叶酸缺乏症。临<br />
床上以生长缓慢,造血机能障碍,繁殖能力低下为主症。<br />
较丰富。<br />
动物中以禽、猪缺乏症多见,其它动物叶酸缺乏症少见。<br />
叶酸,广泛存在于所有绿叶蔬菜中,每千克内含 10mg 叶酸。动物的肝脏和蛋中含量比<br />
【病因与病理】 叶酸是黄色结晶状粉末,无味、无臭,不溶于醇和醚,稍溶于热水中,<br />
它在中性和碱性溶液中稳定,在酸性液中不稳定,烹调中会大大减少它的含量,对光敏感。<br />
叶酸也可由消化道内细菌合成。随饲料进入的叶酸,以蝶酰多聚谷氨酸形式存在,被小肠黏<br />
膜分泌的解聚酶(γ-L-谷氨酸-羧基肽酶)水解成谷氨酸和叶酸,被吸收以后在叶酸还原酶<br />
作用下生成 7,8-二氢叶酸,后者在二氢叶酸还原酶作用下生成 5,6,7,8-四氢叶酸。它<br />
与核苷酸合成有密切关系。许多氨基酸分解过程中产生的一碳基团需结合到叶酸上后,才能<br />
用以合成核苷酸。因此,在遇有下述情况之一,可产生叶酸缺乏症。<br />
①长期以低绿叶植物饲喂,又未补充动物性食物鱼粉、骨肉粉、肝血粉等,可致鸡、猪<br />
叶酸缺乏。②长期大量使用抗菌药物,使体内微生物区系紊乱,尤其是饲料中添加磺胺药<br />
(sulfanamide)、扑癫酮(primidone)等,它是叶酸的拮抗剂,结构与叶酸中的对氨基苯甲<br />
酸(p-aminobenzoid acid)类似,可竞争性抑制菌体内叶酸合成,因而也抑制了一碳基团的<br />
转移,最终出现叶酸缺乏症。③长期胃肠消化障碍,叶酸吸收不足,亦可产生叶酸缺乏症。<br />
叶酸不仅参予一碳基团的转移,而且参予嘌呤、胸腺嘧啶等甲基化合物合成和核酸合成。<br />
缺乏叶酸时因核酸合成障碍,导致细胞生长、增殖受阻,组织退化,特别是细胞生长迅速,<br />
组织退化快的。消化道上皮、表皮、骨髓等处易损伤。动物生长发育缓慢,甚至停止。消化<br />
紊乱。由于胸腺嘧啶脱氧核糖核酸合成减少,使红细胞中 DNA 合成受阻,血细胞分裂增殖,<br />
核糖核酸合成减少,使红细胞中 DNA 合成受阻,血细胞分裂增殖速度减慢,细胞体积增大,<br />
核内染色质疏松,引起巨幼红细胞性贫血。<br />
【临床表现】 叶酸缺乏与VB12缺乏时症状类似,如食欲不振,消化不良,腹泻,皮肤<br />
粗糙,脱毛贫血,呈巨幼红细胞性贫血,伴有白细胞和血小板减少。此外,易患肺炎和胃肠<br />
炎,母猪受胎率与泌乳量减少等一般症状。<br />
禽:缺乏叶酸时,生长缓慢,羽毛脆弱、褪色,全身贫血,出现典型的巨红细胞性贫血<br />
和血小板减少症,胃畸形,火鸡雏鸡的喙变形,颈部肌肉痉挛性收缩,鹅脚无力。后期颈肌<br />
麻痹,头颈伸直,双翅下垂,不停抖动,母鸡产蛋减少,孵化率低,胚胎往往呈髋关节移位,<br />
胫跗骨弯曲,下颌缺损,趾畸形等,死亡率较高、<br />
赛马、赛狗对叶酸需要量较大,在训练期间血液中叶酸浓度下降。<br />
犬、猫叶酸缺乏症与VB12缺乏症状基本相同(见VB12缺乏)。<br />
【诊断】 通常根据病史和临床上产生巨红细胞性贫血,白细胞减少,和特异性骨髓内<br />
巨母红细胞现象,配合临床治疗性试验而诊断。有报道称:给予一定量组氨酸后,测定尿中<br />
狗尿酸,咪唑丙烯酸或甲亚氨基-谷氨酸,当叶酸缺乏时,这些物质尿排泄增多。但该试验<br />
是非特异的。叶酸缺乏与VB12缺乏临床上无法区分。<br />
【防治】 调正日粮组成,尽量增加多叶的蔬菜或青草粉,如苜蓿,豆谷,或青绿饲料,<br />
保持饲料中有充足的叶酸。<br />
药物疗法:临床上使用叶酸制剂,猪 0.1~0.2mg/kg体重,禽 10~15µg/只,内服,或<br />
50~100µg/只肌肉注射,每月一次。使用叶酸同时可给予VB12,剂量参阅VB12缺乏。<br />
动物对叶酸的需要量是:1~60 日龄鸡 0.6~2.0mg/kg 日粮,雏火鸡 0.8~2.0mg/g 日粮;<br />
蛋鸡 0.12~0.42mg/kg 日粮;肉鸡 0.3~1.0mg/kg 日粮;火鸡 0.4~0.7mg/kg 饲料,犬、猫<br />
0.3~0.4mg/kg 体重,貂、狐 0.6mg/kg 体重,赛马和赛狗 15mg/kg 体重,工作马 10mg<br />
88
kg 体重。<br />
FOLIC ACID DEFICIENCY<br />
(HYPOFOLICOSIS)<br />
Folic acid (pteroylglutamic acid) is necessary for nucleic acid metabolism, and its deficiency in<br />
humans leads to the development of pernicious anemia. A dietary source is necessary to all species<br />
and an adequate intake is provided by pasture. Although naturally occurring deficiencies have not<br />
been diagnosed positively in domestic animals, folic acid has numerous and complex<br />
interrelationships with other nutrients and the possibility of a deficiency playing a part in inferior<br />
animal performance should not be overlooked. The vitamin has a particular interest for equine<br />
nutritionists. Permanently stabled horses and some horses in training may require additional folic<br />
acid, preferably on a daily basis by the oral route (1). Folic acid at a dose of 1 mg/kg BW orally<br />
daily for 2 weeks was used successfully for the treatment of acquired alopecia in a 3-week-old<br />
Charolais calf, but spontaneous recovery without treatment was a possibility (2).<br />
REFERENCES<br />
(1)Roberts,M.D.(1983) Aust.Vet.J.,60,106.<br />
(2)Bouvet,A.et al.(1988) Vet.Rec,123,533.<br />
(九)生物素缺乏症(Biotin Deficiency)<br />
饲料中可利用生物素含量过少或因食物中含有生物素拮抗物质造成动物生物素缺乏。临<br />
床上表现为皮炎、脱毛、蹄壳开裂等现象。主要发生于鸡、火鸡、猪、犊牛、羔羊、犬、猫。<br />
成年牛、羊、马的胃、盲肠功能完好时,几乎不发生生物素缺乏症。<br />
【病因】 生物素又称 VH,微溶于水,易溶于醇,不溶于有机溶剂,对热稳定,不被<br />
酸碱分解。它广泛存在于动、植物食品中,瘤胃、盲肠、大肠内细菌可以合成它。生物素在<br />
回肠的前四分之一处吸收,盲肠、大肠内对生物素吸收甚少。前胃功能良好的动物,有食粪<br />
癖的动物如兔,基本上没有生物素缺乏症。猪、鸡及部分毛皮动物肠道合成的生物素,不能<br />
被充分吸收,大多随粪便排出,如不补充它,可酿成缺乏症。<br />
生物素虽广泛存在于动、植物组织中,尤其是肝脏、肾脏内生物素含量很高,天然存在<br />
的 α-生物素,才具有生物活性。但是,有些饲料中如大麦,麸皮、燕麦中生物素的可利用<br />
率很低。仅 10%~30%,有的甚至为 0%,而有些饲料中生物素利用率达 100%,如鱼粉,油<br />
饼粕、黄豆粉、玉米粉等。仅根据饲料中生物素含量不能判断是否缺乏。<br />
生蛋清内含有抗生物素蛋白,称为 Aidin 或卵白素,可与生物素结合而抑制其活性,同<br />
时该结合物不被酶所消化。给小鸡育雏时,如采用过多的生鸡蛋或给小狗小猫用生鸡蛋拌食<br />
可致生物素缺乏。但加热后可将抗生物素蛋白破坏,生物素的某些衍生物亦有拮抗生物素作<br />
用,持续饲喂磺胺类药物或抗生素,可导致生物素缺乏。<br />
【病理】 生物素是糖、蛋白质和脂肪的中间代谢中一个重要的辅酶,它参予很多羧化<br />
反应。不稳定的羧基生物素是一种活泼的二氧化碳形式。它在体内可参加丙酮酸的羧化作用,<br />
形成草酰乙酸。它的转羧基作用促使乙酰辅酶 A 转变成丙二酰辅酶 A 时,需要有生物素参<br />
予。当生物素缺乏时,可使上述代谢改变。<br />
【临床表现】 鸡和火鸡缺乏生物素表现为脚、嘴和眼周围皮肤发炎,生长迟缓,食欲<br />
减少,羽毛干燥、变脆,由于骨和软骨缺损,跖骨歪斜,长骨短而粗,缺乏生物素的鸡所生<br />
的蛋孵化率降低,鸡胚发育缺陷,呈先天性骨短粗症。共济失调和特征性骨骼变形,如胫骨<br />
短而曲屈,跗跖骨很短,翅短,颅骨短,肩胛骨前端短和弯曲(见胚胎病)。肉用仔鸡出生<br />
后 10~20 天时,可发生“脂肪肝和肾综合症”,补充生物素以后可大大减少发病率(见脂肪<br />
肝和肾综合症)。<br />
89
狗用生鸡蛋饲喂时可产生生物素缺乏。动物表现紧张,无目的地行走,后肢痉挛和进行<br />
性瘫痪。皮肤炎症和骨骼变化与其它动物类似。<br />
猪,尤其是集约化饲养条件下的猪,无法接触到垫草和粪便,又以麦类、麸皮为主食时,<br />
易产生生物素缺乏。表现为耳、颈、肩部、尾巴、皮肤炎症,脱毛,蹄底蹄壳出现裂缝。口<br />
腔黏膜炎症、溃疡。国外集约化猪场中有蹄损伤的猪约占 50%,按目前推荐的日粮中生物<br />
素含量,不能减少蹄损伤。建议饲料中应含 200~500µg/kg α-生物素,才可减少损伤和减轻<br />
损伤的程度。然而,圈舍中地面潮湿,粗糙不平,可增加蹄损伤和损伤程度。补充生物素可<br />
减少发病率,补充量越多,康复越怏。另有试验表明,由于饲料中生物素不足,动物繁殖率<br />
不能达最高。补充生物素,使母猪多生 2%~14%的仔猪。断乳后成活率增加 3%~17%。补<br />
充的有效 α-生物素越多,其效果越明显。<br />
【诊断】 日前尚缺乏早期诊断的方法。血浆生物索浓度通常应在 650ng/L 以上,但<br />
个体间差异很大,以猪而言,可在 390~3070ng/L 之间,一般认为当血浆生物素浓低于 600ng<br />
/L 时,则应补充 α-生物素。<br />
饲料中生物素的含量可作为重要参考,但各种饲料中生物素的可利用率相差很多(0~100<br />
%)。因此,必须予以校正后才有价值,一般认为,饲料中有效生物索含量应在 200µg/kg<br />
以上,才能预防猪的蹄损伤和维持最高繁殖性能。鸡饲料中有效生物素含量应在 150µg/kg,<br />
目前N。R。C。推荐的猪、鸡饲料中生物素需要量普遍偏低。<br />
诊断中应与烟酸缺乏、锌缺乏或硫缺乏引起的掉羽或掉毛相区别。应注意测定饲料中烟<br />
酸、锌及其拮抗物质和含硫物质浓度,以免误诊,必要时可作治疗性试验,以便判断是何种<br />
原因引起的缺乏症。<br />
【防治】 许多饲料是生物素的良好补充物质,如黄豆粉、玉水粉、干乳清、啤酒酵母、<br />
鱼粉等。不仅其中 α-生物素含量高,而且生物学效应好,均可达 100%。补充足量生物素可<br />
预防动物缺乏症,但对某些症状,如蹄损伤、提高繁殖性能等,补充生物素后常需几周甚至<br />
数月,才能使症状缓解。<br />
家禽,尤其是雏禽,禁用生蛋清饲喂。可经加热后拌料喂给,有人建议猪饲料中给予<br />
350~500µg/kg α-生物素可成功地防止生物素缺乏。鸡可参照此剂量补充。<br />
BIOTIN DEFICIENCY (HYPOBIOTINOSIS)<br />
Biotin has several important biochemical functions. It is a cofactor in several enzyme systems<br />
involved in carboxylation and transcarboxylation reactions, and consequently has a significant<br />
effect on carbohydrate metabolism, fatty acid synthesis, amino acid deamination, purine synthesis,<br />
and nucleic acid metabolism. Biotin is found in almost all plant and animal materials and, being<br />
required in very smallquantities, is unlikely to be deficient in diets under natural conditions,<br />
especially as microbial synthesis occurs in the alimentary tract.<br />
Swine<br />
The principal source of biotin for the pig is the feed it receives, and feeds vary greatly in their<br />
biotin content and in the biological availability of that biotin. Diets based on cereals with a low<br />
available biotin content may provide insufficient dietary biotin for the maintenance of hoof horn<br />
integrity in pigs. The biotin content in basal diets fed to pigs has varied from 29 to 15 µ/kg<br />
available biotin, and supplementation of these diets has resulted in improvements in litter size.<br />
Continuous feeding of sulfonamidcs or antibiotics may induce a deficiency. An antivitamin to<br />
biotin (avidin) occurs in egg white, and biotin deficiency can be produced experimentally by<br />
feeding large quantities of uncooked egg white (1).<br />
In pigs, experimental biotin deficiency is manifested by alopecia, dermatitis, and painful<br />
cracking of the soles and the walls of the hooves (2,3).<br />
90
Naturally occurring outbreaks of lamenessin gilts and sows associated with lesions of the soles<br />
and the walls of the hooves, which responded to biotin supplementation, have now been<br />
well-described (2,3). The severe lameness and long course of convalescence have been<br />
responsible for a high rate of culling in breeding animals. In gilts fed a basal diet with a low level<br />
of biotin (32µg available biotin/kg) from 25 kg liveweight to 170 days of age, there were no<br />
significant differences in the number of lesions and claws affected compared to gilts fed a<br />
biotin-supplemented diet (350 µg available biotin/kg) (4). However, between 170 days of age and<br />
the first weaning, the incidence of hoof lesions increased markedly. Over the next four litters the<br />
incidence of lesions increased with the age of the sow. The predominant lesions in the foot were<br />
cracks, which occurred mainly in two associated regions: the heel/toe junction and the heel, and<br />
the sidewall and adjacent white-line region of the toe (4). Supplementation of the diet of breeding<br />
sows with biotin at an early stage of development makes a significant contribution to the<br />
maintenance of horn integrity.<br />
Affected animals become progressively lame after being on a biotin-deficient ration for several<br />
months. Arching of the backanda haunchedstancewith the hindlegs positioned forward occurs<br />
initially. This posture has been described as a ‘kangaroo’-sitting posture. The foot pads become<br />
softer and the hoof horn less resilient. The feet are painful and some sows will not stand for<br />
breeding. Deep fissures at the wall-sole junction may extend upwards beneath the wall horn, and<br />
gaping cracks may separate the toe and heel volar surfaces. The foot pads initially show excessive<br />
wear, later longitudinal painful cracks develop. In well-developed cases the foot pads appear<br />
enlarged, the cracks are obvious and covered by necrotic debris. The foot pads of the hindfeet are<br />
usually more severely affected that those of the forefeet and the lateral digit is more frequently<br />
affected. The dewclaws also are affected by cracks and the accumulation of necrotic tissue.<br />
Skin lesions also develop in affected gilts and sows. There is gradual alopecia, particularly over<br />
the back, the base of the tail, and the hindquarters. The hairs are more bristly than normal and<br />
break easily. The alopecia is accompanied by a dryness of the skin.<br />
As the lesions of the feet and skin develop there is a marked drop in the serum biotin<br />
concentrations, which is considered as a sensitive index of biotin deficiency (1). Adequate biotin<br />
status may be indicated by serum biotm level (ng/L) =700; marginal, 600-700; inadequate,<br />
400-600; and deficient below 400 (1). Compression and hardness tests made on external hoof have<br />
also been used as an indirect measure of biotin adequacy in pigs (5). The tests indicate that<br />
significant improvements in the strength and hardness of pig hoof horn are produced by biotin.<br />
Supplementation of the diet with biotin does not affect either horn growth or wear rates (3). Biotin<br />
supplementation does affect the structure of the coronary epidermis; there is an increasein the<br />
density of the horn tubules in the stratum medium, the horny squames in the stratum medium are<br />
more tightly packed, and the tubules are more clearly defined (6).<br />
Reproductive performance of sow s is also influenced by their biotin status (7).<br />
Supplementation of the diet with biotin may increase litter size, increase the number of pigs<br />
weaned, decrease the mean interval in days from weaning to service, and improve conception rate.<br />
Over a period of four parties, piglet production increased by 1.42 pigs/sow year (7).<br />
BIOTIN REQUIREMENTS<br />
Swine<br />
The daily requirements of biotin for swine have not been well-defined, but certain amounts have<br />
been associated with an absence of lameness and improved reproductive performance. Basic diets<br />
91
for gilts contain 35-50 µg/kg, and the addition of 350-500µg/kg is recommended. This provides a<br />
daily intake of 4.0-5.0 mg/sow/d.The response to dietary supplementation may take several<br />
months; therefore, supplementation should begin at weaning. The details of biotin studies in pigs,<br />
including experimental deficiency,the absorption and synthesis of biotin, biotin availability in<br />
feedstuffs,and the biotin requirements of the growing pig are available (8).<br />
Supplementation of a basal diet, calculated to contain 56µg/kg available biotin with daily<br />
allowances of biotin at 1160 µg/sow/d in pregnancy, and 2320 µg/sow/din lactation, produced<br />
significant improvements in litter size in second and fourth parity sows. It is suggested that the<br />
requirement is in excess of 175µg available biotin per kg of diet (7). In a swine herd with a<br />
lameness problem, the supplementation of the sow’s ration during pregnancy and lactation with<br />
daily intakes of biotin of 400 and 800µg/sow/d, respectively, and the rations of the weaners and<br />
growers to 150 and 250 was effective.<br />
Horses<br />
The dietary supplementation of horses with 10-30 mg biotin/d for 6-9 months is considered to be<br />
effective as an aid in the treatment of weak horn hoof in horses (9). The hoof horn quality of more<br />
than two-thirds of the Lipizzaner horses had moderate to severe changes: microcracks visible in<br />
the transition from the middle to the inner zone of the coronary horn; separation of the sole from<br />
the coronary horn in the region within the white zone. Biotin supplementation for 19 months<br />
improved horn quality (10). Continuous dietary supplementation with biotin at a daily dose of 20<br />
mg is necessary to improve and maintain hoof horn quality in horses with less than optimum<br />
quality hoof (11).<br />
REFERENCES<br />
(1)Misir,R.et al.(1986) Can.Vet.J.,60,106.<br />
(2)Thomas,K.W.et al.(1990) Ami.Vet.J.,67,215.<br />
(3)Johnston,A.M.& Penny,R.H.C.(1989) Vet.Rec,125,130.<br />
(4)Simmins,P.H.& Brooks,P.H.(1988) Vet.Rec,122,431.<br />
(5)Webb,N.G.et al.(1984) Vet.Rec,114,185.<br />
(6)Kempson,S.A.et al.(1989) Vet.Rec,124,37.<br />
(7)Simmins,P.H.& Brooks,P.H.(1983) Vet.Rec,112,415.<br />
(8)Kopinski.J.S.et al.(1989) Br.J.Nutr.,62,751,761,767,773, 781.<br />
(9)Comben,N.et al.(1984) Vet.Rec,115,642.<br />
(10)Zcnker,W.et al.(1995) Equine Vet.J.,21,183.<br />
(11)Josseck,H.et al.(1995) Equine Vet.J.,21,175.<br />
五、维生素 C 缺乏症(Vitamin C Deficiency)<br />
除了人及灵长类和豚鼠以外,大多数动物可以自己合成VC,在兽医临床中,天然VC缺<br />
乏症是很少见的。动物VC缺乏症,临床上表现皮肤、内脏出血,贫血,齿龈溃疡、坏死,<br />
关节肿胀,抗病能力下降。<br />
VC是白色结晶,易溶于水,微溶于乙醇和丙酮,0.5%的溶液为酸性(pH=3)。VC广泛<br />
存在于青绿植物中,但幼龄动物和猴、狗、猪有时可产生VC缺乏症。幼畜生后 10~21 天体<br />
内不能合成VC,须从母乳中获取,因此,母乳中含量不足或缺乏,均能引致幼畜发病。VC亦<br />
是强的还原剂,体内所产生的氧化物、过氧化物的毒性可被VC所缓解。VC还参予铁的吸收<br />
和转运、组织修补及伤口愈合。<br />
幼畜VC缺乏,可出现精神不振,食欲减损,病情发展可表现出血性素质,多发生于背<br />
92
和颈部,口腔及齿龈出血。进而形成溃疡,严重时颊和舌也发生溃疡或坏死,或齿糟萎缩致<br />
牙齿松动,甚至脱落。红细胞总数及血红蛋白量下降,逐渐发展为正色素性贫血,并伴发白<br />
细胞减少症。<br />
猪VC缺乏,表现重剧出血性素质,皮肤黏膜出血,坏死,口腔、齿龈、舌最明显。皮<br />
肤出血部位鬃毛软化易脱落,新生仔猪常发生脐管大出血,造成死亡。<br />
禽类嗉囔一般能合成部分VC,较少发病。但VC有较好的抗热性,可提高产蛋量,增加<br />
蛋壳强度,增加公鸡精液生成,增强抵抗感染能力。因此鸡饲料仍应补充VC,即使鸡不致<br />
产生VC缺乏症。<br />
猴VC缺乏与人类相似,齿龈出血,齿龈炎及牙齿松动,皮下微血管出血,特别是在受<br />
压、外伤的部位,可视黏膜、消化道、生殖器官和泌尿器官出血。人工制造的食品中常缺乏<br />
VC,因此小猴子易患VC缺乏症,常有胃口不好,体重减轻,四肢无力,补充蔬菜、水果、<br />
柠檬等,症状迅速改善。<br />
饲料中增加富含VC的青绿饲料,绿叶蔬菜,三叶草等。药物治疗:猪、羊给予VC0.2~0.5g<br />
皮下或静脉注射,连用 7 天,或口服VC片剂,仔猪 0.1~0.2g,成年猪、羊 0.5~l.0g,连用 15<br />
天。<br />
兽医临床实践中,特别是输液,改善血液循环状况时,常加入适量VC,可有助于多种<br />
疾病的治疗。有些尽管没有明显的VC缺乏症,但实践中配合VC治疗,对某些溶血性疾病、<br />
消化道疾病,创伤和手术后促进创口愈合,都取得较好的临床效果。<br />
VITAMIN K DEFICIENCY<br />
A primary deficiency of vitamin K is unlikely under natural conditions in domestic animals<br />
because of the high content of substances with vitamin K activity in most plants, and the<br />
substantial synthesis of these substances by microbial activity in the alimentary canal. Sporadic<br />
cases may occur when impairment of the flow of bile reduces the digestion and absorption of this<br />
fat-soluble vitamin. Experimentally produced vitamin K deficiency in piglets is manifested by<br />
hypersensitivity, anemia, anorexia, weakness, and a marked increase in prothrombi time. The<br />
minimum daily requirement for newborn pigs is 5 µg/kg BW, and the minimum curative injection<br />
dose is four times larger.<br />
A hemorrhagic disease of recently weaned pigs from 6 to 15 weeks of age is considered to be<br />
associated with vitamin K deficiency (1). Affected pigs fail to grow, become pale, develop large<br />
subcutaneous heniatomas, and exhibit lameness and epistaxis(1). Excessive and fatal hemorrhage<br />
following routine castration may occur in pigs from 30 to 40 days of age, but not at 15-20 days of<br />
age (2). Subcutaneous massive hemorrhage is more common in pigs at 40- 70 days of age.<br />
Prothrombin time and activated partial thromboplastin time are prolonged along with decreased<br />
levels of vitamin K-dependent factors II, VII, IX, and X (2). At necropsy, hemorrhages are<br />
extensive in the muscles of the hindlimbs, forelimbs, and axillar and mandibular region.<br />
Vitamin K, or vitamin K2, given at a dose of 3 mg/kg BW IM as a single dose will restore the<br />
blood coagulation. defects to normal (3). Vitamin K3 added to the feed at a rate of 25 mg/kg for 4<br />
days was also effective. The cause of the vitamin K deficiency was considered to be related to the<br />
use of antibacterial drugs in the feed but this has not been substantiated.<br />
The most important therapeutic use of vitamin K in domestic animals is in sweet clover<br />
poisoning where toxic quantities of coumarin severely depress the prothrombin levels of the blood<br />
and interfere with its clotting mechanism. Industrial poisons used in rodent control which contain<br />
anticoagulants of the coumarin type, e.g. warfarin, cause fatal hypothrombinemia; vitamin K is an<br />
effective antidote. For warfarin-induced anticoagulation in the horse, the administration of<br />
93
300-500 mg of vitamin K1 SC every 4-6 hours until the prothrombin time returns to baseline<br />
values is recommended (4).<br />
REVIEW LlTERA<br />
Mount,TURE M. E. & Feldman, B. F. (1982) Vitamin<br />
K and its importance. J. Am. Vet. Med.<br />
Assoc, 180, 1354-1356.<br />
REFERENCES<br />
(1)Newsholme, S. J. et al. (1986) J. South Afi.<br />
Vet. Assoc, 56, 101.<br />
(2)Sasaki, Y. ct al. (1982) Jap.J. Vet. Sci., 44,<br />
933.<br />
(3)Sasaki, Y. et al. (1985) Jap. J. Vet. Sci., 47,<br />
435.<br />
(4)Byars, T. D. et al. (1986) Am.J. Vet. Res.,<br />
47, 2309.<br />
第四节 常量元素营养紊乱性疾病<br />
(Nutritional Disorder of Major Elements)<br />
动物体内的矿物质主要来自地表土壤,动物体内矿物质的含量与地表土中矿物质丰度之<br />
间有惊人地相似之处,可以这么说,地表中的矿物元素在动物体内大致都可以发现。<br />
动物体内的矿物质元素,根据其含量多少,可分为常量元素和微量元素两大类,常量元<br />
素是指动物体内含量较多的元素,常以克或占动物体灰分中的百分数表示。除 C、H、O、<br />
N 以外,还有 Ca、P、Mg、K、Na、Cl、S 七种元素。<br />
疾病。<br />
本节着重介绍钙、磷代谢紊乱,镁缺乏,钾、钠缺乏或中毒,硫及含硫氨基酸缺乏症等<br />
一、钙、磷营养紊乱性疾病(Nutritional Disorder of Calcium and Phosphorous)<br />
钙、磷是动物体内含量最多的矿物质,约占动物灰分重量的 70%。钙、磷是体内硬组<br />
织的主要构成成分,体内 99%的钙、80%的磷存在于骨骼和牙齿中。<br />
钙是在十二指肠的近端吸收的,在VD的活性代谢产物作用下,肠黏膜细胞核染色质合<br />
成了钙结合蛋白,它在肠黏膜细胞刷状缘,有主动捕获肠腔内钙,在ATP作用下,使钙主动<br />
被吸收入血。据报道,VD也可促使小肠远端(空肠)吸收磷,在小肠内磷主要是从高浓度<br />
的肠内容物向低浓度的肠黏膜扩散而吸收。<br />
钙、磷吸收是在三种主要激素调节下进行的,其决定性因素是血钙浓度。VD的活性代<br />
谢产物可作为一种激素,调节钙的肠吸收和肾小管对钙的重吸收(详见VD),以维持血钙和<br />
体内总钙的平衡;当血钙浓度下降时,可促使甲状旁腺分泌甲状旁腺素,其一方面抑制尿钙<br />
排泄,促进钙的吸收,另一方面促进骨骼钙的重溶,增加血钙浓度,保持血钙恒定;当血钙<br />
浓度过高时,流经甲状腺的高钙血,促使甲状腺旁细胞分泌降钙素(calcitonin),它有使血<br />
钙向骨骼和牙齿沉积。在这三种激素作用下,使钙的吸收、沉着、重溶与排泄过程在严格的<br />
有序过程中进行。<br />
大多数动物在通常生理状态下,骨骼、牙齿、血浆内钙与磷的比例约保持在 2:l 的比例。<br />
迄今对磷的吸收与调节机制虽不完全清楚,但一般认为磷常在保持 Ca:P 为 2:1 的前题下,<br />
随钙的吸收而吸收,有相对的被动性。<br />
为了维持体内钙、磷代谢内环境的稳定,保持机体内钙、磷比例的相对稳定,要求饲料<br />
中钙、磷要有一定的量和比例。如果饲料中钙不足,或磷不足,或它们间的比例偏离 2:l~1:1<br />
94
的比值太远,或VD的量不足,就可能产生钙、磷代谢的紊乱。此外甲状腺、甲状旁腺的功<br />
能完好与否,肝、肾功能的正常与否,都可直接和间接影响体内钙、磷代谢。<br />
钙、磷代谢紊乱大致可分为三种类型:<br />
(1)器质性代谢紊乱 主要表现骨组织本身的疾病,如骨软症、佝偻病、纤维性骨营<br />
养不良、笼养鸡疲劳综合征、骨质疏松症、妊娠骨折。<br />
(2)机能性代谢紊乱 主要因血清钙或磷浓度下降,引起全身代谢紊乱,运动失调,<br />
而骨骼器质性变化不明显。如生产瘫痪、生产搐搦症、牛地方性血红蛋白尿、产后血红蛋白<br />
尿等。<br />
(3)钙磷的异位沉着 钙、磷或两者沉着在不该沉积的器官或组织,引起局部组织硬<br />
化、钙化、结石生成。如胆结石、肾结石、尿道结石、涎结石、胰结石、肠结石、禽的软组<br />
织的骨石化症、猫肺的泛在性骨化石化症、动脉粥样硬化、VD过多症等。<br />
(一)器质性钙、磷代谢紊乱疾病<br />
1.佝偻病(Rickets)佝偻病是年青、生长动物的疾病,其特点是生长骨骼钙化不良,软<br />
骨持久性肥大,骺端软骨增大和骨骼弯曲变形。临床表观为消化紊乱、异食癖、跛行、四肢<br />
呈罗圈腿或八字形外展,俗称拐子病。<br />
佝偻病可见于各种家禽、家畜,以雏禽、犊牛、羔羊、仔猪、犬、猫等发病较多。<br />
【病因】<br />
(1)VD缺乏 幼年动物,大多在户内喂养,体内VD主要从母乳中获得,依靠自己的皮<br />
肤制造的VD是很少的。断乳以后如饲料中供给VD不足,导致对钙、磷吸收障碍,这时,即<br />
使饲料中有充足的钙、磷,亦可酿成佝偻病。母乳中VD含量不足,或用代乳品饲喂,或母<br />
禽产蛋期VD缺乏,蛋中VD不足。可产生先天性或后天性VD缺乏所致佝偻病。<br />
(2)钙不足,磷不足,或两者都缺乏,或两者比例严重失调,都可酿成佝偻病,一般<br />
情况下,只要有足够量的VD,上述钙、磷含量和比例稍有偏差时,不会造成佝偻病。只有<br />
同时伴有VD不足,或VD处于临界生理需要时,上述钙、磷营养有偏差,或幼畜生长较快时,<br />
则可产生佝偻病<br />
区别。<br />
(3)猪有遗传性佝偻病 有母猪所生小猪,好发佝偻病,但与营养性佝偻病之间没有<br />
(4)长期腹泻,慢性肝、胆疾病,使VD的吸收、转化受阻,食物中锶、铍含量较高,<br />
这是因为它们可抑制肝、肾内羟化酶活性,从而导致VD活性化受阻,最终引起佝偻病。<br />
总的来说,由于钙、磷及其比例在骨代谢中的重要性已逐渐为人们所认识,临床型佝偻<br />
病发病率已大大下降。但是在某些特定条件下,有时发病率仍很高。如单纯的掠夺性放牧,<br />
在育肥场过度强化饲养,冬季过度依耐湿度大的草场放牧时易呈群发疾病。<br />
牛常因区域性缺磷时产生,幼畜原发性磷缺乏;舍饲犊牛,长期日照不足引起缺乏VD;<br />
羔羊虽不如犊牛对缺磷那么敏感,但长期在禾科牧草场放牧,冬季很少用黑麦草饲喂,可继<br />
发VD缺乏引起佝偻病。仔猪过度集约化饲喂,多在 2~4 月龄发病,因饲料中磷太多(麸皮、<br />
米糠含量多),伴有钙和VD不足时易发生。犬、猫因肾功衰竭而致肾性骨病时,易引起佝偻<br />
病。雏鸡暴露在外的皮肤很少,全部VD必须从饲料中供给,大多在 2~3 周龄时发生。多因<br />
VD补充不足而引起群发。<br />
【病理】 VD缺乏,钙吸收不足,血液中不能运送更多的钙盐向骨组织沉着,造成软<br />
骨内骨盐沉着不良。软骨肥大,骺端软骨增人。同时关节扩大,骨样组织增多。骨骼中钙含<br />
量从 66.33%降低到 18.2%,骨样组织从 30%增加到 70%。由于骨骼中钙盐不足,骨强度下<br />
降,常有骨骼弯曲、变形或形成罗圈腿或形成八字腿。血清无机磷浓度下降。<br />
【临床表现】 早期表现食欲减退,消化不良,随之可出现异食癖,经常卧地,不愿起<br />
立。发育停滞、消瘦。下颌骨增厚,出牙期延迟,齿形不规则。齿质钙化不足,坑凹不平,<br />
95
有沟,有色素沉着,常排列不齐,齿面易磨损不平整。严重时口腔不能闭合,舌突出,流涎,<br />
吃食困难。<br />
骨骼变形:表现在头面部、躯干和四肢骨骼变形。面骨肿胀,突起,站立时拱背,腕关<br />
节曲屈,呈内弧形;后肢跗关节内收,呈八字形。关节增大,仔猪关节轻度肿大,有的成为<br />
僵猪,严重者甚至瘫痪在地,幼禽(10~25 日龄)可出现喙变形,易弯曲,俗称橡皮喙。胫、<br />
跗骨易弯曲,胸骨脊-龙骨弯曲成 S 形。肋骨与肋软骨间及肋骨头与胸椎间有球形扩大,<br />
排列成串珠状。腿软弱无力,常以飞节着地,关节增大,严重者瘫痪,其它家畜亦有类似的<br />
肋骨与肋软骨联结处扩大。<br />
血清碱性磷酸酶活性常升高,无机磷浓度下降(
Differential diagnosis list:<br />
• Epiphysitis<br />
• Congenital and acquired abnormalities<br />
• Infectious synovitis.<br />
Treatment. Vitamin D injections, calcium and phosphate orally.<br />
Control. Supplement deficient diets with calcium, phosphorus, and vitamin D.<br />
ETIOLOGY<br />
Rickets is caused by an absolute or relative deficiency of any or a combination of calcium,<br />
phosphorus or vitamin D in young, growing animals. The effects of the deficiency are also<br />
exacerbated by a rapid growth rate.<br />
An inherited form of rickets has been described in pigs. It is indistinguishable from rickets<br />
caused by nutritional inadequacy.<br />
EPIDEMIOLOGY<br />
Clinical rickets is not as important economically as the subclinical stages of the various dietary<br />
deficiencies that produce it. The provision of diets adequate and properly balanced with respect to<br />
calcium, phosphorus, and sufficient exposure to sunlight, are mandatory in good livestock<br />
production. Rickets is no longer a common disease because these requirements are widely<br />
recognized, but the incidence can be high in extreme environments, including purely exploitative<br />
range grazing, intensive feeding in fattening units, and heavy dependence On lush grazing,<br />
especially in winter months.<br />
Rickets is a disease of young, rapidly growing animals and occurs naturally under the following<br />
conditions.<br />
Calves<br />
Primary phosphorus deficiency in phosphorus-deficient range areas, and vitamin D deficiency in<br />
calves housed for long periods are the common circumstances. Vitamin D deficiency is the most<br />
common form of rickets in cattle raised indoors for prolonged periods in Europe and North<br />
America. Grazing animals may also develop vitamin D deficiency rickets at latitudes where solar<br />
irradiation during winter is insufficient to promote adequate dermal photobiosynthesis of vitamin<br />
D3 from 7-dihydrocholesterol. Rickets has occurred in yearling steers in New Zealand wintered on<br />
swede (Brassica napus) crop deficient in phosphorus (1).<br />
In young, rapidly growing cattle raised intensively indoors a combined deficiency of calcium,<br />
phosphorus, and vitamin D can result in leg weakness characterized by stiffness, reluctance to<br />
move, and retarded growth. In some cases, rupture of the Achilles tendon and spontaneous<br />
fracture occur (2). The Achilles tendon may rupture at the insertion of, or proximal to, the<br />
calcaneus.<br />
Lambs<br />
Lambs are less susceptible to primary phosphorus deficiency than cattle, but rickets does occur<br />
under the same conditions. Green cereal grazing and, to a lesser extent, pasturing on lush rye-grass<br />
during winter months may cause a high incidence of rickets in lambs; this is considered to be a<br />
secondary vitamin D deficiency. An outbreak of vitamin D deficiency rickets involving 50% of<br />
lambs aged 6-12 months grazing new grass and rape occurred during the early winter months in<br />
Scotland (3). In the South Island of New Zealand, where winter levels of solar irradiation are low,<br />
rickets occurs in hoggets grazing green oats, or other green crops, which have been shown to<br />
contain high levels of rachitogenic carotenes (1).<br />
97
Pigs<br />
Rickets in young pigs occurs in intensive fattening units where the effects of diet containing<br />
excessive phosphate (high cereal diets) are exacerbated by vitamin D and calcium deficiencies.<br />
Foals<br />
Rickets is uncommon in foals under natural conditions, although it has been produced<br />
experimentally.<br />
PATHOGENESIS<br />
Dietary deficiencies of calcium, phosphorus, and vitamin D result in defective mineralization of<br />
the osteoid and cartilaginous matrix of developing bone. There is persistence and continued<br />
growth ot hypertroplnc epiphyseal cartilage, increasing the width of the epiphyseal plate. Poorly<br />
calcified spicules of diaphyseal bone and epiphyseal cartilage yield to normal stresses, resulting in<br />
bowing of long bones and broadening of the epiphyses with apparent enlargement of the joints.<br />
Rapidly growing animals on an otherwise good diet will be first affected because of their higher<br />
requirement of the specific nutrients.<br />
CLINICAL FINDINGS<br />
The subclinical effects of the particular deficiency disease will be apparent in the group of animals<br />
affected and have been described in the earlier general section. Clinical rickets is characterized by:<br />
• Stiffness in the gait<br />
• Enlargement of the limb joints, especially in the forelegs<br />
• Enlargement of the costochondral junctions<br />
• Long bones show abnormal curvature, usually forward and outward at the carpus in sheep and<br />
cattle<br />
• Lameness and a tendency to lie down for long periods.<br />
Outbreaks affecting 50% of a group of lambs have been described (3). Arching of the back and<br />
contraction, often to the point of virtual collapse, of the pelvis occur and there is an increased<br />
tendency for bones to fracture.<br />
Eruption of the teeth is delayed and irregular, and the teeth are poorly calcified with pitting,<br />
grooving, and pigmentation. They are often badly aligned, and wear rapidly and unevenly. These<br />
dental abnormalities, together with thickening and softness of the jaw bones, may make it<br />
impossible for severely affected calves and lambs to close their mouths. As a consequence the<br />
tongue protrudes, and there is drooling of saliva and difficulty in feeding. In less severely affected<br />
animals dental malocclusion may be a significant occurrence. Severe deformity of the chest may<br />
result in dyspnea and chronic ruminal tympany. In the final stages, the animal shows<br />
hypersensitivity, tetany, recumbency, and eventually dies of inanition.<br />
CLINICAL PATHOLOGY<br />
The plasma alkaline phosphatase is commonly elevated, but serum calcium and phosphorus levels<br />
depend upon the causative factor. If phosphorus or vitamin D deficiencies are the cause, the serum<br />
phosphorus level will usually be below the normal lower limit of 3 mg/dL. The serum<br />
concentrations of 25-hydroxyvitamin D3 and 25-hydroxyvitamin D2 are markedly decreased in<br />
vitamin D-deficient rickets compared with the normal values of≈ 5 ng/mL (3). Serum calcium<br />
levels will be low only in the final stages. In leg weakness of young, rapidly growing cattle, the<br />
serum concentration of 25-hydroxyvitamin D may be nondetectable and the serum levels of<br />
calcium and inorganic phosphorus may be low (2).<br />
Radiographic examination of bones and joints is one of the most valuable aids in the<br />
98
detection of rickets. Rachitic bones have a characteristic lack of density compared to normal bones.<br />
The ends of long bones have a 'woolly' or 'motheaten' appearance and have a concave or flat,<br />
instead of the normal convex, contour. Surgical removal of a small piece of costochondral junction<br />
for histological examination has been used extensively in experimental work and should be<br />
applicable in field diagnosis.<br />
NECROPSY FINDINGS<br />
Apart from general poorness of condition, the necropsy findings are restricted to abnormal bones<br />
and teeth.The bone shafts are softer and larger in diameter,due in part to the subperiosteal<br />
deposition of osteoid tissue. The joints are enlarged, and on cutting, the epiphyseal cartilage can<br />
be seen to be thicker than usual. Histological examination of the epiphysis is desirable for final<br />
diagnosis. In sheep, the best results are obtained from an examination of the distal cartilages of the<br />
metacarpal and metatarsal bones.<br />
A valuable diagnostic aid is the ratio of ash to organic matter in the bones. Normally the ratio is<br />
three parts of ash to two of organic matter but in rachitic bone this may be depressed to 1:2, or 1:3<br />
in extreme cases. A reduction below 45% of the bone weight as ash also suggests osteodystrophy.<br />
Because of the difficulty encountered in repeating the results of bone ash determinations, a<br />
standardized method has been devised in which the ash content of green bone is determined, using<br />
either the metacarpus or metatarsus, and the ash content related to the age of the animal, as<br />
expressed by the length of the bone. Although normal standards are available only for pigs, the<br />
method suggests itself as being highly suitable for all species.<br />
Samples for confirmation of diagnosis<br />
• Toxicology - long bone (ASSAY(ash)); 500 g feed (ASSAY (Ca) (P)(Vit D))<br />
•Histology - formalin-fixed long bone (including growth plate) (LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
Rickets occurs in young, rapidly growing animals and is characterized by stiffness of the gait and<br />
enlargement of the distal physes of the long bones, particularly noticeable on the metacarpus and<br />
metatarsus as circumscribed painful swellings. A history of a dietary deficiency of any of calcium,<br />
phosphorus, or vitamin D will support the clinical diagnosis. Radiographic evidence of widened<br />
and irregular physes suggests rickets. Copper deficiency in young cattle under 1 year of age can<br />
also result in clinical, radiographic, and pathological findings similar to rickets. Clinically, there is<br />
an arched back, severe stiffness of gait, reluctance to move, and loss of weight. There are marked<br />
swellings of the distal aspects of metacarpus and metatarsus, and radiographically there is a<br />
widened zone of cartilage and lipping of the medial and lateral areas of the physeal plate. Copper<br />
concentration in plasma and liver are low and there is usually dietary evidence of copper<br />
deficiency.<br />
Epiphysitis occurs in rapidly growing yearling cattle raised and fed intensively under<br />
confinement. There is severe lameness, swelling of the distal physes, and radiographic and<br />
pathological evidence of a necrotizing epiphysitis. The etiology is uncertain but thought to be<br />
related to the type of housing.<br />
Congenital and acquired abnormalities of the bony skeletal system are frequent in newborn<br />
and rapidly growing foals. Rickets occurs, but only occasionally. 'Epiphysitis' in young foals<br />
resembles rickets and is characterized by enlargements and abnormalities of the distal physes of<br />
the radius, tibia, third metacarpal and metatarsal bones, and the proximal extremity of the<br />
proximal phalanx. There may or may not be deviation of the limbs caused by uneven growth rates<br />
99
in various growth plates. The suggested causes include improper nutrition, faulty conformation<br />
and hoof growth, muscle imbalance, overweight, and compression of the growth plate. Recovery<br />
may occur spontaneously or require surgical correction.<br />
Rickets in swine is uncommon and the diagnosis may be difficult. The disease is usually<br />
suspected in young, rapidly growing swine in which there is stiffness in the gait, walking on<br />
tiptoes, enlargements of the distal ends of long bones, and dietary evidence of a marginal<br />
deficiency of calcium or phosphorus. The radiographic and pathological findings may suggest a<br />
rickets-like lesion.<br />
Mycoplasmaj synovitis and arthritis clinically resemble rickets of pigs. There is a sudden<br />
onset of stiffness of gait, habitual recumbency, a decrease in feed consumption, and enlargements<br />
of the distal aspects of the long bones which may or may not be painful, spontaneous recovery<br />
usually occurs in 10-14 days. The locomotor problems in young, growing pigs raised in<br />
confinement and with limited exercise must be considered in the differential diagnosis. In<br />
performance testing stations, up to 20% of boars may be affected with leg weakness.<br />
Rickets in lambs must be differentiated from chlamydial and erysipelas arthritis, which are<br />
readily diagnosed at necropsy.<br />
TREATMENT AND CONTROL<br />
Recommendations for the treatment of the individual dietary deficiencies (calcium, phosphorus,<br />
and vitamin D) are presented under their respective headings. Lesser deformities recover with<br />
suitable treatment but gross deformities usually persist. A general improvement in appetite and<br />
condition occurs quickly, and is accompanied by a return to normal blood levels of phosphorus<br />
and alkaline phosphatase. The treatment of rickets in lambs with vitamin A, vitamin D3, calcium<br />
borogluconate solution containing magnesium and phosphorus parenterally, and supplementation<br />
of the diet with bone meal and protein resulted in a dramatic response (3) Recumbent animals<br />
were walking within a few days.<br />
REFERENCES<br />
(1)Thompson, K. G. & Cook, T. G. (1987)<br />
NZ Vet.J., 35, 11.<br />
(2)Sturen, M. (1985) Acta Vet. Scand., 26, 169.<br />
(3)Bonniwell, M. A. et al. (1988) Vet. Rec,<br />
122, 386.<br />
2.骨软症(Osteomalacia) 骨软症是指成年动物,当软骨内矿化作用完成后发生的<br />
一种骨营养不良。骨盐的吸收作用大于骨盐沉积作用,骨骼中钙、磷重新动员入血,呈现骨<br />
质疏松和形成过多的末钙化的骨基质,临床上表现跛行,骨折,异食癖和消化紊乱。<br />
骨软症可发生于各种动物及驯养的野生动物,乳牛、黄牛、绵羊最易发生,山羊、猪和<br />
马的骨软症则以纤维性骨营养不良为特征。水牛、黄牛因缺磷而发生跛行也应属这一范畴,<br />
但有时表现血红蛋白尿。<br />
【病因】 一般说来骨软症发生原因与佝偻病类似,但骨软症常发生于泌乳的牛和妊<br />
娠后期。我国动物骨软症,特别是乳牛和黄牛骨软症的发病原因主要有:<br />
(1)饲料中磷供给不足,钙、磷比例严重失调。许多乳牛场愿意给母牛补充石粉,贝<br />
壳粉等,而骨粉价格明显高于石粉,有些人非法向骨粉中掺入石粉,因而造成饲料中钙、磷<br />
比例严重失调,有人曾对几个大型乳牛牛场监测,饲料中钙、磷的比值(Ca:P)为 6.8:1。<br />
易诱发本病。<br />
100
我国有许多地区属缺磷地区,苏北、皖北、洛阳、黑龙江西部、山西、陕西等省常有因<br />
缺磷后,耕牛、乳牛产生跛行,关节肿大现象,饲料中钙:磷多在(4~5):1,有的甚至为 10:1,<br />
因而产生骨软症,茸鹿、猕猴,鸡、鸭饲料中缺磷亦可产生瘫痪,脚无力,鸭甚至溺死水中。<br />
许多研究表明,当饲料中 Ca:P7 时,可迅速产生骨软症。<br />
当地方性低磷时,亦可产生地方性血红蛋白尿,据赵锡荣等(1991 年)报道,在 11266<br />
头低磷血症牛统计中,骨软症占 98%,地方性血红蛋白尿仅占 1.08%,混合型占 1.4%,尤<br />
其是大涝之后大旱,最易使牛产生骨软症。猪缺磷引起瘫痪亦有报道。<br />
(2)钙、磷同时缺乏或VD缺乏 曾有因第一年水灾,第二年春发生马、黄牛骨软症报<br />
道,由于饲料中磷含量(绝对量)过低,Ca:P达 27。5:1。这时马所表现的不属纤维性骨营养<br />
不良,而是骨软症。VD缺乏在牛的骨软症发生中有较大意义,因为成年牛和狗肾脏疾病,<br />
可致大批牛发生骨软症,犬也散发该病。这可能与VD转化为活性代谢产物,1。25-二羟钙化<br />
醇不足有关。<br />
(3)妊娠后期或产仔太多,乳钙消耗太多等,可酿成骨软症。<br />
【病理】 由于磷过少,体内(骨、血)钙、磷是按照一定比例构成的,当磷太低即使<br />
日粮中有充足的钙,因不成比例,钙的吸收不充分,或因泌乳、妊娠等引起钙的内源性排泄<br />
增多,间接地刺激了甲状旁腺素的分泌,促使骨骼中钙盐重吸收,维持血磷浓度和血钙浓度,<br />
满足妊娠、泌乳、内源性代谢的需求。已经完成了矿化作用的骨骼,呈进行性脱钙,骨中骨<br />
样组织增多,骨密度下降,骨骼硬度不足,当受外力打击,突然负重,滑脱,跌倒时易产生<br />
骨折。<br />
钙缺乏、VD缺乏的结果,钙的吸收量减少,血钙浓度下降的同时,促使甲状旁腺素分<br />
泌。又因VD缺乏,转化为活性代谢产物不足以代偿性地增加钙吸收,减少钙排泄的需要。<br />
骨盐溶解速度加快,最终骨质疏松,骨强度下降。<br />
现代研究证实,骨骼进仃性脱钙,头、面部及脊椎变化最明显,可出现面骨变形,下颌<br />
间隙缩小。四肢骨越是近心端,骨骼受损越严重。因此,动物的骨折,以腰椎、骨盆骨最易<br />
受害。<br />
【临床表现】 早期症状易被忽视或被误认为前胃弛缓,或创伤性网胃炎,继而出现异<br />
食癖,如咀嚼垫草,啃咬骨头,吞食胎衣等,渐渐地呈现跛行,骨关节疼痛,步样强拘,后<br />
躯摇摆,游走性跛行(轮跛)。卧地后不愿起立,某些母牛还可产生蹄病,腱滑脱,有的呈<br />
犬坐姿势。<br />
骨骼变形,脊柱上凸或腰荐下凹,腰椎横突富于弹性,甚至引起腰椎横突骨折,肋骨吸<br />
收。在 3~5 肋与肋软骨处有隆凸,末稍尾椎可有程度不同地被吸收,甚至可将尾盘起来,病<br />
牛不显痛苦。黄牛表现头骨变形,面骨抵抗力下降,异食、腰背疼痛,肢体僵硬。最后两节<br />
尾椎骨消失,跗关节、腕关节肿大。<br />
无论是乳牛、黄牛还是水牛,于妊娠后期、泌乳高峰期,其跛行、骨变形更为明显,俗<br />
称乳跛。最后长时间躺卧,因饥饿而衰竭。<br />
猪断乳以后,或产前产后母猪,因缺乏钙引起瘫痪,肢、体变形,持续疼痛和异嗜为主。<br />
头骨变形,上颌骨肿胀,颚突出,口腔闭合困难。<br />
雏鸡、雏鸭因缺磷可引起肢无力,驱赶时摇摆不定,常常以跗关节着地。病程长者,关<br />
节肿大,腿骨变形。腿朝内或向外弯。剖检可见消瘦,龙骨弯曲、质软,腿骨变弯,骨骼变<br />
脆(日粮中钙占 1.1078%,磷占 0.3066%,有效磷远低于鸡标准)。股骨、小腿骨密度变薄,<br />
长骨两端关节头增大,关节面呈羊毛状。<br />
临床病理学变化:牛、猪、禽均有血钙浓度升高,血磷浓度下降,血钙浓度可达<br />
3.5~4.6mmol/L(14~18.5mg/100m1),血磷浓度可从正常时 1.61~2.26mmol/L 下降至<br />
0.77~1.81mmol/L,血清碱性磷酸酶活性升高。<br />
101
【诊断】 妊娠后期,泌乳过程中出现消化不良、异食癖及骨骼变形者,配合日粮组成<br />
的分析及从治疗效果看,不难识别。碱性磷酸酶活性升高,血磷浓度下降,血钙浓度正常或<br />
升高等,有助于诊断。额骨穿刺及骨硬度测定,对揭示疾病中期或后期有显著意义。X 线骨<br />
密度测定及骨影相分析,对早期发现亚临床状态,估计病情、病性有其优越性。干骺端密度<br />
下降,骨影模糊,呈蛾蚀状,脱钙时,末端尾椎可被吸收等现象,可作进一步诊断。但应与<br />
氟骨症、风湿症,蹄病,低镁血症等相区别。<br />
在猪、骨软症应与椎体脓肿压迫脊髓和由猪丹毒引起的慢性关节炎等相区别。<br />
常见并发症有四肢和腰椎关节扭伤,跟腱剥脱,病理性骨折,久卧不起者有褥疮,甚至<br />
引发败血症。<br />
【防治】 在呈现异食癖阶段,及时补充骨粉可不药而愈,牛每天 250g,5~7 天为一<br />
疗程。严重病例(跛行、骨变性)除给予骨粉外,还应补充磷。以 20%磷酸二氢钠 300~500ml<br />
静脉注射或 3%次磷酸钙 1000ml 静脉注射,每天一次,连续 3~5 天,依病情而定。<br />
补充VA、VD有利于病情恢复,同时服用磷酸二氢钠,增加麸皮、米糠的供给。<br />
日粮中应经常注意调正钙、磷比例。乳牛 2~1.5:1,干乳期即在泌乳前 14 天,改为 0.7~0.8:1<br />
以调动甲状旁腺功能。分娩后恢复到 1.5~2:1,黄牛 2.5:1,猪 1~1.5:1。蛋鸡 6.5:1,特别是<br />
发生干旱、水灾之后,更应注意。添加矿物质时,可供选用的矿物质有南京石粉,贝壳粉,<br />
骨粉,脱氟磷酸钙等。<br />
OSTEOMALACIA<br />
Osteomalacia is a disease of mature animals affecting bones in which endochondral ossification<br />
has been completed. The characteristic lesion is osteoporosis and the formation of excessive<br />
uncalcified matrix. Lameness and pathological fractures are the common clinical findings.<br />
Synopsis<br />
Etiology. Absolute or relative deficiency of any one or combination of calcium, phosphorus, and<br />
vitamin D in adult animals.<br />
Epidemiology. Primarily in cattle and sheep on phosphorus-deficient diets. In feedlot animals due<br />
to excessive phosphorus without complementary calcium and vitamin D.<br />
Signs. Reduced productivity, licking and chewing inanimate objects, stiff gait, moderate non<br />
specific lameness, shifting from leg to leg, crackling sounds while walking, arched back, lying<br />
down for long periods. 'Milk lameness' in high-producing dairy cows on deficient diet<br />
Clinical pathology. Increased alkaline phosphatase, decreased serum phosphorus levels.<br />
Decreased density of long bones radiographically.<br />
Lesions. Decreased density of bones, erosions of articular cartilages.<br />
Diagnostic confirmation. Histology of bones.<br />
Differential diagnosis list:<br />
•Chronic fluorosis<br />
•Polysynovitis and arthritis<br />
•Spinal cord compression.<br />
Treatment. As for calcium, phosphorus, and vitamin D deficiency.<br />
Control. Adequate supplementation of diet.<br />
ETIOLOGY<br />
In general, the etiology and occurrence of osteomalacia are the same as for rickets except that the<br />
predisposing cause is not the increased requirement of growth but the drain of lactation and<br />
pregnancy.<br />
EPIDEMIOLOGY<br />
102
Osteomalacia occurs in mature animals under the same conditions and in the same areas as rickets<br />
in young animals, but is recorded less commonly. Its main occurrence is in cattle in areas seriously<br />
deficient in phosphorus. It is also recorded in sheep, again in association with hypophosphatemia.<br />
In pastured animals, osteomalacia is most common in cattle, and sheep raised in the same area are<br />
less severely affected. In feedlot animals, excessive phosphorus intake without complementary<br />
calcium and vitamin D is likely as a cause, especially if the animals are kept indoors. It also occurs<br />
in sows that have recently weaned their pigs after a long lactation period (6-8 weeks) while on a<br />
diet deficient usually in calcium. A marginal deficiency of both phosphorus and vitamin D will<br />
exaggerate the condition.<br />
PATHOGENESIS<br />
Increased resorption of bone mineral to supply the needs of pregnancy, lactation, and endogenous<br />
metabolism leads to osteoporosis and weakness and deformity of the bones. Large amounts of<br />
uncalcified osteoid are deposited about the diaphyses. Pathological fractures are commonly<br />
precipitated by sudden exercise or handling of the animal during transportation.<br />
CLINICAL FINDINGS<br />
Ruminants<br />
In the early stages, the signs are those of phosphorus deficiency, including lowered productivity<br />
and fertility and loss of condition. Licking and chewing of inanimate objects begins at this stage<br />
and may : bring their attendant ills of oral, pharyngeal and esophageal obstruction, traumatic<br />
reticuloperitonitis, lead poisoning, and botulism.<br />
The signs specific to osteomalacia are those of a painful condition of the bones and joints, and<br />
include a stiff gait, moderate lameness often shifting from leg to leg, crackling sounds while<br />
walking, and an arched back.The hindlegs are most severely affected and thehocks may be rotated<br />
inwards.The animals are disinclined to move, he down for long periods,and are<br />
unwilling togetup.The colloquial names 'pegleg' ,creeps' , 'stiffs', 'cripples' and 'bog-lame' describe<br />
the. syndrome aptly.The names and 'milk-lameness' are commonly applied to the condition when<br />
it occurs in heavily milking 'milkleg' cows. Fractures of bones and separation of tendon<br />
attachments occur frequently, often without apparent precipitating stress. In extreme cases,<br />
deformities of bones occur, and when the pelvis is affected dystocia may result. Finally, weakness<br />
leadsto permanent ; recumbency and death from starvation.<br />
Swine<br />
Affected sows are usually found recumbent and unable to rise from lateral recumbency or from<br />
the dog-sitting position. The shaft of one femur or the neck of the femur is commonly fractured.<br />
The fracture usually occurs within a few days following weaning of the pigs. The placing of the<br />
sow with other adult pigs usually results in some fighting and increased exercise, which<br />
commonly precipitates the pathological fractures.<br />
CLINICAL PATHOLOGY<br />
In general, the findings are the same as those for rickets, including increased scrum alkaline<br />
phosphatase and decreased serum phosphorus levels. Radiographic examination of long bones<br />
shows decreased density of bone shadow.<br />
NECROPSY FINDINGS<br />
It can be difficult to discern any gross changes as the epiphyses are seldom enlarged and the<br />
altered character of cancellous bone may not be macroscopically visible. Cortical bone may be<br />
somewhat thinned and erosions of the articular cartilages have been recorded in cattle suffering<br />
103
from primary phosphorus deficiency. The parathyroid glands maybe enlarged. Histologicially ,<br />
abnormal ostoid covers trabeculae and a degree of fibrous tissue proliferation is often evident.<br />
Analysis reveals the bones to be lighter than normal with a low ratio of ash to organic matter.<br />
Samples for confirmation of diagnosis<br />
•Toxicology – long bone (ASSAY (ash)); 500 g feed(ASSAY (Ca) (P) (Vit D))<br />
•Histology - formalin-fixed bone, parathyroid(LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
The occurrence of non-specific lameness with pathological fractures in mature animals should<br />
arouse suspicion of osteomalacia. There may be additional evidence of subnormal productivity<br />
and reproductive performance, and dietary evidence of a recent deficiency of calcium, phosphorus,<br />
or vitamin D.<br />
A similar osteoporotic disease of cattle in Japan has been ascribed to a dietary deficiency of<br />
magnesium. The cattle are on high-concentrate , low-roughage diets, have high serum calcium<br />
and alkaline phosphatase levels, but a low serum magnesium level. The osteoporosis is observable<br />
at slaughter and clinical signs observed are those of intercurrent disease,especially ketosis, milk<br />
fever, and hypomagnesemia. Reproductive and renal disorders occur concurrently.<br />
In cattle it must be differentiated from chronic fluorosis in mature animals, but the typical<br />
mottling and pitting of the teeth and the enlargements on the shafts of the long bones are<br />
characteristic. In some areas, e.g. northern Australia, where the water supply is obtained from<br />
deep subartesian wells, the two diseases may occur concurrently. Analysis of water supplies and<br />
foodstuffs for fluorine may be necessary in doubtful cases.<br />
In sows, osteomalacia with or without pathological fractures must be differentiated from spinal<br />
cord compression due to a vertebral body abscess and chronic arthritis due to erysipelas.<br />
TREATMENT AND CONTROL<br />
Recommendations for the treatment and control of the specific nutritional deficiencies have been<br />
described under their respective headings. Some weeks will elapse before improvement occurs<br />
and deformities of the bones are likely to be permanent.<br />
3。纤维性骨营养不良(Osteodystrophi Fibrosa) 纤维性骨营养不良是因饲料中磷过多,<br />
钙含量正常或钙不足,而引起马族动物、猪、山羊的一种骨代谢紊乱性疾病。骨盐的吸收作<br />
用大于骨盐沉积作用,引起骨质疏松,骨体积增大,骨盐与骨基质比例下降。与骨软症类似,<br />
在临床上引起异食癖、跛行、骨变形、易骨折等。所不同的是骨软症中形成过多的骨样组织,<br />
其中缺乏成骨细胞;而本病中形成细胞含量丰富的软而细的白纤维。<br />
在发生。<br />
马族动物纤维性骨营养不良常呈地方流行性,冬春发病多,夏秋发病少,其它动物呈散<br />
本病发生原因是用麸皮、米糠或麸皮加稻(麦)草饲喂,因麸皮、米糠中Ca:P分别为<br />
1:5 或 1:17.75,很易诱发本病,猪以麸皮、米糠作为主食,同时缺乏VD时易发生本病。<br />
长期过劳或长期休闲可助长本病发生,饲料中草酸盐含量过多,长期大量用水浮莲饲喂<br />
亦可诱发猪的纤维性骨营养不良,可能与形成不溶性草酸钙而被排泄有关。钙、磷摄入和<br />
VD供给均不足,亦可导致本病。<br />
本病发生与代偿性甲状旁腺机能亢进或狗的原发性甲状旁腺肿瘤所致甲状旁腺素分泌<br />
过多有关,在高饲料磷、高血磷作用下,间接地刺激甲状旁腺素分泌,骨盐重溶,肾脏磷排<br />
泄增多。破骨过程先发生于骨皮质,呈现局限性骨质吸收,进一步在长骨骺端,肋骨与肋软<br />
骨交界处,头骨、下颌骨等处,引起骨疏松,骨体积增大,骨小梁破坏,在细纤维内有大量<br />
104
的破骨细胞和起破骨作用的巨细胞存在。<br />
纤维性骨营养不良的临床表现与骨软症相似(日本至今仍称该病为骨软症)。开始表现<br />
异嗜癖、跛行、拱背、面骨及四肢关节骨增大,尿澄清透明。下颏间隙因下颌骨增大而变小。<br />
接着出现轻度跛行,以后逐渐加重呈四肢轮跛。因跛行,动物易跌倒,甚至骨折。因椎骨增<br />
大,腰荐运动不灵活,出现板腰。跗关节增大,鼻甲骨窿起,严重者面部呈圆筒状。下颌骨<br />
疏松,以至出现臼齿陷入齿槽中,常有咀嚼障碍或吐草现象。骨穿刺时很容易进针、X线检<br />
查,尾骨皮质薄,颅骨表面粗糙,骨质密度不匀,掌骨产生外生骨疣。猪患病症状与马类似,<br />
严重病例亦可出现头面部肿胀,腿骨弯曲。<br />
鹿因饲喂高磷饲料,亦可出现与骨软症十分类似的症状。起卧缓慢,后肢无力,后躯摇<br />
摆,进而后肢负重困难。极易跌倒,骨质疏松,骨骼中 Ca:P 为 1:5.18。<br />
犬缺钙时,下颌骨、颅骨变化显著,由于骨盐从下颌骨内重吸收增多,犬的牙齿可陷入<br />
下颌骨或很易拔出。严重时肋骨、椎骨变形,骨密度下降。<br />
本病诊断与骨软症类似。<br />
防治主要依调整钙、磷比例,增加钙含量。实践证明,只要在饲料中添加南京石粉,使<br />
Ca:P 为 1:1,或在精料中掺入 10%的石粉,经饲喂一段时间后,马的尿由清转为混浊的黄白<br />
色,表明已凑效。再维持一定时间(例如一周),严格将饲料中总的钙、磷调正到 1:1 水平,<br />
不应低于 1:1.4。<br />
但石粉不宜补充太多。因石粉中几乎全都是碳酸钙,钙含量占 40%。钙太多,不仅可<br />
使磷相对减少,引起继发性缺磷,而且钙可干扰多种微量元素的吸收,造成继发性疾病。在<br />
各种动物精料中,控制其中的钙含量在 0.5%~1.0%左右,有效磷含量在 0.45%左右。而泌<br />
乳牛、产蛋鸡则应根据需要,另行补充。<br />
OSTEODYSTROPHIA FIBROSA<br />
Osteodystrophia fibrosa is similar in its pathogenesis to osteomalacia, but differs in that soft,<br />
cellular, fibrous tissue is laid down as a result of the weakness of the bones instead of the<br />
specialized uncalcified osteoid tissue of osteomalacia. It occurs in horses, goats, and swine.<br />
ETIOLOGY<br />
A secondary calcium deficiency due to excessive phosphorus feeding is the common cause in<br />
horses and probably also in pigs. The disease can be readily produced in horses on diets with a<br />
ratio of calcium:phosphorus of 1 :2.9 or greater, irrespective of the totalcalcium intake.<br />
Calcium :phosphoru ratios of 1:0.9 to 1:1.4 have been shown to be preventive and curative. With a<br />
very low calcium intake of 2-3 g/day and a calcium: phosphorus ratio of 1: 13 the disease may<br />
occur within 5 months. With a normal calcium intake of 26 g/day and a calcium: phosphorus ratio<br />
of 1:5, obvious signs appear ; in about 1 year, but shifting lameness may appear as early as 3<br />
months. The disease is reproducible in pigs on similar diets to those described above and also on<br />
diets low in both calcium and phosphorus. The optimum calcium: phosphorus ratio is 1.2:1 and<br />
the intake for pigs should be within the rangeof 0.6-1.2%of the diet.<br />
EPIDEMIOLOGY<br />
Osteodystrophia fibrosa is principally a disease of horses and other Equidae, and to a lesser extent<br />
of pigs. It has also occurred in goats. Amongst horses, those engaged in heavy city work and in<br />
racing are more likely to be affected because of the tendency to maintain these animals on<br />
unbalanced diets. The major occurrence is in horses fed a diet high in phosphorus and low in<br />
calcium. Such diets include cereal hays combined with heavy gram or bran feeding. Legume hays,<br />
because of their high calcium content, are preventive.<br />
The disease may reach endemic proportions in army horses moved into new territories, whereas<br />
105
local horses, more used to the diet, suffer little. Although horses may be affected at any age after<br />
weaning it is the 2-7-year age group that suffer most, probably because they are the group most<br />
likely to be exposed to the rations that predispose to the disease.<br />
A novel occurrence has been recorded of an endemic form of the disease affecting large<br />
numbers of horses at pasture. The dietary intake of calcium and phosphorus, and their proportions,<br />
were normal. The occurrence was thought to be due to the continuous ingestion of oxalate in<br />
specific grasses: Cenchrus ciharis, Panicum maximum var. trichoglume, Setaria anceps,<br />
Brachiaria mutica and Pennisetum clandestinum.<br />
PATHOGENESIS<br />
Defective mineralization of bones follows the imbalance of calcium and phosphorus in the diet,<br />
and a fibrous dysplasia occurs. This may be in response to the weakness of the bones or it may be<br />
more precisely a response to hyperparathyroidism stimulated by the excessive intake of<br />
phosphorus. The weakness of the bones predisposes to fractures and separation of muscular and<br />
tendinous attachments. Articular erosions occur commonly and displacement of the bone marrow<br />
may cause the development of anemia.<br />
CLINICAL FINDINGS<br />
Horse<br />
As in most osteodystrophies, the major losses are probably in the early stages before clinical signs<br />
appear or on diets where the aberration is marginal. In horses, a shifting lameness is characteristic<br />
of this stage of the disease and arching of the back may sometimes occur. The horse is lame, but<br />
only mildly so, and in many cases no physical deformity can be found by which the seat of<br />
lameness can be localized. Such horses often creak badly in the joints when they walk. These<br />
signs probably result from relaxation of tendon and ligaments and appear in different limbs at<br />
different times. Articular erosions may contribute to the lameness. In more advanced cases severe<br />
injuries, including fracture and visible sprains of tendons, may occur but these are not specific to<br />
osteodystrophia fibrosa, although their incidence is higher in affected than in normal horses.<br />
Fracture of the lumbar vertebrae while racing has been known to occur in affected horses.<br />
The more classical picture of the disease has largely disappeared because cases are seldom<br />
permitted to progress to this advanced stage. Local swelling of the lower and alveolar margins of<br />
the mandible is followed by soft, symmetrical enlargement of the facial bones, which may become<br />
swollen so that they interfere with respiration (1). Initially these bony swellings are firm and<br />
pyramidal and commence just above and anterior to the facial crests.The lesions are bilaterally<br />
symmetrical. Flattening of the ribs may be apparent, and fractures and detachment of ligaments<br />
occur if the horse is worked. There may be obvious swelling of joints and curvature of long bones.<br />
Severe emaciation and anemia occur in the final stages.<br />
Swine<br />
In pigs, the lesions and signs are similar to those in the horse and in severe cases pigs may be<br />
unable to rise and walk, show gross distortion of limbs, and enlargement of joints and the face. In<br />
less severe cases there is lameness, reluctance to rise, pain on standing, and bending of the limb<br />
bones, but normal facial bones and joints. With suitable treatment the lameness disappears, but<br />
affected pigs may never attain their full size. The relationship of this disease to atrophic rhinitis is<br />
discussed under the latter heading.<br />
CLINICAL PATHOLOGY<br />
106
There are no significant changes in blood chemistry in horses affected with severe osteodystrophia<br />
fibrosa. However,the serum calcium level will tend to be lower than normal, the serum inorganic<br />
phosphorus higher than normal, and the alkaline phosphatase activity higher than normal. The<br />
levels of diagnostic alkaline phosphatase have not been determined. Affected horses may be<br />
unable to return their serum calcium levels to normal following the infusion of a calcium salt.<br />
Radiographic examination reveals increased translucency of bones.<br />
NECROPSY FINDINGS<br />
The entire skeleton is abnormal in this severe form of metabolic bone disease, but the change is<br />
most notable in the mandibular, maxillary and nasal bones, which may appear thickened and<br />
distorted. The fleshy tissue that replaces normal cancellous bone in these sites is also present in<br />
the metaphyses of the long bones. Microscopically, there is proliferation of fibrous tissue and<br />
markedly increased osteoclast activity along thinned and abnormally oriented bony trabeculae.<br />
The parathyroid glands are enlarged. It must be remembered that osteodystrophia fibrosa is a<br />
lesion, not a disease. The pathway to this lesion usually involves a dietary unbalance in calcium<br />
and phosphorus, but the kidneys should also be examined to rule out the possibility of renal<br />
secondary hyperparathyroidism.<br />
Samples for confirmation of diagnosis<br />
•Toxicology -bone(ASSAY(ash));500 g feed (ASSAY (ca) (P) (Vit D))<br />
•Histologyformalin-fixed bone,parathyroid gland, kidney (LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
In the early stages, the diagnosis may be difficult because of the common occurrence of traumatic<br />
injuries to horses' legs. A high incidence of lameness in a group of horses warrants examination<br />
of the ration and determination of their calcium and phosphorus status. An identical clinical<br />
picture has been described in a mare with an adenoma of the parathyroid gland. Inherited<br />
multiple exostosis has been described in the horse.<br />
In pigs, osteodystrophia can be the result of hypovitaminosis A, and experimentally as a result of<br />
manganese deficiency.<br />
TREATMENT AND CONTROL<br />
A ration adequately balanced with regard to calcium and phosphorus<br />
(calcium:phosphorus should be in the vicinity of 1:1 and not wider than 1:1.4) is preventive in<br />
horses and affected animals can only be treated by correcting the existing imbalance. Even severe<br />
lesions may disappear in time with proper treatment. Cereal hay may be supplemented with alfalfa<br />
or clover hay, or finely ground limestone (30 g daily) should be fed. Dicalcium phosphate or bone<br />
meal are not as efficient because of their additional content of phosphorus.<br />
REFERENCE<br />
(1) Clarke, C.J. et al. (1996) Vet. Rec., 138, 568.<br />
'BOWIE' OR 'BENTLEG'<br />
This is a disease of lambs of unknown etiology. There is a characteristic lateral curvature of the<br />
long bones of the front legs, but the lesions differ from those of ricket. It has been observed only<br />
on unimproved range pasture in New Zealand. The cause is unknown, although phosphorus<br />
deficiency has been suggested.<br />
Improvement of the pasture by top-dressing with superphosphate and sowing-improved grasses<br />
is usually followed by disappearance of the disease.Only sucking lambs are affected and cases<br />
occur only in the spring at a time when rickets does not occur. Up to 40% of a group of lambs may<br />
107
e affected without breed differences in incidence. A similar syndrome has been produced by the<br />
feeding of wild parsnip (Trachemene glautifolia) and, experimentally, by the feeding of a diet low<br />
in both calcium and phosphorus.<br />
The disease has also been reported from South Africa where it occurs primarily in ram lambs<br />
and develops from as early as 3 months up to 1 year of age (1). There is gradual bending of the<br />
forelimbs with hooves turned inwards and the carpal joints turned outwards. Animals of the South<br />
African Mutton Merino breed had significantly higher plasma phosphorus concentrations than<br />
those of the Merino and Dohne Merino breeds. The plasma calcium: phosphorus ratio was lower<br />
in affected lambs and their ewes, and this converse ratio is thought to result in an induced plasma<br />
ionized calcium deficiency leading to improper calcification of bone.<br />
Some tenderness of the feet and lateral curvature at the knees may be seen as early as 2-3 weeks<br />
of age and marked deformity is present at 6-8 weeks with maximum seventy at weaning. The<br />
forelimbs are more commonly affected than the hindlimbs. Medial curvature occurs in rare cases.<br />
The sides of the feet become badly worn, and the lateral aspects of the lower parts of the limbs<br />
may be injured and be accompanied by lameness. The lambs grow well at first, but by the time of<br />
weaning, affected lambs are in poor condition because of their inability to move about and feed<br />
properly. A rather similar syndrome has been observed in young Saanen bucks, but the condition<br />
showed more tendency to recover spontaneously.<br />
At necropsy in spite of the curvature of the limbs there is no undue porosis, and although the<br />
epiphyseal cartilages are thickened they are supported by dense bone. There may be excessive<br />
synovial fluid in the joints and, in the later stages, there are articular erosions. Increased deposition<br />
of osteoid is not observed.<br />
Supplementation of the diet with phosphorus or improvement of the pasture seems to reduce the<br />
incidence of the disease. Dosing with vitamin D or providing mineral mixtures containing all trace<br />
elements is ineffective (2).<br />
REFERENCES<br />
(1)van Niekerk, F. E. c-t al. (1989)J South Ajr.<br />
Vet. hM. Assoc., 60, 36.<br />
(2)Cunningham, I.J. (1957) NZ I'ei.J.. 5, 103.<br />
DEGENERATIVE JOINT DISEASE<br />
Degenerative arthropathy occurs in cattle of all breeds, but reaches its highest incidence as a<br />
sporadic disease of young beef bulls. The disease has been identified as hip dysplasia because of<br />
the pre-existing shallow contour of the acetabulum. It is considered to be inherited as a recessive<br />
characteristic and exacerbated by rapid weight gain in young animals. The occurrence of the<br />
condition in these animals is usually associated with rearing on nurse cows, housing for long<br />
periods, provision of a ration high in cereal grains and byproducts (a high phosphorus:calcium<br />
ratio), and possibly with an inherited straight conformation of the hindlegs. Although the disease<br />
occurs in all beef breeds there is a strong familial tendency which appears to be directly related to<br />
the rate of body weight gain and the straightness of the hindleg. If the potential for rapid weight<br />
gain is being realized in animals being force fed, the rate of occurrence appears to be dependent on<br />
their breeding, and animals in the same herd that are allowed to run at pasture under natural<br />
conditions are either not affected or are affected at a much later age. Thus, animals in a susceptible<br />
herd may show signs as early as 6 months of age if they are heavily hand-fed and raised on dairy<br />
cow foster mothers. In the same herd, signs do not appear until 1-2 years of age if supplementary<br />
108
feeding is not introduced until weaning, and not until 4 years if there is no significant additional<br />
feeding.<br />
Clinically there is a gradual on set of lameness in one or both hindlegs. The disease progresses<br />
with the lameness becoming more severe over a period of 6-12 months. In some animals there is a<br />
marked sudden change for the worse, usually related to violent muscular movements, as in<br />
breeding or fighting. In severely affected animals the affected limb is virtually useless and, on<br />
movement, distinct crepitus can often be felt and heard over the affected joints. This can be<br />
accomplished by rocking the animal from side to side or having it walk while holding the hands<br />
over the hip joints.<br />
An additional method of examination is to place the hand in the rectum close to the hip joint,<br />
whilst the animal is moved. Passive movement of the limb may also elicit crepitus, or louder<br />
clinking or clicking sounds. The hip joints are always most severely affected, but in advanced<br />
cases there may be moderate involvement of the stifles and minimal lesions in other joints.<br />
Affected animals lie down most of the time and are reluctant to rise and to walk. The joints are not<br />
swollen, but in advanced cases local atrophy of muscles may be so marked that the joints appear to<br />
be enlarged. There is a recorded occurrence in which the lesions were confined mainly to the front<br />
fetlocks.<br />
Radiographic examination may provide confirmatory or diagnostic evidence.<br />
At necropsy the most obvious finding is extensive erosion of the articular surfaces, often<br />
penetrating to the cancellous bone, and disappearance of the normal contours of the head of the<br />
femur or the epiphyses in the stifle joint. The synovial cavity is distended, with an increased<br />
volume of brownish, turbid fluid, the joint capsule is much thickened and often contains calcified<br />
plaques. Multiple, small exostoses are present on the periarticular surfaces. When the stifle is<br />
involved the cartilaginous menisci, particularly the medial one, are very much reduced in size and<br />
may be completely absent. In cattle with severe degenerative changes in the coxofemoral joint, an<br />
acetabular osseous bulla may be present at the cranial margin of the obturator foramen (1).<br />
Adequate calcium, phosphorus and vitamin D intake, and a correct calcium:phosphorus ratio in<br />
the ration should be insured. Supplementation of the ration with copper at the rate of 15 mg/kg has<br />
also been recommended for the control of a similar disease.<br />
Degenerative joint disease of cattle is recorded on an enzootic scale in Chile and is thought to<br />
be due to gross nutritional deficiency. The hip and tarsal joints are the only ones affected and<br />
clinical signs appear when animals are 8-12 months old. There is gross lameness and progressive<br />
emaciation. An inherited osteoarthntis is described under that heading. Sporadic cases of<br />
degenerative arthropathy, with similar signs and lesions, occur in heavy-producing, aged dairy<br />
cows, and are thought to be caused by long-continued negative calcium balance. Rare cases also<br />
occur in aged beef cows but are thought to be associated with an inherited predisposition. In both<br />
instances the lesions are commonly restricted to the stifle joints.<br />
REFERENCE<br />
(I) Weaver, A. D. (1982) Br. Vet.J., 138, 123.<br />
4.骨疏松症(Osteoporosis) 骨疏松是指骨骼的有机质形成障碍或形成不足,骨骼疏松、<br />
质轻、脆弱,容易骨折为特点。本病在动物中不常发生,自然状态下,有牛、羊、犬的骨质<br />
疏松症报道。<br />
本病通常属于营养不良所致,并非仅仅由于钙、磷或VD缺乏引起的。羔羊缺铜病可引<br />
109
起骨骼疏松,因成骨细胞活性受损;羔羊铅中毒也可引起骨骼疏松,是因骨样组织生成障碍<br />
所致,恶病质乳牛亦可发生骨疏松症,是因严重营养失调,营养不良引起的。日粮中VA缺<br />
乏,VC、VB2原发性缺乏,亦可使骨基质生成障碍。<br />
由此可见,骨疏松症是属骨病(Osteodystrophy),但又不同于其它因钙、磷代谢障碍或<br />
VD缺乏所引起的骨病。在狗还可因某些抗惊厥药物中毒引起骨疏松症。原发性或营养性甲<br />
状旁腺素分泌过多,继发性肾性甲状旁腺增生,假性甲状旁腺增生,甲状腺素分泌过多,肢<br />
端肥大症,肝毒症,长期四肢瘫痪(废用型),多发性肌瘤,肾上腺皮质分泌过多时,都可<br />
见到骨疏松的现象。所有这些,没有一个是属于原发性骨疏松症,都属于继发性骨疏松症。<br />
骨疏松症最大的特点是骨脆弱,易骨折,骨密度下降,骨皮质变薄,长骨易发生重迭性<br />
骨折,椎骨易发生压迫性骨折,骨骼的基本框架或许存在,但骨样组织数量减少,以甲状旁<br />
腺素分泌过多引起的骨疏松症预后最差。<br />
5。笼养鸡疲劳综合征(Cage Layer Fatigue) 由于钙、磷比例严重失调,钙从体内丢失<br />
过多,引起笼养鸡无力站立和移动困难。长骨变薄,变脆,肋骨与肋软骨结合部膨大,并排<br />
列为串珠状,极易产生骨折的现象,称为笼养鸡疲劳综合征,又称软腿病(Softleg)或笼养<br />
鸡软脚病。<br />
本病主要发生于笼养产蛋母鸡。尤其是产蛋后期的母鸡,产蛋率越高,发病可能性越大。<br />
发病率在 1%~2%之间。但不同品系之间笼养鸡发病率有很大差别,在生产率高,饲料利用<br />
好的幼母鸡,亦常发生。<br />
【病因】 本病发生的真正原因还不十分清楚,但与钙、磷比例失调,磷过低,钙供给<br />
不足有密切关系。有人用低磷(0.34%)和合适钙(3%),合适磷(0.7%)和钙(3%),低<br />
钙(2%)和合适磷(0.7%)三组饲料,饲喂笼养鸡 90 天,发现低磷组鸡发生软腿病较多,<br />
其余两组未显明显异常。<br />
笼养蛋鸡全部矿物质必须从饲料中获得,每产一只蛋约需 2~3g 钙,年产 250~300 枚蛋<br />
的母鸡,形成的蛋壳所需的纯钙不低于 600~670g。这就意味着要消耗相当于它本身体重的<br />
两倍的碳酸钙。因此,产蛋母鸡日粮中含钙量应为 3.0%~3.5%,含磷量应为 0.9%才合适。<br />
平养鸡还可从垫料中获得部分钙和磷。当日粮中钙供给不足时,必然动用机体本身的钙、磷<br />
贮备,通常情况下,蛋壳中钙约有 30%~40%来自骨骼,但又从饲料中及时得到补充,使骨<br />
骼处于动态平衡。若钙供给不足,或钙代谢障碍时,骨骼得不到钙的补充,处于钙的负平衡,<br />
则就产生骨骼变薄、变脆。<br />
VD3供给不足,或VD3在体内代谢障碍,亦可诱发本病。VD不仅有利于钙的吸收,而且<br />
有利于骨骼中钙交换。但肝机能不全,肾出现尿酸盐沉着,或因传染病支气管炎,引起肾炎、<br />
肾病综合征时,或脂肪代谢障碍时,干扰了VD的吸收和代谢,影响了钙的吸收和利用,可<br />
诱发本病。<br />
此外,产蛋应激作用,似乎与本病发生有一定关系。产蛋越多,发病也越多。<br />
【临床表现】 病鸡表现腿肌无力,站立困难,常伴有脱水和体重下降现象。体况越好、<br />
产蛋越多、生长越快的鸡,越易发生。患禽躺卧或蹲伏不起,接近食槽或饮水器很困难,由<br />
于骨骼薄、脆,肋骨、胸骨变形,有的在笼内就已发生骨折。有的在转换笼舍时,或捕捉时,<br />
发生多发性骨折,引起呼吸困难,胸椎骨折,引起脊椎变性,截瘫。淘汰鸡于屠宰、拔毛加<br />
工过程中,多处骨折。肌肉中夹杂有小骨刺,或出血,使鸡肉等级下降。<br />
组织学变化显示,除骨组织疏松,正常结构破坏以外,关节呈痛风性损伤。组织出血性<br />
炎症,肾盂有时呈急性扩张,肾实质囊肿,甚至尿酸盐沉着,血清碱性磷酸酶活性升高。尽<br />
管病禽呈严重缺钙,但产蛋量、蛋壳和蛋白质量无明显降低,鸡照常采食和饮水(如果能够<br />
接近食槽和饮水器的话)。轻型病鸡如移至平养,并人工饲喂,使其能吃到饲料或饮水,亦<br />
有自然康复的现象。<br />
110
【防治】 由于病因尚不完全明确,预防措可试用以下方法:<br />
母鸡,尤其是产蛋母鸡应供给 3.5%的钙,0.9%的磷,2%~3%的脂肪或植物油,及VD3<br />
37.5µg/kg,以便使VD、石粉和贝壳粉充分粘附于饲料表面,防止沉淀在饲槽底部,而未真<br />
正食用。<br />
小母鸡舍饲、平养期间,应给予足够的钙、磷、VD3,使骨骼发育坚实,至 19~20 周龄,<br />
关入笼内饲养时,即开始用产蛋期饲料,日粮中磷供给比平养增加 0.2%。<br />
鸡舍内温度应控制在 20~27℃之间,尽量减少应激刺激,让母鸡有适当的活动空间,不<br />
要使鸡在笼内过度拥挤,每鸡占有面积不少于 380cm 2 ,使其能较方便地接近饲槽和饮水器等<br />
措施,可防止疾病发生。<br />
6。妊娠性骨折(Fracture of Pregnancy) 母畜妊娠后期,因骨骼疏松,在突发性外伤损<br />
害下,引起骨盆骨、椎骨骨折现象,称为妊娠性骨折。牛、羊最易引起妊娠骨折,其他家畜<br />
亦可发生。<br />
妊娠期间,尤其是妊娠后期,由于母畜经常处于钙、磷负平衡,骨盐溶解作用大于沉积<br />
作用,骨骼疏松,当遇到某些意外伤害的情况下,可引起骨折。如母畜急速转弯,滑跌,通<br />
过太窄的门道,突然倒卧在坚硬的地面上,甚至被公畜爬跨,过度拥挤等,都可以引起骨折。<br />
骨折的部位常因外力损伤的方向而异,通常为髋骨翼、坐骨结节、髋臼窝外沿、耻骨联合、<br />
腰荐椎骨折多见。<br />
一开始,患畜表现程度不等的跛行,甚至发展为卧地不起,髂骨骨折,表现为尻部高度<br />
不对称,当动物行走时,有时可听到霹拨声或捻发音。直肠触诊可感觉到骨折处肿胀、疼痛、<br />
手压尻部可有捻发样感觉,基本上可以确定骨折部位。耻骨骨折,或耻骨联合分离,尻部外<br />
观虽尚对称,但触诊剧痛,肿胀明显。腰椎、荐椎骨折,常可引起截瘫或后肢瘫痪、麻痹等。<br />
本病仅能预防,从妊娠一开始,就应注意动物饲料中VD、钙、磷的供给,妊娠后期应<br />
加强管理,防止滑跌或受外力打击,切勿急转弯。一旦发生骨折,应使动物躺卧在松软垫料<br />
的地上,待创伤炎症消退,胎儿出生后,母畜常归于淘汰。<br />
(二)机能性钙、磷代谢紊乱性疾病<br />
1。生产瘫痪(Parturient Paresis) 生产瘫痪是成年母牛于分娩前后发生的一种代谢病,<br />
称为乳热症(Milk Fever),临床上以血钙浓度下降,全身肌肉虚弱、躺卧、循环虚脱和精神<br />
沉郁为特征。<br />
【流行病学】 本病多发生于高产奶牛,奶产量越高,发病越多,年发病率一般在 3.5<br />
%~8.8%。有些农场发生率很低,在 1.2%左右;但有些场竟可高达 25%~30%。本病多发<br />
生于 3~7 胎次(5~10 岁)以上母牛,第 1~2 胎次母牛很少发生。一年四季均有发生,呈散<br />
发。与母牛所产犊牛的性别、胎儿大小、死胎与否、单胎和双胎之间关系不大。本病多在妊<br />
娠最后几天或分娩期间发生,分娩后第一天发病占 83%,48h 内发病的占 86%,但也有在<br />
产后 10 天内发病的,甚至在产后 6~8 周内发病。发病越迟,血清钙下降程度越小。品种不<br />
同,对本病的易感性不一样,娟姗牛最易感,占 33%,而其他品种牛易感性较低,约为 9.6%<br />
(5.6%~15.3%)。<br />
生产瘫痪在猪、羊中亦可见到,母猪发病甚少,尤其是用商品日粮饲喂的母猪。但绵羊<br />
有时可呈暴发流行,同一群羊中可能有 25%受影响。绵羊多在妊娠后期和泌乳早期,年青<br />
羊有的在 1 岁龄时采食绿色燕麦时容易发生。母山羊在 4~6 岁龄时最易受影响,一般多在分<br />
娩前后发生,但也有的在分娩后 3 周内发生。猪生产瘫痪仅呈散发,但在强迫运动、长途运<br />
输、禁食或采食含大量草酸盐饲料后,暴发低血钙性瘫痪,尤其是产羔后的 6~10 周内母羊<br />
特别敏感。<br />
本病在妊娠肉牛、水牛中也可发生。特别是妊娠期间饲以饲料单一、品质较差的饲料,<br />
或在他们发情期间,或于饥饿 48h 后,亦会出现瘫痪。从这个意义讲本病已不仅仅限于分娩<br />
111
与产乳这两个因素了。<br />
【病因】 生产瘫痪牛最大的特点是血清总钙、血清钙离子成比例下降。可见血钙下降<br />
是发生本病的主要原因。影响血清钙浓度的因素有三:<br />
(1)初乳中钙含量较高。大量的钙从初乳中丢失,体内钙丢失速度超过了钙从小肠或<br />
骨骼中重吸收速度。各个个体不同,初乳中钙含量及初乳量多少不一样,血钙下降的速度也<br />
不一样。<br />
(2)钙从肠道中吸收受影响,尤其是分娩应激作用,动物采食量及胃肠道吸收能力方<br />
面均受影响。使钙吸收率及吸收总量减少。<br />
(3)钙从钙库中动员速度和重吸收的量,不能满足维持血钙浓度处于正常水平的需要,<br />
造成血钙下降。如静脉注射选择性骨吸收抑制剂 EHDP,可实验性出现乳热症。<br />
钙从骨骼中重吸收速度减慢,最重要的原因是甲状旁腺功能未充分发挥。例如,在干奶<br />
期饲料中钙含量过多、磷含量不足或正常,血钙始终维持在较高水平,甲状旁腺功能长期受<br />
抑制,分娩前后或当泌乳时,由于血钙突然下降,甲状旁腺活动处于“静止”(quiescent)<br />
状态,不能大量分泌并动员骨钙入血。事实上,在干乳期喂给高磷、低钙日粮,可以防止该<br />
病发生。这种日粮可刺激甲状旁腺在干乳期处于活泼状态;并分泌甲状旁腺素。因而当泌乳<br />
开始后,由于骨骼钙能顺利地被重吸收而防止该病发生。调节钙代谢的内分泌活动失调,还<br />
表现在当干乳期喂给高钙饲料时,降钙素分泌增多,从而在分娩后,过多的降钙素还继续影<br />
响血钙浓度,最终使血钙浓度迅速下降。<br />
因此,可以认为奶牛的生产瘫痪是由血钙浓度下降所致。有 3 个因素可造成低钙血症:○1<br />
钙不能迅速从钙库中被重新动员。○2 在妊娠后期,动物处于钙的负平衡状态。③分娩应激和<br />
初乳分泌加速了钙负平衡的进程。饲料中VD不足,钙、磷比例不当都可加速钙负平衡。<br />
低钙血症,也可在非分娩前后发生。如过食容易发酵的碳水化合物饲料的早期和中期,<br />
静脉注射氨基糖甙类抗生素,如新霉素、双氢链霉素、庆大霉素也可引起血清钙离子浓度下<br />
降。并产生与乳热症类似的症状发作。因此在治疗生产瘫痪过程中,使用这类药应慎重。<br />
在母山羊分娩时,血清钙、磷浓度下降时,与母牛类似。但母绵羊血清钙浓度在产羔时,<br />
并不降低,还需其他辅助因子作用,如突然禁食,强迫运动,才引起血清钙明显下降。在早<br />
期泌乳过程中由于钙的负平衡,血钙浓度可明显降低,并产生瘫痪观象。<br />
【临床表现】<br />
(1)牛 牛生产瘫痪时,症状发展有三个明显阶段。<br />
第一阶段为前趋症状。呈现短暂的兴奋,头、肢部肌肉震颤,食欲废绝,站立不动,摇<br />
头、伸舌、磨牙、直肠温度正常或略有升高。后肢僵硬,平衡失凋,甚至跌倒。当挣扎起立<br />
后,试图运步,但因平衡障碍,可再度跌倒。有时只见前肢尚能支撑爬起,但后肢无力,呈<br />
犬坐势。<br />
第二阶段为卧地不起阶段,此期精神沉郁,闭目欲睡,或后躯坐地,或呈伏卧状态。四<br />
肢缩于腹下,颈部弯向外侧,呈 S 状。有的把头转向后方,置于一侧肋部。四肢痉挛现象<br />
虽停止,但牛不能站立。鼻镜干燥,皮温下降,肢端发凉,体温略低(36~38℃)。瞳孔扩大,<br />
眼干瞪着。肛门松弛,肛反射减弱;心音减弱,频率增多达 80 次/min。脉搏微弱,静脉<br />
压下降,因全身循环血量减少之故。瘤胃弛缓、便秘、瞳孔对光反应迟钝或缺失,瞳孔大小<br />
不一。<br />
第三阶段,即昏迷状态阶段。患牛呈侧卧状态,近乎昏迷,但四肢有时还可蹬地,肌肉<br />
呈不完全松弛,还可作被动运动。体温下降和心血管症状更明显。大多数病牛呈不感脉,心<br />
音几乎听不到,心率增达 120 次/min,颈静脉无法显露,瘤胃鼓气是常见的现象。<br />
(2)羊 当并发低镁血症时,其搐搦和感觉过敏现象不限于在第一阶段出现,眼睑跳<br />
动和吊眼,当听到声音或触摸畜体时,可出现痉挛发作。牙关紧闭,心跳快速,呼吸急迫,<br />
112
心音亢进,在痉挛发作时如不及时抢救,可迅速死亡。<br />
能站立。<br />
当伴有低磷血症时,其临床表现与生产瘫痪很相似,但对钙剂治疗效果良好,但动物不<br />
(3)绵羊 临床表现与牛类似。早期亦表现粘着步,肌震颤,尤其是肩部肌肉震颤。<br />
随后躺卧,有时四肢抽搐,头颈弯曲,四肢集于腹下,或向后方伸展。瘤胃蠕动音消失,头<br />
伏于地上,鼻有粘性分泌物。呼吸增快,静脉血压降低,不感脉,精神抑郁,动物嗜睡。角<br />
膜反射迟钝。常有便秘,对钙治疗反应快速,皮下注射后 30min 可好转。如不及时治疗,<br />
于 6~12h 可毙命。妊娠和泌乳母羊表现更为严重。<br />
(4)猪 症状在产后数小时内发生。表现不安,体温正常、不能站立、食欲下降,侧<br />
卧和昏迷,泌乳减少。<br />
【临床病理】 目前尚无理想的方法用作田间监测,用 EDTA 法测定血清钙,仅起<br />
定量作用。因在制备血清时,会有部分钙随凝血而损失。尽管如此,目前还是用测定血清钙<br />
来估测生产瘫痪的可能性和作诊断依据。乳牛正常的血清钙浓度为 2.35~3.0mmol/L<br />
(9.4~12mg/100ml),而病牛血清总钙含量可降为 2.0~0.5mmol/L(8~2mg/100ml)。通常情<br />
况下,病牛血清钙降低,但并不总是降低。降低越多,病情越重。健康乳牛血镁浓度通常为<br />
0.49~1.44mmol/L(1.2~3.5mg/100ml),生产瘫痪牛,血镁浓度可升高到 l.64~2.06mmol/L<br />
(4~5mg/100ml)。但在有些地区血镁浓度还有所下降,特别是在草地放牧的牛,血镁浓度<br />
可降低。血清无机磷浓度通常为 1.45~2.97mmol/L ( 4.5~9.3mg/100ml ),病牛可降到<br />
0.48~0.97mmol/L(1.5~3.0mg/100ml)。血糖浓度变化不大,但伴发酮病时,血糖浓度下降。<br />
病程长的病例,血糖浓度甚至高于正常。1,6-二磷酸匍萄糖,谷草转氨酶(GOT),肌酸磷<br />
酸激酶(CPK)活性通常升高,可能与肌纤维膜损伤有关。血液中其它参数变化颇不稳定,<br />
诊断中参考价值不很大。<br />
【诊断】 诊断中应掌握如下一些要点:①产后不久立即发生,常在 1~3 日内发病。②<br />
精神沉郁,体温下降,躺卧不起是三大主要症状。③本病对钙剂治疗反应迅速且良好。④血<br />
液化学测定可见血清钙、磷浓度下降,反应肌损伤的酶(GOT、CPK)活性上升。<br />
母羊瘫痪亦依病史(妊娠后期)、产前应激因素等,并参考牛生产瘫痪要点进行诊断。<br />
生产瘫痪可与低镁性搐搦症、产后毒血症、难产性瘫痪、母牛卧倒不起综合征、外伤性<br />
不能站立等区别开来:<br />
(1)低镁血症 发病不受品种、年龄限制,多数为最近分娩母牛,有时在产后数日才<br />
发生。特征表现是兴奋,敏感性升高,搐搦伴强直性惊厥,血镁浓度明显低于 0.49mmol/L<br />
以下,对钙治疗反应缓慢。<br />
(2)产后毒血症 本病仅呈散发,乳房炎,子宫破裂、子宫炎或阴道破裂等可引起严<br />
重的腹膜炎,并发毒血症。动物表现心率增快,体温先升高后降低,精神极度沉郁,以至昏<br />
迷。乳汁检查和血象检查可见乳汁中细胞数增多,血液中白细胞减少,血钙浓度亦可低于<br />
1.75~2.0mmol/L,产后多不良。用钙、镁治疗可引起死亡,常因治疗不及时或措施不当而<br />
引起休克死亡。<br />
(3)难产性瘫痪(maternal obstertrical paresis,MOP) 主要发生于初产母牛或因胎儿<br />
过大,胎位不正等引起难产。但动物一般表现精神尚好,反应敏捷,照吃照饮。大便、小便<br />
不甚异常。卧地动物始终想站起,但较困难或滑跌,甚至伤及肌肉、骨骼致残。本病对临床<br />
治疗反应较差。适当使用吊带吊起或铺以厚垫草,并经常翻转身体,经治疗 3 天不愈者,预<br />
后需慎重。<br />
(4)卧倒不起综合征 见下节。<br />
(5)理学损伤 如滑跌,骨疏松症,腓肠肌损伤等,血液中 CPK 和 GOT 升高,常需<br />
要作支持治疗,铺厚垫草,经常翻身体,防止褥疮生成。<br />
113
(6)瘤胃酸中毒 过食谷类饲料后,血钙浓度亦可下降,乳酸过多呈现卧倒不起,嗜<br />
睡甚至休克。但本病脱水严重,血乳酸升高。血糖降低至 5.32mmol/L(25mg/100m1)以<br />
下,使用钙剂可加速病情恶化。<br />
(7)绵羊低钙血症性瘫痪 本病常因大脑疾病引起,对钙剂治疗反应较差,亦可表现<br />
酮尿,山羊肠毒血症和低糖血症时亦可表现瘫痪应注意区别。猪的生产瘫痪一般体温正常,<br />
可与子宫炎、乳房炎引起的不愿站立相区别。<br />
【治疗】 当母牛出现生产瘫痪症状后,应立即治疗。治疗越早(特别是在前趋症状期)<br />
疗效也越高,如治疗不及时常招致局部肌肉缺血性坏死,并发展为母牛躺卧综合征,使治疗<br />
更为困难。目前有以下几种治疗方法:<br />
(1)钙剂治疗或标准治疗 葡萄糖硼酸钙以 20%~30%溶液,100~200g 作静脉注射,<br />
或用 25%葡萄糖酸钙 400~800ml 静脉注射。山羊给予 15~20g 静脉注射,并用 5~10g 溶液作<br />
皮下注射,关于剂量问题可因牛的大小而定,有人建议,对大型乳牛,体重为 550~600kg<br />
时,25%葡萄糖硼酸钙一次可用 800~1000ml,300~360kg 重小牛,一次静注 400~500ml,1<br />
天 2 次。未发现有中毒倾向。剂量不足,病牛虽有好转,但不能站立。如用氯化钙,牛 1<br />
次可用 12g 钙。静脉注射钙剂,反应快,效果确实,但有些牛如怕心脏受不了大剂量的钙剂<br />
刺激,亦可用葡萄糖硼酸钙,作皮下注射,一般是静脉注射一半量,皮下注射另一半量,这<br />
样不仅反应快,而且维持作用时间长。母羊、猪以 15%葡萄糖酸钙 100~150ml,一次静脉<br />
注射,典型的产后瘫痪,在注射钙剂后表现肌肉震颤,打嗝,鼻镜出现水珠,排粪,心音宏<br />
亮,脉搏平稳而有力。有时四肢肌肉还有轻度搐搦。一般有 37%的患牛中注射钙后 10min<br />
可站立,50%的牛稍慢甚至需人工辅助,但也有 14%的牛不能恢复被淘汰。应注意的是,<br />
注射钙剂速度宜慢不宜快,否则心脏承受不了。氯化钙只能作静脉注射,不能注入或漏入皮<br />
下,对瘫痪同时伴有体温升高或因腹膜炎、子宫炎、乳房炎引起动物瘫痪时,不宜用钙剂,<br />
更不能使用过量钙。否则可引起急性死亡,宜先治原发病,抗菌、消炎、消除毒血症。待体<br />
温恢复正常后再用钙剂。<br />
注射钙剂后不能马上离开,注射过程中或注射之后应密切注意心脏功能,包括听诊心音<br />
频率、强度、节律,如果注射后病牛十分激动或恐惧或畜体周围气温过高,太阳暴晒、闷热<br />
等,大剂量钙注射后可引起突然死亡。<br />
钙剂治疗效果一般是可靠的,但遇到下列情况,其效果不理想。①48h 前先期曾用钙治<br />
疗过,而复发者。③中年娟姗牛曾多次发生过生产瘫痪者。③老年母牛。④病程已较长者。<br />
⑤治疗时动物姿势很重要,侧卧牛对钙剂治疗反应不如伏卧牛敏感。<br />
多次使用钙剂效果仍不明显时,可用 15%~20%磷酸二氢钠 200~400m1 静脉注射,或<br />
者与钙剂交换使用,也可使用 50%葡萄糖 400ml,15%磷酸氢钠 200m1,15%硫酸镁<br />
200~400ml,首次合用,特别是当患有生产瘫痪并伴有其他代谢病如青草搐搦,骨软症等情<br />
况时,用此类复合剂效果更好。<br />
(2)乳房送风,又称乳房充气治疗法 将患牛乳房洗净,用酒精棉球擦净消毒,将消<br />
毒过的导乳管插入乳头内,外接乳房送风器,向内打气。先从接近地面的两个乳头开始,然<br />
后向其余乳头送气,打满气后用绷带扎紧乳头以防气体回流,打入气量以乳房皮肤紧张,乳<br />
区界限明显为准。气量过多,可引起腺泡损伤,充气量不足影响疗效。<br />
乳房充气目的在于使乳腺受压迫,停止泌乳,减缓钙、磷从乳汁中丢失,对单用钙剂治<br />
疗效果不佳的病畜。用此法或与钙治疗并用效果较好。在乳房充气后,随即继续用钙剂治疗。<br />
可防止复发。<br />
(3)牛乳疗法 产后不久发病母牛,可用健康牛新鲜乳 3000~4000ml,分别注入患病<br />
牛四个乳区内,亦可起冶疗作用。其原理与乳房送风相同。<br />
(4)病畜护理 对治疗结果影响很大,所产犊牛要迅速移开,48h 内仅在吸初乳时放<br />
114
回母牛处。患牛应尽可能保持伏卧或坐位。这样一方面可防止肌肉缺血性损伤,另一方面亦<br />
可防止吸入性肺炎。每天至少要翻 3~4 次身,如缺乏遮阳棚的,可临时搭建,不应于强日光<br />
下暴晒,否则引起中暑后更难治疗。<br />
【预防】 加强干乳期母牛的饲养管理,提高母牛的抗病能力。<br />
①控制精料的喂量,并适当限制饲喂量,防止母牛过肥,混合精料每天不超过 3~4kg,<br />
并保证有充足的干草。②充分注意钙、磷供给与比例,据报道干乳期日粮中含 137g/kg钙,<br />
8.5g/kg磷,Ca:P为 1.61:1 可使生产瘫痪发病率从 74%下降为 16%。Boda和Cole在母牛妊<br />
娠最后 1 个月饲以高磷,低钙日粮,使Ca:P为 1:1,仅有 15%牛发病如Ca:P为 1:3.3 则发病<br />
率为 0。此日粮对泌乳虽没有明显影响,但如持续时间过长。可酿成骨疏松症。他们建议在<br />
日粮中给予 5%的磷酸二氢钠,有明显的防止乳热症发生作用。但为了不至于使钙的负平衡<br />
太严重,建议乳牛日粮中钙仍需要 100~125g/天。这样不仅可促进肠钙吸收;同时可减少<br />
钙从尿中丢失。③此期间使牛舍保持清洁,给牛以适当运动,产前 48h,产后 48h密切注意<br />
观察乳牛体况,一旦有前趋症状出现,立即治疗。④在产犊期给牛喂胶体钙(calcium gel),<br />
然后立即用高钙日粮(干物质计钙含量超过 1%),并每天补充 60g氧化镁,这样可大大减少<br />
乳热的发病率。具体做法是,产前 24h、1~2h和产后 10~14h,人工投服胶体钙,或氯化钙<br />
150g,则可大大降低乳热的发生。⑤产前 5 天口服 200 万单位VD2,同时肌肉注射VD3,一<br />
次量为 1000 万单位或每 45kg重给予 100 万单位亦可减少乳热发病率。如果牛口服和肌注VD<br />
后,超过 8 天仍未分娩,可按此量再用一次。而且每 8 天可重复一次,直至分娩后停用。长<br />
期用大剂量维生素D注射,有产生钙异位沉着的危险。肌肉注射二羟VD3效果更好。一次注<br />
射 100mg,24h后即可使血钙迅速上升,并可维持 72h。因而产后立即注射该药对预防乳热<br />
发生是有价值的。还可用 25-羟胆骨化醇 8mg于产前 3~10 天注射,以后每周 1 次,每次 4~8mg,<br />
亦可有效地提高血钙浓度,预防本病发生,并可防止复发。⑥产前几周每天喂给 100g氯化<br />
铵可使日粮酸化,亦可减少乳热的发生率。<br />
PARTURIENT PARESIS (MILK FEVER)<br />
A disease of cattle, sheep and goats occurring around the time of parturition and caused by<br />
hypocalcemia and characterized by weakness, recumbency and ultimately shock and death.<br />
Synopsis<br />
Etiology. Hypocalcemia just before or after parturition.<br />
Epidemiology. Adult dairy cows in third parity and older; 4-9% with low case fatality. Most<br />
commonly within 48 h after calving but also occurs several weeks before or after. Occurs in beef<br />
cattle in epidemics. Occurs in sheep and goats in epidemics usually following stressors. Prepartum<br />
diets high in calcium.<br />
Signs. Three progressively worse stages including the following signs<br />
•Anorexia<br />
•Ruminal atony<br />
•Scant feces<br />
•Inactivity<br />
•General muscular weakness leading to sternal recumbency with lateral kink of neck<br />
•Circulatory collapse with collapsed veins and weak pulse<br />
•Dry muzzle<br />
•Mental depression<br />
•Hypothermia<br />
•Weak heart sounds<br />
•Dilated and sluggish pupils<br />
115
•Ruminal stasis and bloat<br />
•Lateral recumbency<br />
•Tachycardia<br />
•Death in few to several hours.<br />
Clinical pathology. Hypocalcemia, hypophosphatemia, variable serum magnesium. Increased<br />
creatine phosphokinase (CPK) and aminotransferase (AST) due to ischemic muscle necrosis.<br />
Lesions. No specific lesions. Ischemic muscle necrosis of large muscles of pelvic limbs because<br />
of prolonged recumbency.<br />
Differential diagnosis list: Cattle: Metabolic and nutritional disease:<br />
•Hypophosphatemia (p. 1537)<br />
•Hypomagnesemia (pp. 1442, 1510)<br />
•Downer cow syndrome (p. 1435)<br />
•Fat cow syndrome (p. 1462)<br />
•Carbohydrate engorgement (p. 284).<br />
Toxemias:<br />
•Peracute coliform mastitis (p. 639)<br />
•Aspiration pneumonia (p. 450)<br />
•Acute diffuse peritonitis (p. 251).<br />
Injuries to pelvis and pelvic limbs:<br />
•Maternal obstetrical paralysis (p. 1427)<br />
•Dislocation of coxofemoral joint.<br />
Sheep and goats:<br />
•Pregnancy toxemia (p. 1452)<br />
•Enterotoxemia (pp. 769, 770).<br />
Diagnostic confirmation. Hypocalcemia and response to treatment with calcium borogluconate.<br />
Treatment. Calcium borogluconate IV.<br />
Calcium chloride in oral gel.<br />
Control. Dietary management to reduce prepartum intake of calcium. Calcium gel oral dosing<br />
before calving, at calving, and 12 and 24 h after calving. Parenteral vitamin D and analogs.<br />
ETIOLOGY<br />
A depression of the levels of ionized calcium in tissue fluids is the basic biochemical defect in<br />
milk fever. A transient period of hypocalcemia occurs at the onset of lactation caused by an<br />
imbalance between calcium output in the colostrum and influx of calcium to the extracellular pool<br />
from intestine and bone. The onset of lactation results in a sudden large demand on the calcium<br />
homeostasis. A cow producing 10 kg of colostrum (2.3 g of Ca/kg) will lose 23 g of calcium in a<br />
single milking. This is about nine times as much calcium as that present in the entire plasma<br />
calcium pool of the cow (1). Calcium lost from the plasma pool must be replaced by increasing<br />
intestinal absorp¬tion and bone resorption of calcium. During the dry period, calcium<br />
requirements are minimal at about 10-12 g/d. At parturition, the cow must mobilize about 30 g or<br />
more of calcium into the calcium pool per day. Hypocalcemia occurs in spite of apparently<br />
adequate function of the parathyroid and vitamin D endocrine system and most cows adapt within<br />
48 h after calving by increases in plasma concentrations of parathyroid hormone and 1,25-(OH)2<br />
D vitamin at the onset of the hypocalcemia and mobilize calcium by increasing intestinal<br />
absorption and bone resorption.<br />
116
About 5--20% of adult cows are unable to maintain plasma calcium and consequently develop<br />
severe hypocalcemia or clinical milk fever which requires treatment (2).<br />
EPIDEMIOLOGY<br />
Occurrence<br />
Cattle<br />
The disease occurs most commonly in high-producing adult lactating dairy cattle. Lactating beef<br />
cows are affected but less commonly.<br />
AGE Mature dairy cows are most commonly affected in the 5-10-year age group, although rare<br />
cases have been observed at the first and second calvings. The hypocalcemia at calving is also age<br />
related and most marked in cows at their 3rd to 7th parturition; it is infrequent at the first<br />
parturition.<br />
BREED There are differences in susceptibility between the breeds. Jerseys are most susceptible,<br />
an incidence of 33% was observed in a sample compared with 9.6% incidence in other breeds. In a<br />
data set of 61-124 Finnish Ayrshire lactations, cows in higher producing herds were at increased<br />
risk of milk fever and ketosis (3). The disease in beef cattle breeds occurs either in individual<br />
cows or in herd outbreaks (4).<br />
INDIVIDUAL cows Individual cows, and to some extent families of cows, are more susceptible<br />
than others; the disease tends to recur at successive parturitions. The hcritability of susceptibility<br />
to milk fever and hypocalcemia has been assessed as insignificant; in several breeds examined it<br />
was of the order of 6-12%. Complete milking in the first 48 h after calving, as opposed to normal<br />
sucking by a calf, appears to be a precipitating factor.<br />
TIME OF OCCURRENCE in Cattle,milk fever occurs at three main stages in the lactation cycle.<br />
Most prepartum cases occur in the last few days of pregnancy and during parturition but rare cases<br />
occur several weeks before calving. Some cases will occur a few hours before parturition or at the<br />
time of parturition when the attendant expects the cow to calve and the second stage of parturition<br />
does not occur because of uterine inertia due to hypocalcemia. Most cases occur within the first 48<br />
h after calving and the danger period extends up to about the 10th post-partum day. Up to 20% of<br />
cases can occur subsequent to the 8th day after calving. In such cases the declines in serum<br />
calcium and phosphorus levels are smaller and the increases in serum magnesium levels are<br />
greater than in parturient cows. The clinical signs are also less severe and there are fewer relapses<br />
after treatment. Occasional cases occur 6 8 weeks after parturition (mid-lactation). Such cases are<br />
most often recurrences of the disease in highly susceptible cows which were affected at calving.<br />
Undue fatigue and excitement may precipitate such attacks and there is a special susceptibility at<br />
estrus. In the latter case, the depression of appetite by the elevation of blood estrogen levels may<br />
be a significant factor.<br />
STRESSORS Starvation for 48 h also causes severe depression of serum calcium levels and this<br />
may be of importance in the production of hypocalcemic paresis in this species at times other than<br />
in the postparturient period. Pregnant beef cattle may develop hypocalcemic paresis during the<br />
winter months when they are fed on poor-quality roughage; within a group of such cows the less<br />
aggressive ones may suffer selective malnutrition. The disease has also been recorded in beef<br />
cows affected with diarrhea of undetermined etiology (5). As another explanation of the<br />
heightened susceptibility of cows at estrus, a possible depression of the degree of ionization of<br />
calcium under the influence of increased serum estrogens is suggested. However, there were no<br />
117
significant differences in total serum calcium or plasma ionized calcium values in cows from 48 h<br />
before and after estrus.<br />
Subclinical hypocalcemia occurs in dairy cattle during the first few weeks of lactation. Up to<br />
50% of aged cows may be unable to maintain plasma calcium above the lower normal limit (2.18<br />
mmol/L) as defined by the 99% confidence interval of plasma calcium concentrations in cows<br />
outside the first month of lactation. The plasma levels of phosphorus also decrease and the plasma<br />
levels of magnesium increase as occurs in cows at the time of parturition. Hypocalcemic episodes<br />
lasting 1-2 d may occur two or three times with a periodicity of about 9 d. These cows are referred<br />
to as 'calcium cyclers' and the magnitude of the cycling was increased by feeding cows 200 g/d of<br />
1,25-dihydroxyvitamin D for 5 d around the time of parturition. Fluctuations in the intestinal<br />
absorption of calcium during this period may be the cause of calcium cycling. Subclinical<br />
hypocalcemia is of major significance because it inhibits reticulorumen motility, which affects<br />
appetite and exacerbates the negative energy balance already existing in the cow in first month of<br />
lactation.<br />
Episodes of subclinical hypocalcemia occur in up to 50% of adult cows during the first few<br />
weeks of lactation. It is suggested that these calcium cyclers are animals whose calcium<br />
homeostatic mechanisms have not adapted well enough.<br />
Hypocalcemic syndromes in ruminants are also observed at times other than related to<br />
parturition. Thus, it can be part of an early or mild overeating of fermentable carbohydrate. The IV<br />
administration of certain aminoglycosides, especially neoniycm, dihydrostrepto-mycin and<br />
gentamicin, may cause a reduction in the degree of ionization of serum calcium and a syndrome<br />
similar to milk fever. Oral dosing with zinc oxide (40 or 120 mg Zn/kg BW) as a prophylaxis<br />
against facial eczema in ewes causes a serious fall in serum calcium levels 24 h later. Caution is<br />
recommended with the use of these drugs in parturient cows.<br />
Sheep and goats<br />
In sheep, the disease commonly occurs in outbreaks in groups of ewes exposed to forced exercise,<br />
long-distance transport, sudden deprivation of food, and grazing on oxalate-containing plants or<br />
green cereal crops. These circumstances commonly precipitate outbreaks of hypocalcemic paresis<br />
in sheep, mature ewes are the most susceptible, particularly in the period from 6 weeks before to<br />
10 weeks after lambing. Up to 25% of the flock maybe affected at one time. The disease also<br />
occurs in young sheep up to about 1 year old, especially when they graze green oats, but also<br />
when pasture is short in winter and spring, as in southeast Australia. The disease is manifested by<br />
paresis but in the rest of the flock poor growth, lameness and bone fragility can be detected. A<br />
sudden deprivation of feed or forced exercise of ewes can cause marked depression of the serum<br />
calcium levels. However, ewes are in a susceptible state in early lactation because they are in<br />
negative calcium balance. In late lactation a state of positive balance is due to a low rate of bone<br />
resorption. There is an unexplained occurrence of hypocalcemia in sheep fed on hay when they are<br />
supplemented with an energy-rich concentrate which increases their calcium intake. Some of the<br />
concentrates fed to ewes in feedlots contain supplementary magnesium as a prevention against<br />
hypomagnesemia, which may affect calcium absorption and precipitate hypocalcemia in<br />
susceptible ewes. Another occurrence in ewes is at the end of a drought when the pasture growth<br />
is lush and very low in calcium content. The incidence may be as high as 10% and the<br />
case-fatality rate 20% in ewe flocks in late pregnancy or early lactation.<br />
In goats, a depression in serum levels of calcium and phosphorus occurs similar to that in cows<br />
118
ut in ewes no such depression occurs at lambing and the intervention of a precipitating factor<br />
appears to be necessary to further reduce the serum calcium level below a critical point.<br />
Milking goats become affected mostly during the 4-6-year age group. Cases occur before and<br />
after kidding, some later than 3 weeks after parturition. Clinical syndromes are identical to those<br />
in cows, including the two stages of ataxia and recumbency. Serum calcium levels are reduced<br />
from normal levels for partunent does of 9.4-3.6 mg/dL (2.35-0.9 mmol/L).<br />
Morbidity and case fatality<br />
Annual morbidity rates of 3.5 and 8.8% of susceptible adult cows have been recorded. The<br />
incidence has increased in the last three decades coincident with an increase in milk production. In<br />
Australia, about 3.5% of cows are at risk and in Finnish Ayrshires, the rate is 3.8% (6). Generally<br />
the disease is sporadic but on individual farms the incidence may rarely reach 25-30% of high-risk<br />
cows. With early treatment relatively few deaths occur in uncomplicated cases but incidental<br />
losses due to aspiration pneumonia, mastitis and limb injuries may occur. From 75-85% of<br />
uncomplicated cases respond to calcium therapy alone. A proportion of these animals require<br />
more than one treatment, either because complete recovery is delayed, or because relapse occurs.<br />
The remaining 15-25% are either complicated by other conditions or incorrectly diagnosed.<br />
Risk factors<br />
Major risk factors include:<br />
1.Increasing age of cow<br />
2.High-producing dairy cattle<br />
3.Dry period nutrition<br />
4.Housing.<br />
Animal risk factors<br />
Serum calcium levels decline in all adult cows at calving due to the onset of lactation. Serum<br />
calcium levels decline to lower levels in some cows than in others and it is this difference which<br />
results in the varying susceptibility of animals to parturient paresis. First-calf heifers rarely<br />
develop milk fever because while some degree of hypocalcemia occurs during the first few days<br />
of lactation, they are able to adapt rapidly to the high demands of calcium for lactation. With<br />
increasing age, this adaptation process is decreased and results in moderate-to-severe<br />
hypocalcemia in most adult cows. The adaptation mechanism is directly related to the efficiency<br />
of intestinal absorption of calcium, which decreases with increasing age.<br />
CALCIUM HOMEOSTASIS<br />
Three factors affect calcium homeostasis and variations in one or more of them may be important<br />
in causing the disease in any individual:<br />
1.Excessive loss of calcium in the colostrum beyond the capacity of absorption from the intestines<br />
and mobilization from the bones to replace.<br />
Variations in susceptibility between cows could be due to variations in the concentration of<br />
calcium in the milk and the volume of milk secreted<br />
2.Impairment of absorption of calcium from the intestine at parturition<br />
3.Mobilization of calcium from storage in the skeleton may not be sufficiently rapid to maintain<br />
normal serum levels. The calcium mobilization rate and the immediately available calcium<br />
reserves are sufficiently reduced incows in later pregnancy to render them incapable of<br />
withstanding theexpected loss of calcium in the milk. In older cows, bone resorption makes only a<br />
minor contribution to the total rate of calcium mobilization at parturition and is therefore of minor<br />
119
importance for the prevention of periparturient hypocalcemia. Osteoblasts are the only type of<br />
bone cell to express the 1,25-(OH)2 D receptor protein, and the decrease in the numbers of<br />
osteoblasts with increasing age could delay the ability of bone to contribute calcium to the plasma<br />
calcium pool (1).<br />
It was once postulated that failure to secrete sufficient levels of parathyroid hormone or<br />
1,25-dihydroxyvitainin D was the primary defect in cows which developed milk fever. While it is<br />
accepted that the calcium homeostatic mecha¬nisms, regulated by parathyroid hormone and<br />
1,25-dihydroxyvitamin D, fail to maintain normal blood calcium concentrations resulting in severe<br />
hypocalcemia, the nature of the endocrine defect is not well understood. It was also once thought<br />
that calcitonin, a hormone which inhibits bone calcium resorption was a cause of milk fever but<br />
this has not been demonstrated in cows with milk fever (1). Recent studies have shown that the<br />
secretion of parathyroid hormone and the production of 1,25-dihydroxyvitamin D is similar in<br />
most cows with or without milk fever (1). However, about 20% of cows treated for parturient<br />
paresis experience relapsing episodes of hypocalcemia which require further treatment. These<br />
cows fail to produce adequate levels of 1,25-dihydroxyvitamin D at the onset of lactation (7). Both<br />
relapsing and non-relapsing cows develop the same degree of hypocalcemia and secondary<br />
hyper-parathyroidism, but production of 1,25-dihydroxyvitamin D is about two-fold greater in<br />
non-relapsing cows than relapsing cows. Following treatment of parturient hypocalcemia with<br />
calcium salts IV and restoration of rumenal and intestinal motility, non-relapsing cows establish<br />
calcium homeostasis over the next 3-4 d by increasing intestinal absorption of calcium which is<br />
activated by a sufficient level of 1,25-dihydroxyvitamin D. In relapsing cows, even when rumen<br />
and intestinal motility are restored after treatment, hypocalcemia and paresis are likely to occur<br />
because of insufficient plasma 1,25-dihydroxyvitamin D. These cows may-remain in this stage of<br />
prolonged hypocalcemia for several days, and only after a few days and several repeated<br />
treatments with calcium will the plasma levels of 1,25-dihydroxyvitamin D increase to an<br />
adequate level to maintain calcium homeostasis. It is also unlikely that the parathyroid<br />
hormone-related protein in the colostrum of milk fever cows is involved in the disease (8).<br />
Tissue 1,25-dihydroxyvitamin D receptor concentrations decline with age, which renders older<br />
cows less able to respond to 1,25-dihydroxyvitamin D (1). The intestinal 1,25-(OH)2 D receptor<br />
numbers decline with age in the cow and thus the older cow is less able to respond to the hormone<br />
and will take longer to adapt intestinal calcium absorption mechanisms to meet lactational<br />
demands for calcium (9).<br />
A perplexing situation in dairy practice is the recently calved cow with peracute coliform<br />
mastitis which may also be mildly hypocalcemic and have some of the clinical signs of milk fever.<br />
The Escherichia coli endotoxin given IV depresses serum calcium and phosphate levels so that<br />
coliform mastitis may contribute to a degree of hypocalcemia in individual cows. However, there<br />
is no evidence that cows with peracute coliform mastitis require calcium therapy similar to that<br />
used in typical milk fever.<br />
Dietary and environmental risk factors<br />
Several dietary factors of the pregnant cow during the prepartum period (last 4 weeks) can<br />
influence the incidence of milk fever in cattle.<br />
DIETARY CALCIUM Feeding more than 100 g of calcium daily during the dry period is<br />
associated with an increased incidence of milk fever (10). A 500 kg cow requires only about 31 g<br />
of calcium to meet daily maintenance and fetal demands in late gestation. When a cow is fed a<br />
120
high calcium diet (>100 g Ca/d), its daily requirement for calcium can be met almost entirely by<br />
passive absorption of dietary calcium. The active transport of calcium from the diet and bone<br />
calcium resorption mechanisms are homeostati-cally depressed and become quiescent. As a<br />
consequence, at calving, the cow is unable to use bone calcium stores or intestinal calcium<br />
absorption mechanisms and is susceptible to severe hypocalcemia until these mechanisms can be<br />
activated, which may take several days. In a survey of dairy herds in France, the incidence of milk<br />
fever was higher in herds which had a higher dietary calcium in the mineral supplement during the<br />
total dry period and by longer feeding of soybean meal to dry cows (11). Alkaline diets containing<br />
an excessive concentration of sodium and potassium can result in an increased incidence of the<br />
disease.<br />
Feeding prepartum diets containing a low concentration of calcium prevents milk fever by<br />
activating calcium transport mechanisms in the intestine and bone prior to parturition, thus<br />
allowing the animal to adapt more rapidly to the lactational drain of calcium. Feeding diets high in<br />
calcium just before parturition may also lower the incidence of milk fever by increasing the<br />
absorption of calcium. This will provide sufficient calcium to overcome the relative lack of<br />
calcium from bone resorption which results from a high calcium intake (12).<br />
In sheep, hypocalcemia may occur in pregnant ewes fed a calcium-deficient diet over a prolonged<br />
period. A high dietary level of magnesium in late pregnancy may also predispose to hypocalcemia<br />
in pregnant ewes but this has not been documented. Ewes fed a diet with a fixed cation excess<br />
(82.3 mEq/100 g DM) had higher urine pH and lower urine calcium concentrations, lower blood<br />
ionized calcium concentrations after an overnight fast, and tended to develop hypocalcemia more<br />
rapidly after an ethylenediamine tetra-acetatc (NaEDTA) infusion (13). This suggests that a<br />
dietary fixed cation-anion balance may be a risk factor for hypocalcemia in pregnant ewes.<br />
DIETARY PHOSPHORUS Prepartum diets high in phosphorus (>80 g of P/d) also increases the<br />
incidence of milk fever and the severity of hypocalcemia (1). High dietary levels of phosphorus<br />
increase the serum level of phosphorus which is inhibitory to the renal enzymes that catalyze<br />
production of 1,25-(OH)2 D, which when decreased reduce the intestinal calcium absorption<br />
mechanisms prepartum.<br />
ANION-CATION DIETARY BALANCE The anion-cation dietary balance exerts a strong,<br />
linear effect on the incidence of milk fever. Recent studies indicate that the anion-ation balance<br />
(ACB) in the prepartum diet may be more important than the level of dietary calcium as a risk<br />
factor for milk fever. Prepartum diets high in cations such as sodium and potassium are associated<br />
with an increased incidence of milk fever, while diets high in anions, especially chloride and<br />
sulfur, are associated with a decrease in the incidence of the disease. Most forages such as<br />
legumes and grasses are high in potassium and are alkaline. The high anion content of acidic diets<br />
tends to induce a metabolic acidosis which facilitates bone resorption of calcium.<br />
A meta-analysis of 75 feeding trials designed to study the nutritional risk factors for milk fever<br />
in dairy cattle found that the prepartuni dietary concentrations of S and dietary anion-cation<br />
balance [(Na+K)-(Cl+S)] were the two nutritional factors most strongly correlated to the incidence<br />
of milk fever (12). Dietary S acts as a strong anion and reduces the risk of milk fever and<br />
increasing the dietary S concentrations lowers the odds ratio of developing milk fever. Increasing<br />
dietary Na and crude protein increased the odds ratios, but to lesser extent.<br />
Because sodium is a strong cation, it increases the risk of milk fever. The incidence of milk<br />
fever has been decreased by the addition of chloride and sulfur in excess relative to sodium and<br />
121
potassium in the prepartum diet of Holstein cows. High anion diets increase the plasma levels of<br />
1,25-(OH)2 D prior to parturition, activating intestinal calcium absorption and possibly bone<br />
calcium resorption mechanisms prior to onset of lactation (14).<br />
The mechanism of the positive effect of crude protein on incidence of milk fever is uncertain.<br />
Crude fiber was also significantly correlated to the incidence of milk fever. Other dietary<br />
electrolytes such as K and Cl were not associated with milk fever.<br />
ECONOMIC IMPORTANCE<br />
Compared to many years ago, the economic losses from milk fever have decreased because<br />
calcium borogluconate is an effective treatment which many owners can administer. Significant<br />
costs are associated with veterinary intervention and losses due to complications. However, while<br />
veterinarians now treat fewer cases of uncomplicated milk fever, there may be an increase in cases<br />
which are complicated by factors other than hypocalcemia. There is a highly significant<br />
relationship between milk fever and dystocia, retained fetal membranes, ketosis and mastitis.<br />
Cows which recover from milk fever are more likely to develop ketosis and mastitis compared to<br />
those which do not have milk fever. Milk fever in dairy cattle is a risk factor for several<br />
reproductive diseases such as dystocia, retained placenta, metritis and uterine prolapse (15). Some<br />
studies have found that milk fever directly increased the likelihood of developing<br />
hypomagnesemia, abomasal disease and ketosis (3). Dairy cows with hypocalcemia at parturtion<br />
had a 4.8-times greater risk of developing a left-sided displacement of the abomasum than cows<br />
with normal levels of serum calcium (16). The overall net effect is that j an incident of milk fever<br />
potentially reduces the mean productive life of a dairy cow by about 3 years.<br />
PATHOGENESIS<br />
Hypocalcemia<br />
Hypocalcemia is the cause of the signs of typical'milk fever'.Atonyof skeletalmuscle and plain<br />
muscle are well-knownphysiologicaleffects ofhypocalcemia. Hypophosphatemia and variations in<br />
levels of serum magnesium also occur and have secondary roles.In experimental hypocalcemia in<br />
cattle, there is:<br />
•A marked reduction in the stroke volume and cardiac output<br />
•A50%reductioninarterialblood pressure<br />
•A reduction in ruminal and abomasal tone and motility.<br />
There is some conflicting evidence about the effects of hypocalcemia on abomasal motility (17). If<br />
these changes occur in naturally occurring cases they would account for the muscle weakness,<br />
hypothermia and depression of consciousness. In calves infused with NaEDTA, the systemic<br />
arterial pressure and amplitude of ruminal contractions are severely decreased (18).<br />
Experimental hypocalcemia<br />
In experimental hypocalcemia in sheep, blood flow is reduced by about 60% to all tissues except<br />
kidney, heart, lung and bladder in which the reduction is not as high (19). During periods of<br />
prolonged hypocalcemia in cows and ewes, blood flow to skeletal muscles and the alimentary tract<br />
may be reduced to 60--70% of normal for a long period and predispose to the downer cow<br />
syndrome (20). In both cows and sheep there is a significant increase in PO2 causing an<br />
impairment of oxygen uptake by the pulmonary blood flow and an impairment of peripheral tissue<br />
uptake of oxygen during hypocalcemia in cows and sheep. Serum calcium and serum phosphate<br />
levels are significantly lower in clinical cases than in normal, comparable cows and there is some<br />
relationship between the severity of the signs and the degree of biochemical change. The complete<br />
122
esponse to the parenteral administration of calcium salts in most cases, and the occurrence of<br />
tetany coincident with hypocalcemia after the IV administration of NaEDTA is further evidence of<br />
the importance of hypocalcemia. In addition, some signs indicative of parathyroprivical tetany in<br />
other species are observed in the initial stages of milk fever:<br />
•Early excitement<br />
•Muscle twitching<br />
•Tetany, particularly of the hindlimbs<br />
•Hypersensitivity and convulsive movements of the head and limbs.<br />
The IV infusion of EDTA into cows over a period of 4-8 h results in severe hypocalcemia and<br />
paresis which is a reliable model for the reproduction of the disease. In the experimental disease,<br />
there are additional signs such as excessive salivation, excessive lip and tongue actions and tail<br />
lifting (21). The serum muscle enzyme levels of creatine phosphokinase (CPK) and<br />
aminotransferase (AST) increase due to muscle injury associated with prolonged recumbency.<br />
Blood glucose levels increase, and serum phosphorus and potassium levels decrease. A<br />
prolongation of the ST interval of the electrocardiogram (ECG) occurs, which may be useful as a<br />
diagnostic aid if suitable mini-ECG recorders could be made available for field use.<br />
The prolonged infusion of EDTA in sheep over 18 h at a rate to induce hypocalcemia and<br />
maintain recumbency resulted in prolonged periods of recumbency ranging from 36 -64 h before<br />
the animals were able to stand (10). There are also decreases in plasma sodium, plasma potassium<br />
and erythrocyte potassium and prolonged increases in packed cell volumes, which suggests that<br />
fluid replacement therapy may be indicated in cattle with prolonged recumbency associated with<br />
hypocalcemia (22). A 4-hour IV infusion of EDTA in high erythrocyte potassium and low<br />
erythrocyte potassium dairy cows causes decreases in plasma inorganic phosphorus and plasma<br />
potassium which are still below normal 24 h later (23). The AST(SGOT), CPK, and packed cell<br />
volumes (PCVs) and white blood cell (WBC) counts are also elevated 24 h later.Plasma<br />
magnesium and erythrocyte sodium and potassium were decreased but tins action was delayed.<br />
The increase in PCV was most pronounced in the low erythrocyte potassium cows, which may<br />
provide some clues about the pathogenesis of the downer cow syndrome. Some cows may have a<br />
more precipitate increase in PCVs due to loss of plasma volume and an inability to mobilize<br />
calcium. A 200 mL solution of 10 g of sodium chloride and 0.5 g of potassium chloride can be<br />
given IV to sheep safely over a period of 4-8 min to study the effects of administering such<br />
hypertonic solutions in downer animals (23).<br />
Peripartunent hypocalcemia may also result in some degree of impaired immune cell function<br />
but this effect is not well understood (24). A decline m concentrations of plasma zinc is more<br />
severe in cows with milk fever compared to parturient cows without milk fever but the<br />
significance is uncertain (25). Hypocalcemia in late pregnant ewes could induce neonatal<br />
hyperthyroidism, hypomsuhne-mia and metabolic alterations in their progeny (26).<br />
Hypomagnesemia<br />
When hypomagnesemia coexists with hypocalcemia the clinical signs continue but with normal or<br />
higher than normal levels, relaxation, muscle weakness, depression and coma supervene. It is<br />
likely that the hypocalcemic tetany is overcome by the relative hypermagnesemia (the ratio of<br />
Ca:Mg may change from 6:1 to 2:1) approximating the ratio at which magnesium narcosis<br />
develops. There is normally a rise in serum magnesium levels at calving but in those cases of<br />
parturient paresis in which tetany is a feature serum magnesium levels are low. These low levels<br />
123
are in many cases expressions of a seasonal hypomagnesemia.<br />
Hypophosphatemia<br />
Low serum phosphorus levels occur in milk fever and contribute to the clinical signs. Some cases<br />
of milk fever may not respond to calcium injections even though the serum calcium levels return<br />
to normal but may appear to recover when the udder is inflated and serum phosphorus levels rise.<br />
Field observations indicate sodium acid phosphate given orally or IV may result in recovery of<br />
cases not responding initially to calcium salts. However, it is difficult to reconcile the biochemical<br />
and clinical findings with low serum phosphorus levels because of the absence of recumbency in<br />
other animals with profound hypophosphatemia for long periods. A possible explanation is that<br />
the hypophosphatemia which occurs in milk fever is secondary to the hypocalcemia and<br />
recumbency rather than being a concurrent event. I here is experimental evidence to support this<br />
and it also seems probable that the hypophosphatemia could prolong the duration of recumbency.<br />
CLINICAL FINDINGS<br />
Cattle<br />
Three stages of milk fever in cattle are commonly recognized and described.<br />
Stage 1<br />
In the first stage the cow is still standing. This is also the brief stage of excitement and tetany with<br />
hypersensitivity and muscle tremor of the head and limbs. The animal is disinclined to move and<br />
does not eat. There may be a slight shaking of the head, protrusion of the tongue and grinding of<br />
the teeth. The rectal temperature is usually normal to slightly above normal. Stiffness of the<br />
hindlegs is apparent, the animal is ataxic and falls easily and, on going down, the hindlegs are<br />
stuck out stiffly.<br />
Careful observations by owners and veterinarians have revealed an even earlier stage than the first<br />
one. It is characterized by anorexia, agalactia, rumen stasis, scant feces and a normal temperature,<br />
heart rate and respirations. There are no obvious signs of excitement and hypersensitivity<br />
characteristic of the first stage. Affected cows may remain in this prodromal stage for several<br />
hours; they are perplexing diagnostically and respond quickly to calcium therapy. Cows with this<br />
form of hypocalcemia may be the 'calcium cyclers' described earlier.<br />
Stage 2<br />
The second stage is prolonged sternal recumbency. Consciousness is usually depressed; the cow<br />
has a drowsy appearance in sternal recumbency, usually with a lateral kink in the neck or the head<br />
turned into the flank. When approached, some of these cows will open their mouths, extend their<br />
head and neck and protrude their tongues, which may be an expression ot apprehension and fear in<br />
an animal unable to stand. The tetany of the limbs present in the first stage is not present and the<br />
cow is unable to stand. The muzzle is dry. the skin and extremities cool, and the rectal temperature<br />
subnormal (36-38℃, 97-101℉). There is a marked decrease in the absolute intensity of the heart<br />
sounds and an increase in rate (about 80 bpm). The arterial pulse is weak and the venous pressure<br />
is also low, making it difficult to raise the jugular veins. The respirations are not markedly<br />
affected, although a mild forced expiratory grunt or groan is sometimes audible.<br />
The eyes are usually dry and staring. The pupillary light reflex is incomplete or absent and the<br />
diameter of the pupil varies from normal to maximum dilatation. A detailed examination of the<br />
pupils of cows with parturient paresis, non-paretic disorders and non-parturient paresis found that<br />
the mean sizes of the pupils were not significantly different from one another (27). Rather,<br />
disparity of the size of the pupils was common. Ruminal sta¬sis and secondary bloat are common<br />
124
and constipation is characteristic. There is also relaxation of the anus and loss of the anal reflex.<br />
In cows which develop hypocalcemia a few hours before or at the time of parturition, the<br />
second stage of parturition may be delayed, which is unexpected in a mature cow. Examination of<br />
the reproductive tract usually reveals a fully dilated cervix and normal presentation of the fetus.<br />
The cow may be in any stage of milk fever, and administration of calcium borogluconate IV will<br />
usually result in a rapid beneficial response and normal parturition.<br />
Prolapse of the uterus is a common complication of milk fever and often the calcium levels are<br />
lower than in parturient cows without uterine prolapse. Thus it is standard practice to treat cases of<br />
uterine prolapse with calcium salts IV.<br />
Stage 3<br />
The third stage is lateral recumbency. The cow is almost comatose and although the limbs may be<br />
stuck out there is complete flaccidity on passive movement and the cow cannot assume sternal<br />
recumbency on its own. In general, the depression of temperature and the cardiovascular system<br />
are more marked. The heart sounds are almost inaudible and the rate increased to up to 120 bpm;<br />
the pulse is almost impalpable and it may be impossible to raise the jugular veins. Bloat is usual<br />
because of lateral recumbency. Without treatment, a few animals remain unchanged for several<br />
hours but most become progressively worse during .a period of several hours and dye quietly from<br />
shock in a state of complete collapse.<br />
CONCURRENT HYPOMAGNESEMIA. Mild to moderate tetany and hyperesthesia persisting<br />
beyond the first stage suggests a concurrent hypomagnesemia. There is excitement and fibnllary<br />
twitching of the eyelids, and tetanic convulsions are readily precipitated by sound or touch.<br />
Trismus may be present. The heart and respiratory rates are increased and the he,in sounds are<br />
much louder than normal. Without treatment death occurs during a convulsion.<br />
CONCURRENT HYPOFHOSPHATEM1A.<br />
With a concurrent hypophosphatemia, the clinical findings are typical of milk fever which<br />
responds to calcium therapy in all respects except that the cow is unable to stand after treatment.<br />
Sheep and goats<br />
The disease in pastured ewes is similar to that in cattle. The early signs include a Stilty, proppygait<br />
andtremorof the shoulder muscles. Recumbency follows, sometimes with tetany of the limbs but<br />
the proportion of ewes with hypocalcemia which are recumbent in the early stages is much less<br />
than in cattle. A similar generalization applies to female goats. The characteristic posture is sternal<br />
recumbency, with the legs under the body or stretched out behind. Ruminal movements are absent,<br />
the head is rested on the ground, there may be an accumulation of mucus exudate in the nostrils<br />
and the respiratory rate is increased. The venous blood pressure is low and the pulse impalpable.<br />
Mental depression is evidenced by a drowsy appearance and depression of the cornea reflex.<br />
Constipation is usual. Response to parenteral treatment with calcium salts is rapid, the ewe is<br />
normal 30 min after a SC injection. Death often occurs within 6-12 h if treatment is not<br />
administered. The syndrome is usually more severe in pregnant than in lactating ewes, possibly<br />
because of the simultaneous occurrence of pregnancy toxemia or hypomagnesemia. Fat late<br />
pregnant ewes on high grain diets indoors or in feedlots ; show a similar syndrome accompanied<br />
by prolapses of the vagina and intestine.<br />
Swine<br />
As in cattle, signs develop within a few hours of farrowing. There is restlessness, a normal<br />
temperature and anorexia followed by inability to rise and later lateral recumbency and coma.<br />
125
Milk How is decreased.<br />
CLINICAL PATHOLOGY<br />
Total serum calcium levels are reduced tobelow 8 mg/dL (2.0 mmol/L), usually to below 5 mg<br />
(1.2 mmol/L) and sometimes toas low as 2 mg (0.5 mmol/L).The reduction is usually, but not<br />
always, proportional to theseverity of the clinical syndrome. Average figures for total serum<br />
calcium levels in thethreespeciesare cows5.2+1.2 mg/dL(1.30+0.30 mmol/L), ewes 4.6+1.5<br />
mg/dL (1.15+0.37 mmol/L),goatdoes 3.8+0.6mg/dL (0.94+0.15 mmol/L).<br />
Total serum calcium levels are a basis for comparison between species. Blood levels of ionized<br />
calcium are a better indicator of calcium status but their estimation has been too difficult until<br />
recently. Although total serum calcium levels are used to express the animals' status with regard to<br />
calcium, it is possible that differences between the ionized and non-ionized compartments of total<br />
calcium may be more important than the total level. The development of a reliable calcium<br />
ion-selective electrode now makes it possible quickly and directly to determine the biologically<br />
active portion of calcium in plasma or serum (28). However, the correlation between ionized and<br />
total calcium is excellent (29). Equine, bovine, and ovine blood may be stored for up to 48 h<br />
without any clinically relevant alteration of blood calcium ion concentration (30).<br />
Normal levels of ionized calcium (as CaF) in venous whole blood of cows are 4.3-5.1<br />
mg/dL(1.06-1.26 mmol/L) serum, slight hypocalcemia 4.2-3.2 mg/dL (1.05-0.80 mmol/L),<br />
moderate 3.2-2.0 mg/dL (0.79-0.50 mmol/L) and severe hypocalcemia
A diagnosis of milk fever is based on the occurrence of paresis and depression of consciousness in<br />
animals following parturition. The diagnosis is supported by a favorable response to treatment<br />
with parenteral injections of calcium solutions, and by biochemical examination of the blood. In<br />
ewes, the history usually contains some reference to recent physical stress and the disease is more<br />
common in the period preceding lambing.<br />
In the immediate postpartum period, there are several diseases which cause recumbency in cows<br />
and their differentiation is summarized in Table 28.1.<br />
Several diseases which occur at the time of parturition must be differentiated from milk fever in<br />
cattle. These are grouped here according to:<br />
1.Other metabolic diseases<br />
2.Diseases associated with toxemia and shock<br />
3.Injuries to the pelvis and pelvic limbs<br />
4.Degenerative myopathy<br />
5.Downer cow syndrome.<br />
Table 28.1 Differential diagnosis of common causes of recumbency in parturient adult cattle<br />
Disease Epidemiology Clinical signs Clinical pathology Response to<br />
Milk fever<br />
(parturient<br />
paresis)<br />
Hypomagnesemia<br />
(lactation, grass<br />
tetany)<br />
Mature cows,<br />
within 48 h of<br />
calving, some<br />
in mid-lactation<br />
All classes of<br />
cattle, but most<br />
recently calved<br />
cows. Age no<br />
barrier and<br />
cases occur up<br />
to several<br />
months after<br />
calving. May<br />
Early excitement<br />
and tetany, then<br />
depression, coma,<br />
hypothermia,<br />
flaccidity, pupil<br />
dilatation, weak<br />
heart sounds. No<br />
rumen<br />
movements. Heart<br />
rate increases and<br />
worsens<br />
Excitement,<br />
hypersensitivity,<br />
muscle tremor,<br />
tetany. Recumbent<br />
with tetanic<br />
convulsions, loud<br />
heart sounds, rapid<br />
rate. Subacute<br />
cases remain<br />
127<br />
Hypocakemia, less<br />
than 5<br />
mg/dl(1.25mmol/l)<br />
calcium. High<br />
serum magnesium,<br />
over 3 mg/dL (1.25<br />
mmol/l), low<br />
inorganic<br />
phosphate, less<br />
than 3 mg/dL (0.9<br />
mmol/l)<br />
Low serum<br />
magnesium, less<br />
than 1.2 mg/dL<br />
(0.5 mmol/l)<br />
treatment<br />
Rapid,<br />
characteristic<br />
response<br />
(muscle<br />
tremor,<br />
sweating on<br />
muzzle,<br />
defecation,<br />
urination, pulse<br />
amplitude and<br />
heart sound<br />
intensity<br />
improves first)<br />
after IV<br />
injection<br />
soluble<br />
calcium salt<br />
Even after IV<br />
injection,<br />
response in a<br />
severe case<br />
may take 30<br />
min, much<br />
slower than<br />
response to<br />
calcium in
Severe toxemia<br />
(acute diffuse<br />
peritonitis,<br />
coliform mastitis)<br />
Maternal<br />
obstetrical<br />
paralysis (MOP)<br />
Fat cow<br />
syndrome<br />
occur in<br />
pregnant beef<br />
cattle<br />
Sporadic only.<br />
Mastitis most<br />
common where<br />
hygiene poor.<br />
Peritonitis due<br />
to foreign body<br />
perforation of<br />
reticulum,<br />
rupture of<br />
uterus or<br />
vagina<br />
Prolonged<br />
difficult<br />
calving. Heifers<br />
and young<br />
cows or large<br />
calves<br />
delivered with<br />
excessive<br />
traction<br />
Fat dairy or<br />
beef cows in<br />
late gestation or<br />
at parturition.<br />
Some<br />
predisposing<br />
cause<br />
precipitates<br />
illness in fat<br />
animals<br />
standing<br />
Recumbency,<br />
depression to<br />
coma, sleepy, dry<br />
nose, hypothermia,<br />
gut stasis, HR over<br />
100 bpm, may be<br />
grunting. Examine<br />
mammary gland.<br />
Examine abdomen<br />
for abdominal<br />
disease<br />
Bright, alert, eat,<br />
drink, defecate, try<br />
to rise and cannot<br />
quite make it or do<br />
splits. TRP and<br />
rumen movements<br />
normal<br />
Excessive body<br />
condition,<br />
anorexia, apathy,<br />
depression,<br />
recumbency and<br />
looks like milk<br />
fever, scant soft<br />
feces, ketonuria<br />
Profound<br />
leukopenia. Serum<br />
calcium may be as<br />
low as 7-8 mg/dL<br />
(1.75-2.0 mmol/l).<br />
Examine milk<br />
(CMT)<br />
Normal. CPK may<br />
become high if<br />
much muscle<br />
damage<br />
Evidence of<br />
hepatic disease<br />
milk fever<br />
Require<br />
supportive<br />
response for<br />
toxemia and<br />
shock.<br />
Response is<br />
poor and<br />
temporary.<br />
Prognosis very<br />
bad. May die if<br />
treated IV with<br />
calcium or<br />
magnesium<br />
salts<br />
Nil to clinical<br />
treatments.<br />
Need slinging<br />
by hip sling or<br />
nursing on<br />
deep straw<br />
with frequent<br />
movement. If<br />
not recovered<br />
by third day,<br />
prognosis may<br />
be unfavorable<br />
Will recover if<br />
cows begin to<br />
eat. Treat with<br />
fluids, glucose,<br />
insulin.<br />
Provide good<br />
quality<br />
palatable<br />
roughage<br />
Downer cow Most common Moderately bright Variable. May be Variable<br />
128
syndrome in situation<br />
where milk<br />
fever and<br />
lactation tetany<br />
common and<br />
intensity of<br />
treatment is lax<br />
cows are left<br />
down too long<br />
before<br />
treatment<br />
Physical injuries Ruptured<br />
Acute<br />
hypokalemia<br />
Metabolic diseases<br />
gastrocnemius,<br />
dislocation of<br />
hip, etc.<br />
Sporadic<br />
sequelae to<br />
milk fever, may<br />
be contributed<br />
to by<br />
osteoporosis,<br />
slippery ground<br />
surface,<br />
stimulating to<br />
rise too early<br />
Postpartum<br />
cows treated<br />
with<br />
soflupredone<br />
active, eating.<br />
Temperature<br />
slightly raised, HR<br />
80-100 bpm.<br />
Unable to stand<br />
but tries<br />
-'creepers'. When<br />
dull and<br />
depressed, are<br />
'non-alert<br />
downers'. Long<br />
course 1-2 weeks<br />
As for MOP with<br />
ruptured<br />
gastrocnemius,<br />
hock remains on<br />
ground when<br />
standing.<br />
Excessive lateral<br />
mobility of limb<br />
with hip<br />
dislocation<br />
Recumbent, weak,<br />
faccid, unable to<br />
hold head off<br />
ground. Cardiac<br />
arrhythmia<br />
low inorganic<br />
phosphate, or<br />
potassium, or<br />
glucose. Ketonuria,<br />
usually proteinuria.<br />
CPK and AST<br />
elevated<br />
Increased CPK and<br />
SGOT<br />
Lower potassium,<br />
below 2.3m Eq<br />
response to<br />
calcium,<br />
phosphorus<br />
and potassium<br />
salts. Fluid<br />
therapy and<br />
provision of<br />
deep bedding<br />
and hourly<br />
rolling from<br />
side to side are<br />
necessary<br />
Supportive<br />
therapy, deep<br />
bedding and<br />
frequent rolling<br />
Potassium<br />
Chloride IV<br />
and oral<br />
Hypomagnesemia may occur as the sole cause of recumbency or it may accompany a primary<br />
hypocalcemia so that the case presented is one of parturient paresis complicated by lactation<br />
tetany. Hyperesthesia, tetany, tachycardia and convulsions are common instead of the typical<br />
findings of depression and paresis in milk fever.<br />
Hypophosphatemia, which commonly accompanies milk fever, is suggested as a cause of<br />
continued recumbency in cows after partial response to calcium therapy; serum inorganic<br />
phosphorus levels are low and return to normal if the cow stands or following treatment with<br />
phosphate salts. A sudden onset of recumbency in dairy cows associated with a marginal<br />
deficiency of phosphorus has been reported (31).<br />
Hypokalemia in dairy cows is characterized by extreme weakness or recumbency, especially<br />
129
after treatment for ketosis with isoflupredone (32). Hypokalemia is marked as ranging from 1.4 to<br />
2.3 mEq/L. The case-fatality rate is high in spite of therapy with potassium. Hypokalemic<br />
myopathy is present at necropsy.<br />
Ketosis may complicate milk fever, in which case the animal responds to calcium therapy by<br />
standing but continues to manifest the clinical signs of ketosis, including in some cases the<br />
nervous signs of licking, circling and abnormal voice.<br />
Diseases associated with toxemia and shock<br />
During the immediate postparturientperiod, several diseases occur commonly and are<br />
characterized by toxemia.<br />
Peracute coliform mastitis is characterized by:<br />
•Fever initially followed by hypothermia<br />
•Tachycardia<br />
•Dehydration<br />
•Weakness and recumbency<br />
•Depression<br />
•Ruminal stasis<br />
•Diarrhea in some<br />
•Enlarged mammary gland(s) with watery and serous-like secretions with<br />
small particles barely visible.<br />
Aspiration pneumonia secondary to regurgitation and aspiration of rumen contents may occur as<br />
a complication of third-stage milk fever. Fever, dyspnea, expiratory grunt, severe depression and<br />
anxiety are common. Auscultation of the lungs reveals the presence of abnormal lung sounds.<br />
Aspiration pneumonia should be suspected if the animal has been lying on its side, especially if<br />
there is evidence of regurgitation of ruminal contents from the nostrils, no matter how small the<br />
amount, or if there is a history of the animal having been drenched. Abnormal auscultatory<br />
findings may not be detectable until the second day. Early diagnosis is imperative if the animal is<br />
to be saved and the mortality rate is always high.<br />
Acute diffuse peritonitis resulting from traumatic perforation of the reticulum or uterus is<br />
characterized by:<br />
•Severe depression<br />
•Fever<br />
•Weakness and recumbency<br />
•Ruminal stasis<br />
•Dehydration<br />
•Grunting or groaning with each respiration<br />
•Tachycardia<br />
•Fluid splashing sounds on ballottement of the abdomen (paralytic ileus).<br />
Carbohydrate engorgement results in:<br />
•Depression<br />
•Weakness<br />
•Sternal recumbency<br />
•Dehydration<br />
•Tachycardia<br />
•Ruminal stasis and moderate bloat<br />
130
•Fluid-splashing sounds over rumen<br />
•Low rumen juice pH<br />
•Diarrhea<br />
•Hypothermia<br />
•Cool extremities<br />
•Progressive worsening if not treated.<br />
Many cases resemble second-stage milk fever.<br />
Toxemic septic metritis occurs most commonly within a few days after parturition and is<br />
characterized by:<br />
•Depression<br />
•Anorexia<br />
•Fever<br />
•Tachycardia (100-120 bpm)<br />
•Ruminal stasis<br />
•Presence of foul-smelling uterine discharge found on vaginal examination.<br />
The fetal placenta may be retained. Some affected cows are weak and prefer recumbency,<br />
which resembles milk fever. Prolapse and rupture of uterus causes varying degrees of:<br />
•Shock with tachycardia<br />
•Flypothermia and cool extremities<br />
•Weakness and recumbency<br />
•Rapid death.<br />
A history of difficult parturition or assisted dystocia with fetotomy may be associated with<br />
rupture of the uterus. The administration of calcium salts may cause ventricular fibrillation and<br />
sudden death.<br />
Although some elevation of the temperature may be observed in these severe toxemic states, it<br />
is more usual to find a subnormal temperature. The response to calcium therapy is usually a<br />
marked increase in heart rate, and death during the injection is common. Every case of<br />
recumbency must be carefully examined as these conditions may occur either independently or as<br />
complications of parturient paresis. In our experience, about 25% of cases of postparturient<br />
recumbency in cows are due primarily to toxemia or injury rather than to hypocalcemia.<br />
Injuries to the pelvis and pelvic limbs<br />
Injuries to the pelvis and pelvic limbs are common at parturition because of the marked relaxation<br />
of the ligaments of the pelvic girdle. Seven types of leg abnormality have been described in this<br />
group at an incidence level of 8.5% in 400 consecutive cases of parturient paresis (33). The<br />
abnormalities included radial paralysis, dislocation of the hips and rupture of gastrocnennus<br />
muscle. In most instances the affected animals are down and unable to stand but they eat, drink,<br />
urinate and defecate normally, have a normal temperature and heart rate and make strong efforts to<br />
stand, particularly with the forelimbs.<br />
Maternal obstetrical paralysis is the most common injury. Although this occurs most frequently<br />
in heifers after a difficult parturition, it may also occur in adult animals following an easy birth,<br />
and occasionally before parturition, especially in cows in poor body condition. The mildest form is<br />
evidenced by a frequent kicking movement of a hindleg as though something was stuck between<br />
the claws. All degrees of severity from this, through knuckling and weakness of one or both<br />
hindlegs, to complete inability to rise may occur, but sensation in the affected limb is usually<br />
131
normal. There is traumatic injury to the pelvic nerves during passage of the calf. There are often<br />
gross hemorrhages, both deep and superficial, and histopathological degeneration of the sciatic<br />
nerves. In individual animals, injury to the obturator nerves is common and results in defective<br />
adduction of the hindlimbs. The position ot the hindlimbs may be normal but in severe cases,<br />
especially those with extensive hematoma along the sciatic nerve trunk, the leg may be held<br />
extended with the toe reaching the elbow as in dislocation of the hip; however in the latter case<br />
there is exaggerated lateral mobility of the limb. Additional injuries causing recumbency near<br />
parturition include those associated with degenerative myopathy, dislocation of the hip and ventral<br />
hernia.<br />
Dislocation ot the coxofemoral joint can cause recumbency and inability to stand in some cows,<br />
while others can stand and move around (34). Recumbent cows are usually in sternal recumbency<br />
and the affected limb is abducted excessively. In standing cows, the affected limb is usually<br />
extended, often difficult to flex and often rotated about its long axis. The diagnostic criteria are:<br />
1.Sudden onset of lameness with the affected limb extended and possibly rotated<br />
2.Displacement of the greater trochanter of the femur from its normal position relative to the<br />
ischiatic tuber and coxal tuber of the pelvis<br />
3.Ability to abduct the limb manually beyond its normal range<br />
4.CrepitUS in the hip on abduction and rotation of the limb<br />
5.Ability to palpate the femoral head per rectum or per vaginum against the cra nial border of the<br />
ilium or pubis in cases of cranioventral dislocation, or in the obturatorforamenincasesof<br />
caudoventral dislocation.<br />
Manual replacement by closed reduction is successful in 80% of craniodorsal dislocation and<br />
65% in caudodorsal dislocation. The ability to stand before reduction is the most useful prognostic<br />
aid (35).<br />
Degenerative myopathy (ischemic muscle necrosis)<br />
Degenerative myopathy affecting primarily the large muscles of the thighs, occurs commonly in<br />
cattle which have been recumbent for more than several hours. At necropsy, large masses of pale<br />
muscle are present surrounded by muscle of normal color. Clinically it is indistinguishable from<br />
sciatic nerve paralysis. Markedly increased serum levels of CPK occur in cows recumbent for<br />
several hours following the initial episode of milk fever due to ischemic necrosis. Persistent<br />
elevation of CPK indicates progressive ischemic muscle necrosis due to continued compression of<br />
large muscle masses of the pelvic limbs. Rupture of the gastrocneniius muscle or separation of its<br />
tendon from either the muscle or the tuber calcis may also cause myopathy.<br />
Downer cow syndrome<br />
Downer cow syndrome is a common sequel to milk fever in which the cow was in sternal<br />
recumbency for several hours before being treated with calcium. Following treatment, most of the<br />
clinical findings associated with milk fever resolved except the animal was unable to stand.<br />
Clinically the animal may be normal except for recumbency and will commonly recover and stand<br />
normally within several hours or a few days. Most downer cows eat and drink normally, their vital<br />
signs are within the normal range, and their alimentary tract function is normal. However. some<br />
are anorexic, may not drink, exhibit bizzare movements of lying in lateral recumbency and<br />
dorsally extend their head and neck frequently, moan and groan frequently, assume a frog-legged<br />
posture with their pelvic limbs and crawl or creep around the stall, and may die or are euthanized<br />
for humane reasons in a few days. The diagnostic dilemma with these cows is that they resemble<br />
132
milk lever and whether or not to treat them with additional amounts of calcium salts is<br />
questionable.<br />
Non-parturient hypocalcemia<br />
Paresis with mental depression and associated with low total scrum calcium levels can occur in<br />
cows at times other than at parturition. The cause is largely unexplained but the syndrome occurs<br />
rarely in animals other than ruminants. Hypocalcemia may occur after gorging on gram and may<br />
be a significant factor in particular cases. Sudden rumen stasis due to traumatic reticulitis may<br />
rarely cause hypocalcemic paresis. Diarrhea, particularly when cattle or sheep are placed onnew<br />
lush pasture, may also precipitate an attack. Access to plants rich in oxalates may have a similar<br />
effect, particularly if the animals are unaccustomed to the plants. Affected animals respond well to<br />
calcium therapy but relapse is likely unless the primary cause is corrected. The differential<br />
diagnosis of diseases of non-parturient cows manifested principally by recumbency is also<br />
summarized in Table 28.1.<br />
Hypocalcemic paresis in sheep and goats<br />
Hypocalcemia in sheep must be differentiated from pregnancy toxemia in which the course is<br />
much longer, the signs indicate cerebral involvement and the disease is restricted to pregnant ewes.<br />
There is no response to calcium therapy and a positive test for ketonuria is almost diagnostic of<br />
the disease. At parturition, goats are susceptible to enterotoxemia and hypo-glycemia (rarely),<br />
both of which present clinical signs similar to parturient paresis.<br />
Hypocalcemia in sows<br />
Hypocalcemia is rare in sows. The disease must be differentiated from the mastitis, metritis, and<br />
agalactia complex, which is characterized by:<br />
•lever<br />
•Agalactia<br />
•Anorexia<br />
•Toxemia<br />
•Enlarged mammary glands.<br />
Treatment<br />
Every effort should be made to treat affected cows as soon as possible after clinical signs are<br />
obvious. Treatment during the first stage of the disease, before the cow is recumbent, is the ideal<br />
situation. The longer the interval between the time the cow first becomes recumbent and treatment,<br />
the greater the incidence of the downer cow syndrome due to ischemic muscle necrosis from<br />
prolonged recumbency. Complications of milk fever occur when cows have been in sternal<br />
recumbency for more than 4 h. Farmers must be educated to appreciate the importance of early<br />
treatment. Cows found in lateral recumbency (third stage) should be placed in sternal recumbency<br />
until treatment is available. This will reduce the chances of aspiration if the cow regurgitates.<br />
Cows that have difficulty finding solid, non-slip footing beneath them, for example, a slippery<br />
barn floor or slippery mud, will often not try to stand and may develop ischemic myonecrosis.<br />
Avoidance of this complication necessitates the placement of rubber or other mats under the cow<br />
or transportation of the cow to a piece of pasture with a dense sward on it. A temperature of<br />
greater than 39℃(102℉) is an indication of a higher than average mortality rate due to<br />
pre-existing complications.<br />
Standard treatment<br />
133
Calcium borogluconate at 100 -200 g is the treatment of choice. The solutions available vary from<br />
18-40% calcium borogluconate. Most cows with milk fever can be treated successfully with 8-10<br />
g of calcium (calcium borogluconate is 8.3% calcium). For cattle, 400-800 mlof a 25% solution is<br />
the usual dose. The dose rate of calcium is frequently under discussion (25). There is a general<br />
tendency for veterinarians to underdose with calcium salts, largely because of toxic effects which<br />
tend to occur when all of the calcium is given intravenously. As an initial dose a large cow<br />
(540-590 kg) requires 800-1000 ml of a 25% solution and a small cow (320-360 kg) 400-500 ml..<br />
Underdosing increases the chances of incomplete response, with inability of the cow to rise, or of<br />
relapse. In general, 12 g of calcium is superior to 8 g, whichin turn is superior to 6 g.<br />
In sheep and goats, the recommended amount is 15-20 g IV with an optional 5-10 g SC. Sows<br />
should receive 100-150 mL of a similar solution IV or SC.<br />
Routes of administration<br />
IV and SC routes<br />
The intravenous route is preferred because the response is rapid and obvious. The heart should be<br />
auscultated throughout the intravenous administration for evidence of gross arrhythmia,<br />
bradycardia and tachycardia. If any of these occurs, the intravenous administration should be<br />
interrupted and continued only after the heart sounds return to normal. If the cardiac irregularity<br />
continues, the remainder of the solution can be given subcutaneously. The best recommendation is<br />
to give as much of the solution as possible intravenously and the remainder subcutaneously. The<br />
common practice of giving half the does intravenously and half subcutaneously is a reasonable<br />
compromise because with this method there are fewer relapses. If a cow has been previously<br />
treated subcutaneously by the farmer, additional calcium given intravenously may cause toxicity if<br />
the improved circulation enhances the absorption of the subcutaneous calcium.<br />
SC route<br />
The SC route is commonly used by farmers who treat affected cows at the first sign of<br />
hypocalcemia, preferably during the first stage when the cow is still standing or as prophylaxis to<br />
all high-risk cows immediately after calving. The SC route has also been used by veterinarians<br />
when the effects of IV administration of calcium are uncertain or if an unusual response occurs<br />
during IV administration. There are limitations to the effectiveness of SC calcium solutions given<br />
to cows with milk fever (36). Cows given 300 mL of 33.3% or 40% calcium borogluconate SC<br />
had serum calcium levels of 1.4 mmol/L; those receiving 600 mL had serum calcium levels of 2.1<br />
mmol/L, at mean intervals of 4.8 and 12.0 h between treatment by the herdman and veterinary<br />
attention (36). At the time of sampling, 48% of cows receiving 600 mL of calcium borogluconate<br />
had a serum calcium level below 2.0 mmol/L. If the veterinarian is unable to treat the cow within<br />
1 hour, a dose of 600 ml. of 40% calcium borogluconate should be given SC in two sites and<br />
massaged well to promote absorption. Waiting for more than 1 hour to assess the effect of one<br />
treatment SC is regarded as conducive to development of the downer cow syndrome. The cow<br />
should then be placed in a dry area with her limbs positioned to minimize ischemic necrosis and<br />
covered with straw and tarpaulins until the veterinarian arrives.<br />
Toxemic cows are very susceptible to the IV administration of calcium borogluconate and death<br />
may occur. In such cases the heart rate increases markedly (up to 160 bpm), there is respiratory<br />
distress, trembling and collapse and the cow dies within a few minutes. SC or IP administration is<br />
preferred in cows with severe toxemia due to aspiration pneumonia, metritis and mastitis.<br />
Oral route<br />
134
A further aid to parenteral therapy with solutions of calcium salts, especially for the purpose of<br />
increasing recovery rates andpreventing relapses, is the oral administration of gels containing<br />
calcium chloride, which are described under prevention.<br />
Typical response to calcium borogluconate<br />
Cows with milk fever exhibit a typical pattern of response to calcium borogconate IV if the<br />
response is favorable, including:<br />
•Belching<br />
•Muscletremor,particularlyofthe flanksandoftenextending tothe whole body<br />
•Slowingandimprovementin the amplitude and pressures of the pulse<br />
•Increase in the intensity of the heart sounds<br />
•Sweating of the muzzle<br />
•Defecation.<br />
The feces arc in the form of a firm fecal ball with a firm crust and covered with mucus,<br />
occasionally with a few flecks of blood. Urination usually does not follow until the cow stands. A<br />
slight transitory tetany of the limbs may also be observed. Many cows will eat and drink within<br />
minutes following successful treatment if offered feed and water.<br />
The rate of response to treatment is affected by many factors as set out below and it is unwise to<br />
quote what might be expected as an acceptable rate of recovery after treatment. This is particularly<br />
true if cows are treated by the farmer, and only difficult cases are presented to the veterinarian. In<br />
general, if all cases are considered and there are no exceptional circumstances, recovery can be<br />
expected immediately after treatment in about 60% of cases and in a further 15% after 2h -10%<br />
have recoveries complicated by one of the diseases discussed earlier and 15% can be expected<br />
either to die or to require disposal. Of those which recover after one treatment, 25-30% can be<br />
expected to relapse and require further treatment.<br />
Unfavorable response to calcium borogluconate<br />
An unfavorable response is characterized by a marked increase in heart rate in cows affected with<br />
toxemia and acute heart block in apparently normal animals especially with overdosage, with too<br />
rapid injection and in cases in which treatment has been unduly prolonged. In the latter,the<br />
maximum tolerated dose of calcium borogluconate by IV administration is about 250 mL of a<br />
25% solution. Overdosage may occur when farmers treat cases unsuccessfully by multiple SC<br />
injections and these are followed by an IV dose. When the peripheral circulation is poor, it is<br />
probable that the calcium administered SC is not absorbed until the circulation improves following<br />
the IV injection, and the large doses of calcium then absorbed cause acute toxicity. In all cases of<br />
IV injection, the circulation must be monitored closely. Some degree of arrhythmia occurs in most<br />
cases but if there is gross arrhythmia or a sudden increase in heart rate, the injection should be<br />
stopped temporarily or continued with great caution. In normal circumstances at least l0 min<br />
should be taken to administer the standard dose. The acute toxic effect of calcium salts seems to<br />
be exerted specifically on heart muscle with a great variety of defects occurring in cardiac action;<br />
the defect type depends on the specific calcium salt used and the speed of injection. ECG changes<br />
after induced hypercalcemia show increased ventricular activity and reduced atrial activity.<br />
Atropine is capable of abolishing the resulting arrhythmia.<br />
Sudden death may also occur after calcium injections if the cow is excited or frightened, which<br />
may be due to an increased sensitivity to epinephrine. When affected cows are exposed to the sun<br />
or a hot, humid atmosphere, heat-stroke may be a complicating factor. In such cases an attempt<br />
135
should be made to reduce the temperature to below 39.5℃ (103 ℉) before the calcium is<br />
administered. The incidence of cardiac arrhythmia and other abnormalities as detected by ECG<br />
during treatment with calcium salts IV is so high that there are doubts expressed about the<br />
suitability of this form of treatment.<br />
Chronic toxicity may also occur. In laboratory animals, severe uremia due to extensive calcium<br />
deposits in the kidney occur after the SC injection of calcium chloride and borogluconate, and<br />
similar deposits are often seen at necropsy in cows dying after multiple injections of calcium salts<br />
administered at short intervals.<br />
Failure to respond to treatment<br />
A failure to respond favorably to treatment may be due to an incorrect or incomplete diagnosis, or<br />
inadequate treatment. A poor response to treatment includes (1) no observable changes in the<br />
clinical findings immediately following the calcium administration or (2) the animal may respond<br />
to the calcium in all respects with the exception of being unable to stand for varying periods of<br />
time following treatment. An indequate response also includes relapses after successful recovery,<br />
which usually occur within 48 h of the previous treatment. Relapses are more common in certain<br />
individual cows such as mature Jersey cows which may experience as many as five or six episodes<br />
around one calving. Also, the incidence of relapses is much higher in cases which occur just<br />
before calving than in those which occur afterwards. The needs of individual animals for calcium<br />
replacement vary widely, depending on their body weight and the degree of hypocalcemia.<br />
Incomplete responses may be more common in older cows and may be associated with diminished<br />
skeletal reserves of calcium and inability of the normal mechanisms to maintain serum calcium<br />
levels during the period of excessive demands of lactation. The duration of the illness and the<br />
posture of the cow also affect the response. In an extensive field study, there were no downer<br />
cows or deaths in cows still standing when first treated, 13% of downers and 2% of deaths<br />
occurred in cows in sternal recumbency, and 37% of downers and 12% of deaths occurred in cows<br />
in lateral recumbency when first treated (37). Therefore, in general, the longer the period from<br />
onset of milk fever to treatment, the longer the period of post-treatment recumbency and the<br />
higher the case-fatality rate. In another study, 67% of cows recovered after a single treatment,<br />
90% after two treatments and 92-99% after three treatments. After routine treatment, 37% of cases<br />
rose unassisted within 10 min 23% required some-assistance, 26% recovered after longer periods<br />
of recumbency and 14% died or were destroyed or sold for slaughter. The best procedure to follow<br />
if response does not occur is to revisit the animal at 12-hourly intervals and check the diagnosis. If<br />
no other cause of the recumbency can be determined the initial treatment can be repeated on a<br />
maximum of three occasions. Beyond this point further calcium therapy is seldom effective. A low<br />
body temperature, due probably to exposure to low environmentaltemperature,and increased wind<br />
velocities, is positively correlated with a high proportion of deaths and poor responses.<br />
At the second visit, solutions containing either phosphorus, magnesium or dextrose may be<br />
administered, depending upon the clinical signs presented and the results of available biochemical<br />
tests. Glucose is usually administered as 500 mL of a 40% solution, sodium acid phosphate as 200<br />
mL of a 15% solution, and magnesium sulfate as 200-400 mL of a 15% solution. Composite<br />
solutions containing calcium, magnesium, phosphorus and glucose are also in common use as<br />
initial treatments. There is controversy about these so-called 'polypharmacy' preparations. They<br />
have no advantage, but are likely to remain popular when milk fever cases are complicated by<br />
metabolic disorders other than hypocalcemia. They have no effect on the relapse rate when<br />
136
compared with calcium salts alone.<br />
Udder insufflation<br />
Insufflation of the udder with air was an alternative treatment for cows which continued to relapse<br />
following repeated calcium injections. With the availability and effectiveness of orally<br />
administered calcium gels, udder insufflation cannot be recommended.<br />
GENERAL MANAGEMENT AND CLINICAL CARE PROCEDURES<br />
The care of the cow and the calf following milk fever is important. The calf should be removed<br />
from the cow and for the first 48 h only sufficient milk drawn for the calfs maintenance. A gradual<br />
return to full milking can then be permitted. If the cow is recumbent for any length of time, she<br />
must be kept propped up in sternal recumbency and not left in lateral recumbency, which may<br />
result in regurgitation and aspiration pneumonia. The cow should be rolled from side to side every<br />
few hours and provided with adequate bedding or moved to a suitable non-slip ground surface. In<br />
extreme climatic conditions, erection of a shelter over the cow is advisable if she cannot be moved<br />
to permanent shelter. It a cow is recumbent for more than 48 h, assisted lifting using appropriate<br />
cow lifters several times daily should be considered. However, heroic measures to get cows to<br />
stand should be avoided. Gentle nudging in the ribs or the use of an electric prod are the maximum<br />
stimulants advised.The best assistance that can be given to a cow attempting to stand is a good<br />
heave at the base of the tail when she is halfway up.<br />
CONTROL<br />
Various methods for the control of milk fever in ruminants, especially dairy cows, are available.<br />
They include dietary management during the prepartum period, administration of calcium gels<br />
orally at the time of parturition, and administration of vitamin D and its metabolites and analogs<br />
immediately before parturition to enhance the mobilization of calcium. When the incidence of<br />
milk lexer increases to above 10% of high-risk cows (third or later lactations), a specific control<br />
program is necessary. When the incidence is low, a specific control program may not be<br />
economical and the alternative is to monitor cows carefully at the time of parturition and for 48 h<br />
after parturition and treat affected animals during the first stage of the disease if possible.<br />
Dietary management during prepartum period<br />
Level of calcium in diet<br />
Diets high in calcium during the prepartum period can result in a high incidence of milk fever, and<br />
diets low in calcium will reduce the incidence of milk fever in dairy cows. Feeding more than 100<br />
g of calcium daily during the dry period is associated with an increased incidence of milk fever. A<br />
cow weighing 500 kg requires only about 30 g of calcium to meet maintenance and fetal calcium<br />
demands in late gestation. Low calcium diets (20 g Ca/d) fed during the. last 2 weeks before<br />
parturition are highly reliable and effective.<br />
Level of phosphorus in diet<br />
Increased levels of dietary phosphorus, greater than 80 g per head per day, can also increase the<br />
incidence of milk fever. The increased intake increases the serum level of phosphorus which has<br />
an inhibitory effect on renal enzymes. These enzymes catalyze the production of 1,25-(OH)2D,<br />
which when lowered will reduce intestinal calcium absorption. If the reduction of calcium is<br />
impractical, the lowering of phosphorus to below requirements may be beneficial.<br />
Calcium and phosphorus ratio in diet<br />
If the ration is low in calcium, the resultnig negative balance of calcium can be expected to<br />
stimulate activity of the parathyroid gland. Early researchers made use of this physiological<br />
137
mechanism by feeding a high phosphorus/low calcium ration to cows during the last month of<br />
pregnancy. With a Ca:P ratio of 6:1, 30% of cows developed parturient paresis; at a Ca:P ratio of<br />
1:1, 15% developed the disease; and at a ratio of 1:3.3, no cases occurred. Although there is no<br />
apparent effect on the subsequent lactation there is the possibility, if the negative balance of<br />
calcium is prolonged or repeated frequently, that such a ration may contribute to the development<br />
of oesteoporosis. Dietary phosphorus concentrations can have an influence on calcium<br />
homeostasis.<br />
Practicality of feeding diets low in calcium<br />
There arc practical problems with the implementation of the recommendation to feed diets low in<br />
calcium. It is difficult to reduce the amounts of calcium and phosphorus led to cows for several<br />
reasons:<br />
1.Inability to grow sufficient quantities of feeds, such as corn silage, for the entire herd<br />
2.Suitability of land for legume crops which are high in calcium<br />
3.Inability to add sufficient phosphorus to lower the ratio of calcium to phosphorus to palatability<br />
when quantities of phosphorus are added to the ration.<br />
Most farms utilizing home-grown forages, especially alfalfa, find it difficult to obtain forages<br />
which are low in calcium. In addition, while feeding diets low in calcium during the prepartum<br />
period is very effective, the very low calcium intake required necessitates that the cow be in<br />
negative calcium balance and in a state of withdrawal of calcium from bone.<br />
Dietary cationanion difference<br />
A more reliable method of controlling milk fever in dairy cows when the calcium intake exceeds<br />
NRC requirements is to manipulate the dietary cation-anion difference (DCAD) (38). Diets high in<br />
cations, especially sodium and potassium, tend to induce milk fever compared with those high in<br />
anions, primarily chloride and sulfur, which can reduce the inci¬dence. Because most legumes and<br />
grasses are high in potassium, many of the com¬monly used prepartum diets are alkaline. The<br />
feeding of diets which are high in ratio of calcium to phosphorus and containing an excess of<br />
anions relative to cations will result in increased concentrations of serum calcium due to an<br />
increase in the intestinal absorption of calcium.<br />
In one study, the incidence of milk fever was 47% when prepartum cows were fed a ration with<br />
a DCAD of +330.5 mEq/kg dietary DM and 0% incidence when the prepartum ration had a<br />
balance of-128.5 mEq/kg dietary DM (38). The incidence of milk fever was reduced by the<br />
addition of chloride and sulfur in excess relative to sodium and potassium in the diet (38). Because<br />
anions are considered acidogeme and cations alkalogenic, an excess of acid-forming elements in<br />
periods of calcium stress will increase the concentration of calcium in the blood, either by<br />
intestinal absorption or bone mobilization (2. 39). Cows fed prepartum diets containing alfalfa<br />
haylage with added chlorides of magnesium, ammonia and calcium tended to have higher plasma<br />
calcium concentrations of calcium and a lower incidence of milk fever than did cows fed cither of<br />
two cationic diets. Plasma hydroxyproline an index of bone resorption, also increases prior to<br />
parturition in cows fed a high anion diet. The plasma levels of 1,25-(OH)2 D also increase prior to<br />
parturition in cows fed a high anion diet, which increases calcium absorption and bone resorption<br />
(39). Feeding rations with reduced mEq of dietary ([Na + + K + ]-[CI + SO4=]) to -4 mEq/kg dietary<br />
DM to dry cows significantly affected some of the parameters of bone formation but did not<br />
enhance the rate of bone resorption (40). Feeding acid diets to pregnant cows during the last 28 d<br />
of pregnancy increased the mobilization of calcium by 13% 14 d before parturition and 28% by<br />
138
the time of parturition, whereas it had declined by 14% at 14 d before parturition in alkali- fed<br />
cows (41). The increased concentrations of 1,25-(OH)2 D were responsible for the stimulation of<br />
both intestinal calcium absorption and bone resorption. which helped to prevent severe parturient<br />
hypocalcemia (41).<br />
Ammonium chloride<br />
The addition of ammonium chloride salts to prepartum diets offers considerable promise as a<br />
practical and reliable method of control of milk fever. Experimentally, the addition of ammonium<br />
chloride and ammonium sulfate, each at lOOg/head per day, to the prepartum diets 21 d prior to<br />
parturition, decreased the incidence of milk fever from 17% in the unsupplemented group to 4% in<br />
the supplemented group. The advantages of ammonium salts are that they<br />
1.Do not require the vise of diets low in calcium<br />
2.Are relatively inexpensive<br />
3.Are convenient to use<br />
4.Are safe to feed.<br />
The cation-anion balance of the diets, calculated as (Na+K)-(CI+S), was -75 mEq/kg dietary DM<br />
with ammonium salts and +189 mEq/kg dietary DM without ammonium salts (42). Analyzing the<br />
feedstuffs for sodium, potassium, chloride and sulfur, and adjusting the value (Na+K)-(C1 + S) to<br />
produce a significantly negative total will effectively prevent parturient paresis. It has been<br />
suggested that the sum (Na + K-CI) might be useful for prediction, and that if the total were less<br />
than 10 mEq per 100 g of dry matter, parturient paresis would be prevented. Another suggestion is<br />
an 'ion balance' equation in which calcium, phosphate, sodium and potassium are considered<br />
alkalogenic and sulfur and chloride are acidogenic. Using this equation, a prepartal diet providing<br />
more than 8000 mEq of excess alkalogenic ions is at considerable risk of inducing milk fever. To<br />
prevent the occurrence of milk fever when high calcium diets are fed to dry cows, dietary<br />
cation-anion balance must be reduced below -3 mEq/100 g of diet dry matter (33). In cows fed<br />
prepartum canonic diets, two processes under the control of parathyroid hormone, the renal<br />
production of 1,25-(OH)2 D and osteo-clastic bone resorption. were temporarily refractory to<br />
parathyroid stimulation (43).<br />
Management practices<br />
The following management practices are suggested:<br />
• Avoid excessive calcium intake during the dry period<br />
• Feed an adequate amount of phosphous to meet requirements and limit calcium intake to no<br />
more than 100-125g/d. This appears to be a more practicalapproach to maintaining calcium<br />
homeostasis during the period when cows are most pronetomilk fever than establishing a given<br />
Ca:P ratio. Since intestinal absorption is a major inflow source of serum calcium during this<br />
period, keeping cows on feed is essential. This may also reduce outflow of serum calcium<br />
•Avoid overfattening by either reducing the energy concentration of the ration or restricting the<br />
intake during the prepartum period.This also appears to stimulate appetite,thuskeeping cows on<br />
feed<br />
•Avoid stresses at the time of parturition<br />
•Provide a clean well-bedded box stall with conditions conducive to cow comfort and allow the<br />
animal to exercise<br />
•Make frequent observations of cows prone to milk fever from 48 h before to 48 h after parturition<br />
for evidence of milk fever and immediate treatment will reduce the incidence of the downer cow<br />
139
syndrome associated with milk fever<br />
•At calving the cow should receive an oral dose of a calcium salt in a gel, as set out later, followed<br />
by a diet with a high calcium content (over 1% of dry matter). The critical day is the day of<br />
calving, and a sharp increase in calcium intake on this day can significantly reduce the occurrence<br />
of milk fever<br />
•If hypomagnesemia is alikely concomitant, the diet should be supplemented with 60 g<br />
magnesium oxide daily.<br />
Calcium gel dosing<br />
The oral administration of a gel containing 49% calcium chloride strategically before calving, at<br />
calving, and at intervals within 1 day after calving is effective in preventing milk fever. One tube<br />
of gel (355 g) containing 54 g of elemental calcium from a combination of calcium chloride (70%)<br />
and tricalcium phosphate (30%) given approximately 12 h before calving, immediately after<br />
calving, 12 h after calving, and 24 h after calving significantly increased serum calcium<br />
concentrations on the first and second day after calving, especially in third-parity cows or older<br />
cows (44). The incidence of milk fever, parturient hypocalcemia and displaced abomasum was<br />
also lower than in control cows. The oral administration of two tubes within 1 h after parturition is<br />
also effective (45). Rectal administration is not recommended (46). Calcium chloride is caustic<br />
and can cause oral lesions. Oropharyngeal abscesses secondary to<br />
trauma and laceration caused by the administration of the boluses may occur (47). Field trials<br />
using calcium propionate paste given orally at calving and repeated 12 h later reduced the<br />
incidence of milk fever from 50% in control cows to 29% in treated cows (48).<br />
Vitamin D and its metabolites or analogs<br />
Vitamin D3 (cholecalciferol) administered parenterally was historically, a popular prophylactic<br />
against milk fever. In an attempt to reverse the negative calcium balance of susceptible cows the<br />
administration of vitamin D and its analogs have been used to increase intestinal absorption of<br />
calcium. Vitamin D3 is hydroxylated in the liver and the resulting metabolite is<br />
25-hydroxycholecalciferol. This is metabolized in the kidney to 1,25-dihydroxycholecalciferol,<br />
which has an active hypercalcemic effect but is difficult to synthesize. One of its analogs,<br />
1-alphahydroxycholecalciferol is as active, is easy to prepare and is used pharmacologically.<br />
Oral dosing with vitamin D2 and the parenteral administration of vitamin D3 and<br />
dihydrotachysterol all have their pro¬ponents. Oral dosing with 20 million units of vitamin D2,<br />
per day for 5 d to cows immediately prior to calving can markedly reduce the expected incidence<br />
of milk fever. The exact date of calving is often difficult to determine and if the administration is<br />
discontinued for up to 4 d before calving, an unusually high incidence of the disease may follow,<br />
probably because of the depression of parathyroid activity which follows the administration. The<br />
danger of causing metastatic calcifcation also exists as this has been produced with smaller doses<br />
(10-20 million units daily for 10 d). Pregnant cows are more susceptible to calcification than<br />
non-pregnant animals. Treatment with larger doses or for longer periods than those recommended<br />
earlier should be avoided because of the danger of toxic effects. Smaller doses reduce the risk of<br />
calcification but also reduce the degree of calcium retention.<br />
A single dose of 10 million units of vitamin D3 IM given 2-8 d before parturition lias been<br />
considered as optimal. A dose of 1 million units per 45 kg BW has given consistently better results.<br />
This may explain the variable results and why results have been more favorable in Jersey cattle. If<br />
the cow fails to calve after the 8th day, another 10 million units may be administered and repeated<br />
140
every 8 d until the cow calves. Subclinical calcification may occur in vessel walls but this is<br />
unlikely if dietary calcium and phosphorus intake is adequate. Single doses of 40 million units of<br />
vitamin D can be lethal. One of the disadvantages of this method is the likelihood that cows which<br />
do not calve at the anticipated time can be more seriously affected than if they receive no<br />
treatment. The hypercalcemic effect of cholecalciferol by injection is very much longer when it is<br />
administered by IM injection (up to 25 d) than by IV injection (up to 3 d). for this reason and<br />
because occasional cases of shock occur after the IV administration, especially if more than one<br />
injection is given, the IM route is preferred. The injection of vitamin D is preferred to feeding it<br />
and a protection rate of up to 80% can be anticipated. It is estimated that 95% of Jersey cattle are<br />
protected.<br />
In spite of the very variable results obtained, the injection of vitamin D3 is still the most<br />
commonly used method of prevention, principally because of its simplicity.But there are obvious<br />
differences in response between breeds and between individual veterinarians<br />
Other compounds with vitamin D activity but which avoid the possibility of causing<br />
hypervitaminosis D and are therefore useful in the prevention of milk fever are:<br />
1.25-Hydroxycholecalciferol injected IM at 8 mg 3-10 d before calving and<br />
repeated at weekly intervals. Single doses of 4 mg are not effective in<br />
reducing the occurrence of parturient hypocalcemia or milk fever.<br />
2.1,25-Dihydroxyvitamin D3 given at 200 µg daily, orally, to calving cows<br />
reduces the development of hypocalcemia but does not completely revent milk fever (42). When<br />
1,25-(OH)2 D is given IM between 1 and 4 d of calving, it is effective in pre venting milk fever.<br />
When adminis tered less than 24 h or more than 4 d before calving, parturient paresis is not<br />
effectively prevented (49). Repeated injections at 4-7-day intervals until calving can be used, but<br />
toxicity can be a problem. A third problem with this metabolite is that the IM injection can result<br />
in milk fever 1-2 weeks<br />
after parturition because the exogenous metabolite may inhibit the<br />
endogenous production in some cows, and when the exogenous product is cleared from the body,<br />
the cow is unable to produce sufficient 1,25-(OH)2 D to maintain enhanced intestinal absorption of<br />
calcium.<br />
3.24-F-l,25-dihydroxyvitamin D3 given at 100-150 µg 5d before the<br />
expected date of parturition was effec tive (50). Cows which did not calve<br />
within 7 d were given a second dose. The incidence of milk fever in<br />
untreated controls, those receiving 100, and 150 µg, was 85%, 43% and<br />
29%, respectively. The use of SC- released product implanted 7 d before<br />
parturition and repeated at 7-day intervals until calving resulted in milk<br />
fever in 80% of controls and 9% in treated cows (49). The SC pellet<br />
maintained levels of the vitamin D metabolite for about l0d, compared<br />
with the IM injection, which results in very high concentrations in the plasma in the first 48 h after<br />
injection.<br />
4.1-Alpha hydroxyvitamin D3 at 350 µg IM is effective as a preventive to milk fever if given 72<br />
and 24 h before parturition. If calving has not occurred naturally within 72 h, a second injec tion is<br />
given (51). Parturition is induced if calving has not occurred 2 d after the second injection. The<br />
preferred site of injection is the serratus muscle of the neck, which results in a more effective<br />
response. To avoid the problems created by cows not calving at the predicted time, a combined<br />
141
egimen including induction of parturition by the administration of corticosteroid with the<br />
injection of 1- alpha-hydroxycholecalciferolis<br />
reported to be successful. Injection of cows with the same vitamin D analog<br />
plus a prostaglandin (cloprostenol) was unsuccessful in preventing milk fever. A dose of 700 µg<br />
given 6-8 d before calving is also recommended (52). Another recommendation suggests 500 µg at<br />
2-5 d prior to parturition. An evaluation of routine use of 1-alpha-hydroxyvitamin D3 indicated<br />
that cows which developed retained placenta and metritis may be at greater risk of not conceiving<br />
within 150 d from calving (53). There is some transfer of the metabolite from the maternal to fetal<br />
plasma. Injection within 24 h of the onset of milk fever is ineffective, but if it is given more than<br />
24 h and less than 1 week before the onset of the disease, the protection is excellent .<br />
Miscellaneous prophylactic measures<br />
There are a number of prophylactic measures currently in use, including:<br />
.Incomplete milking after calving, which is unreliable<br />
•Prophylactic injection of calcium solutions as soon after calving as possible, which is effective<br />
but may be impractical<br />
•Feeding of ammonium chloride to induce acidosis and enhance calcium<br />
mobilization and ionization, has been recommended and there is some sup<br />
port for its use. The ammonium chloride is fed with grain over the last few weeks of pregnancy,<br />
commencing with 25 g and increasing to 100 g/d at calving.<br />
The heritability of susceptibility to milk fever is thought to be high but there is a lack of good<br />
evidence to support this view. When breeding plans and selection of bulls are being considered,<br />
attention should be given to the use or deletion of susceptible cows as dams of bulls to be used in<br />
artificial insemination.<br />
In species other than cattle the disease is commonly caused by errors in management and<br />
prevention depends on their avoidance. High calcium intakes before parturition in ewes have also<br />
been thought to contribute to the development of hypocalcemia. However, the maintenance of<br />
appetite and the avoidance of alimentary tract stasis in late pregnancy appear to be important<br />
preventive measures which are likely to insure an adequate calcium absorption. Pregnant and<br />
lactating ewes and cows should not be subjected to unnecessary exercise or excitement. It is good<br />
practice to improve the plane of nutrition during late pregnancy in ewes to avoid pregnancy<br />
toxemia but changes, particularly to lush pasture, should be made gradually, and sheep moved<br />
from wooded pasture to open fields with little natural shelter should be provided with some<br />
protection weather.<br />
2.躺卧母牛综合征(Downer Cow Syndrome) 躺卧母牛综合征最常继发于生产瘫痪,<br />
临床上表现长时间躺卧,用钙剂治疗 2 次,还不能站立者,多认为是本病。剖检可表现四肢<br />
肌肉和神经损伤,缺血性肌坏死,心肌炎,肝脏脂肪浸润和变性等。<br />
关于本病的命名问题,仅以临床上卧倒不起为依据,易造成模糊慨念,因引起卧倒不起<br />
的原因甚多。目前倾向于认为该病是乳热症的重剧表现,例如牛分娩前后无任何明确原因致<br />
瘫痪而在 24h 内仍不能站立者,乳热症牛用钙剂治疗后 10min 内不能站立者,乳热症中经<br />
第二次用钙剂治疗 24h 内仍不能站立者,方可认为是躺卧母牛综合征。<br />
【病因】 本病病因有三类:代谢性、产科性和外伤性。<br />
(1)代谢性病因是因血钙过低 凡引起生产瘫痪的原因均可酿成本病,对生产瘫痪治<br />
疗不及时,钙剂用量不足,又未及时追加钙用量,常可发展为躺卧母牛综合征。有人报道乳<br />
142
热症牛中,有 4%~35%病牛可发展为躺卧综合征。乳热牛在地上躺卧 4~6h 以上,就可引起<br />
局部肌肉缺血性坏死,受影响的主要是后肢,表现肿胀、僵硬。<br />
除钙代谢障碍外,低磷血症、低镁血症并伴发低钙血症时,可酿成卧倒不起。至于低钾<br />
血症与本病的关系尚有争议,因本病主要涉及后肢。当低钾血症伴发低磷血症时,通常都引<br />
起躺卧综合征。有的牛后肢向后移位,发展为在地上爬行(creeper)。<br />
(2)产科性原因 包括胎儿过大,产道开张不全,助产粗鲁,损伤产道及周围神经,<br />
髋臼脱位,犊牛产出后,母牛发生麻痹,如同时伴有低钙血症,一般皆发展为躺卧母牛综合<br />
征。<br />
(3)外伤性原因 主要指大腿肌肉及关节周围组织损伤,或因压迫性损伤,引起卧倒<br />
不起。如在分娩时,母牛两后腿伸展站立,若稍不平衡而摔倒,或者母牛躺卧时,强迫它起<br />
身,不慎跌倒,或因产房地面太滑而跌倒等,均可引起后躯肌肉、神经损伤。一旦伴有低钙<br />
血症,经钙剂治疗后,病牛无法站立,而且很少有恢复的可能。<br />
至于某些重剧疾病,如肾机能衰竭,子宫内膜炎,中枢疾患等,引起病牛卧倒不起现象,<br />
不应与躺卧母牛综合征混同。<br />
【病理】 由于产前、产后血钙浓度下降,母牛处于低血钙性生产瘫痪,如不能及时治<br />
疗,或钙剂用量不足,母牛长时间躺卧于地,局部血管受压迫,体型越大,压迫越严重,血<br />
管受压时间过长,局部形成缺血性坏死或者因分娩过程中因损伤产道及周围神经、肌肉,动<br />
物不能站立,最终引起细胞肌纤维膜通透性增加,使肌内钾离子外溢,并被排泄。又因母牛<br />
产后应激,采食甚少,可造成轻度低钾血症和肌细胞内钾浓度下降,肌肉松弛。一旦后躯肌<br />
肉损伤,同时伴有血磷或血镁浓度下降,动物常常无法起立。可见本病最主要起因于生产瘫<br />
痪,而分娩过程中,或躺卧时间过长造成腿部肌肉损伤是引起本病发生的主要原因。<br />
在躺卧综合征中,几乎 100%病牛有局灶性心肌炎,造成心跳过速,心律不齐,甚至静<br />
脉注射钙剂也反应迟钝。反复使用钙剂治疗,则可加重心肌炎症。躺卧综合征中,还多有蛋<br />
白尿,可能与肌肉损伤时肌蛋白释放有关。<br />
【临床表现】 持续躺卧是本病主要表现。但病牛神志清醒,反应敏捷,食欲正常或减<br />
退,心动过速达 80~100 次/min,有的心律不齐,如急于继续补充钙剂,可引起突然死亡。<br />
有些牛几乎无站立的欲望,多数牛企图挣扎站立,但终于失败。最后,后肢伸展或呈部<br />
分屈曲,或仅能使后躯略有提高,前肢因未受影响,使牛在地面爬行,尤其在地面光滑时,<br />
表现明显。如人工辅助,尚可免强站立。但有些牛无法站立欲望,人工辅助亦属徒劳。<br />
有些严重病例常呈侧卧姿势,头向后仰,四肢抽搐,对刺激敏感,废食、停饮,这些牛<br />
称为不机敏卧倒母牛,其大脑可能已受伤害,预后多不良。有的可并发严重的乳房炎,有的<br />
因发展为肘、跗关节及坐骨、髋骨等突出部发生褥疮,大多归于死亡或被迫淘汰。<br />
如精心治疗和护理,大约有 50%患牛可于 4 天内才能站立,如一周以上还不能站立时,<br />
大多归于死亡。有些牛如心肌炎症较重,亦可能在发病后 48~72h 内死亡。<br />
本病大多呈低钙血症、低磷血症、低镁血症。但血清、钙、磷、镁浓度亦有在正常范围<br />
内的。血糖浓度正常,血清肌酸磷酸激酶(CPK)和谷草转氨酶(GOT),在躺卧 18~24h<br />
后即明显升高,并可持续数天,表明肌肉损伤严重。有些牛有轻度酮尿、血压下降和心电异<br />
常。经治疗站立后,复又卧倒不起者,顸后多不良。<br />
【诊断】 本病诊断首先在于排除其它原因引起的瘫痪,同时患牛有低血钙性生产瘫痪<br />
的病史,经 2 次钙剂治疗后 24h 不能站立者,可认为是躺卧母牛综合征。导致躺卧的原因尚<br />
有:中枢或外周神经麻痹,肌肉部分或大部分损伤,肌、膝关节脱位或腱断裂,后肢骨折,<br />
肠骨挫伤,产后肝机能不全,麻痹性乳房炎等。尽管区别这些病较麻烦,但通过临诊检查及<br />
病史调查,还是可以实现的。<br />
生化检验对本病诊断有重要帮助,如尿蛋白浓度、CPK、GOT 活性升高,均不同于生<br />
143
产瘫痪。<br />
【防治】 本病治疗首先应判断瘫痪的性质,如属于骨折、腱断裂、关节脱位、肌肉大<br />
面积损伤者,应及早淘汰。对于原发性由生产瘫痪引起的躺卧,宜采取多种电解质并用和对<br />
症治疗。可采用 20%葡萄糖酸钙(内含 4%硼酸)500~1000ml并配合VB1、VC适量,一次静<br />
注,每天 2~3 次;13%磷酸二氢钠 200~300ml,或 10%氯化钾 50ml,5%葡萄糖 500ml,缓<br />
慢静脉注射;25%硫酸镁 100~200ml皮下注射。充分保证血钙处于正常浓度下,上述方法交<br />
替使用,有些患牛可于l~2 天自行站立或人工辅助下站立。用吊带把牛吊起,有条件亦可用<br />
于减少缺血性肌坏死。最为重要的是,要使牛卧在垫草松软厚实地上,并每天使牛翻身数次,<br />
防止牛滑倒或在翻身过程中再受损伤。已站立起来的牛,应继续治疗 2~3 天,巩固疗效,防<br />
止再次卧倒。牛人工辅助站立后,还需用草把或破麻袋之类,揉擦腿部肌肉,促进局部血液<br />
循环。<br />
对于低血钙性产后瘫痪,应及早诊断和及时治疗。而且首次钙剂用量要足够。一旦病牛<br />
首次用药后尚未站立者,尚应及时重复给药,以防止发生躺卧综合征。牛一旦躺卧,应立即<br />
给予厚实松软垫料,产房内应铺以松软垫草,牛在产房内至少要等到产后 48~72h 后才能离<br />
开。<br />
伤。<br />
母牛如有难产先兆,应及时检查胎儿、胎位。助产应仔细,不要过度牵拉,防止产道损<br />
分娩前 8 天开始注射VD31000 万单位,如 8 天后仍未分娩,尚需重复注射。预产前 3~5<br />
天静脉注射 20%葡萄糖酸钙 500ml,每天 1 次连用 3~5 天,产后一旦牛不愿起立,应立即<br />
静脉注射钙制剂,不可延误而酿成躺卧综合征。<br />
DOWNER COW SYNDROME<br />
Synopsis<br />
Etiology. Ischemic necrosis of large muscles of pelvic limbs secondary to prolonged recumbency<br />
associated with milk fever .Other causes of recumbency can also result in downer cow syndrome.<br />
Epidemiology. Most common in dairy cows which have had milk fever but are unable to stand<br />
following treatment with calcium Delay of more than 4 h in treatment for recumbent milk fever<br />
cows Hypophosphatemia and/or hypokalemia may be risk factors.<br />
Signs. Unable to stand following treatment for miIk fever. Sternal recumbency. Normal mental<br />
status, vital signs and alimentary tract. Appetite and thirst normal. Most will stand in few days if<br />
provided good c1inical care and secondary muscle necrosis minimized. Some cases have bizarre<br />
behavior of lateral recumbency, abnormal position of legs, groaning, anorexia and die in several<br />
days.<br />
Clinical pathology. Increased serum levels of creatine phosphokinase (CPK) and<br />
aminotransferase (AST); serum phosphorus and potassium levels may be subnormal.<br />
Lesions. Ischemic necrosis, edema and hemorrhage of large medial thigh muscles.<br />
Diagnostic confirmation. Increased serum levels of CPK, AST, proteinuria; necropsy lesions in<br />
cow unable to rise with no other lesions<br />
Differential diagnosis list:<br />
•See differential diagnosis of milk fever(p.1421)and Table 28.1<br />
•Common causes of recumbency in dairy cows around time of parturition<br />
include:<br />
•Milk fever (p.1420)<br />
•Hypomagnesemia (pp. 1442, 1510)<br />
•Peracute coliform mastitis (p. 639)<br />
144
•Maternal obstetrical paralysis (p. 1427)<br />
•Fat cow syndrome (p. 1462)<br />
•Physical injuries of pelvic lambs (dislocation of hip joints, rupture of gastrocnemius,<br />
femoral fracture)<br />
•Acute diffuse peritonitis(ruptured uterus, other causes).<br />
Treatment. Provide feed and water and excellent bedding or ground surface like sand or dirt pack.<br />
Roll animal from side to side every few hours. Fluid and electrolyte therapy as necessary<br />
Control. All recently calved dairy cows which are at high risk for milk fever must be observed<br />
closely 12-24 h before and after calving for evidence of milk fever and while still standing; if<br />
recumbent do not delay treatment for more than 1 hour. Can treat all high-risk cows with calcium<br />
chloride gel orally to prevent clinical milk fever.<br />
ETIOLOGY<br />
Most commonly the downer cow is a.complication of milk fever (I). Ischemic necrosis of the large<br />
muscles of the pelvic limbs and injuries to the tissues around the hip joint and of the obturator<br />
muscles are common in cows which do not fully recover and stand but remain recumbent<br />
following treatment for milk fever. The injuries may also be the result of cows 'spread-eagling'<br />
their hindlimbs it they are unsteady during parturition or forced to stand or walk on a slippery<br />
floor immediately before or following parturition. Dystocia due to an oversized calf may result in<br />
extensive edema of the pelvic tissues and vulva, and failure of the cow to stand following<br />
parturition. If these cows develop milk fever, it is unlikely they will be able stand following<br />
treatment with calcium.<br />
EPIDEMIOLOGY<br />
Occurrence<br />
The disease occurs most commonly within the first 2 or 3 d after calving in high-producing dairy<br />
cows immediately following milk fever. Cattle may also become persistently recumbent tor many<br />
reasons other than complications of milk lever such as peracute coliform mastitis and<br />
carbohydrate engorgement.<br />
Incidence<br />
The incidence as a complication of milk lever is high because many affected animals are high<br />
producers and of high economic value. Accurate data on the incidence are not available because of<br />
variations in the nomenclature used and the accuracy of diagnoses. For example, some<br />
observations report that all cases are caused by nerve injury (2). Cases included in this<br />
classification are classified by others as maternal obstetric paralysis, obturator paralysis or<br />
hypophosphaterrua. Because it is a syndrome lacking in clinical definition and includes all those<br />
'other cases' which cannot be otherwise classified, the incidence varies depending on the clinical<br />
acuity of the individual veterinarian, and on various environmental factors in different areas.<br />
However, the incidence seems to be increasing, particularly in intensive dairy farming areas,<br />
although this impression could arise from the increased necessity to effect a cure in valuable<br />
animals.<br />
A mail survey of 723 dairy herds in Minnesota found an incidence of 21.4/1000 cow years at<br />
risk (2). The overall outcome was that 33% recovered, 23% were slaughtered and 44% died. The<br />
owners perceived that downer cows were high producers (48%) or average producers (46%), with<br />
only 6% being low producers. Approximately 58% occurred within 1 d of parturition and 37%<br />
occurred during the first 100 d of lactation. The incidence was highest (39%) during the three<br />
145
coldest months: December, January and February. In New Zealand, the prevalence ranges from 3<br />
5% of all dairy cows at calving time (3).<br />
In a clinical and laboratory survey of 433 periparturient recumbent cows in New Zealand, 39%<br />
recovered, 30% died and 52% were destroyed (3). The case-fatality rate was 11% higher in<br />
precalving recumbent cows than postcalving cows.<br />
Risk factors<br />
Animal risk factors<br />
COMPLICATION OF MILK FEVER Prolonged recumbency after a long delay in the<br />
treatment of milk fever is a major risk factor. Prolonged recumbency before treatment for milk<br />
fever (more than 4-6 h) results in ischemic necrosis due to obstruction of the blood supply,<br />
especially in a heavy cow if she lies on one leg tor a long period (4). Cows which develop milk<br />
fever while in a standing tie-stall may slide backwards into the gutter behind the stall, resulting in<br />
extreme pressure to their pelvic limbs and leading to ischemic necrosis.<br />
A case-control study to identity risk factors tor the development of downer cow syndrome<br />
within 30 d postpartumin 12 dairy herds over 2705 lactations found that clinical hypocalcemia and<br />
stillbirth increased the risk of the disease five-fold (5). Cows with retained placenta and dystocia<br />
were also more likely to develop downer cow syndrome than cows without either problem.<br />
A marked increase in the CPK levels in cows with milk fever and failure to stand after repeated<br />
treatments is supporting evidence for ischemic necrosis associated with prolonged recumbency as<br />
a major cause of downer cow syndrome (1). The CPK levels increase markedly between the first<br />
and second treatments, which indicates that muscle damage has occurred and the levels are highest<br />
in cows which do not recover.<br />
Experimentally, enforced recumbency of cattle for 6, 9 or 12 h with one<br />
hindlimbpositionedunder thebody results in downer cow syndrome. Affected cows are unable to<br />
stand and the affected limb is swollen and held rigid similar to the injured limbs of human patients<br />
with compartmental/crush syndrome.<br />
TRAUMATIC INJURIES TO PELVIS AND PELVIC LIMBS Traumatic injuries to the<br />
nerves of the pelvis and hindlimbs are present in 25% or more of downer cows (1). The sciatic and<br />
obturator nerves are vulnerable to injury by pressure from the calf moving through the pelvic<br />
canal during parturition. Pressure injuries on the superficial nerves (radial and peroneal) of the<br />
extremities also occur in recumbent cows.<br />
SERUM ELECTROLYTE IMBALANCES Serum electrolyte imbalances or deficits may be<br />
associated with prolonged recumbency following treatment for parturient paresis.<br />
HYPOCALCEMIA A persistent hypocalcemia following treatment for milk fever may exist in a<br />
downer cow but is unlikely to be the principal cause because treatment with calcium salts does not<br />
resolve the signs, even temporarily. However, the use of an insufficient amount of calcium for the<br />
initial treatment of milk fever in large, heavy cows may result in an incomplete response and<br />
failure of the cow to stand. It these cows are not retreated soon enough with an adequate amount<br />
ot calcium, ischemic necrosis of the limb muscles occurs and leads to prolonged recumbency. In<br />
many cases, even after the cow is given a sufficient amount of calcium, prolonged recumbency<br />
occurs due to the ischemic necrosis.<br />
HYPOPHOSPHATEMIA The serum levels of inorganic phosphorus decline to below normal<br />
along with a hypocalcemia in cases of milk fever. Following treatment ot milk fever with calcium<br />
borogluconate, the levels of serum calcium and phosphorus return to normal if the animal<br />
146
esponds favorably and stands normally. Following treatment for milk fever, some cows do not or<br />
are unable to stand and their serum phosphorous levels are subnormal. This persistent<br />
hypophosphatemia has been regarded as a cause of downer cow syndrome associated with milk<br />
fever. Many veterinarians claim that these cows respond to treatment with phosphorus. However,<br />
persistent recumbency is associated with subnormal levels of serum phosphorus which increase to<br />
normal if the cow stands regardless of treatment with or without phosphorus. Mature dairy cows<br />
may become recumbent in early lactation and subnormal levels of scrum phosphorus may be<br />
present (6). Other cows in the herd may be lame due to demineralization of bones associated with<br />
a dietary deficiency of phosphorus.<br />
HYPOMAGNESEMIA A long-term low-level hypoinagnesemia has been associated with the<br />
downer cow, especially when it accompanies hypocalcemia. But it is usually manifested by a<br />
tetanic hyperesthetic state which is not part of downer cow syndrome. Hypokalemia is, with<br />
hypophosphatemia, the most commonly quote cause, especially in the so-called 'creeper' cows,<br />
which are bright and alert and crawl about, but are unable to rise (7).<br />
HYPOKALEMIA Ischemia due to prolonged recumbency associated with milk fever, may<br />
increase the cell membrane permeability of muscle fibers and allow the loss of potassium from the<br />
cell; this in turn causes the myotonia, which appears to be the basis of downer cow syndrome.<br />
This view is supported by the low serum and muscle potassium levels in downer cows. Claims are<br />
made that potassium salts are successful in treatment but these have been difficult to evaluate (3).<br />
Hypokalemia occurs in dairy cows which have been treated with isopflupredone acetate for<br />
ketosis (8). Affected animals are weak, recumbent and severely hypokalemic with serum<br />
potassium levels ranging from 1.4-2.3 mEq/L.<br />
Environmental and management risk factors<br />
A slippery ground surface is a major risk factor. Cattle which must walk across slippery floors,<br />
especially at the time of calving, may slip and fall and injure the large muscles of the pelvic limbs,<br />
resulting in an inability to stand. Prolonged recumbency results in ischemic necrosis and downer<br />
cow syndrome.<br />
Summary<br />
Downer cow syndrome is a complication of the recumbency associated with milk fever. A delay<br />
of 4 h or more in the treatment of cows with milk fever may result in ischemic necrosis of the<br />
muscles of the pelvic limbs.Traumatic injury to leg muscles at the time of parturition or when the<br />
cow is unsteady and falls during the first stage of milk fever will also result in the inability of the<br />
cow to stand following treatment of milk fever.<br />
PATHOGENESIS<br />
Several different primary factors or diseases can result in recumbency.<br />
Prolonged recumbency before treatment<br />
A long delay in the treatment of milk fever can result in pressure damage and the subsequent<br />
inability to stand after treatment for the primary disease. Prolonged recumbency results m pressure<br />
damage, which occurs secondarily and is a factor common to all cases (2).<br />
Regardless of the cause, the prolonged recumbency results in varying degrees of ischemic<br />
necrosis of major muscles of the hindlimbs, particularly the semitendinous muscle and muscles<br />
caudal to the stifle. Prolonged compression of the muscle leads to tissue anoxia, cell damage and<br />
inflammation which causes swelling: the swelling causes a further increase in pressure which<br />
limits tissue perfusion and leads to a detrimental cascade of events. The thick fascial boundaries of<br />
147
the semitendinous muscle prevents expansion which results in pressure-induced compartmental<br />
syndrome. Sciatic nerve damage due to pressure also occurs and may contribute to downer cow<br />
syndrome. Experimental external compression of the pelvic limb of the goat, to simulate limb<br />
compression in recumbent cows, resulted in a marked reduction in nerve condition velocity of the<br />
peroneal nerve which was associated with clinically evident limb dysfunction. Damage to the<br />
peroneal nerve will result m hyperflexion of the fetlock if and when the cow is able to stand.<br />
Traumatic injury to limb muscles and nerves immediately prior to parturition or at the time of<br />
parturition can also result in prolonged recumbency and subsequent pressure damage (1).<br />
Experimental sternal recumbency<br />
Experimentally induced sternal recumbency with one hindlimb positioned under the body to<br />
simulate prolonged recumbency will result in a swollen rigid limb within 6-9 h (9). Following<br />
injury to the muscle cells, the serum levels of CPK are markedly elevated at about 12 h after the<br />
onset of recumbency. Proteinuria and in some severe cases myoglobinuna occur between 12 and<br />
36 h after the onset of prolonged recumbency, due to the release of myoglobin from damaged<br />
muscles. In cows which make efforts to stand but cannot do so, continued struggling results in<br />
rupture of muscle fibers and hemorrhage which increases the seventy.<br />
Acute focal myocarditis may occur in about 10% of cases resulting in tachycardia, arrhythmia<br />
and the unfavorable response to IV calcium salts observed in some cases. The cause of the<br />
myocardial lesion is unknown but repeated administration of calcium salts has been suggested (1).<br />
Downer cows with a poor prognosis also have greatly enhanced adrenocortical function (7).<br />
The prolonged recumbency can result in additional complications such as acute mastitis,<br />
decubitus ulcers and traumatic injuries of the limbs.<br />
The pathogenesis of the non-alert downer cow is not understood (10). Most have had an initial<br />
episode of milk fever but do not respond satisfactorily. Within 1 or 2 d, affected cows have a<br />
preference for lateral recumbency anjd exhibit expiratory moaning and groaning. They represent<br />
about 2% of all cases of milk fever.<br />
Experimental prolonged hypocalcemia<br />
Experimental prolonged hypocalcemia may provide some clues about the pathogenesis of downer<br />
cow syndrome as a complication of milk fever. The prolonged infusion of ethylenediamine<br />
tetraacetic acid (EDTA) in sheep over 18 h at a rate to induce hypocalcemia and maintain<br />
recumbency results in prolonged periods of recumbency ranging from 36-64 h before the animals<br />
are able to stand (11). There are also decreases in plasma sodium, plasma potassium and<br />
erythrocyte potassium and prolonged increases in packed cell volumes, which suggests that fluid<br />
replacement therapy may be indicated in cattle with prolonged recumbency associated with<br />
hypocalcemia (12). A 4-hour IV infusion of EDTA in high erythrocyte potassium and low<br />
erythrocyte potassium dairy cows causes decreases in plasma inorganic phosphorus and plasma<br />
potassium which are still below normal 24 h later (13). The AST, CPK, and PCVs and WBC<br />
counts are also elevated 24 h later. Plasma magnesium and erythrocyte sodium and potassium<br />
were decreased but this was delayed. The increase in PCV was most pronounced in the low<br />
erythrocyte potassium cows, which may provide some clues about the pathogenesis of downer<br />
cow syndrome. Some cows may have a more precipitate increase in PCVs due to loss of plasma<br />
volume and an inability to mobilize calcium. As a basis for studying the effects of hypertonic<br />
solutions to correct these abnormalities in downer animals, a 200 mL solution of 10 g of sodium<br />
chloride and 0.5 g of potassium chloride can be given IV to sheep safely over a period of 4-8 min<br />
148
(14).<br />
CLINICAL FINDINGS<br />
Downer cow syndrome may occur independently, or follow apparent recovery after treatment for<br />
milk fever, except for the prolonged recumbency. In the typical case, affected cows either make no<br />
effort or are unable to stand following treatment for parturient paresis. About 30% of cows treated<br />
for milk fever will not stand for up to 24 h following treatment. Those which are unable to stand<br />
after 24 h and after two treatments are classified as downers. They are usually bright and alert and,<br />
although the appetite is reduced, the cow eats and drinks moderately well. The temperature is<br />
normal and the heart rate may be normal or elevated to 80-100 bpm. Tachycardia and arrhythmia<br />
occur in some cows, especially immediately following the administration of calcium IV and<br />
sudden death has occurred. Respirations are usually unaffected. Defecation and urination are<br />
normal but proteinuria is common and if marked may indicate extensive muscle damage.<br />
Some affected cows may make no effort to stand. Others will make frequent attempts to stand<br />
but are unable to fully extend their pelvic limbs and lift their hindquarters more than 20-30 cm<br />
from the ground. These frequent attempts to stand result in 'crawling' or 'creeping' along the<br />
ground with both hindlcgs in a partially flexed position and displaced posteriorly the froglcg<br />
attitude. On a non-slippery surface (bare ground, sand pack, or deep bedding) some cows are able<br />
to stand with some assistance by lifting on the tail head or with the use of hip slings. Those cows<br />
which do not make an effort to stand usually cannot stand even with assistance and if supported<br />
with hip slings will usually make no effort to bearweight with either the hindlimbs or the<br />
forelimbs. Their limbs appear stiff, painful or numb and they are unable or reluctant to bear weight.<br />
Damage to the peroneal nerve is usually present when there is hyperflexion of the fetlock joints,<br />
which is evident if and when the cow is able to stand and bear weight on the hindlimbs.<br />
In some cases, the hindlimbs are extended on each side of the cow and reach up to the elbows<br />
on each side. In this position, the cow is bearing considerable weight on the medial thigh<br />
musculature and causing ischeniic necrosis. This abnormal position of the legs may also be due to<br />
dislocation of one or both hip joints or associated with traumatic injuries surrounding the hip<br />
joints with or without rupture of the ligamentum teres. Regardless of the cause, the cow prefers<br />
this leg position and invariably will shift the legs back to the abnormal position if they arc placed<br />
in their normal position.<br />
In some cows the signs may be more marked and bizarre, including a tendency to lie in lateral<br />
recumbency with the head drawn back. When placed and propped up in sternal recumbency, these<br />
cows appear almost normal but. when they are left alone, within a short period of time they revert<br />
to the position of lateral recumbency. Still more severe cases are . hyperesthestic .mil the limbs<br />
may be slightly stiff but only when the cow is lying in Literal recumbency. I hese severe cases do<br />
not usually eat or drink, have been described as 'non-alert downers', and are thought to have brain<br />
damage which has not been documented (10).<br />
Complications in the downer cow syndrome are common and often result in . death or the need<br />
for euthanasia. Collform mastitis, decubitus ulceration, especially over the prominences of the<br />
hock and elbow joint, and traumatic injuries around the tuber coxae caused by the hip slings arc<br />
common. When these complications occur in the early stages of the disease, they commonly<br />
interfere with any progress being made and become the focus of clinical attention.<br />
The course of the disease is variable and dependent on the nature and extent of the lesions and<br />
the quality of the care and comfort winch is provided for the cow during the first few clays. About<br />
149
50% j of downer cows will stand within 4 d or less if cared for properly. The prognosis is poor for<br />
those which are still recumbent after 7 d, althoughsome affected cows have been down for 10-14 d<br />
and subsequently stood up and recovered. Death may occur in 48-72 h following the onset and is<br />
usually associated with myocarditis.<br />
CLINICAL PATHOLOGY<br />
The calcium, phosphorus, magnesium and glucose levels of the blood are within the normal range<br />
and the results of hematological examinations are usually consistent with those found in normal<br />
cows which have recently calved. The CPK and AST levels are usually markedly elevated by<br />
18-24 h after the onset of recumbency and continue to elevate within the next few days. Continued<br />
elevation of CPK levels indicates continued muscle damage. In experimentally induced<br />
recumbency m cows, the CPK levels remained within normal limits for the first 6 h. However, by<br />
12 h there was a marked increase to mean values of 12 000 m/L rising to 40 000 iu/L by 24 h.<br />
There may be moderate ketonuria. A marked proteinuria is usually evident by 18-24 h after the<br />
onset of recumbency. The proteinuria may persist for several days or be absent within a few days.<br />
In severe cases, the urine may be brown and turbid because of severe myoglobinuria. Low arterial<br />
blood pressures and abnormal electrocardiograms (ECGS) have been observed in some animals.<br />
Elevations of serum urea, muscle enzymes, and laboratory evidence of inflammation are<br />
considered the best prognostic indicators of an unfavorable recovery (3). Cows with a serum urea<br />
level above 25 mmol/L and serum creatinine levels above 130 mmol/L had a poor prognosis. The<br />
recovery rate was lower in cows with a total protein: fibrinogen ratio less than 10:1. and evidence<br />
of neutropenia and/or left shift (3). The CPK levels need to be interpreted in relation to the days of<br />
recumbency when the sample was taken. Critical levels may be highest initially (up to 50 times<br />
the upper normal reference range) and reduce to 10 times normal range at 7 d of recumbency.<br />
NECROPSY FINDINGS<br />
Hemorrhages and edema of the skin of traumatic origin are common. The major pathological<br />
changes consist of hemorrhages and degeneration of the medial thigh muscles. Hemorrhages<br />
around the hip joint with or without rupture of the ligamentum teres are also common. Local areas<br />
of ischemic necrosis of the musculature (gracilis, pectineus and adductor muscles) occur at the<br />
anterior edge of the pelvic symphysis (1). Eosinophilic infiltration of ruptured necrotic thigh<br />
muscles of downer cows has been described (15). Hemorrhages and edema of the nerves of the<br />
limbs (obturator, ischiatic, peroneal, radial) are also common and usually associated with severe<br />
muscle damage. The heart is dilated and flabby and histologically there is focal mycoarditis. There<br />
is fatty degeneration of the liver and the adrenal glands are enlarged. Histologically there are also<br />
degenerative changes in the glomerular and tubular epithelium of the kidneys.<br />
DIFFERENTIAL DIAGNOSIS<br />
The diagnosis of downer cow syndrome is made after all other known causes of recumbency have<br />
been eliminated in a cow which had milk fever and failed to stand within 24 h following two<br />
successive courses of treatment. The other common causes of prolonged recumbency are<br />
described under the differential diagnosis of milk fever (Table 28.1). It is difficult and time<br />
consuming to examine a downer cow thoroughly to eliminate all other causes of recumbency.<br />
Only by repeated careful clinical examination will the clinician avoid the embarrassment of failing<br />
to detect the presence of coliform mastitis, a fractured leg or a dislocated hip.<br />
TREATMENT<br />
Fluid and electrolyte therapy<br />
150
Many treatments including the injections of magnesium salts, phosphates, corticostcroids,<br />
stimulant tonics and vitamin E and selenium have been used without consistent success. The use<br />
of parenteral solutions containing potassium, calcium, magnesium and phosphorus has been<br />
recommended (7) but there is no scientific evidence that these electrolytes,in addition to what was<br />
probably given to the cow already, are indicated or are of any beneficial value. Large quantities of<br />
fluid and multiple electrolyte therapy by the oral or parenteral route is indicated for cows which<br />
may not be drinking normal quantities of water. Multiple electrolytes can be added to the drinking<br />
water if the cow is drinking normally.<br />
Bedding and clinical care<br />
The most important aspect of treatment is to provide the most comfortable bedding possible and to<br />
roll the cow from side to side several times daily to minimize the extent of ischemic necrosis and<br />
para-analgesia which results from prolonged recumbency. With conscientious care and the<br />
provision of good bedding, palatable feed and liberal quantities of water, most cows will attempt<br />
to stand with some difficulty and assistance within 24 h, and will stand unassisted and normally a<br />
day or two later. A sand or dirt pack is the ideal ground surface which facilitates standing when<br />
downer cows attempt to stand (9). If affected cows are left on a slippery ground surface, they will<br />
not make an effort to stand and will become progressively worse. Cows should be milked<br />
normally and the udder kept clean by washing with germicide soap before milking, and<br />
postmilking teat dips applied.<br />
Assisted lifting to aid standing<br />
The clinician and fanner are commonly faced with the questions of whether or not to lift a<br />
recumbent cow which has not attempted to stand within a tew hours after treatment for milk fever.<br />
The guiding principle should be the behavior of the cow. If the cow makes an effort to stand on<br />
her own or by some coaxing such as a gentle lenudge m the ribs, she should be assisted to stand by<br />
insuring a good non-slip ground surface, deep bedding are lifting up on the tail head when she<br />
attempts to stand. The cow should be rolled from side to side every few hours and encouraged to<br />
stand a few times daily. With good clinical care, most cows with the uncomplicated form of<br />
downer cow syndrome secondary to milk fever will stand in 12-24 h.<br />
Lifting devices<br />
Several different kinds of cow lifting devices have been used to assist downer cows to stand. Hip<br />
lifters, which fit and tighten over the tuber coxae, and body slings like harnesses are designed to<br />
fit around the abdomen and thorax of the animal. These devices can assist a downer cow to stand<br />
it she makes some effort on her own and it appears that 'if she were given some help she could<br />
stand'. For those cows which make some effort to stand, the hip lifters or slings can be applied and<br />
the animal lifted to the standing position. If the animal bears weight on all four legs she should be<br />
allowed to stand with the aidofthedevices for 20-30 min and then lowered down. This procedure<br />
should be repeated several times daily. In most cases, such downer cows will stand on their own<br />
within a few days. While the cow is in the standing position she can be milked and other clinical<br />
examinations can be carried out.<br />
The hip lifters can result in traumatic injuries to the tissues surrounding the tuber coxae if not<br />
used judiciously Animals which make no effort to stand and bear weight on their own must not be<br />
left suspended in the lifter for more than a few minutes but lowered immediately. If the hip lifters<br />
are not applied carefully, the animal may slip out of the device while she is being lifted, which<br />
commonly results in tissue injury around the tuber coxae; fractures of the coxae have even<br />
151
occurred. These injuries are often unnoticed clinically, contribute to persistent recumbency and the<br />
true extent of the lesions are evident at necropsy. Lifting devices must be used carefully by<br />
experienced personnel.<br />
Body slings which fit around the abdomen and thorax of the animal appear to be the ideal<br />
'animal lifter' because they distribute the weight over several sites in contrast to the hip lifters,<br />
which concentrate the weight over the tuber coxae. However, the body slings are cumbersome to<br />
apply to a recumbent annual, and require more time and experienced personnel to insure proper<br />
application. When the slings are applied properly, they do appear to allow the lifted animal to<br />
stand comfortably for 30 min or more and promote recovery.<br />
Lifting cows which make no effort to stand on their own is usually unsuccessful. When<br />
lifted they usually do not bear any significant weight.<br />
A water flotation tank has been designed for the management of downer cows (16). A<br />
prototype consists of a metal tub with inside dimensions of 92 in long, 43 in wide, and 51 in deep.<br />
The system is affordable, portable, durable, effective and simple to use. The downer cow is pulled<br />
into the tub on a mat and the ends of the tub closed to make a water-tight container with an open<br />
top like a bath tub. With the cow's head held up by a halter, the tub is filled with water at<br />
100-102℉ as quickly as possible. Cows in lateral recumbency will roll into sternal recumbency<br />
when 12-24 inches of water are in the container and will usually attempt to stand when the tub is<br />
one-half to two-thirds full. Cows are allowed to stand in the water for 6-8 h. If the water<br />
temperature falls below 95 0 F more hot water is added. When the decision is made to remove the<br />
cow, the water is drained and the end of the tub opened, which allows the cow to walk out<br />
preferably onto a ground or grass surface. A success rate of 46% has been reported (16). However,<br />
the success rate could be higher if the selection of cases for flotation arc more rigorous. Cows with<br />
ruptured tendons, fractures, luxated coxofemoral joints, septic polyarthritis and other physical<br />
injuries of the musculoskeletal system are not good candidates lor flotation. The most suitable<br />
case for flotation would appear to be the downer cow as a sequel to milk fever.<br />
Animal welfare issue<br />
The downer cow syndrome is an animal welfare issue and the veterinarian should be proactive<br />
about the problem. Society is concerned about how downer animals are cared for and handled and<br />
the methods used for their disposition (17). It recovery does not occur within a tew days the<br />
prognosis is uncertain and the owner and veterinarian must decide whether to continue providing<br />
clinical care to the downer cow or if the animal should be slaughtered for salvage or euthanized.<br />
Commercial slaughter ot recumbent cattle for human consumption is esthetically undesirable and<br />
emotionally charged. However, recumbent cattle represent an important source of income for<br />
cattle producers and others in the meat industry. In the United States in 1990-1992, 117301<br />
recumbent cattle were slaughtered at federally inspected abattoirs. Many consumers believe that<br />
meat derived from any animal which cannot stand is unwholesome. However, most recumbent<br />
cattle slaughtered for edible beef are not contaminated by bacteria but the viscera, especially the<br />
liver, may present a food safety problem because of multifocal foci of hepatitis (18).<br />
Government animal health regulatory agencies, livestock associations and veterinary<br />
associations are now involved m drafting regulations on the care and handling ot non-ambulatory<br />
recumbent animals like the downer cow (19). The principles of the humane movement of<br />
recumbent animals includes:<br />
152
1.Not dragging the animal but placing it on some type of sled<br />
2.Using ramps rather than dumping animals<br />
3.Not mixing with other animals<br />
4.Moving animals directly to slaughter and stunning them prior to unloading at the abattoir.<br />
CONTROL<br />
The early detection and treatment of milk fever will reduce the incidence and severity of downer<br />
cow syndrome. Under ideal conditions, cows should be treated during the first stage ot milk fever<br />
before they become recumbent. Once recumbent cows should be treated as soon as possible and<br />
not delayed for more than 1 hour. Cows with milk fever should be well bedded with liberal<br />
quantities of straw or moved to a soft-ground surface. Recumbent cows should be coaxed and<br />
assisted to stand if possible after treatment for milk fever. If they are unable to stand, they should<br />
be rolled from one side to the other every few hours if possible. It is usually difficult to get owners<br />
to comply with this recommendation but frequent rolling from side to side is necessary to<br />
minimize the isehemic necrosis. Dairy cows should be placed in a comfortable well-bedded box<br />
stall prior to calving and should be left in that box stall until at least 48 h after partition in the<br />
event that milk fever develops.<br />
REVIEW LITERATURE<br />
Cox, V. S. (1988) Nonsystemic causes of the downer cow syndrome. I W Clin. North Am.: Food<br />
Anim. Praa.. 4. 413-433.<br />
REFERENCES<br />
(1)Cox, V. S. (1988) Vet Clin. North An,.:Food Anim. Praa., 4, 413.<br />
(2)Cox. V. S. ct al. (1986) Ptev. Vet. Mai., 4.249.<br />
(3)Clark, R. G. et al. (1991) NZ Vet.J., 35.126.<br />
(4)Fenwick, D. C. (1969) Aust. Vet.]., 45, 184.<br />
(5)Corri-.i, M T. et al. (1993) J. Dairy Sci.,76, 3460.<br />
(6)Gerloff, IS. J. & Swenson, E. P. (1996) j.Am. Vet. Med. Assoc., 208, 716.<br />
(7)Nakao, T. & Grunnert, H. (1990)/. Vet.Mai.. Series A, 37, 610.<br />
(8)Sielman, E. S. et al. (1997)/ Am. Vet.Med. Assoc, 210, 240.<br />
(9)Cox, V. S. & Marion, R S. (1992) Vet.Rcc, 130, 74.<br />
(10)Fenwick, D. C. et al. (I486) Vet. Rec,118, 124.<br />
(11)Fenwick, D. C. & Daniel, R. C W.(1992) Br. Vet.J., 148, 425.<br />
(12)Fenwick, D. C. & Daniel, R. C. W.(1992) Br. Vet.J., 148, 301.<br />
(13)Fenwick, D. C. & Daniel, R. C. W.(1992) Br. Vet.J., 148,283.<br />
(14)Fenwick, D. C. (1992) Br Vet.J., 148,413.<br />
(15)Bindseil, E. (1987) Vet. Rec, 120, 183.<br />
(16)Smith, B. I', ft al. (1997) Proc. Am. Assoc.Bov. Praa., 30, 43.<br />
(17)Stark. D. A. (1995) Bov. Pract., 29, 125.<br />
(18)Edwards, J. F. et al. (1995) J. Am. Vet.Med. Assoc, 207, 1174.<br />
(19)Livestock Conservation Institute (1992)Proper handling techniques for non- ambulatory<br />
animals. Madison, WI.<br />
3.母牛血红蛋白尿(Hoemoglobinuria of Cows) 母牛血红蛋白尿是指母牛尿液中含有<br />
数量不等的血红蛋白,临床上以尿液呈红色、暗红色甚至咖啡色,有严重的血管内溶血。血<br />
液无机磷浓度下降为特点。<br />
153
引起牛尿液中血红蛋白增加的原因很多,许多溶血性传染病,如牛的钩端螺旋体病、血<br />
液原虫病及中毒病等,但这些病有各自的特点,也无性别间差异,不属本病描述范围。这里<br />
所介绍的是一种非传染性疾病,在临床上以母牛发病较多,而公牛、阉牛、肉牛很少发生,<br />
分娩后的乳牛和母水牛(不论其怀孕与否,产犊后多长时间)发病较多,公水牛、阉公水牛<br />
有时也有发生,但与母牛相比发病率较低。役用黄牛发病率明显比水牛低。不论是分娩后奶<br />
牛或是水牛的血红蛋白尿,其共同特点是:①血清无机磷浓度下降;②血红蛋白尿;③共同<br />
的治疗方法——大剂量补磷,效果良好。<br />
母牛产后血红蛋白尿首次报道于苏格兰,现今在欧、美、亚、澳及非洲各地都有报道。<br />
但所用名称可能各不相同。如血红蛋白尿、营养性血红蛋白尿、红尿病、地方性血红蛋白尿、<br />
水牛分娩性血红蛋白尿等。不论是中国水牛,还是印度或埃及水牛都有许多类似的报道。在<br />
这些报道中提及的病例,均以母牛为主,故该病似可称为母牛血红蛋白尿。<br />
【病因】 饲料中磷缺乏,而又未能恰当地补充磷是引起本病的主要原因。已有实验证<br />
明,3 头母牛,用低磷饲料饲喂 18 个月,1 头妊娠母牛发生血红蛋白尿,用磷制剂治疗或补<br />
充骨粉后又迅速康复。有报道表明,干乳期母牛、1 岁龄小犊牛尽管血清无机磷浓度正常,<br />
偶尔也有血红蛋白尿。正在泌乳的牛,尽管血清无机磷仅略偏低,妊娠母牛产犊前 2 个月,<br />
血磷浓度常有偏低的现象。用过多能量物质喂给糖尿病的狗,也可引起血磷下降,并产生血<br />
红蛋白尿和血管内溶血。因此,血磷下降是本病的预置因子。<br />
干旱年份收获的牧草和稻草,为牛采食后,于当年冬季或次年春天容易发生血红蛋白尿<br />
症。认为与牧草中磷含量下降有关,严重缺磷的地区,本病发生较多。有些牧场更易发生本<br />
病。<br />
但是血磷下降,低磷血症的牛并非都发生血红蛋白尿。有些牛可引起严重的骨软症,但<br />
无血红蛋白尿现象,认为可能还有某些诱因存在。有报道认为,牛大量采食甜菜叶、苜蓿干<br />
草和十字花科植物如油菜、萝卜和大量甜菜渣、甘蓝等容易引起血红蛋白尿。一方面因甜菜<br />
糖渣含磷仅 0.1%,大头菜中含磷 0.2%,另一方面甜菜、苜蓿中皂角苷含量较多,十字花科<br />
植物中的二甲基二硫化物,即 S-甲基半胱氨酸二亚砜(SMCO),能使血红蛋白变性,生成<br />
Heinz 小体,每 100kg 体重牛吃入 15g SMCO,可引起致死性贫血,吃入 10g 引起亚临床贫<br />
血。江苏水牛血红蛋白尿可因吃入大量水浮莲、水花生或某些干稻草而引起,其真正的诱因<br />
尚难肯定。<br />
铜中毒时,可因大量铜离子作用,使血红蛋白变性,形成 Heinz 小体和红细胞膜变脆(Soli<br />
N.E.等,1977),但母牛一般很少有铜中毒现象。铜缺乏时,据新西兰报道,当用石灰改造<br />
土壤和大量施铜肥的草地上,在以三叶草为主的草场放牧的牛,患血红蛋白尿症增多,因而<br />
认为血红蛋白尿与缺铜有关,但此说尚缺乏实验依据。<br />
糖尿病的狗,当大量使用胰岛素和补液,纠正酮酸血症(Ketoacidosis)时,可使磷从<br />
尿液中过多排泄,引起低磷血症,并产生血红蛋白尿和红细胞溶解。<br />
母牛血红蛋白尿的发病率一般不高,同样在缺磷草地放牧,同用缺磷饲料饲喂,发病仅<br />
是个别现象,同一居民组内所养的黄牛与水牛,其中水牛发病明显多于黄牛,所有这些现象<br />
与动物的基因型是否有关,至今尚未见报道。<br />
【发病机理】 本病发生基于两点,一是磷摄入减少,因干旱或因土壤中缺磷又未补充<br />
磷;同时因产后泌乳牛奶中磷含量达 1.05g/kg,每产 1kg 奶,净需磷量为 1.9g,一天产 20kg<br />
奶的牛,饲料中至少应供给 48g 磷,如饲料中磷供给不足,很易造成缺乏。二是红细胞代谢<br />
紊乱,引起红细胞溶解的基础是:①红细胞膜上蛋白质的巯基(SH)键被转化为二硫键,可<br />
能是与血红蛋白上二硫键混合在一起,亦可能是与红细胞内部的变性血红蛋白—Heinz 小体<br />
结合形成二硫键,使膜结构损伤。②红细胞膜上的酯质被过氧化作用,引起膜结构受损;③<br />
红细胞糖酵解作用受影响,通过糖酵解而合成的三磷酸腺苷(ATP)不足,红细胞表面 ATP<br />
154
依赖性钠-钾泵功能受影响,因而钠离子向红细胞流进远多于钾离子从细胞内外流,使红细<br />
胞变形,趋向球状,最后导致溶血。母牛血红蛋白尿时,血磷浓度明显下降。许多学者证明,<br />
磷与红细胞无氧糖酵解正常进行有密切关系,磷不足,则意味着糖酵解终产物 ATP 不足,<br />
钠-钾泵功能则难以维系。此外,母牛血红蛋白尿时,另一特点是红细胞内出现 Heinz 小体,<br />
Rifkin 和 Danon(1965)用电镜观察到当小体形成后即相互凝结或聚合在一起,并向红细胞<br />
膜靠近,最后附着到红细胞膜上,与膜上的巯基键一起混合形成二硫键,使细胞膜变硬,可<br />
塑性下降,这种红细胞通过脾脏时,则很易被清除,产生体内溶血。至于无机磷经何途径,<br />
在哪一步骤影响糖酵解作用,及为什么在没有食入含 SMCO 饲料时,红细胞内是否都有<br />
Heinz 小体形成。另外,即使有 Heinz 小体,也不一定有血红蛋白尿等,这些现象还难以解<br />
释。<br />
此外,有些饲料如甘蓝含有硫氰酸盐、硝酸盐和磺酸化合物等强力溶血物质,还有认为<br />
分娩、妊娠、寒冷、炎热等应激作用在疾病发生中,也可能起诱发作用。<br />
大量血管内溶血,机体缺氧是造成动物死亡的直接原因。<br />
【症状】 病牛大多为第 3~6 胎高产母牛,发病于产后 4 天至 4 周。肉用牛和 3 岁以<br />
下的奶牛极少发生。中国水牛大多在怀孕第 3~5 个月,喂乳 6~7 个月时发病,但空怀牛,<br />
甚至公水牛也有发生,印度水牛多于产后,埃及水牛多于怀孕后期发病。经治疗,尿色逐渐<br />
由褐变为紫红、淡红,最后正常。<br />
红尿是本病早期唯一的症状,病牛尿液突然变红,尿液在最初 l~3 天内逐渐由淡红、红<br />
色、暗红色直至紫红色和棕褐色。由于血红蛋白对肾脏和膀胱的刺激作用,排尿次数增加,<br />
但各次排尿量相对减少,收集尿液并静置 24h 后,呈上下一致红褐色,以至黑色,一般无红<br />
细胞沉积在杯底,目测可见。<br />
血液稀薄,随病程发展,病情加重,红细胞溶解增多,红细胞数由正常时的 5×10 12 ~6<br />
×10 12 个/L(500 万~600 万个/mm 3 )降低至 1×10 12 ~2×10 12 个/L(100 万~200 万个/<br />
mm 3 ),血红蛋白由正常时的 50%~70%降低为 20%~40%,红细胞压积正常时 40%降至 30<br />
%甚至低至 20%。奶牛血清无机磷浓度可从正常时 1.71mmol/L(5.29mg/100m1)降为<br />
0.13~0.48mmol/L(0.4~1.5mg/100m1),亚临床病例血磷浓度也明显降低 0.65~0.97mmol<br />
/L(2~3mg/100m1)。中国水牛血清无机磷浓度可从 1.61mmol/L(4.99mg/100m1)降<br />
为 0.97mmol/L(3mg/100m1)以下。血清钙离子浓度在正常范围内 2.5mmol/L(约 10mg<br />
/100m1)。<br />
血液涂片中可以发现红细胞内有 Heinz 小体。有些病例中还出现变形红细胞。在各种病<br />
例中,红细胞脆性不增加。<br />
奶牛的采食、饮水照常,但乳产量下降,在尿色转为正常后 24h,产乳量才恢复正常,<br />
有明显的脱水现象,粪便干燥,体温略有升高。因溶血,黄疸现象明显。病程延至 3~5 天后,<br />
病奶牛虚弱,心搏动急速而强,可有颈静脉怒张,明显的颈静脉搏动。呼吸短促,行走时步<br />
样不稳,最终卧地不起,数小时后迅速死亡。<br />
水牛除了血红蛋白尿、贫血、黄疸外,体温、呼吸、食欲无明显变化。严重贫血时,食<br />
欲稍有下降。呼吸次数稍增加,但均不明显。也极少出现胃肠及肺的并发症。脉增数,因贫<br />
血和稀血,心音有稀血性杂音。<br />
奶牛死亡率达 50%,水牛很少有死亡者,如抢救不及时,亦可引起死亡。死后剖检,<br />
表现消瘦、黄疸、肝肿大和脂肪浸润,膀胱内有残留的红色尿液。<br />
【诊断】 奶牛有特征性的在产后几天至 4 周内突然呈现血红蛋白尿,水牛可不明原因<br />
地突然出现血红蛋白尿,全身其余状况尚好者,通常作为该病诊断,如配合血液无机磷浓度<br />
测定,血液学检查不难作出诊断。但引起血红蛋白尿的原因很多,如钩端螺旋体、梭菌毒素<br />
中毒、焦虫病、慢性铜中毒、犊牛水中毒、油菜、甘蓝中毒、输血及药物性(吩噻嗪、大黄<br />
155
等)中毒,洋葱中毒等都可引起血红蛋白尿,应根据各种疾病的流行病学和自身特点,逐一<br />
进行区别。蕨类中毒、地方性肾盂肾炎、急性肾小球性肾炎、血栓性肾炎、肾梗死、出血性<br />
膀胱炎、尿石症、尿道出血、泌尿系统肿瘤等,其主要症状为血尿,将尿液静置 24h 后,下<br />
层有红细胞沉淀物,可予以区别。<br />
【治疗】 补磷有良好的效果,一方面用磷制剂作静脉注射,同时在饲料中补充含磷丰<br />
富的食物如麸皮、米糠、花生饼、豆饼、骨粉等。<br />
磷制剂是用 20%磷酸二氢钠溶液,奶牛产后血红蛋白尿用 300ml,水牛用 300~500ml<br />
静脉注射,随后每隔 12h 皮下注射,一般注射 1~2 次后,红尿颜色逐渐变淡,重症多需注射<br />
3~4 次,红尿完全消失,切勿用磷酸二氢钾代替,以免引起心跳骤停。静脉输血;口服骨粉,<br />
一天 2 次,水牛 250g 一次,或过磷酸钙,每次 15g,一天 3 次,并配合硫酸亚铁、硫酸钴<br />
治疗,可促进动物康复。治疗中配合注射高糖,以纠正奶牛的酮病也是必要的。<br />
【预防】 乳牛应给予足够的钙、磷,并按一定比例供给,尤其是泌乳早期。据新西兰<br />
报道,在施钼肥地区补充铜可减少奶牛的发病,水牛饲料中应注意补磷,特别是在干旱、寒<br />
冷年份,应调整饲料中钙、磷比例,以减少疾病发生。<br />
(三)钙、磷异位沉着症<br />
钙、磷除以离子态形式存在于血浆、组织液中外,绝大部分沉着在骨骼、牙齿等硬组织<br />
中,当受到各种致病因素及钙、磷、VD本身代谢紊乱,而使钙、磷化合物沉着在肠腔、肾<br />
脏、膀胱、胆囊、肺、甚至肌肉、血管壁内的现象称为钙、磷异位沉着症,如肠结石,胆结<br />
石、肾结石、膀胱结石、尿道结石、胰结石、涎结石等,软组织中大量钙的异位沉着可见于<br />
鸡骨化石病和犬、猫的广泛性肺钙化石化症。<br />
1.尿石症(Urolithiasis) 在尿路中形成大小不等的矿物质结晶物称为尿石(urinary<br />
calculus)。尿石是典型的常见的钙、磷异位沉着症,尿石多存在于尿路中直径较宽大的部位,<br />
如肾盂、膀胱等。尿石的大小、形状不一致,最细的如砂子,称为尿砂,大的如绿豆、蚕豆,<br />
甚至大如拳。由尿石引起尿路较细部位的阻塞不畅,排尿困难的现象称为尿道结石症。多发<br />
生于公牛、公羊、公猪,尤其是去势后的肉牛、水牛。母畜亦可发生尿石,但因尿路较短,<br />
引起阻塞现象较少。马有时亦可发生。<br />
【病因及病理】 病因至今尚未完全阐明。目前普遍认为尿石的形成是多种因素综合作<br />
用的结果,但主要与饲料及饮水质量和数量、机体矿物质代谢状态,以及泌尿器官,特别是<br />
肾脏的机能活动有密切的关系。<br />
尿石是由核心物质和矿物质盐类构成。前者如粘液、凝血块、脱落上皮细胞、坏死组织<br />
碎片、红细胞、微生物、纤维蛋白、异物等,称为尿石的基质,后者为钙、氨及镁的碳酸盐、<br />
磷酸盐、硅酸盐、草酸盐、尿酸盐等与某些胶体物质,如粘蛋白、核酸、粘多糖等沉着在核<br />
心的外围,构成尿石的实体。<br />
在正常尿液中,含有大量呈溶解状态的盐类晶体及一定量的胶体物质,晶体盐类与胶体<br />
物质之间保持着相对平衡。一旦这种平衡破坏,即晶体超过正常的饱和浓度,或胶体物质由<br />
于不断丧失其分子间的稳定性结构,核心物质又不断产生时,则尿中盐类晶体就不断析出,<br />
进而凝结成尿石。促使尿石形成的因素,可归纳为下列几方面。<br />
(1)饮食不当 如饲喂高钙饲料时,形成高钙血症和高钙尿症,有利于碳酸钙尿石的<br />
形成;牛采食含硅量高的青草或粗饲料造成硅酸盐在尿中沉淀而形成硅尿石。饲料中磷酸盐、<br />
镁含量过高容易形成磷酸氨镁性结石。<br />
(2)长期饮水不足 饮水不足时则尿液浓缩,致盐类浓度过高而促进盐类结晶。<br />
(3)尿钙过高 甲状旁腺机能亢进,肾上腺皮质激素分泌增多,过量服用维生素 D 等,<br />
使尿钙增高,促进尿石形成。<br />
(4)尿液理化性质改变 尿液潴留,其中尿素分解生成氨,使尿液碱化,易形成碳酸<br />
156
钙、磷酸钙、磷酸铵镁等尿石;酸性尿易促进尿酸盐结石的形成。尿中柠檬酸含最下降,易<br />
发生钙盐沉淀。<br />
(5)尿中粘蛋白、粘多糖增多 精料饲喂过多,或肥育时应用雌激素,尿中粘蛋白、<br />
粘多糖增加,有利于尿石的形成。<br />
(6)维生素 A 缺乏 维生素 A 缺乏,使中枢神经调节盐类代谢功能发生紊乱,尿路上<br />
皮角化及脱落,促进尿石形成。<br />
(7)肾及尿路感染、炎症 饲喂棉籽饼的公畜尿石症发生率较高,可能与其引起尿路<br />
粘膜损伤有关。并发现应用某些磺胺类药物(乙酰化率高的制剂)治疗病畜时出现尿石症病<br />
例增多。<br />
尿石形成的原始部位主要是肾脏,以后可转移至膀胱,膀胱中继续增大,并可移行至尿<br />
道发生阻塞,引起排尿障碍,如在初期呈现不全阻塞时,见有少量尿液呈滴状流出,以后完<br />
全阻塞时,则发生尿闭、膀胱积尿、逐渐膨大而导致麻痹,甚至发生破裂。<br />
【临床表现及诊断】 突出症状为排尿障碍、肾性腹痛和血尿,但因尿石存在部位及其<br />
对有关器官损害程度不同,表现症状各异。<br />
结石位于肾盂时,多呈肾盂炎症状,并出现血尿,严重时形成肾盂积水。患畜肾区疼痛,<br />
运步强拘,步态紧张。<br />
肾石移行至输尿管而刺激或阻塞输尿管时,病畜表现剧烈疼痛不安,单侧输尿管阻塞时,<br />
不出现尿潴留现象。直肠内触诊可感觉阻塞部前(近肾端)方输尿管紧张且膨胀,波动感,<br />
而阻塞后方呈正常柔软之感觉。<br />
尿石位于膀胱腔时,一般不呈现任何症状,但大多数病畜表现频尿或血尿,膀胱敏感性<br />
增高。公牛、公羊阴茎包皮周围常附有干燥细砂粒样物。尿石位于膀胱颈部时,呈现明显疼<br />
痛和排尿障碍,频频呈排尿动作,但尿量较少或无尿排出,患畜呻吟,腹壁抽缩。<br />
尿道结石,公牛、公猪多阻塞于 S 状曲或会阴部位,公马则多发生于骨盆终部。尿道<br />
不完全阻塞时,病畜排尿痛苦且排尿时间延长,尿液呈断续或点滴状流出,有时出现血尿,<br />
当尿道完全阻塞时,出现尿潴留及肾性腹痛现象,病畜后肢叉开,拱背缩腹,举尾,阴茎抽<br />
动,屡呈排尿动作,但无尿排出。尿道探诊,可触及尿石所在部位,尿道外部触诊有时可摸<br />
到硬块,有疼痛感。直肠检查,膀胱膨大,充满尿液,按压也不能使尿液排出。长期尿潴留<br />
可引起尿毒症及发生膀胱破裂。一旦膀胱破裂,由尿路阻塞引起的努责、疼痛不安及频频排<br />
尿动作突然消失,直检膀胱空虚或收缩呈梨状物。下腹部迅速膨大,冲击式触诊有振水音,<br />
腹腔穿刺有大量液体流出,呈淡黄色或红色,有尿臭味。当尿砂位于龟头时,呈现包皮膨大,<br />
滴尿,手指探诊,可发现有尿砂或结石块。<br />
【防治】<br />
(1)有地方性尿石生成倾向的地区,可通过改善饲养条件,如给牛、猪以大量饮水和<br />
多汁饲料,必要时可适当使用利尿剂,以形成大量稀释尿,减少尿液晶体析出并防止沉淀,<br />
为保证足够饮水,可添加适量的盐。<br />
状尿石。<br />
(2)水冲洗。用导尿管插入尿道或膀胱,注入清洁水反复冲洗,适用于粉末状或砂砾<br />
(3)手术治疗。大多数完全阻塞或不完全阻塞块,多采用尿道或膀胱切开,取出结石。<br />
必要时可作尿道改向手术或阴茎切除手术。<br />
(4)防止长期单调以某种富含矿物质的饲料和饮水饲喂家畜。饲料中钙、磷比例应保<br />
持在 1.2~1.5:1,并注意维生素 A 的供给。<br />
(5)有报道,补饲氯化铵(阉牛 45g/日,绵羊 10g/日)可预防磷酸盐尿结石形成,<br />
而氯化钠可预防硅酸盐结石。<br />
2.肠石病(Enterolithiasis) 肠腔内为结石阻塞,妨碍内容物后移,引起动物剧烈腹<br />
157
痛的现象称为肠石症。临床上以慢性消化不良,反复发作性腹痛,伴以食欲废绝、肠音衰沉、<br />
继发臌气等,以老龄马多发,其它家畜少见。<br />
由矿物性凝集物构成的结石称为真性肠结石俗称马宝,呈圆形、椭圆形或多边形,体积<br />
从豆粒至柚子大不等,外表圆滑,结构致密,质地坚实而沉重;剖面呈轮层状,中央部有核<br />
心体,系各种异物;外周为沉积的矿物质,主要成分为磷酸铵镁(占 78%左右)。假性肠结<br />
石也称粪石,多由纤维毛球和异物构成,结构疏松,剖面无核心,不显轮层,中央为植物纤<br />
维等,周围有无机盐沉积或只裹一层薄层,主要矿物成分是磷酸钙和碳酸钙。<br />
一般认为,马肠结石形成需 4 个基本条件,即饲料内含大量磷酸镁,且小肠对磷酸镁的<br />
吸收障碍;大肠内有大量氨存在;有异物或食物残片作为晶核;肠管某段处于相对静息状态。<br />
经常大量应用麸皮、米糠等含磷丰富的精料饲喂马、骡的地区多发肠石症。<br />
肠石症的诊断可根据长期大量饲喂富磷精料的生活史,慢性消化不良和轻度腹痛反复发<br />
作的病史,投以泻剂后病情反而增重等作出可疑诊断,确诊应依据直肠检查或剖腹探查结果,<br />
直检时有时可触及坚硬石块,沉于腹腔下方,触之极痛,如结石块较大,多位于右上大结肠<br />
或胃状膨大部,使阻塞肠段移位,偏于腹下方而诊断。<br />
对急性发作的肠石症,不应投服泻剂,可先按急腹症实施解痉镇痛、肠内减压、补液强<br />
心等对症治疗。对小结肠起始部堵塞,可反复进行高压灌肠,使结石还退回到胃状膨大部,<br />
可获得相对治愈。如确诊在小结肠或胃状膨大部结石,应迅速采取肠管切开术取出肠结石。<br />
3.胆石病(Cholelithiasis) 胆管或胆囊内形成结石,在人发病率比较高,而在兽医临<br />
床上偶可见到牛的胆囊结石,俗称牛黄。动物胆石病的发生无品种和性别差异,2 岁以上发<br />
病较多。发病原因有待阐明,可能与胆囊慢性炎症有关。犬、猫胆石成分分析表明,其主要<br />
含有胆固醇、胆红素、钙、镁及草酸盐等。<br />
胆石病并不总是出现明显的异常表现,仅在某些情况下才出现呕吐和腹痛,当结石穿透<br />
胆囊壁时,可出现胆汁性腹膜炎。当胆石矿物质含量较高,在为其它目的作腹部 X 光检查<br />
时,偶尔可在胶片上呈现亮点而检查出来。多数病例是在作尸体解剖时才发现结石的。<br />
在胆管或胆囊内形成的胆石可移行至胆总管形成永久性或暂时性堵塞。永久性堵塞需作<br />
手术解除。暂时性反复发作性胆总管堵塞,往往有反复发作性黄疸表现。肝内或肝外胆管阻<br />
塞引起的胆总管结石总是出现黄疸,且有结合胆红素含量超过总胆红素 50%的特点。随着<br />
阻塞的不同时期,可能因继发肝坏死而出现血清转氨酶升高,碱性磷酸酶活性通常升高。<br />
4.鸡骨化石病(Osteopetrosis) 鸡骨化石病,曾称作厚腿病或大理石骨病,以骨骼尤<br />
其是长骨和胸骨呈均匀或不规则的增厚,骨髓腔减小,骨膜完整性破坏为特征。临床表现为<br />
懒动,行走艰难,鸡冠苍白,骨骼肌萎缩等。大多认为由禽白血病、肉瘤病毒群的某些型病<br />
毒引起。用成红细胞性白血病病毒(RPL12-L29)及有关病毒对 1 日龄雏鸡作静脉注射接种,<br />
1 月龄后可发生本病。自然发病最常见于 8~12 周龄。本病起因虽与马立克氏病和白血病有<br />
关,但表现结果却为钙在软组织中异位沉着。<br />
【临床表现】 最常侵害肢体的长骨,尤其胫骨、骨干或干骺端可见均匀或不规则增厚、<br />
肿大,骨干呈纺锤形,由于胫骨肿胀,表现出特征性“长靴样”外观。病鸡常发育不良,精<br />
神倦怠、懒动,全身无力,鸡冠苍白或发绀,虚弱,消瘦,有时腹泻,行走艰难。步行拘谨<br />
或跛行,病程从几天至几个月不等。<br />
【病理变化】 肉眼可见病变最先发生于胫骨、跗骨和跖骨骨干,后见于其它长骨、骨<br />
盆、肩和肋骨,趾骨常无变化。病变常呈两侧对称,起初有骨头上出现浅黄色病灶。骨膜增<br />
厚,骨骼呈海绵样,易被折断。病变逐渐向周围扩散,并进入干骺端,发展为梭形骨骼,病<br />
变可由轻度外生骨疣,至巨大的不对称增大,以至完全堵塞骨髓腔。后期骨质石化,异常坚<br />
硬,表面多孔、不平且不规则。<br />
显微变化显示骨膜增厚,海绵骨向心地向骨干中央汇合,哈佛氏管体积不规则,腔隙数<br />
158
目和体积增加,位置改变,骨细胞数增多,体积变大,呈嗜酸性染色。<br />
【诊断】 晚期骨骼病变具明显特征,增粗、坚硬、石化、骨疣等,不难诊断。须与佝<br />
偻病、骨质疏松症等相区别。佝偻病主要产生骨变形、龙骨脊柱弯曲呈 S 形,肋骨与肋软<br />
骨间增粗如串珠状。骨骼疏松症主要在骺端显示多孔状,骨易折断等。<br />
【防治】 有人曾尝试用病毒制备灭活菌,但效果不佳。本病发病率低,一旦确诊,应<br />
即淘汰处理。<br />
5.广泛性肺钙化和骨化症(Generalized Pulmonary Calcification and Ossification) 广<br />
泛性肺钙化和骨化症,在狗又称为肺石症、浮石肺、肺泡微结石症,在猫常称作细支气管微<br />
结石症,即肺泡和细支气管内形成无数细小钙球(钙粒与细胞间质形成的球形小体),肺叶<br />
坚硬而重实,仅偶尔发生。病因尚不明,有人认为猫广泛性肺钙化是在肉芽肿和细支气管炎<br />
基础上导致微结石形成的。<br />
广泛性肺钙化和骨化的 X 线检查特征为出现网状结节,线状或细小结节结构,密度增<br />
加,其细小网状结节结构与肺间质钙化相似,结节的数量超过其它任何类型的肺钙化,诸如<br />
肺骨瘤、霉菌肉芽肿钙化等,该病无有效治疗办法。<br />
二、镁营养紊乱性疾病(Nutrtional Disorder of Magnesium)<br />
(一)青草搐搦(Grass tetany)<br />
青草搐搦,又称为泌乳搐搦(lactation tetany),或青草蹒跚(grass stagger),麦类牧草<br />
中毒(wheat pasture poisoning)。是反刍动物高度致死性疾病。以血镁浓度下降和伴有血钙<br />
浓度下降为特点。临床上以强直性和阵发性肌肉痉挛、惊厥、呼吸困难和急性死亡为特点。<br />
青草搐搦主要发生于泌乳母牛和母羊。犊牛、小公牛也能发生。因本病死亡率高,经济<br />
损失较大。<br />
【病因】 镁摄入不足,泌乳母牛饲料中有效镁含量不能满足其本身需要。或因春季来<br />
临,牛群从舍饲吃干草和青贮料,突然转入放牧吃多汁、幼嫩的青草,不仅草中镁含量不足,<br />
而且镁的吸收、利用率较差。江苏沿长江各县、市早春于江边滩地放牧时,有时可见破伤风<br />
样症状的小牛,据称与缺镁有关。绵羊饥饿 24h 后进入草地,就可发生搐搦症。禾科牧草尤<br />
其是用大量氮肥和钾肥施肥的谷草,因镁含量不足易发生该病。<br />
镁摄入不能满足镁排泄的需要,如乳牛尤其是高产乳牛,每天从泌乳中丢失约 3.0g 镁,<br />
不论血浆镁浓度的高低,这一量是恒定的。每天内源性损耗的镁大约 2~3g,如饲料中粗纤<br />
维多,唾液分泌增多,镁内源性损耗更多,约 4~5g。镁的吸收率约 20%,经计算,每天必<br />
须食入 20~25g 镁,才能满足机体需要。冬季舍饲期牛,每天可采食 32~34g 镁,基本已满<br />
足需要,而夏季有些牛仅获得 10~22g/天,加之初入草场,常伴有拉稀,食物在肠道内停<br />
留时间短,真正吸收的镁,不能满足其本身需要。<br />
镁在体内保存的量有限。一头牛约可保存 20g 镁,其中 70%存在骨骼中,软组织内占<br />
29%,血镁仅占 1%(仅 0.2g)。除犊牛外,骨骼中镁很难被动员入血。组织中仅有 4%的镁,<br />
可以交换。因此,血镁很易被损耗,尿镁可随摄入蛋白质增多而增多,但对总排泄量影响不<br />
大。血镁浓度可随季节而波动,如血镁浓度已呈亚临床性减少,而饲料中供镁不足,可引起<br />
低镁血症。<br />
与饲料中镁的可利用性差有关,有些牛所食草中镁含量并不低,但因饲料中蛋白质含量<br />
过多,瘤胃内氨浓度增加,瘤胃内碱性基团增多,可减少镁的利用。饲料中硫酸盐含量较高,<br />
钠盐含量低,大量使用氮肥或钾肥,或同时使用氮肥和钾肥,影响植物对镁的吸收也可影响<br />
动物对镁的利用。大量使用磷肥,在消化道内形成不溶性磷酸氨镁,减少了镁的吸收。饲料<br />
中长链脂肪过多,形成皂化反应,使镁丢失。<br />
钙与镁有共同的吸收部位,它们是相互拮抗的。钙太多镁吸收减少。<br />
体内激素水平对镁的吸收利用有明显影响,甲状旁腺素减少,甲状腺素分泌过多,应激<br />
159
因素等都可促使低镁血症。<br />
【临床表现】 本病一年四季都可发生,但大多在春季,舍饲后放牧于多汁草场。即使<br />
在冬季,因产犊后泌乳,或在小牛断乳时,可发生低镁血症。一般情况下,发病率为 2%~12<br />
%。死亡率多在 20%~30%左右。以麦类牧草饲喂,发病率最高。如燕麦、大麦等,生长早<br />
期麦苗最危险。气候条件恶劣时可加速发病。母牛产后 2 个月内发病较多,故称为泌乳性搐<br />
搦。4~7 岁龄发病率最高。但干乳期母牛,肉牛甚至公牛也可发生。而粗放饲养,发病较少。<br />
根据临床表现和病程,可分为急性型、亚急性型和慢性型。<br />
急性型:于采食过程中突然停止采食,甩头、吼叫、奔跑、肌肉抽搐、行走时摇晃欲醉,<br />
最终跌倒。四肢强直,随后阵发性痉挛,并持续 1min 左右。痉挛期间,牙关紧闭,眼球震<br />
颤,口吐白沫,耳廓竖起,眼睑退缩。略安静片刻,又重新发作,严重挣扎后,体温达 40~40.5<br />
℃,呼吸、脉搏加快,心音亢进,几步之外都可听到心音。通常于 30~60min 内死亡,常来<br />
不及治疗而毙命。<br />
亚急性型:病程约 3~4 天,病的发展呈渐进性。开始时,食欲略下降,四肢运动不自如,<br />
步样强拘,对触诊和声音过敏,频频排尿,排粪,瘤胃运动减弱,乳产量下降,肌肉震颤,<br />
牙关紧闭,状似破伤风。后肢及尾轻度强直,强制性用针扎动物,可引起强烈惊厥。<br />
慢性型:除有血镁浓度下降外,不表现临床症状。有时也有反应迟钝,不活泼,无选择<br />
地采食,可能转化为急性或亚急性,也可能在亚急性型的恢复过程中出现。<br />
水牛青草搐搦常呈亚急性经过。卧地不起,颈呈一定程度的 S 形扭转姿势,惊厥严重,<br />
受外界刺激时肌震颤、角弓反张、四肢划动,呼吸加深,抽搐加剧,体温正常。少数急性发<br />
作。表现兴奋、不安、狂怒、奔跑、凶猛状。倒地后搐搦,抽搐,甚至死亡。血镁浓度降至<br />
0.78mmol/L(1.9mg/100m1)以下。<br />
临床病理学变化:健康牛血镁浓度为 0.70~1.23mmol/L,季节不同而有波动。亚临床低<br />
镁血症时,血镁可降至 0.41~0.82;通常在 0.33mmol/L以下时,就出现临床症状。一般病<br />
牛血镁浓度为 0.21mmol/L,甚至低至 0.06mmol/L。但绵羊血镁浓度低至 0.16mmol/L,<br />
未必出现惊厥。血钙浓度亦降至 1.25~2mmol/L,实验性低镁血症时,血镁浓度可降为<br />
0.21mmol/L。血钙浓度降到 1.13~1.73mmol/L,血磷浓度也从正常时的 1.84,降至<br />
0.29~0.39mmol/L。血钾浓度升高,这是危险的征兆,可引起高血钾性死亡。动物进入低镁<br />
草地 24h后,尿镁浓度下降,从 3~4g/天降为 1.5g/天,至第 8 天减至 0.2g/天。脑脊液中<br />
Mg 2+ 浓度从 0.82 降至 0.51mmol/L,这时血镁、尿镁浓度都下降。<br />
【诊断】 反刍动物,尤其是牛,从舍饲转入多汁草地放牧,突然发生运动不协调。状<br />
似破伤风者可疑为此病。血液中镁、钙、钾离子测定及脑脊液中镁离子测定,可进一步确诊。<br />
但诊断中应与破伤风、狂犬病、急性肌风湿和神经型酮病相区别。破伤风对声、光刺激敏感,<br />
且有臌气现象,病程也较长。狂犬病呈紧张、恐水和上行性麻痹,感觉消失。缺乏搐搦症状。<br />
急性肌风湿与本病十分类似;但对水杨酸制剂治疗敏感。神经型酮病可有血糖浓度下降。<br />
绵羊的低镁血症与低钙血症很难区别,但低镁血症常发生于新近产羔的母羊,又是在多<br />
汁的草场放牧后发病的,测定血清镁和用血清镁治疗效果显著,可作出诊断。<br />
【防治】 对亚急性病例或尚未来得及救治的急性病例,可用 25%的葡萄糖硼酸钙和 5<br />
%的次磷酸镁混合液,牛 500ml、羊 50ml 慢速静脉注射。接着用 50%的硫酸镁作皮下注射,<br />
随后再用 20%的硫酸镁 200~300ml 作皮下注射时,血镁可很快升高。但于 3~6h 内又恢复到<br />
注射前水平,给于钙、镁制剂的同时,作对症治疗,如氯丙嗪、巴比妥等可暂时控制疾病。<br />
每天给予 60g 氧化镁(≈38g 镁),可防止血清镁季节性下降,但不一定能防止低镁血<br />
症。如每天供给 120g 氧化镁,既安全也有效。如给予 180g 氧化镁可产生拉稀。羊每天给予<br />
7g 或每隔一天给予 14g 镁是有效的。<br />
160
HYPOMAGNESEMIC TETANY (LACTATION TETANY, GRASS TETANY, GRASS<br />
STAGGERS, WHEAT PASTURE POISONING)<br />
Synopsis<br />
Etiology. The etiology is multifactorial, related to magnesium concentration in the diet and the<br />
presence of competing cations such as potassium and sodium that affect either herbage<br />
magnesium status or magnesium absorption.<br />
Epidemiology. Disease of all classes of ruminants but reaches its highest incidence in older<br />
lactating cows exposed to bad weather or grazing green cereal crops or lush grass-dominant<br />
pasture.<br />
Clinical findings. Incoordination, hyperesthesia and tetany, tonic-clonic muscular spasms and<br />
convulsions. High case fatality without treatment.<br />
Clinical pathology. Serum, urine or cerebrospinal fluid (CSF) magnesium concentrations.<br />
Hypomagnesemia, and in some circumstances hypocalcemia. Necropsy findings. None specific.<br />
Diagnostic confirmation. Response to treatment, serum or urinary magnesium concentrations.<br />
Treatment. Magnesium or combined calcium/magnesium solutions administered IV and/or SC.<br />
Control. Magnesium supplementation but a palatable and practical delivery method is a problem.<br />
Magnesium applied to pastures. Avoidance of movement and food deprivation at risk periods.<br />
ETIOLOGY<br />
Magnesium is the major intracellular divalent cation, and is an essential clement in a large<br />
number of enzymic activities in the body. For this reason it might be expected that<br />
hypomagnesemia would be rare. However, because, of the peculiarities of absorption of<br />
magnesium in the ruminant forestomachs, and the use of animal and pasture management systems<br />
that can lead to marginal magnesium uptake, ruminants are at risk of hypomagnesemia.<br />
Magnesium homeostasis<br />
There is no feedback regulatory mechanism to control concentrations of magnesium in the body<br />
of ruminants. As a consequence, magnesium concentrations in blood and extracellular fluid are<br />
essentially determined by the balance between dietary intake of magnesium, loss in feces and milk<br />
and the modulating effect of magnesium homeostasis by the kidney.<br />
Dietary intake<br />
In normal circumstances, magnesium absorbed from the diet is sufficient to meet the requirements<br />
of the body and excess amounts are excreted in the urine.<br />
Renal excretion<br />
The kidney is the major organ of homeostasis and can act to conserve magnesium. Magnesium is<br />
freely filtered across the renal glomerulus and is reabsorbed within the renal tubules, the degree of<br />
reabsorption acting in homeostasis. When the dietary intake of magnesium is decreased, blood and<br />
interstitial fluid magnesium concentrations fall; excretion of magnesium in the urine will cease<br />
when serum concentrations fall below 1.8 mg/dL. The renal threshold for magnesium excretion<br />
is partially under the control of parathyroid hormone and increased levels of parathyroid hormone<br />
will act to conserve magnesium.<br />
Magnesium reserves<br />
There are large stores of magnesium in the body, especially in bone. These are available to the<br />
young calf but mobilization decreases with age and in the adult ruminant there is little<br />
mobilization in response to short-term deficits of magnesium (1). In ruminants, this control<br />
mechanism for magnesium can maintain adequate concentrations of magnesium in bodily fluids in<br />
161
most production circumstances but it can fail where there is a high requirement for magnesium<br />
coupled with a decreased intake. This combination leads to hypomagnesemia and<br />
hypomagnesemic tetany is a possible outcome.<br />
Lactation<br />
Increased requirement for magnesium is almost always associated with the loss of magnesium in<br />
the milk during lactation. Whereas the amount of magnesium in milk is not high (12mg/kg) the<br />
loss of magnesium to milk represents a significant proportion of the dietary intake of magnesium.<br />
As a consequence of this drain, most instances of hypomagnesemia occurin lactating animals<br />
around the period of peak milk production, although in some circumstances the demands of late<br />
pregnancy are the cause of the increased requirement. The decreased intake of magnesium can<br />
result from an absolute deficiency of magnesium in the diet or because the availability or<br />
absorption of magnesium from the diet is impaired. These factors determine the circumstances of<br />
occurrence of the disease and are the factors that can be manipulated for control.<br />
Factors influencing aborption of magnesium<br />
In the adult ruminant, magnesium absorption occurs in the torestomach with little absorption in<br />
the abomasum and small intestine. Some absorption occurs in the large intestine, particularly in<br />
sheep (2), however it cannot compensate for malabsorption in the forestomach.<br />
Na:K ratio in rumen<br />
Magnesium is transported across the epithelium of the forestomachs by an active sodium-linked<br />
ATPase-dependent transport system. Absorption, and the serum magnesium concentration, is<br />
influenced by the Na:K ratio in the rumen, which is determined by the dietary and salivary<br />
concentrations of sodium and potassium (3, 4). Absorption of magnesium increases with an<br />
increasing Na:K ratio to plateau at a ratio of 5:1. Absorption is significantly impaired if the Na:K<br />
ratio is less than 3:1.<br />
Young rapidly growing grass is low in sodium and high in potassium and can significantly<br />
depress the Na:K ratio in the rumen fluid, causing impairment ot magnesium absorption.<br />
Depression is observed at dietary potassium concentrations of greater than 22 g/kg dry matter.<br />
Saliva normally has a high Na:K ratio but where there is a deficit of sodium in the diet, a<br />
proportion of sodium in saliva may be replaced with potassium under the influence of aldosterone,<br />
which further negatively influences the uptake of magnesium.<br />
Approximately 40% of the total magnesium available in extracellular fluid is secreted daily in<br />
saliva and 20% of this is reabsorbed in the forestomach. When animals are on tetany-prone grass,<br />
this absorption is impaired, which accounts for the susceptibility ot ruminants to hypomagnesemia<br />
compared to monogastric animals (3).<br />
Other factors influencing absorption<br />
Young grass fertilized with nitrogenous fertilizers has an increased crude protein which is readily<br />
fermentable and leads to increased ammonia concentrations. A sudden rise in ruminal<br />
concentrations of ammonia impairs magnesium absorption in the rumen (5, 6). The uptake of<br />
magnesium is also influenced by the carbohydrate content of the diet, magnesium absorption is<br />
improved with increasing amounts of readily degradable carbohydrates (7). The mechanism of this<br />
action is not known but low concentrations of readily degradable carbohydrate in tetany-prone<br />
pastures in combination with high concentrations of protein maybe important to the occurrence of<br />
the syndrome (5). Volatile fatty acids provide the energy for the active transport of magnesium<br />
across the rumen wall and increase magnesium absorption.<br />
162
Other dietary substances have been proposed to influence the absorption of magnesium<br />
including calcium and phosphorus, organic acids such as citric acid and transaconitate, fatty acids<br />
and aluminum, but the significance of their role is controversial (5).<br />
Magnesium in pastures and tetany hazard<br />
The dietary intake of magnesium in grazing animals is directly related to the<br />
magnesiumconcentration inpasturesbut other elements in pastures also influencemagnesium<br />
absorption by the ruminant as detailed earlier.<br />
Required magnesium concentrations<br />
Hypomagnesemia can result from the ingestion of pastures that have insufficient magnesium to<br />
meet dietary requirements. The estimated magnesium concentration in pasture required to meet<br />
the dietary requirement tor pregnant or lactating cattle varies from 1.0-1.3 g/kg dry matter for<br />
pregnant cattle, depending upon the stage of pregnancy, and 1.8-2.2 g/kg dry matter for lactating<br />
cattle with both estimates assuming minimal interference of absorption by other elements in the<br />
pasture (8).<br />
The recommended minimal 'safe' concentration of magnesium in pastures is 2g/kg dry matter<br />
for lactating and pregnant cattle with a preference for a concentration of 2.5 g/kg dry matter.<br />
Magnesium availability in pastures and hazard<br />
Hypomagnesemia can also occur in animals grazing pastures with adequate concentrations of<br />
magnesium but that contain high concentrations of potassium and nitrogen, which as detailed<br />
earlier, impair absorption of magnesium in the rumen. Pastures with concentrations of potassium<br />
of greater than 30 g K/kg dry matter ami nitrogen greater than 40 g N/kg dry matter are<br />
considered hazardous.<br />
An alternate method for estimating the potential hazard of a pasture is to calculate the K/(Ca<br />
+ Mg) ratio using milliequi valentvalues for this estimate.<br />
Pastures with ratios above 2.2 are considered a risk (9).<br />
Winter hypomagnesemia<br />
The occurrence of hypomagnesemia is not restricted to cattle grazing lush pastures and it also<br />
occurs in the winter periods. In housed lactating dairy cattle being fed conserved feeds,<br />
hypomagnesemia probably has the same genesis as that in grazing cattle being associated with a<br />
high lactational dram of magnesium in combination with the feeding of conserved feeds prepared<br />
from pastures with marginal magnesium concentrations. It also occurs in cattle outwintered on<br />
poor quality teed.<br />
Hypomagnesemia and hypocalcemia<br />
In some outbreaks of hypomagnesemic tetany, there is also hypocalcemia and, although it is of<br />
less severe degree than in parturient paresis, there is increasing evidence that the actual onset of<br />
clinical tetany may be associated with a rapid fall in serum calcium levels superimposed on a<br />
pre-existing hypomagnesemia. This is particularly true tor wheat pasture poisoning but can also<br />
apply to outbreaks with different predisposing factors.<br />
Chronic hypomagnesemia can have a profound effect on calcium homeostasis.<br />
Hypomagnesemia reduces the production and secretion of parathyroid hormone, reduces<br />
hydroxylation ot vitamin D in the liver, and also causes target organ insensitivity to the<br />
physiological effects of parathyroid hormone Mid 1,25-dihydr-oxyvitamin D3 (6, 10, 11). Chronic<br />
subclinical hypomagnesemia can increase susceptibility to milk fever and can predispose to<br />
episodes of milk fever and downer cows in lactating dairy cows during the period of peak lactation.<br />
163
Summary of etiology<br />
In summary, it appears that a number of factors are capable of causing hypomagnesemia in<br />
ruminants and that under particular circumstances one or other of them may be of major<br />
importance.<br />
In lactation tetany of cows and ewes turned onto lush pasture in the spring, a primary dietary<br />
deficiency of magnesium or the presence of high relative concentrations of potassium and nitrogen<br />
in the diet reduces the absorption of magnesium and possibly calcium.<br />
In wheat (cereal) pasture poisoning, the ingestion of abnormally large amounts of potassium<br />
and low levels of calcium in the diet leads to hypomagnesemia and also hypocalcemia.<br />
Hypomagnesemic tetany in cattle wintered at pasture and exposed to inclement weather is<br />
associated with low magnesium intake and inadequate caloric intake, and possibly to the resultant<br />
hyperactivity of the thyroid gland.<br />
Although the above suggestions as to the most important etiological factors in each set of<br />
circumstances in which lactation tetany occurs may be valid, undoubtedly combinations of these<br />
and other factors have etiological significance in individual outbreaks of the disease. The worst<br />
combination of causative factors, and the most common circumstances in which the disease<br />
occurs, is inadequate energy intake with a low dietary content of magnesium (grass pasture) in<br />
recently calved cows during a spell of cold, wet and especially windy weather.<br />
One other important factor is the variation between individual animals in susceptibility to<br />
hypomagnesemia and to the clinical disease. These variations are quite marked in cattle and in<br />
intensively managed, high-producing herds it is probably worthwhile to identify susceptible<br />
animals and give them special treatment (12).<br />
EPIDEMIOLOGY<br />
Occurrence and risk factors for lactation tetany<br />
Lactation tetany in dairy and beef cattle turned out to graze on lush, grass-dominant pasture after<br />
winter housing is common in northern Europe, the United Kingdom and the northern parts of<br />
North America. Grass tetany also occurs in Australia and New Zealand, where the cows are not<br />
housed in winter but have access to a phenomenal flush of pasture growth in the spring (13). This<br />
also commonly occurs m beef cattle in all countries.<br />
With housed cattle, or cattle fed conserved feed during the winter, most cases occur during the<br />
first 2 weeks after the cattle are turned out to spring pasture. Pasture which has been heavily<br />
top-dressed with fertilizers rich in nitrogen and potash is potentially the most dangerous. The<br />
disease may also occur on this type of pasture even when the cattle have wintered on pasture in<br />
temperate regions. In regions where there is an autumn flush of pasture, a high incidence ot<br />
hypomagnesemic tetany may occur in the autumn or early winter.<br />
Cattle in the first 2 months of lactation and 4-7 years of age are most susceptible, which<br />
probably reflects an increased risk due to a higher loss of magnesium in milk. Friesian cows have<br />
lower magnesium concentrations than Jerseys grazed under the same conditions (14).<br />
In the northern parts of the United States, outbreaks commonly occur during periods of low<br />
barometric pressure when the ambient temperature ranges between 7℃ (45℉) and 15.5℃<br />
(60℉) and soil temperatures are below 7℃ (45℉). Outbreaks may be precipitated by inclement<br />
weather. In beef cattle there is commonly a history of poor nutrition and falling body condition in<br />
the past few-weeks due to diminishing hay supplies.<br />
Occurrence and risk factors for wheat (cereal) pasture poisoning<br />
164
Wheat pasture poisoning is a misnomer as it can occur with grazing of any smallgram cereal<br />
pasture. It has been recorded in many countries but is most prevalent where young cereal crops<br />
are utilized for 'winter grazing’.The southwestern United States has experienced heavy losses of<br />
cattle caused by this disease. This pasture can induce hypomagnesemia in pregnant and lactating<br />
cattle and sheep,the risk is with young rapidly growing pasture, either in the spring, or in the<br />
autumn and winter with pastures planted in late summer. The pasture is usually dangerous for<br />
only a few weeks but heavy losses may occur in all classes ot sheep and cattle. Bos taunts breeds<br />
are more susceptible to the development of hypomagnesemia than Bos indicia (15).<br />
Occurrence and risk factors for winter hypomagnesemia<br />
Hypomagnesemic tetany in cattle wintered in the open causes some losses in the United Kingdom,<br />
New Zealand, southern Australia and the east-central states and Pacific slope of the United States.<br />
It occurs in cattle grazed on pasture in the winter with minimal supplemental hay and in cattle<br />
grazed on aftermath crops and corn stover. The disease occurs in regions with temperate climates,<br />
and risk is increased by exposure to bad weather, which is exacerbated by absence of trees or<br />
other shelter in fields and by failure to supply supplementary feed during these cold spells. The<br />
disease does not seem to occur in cattle kept outside in prolonged winters where environmental<br />
temperature is consistently very low and there is adequate feed. Hypomagnesenna is recorded in<br />
housed cattle in the winter in Europe.<br />
Morbidity and mortality<br />
In all of these forms of the disease, the morbidity rate is highly variable, reaching as high as 12%<br />
in individual herds, and up to 2% in particular areas. The incidence varies from year to year<br />
depending largely on climatic conditions and management practices, and the disease is often<br />
limited in its occurrence to particular farms and even to individual fields.<br />
Although an effective treatment is available, the case-fatality rate is high because of the short<br />
course. Since animals die before they are observed to be ill, there are not accurate figures on case<br />
fatality, but it is probably of the order of 30% in dairy cattle and considerably higher in beef cattle.<br />
There have been few epidemiological studies specifically addressing the importance of the<br />
syndrome. In Finland a lactational incidence rate varying between 0.1% and 0.3% is recorded,<br />
with an increase in parity to at least 6 for lactation tetany occurring on pasture but not for indoor<br />
tetany (15). No association with other diseases was found other than for milk fever. In Northern<br />
Ireland, approximately 10% of dairy cows and 30% of beef cows have subnormal or deficient<br />
blood magnesium concentrations during the grazing season and hypomagnesemia is considered<br />
the cause of 20% of the 'sudden death' mortality in beef cattle (I6, 17). Surveys of beef cattle<br />
owners of the relative importance of different diseases invariably rate hypomagnesemia high in<br />
importance.<br />
Pasture risk factors<br />
In most areas of the world there is a strong association between risk for hypomagnesemia and<br />
systems of pasture improvement and pasture fertilization to increase forage yield. There are a<br />
number of influences on the concentration of magnesium and other elements in pasture.<br />
Pasture species<br />
Hypomagnesemia is a problem on grassdominant pastures. Concentrations of calcium and<br />
magnesium are higher in legumes and forbs than in grasses. Within the grasses, different<br />
genotypes of the same species can differ markedly in calcium and magnesium concentrations and<br />
most cool season grasses have the potential to produce hypomagnesemia. However, there are<br />
165
some differences and grasses with a high ratio of potassium to calcium and magnesium (e.g.<br />
Dactylisglomerata, Loliumperenne, Phalaris arundinacea) are more likely to cause grass tetany<br />
than those with low ratios (e.g. Bromus inermis, Poa pratensis, Agrostis spp.) (9). On soil types<br />
where the disease is common, cool-season grass pastures top-dressed with nitrogenous fertilizers<br />
are dangerous and their toxicity may be increased by the application of potash. Warm-season<br />
grasses do not have the same risk and grass tetany is not a problem in cattle grazing tropical<br />
grasses.<br />
Cereal pastures<br />
The greater tendency of cereal grazing to cause hypomagnesemia, is related to a high content of<br />
potassium as well as a low content of magnesium. Tetany hazard, in order of decreasing hazard, is<br />
wheat, oats, barley, rye (14).<br />
Season<br />
High concentrations of potassium and nitrogen and low concentrations of sodium and soluble<br />
carbohydrates occur in pastures during the early growing season and during rapid growth<br />
following cold, wet periods. Pasture magnesium concentrations may not be depressed but the<br />
K/(Ca+Mg) ratio is increased (18).<br />
Fertilization<br />
Application of potash and nitrogenous fertilizers to pastures will decrease the concentration of<br />
calcium and magnesium in plants and will also increase the concentration of potassium and<br />
nitrogen. There is some evidence that nitrate sources of nitrogen depress magnesium less than<br />
ammonium sources of nitrogen.<br />
Soil type<br />
The availability of magnesium to the plant is influenced by soil type and some deficiencies in<br />
plant magnesium can be corrected by soil fertilization with magnesium (19). There is no strong<br />
association with any one soil type but high potassium concentrations are consistently associated<br />
with increased risk for tetany.<br />
Highly leached, acid, sandy soils are particularly magnesium deficient and the most likely to<br />
respond to liming and magnesium fertilization (8). In very acidic soils, high aluminum<br />
concentrations may depress magnesium uptake by plants.<br />
A local knowledge of soil type and its influence on magnesium, potassium, calcium and<br />
nitrogen uptake by pastures can allow the judicious selection or avoidance of the use of pastures<br />
for at-nsk groups during periods of risk for hypomagnesemia (12).<br />
Animal and management risk factors<br />
Dry matter intake<br />
The dry matter and energy intake of ruminants can influence susceptibility to hypomagnesemia<br />
(20). A reduction in dry matter intake must reduce the magnesium intake and, in situations where<br />
hypomagnesemia is already present, a further depression of serum magnesium levels can be<br />
anticipated when complete or partial starvation occurs. An insufficient intake of fiber in the<br />
winter months can precipitate hypomagnesemia in pastured cows and ewes and lipolysis is<br />
accompanied by a fall in serum magnesium.<br />
Period of food deprivation<br />
Many outbreaks of hypomagnesemia are preceded by an episode of stress or temporary starvation.<br />
Whether chronic hypomagnesemia pre-exists or not, a period of starvation in lactating cows and<br />
ewes is sufficient to produce a marked hypomagnesemia and the fall may be sufficiently great to<br />
166
cause clinical tetany. A period of bad weather, yarding, transport or movement to new pastures<br />
or the introduction to unpalatable pastures may provide such a period of partial starvation.<br />
Alimentary sojourn<br />
Diarrhea is commonly associated with lactation tetany on spring pasture and by decreasing the<br />
alimentary sojourn may also reduce magnesium absorption.<br />
Climate<br />
A close association between climatic conditions and serum magnesium levels has also been<br />
observed. Reduced levels occur in adult cattle and sheep exposed to cold, wet, windy weather with<br />
little sunshine and no access to shelter or supplementary feed. Supplementary feeding appears to<br />
reduce the effect of inclement weather on serum magnesium levels and it is possible that failure to<br />
eat, or depression of appetite, and a negative energy balance during bad weather may be a basic<br />
contributing cause to hypomagnesemia in these circumstances.<br />
Animal movement<br />
Epinephrine release will result in a precipitous tall in serum magnesium and tins may explain the<br />
common observation that clinical cases are often precipitated by excitement or movement of the<br />
herd.<br />
Intensive dairies<br />
Intensive dairies that apply effluent on a limited land base can build soil potassium to high<br />
concentrations. Silage from these grounds can have a high risk for inducing hypomagnesemia.<br />
Hypomagnesemia in sheep<br />
Hypomagnesemia occurs in sheep, particularly in Australia and the United Kingdom. The disease<br />
is not common but appears to be increasingly associated with pasture improvement practices, and<br />
can cause heavy losses in individual flocks. It is more common in ewes bred for milk and lamb<br />
production. In outbreaks, ewcs with twins are more liable to develop clinical disease than those<br />
with singles and the mam occurrence is in ewes 1-4 weeks after lambing with cases up to 8<br />
weeks after lambing.<br />
Disease is often precipitated by a management procedure involving movement and temporary<br />
food deprivation and cases will occur within the first 24 h following this and for a few days<br />
afterwards. As in cattle, disease occurs when ewes are placed on lush grass pastures but it is<br />
especially common where ewes in early lactation are placed on young cereal pastures. Losses<br />
usually cease when the flock is moved onto rough, unimproved pasture.<br />
Cases also occur in sheep which are exposed to inclement weather when on a low nutritive<br />
intake. Simultaneous hypomagnesemia and ketosis can occur in ewes after lambing it they are<br />
exposed to low teed availability. Thesc cases do not respond well to treatment. Hypomagnesemia<br />
in ewes is predisposed by prior pregnancy toxemia in the Hock.<br />
PATHOCF.NESIS<br />
Most evidence points to hypomagnesemia as the cause of the tetanic signs observed but the<br />
concurrent hypocalcemia may have a contributory effect and m many instances may even be the<br />
dominant factor. Most clinical cases of the disease have serum magnesium levels below 1 mg/dL<br />
(0.41 mmol/L) compared with the normal levels in cattle of 1.7-3 mg/dL (0.70-1.23 mmol/L) and<br />
there is a striking relationship between the incidence of the clinical disease and the occurrence of a<br />
seasonal hypomagnesemia.<br />
The reduction in serum levels of magnesium is concurrent with a marked fall in the excretion of<br />
magnesium in the urine. In affected herds and flocks, many clinically normal cows and sheep have<br />
167
low serum magnesium levels. In some of these circumstances a concurrent hypocalcemia may be<br />
the precipitating cause.<br />
Magnesium has many influences on impulse transmission at the neuromuscular system,<br />
including effects on the release of acerylcholine, on the sensitivity of the motor end plate, on the<br />
threshold of the muscle membrane and on activation of the chohnesterase system. These offer an<br />
attractive hypothesis for the muscular irritability seen with the disease. However, it has also been<br />
established that magnesium concentrations in the cerebrospinal fluid are more predictive of<br />
clinical disease than those in serum, which would indicate that alterations in CNS function are<br />
more important than alterations in peripheral nerve function. It is also evident that CSF levels of<br />
magnesium in hypomagnesemic animals rise significantly after treatment with a magnesium salt<br />
(21). The need for this to happen would explain the delay of about 30 mm after an IV injection<br />
before recovery occurs.<br />
QLINICAL FINDINGS<br />
For convenience, lactation tetany is described in acute, subacute and chronic forms.<br />
Acute lactation tetany<br />
The animal may be grazing at the time and suddenly cease to graze, adopt a posture of unusual<br />
alertness and appear uncomfortable; twitching of the muscles and ears is also evident. There is<br />
severe hyperesthesia and slight disturbances precipitate attacks of continuous bellowing and<br />
frenzied galloping. The gait becomes staggering and the animal falls with obvious tetany of the<br />
limbs, which is rapidly followed by clonic convulsions lasting for about a minute. During the<br />
convulsive episodes there is:<br />
·Opisthotonos<br />
·Nystagmus<br />
·Champing of the jaws<br />
·Frothing at the mouth<br />
·Pricking of the ears<br />
·Retraction of the eyelids.<br />
Between episodes, the animal lies quietly but a sudden noise or touch may precipitate another<br />
attack.<br />
The temperature rises to 40-40.5 ℃(104-105℉) after severe muscle exertion the pulse and<br />
respiratory rates are also high. The absolute intensity of the heart sounds is increased so that they<br />
can be heard some distance away from the cow. Death usually occurs within 5-1 h and the<br />
mortality rate is high because many die before treatment can be provided. The response to<br />
treatment is generally good if the animal is treated early.<br />
Subacute lactation tetany<br />
In this form of the disease, the onset is more gradual. Over a period of 3-4 d, there is slight<br />
mappctence, wildness of the facial expression and exaggerated limb movements. The cow often<br />
resists being driven and throws her head about as though expecting a blow. Spasmodic urination<br />
and frequent defecation are characteristic. The appetite and milk yield are diminished and ruminal<br />
movements decrease. Muscle tremor and mild tetany of the hindlegs and tail with an unsteady,<br />
straddling gait may be accompanied by retraction of the head and trismus. Sudden movement,<br />
noise, the application of restraint or insertion of a needle may precipitate a violent convulsion.<br />
Animals with this form of the disease may recover spontaneously within a few days or progress<br />
to a stage of recumbency with a similar but rather milder syndrome than in the acute form.<br />
168
Treatment is usually effective but there is a marked tendency to relapse.<br />
Chronic hypomagnesemia<br />
Many animals m affected herds have low serum magnesium levels but do not show clinical signs.<br />
There may be sudden death. A few animals do evidence a rather vague syndrome including<br />
dullness, unthriftmess and indifferent appetite and may subsequently develop one of the more<br />
obvious syndromes. In lactating cows, this may be the development of paresis and a milk<br />
fever-like syndrome that is poorly responsive to calcium treatment. Depressed milk production has<br />
also been attributed to chronic hypomagnesemia in dairy herds in New Zealand (22, 23). The<br />
chronic type may also occur in animals which recover from the subacute form of the disease.<br />
Parturient paresis with hypomagnesemia<br />
This syndrome is described under parturient paresis (p. 1425) and consists of paresis and<br />
circulatory collapse in an adult cow which has calved within the preceding 48 h but in which<br />
dullness and flaccidity are replaced by hyperesthesia and tetany.<br />
CLINICAL PATHOLOGY<br />
Serum or urinary magnesium concentrations can be used for clinical cases. Where an animal is<br />
dead and hypomagnesemia is suspect, a presumptive diagnosis can be made from samples taken<br />
from other at-risk animals in the group, or from the vitreous humor of the dead animal.<br />
Serum magnesium concentrations<br />
Normal serum magnesium concentrations are 1.7-3 mg/dL (0.70-1.23 mmol/L). These levels in<br />
cattle are often reduced in seasonal subclinical hypomagnesemia to between 1 and 2 mg/dL (0.41<br />
and 0.82 mmol/L) but risk for tetany is not present until the level falls to below 1.2 mg/dL (0.49<br />
mmol/L).<br />
The average level at which signs occur is about 0.5 mg/dL (0.21 mmol/L) and in sheep it is<br />
suggested that clinical tetany does not occur until the serum magnesium level is below 0.5 mg/dL<br />
(0.21 mmol/L).<br />
Serum magnesium in some animals may fall to as low as 0.4 mg/dL (0.16 mmol/L) without<br />
clinical illness. This may be due to individual animal variation in the degree of ionization of the<br />
serum magnesium and in the difference between serum and CSF concentrations. It is also possible<br />
that a transitory elevation of serum concentrations occurs after violent muscular exercise.<br />
Total serum calcium levels are often reduced to 5-8 mg/dL (1.25-2.00 mmol/L) and this may<br />
have an important bearing on the development of clinical signs. Serum inorganic phosphate levels<br />
may or may not be low.<br />
In wheat pasture poisoning of cattle there is hypocalcemia, hypomagnesemia and hyperkalemia.<br />
In acute tetany, serum potassium levels are usually dangerously high and may contribute to the<br />
high death rate.<br />
CSF magnesium concentrations<br />
Magnesium concentrations in CSF can be used as a diagnostic procedure but CSF is not easily or<br />
safely collected in tetany cases. Fluid collected up to 12 h after death can be used diagnostically.<br />
Levels in CSF of 1.25 mg/dL (0.51 mmol/L) magnesium were round in tetanic cows with<br />
hypomagnesemia (serum magnesium levels of 0.54 ± 0.41 mg/dL; 0.22 ±0.17 mmol/L). In<br />
clinically normal cows with hypomagnesemia comparable levels in CSF were 1.84 mg/dL (0.74<br />
mmol/L) and in serum 0.4 mg/dL (0.16 mmol/L). In normal animals CSF levels are the same as in<br />
plasma, i.e. 2.0 mg/dL (0.82 mmol/L) and up. The magnesium content of ventricular CSF may be<br />
quite different to that of lumbar CSF. It is also more responsive to changes in magnesium levels of<br />
169
the blood and is preferred for diagnosis at necropsy (24).<br />
Urine magnesium concentrations<br />
The occurrence of low urine magnesium levels is good presumptive evidence of hypomagnesemia<br />
(25).<br />
Herd diagnosis<br />
The kidney is the major organ of homeostasis and it has been argued that analysis of urine<br />
magnesium status is a more accurate method of assessing herd magnesium status than serum<br />
magnesium concentrations (26). The magnesium status of a herd, and the need to supplement the<br />
diet to prevent lactation tetany, can be established from (1) serum magnesium levels, (2) urinary<br />
magnesium fractional clearance ratios or (3) creatinine-cor-rected urinary magnesium<br />
concentrations.<br />
Laboratory charges for urinary magnesium fractional clearance ratios are expensive. The<br />
determination of the creatinine-corrected urinary magnesium concentration from 10 cows in a<br />
herd has been found to be a more sensitive indicator of magnesium status of the herd than<br />
estimates from serum, and a better predictor of response to supplementation. Values of less than<br />
1.0 mmol/L indicate that a positive response to supplementation is likely (26).<br />
NECROPSY FINDINGS<br />
There are no specific findings. Extravasations of blood may be observed in SC tissues and under<br />
the pericardium, endocardium, pleura, peritoneum and intestinal mucosa. Agonal emphysema may<br />
also be present. The magnesium content of the bovine vitreous humor is considered to be an<br />
accurate estimate of magnesium status for 48 h after death, provided the environmental<br />
temperature does not exceed 23℃ (73℃) (24). Concentrations in the aqueous humor are not<br />
diagnostic (27).<br />
DIFFERENTIAL DIAGNOSIS<br />
Cattle<br />
•Acute lead poisoning (p. 1578)<br />
•Rabies (p. 1201)<br />
•Nervous ketosis (p. 1453)<br />
•Bovine spogiform encephalopathy (p.1233).<br />
Sheep<br />
•hypocalcemia (p. 1429)<br />
•Phalaris poisoning (p. 1651)<br />
•'Stagger'syndromes (pp. 1689, 1698,1703).<br />
TREATMENT<br />
IV administration of preparations containing magnesium or magnesium and calcium are used. The<br />
efficiency of the various treatments appears to vary from area to area, and even within areas under<br />
different conditions of management and climate. Response rates and recovery rates are much<br />
higher in cases treated early in the clinical course. IV chloral hydrate may be administered to<br />
reduce the severity of convulsions during treatment with magnesium. Case fatality, even with<br />
therapy, can be high, especially in advanced cases.<br />
Combined calcium/magnesium therapy<br />
The safest general recommendation is to use a combined calcium-magnesium preparation (e.g.<br />
500 mL of a solution containing 25% calcium borogluconate and 5% magnesium hypophosphite<br />
for cattle, 50 mL for sheep) IV followed by a SC injection of a concentrated solution of a<br />
170
magnesium salt. The details and risks of administration of the type of solution is given in the<br />
section on parturient paresis (p. 1430). A combination of 12% magnesium adipate and 5% calcium<br />
gluconate at a dose rate of 500 mL is also used.<br />
Magnesium therapy<br />
When magnesium solutions are used 200-300 mL of a 20% solution of magnesium sulfate may be<br />
injected IV; this is followed by a rapid rise in serum magnesium concentration which returns to<br />
preinjection levels within 3-6 h. A much slower rise and fall occurs after SC injection and for<br />
optimum results the SC injection of 200 niL of a 50% solution of magnesium sulfate has been<br />
recommended. A rise in serum magnesium of 0.5 mg/dL (0.21 mmol/L) occurs within a few<br />
minutes and subsequent levels do not go above 5 mg/dL (2.06 mmol/L). In cases where serum<br />
magnesium levels are low because of a seasonal hypomagne-semia, the injection of magnesium<br />
salts is followed by a rise and then a return to the subnormal preinjection levels.<br />
The IV injection of magnesium salts is not without danger. It may induce cardiac dysrhythmia,<br />
or medullary depression may be severe enough to cause respiratory failure. If signs ot respiratory<br />
distress or excessive slowing or increase in heart rate are noticed, the injection should be stopped<br />
immediately and, if necessary, a calcium solution injected.<br />
The substitution of magnesium lactate for magnesium sulfate has been recommended to provide<br />
a more prolonged elevation of serum magnesium levels. A dilute solution (3.3%) causes minimal<br />
tissue injury and cm be administered IV or SC. Magnesium gluconate has also been used as a 15%<br />
solution at dose rates of 200-400 mL. High serum magnesium levels are obtained more slowly and<br />
are maintained longer than with magnesium sulfate.<br />
The feeding ot magnesium-rich supplements, as described under control later, is recommended<br />
after parenteral treatment.<br />
Provision for further cases<br />
The predisposing factors that lead to a case of hypomagnesemia apply to the herd as a whole and it<br />
is probable that further clinical cases will occur before the effects of corrective strategies are in<br />
effect. In extensive range situations, it is advisable to instruct the owner on how to treat cases as a<br />
delay in treatment can markedly increase the rate of treatment failures. SC treatment is within the<br />
realm of most, but successful therapy is also recorded by the rectal infusion of 30 g of magnesium<br />
chloride in a 100 mL solution; serum concentrations of magnesium return to normal levels within<br />
10 min of administration (28).<br />
CONTROL<br />
Where possible, animals at high risk should be moved to low-risk pastures<br />
during the grass tetany season. High-risk pastures can be grazed by low-risk animals, steers or<br />
yearling heifers for example, during this period.<br />
The occurrence of hypomagnesemia can be corrected by the provision of adequate or increased<br />
amounts of magnesium in the diet. The problem is in determining an adequate delivery system<br />
and this will vary according to the management system. Thus blocked minerals containing<br />
magnesium or foliar dressing of magnesium may be adequate delivery systems where there is a<br />
high stocking density of cattle, but they are totally inadequate or economically unfeasible on range<br />
with one cow per 20 acres.<br />
Magnesium oxide is commonly used for supplementation but other magnesium salts can be<br />
used and they have an approximate equivalent availability (29). The biological availability of<br />
magnesium from magnesium carbonate, magnesium oxide and magnesium sulfate for sheep has<br />
171
een determined as 43.8%, 50.9% and 57.6%, respectively.<br />
Feeding of magnesium supplements<br />
The preventive measure which is now universally adopted is the feeding of magnesium<br />
supplements to cows during the danger period. The feeding of magnesite (containing not less than<br />
87% magnesium oxide), or other sources of magnesium oxide, prevents the seasonal fall in serum<br />
magnesium levels. Daily administration by drenching, or in the feed, of at least 60 g of<br />
magnesium oxide per day is recommended to prevent the disease. This is not always completely<br />
effective and m some circumstances large doses may be necessary. Daily feeding of 120 g is safe<br />
and effective but 180 g daily may cause diarrhea. The dose for sheep is 7 g daily or 14 g every<br />
second day. Magnesium phosphate (53 g/d) is also a safe and effective way of insuring a good<br />
intake of magnesium. The protection afforded develops within several days of commencing<br />
administration and terminates abruptly after administration ceases.<br />
Problems with palatability<br />
The problem with magnesium supplements is with getting the stock to eat the required amount as<br />
they are unpalatable. This can be partially countered by mixing the supplement with molasses in<br />
equal parts and allowing free access to the mixture, or feeding it in ball feeders,<br />
but uniform intake by all animals does not occur and at-risk animals may still develop<br />
hypomagnesemic tetany. Similarly, magnesium blocks may have limited efficacy in preventing<br />
hypomagnesemia (16, 17).<br />
Spraying on hay<br />
One method of attempting to insure an adequate intake of magnesium is to spray it on hay and to<br />
feed this hay as a supplement during periods of grass tetany risk. The common practice is to:<br />
1.Mix magnesite with molasses<br />
2.Dilute mixture with water<br />
3.Spray mixture onto hayin the windrows when it is being made<br />
4.Inject mixture into the bales before<br />
feeding or spray onto the hay at feeding<br />
5.Determine the level of application by<br />
the amount of hay intended to be fed.<br />
Depending upon local circumstances, this method may or may not be effective, as cattle and<br />
sheep will frequently not eat hay when on spring pasture unless they are confined for that purpose.<br />
Pellets<br />
Magnesium-rich pellets suggest themselves as a means of supplementation when the additional<br />
cost can be borne. Palatability is again a problem and care needs to be taken to include palatable<br />
material in the pellets; alternatively they may be mixed with other grain or molasses for feeding.<br />
Calves should be restricted from access as magnesium oxide at high levels of intake (2% and 4%<br />
of the ration) is toxic to calves and causes diarrhea with much mucus in the feces.<br />
In some high-risk situations it may be advisable to provide magnesium in several forms to<br />
insure adequate intake.<br />
Routine daily drenching<br />
A once-daily oral administration of magnesium oxide or magnesium chloride to lactating dairy<br />
cows (to provide 10 g magnesium per cow), administered with a drenching gun just before the<br />
cows leave the milking parlor, is used in New Zealand to insure adequate supplemental<br />
172
magnesium during periods of high risk. The cows become used to the procedure (and the farmers<br />
adept at carrying it out) and it causes minimal disruption of management.<br />
Heavy magnesium 'bullets'<br />
The use of heavy 'bullets' of magnesium to prevent hypomagnesemia has been effective in<br />
laboratory trials and they are available commercially in some countries. The objective is to place a<br />
heavy 'bullet' of magnesium in the reticulum from which site it constantly liberates small amounts<br />
of magnesium - about 1 g/d. This objective is achieved and the occurrence of the clinical disease is<br />
usually greatly reduced but not eliminated. In dangerous situations, it is customary to administer<br />
up to four bullets at a time. As with all bullets, there is a proportion lost by regurgitation and by<br />
passage through the gut. A special sheep-sized 'bullet' is used in ewes with similar results.<br />
Top dressing of pasture<br />
This, together with magnesium-rich fertilizers, raises the level of magnesium in the pasture and<br />
decreases the susceptibility of cattle to hypomagnesemia. For top dressing, calcined magnesite<br />
(1125 kg/ha) or magnesic limestone (5600 kg/ha) are satisfactory, the former resulting in a greater<br />
increase in pasture magnesium.<br />
Other magnesium-containing fertilizers can be used depending on cost. The duration of the<br />
improved magnesium status varies with the type of soil: greatest on light sandy loams on which a<br />
dressing of 560 kg/ha of calcined magnesium can provide protection for 3 years. On heavy soils<br />
protection for only 1 year is to be expected. To avoid unnecessary expense, it may be possible to<br />
top dress one field with the magnesium fertilizer and keep this field in reserve for spring grazing.<br />
Fertilization with magnesium is expensive and the response of pastures varies markedly with the<br />
soil type. It is advisable to seek agronomic advice.<br />
Foliar dusting and spraying<br />
The magnesium content of pastures can be raised much more quickly by spraying with a 2%<br />
solution of magnesium sulfate at fortnightly intervals or by application of very finely ground<br />
magnesium oxide to the pasture (30 kg/ha) before grazing commences. The technique is referred<br />
to as 'foliar dusting or spraying' and has the advantage over feed supplementation that the intake is<br />
standard. It is very effective in cattle in maintaining serum magnesium levels and preventing the<br />
occurrence of the clinical disease.<br />
Dusting is with 20-50 kg MgO/ha can provide protection for up to 3 weeks but the duration is<br />
adversely influenced by wind and rain. A MgO-bentonite-water slurry sprayed onto pastures (26<br />
kg MgO and 2.6 kg bentonite/ha) is effective in providing protection in high rainfall periods.<br />
Provision in drinking water<br />
The problem with water medication is that the water intake of the group to be treated is not known<br />
but may be minimal on rapidly growing pastures. However, water medication may provide a<br />
delivery system for magnesium on management systems such as extensive range pastures where<br />
other methods may have limited success. Water sources other than the medicated supply need to<br />
be fenced off or otherwise restricted. The addition of magnesium sulfate (500 g/100 L) or<br />
mag¬nesium chloride hexahydrate (420 g/ 100 L) to the water supply during the risk period for<br />
hypomagnesemia has proved effective.<br />
Management of pasture fields<br />
The economics of daily farming make it necessary to produce maximum pasture growth, and the<br />
development of tetanyprone pastures is unavoidable in many circumstances. In some areas it may<br />
be possible to reduce the danger of such pastures by encouraging the development of legumes. In<br />
173
other areas the period of legume growth does not coincide with the period of maximum risk for<br />
grass tetany.<br />
Restricting the amount of potash added to pastures, especially in the period immediately<br />
preceding the risk period for tetany, or using potash fertilizers m the autumn or late spring after<br />
the period of risk, can reduce risk of the disease. The grazing of low-risk animals on high-risk<br />
pastures is another strategy. Insuring that ample salt is available during the danger period to<br />
counteract the high intake of potassium can also reduce risk of the disease.<br />
Plant geneticists are developing cultivars of cool-season grasses with high magnesium content<br />
that could be used for grazing during the tetany season. Lactating sheep grazing a high<br />
magnesium cultivar of perennial rye grass (Lolium perenne cv Radmore) in the spring have<br />
shown higher blood magnesium concentrations than sheep grazing control cultivar (30).<br />
Provision of shelter<br />
In areas where winter pasturing is practiced, the observation that serum magnesium levels fall<br />
during the winter and in association with inclement weather suggests that cattle and sheep should<br />
be provided with shelter at such times. If complete housing is impractical, it may be advisable to<br />
erect open access shelters in those fields that have no tree cover or protection from prevailing<br />
winds. Fields in which lactating cows are kept should receive special attention in this regard.<br />
Unfortunately, the disease is most common on highly improved farms, where most natural shelter<br />
has been removed and it is desired to keep the cows on the highly improved pasture to maintain<br />
milk production or fatten calves rapidly.<br />
Time of calving<br />
In areas where the incidence of the disease is high, it may be advisable to avoid having the cows<br />
calve during the cold winter months when seasonal hypomagnesemia is most likely to develop.<br />
Unfortunately it is often important to have cows calve in late winter to take advantage of the flush<br />
of spring growth when the cows are at the peak of their lactation.<br />
Feeding on hay and unimproved pasture<br />
Because of the probable importance of lush, improved, grass pasture in producing the disease, the<br />
provision of some gram, hay or rough grazing may reduce its incidence. It is most important that<br />
the periods of fasting, such as occur when cattle or sheep are yarded or moved or during bad<br />
weather, should be avoided, especially in lactating animals and when seasonal hypomagnesemia is<br />
likely to be present.<br />
REVIEW LITERATURE<br />
Rendig, V. V. &; Grimes, I). L. (1979) Grass tetany. Special Publication No., 35, American<br />
Society of Agronomy, Wisconsin, USA.<br />
Rohcrson, D. L., Koppel, L. C. & BolingJ. A. (1989) Management practices to overcome the<br />
incidence of grass tetany. J. Anim. Sd., 67, 3470-3484.<br />
Rogers, P. A. M. (1979) Hypomagnesemia and its clinical syndromes in cattle: a review. Irish<br />
Vet. J., 35, 115.<br />
Littledike, E. T , Young, J. W. & Beitz, D. C. (1981) Common metabolic diseases of cattle:<br />
ketosis, milk fever, grass tetany, and the downer cow complex.J. Dairy Sci., 64, 1465-1482.<br />
Fontenot,J. P., Allen, V. G., Bence, G. E. & Goff, J. P. (1989) Factors influencing magnesium<br />
absorption and metabolism in ruminants. J. Anim. Sci., 67, 3445 3455.<br />
Hoffsis, G. E., Saint-Jean. G. & Rings, D. M. (1989) Hypomagnesemia in ruminants. Comp.<br />
Com. F.iluc. Pract. Vet., 11(4), 519-526.<br />
174
McCaughan, C.J. (1992) Treatment of mineral disorders in cattle. Vet. Clitt. North Am.: Food<br />
Anim. Pract., 8(1), 107-145.<br />
Dua, K. & Care, A. D.(1995) Impaired absorption of magnesium in the aetiology of grass tetany.<br />
Br. Vet.J., 151, 413-426.<br />
REFERENCES<br />
(1)Ritter, R.J. (1984)J. Anim. Sci., 59, 197.<br />
(2)Robson, A. IS. et al. (1997) Br. J. Nutril.,78, 975.<br />
(3)Mann, G. E. & 1.miming, G. E. (1995) Br.Vet.J., 151,427.<br />
(4) D.illey, D. E. et al. (1997) J. Agric. Sci., 129, 99.<br />
(5)FontenotJ. R. et al. (1989)J. Anim. Sci.,67, 3445.<br />
(6)Schnieder, K. M. et al. (1985) Aim. Vet. J.,62, 82.<br />
(7)Giduch, S. P. et al. (1988) J. Abum. Sci.,66,532.<br />
(8)Robinson,D. L. et al. (1989)J Anim. Sci.,67.3470.<br />
(9)Wilkerson, S. R. et al. (1987) Magnesium,6, 74.<br />
(10) Van, de Uraak. A. E. et al. (1986) Res. Vet.Sd, 42, 101.<br />
(11) Van, Mosel, M. et al. (1990) Res. Vet. Sci.,48. 280.<br />
(12)McCaughan. C.J. (1992) Vet. Clin. North Am.: Food Anim. Pract., 8(1), 107.<br />
(13)Morns, C. A. (1994) NZ. J. Agric. Res.37, 59.<br />
(14)Greene, 1.. W. et al. (1989)J. Anim. Sci.,67, 3463.<br />
(15)Erb, 11. N. & Grohn, V. T. (1988) J. Limy Sci., 71, 2557.<br />
(16)McCoy, M. A. et al. (1996) Vet. Rec, 158,41.<br />
(17)Menzies, F. D. et al. (1995) Vet. Rcc. 157,531.<br />
(18)Cheyney, D.J. R. & Robinson, D. L.<br />
(1985) Argon.J, 77, 827.<br />
(19) Mayland, H. F. & Wilkerson, S. R. (1989)J. Anim. Sa., 67, 3437.<br />
(20) Feyter, C. et al. (1986) NZ. J. Exp. Agric,14. 183.<br />
(21)Meyer. 11. (1977) Vet. Sci. Commum., I. 43.<br />
(22)Anonymous (1984) Surveillance,11(1), 5.<br />
(23)Caple, I. W. & 1 lalpin, C. G. (1985) Sydney Pert Grai. Course Dairy Production,76, 307.<br />
(24)Lincoln, S. D. & Lane, V. M. (1985) Am.J Vet. Res , 46. 160.<br />
(25)Allsop, T. F. & I'.iuh, J. V. (1985) Res. Vet Sd . 38, 61.<br />
(26)Sutherland. R.J. et al. (1986) NZ vet.J,54. 133.<br />
(27)Whitaker, D. A. et al. (1986) Vet. Rec.118, 570.<br />
(28)Bacon, J. A. et al. (1990)J. Dairy Sci.. 75,470.<br />
(29)Davenport. G. M. et al. (1990) J. Anim.Sd., 68, 3765.<br />
(30) Binnie, R. C. ct al. (1996) Crass Forage Sci., 51, 456.<br />
(二)犊牛低镁血症(Hypomagnesemia of Calves)<br />
犊牛血液中镁离子浓度下降,可出现临床低镁性搐搦 tetany 症。临床上表现为强直或阵<br />
发性痉挛,缺氧,甚至死亡。2~6 个月龄的犊牛可发生该病,2~4 月龄发病最多。<br />
长期用乳饲喂,乳中镁离子不能满足机体的需要,特别是体重 50kg以上时,如不给代<br />
乳品中添加镁,就可使血镁浓度下降。如伴有慢性拉稀,或消化率下降,吸收的镁更少。饲<br />
料中钙太多或磷太多,VD不足,可诱发低镁血症。<br />
早期病犊表现摇头,感觉过敏,腱挛缩,运动障碍,头后仰,角弓反张。当人接近时,<br />
眼睑跳动,对刺激过敏,但无搐搦症状。体温不高。接着肌震颤、踢腹、口吐白沫,四肢痉<br />
175
挛、惊厥、牙关紧闭、四肢强直与阵挛,尿、粪失禁。年龄稍大的犊牛,惊厥发作后 20~30min<br />
内死亡。年龄较小的,在两次发作期间有假死现象。<br />
血镁浓度通常为 0.74mmol/L 以下称为低镁血症,在 0.33mmol/L 以下出现临床低镁<br />
性搐搦症,有的甚至可降至 0.12~0.29mmol/L。血镁浓度下降的同时,血钙浓度亦下降,<br />
肌酸磷酸激酶活性升高。<br />
临床上应与破伤风相区别。VA缺乏、脑软化、脑膜脑炎等易与本病混淆,应注意区别。<br />
VA缺乏常有视力下降,神经症状明显;病毒性脑炎常有体温升高等,可区别之。<br />
应及时使用 25%硫酸镁,100ml 静脉注射,可消除症状。饲料中添加氧化镁和碳酸镁<br />
配合对症治疗,镇静、解痉。<br />
犊牛生后 10 天就应开始补充适量镁,可以防止镁过度下降。至少要补至 10 周龄,剂<br />
量是 1~5 周龄时,每天 1g 氧化镁;5~10 周龄每天 2g;10~15 周龄每天 3g。碳酸镁用量加<br />
倍。血镁浓度校正后,血钙浓度恢复正常。<br />
HYPOMAGNESEMIC TETANY OF CALVES<br />
Synopsis<br />
Etiology. Hypomagnesemia, resulting from inadequate magnesium in the diet. Epidemiology.<br />
Most commonly calves 2-4 months of age, on whole milk or milk replacer diets and poor or no<br />
roughage. Diarrhea and chewing bedding or other coarse fiber may exacerbate the deficiency.<br />
Clinical findings. Apprehension, agitation, hypersensitivity to all external stimuli, fine muscle<br />
tremors progressing to spasticity and violent convulsions. Rapid course and high case-fatality rate.<br />
Clinical pathology. Serum magnesium levels below 0.8 mg/dl, bone calcium:magnesium ratio<br />
above 90:1.<br />
Necropsy findings. Calcification of the spleen, diaphragm and endothelium of the aorta and<br />
endocardium. Enzootic muscular dystrophy is often concurrent.<br />
Diagnostic confirmation. Blood magnesium and response to treatment. Bone calcium:magnesium<br />
ratios.<br />
Treatment and control. Magnesium injection and dietary supplementation with magnesium<br />
compounds.<br />
ETIOLOGY<br />
The disease results when the dietary intake ot magnesium is inadequate for the requirements of the<br />
calf. Affected animals may have concurrent hypocalcemia.<br />
Magnesium homeostasis in the calf<br />
Milk has low concentrations ot magnesium. A milk diet provides adequate magnesium for the<br />
requirements of a growing calf up to a body weight of approximately 50 kg, but if milk is the sole<br />
diet, the intake of magnesium will be inadequate for requirements once Ins body weight is reached<br />
(1). The deficit will perpetuate if the other feeds that are fed are also low in magnesium.<br />
In the young calf, magnesium is absorbed in the intestine; however, the efficiency of<br />
magnesium absorption decreases markedly up to about 3 months of age, when maximum<br />
susceptibility to the disease occurs. The efficiency of absorption is decreased by a reduction in<br />
transit time in the intestine caused by diarrhea.<br />
In contrast to adult cattle,young calves can mobilize body stores of magnesium, which are<br />
principally located in the skeleton. Approximately 40% of the magnesium stored in the skeleton<br />
can be mobilized, which will protect against a short-term deficit (1).<br />
Hypomagnesemic tetany in calves is often complicated in field cases by the coexistence of other<br />
176
diseases, especially enzootic muscular dystrophy.<br />
EPIDEMIOLOGY<br />
Occurrence<br />
The disease is not common. Cases may occur sporadically or a number of deaths may occur on the<br />
one farm within a short period of time.<br />
Risk factors<br />
The disease can occur under a number of different circumstances.<br />
Most commonly, hypomagnesemic tetany occurs in calves 2-4 months of age or older which<br />
are fed solely on a diet of whole milk, and calves receiving the greatest quantity of milk and<br />
growing most rapidly are more likely to be affected because of their greater need for magnesium<br />
tor incorporation into developing soft tissues. It is most likely to occur in calves being fattened for<br />
veal. Those cases winch occur on milk replacer appear to be related to chronic scours and low<br />
magnesium content of the replacer. This problem is less common than it once was because most<br />
modern commercial milk replacers have added adequate magnesium.<br />
A significant loss of magnesium in the feces also occurs in calves allowed to chew fibrous<br />
material such as bedding; the chewing stimulates profuse salivation and creates greater loss of<br />
endogenous magnesium. Peat and wood shavings are bedding materials known to have this effect.<br />
Cases have also been reported in calves fed milk-replacer diets or milk, concentrates and hay,<br />
and in calves running at pasture with their clams. Deaths due to hypomagnesemic tetany have also<br />
occurred in 3-4-months-old calves whose hay and silage rations were low in magnesium content<br />
(2).<br />
Hypomagnesemia also occursin young cattle, about 6 months of age, which are being fattened<br />
intensively indoors for the baby beef market. The phosphorus content of their diet is high and a<br />
lack of vitamin D is probable. The situation is exacerbated by a shortage of roughage. The<br />
hypomagnesemia is accompanied by a hypocalcemia.<br />
Experimental reproduction<br />
A condition closely resembling the field syndrome has been produced experimentally by feeding<br />
an artificial diet with a very low content of magnesium; a high calcium content and biochemical<br />
hypomagnesemia is readily produced in calves with a diet based on skim milk and barley straw (3).<br />
Hypomagnesemia hasas also been produced experimentally in very young foals by feeding a diet<br />
with a very low magnesium content. The clinical signs are similar to those in calves, and the<br />
calcification found in the walls of vessels of calves also occurs in foals.<br />
PATHOGENESIS<br />
On affected farms, calves are born with normal serum magnesium levels of 2-2.5 mg/dL<br />
(0.82-1.03 mmol/L) but the levels fall gradually in the succeeding 2-3 months, often to below 0.8<br />
mg/dL (0.33 mmol/L). Tetany does not occur until the serum magnesium falls below this<br />
concentration and is most severe at concentrations below 0.6 mg/dL (0.25 mmol/L), although<br />
some calves in a group may have concentrations even lower than this and show few clinical signs.<br />
Magnesium deficiency inhibits the release and action of parathyroid hormone and this is<br />
believed to be the genesis of the concurrent hypocalcemia (4). It is probable that depression of the<br />
serum calcium level precipitates tetany in animals rendered tetany prone by low serum magnesium<br />
levels. Tetanic convulsions can occur in hypocalcemic calves in the absence of hypomagnesemia.<br />
Hypomagnesemic tetany is not related in any way to enzootic muscular dystrophy, although the<br />
diseases may occur concurrently.<br />
177
CLINICAL FINDINGS<br />
The first sign in the experimental disease is constant movement of the ears. The temperature is<br />
normal and the pulse rate accelerated. Hyperesthcsia to touch, and grossly exaggerated tendon<br />
reflexes with clonus, are present. Shaking of the head, opisthotonos, ataxia without circling, and a<br />
droopy, backward carriage of the ears are constant. There is difficulty in drinking due to the<br />
animal's inability to get to the bucket.<br />
Initially, the calves arc apprehensive, show agitation and retraction of the eyelids when<br />
approached, and are hypersensitive to all external stimuli but show no tetany. Later, fine muscle<br />
tremors appear, followed by kicking at the belly, frothing at the mouth and spasticity of the limbs.<br />
Convulsions follow, beginning with stamping of the feet, head retraction, champing of the jaws<br />
and falling.<br />
During the convulsions the following signs are present:<br />
•Jaws are clenched<br />
•Respiratory movements cease<br />
•There are tonic and clonic movements of the limbs<br />
•There is involuntary passage of urine and feces<br />
•There are cycles of protrusion and retraction of the eyeballs.<br />
The pulse rate rises to 200-250/min and the convulsions disappear terminally. The pulse<br />
becomes impalpable and cyanosis appears before death.<br />
In field cases the signs are almost identical but are rarely observed until the terminal tetanic<br />
stage. Older calves usually die within 20-30 min of the onset of convulsions but young calves may<br />
recover temporarily only to succumb to subsequent attacks. Cases which occur in young calves<br />
with scours, usually at about 2-4 weeks of age, show ataxia. hyperesthesia, opisthotonos and<br />
convulsions as the presenting signs (5). The convulsion is usually continuous and the calves die<br />
within 1 h.<br />
CLINICAL PATHOLOGY<br />
Serum magnesium levels below 0.8 mg/dL (0.33 mmol/L) indicate severe hypomagnesemia and<br />
clinical signs occur with levels of 0.3-0.7 mg/dL (0.12-0.20 mmol/L). Normal values are 2.2-2.7<br />
mg/dL (0.9-1.1 1 mmol/L). Erythrocyte magnesium concentrations are also low. indicating a<br />
chronic deficiency. Serum calcium levels tend to fall when serum magnesium levels become very<br />
low and are below normalin most clinical cases.<br />
The estimation of the magnesium in bone (particularly ribs and vertebrae) is a reliable<br />
confirmatory test at necropsy. Values below a ratio of 70:1 for calcium: magnesium may be<br />
regarded as normal and above 90:1 are indicative of severe magnesium depletion. In the normal<br />
calf the ratio is about 55:1. Absolute bone calcium values are not decreased and ar often slightly<br />
elevated. An incident; change is the marked increase in serur creatinme phosphokinase levels<br />
observe in calves after an acute attack of hypomagnesemic tetany.<br />
NECROPSY FINDINGS<br />
There is a marked difference between th necropsy lesions of some natural cases and those m the<br />
experimental disease. In field cases, there is often calcification of the spleen and diaphragm, and<br />
calcifiei plaques are present in the aorta and endo cardium, together with hyaline degeneration and<br />
musculature. In other case necropsy lesions similar to those ii enzootic muscular dystrophy occur.<br />
In experimentally produced case these lesions are not evident but there extensive congestion in<br />
all organs, and hemorrhages in unsupported organs including the:<br />
178
•Gallbladder<br />
•Ventricular epicardium<br />
•Pencardiium fat<br />
•Aorta<br />
•Mesentery wall<br />
•Intestinal wall.<br />
The lesions are obviously terminal and are associated with a terminal venous necrosis. Some field<br />
cases present a picture identical to this.<br />
DIFFERENTIAL DIAGNOSIS<br />
•Acute lead poisoning<br />
•Enterotoxemia caused by Closthdium perfringens Type D<br />
•Polioencephalomalacia<br />
•Tetanus<br />
•Vitamin A deficiency<br />
•Meningitis.<br />
TREATMENT<br />
Response to magnesium injections (100 mL of a 10% solution of magnesium sulfate) is only<br />
transitory because of the severe depletion of bone reserves of magnesium. This dose provides only<br />
a single day's requirements. Follow-up supplementation of the diet with magnesium oxide or<br />
carbonate as described later is advisable. Chloral narcosis or tranquilization with an ataractic drug<br />
may be essential to avoid death due to respiratory paralysis during convulsions.<br />
CONTROL<br />
The provision of a hay that is high in magnesium, such as alfalfa, helps to prevent the disease as<br />
will well-formulated concentrates.<br />
Supplementary feeding of magnesium<br />
If begun during the first 10 days of life, supplementary magnesium feeding will prevent excessive<br />
falls of serum magnesium, but if begun after the calf is 7 weeks old, may not prevent further<br />
depression of the levels. Supplementation should continue until at least 10 weeks of age. Daily<br />
feeding of the magnesium compound and fairly accurate dosing are necessary to avoid scouring or<br />
inefficient protection. For calves of average growth rate appropriate close rates are 1 g/d for calves<br />
to 5 weeks of age, 2 g/d for calves 5 10 weeks of age and 3 g/d for calves 10 15 weeks of age of<br />
magnesium oxide or twice this dose of carbonate. Supplementation of the diet with magnesium<br />
restores serum calcium levels to normal as well as correcting the hypomagnesemia.<br />
Magnesium alloy bullets<br />
Two bullets of the sheep size (together releasing approximately 1 g/d of magnesium) per calf,<br />
have shown high efficiency in preventing the clinical disease and also the hypomagnesemia which<br />
precedes it. Calves kept indoors and fed largely on milk should get adequate mineral supplement<br />
and vitamin D (70 000 in vitamin D3/d). Magnesium utilization will not be affected but calcium<br />
absorption, which is often sufficiently reduced to cause a concurrent hypocalcemia, will be<br />
improved.<br />
REFERENCES<br />
(1)Sansom, B. F. (1981) Vet. Ann., 21, 74.<br />
(2)Rayssiguier, P.J. et al. (1977) Vet. Sii.<br />
Commun., 1, 235.<br />
179
(3)Mulci, C. M & Daniels, R. C. W. (1989)J<br />
Vet. Med., 36, 783.<br />
(4)Schnieder, K. M. et al. (1985) Ami. Vet.J.,<br />
62, 82.<br />
(5)Mills, J. (1992) Vet. Rec, 131,60.<br />
三、低钾血症(Hypokalemia)<br />
动物因钾摄入不足,或从汗、尿、粪中钾丢失太多,引起血清钾浓度下降,全身骨骼肌<br />
松弛,异嗜,生产能力下降的现象称为低钾血症。<br />
兽医临床上原发性低钾血症是很少的。它多继发于生产瘫痪、肠阻塞、顽固性前胃或真<br />
胃疾病,造成长时间停食或因大出汗、呕吐、腹泻情况下的单纯补液之后,有些母牛产后的<br />
“卧倒爬不起来综合征”,对钙剂治疗反应甚差,补钙的同时补钾效果明显。<br />
【病因与病理】 动物,尤其是反刍动物一般不存在缺钾现象。因为植物性饲料中钾含<br />
量是丰富的,大多数谷物中含钾在 0.5%以上,牧草中钾含量多在 1%以上,有的甚至达 2<br />
%~3%(干物质计)。绵羊饲料钾的含量在 0.7%以上,肉用牛有 0.6%~0.8%以上,乳牛为<br />
0.8%~1.0%(约 30g 钾),就可防止缺钾。而在生长良好的草地上放牧的牛,每天可从饲料<br />
中摄入约 500g 钾。以食草和青贮料为主的动物,不致于缺乏钾。但是现代畜牧生产中,尤<br />
其是对高产乳牛、肉牛的育肥期,多以大量精料取代粗纤维,以提高他们的生产能力,因而<br />
有可能使动物钾摄入减少。<br />
此外,当动物遇有顽固性前胃弛缓,瘤胃积食,真胃积食等疾病时,由于大量的液体移<br />
向消化道,使血液中K + 转移到胃肠液中,继而被排泄。或当大量胃酸分泌入真胃内,H + 和<br />
Cl –<br />
转移入胃,造成代谢性碱中毒,肾脏为了保H + ,则以排K + 代之。此时不仅有低钾血症,<br />
同时会有低氯血症。<br />
当动物呕吐、腹泻,或从事重役、激烈奔跑等引起大出汗,体内失水过多,给动物补钠<br />
的同时未补钾,造成血液中钾浓度下降。长期便秘,停食,动物不能从食物中补充钾,但仍<br />
要从尿液向外排泄钾,因而造成体内钾消耗过多,血钾浓度下降。<br />
生产瘫痪牛,由于血钙浓度下降,长时间躺卧,造成局部肌肉缺血性损伤,增加了肌细<br />
胞膜的通透性。肌细胞内钾离子流向细胞外。临床测定表明,当母牛卧倒爬不起来达 6h,<br />
血钾降为 4mmol/L,卧倒爬不起来达 16h,血钾降为 2~3mmol/L,细胞内钾离子浓度也<br />
下降。正因细胞内钾离子浓度下降,肌纤维松弛。随着躺卧时间延长,血钾浓度下降增多,<br />
肌肉松弛现象也愈重。<br />
【临床表现】 患病动物最明显的表现是卧地爬不起来,肌肉松软无力,侧卧在地。时<br />
间长的甚至有褥疮现象。但病牛神志清醒,饮欲、食欲可随原发病不同而不同。有的病牛,<br />
饮、食欲尚存,但有些病牛则停食停饮。<br />
实验性低钾血症是用含 0.06%的钾的饲料饲喂健康牛犊引起的,经 3~4 周后,动物表现<br />
食欲下降,体增重几乎停止,异嗜,如舔毛、啃咬木质栅栏,憔悴无神,后期虚弱,驱赶时,<br />
后躯摇晃,步样不协调,血钾浓度从 5.0mmol/L 降为 3.7mmol/L。血清磷浓度明显升高,<br />
泌乳牛缺钾时,乳产量直线下降。乳中钾离子浓度也明显下降,钠离子浓度相对升高。<br />
羔羊缺钾时表现采食减少,日渐消瘦,血球比容增多,全血钾浓度下降,红细胞内钠离<br />
子浓度增加,钙离子浓度下降,用含 0.1%的钾的饲料喂羔羊 10 天,就可呈现血钾浓度下降。<br />
异食、啃咬、甚至拉自己身上的毛的现象。<br />
猫、狗因呕吐、腹泻、酸中毒、胃肠弛缓;或因肾脏本身的疾病,如慢性化脓性肾炎、<br />
急性肾小管坏死引起的尿崩;及内分泌方面的障碍,如醛固酮分泌过多,垂体性嗜碱性细胞<br />
增多症等,也可导致低钾血症。患病猫、狗除有原发性病本身的各种症状外,还呈现虚弱、<br />
180
躺卧、血钾浓度明显下降等。<br />
【防治】 防治低钾血症的原则是首先治疗原发病,同时注意给动物补充钾。只要动物<br />
可以喝水,可在饮水中掺入氯化钾。口服钾的毒性作用很小,饮水中氯化钾浓度为 1%~2%,<br />
每次 200~250g;亦可静脉注射氯化钾,但静脉注射高钾溶液必须慎重,10%氯化钾 50~100ml,<br />
慢速滴注,当心功能衰竭时,切勿注射氯化钾。以免心脏骤停于心舒张状态,引起突然死亡。<br />
治疗中应加强护理,经常给动物翻身,增加垫草,防止褥疮生成,使病情恶化。<br />
ACUTE HYPOKALEMIA IN CATTLE<br />
Hypokalemia in cattle may occur secondary to:<br />
•Anorexia<br />
•Diarrhea<br />
•Upper gastrointestinal obstruction<br />
•Right-sided displacement and torsion of the abomasum<br />
•Impaction of the abomasum.<br />
In most cases, the hypokalemia is not severe enough to cause weakness and recumbency.<br />
hypokalemia resulting in severe weakness and recumbency has occurred in dairy cattle treated<br />
with isoflupredone acetate for ketosis (I). Serum potassium levels were below 2.3 mEq. Cows<br />
ranged in age from 2-7 years, all had a history of moderate to severe ketosis and had calved within<br />
the previous 30 d. Most had been also treated with insulin, IV glucose, and oral propylene glycol.<br />
Affected cows were recumbent, profoundly weak, appeared flaccid and lay in sternal or lateral<br />
recumbency. They were unable to support the weight of their heads off the ground and they were<br />
commonly held in their flanks. Anorexia was common. Cardiac arrhythmias were detectable on<br />
auscultation and atrial fibrillation was confirmed on electrocardiography. Treatment included IV<br />
and oral administration of potassium chloride and fluid therapy but the response was ineffective.<br />
Most affected cattle died or were euthanized. At necropsy, muscle necrosis was present in the<br />
pelvic limbs and histological examination of non-weight bearing muscle revealed multifocal<br />
myonecrosis with microphage infiltration and myofiber vacuolation, which is characteristic of<br />
hypokalemic myopathy in man and dogs. It is important to note that myopathy was also present in<br />
muscles not subject to ischemia of recumbency.<br />
Potassium excretion by the kidneys is via secretion by the distal tubular cells. Aldosterone or other<br />
steroids with mineralocorticoid activity enhance distal tubular secretion of potassium by<br />
increasing permeability of the tubular luminal membranes to potassium and increasing losses of<br />
potassium in the urine. Glucocorticoids are often used to treat ketosis and the most commonly<br />
used are dexamethasone and isoflupredone acetate. Dexamethasone has little niineralocorticoid<br />
activity compared to prednisone and prednisolone, which arc related chemically to isoflupredone.<br />
Dexamethasone is recommended for the treatment of ketosis in dairy cattle at a single dose of<br />
10-20 mg IM, and repeated if necessary, 12-24h later. Field observations indicate that repeated<br />
doses of isoflupredone acetate decrease plasma concentrations of potassium by 70-80%, which<br />
suggests a strong niineralocorticoid activity. It is recommended that isoflupredone be used<br />
judiciously and animals be monitored tor plasma potassium and any evidence of weakness and<br />
recumbency. Treatment with oral potassium choride may be required but treatment may be<br />
ineffective.<br />
REFERENCE<br />
(1) Sielman, P.. S. ei a). (1997)J Am. Vet. Med. Assoc, 210, 240.<br />
181
四、钠营养紊乱性疾病(Nutritional Disorder of Sodium)<br />
(一)钠缺乏症(Sodium Deficiency)<br />
动物因钠摄入不足或因钠排泄太多,造成血钠浓度下降。临床上表现异食、脱水、肌肉<br />
虚弱,精神抑郁等特征,但许多情况下,没有特征性表现。<br />
动物中低钠血症远比低钾血症多,可发生于牛、羊、猪、禽,特别是野生动物,如野鹿、<br />
羊、野兔等。<br />
【病因】 食草动物饲料中钾含量丰富,但钠含量仅有 0.01%~0.05%,谷物中钠含量<br />
仅 0.01%~0.06%,每天从草中仅能获得 0.2~1.0g 钠,用 50%粗料饲喂时,小牛需盐 31g,<br />
每天泌 20kg 乳的牛需盐 30g 以上,因此必须给食草动物补盐。用钾肥施草地,限制了植物<br />
对钠的摄取,促使动物缺钠。<br />
以玉米、大豆为主食的猪饲料中通常含 0.08%~0.1%的钠,显然也不能满足猪生长需要,<br />
猪的日粮中应含 0.25%的钠盐,甚至 0.5%的盐也不过多。鸡的饲料中应含 0.31%的盐,而<br />
天然饲料中仅含 0.1%的盐,产蛋鸡饲料中应含 0.35%的盐,成年火鸡饲料中应含 0.4%的盐。<br />
兔饲料中应含 0.4%~0.5%盐,可见,天然饲料中钠含量远不能满足猪、禽、兔生长、繁殖、<br />
产蛋的需要,必须额外补充盐。<br />
食肉动物中,肉、骨中钠含量较多,一般在 0.1%~0.8%之间。狗、猫食物中钠含量是:<br />
幼畜,0.53%;成年动物,0.37%,亦有报告称猫、狗食物中盐含量应为 0.5%~1.0%,因此,<br />
全部以肉食饲喂,不补充盐亦可,但当以米饭、面条、夹杂骨、肉饲喂时,亦应添加盐。<br />
有些野生动物靠舔食泥土、岩石、山洞渗水获得盐,有的甚至经“盐道”,不顾冒生命<br />
危险去盐湖、海边获得盐。如野鹿、野兔、黄羊等。<br />
盐排泄太多,也是低钠血症重要原因。夏天劳役、大出汗、大面积烧伤、剧烈呕吐或腹<br />
泻,尤其是新生畜腹泻,常导致体内钠丢失,给动物补液时,单纯使用 5%葡萄糖而忽视了<br />
对钠的补充或补充不足等都可造成低钠血症。便秘时由于动物停食,每天从肠道内吸收的钠<br />
不能弥补尿液中钠的排泄,则可能引起动物缺钠。醛同酮分泌不足,可能导致大量钠从尿液<br />
中丢失。<br />
当动物钠摄入不足,同时又伴有钠排泄过多,则可迅速导致低钠血症。<br />
【病理】 钠是细胞外液中主要电解质,也是构成细胞外液渗透压的主要物质成分,当<br />
血钠浓度下降,导致排尿增多,以便维持渗透压恒定,结果出现机体内失水,细胞外液丢失,<br />
循环血量减少,外周循环衰竭,肌肉虚弱,体温下降等一系列临床症状。<br />
肠道内对钠的吸收是充分的,几乎进入机体内的可溶性钠都可被吸收,但只要饮水充分,<br />
过多的钠可以迅速排泄。<br />
动物有很强的调节钠代谢的功能,当血钠下降时,醛固酮分泌而使钠排泄减少,或者借<br />
乳产量减少或延缓生长速度而维持细胞外液中钠的恒定。但如缺钠过多,靠有限的调节作用,<br />
不能根本改善和维持体液中渗透压时,动物出现强烈的嗜盐欲,表现互相舔食被毛、粪尿、<br />
饲养员衣物、手、鞋等一切可能含盐的东西,并出现异食癖。<br />
【临床表现】 牛缺盐早期,动物互相舔毛(汗中盐可达 4%)、舔食粪尿,2 个月后发<br />
展为异食癖,喜食被尿液浸渍的饲草,舔食泥土和栅栏,10~11 个月后体重下降,采食量减<br />
少,最终厌食,被毛粗乱,皮肤干燥,乳产量下降,乳脂含量降低,有的甚至搐搦,不安,<br />
步样强拘,后肢尤为明显,有的牛甚至虚脱和死亡。<br />
病牛心率不整,血钠浓度仅略有下降,从 145mmol/L 降为 125mmol/L,肾上腺肥大,<br />
唾液钠与钾的含量比,通常为 20(140/7),缺钠时这一比值可降为 10~15:1 甚至 1:1 或 0.5:1。<br />
有试验表明,乳牛每天摄入 3.2~5.5g 钠时,在泌乳头 7 周内乳产量能基本正常,体内钠贮可<br />
耗损 190g,然后乳产量可迅速下降,以缓解体内钠的负平衡。尽管体内缺钠,尿钠减少,<br />
而乳中钠仍与血浆内钠浓度相等,血浆总容量下降,血球比容增加,血清氯离子浓度也从<br />
182
100mmol/L 降至 90mmol/L,高产乳牛产犊后不久严重缺钠可致牛突然倒地,虚脱死亡。<br />
亚临床缺钠可致乳产量下降,乳脂含量减少。分娩前缺钠,乳腺发育障碍,胎衣滞留等。<br />
绵羊、山羊对低钠饲料较能耐受,但唾液中钠离子浓度可从 173mmol/L 降至 38mmol<br />
/L,钾离子可从 5mmol/L 升高到 96mol/L。只要饲料中补充盐以后,唾液中 Na:K 可迅<br />
速恢复正常。<br />
生长猪、家禽缺钠时,几周内可表现食欲下降,生长阻滞,饲料消耗减少,饲料报酬下<br />
降,饮水增加。低盐日粮下,产蛋母鸡体重下降,有食蛋癖,蛋白体积变小,有的鸡群产蛋<br />
量降低 60%甚至降低 80%。尽管如此,血钠浓度尚能维持在正常范围内。动物有能力借减<br />
少钠向尿、蛋中排泄而维持血浆钠浓度的恒定。为了维持渗透压,当血浆钠浓度下降时,血<br />
浆钾浓度升高,这是危险的,因血钾浓度过高,可抑制心功能,甚至在某些应激因素下猝死。<br />
【诊断】 嗜盐是最明显、最典型的特点,如舔被毛、衣物、粪尿等一切可能沾盐的用<br />
物。但此现象应与缺磷或缺乏其它矿物质引起的异食癖相区别。同时,各个个体需盐量也不<br />
一样。血浆钠离子浓度对诊断价值不大,但唾液中钠、钾浓度及其比率的变化有重要诊断意<br />
义。<br />
【防治】 动物饲料中应补充盐,鸡饲料中盐含量应为 0.3%~0.4%,猪饲料中应含盐<br />
0.35%~0.5%,如果饲料中鱼粉含量高,可减至建议量的一半。泌乳奶牛精料中应含 0.38%<br />
的盐。草场收牧的奶牛,应在草场内放置盐砖。<br />
使用深井水作饮水,对防止缺盐有一定价值。但牛每天饮水量个体间有很大差异,通常<br />
情况下,按每头每天饮 40L 水计。饮水中含盐为 0.05%,则获得 20g 盐,应能满足牛对钠<br />
的需要,即使饮用水中含 0.5%的盐,对牛仍是安全的。含 0.7%的盐,对泌乳牛和绵羊也是<br />
安全的。饮水量与气温间关系密切,夏季饮水多,盐的浓度略低些,冬季饮水少,盐的浓度<br />
可高些。<br />
尽管猪的饮水中含 1%的盐,只要有足够饮水,仍可耐受,但应以 0.05%为宜。鸡饮水<br />
中以 0.1%的盐,可达到补盐的目的。饮水充足时,即使食盐过多,动物可把过多盐排泄掉。<br />
不致引起中毒。<br />
如饲料中已供给足够的盐,则不必在饮水中另补充盐、重碳酸钠、丙酸钠、磷酸氢二钠<br />
等,都可达到补充钠离子的目的,因而在缓解酸中毒或补充无机磷的同时,也补充了钠。<br />
SODIUM CHLORIDE DEFICIENCY<br />
A dietary deficiency of sodium is most likely to occur:<br />
•During lactation, as a consequence of losses of the element in the milk, in rapidly growing young<br />
animals fed on low-sodium, cereal-based diets<br />
•Under very hot environmental conditions where large losses of water and sodium occur in the<br />
sweat and where the grass forage and the seeds may be low in sodium<br />
•In animals engaged in heavy or intense physical work and in animals grazing pastures on sandy<br />
soils heavily fertilized with potash, which depresses forage sodium levels (1).<br />
Naturally occurring salt deficiency causing illness in grazing animals is uncommon except<br />
under certain circumstances. The most commonly cited occurrences are on alpine pastures and<br />
heavily fertilized pasture leys. Pasture should contain at least 0.15g/100g dry matter (DM) and<br />
clinical signs are evident after about 1 month on pasture containing 0.1 g/100g DM. Under<br />
experimental conditions, lactating cows give less milk until the chloride deficiency is<br />
compensated. After a period of up to 12 months there is considerable deterioration in the animal's<br />
health and anorexia, a haggard appearance, lusterless eyes, rough coat and a rapid decline in body<br />
weight occur. high-producing animals are most severely affected and some may collapse and die.<br />
The oral administration of sodium chloride is both preventive and rapidly curative. Experimental<br />
183
sodium depletion in horses for up to 27 days has no deleterious effect on general health.<br />
In dairy cattle on a sodium-deficient diet there is polyuria, polydipsia, salt hunger, pica,<br />
including licking dirt . and each other's coats, drinking urine, loss of appetite and weight, and a fall<br />
in milk production (2). Urination is frequent and the urine has a lower than normal specific gravity<br />
and the urine concentrations of sodium and chloride are decreased and the potassium increased.<br />
The salivary concentration of sodium is markedly decreased, the potassium is increased and the<br />
salivary sodium:potassium ratio is decreased. The concentration of serum sodium and chloride are<br />
also decreased, but the measurement of urinary or salivary sodium concentration is a more<br />
sensitive index of sodium intake than plasma sodium concentration (2). Of these, it is urinary<br />
sodium which is depressed first and is therefore the preferred indicator in cattle (3) and horses (4).<br />
The polyuria associated with severe sodium depletion may be an antidiuretic hormone<br />
insensitivity due to lack of an effective countercurrent mechanism and hyperaldosteronism (2).<br />
Experimental restriction of chloride in the diet of dairy cows in early lactation results in a<br />
depraved appetite, lethargy, reduced feed intake, reduced milk production, scant feces, gradual<br />
emaciation, and severe hypochloremia and secondary hypokalemic metabolic alkalosis (5).<br />
Lethargy, weakness, and unsteadiness occur after about 6 weeks on the chloride-deficient diet (6).<br />
Bradycardia is also common. The concentration of chloride in cerebrospinal fluid is usually<br />
maintained near normal while the scrum concentrations decline (7). The experimental induction of<br />
a severe, total body chloride deficit by the provision of a low-chloride diet and the daily removal<br />
of abomasal contents results in similar clinical findings to those described above and lesions of<br />
nephrocalcinosis (8).<br />
The diagnosis of salt deficiency is dependent on the clinical findings, analysis of the feed and<br />
water supplies, serum levels of sodium and chlorine, and determination of the levels of sodium in<br />
the saliva, urine and feces of deficient animals (9). The concentration of sodium in saliva is a<br />
sensitive indicator of sodium deficiency. In cattle receiving an adequate supply of sodium and<br />
chlorine, the sodium levels in saliva vary from 140 to 150 mmol/L, in deficient cattle the levels<br />
may be as low as 70-100 mmol/L (9). The levels of sodium in the urine are low, with a reciprocal<br />
rise in potassium (4). The serum sodium levels are less reliable, but licking begins when the level<br />
falls to 137 mmol/L and signs are intense at 135 mmol/L.<br />
Experimentally induced sodium deficiency in young pigs causes anorexia, reduced water<br />
intake and reduced weight gains (10).<br />
The provision of salt in the diet at a level of 0.5% is considered to be fully adequate for all farm<br />
animal species. Under practical conditions, salt mixes usually contain added iodine and cobalt. In<br />
some situations the salt mixes are provided on an ad libitum basis rather than adding them to the<br />
diet. However, voluntary consumption is not entirely reliable. The daily amount consumed by<br />
animals having unrestricted access to salt can be highly variable and often wasteful. Two factors<br />
influencing voluntary salt intake include the physical form of the salt and the salt content of the<br />
water and feed supplies. Some cattle consume much more loose than block salt, though the lower<br />
intakes of block salt may be adequate. Also, animals dependent on high saline water for drinking<br />
consume significantly less salt than when drinking non-saline water. Voluntary salt consumption is<br />
generally high in cows on low-sodium pastures, which are low inherently or as a result of heavy<br />
potash fertilization. Lactating gilts may require 0.7% salt in their diets (11) and energy efficiency<br />
in feedlot cattle may be improved by feeding high levels (5% of diet) of salt in the diet of finishing<br />
steers (12).<br />
184
REVIEW LITERATURE<br />
Aitkcn, F. C. (1976) Sodium and potassium in nutrition of mammals. Commw. Bur. Anim.<br />
Nutr. Techn. Commun., 26. Michel], A. R. (1985) Sodium in health and disease: a comparative<br />
review with emphasis on herbivores. Vet. Rec, 116, 653 657.<br />
REFERENCES<br />
(1)Underwood, E.J. (1981) The Mineral Nutrition of Livestock, 2nd edn. Farnham Royal,<br />
Commonwealth AgriculturaI3ureaux.<br />
(2)Whitloik, R. H. etal. (1975) Cornell Vet..65, 512.<br />
(3)Launer, P. & Storm, R. (1979) Mh. Vet.Med., 34, 364.<br />
(4) Meyer, H. & Ahlswede, L. (1979) Zentralbl. Veterinarmed., 26A, 212.<br />
(5)Fettman, M. J. et al. (1984)/. Dairy So.,61, 2321.<br />
(6)Fettman, M.J. etal. (1984)J. Am. Vet.Med. Assoc, 185, 167.<br />
(7)Fettman, M.J. et al. (1984) Am. J. Vet.Res., 45, 403.<br />
(8)Blackmon, D. M. et al. (1984) Am.J. Vet.Res., 45, 1638.<br />
(9)Murphy, G. M. & Gartner. R. J. W.(1974) Aust. Vet.J., 50, 280.<br />
(10) Yusken.J. W. & Reber, E. F. (1957)<br />
Trans. 111. Acad. Sci., 50, 118. (1 1) Friend. D. W. & Wolynetz, M. S. (1981)<br />
Can. J.Anim. So., 61, 429. (12) Croom, W. J. et al. (1982) Can.). Anim.<br />
Sci., 62, 217.<br />
(二)钠盐中毒(Sodium Poisoning) 猪、鸡、鸭等动物因食入过量的盐,同时饮水<br />
受限制时,即可产生钠盐中毒。临床上以间隙性发生痉挛,抽搐,口吐白沫等神经症状为特<br />
征。<br />
各种动物对盐的耐受量不一样,以猪最易中毒,其次是禽、野鸟、野兽乃至大象也可发<br />
生。牛可实验性引起食盐中毒,马属动物,则很难引起食盐中毒。<br />
不仅食盐(氯化钠)可引起中毒,而且,碳酸钠、丙酸钠、乳酸钠等可引起与食盐中毒<br />
时一样的症状,因此本病定名为钠盐中毒。但因食盐后仅在饮水受限制时才发生,故又称为<br />
水剥夺性钠盐中毒(sodium salt poisoning depraved water)。<br />
【病因】 动物因一次大量采食含盐过多的饲料或盐水而造成中毒,如淹菜卤、肉卤、<br />
泡菜卤、酱渣以及食入残羹剩菜过多而引起中毒。在补饲食盐时,由于饲喂量不当或未拌匀,<br />
个别动物因食入过量盐而中毒,饮水不足在病的发生上有重要意义。据记载,只要有充足的<br />
饮水,猪日粮中食盐比例即使达 13%时,也未必产生中毒。动物发病与否与年龄、性别无<br />
关,主要与动物品种、食入盐的量及平时有无饲盐习惯和饮水是否受限制有关。平时有饲盐<br />
习惯,动物对盐的耐受量较高;如处于盐饥饿时,则耐受性较小。维生素 E 和含硫氨基酸<br />
等营养成分缺乏时,可使猪对食盐的敏感性升高。机体水盐平衡状态的稳定性,可直接影响<br />
机体对食盐的耐受性。如环境温度较高,机体大量散失水分时,可使牲畜不能耐受冬季所用<br />
的盐饲喂量。又如泌乳期高产乳牛,可比干乳期乳牛及肉牛和绵羊对盐的耐受性更高。<br />
鸡中毒可因 V 型食槽底部沉积食盐结晶,而当饥饿时食入大量槽底缝隙中盐粒而中毒。<br />
有时使用高盐米饭作为毒谷而引起鸡中毒。配合饲料中所用鱼粉或鱼干的含盐量过高,也常<br />
引起鸡中毒。小鸡由于味觉较差,加之肾小球滤过作用比哺乳动物低,血浆蛋白浓度较低,<br />
容易发生水肿,故中毒机会较多,死亡率亦较高。雏鸡饲料含盐量达 1%,成年鸡饲料含盐<br />
量达 3%,能引起大批中毒死亡。鸭子对食盐似乎更敏感。<br />
【剖检变化】 中毒猪病理变化在脑、脑膜和骨髓。这些部位可有不同程度的充血、水<br />
肿、尤其是急性病例的软脑膜和大脑实质最明显。脑回展平,表现水样光泽。组织学检查,<br />
不仅有软脑膜和大脑皮质的充血、水肿,尤其在血管周围,有多量的嗜酸性白细胞和淋巴细<br />
185
胞积聚,形成“袖套”(cuffing)。故又称嗜酸性颗粒白细胞性脑膜脑炎(eusinophilic<br />
menigoencephalitis)。这时外周血中嗜酸性白细胞消失。但病猪如能活到 3~4 天,嗜酸性白<br />
细胞就明显地离开大脑而回到循环血中去,在原占据的部位留下一个空缺的空间,并逐渐为<br />
淋巴细胞、组织细胞和增生的血管所替换。此外小静脉和微血管的内皮细胞肿大、增生,呈<br />
脑白质软化症(polioencephalomalacia)。脑灰质亦有充血和呈局灶性或弥蔓性水肿等特征。<br />
除了脑部特征外,胃有明显的炎症和溃疡。胃黏膜潮红,肿胀,出血,以致脱落。但可<br />
能无明显的变化,肺可充血,水肿,膀胱黏膜发红充血。<br />
【病理】 真正的中毒机理还不十分清楚,目前有三种学说:①水盐代谢障碍说;②钠<br />
离子中毒说;③过敏学说。<br />
水盐代谢障碍论者认为:当过量的食盐吸收入血后,血中钠离子浓度升高,通过离子扩<br />
散方式,大量钠离子通过脑屏障进入脑脊髓液中,这是一种被动扩散作用。但如果钠离子从<br />
脑脊液重新回到血中,则必须消耗能量,此为主动输送过程。实验室检查指出,在中毒初期,<br />
血液中钠离子浓度可高达 150~190mmol/L。但当出现神经症状之后,钠的浓度并不高,而<br />
脑脊液中钠浓度却升高到 145~185mmol/L(正常猪脑脊液中Na + 浓度为 139.6±5.17mmol<br />
/L),导致脑细胞内钠离子积聚。<br />
由于血钠、脑脊液中钠离子浓度升高,垂体后叶分泌抗利尿激素,尿液减少,血液中水<br />
分甚至某些代谢产物、尿素、非蛋白氮、尿酸等,也随之进入脑脊液和脑细胞,产生脑水肿,<br />
并出现神经症状。因此,在中毒初期,当血钠浓度升高时,给予大量饮水,促使钠离子经尿<br />
排出是有意义的。一旦出现神经症状以后,再给予大量饮水,甚至灌水,只能使脑水肿加重。<br />
钠离子中毒学说认为:一方面因多种钠盐都可引起中毒,另一方面细胞外钠离子浓度升<br />
高,“钠泵”作用不能维持。Na + 有刺激ATP向ADP和AMP转化并释放能量,以维持“钠泵”<br />
的功能;但大量AMP积聚在细胞内,不易被清除。AMP因缺乏能量不能转化为ATP,过量<br />
的AMP还有抑制葡萄糖酵解过程;因而脑细胞能量进一步缺乏,“钠泵”作用难以维持。细<br />
胞内钠离子向细胞外液和血液内运送几乎停止,脑水肿更趋严重,但当AMP在某种条件下,<br />
转化为ATP后,动物显平静。<br />
以上两种学说成功地解释了血浆钠离子从升高转为正常,脑脊液中钠维持高浓度和脑水<br />
肿发生及间隙性神经发作的机理。但不能解释食盐中毒为什么在血管周围会出现嗜酸性白细<br />
胞从集聚到游走,淋巴细胞相继进入这些现象。<br />
过敏学说提出者认为,在钠离子作用于脑细胞之后,一方面刺激脑细胞并引起神经症状,<br />
同时脑细胞释放出组织胺、五羟色胺等化学趋向物质,引起嗜酸性细胞的接近和积聚作用,<br />
而且大多在血管周围出现这种现象。<br />
全搞清。<br />
总之,这三种学说只从某个角度出发,对中毒机制进行解释,但中毒的真正机理尚未完<br />
【临床表现】 最急性中毒的病猪,自始至终表现显著衰弱,肌肉震颤,瘙痒,后来躺<br />
卧,四肢作游泳状动作,很快虚脱,以至昏迷而死。急性病例的病程在两天以上,亚急性病<br />
例的病程可达 5~7 天或更长。有些猪采食含盐饲料后可延迟数天才发病,最初饮欲增加,皮<br />
肤瘙痒,尿少,便秘以及可视黏膜潮红,继则因视、听觉机能障碍,对周围显得淡漠,对光、<br />
声、食物缺乏反应,并无目的地徘徊或转圈。有的表现为吻突和上下颌和颈部肌肉不断抽搐,<br />
头部渐次升高,直至前肢提空或两后肢蹲地,呈犬坐姿势。倒地后病猪极度虚弱,躺卧不动<br />
或呈昏迷状态。经短暂休息后又可起立,摇晃,行走或依墙而行,发作时还可见到空口咀嚼,<br />
口角边沾满白色唾沫,呼吸迫促,脉搏快速,皮肤黏膜发绀。但在发作过后的间歇期内,轻<br />
症病猪可与健康猪无明显区别,病猪体温始终正常,但在惊厥性发作时,体温有时升高。<br />
除神经症状外,尚有消化功能障碍,不吃,后期很少饮水。<br />
牛中毒呈现食欲减退、呕吐、腹痛和腹泻。同时,视觉障碍,最急性者可在 24h 内发生<br />
186
麻痹,球节挛缩而死亡。病程较长者,可能出现皮下水肿,顽固性消化障碍,并常可见到多<br />
尿、鼻漏、失明、惊厥发作,或呈部分麻痹等神经症状。<br />
禽:有试验表明,每吨饲料中加进 9~10kg 盐,而且供水不足,禽舍温度太高,可引起食<br />
盐中毒。病鸡表现为烦渴、停食、喉头分泌物增多、下痢、腹水,进行性肌肉虚弱,不能站<br />
立,痉挛、惊厥,内脏器官广泛水肿,如心包、肺、肠壁水肿等。肾炎、心肌出血。<br />
【诊断】 根据病史调查,若吃入多量食盐,同时未给予充分饮水,结合神经症状,基<br />
本上可以确诊。<br />
临床病理学检查方面:单纯测定血清钠离子浓度,对本病诊断意义不大。脑脊液中钠离<br />
子浓度和死猪脑组织的钠离子浓度,有一定诊断意义。当脑脊液中Na + 浓度超过 160mmol/<br />
L,脑组织中钠超过 1800µg/g时,就可认为是钠盐中毒。确诊依靠病理组织学变化,脑血<br />
管周围有多量嗜酸细胞浸润,形成“袖套”现象。<br />
饲料中盐含量测定,对疾病诊断的意义不大。因为会不会产生中毒除与摄入食盐的量有<br />
关,更与食盐后的饮水多少有关。<br />
由于脑炎引起的惊厥症状,体温有时升高,可与病毒性脑脊髓炎相混淆。猪传染性脑脊<br />
髓炎可发生于任何年龄;伪狂犬病只发生于乳猪,同时伴有皮肤奇痒和啮齿动物活跃的地方;<br />
李氏杆菌病引起四肢瘫痪,单核细胞增多;猪水肿病多发生于长得快的猪,并发出尖叫声;<br />
缺硒引起桑葚心,常限于个体较大的猪。总之,猪的食盐中毒时对病史调查,在诊断中应十<br />
分注意。<br />
【防治】 由于发生机理不清楚,治疗中多取对症治疗。首先应给全群中尚未出现神经<br />
症状的猪饮用新鲜水,并注意少量多次给予,以利血液中盐尽快经尿液排出。已经出现神经<br />
症状的猪,不应再给予饮水,否则脑水肿更严重。有人认为一价离子(Na + 、K + )可致神经<br />
兴奋,二价离子(Ca 2+ 、Mg 2+ )可致神经抑制,它们在血浆内应保持平衡,食盐中毒时打乱<br />
了这一平衡,应给中毒猪皮下注射 5%氯化钙明胶溶液(氯化钙 10.0g,l%明胶 200m1),<br />
剂量按 0.2g/kg体重氯化钙计算,每注射点不得超过 50ml,大动物可直接用氯化钙静脉注<br />
射。<br />
为了缓解脑水肿,降低颅内压,可静脉注射 25%的山梨醇或高渗葡萄糖。为促进毒物<br />
排除,可用双氢克尿噻利尿,并可抑制肾小管对钠和氯的吸收,使血中钠离子尽可能地从尿<br />
中排出。为抑制中枢兴奋,可给予溴化钾和溴化铵。酌情采用灌肠和轻泻法,使钠离子反渗<br />
入肠内而排出。<br />
各种动物对盐的耐受相差很多,猪、马、牛的中毒剂量为 2.2g/kg 体重,绵羊为 6g/<br />
kg 体重,家禽为 2g/kg 体重。各种动物饲料中应给予盐,除应拌匀外,尚需给予充足饮水。<br />
各种含盐量高的饲料,如酱渣、咸菜卤、咸肉(鱼)水,不要长期饲喂或一次喂给太多。平<br />
时不应使动物产生盐饥饿,造成一次食盐太多。<br />
五、硫营养紊乱性疾病(Nutritional Disorder of Sulfur)<br />
硫是机体内多种物质的构成成分,体内有 21.5%的氨基酸内含有硫,如甲硫氨基酸、胱<br />
氨酸、同型半胱氨酸、胱硫醚、牛磺酸,许多维生素内亦含有硫,如硫胺素、生物素等,许<br />
多蛋白质中含有硫如角蛋白,硫酸软骨素、肝素、谷胱甘肽等,被毛和羽毛中,硫的含量特<br />
别丰富,被毛与头发中含硫量是分别为 4%和 5%,鸡的羽毛中含硫量随年龄而增多,成年<br />
鸡羽毛中含 2.2%~2.95%的硫。因此硫缺乏将可引起被毛生长,骨骼发育的一系列症状。<br />
(一)硫缺乏症(Sulfur Deficiency)<br />
动物因硫摄入不足产生羽毛生长不良,舔毛,拉自己身上的毛,甚至引起毛球阻塞的现<br />
象称硫缺乏症。硫缺乏症常见于绵羊、毛兔、皮毛动物和家禽。<br />
【病因】 饲料中缺乏无机硫、蛋氨酸、胱氨酸等含硫物质,可引起硫缺乏症。毛、羽<br />
中硫含量丰富,动物每年更换羽毛和被毛,此期饲料中如缺乏蛋氨酸、胱氨酸及无机硫化合<br />
187
物,则可使换毛延迟,毛、羽生长不良,有的甚至全身掉毛后,迟迟不能生长。<br />
饲料中锌的含量太多(2.5%氧化锌)可强制性引起换羽,但一旦停止补锌后又可使羽<br />
重新生长。<br />
乏症。<br />
反刍动物瘤胃内细菌可将无机硫转化为有机硫,因此饲料中缺乏硫酸盐,亦可产生硫缺<br />
以玉米和豆饼为主食的鸡和猪饲料中必须补充含硫氨基酸,因其中硫含量较低(分别为<br />
0.004%~0.3%;0.002%~0.45%),当饲料中硫含量在 2.3~2.5mg/kg 以下时,可产生临床的<br />
和亚临床硫缺乏症。饲料中蛋白质含量突然减少,亦可引起大量掉毛。<br />
【临床表现】 禽缺乏硫或含硫氨基酸时,青年鸡生长缓慢,成年鸡繁殖力下降,最典<br />
型的表现呈现裸躯病。当禽羽毛生成后出现部分或全部掉毛,不再长出新羽现象称为脱羽病。<br />
病禽尾、颈背部羽毛脱落,常被其它同伴啄食,引起皮肤感染,甚至出现同类相残,相互攻<br />
击致死。母鸡产蛋减少或停止生长,常有吞食羽毛的现象。<br />
绵羊饲料中缺乏硫或含硫氨基酸,可造成食欲下降,消瘦,用嘴拉自已身上的毛,吞食<br />
掉在地上的毛及出现异食癖。饲料中氮和硫的比例应为 10:1,泌乳羊每泌 1 升乳应供给 0.5g<br />
硫,每产 1kg 净毛,应给 70g 硫。当饲料中硫供给不足,乳产量和毛产量减少。幼畜经常吞<br />
食脱落被毛,可引起毛球阻塞,当阻塞幽门或小肠时,可引起肚胀、不排粪、磨牙、腹痛(咩<br />
叫、回头顾腹、弯腿而行、猝然倒地等)等症状。<br />
皮毛动物缺乏硫时,兔毛生长不良,长短参差不齐,毛产量减少。貂、狐等动物出现自<br />
咬症、啃食被毛,毛尖分叉,容易脱落或折断。<br />
【诊断】 本病出现的症状之一是异食癖,但以食毛、食羽,毛、羽生长不良为特点,<br />
不难作出诊断。但应与皮肤寄生虫引起的掉毛相区别,羽虱、羽螨引起羽毛折断,仔细检查<br />
可发现寄生虫本身。螨病主要发生在头面、四肢内侧,而且有结痂现象。<br />
微量元素铊中毒可引起斑秃,并常呈地方性流行。但仅限于局部地区,当地的苞菜,牛<br />
皮菜生长特别良好。<br />
当出现毛球阻塞时,应与其它腹痛性疾病相区别。<br />
【防治】 饲料中应供给足量的硫及含硫氨基酸,禽饲料中胱氨酸、蛋氨酸、硫酸盐之<br />
间的比例应为 50:41:9,反刍动物瘤胃微生物可将无机硫转变为有机硫,因此,硫酸盐比例<br />
可适当提高,目前在青贮饲料中掺入硫酸盐,有利于防止硫缺乏症,但蛋白质与硫之间应有<br />
一定比例,N:S 为 10:1;尤其是用尿素作蛋白质代用品时,应添加硫。<br />
各种动物对硫的需要量,羔羊饲料中以干物质计应含 0.64%蛋氨酸或 1.27%的硫酸钠或<br />
0.47%的元素硫,成年羊每天应供给 0.48g硫,乳牛应供给 0.18%的硫,每天产 8~37kg乳的<br />
牛,至少要摄入 4g硫。鸡饲料中应含硫 2.3~2.5mg/kg,应注意在饲料中添加蛋氨酸和赖氨<br />
酸或添加鱼粉、血粉或羽毛粉及补充VB12。<br />
(二)硫中毒(Sulfur Poisoning)<br />
硫是动物必需元素之一,但供给的量太多或在烟雾笼罩下长期生活,或在酸雨严重的地<br />
区生活,可引起动物中毒。临床上可引起失明、腹泻、昏迷、死亡。甚至引起低磷血症,佝<br />
偻病等。<br />
硫对动物的毒性作用因含硫化合物而定,硫酸、硫化氢毒性最大,元素硫毒性最小。生<br />
产中元素硫粉末常用作青贮料添加剂作为营养强化剂,同时还可驱除体表寄生虫。尽管硫化<br />
氢、二氧化硫对动物的毒性作用较强,在生产上真正因硫化氢和二氧化硫所致中毒者较少。<br />
大多是因用元素硫添加到育肥牛、羊饲料中,以便限制其采食量和减少肠毒血症,因使用得<br />
太多而中毒。小量硫是无毒的,而大剂量则可引起致死性胃肠炎和脱水症。每头牛饲以<br />
85~450g硫可引起死亡,45g硫可引起母羊死亡。以 10g/kg体重剂量硫(含硫蛋白)饲喂绵<br />
羊,可引起死亡。以每天每羊 7g元素硫,饲喂成年羊,持续一段时期亦可致死羊。口粮中<br />
188
蛋白质浓度越高,硫的毒性越强。VA缺乏,可影响肠黏膜内硫转移酶的活性,使硫酸根与<br />
葡萄糖合成粘多糖受阻,因而增加了硫的毒性作用。饲料中氟、铜、钼等元素则可降低硫的<br />
毒性作用。<br />
硫中毒的症状因硫化物种类不同而不同。一般因硫化氢的刺激作用,可引起羞明、流泪、<br />
咳及呼吸道和肺部炎症。<br />
牛中毒时,表现迟钝、腹痛、肌肉拧转、排黑色稀粪和呼出气显浓的硫化氢气味。机体<br />
脱水严重。动物很快躺卧,呼吸困难,惊厥,在昏迷中死亡。剖检,肺充血、水肿,肝色白,<br />
肾充血,显黑色,有严重的弥散性胃肠炎,全身呈点状出血。<br />
羊的症状与牛类似,唯对过量硫的耐受性稍强。<br />
猪似乎能耐受较大剂量硫,当生活在含 28mg/m 3 H2S的气体中,猪仅有嗅觉丧失。2<br />
周龄仔猪生活在含 5~20mg/m 3 SO2气体下,每天 5~6h,70 天后才陆续死亡。但有曾因误将<br />
硫磺粉当作糠粉致使 16 头猪相继中毒的报道,病猪表现惊恐、兴奋、不安、减食或停食,<br />
体温 40.5~42℃,稽留不退,粪灰黄,稀糊状,中后期沉郁、甚至昏迷卧地不起,腹泻加剧,<br />
多数表现呼吸困难,呈犬坐姿势,少数病猪,抽搐,原地转圈或躺卧于地,四肢作游泳状,<br />
剖检,显消化道黏膜炎症、溃烂,肺水肿,喉出血。<br />
鸡饲料中含 0.27%的有机硫化合物,将引起 40%鸡生长缓慢,低血糖症,及鸡的佝偻<br />
病、胃肠炎等。<br />
狗对亚硫酸氢钠较敏感,按 30mg/kg 静脉注射,可引起急性中毒。表现呕吐、腹痛、<br />
厌食、行走不稳和死亡。<br />
鱼对过量硫似乎更敏感。工业发达地区,通过燃煤向空气中释放大量SO2,遇水后形成<br />
硫酸,即所谓酸雨,落入湖泊河流中,可使鱼、虾死亡,形成无鱼的死湖。<br />
有研究表明,羊的饲料中硫含量不得超过 0.4%,鸡不得超过 0.2%,狗不得超过 0.28<br />
%,否则可引起中毒。<br />
一旦硫化氢中毒,应尽快使用解毒剂。细胞色素 C 可矫正细胞呼吸障碍,一般用<br />
200~300mg,配合 10%葡萄糖一次静注。<br />
美兰:高浓度美兰,可使血红蛋白氧化为高铁血红蛋白,后者三价铁与硫有亲和作用,<br />
夺取已和细胞色素氧化酶结合的硫离子,并恢复酶的活性。用 l%的美兰乙醇液,大动物按<br />
0.3~0.5ml/kg 体重,中小家畜 0.5~1.0ml/kg 体重与 25%~50%的葡萄糖混合注射。配合对<br />
症治疗,如 20%碳酸氢钠水洗眼,硼酸水湿敷等。<br />
第五节 微量元素营养紊乱性疾病<br />
(Nutritional Disorder of Trace Elements)<br />
微量元素是指在动物体内含量甚少的那些元素,常以 mg 或 µg 计,有的甚至以 ng 计算。<br />
体内微量元素大致可分为三大类:<br />
①必需微量元素是指那些元素存在于所有健康组织内,从亲代到子代,这类元素含量恒<br />
定;如果从体内排除它,可产生生理和结构异常;并伴有生物化学异常;动物获得这种元素<br />
后,可以防止和治疗异常的生理现象等 5 个条件。符合这 5 个条件的元素有 15 种。即铜、<br />
铁、锌、锰、硒、铬、钴、碘,钼、氟、锡、砷、硅、矾、镍。最后这 6 种元素称为新 6<br />
种必需微量元素。②第二类元素存在于机体内是有害元素,如镉、铅、汞、锑、铋、铍等,<br />
称为有毒元素,含量越多,危害越大。③第三类是介于上述两类作用之间,虽并非属必需,<br />
但也无太大毒性,故称为非必需微量元素,如铝、硼、银、金等。<br />
微量元素在体内的生物学作用与含量之间有密切关系,即使必需微量元素亦如此。当它<br />
们在体内含量低至一定限度后,就可产生该元素缺乏症。随着饲料中补充后,生物学活性逐<br />
渐恢复,直至正常。当继续长期供给过多,则又可产生该元素中毒症,甚至引起动物死亡。<br />
本节着重介绍生产中常见的微量元素硒、铜、铁、锌、锰、碘、钴缺乏与中毒。<br />
189
一、硒营养紊乱性疾病(Nutritional Disorder of Selenium)<br />
(一)硒缺乏症(Selenium Deficiency)<br />
硒缺乏症主要是饲料和饮水硒供给不足或缺乏,引起多种器官组织膜变性,细胞坏死、<br />
瘪缩等一系列营养障碍性疾病。临床上常有肌营养性坏死,心肌出血,肝坏死及繁殖机能紊<br />
乱为特征。本病亦称为硒反应性疾病(selenium response disease)。<br />
硒是动物的必需微量元素之一,当动物饲料、饮水及环境中硒含量太少时,可引起硒缺<br />
乏症。各种动物均可发生,但以幼畜为多见,如羔羊、犊牛、牦牛、水牛犊、马驹、骆驼、<br />
仔猪、雏鸡、雏鸭、雏雉、雏鸽、兔、幼貂、长颈鹿、羚羊、袋鼠、均可发生硒缺乏的典型<br />
症状—肌肉营养性坏死,成年动物缺硒主要引起繁殖机能障碍,如流产、胎衣滞留等。然而,<br />
饲料中硒的供给要适量,供硒过多则可引起中毒(见硒中毒)。据报道硒不足或过量可引起<br />
40 多种动物产生 20 多种疾病或病变。<br />
【病因】 硒缺乏的原因是复杂的,主要是因饲料、饮水中硒供给不足但许多其它因素<br />
亦可促进硒反应性疾病发生,例如应激、VE及含硫氨基酸缺乏,饲料中不饱和脂肪酸含量<br />
过多,生长过快等。<br />
动物的硒缺乏症起源于土壤中缺硒,世界上有许多缺硒的地区。凡由火成岩风化的土壤<br />
中,硒的含量较低(Se
些地区生活的动物易发硒缺乏症。然而,随着市场经济的发育,畜禽规模饲养,饲料运输,<br />
将改变其流行规律。但每年冬季初春,尤以 2~5 月的繁殖旺季期间最为多发。而非低硒地区,<br />
本病发生则与使用来自低硒地区的饲料有关。<br />
各种动物均以幼龄动物发病最多,成年动物通常缺乏明显的临床症状,但在妊娠、分娩、<br />
泌乳等应激因素刺激下可诱发临床硒缺乏症。<br />
【病理】 硒在体内是谷胱甘肽过氧化物酶(GPX)的构成成分,每个GPX分子内含 4<br />
个原子硒,以硒代半胱氨酸形式,成为GPX的活性中心。全血中GPX的活性与血硒浓度间在<br />
一定范围内成正比。谷胱甘肽过氧化酶可将细胞代谢活动中所产生的有机氧化物(ROOH)<br />
和无机过氧化物(H2O2)转变为羟基化合物和水而解毒。硒只有在GPX中才起作用,饲料<br />
中硒过多(>5mg/kg),GPX活性不再继续升高,并可产生中毒。<br />
过氧化物对各种富含有不饱和脂肪酸的脂质膜是很毒的,在它们作用下,产生“脂质过<br />
氧化作用”,可造成细胞膜、亚细胞膜结构及功能损坏。因此当红细胞膜损伤,则产生溶血<br />
和渗出性素质;毛细血管膜破坏,则产生出血如心肌出血、肌肉营养性坏死;亚细胞成分如<br />
线粒体、微粒体,滋养泡膜结构破坏时,则产生细胞坏死、液化和软化,如肝坏死、脑坏死、<br />
当细胞液流失后细胞瘪缩,纤维素增生等等。<br />
硒能增强VE的抗氧化作用,二者在这方面有协同作用,补充硒或VE可达到互补和纠正<br />
各自的缺乏症。但有些情况下VE不能代替硒,而硒则在很大程度上可代替VE。<br />
硒和VE之间相互作用可用图 2~l表示。<br />
硒的抗氧化作用还表现在有清除体内自由基(free radical)的作用。在氧存在的情况下<br />
自由基可作为引发剂(initiator),激发氧化作用,使细胞内外多种成分被氧化,使细胞及亚<br />
细胞成分功能受损,DNA、RNA酶活性异常并干扰核酸、蛋白质、粘多糖酶的合成作用,<br />
直接影响细胞分裂、生长发育、繁殖和遗传,因此自由基已成了诱发许多疾病的重要因子,<br />
硒可通过谷胱甘肽过氧化物酶及在辅酶II、β-磷酸葡萄糖酶等配合下,使自由基(HOO – ,<br />
O2 – ,R – ,ROO – )被清除转化,从而保护细胞正常的生理活动。反之,动物生长缓慢、发<br />
育不良,并引起一系列硒反应性疾病。<br />
硒可增强细胞免疫机能,动物缺硒,使体液免疫功能降低,抗体产生受阻,鸡、猪对<br />
----------→H2O+O2→<br />
黄嘌呤氧化酶 | 谷胱甘肽过氧化物酶<br />
各种底物---O2---→H2O2-------------------→2H2O<br />
↓ ↑<br />
2GSH GSSG<br />
↓ ↓<br />
不饱和脂质(RH)-------→ROOH-----------→ROH + H2O<br />
↑ ↓<br />
VE ↓<br />
促使脂质过氧化<br />
形成丙二酸二醛<br />
等导致细胞损伤<br />
图 2-1 硒、VE对某些过氧化物降解的影响<br />
大肠杆菌、球虫等抵抗力下降。缺硒时猪水肿病发病率增多,鸡生长缓慢、矮小并容易患禽<br />
白痢和副伤寒,使有些疫苗的保护力减弱。硒缺乏还可诱发细胞核染色体突变,使癌症发病<br />
率提高。<br />
【临床表现】 畜禽种属间差异,受损的器官和组织不同,所呈现的病理变化不一致,<br />
各种动物硒缺乏症的病名亦不一致,见表 2-2。<br />
191
由于硒缺乏症病型不同,所呈现的症状也不完全一致。但罹病畜禽一般呈现程度不同的<br />
基本症状(共同症状)。如:<br />
运动机能障碍:动物喜卧,活动起立困难,肢腿僵硬,步态强拘,行动缓慢,跛行,共<br />
济失调,跪立,爬行,行动缓慢,跛行。<br />
心脏功能障碍:心跳加快,脉搏细弱,节律不齐,特别是在剧烈运动、奔跑、追逐过程<br />
中突然死亡,俗称猝死症。<br />
迷等。<br />
消化机能紊乱:消化不良,食欲减退以至废绝,顽固性腹泻,个别见有吞咽障碍。<br />
神经机能紊乱:伴有VE缺乏更为明显,因脑软化,常呈现兴奋、抑郁、痉挛、抽搐、昏<br />
表 2-2 各种动物硒缺乏症<br />
牛 羊 马 猪 禽<br />
肌营养不良 肌营养不良 肌营养不良 肌营养不良 肌营养不良<br />
胎衣滞留<br />
消瘦病<br />
牙周炎<br />
消瘦病<br />
幼驹腹泻<br />
肝营养不良<br />
桑葚心<br />
渗出性素质<br />
渗出性素质<br />
胰腺纤维素性<br />
增生肌胃变性<br />
繁殖机能减退<br />
贫血<br />
肉用仔鸡苍白<br />
水肿病(?) 综合征(?)<br />
繁殖机能障碍:公畜精液不良,受精能力下降,母畜受胎率降低,甚至不孕,流产、早<br />
产、死胎,产后胎衣不下,泌乳动物乳产量降低或停止,母鸡产蛋减少,蛋的受精率、孵化<br />
率下降,缺硒母畜(禽)所生仔畜(雏)将引起先天性白肌病,产生弱胎,或生后不久死亡。<br />
硒缺乏病涉及器官多,各种动物表现的症状不同,现分述如下:<br />
1.禽类硒缺乏症 在我国已报道的禽类硒缺乏包括鸡、火鸡、鸭、鹅、雉、鹌鹑、肉鸽<br />
等,各种年龄均有发生,涉及病种有:<br />
【营养性肌坏死】(Nutritional Muscular Dystrophy) 营养性肌坏死又称为白肌病,<br />
火鸡、鸡、鸭、鹅、雉、鸽、鹌鹑及其它观赏鸟均可发生。大多于生后 2~3 周龄发生,但先<br />
天性白肌病可于出壳后 3~4 天内即可发生,火鸡最易发生,雏鹅于出壳后 6~10 日龄发生。<br />
成年鸡饲料中硒含量低于 0.02mg/kg时,产蛋母鸡所生的蛋孵化的雏鸡容易发生白肌病,<br />
VE缺乏、蛋氨酸缺乏可促使白肌病发病率增加,不饱和脂肪酸含量过多、粗蛋白供给不足<br />
可促使本病发生。病雏表现衰弱无力,体温正常情况下,萎靡不振,行动不稳,活动受限制,<br />
跛行可能发生水肿,关节肿大,肢体屈曲,个别雉发生麻痹,两翅下垂,羽毛蓬松,腹泻,<br />
小鸭、小鹅因两肢麻痹,不能从水中游至岸边甚至溺水死亡。小鹅病程可持续 5~20 天,死<br />
亡率在 20%~45%。6 日龄雏鸭即可发病、17 日龄大批发病,剖检可见小腿、大腿及臀部肌<br />
肉变性、松弛、呈不均匀亮灰色,切面干燥并呈明显花纹,心肌松弛,失去弹性,有时有细<br />
条状白色坏死,肌胃肿大,切面和浆膜下有许多白色坏死灶,角质层呈深绿色或深棕色,伴<br />
有石灰样沉积物和溃疡,严重时肌胃肌肉厚度仅相当于正常鸡三分之一,硬度增加。骨骼骨<br />
肉营养不良、色呈条索状煮肉样故称为白肌病,体型大长得快的鸡死亡也快。<br />
环颈雉在(6~10)日龄时有零星发生,11~17 日龄发病高峰,多数呈现腿软、不稳、跛<br />
行或瘫痪,翅下垂,呆立或昏睡,频死时抽搐、鸣叫,剖检可见,腿肌呈显著的煮肉状或鱼<br />
肉状,肌纤维脆弱易碎,心肌褪色,心内膜出血。<br />
肉鸽多于 20 日龄开始发病,除共同表现跛行、垂翅外。腿脚无力,心肌灰白色变性、<br />
192
坏死,胰变性,布满白色斑点,肌胃变性,角质层下有若干出血点和凹状溃疡、胸肌、腿肌<br />
色淡,干燥有斑块状出血。<br />
组织学变化基本类似,肌纤维凝固性坏死,肌浆内有透明小体,嗜酸性细胞浸润,特别<br />
是积聚在血管周围。<br />
血液中肌酸、肌酸磷酸激酶(CPK)及谷草转氨酶活性升高。<br />
【渗出性素质】(Exudative Diatheasis) 本病多发生于 3~6 周龄鸡,火鸡、鸭、鹅及<br />
其它禽类发病率较低,表现为胸、腹皮下水肿,因而又称为小鸡水肿病。<br />
病因与后天性白肌病类似,但本病属后天性的。是指禽缺硒时毛细血管通透性增加,血<br />
浆蛋白质和崩解的红细胞内释放的血红蛋白进入皮下,使皮肤呈淡蓝,淡绿色。这是因红细<br />
胞膜结构和血管内皮受损,内皮细胞坏死,通透性增加,血红蛋白等漏入皮下,并形成变性<br />
血红蛋白之故。<br />
患病鸡精神沉郁,不愿活动,腹部皮下血管呈轻微紫红色,继则皮下呈淡紫绿色,腿、<br />
颈、翼下水肿,穿刺患处有蓝绿色液体流出,故称为渗出性素质。渗出区域或其附近常有点<br />
状或斑纹状皮下出血,有时伴有凝固样肌肉坏死,个别鸡在胸肌和股内侧出现灰白色条纹,<br />
肌胃脂肪出血,有时呈现严重的巨细胞性贫血。<br />
出现渗出性素质后,全身体况迅速下降,起立困难,站立时两翅展开,保持平衡,运步<br />
障碍,共济失调,最后衰竭死亡。<br />
组织学变化:肌肉凝固性坏死与白肌病同。<br />
【胰腺纤维素性增生】(Pancreatic Fibrosis) 该病是指胰腺萎缩,腺细胞内空泡形成,<br />
并形成透明小体,最终腺泡区消失。患病鸡迅速死亡,常因先天性缺硒所致。6 日龄雏发病<br />
率最高,雏鸡饲料中缺硒,可加速此病的发生。本病与VC缺乏无关。<br />
主要病理变化是腺泡腔扩大,成纤维细胞侵入腺泡腔,原来的腺细胞瘪缩后,仅留下浓<br />
染的细胞核,排成一圆圈结构。圆圈外周为纤维组织环绕,补硒后两周内胰腺结构可恢复正<br />
常。患病鸡生前无特征性变化,仅表现突然死亡,亚急性鸡可有生长不良、羽毛蓬松、血浆<br />
中酸性磷酸酶、溶菌酶活性增加,但血浆和胰腺内谷胱甘肽过氧化物酶活性变化与病情轻重<br />
无关。实验性胰腺纤维素增生(黄美玉等,1987)发现 6 日龄开始发病,18 日龄腺上皮细<br />
胞浆内出现玻璃小体和萎缩,24 日龄出现腺空泡增多,细胞呈蜂窝状,30 日龄腺泡内出现<br />
纤维化,40 日龄胰腺萎缩。<br />
【脑软化症】(Encephalomalacia) 见VE缺乏症。<br />
【肌胃变性】(Gizzard Degeneration) 肌胃变性是硒缺乏症的症状之一,病理变化仅<br />
主要局限于肌胃。出壳后 7~10 天死亡。雏鸡表现全身虚弱,抑郁,羽毛蓬乱,消化紊乱,<br />
一般呈亚急性和慢性,发育不良,粪便呈暗色,常有少量未消化的饲料,死亡的病雏,角膜<br />
上可见由小到大的表层损伤,深层角质膜的破坏,并有大量渗出性出血。<br />
【肉用仔鸡苍白综合征】(Pale Syndrome of Broilers) 本病多发生于 12~30 日龄肉用<br />
仔鸡,50 日龄后不再发生,发病率可在 10%~33%之间,死亡率可达 20%~30%,主要表现<br />
翅羽基部不全断裂,断裂羽毛与体躯垂直,如同飞机螺旋浆一样,又称螺旋浆病。生长良好<br />
的鸡,突然产生软脚,蹲地啄食,进而两脚瘫痪,完全不能站立,侧卧,两脚软,一侧或一<br />
前一后叉开躺卧,典型特征是腺胃炎症,腺胃与肌胃交界处出血,乳头糜烂出血,肌胃萎缩。<br />
很易与鸡瘟混淆。但用鸡瘟疫苗紧急预防注射,死亡更多。<br />
有人认为本病是由呼肠孤病毒引起。用病毒接种 1 日龄雏鸡,可复制该病。但用 0.1%<br />
亚硒酸钠,可预防和冶疗该病。<br />
【成年鸡硒与VE缺乏症】(Seleniun and Vitamine E Deficiency of Adult Poultry) 成年鸡<br />
硒和VE缺乏或者是因小鸡缺硒和VE后留下的后遗症,或者是因饲料中硒含量较小,添加蚕<br />
蛹、变质鱼粉后引起VE丧失,硒丢失而造成病鸡曲颈,扭颈,走路时平衡失调,倒地滚转,<br />
193
特别是在被追逐驱赶时如此。另一类型鸡,大多伏地不起,仍有食欲,驱赶时腿弯曲行走,<br />
数步即停,冠苍白,干燥,排白色稀粪。剖检皮下有蓝色胶冻状液体,心包液增多,心肌松<br />
软,肌胃变薄,并发生腿肌萎缩。产蛋率下降,产蛋高峰期维持短,有的鸡卵巢完全未发育,<br />
呈灰白色和秽绿色,输卵管窄小,无弹性。鸡蛋的受精率下降,鸡胚死亡增多,孵化率下降。<br />
禽硒缺乏症的诊断要点 主要根据剖检变化。胸肌,大腿内侧肌肉有条索状白色坏死,<br />
肌胃肿大或变薄,心肌有出血点或出血斑,皮下水肿,腹下方有蓝色或绿色渗出液及水肿液,<br />
死亡迅速,长得快,发病也快,死亡也快。鸡群中补充硒和VE,可迅速控制疾病的发展。<br />
生长鸡群中出现扭颈,平衡失调,母鸡群中产蛋率一直低下,孵化率、出壳率均甚低,剖检<br />
未发现明显的的沙门氏菌,而卵巢发育不良或发育停滞,饲料中去除变质鱼粉和含脂高的成<br />
分,添加VC和硒后,可使产蛋率、孵化率提高,死胚减少等都可作为临床诊断依据。<br />
血液中谷胱甘肽过氧化物酶活性下降,肌酸磷酸激酶活性提高是主要的诊断依据,血液、<br />
肝、肾中硒含量测定对疾病诊断可提供可靠依据。<br />
禽硒缺乏症的防治 全群鸡立即在饲料中掺入 0.2mg/kg 硒,充分拌匀,以防病情扩<br />
大,按含 5mg/kg 硒的饮水(10mg/kg 亚硒酸钠),亦可防止病势继续扩大,同时饲料中<br />
增加蛋氨酸供给。<br />
患病鸡用l%的亚硒酸钠滴服,一日两次,每次一滴,连用 3 日,重症鸡 70%可治疗,<br />
轻症鸡 100%可治疗,如用VE胶囊(内含 50mg),每天二次,每次一粒,连服 3 日,重症鸡<br />
治疗率达 50%,轻症鸡治疗率 100%。<br />
2.猪的硒缺乏症<br />
【营养性肝坏死】(Hepatosis Dietetica) 营养性肝坏死,又称仔猪肝营养不良,营养<br />
性肝病。在喂饲高能量日粮(玉米、黄豆、大麦等)条件下易发生。本病主要发生于 3 周龄<br />
至 4 月龄,特别是断乳前后的仔猪,大多于断乳之后死亡,急性病例多为体况良好、生长迅<br />
速的仔猪,预先没有任何症状,突然发病死亡,存活仔猪常有严重呼吸困难,黏膜发绀,躺<br />
卧不起,强迫走动能引起立即死亡,约 25%的猪有消化道症状,如食欲不振、呕吐、腹泻、<br />
粪便带血等,仔细检查可视黏膜发绀,后肢衰弱,臀及腹部皮下水肿,病程长者可出现黄疸、<br />
腹胀和发育不良,同窝仔猪于几周内死亡数头,群死率在 10%以上,冬末春初发病率最高。<br />
典型的剖检变化有二:①花肝,即正常肝组织与红色出血性坏死的肝小叶及白色或淡黄<br />
色缺血性凝固性坏死的小叶混杂在一起,形成彩色多斑的嵌花式外观。②表面坑凹,再生的<br />
肝小叶可突起于表面,形成肝表面凹凸不平。<br />
【桑葚心】(Mulberry Heart Disease) 桑葚心发生于仔猪和快速生长的猪(体重<br />
60~90kg),营养状况良好,饲以高能饲料,如玉米、豆饼、大麦。玉米中VE含量较低,尤<br />
其是化学浸油后的饼粕中,VE含量甚微。玉米中水分含量高,可加速VE丧失,不饱和脂肪<br />
酸含量高可加速发病,本病发病率为 25%,死亡率达 90%。病猪可在没有任何征兆下突然<br />
死亡,幸存猪显示严重呼吸困难,发绀、躺卧,强迫行走时可突然死亡,亚临床型常有消化<br />
紊乱,任何应激因素,如气候突然变化,运输等可转为急性,几分钟内突然抽搐,大声嚎叫<br />
而死亡。皮肤有不规则紫红斑点,多在两腿内侧,一些斑点甚至可遍及全身。<br />
典型的剖检变化是:心脏扩大,横径变宽呈圆球状,沿心肌纤维走向,发生多发性出血<br />
而呈红紫色(营养性毛细血管病),外观颇似桑葚样,故称桑甚心,心内、外膜有大量出血<br />
点或弥漫性出血,心肌间有灰白或黄白色条纹状变性和斑块状坏死区。肝有斑块状坏死,心<br />
包、胸腔、腹腔积液、色深、透明、显橙黄色。肺水肿、胃黏膜潮红。组织学变化是广泛的<br />
心肌充血、出血、实质变性及大脑白质溶解,心肌毛细血管内有透明微栓生成。<br />
【营养性肌坏死】(Nutritional Muscular Dystrophy) 本病可与营养性肝病和桑葚心伴<br />
发,先天性白肌病死亡最小为 8 日龄,最大为 20 日龄,但多见于 1~3 日龄猪发病,但也可<br />
单独发生于头胎小母猪(10~12 月龄),于产后 48h 突然死亡,它们多因饲以大麦,羽扇豆<br />
194
种子而发病(其中含 Se0.03mg/kg),病猪精神不振,站立困难常呈前肢下跪,或作犬坐姿<br />
势,继则转为四肢麻痹,剖检多呈双侧性肌肉萎缩,横纹肌坏死或透明变性(ZenKer’s<br />
degeneration),肌纤维碎裂,肌纹理紊乱,有些病例可选择性地作用某些肌群。如背部、臀<br />
部肌肉坚实、疼痛,压之尖叫、声嘶哑,肌颤抖。在肌纤维中可见有高梁米粒至黄豆大小的<br />
黄白色斑块,背长肌最严重,组织学检查可见肌纤维横纹消失,胞浆凝聚成块状匀质,多处<br />
肌纤维溶解至消失,仅存完整的内膜,细胞核呈链状排列,心、肝、肾明显颗粒变性。<br />
【仔猪水肿病】(Piglet Edema Disease} 近年来在江苏、浙江及全国一些地区断乳仔猪、<br />
生长猪发生以皮下、胃肠黏膜水肿为特征的疾病。临床上呈进行性运动不稳,四肢瘫痪,死<br />
亡率很高。一直认为是由溶血性大肠杆菌O138,O13,O140等菌株产生,而且用病猪肠内容物<br />
上清液静脉注射,可复制该病,病程 8~15 天。但许多报道证明,在母猪妊娠期间注射长效<br />
硒或 0.1%亚硒酸钠 8~10ml,或补硒(诸明铮,1992)可预防该病。患病仔猪用亚硒酸钠注<br />
射亦可减少死亡。因而疑为因硒的缺乏,机体免疫机能下降,致使大肠杆菌活跃而致死。<br />
病猪典型特征是:轻者走路踉跄,重者瘫痪倒地,四肢呈划水状(游泳状),病后 1~2 天<br />
倒毙。体温正常甚至下降,剖检可见肺间质水肿,充血,出血,胃黏膜水肿,出血,胃大弯、<br />
肠系膜呈胶冻样水肿,肠系膜淋巴结水肿、充血、出血,腹腔积液达 200~500ml,心包积液<br />
达 15~20ml。<br />
母猪于妊娠第 30 天、分娩前 21 天两次注射亚硒酸钠可成功地预防本病。仔猪生后第 7<br />
天,断乳后(即生后 56 天)注射 0.1%的亚硒酸钠,亦可防止本病发生。近年来有报告对水<br />
肿病多发猪群的仔猪,断乳后每天每头口服 5g硫酸镁(MgSO4),分两次拌入饲料中自食,<br />
持续 35 天,亦可大大减少水肿病发生。这可能与促进肠内容物迅速外排,减少毒素吸收有<br />
关。<br />
【成年猪硒缺乏症】(Selenium Deficiency of Swine) 成年猪缺硒病程一般较长,呈慢<br />
性经过,病愈率高,大多表现繁殖机能障碍,屡配不孕,妊娠母猪早产、流产、死胎,所产<br />
仔多孱弱,产后易发生乳房炎-子宫炎-泌乳缺乏综合征。<br />
猪硒缺乏症的诊断要点 主要根据流行病学:突然发病,突然死亡,长得越快死得越快;<br />
结合剖检变化:心肌出血,肝坏死,背部、臀部肌肉凝固性坏死;胃肠充血,水肿,皮下水<br />
肿渗出等病理变化及临床上试验性治疗的结果等,可作出临床诊断。而测定血清中谷草转氨<br />
酶(GOT)、肌酸磷酸激酶(CPK)、乳酸脱氢酶(LDH)和异柠檬酸脱氢酶(ICD),有助<br />
于硒缺乏临床发作型监测,但通常不作为诊断目的使用。红细胞内脂质过氧化物(red blood<br />
cell lipid peroxides)浓度可作为VE和硒缺乏时可靠指标。饲料、组织和血液中硒测定常可帮<br />
助诊断。正常猪肝硒含量为 0.300mg/kg,猪心内含 0.164mg/kg,病猪肝为 0.068mg/kg,<br />
病猪心肌内含硒 0.051mg/kg。发病群饲料中硒
白肌病(NMD),多见于 1~120 日龄羔羊,尤其是 5~30 日龄容易发生。犊牛一般在 10~120<br />
日龄,其主要临床表现分为急性型、亚急性型和慢性型及隐性型四种。<br />
急性型:突然死亡(多死于休克或心性猝死),生前不表现任何症状,剖检为心肌营养不<br />
良,多见于羔羊、犊牛、犊牦牛。<br />
亚急性型:主要见于年龄稍大的羔羊、犊牛(1.5~3 个月龄),以骨骼肌营养不良为主。<br />
慢性型:多见于 4~6 月龄羔羊和犊牛,生长发育迟缓,运动障碍,心功能不全,顽固性<br />
腹泻,由亚急性转化所致。<br />
隐性型:通常不见明显或典型的症状,一般表现消瘦,持续腹泻,遇到某些应激因素刺<br />
激(如过度驱赶,剧烈活动,骚扰惊恐,捕捉挣扎)可促使临床发病。<br />
白肌病的共同症状(基本症候群) 主要是机体衰弱,运动障碍,消化扰乱等。<br />
运动机能障碍:新生幼畜体弱,不能自行起立,不愿活动,驻立时四肢僵硬,运动强拘,<br />
躯体摇摆,腰背拱起。重症者起立困难,站立或运动时肌肉震颤,行动迟缓,原因不明的跛<br />
行,共济失调,有时跪行,有时犬坐,甚至卧地不起,触诊腰背、臀部肌群坚实、僵硬、疼<br />
痛、躲闪。<br />
心力衰竭:心跳加快,心律不齐,脉搏细弱,尤其在兴奋或运动时更为明显,有时在惊<br />
吓或剧烈运动时,因心力衰竭而猝死。<br />
肿。<br />
消化机能紊乱:持续性腹泻,食欲减退,消化不良,有时有异嗜和吞咽困难现象。<br />
精神沉郁,生长缓慢,皮肤、黏膜苍白(贫血),或黄染(肝病、溶血),胸、腹皮下水<br />
羔羊:除有上述共同症状外,大多不能自行起立,行走不稳,共济失调,心搏动 200 次<br />
/min,有时仅能听到一个心音,大多有下痢,但也有便秘的,呼吸浅而快,达 80~90 次/<br />
min,角膜浑浊、软化甚至失明,尿淡红色或红褐色,尿糖、尿蛋白增多。<br />
犊牛:除有上述症状外,并有站立不稳、共济失调,肌肉震颤,心搏增快,达 140 次/<br />
min,呼吸达 80~90 次/min,多数有结膜炎,甚至角膜混浊或软化,排尿次数增多,尿糖、<br />
尿蛋白、尿酸含量升高,最后食欲废绝,卧地不起,角弓反张等神经症状,多死于心力衰竭<br />
或肺水肿。拉黑色、灰绿色稀粪。<br />
病理剖检:主要是腰、背、臀部肌群、膈肌、心肌肌肉变性、色淡。似煮肉状,呈灰黄<br />
色、黄白色的点状、条状或片状不等,横断面有灰白色、淡黄色斑纹,质地变脆、变软、钙<br />
化,心肌扩张、变薄,以左心室为明显,多在乳头肌膜有出血点,心内膜、心外膜下有与肌<br />
纤维走向一致的条纹斑。除心肌外,其余肌肉变化多为对称性的,犊牛亦可呈现桑葚心样变<br />
化,肺瘀血、水肿。镜检多显肌纤维断裂,横纹消失,凝固性坏死。宣长和(1984)等还对<br />
坏死心肌亚微结构变化用电镜作了观察研究。<br />
据报道成年牛亦可发生白肌病,主要见于分娩前后。高产乳牛、母羊、母马有时也有发<br />
生,主要表现为心肌变性、心力衰竭和出血性紫斑,母牛常有肉垂水肿,可视黏膜出血斑,<br />
子宫出血,便血,红尿,胎衣不下,并发子宫炎,多显贫血,血红蛋白 60g/L,剖检心肌<br />
色淡,有蚕豆大白色坏死灶,似煮肉状,典型的凝固性坏死。<br />
长颈鹿、骆驼、牦牛缺硒,多表现白肌病及心脏病理。骨骼肌褪色,呈鱼肉状或呈半煮<br />
肉状和腊肉样。运动时后躯僵硬、前肢粘着后肢拖,易骨折。常有拉稀,拉黑色、灰黑色稀<br />
粪,角膜浑浊或溃疡。<br />
【硒反应性消瘦病】(Selenium Response Unthriftness) 有许多病,因补硒而得以纠正。<br />
如羔羊和犊牛,放牧时生长发育不良,活力不旺,引起的不景气症或消瘦(illthrift)、母畜<br />
繁殖机能障碍、不孕、年龄较大的犊牛拉稀、泌乳母羊拉稀等,都可借补充硒而受益,可能<br />
这些动物仅处于亚临床缺硒。多数情况下,在这些地区或多或少存在着白肌病和其它硒缺乏<br />
症,但是因缺硒引起母羊繁殖性能下降,尚未由实验证明。在新西兰,经补硒后可缓解羊的<br />
196
消瘦病问题引起很大关注,但在澳大利亚对补硒后改善动物消瘦情况收效并不大。从断乳至<br />
l 岁龄的羔羊,补硒后体增重确可加快,而且羔羊毛产量也增加。<br />
【胎衣滞留和流产】(Retained Placenta and Abortion) 近年来已经注意到在低硒地区<br />
母牛、母羊经常发生流产,胎衣滞留。曾志明(1992)等对某乳牛场调查,85 头牛有 12.23<br />
%发生流产,患牛一般不出现任何先兆而发生流产,有的先出现阴唇红肿,阴道内有数量不<br />
等的粘液,流产过程短,速度快,出现预兆 1h流产,预兆时间短,胎儿有可能存活,否则<br />
为死胎,所有流产母牛发生胎衣滞留。经查该场牛饲料中含硒 0.01mg/kg以下。GPX活性<br />
下降,患病牛群血硒浓度下降,产前 20 天每牛给予 50mg硒,17mgVE可有效地减少胎衣滞<br />
留和流产发生率。据研究,当血硒浓度在 0.02~0.05mg/L时,牛群中胎衣滞留占 51%,而<br />
血硒浓度在 0.08~0.1mg/L时。胎衣滞留仅 9%,饲料中含硒 0.1mg/kg时发病率最低。<br />
反刍动物硒缺乏症诊断要点 反刍动物最易患白肌病,根据临床表现跛行,站立不稳,<br />
腰背臀肌疼痛及心跳呼吸和消化机能障碍。地区性缺硒,土壤中 Se
可随胃内容物进入肠最终排出体外,据试验约有 15%的羊可排斥铁丸,在群畜中又难以鉴<br />
定哪些动物已将其排出了。<br />
4.犬、猫硒缺乏症 犬、猫饲料中缺硒或VE可引起肌纤维坏死和钙化作用,俗称白肌病。<br />
患病幼犬和幼猫,很难站立,步伐僵硬,拖曳而行,全身虚弱,肌肉显蜡样,透明样变性,<br />
横纹消失,有吞噬作用的组织细胞及各种白细胞浸润,许多坏死肌肉纤维可能钙化,早期患<br />
畜对VE治疗反应良好,严重时因心肌损伤可引起死亡。当母兽饲料中缺乏VE和Se,而仔畜<br />
全身肌肉虚弱时应怀疑为Se、VE缺乏。<br />
在新西兰、澳大利亚等严重缺硒地区,犬、猫幼崽可自然发生两侧性心肌损伤,用VE-Se<br />
治疗效果良好。<br />
5.鱼、虾硒缺乏症 用硒和VE缺乏性饲料喂鱼 16 周后,可引起鱼的白肌病,表现为背<br />
部肌肉营养性坏死,肌纤维束界限模糊。<br />
(二)硒中毒(Selenium Poisoning) 硒中毒仅在特定地区或特定条件下发生,多数因<br />
土壤中硒含量较高。急性硒中毒临床上以神经症状为主,表现失明,行走不稳,如醉酒状。<br />
慢性硒中毒则表现消瘦,跛行和掉毛。<br />
在我国硒中毒主要发生于湖北与四川、湖南交界的恩施地区及陕西的紫阳县。各种动物<br />
均可发生,以马、猪和禽最易引起中毒,其次是绵羊、牛和狗。急性硒中毒多因错误用药引<br />
起,而慢性硒中毒有两种:即瞎闯症(Blind stagger)和碱质病(alkaline disease)。<br />
【病因】<br />
1.一般说硒中毒主要发生于土壤中硒含量比较高的地区,尤其是沉积岩地区(硅质沉积<br />
岩,碳质沉积岩)。病区土壤中硒含量为 14.05mg/kg,恩施地区自从用石煤作为燃料后,<br />
该病发病率增多。因石煤中含硒 130.44(43.18~262.22)mg/kg。在这些土地上生长的粮食<br />
中硒含量亦很高,玉米中含硒 9.31(5.41~14.97)mg/kg,泉水中硒含量为 0.003~0.02mg<br />
/kg。火山灰烬中硒含量亦很高。<br />
2.有些地区土壤中硒含量不高,甚至低于 0.1mg/kg。但有些植物可富集硒。这些植物<br />
称为硒转换性植物,或称为硒指示性植物。如紫云英、黄芪属、棘豆属植物,木质紫菀等硒<br />
的含量较高。据记载有的植物中硒含量高达 2000~6000mg/kg,最高可达 14900mg/kg 以<br />
上,动物一般不采食这类植物,因有蒜臭味。但在过度饥饿或没有其它饲料可食时,有可能<br />
采食并产生中毒病。<br />
工业污染的废水、废气中含有硒。硒容易挥发为气溶胶,在空气中形成二氧化硒,人、<br />
畜呼吸后亦可引起硒慢性中毒。<br />
在缺硒地区补硒过多。曾有为防止水肿病而配置的 0.1%的亚硒酸钠,误配为 1%浓度,<br />
注射后引起猪中毒。<br />
有些因素可增加植物对硒的吸收。如盐碱土、干旱贫瘠的土。有些因素可增加动物对硒<br />
的易感性,如蛋白质浓度低、钴缺乏,植物中有机硒化合物可能比无机硒化合物更有毒。<br />
各种硒化合物的毒性,以大鼠为例,毒性作用由大到小排列顺次为:亚硒酸钠>硒酸钠><br />
硫化硒>联苯硒>二甲基硒>元素硒。<br />
饲料中含 5mg/kg 硒就可引起中毒。各种动物最小中毒剂量是:马,44mg/kg;猪,11mg<br />
/kg;羊,2mg/kg(或按 0.25mgSe/kg 体重);牛,8mg/kg;鸡,15mg/kg;猴,10mg<br />
/kg;大鼠,4~16mg/kg 硒就可引起中毒。<br />
【病理】 硒可引起毛细血管扩张和通透性增加,引起肺及胃肠道黏膜充血、水肿。硒<br />
与植物中含硫氨基酸中的硫是类似的,它可置换动植物体内某些酶系里的硫,因而干扰了酶<br />
的生物活性,与砷和锑中毒机理一样,事实上可用砷酸盐防治硒中毒。硒可减少羊肝内硫和<br />
蛋白质含量,食物中蛋白含量高,可缓解硒中毒。硒在肝、肾、被毛内沉着较多,对骨骼肌<br />
有明显的破坏作用。<br />
198
硒因取代半胱氨酸中的硫,而影响谷胱甘肽的合成。谷胱甘肽是炎性细胞和其它体液细<br />
胞的化学趋向物质,因而硒中毒可影响机体抵抗力。硒与VA、VC、VK的代谢有关。VA缺乏<br />
可加速视力障碍。硒可通过胎盘屏障,使母畜繁殖能力下降,胎儿生长发育停滞和畸形,羔<br />
羊生后不久死亡。仔猪生后脚爪出血,或生后不久死亡。<br />
【临床表现】 急性中毒:多因注射过量硒引起的。有人误把 1%亚硒酸钠当作 0.1%浓<br />
度给仔猪注射,每猪 1.5~2.0ml,2h 后中毒死亡。动物表现严重呼吸困难,水样拉稀,发热,<br />
心动过速,异常姿势和步样,发病不久死亡。剖检肺和气管内有出血斑、水泡,肝呈紫黑色,<br />
淋巴结出血,皮肤出血等。<br />
瞎闯症:也属慢性型一种(亦有人认为属急性中毒),病畜表现视力逐步减弱,以至失明,<br />
眼肿,流泪,角膜变成白色或不透明,可表现异嗜,流涎,磨牙,腹痛,无目的地行走,转<br />
圈,头低垂,末期瘫痪,因呼吸衰竭而死。实验性仔猪硒中毒,表现呕吐,腹泻,困倦,呼<br />
吸困难和昏迷。后期头低垂,躺卧,昏厥。<br />
碱质病:是典型的慢性中毒,表现精神迟钝,消瘦,被毛粗乱,活力缺乏,步伐僵硬,<br />
跛行,牛、马、驴的尾毛可抹去,猪、马全身掉毛。蹄壳异常,包括蹄冠肿胀、变形、蹄脱<br />
落。动物严重跛行。马、牛、猪均可发生掉蹄现象。中毒母畜所生仔畜可出现先天性蹄变形<br />
现象。如轻度中毒,可表现妊娠比例下降,新生仔畜死亡增多。陕西紫阳县某地玉米含硒<br />
23.74mg/kg,用它饲喂 15 天,猪发病,呈现呕吐、消化紊乱、黏膜黄染、贫血、流泪、磨<br />
牙。中期被毛粗乱无光。后期拱腰凹背,后肢无力,蹄肿胀,蹄冠松动,裂开。至第 63 天,<br />
昏迷,肌震颤,麻痹死亡。恩施玉米平均含硒 9.31mg/kg,猪中毒可表现全身掉毛,边掉<br />
边长,被毛长短参差不齐。11 头母猪产 66 头仔猪,死亡 51 头,部分猪于妊娠期间,胎死<br />
腹中。<br />
鸡亦可发生中毒。主要表现繁殖机能变化,饲料中含硒过多,可使孵化率下降,甚至为<br />
零。死亡胚上喙短,呈球形头。头、颈水肿,有的鸡没有眼睛,或没有脚趾,或翅扭转。支<br />
气管和肺泡有出血性渗出物,毛细血管扩张,肝坏死、出血、纤维素生成。肾小管变形。肾<br />
小球性肾炎,全身水肿,腹水是常见的病理现象。生长鸡食物摄入减少,生长速度减慢,逐<br />
渐消瘦、死亡。<br />
剖检:急性中毒动物肝、肺、心肌广泛损伤,并有胸水、肺水肿。慢性中毒动物心脏松<br />
弛、缩小,肝萎缩、切面深黄或浅黄色,胆囊肿大,胆汁呈煤焦油状,肝细胞空泡变性,脂<br />
肪变性,脑硬脑膜下充血,脑皮质有针尖样病灶,呈海绵样空泡状。肾小球肾炎,中等程度<br />
胃肠炎,关节表面糜烂,脚变形。<br />
慢性硒中毒血液硒可达 3mg/L,尿硒达 4mg/L,毛硒可达 10mg/kg 以上,肝硒可<br />
达 20~30mg/kg。<br />
【诊断】 本病诊断主要依据局部所出现的临床症状,如掉毛、掉蹄、繁殖机能变化。<br />
胎儿畸形等可疑似本病。动物饲料中硒浓度长期维持在 5mg/kg 以上(亦有认为在 10~25mg<br />
/kg 以上),血、尿硒浓度升高,毛硒浓度在 5~10mg/kg 之间,可疑为硒中毒。而 10mg<br />
/kg 以上可认为是硒中毒。肝、肾硒在 10~25mg/kg,蹄壳硒在 8~10mg/kg 时,亦可认<br />
为是硒中毒。<br />
【防治】 本病至今虽曾用多种化学制剂试治,如碘化钾、VC、二巯基丙醇等,收效<br />
甚微。对氨基苯胂酸或砷酸钠拌入饲料中,浓度为 40~60mg/kg砷或 100~200mg/kg的砷<br />
酸盐,可缓解日粮中含 10mg/kg Se的毒性作用。肉牛日粮中每天给予含 100mg/kg苯胂酸<br />
或每天供给 500mg的砷酸盐,饲料中添加亚麻籽油,亦可有保护作用。猪、鸡高铜饲料可防<br />
止硒中毒。<br />
在富硒地区可施酸性肥料、含硫化合物,因在酸性条件下硒与铁形成复合物,硫可排<br />
斥硒进入动物组织内,因而可起预防硒中毒作用。<br />
199
SELENIUM AND/OR VITAMIN E DEFICIENCIES<br />
Several diseases of farm animals are caused by, or associated with, a deficiency of either selenium<br />
or vitamin E alone or in combination, usually in association with predisposing factors such as<br />
dietary polyunsaturated fatty acids, unaccustomed exercise, and rapid growth in young animals.<br />
These are summarized in Table 29.5. All of these diseases are described under one heading<br />
because both selenium and vitamin E are important in the etiology, treatment and control of the<br />
major diseases caused by their deficiencies.<br />
They are also known as selenium-vitamin E-responsive diseases because, with some exceptions,<br />
they can be prevented by adequate supplementation of the diet with both nutrients.<br />
The term 'selenium-responsive disease' has created some confusion relative to the<br />
selenium-deficiency diseases. In some regions of the world, particularly New Zealand, and in parts<br />
of Australia and North America, diseases such as ill-thrift in sheep and cattle, and poor<br />
reproductive performance respond beneficially to selenium administration. While these usually<br />
occur in selenium-deficient regions, they may not be due solely to selenium deficiency. Thus,<br />
there are some reasonably well-defined selenium deficiency diseases, and some ill-defined<br />
'selenium-responsive' diseases.<br />
Synopsis<br />
Etiology. Dietary deficiencies of selenium and vitamin E, and conditioning factors like dietary<br />
polyunsaturated fatty acids.<br />
Epidemiology<br />
•Enzootic muscular dystrophy occurs in young growing calves, lambs, goat kids,and foals born<br />
to dams in selenium-deficient areas and unsupplemented.Occurs worldwide and common in<br />
Australasia, United Kingdom, Great Plains of North America where soils are deficient in selenium.<br />
Vitamin E deficiency in animals fed poor quality forage and diets high in polyunsaturated fatty<br />
acids. Outbreaks of muscular dystrophy precipitated by exercise.<br />
•Mulberry heart disease in finishing pigs.<br />
•Selenium-responsive diseases occur in Australasia and are not obvious clinically but respond to<br />
selenium supplementation. Selenium and vitamin E deficiency may be involved in reproductive<br />
performance, retained placenta in cattle, resistance to infectious disease like bovine mastitis.<br />
Controversial.<br />
Signs. Muscular dystrophy characterized by groups of animals with stiffness, weakness,<br />
Table 29.5 Diseases considered to be caused by or associated with a deficiency of either selenium<br />
or vitamin E or both (including 'selenium-responsive' diseases)<br />
Cattle Horse Swine<br />
Nutritional<br />
(enzootic)<br />
muscular<br />
dystrophy<br />
Retained fetal<br />
membranes<br />
Resistance to<br />
Nutritional<br />
muscular<br />
dystrophy<br />
Mulberry heart<br />
disease Hepatosis<br />
dietetica<br />
Exudative<br />
diathesis Iron<br />
hypersensitivity<br />
Nutritional<br />
muscular<br />
200<br />
Sheep<br />
Nutritional (enzootic) muscular<br />
dystrorrropf<br />
Reproductive inefficiency<br />
Bone marrow abnormalities<br />
'selenium responsive'
mastitis<br />
1516<br />
dystrophy<br />
Anemia<br />
recumbency, severe in myocardial form.Mulberry heart disease characterized by outbreaks of<br />
sudden death in finishing pigs.<br />
Clinical pathology. Increased plasma levels of creatine kinase. Low serum levels of selenium and<br />
vitamin E. Glutathione peroxidase activity.<br />
Lesions. Bilaterally symmetrical pale skeletal muscle, pale streaks in myocardial muscle. Hyaline<br />
degeneration of affected muscle.<br />
Diagnostic confirmation. Low selenium and vitamin E in diet and tissues, increased creatine<br />
kinase and muscle degeneration.<br />
Differential diagnosis list:<br />
Acute muscular dystrophy in calves and yearlings:<br />
•Haemophilus somnus septicemia (p. 895)<br />
•Pneumonia (p. 443).<br />
Subacute enzootic muscular dystrophy:<br />
•Musculoskeletal diseases-plyarthritis, traumatic or infectious myopathies (blackleg),<br />
osteodystrophy, and fractures of long bones (Chapter 13)<br />
•Diseases of the nervous system-spinal cord compression (p. 543), Haemophilus somnus<br />
meningoencephalitis (pp. 528, 895), and myelitis (p. 546), organophosphatic insecticide poisoning<br />
(p. 1615)<br />
•Diseases of the digestive tract-arbohydrate engorgement resulting in lactic acidosis, shock,<br />
dehydration, and weakness (p. 284).<br />
•Muscular dystrophy in lambs and kids-zootic ataxia and swayback (p. 1495)<br />
•Muscular dystrophy in foals-raumatic injury to the musculoskeletal system and polyarthritis<br />
(Chapter 13); meningitis (pp. 538, 708); traumatic injury to the spinal cord.<br />
Treatment. Vitamin E and selenium parenterally.<br />
Control. Selenium and vitamin E supplementation of diet, strategic oral and/or parenteral vitamin<br />
E and selenium to pregnant dams or young animals on pasture.<br />
ETIOLOGY<br />
The selenium- and vitamin E-responsive or deficiency diseases of farm animals are caused by<br />
diets deficient in selenium and/or vitamin E, with or without the presence of conditioning factors<br />
such as an excessive quantity of polyunsaturated fatty acids in the diet. Almost all of the diseases<br />
that occur naturally have been reproduced experimentally using diets deficient in selenium and/or<br />
vitamin E. Conversely, the lesions can usually be prevented with selenium and vitamin E<br />
supplementation. In certain instances, as for example in hand-fed dairy calves, the incorporation of<br />
excessive quantities of polyunsaturated fatty acids was a major factor in the experimental disease<br />
and this led to the conclusion that certain myopathic agents were necessary to produce the lesion,<br />
which is no longer tenable. The presence of polyunsaturated fatty acids in the diet may cause a<br />
conditioned vitamin E deficiency because the vitamin acts as an antioxidant. In the case of<br />
naturally occurring muscular dystrophy in calves, lambs and foals on pasture, the myopathic agent,<br />
if any, is unknown and selenium is protective. However, selenium is not protective against the<br />
muscular dystrophy associated with the feeding of cod liver oil to calves.<br />
201
Selenium is an essential nutrient for animals, and diseases due to selenium inadequacy in<br />
livestock are of worldwide distribution (1). Selenium is a biochemical component of the enzyme<br />
glutathione peroxidase (GSH-PX). The activity of the enzyme in erythrocytes is positively related<br />
to the blood concentration of selenium in cattle, sheep, horses and swine, and is a useful aid for<br />
the diagnosis of selenium deficiency and to determine the selenium status of the tissues of these<br />
animals. The enzyme from the erythrocytes of both cattle and sheep contains 4 g atoms of<br />
selenium per mol of enzyme (1). Selenium is also a component of thyroid gland hormones.<br />
Plasma GSH-PX protects cellular membranes and lipid-containing organelles from<br />
peroxidative damage by inhibition and destruction of endogenous peroxides, acting in conjunction<br />
with vitamin E to maintain integrity of these membranes (1). Hydrogen peroxide and lipid<br />
peroxides are capable of causing irreversible denaturation of essential cellular proteins, which<br />
leads to degeneration and necrosis. GSH-PX catalyzes the breakdown of hydrogen peroxide and<br />
certain organic hydroperoxides produced by glutathione during the process of redox cycling. This<br />
dependence of GSH-PX activity on the presence of selenium offers an explanation for the<br />
interrelationship of selenium, vitamin E, and sulfur-containing amino acids in animals. The<br />
sulfur-containing amino acids maybe precursors of glutathione, which in turn acts as a substrate<br />
for GSH-PX and maintains sulfhydryl groups in the cell. Selenium is also a component of several<br />
other proteins such as selenoprotein of muscle, selenoflagellin, Se-transport proteins, and the<br />
bacterial enzymes, formate dehydrogenase and glycine reductase. Selenium also facilitates<br />
significant changes in the metabolism of many drugs and xenobiotics. For example, selenium<br />
functions to counteract the toxicity of several metals such as arsenic, cadmium, mercury, copper,<br />
silver, and lead.<br />
Vitamin E is an antioxidant that prevents oxidative damage to sensitive membrane lipids by<br />
decreasing hydroperoxide formation (1). The vitamin has a central role in protection of cellular<br />
membranes from lipoperoxidation, especially membranes rich in unsaturated lipids, such as<br />
mitochondria, endoplasmic reticulum, and plasma membranes.<br />
An important interrelationship exists between selenium, vitamin E, and the sulfur-containing<br />
amino acids in preventing some of the nutritional diseases caused by their deficiency. If vitamin E<br />
prevents fatty acid hydroperoxide formation, and the sulfur amino acids (as precursors of GSH-PX)<br />
and selenium are involved in peroxide destruction, these nutrients would produce a similar<br />
biochemical result, that is, lowering of the concentration of peroxides or peroxide-induced<br />
products in the tissues (1). Protection against oxidative damage to susceptible non-membrane<br />
proteins by dietary selenium, but not by vitamin E, might explain why some nutritional diseases<br />
respond to selenium but not to vitamin E. On the other hand, certain tissues or subcellular<br />
components may not be adequately protected from oxidant damage because they are inherently<br />
low in GSH-PX even with adequate dietary selenium. Damage to such tissues would be expected<br />
to be aggravated by diets high in unsaturated fatty acids and to respond adequately to vitamin E<br />
but not to selenium. The variations in GSH-PX activity between certain tissues, such as liver, heart,<br />
skeletal and myocardial muscles, would explain the variations in the severity of lesions between<br />
species.<br />
There are both selenium-dependent GSH-PX and non-selenium-dependent GSH-PX activities<br />
in the tissues and blood. The non-selenium-dependent enzyme does not contain selenium and does<br />
not react with hydrogen peroxide but shows activity toward organic<br />
202
hydroperoxide substrates. The spleen, cardiac muscle, erythrocytes, brain, thymus, adipose tissue,<br />
and striated muscles of calves contain only the selenium-dependent enzyme. The liver, lungs,<br />
adrenal glands, testes, and kidney contain both enzymes. Hepatic tissue contains the highest level<br />
of non-selenium-dependent enzyme.<br />
EPIDEMIOLOGY<br />
Enzootic nutritional muscular dystrophy (NMD)<br />
Occurrence<br />
This muscular dystrophy occurs in all farm animal species, but most commonly in young, rapidly<br />
growing calves, lambs, goat kids, and foals born from dams that have been fed for long<br />
periods,usually during the winter months, on diets low in selenium and vitamin E (2). It is an<br />
important cause of mortality in goat kids from birth to about 3 months of age(3). Goat kids may<br />
require more selenium than lambs or calves, which may explain the higher incidence of the<br />
disease in kids.The disease in kids may also be associated with low α-tocopherol levels and<br />
normal selenium status (4).<br />
NMD in horses occurs most commonly in foals to about 7 months of age (5). In reported cases,<br />
the concentration of selenium in the blood of the mares was subnormal, the concentrations of<br />
selenium and vitamin E in the feedstuffs were subnormal, the level of unsaturated fatty acids in<br />
the feed was high and vitamin E and selenium supplementation prevented the disease. The disease<br />
is not well-recognized in adult horses, but sporadic cases of dystrophic myodegeneration are<br />
recorded in horses from 5 to 10 years of age (5). Some baseline data for selenium and vitamin E<br />
concentration in horses from breeding farms is available (6).<br />
The disease also occurs in grain-fed yearling cattle. Stressors such as being turned outdoors<br />
after winter housing, walking long distances, the jostling and movement associated with<br />
vaccination and dehorning procedures and the like are often precipitating factors. The disease has<br />
occurred in steers and bulls 12-18 months of age under feedlot conditions. There may even be<br />
laboratory evidence of subclinical myopathy in normal animals in a group from which an index<br />
case occurred. Outbreaks of severe and fatal NMD have occurred in heifers at the time of<br />
parturition which were previously on a diet deficient in both selenium and vitamin E. The disease<br />
may also occur sporadically in adult horses that are deficient in selenium.<br />
There are two major syndromes:<br />
•An acute form - myocardial dystrophy, which occurs most commonly in young calves and lambs,<br />
and occasionally foals<br />
•A subacute form - skeletal muscular dystrophy, which occurs in older calves and yearling cattle.<br />
The two forms are not mutually exclusive.<br />
Geographical distribution<br />
NMD occurs in most countries of the world but is common in the United Kingdom, the United<br />
States, Scandinavia, Europe, Canada, Australia, and New Zealand. In North America, it is<br />
common in the northeast and northwest and uncommon on the relatively high selenium soils of the<br />
Great Plains, where selenium toxicity has occurred. It is one of most common deficiency diseases<br />
of farm livestock in the United States (7). Soils, and therefore the pastures they earn vary widely<br />
in their selenium content, depending largely on their geological origin. In general, soils derived<br />
from rocks of recent origin, e.g. the granitic and pumice sands of New Zealand, are notably<br />
deficient in selenium. Soils derived from igneous rocks are likely to be low in selenium.<br />
Sedimentary rocks, which are the principal parent material of agricultural soils, are richer in<br />
203
selenium. Forage crops, cereal grains and corn grown in these areas are usually low in selenium<br />
content (below 0.1 mg/kg dry matter (DM)), compared to the concentration in crops (above 0.1<br />
mg/kg DM) grown in areas where the available soil selenium is much higher and usually adequate.<br />
The disease occurs in pigs, usually in association with other more serious diseases, such as<br />
mulberry heart disease and hepatosis dietetica.<br />
Selenium in soil and animals<br />
In the United States, the States of the Pacific northwest and of the northeastern and southeastern<br />
seaboard are generally low in selenium (2). In Canada, western prairie grains generally contain<br />
relatively high levels of selenium, whereas in the eastern provinces, soils and feedstuffs usually<br />
have low selenium concentrations. Most soils in the Atlantic provinces of Canada are acidic and,<br />
consequently, the forages are deficient in selenium. Most forage samples contain less than 0.10<br />
mg/kg DM of selenium, and enzootic nutritional muscular dystrophy is common throughout the<br />
region.<br />
Surveys in the United Kingdom found that the selenium status may be low in sheep and cattle<br />
fed locally produced feedstuffs without any mineral supplementation. In some surveys, up to 50%<br />
of farms are low in selenium, which places a large number of animals at risk. There are also<br />
differences in the selenium concentrations of different feeds grown in the same area. For example,<br />
in some areas 75% of cattle fed primarily corn silage, or 50% of the cattle fed sedge hay, might be<br />
receiving diets inadequate in selenium.<br />
There may be wide variations in the serum selenium concentrations and glutathione peroxidase<br />
activities in cattle grazing forages of various selenium concentrations within the same<br />
geographical area. The selenium status of beef cows can vary between geographical areas within a<br />
region of a country, which is likely due to variations in selenium concentration of the soil and<br />
plants in these areas (8). Beef herds from areas with adequate soil levels of selenium, herds<br />
provided with supplemental feed on pasture, and herds in which pregnancy diagnosis was done,<br />
had higher average herd blood selenium values than other herds (8).<br />
Several factors influence the availability of soil selenium to plants.<br />
•Soil pH - alkalinity encourages selenium absorption by plants and the presence of a high level of<br />
sulfur,which competes for absorption sites with selenium in both plants and animals,are two<br />
factors reducing availability<br />
•Variation between plants in their ability to absorb selenium; ‘selector' and ‘converter'plants are<br />
listed under the heading of selenium poisoning;legumes take up much less selenium than do<br />
grasses<br />
•Seasonal conditions also influence the selenium content of pasture, the content being lowest in<br />
the spring and when rainfall is heavy. Blood selenium in dairy cows in the United States were<br />
lower during the summer and fall than during the winter and spring (9).<br />
In this way a marginally deficient soil may produce a grossly deficient pasture if it is heavily<br />
fertilized with superphosphate, thus increasing its sulfate content, if the rainfall is heavy and the<br />
sward is lush and dominated by clover as it is likely to be in the spring months.<br />
Environmental sulfur from various anthropogenic activities has been suspected to be a<br />
significant factor in contributing to several health problems in livestock (10). Livestock producers<br />
near natural sour gas desulfurization plants have reported that sulfur emissions are responsible for<br />
an increased occurrence of nutritional muscular dystrophy, weak calves, and retarded growth.<br />
Experimentally, a moderate increase in dietary sulfur does not impair selenium and copper status,<br />
204
or cause related disease in cattle (10).<br />
Vitamin E<br />
Vitamin E deficiency occurs most commonly when animals are fed inferior quality hay or straw or<br />
root crops. Cereal grains, green pasture, and well-cured fresh hay contain adequate amounts of the<br />
vitamin.<br />
α-Tocopherol levels are high in green grasses and clovers, but there are wide variations in the<br />
concentrations from one area to another. The serum tocopherol levels are higher in calves born<br />
from cows fed grass silage than in those born from cows fed the same grass as hay. Many factors<br />
influence the tocopherol content of pasture and hence the animals' intake. The level of tocopherol<br />
in pasture declines by up to 90% as it matures. Levels as low as 0.7 mg/kg DM have been reported<br />
in dry summer pastures grazed by sheep. The α-tocopherol content of rye-grass and clover pasture<br />
ranges from 22 to 350 and 90 to 210 mg/kg DM, respectively. After harvesting and storage, the<br />
tocopherol content of pasture and other crops may fall further, sometimes to zero. Preservation of<br />
grain with propionic acid does not prevent the decline. Thus, the dietary intake of α-tocopherol by<br />
cattle and sheep may be expected to vary widely and lead to wide variations in tissue levels. The<br />
plasma vitamin E status of horses is highest from May to August in Canada when fresh grass is<br />
being grazed and lowest when the horses are being fed harvested or stored feed during the same<br />
period (11). Plasma vitamin E levels in dairy cows in the United States were higher during the<br />
summer and fall than during the winter and spring (9).<br />
Outbreaks of NMD may occur in yearling cattle fed on high-moisture grain treated with<br />
propionic acid as a method of inexpensive storage and protection from fungal growth. There is a<br />
marked drop in the vitamin E content of acid-treated grain, and an increase in the levels of<br />
peroxides of fat, which is consistent with a loss of naturally occurring antioxidants such as the<br />
tocopherols (secondary vitamin E deficiency). In these situations, the levels of selenium in the<br />
feed were below 0.05 mg/kg DM, which is inadequate and emphasizes the interdependence of<br />
selenium and vitamin E. The tocopherol content of moist grain (barley and maize) stored for 6<br />
months, with or without propionic acid, falls to extremely low levels compared to conventionally<br />
stored grain in which the tocopherol levels usually persist over the same length of time.<br />
Selenium-deficient barley treated with sodium hydroxide to deplete it of vitamin E can be used to<br />
induce NMD when fed to yearling cattle. The disease may occur in sucking lambs with low<br />
plasma α-tocopherol levels and an adequate selenium status, which indicates that the sparing<br />
effect of each nutrient may not occur over the broad spectrum of clinical deficiencies.<br />
Polyunsaturated fatty acids (PUFAs) in diet<br />
Diets rich in PUFA such as cod liver oil,other fish oils, fishmeal used as a protein<br />
concentrate, lard, linseed oil, soybean and corn oils have been implicated in the production of<br />
NMD, particularly in calves fed milk replacers containing these ingredients. The disease can be<br />
reproduced experimentally in young ruminant cattle 6-9 months of age, by feeding a diet low in<br />
vitamin E and selenium, and adding a linolenic acid. There are widespread<br />
lesions of myodegeneration of skeletal and myocardial muscles (12). Fresh spring grass containing<br />
a sufficient concentration of linolenic acid to equal the amount necessary to produce NMD in<br />
calves may explain the occurrence of the naturally occurring disease in the spring months. The<br />
oxidation during rancidification of the oils causes destruction of the vitamin ,thus increasing the<br />
dietary requirements (a conditioned vitamin E deficiency), and the presence of myopathic agents<br />
in the oils may also contribute to the occurrence of the disease. A secondary vitamin E deficiency<br />
205
occurs when NMD develops on rations containing vitamin E in amounts ordinarily considered to<br />
be adequate, but the disease is prevented by further supplementation with the vitamin. The lack of<br />
specificity of vitamin E in the prevention of muscular dystrophy in some circumstances is<br />
indicated by its failure, and by the efficiency of selenium, as a preventive agent in lambs on lush<br />
legume pasture.<br />
Other myopathic agents in diet<br />
Not all of the myopathic agents that maybe important in the development of NMD in farm animals<br />
have been identified. Unsaturated fatty acids in fish and vegetable oils may be myopathic agents in<br />
some outbreaks of NMD of calves and lambs. Lupinosis-associated myopathy in sheep is a<br />
substantial skeletal muscle myopathy encountered in weaner sheep grazing lupin stubbles infected<br />
with the fungus Phomopsis spp. (13). Affected sheep have a stiff gait, walk reluctantly, stand with<br />
their back humped and their feet under the body.and have difficulty getting to their feet.<br />
Unaccustomed exercise<br />
Historically, NMD occurred most commonly in rapidly growing, well-nourished beef calves 2-4<br />
months of age, shortly following unaccustomed exercise. This was commonplace in countries<br />
where calves were born and raised indoors until about 6-8 weeks of age when they were turned<br />
out onto new pasture in the spring of the year. This has been a standard practice in small beef<br />
herds in the United Kingdom, Europe, and North America. A similar situation applies for ewes<br />
that lambed indoors and the lambs were let out to pasture from 1 to 3 weeks of age. Thus,<br />
unaccustomed activity in calves and lambs running and frolicking following their turnout onto<br />
pasture is an important risk factor but is not necessarily a prerequisite for the disease. In lambs, the<br />
vigorous exertion associated with running and sucking may account for the peracute form of<br />
myocardial dystrophy in young lambs on deficient pastures and from deficient ewes. In older<br />
lambs up to 3 months of age, outbreaks of acute NMD and stifflamb disease may be associated<br />
with the driving of flocks long distances. A similar<br />
1519<br />
situation applies for calves that are moved long distances from calving grounds and early spring<br />
pastures to lush summer pastures. The wandering and bellowing that occurs in beef calves weaned<br />
at 6-8 months of age may precipitate outbreaks of subacute NMD. Degenerative myopathy of<br />
yearling cattle (feedlot cattle, housed yearling bulls and heifer replacements) is now being<br />
recognized with increased frequency (14). The disease resembles subacute NMD of calves, and in<br />
the United Kingdom is often seen when yearlings are turned outdoors in the spring of the year<br />
after being housed during the winter and fed a poor quality hay or straw or propionic acid-treated<br />
grain. Unaccustomed exercise is a common precipitating factor. However, the disease has<br />
occurred in housed yearling bulls with no history of stress or unaccustomed exercise but whose<br />
diet was deficient in selenium and vitamin E.<br />
In horses subjected to exercise there is an increase in erythrocyte malondialdehyde, a product of<br />
peroxidation, but selenium supplementation has no beneficial effect. There is inconclusive<br />
evidence that a selenium-vitamin E deficiency causes NMD in adult horses. There is no evidence<br />
that paralytic myoglobinuria and the 'tying-up' syndrome are due to a deficiency of selenium and<br />
vitamin E.<br />
Congenital nutritional muscular dystrophy<br />
Congenital NMD is rare in farm animals. Isolated cases have been reported but not<br />
well-documented. Similarly, NMD can occur in calves and lambs only a few days of age but<br />
206
arely. Selenium readily crosses the bovine placenta and fetal selenium is always higher than the<br />
maternal status (15). There is no evidence that the weak-calf syndrome is associated with selenium<br />
deficiency (16). Long-term parenteral supplementation with neither selenium alone nor in<br />
combination with vitamin E had any effect on the incidence of the weak-calf syndrome.<br />
In pigs, NMD has been produced experimentally on vitamin E - and selenium-deficient rations<br />
but is usually only a part of the more serious complex of mulberry heart disease and hepatosis<br />
dietetica.<br />
Vitamin E-Selenium Deficiency (VESD) syndrome<br />
Mulberry heart disease, hepatosis dietetica, exudative diathesis and nutritional myopathy,<br />
also known as the VESD syndrome (vitamin E and selenium deficiency), occurs naturally in<br />
rapidly growing pigs, usually during the postweaning period (3 weeks to 4 months), particularly<br />
during the finishing period. It is usually associated with diets deficient in both selenium and<br />
vitamin E and those that may contain a high concentration of unsaturated fatty acids. Such diets<br />
include those containing mixtures of soybean, high-moisture corn, and the cereal grains grown on<br />
soils with low levels of selenium. The feeding of a basal ration of cull peas, low in selenium and<br />
vitamin E, to growing pigs can cause the typical syndrome, and low tissue levels of selenium are<br />
present in pigs with spontaneously occurring hepatosis dietetica. However, there are reports of<br />
naturally occurring cases of mulberry' heart disease of swine in Scandinavia in which the tissue<br />
levels of selenium and vitamin E are within normal ranges compared to normal pigs (17). In<br />
Ireland, in spite of supplementation of pig rations with vitamin E and selenium at levels higher<br />
than that necessary to prevent experimental disease, spontaneous mulberry heart disease may still<br />
occur (18). Affected pigs have lower tissue vitamin E levels than control pigs, which suggests an<br />
alteration in а-tocopherol metabolism unrelated to dietary selenium and PUFA contents.<br />
Natural occurrence of the disease complex in swine is not uncommonly associated with diets<br />
containing 50% coconut meal, fish-liver oil emulsion, fish scraps with a high content of<br />
unsaturated fatty acids, or flaxseed, which produces yellow and brown discoloration of fat<br />
preventable by the incorporation of adequate amounts of а-tocopherol or a suitable antioxidant.<br />
The quality of the dietary fat does not necessarily influence blood vitamin E levels, but the<br />
presence of oxidized fat reduces the resistance of the red blood cells against peroxidation. The<br />
higher requirement for vitamin E by pigs fed oxidized fat may be due to the low vitamin E content<br />
in such fat.<br />
Mulberry heart disease<br />
This is the most common form of selenium and vitamin E deficiency of swine. It occurs most<br />
commonly in rapidly growing feeder pigs (60-90 kg) in excellent condition being fed on a<br />
high-energy diet low in vitamin E and selenium. The diets most commonly incriminated are<br />
soybean, corn, and barley. The а-tocopherol content of corn is usually low and it is virtually<br />
absent from solvent-extracted soybean meal. Both are low in selenium. The use of high-moisture<br />
corn may further exacerbate the tocopherol deficiency. The level of PUFAs in the diet was thought<br />
to be an important etiological factor but this is now not considered to be a necessary prerequisite.<br />
Outbreaks of the disease may occur in which 25% of susceptible pigs are affected, and the case<br />
mortality rate is about 90%. The disease has occurred in young piglets and in adult sows.<br />
Hepatosis dietetica<br />
Hepatosis dietetica appears to be less common than mulberry heart disease but the<br />
epidemiological characteristics are similar. It affects young growing pigs up to 3-4 months of age.<br />
207
NMD in swine usually occurs in cases of mulberry heart disease and hepatosis dietetica but it has<br />
occurred alone in gilts (11-12 months of age) 48 hours after farrowing. The gilts had been fed on a<br />
diet of barley and lupin seed which contained only 0.03 mg/kg of selenium.<br />
Selenium-responsive unthriftiness<br />
In New Zealand, a variety of diseases have been known as selenium-responsive diseases (19),<br />
because they respond beneficially to the strategic administration of selenium. These include<br />
ill-thrift in lambs and calves on pasture, ewe infertility, and diarrhea in older calves and<br />
lactating ewes. The pathogenesis of these selenium-responsive diseases is not known but it would<br />
appear that the selenium deficiency is only marginal. Most investigations into selenium-responsive<br />
diseases have occurred in selenium-deficient areas in which diseases such as NMD of calves and<br />
lambs occur (19). The evidence that selenium deficiency in breeding ewes can result in a decline<br />
in reproductive performance has not been substantiated experimentally. Reproductive performance<br />
was not affected in ewes on a selenium-depleted diet. A recent report indicated that<br />
selenium-responsive infertility in ewes may be present when the whole blood levels of selenium<br />
are below 10 ng/mL (12.7 nmol/L) (19).<br />
Selenium-responsive unthriftiness in sheep has received considerable attention in New Zealand<br />
where the response to selenium administration<br />
has been most dramatic compared to Australia where the syndrome has also been recognized but<br />
where the response is much smaller. The oral administration of selenium to lambs in these areas<br />
results in greater body weight gains from weaning to 1 year of age compared to lambs not<br />
receiving selenium supplementation (19). The mean fleece weight of selenium-treated lambs is<br />
also greater.<br />
The diagnosis of selenium-responsive unthriftiness depends on analyses of the soil, pasture and<br />
animal tissues for selenium, and response trials to selenium supplementation. A deficiency state<br />
might be encountered when the selenium content of the soil is below 0.45 mg/kg, the pasture<br />
content below 0.02 mg/kg DM, the liver content below 21ug/kg (0.27 µmol/kg) (WW) and wool<br />
concentrations below 50-60µg/kg (0.63-0.76 µmol/kg). For the blood in selenium-responsive<br />
unthriftiness of sheep the following criteria are suggested (19):<br />
•Mean blood selenium<br />
•Selenium status (ug/dL)<br />
Deficient = 1.0<br />
•Doubtful 1.1-1.9<br />
•Normal~2.0.<br />
The GSH-PX activity is a good index of the selenium status of sheep with a<br />
selenium-responsive disease. If measured on a regular basis, it can provide an indication of the<br />
selenium status of grazing sheep in individual flocks. Single measurements of GSH-PX activity<br />
may fail to detect recent changes in grazing area, differences in pasture species and pasture<br />
composition, and alterations in the physiological state of the animals.<br />
Subclinical selenium insufficiency<br />
Subclinical insufficiencies of selenium in grazing ruminants are widespread over large areas of<br />
southern Australia (20). The plasma concentrations of affected sheep flocks are low, there are no<br />
obvious clinical signs of insufficiency in the ewes, and there are significant responses in wool<br />
production and fiber diameter to selenium supplementation. The incidence of estrus and fertility is<br />
not affected by selenium supplementation (21). Liveweights at birth, in mid-lactation and at<br />
208
weaning were increased in lambs born to selenium-supplemented and crossbred ewes, and in<br />
lambs born as singletons (22).<br />
Clean fleece weight at 10 months of age was increased by 9.5% and fiber diameter by 0.3um in<br />
lambs born to ewes that had received supplementary selenium. Differences in fleece weight and<br />
liveweight were not detected at 22 months, suggesting that subclinical selenium insufficiency in<br />
early life did not permanently impair productivity if selenium status subsequently increased.<br />
Selenium is a component of type-I iodothyronine deiodinase, which catalyzes the extrathyroidal<br />
conversion of thyroxine (T4) to the more active triiodothyronine (T3). Sheep grazing pastures low<br />
in selenium frequently have higher circulating T4 and lower circulating T3 concentrations than<br />
sheep receiving selenium supplementations.<br />
When ewes grazing pastures low in selenium were supplemented thiocyanate (to cause iodine<br />
insufficiency), iodide and selenium, there was no evidence of clinical deficiencies (23). Growth<br />
rates of lambs were not affected by thiocyanate of their dams during midpregnancy, but plasma T3<br />
and T4 concentrations were depressed in ewes receiving thiocyanate. The iodide supplementation<br />
increased thyroid hormone concentrations in ewes, but depressed plasma T3 concentrations in<br />
lambs. Supplementation of sheep grazing pastures low in selenium with both selenium and thyroid<br />
hormones improved wool characteristics, liveweight gain, and blood selenium, but there was no<br />
evidence of an interaction between the selenium and the hormones (24). Thus it seems unlikely<br />
that the decline in the quantity of T3 produced, or of T4 utilized for T3 production, in<br />
selenium-deficient sheep is responsible for the observed differences in the productivity of<br />
selenium-deficient and supplemented sheep. The thyroids have a major role in regulating<br />
thermogenesis, and lambs born to ewes supplemented with iodide tend to have higher rectal<br />
temperatures during cold stress (25). The thermoregulatory ability of the perinatal lamb is not<br />
adversely affected by subclinical selenium deficiency.<br />
Reproductive performance<br />
The published information on the effects of vitamin E and selenium deficiency or of dietary<br />
supplementation with one or the other or both on reproductive performance in farm animals are<br />
conflicting and controversial. Reproductive performance is complex and dependent on the<br />
interaction of many factors. Reproductive inefficiency is likewise complex, and it is difficult to<br />
isolate one factor like a deficiency of vitamin E or selenium as a cause of reproductive<br />
inefficiency. Conversely, it is difficult to prove that supplementation with these nutrients will<br />
insure optimum reproductive performance.<br />
Sheep<br />
The evidence about the effect of selenium and vitamin E deficiency on reproductive performance<br />
in sheep is conflicting. Observations in the 1960s concluded that selenium deficiency caused<br />
embryonic deaths 20-30 days after fertilization in ewes. But supplementation of ewes, low or<br />
marginal in selenium status, with selenium did not improve reproductive performance.<br />
Experimental studies using selenium-deficient diets in ewes have been unable to find any adverse<br />
effect of selenium depletion on ewe conception rates, embryonic mortality or numbers of lambs<br />
born. The parenteral administration of selenium to pregnant ewes between 15 and 35 days after<br />
mating resulted in a reduced embryonic survival rate and is not recommended during the first<br />
month of pregnancy (26).<br />
Cattle<br />
209
The importance of selenium and vitamin E for the maintenance of optimum reproductive<br />
performance is not clear. The IM injection of dairy cattle with selenium and vitamin E 3 weeks<br />
prepartum did not have any effect on average days to first estrus or first service, average days to<br />
conception, services per conception, or number of uterine infusions required. The prepartum IM<br />
injection of vitamin E and selenium 3 weeks prepartum increased the percentage of cows pregnant<br />
to first service, reduced the number of services per conception, decreased the incidence of retained<br />
placenta, and reduced the interval from calving to conception (27). In a randomized field trial in a<br />
large dairy herd in the United States, oral supplementation of pregnant first-calf dairy heifers with<br />
selenium using a commercially available sustained-release intraruminal selenium bolus, increased<br />
blood selenium concentrations in treated animals at 30 days after treatment until after calving (28).<br />
However, based on data analyzed midlactation and late lactation, there were no differences<br />
between treated and control groups in somatic cell count, days not pregnant, total milk production,<br />
or times bred. The use of an intra-ruminal pellet of selenium at two different levels in dairy herds<br />
in New Zealand was evaluated in yearling heifers (29). The recommended dose was effective in<br />
elevating whole blood GSH-FX activity and selenium concentrations to over 10 times those of<br />
control animals. Milk production was increased and there was a trend to decreased somatic cell<br />
counts. There were no differences in calving-first-service or calving-conception intervals, or in the<br />
percentage of animals pregnant to first or all services. In other observations, following the<br />
treatment of dairy cows with oral selenium pellets there was an improvement in first service<br />
conception rate and significantly higher blood levels of GSH-PX. The inconsistent results<br />
obtained following the use of selenium and vitamin E in pregnant cows may be related to the<br />
selenium status of the animals; in some herds the blood levels are marginal and in others the levels<br />
are within the normal range.<br />
Retained fetal placenta<br />
A high incidence (more than 10%) of retained fetal membranes has been associated with marginal<br />
levels of plasma selenium compared with herds without a problem. In some cases, the incidence<br />
could be reduced to below 10% by the injection of pregnant cattle with selenium and vitamin E<br />
about 3 weeks prepartum, while in other studies similar prepartum injections neither reduced the<br />
incidence nor improved reproductive performance. A single injection of selenium 3 weeks<br />
prepartum can reduce the number of days postpartum required for the uterus to reach minimum<br />
size and to reduce the incidence of metritis and cystic ovaries during the early postpartum period.<br />
The parenteral administration of a single injection of 3000 mg vitamin E prepartum to dairy cows<br />
of all ages decreased the incidence of retained placenta and metritis to 6.4% and 3.9%,<br />
respectively, in the treated group, compared to 12.5% and 8.8%, in the control group (30). The<br />
injection, 20 days prepartum, of 50 mg of selenium and 680 IU of vitamin E reduced the incidence<br />
of retained fetal membranes in one series, but did not in another series. The plasma selenium<br />
concentration at parturition ranged from 0.02 to 0.05 ppm in control cows in winch there was an<br />
incidence of 51% retained membranes, and from 0.08 to 0.1 ppm in treated cows in which the<br />
incidence was reduced to 9%. A dietary level of 0.1 mg/kg DM selenium is recommended to<br />
minimize the incidence of the problem. The complex nature of the etiology of retained fetal<br />
membranes also requires a well-designed experimental trial to account for all of the possible<br />
factors involved.<br />
Resistance to infectious disease<br />
Many studies have examined the role of selenium and vitamin E resistance to infectious disease<br />
210
(31). Most of the evidence is based on in vitro studies of the effects of deficiencies of selenium or<br />
vitamin E or supplementation with the nutrients on leukocyte responses to mitogens, or on the<br />
antibody responses of animals to a variety of pathogens. The status of selenium and vitamin E in<br />
an animal can alter; antibody response, phagocytes function, lymphocyte response, and resistance<br />
to infectious disease (31). In general, a deficiency of selenium results in immunosuppression, and<br />
supplementation with low doses of selenium augments immunological functions. A deficiency of<br />
selenium has been shown to inhibit:<br />
• Resistance to microbial and viral infections<br />
• Neutrophil function<br />
• Antibody production<br />
• Proliferation of T and B lymphocytes in response to mitogens<br />
•Cytodestruction of T lymphocytes and natural killer lymphocytes (32).<br />
Vitamin E and selenium have interactive effects on lymphocyte responses to experimental<br />
antigens (33).<br />
Neutrophil function<br />
Selenium deficiency can affect the function of polymorphonuclear neutrophils (PMNs), which are<br />
associated with physiological changes in GSH-PX levels. In calves on an experimental<br />
selenium-deficient diet, the oxygen consumption and the activities of GSH-PX are lower than<br />
normal in neutrophils. The feeding of 80-120 mg of selenium/kg of mineral mixture provided ad<br />
libitum is an effective method of increasing blood selenium in a group of cattle and optimizing the<br />
humoral antibody response experimentally. It is suggested that blood selenium levels over 100<br />
(Jg/L are necessary to maintain optimum immunocompetence in growing beef cattle (34). In<br />
selenium-deficient goats, the production of leukotriene B4, a product of neutrophil arachidonic<br />
acid lipoxygenation and a potent chemotactic and chemokinetic stimulus for neutrophils, is<br />
decreased, resulting in dysfunction of the neutrophils. A deficiency of selenium in pregnant sows<br />
impairs neutrophil function, and vitamin E deficiency impairs function of both neutrophils and<br />
lymphocytes, which may result in increased susceptibility of their piglets to infectious diseases<br />
(35). It is suggested that selenium supplementation be maintained at 0.3 mg/kg of the diet.<br />
Immune response<br />
The effects of selenium deficiency and supplementation on the immune response of cattle to<br />
experimental infection with the infectious bovine rhinotracheitis virus, and sheep to<br />
parainfluenza-3 virus indicate that a deficiency can affect the humoral response and<br />
supplementation enhances the response. Pigs fed a vitamin E and selenium-deficient diet develop<br />
an impaired cell-mediated immunity as measured by lymphocyte response to mitogenic<br />
stimulations. Supplementation of the diets of young swine with selenium at levels above those<br />
required for normal growth has increased the humoral response, but not in sows. The wide<br />
variations in antibody responses that occur in these experiments indicate that there is a complex<br />
relationship between the selenium status of the host, humoral immune responses, and protective<br />
immunity. The concept of using selenium supplementation to enhance antibody responses in sheep<br />
to vaccines is probably unfounded.<br />
Vitamin E can stimulate the immune defense mechanisms in laboratory animals and cattle,<br />
experimentally (36). In most cases, the immunostimulatory effects of additional vitamin E are<br />
associated with supplementation in excess of levels required for normal growth. The parenteral<br />
administration to calves of 1400 mg of vitamin E weekly increases their serum vitamin E<br />
211
concentrations and lymphocyte stimulation indices. Similarly in growing pigs, a serum vitamin E<br />
concentration above 3 mg/L was necessary to achieve a significant response of the lymphocytes to<br />
stimulation with mitogens.<br />
General resistance<br />
These changes may render selenium-deficient animals more susceptible to infectious disease, but<br />
there is no available evidence to indicate that naturally occurring selenium and vitamin E<br />
deficiencies are associated with an increase in the incidence or severity of infectious diseases.<br />
Neutrophils from selenium-deficient animals lose some ability to phagocytose certain organisms,<br />
but how relevant this observation is in naturally occurring infections is unclear. Field studies of<br />
the incidence and occurrence of pneumonia in housed calves found that selenium status was not a<br />
risk factor.<br />
Neonatal morbidity and mortality<br />
Based on some preliminary observations of the selenium content of hair samples of young calves,<br />
higher selenium levels in newborn calves may have some protective effect against morbidity due<br />
to neonatal disease. Similarly, neonatal piglets with high blood levels of GSH-PX activity may be<br />
more resistant to infectious diseases or other causes of neonatal mortality. Administration of<br />
vitamin E and selenium to dairy cows in late pregnancy resulted in the production of increased<br />
quantities of colostrum and the calves have increased quantities of GSH-PX at birth and 28 days<br />
of age, but the improved selenium status did not provide any improvement in passive immunity or<br />
growth (37). Supplementing selenium to beef cows grazing selenium-deficient pastures with a salt<br />
mineral mix containing 120 mg selenium/kg of mix increased the selenium status of the cows and<br />
increased the serum IgG concentration, or enhanced transfer of IgG from serum to colostrum and<br />
increased the selenium status of the calves (38). The parenteral administration of 0.1 mg Se and 1<br />
mg ot vitamin E/kg BW at midgestation did not affect the production of systemic or colostrai<br />
antibodies. Supplementation of dairy cows at dry-off with selenium at 3 mg/d as selenite via an<br />
intrarurninal bolus resulted in sufficient transfer of selenium to meet a target concentration of<br />
more than 2.2 p.g of selenium/g of liver DM in newborn calves (39).<br />
Mastitis in dairy cattle<br />
There is some evidence that a dietary deficiency of vitamin E may be associated with an<br />
increased incidence of mastitis in dairy cattle (40). An increased incidence of mastitis during the<br />
early stages of lactation coincides with the lowest plasma concentration of vitamin E.<br />
Supplementation of the diet of dairy cows beginning 4 weeks before and continuing for up to 8<br />
weeks after parturition with vitamin E at 3000 IU/cow/d combined with an injection of 5000 IU, 1<br />
week before parturition, prevented the suppression of blood neutrophil and macrophage function<br />
during the early postpartum period compared to controls (40). The vitamin E prevented the<br />
suppression of blood neutrophils during the postpartum period (41). Cows in both the treated and<br />
control groups were fed diets containing selenium at 0.3 ppm of total dry matter. When selenium<br />
status in dairy cows is marginal, plasma concentrations of a-tocopherol should be at least 3 µg/mL<br />
(42). Cows receiving a dietary supplement of about 1000 IU/d of vitamin E had 30% less clinical<br />
mastitis than did cows receiving a supplement of 100 lU/d of vitamin E (42). The reduction was<br />
88% when cows were fed 4000 IU/d of vitamin E during the last 14 days of the dry period (42).<br />
The selenium status of dairy cows may also have an effect on the prevalence of mastitis and<br />
mammary gland health (43, 44). Dairy herds with low somatic cell counts had significantly higher<br />
mean blood GSH-PX and higher whole blood concentrations of selenium than in herds with high<br />
212
somatic cell counts (44). The prevalence of infection due to Streptococcus agalactiac and<br />
Staphylococcus aureus was higher in herds with the high somatic cell counts compared to those<br />
with the low somatic cell counts. This suggests that phagocytic function in the mammary gland<br />
may be decreased by a marginal selenium deficiency. In a survey of cattle in herds in Switzerland,<br />
those with chronic mastitis had lower serum levels of selenium than healthy control herds (45).<br />
Experimental coliform mastitis in cattle is much more severe in selenium-deficient animals than<br />
selenium-adequate animals (46). The severity was in part due to the increased concentrations of<br />
eicosanoids.<br />
Milk neutrophils from cows fed a selenium-deficient diet have significantly reduced capacity to<br />
kill ingested Escherichia coli and Staph. aureus, compared to cells from cows fed a<br />
selenium-supplemented diet (47). However, other experimental results are not as convincing.<br />
Blood abnormalities<br />
In young cattle from areas where NMD is endemic, and particularly at the end of winter housing,<br />
the erythrocytes have an increased susceptibility to hemolysis following exposure to hypotonic<br />
saline. During clinical and subclinical white muscle disease in calves, there is a significant<br />
increase in both the osmotic and the peroxidative hemolysis of the erythrocytes. This defect is<br />
thought to be the result of alterations in the integrity of cell membranes of which tocopherols are<br />
an essential component. Abnormalities of the bone marrow associated with vitamin E deficiency<br />
in sheep have been described, and abnormal hematological responses have been described in<br />
young growing pigs on an experimental selenium and vitamin E deficient diet. Vitamin E<br />
deficiency in sheep results in increased hemolytic susceptibility of erythrocytes, which may<br />
provide a basis for a single functional test for vitamin E deficiency in sheep (48).<br />
Anemia characterized by a decreased packed cell volume, decreased hemoglobin concentration,<br />
and Heinz body formation has been observed in cattle grazing on grass grown on peaty muck soils<br />
in the Florida everglades. Selenium supplementation corrected the anemia, prevented Heinz body<br />
formation, increased the body weight of cows and calves, and elevated blood selenium.<br />
Equine degenerative myeloencephalopathy<br />
Equine degenerative myeloencephalopathy, which may have an inherited basis (49), has been<br />
associated with a vitamin E deficiency. The vitamin E status is low in some affected horses and<br />
supplementation with the vitamin was associated with a marked reduction in the incidence of the<br />
disease. However, scrum vitamin E and blood GSH-PX activities determined in horses with<br />
histologically confirmed diagnosis of the disease compared to age-matched controls failed to<br />
reveal any differences, and the findings did not support a possible role for vitamin E deficiency as<br />
a cause (50). Foals sired by a stallion with degenerative myeloencephalopathy and with<br />
neurological deficits consistent with the disease during their first year of life had lower plasma<br />
levels of a-tocopherol when the levels were determined serially beginning at 6 weeks to 10 months<br />
of age than age-matched controls (51). Absorption tests with vitamin E revealed that the lower<br />
a-tocopherol levels were not due to an absorption defect (51). The protocol for the oral vitamin E<br />
absorption test has been reported (52).<br />
Equine motor neuron disease<br />
This a neurodegenerative disease of the somatic lower motor neurons resulting in a syndrome of<br />
diffuse neuromuscular disease in the adult horse (53). Case-control studies found the mean plasma<br />
vitamin E concentrations in affected horses were lower than that of control horses. Adult horses<br />
are affected with the risk peaking at 16 years of age. In addition to the role of vitamin E depletion,<br />
213
other individual and farm-level factors, contribute to the risk of developing the disease.<br />
Generalized steatitis<br />
Steatitis in farm animals and other species may be associated with vitamin E and/or selenium<br />
deficiency. Most cases in horses have involved nursing or recently weaned foals. Generalized<br />
steatitis in the foal has been described as either generalized cachexia due to steatitis alone, or as a<br />
primary myopathy or myositis with steatitis of secondary importance. The terms used have<br />
included steatitis, generalized steatitis, fat necrosis, yellow fat disease, polymyositis, and muscular<br />
dystrophy. The relationships between steatitis and vitamin E and selenium deficiency in the horse<br />
are not clear and there may be none. Many more clinical cases must be examined in detail before a<br />
cause-effect relationship can be considered.<br />
PATHOGENESIS<br />
Dietary selenium, sulfur-containing amino acids and vitamin E act synergistically to protect<br />
tissues from oxidative damage (1). GSH-PX, which is selenium-dependent, functions by<br />
detoxifying lipid peroxides and reducing them to nontoxic hydroxy fatty acids. Vitamin E prevents<br />
fatty acid hydroperoxide formation. High levels of PUFAs in the diet increase the requirements for<br />
vitamin E and, with an inadequate level of selenium in the diet, tissue oxidation occurs, resulting<br />
in degeneration and necrosis of cells. Vitamin E protects cellular membranes from<br />
lipoperoxidation, especially membranes rich in unsaturated lipids, such as mitochondric,<br />
endoplasmic reticulum, and plasma membranes. Thus dietary PUFA are not a prerequisite for the<br />
disease. Diets low in selenium and/or vitamin E do not provide sufficient protection against the<br />
'physiological' lipoperoxidation that occurs normally at the cellular level.<br />
The relative importance of selenium, vitamin E and sulfur-containing amino acids in providing<br />
protection in each of the known diseases caused by their deficiency is not clearly understood.<br />
Selenium has a sparing effect on vitamin E and is an efficient prophylactic against muscular<br />
dystrophy of calves and lambs at pasture, but does not prevent muscular dystrophyin calves fed on<br />
a diet containing cod liver oil. The current understanding of the biochemical function of selenium<br />
and its relation to vitamin E and the mechanisms of action of selenium and vitamin E in protection<br />
of biological membranes has been reviewed (54).<br />
Nutritional muscular dystrophy<br />
A simplified integrated concept of the pathogenesis of the NMD would be as follows. Diets<br />
deficient in selenium and/or vitamin E permit widespread tissue lipoperoxidation leading to<br />
hyalineh degeneration and calcification of muscle fibers. One of the earliest changes in<br />
experimental selenium deficiency in lambs is the abnormal retention of calcium in muscle fibers<br />
undergoing dystrophy, and selenium supplementation prevents the retention of calcium.<br />
Unaccustomed exercise can accelerate the oxidative process and precipitate clinical disease.<br />
Muscle degeneration allows the release of enzymes, such as lactate dehydrogenase, aldolase and<br />
creatine phosphokinase, the last of which is of paramount importance in diagnosis. Degeneration<br />
of skeletal muscle is rapidly and successively followed by invasion of phagocytes and<br />
regeneration. In myocardial muscle, replacement fibrosis is the rule.<br />
In calves, lambs, and foals the major muscles involved are skeletal, myocardial, and<br />
diaphragmatic. The myocardial and diaphragmatic forms of the disease occur most commonly in<br />
young calves, lambs and foals, resulting in acute heart failure, respiratory distress and rapid death,<br />
often in spite of treatment. The skeletal form of the disease occurs more commonly in older calves,<br />
yearling cattle and older foals, and results in weakness and recumbency, is usually less severe and<br />
214
esponds to treatment. The biceps femoris muscle is particularly susceptible in calves, and muscle<br />
biopsy is a reliable diagnostic aid.<br />
In foals with NMD there is a higher proportion of type IIC fibers and a lower proportion of type<br />
I and IIA fibers than in healthy foals. The type IIC fibers are found in fetal muscle and are<br />
undifferentiated and still under development. During the recovery period, fibers of types IIA and<br />
IIB increase and the proportion of type IIC fibers decreases. A normal fiber type composition is<br />
present in most surviving foals 1-2 months after the onset of the disease.<br />
Acute NMD results in the liberation of myoglobin into the blood, which results in<br />
myoglobinuria. This is more common in horses, older calves and yearling cattle, than in young<br />
calves whose muscles have a lower concentration of myoglobin. Hence, the tendency to<br />
myoglobinuria will vary depending on the species and age of animal involved.<br />
Subclinical selenium insufficiency<br />
Selenium deficiency affects thyroid hormone metabolism and may explain the cause of ill-thrift.<br />
The conversion of the iodine-containing hormone, thyroxine (T4) to the more potent<br />
triiodothyronine (T3) is impaired in animals with low selenium status and<br />
iodothyroninedeiodinase is a selenoprotein which mediates this conversion (54).<br />
VESD syndrome and others<br />
The pathogenesis of mulberry heart disease, hepatosis dietetica, exudative diathesis, and muscular<br />
dystrophy of swine is not yet clear. Vitamin E and selenium are necessary to prevent widespread<br />
degeneration and necrosis of tissues, especially liver, heart, skeletal muscle, and blood vessels.<br />
Selenium and vitamin E deficiency in swine results in massive hepatic necrosis (hepatosis<br />
dietetica), degenerative myopathy of cardiac and skeletal muscles, edema, microangiopathy, and<br />
yellowish discoloration of adipose tissue. Myocardial and hepatic calcium concentrations are<br />
increased in pigs with mulberry heart disease (55). In addition, there may be esophagogastnc<br />
ulceration, but it is uncertain whether or not this lesion is caused by a selenium and/or vitamin E<br />
deficiency. Anemia has also occurred and has been attributed to a block in bone marrow<br />
maturation, resulting in inadequate erythropoiesis, hemolysis or both. However, there is no firm<br />
evidence that anemia is a feature of selenium and vitamin E deficiency in swine. The entire<br />
spectrum of lesions has been reproduced experimentally in swine with natural or purified diets<br />
deficient in selenium and vitamin E, or in which an antagonist was added to inactivate vitamin E<br />
or selenium. However, in some studies, the selenium content of tissues of pigs that died from<br />
mulberry heart disease was similar to that of control pigs without the disease.<br />
The extensive tissue destruction in pigs may account for the sudden death nature of the complex<br />
(mulberry heart disease and hepatosis dietetica) and the muscle stiffness that occurs in some<br />
feeder pigs and sows of farrowing time with muscular dystrophy. The tissue degeneration is<br />
associated with marked increases in serum enzymes related to the tissue involved. An indirect<br />
correlation between vitamin E intake and peroxide hemolysis in pigs on a deficient diet sugests<br />
that lipoperoxidation is the ultimate biochemical defect in swine and that vitamin E and selenium<br />
are protective.<br />
CLINICAL FINDINGS<br />
Acute enzootic muscular dystrophy<br />
Affected animals may collapse and die suddenly after exercise without any other premonitory<br />
signs. The excitement associated with the hand-feeding of dairy calves may precipitate peracute<br />
death. In calves under dose observation, a sudden onset of dullness and severe respiratory distress,<br />
215
accompanied by a frothy or blood-stained nasal discharge, may be observed in some cases.<br />
Affected calves, lambs, and foals are usually in lateral recumbency and may be unable to assume<br />
sternal recumbency even when assisted. When picked up and assisted to stand, they feel and<br />
appear limp. However, their neurological reflexes are normal. Their eyesight and mental attitude<br />
are normal and they are usually thirsty and can swallow unless the tongue is affected. The heart<br />
rate is usually increased up to 150-200/min and often with arrhythmia, the respiratory rate is<br />
increased up to 60-72/min and loud breath sounds are audible over the entire lung fields. The<br />
temperature is usually normal or slightly elevated. Affected animals commonly die 6-12 hours<br />
after the onset of signs in spite of therapy. Outbreaks of the disease occur in calves and lambs in<br />
which up to 15% of susceptible animals may develop the acuteform, and the case fatality<br />
approaches100%.<br />
Subacute enzootic muscular dystrophy<br />
This is the most common form in rapidly growing calves, 'white muscle disease', and in young<br />
lambs, 'stiff-Iamb disease'.Affected animals may be found in sternal recumbency and unable to<br />
stand but some make an attempt to stand. If they are standing, the obvious signs are stiffness,<br />
trembling of the limbs, weakness and, in most cases, an inability to stand for more than a few<br />
minutes. The gait in calves is accompanied by rotating movements of the hocks, and in lambs a<br />
stiff, goose-stepping gait. Muscle tremor is evident if the animal is forced to stand for more than a<br />
few minutes. On palpation the dorsolumbar, gluteal, and shoulder muscle masses may be<br />
symmetrically enlarged and firmer than normal (although this may be difficult to detect). Most<br />
affected animals retain their appetite and will suck if held up to the dam or eat if hand-fed. Major<br />
involvement of the diaphragm and intercostal muscles causes dyspnea with labored and<br />
abdominal-type respiration. The temperature is usually in the normal range but there may be a<br />
transient fever (41℃, 105℃) due to the effects of myoglobmemia and pain. The heart rate may be<br />
elevated, but there are usually no rhythmic irregularities. Following treatment, affected animals<br />
usually respond in a few days, and within 3-5 days they are able to stand and walk unassisted.<br />
In some cases, the upper borders of the scapulae protrude above the vertebral column and are<br />
widely separated from the thorax. This has been called the 'flying scapula' and has occurred in<br />
outbreaks in heifers from 18 to 24 months of age within a few days after being turned out in the<br />
spring following loose-housing throughout the winter (56, 57). The abnormality is due to bilateral<br />
rupture of the serratus ventralis muscles (58) and has been reported in a red deer (59).<br />
Occasionally, the toes are spread and there is relaxation of carpal and metacarpal joints or<br />
knuckling at the fetlocks and standing on tip-toe, inability to raise the head, difficulty in<br />
swallowing, inability to use the tongue, and relaxation of abdominal muscles. Choking may occur<br />
when the animal attempt to drink. In 'paralytic myoglobinuria' of yearling cattle, there is usually a<br />
history of recent turning out on pasture following winter housing. Clinical signs occur within 1<br />
week and consist of stiffness, recumbency, myoglobinuria, hyperpnea, and dyspnea. Severe cases<br />
may die within a few days and some are found dead without premonitory signs. In rare cases,<br />
lethargy, anorexia, diarrhea, and weakness are the first clinical abnormalities recognized, followed<br />
by recumbency and myoglobinuria.<br />
Subcapsular liver rupture in lambs has been associated with vitamin E deficiency in lambs<br />
usually under 4 weeks of age (60). Affected lambs collapse suddenly, become limp, and die within<br />
a few minutes or several hours after the onset of weakness.<br />
In foals, muscular dystrophy occurs most commonly during the first few months of life and is<br />
216
common in the first week. The usual clinical findings are failure to suck, recumbency, difficulty in<br />
rising, and unsteadiness and trembling when forced to stand. The temperature is usually normal<br />
but commonly there is polypnea and tachycardia.<br />
In adult horses with muscular dystrophy, a stiff gait, myoglobinuria, depression, inability to<br />
eat, holding the head down low, and edema of the head and neck are common. The horse may be<br />
presented initially with clinical signs of colic.<br />
In pigs, muscular dystrophy is not commonly recognized clinically because it is part of the<br />
more serious disease complex of mulberry heart disease and hepatosis dietetica. However, in<br />
outbreaks of this complex, sucking piglets, feeder pigs, and sows after farrowing may exhibit an<br />
uncoordinated, staggering gait suggestive of muscular dystrophy.<br />
Subclinical nutritional muscular dystrophy occurs in apparently normal animals in herds at<br />
the time clinical cases are present. The serum levels of creatine phosphokinase levels may be<br />
elevated in susceptible animals for several days before the onset of clinical signs; following<br />
treatment with vitamin E and selenium the level of serum enzymes returns to normal. Grossly<br />
abnormal electrocardiograms occur in some animals and may be detectable before clinical signs<br />
are evident.<br />
Mulberry heart disease<br />
In mulberry heart disease, affected animals are commonly found dead without premonitory signs.<br />
More than one pig may be found dead. When seen alive, animals show severe dyspnea, cyanosis<br />
and recumbency, and forced walking can cause immediate death. In some outbreaks, about 25% of<br />
pigs will show a slight inappetence and inactivity, these are probably in the subclinical stages of<br />
the disease.The stress of movement, inclement weather or transportation will precipitate further<br />
acute deaths. The temperature is usually normal, the heart rate rapid,and irregularities maybe<br />
detectable. The feces are usually normal.<br />
Hepatosis dietetica<br />
In hepatosis dietetica, most pigs are found dead. In occasional cases, before death there will be<br />
dyspnea, severe depression, vomiting, staggering, diarrhea and a state of collapse. Some pigs are<br />
icteric. Outbreaks also occur similar to the pattern in mulberry heart disease. Muscular dystrophy<br />
is almost a consistent necropsy finding in both mulberry heart disease and hepatosis dietetica but<br />
is usually not recognized clinically because of the seriousness of the two latter diseases. Clinical<br />
muscular dystrophy has been described in gilts at 11 months of age. About 48 hours after<br />
farrowing, there was muscular weakness, muscular tremors, and shaking. This was followed by<br />
collapse, dyspnea, and cyanosis. There were no liver or heart lesions. In experimental selenium<br />
and vitamin E deficiency in young growing pigs, a subtle stiffness occurs along with a significant<br />
increase in the creatinine phosphatase (CPK) and serum glutamicoxaloacetic transaminase (SGOT)<br />
values.<br />
CLINICAL PATHOLOGY<br />
Myopathy<br />
Plasma creatine kinase (CK)<br />
This is the most commonly used laboratory aid in the diagnosis of NMD. The enzyme is highly<br />
specific for cardiac and skeletal muscle and is released into the blood following unaccustomed<br />
exercise and myodegeneration. In cattle and sheep, its half-life is 2-4 hours and plasma levels<br />
characteristically decline quickly unless there is continued myodegeneration, but remain a good<br />
guide to the previous occurrence of muscle damage for a period of about 3 days. The normal<br />
217
plasma levels of CK (IU/L) are: sheep 52 +/- 10; cattle 26 +/- 5; horses 58 +/-6; and pigs 226 +/-<br />
43. In cattle and sheep with NMD, the CK levels will be increased usually above 1000 IU/L,<br />
commonly increased to 5000-10000 IU/L and not uncommonly even higher. Following turnout of<br />
housed cattle onto pasture the CK levels will increase up to 5000 IU/L within a few days. The CK<br />
levels will usually return to normal levels within a few days following successful treatment.<br />
Persistent high levels suggest that muscle degeneration is still progressive or has occurred within<br />
the last 2 days. Measurement of plasma CK activity could be used to monitor recovery of animals<br />
treated for nutritional myopathy (61).<br />
Aspartate aminotransferase<br />
Aspartate aminotransferase (AST) activity is also an indicator of muscle damage, but is not as<br />
reliable as the CK because increased AST levels may also indicate liver damage. The AST activity<br />
remains elevated for 3-10 days because of a much longer half-life than CK. In acute cases, levels<br />
of 300-900 IU/L in calves and 2000-3000 IU/L in lambs have been observed. In normal animals of<br />
these species, serum levels are usually less than 100 IU/L.<br />
The magnitude of the increase in AST and CK is directly proportional to the extent of muscle<br />
damage. Both are elevated initially; an elevated AST and declining CK would suggest that muscle<br />
degeneration is no longer active. The levels of both enzymes will be increased slightly in animals<br />
that have just been turned out and subjected to unaccustomed exercise, horses in training, and in<br />
animals with ischemic necrosis of muscle due to recumbency caused by diseases other than<br />
muscular dystrophy. However, in acute muscular dystrophy, the levels are usually markedly<br />
elevated.<br />
Selenium status<br />
Although information on the critical levels of selenium in soil and plants is accumulating<br />
gradually, the estimations are difficult and expensive. Most field diagnoses are made on the basis<br />
of clinicopathological findings, the response to treatment and control procedures using selenium.<br />
The existence of NMD is accepted as presumptive evidence of selenium deficiency, which can<br />
now be confirmed by analyses of GHS-PX and the concentrations of selenium in soil, feed<br />
samples, and animal tissues. Tentative critical levels of the element are as follows:<br />
•Forages and grains - A content of 0.1 mg/kg DM is considered adequate<br />
•Soil - Soils containing less than 0.5 mg/kg are likely to yield crops inadequate in selenium<br />
concentration (2)<br />
•Animal tissues, blood, and milk -<br />
The concentration of selenium in various tissues are reliable indicators of the selenium status of<br />
the animal.There is a positive correlation between the selenium content of feed and the selenium<br />
content of the tissues and blood of animals ingesting that feed and the values fluctuate with the<br />
dietary intake of the element (2).<br />
Kidney cortex and liver<br />
Normal liver selenium concentrations range from 1.2 to 2.0 µg/g DM, regardless of species or age<br />
(62). Levels of 3.5-5.3 mg/g (67-101 nmol/g) DM in the kidney cortex and 0.90-1.75 µg/g (11-22<br />
nmol/g) DM in the liver of cattle are indicative of adequate selenium. Levels of 0.6-1.4 µg/g (8-18<br />
nmol/g) in the kidney cortex and 0.07-0.60 µg/g (0.9-8 nmol/g) in the liver represent a deficient<br />
state.<br />
The selenium content of bovine fetal liver samples collected at an abattoir contained<br />
0.77(µg/mL WW. and 0.13 µg/mL WW, from dairy breeds and beef breeds of cattle, respectively<br />
218
(63). Mean liver selenium levels from aborted bovine fetuses with myocardial lesions were<br />
5.5 .µmol/kg, 6.5 µmol/kg in fetuses without myocardial lesions and 7.5 µmol/kg in fetuses from<br />
the abattoir, which suggests that selenium deficiency may be the cause of abortion (64).<br />
Blood and milk<br />
Blood and milk levels of selenium are used as indicators of selenium status in cattle and the effect<br />
of dietary supplementation (65). Serum selenium values increase gradually with age from starting<br />
ranges for neonates of 50-80 ng/L for calves and sheep, and 70-90 for foals and pigs (62).<br />
Expected or normal values for adults are in the ranges of 70-100 for cattle, 120-150 for sheep,<br />
130-160 for horses, and 180-220 for swine.<br />
Dams of affected calves have had levels of 1.7ng/ml (2.2 nmol/L) (blood) and 4.9 ng/mL(6.2<br />
nmol/L) (milk); their calves have blood levels of 5 8 ng/mL (6.3-10.1 nmol/L). Normal<br />
selenium-supplemented cows have 19-48 ng/mL (24.1-60.8 nmol/L) in blood and 10-20 ng/mL<br />
(12.7-25.3 nmol/L) in milk, and their calves have blood levels of 33-61 ng/mL (41.8-77.2 nmol/L).<br />
Mean selenium concentrations in the blood of normal mares have been 26-27 ng/mL (32.9-34.2<br />
nmol/L). In Thoroughbred horses, selenium concentrations in serum range from 39.5 to<br />
118.5mg/mL (50-150 µmol/L) and there arc significant differences between various stables of<br />
horses.<br />
Bulk tank milk<br />
The bulk tank milk selenium levels are closely related to the mean herd blood and milk levels and<br />
have the potential to be a low-cost, non-invasive means of evaluating herd selenium levels in order<br />
to determine selenium deficiency in the dairy herd (66).<br />
Glutathione peroxidase<br />
There is a direct relationship between the GSH-PX activity of the blood and the selenium levels of<br />
the blood and tissues of cattle, sheep, horses, and pigs (1). The normal selenium status of cattle is<br />
represented by whole blood selenium concentration of 100 ng/mL (126.6 nmol/L) and blood<br />
GSH-PX activity of approximately 30 mU/mg hemoglobin (67). There is a high positive<br />
relationship (r = 0.87-0.958) between blood GSH-PX activity and blood selenium concentrations<br />
in cattle (67). Blood selenium levels less than 50 ng/mL are considered as selenium-deficient,<br />
while levels between 50 and 100 ng/mL (126.6 nmol/L) are marginal, and greater than 100 ng/mL<br />
are adequate (1). Comparable whole blood levels of GSH-PX are deficient if less than 30 mU/mg<br />
hemoglobin, marginal if 30-60 mU/mg, and adequate if greater than 60 mU/mg hemoglobin (1).<br />
There is some evidence of variation in GSH-PX activities between breeds of sheep; levels may<br />
also decrease with increasing age. Low levels in some breeds of sheep may also be a reflection of<br />
adaptation to low selenium intake because of low levels of selenium in the soil and forages.<br />
The GSH-PX activity is a sensitive indicator of the level of dietary selenium intake and the<br />
response to the oral or parenteral administration of selenium (1, 2). Because selenium is<br />
incorporated into erythrocyte GSH-PX only during erythropoiesis, an increase in enzyme activity<br />
of the blood will not occur for 4-6 weeks following administration of selenium (1). Plasma<br />
GSH-PX will rise more quickly and will continue to increase curvihnearly with increasing dietary<br />
selenium levels because it is not dependent on incorporation of the selenium into the erythrocytes.<br />
The liver and selenium concentration and scrum GSH-PX activity may respond to changes in<br />
dietary selenium more rapidly than either whole blood selenium or erythrocyte GSH-PX activity.<br />
The response in GSH-PX activity may depend upon the selenium status of the animals at the time<br />
when selenium is administered. Larger increases in the enzyme activity occur in<br />
219
selenium-deficient animals. The GSH-PX activity in foals reflects the amount of selenium given to<br />
the mare during pregnancy.<br />
The sandwich ELISA is a simplified method for the estimation of GSH-PX activity and<br />
selenium concentration in bovine blood, and can be used for rapid screening of the selenium status<br />
of a large number of cattle (68).<br />
The GSH-PX activity can be determined rapidly using a spot test which is semiquantitative and<br />
can place a group of samples from the same herd or flock into one of three blood selenium<br />
categories: deficient, low marginal, and marginal adequate (69). A commercial testing kit known<br />
as the Ransel Kit is now available (70). Because of the instability of GSH-PX plasma, GSH-PX<br />
activity in sheep, cattle, and pigs should be measured in fresh plasma or stored at -20℃ (-4℉).<br />
For absolute measurements, it is suggested that swine plasma GSH-PX activity be measured<br />
immediately after separation from the blood cells, or be assayed within 24 hours under specified<br />
laboratory conditions (71).<br />
Vitamin E status<br />
Vitamin E occurs in nature as a mixture of tocopherols in varying proportions. They vary widely<br />
in their biological activity so that chemical determination of total tocopherols is of much less<br />
value than biological assay. Tocopherol levels in blood and liver provide good information on the<br />
vitamin E status of the animal. However, because of the difficulty of the laboratory assays of<br />
tocopherols, they are not commonly done and insufficient reliable data available. Analysis of liver<br />
from clinically normal animals on pasture reveal a mean a-tocopherol level of 20 mg/kg WW for<br />
cattle and 6 mg/kg WW for sheep. The corresponding ranges were 6.0-53 WW mg/kg for cattle<br />
and 1.8-17 mg/kg WW in sheep. The critical level below which signs of deficiency may be<br />
expected are 5 mg/kg WW for cattle and 2 mg/kg WW for sheep. Tocopherol levels in the serum<br />
of less than 2 mg/L in cattle and sheep are considered to be critical levels below which deficiency<br />
diseases may occur. However, if the diet contains adequate quantities of selenium, but not an<br />
excessive quantity of PUFAs, animals may thrive on low levels of serum tocopherols. In growing<br />
pigs, the serum vitamin E levels are between 2 and 3 mg/L (72). In summary, there are insufficient<br />
reliable data available on the vitamin E status on animals with NMD to be of diagnostic value.<br />
The mean plasma vitamin E levels in clinically normal horses of various ages and breeds were<br />
2.8 µg/mL (73). The optimal method for storing equine blood prior to a-tocopherol analysis is in<br />
an upright position in the refrigerator for up to 72 hours (74). If a longer period is needed, the<br />
serum or plasma should be separated, blanketed with nitrogen gas, and frozen in the smallest<br />
possible vial; the a-tocopherol in these samples will be stable at 16 for at least 3 months.<br />
A summary of the GSH-PX activity, tocopherol and selenium levels in blood and body tissues<br />
of animals deficient in selenium appears m Table 29.6. Normal values are also tabulated for<br />
comparison (75). Both the abnormal and normal .values should be considered as guidelines for<br />
diagnosis because of the wide variations in levels between groups of animals. The level of dietary<br />
selenium may fluctuate considerably, which may account for variations in GSH-PX.<br />
Swine<br />
An increase in the activity of several plasma enzymes occurs in selenium and vitamin E<br />
deficiencies of swine. The measurement of AST, CPK, lactic acid dehydrogenase and isucitrate<br />
dehydrogenase can be used to detect the onset of degeneration of skeletal and myocardial muscles<br />
and liver. However, these are not commonly used for diagnostic purposes because of the acuteness<br />
220
of the illness.<br />
The determination of the levels of selenium in feed supplies,tissues,and<br />
1527<br />
Table 29.6 Glutathione peroxidase (GSH-PX) activity and selenium levels in blood and body<br />
tissues of animals deficient in selenium<br />
species<br />
Catter<br />
sheep<br />
pigs<br />
horse<br />
Clinical state or<br />
degree of deficiency<br />
Normal or adequte<br />
marginal<br />
deficient<br />
normal or adequte<br />
marginal<br />
deficient<br />
adequte<br />
deficient<br />
adequte<br />
deficien<br />
Erythrocyte gsh-px<br />
activity µmol/min at<br />
37.℃ /g hemoglobin<br />
19.0-36.0<br />
10.0-19.0<br />
0.2-10.0<br />
60-180<br />
8-30<br />
2-7<br />
100-200<br />
normal muscle or as a peripheral boundary around a core of normal muscle. In the diaphragm, the<br />
distribution of damaged bundles gives the tissue a radially striated appearance. The affected<br />
muscle is friable and edematous and may be mineralized. Secondary pneumonia often occurs in<br />
cases where the muscles of the throat and chest are affected. In cases with myocardial involvement,<br />
white areas of degeneration are visible, particularly under the endocardium of the left ventricle in<br />
calves and of both ventricles in lambs. The lesions may extend to involve the inter-ventricular<br />
septum and papillary muscles and have a gritty character consistent with mineralization.<br />
Pulmonary congestion and edema is common.<br />
Histologically, the muscle lesions are non-inflammatory.Hyaline degeneration is followed by<br />
coagulation necrosis and variable degrees of mineralization.<br />
A generalized steatitis has been described in newborn foals less than 2 months of age. The<br />
microscopic appearance of this yellow-brown fat consists of necrotic fat infiltrated by neutrophils,<br />
macrophages, and giant cells. Supplemental vitamin E is believed to protect against this condition.<br />
In mulberry heart disease the carcass is in good condition. All body cavities contain excessive<br />
amounts of fluid and shreds of fibrin. In the peritoneal cavity, the fibrin is often in the form of a<br />
lacy net covering all the viscera. The liver is enlarged, mottled, and has a characteristic nutmeg<br />
appearance on the cut surface. The lungs are edematous and excessive fluid in the pleural cavities<br />
is accompanied by collapse of the ventral lung field. The pericardia! sac is filled with gelatinous<br />
fluid interlaced with bands of fibrin. Beneath the epicardium and endocardium are multiple<br />
hemorrhages of various sizes. Usually, this hemorrhage is more severe on the right side of the<br />
heart. Histologically, the characteristic lesion is widespread myocardial congestion, hemorrhage,<br />
and myofiber degeneration. Multiple fibrinous microthrombi are within the myocardial capillaries<br />
and, occasionally, degenerative changes are visible in walls of small arterioles in many organs,<br />
including the heart. Malacia of cerebral white matter, or more rarely the molecular layer of the<br />
cerebellum, may occur and is attributable to microvascular damage. It should be stressed that, in<br />
some cases, the disease course is so rapid that morphologic changes are not discernible in the<br />
myocardial cells. Since it can be extremely difficult to distinguish mulberry heart disease from<br />
Strep, suis septicemia histologically, it is prudent to also attempt bacteriologic culture when<br />
attempting to confirm the diagnosis.<br />
In hepatosis dietetica the liver is swollen and has a mottled to mosaic-like appearance throughout<br />
its lobes. Typically, the disease course is so rapid that jaundice does not develop. Histologically,<br />
there is a distinct lobular distribution of hemorrhage, degeneration, and necrosis. In NMD of<br />
swine the lesions are often only visible at the microscopic level and consist of areas of bilaterally<br />
distributed areas of muscular degeneration. The changes include hyalinization, loss of striations,<br />
and fragmentation of myofibers. A mild degree of NMD may accompany some cases of hepatosis<br />
dietetica.<br />
Samples for confirmation of diagnosis<br />
•Toxicology - 50 g liver (ASSAY (Se) (Vit E))<br />
•Histology-formalin-fixedskeletal muscle (multiple sites), heart (both left and right ventricular<br />
walls), brain (including cerebral hemisphere) (LM) Bacteriology (for mulberry heart disease<br />
only)-heart, liver, swab from pericardia sac (CULT).<br />
DIFFERENTIAL DIAGNOSIS<br />
Nutritional muscular dystrophy<br />
NMD is most common in young rapidly growing animals fed a selenium-vitamin E deficient<br />
222
ation or whose dams were on a deficient, unsupplemented ration throughout the winter months.<br />
Characteristically, the disease is sudden in onset, and several animals are affected initially or<br />
within a few days, particularly following unaccustomed exercise. In the acute form, generalized<br />
weakness and a state of collapse are common. In the subacute form, the major clinical findings are<br />
stiffness in walking, long periods of recumbency or total recumbency, inability to stand, a normal<br />
mental attitude and appetite, and no abnormal neurological findings to account for the recumbency.<br />
The CP levels are markedly elevated.<br />
Calves and yearlings<br />
Acute enzootic muscular dystrophy in calves with myocardial involvement must be<br />
differentiated from other diseases causing generalized weakness, toxemia and shock. These<br />
include:<br />
•Septicemias-Haemophilus septicemia resulting in weakness, recumbency, and fever<br />
•Pneumonia-Pneumonic pasteurellosis causing dyspnea, toxemia, fever, and weakness,. .<br />
Subacute enzootic muscular dystrophy in which skeletal muscle lesions predominate must be<br />
differentiated from other diseases of young calves and yearlings characterized clinically by paresis<br />
and paralysis. The subacute form is more common in yearlings and young cattle, and is<br />
characterized by recumbency with other body systems being relatively within normal ranges. The<br />
other diseases include:<br />
•Musculoskeletal diseases - Polyarthritis, traumatic or infectious myopathies (blackleg),<br />
osteodystrophy and fractures of long bones<br />
•Diseases of the nervous system-Spinal cord compression, Haemophilus meningoencephalitis<br />
and myelitis, organophosphatic insecticide poisoning<br />
•Diseases of the digestive tract-Carbohydrate engorgement resulting in lactic acidosis, shock,<br />
dehydration, and weakness.<br />
Lambs and kids<br />
In lambs with 'stiff-lamb' disease there is stiffness and a stilted gait, affected animals prefer<br />
recumbency, they are bright and alert, and will suck the ewe if assisted. The serum levels of CPK<br />
and SGOT are also markedly elevated. Differentiation may be necessary from enzootic ataxia and<br />
sway-back, but in these two diseases stiffness is not characteristic but rather weakness and paresis.<br />
Foals<br />
In foals, NMD must be differentiated from acute diseases of the musculoskeletal and nervous<br />
system causing abnormal gait, weakness and recumbency. They include:<br />
•Traumatic injury to the musculoskeletal system<br />
•Polyarthritis . .<br />
•Meningitis<br />
•Traumatic injury to the spinal cord.<br />
Mulberry heart disease<br />
Mulberry heart disease must be differentiated from other common causes of sudden death in pigs<br />
in which the diagnosis is made at necropsy and include:<br />
•Acute septicemias due to salmonellosis, erysipelas, pasteurellosis, and anthrax<br />
•Porcine stress syndrome<br />
•Gut edema<br />
•Intestinal volvulus, heat exhaustion, suffocation during transportation.<br />
TREATMENT<br />
223
Because of the overlapping functions of selenium and vitamin E, and because it is not always<br />
possible to know the relative etiological importance of one nutrient or the other in causing some of<br />
the acute conditions already described, it is recommended that a combined mixture of selenium<br />
and α-tocopherol be used in treatment. α-Tocopherol is the most potent form of the tocopherols<br />
and is available in a number of pharmaceutical forms, which also vary in their biological activity.<br />
It has become necessary to express the unitage of vitamin E in terms of international units of<br />
biological activity. (1 IU:1 mg synthetic racemic α-tocopherol acetate. Natural D-α-tocopherol<br />
acetate 1 mg: 1 IU and natural D-α-tocopherol mg:0.92 IU).<br />
Nutritional muscular dystrophy<br />
For treatment of NMD in calves, lambs, and foals a mixture containing 3 mg<br />
selenium (as sodium or potassium selenite) and 150IU/mL of DL-α-tocopherol acetate, given IM<br />
at 2 mL/45 kg BW is recommended. One treatment is usually sufficient. Animals with severe<br />
myocardial involvement will usually not respond to treatment, and the case mortality rate is about<br />
90%. However, all incontact animals in the herd (calves, lambs, and foals) should be treated<br />
prophylactically with the same dose of selenium and vitamin E. They should be handled carefully<br />
during treatment to avoid precipitating acute muscular dystrophy. Animals with subacute skeletal<br />
muscular dystrophy will usually begin to improve by 3 days following treatment and may be able<br />
to stand and walk unassisted within a week.<br />
Mulberry heart disease<br />
In outbreaks of mulberry heart disease, hepatosis dietetica, and related selenium and vitamin E<br />
deficiency diseases in pigs, all clinically affected pigs and all pigs at risk should be treated<br />
individually with a combination of selenium and vitamin E parenterally.<br />
CONTROL<br />
The control and prevention of the major diseases caused by selenium and vitamin E deficiencies<br />
can generally be accomplished by the provision of both nutrients to susceptible animals fed on<br />
deficient rations. The following points are relevant and applicable to most situations:<br />
•Provide selenium and vitamin E<br />
•Maternal transfer to newborn<br />
•Selenium potentially toxic<br />
•Selenium in milk supplies<br />
•Dietary requirement of selenium<br />
•High sulfate diets<br />
•Gluthathione peroxidase activity<br />
•Different methods of supplementation.<br />
Provide selenium and vitamin E<br />
While selenium alone is protective against a greater spectrum of diseases than is vitamin E, there<br />
are situations in which vitamin E is more protective. Both selenium and vitamin E should be<br />
provided when the diets are deficient in both nutrients, but this may not apply in every situation.<br />
NMD can occur in ruminants with vitamin E deficiency and an adequate selenium status (76).<br />
Most of the emphasis has been on selenium supplementation at the expense of vitamin E, which is<br />
more expensive and less stable. Most injectable vitamin E and selenium preparations are adequate<br />
in selenium but insufficient in vitamin E.<br />
Maternal transfer to newborn<br />
Diseases caused by selenium deficiency are preventable by the administration of selenium to the<br />
224
dam during pregnancy or directly to the young growing animal. Selenium is transported across the<br />
placenta and provides protection for the neonate. Oral supplementation of beef cattle with<br />
selenium will provide sufficient to maintain blood levels in the dam and for adequate transfer to<br />
the fetus, ; which can sequester selenium when the levels are low in the dam. The colostrum of<br />
selenium-supplemented cattle also contains an adequate amount of selenium to prevent severe<br />
selenium-deficiency diseases (39). However, by 7 days after parturition, the levels in milk may be<br />
inadequate to maintain adequate serum levels in calves. The strategic administration of selenium<br />
and vitamin E before the expected occurrence of the disease is also a reliable method of<br />
preventing the disease.<br />
Selenium potentially toxic<br />
Selenium is toxic, and any treatment and control program using it must be carefully monitored.<br />
Selenium injected into or fed to animals concentrates in liver, skeletal muscle, kidney and other<br />
tissues, and withdrawal periods before slaughter must be allowed. There is some concern that<br />
selenium may be a carcinogen for man. The only tissues that appear likely to consistently<br />
accumulate more than 3-4 mg/kg of selenium are the kidney and liver, and these are very unlikely<br />
to constitute more than a very small part of the human diet. There have been no reports of<br />
untoward effects of selenium on human health when it has been used at nutritional levels in<br />
food-producing animals. The incorporation of selenium into commercially prepared feeds for<br />
some classes of cattle and swine has been approved in some countries.<br />
Selenium in milk supplies<br />
The use of selenium in the diet of lactating dairy cows has caused concern about possible<br />
adulteration of milk supplies. However, the addition of selenium to the diets of lactating dairy<br />
cows at levels that are protective against the deficiency diseases does not result in levels in the<br />
milk that are hazardous for human consumption. The feeding of excessive quantities of selenium<br />
to dairy cattle would cause toxicity before levels became toxic for man.<br />
Dietary requirement of selenium<br />
The dietary requirement of selenium for both ruminants and non-ruminants is 0.1 mg/kg DM of<br />
the element in the diet. There may be nutritionally important differences in the selenium status<br />
between the same feeds grown in different regions and between different feeds within a region.<br />
Even within a region featuring high selenium concentrations, some feeds may contain levels of<br />
selenium below the 0.1 mg/kg minimum requirement for livestock. Thus a selenium analysis of<br />
feeds appears necessary in order to supplement livestock appropriately. Some geographical areas<br />
are known to be deficient in selenium and the feeds grown in these areas must be supplemented<br />
with selenium and vitamin E on a continuous basis.<br />
High sulfate diets<br />
Avoidance of high sulfate diets is desirable, but provision of adequate selenium overcomes the<br />
sulfate effect.<br />
Glutathione peroxidase activity<br />
Whole blood GSH-PX activity is a reliable and useful index for monitoring the selenium status of<br />
cattle and sheep, perhaps not as reliable in pigs, and not a good indicator in the horse.<br />
Different methods of supplementation<br />
The prevention of the major diseases caused by selenium and vitamin E deficiencies can be<br />
achieved by different methods, including:<br />
•Dietary supplementation in the feed or water supplies<br />
225
•Individual parenteral injections<br />
•Oral administration<br />
•Pasture top-dressing.<br />
The method used will depend on the circumstances of the farm, ease of administration, cost, the<br />
labor available, severity of the deficiency that exists, and whether or not the animals are being<br />
dosed regularly for other diseases such as parasitism. The subcutaneous injection of barium<br />
selenate, the administration of an intraruminal pellet, and the addition of selenium to the water<br />
supply were compared in cattle; each method was effective for periods ranging from 4 to 12<br />
months.<br />
Dietary supplementation<br />
The inclusion of selenium and vitamin E in the feed supplies or salt and mineral mixes has been<br />
generally successful in preventing the major diseases caused by deficiencies of these two nutrients.<br />
Muscular dystrophy<br />
Under most conditions, NMD of calves and lambs can be prevented by providing selenium and<br />
vitamin E in the diets of the cow or ewe during pregnancy at 0.1 mg/kg DM of actual selenium,<br />
and (a-tocopherol at 1 g/d/cow and 75 mg/d/ewe. If possible, the supplementation should be<br />
continued during lactation to provide a continuous source of selenium to the calves and lambs.<br />
Under some conditions the level of 0.1 mg/kg DM may be inadequate. In some circumstances the<br />
optimal selenium concentration in the feed is considerably higher than 0.1 mg/kg DM, and levels<br />
up to 1.0 mg/kg DM in the feed result in increases in GSH-PX activity which may be beneficial;<br />
however, the cost-effectiveness has not been determined. Pregnant ewes being fed on alfalfa hay<br />
may require selenium at a level of up to 0.2 mg/kg DM to prevent white muscle disease in their<br />
lambs. Young growing cattle, particularly beef cattle likely to receive hay and straw deficient in<br />
selenium and those which are fed high-moisture grain, should receive a supplement of selenium at<br />
the rate of 0.1 mg/kg DM and a-tocophero] at 150 mg/d/head. If selenium-supplemented<br />
concentrates are used as part of a feeding program for dairy cows, it is not necessary to provide<br />
additional selenium by parenteral injection.<br />
Lambs are born with a low serum level of vitamin E but the concentration increases rapidly<br />
after the ingestion of colostrum (77). Supplementation of pregnant ewes with a-tocopherol, either<br />
as a single IM dose (500 mg 2 weeks before lambing) or orally (150 mg daily during 3-4 weeks<br />
before lambing) results in a marked increase in the levels of the vitamin in the serum and<br />
colostrum. The vitamin E concentration in colostrum was 5-11 times higher than in milk 1 week<br />
after lambing.<br />
Vitamin E supplementation of the feed of weaner sheep by oral drench or feed additive is<br />
effective in increasing plasma α-tocopherol concentrations. This is the most practical method for<br />
housed sheep and prevents subclinica] myopathy (78). The IM oily injection was slow to increase<br />
plasma levels of tocopherols and did not prevent myopathy in grazing experiments. Vitamin E<br />
supplements have no beneficial effects on wool quality or quantity in grazing sheep, and unless<br />
certain flocks are susceptible to vitamin E deficiency myopathy it is not recommended.<br />
Salt-mineral mixture<br />
NMD can be prevented in unweaned beef calves and lambs by the inclusion of selenium (14.8<br />
mg/kg) and vitamin E (2700 IU/kg) in the mineral supplement provided ad libitum to the pregnant<br />
cows and ewes on a selenium-deficient ration during the latter two-thirds of gestation and for the<br />
first month of lactation. Under most conditions this will provide selenium at 0.1 mg/kg DM in the<br />
226
diet.<br />
The provision of sodium selenite in a salt-mineral mixture to provide 90 mg of selenium/kg<br />
salt-mineral mixture on a year-round basis, even under range conditions, increased GSH-PX<br />
activity levels into normal ranges in beef cows for 3 months when fed to extremely deficient<br />
animals. Calves of these cows had increased weaning weights and decreased incidence of<br />
infectious diseases, but the trial was uncontrolled. The provision of 30 mg selenium/kg<br />
salt-mineral mixture was insufficient to raise the GSH-PX activity levels to normal ranges. Peak<br />
blood selenium levels were achieved in wearied beef calves supplemented with 80 and 160 mg<br />
selenium/kg in free-choice salt-mineral mixtures for a period of 108 days. In some jurisdictions, it<br />
may be necessary for the veterinarian to prescribe a supplement containing higher levels than<br />
those permitted by legislation. A level of 25 mg/kg selenium of a salt-mineral mixture provided ad<br />
libitum for sheep will result in sufficient levels of selenium in the dam's blood and milk to prevent<br />
selenium deficiency diseases. Each ewe must consume from 8 to 12 g of the salt-mineral mixture<br />
per day.<br />
Daily cattle<br />
The legal commercial selenium supplementation of complete rations for dairy cattle in the United<br />
States has recently been increased from 0.1 to 0.3 mg/kg DM of complete feed (79). At this rate, a<br />
lactating cow consuming 20 kg of DM/d would consume about 6 mg supplemental selenium in<br />
addition to that naturally present in the feedstuffs. Current recommendations indicate that<br />
selenium intake for lactating and gestating dairy cattle should range from 5 to 7 mg/d for adequate<br />
concentrations in serum or plasma which would range from 70 to 100 ng of selenium/ml., serum<br />
(80). Such supplementation should result in improved selenium status of the newborn, improved<br />
concentration of selenium in colostrum, and improved health of the calves. The effects of<br />
selenium supplementation in dairy cattle on reproductive performance is equivocal. Some studies<br />
over a period of two lactations revealed no effect on reproductive performance (79), while others<br />
report an improvement in dairy cattle in a district considered to be marginally deficient in<br />
selenium. Intakes of inorganic selenium as sodium selenite in amounts of 50 mg/d for 90 days or<br />
100 mg/d for 28 days by adult dairy cows (10-30 times the nutritional requirement) did not cause<br />
any health problems (81). The toxic dose for cattle ranges from 0.25 to 0.5 mg/kg BW.<br />
Milk replacers for dairy calves should contain a suitable antioxidant and be supplemented with<br />
300 IU/kg DM of a-tocopherol acetate at the rate of 0.1 mg/kg DM of the milk replacer.<br />
Swine<br />
In growing swine, both selenium and vitamin E at 30 IU/kg DM of feed are necessary for the<br />
prevention of the diseases caused by diets deficient in vitamin E and selenium. Supplementation<br />
of the diet of the sow will result in an adequate transfer to the piglets. Satisfactory protection of<br />
the diseases of swine caused by vitamin E selenium deficiency depends on the correct balance<br />
between selenium, α-tocopherol, PUFAs in the diet, and the presence of a suitable antioxidant to<br />
conserve the a-tocopherol.<br />
Selenium dose<br />
The generally recommended dose of selenium is 0.1 mg/kg BW SC. The GSH-PX activity will<br />
increase to peak levels at about 30 days following the administration of the selenium. The SC<br />
administration of selenium at 0.10 or 0.15 mg/kg BW, as sodium selenate, will increase and<br />
maintain the blood selenium and GSH-PX activity in dairy cattle for up to 6 months following<br />
injection. A single SC or oral dose of 5 mg of selenium at strategic intervals to prevent or treat<br />
227
selenium deficiency in weaned lambs will increase the selenium residues in the meat, but not at<br />
levels considered hazardous to the public.<br />
Individual injections<br />
Injections of selenium and vitamin E have been used successfully for prevention, particularly in<br />
circumstances where the diet cannot be easily supplemented. Following IM injections of sodium<br />
selenite into calves, lambs and piglets, the selenium concentration of the tissues, particularly the<br />
liver, increases and then declines to reach preinjection levels in 23 days in calves, and 14 days in<br />
lambs and piglets. Adequate sources of vitamin E also must be provided. Injectable preparations<br />
of selenium and vitamin E are usually adequate in selenium and deficient in vitamin E and it may<br />
not be possible to correct a marginal deficiency of vitamin E in pregnant beef cattle, for example,<br />
by IM injection of a selenium and vitamin E preparation which contains an inadequate<br />
concentration of vitamin E (82). The current label dose of injectable selenium, 0.055 mg<br />
selenium/kg BW, which is therapeutically adequate for NMD, is not sufficient for long-term<br />
selenium supplementation of cattle on a selenium-deficient diet (83). Copper and selenium<br />
supplementation by parenteral administration can be combined when both deficiencies are present<br />
(84).<br />
Subcutaneous injection<br />
A slow-release preparation of barium selenate for SC injection is now available for use in cattle<br />
and sheep (69). A SC injection of 1 mg selenium/kg BW to ewes 3 weeks before breeding<br />
elevated the selenium level in milk during lactation, and increased the selenium concentration and<br />
GSH-PX in the blood of the lambs during the period when they are at greatest risk from<br />
selenium-deficiency diseases (85). At a dose of 1 mg selenium/kg BW to pregnant ewes, the<br />
GSH-PX activity is increased and maintained at adequate levels for up to 5 months. There is<br />
adequate transfer of selenium to the lambs, providing protetion for up to 12 weeks of age, which<br />
covers the period when lambs are at greatest risk. A dose of 1.2 mg selenium/kg BW provided<br />
adequate selenium status for as long as two consecutive lambing seasons. Barium selenate at 1 mg<br />
selenium/kg BW SC provides protection in young sheep for at least 3 months and is not associated<br />
with risk of selenium toxicity or unacceptable residues of selenium in tissues other than the site of<br />
injection (69). A dose of 1 mg selenium/kg BW (barium selenate) to cattle SC increased the<br />
GSH-PX activity within 4 weeks and was maintained at high levels for up to 5 months.<br />
The SC injection of barium selenate of pregnant sows at 0.5-1.0 mg selenium/kg BW resulted in<br />
a significant difference in GSH-PX activity in the piglets from treated sows compared to untreated<br />
controls. The SC injection of barium selenate .it 2.5 mg selenium/kg BW into pigs weighing 20 kg<br />
also maintained blood levels of selenium and GSH-PX activity during the most rapid growing<br />
period. The relative safety of barium selenate is due to its slow rate of release from the site of<br />
injection. By comparison, when selenium is administered as a soluble salt, such as sodium<br />
selenate, acute toxicity may occur at doses of 0.45 mg selenium/kg BW. Treatment with barium<br />
selenate increases the concentration of selenium in blood, liver and muscle, and persists for at<br />
least 4 months. One disadvantage of barium selenate is that a large residue persists at the site of<br />
injection for long periods. The use of sodium selenate also increases tissue and blood<br />
concentrations of selenium, but they begin to decline by 23 days. The bovine liver rapidly<br />
removes approximately 40% of injected selenium salts (soluble) from the systemic plasma, binds<br />
it to a plasma component, and within 1 hour of injection releases it back into circulation.<br />
NMD in the neonate<br />
228
If the risk of NMD is high in the first few weeks of life for any of the species, selenium can be<br />
given to the dam; if it is later, at say 2-3 months of age, it is administered to the lamb or calf. The<br />
recommended dose rates of repeated injections at monthly intervals are: 1 mg of selenium to<br />
lambs, 5 mg to ewes, 10 mg to calves, and 30 mg to adult cattle. The injections are administered<br />
about 1 month before the anticipated danger period. In calves on a selenium-deficient pasture a<br />
dose of 0.1 selenium mg/kg BW every 2 months or 0.2 selenium mg/kg BW every 4 months may<br />
be necessary. Comparable dose rates of the various compounds in use are: 1 mg selenium is<br />
equivalent to 2.2 mg anhydrous sodium selenate, 2.4 mg anhydrous sodium selenate, or 4.7 mg<br />
hydrated sodium selenate. These doses may be repeated without danger at monthly intervals. A<br />
mixture of selenium and vitamin E can also be used as a preventive at half the dose recommended<br />
under the heading of treatment above. It can be administered to the young or to the dam and<br />
repeated at 2-4 week intervals.<br />
The prevention of NMD and lupinosis-associated myopathy in weaner sheep at 6-12 months of<br />
age in Western Australia can be achieved by the SC injection of selenomethionine (0.1 mg<br />
selenium/kg BW) and α-tocopherol acetate (2000 iU per sheep) (13). The SC treatment was highly<br />
effective in preventing lupinosis-associated myopathy, and also produced the highest vitamin E<br />
concentrations in plasma and liver. The supplemental vitamin E was more efficacious than<br />
supplemental selenium. An oral dose of vitamin E was the least effective method of increasing<br />
concentrations in liver.<br />
Weak-calf syndrome<br />
The parenteral injection of selenium and iodine to pregnant cattle in Ireland did not significantly<br />
reduce the incidence of the weak-calf syndrome, which is often attributed to a selenium deficiency<br />
(16).<br />
Swine<br />
The injection of selenium 0.06 mg/kg BW into piglets under 1 week of age, repeated at weaning<br />
time and into the sow 3 weeks before farrowing will be effective. The minimum lethal dose of<br />
selenium for piglets is 0.9 mg/kg BW, which provides a reasonably wide range of safety. A high<br />
concentration of selenium in the diet of pregnant sows in the last half of gestation has been<br />
associated with hemorrhagic lesions on the claws of newborn piglets (86).<br />
Horses<br />
Little information is available on the need of horses for selenium but the optimum intake is 6<br />
mg/week or 2.4ug/kg BW daily. The oral supplementation of 1 mg selenium/d increases blood<br />
selenium concentrations above levels associated with myodegeneration in horses and foals. To<br />
insure nutritional adequacy, and to have an adequate safety margin, adult Standardbred horses<br />
should receive 600-1800 mg DL-a-tocopherol daily in their feed. The parenteral administration of<br />
vitamin E and selenium to mares in late pregnancy, and to their foals beginning at birth, will<br />
increase blood selenium to adequate levels. In selenium-deficient areas or when mares are fed<br />
selenium-deficient hay, the prepartum injections of selenium and vitamin E are indicated followed<br />
by intermittent injection of the foals, or supplementation of the diet with selenium at 0.1 mg/kg<br />
DM.<br />
Intra-ruminal selenium pellets<br />
Sheep<br />
Intra-ruminal selenium pellets, similar to those used in cobalt deficiency, have produced<br />
satisfactory blood levels of selenium for up to 4 years in ewes at pasture (69). A satisfactory pellet<br />
229
is composed of 0.5 g elemental selenium and finely divided metallic iron. The technique is<br />
efficient, but not completely, due to wide variations between animals in the absorption rate of the<br />
selenium. The average delivery of selenium is 1 mg/d and there is no danger of toxicity. In sheep<br />
grazing selenium-deficient pastures, the ruminal pellets increase the selenium status and weight<br />
gains compared to controls. About 15% of treated sheep reject the pellets within 12 months and in<br />
varying degrees the pellets acquire deposits of calcium phosphate. Sheep fed pellets recovered<br />
from sheep have low selenium levels, which suggests a low release of selenium from pellets that<br />
have been in the rumen of other sheep for several months. The peak levels of selenium occur 3<br />
months after administration; there is a rapid decline in activity between 5 and 13 months.<br />
Sustained-released boluses containing sodium selenate, cobalt sulfate, potassium iodide,<br />
manganese sulfate, zinc oxide and sulfate, and vitamins A, D and E have also been formulated to<br />
provide long-term maintenance of selenium (87).<br />
Cattle<br />
A selenium pellet containing 10% selenium and 90% iron grit is available for cattle and will<br />
maintain plasma selenium and GSH-PX activity above the critical level for up to 2 years (88).<br />
When given to beef cows in the last 3 months of pregnancy, the selenium levels in milk are higher<br />
than in controls, and the selenium status of the calves was sufficient to prevent NMD. The use of<br />
these pellets at two, three and four times the recommended dose in growing cattle weighing<br />
300-350 kg did not cause toxicosis, and the selenium levels in the tissues at slaughter were not a<br />
risk for humans (89).<br />
Use of the intra-ruminal selenium pellets in dairy cattle in New Zealand resulted in improved<br />
growth and milk production in herds where the selenium status was below the adequate range, but<br />
there was no effect on udder health and reproductive performance (29).<br />
A sustained-release intra-reticular bolus is an osmotic pump designed to release 3 mg selenium<br />
into the reticulorumen (88). It is intended to provide selenium supplementation for 120 days in<br />
grown heifers and pregnant beef cattle.<br />
Oral selenium and anthelmintics<br />
Oral dosing using sodium selenate is sometimes combined with the administration of<br />
anthelmintics and vaccinations. The dose should approximate 0.044 mg/kg BW. A routine<br />
program in a severely deficient area comprises three doses of 5 mg of selenium (11 mg sodium<br />
selenate) each to ewes, one before mating, one at mid-pregnancy, and one 3 weeks before lambing,<br />
and four doses to the lambs. The first dose to lambs (of 1 mg) is given at docking and the others (2<br />
mg each) at weaning and then at 3-month intervals. A 100-day controlled release anthelmintic<br />
capsule containing 13.9 mg of selenium will protect lambs from selenium deficiency for at least<br />
180 days (90).<br />
Both selenium and cobalt can be incorporated into an anthelmintic program. The levels of<br />
GSH-PX activity may be monitored on a regular basis following the drenching with selenium and<br />
provide a good indication of selenium availability and selenium status of grazing sheep.<br />
Selenium toxicity and residues<br />
Selenium intoxication can occur follow ng the administration of toxic amounts of a selenium salt.<br />
The use of selenium selenate instead of sodium selenate and giving a dose of five times the<br />
intended dose resulted in a high mortality within several hours after administration (91). Animals<br />
deficient in selenium are more susceptible to selenium toxicosis than those that are<br />
selenium-adequate. The pharmacokineaics of selenium toxicity in sheep given selenium selenate<br />
230
parenterally has been examined. When oral preparations of selenium and monensin are given<br />
concurrently as part of a routine dietary management practice, there is greater risk of selenium<br />
intoxication than if the selenium is given alone (92). Administration of monensin sodium at a<br />
constant, safe dosage enhanced the toxicity of selenium as demonstrated by increased severity of<br />
the signs of intoxication, fatalities, tissue selenium concentrations and intensified gross,<br />
histopathological, and biochemical changes (93). There is some concern about selenium<br />
supplementation of beef cattle being a potential source of contamination for nearby aquatic<br />
systems, but there is no evidence that this has occurred (94).<br />
Pasture top-dressing<br />
The application of sodium selenate as a top-dressing to pasture is now practiced and permitted in<br />
some countries (95). Top-dressing at the approved rate of 10 g selenium/hectare is effective for 12<br />
months and has a toxicity margin of safety of about 20 times. Sodium selenate is now used in<br />
preference to sodium selenate because only about one-fifth is required to raise the pasture level of<br />
selenium to the same concentrations provided by sodium selenate. Top-dressing severely deficient<br />
pumice soils in New Zealand prevented deficiency for at least 12 months, sheep were protected<br />
against white muscle in lambs, and reproduction performance and weight gains were improved. It<br />
is recommended that sodium selenate be applied annually to all selenium-deficient soils at the rate<br />
of 10 g selenium/hectare added to the superphosphate fertilizer, or as prills of sodium selenate<br />
alone. Top-dressing is an economical alternative to individual animal dosing, particularly in<br />
severely deficient areas with a high stocking rate. At the approved rate no adverse effects are<br />
anticipated in human or animal health or on the environment.<br />
REVIEW LITERATURE<br />
Gerloff, B.J. (1992) Effect of selenium<br />
supplementation on dairy cattle. J. Anim. Sci., 70, 3934-3940.<br />
Macphereon, A. (1994) Selenium, vitamin E and biological oxidation. In: Recent Advances in<br />
Animal Nutrition. Eds. Garnsworthy, P. C. & Cole, D.J. A. Nottingham: Nottingham Press, pp.<br />
3-30.<br />
REFERENCES<br />
(1)Roller, L. D. & Exon.J. H. (1986) Can. j. Vet. Res., 50, 297.<br />
(2)National Academy of Science (1983) Selenium in Nutrition. Washington, DC: National<br />
Research Council.<br />
(3)Rammcll, C. G. et al. (1989) NZ Vei.J., 37, 4.<br />
(4)Bryne, IX J. (1992) Coat Vet. Soc, 13(2), 1.<br />
(5)Step, D. L. et al. (1991) J. Am. Vet. .Wed. Assoc, 198, 117.<br />
(6)Cannel, D. K. et al. (1990) Cornell Vet., 80,251.<br />
(7)Edmondson, A. J. et al. (1993) J. Am. Vet. Wed. Assoc, 202, 865.<br />
(8)Campbell,J. R. et al. (1995) Can. Vet.)., 36, 698.<br />
(9)Miller, G. Y. et al. (1995) J Am. Vet. Med. Assoc, 206, 1369.<br />
(10) Khan, A. A. et al. (1989) Can.J. Vet. Res., 51, 174. (1 1) Blaklay, B. R & Bell. R.JI (1994)<br />
Can. Vet.J., 35, 297.<br />
(12)Kennedy, S. & Rice, D. A. (1992) Vet. Palhoi, 29, 129.<br />
(13)Smith, G. M. & Allen, J. G. (1997) Aust. Vet.J., 75, 341.<br />
(14)Smith, D. L et al. (1985) Can. Vet. J., 26, 385.<br />
(15)Gooneratne, S. R. & Christensen, D. A. (1989) Can.J Anim. Sci., 69, 151.<br />
231
(16)McCoy, M. A. et al. (1995) Vet. Rec, 136, 124.<br />
(17)Nielsen. T. K. et al. (1989) Vet, Rec, 124, 535.<br />
(18)Rice, D. A. & Kennedy, S. (1989) Am.J. Vet. Res., 50, 2101.<br />
(19)Sheppard, A. D. et al. (1984) NZ Vet. J., 32, 91.<br />
(20)Langlands,J. P. et al. (1991) Aust.J. Exp. Agr.. 31, 25.<br />
(21)Langlands.J. P, et al. (1991) Aust.J. Exp. Agr., 31, 33.<br />
(22)Unglands.J. P. et al. (1991) Aust.J. Exp. Agr., 31, 37.<br />
(23)Donald, G. E. et al. (1993) Aust.J. Exp. Agr., 33, 411.<br />
(24)Donald, G. E. et al. (1994) Aust.J. Exp. Agr., 34, 13.<br />
(25)Donald, G. E. et al. (1994) Aust.J. Exp. Agr., 34, 19.<br />
(26)van Niekcrk. F. E. et al. (1996) J. South Ajr. Vet. Ass., 67, 209.<br />
(27)Arechiga, C. F. et al. (1994) Thetiogenology., 41, 1251.<br />
(28)Coe, P. 11 et al. (1993) J. Am. Vet. Med. Assoc. 202, 875.<br />
(29)Wichtel, J.J. et al. (1994) NZ Vet.J., 42, 205.<br />
1533<br />
(30)Erskine, R. J. et al. (1997)J Am. Vet.Med. Assoc, 211, 466.<br />
(31)Finch, J. M. & Turner, R. J. (1996) Res.Vet. Sci., 60, 97.<br />
(32)Stabel.J. R. et al. (1996) Nutr. Res., 10,1053.<br />
(33)Pollock, J. M. et al. (1994) Res, Vet. Sci.,56, 100.<br />
(34)Nicholson, J. W. G. et al. (1993) Can.J.Anim. Sci., 13, 355.<br />
(35)Wuryastuti, W. et al. (1993) J. Anim. Sci.,71, 2464.<br />
(36)Pehrson, D. et al. (1991) J. Dairy Sci., 14,1054.<br />
(37)Lacerta, N. et al. (1996) Am.J. Vet. Res.,.57, 1176.<br />
(38)Swecker, W. S. Jr. ct al. (1995) Am. J. Vet.Res., 56, 450.<br />
(39)Abdelrahman, M. M. & Kincaid, R. L.(1995) J. Diary Sci., 78, 625.<br />
(40)Polios, 1. et al. (1995) Am.J. Vet. Res., 56,179.<br />
(41)Politis, I. et al. (1996) Am.J. Vet. Res., 57,468.<br />
(42)Weiss, W. P. et al. (1997)J Dairy Sci., 80,1728.<br />
(43)Weiss, W. P. et al. (1990) J Dairy Sri., 73,381.<br />
(44)Erskine, R. J. et al. (1987)J. Am. Vet.Med. Assoc, 190, 1417.<br />
(45)Braun, U. et al. (1991) Vet. Rec, 128, 543.<br />
(46)Maddox, J. F. et al. (1991) Proslaglandins,42, 369.<br />
(47)Grasso, P. J. et al. (1990) Am.J. Vet. Res .<br />
51,269.<br />
(48)Stevenson, L M. & Jons, D. G. (1989) J.Comp. Pathol., 100, 359.<br />
(49)Mayhew, I. G. et al (1987) J. Vet. Intern.Med., 1, 45.<br />
(50)Dill S. G. et al. (1989) Am. J. Vet. Res., 50,166.<br />
(51)Blythe, 1.. 1-. et al. (1991) Am.J. Vet. Res.,<br />
52,908.<br />
(52)Craig, A. M. et al. (1991) Am.J. Vet. Res.,52, 912.<br />
(53)De La Rua-Domenech, R. et al. (1997)Vet.J., 154, 203.<br />
(54)David, G. P. & Winterbottom, A.J. (1996)Vet. Rec, 139, 20.<br />
(55)Korpela, H. (1991)J. Am. Coll. Nutr., 10,127.<br />
(56)Gunning, R. F. & Wallers. R..J. W.(1994) Vet. Rec, 135, 433.<br />
232
(57)Hannani, 1). A. R. et al. (1994) Vet. Rec.134. 356.<br />
(58)Buergelt, C. D. et al. (1996) J. Com;.Pathol, 114, 445.<br />
(59)Macpherson, A. (1994) In: Recent Advancesin Animal Nutrition. Eds. Garnsworthy, P.C. &<br />
Cole, I. J. A. Nottingham:Nottingham Press, pp 3-30.<br />
(60)Green. L. E. et al. (1995) Vet. Rec, 136,197.<br />
(61)Smith, G. M. et al. (1994) Aust. Vet. J.. 71,12.<br />
(62)Stowe, H. D. & Herdt, T H. (1992)J Anim. Sci., 70, 3928.<br />
(63)Kirk.J. Ff. et al. (1995) Am.J. Vet. Res.,56, 1460.<br />
(64)Orr.J. P. & Blakley, B. R. (1997) J. Vet.Diagn. Invest., 9, 172.<br />
(65)Zust.J. et al. (1996) Vet. Rec. 139, 391.<br />
(66)Lean, I. J. et a!. (1990) Cornell Vet., HO, 41.<br />
(67)Roller, L. D. et al. (1984) Can.J. Comp.Med. 48, 431.<br />
(68)Kinoshita, C. et al. (1996) J. Dairy Sci., 19,1543.<br />
(69)Archer, J. A. &Judson, G.J. (1994) Aust.J. Exp.Agric, 34, 581.<br />
(70)Rice, D. A. & Blanchflowcr, W.J. (1986) Vet. Rec, 118,419.<br />
(71)Davidson, W. B. et al. (1990) Vet. Res.Commun., 14, 441.<br />
(72)Jensen, M. et al. (1990) Ada Vet. Scancl.,31, 129.<br />
(73)Steiss.J. E. et al. (1994) Equine Vet.J., 26,417.<br />
(74)Craig, A. M. et al. (1992) Am.J. Vet. Res.,53, 2228.<br />
(75)Puls, R. (1981) Veterinary Trace MineralDeficiency and Toxicily Information.Publication No.<br />
5139. Ottawa:Information Serives, Agriculture Canada.pp. 1 101.<br />
(76)Radostits, O. M. et al. (1992) Proc Am.Assoc. Bovine Pract., 24, 101.<br />
(77)Pehrson, B. et al. (1990) Ada Vet. Scand.,<br />
31,359.<br />
(78)Fry.J. M. et al. (1996) Aust.J. Agric. Res.,41, 853 & 869.<br />
(79)Stowe, H. D. et al. (1988) J. Dairy Sci., 11,1 830.<br />
(80)Cerloff, B.J. (1992) J. Anim. Sci., 10, 3934.<br />
(81)Ellis, R. A. et al. (1997) Am.J. Vet. Res.,58, 760.<br />
(82)Cohen, R. D. FI. et al. (1991) Can. Vet.J.,<br />
32.113.<br />
(83)Maas, J. et al. (1993) J. Vet. Int. Med., 7, 342.<br />
(84)Van Niekerk, F. E. et al. (1995) J South Afr. Vet. Assoc, 66, 11.<br />
(85)Zachara, B. A. et al. (1993) Small Rum. K ., J, 135.<br />
(86)Mensink, C. G. et al. (1990) Vet. Rec. 126, 620.<br />
(87)Lawson, D. C. et al. (1990) Vet. Rec, 121, 67.<br />
(88)Campbell, D. T. et al. (1990) Am. J. Vet. Res., 5!. 813.<br />
(89)Wilson, D.J. et al. (1991) Am.J. Vet. Res., 52, 1866.<br />
(90)Grace. N. D. et al. (1994) NZ Vet,J., 42. 63.<br />
(91)Kyle, R. & Allen, R. M. (1990) Vet. Res., 126, bin.<br />
(92)Wang.J. 11. et al. (1990) J. Vet. Pharmacol. The,., 13. 378.<br />
(93)Smyth, J. B. A. et al. (1990) J. Comp. Pathol., 102. 443.<br />
(94)Norman, B. et al. (1992) J Am. Vet. Med. Assoc, 201, 869.<br />
(95)Sansom, R. L. (1990) NZ Vet.J 38, 1.<br />
233
二、铜营养紊乱性疾病(Nutritional Disorder of Copper)<br />
(一)铜缺乏症(Copper Deficiency)<br />
铜缺乏症又称低铜病(Hypocuprosis),分为原发性和继发性两种。原发性缺铜是因饲<br />
料中铜含量太少,铜摄入不足,又称为单纯性缺铜症。主要表现为含铜酶活性下降及相关联<br />
症状。继发性缺铜症是因饲料中可干扰铜吸收利用的物质如钼、硫等含量太多,即使铜含量<br />
正常,仍可造成铜摄入不足、铜排泄过多,引起铜缺乏症。临床上以拉稀、神经脱髓鞘为主。<br />
又称为条件性缺铜。自然条件下,原发性缺铜症可发生于牛、羊、猪、马驹及许多其它食草<br />
动物。条件性缺铜症多发生于牛,其次是绵羊、鹿和猪。马属动物极少发生。羔羊摇背症<br />
(swayback),牛的舔(盐)病(licking sickness)、摔倒病(failing disease)和猪铜缺乏症都<br />
属于原发性缺铜;泥炭泻(peat Scouring)、英国牛羊“晦气”病(teart)、犊牛消瘦病<br />
(unthriftness)、牛的废用性病(wasting disease:)及羔羊地方性运动失调(enzootic ataxia)<br />
等。属于条件性低铜病,海岸病和盐病(salt disease)属缺铜又缺钴。<br />
【病因】 原发性缺铜因土壤中铜含量低引起。土壤中通常含铜 18~22mg/kg,植物<br />
中含铜 11mg/kg。但在沙土地,严重贫嵴的土壤,表土太薄的地区、海岸、沼泽地中,土<br />
壤铜含量仅 0.1~2mg/kg,植物中含铜仅 3~5mg/kg。有些土壤中形成不溶性有机铜化合物,<br />
不利于植物吸收利用。<br />
条件性缺铜症常因土壤中钼和硫酸盐含量过多。钼浓度在 10~100mg/kg(干物质计)<br />
以上,易引起条件性缺铜。高度碱化的土壤,或碳酸钙含量高的土壤,有利于植物对钼的吸<br />
收。土壤中锌、铁含量太高,都可诱导条件性缺铜。<br />
牧草中 Cu
胞色素氧化酶活性下降,造成神经脱髓鞘作用和神经系统损伤,产生运动失调。由于体内二<br />
硫(—S—S—)键合成障碍,造成毛羽内巯基键(—SH)过多,使毛失去弹性。并形成钢<br />
丝毛;由于赖氨酰基氧化酶活性和单胺氧化酶活性下降,血管壁内锁链素和异锁链素增多,<br />
血管壁弹性下降,因而引起鸡动脉破裂及骨骼中胶原稳定性下降,骨端变形。<br />
通常情况下,血浆铜浓度有 0.8mg/kg 以上时,临床上不表现异常,但补铜后对生产能<br />
力可大大改善。原发性缺铜和继发性缺铜的症状略有不同。<br />
【临床表现】 原发性缺铜症,患畜表现精神不振,产乳量减少和贫血。被毛缺乏光泽,<br />
粗乱、红毛变为淡锈红色,以至黄色,黑毛变成淡灰色,犊牛生长缓慢,腹泻,易骨折,特<br />
别是骨盆骨与四肢骨易骨折。驱赶运动时行动不稳,甚至呈犬坐姿势。稍事休息后,则恢复<br />
“正常”,有些牛有痒感和舔毛,腹泻呈间歇性,部分犊牛表现关节扩大,步样强拘,屈肌<br />
腱挛缩,行走时呈指尖着地,这些症状可以在出生时发生,或于断乳时发生,瘫痪和运动不<br />
协调等症状少见。<br />
条件性缺铜症:其主要症状与原发性缺铜类似,但贫血现象少见,腹泻现象明显,这与<br />
某些“条件因子”减少铜的可利用性有关,腹泻严重程度与钼摄入量成正比。<br />
因缺铜所致的疾病还有其自身特点:<br />
牛的摔倒病(falling disease)以突然伸颈,吼叫,跌倒,并迅速死亡为特征。全部病程<br />
多在 24h 结束。因心肌贫血、缺氧和传导阻滞所致。<br />
泥炭泻(peat scouring)是在高钼泥炭地草场放牧数天后,发生稀水样粪便。粪便无臭<br />
味,常不自主外排,久之出现后躯污秽,被毛粗乱,褪色为特点,铜制剂治疗有显效。<br />
消瘦病(unthriftness;pine disease)呈慢性经过,开始表现步样强拘,关节硬性肿大,<br />
屈腱挛缩、消瘦、虚弱,多于 4~5 个月后死亡。被毛粗乱,褪色,仅少数病例表现拉稀。<br />
羊缺铜症:原发性缺铜羊被毛绒化,卷曲消失,形成直毛或钢丝毛,毛纤维易断。但各<br />
品种羊对缺铜的敏感性不一样,如羔羊摇背症,是先天性营养性缺铜症(亦有人认为是遗传<br />
性缺铜)。表现为生后即死,或不能站立,不能吮乳,快步运动时后躯摇晃,故称为摇背症。<br />
有的在妊娠 120 天时,胎儿脑部结构就发生白质软化,空泡形成。有的于生后数天死亡,剖<br />
检表现小脑肿胀,甚至有失明现象。条件性缺铜的特征性表现是地方性运动失调,多发生于<br />
1~2 个月龄,少数于生后即出现,主要表现运动不稳,后躯萎缩,驱赶或行走时易跌倒,后<br />
肢软弱而坐地,持续了 3~4 天后,多数患羔可以存活,易骨折,少数病例可表现下泻,如波<br />
及前肢,则动物卧地不起。<br />
山羊缺铜与羔羊运动失调类似,但仅发生于幼羔至 32 月龄。<br />
鹿缺铜症与羔羊缺铜症状类似,仅发生于年轻的未成年鹿,刚断乳或断乳以后,成年母<br />
鹿发病少,临床上表现运动不稳,后躯摇晃,呈犬坐姿势,脊髓神经脱髓鞘,中脑神经变性<br />
(参见第 5 章第 3 节)。<br />
猪缺铜症,自然发生猪缺铜病例极少。病畜表现轻瘫,运动不稳,肝铜浓度降至 3~14mg<br />
/kg,实验性用低铜饲料喂猪,可产生典型的运动失调,跗关节过度屈曲,呈犬坐姿势,用<br />
补铜治疗,效果显著。<br />
自然发生的鸡缺铜症,可有主动脉破裂,突然死亡。但发病率低,母鸡所产蛋的胚胎发<br />
育受阻,孵化 72~96h,分别见有胚胎出血和单胺氧化酶活性降低。<br />
临床病理方面有:贫血,血红蛋白浓度降为 50~80g/L红细胞数降为 2×10 12 ~4×10 12 个<br />
/L,有相当高比例红细胞内有亨氏(Heinz)小体,但无明显的血红蛋白尿现象,贫血程度<br />
与血铜浓度下降成比例。<br />
牛血浆铜浓度从 0.9~1.0mg/L 降至 0.7mg/L 时,称为低铜血症。继续降至 0.5mg/L<br />
以下,则出现临床缺铜症。但继发性缺铜早期,可因高钼摄入而诱发血浆铜浓度升高,TCA<br />
可溶性铜变化不大,现在把 TCA 不溶性铜浓度升高,TCA 可溶性铜与不可溶性铜间的比值<br />
235
下降,作为监测条件性缺铜的指标。<br />
肝铜浓度变化非常显著,初生动物,幼畜肝铜浓度都较高,如牛在 380mg/kg,羊在<br />
74~430mg/kg,猪在 233mg/kg,但生后不久因合成铜蓝蛋白,则迅速下降。成年牛缺铜<br />
时,肝铜从 100mg/kg,降至 15mg/kg,甚至仅 4mg/kg。羊从 200mg/kg 以上降至 25mg<br />
/kg 以下。可见幼畜缺铜时,肝铜浓度变化甚大,牛为 8~109mg/kg,羔羊为 4~34mg/kg,<br />
很难以一个标准来判断。<br />
缺铜时某些含铜酶活性改变,血浆铜蓝蛋白酶活性下降,下降程度与血浆铜浓度成比例,<br />
常用作田间普查,可避免因沾污而影响测定血清铜的结果。随后细胞色素氧化酶和单胺氧化<br />
酶活性下降,它们对慢性肝铜耗竭有诊断意义。最后,当血铜浓度
用上法预防铜缺乏症。<br />
(二)铜中毒(Copper Poisoning)<br />
动物因一次摄大剂量铜化合物,或长期食入含过量铜的饲料或饮水,引起腹痛、腹泻、<br />
肝功能异常和溶血危象,称为铜中毒。<br />
根据病程可分为急性铜中毒和慢性铜中毒。根据发病起始原因,又可分为原发性铜中毒<br />
和继发性铜中毒。前者是因摄入过量铜所致,后者是因食入某些植物,引起肝铜积累增多,<br />
肝损伤,从而诱发溶血危象,并产生慢性铜中毒。<br />
动物中以羔羊对过量铜最敏感,其次是绵羊、山羊、犊牛、牛等反刍动物。单胃动物对<br />
过量铜较能耐受,猪、狗、猫时有发生铜中毒的报告,兔、马、大鼠却很少发生铜中毒。家<br />
禽中以鹅对铜较敏感,鸡、鸭对铜耐受量较大。鲤鱼和鲫鱼对过量铜似乎很敏感,饮水中含<br />
0.5mg/L 铜,一周内可致死。<br />
【病因】 急性铜中毒多因一次注射或误食大剂量可溶性铜的意外事故所引起。如羔羊<br />
在被用含铜药物喷洒过的草地放牧,或饮用含铜浓度较高的饮水(因用硫酸铜鱼池灭杂鱼及<br />
螺丝),缺铜地区给动物不确当地补充过量铜制剂等。慢性铜中毒常因环境污染或土壤中铜<br />
含量太高,所生长的牧草和饲料中铜含量偏高,如矿山周围、铜冶炼厂、电镀厂附近,因含<br />
铜灰尘、残渣、废水中的含铜化合物污染了饲料及周围环境。长期用含铜较多的猪粪、鸡粪<br />
施肥的草场,亦可引起在该草场放牧的绵羊铜中毒。用含铜较多的饲料喂鸡,将鸡粪烘干除<br />
臭后喂羊,亦可引起慢性铜中毒。猪、鸡饲料中常添加了过量的铜(>250mg/kg),因未予<br />
拌匀、碾细,亦可引起铜中毒。某些植物,如地三叶草(Subterranaen clover),天芥菜属<br />
(Heliotropum european)可引起肝脏对铜的亲和力增加,铜在肝内蓄积,加之这些植物中肝<br />
毒性生物碱引起肝损伤,易诱发溶血危象,并产生慢性铜中毒急性发作,特别是英国品种绵<br />
羊及其美利奴羊的杂交后代易中毒。有些狗可能是遗传基因缺陷,产生类似人的遗传病<br />
(Wilson 氏病)样的遗传性铜中毒。<br />
各种动物对铜的耐受量不同,绵羊、犊牛按 20~110mg/kg 体重一次静脉注射,山羊一<br />
次按 2.5mg/kg 体重剂量,静脉注射,可产生急性死亡。羔羊日粮中含 20mg/kg 铜则可引<br />
起发病,用含 27mg/kg 铜的日粮喂羔羊,16 周内可引起死亡。但江苏小型山羊按 8mg/<br />
kg 体重铜内服,连续 19 周,仅产生肝铜浓度增加,肝功能时有变化的亚临床表现。大量研<br />
究证明,当饲料中锌、铁、钼、硫含量适当时,绵羊对饲料中铜的耐受量为 25mg/Kg,牛<br />
100,猪 250,兔 200,马 800,大鼠 1000,鸡、鸭 300,鹅 100。<br />
各种铜化合物对动物的毒性作用也不一样,它们依次为CuCO3>Cu(NO3)2>CuS04)CuCl2<br />
>Cu2O>CuO(粉)>CuO(针)>Cu(铜丝)。甘氨酸铜软膏毒性很小,依地酸铜(copper edetate)<br />
溶液剂量较大亦可中毒。蛋氨酸铜按 6mg/kg体重剂量是无毒的,但EDTA-Cu、Ca按 3~4mg<br />
/kg体重剂量,可在 48h内致死动物。<br />
【病理】 静脉注射或内服大量溶液态铜盐,对胃肠黏膜可产生直接刺激作用,引起急<br />
性胃肠炎、腹痛、腹泻。高浓度铜溶液在血浆中可直接与红细胞表面蛋白质作用,引起红细<br />
胞膜变性、溶血和死亡。如用硫钼酸盐激发血浆白蛋白,将游离的铜结合到白蛋白上,可缓<br />
解铜中毒。肝脏是体内铜贮存的主要器官,大量铜可集聚在肝细胞的细胞核、线粒体及肝细<br />
胞浆内。可损伤这些细胞的亚细胞结构,在溶血危象发生前几周出现肝功能异常,SGOT、<br />
ARG 酶活性升高,当肝内铜浓度达相当多程度(一般在 6 个月左右),在某些诱因作用下,<br />
可使肝细胞内铜迅速释放入血,血浆铜浓度大幅升高,红细胞变性,红细胞内亨利氏(Heinz)<br />
小体生成,溶血,PCV 下降,血红蛋白尿,黄疸,动物体况迅速下降并死亡。甚至在停止<br />
采食高铜饲料后,亦可发生溶血。有“病”动物在出现溶血危象前,临床上表现健康,一旦<br />
溶血后,多因急性贫血和血红蛋白尿性肾炎而在 48h 内死亡。<br />
应激作用,如营养状况下降、长途运输、泌乳过程等,可诱发肝铜释放。至于产生血管<br />
237
内溶血的机制,目前有多种解释:有人认为是因为大剂量游离态铜对红细胞膜损伤作用;亦<br />
有人认为大量Cu 2+ 可将还原型谷胱甘肽转变为氧化型谷胱甘肽,将血红蛋白氧化为高铁血红<br />
蛋白和变性血红蛋白沉淀物,在红细胞内产生硬而实的Heinz小体,由于该小体在细胞膜内、<br />
外表面机械的和化学的(与红细胞膜表面二硫键)作用,加速了细胞破裂;还有人认为因铜<br />
在体内积累作用,使红细胞转化为自家抗原,并进一步诱导自家抗体生成,形成自体免疫反<br />
应,导致溶血。<br />
肾脏也是铜贮存和排泄器官之一,疾病早期,肾损伤不明显,而溶血危象出现后,产生<br />
肾小管坏死和肾功能衰竭。<br />
【病理变化】 急性铜中毒时,胃肠炎明显。尤其是真胃、十二指肠充血、出血甚至溃<br />
疡,间或真胃破裂。胸、腹腔黄染并有红色积液。膀胱出血。内有红色以至褐红色尿液。慢<br />
性铜中毒时,羊肝呈黄色、质脆,有灶性坏死。肝窦扩张,肝小叶中央坏死,胞浆严重空泡<br />
化,肝脾细胞内有大量含铁血黄色素沉着,肝细胞溶解,电镜观察,肝细胞内线粒体肿胀,<br />
空泡形成。肾肿胀呈黑色,切面有金属光泽,肾小管上皮细胞变性,肿胀,肾小球萎缩。脾<br />
脏肿大,弥漫性瘀血和出血。<br />
猪铜中毒,肝肿大一倍以上、黄染,胆囊扩大,肾、脾肿大、色深,肠系膜淋巴结弥蔓<br />
性出血,胃底黏膜严重出血,食道和大肠黏膜溃疡,组织学变化与羊类似。<br />
狗的铜中毒,肝脏呈灶性坏死。中等程度炎症,后期呈慢性活动期肝炎和肝纤维素性增<br />
生。最终因肝功能衰竭和溶血危象,死亡。<br />
【症状】 羊急性铜中毒时,有明显的腹痛,腹泻,惨叫,频频排出稀水样粪便,有时<br />
排出淡红色尿液,猪、狗可出现呕吐,粪及呕叶物中含绿色至蓝色粘液,呼吸增快,脉博频<br />
数,后期体温下降、虚脱、休克,在 3~48h 内死亡。<br />
慢性铜中毒羊,临床上可分为三个阶段:早期是铜在体内积累阶段,除肝、肾组织铜大<br />
幅度升高、体增重减慢,谷草转氨酶(SGOT),精氨酸酶(ARG)、山梨醇脱氨酶(SDH)<br />
活性短暂升高外,可不显任何临床症状。中期为溶血危象前阶段,肝功能明显异常,SGOT,<br />
SDH,ARG 活性迅速升高,血浆铜浓度也逐渐升高,但精神、食欲变化轻微,此期因动物<br />
个体差异,可维持 1~6 周。后期为溶血危象阶段,动物表现烦渴,呼吸困难、极度干渴,卧<br />
地不起,血液呈酱油色,血红蛋白浓度下降至 52g/L,可视黏膜黄染,红细胞形态异常,<br />
红细胞内出现 Heinz 小体,PCV 下降至 19%,甚至低至 10%。血浆铜浓度急剧升高达 1~7<br />
倍,病羊可在 1~3 天内死亡。<br />
猪中毒时,食欲下降,消瘦,粪稀,有时呕吐。可视黏膜淡染,贫血,后期部分猪死亡。<br />
鹅生活在含 100mg/LCu 的池塘水内,可产生急性中毒死亡。剖检可见腺胃、肌胃坏<br />
死,肺呈淡绿色。成年母鸡喂给含 800~1600mg/kg 铜的日粮,生长缓慢,贫血,有三分之<br />
一鸡死亡。<br />
狗中毒时,呼吸困难,昏睡,可视黏膜苍白,黄染,肝脏变小,体重下降,腹水增多。<br />
鱼的铜中毒见第五章第十一节。<br />
【诊断】 急性铜中毒可根据有接触含高铜的饲料或饮水的病史,结合腹痛、腹泻、<br />
PCV 值下降而初诊。饲料、饮水中铜含量测定有重要意义。慢性铜中毒有赖于对肝脏、肾<br />
脏、血液中铜浓度及酶活性测定。当肝铜浓度>500mg/kg,肾铜>80~130mg/kg(干重)。<br />
各种动物血浆铜浓度多在 0.7~1.2mg/L,若铜浓度大幅度上升,为溶血危象先兆。反刍动<br />
物饲料中铜浓度>30mg/kg,猪、鸡饲料中铜浓度>250mg/kg,或因含铜饲料补充剂未碾<br />
细、未拌匀时可作出进一步诊断。此外血清 SGOT、ARG、SDH 等酶活性稳步上升,PCV<br />
下降,血清胆红素浓度增加,血红蛋白尿及较多红细胞内产生 Heinz 小体,可确诊。但应注<br />
意与其它引起溶血、黄疸的疾病区别。例如,钩端螺旋体病,产后血红蛋白尿,杆菌性血红<br />
蛋白尿,菜籽饼中毒和急性巴氏杆菌病等。但这些病尽管有血红蛋白尿,肝铜浓度却没有变<br />
238
化。<br />
【治疗】 铜中毒的治疗原则是立即中止铜供给、迅速使血浆中游离铜与血浆白蛋白结<br />
合,促进铜排出。<br />
硫钼酸钠不仅可促使Cu 2+ 与白蛋白结合,而且可促进肝铜通过胆汁排入肠道。按<br />
0.5mgMo/kg体重的三硫钼酸钠,稀释成 100ml溶液,缓慢静脉注射,3h后,根据病情还可<br />
追加等剂量钼的硫钼酸钠静脉注射,对急性铜中毒和溶血危相期铜中毒的羊有保护作用。四<br />
硫钼酸钠亦有同样效果,剂量与三硫钼酸钠同。对亚临床铜中毒及经用硫钼酸盐抢救脱险的<br />
动物,每天按在日粮中补充 100mg钼酸铵和 1g无水硫酸钠或 0.2%的硫黄粉,拌匀饲喂,连<br />
续数周,直至粪便中铜降为接近正常时为止。<br />
【预防】 在高铜草地放牧的羊,可在精料中添加 7.5mg/kg 的钼,50mg/kg 锌及 0.2<br />
%的硫,不仅可预防铜中毒,而且有利于被毛生长。鸡粪重加工后不应喂羊。猪、鸡饲料中<br />
补充铜时应充分拌匀,同时应补充锌 100mg/kg,铁 80mg/kg,则可减少铜中毒的机率。<br />
应特别小心,不应将喂猪、鸡的饲料喂羊。<br />
因植物源性发生的铜中毒,秋季应避免在多汁的以三叶草为主的牧场上放牧。减少应<br />
激原性刺激,同时配合补充少量钼酸铵(7mg/kgMo),可预防中毒。对已经有中毒的羊群,<br />
可按每头羊补充 50~l00mg 钼酸铵和 0.3~1.0g 的硫酸钠,连续 3 天,可使死亡现象停止。<br />
COPPER DEFICIENCY<br />
Synopsis<br />
Etiology. Primary copper deficiency due to inadequate levels in diet. Secondary copper deficiency<br />
due to conditioning factors such as excess molybdenum and sulfur in diet. Epidemiology.<br />
Primarily in young pastured ruminants in spring and summer. Primary deficiency occurs in sandy<br />
soil and heavily weathered areas; secondary in peat or muck soil areas. Feed and water supplies<br />
may contain molybdenum, sulfate and iron salts, which interfere with copper metabolism. May be<br />
congenital in newborn lambs (swayback) if ewes deficient or delayed in nursing lambs (enzootic<br />
ataxia). Some breeds of sheep highly susceptible.<br />
Signs. Herd problem. Young growing ruminants on pasture. Unthriftiness, changes in hair color,<br />
chronic diarrhea in molybdenosis (secondary deficiency), chronic lameness, neonatal ataxia,<br />
anemia later stages of deficiency, and falling disease in adult cattle.<br />
Clinical pathology. Low serum and hepatic copper. Ceruloplasmin. Anemia.<br />
Lesions. Anemia, emaciation, hemosiderosis, osteodystrophy, demyelination in enzootic ataxia,<br />
myocardiopathy.<br />
Diagnostic confirmation. Low serum and hepatic copper and response to treatment.<br />
Differential diagnosis list<br />
Copper deficiency must be differentiated from herd problems associated with the following<br />
clinical findings:<br />
•Unthriftiness due to intestinal parasitism (Chapter 26)<br />
•Malnutrition due to energy-protein deficiency (p. 100)<br />
•Lameness caused by osteodystrophy due to calcium, phosphorus and vitamin D imbalance (pp.<br />
561, 1533)<br />
•Anemia due to pediculosis (p. 1398)<br />
•Neonatal ataxia in lambs (congenital swayback and enzootic ataxia) from border disease (p.<br />
1238); cerebellar hypoplasia (daft lamb disease) (p. 1740); hypothermia (pp. 52, 129); meningitis<br />
(p. 538)<br />
239
•Sudden death due to other causes(p. 75).<br />
Treatment. Copper sulfate orally; copper glycinate parenterally.<br />
Control. Provide source of copper by oral dosing or dietary supplementation in feed or on pasture.<br />
Parenteral administration of copper at strategic times. Copper oxide needles orally for prolonged<br />
effectiveness. Controlled-release boluses. Genetic selection. Removal of sulfates from water<br />
supply.<br />
ETIOLOGY<br />
Copper deficiency may be primary, when the intake in the diet is inadequate, or secondary<br />
(conditioned) when the dietary intake is sufficient but the utilization of the copper by tissues is<br />
impeded.<br />
Primary copper deficiency<br />
The amount of copper m the diet may be inadequate when the forage is grown on deficient soils or<br />
on soils in which the copper is unavailable.<br />
Secondary copper deficiency<br />
In secondary copper deficiency, the amount of copper in the diet is adequate, but conditioning<br />
dietary factors interfere with the utilization of the copper. Such secondary copper deficiencies are<br />
summarized in Table 29.2. The administration of copper is preventive and curative. The<br />
conditioning factor is known only in some instances, but a dietary excess of molybdenum is one of<br />
the most common. A high molybdenum intake can induce copper deficiency even when the<br />
copper content of the pasture is quite high, and a higher copper intake can overcome the effect of<br />
the molybdenum. Conversely, supplementation of the diet with molybdenum can be used to<br />
counteract the copper intake when its content in the diet is dangerously high. There are species<br />
differences in response to high copper and molybdenum intake; sheep are much more susceptible<br />
to copper poisoning, cattle to excess molybdenum.<br />
Zinc, iron, lead, and calcium carbonate are also conditioning factors, and in New Zealand the<br />
administration of selenium to sheep on copper-deficient pastures increases copper absorption and<br />
improves the growth rate of lambs. The use of zinc sulfate for the control official eczema may<br />
cause a depression of plasma copper levels, which can be alleviated by the injection of copper<br />
glycinate.<br />
Dietary inorganic sulfate in combination with molybdenum has a profound effect on the<br />
uptake of copper by ruminants. Sheep consuming a complete diet, low in sulfur and molybdenum<br />
and with a modest I 2-20 mg copper/kg dry matter (DM), may die from copper toxicity, while<br />
others grazing pasture of similar copper content but high in molybdenum and sulfur can give birth<br />
to lambs affected with the copper deficiency disease sway-back (1). An increase of sulfate<br />
concentration m a sheep diet from 0.1 to 0.4% can potentiate a molybdenum content as low as 2<br />
mg/kg (0.02 mmol/kg) to reduce copper absorption to below normal levels. Additional sulfate in<br />
the diet also has a depressing effect on the absorption of selenium so that areas of a country with<br />
marginal copper and selenium levels in the soil may produce deficiency syndromes in animals if<br />
sulfate is added; this is likely to happen when heavy dressings of superphosphate are applied. Such<br />
combined deficiencies are becoming more common. The possibility of interaction between copper<br />
and selenium must also be considered because of the reported failure of animals to respond to<br />
treatment unless both elements are provided.<br />
EPIDEMIOLOGY<br />
240
Occurrence<br />
Copper deficiency is endemic worldwide and causes diseases of economic importance that may be<br />
severe enough to render large areas of otherwise fertile land unsuitable for grazing by ruminants<br />
of all ages, but primarily young, growing ruminants. Based on serum copper surveys of cattle<br />
herds in Britain, copper deficiency constitutes a serious problem requiring vigilance. It is<br />
estimated that characteristic clinical signs of copper deficiency develop annually in about 0.9% of<br />
the cattle population in the United Kingdom. In some surveys, the lowest levels of serum copper<br />
were in heifers being reared as heifer replacements. Although heavy mortalities occur m affected<br />
areas, the major loss is due to failure ot animals to thrive. Enzootic ataxia may affect up to 90% of<br />
a lamb flock in badly affected areas and most of these lambs die of inanition. In falling disease, up<br />
to 40% of cattle in affected herds may die.<br />
Geographical distribution<br />
Primary copper deficiency<br />
The diseases caused by ciency of copper in a primary deficiency of copper in ruminants are<br />
enzootic ataxia of sheep in Australia, New Zealand and the United States, licking sickness, or<br />
liksucht of cattle in Holland, and falling disease of cattle in Australia.<br />
Table 29.2 Secondary copper deficiency status<br />
Disease Country Species affected<br />
Swayback<br />
Renguerra<br />
Teart<br />
Scouring disease<br />
Peat scours<br />
Peat scours<br />
Peat scours<br />
Salt sick<br />
Pine (unthrifty)<br />
Britain,united states<br />
Peru<br />
Britain<br />
Holland<br />
New zealand<br />
Britain<br />
Canada<br />
United states(florida)<br />
Scotland<br />
Sheep<br />
Sheep<br />
Sheep and cattle<br />
Cattle<br />
Cattle<br />
Cattle<br />
Cattle<br />
Cattle<br />
Cattle<br />
Copper level in<br />
liver<br />
Low<br />
Low<br />
Unkonw<br />
Unkonw<br />
Low<br />
Unkonw,low<br />
level in blood<br />
Unkonw<br />
Unkonw<br />
Low<br />
A concurrent deficiency of both copper and cobalt occurs in Australia (coast disease) and<br />
Probable<br />
conditionin<br />
g factor<br />
Unkonw<br />
Unkonw<br />
Molybdenu<br />
m<br />
Unkonw<br />
Molybdenu<br />
m<br />
Unkonw<br />
Moiybdenu<br />
m<br />
Unkown<br />
Unkonw<br />
Florida in the United States (salt sickness) and is characterized by the appearance- of clinical signs<br />
of both deficiencies in all species of ruminants. The disease is controlled by supplementation of<br />
the diet with copper and cobalt.<br />
In pigs, copper deficiency may cause anemia in sucking pigs, and reduced growth rate and<br />
cardiac disease in growing pigs. Adult horses are unaffected, but abnormalities of the limbs and<br />
joints of foals reared in copper-deficient areas do occur. Osteochondrosis is associated with a<br />
copper deficiency in young, farmed red deer and wapiti X red deer hybrids in New Zealand (2).<br />
Secondary copper deficiency<br />
241
The diseases caused by secondary copper deficiency, mostly due to high dietary intakes of<br />
molybdenum and sulfate, arc-listed in Table 29.2. They include syndromes characterized by<br />
diarrhea or by unthriftiness. Yellow calf, a disease of nursing calves occurs on Hawaii's<br />
range-land where copper content of forages ranges from 2.6 to 11.8 mg/kg and the molybdenum<br />
from less than 1 to 39 mg/kg. Swayback of lambs in the United Kingdom has been classed as a<br />
secondary copper deficiency, but no conditioning factor has been determined. While swayback is<br />
a naturally occurring disease caused by a primary deficiency of copper, identical lesions occur<br />
experimentally by feeding molybdenum and sulfate to the ewes. There is some evidence that<br />
heavy lime dressing of a pasture may predispose to swayback. A wasting disease similar to peat<br />
scours, and preventable by the administration of copper, and unthriftiness ('pine') of calves, occur<br />
in the United Kingdom, but in both instances the copper and molybdenum intakes are normal.<br />
Molybdenum appears to be the conditioning agent in enzootic ataxia in the United States. A<br />
dietary excess of molybdenum is known to be the conditioning factor in the diarrheic diseases,<br />
peat scours in New Zealand, California, and Canada, and 'teart' in Britain.<br />
A survey in Saskatchewan, Canada, found that 67% of slaughter cattle had liver levels lower<br />
than 10 mg copper/kg on a wet weight (ww). A survey of the copper status of the fetuses and<br />
livers from adult animals found that 20% of steers, 54% of pregnant cows, 52%) of heifers, and<br />
77% of non-pregnant cows had liver levels less than 25 mg/kg DM (3). The concentrations of<br />
copper in the liver of the fetuses were directly proportional to the liver copper concentrations in<br />
the darns (3). Liver copper levels of fetuses from dams with liver copper greater than 25 mg/kg<br />
DM were higher than those in fetuses from dams with liver copper levels lower than 25 mg/kg<br />
DM. During gesta¬tion, the level of copper progressively increased in the fetal liver and decreased<br />
in the maternal liver. The concentration of copper in fetal livers increased with increasing fetal age<br />
and at term the new¬born calf has high levels of liver copper to meet postnatal requirements<br />
because cows' milk is a poor source of copper. The magnitude of copper deficiency in \ some<br />
areas is extensive and emphasizes the importance of adequate copper nutrition in pregnant cattle in<br />
order to maintain adequate fetal levels of copper.<br />
Seasonal incidence<br />
Both primary and secondary copper deficiency occur most commonly in spring and summer<br />
coinciding with the lowest levels of copper in the pasture.<br />
Large monthly variations occur in the serum levels of copper in both beet and dairy cattle and<br />
are commonly correlated with the rainfall; the higher the rainfall the lower the copper level.<br />
The incidence of secondary copper deficiency may be highest at other times, depending upon<br />
the concentration of the conditioning factor in the forage. For example, the molybdenum content<br />
may be highest in the autumn when rains stimulate a heavy growth of legumes.<br />
Risk factors<br />
Several factors influence the plasma and tissue concentrations of copper, particularly in ruminants,<br />
including:<br />
•Age of animal<br />
•Demands of pregnancy and lactation<br />
•Stage of growth<br />
•Copper sources available to the animals<br />
•Mineral composition of feed<br />
•Season of the year<br />
242
•Soil characteristics and its mineral composition<br />
•Breed of animal<br />
•Concentration of minerals, such as sulfur and molybdenum, which can interfere with the<br />
availability of copper (4, 5).<br />
Animal factors<br />
Age susceptibility<br />
Young animals are more susceptible to primary copper deficiency than adults. Calves on dams fed<br />
deficient diets may show signs at 2-3 months of age. As a rule, the signs are severe in calves and<br />
yearlings, less severe in 2-year-olds, and of minor degree in adults. Enzootic ataxia is primarily a<br />
disease of sucking lambs whose dams receive insufficient dietary copper. Ewes with a normal<br />
copper status take some time to lose their hepatic reserves of copper after transfer to<br />
copper-deficient pastures and do not produce affected lambs for the first 6 months. The occurrence<br />
of the disease in sucklings, and its failure to appear after weaning, point to the importance of fetal<br />
stores of copper and the inadequacy of milk as a source of copper. Milk is always a poor source of<br />
copper and when it is the sole source of nourishment the intake of copper will be low. Milk from<br />
normal ewes contains 20-60 ug/dL (3.1-9.4 umol/L) copper, but under conditions of severe copper<br />
deficiency this may be reduced to 1 2 (0.16-0.31 umol/L).<br />
Breed susceptibility<br />
There are marked genetic differences in copper metabolism between breeds of sheep. The Welsh<br />
Mountain ewe can absorb copper 50% more efficiently than the Scottish blackface (6), and the<br />
Texel cross blackface 145% more efficiently than pure blackface lambs (6). The susceptibility to,<br />
or protection from, the effects of copper deficiency, and also copper poisoning, is influenced from<br />
birth by genetic effects. These affect copper status of the lamb at birth, through the maternal<br />
environment controlled by the dam's genes and through the effect of the lamb's own genes. Later<br />
in life, the animal's own genes become the predominant influence determining its copper status on<br />
any given nutritional regimen. These genetic differences have physiological consequences<br />
reflected in differences m the incidence of swayback, both between and within breeds, and in<br />
effects on growth and possibly on reproduction. The differences observed are due to genetic<br />
differences in the efficiency of absorption of dietary copper.<br />
The genetic effects determining the copper status of the lamb are already present in utero, and<br />
the effects are not controlled by the lamb's own genotype but by that of its dam. The maternal<br />
effect is still present at weaning at 9 weeks of age, but disappears after weaning when the genetic<br />
differences are due to the sheep's own genotype.<br />
The existence of genes determining plasma copper has been shown by the successful continued<br />
selection for high and low concentrations in closed lines of a single breed type. Ram selection is<br />
made on the basis of plasma copper concentrations at 18 and 24 weeks of age. The proportion of<br />
the normal variation in plasma copper that is heritable is 0.3. I he high-line female sheep retain<br />
more copper in the liver than the low-line females, caused by a positive correlation between the<br />
concentration of copper in plasma and the efficiency of absorption (7).<br />
The genetic variation in the copper metabolism of sheep has important physiological<br />
consequences. Breeds show wide variation in their susceptibility to sway-back; the incidence of<br />
swayback may vary from 0 to 40% between breeds within one Hock, and the incidence according<br />
to breed type is closely related to the differences in the concentration of copper in the liver than in<br />
blood. When these high and low female lines are placed on improved and limed pasture, which<br />
243
can induce a severe copper deficiency, soon after birth there are indications of sway-back, general<br />
dullness, lack of vigor and mortality m the lambs. By 6 weeks of age the mortality rate is higher in<br />
the lambs from the low copper line than in those from the high copper line. In addition, at 6 weeks<br />
of age, lambs from the low line are 2 kg lighter than those in the high line.<br />
Certain breeds of cattle, e.g. the Simmental and Charolais, may haw: higher copper<br />
requirements than other breeds, e.g. Angus, and these differences may be related to differences in<br />
copper absorption in the gastrointestinal tract (8, 9).<br />
Fetal liver copper<br />
During gestation, the copper concentration increases progressively in the ovine and bovine fetal<br />
liver and decreases in the maternal liver (10). The developing bovine fetus obtains its copper by<br />
placenta] transfer and at birth the liver concentration of copper is high and declines postnatally<br />
to adult levels within the first few months (3). Placental transfer is less efficient in sheep, and<br />
lambs are commonly born with low liver reserves, making the neonatal lambs susceptible to<br />
copper deficiency (10). In copper-deficient cattle, the accumulation of liver copper in the fetus<br />
continues independent of the dam's liver copper until the fetus is about 180 days, then a gradual<br />
decline in fetal liver copper occurs. The liver copper concentration in fetuses from dams on a<br />
copper-adequate diet continues to increase and not decline at 180 days of gestation. All of this<br />
indicates an increase in copper requirements by the dam during pregnancy; during the last month<br />
of pregnancy, the daily requirement for copper in cattle increases to approximately 70% above the<br />
mainte¬nance requirements, which means that the dietary allowance of 10 mg/kg DM needs to be<br />
increased up to 25 mg/kg DM during pregnancy (10). The concentrations of copper, iron,<br />
manganese, and zinc are consistently lower than normal in the livers of aborted fetuses, indicating<br />
a non-specific change in trace element status which is probably an effect of abortion, and not a<br />
cause (11).<br />
Colostrum is rich in copper, allowing the newborn with its preferential ability to absorb copper<br />
to increase hepatic stores. Later, the copper content of milk declines rapidly so that it is usually<br />
insufficient to meet the requirements of the sucking neonate for copper. The young milk-fed<br />
animal is able to absorb about 80% of its copper intake, but the efficiency of absorption declines<br />
with age as the rumen becomes functional, when only 2-10% of available copper is absorbed.<br />
Dietary factors<br />
Pasture composition<br />
The absorption (or availability) of copper is influenced by the type of diet, the pres¬ence of other<br />
substances in the diet such as molybdenum, sulfur and iron, the interaction between the type of<br />
diet and the chemical composition of the diet, and the genetic constitution of the animals (6).<br />
Copper is well-absorbed from diets ' low in fiber, such as cereals and brassicas, but poorly<br />
absorbed from fresh forage. Conservation of grass as hay or silage generally improves its<br />
availability. This explains why copper deficiency is a problem of the grazing animal and seen only<br />
rarely in housed ruminants receiving diets that are commonly adequate in copper.<br />
Molybdenum and sulfur<br />
Only small increases in the molybdenum and sulfur concentration of grass will cause major<br />
reductions in the availability of copper (6). This is especially notable in ruminants grazing<br />
improved pastures in which the molybdenum and sulfur concentrations were increased. The<br />
copper content of feedstuffs should be expressed in terms of available copper concentration, using<br />
appropriate equations, which permits a more accurate prediction of clinical disease and can be<br />
244
used for more effective control strategies.<br />
The effect of changes in molybdenum and sulfur concentrations m grass on the availability of<br />
copper is changed by conservation. At a given concentration of sulfur, the antagonistic effect of<br />
molybdenum is proportionately less in hay than in fresh grass. At a low concentration of<br />
molybdenum the effect of sulfur is more marked in silage than in fresh grass. The use of<br />
formaldehyde as a silage additive may weaken the copper sulfur antagonism and yield material of<br />
high availability (6). Thus, fields of herbage high in molybdenum should be used for conservation<br />
when possible, and sulfuric acid should not be used as an additive for silage unless accompanied<br />
by a copper salt because it significantly raises the sulfur concentration of the silage.<br />
Copper in diet<br />
For general purposes, pasture containing less than 3 mg/kg DM of copper will result in signs of<br />
deficiency m grazing ruminants. Levels of 3-5 mg/kg DM can be considered as dangerous, and<br />
levels greater than 5 mg/kg DM (preferably 7 12) are safe unless complicating factors cause<br />
secondary copper deficiency. The complexity of minimum copper requirements, affected as they<br />
are by numerous conditioning factors, necessitates examination under each particular set of<br />
circumstances. For example, plant molybdenum levels are related directly to the p}l reaction of<br />
the soil. Grasses grown on strongly acidic molybdenum-rich soils are characterized by low<br />
molybdenum values (less than 3 mg/kg DM), whereas those associated with alkaline<br />
molybdenum-poor soils may contain up to 17 mg/kg DM. Thus, it seems likely that conditioned<br />
copper deficiency can be related to regionally enhanced levels of plant available rather than soil<br />
molybdenum.Heavily limedpastures are often associated with a less than normal copper intake and<br />
a low copper status of sheep grazing them. Secondary copper deficiency is also recorded in pigs<br />
whose drinking water contains very large amounts of sulfate.<br />
Dietary iron<br />
A dietary intake of iron can interfere with copper metabolism (12). Dietary levels of iron in the<br />
range of 500-1500 mg/kg DM, within the range of their fluctuation in silage and forage, and<br />
higher levels, are a risk of inducing copper deficiency in ruminants, especially when the copper<br />
intake is marginal. Ruminants obtain iron from ingested soil and mineral supplements and, in<br />
areas where hypocuprosis is likely to occur, the risk can be minimized by avoiding the use of<br />
mineral supplements of high iron content, minimizing the use of bare winter pasture and avoiding<br />
the excessive contamination of silage with soil during harvesting.<br />
Molybdenum-induced secondary copper deficiency in cattle occurred when motor oil<br />
containing molybdenum bisulfide was spilled on a pasture located on the side of a railway bed<br />
near the farm (13).<br />
Stored feeds<br />
Livestock that are housed are in a different position to those on pasture. Concentrates and<br />
proprietary feeds usually contain adequate copper. Pasture is less likely to contain sufficient<br />
copper, especially in early-spring when the grass growth is lush, and silage and haylage may be<br />
deficient. lay is more mature and usually contains more of all minerals, so that animals housed for<br />
the winter are protected against copper deficiency for ,a few weeks after they come out onto<br />
pasture in the spring. Young, growing animals will be first affected. These comments should not<br />
be interpreted to mean that housed or feedlot animals cannot be affected by hypocuprosis; they<br />
can if the locally produced feed is copper-deficient, or more likely has a high concentration of<br />
molybdenum. Both are likely to be prevented, or less severe, it there is some supplementary<br />
245
feeding.<br />
Soil characteristics<br />
Copper deficiency<br />
In general, there are two types of soil on which copper-deficient plants are produced. Sandy soils,<br />
poor in organic matter and heavily weathered, such as on the coastal plains of Australia, and in<br />
marine and river silts, are likely to be deficient in copper as well as other trace elements,<br />
especially cobalt.<br />
The second important group of soils are 'peat' or muck soils reclaimed from swamps, and<br />
are soils more commonly associated with copper deficiency in the United States, New Zealand,<br />
and Europe. Such soils may have an absolute deficiency of copper, but more commonly the<br />
deficiency is relative in that the copper is not available and the plants growing on the soils do not<br />
contain adequate amounts of the element.<br />
The cause of the lack of availability of the copper is uncertain, but is probably the formation of<br />
insoluble organic copper complexes. An additional factor is the production of secondary copper<br />
deficiency on these soils due to their high content of molybdenum. A summary of the relevant<br />
levels of copper in soils and plants is given in Table 29.3.<br />
Molybdenum excess<br />
Pastures containing less than 3 mg/kg DM of molybdenum are considered to be safe, but disease<br />
may. occur at 3-10 mg/kg DM if the copper intake is low. Pastures containing more than 10 mg/kg<br />
DM of molybdenum are dangerous unless the diet is supplemented with copper. Excess<br />
molybdenum may occur in soils up to levels of 10 and even 100 mg/kg. Perhaps more dangerous<br />
is the risk that overzealous application of molybdenum to pasture to increase bacterial nitrogen<br />
fixation may have similar effects, which are likely to be long-lasting.<br />
In the United Kingdom appreciable land is underlain by marine black shales rich in<br />
molybdenum, resulting in a high content of molybdenum in the soil and pastures, and in a<br />
secondary copper deficiency that, potentially, limits livestock performance. Secondary<br />
(conditioned) copper deficiency is now recognized in cattle in many parts of Canada. Large areas<br />
of west-central Manitoba are underlain by molybdeniferous shale bedrocks and the soils contain<br />
up to 20 mg/kg of molybdenum. However, in the same geographical location, hypocupremia may<br />
be associated with a primary deficiency of copper in the forage, or a secondary copper deficiency<br />
clue to molybdenum in the forages.<br />
PATHOCLNES1S<br />
Effects on tissues<br />
Copper is necessary in tissue oxidation by either supplementing cytochrome oxidase systems or<br />
entering into their formation. Ceruloplasmin is the copper-containing enzyme through which<br />
copper exerts its physiological function. The pathogenesis of most of the lesions of copper<br />
deficiency has been explained in terms of faulty tissue oxidation because of failure of these<br />
enzyme systems. This role is<br />
Table 29.3 Copper levels of soils and plants in primary and secondary copper deficiency<br />
Condition Area<br />
Soil type Soil copper<br />
246<br />
mg/kg<br />
Plant<br />
copper<br />
(mg/kg dry<br />
matter)
Normal<br />
Primary copper<br />
deficiencyWes<br />
Secondary copper<br />
deficiency<br />
-<br />
West Australia<br />
New Zealand<br />
New Zealand<br />
HollandSand<br />
New Zealand<br />
Britain<br />
Britain<br />
Britain<br />
Ireland<br />
Holland<br />
Canada<br />
-<br />
various<br />
Sand<br />
Peat<br />
Sand<br />
Peat<br />
Peat<br />
Limestone<br />
Stiff clay<br />
Shale deposits,<br />
peat marine alluvial soils<br />
sand<br />
Burned-over peat<br />
18-22<br />
1-2<br />
0.1-0.6<br />
-<br />
-<br />
5<br />
-<br />
-<br />
-<br />
-<br />
20-60<br />
exemplified in the early stages of copper deficiency by the changes in the wool of sheep.<br />
Wool<br />
11<br />
3-5<br />
3<br />
3<br />
5<br />
10-25<br />
The straightness and stringiness of this wool is due to inadequate keratinization, probably due to<br />
imperfect oxidation of free thiol groups. Provision of copper to such sheep is followed by<br />
oxidation of these free thiol groups and a return to normal keratinization within a few hours.<br />
Body weight<br />
In the later stages of copper deficiency the impairment of tissue oxidation causes interference with<br />
intermediary metabolism and loss of condition or failure to grow.<br />
Diarrhea<br />
The pathogenesis of copper deficiency in causing diarrhea is uncertain and there is little evidence<br />
that a naturally-occurring primary copper deficiency will cause diar-rhea. There are no histologica]<br />
changes in gut mucosa, although villous atrophy is recorded in severe, experimentally produced<br />
cases. Diarrhea is usually only .a major clinical finding in secondary copper deficiency associated<br />
with molybdenosis.<br />
Anemia<br />
The known importance of copper in the formation of hemoglobin accounts for the anemia in<br />
copper deficiency. The presence of hemosiderin deposits in tissues of copper-deficient animals<br />
suggests that copper is necessary for the reutilization of iron liberated from the normal breakdown<br />
of hemoglobin. There is no evidence of excessive hemolysis in copper-deficiency states. Anemia<br />
may occur in the later stages of primary copper deficiency, but is not remarkable in the secondary<br />
form unless there is a marginal copper deficiency, as occurs in peat scours in New Zealand. The<br />
unusual relation¬ship in New Zealand between copper deficiency and postparturient<br />
hemoglobinuria is unexplained. Heinz body ane-mia in lambs with deficiencies of copper or<br />
selenium and moved from improved pasture to rape (Brassicaa napus) has been reported.<br />
Bone<br />
The osteoporosis that occurs in some natural cases of copper deficiency is caused by the<br />
depression of osteoblastic activity (14).<br />
In experimentally induced primary copper deficiency, the skeleton is osteoporotic and there is a<br />
247
significant increase in osteoblastic activity. There is a marked overgrowth of epiphyseal cartilage,<br />
especially at costochondral junctions and in metatarsal bones. This is accompanied by beading of<br />
the ribs and enlargement of the long bones. There is also an impairment of collagen formation.<br />
When the copper deficiency is secondary to dietary excesses of molybdenum and sulfate, the<br />
skeletal lesions are quite different and characterized by widening of the growth plate and<br />
metaphysis, and active osteoblastic activity.<br />
Copper deficiency in foals causes severe degenerative disease of cartilage, characterized by<br />
breaking of articular and growth plate cartilage through the zone of hypertrophic cells, resulting in<br />
osteochondrosis of the articular-epiphyseal complex (A-E complex) (5). The incidence and<br />
severity of osteochondrosis in foals can be decreased by supplementation of the diets of mares<br />
during the last 3-6 months of pregnancy and the first 3 months of lactation (4). Foals from<br />
non-supplemented mares have separation of the thickened cartilage from the subchondral bone.<br />
Clinical, radiographic, and biochemical differences occur between copper-deficient and<br />
copper-supplemented foals (16), and there may be a relationship between low copper intakes in<br />
rapidly growing horses, inferior collagen quality, biomechanically weak cartilage, and<br />
osteochondritis (17).<br />
Copper is essential for metalloenzyme lysyl oxidase, which produces aldehydic groups on<br />
hydroxylysine residues as a prerequisite for eventual cross-link formation in collagen and elastin.<br />
Similar lesions in foals have been attributed to zinc toxicity from exposure of affected animals to<br />
pasture polluted by smelters. Experimentally, the addition of varying amounts of zinc to the diet of<br />
foals containing adequate copper will result in zinc-induced copper deficiency (5), but there are no<br />
effects with zinc intakes up to 580 ppm and it is suggested that 2000 ppm or higher are necessary<br />
to affect copper absorption in horses (18). Similar lesions of osteochondrosis have occurred in<br />
young tanned red deer and wapiti X red deer hybrids in New Zealand (2).<br />
Connective tissue<br />
Copper is a component of the enzyme lysyl oxidase, secreted by the cells involved in the synthesis<br />
of the elastin component of connective tissues and has important functions in maintaining the<br />
integrity of tissues such as capillary beds, ligaments, and tendons.<br />
Heart<br />
The myocardia] degeneration of falling disease may be a terminal manifestation of anemic anoxia,<br />
or be due to interference with tissue oxidation. In this disease it is thought that the stress of calving<br />
and lactation contribute to the development of heart block and ventricular fibrillation when there<br />
has already been considerable decrease in cardiac reserve. Experimentally induced copper<br />
deficiency in piglets causes a marked reduction in growth and hematocrit, and cardiac pathology<br />
and electrical disturbances (19).<br />
Blood vessels<br />
Experimentally produced copper deficiency has also caused sudden death due to rupture of the<br />
heart and great vessels in a high proportion of pigs fed a copper-deficient diet. The basic defect is<br />
degeneration of the internal elastic laminae. I here is no record of a similar, naturally occurring<br />
disease. A similar relationship appears to have been established between serum copper levels and<br />
fatal rupture of the uterine artery at parturition in aged mares.<br />
Pancreas<br />
Lesions of the pancreas may be present in normal cattle with a low blood copper status. The<br />
lesions consist of an increase in dry matter content and a reduction in the concentrations of protein<br />
248
and copper in wet tissue. The cytochrome oxidase activity and protein: RNA ratio are also reduced.<br />
There are defects in acinar basement membranes, splitting and disorganization of acini, cellular<br />
atrophy and dissociation, and stromal proliferation.<br />
Nervous tissue<br />
Copper deficiency halts the formation of myelin and causes demyelination in lambs, probably by a<br />
specific relationship between copper and myelin sheaths. Defective myelination can commence as<br />
early as the midpoint of the fetus's uterine life. The focus of lesions in the white matter shifts from<br />
the cerebrum in lambs affected at birth (congenital swayback) to the spinal cord in delayed cases,<br />
which may reflect respective peaks of myelin development at those sites at 90 days of gestation<br />
and 20 days after birth. The postnatal development of delayed sway-back has been confirmed<br />
through its control by copper supplementation after birth. In experimental animals it has been<br />
shown that copper deficiency does interfere with the synthesis of phospholipids. While anoxia is a<br />
cause of demyelination, an anemic anoxia is likely to occur in highly deficient ewes, and anemic<br />
ewes produce a higher proportion of lambs with enzootic ataxia, there is often no anemia in ewes<br />
producing lambs with the more common subacute form of the disease. Severely deficient ewes<br />
have lambs affected at birth .and in which myelin formation is likely to have been prevented. The<br />
lambs of ewes less severely deficient have normal myelination at birth, and develop demyelination<br />
in postnatal life.<br />
Reproductive performance<br />
There is no evidence that copper deficiency causes reproductive failure in dairy cows. Copper<br />
glycinate given to dairy cattle does not affect the average interval in days between calving and<br />
first observed heat, services per conception, or first service conception rate compared to untreated<br />
cows in the same population. Experimentally, the addition of molybdenum to the diet of heifers<br />
delayed the onset of puberty, decreased the conception rate, and caused anovulation and anestrus<br />
in cattle without accompanying changes in copper status or in liveweight gain. Thus, the presence<br />
of molybdenum rather than low copper status may affect reproductive performance of cattle.<br />
Geo-chemical data indicate that approximately 10% of the cultivated area of England and Wales<br />
have soils that may result in forage molybdenum concentrations similar to those used in the above<br />
experimental diet. It appears inadvisable to ascribe poor reproductive performance to subclinical<br />
hypocuprosis on the evidence of blood copper analysis alone. Other factors, such as management<br />
and energy and protein intake, should be examined.<br />
Immune system<br />
Copper deficiency results in decreased humoral and cell-mediated immunity, as well as decreased<br />
non-specific immunity regulated by phagocytic cells, such as macrophages and neutrophils. The<br />
decreased resistance to infection in sheep is amenable to treatment with copper and genetic<br />
selection. In lambs genetically selected for low and high concentrations of plasma copper, the<br />
mortality from birth to 24 weeks of age in the high line was half that in the low line. Most of the<br />
losses were due to a variety of microbial infections. Experimental viral and bacterial infections of<br />
cattle can cause a rapid, though transient, increase in serum ceruloplasmin and plasma copper in<br />
copper-replete animals, suggesting a major protective role for copper in infectious diseases (20).<br />
These changes in copper metabolism evolve from an interleukin-1 mediated increase in hepatic<br />
synthesis and release of ceruloplasmin, an acute phase protein (20). Copper concentrations in<br />
organs involved in immune regulations such as liver, spleen, thymus, and lung are substantially<br />
reduced by copper deficiency, suggesting that copper-deficient animals are at greater risk for<br />
249
infection than copper-adequate animals. Experimental copper depletion and repletion did not<br />
affect neutrophil or lymphocyte function in growing beef cattle heifers (21).<br />
The severity of copper depletion needed for immune dysfunction is less than required to induce<br />
clinical signs of copper deficiency, and endogenous copper may contribute to the regulation of<br />
both non-immune and immune inflammatory responses. Low molecular weight complexes may<br />
have an anti-inflammatory effect in animal models of inflammation, and it is postulated that the<br />
elevation of plasma copper-containing components during inflammatory disease represents a<br />
physiological response.<br />
Sequence of clinical signs development<br />
In experimental copper deficiency in calves, beginning at 6 weeks of age, sub-clinical and<br />
clinical abnormalities appear after the following intervals: hypocupremia at 15 weeks, growth<br />
retardation from 15 to 18 weeks, rough hair coat at 17 weeks, diarrhea at 20 weeks, and leg<br />
abnormalities at 23 weeks. These signs correlate well with the onset of hypocupremia and are<br />
indicative of a severe deficiency. Even with these signs of deficiency, the histological<br />
abnormalities may be only minor in degree.<br />
In experimental primary copper deficiency in calves, beginning at 12 weeks of age, clinical<br />
signs of the deficiency may not become apparent for about 6 months. Musculoskeletal<br />
abnormalities include a stilted gait, a ‘knock-kneed' appearance of the forelimbs, overextension of<br />
the flexors, splaying of the hooves, and swellings around the etacarpophalangeal and<br />
carpometacarpal joints. Changes in hair pigmentation occur after about 5 months, and diarrhea<br />
between 5 and 7 months. The diarrhea ceased 12 hours after oral administration of a small amount<br />
(10 mg) of copper.<br />
Copper-molybdenum-sulfate relationship<br />
The interaction between copper, molybdenum, and sulfur in ruminant nutrition is unique in its<br />
effects on health and production. Copper, molybdenum, and sulfur from organic or inorganic<br />
sources can combine in the rumen to form an unabsorbable triple complex, copper<br />
tetrathiomolybdate, and deplete the host tissues of copper (1).<br />
Secondary or conditioned copper deficiency occurs when the dietary intake of copper is<br />
adequate, but absorption and utilization of the copper are inadequate because of the<br />
presence of interfering substances in the diet (1). Molybdenum and sulfate alone orin<br />
combination can affect copper metabolism and the mechanisms by which this occurs are now<br />
being clarified. This effect also operates in the fetus and interferes with copper storage in the fetal<br />
liver. Besides the relationship with molybdenum, an interaction between the absorption of copper<br />
and selenium has been demonstrated, the administration of selenium to sheep on copper-deficient<br />
pastures causing an improvement in copper absorption.<br />
The toxicity of any level of dietary molybdenum is affected by the ratio of the dietary<br />
molybdenum to dietary copper. The critical copper:molybdenum ratio in animal feeds is 2, and<br />
feeds or pasture with a lower ratio may result in conditioned copper deficiency. In some regions of<br />
Canada, the copper: molybdenum ratio will vary from 0.1 to 52.7 (5). Higher critical ratios closer<br />
to 4.1-5.1 have been recommended for safety (5). The influence of dietary molybdenum on copper<br />
metabolismin ponies has been examined experimentally.<br />
The copper status of growing calves can also be affected to a similar degree by the inclusion of<br />
appropriate levels of supplementary iron or molybdenum in the diet. Following such inclusion, the<br />
liver and plasma concentrations of copper will decline within 12-16 weeks to levels indicating<br />
250
severe copper deficiency. The clinical signs of copper deficiency, as indicated by reduced growth<br />
rate and changes in the hair texture and color, are evident after 16-20 weeks only in animals<br />
supplemented with molybdenum. The reduced growth rate was accompanied by a decreased feed<br />
intake and reduced efficiency of feed utilization.<br />
Copper absorption<br />
On the basis of a response to copper injections and no response to copper administered orally to<br />
sheep on a high molybdenum intake, it is suggested that interference occurs with the absorption of<br />
copper from the gut.<br />
It is proposed that thiomolybdates from in the rumen from the reaction of dietary molybdenum<br />
compounds with sulfides produced from the reduction of dietary sulfur compounds by rumen<br />
bacteria. The thiomolybdates reduce the absorption of dietary copper from the intestine and also<br />
inhibit a number of copper-containing enzymes. including ceruloplasmin, cytochrome oxidase,<br />
superoxide dismutase, and tyrosine oxidase.<br />
Copper utilization<br />
Sulfate and molybdate can interfere with mobilization of copper from the liver, inhibition of<br />
copper intake by the tissues, inhibition of copper transport both into and out of the liver, and<br />
inhibition of the synthesis of copper-storage complexes and ceruloplasmin.<br />
The clinical signs of hypocuprosis (such as steely wool) can occur in sheep on diets containing<br />
high levels of molybdenum and sulfate, even though blood copper levels are high. Tins suggests<br />
that under these circumstances copper is not utilizable in tissues and the blood copper rises in<br />
response to the physiological needs of the tissues for the element. In pigs, a copper-molybdenum<br />
complex can existin animals and that in this form the copper is unavailable. This would interfere<br />
with hepatic metabolism of copper and the formation of copper-protein complexes such as<br />
ceruloplasmin.<br />
Hepatic storage<br />
The copper status of the liver depends on whether the animals are receiving adequate dietary<br />
copper. With adequate dietary levels, the liver copper levels are less in the presence of molybdate<br />
and sulfate. If the animals are receiving a copper-deficient diet such that copper is being removed<br />
from the liver, then the molybdate plus sulfate animals retain more copper in their liver than<br />
copper-deficient animals not receiving sulfate plus molybdate. This supports the hypothesis that<br />
molybdate and sulfate together impair the movement of copper into or out of the liver, possibly by<br />
affecting copper transport. Sulfate alone exerts an effect. An increasein intake reduces hepatic<br />
storage of both copper and molybdenum.<br />
Phases of copper deficiency<br />
The development of a deficiency can be divided into tour phases:<br />
1.Depletion<br />
2.Deficiency (marginal)<br />
3.Dysfunction<br />
4.Disease.<br />
During the depletion phase there is loss of copper from any storage site, such as liver, but the<br />
plasma concentrations of copper may remain constant. With continued dietary deficiency the<br />
concentrations of copper in the blood decline during the phase of marginal deficiency. However, it<br />
may be some time before the concentrations or activities of copper-containing enzymes in the<br />
tissues begin to decline and it is not until this happens that the phase of dysfunction is reached.<br />
251
There may be a further lag before the changes in cellular function are manifested as clinical signs<br />
of disease.<br />
Summary<br />
The overall effect of these interactions is as follows. Molybdate reacts with sulfides to produce<br />
thiomolybdatesin the rumen.The subsequent formation of copper-thiomolybdate complexes<br />
isolates the copper from being biologically available (1). The thiomolybdates reduce the<br />
effectiveness of enzymes containing copper and there are some significant interactions between<br />
copper, zinc, and iron.<br />
CLINICAL FINDINGS<br />
The general effects of copper deficiency are the same in sheep and cattle, but in addition to these<br />
general syndromes there are specific syndromes more or less restricted to species and to areas.<br />
What follows is a general description of the disease caused by copper deficiency, in turn followed<br />
by the specific syndromes of enzootic ataxia, swayback, falling disease, peat scours, teart, and<br />
unthriftiness (pine).<br />
Cattle<br />
Subclinical hypocuprosis<br />
No clinical signs occur, blood copper levels are marginal or below 57 mg/dL (9.0 mmol/L) and<br />
there is a variable response in productivity after supplementation with copper. Some surveys in<br />
copper-deficient areas found that about 50% of beef herds and 10% of dairy herds within the same<br />
area have low blood levels of blood copper associated with low copper intake from natural forages.<br />
The deficiency is likely to be suspected only if production is monitored and found to be<br />
supoptimal.<br />
A perplexing feature of subclinical hypocuprosis is the wide variation in improved growth rate<br />
obtained when cattle of the same low copper status are given supplementary copper under field<br />
conditions.<br />
General syndrome<br />
Primary copper deficiency<br />
Primary copper deficiency causes unthriftiness. loss of milk production, and anemia in adult cattle.<br />
The coat color is affected, red and black cattle changing to a bleached, rusty red. and the coat itself<br />
becomes rough and staring. In severely deficient states, which are now uncommon, calves grow<br />
poorly, and there is an increased tendency for bones to fracture, particularly the limb bones and<br />
the scapula. Ataxia may occur after exercise, with a sudden loss of control of the hindlimbs and<br />
the annual tailing or assuming a sitting posture. Normal control returns after rest. Itching and<br />
hair-licking are also recorded as manifestations of copper deficiency in cattle. Although diarrhea<br />
may occur, persistent diarrhea is not characteristic of primary copper deficiency and its occurrence<br />
should arouse suspicion of molybdenosis or helminthiasis. In some affected areas, calves develop<br />
stiffness and enlargement of the joints and contraction of the flexor tendons causing the affected<br />
animals to stand on their toes. These signs may be present at birth or occur before weaning.<br />
Paresis and incoordination are not evident.<br />
An increased occurrence of postparturient hemoglobinuria is also recorded, but only in New<br />
Zealand, and may be unrelated to copper deficiency.<br />
Secondary copper deficiency<br />
This syndrome includes the signs of primary copper deficiency, except that anemia occurs less<br />
commonly, probably due to the relatively better copper status in the secondary state, anemia being<br />
252
largely a terminal sign in primary copper deficiency. For example, anemia occurs in peat scours of<br />
cattle in New Zealand, but in this instance the copper intake is marginal. In addition to the other<br />
signs, however, there is a general tendency for diarrhea to occur, particularly in cattle. Because<br />
diarrhea is not a major sign in naturally occurring primary copper deficiency it is possible that it is<br />
due to the conditioning factor, which reduces the availability of copper. For example, the severity<br />
of the diarrhea is roughly proportional to the level of intake of molybdenum.<br />
Falling disease<br />
The characteristic behavior in falling disease is for cows in apparently good health to throw up<br />
their heads, bellow, and fall. Death is instantaneous in most cases, but some fall and struggle<br />
feebly on their sides for a few minutes with intermittent bellowing, and running movement<br />
attempts to rise. Rare cases show signs for up to 24 hours or more. These animals periodically<br />
lower their heads and pivot on the front legs. Sudden death usually occurs during one of these<br />
episodes.<br />
Peat scours (‘teart')<br />
Persistent diarrhea with the passage of watery, yellow-green to black feces with an inoffensive<br />
odor occurs soon after the cattle go on to affected pasture, in some cases within 8-10 days. The<br />
feces are released without effort, often without lifting the tail. Severe debilitation is common,<br />
although the appetite remains good. The hair coat is rough and depigmentation is manifested by<br />
reddening or gray flecking, especially around the eyes, in black cattle. The degree of abnormality<br />
varies a great deal from season to season and year to year, and spontaneous recovery is common.<br />
Affected animals usually recover in a few days following treatment with copper.<br />
Unthriftiness (pine) of calves<br />
The earliest signs are a stiffness of gait and unthriftiness. The epiphyses of the distal ends of the<br />
metacarpus and metatarsus may be enlarged and resemble the epiphysitis of rapidly growing<br />
calves deficient in calcium and phosphorus or vitamin D. The epiphyses are painful on palpation<br />
and some calves are severely lame. The pasterns arc upright and the animals may appear to have<br />
contracted flexor tendons. The unthriftiness and emaciation are progressive and death may occur<br />
in 4-5 months. Grayness of the hair, especially around the eyes in black cattle, is apparent.<br />
Diarrhea may occur in a few cases.<br />
Sheep<br />
General syndrome<br />
Primary copper deficiency<br />
Abnormalities of the wool are the first observed signs, and may be the only sign in areas of<br />
marginal copper deficiency. Fine wool becomes limp, glossy and loses its crimp, developing a<br />
straight, steely appearance. Black wool shows depigmentation to gray or white, often in bands<br />
coinciding with the seasonal occurrence of copper deficiency. The straight, steely defect may<br />
occur in similar bands, and the staple may break easily. There appear to be some differences<br />
between breeds in susceptibility to copper deficiency. Merino sheep appearing to have a higher<br />
copper requirement than mutton sheep. The fleece abnormalities of Merino sheep in Australia<br />
have not been observed in Romney Marsh sheep in copper-deficient areas in New Zealand, but<br />
this may be due in part to the difficulty of detecting abnormality in wool that is normally rather<br />
straight and steely. Anemia, scouring, unthriftiness, and infertility may occur in conditions of<br />
extreme deficiency, but in sheep the characteristic findings are in the lamb, the disease enzootic<br />
ataxia being the major manifestation. Retardation of growth, diarrhea, delay to marketing, and<br />
253
increased mortality are common clinical findings in lambs genetically selected for low plasma<br />
copper and placed on improved and limed upland pastures. Osteoporosis, with increased tendency<br />
of the long bones to fracture, has also been recorded under conditions of copper deficiency<br />
insufficient to cause enzootic ataxia.<br />
Swayback and enzootic ataxia in lambs and goat kids<br />
These diseases have much in common, but there are differences in epidemiology and some subtle<br />
clinical ones.<br />
SWAYBACK is the only authentic manifestation of a primary nutritional deficiency of copper in<br />
the United Kingdom. The incidence can vary greatly among breeds of sheep, reflecting the genetic<br />
differences in copper metabolism both between and within breeds of sheep. The disease occurs in<br />
several forms.<br />
A congenital form, cerebrospinal swayback, occurs only when the copper deficiency is<br />
extreme. Affected lambs are born dead or weak and unable to stand and suck. Incoordination and<br />
erratic movements are more evident than in enzootic ataxia and the paralysis is spastic in type.<br />
Blindness also occurs occasionally. There is softening and cavitation of the cerebral white matter<br />
and this probably commences about day 120 of gestation.<br />
Progressive (delayed) spinal swayback begins to develop some weeks after birth with lesions<br />
and clinical signs appearing at 3-6 weeks of age.<br />
Postnatal acute fatal swayback may be a third form of the disease, and appears to occur only in<br />
Wales. It resembles the more usual delayed form, but develops suddenly. There is a sudden onset<br />
of recumbency with death occurring 1-2 days later due to acute swelling of the cerebrum.<br />
ENZOOTIC ATAXIA affects only un-weaned lambs. In severe outbreaks the lambs may be<br />
affected at birth, but most cases occur in the 1-2-month age group. The seventy of the paresis<br />
decreases with increasing age at onset. Lambs affected at birth or within the first month usually<br />
die within 3-4 days. The disease in older lambs may last for 3-4 weeks and survival is more likely,<br />
although surviving lambs always show some ataxia and atrophy of the hindquarters. The first sign<br />
to appear in enzootic ataxia is incoordination of the hindlimbs. appearing when the lambs are<br />
driven. Respiratory and cardiac rates are also greatly accelerated by exertion. As the disease<br />
progresses, the incoordination becomes more severe and may be apparent after walking only a few<br />
yards. There is excessive flexion of joints, knuckling over of the fetlocks, wobbling of the<br />
hindquarters and finally falling. The hindlegs are affected first and the lamb may be able to drag<br />
itself about in a sitting posture. When the forelegs eventually become involved recumbency<br />
persists and the lamb dies of inanition. There is no true paralysis, the lamb being able to kick<br />
vigorously even in the recumbent stage.the appetite remains unaffected.<br />
Enzootic ataxia due to copper deficiency has been reported in young goat kids. The disease is<br />
similar in most respects to the disease in lambs. Kids may be affected at birth, or the clinical signs<br />
may be delayed until the animals are several weeks of age. Cerebellar hypoplasia is a frequent<br />
finding in goats.<br />
Other species<br />
Deer<br />
Enzootic ataxia in red deer is remarkably different from the disease in lambs in that it develops<br />
in young adults well past wearning age, and in adults. The clinical signs include ataxia, swaying of<br />
the<br />
hindquarters, a dog-sitting posture and,eventually, inability to use the hindlimbs.Spinal cord<br />
254
demyelination and midbrain neuronal degeneration are characteristic. osteochondrosis of young,<br />
farmed deer with copper deficiency is characterized by lameness, one or more swollen joints, and<br />
an abnormal ‘bunny-hopping' gait or ‘cow-hocked' stance (2). Copper deficiency in red deer in<br />
Australia during a period of drought caused loss of weight in lactating hinds after calving and<br />
steely hair coats (the hair had a lustre resembling that of so-called steely wool of copper-deficent<br />
sheep). Both adult and yearling stags had normal hair coats but those of the yearling hinds were<br />
patchy, with large areas of harsh, light colored, steely hair (22). The high sulfur content of the diet<br />
and possible accidental iron ingestion from being fed on the ground may have resulted in<br />
secondary copper deficiency.<br />
Pigs<br />
Naturally occurring enzootic ataxia has occurred in growing pigs 4-6 months of age. Posterior<br />
paresis progresses to complete paralysis in 1-3 weeks. Dosing with copper salts had no effect on<br />
the clinical conditions, but hepatic copper levels were 3-14 mg/kg (0.05-0.22 mmol/kg). Copper<br />
deficiency in piglets 5-8 weeks of age has been reported and was characterized clinically by ataxia,<br />
posterior paresis, nystagmus, inability to stand, paddling movements of the limbs and death in 3-5<br />
days. Demyelination of the spinal cord, and degenerative lesions of the elastic fibers of the walls<br />
of the aorta and pulmonary arteries were present.<br />
The inclusion of copper sulfate, at levels of 125-250 mg/kg of copper, in the diets of pigs 11-90 kg<br />
liveweight and fed ad libitum, results in slight improvements in growth rate and feed efficiency,<br />
but has no significant effect on carcass characteristics (23). The supplemental copper causes a<br />
marked increase in liver copper concentration which poses a potential hazard and it is<br />
recommended that copper supplementation be limited to starter and grower diets fed to pigs<br />
weighing less than 50 kg liveweight.<br />
Horses<br />
Adult horses are unaffected by copper deficiency, but there are unconfirmed reports of<br />
abnormalities of limbs of foals. Foals in copper-deficient areas may be unthrifty and slow-growing,<br />
with stiffness of the limbs and enlargement of the joints. Contraction of the flexor tendons causes<br />
the animal to stand on its toes. There is no ataxia or indication of involvement of the central<br />
nervous system. Signs may be present at birth or develop before weaning. Recovery occurs slowly<br />
after weaning and foals are unthrifty for up to 2 years.<br />
CLINICAL PATHOLOGY<br />
The laboratory evaluation of the copper status of form animals is complex because the<br />
biochemical values are often difficult to interpret and to correlate with the clinical state of the<br />
animal. Interpretation of the copper status of an individual animal is more difficult than of a herd.<br />
The guidelines for the laboratory diagnosis of primary and secondary copper deficiency in cattle<br />
and sheep are summarized in Table 29.4.<br />
HERD DIHAGNOSIS The diagnosis of copper deficiency in a herd of animals is based on a<br />
combination of collection and interpretation of the history, clinical examination of the affected<br />
animals, laboratory tests on serum and liver samples, and examination of the environment<br />
including analysis of the feed and water supplies, and perhaps soil analysis (24).<br />
It is necessary to be especially careful when collecting specimens for copper analysis to avoid<br />
contamination by needles, copper distilled water, vial caps, cans for liver specimens, and other<br />
possible sources of copper. An additional problem is the possible effect of intercurrent disease on<br />
plasma levels of copper.<br />
255
TREATMENT RESPONSE TRIAL A comparison of health and production variables in a group<br />
of animals treated with copper, and a similar group not treated with copper, is also desirable.<br />
Variables include calf growth rates, calf mortality, and reproductive performance.<br />
COPPER STATUS OF HERD In order to assess the copper status of herd, a standard practice is<br />
to take blood samples at random from at least 10% of clinically affected animals and from 10% of<br />
normal animals. however, this may be inapprot<br />
Table 29.4 Copper levels in body tissues and fluids in primary and secondary copper deficiency<br />
Species and tissue Normal level<br />
Cattle<br />
Blood plasma<br />
(fig/mL) (convert to<br />
SI units by<br />
multiplying<br />
by 15.7 which gives<br />
nmol/L). Adult liver<br />
(mg/kg dry matter)<br />
(convert to SI units by<br />
multiplying by 0.0157<br />
which gives mmol/kg)<br />
Milk (mg/L) Hair<br />
(mg/kg)<br />
Sheep<br />
Blood plasma (ug/mL)<br />
Adult liver (mg/kg dry<br />
matter)<br />
1.26±31<br />
More than 100<br />
(usually 200)<br />
0.05-0.20<br />
6.6-10.40.7-1.3More<br />
than 200 (usually<br />
350+)<br />
Primary copper<br />
deficiency<br />
Less than 0.5 and as<br />
low as 0.1-0.2<br />
Less than 20 and as<br />
low as 4<br />
0.01-0.02<br />
1.8-3.4<br />
0.1-0.2<br />
20<br />
Secondary copper<br />
deficiency<br />
Less than 0.5 and as<br />
low as 0.2-0.3<br />
Less than 10<br />
5.5<br />
0.4-0.7<br />
15-19<br />
priate when there may be a wide variation in the serum copper concentration within a herd. In<br />
some cases, a 10% sample may be too large and in other cases too small. The minimal sample size<br />
for random samples from a finite population of a normal continuously distributed variable has<br />
been calculated as follows:<br />
[n = Nt2cv2/[(N-1)E2 t2cv2 ]]<br />
Where n = minimal sample size; N= herd size; = Student t value; cv = coefficient of variation; and<br />
E = allowable error. Initial testing can be used to estimate variability of serum copper<br />
concentration within a herd, and a minimal sample size may be calculated. Each class of animal<br />
according to age groups, diet, and production status should also be sampled. Follow-up samples<br />
should be taken from the same animals following therapy or the institution of control measures.<br />
Laboratory diagnosis<br />
Historically, the laboratory diagnosis of copper deficiency in cattle and sheep centered on the<br />
determination of serum or plasma copper and liver copper. However, it is now known that serum<br />
copper levels alone are not reliable as indicators of copper status, and liver samples collected<br />
either by liver biopsy or at slaughter should be used to accurately assess copper status in cattle (25,<br />
26). Clinically normal animals may have marginal levels of serum copper, or unthrifty animals<br />
may have marginal or deficient serum levels of copper. Furthermore, when either the normal<br />
256
animals with the marginal levels of copper or the unthrifty animals with the marginal or deficient<br />
levels are treated with copper there may or may not be an improvement in weight gain as might be<br />
expected in the former, or improvement in clinical condition in the latter.<br />
Phases<br />
The development of a deficiency can be divided into four phases:<br />
1.Depletion<br />
2.Deficiency (marginal)<br />
3.Dysfunction<br />
4.Disease.<br />
During the depletion phase, there is loss of copper from any storage site, such as liver, but the<br />
plasma concentrations of copper may remain constant. With continued dietary deficiency the<br />
concentrations of copper in the blood will decline during the phase of marginal deficiency.<br />
However, it may be some time before the concentrations or activities of copper-containing<br />
enzymes in the tissues begin to decline, and it is not until this happens that the phase of<br />
dysfunction is reached. There may be a further lag before the changes in cellular function are<br />
manifested as clinical signs of disease.<br />
Interpretation of laboratory results<br />
The three principles governing the interpretation of biochemical criteria of trace element status<br />
include:<br />
•The relationships between the concentration of the marker and the intake of the element<br />
•The time the animal is on an adequate diet<br />
•Disturbances of tissue function.<br />
From these principles, the concentrations of liver copper are insensitive indices of deficiency,<br />
but good indicators of excess. Plasma copper less than 57µg/dL (9 µmol/L) is a good index of<br />
marginal deficiency, but values may have to fall to below 19µg/dL.(3µmol/L) before there is a risk<br />
of dysfunction and loss of production in sheep and cattle. However, these are only guidelines. The<br />
range of values and the cut-off levels above which animals are normal, or below which they<br />
are deficient, have not been well-established. There is considerable biological variation<br />
dependent on the species, the breed of animal, the length of time over which the depletion has<br />
occurred, and the presence of intercurrent disease.<br />
Concentrations of copperin liver and blood may be of diagnostic value but should be interpreted<br />
with caution since clinical signs of copper deficiency may appear before there are significant<br />
changes in the levels of copper in the blood and liver. Conversely, the plasma levels of copper<br />
may be very low in animals that are otherwise normal and performing well. There is a tendency to<br />
overestimate the presence of copper deficiency because veterinarians use a diagnostic threshold<br />
for copper deficiency that is too high (27). Among veterinary laboratories, there is a wide<br />
variation in the normal range currently used for equine serum copper values (28).<br />
Plasma and hepatic copper levels<br />
Cattle and sheep<br />
In cattle and sheep, plasma copper levels between 19µ g/dL and 57 µg/dL (3.0 and 9.0 µmol/L)<br />
represent marginal deficiency, and levels below 19µg/dL (3 µmol/L) represent functional<br />
deficiency or hypocuprosis. The internationally recognized threshold to assess copper deficiency<br />
is 9.4µ mol/L (27). In both species。a value for plasma or serum of 11.0 µmol/L can be associated<br />
with a liver concentration from 789 to 3786 µmol/kg DM (50-240 mg/kg). By contrast, a value of<br />
257
9.3µ mol/L will usually be associated with liver copper values of 315-789 µmol (20-50 mg/kg<br />
DM), which are regarded as marginally inadequate. Plasma copper levels of 49.9 µg/dL (7.85<br />
µmol/L) or less are indicative of low liver copper levels. Plasma copper levels above 90.2 µg/dL<br />
(14.2 µmol/L) are usually associated with liver levels above 38.1 mg/kg (0.6 mmol/kg) DM. Of<br />
the two estimations, that on liver is the most informative as levels in blood may remain normal for<br />
long periods after liver copper levels commence to fall and early signs of copper deficiency appear.<br />
Levels of copperin adult liver above 200 mg/kg DM (3.14 mmol/kg) in sheep, and above 100<br />
mg/kg DM (1.57 mmol/kg) in cattle are considered to be normal.. Levels of less than 80 mg/kg<br />
DM (1.5 mmol/kg) in sheep, and less than 30 mg/kg DM (0.5 mmol/kg) in cattle are classed as<br />
low. Liver copper levels in fetuses and neonates are usually much higher than in adults, and<br />
normal foals have had levels of 219 mg/kg (3.4 mmol/kg DM) compared to a normal of 31 mg/kg<br />
(0.49 mmol/kg DM) in adults.<br />
Milk and hair copper<br />
The levels of copper in milk and hair are also lower in deficient than in normal cattle and<br />
estimation of the copper content of hair is now acceptable as a diagnostic aid. It has the advantage<br />
of providing an integrated progressive record of nutritional intake. The levels of copper in bovine<br />
hair are more markedly depressed when extra molybdenum is fed.<br />
Ceruloplasmin<br />
The difficulty of interpreting plasma levels of copper led to the estimation of plasma levels of<br />
copper-protein complexes, especially ceruloplasmin. Ceruloplasmin contains greater than 95% of<br />
the circulating copper in normal animals. There is a highly significant correlation between plasma<br />
copper levels and plasma ceruloplasmin activity, which is a less complicated and more rapid<br />
procedure than plasma copper. The regression analyses indicate a strongly positive correlation<br />
coefficient of ceruloplasmin with serum of cattle and sheep of 0.83 and 0.92,respectively. The<br />
correlation between serum ceruloplasmin activity and hepatic copper concentrations in cattle was<br />
only 0.35, indicating an unreliable relationship. Normal plasma ceruloplasmin levels in sheep are<br />
in the region of 45-100 mg/L. Normal levels of serum ceruloplasmin activity in cattle range from<br />
120 to 200 mg/L. The mean copper and ceruloplasmin levels are higher in plasma than serum; the<br />
percentage of copper associated with ceruloplasmin is lessin serum (55%) thanin plasma (66%).<br />
Normal plasma ceruloplasmin levelsin sheep range from 4.5 to 10 mg/dL. In experimental primary<br />
copper deficiencyin calves, rapid decreases occurin plasma ceruloplasmin activity at least 80 days<br />
before overt clinical signs of deficiency.<br />
Erythrocyte dismutase<br />
The measurement of the activity of erythrocyte superoxide dismutase (ESOD), a<br />
copper-containing enzyme, is now being evaluated as a procedure for the diagnosis of copper<br />
deficiency. The activity of this enzyme decreases more slowly than plasma or liver copper in<br />
copper-deficient animals and may be more closely correated with the presence of imminence of<br />
hypocuprosis. In marginal deficiency, the ESOD value ranges from 2 to 5 U/mg hemoglobin, and<br />
in functional deficiency the value is below 2 (29).<br />
Hepatic copper<br />
Because the liver is a storage compartment for copper, the concentrations of liver copper indicate<br />
the state of depletion rather than deficiency. There is no particular threshold value for liver copper<br />
below which the performance and health of livestock are likely to be impaired. A broad range of<br />
values may, for example, coincide with the marginally deficient state, e.g. 5.1-20.3 mg (0.08-0.32<br />
258
mmol) copper/kg liver DM. The concentration of hepatic copper in sheep is uniform, and a single<br />
biopsy sample should be representative of the whole liver. The technique of liver biopsy for<br />
assessing the copper status of sheep has been evaluated. Frequency of biopsy does not affect<br />
copper concentration, the variability between successive samples is small, and the biopsy<br />
procedure does not reduce body weight or rate of gain. Copper concentrations in the kidney cortex<br />
may be of more diagnostic value because concentrations are normally within a narrow range of<br />
12.7-19.0 mg/kg DM (0.2-0.3 mmol/kg DM). Thus, concentrations below 12.7 mg/kg DM (0.2<br />
mmol/kg DM) in the kidney may be a more reliable indicator of dysfunction than liver copper<br />
concentration.<br />
Horses<br />
A threshold level of plasma copper of 16 umol/L is used to distinguish between the normal and<br />
subnormal values (30). Liver copper from horses sampled at slaughter vary widely about a mean<br />
of 113.7n.mol/kg WW (30). The threshold of 52.5 umol/kg WW of copper in liver is proposed to<br />
distinguish deficient from marginal liver copper status. Many healthy horses have serum values<br />
between 12 and 16 umol/L.<br />
The mean hepatic copper concentrations of horses fed diets containing 6.9-15.2 mg copper/kg<br />
DM were 17.1-21.0 µg/g DM (0.27-0.33 umol/g DM) tissue. The plasma copper concentrations<br />
ranged from 3.58 to 4.45 ug/dL (22.8-28.3 umol/L). There was no simple mathematical<br />
relationship between plasma and hepatic copper concentrtions. The range of serum copper<br />
concentrations in Thoroughbred horses at grass was 63-196 ug/dL (9.91-30.85 mmol/L), and in<br />
stabled Thoroughbreds the range was 47-111 ug/dL (7.40-17.47 mmol/L).<br />
Hematology<br />
Anemia may occur in advanced cases of primary copper deficiency, hemoglobin levels being<br />
depressed to 50- 80 g/L and erythrocytes to 2-4 X 10 12 /L. A high proportion of cows in problem<br />
herds may have a Heinz-body anemia without evidence of hemoglobinuria, and the severity of the<br />
anemia will be related to the hypocupremia.<br />
NECROPSY FINDINGS<br />
The characteristic gross findings in copper deficiency of ruminants are those of anemia and<br />
emaciation. Hair and wool abnormalities may be present as already described. Extensive deposits<br />
of hemosiderin can cause darkening of the liver, spleen and kidney in most cases of primary<br />
copper deficiency, and in the secondary form if the copper status is sufficiently low. In lambs<br />
there may be severe osteoporosis and long bone fractures. Osteoporosis is less evident in cattle,<br />
but can be confirmed radiographically and histologically. In naturally occurring secondary copper<br />
deficiency in cattle, associated with high dietary molybdenum and sulfate, there is widening of the<br />
growth plates due to abnormal mineralization of the primary spongiosia, resulting in a grossly<br />
rachitic appearance to the bones.<br />
The most significant finding in enzootic ataxia is the degeneration of axons and myelin within<br />
the cerebellar and motor tracts in the spinal cord, a change only evident at the microscopic level.<br />
Chromatolysis of neurons in a variety of locations within the central nervous system is usually<br />
detectable. In a few extreme cases, and in most cases of sway-back, the myelin loss also involves<br />
the cerebrum, where there is destruction and cavitation of the white matter. There is marked<br />
internal hydrocephalus in such cases and the convolutions of the cerebrum are almost obliterated.<br />
Acute cerebral edema with marked brain swelling and cerebellar herniation, reminiscent of<br />
polioencephalomalacia, may also accompany the more typical myelopathy and multifocal cerebral<br />
259
leukomalacia in lambs with hypocuprosis.<br />
In falling disease, the heart is flabby and pale. There is generalized venous congestion and the<br />
blood may appear watery. The liver and spleen are enlarged and dark. Histological examination<br />
reveals atrophy of the cardiac muscle fibers and considerable cardiac fibrosis. Deposits of<br />
hemosiderin are present in the liver, spleen and kidney.<br />
Necropsy findings associated with copper deficiency in non-ruminant species are not<br />
well-documented. Degenerative changes with subsequent rupture of the aorta have been<br />
experimentally induced in swine, but this has not been described as a naturally occurring disease.<br />
A myelopathy with white matter changes similar to those of enzootic ataxia has also been reported<br />
in 4-5-month-old copper-deficient pigs. Musculoskeletal changes similar to those described for<br />
calves have also been reported in foals with hypocuprosis.<br />
Necropsy examinations should include assay of copper in viscera .The levels of copper in liver<br />
are usually low (see Table 29.4), and in secondary copper deficiency there may be a high level of<br />
copper in the kidney, and high levels of molybdenum in the liver, kidney, and spleen. Copper<br />
levels in body tissues and Hinds in primarm and secondary copper deficiency are listed in Table<br />
29.4.<br />
Samples for confirmation of diagnosis<br />
•Toxicology - 50 g liver, kidney(ASSAY (Cu) (Mo)).<br />
•Histology - formalin-fixed samples of:long bone (including growth plate),skin, liver, spleen.<br />
Enzootk ataxia/<br />
swaybaik: halt of midsagittally-sectioned brain, lumbar and cervical spinal cord. Falling disease:<br />
heart (several sections), bone marrow, spleen(LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
The clinical findings which are common in young, growing ruminants, include a herd problem of<br />
unthriftiness and progressive loss of weight, changes in hair coat color or texture of wool, chronic<br />
lameness, neonatal ataxia in lambs and kids, and terminal anemia. In adult cattle on pasture with<br />
excess molybdenum, chronic diarrhea is charactic. A combination of serum and liver copper, and<br />
serum molybdenum, are major diagnostic aids in distinguishing between copper deficiency and<br />
the other diseases.<br />
Several disease complexes that are herd or flock problems in cattle and sheep may resemble<br />
both primary and secondary copper deficiency. The emphasis is on many animals being affected at<br />
about the same time, with a chronic debilitating disease complex, under the same dietary and<br />
seasonal circumstances.<br />
Cattle<br />
Unthriftiness and progressive weight loss may be due to protein-energy malnutrition and<br />
examination of the diet will reveal the cause.<br />
Changes in hair coat color in young growing cattle is caused only by copper deficiency.<br />
Chronic lameness in young growing cattle may be caused by a calcium, phosphorus and<br />
vitamin D imbalance,which is determined by examination of the diet and radiography of the long<br />
bones. The radiographic changes in cattle with secondary copper deficiency consist of widened<br />
irregular epiphyseal plates with increased bone density in the metaphysis and metaphyseal lipping.<br />
These findings are similar to those described for rickets and secondary nutritional<br />
hyperparathyroidism in cattle.<br />
Chronic diarrhea in young cattle may be due to intestinal parasitism and fecal examination<br />
260
and response to therapy are diagnostic. Diarrhea in a group of adult cattle on pasture known to be<br />
high in molybdenum is probably due to secondary copper deficiency and response to therapy is<br />
diagnostic.<br />
Winter dysentery of cattle, salmonellosis, coccidiosis and mucosal disease are acute diseases<br />
characterized by diarrhea but are accompanied by other signs and clinicopathological findings<br />
which facilitate their identification. Many poisons, particularly arsenic, lead and salt, cause<br />
diarrhea in ruminants but there are usually additional diagnostic signs and evidence of access to<br />
the poison. Assay of feed and tissues helps to confirm a diagnosis of poisoning.<br />
A diagnosis of peat scours is usually made if there is an immediate response to oral dosing<br />
with a copper salt.<br />
Falling disease occurs only in adult cattle and must be differentiated from other causes of<br />
sudden death. Poisoning by the gidgee tree (Acacia georginaa) produces a similar syndrome in<br />
cattle.<br />
Sheep and goats<br />
Unthriftiness and abnormal wool or hair as a flock or herd problem are characteristic of copper<br />
deficiency in sheep and goats, which must be differentiated from protein-energy malnutrition,<br />
intestinal parasitism, cobalt deficiency, and external parasites.<br />
Lameness in a group of lambs several weeks of age must be differentiated from nutritional<br />
osteodystrophy due to a calcium, phosphorus and vitamin D deficiency or imbalance, stiff lamb<br />
disease due to enzootic muscular dystrophy.<br />
Neonatal ataxia caused by congenital swayback and enzootic ataxia in newborn lambs and kids<br />
due to maternal copper deficiency must be differentiated from border disease of newborn lambs,<br />
characterized by an outbreak of newborn lambs with hairy fleece and tremors, cerebellar<br />
hypoplasia (daft lamb disease), and hypothermia.<br />
TREATMENT<br />
The treatment of copper deficiency is relatively simple, but it advanced lesions are already present<br />
in the nervous system or myocardium complete recovery will not occur. Oral dosing with 4 g of<br />
copper sulfate for calves from 2 to 6 months of age and 8-10 g for mature cattle given weekly for<br />
3-5 weeks is recommended tor the treatment of primary or secondary copper deficiency.<br />
Parenteral injections of copper glycinate may also be used and the dosages are given under control.<br />
The diet of affected animals should also be supplemented with copper. Copper sulfate may be<br />
added to the mineral-salt mix at a level of 3-5% of the total mixture. A commonly recommended<br />
mixture for cattle is 50% calcium-phosphorus mineral supplement. 45% cobalt-iodized salt, and<br />
3-5% copper sul-tate. This mixture is offered free of choice or can be added to a complete diet at<br />
the rate of 1% of the total diet.<br />
CONTROL<br />
Dietary requirements<br />
The minimum dietary requirement for copper for cattle is 10 mg copper/kg DM and 5 mg/kg DM<br />
for sheep.<br />
The requirement necessary to prevent subclinical or clinical copper deficiency will depend on<br />
the presence of interfering substances such as molybdenum, sulfur and iron in the diet and<br />
possibly the genotype of the animal. Copper sulfate is considered a better supplement than copper<br />
oxide needles or injectable copper for cattle consuming diets containing excess molybdenum or<br />
molybdenum plus sulfur. Although there is a marked difference between breeds of sheep in their<br />
261
susceptibility to hypocuprosis, this would not seem to have an immediate practical application.<br />
The estimated copper requirement in the diet of mature ponies is 3.5 mg/kg DM.<br />
Copper can he supplied by several different methods as outlined below. The dose rates given<br />
are those recommended for the control of primary copper deficiency, and these may have to be<br />
increased or treatment given more frequently in some instances of secondary copper deficiency. In<br />
these circumstances it is often necessary to determine the most satisfactory dosing strategy by a<br />
field trial.<br />
Copper sulfate<br />
Oral closing<br />
Oral dosing with copper sulfate (5 g tocattle, 1.0 g to sheep, weekly) is adequate<br />
as prophylaxis and will prevent the occurrence of swayback in lambs if the ewes are dosed<br />
throughout pregnancy. Lambs can be protected after birth by dosing with 35 mg of copper sulfate<br />
every 2 weeks. However, regular oral dosing with copper sulfate is laborious and time-consuming<br />
and is no longer widely practiced.<br />
Dietary supplementation<br />
The copper sulfate may be mixed with other minerals into a mineral premix, which is then<br />
incorporated into the concentrate part of the ration. The final concentration of copper is usually<br />
adjusted to provide an overall intake of at least 10 ppm of copper in the DM of the final ration. If<br />
the forage components of the ration contain much less than 10 ppm, the concentrate part of the<br />
ration may need to contain much larger concentrations of copper. Where a secondary copper<br />
deficiency is due to molybdenum in the forage, up to 1200 mg copper (approximately 5 g of<br />
hydrated copper sulfate) is added to the concentrate daily. When sheep are grazing toxic lupin<br />
stubble, the signs of lupinosis may be exacerbated by the supplementation of only 10 mg<br />
copper/kg DM as copper sulfate, and therefore the supply of copper in the absence of suitable<br />
amounts of molybdenum and sulfur should be kept to a minimum (31).<br />
If animals are not receiving concenrates containing copper, an alternative is to provide free<br />
access to a mineral mixture or salt-lick containing 0.25-0.5% of copper sulfate for sheep and 2%<br />
for cattle, which will supply sufficient copper provided an adequate intake of the mixture is<br />
assured. The mineral mixture usually contains iodized salt, cobalt, calcium, phosphorus, and other<br />
trace minerals.<br />
In some deficient areas, an effective method of administering copper is by the annual<br />
top-dressing of pasture with 10 kg/hectare copper sulfate, although the amount required mayvary<br />
widely with the soil type and the rainfall. Top-dressing may cause copper poisoning if livestock<br />
are turned onto pasture while the copper salt is still adherent to the leaves. Treated pasture should<br />
be left unstocked for 3 weeks or until the first heavy rain. It is also possible that chronic copper<br />
poisoning may result if the copper status of the soil increases sufficiently over a number of years.<br />
Addition of copper salts to drinking water is usually impractical because the solution corrodes<br />
metal piping, and maintenance of the correct concentration of copper in large bodies of water is<br />
difficult. However, if the need is great, some way around these difficulties can usually be found<br />
and a system has been devised for automatic supplementation for short periods via the drinking<br />
water, and has been effective in controlling copper deficiency in cattle. Copper pellets which<br />
provide 2-3 mg copper/L of water have been recommended for cattle. Calves can tolerate copper<br />
in milk replacers at a concentration of 50 ppm but there is no advantage in providing more than 10<br />
ppm.<br />
262
There is no evidence that copper or molybdenum supplementation of the diets of pregnant ewes<br />
and lambs at 10 mg/kg DM had any effect on selenium status.<br />
Removal of sulfates<br />
The removal of sulfates from drinking water by water purification, using a process of reverse<br />
osmosis, may have a positive effect on the copper status of beef cows. Cows drinking desulfated<br />
water had an increased availability of copper compared to those drinking water containing a large<br />
concentration of sulfates.<br />
Parenteral injections of copper<br />
To overcome the difficulty of frequent individual dosing or top-dressing of parture, periodic<br />
parenteral injection of copper compounds that release copper gradually has given good results.<br />
They can be given at strategic times depending on the circumstances. They also have the<br />
advantage of avoiding fixation of copper by molybdenum in the alimentary tract. Injectable<br />
preparations of copper are now the method of choice for the prevention of swayback in lambs. The<br />
following have been evaluated under field conditions:<br />
•Copper calcium ethylenediamine tetra-acetate (copper calcium<br />
edetate)<br />
•Copper methionate<br />
•Copper heptonate<br />
•Copper glycinate<br />
•Copper oxyquinoline sulfonate.<br />
The criteria used to judge these injections are minimal damage at the site of injections,<br />
satisfactory liver storage (90-100%) of the administered dose, and a safe margin between<br />
therapeutic and toxic doses. The dose of copper in any of the compounds for cattle is 400 mg and<br />
for sheep 150 mg. Copper heptonate at the rate of 25 mg of copper in 2 mL of preparation given<br />
by IM injection to ewes in mid-pregnancy was successful in preventing swayback in lambs.<br />
Copper calcium edetate has the advantage of giving maximum copper storage very quickly - 1<br />
week after injection - and blood levels are elevated within a few hours. Because of the rapidity of<br />
the absorption, toxic effects can be encountered unless proper dose levels are observed. As well as<br />
deaths from serious overdosing, some deaths occur in groups of sheep for unexplained reasons. It<br />
is suggested that stress be minimized and simultaneous other therapy be avoided.<br />
A marked local reaction occurs at the site of injection so that SC injection is preferable in<br />
animals to be used for meat, although to avoid an unsightly blemish, breeding animals should<br />
receive an IM injection. The injections are a small risk for precipitating blackleg in cattle on farms<br />
where this disease occurs. For sheep, a single injection of 45 mg of copper as copper glycinate in<br />
midpregnancy is sufficient to prevent swayback in the lambs.<br />
The SC injection of copper calcium edetate or copper oxyquinoline sulfonate into sheep<br />
results in a rapid increase in the concentration of copper in whole blood, serum, and urine within<br />
the first 24 hours. Following the injection of copper methionate, the concentration of. copper in<br />
blood and serum rises steadily over a period of 10 days, and there is no detectable increase in<br />
urinary copper. After the injection of any of the three compounds, there is a steady increase in<br />
serum ceruloplasmin activity over a period of 10-20 days, followed by a slow fall to preinjection<br />
activity by 40 days. The lower toxicity of copper injected as methionate compared with that as<br />
copper calcium edetate or copper oxyquinoline sulfonate is due to the slower absorption and<br />
transport of the copper to the liver and kidney. Death has occurred in sheep following the<br />
263
parenteral administration of diethylamine oxyquinoline sulfonate at recommended doses. Affected<br />
sheep manifested signs of hepatic encephalopathy, and at necropsy there was acute, severe,<br />
generalized, centrilobular hepatocellular necrosis. The use of copper disodium edetate at<br />
recommended doses in calves has also resulted in deaths associated with liver necrosis and clinical<br />
signs of hepatic encephalopathy.<br />
Injectable copper glycinate is an excellent source of supplementary copper for increasing the<br />
concentration of copper in the serum of copper-deficient cattle and maintaining grazing cattle in<br />
an adequate copper status. One dose of copper glycinate will maintain adequate copper levels for<br />
about 60-90 days. The recommended dose in beef herds is 120 mg of copper for adult cattle and<br />
60 mg of copper for calves. A supplemental source of copper is required for the calf during the<br />
pasture season because milk is a poor source of copper, particularly from copper-deficient cows,<br />
and calves do not have the opportunity to increase or maintain body stores of copper while grazing.<br />
When the dam is severely hypocupremic in the spring, the calf is also severely hypocupremic or<br />
copper-deficient. Insufficient copper is secreted into the milk of copper-treated cows. Therefore,<br />
where the dam has not received an adequate copper intake during pregnancy, direct treatment of<br />
the calf will be required in early life. The copper reserves of newborn calves are increased in fetal<br />
liver at the expense of copper stores in the dam's liver, which are dependent on the availability ot<br />
dietary or supplemental copper to the dam. Calves usually have sufficient liver copper at birth and<br />
do not need an injection of 50 mg until they are 6 weeks old. Because of the higher requirements<br />
for copper during the last trimester of pregnancy (demands of the fetal liver), a program of copper<br />
supplementation should involve the use of copper supplements, throughout the year as required.<br />
One dose of copper glycinate is sufficient when cattle are grazing forage that contains no more<br />
than 3 mg/kg DM of molybdenum and 3 g/kg DM of sulfur. With higher levels of molybdenum<br />
and sulfur, repeated injections of copper glycinate are recommended. The injectable copper may<br />
be supplemented by the use of copper sulfate in a mineral supplement at a level of 1%. The<br />
inclusion of copper sulfate in the mineral supplement may be adequate for cows, but the calves<br />
may not consume an adequate amount of mineral and injectable copper. The level of<br />
supplementation required to prevent a drop in serum copper over the pasture season will depend<br />
upon the concentration of dietary molybdenum and sulfur and their effect upon the coefficient of<br />
absorption of copper.<br />
Injectable copper complex compounds have been evaluated as supplementary copper for<br />
grazing beef cattle under Canadian conditions. Copper edetate at 100 mg of copper, copper<br />
glycinate at 120 mg, and copper methionate at 120 mg were used and were equally effective in<br />
improving copper status of copper-deficient cattle and maintaining them in an adequate copper<br />
status for 90 days (32). The copper methionate was least acceptable because of the incidence and<br />
severity of reactions at the site of injection.<br />
Controlled-release glass<br />
Death due to poisoning is one of the dangers of parenteral administration because it is difficult to<br />
control the rate at which the supplement releases the copper, especially if the controlling<br />
mechanism is chemical binding. Methods used to control the release include the development of<br />
soluble controlled-release glass for oral administration to sheep and cattle. The copper is slowly<br />
released, absorbed, and stored in the liver. Initial field evaluations indicate that the boluses may<br />
not contain sufficient copper to maintain normal levels of copper for a sufficient length of time<br />
compared to the use of copper oxide needles.<br />
264
Boluses of a soluble copper-containing controlled-release glass have been devel¬oped and<br />
evaluated. The boluses are based on a phosphate-type glass into which appropriate quantities of<br />
trace elements are incorporated. The boluses lodge in the rumen and release copper at a slow rate.<br />
They can provide additional supplies of copper to ruminants at an almost uniform rate for many<br />
months. One commercial product contains selenium and cobalt, and in one experiment increased<br />
ceraloplasmin activity for at least 1 year. In one field study, the admin¬istration of two<br />
commercial soluble glass boluses containing copper and selenium, the selenium levels were<br />
increased from marginal to adequate, but adequate copper levels were not maintained.<br />
Copper oxide needles<br />
Copper oxide needles or wire particles (fragments of oxidized copper wire up to 8 mm in length<br />
and 0.5 mm in diameter) are used for oral dosing and one of the most effective and safest methods<br />
for the control of copper deficiency in ruminants. Its major advantages are prolonged effectiveness<br />
and low cost. A single treatment can be effective for an entire summer or winter season. The<br />
needles are retained in the forcstomachs and aboma-sum for up to 100 days or more and the<br />
copper is slowly released, absorbed, and stored in the liver. A dose of 0.1g/kg live weight (5g) in<br />
sheep is safe and does not induce copper toxicity in the susceptible North Ronaldsay breed. The<br />
response in liver copper concentrations is dose-dependent. In sheep given doses ranging from 2.5<br />
to 20 g per animal, the liver cop¬per concentrations will peak 10 weeks after administration and<br />
will thereafter decline in a linear fashion over the next 40 weeks. A single dose of 20g of copper<br />
oxide needles to hypocupremic suclder cows was sufficient to maintain adequate copper status for<br />
at least 5 months. The use of 20 g of copper oxide needles to young cattle weighing 190 kg<br />
effectively prevented growth retardation and severe hypocuprcrma, which occurred in an undosed<br />
control over a 70-day trial period. The currently recommended doses for beef cattle are 5 g for<br />
calves, 10 g for yearlings and 20 g for heavier or adult cattle, which will give protection for at<br />
least 6 months. A single oral dose of 20 g of copper oxide needles at the beginning of the grazing<br />
season is effective in increasing or maintaining stores of copper in the liver of grazing cows and<br />
calves consuming low-copper, high-molybdenum forage and high-sulfate water supplies. The use<br />
of 50 g of needles in adult cows (55 kg BW) sustained higher levels of plasma concentrations than<br />
the SC injection of copper glycinate, and 100, 200 or 300 g of needles given orally did not cause<br />
clinical effects. The administration of a single dose of 2 g cupric oxide needles orally to lambs<br />
between 3 and 5 weeks of age is an effective method for the prevention of induced hypocuprosis<br />
manifested as ill-thrift in lambs grazing pastures improved by liming and reseed-ing. The<br />
treatment maintained the lambs in norrnocupremia, provided adequate liver copper reserves,<br />
prevented clinical signs of hypocuprosis, and produced a liveweight gain advantage. The<br />
administration of the needles to ewes in the first half of pregnancy is also effective for the<br />
prevention of swayback in their lambs. The administration of cupric oxide needles to ewes at<br />
parturition is effective in preventing hypocupremia for up to 17 weeks in animals on pasture<br />
previously shown to cause a molybdenum-sulfur-induced copper deficiency. The treat-ment of the<br />
ewes at parturition also resulted in higher concentrations of cop- per in the milk in the initial<br />
weeks of lactation. However, this increase in milk copper will not be effective in preventing<br />
hypocupremia and hypocuprosis in the lambs, which can be treated with cupric oxide needles at 6<br />
weeks of age. Because some breeds of sheep may have a propen-sity to concentrate excess<br />
quantities of copper in the liver, it is important to adhere to the recommended dosage. Cupric<br />
oxide needles at a dose of 4 g per animal have also been used for the prevention of swayback in<br />
265
goats, and to maintain liver copper levels for up to 5 months in farmed red deer grazing on a<br />
marginally copper-deficient pasture.<br />
Copper oxide powder<br />
Copper oxide powder administered in the form of experimental, sustained-release rumen boluses<br />
significantly increased blood and liver copper concentrations in growing sheep, in out-wintered<br />
stickler cows during late pregnancy and early lactation, and m growing cattle at grass in the<br />
summer periods over periods of at least 170 and 123 days, respectively (33).<br />
Genetic selection<br />
It is now possible to manipulate trace element metabolism by genetic selection in farm animals.<br />
Within a period of 5 years, selection of sheep based on plasma concentration of copper resulted in<br />
two divergent sets of progeny, one with a high level of copper status, the other with a low level,<br />
which resulted in clinical manifestations of copper deficiency in the low level and protection in<br />
the high level.<br />
General guidelines<br />
Several rules of thumb are important and useful.<br />
•A dietary intake of copper equivalent to l0mg/kg DM will prevent the<br />
occurrence of primary copper deficiency in both sheep and cattle •Diets containing less than 5<br />
mg/kg DM will cause hypocuprosis<br />
•Diets with copper: molybdenum ratios of less than 5:1 are conducive to conditioned (secondary)<br />
hypocuprosis<br />
•The newborn calf is protected against neonatal hypocuprosis by donations from the dam, but<br />
newborn lambs assume the same copper status as the ewe •Cattle are more susceptible to copper<br />
deficiency than are sheep.<br />
REVIEWUTERATUE Gooneratne, S. R., Buckley, W. T. & Christensen, D. A. (1989) Review of<br />
copper<br />
deficiency and metabolism in ruminants. Can.J.Anim.Sci.,69,819-5. Smart, M. E., Cymbaluk, N. .<br />
f& Christensen,<br />
D. A. (1992) A review of copper status of cattle in Canada ami recommendations for<br />
supplementation. Can. Vet.J, 33, 163-170. Suttle, N. F. (1986) Problems in the diagnosis and<br />
anticipation of trace element deficiencies in grazing livestock. Vet.Rec, It9, 148-152.<br />
Suttle, N. F. (1986) Copper deficiency in ruminants, recent developments. Vet. Rec, 119, 519-522.<br />
Suttle, N. F. (1987) The nutritional requirement for copper in animals and man. In: Copper in<br />
Animals and Mem. Volume I. Eds HoweU,<br />
M. & Gawthorne, J. M. Boca Raton, FL:<br />
CRC Press, pp. 21-43. Suttle, N. F. (1991) The interactions between copper, molybdenum, and<br />
sulphur in ruminant nutrition. Ann. Rcir. Nutr., 1 /, 121-140.<br />
Suttle, N. F. (1994) Meeting the copper requirements of ruminants: In: Recent Advances in<br />
Animal Nutrition. Eds Garnsworthy, P. C. & Cole, D.J. A.<br />
Nottingham: Nottingham Univ. Press, pp. 173-187. Wikse, S. E., Herd, IX, Field, R. & Holland, P.<br />
(1992) Diagnosis of copper deficiency m cattle./ Am. Vet. Med. Assoc, 200, 1625-1629.<br />
REFERENCES<br />
(1)Suttle, N. F. (1992) Ann. Rev. Nutr., II, 121.<br />
(2)Thompson, K. G. el al. (1994) NZ Vei.J., 42, 137.<br />
(3)Gooneratne, S. R. & Christensen, D. A. (1989) Can. J. Anim. Sci., 69, 141.<br />
266
(4)Knight, D. A. et al. (1990) Equine Vet.J., 22, 426.<br />
(5)Smart, M. E. et al. (1992) Can. Vet.}., 33, 163.<br />
(6)Suttle, N. F. (1986) Vet. Rec. 119, 519.<br />
(7)WooliamsJ. A. et al. (1985) Anim. Prod., 41, 219.<br />
(8)WardJ. D. et al. (1995) /. Anim. Sci., 13, 571.<br />
(9)Gooneratne, S. R. et al. (1994) Can). Anim. Sci., 14, 315.<br />
(10)Gooneratne. S. R. et al. (1989) Can.}. Anim. Sci., 69, 819.<br />
(11)Graham, T. W. et al. (1994)J. Vet. Diagn. Invest., 6, 77.<br />
(12)SchonewilleJ. T. et al. (1995) Vet. Quart.. 11, 14.<br />
(13)Sas, B. (1989) Vet. Hum. Toxuol., 31. 29.<br />
(14)Suttle, N. F. (1987) In: Copper in Animals and Man Volume I. Eds HowellJ. M. & Gawthorne,<br />
J. M. Boca Raton, FL: CRC Press, pp. 21 43.<br />
(15)Bridges, C. H. & Moffitt, P. G. (1990) Am.]. Vet. Res., 51, 275.<br />
(16)Flurtig, M. et al. (1991) Proc. Amu Cow. Am. Assoc. Equine Pract., 36, 637.<br />
(17)Hurtig, M. ct al. (1993) Equine Vet.J., Suppl., 16, 66.<br />
(18)Hoyt, Z. K. et al. (1995)7. Equine. Vet. Sci., 15, 357.<br />
(19)Wildman, R. E. C. et al. (1996) Biol. Trace Element. Res., 55, 55.<br />
(20)Stabel.J. R. et al. (1993)/ Anim. Sci., 11, 1247.<br />
(21)Arthington.J. D. ct al. (1995) /. Anim. Sci., 13, 2079.<br />
(22)Fyffe.J.J. (1996) Aust. Vet.J., 13, 188.<br />
(23)BowlandJ. V. (1990) % News & Info., 11, 163.<br />
(24)Wikse, S. E. et al. (1992) /. Am. Vet. Med. Assoc, 200, 1625.<br />
(25)Vermunt, J. J. ik West, D. M. (1994) NZ Vet.J., 42, 194.<br />
(26)Clark, R. G. & Ellison, R. S. (1993) NZ Vet.J., 41, 98.<br />
(27)Suttle, N. F. (1993) Vet. Rec, 133, 123.<br />
(28)Mee.J. F. & McLaughlm, J. (1995) Vet. Rec, 136. 275.<br />
(29)Suttle, N. F. (1986) Vet. Rec, 119, 148.<br />
(30)Suttle, N. F. et al. (1996) Equine Vet.J..2H, 497.<br />
(31)White. C. F. et al. (1994) Ausl.J. Agr.Res., 45, 279.<br />
(32)Boila, R. J. et al. (1984) Can.}. Arum. Sci.,64. 365.<br />
(33)Parkins, J. J. et al. (1994) Br. Vet.J., 150,547.<br />
三、铁营养紊乱性疾病(Nutrtional Disorder of Iron)<br />
(一)铁缺乏症(Iron Deficiency)<br />
因饲料中缺乏铁,或因种种原因造成铁摄入不足或铁从体内丢失过多,引起动物贫血、<br />
易疲劳、活力下降的现象,称为铁缺乏症。主要发生于幼年动物。单纯依靠吮乳或食代乳品,<br />
其中铁含量不足时而发生。多见于仔猪,其次为犊牛、羔羊和幼年小狗。禽也可发生铁缺乏<br />
症。<br />
【病因】 原发性铁缺乏症,常发生于新生后不久的幼畜,如 3~6 周龄仔猪。完全关<br />
禁饲养,并依靠喂给牛乳和代乳品的犊牛、羔羊,乳中铁含量很少,不能满足快速生长幼畜<br />
对铁的需要。<br />
大量吸血性内、外寄生虫,如虱子、园线虫等侵袭,造成慢性失血,铁从体内、体表丢<br />
失;用高铜饲料喂猪,干扰了铁的吸收;用尿素或棉籽饼作为动物蛋白质来源,又未给它们<br />
补充铁,或完全关禁式集约饲养,饲料中铁含量不足,或干扰铁吸收的物质太多等,都可引<br />
267
起铁缺乏症。<br />
有人认为在生后头几周内死亡的仔猪,有 30%与缺铁有关。初生仔猪并无贫血现象,<br />
但因体内贮铁较少(一般 50mg),仔猪每增重 1kg,需 21mg 铁,每天从乳汁中能获得 1mg<br />
铁,大约要动用 6mg 贮铁。因此,只要 l~2 周,就可把贮铁耗尽。长得越快的猪,贮铁消<br />
耗越快。黑毛仔猪更易患缺铁性贫血,有些猪场仔猪贫血可达 90%,用水泥地面的圈舍饲<br />
养,仔猪获得铁的唯一来源是母乳,更易患铁缺乏症,造成大批仔猪死亡,生活能力下降,<br />
产生很大的经济损失。<br />
关禁饲养的犊牛、羔羊,唯一的铁的来源是乳和代乳品中的铁。有资料表明,犊牛,羔<br />
羊食物中铁含量低于 19mg/kg(干物质计),就可出现贫血。犊牛每天从乳中仅获得 2~4mg<br />
铁,4 个月龄内每天需铁约 50mg,如不注意在乳中加入可溶性铁强化,可出现贫血。<br />
产蛋率高的母鸡,有时也可发生贫血。每产一只蛋,要丢失 1mg 铁,一周内产 6 只蛋<br />
汁,必须从饲料中多摄入 6~7mg 铁。<br />
【病理】 一条 600kg 重的牛,体内含 36g 铁;500kg 重的马,体内约含 33g 铁;100kg<br />
重的猪,含 5g 铁;2kg 重的鸡,含铁 0.16g。幼年动物中,除了兔子以外,其它动物从母亲<br />
获得的贮铁都很少。体内有一半以上的铁,作为血红蛋白的成分之一。以狗为例,血红蛋白<br />
铁占 57%,肌红蛋白中铁占 7%,肝脏、脾脏贮铁各占 10%,肌肉中铁占 8%,骨骼中铁占<br />
5%,其它器官和组织仅占 2%。各种动物的血红蛋白中铁含量在 0.35%左右,所以每合成<br />
1g 血红蛋白,则需要 3.5mg 铁。此外铁还与许多酶活性有关,如细胞色素氧化酶;过氧化<br />
氢酶,在三羧循环中,有一半以上的酶中含有铁,当机体缺乏铁时,首先影响血红蛋白、肌<br />
红蛋白及多种酶的合成和功能。随着体内贮铁耗竭,最早出现的是血清铁浓度下降,血清铁<br />
饱和度减少,肝、脾、肾中血铁黄蛋白铁含量减少。接着即影响血红蛋白浓度下降,血色指<br />
数降低,动物品种不一,各种成分减少的程度也不同。猪除了血红蛋白浓度下降外,肌红蛋<br />
白含量减少,细胞色素 C 活性降低。狗则仅表现血红蛋白浓度降低,肌红蛋白,含铁酶活<br />
性变化不明显。鸡最早表现为血红蛋白减少,然后才有肌红蛋白、肝脏细胞色素 C 和琥珀<br />
酸脱氢酶活性的变化。而猪、犊牛及大鼠的过氧化氢酶活性均明显降低。当血红蛋白降低<br />
25%以下后,则意味着贫血。降低 50%~60%,将出现临床症状。如生长迟缓,可视黏膜淡<br />
染,易疲劳,易气喘,易受病原菌侵袭致病等。当突然奔跑和激烈运动时,可产生突然死亡。<br />
【临床表现】 幼畜缺铁的共同症状是贫血。可视黏膜微黄或淡白,懒动,易疲劳,稍<br />
事运动则喘息不止,易受感染,易死亡。最明显的症状有:<br />
贫血:常表现为低染性小细胞性贫血,并伴有成红细胞性骨髓增生。肝、脾、肾中几乎<br />
没有血铁黄蛋白。血清铁、血清铁蛋白浓度低于正常,血清铁结合力增加,铁饱和度降低。<br />
血脂浓度升高:缺铁的鸡、大鼠,其血清甘油三酯、脂质浓度升高,血清和组织中脂蛋<br />
白脂酶活性下降。<br />
肌红蛋白浓度下降:年青的小狗,小猪、鸡和大鼠,实验性铁缺乏时,可表现为肌红蛋<br />
白浓度下降,骨骼肌比心肌、膈肌更敏感。<br />
含铁酶活性下降:缺铁的仔猪、犊牛、大鼠体内含铁酶如过氧化氢酶、细胞色素 C 活性<br />
下降明显,肌肉中细胞色素 C 降至正常时的一半,过氧化氢酶活性下降幅度更大。<br />
生产实践中缺铁性贫血主要见于仔猪,其次是犊牛、羔羊。<br />
仔猪铁缺乏:仔猪贫血多发于后 3~6 周龄,3 周龄为发病高峰,特别是关禁饲养在全水<br />
泥地面、封闭式圈舍中。仔猪无法接触铁含量丰富的泥土,新鲜蔬菜。饲以高铜饲料的猪,<br />
年龄较大的猪,有时也可发生贫血。发病前仔猪,有的生长特别好,但也有生长缓慢的仔猪。<br />
采食量突然下降,拉稀,粪色无异常。生长进一步缓慢,严重时呼吸困难,昏睡。运动时心<br />
搏加剧,可视黏膜淡染,甚至苍白。白色小猪黏膜淡黄色,头部、前驱水肿,似乎较胖,但<br />
多数猪消瘦,大肠杆菌感染率高,很易诱发仔猪白痢。有的易受链球菌感染,发生心包炎。<br />
268
如能耐过 6~7 周龄,开始采食后,才逐渐恢复。初生仔猪血红蛋白浓度为 80g/L,但生后<br />
可低至 40~50g/L,这属生理性血红蛋白浓度下降,如低至 20~40g/L,红细胞数从正常时<br />
5×10 12 ~8×10 12 /L,降至 3×10 12 ~4×10 12 个/L,呈典型的低染性小细胞性贫血。<br />
剖检可见心肌松弛,心包液增多,肺水肿,胸膜腔充满清亮淡黄色液体,血液稀薄如红<br />
墨水样,不易凝固。<br />
犊牛、羔羊铁缺乏症:当大量吸血昆虫侵袭时,犊牛、羔羊可患缺铁性贫血。因铁丢失<br />
过多、铁补充不足,血红蛋白浓度下降、红细胞数减少,呈低染性小细胞性贫血。血清铁浓<br />
度从正常时 1.7mg/kg 降至 0.67mg/kg。<br />
鸡未见自然发生铁缺乏症的病例。实验性铁缺乏症亦表现为贫血,通常情况下,鸡饲料<br />
中含丰富的铁,但如用大量棉籽饼代替豆饼时,由于棉酚和铁作用,影响雏鸡对铁吸收。这<br />
时需补充铁。<br />
狗和猫铁缺乏症:多因体内慢性失血,如钩虫,或因消化道对铁吸收不足引起。单纯以<br />
吃奶为生的狗崽和猫崽,可出现生理性贫血。血球比容可降为初生时的 25%~30%。狗、猫<br />
缺铁性贫血表现为小细胞性、低染性贫血。细胞大小不均,骨髓中原正成细胞,嗜碱性正成<br />
细胞明显增多,多染性细胞减少,网织红细胞消失。<br />
【诊断】 本病有耐于测定血红蛋白、红细胞、血细胞压积(PVC)及用铁治疗和预防<br />
的效果来判定。但应注意与自家免疫性贫血相区别。后者属溶血性贫血,常有血红蛋白尿和<br />
黄疸,而且发病年龄更早。猪附红细胞体病,可发生于各种年龄猪,红细胞内可见到寄生原<br />
虫。<br />
造成贫血的原因很多,如缺乏铜、钴、VB12叶酸等应注意区别。<br />
【防治】 必须从补铁入手。给母畜补充铁,无论在妊娠期,还是分娩期以后,收效甚<br />
微。因为并不能增加新生仔猪体内铁贮备和乳中铁浓度。改善仔猪饲养管理,让仔猪有机会<br />
接触垫草、泥土或灰尘。即使仔猪每天仅食入几克泥土,也可有效地防止缺铁性贫血。每天<br />
给母猪供给几颗带泥的新鲜蔬菜,也有较好预防作用。口服或肌肉注射铁制剂。生后 2~4<br />
天补充一次,10~14 天再补充一次,用 1~2ml 葡聚糖铁(Iron dextran),含 100~200mg Fe,<br />
或山梨醇铁、柠檬酸复合物,葡萄糖酸铁等,剂量为 0.5~1.0g 元素铁,每周一次,或掺入含<br />
糖饮水中,亦能有效地防治仔猪缺铁性贫血。有些注射剂因有刺激作用,注射局部出现肿胀,<br />
坏死,固宜深部肌肉注射。<br />
硫酸亚铁 2.5g、氯化钴 2.5g、硫酸铜 1.0g,常水加至 500~1000ml,混合后用纱布过滤,<br />
涂在母猪乳头上,或混于饮水中或代乳料中,让仔猪自饮、自食,对大群猪场是有效的。<br />
每天给予 4ml1.8%的硫酸亚铁,或每天给予 300mg 正磷酸铁,连续 7 天口服,或于生<br />
后 12h,一次口服葡聚糖铁或乳糖铁,以后每周一次,每次 0.5~1.0g,可充分防止贫血。<br />
国产右旋糖酐铁于生后第 3 天,用 200mg Fe 作深部肌肉注射,不仅可防止贫血,而且<br />
可促进生长。<br />
犊牛所饮的乳中适当添加硫酸亚铁,或随群放牧的牛犊,多可获得较多的铁,可防止缺<br />
铁性贫血。<br />
葡聚糖铁或葡萄糖酸铁,供铁总量在 200mg可防止贫血。为防止亚临床缺铁,饲料中应<br />
含 240mg/kg铁。母猪于怀孕期间缺乏VE和硒时,注射大剂量铁有副作用。如呕吐、腹泻<br />
等甚至于注射铁后 1~2h,急性铁中毒死亡。剖检表现骨骼肌严重变性,这是因VE或硒缺乏<br />
时,肌纤维膜受损、造成许多生化成分改变,如细胞外液中钾浓度剧增,心跳骤停。2 日龄<br />
仔猪比 8 日龄仔猪对高铁制剂更敏感,可能因 2 日龄猪肾脏排铁功能不完善所致。这种现象<br />
在先天性缺硒的牛、羔羊、马驹有同样结果,应予以警惕。<br />
成年牛、马因吸血寄生虫感染造成贫血时,亦可用葡聚糖铁治疗,但不经济,而且有时<br />
可造成注射后迅速死亡。特别是马,可在注射后几分钟内毙命。最便宜的办法是每天用 2~4g<br />
269
硫酸亚铁口服,连续 2 周可取得明显效果。<br />
食物中补铁。仔猪尽可能提前开食,犊饲料中应含 25~30mg/kg 可溶性铁,否则食欲<br />
迅速下降。<br />
(二)有机铁化合物中毒(Poisioning by Organic Iron Compounds)<br />
新生仔猪在注射有机铁化合物后不久死亡,临床上主要表现为呕吐、腹泻和骨骼肌严重<br />
变性等特征,称为有机铁中毒。<br />
新生仔猪为了预防缺铁性贫血,常用葡聚糖铁等铁的有机化合物注射,但注射后l~2h<br />
引起急速死亡的现象,国外已有许多报道。尤其是因硒和VE缺乏的母猪所生的仔猪,注射<br />
有机铁后更易发病,有机铁化合物中含离子态铁越多,则毒性越大,因其易于吸收。当维生<br />
素E缺乏时,由于细胞膜结构损伤,细胞外液中钾离子浓度升高,可引起心肌舒张,并产生<br />
突然死亡。年龄小的猪,注射有机铁化合物(如 2 日龄)比年龄大的猪(8 日龄)更易中毒,<br />
可能与肾脏排泄功能不完善有关,或者与年龄较大猪体内铁、钙间的运动有关。因过多铁可<br />
引起钙的异位沉着,特别是在损伤的组织内沉着。此现象与注射铁剂的前 24h用VD3注射,<br />
引起的钙盐异位沉着的现象类似。也有人认为过多有机铁可能有封闭网状内皮系统,妨碍该<br />
系统对各种有毒物质的缓解作用有关,其说法尚无定论。<br />
有机铁对后肢肌肉还可产生非对称性损伤,对肌肉的组成成分没有影响,可能与两肢血<br />
液供应不完全一致有关。<br />
有机铁也可引起马属动物急性死亡,肌肉注射后几分钟内马急性死亡的现象已有报道<br />
(Lannek N,1972),这可能与马急性心力衰竭引起致死性休克有关。<br />
IRON DEFICIENCY<br />
Synopsis<br />
Etiology. Dietary deficiency of iron<br />
Epidemiology. Young animals on milk diet; most commonly nursing piglets which have not<br />
received supplemental iron. Housed nursing lambs. Occurs in veal calves fed milk with limited<br />
quantities of iron. Continued blood loss due to hemorrhage (lice, blood sucking helminths).<br />
Subclinical iron deficiency occurs in calves and foals of doubtful significance. May be more<br />
susceptible to infectious diseases.<br />
Signs. Pale white skin of well grown nursing piglets, dyspnea, pallor of mucosae, sudden death<br />
may occur. Stillbirths if sows iron deficient. Secondary infectious diseases.<br />
Clinical pathology. Subnormal levels of hemoglobin of serum iron, microcytic hypochromic<br />
anemia.<br />
Lesions. Pallor, thin watery blood, anasarca, dilated heart, enlarged liver.<br />
Diagnostic confirmation. Low serum hemoglobin and serum iron with microcytic hypochromic<br />
anemia. Response to iron therapy.<br />
Differential diagnosis. Other causes of anemia (p. 414).<br />
Treatment. Parenteral and oral iron salts.<br />
Control. Insure adequate iron intake. Parenteral iron dextran to nursing piglets and lambs.<br />
ETIOLOGY<br />
Iron deficiency is usually primary and most likely to occur in newborn animals whose sole source<br />
of iron is the milk of the dam, milk being a poor source of iron. Deposits of iron in the liver of the<br />
newborn are insufficient to maintain normal hemopoiesis for more than 2-3 weeks, and are<br />
particularly low in piglets.<br />
EPIDEMIOLOGY<br />
Iron-deficiency states are not common in farm animals except in the very young confined to a<br />
270
milk diet.<br />
Iron deficiency anemia occurs in nursing piglets for three reasons:<br />
1.They do not have access to soil, which is a main source of iron for young farm animals<br />
2.They grow rapidly and their absolute requirements for iron are high<br />
3.Milk is a poor source of iron.<br />
The administration of iron dextran to the piglets at a few days of age is preventive and is a<br />
routine health management strategy in modern swine production. If<br />
they do not receive supplemental iron dextran, clinical disease occurs usually when the piglets are<br />
3-6 weeks old. The losses that occur include those due to mortality, which may be high in<br />
untreated pigs and to failure to thrive. Under modern swine production systems piglets do not have<br />
access to sufficient dietary iron until they are weaned to a dry diet containing supplemental iron.<br />
Thus, the need for parenteral iron dextran at a few days of age.<br />
Iron deficiency anemia occurs in nursing lambs that are housed and do not have access to<br />
soil, do not consume much feed other than their dam's milk for the first 7-10 days of life, and grow<br />
at 0.4 kg per day (1). The parenteral administration of iron dextran at 24 hours of age prevents the<br />
anemia (1).<br />
Continued blood loss by hemorrhage in any animal may result in subclinical anemia and iron<br />
deficiency. Cattle heavily infested with sucking lice may develop serious and even fatal anemia.<br />
The chronic form is characterized by a non-regenerative anemia with subnormal levels of serum<br />
iron, and treatment with iron is necessary for an optimal response. Horses carrying heavy burdens<br />
of bloodsucking strongylid worms often have subnormal hemoglobin levels and respond to<br />
treatment with iron. On occasions veal calves, and possibly young lambs and kids, may also suffer<br />
271
from an iron deficiency.<br />
Good quality veal is traditionally pale in color and is produced by feeding calves an all-liquid<br />
milk replacer diet with a low concentration of available iron (2, 3). The pallor of veal is due<br />
largely to low concentrations of myoglobin and other iron-containing compounds in muscle. Milk<br />
replacers containing only 10 mg iron/kg DM results in marked anemia and reduced growth<br />
performance (3). Feeding milk replacers with 50 mg iron/kg DM is considered, physiologically,<br />
the optimum amount of iron for veal calves but may be too high for acceptable carcass yield in<br />
some countries (3). A severe iron defi¬ciency with reduced growth rate in veal calves may be<br />
associated with a higher incidence of infectious disease because of an unpaired immune system (4).<br />
The objective in veal calf management is to walk the narrow line between the maximum<br />
production of white meat and a degree of anemia insufficient to interfere with maximum<br />
production.<br />
Subclinical iron-deficiency anemia also occurs in newborn calves and kids but there is debate<br />
as to wheteher the condition has practical significance. In newborn calves affected with a<br />
nor-mochromic, normocytic, and poikilo-cytic anemia the levels of serum iron are not<br />
significantly different from normal calves (5). It has been proposed that severe poikilocytosis in<br />
calves is associated with abnormalities of hemoglobin com¬position and protein 4.2 in the<br />
erythro-cyte membrane, and iron deficiency is the cause of moderate poikilocytosis in calves (6).<br />
Clinicopathological anemia, without clinical signs, is most likely to occur when calves are born<br />
with low hemoglobin and hematocrit levels, a relatively common occurrence in twins. It is<br />
possible that suboptimal growth may occur during the period of physiological anemia in early<br />
postnatal life. There is some evidence for this in calves in which hemoglobin levels of 11 g/dL at<br />
birth fall to about 8 g/dL between the 30th and 70th days and only begin to rise when the calves<br />
start to eat roughage. The daily intake of iron from milk is 2-4mg in calves, and their daily<br />
requirement during the first 4 months of life is of the order of 50 mg, so that iron supplementation<br />
of the diet is advisable if the calves are fed entirely on milk. Even when hay and gram are fed to<br />
calves and lambs in addition to milk, there is a marked growth response to the administration of<br />
iron-dextran preparations at the rate of 5.5 mg/kg BW. The dietary iron requirement for<br />
fast-growing lambs is between 40 and 70 mg/kg BW, and growth rate is suboptimal on diets of<br />
less than 25 mg/kg BW.<br />
Low serum iron concentration and low serum ferritin have been observed in hospitalized<br />
young foals (7). Hemoglobin concentrations and packed cell volume decrease in foals from values<br />
at birth, which are similar to those for adult horses, to mean values during the first weeks and<br />
months of life below those reported in adults. Serum iron concentration, total iron-binding<br />
capacity, and packed cell volume decreased during the foal's first 24 hours of life (8). Based on the<br />
studies of foals from birth to 1 year of age, the potential for iron deficiency developing under 5<br />
weeks of age is possible because 65% of foals had minimum ferritin concentrations =45 ng/mL,<br />
and 81% of foals had these minimum values recorded between 2 and 4 weeks.<br />
Competition horses are frequently given iron supplementation to treat anemia and to<br />
improve performance despite the fact that neither application has any scientific basis (7). In<br />
contrast, iron overload and toxicity have occurred in competition horses (9, 10). Some studies<br />
have shown high total plasma iron in British 3-day event team horses prior to transport (77µM)<br />
compared to normal levels of 24 µM. Immediately after travelling for 3 days on the road, the<br />
plasma levels had declined to 29 µM (11). The iron-binding antioxidant activity, an indicator of<br />
272
transfernn saturation, had also declined, suggesting greater saturation of available transfernn in the<br />
plasma or a decreased capacity to sequester iron. The saturation of mechanisms to sequester iron,<br />
such as may occur with excessive supplementation, may predispose the horses to iron-catalyzed<br />
oxidant injury (11). The total iron intake exceeded the normal recommendation of between 550<br />
and 600 mg/day. Anemia (or a low packed cell volume) is not synonymous with iron deficiency<br />
but is frequently associated with disease processes. Poor performance in an iron-deficient animal<br />
is more likely due to a reduction in the activity of metabolically active iron-containing enzymes<br />
rather than a reduction in oxygen transport. In addition, iron deficiency is unlikely to occur in<br />
healthy horses.<br />
Calcium carbonate added to the diet of weaned and finishing pigs may cause a conditioned<br />
iron deficiency and a moderate anemia but this effect is not apparent in mature pigs. Manganese<br />
may exert a similar antagonistic effect.<br />
PATHOGENESIS<br />
More than half the iron in the animal body is found as a constituent of hemoglobin. A relatively<br />
small amount is found in myoglobin and in certain enzymes which play a part in oxygen<br />
utilization.<br />
Piglets at birth have hemoglobin levels of about 90-110g/L. A physiological fall to 40-50 g/dL<br />
occurs in all pigs, the lowest levels occurring at about the 8th--10th day of life. Levels of iron in<br />
the liver at birtli are unusually low in this species and cannot be increased appreciably by<br />
supplementary feeding of the sow during pregnancy. The IM injection of iron-dextran preparations<br />
to sows during late pregnancy docs elevate the hemoglobin levels of the piglets during the first<br />
few weeks of life but not sufficiently to prevent anemia in them. Piglets with access to iron show a<br />
gradual return to normal hemoglobin levels starting at about the 10th day of life, but in pigs denied<br />
this access the hemoglobin levels continue to fall.<br />
One of the important factors in the high incidence of anemia in piglets is the rapidity with<br />
which they grow in early postnatal life. Piglets normally reach four to five times their birth weight<br />
at the end of 3 weeks, and eight times their birth weight at the end of 8 weeks. The daily<br />
requirement of iron during the first few weeks of life is of the order of 15 mg. The average intake<br />
in the milk from the sow is about 1 mg/day and the concentration in sow's milk cannot be elevated<br />
273
y feeding additional iron during pregnancy or lactation. Apart from the specific effect on<br />
hemoglobin levels, iron-deficient piglets consume less creep feed, and after the first 3 weeks of<br />
life make considerably slower weight gains than supplemented piglets. Although specific<br />
pathogen-free pigs show a less marked response to the administration of iron than pigs reared in<br />
the normal manner, it is obvious that they need supplementary iron to prevent the development of<br />
anemia. Iron-deficient piglets appear to be more susceptible to diarrhea at about 2 weeks of age<br />
than are piglets that have received iron. A marked impairment of gastric secretion of acid and<br />
chloride and atrophic gastritis occurs in iron-deprived piglets. Villous atrophy of the small<br />
intestine and changes in the gastrointestinal flora also occur in iron-deficient piglets which may<br />
contribute to the increased susceptibility to diarrhea.<br />
Severe iron deficiency in veal calves is characterized by impaired growth and reduced feed<br />
intake and utilization. The growth rate is reduced only when hemoglobin concentrations fall below<br />
70g/L (12). The reduced growth rate may be due to reduction in the half-life of growth hormone.<br />
CLINICAL FINDINGS<br />
The highest incidence of iron deficiency anemia in piglets occurs at about 3 weeks of age, but it<br />
can occur up to 10 weeks of age.<br />
Affected pigs may be well grown and in good condition, but the growth rate of anemic pigs is<br />
significantly lower than that of normal pigs and feed intake is reduced. A mild diarrhea may occur<br />
but the feces are usually normal in color. Dyspnea, lethargy, and a marked increase in amplitude<br />
of the apex beat of the heart can be felt after exercise. The skin and mucosae are pale and may<br />
appear yellow in white pigs. Edema of the head and forequarters, giving the animal a fat,<br />
puffed-up appearance may be present. A lean, white hairy look is probably more common. Death<br />
usually occurs suddenly, or affected animals may survive in a thin, unthrifty condition. A high<br />
incidence of infectious diseases, especially enteric infection with Escherichia coli, is associated<br />
with the anemia, and streptococcal pericarditis is a well-recognized complication. Under<br />
experimental conditions, similar signs occur in calves and there is, in addition, an apparent<br />
atrophy of the lingual papillae. A high incidence of stillbirths is recorded in the litters of sows<br />
suffering from iron-deficiency anemia.<br />
CLINICAL PATHOLOGY<br />
In normal piglets there is a postnatal fall of hemoglobin levels to about 8g/L and sometimes to as<br />
low as 4-5g/L during the first 10 days of life. In iron-deficient pigs there is a secondary fall to<br />
20-40g/L during the 3rd week. The hemoglobin level at which clinical signs appear in pigs is<br />
about 40g/L (13). Erythrocyte counts also fall from a normal of 5-8 × 10 12 /L down to 3-4 ×10 12 /L<br />
and may be a better index of iron status than hemoglobin levels. Iron-deficiency anemia in piglets<br />
is a microcytic hypochromic anemia. In chronic blood loss anemia in cattle infested with sucking<br />
lice, there is a non-regenerative anemia and a decrease in serum iron levels. Serum levels of iron<br />
considered to be normal in sheep and cattle are 100-200 µg/dL (17.9-35.8 (µmol/L). In newborn<br />
calves, the levels are 170 µg/dL (30.4µmol/L) at birth and 67µg/dL (12.0µmol/L) at 50 days of age.<br />
Serum ferntin concentration is an index for monitoring prelatent iron deficiency of calves (14).<br />
The borderline of iron-deficiency anemia of veal calves at 16-20 weeks of age has been defined<br />
as a hemoglobin concentration of 9g/L and a saturation of total iron binding capacity of 10% (15).<br />
NECROPSY FINDINGS<br />
The carcass is characterized by pallor, watery blood, and moderate anasarca. The heart is always<br />
dilated, sometimes extremely so. The cardiac dimensions in severely anemic neonatal pigs<br />
274
indicate that dilatation and hypertrophy occur consistently. The liver in all cases is enlarged, and<br />
has a mottled tan-yellow appearance. Histological examination of the bone marrow reveals<br />
maturation asynchrony of the erythroid line and a lack of hemosiderin stores. Other microscopic<br />
changes described include periacinar hepatocellular changes typical of hypoxia and decreased<br />
numbers of parietal cells in the gastric mucosa.<br />
Samples for confirmation of diagnosis<br />
•Toxicology - 50 g liver (ASSAY (Fe))(Note that serum ferritin from surviving littermates is a<br />
better indicator ofiron status)<br />
•Histology - liver, heart, bone marrow,stomach (LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
Confirmation of the diagnosis will depend upon hemoglobin determinations and curative and<br />
preventive trials with administered iron. The possibility that anemia in piglets may be caused by<br />
copper deficiency should not be overlooked especially if the response to administered iron is poor.<br />
Isoimmunization hemolytic anemia can be differentiated by the presence of jaundice and<br />
hemoglobinuria, and the disease occurs in much younger pigs. Eperythrozoonosis occurs in pigs<br />
of all ages and the protozoan parasites can be detected in the erythrocytes.<br />
TREATMENT<br />
The recommendations for the prevention of the disease are set out below and can be followed<br />
when treating clinically affected animals. Horses with poor racing performance often have<br />
suboptimal blood levels of hemoglobin and a blood loss anemia due to parasitism, and respond<br />
well to treatment with iron. Treatment is usually parentcral and consists of organic iron<br />
preparations such as iron-dextran, iron-sorbitol-citric acid complex, iron saccharate or gluconate.<br />
These must be given exactly as prescribed by the manufacturer as some are quite irritant, causing<br />
large sloughs when injected IM. The dose rate is 0.5-1 g elemental iron in one injection per week.<br />
When given IV, or even IM, some horses show idiosyncratic reactions and literally drop dead.<br />
Vitamin B12 (cyanocobalamin) is often used in the same injection at a dose rate of 5000 µg<br />
275
per week in a single dose. Other additives, especially folic acid and choline, are also used but with<br />
little justification. Oral treatment with iron sulfate or gluconate at a dose rate of 2-4 g daily for 2<br />
weeks is as effective and much cheaper, but lacks the style of the parenteral injection. It has the<br />
disadvantage of being unpalatable and is best dispensed in liquid form to be mixed with molasses<br />
and poured onto dry feed.<br />
CONTROL<br />
Preventive measures must be directed at the neonatal piglets because treatment of the sows before<br />
or after farrowing is generally ineffective, although some results are obtained if the iron<br />
preparations are fed at least 2 weeks before farrowing. Ferric choline citrate appears to have some<br />
special merit in this field. Allowing the nursing piglets access to pasture or dirt yards, or<br />
periodically placing sods in indoor pens, offer adequate protection. Where indoor housing on<br />
impervious floors is necessary, iron should be provided at the rate of 15 mg/day until weaning<br />
either by oral dosing with iron salts of a commercial grade or by the IM injection of organic iron<br />
preparations. These methods are satisfactory, but the results are not usually as good as when<br />
piglets are raised outdoors. However, indoor housing is practiced in many areas to avoid exposure<br />
to parasitic infestation and some bacterial diseases, especially erysipelas. If sods are put into pens<br />
care must be taken to insure that these diseases are not introduced.<br />
Dietary supplementation<br />
Sows<br />
Feeding sows a diet supplemented with 2000 mg iron/kg DM of diet will satisfactorily prevent<br />
iron-deficiency anemia in the piglets. The piglets will ingest about 20g of sows feces per day,<br />
which will contain sufficient iron and obviate the need for IM injection of iron-dextran. The<br />
piglets grow and thrive as well as those receiving the iron-dextran.<br />
Veal calves<br />
Milk replacers for veal calves may contain up to 40 mg/kg DM of iron for the first 2 months, but<br />
commonly only 10-15 mg/kg DM for the finishing period. The best indicator of the onset of<br />
anemia in calves on vealer diets is loss of appetite, which is a more sensitive indicator than<br />
biochemical measurement.<br />
Heifer calf herd replacements<br />
The National Research Council recommends that milk replacers fed to herd replacements or dairy<br />
beef contain 100 mg/kg of DM, with an upper limit of 1000 mg/kg DM (13). The preruminant calf<br />
can tolerate between 2000 and 5000 ppm DM iron in milk replacer (13).<br />
Oral dosing<br />
Daily dosing with 4 mL of 1.8% solution of ferrous sulfate is adequate. Iron pyrophosphatc may<br />
also be used (300 mg/day for 7 days). To overcome the necessity for daily dosing, several other<br />
methods of administering iron have been recommended. A single oral treatment with iron-dextran<br />
or iron-galactan has been recommended, provided an excellent creep feed is available, but the<br />
method seems unnecessarily expensive. With this oral treatment it is essential that the iron be<br />
given within 12 hours of birth because absorption has to occur through the perforate neonatal<br />
276
intestinal mucosa; later administration is not followed by absorption. Reduced iron (British<br />
Veterinary Codex) can be administered in large doses because it does not cause irritation of the<br />
alimentary mucosa. A single dose of 0.5-1g once weekly is sufficient to prevent anemia.<br />
Alternatively, the painting of a solution of ferrous sulfate on the sow's udder has been<br />
recommended (450g ferrous sulfate, 75g copper sulfate, 450g sugar, 2L water - applied daily) but<br />
has the disadvantage of being sticky and of accumulating litter. Pigs raised on steel gratings can<br />
derive enough iron from them to avoid the need for other supplementation. Excessive oral dosing<br />
with soluble iron salts may cause enteritis, diarrhea, and some deaths in pigs. High intakes of<br />
ferric hydroxide cause diarrhea, loss of weight, and low milk production in cattle. The presence of<br />
diarrhea in a herd prevents absorption of orally administered iron, and treatment by injection is<br />
recommended in this circumstance.<br />
Intramuscular injection of iron preparations<br />
Suitable preparations must be used and are usually injected IM in piglets on one-occasion only,<br />
between the 3rd and 7th day of life. Iron-extran, fumarate, and glutamate are most commonly used.<br />
A dose of 200 mg of a rapidly absorbed and readily utihzablc form of iron within the first few<br />
days of life will result in greater body weights at 4 weeks of age than piglets given only 100 mg<br />
(16). Multiple injections give better hemoglobin levels but have not been shown to improve<br />
weight gain and, thus, a second injection at 2-3 weeks of age may not be economical. A total dose<br />
of 200 mg is usually recommended as being required to avoid clinically manifest iron-deficiency<br />
anemia, but in order to avoid any chance of a subclinical deficiency the feed should contain<br />
additional iron at the level of 240 mg/kg. A new preparation (Heptomcr) contains 200mg/mL of<br />
iron, permitting a full dose in one injection. Contrasting information is that one injection of 100<br />
mg of iron is adequate for baby pigs. Acute poisoning and rapid death occurs in piglets given<br />
iron-dextran compounds parenterally if the piglets were born from sows which were deficient in<br />
vitamin E and selenium during gestation. This is discussed under iron-dextran poisoning. In<br />
normal piglets the iron-dextran com¬pounds are safe and are usually not toxic even on repeated<br />
injection. These preparations are ideal for treatment because of the rapid response they elicit and<br />
the absence of permanent discoloration of tissues after their use if given during the first month of<br />
life. A combination of sodium selenite and iron-dextran has been given to piglets at 3 days of age<br />
and is superior to treatment with iron alone when the piglets are deficient in selenium.<br />
Iron deficiency anemia in housed lambs is preventable by the IM injection of 300 mg iron<br />
dextran at 24 hours of age (1). At 12 and 24 days after treatment, the liematological values in the<br />
treated group were significantly different than the unsupplemented group, and at weaning the<br />
treated lambs were 1.0 kg heavier than untreated lambs (1).<br />
Comparable doses of parenteral iron-dextran compounds have been used for the treatment of<br />
iron-deficiency or iron-loss anemias in other species, but accurate doses have not been established<br />
and the use of these preparations in cattle and horses is expensive. In addition, iron-dextran<br />
preparations given IM to horses may cause death within a few minutes after administration. The<br />
most inexpensive method of supplying iron is to use ferrous sulfate orally at a dose of 2-4 g daily<br />
for 2 weeks to adult cattle and horses with iron-deficiency anemia.<br />
Iron injection of beef calves in the first week alter birth will result in an increase in packed cell<br />
volume (PVC), hemoglobin (Hb), mean corpuscular volume (MCV), and mean corpuscular<br />
hemoglobin (MCH) which persists for 12 weeks. However, weight gains during the first 18 weeks<br />
of life were not affected.<br />
277
REFERENCES<br />
(1)Green, L. E. et al. (1997) Vet. Rec, 140,219.<br />
(2)Limit, F. & BlumJ. W. (1994)J. Vet.Med, A. 41, 237.<br />
(3)Limit, F. & Blum.J. W. (1994)/ Vet.Med., A. 41, 333.<br />
(4)Gygax, M. ct al. (1993) /. Vet. Med. A.,40. 345.<br />
(5)McGillivray, S. R. el al. (1985) Can.].Comp. Med.. 49, 286.<br />
(6)Okabe.J. et al. (1996) J. Vet. Med. Sci., 58,629.<br />
(7)Smith, J. E. et al. (1986)/ Am. Vet. Med.Assoc, 188, 285.<br />
(8)Harvey, J. W. et al. (1987) Am.). Vet.Res., 48, 1348.<br />
(9)Edens, 1. M. et al. (1993) Equine Vet.J..25, 81<br />
(10)LavoieJ. P. & Teuscher, E. (1993) EquineVet. J.. 25, 552.<br />
(11)Mills, V. C. & Marlin, D.J. (1996) Vet.Ret., 139. 215.<br />
(12)Ceppi, A. et al. (1994) Ann. Nutr. Metal,.,38, 281.<br />
(13)Jenkins, K.J. & Hidiroglou, M. (1988) J.Dairy Sci., 70, 2349.<br />
(14)Mivata, Y. et al. (1984) J. Dairy Set. 61,1256.<br />
(15)Wekhnun, D.DeB, et al. (1988) Vet.Ret.. 123, 505.<br />
(16)Daykm, M. M. et al. (1982) Vet. Rec, 110. 535.<br />
四、锌营养紊乱性疾病(Nutritional Disorder of Zinc)<br />
(一)锌缺乏症(Zinc Deficiency)<br />
因地区性缺锌,饲料中锌含量不足,或其它因子干扰了锌的吸收,引起一种非炎性、非<br />
热性皮肤及其衍生物的疾病。临床表现为皮肤皲裂、皮屑增多、蹄壳变形、开裂、甚至磨穿、<br />
生长缓慢、骨骼发育异常和繁殖机能下降等特征。<br />
锌缺乏症可发生于各种动物。尤其是猪、禽、犊牛、羊也可发生。有些皮毛动物因缺锌<br />
产生掉毛、消瘦而影响自身价值。<br />
【病因】 锌缺乏症可因地区性缺锌引起。我国大多数省份属贫锌或缺锌,例如北京、<br />
河北、湖南、江西、江苏、新疆、四川等有 30%~50%的土壤属缺锌土壤。我国土壤中含锌<br />
在 10~300mg/kg,南方土壤锌较高于北方,由石灰岩风化的土壤、盐碱土及用大量石灰改<br />
造的土壤中锌含量低,或不易被植物吸收。据报道我国每两个儿童中有一个是缺锌的,在上<br />
述省份都有不同程度的动物锌缺乏症报道。<br />
锌是植物的必需微量元素。参予植物的激素、蛋白质、叶绿素的合成。各种植物中锌<br />
的含量不一样,一般野生牧草中锌含量较高,而玉米、高粱、稻谷、稻草、麦秸、苜蓿、三<br />
叶草、苏丹草、水果、蔬菜(特别是无叶菜)、块茎类饲料等锌含虽比较低,一般不能满足<br />
动物需要。而牡蛎(Zn,1000mg/kg)等海洋生物、鱼粉、骨粉、麸皮、糠等饲料含锌较<br />
多。动物对锌的需要量至少为 40mg/kg,如遇到饲料中 Ca、P、植酸等干扰因素,其需要<br />
量增多。一般以 6~80mg/kg 为宜。动物性食物中锌容易吸收利用,生物学效应高,植物锌<br />
与植酸结合在一起,不利于吸收,生物效应低,例如黄豆粉中锌可吸收率较低。<br />
饲料中钙、磷太多,其次,铜、铁、锰、及镉、钼等二价元素过多,可干扰锌的吸收。<br />
我国有许多种畜场,特别是种猪场为防止缺钙、防止骨软症,添加了过量的南京石粉,常引<br />
起动物皮肤皲裂、增厚、皮屑增多,蹄壳变形、磨穿等现象。现在各种添加剂。预混药品中,<br />
大多以石粉为填充料或载体,增加了动物锌缺乏症的发生。二价元素,外层电子容易散落,<br />
成为带正电荷的阳离子,它们在体内可形成各种化合物、复合物,由于其外层结构的相似性,<br />
互相间可置换,因而某一种元素过多,可干扰另一种元素的吸收,饲料中 Ca:Zn=(100~150):1<br />
为宜,如饲料中 Ca 达 0.5%~1.5%,锌仅 34~44mg/kg,猪很易产生锌缺乏症。<br />
278
饲料中必需脂肪酸缺乏。当饲料中钙太多,可干扰脂肪的利用。快速生长的猪,可导致<br />
必需脂肪酸相对缺乏,补充豆油和血粉可缓解皮肤角化症。因血粉、组氨酸含量较高,豆油<br />
中必需脂肪酸含量较高。<br />
消化机能障碍,慢性拉稀,可影响由胰腺分泌的“锌结合因子”(Zinc binding factors)<br />
在肠腔内停留,而致锌摄入不足。<br />
遗传因素:伏里森(Friensian)牛,丹麦黑斑牛容易患锌缺乏症。于 4~8 周龄牛,皮肤增<br />
厚,皮屑增多。这是常染色体隐性遗传疾病,足因小肠上皮吸取和浓集锌的机能缺陷,锌吸<br />
收减少,引起锌缺乏。<br />
【病理】 锌是动物乃至一切生物最重要的生命元素,因它参予合成、激活体内 200<br />
种以上的酶的活性。锌有“生命的火花”之称。缺锌首先影响如 DNA 聚合酶、碱性磷酸酶、<br />
碳酸酐酶,乳酸脱氢酶等重要的酶活性,缺锌则可影响骨骼生长,机体发育,毛囊角化等一<br />
系列重要生命活动。<br />
锌是味觉素(gustin)的构成成分,每个味觉素内含 2 个锌原子。缺锌则可使食欲下降,<br />
采食减少,锌参予激素合成,缺锌大鼠血中生长素含量减少。性激素浓度下降。<br />
锌在睾丸、精液、前列腺、眼组织中含量特别高。锌可直接影响精子生成、成活、发育<br />
及VA作用的发挥。缺锌时可引起雄性动物生殖能力下降,和顽固的夜盲症。补充VA不能治<br />
疗,补充锌则可很快治愈。缺锌还可使母畜卵巢发育停滞,子宫上皮发育障碍。也可影响母<br />
畜繁殖机能。 、<br />
锌还可促进肉芽生长,促进创伤愈合。我国很早就采用炉甘石治疗局部创伤,使用硫酸<br />
锌软膏敷伤口,加速伤口愈合。<br />
【临床表现】 锌缺乏症以慢性、非炎性皮炎为特征。该病以无热候,皮肤增厚、皮屑<br />
增多、掉毛、擦痒为特征。缺锌动物食欲减少,生长缓慢,睾丸萎缩,精子发育成活受阻。<br />
骨骼发育障碍,骨短、粗,长骨弯曲,关节僵硬等共同症状。<br />
猪缺锌:猪很易引起皮肤角化现象。特别是生长快速,给饲料中添加促生长素的那些猪。<br />
断乳后 7~10 周龄最易发生,用干粉料饲喂的猪比用湿粉饲喂更易发生。病猪体增重减少,<br />
饲料报酬下降,皮肤上开始出现红斑,两腿内侧及腹部尤为明显。红斑逐渐转为丘疹样突起,<br />
颜色变暗黑,随之很快增厚,于四肢、耳、尾等部位,基本对称分布。疤块渐转为疤裂和皲<br />
裂。甚至增厚达 5~7mm,容易从皮肤上剥掉,疤块易碎,形成薄片和鳞屑状。除裂隙处有<br />
粘稠分泌物外,蹄壳变薄、甚至磨穿,在行走过程中留下血印。<br />
犊牛:严重缺锌病牛,有皮肤角质化生和掉毛现象,受影响体表可达 40%,在嘴圈、阴<br />
户、肛门、尾端、耳廓、后腿的背侧,膝、腹部、颈部最明显。多数动物体况下降,用嘴啃<br />
皮肤,有痒感,皮肤逐渐增厚,继有皮屑,生长停滞,用锌治疗,1 周内明显好转,3 周内<br />
康复。实验性锌缺乏动物生长缓慢,运步僵硬,蹄冠、关节、肘部、跗关节及腕部肿胀,跗<br />
关节软肿,患处掉毛,牙周出血,牙龈溃疡。<br />
绵羊:自然病例表现掉毛,皮肤增厚,皱裂,羔羊生长缓慢。流涎,跗关节肿胀,眼、<br />
蹄冠皮肤肿胀、皱裂。公羊羔睾丸萎缩,精子生成完全停止,当饲料中锌达 32.4mg/kg,<br />
可恢复精子生成。母羊缺锌时,繁殖力下降。<br />
山羊:实验性缺锌引起生长缓慢,食物摄入减少,睾丸萎缩,被毛粗乱,脱落,在后躯、<br />
阴囊、头、颈出现皮肤角质化生。四肢下部出现裂隙、渗出。<br />
禽缺锌:鸡、火鸡最易缺锌,野鸡、鹌鹑亦可发生。表现生长停滞,生毛泡变性,羽囊<br />
角化变性,羽毛稀疏,脚爪软弱,关节肿胀,皮炎,皮肤鳞屑生成。仅以植物性饲料饲喂,<br />
可发生原发性缺锌,而加以大量钙、磷,可产生继发性缺锌。缺锌时,皮肤角化,表皮增厚,<br />
以翅、腿、趾部为明显。长骨粗短,跗关节肿大,产蛋少,蛋壳薄,易碎,孵化率下降,胚<br />
胎畸形。主要表现躯干和肢体发育不全,有的脊柱弯曲缩短,肋骨发育不全或易产生胚胎死<br />
279
亡。<br />
野生动物、皮毛动物缺锌:有流涎,鼻、胸腹、颈部脱毛。先天性缺陷时,皮肤角化,<br />
皮屑增多,皮张质量下降。犬、猫可有生长缓慢,消瘦、呕吐、结膜炎、角膜炎。腹部、肢<br />
端发炎。灵长类食欲下降,舌背面角化不全,角膜炎并伴有脱毛。<br />
血清碱性磷酸酶活性下降至正常时的一半。血清锌浓度下降,至 0.3~0.4mg/L,但血<br />
清锌易受应激因素影响,有人提出测定血浆金属硫蛋白中锌更有意义。<br />
【诊断】 本病根据特征性临床症状,如皮屑增多,掉毛、皮肤开裂,经久不愈,骨短<br />
粗等而作初步诊断。补锌后经 1~3 周,临床异常迅速好转。<br />
饲料中钙、磷、锌含量测定,钙、锌比率的测定,可有助于诊断。但应防止滞后效应,<br />
产生临床缺锌症状的饲料,目前可能已不再饲喂,应具体分析所测数据。<br />
诊断本病时应与螨病、湿疹、锰缺乏、VA缺乏、烟酸、泛酸缺乏等相区别。<br />
【防治】 一旦出现疾病,应迅速调正饲料锌的含量。如加入 0.02%的碳酸锌(≈100mg<br />
/kg 锌),肌肉注射液剂量按 2~4mg/kg 体重,连续 10 天,补锌后食欲迅速恢复,3~5 周<br />
内皮肤症状消失。<br />
应保证日粮中含有足够的锌。使 Ca:Zn=100:1,各种动物对锌的需要量一般在 35~45mg<br />
/kg,但因饲料中干扰因素影响,常在此基础上再增加 50%的量可防止锌缺乏症。如增加<br />
一倍量还可提高机体抵抗力,体增重加快。<br />
Lamond提出把锌粉与注射用油混合后,绵羊一次注射 300mg 锌,牛 600mg 锌的油剂,<br />
1~2 个月内可维持血锌浓度正常。<br />
地区性缺锌时,可施用锌肥。每公顷施 7.5~22.5kg 硫酸锌,可拌在有机肥内施用,国外<br />
施用量更大。此法对防治植物缺锌有效,但代价大。现在已有用锌和铁混在一起,制成锌铁<br />
丸,或把锌掺入可溶性玻璃内,投放入胃一次可维持 6~8 周,缺点是容易随粪外排,失去补<br />
锌作用。<br />
(二)锌中毒(Zinc Poisoning)<br />
锌相对是无毒的。许多动物能耐受含 1000~2000mg/kg 的锌日粮,对生长、发育、繁<br />
殖没有影响。火鸡甚至可耐受 4000mg/kg 锌的日粮。但如饲料中锌过多,亦可产生锌中毒。<br />
如母鸡强制换羽时,可用含 2.5%的氧化锌(含 Zn≈7850mg/kg)饲喂,可使产蛋停止,<br />
换羽,甚至引起个别鸡死亡。但改为正常饲料后 18~22 天,又重新产蛋,56 天后半数以上<br />
开始产蛋。鸭喂给含 3000~12000mg/kg Zn 的日粮,可出现贫血、跛行,体重下降,并引<br />
起死亡,甚至缺硒引起渗出性素质,因 Zn 可干扰 Se 吸收和利用。<br />
锌可干扰铁、铜的吸收,引起贫血。<br />
牛的饮水中含 6~8mg/L Zn,可引起牛便秘。饲料中含 0.1%的锌可引起猪的关节炎。<br />
在矿山、工厂附近,因粉尘关系,如每公斤体重摄入 50~100mg 锌,可引起羊严重的真胃、<br />
胰腺损伤,羊死亡。镀锌水管,油漆中含锌较多,幼畜啃咬,舔食剥落的油漆。可引起中毒。<br />
猪因饲喂乳品厂的油乳浆(butter-milk),经长的管道流入猪舍,当余奶变酸,与管内锌形成<br />
乳酸锌。可引起慢性中毒。加上饲以高锌饲料,可促使锌中毒,因而引起食欲下降,关节炎,<br />
毛细血管内溶血,胃肠炎等。中毒动物可于 3 周内死亡。猪中毒的另一个原因是用鸡强制换<br />
羽的饲料来喂猪,引起关节炎、胃肠炎症为主的疾病。<br />
只要调正饲料中锌的含量,动物可很快恢复。如用管道输送液状饲料的集约化猪场,<br />
应经常用清水冲洗管道,防止管壁腐蚀。猪的锌中毒用VK止血,配合对症治疗,如葡萄糖<br />
静注,VD皮下注射,可迅速康复。<br />
ZINC DEFICIENCY (PARAKERATOSIS)<br />
Synopsis<br />
Etiology. Dietary deficiency of zinc and factors which interfere with zinc<br />
280
utilization.<br />
Epidemiology. Growing pigs, cattle and sheep. Excess of calcium favors disease in pigs.<br />
Signs.<br />
Pigs: Loss of body weight gain.<br />
Symmetrical, crusty skin lesions (parakeratosis) over dorsum and ears, tail;become thick and<br />
fissured. No pruritus.<br />
Ruminants: Alopecia, over muzzle, ears,tail-head, hindlegs, flank and neck. Stiff gait and<br />
swelling over coronets. Loss of wool and thickened skin is sheep.Infertility in rams.Poor growth in<br />
goats and skin lesions.<br />
Clinical pathology. Serum zinc levels lower than normal.<br />
Lesions. Parakeratosis.<br />
Diagnostic confirmation. Histology of skin lesions and serum zinc levels.<br />
Differential diagnosis list:<br />
•Sarcoptic mange in cattle and pigs<br />
•Exudative epidermitis in piglets.<br />
Treatment. Add zinc to diet.<br />
Control. Supplement zinc in diet.<br />
ETIOLOGY<br />
Swine<br />
A zinc deficiency in young, growing swine can cause parakeratosis, but it is not due to a simple<br />
zinc deficiency. The availability of zinc in the diet is adversely affected by the presence of phytic<br />
acid, a constituent of plant protein sources such as soybean meal (1). Much of the zinc in plant<br />
protein is in the bound form and unavailable to the monogastric animal such as the pig (2). The<br />
use of meat meal or meat scraps in the diet will prevent the disease because of the high availability<br />
of the zinc. Another unique feature of the etiology of parakeratosis in swine is that an excess of<br />
dietary calcium (0.5-1.5%) can favor the development of the disease, and the addition of zinc to<br />
such diets at levels much higher (0.02% zinc carbonate or 100 mg/kg zinc) than those normally<br />
required by growing swine prevents the occurrence of the disease. The level of copper in the diet<br />
may also be of some significance, increasing copper levels decreasing the requirement for zinc. A<br />
concurrent enteric infection with diarrhea exacerbates the damage done by a zinc deficiency in<br />
pigs.<br />
Ruminants<br />
A primary zinc deficiency due to low dietary zinc in ruminants is rare but does occur (3). Many<br />
factors influence the availability of zinc from soils, including the degree of compaction of the soil,<br />
and the nitrogen and phosphorus concentration. The risk of zinc deficiency increases when soil pH<br />
rises above 6.5 and as fertilization with nitrogen and phosphorus increases. Some legumes contain<br />
less zinc than grasses grown on the same soil, and zinc concentration decreases with aging of the<br />
plant. Several factors may deleteriously affect the availability of zinc to ruminants and cause a<br />
secondary zinc-deficiency. These include the consumption of immature grass, which affects<br />
digestibility, the feeding of late-cut hay, which may be poorly digestible, and the presence of<br />
excessive dietary sulfur. The contamination of silage with soil at harvesting can also affect the<br />
digestibility of zinc (3).<br />
EPIDEMIOLOGY<br />
281
Swine<br />
Parakeratosis in swine was first recorded in North America in rapidly growing pigs, particularly<br />
those fed on diets containing growth promoters. The disease occurs most commonly during the<br />
period of rapid growth, after weaning and between 7 and 10 weeks of age. From 20-80% of pigs in<br />
affected herds may have lesions, and the main economic loss is due to a decrease in growth rate.<br />
In general, the incidence is greater in pigs fed in dry lot on self-feeders of dry feed than in pigs<br />
with access to some pasture, which is preventive and curative.<br />
A low level of dietary zinc intake during pregnancy and lactation of gilts can result in skin<br />
lesions, stressful parturition and an increased incidence of intrapartum mortality of piglets and<br />
deleterious effects on neonatal growth (4).<br />
It has been suggested that parakeratosis occurs because very rapidly growing pigs outstrip their<br />
biosynthesis of essential fatty acids, and when the diet is high in calcium the digestibility of fat in<br />
the diet is reduced at the same time. The net effect in rapidly growing pigs could be a relative<br />
deficiency of essential fatty acids.<br />
Ruminants<br />
There are naturally occurring cases in cattle, sheep, and goats. The disease is well-recognized in<br />
Europe, especially in calves. It is common in some families of cattle and an inherited increased<br />
dietary requirement for zinc is suspected. The inherited disease occurs in Friesian and Black pied<br />
cattle and is known as lethal trait A46 (5). Signs of deficiency appear at 4-8 weeks of age. The<br />
main defect is an almost complete inability to absorb zinc from the intestine; zinc administration is<br />
curative.<br />
The disease in cattle has been produced experimentally on diets low in zinc, and naturally<br />
occurring cases have responded to supplementation of the diet with zinc (3). Calves remain<br />
healthy on experimental diets containing 40 mg/kg zinc, but parakeratosis has occurred in cattle<br />
grazing pastures with a zinc content of 20-80 mg/kg (normal 93 mg/kg) and a calcium content of<br />
282
0.6%. There is also an apparently improved response in cattle to zinc administration if copper is<br />
given simultaneously. Parakeratosis has also been produced experimentally in goats and sheep.<br />
Outbreaks of the disease have occurred in Sudanese Desert ewes and their lambs fed on a<br />
zinc-deficient diet of Rhodes grass containing less than 10 mg/kg of zinc. The disease has also<br />
been diagnosed in mature sheep and goats and the cause of the deficiency could not be<br />
determined. A marginal zinc deficiency, characterized by subnormal growth and fertility and low<br />
concentration of zinc in serum, but without other clinical signs, can occur in sheep grazing<br />
pastures containing less than 10 mg/kg zinc (6).<br />
PATHOGENESIS<br />
The pathogenesis of zinc deficiency is not well-understood. Zinc is a component of the enzyme<br />
carbonic anhydrase, which is located in the red blood cells and parietal cells of the stomach, and is<br />
related to the transport of respiratory carbon dioxide and the secretion of hydrochloric acid by the<br />
gastric mucosa. Zinc is also associated with RNA function and related to insulin, glucagon, and<br />
other hormones. It also has a role in keratinization, calcification, wound healing, and somatic and<br />
sexual development. Because it has a critical role in nucleic acid and protein metabolism a<br />
deficiency may adversely affect the cell-mediated immune system.<br />
A zinc deficiency results in a decreased feed intake in all species (6) and is probably the reason<br />
for the depression of growth rate in growing animals and body weight in mature animals. Failure<br />
of keratimzation resulting in parakeratosis, loss and failure of growth of wool and hair, and lesions<br />
of the coronary bands probably reflect the importance of zinc in protein synthesis. There are<br />
lesions of the arteriolar walls of the dermis. The bones of zinc-deficient ruminants reveal<br />
abnormal mineralization and reduction of zinc concentration in bones. Retarded tcsticular<br />
development occurs in ram lambs, and complete cessation of spermatogenesis suggests<br />
impairment of protein synthesis.<br />
CLINICAL FINDINGS<br />
Pigs<br />
A reduced rate and efficiency of body weight gain is characteristic. Circumscribed areas of<br />
erythema appear in the skm on the ventral abdomen and inside the thigh. These areas develop into<br />
papules 3-5 mm in diameter, which are soon covered with scales followed by thick crusts. These<br />
crusts arc most visible in areas about the limb joints, ears and tail, and are distributed<br />
symmetrically in all cases. The crusts develop fissures and cracks, become quite thick (5-7 mm)<br />
and easily detached from the skin. They are crumbly and not flaky or scaly. No greasiness is<br />
present except in the depths of fissures. Little scratching or rubbing occurs. Diarrhea of moderate<br />
degree is common. Secondary subcutaneous abscesses occur frequently, but in uncomplicated<br />
cases the skin lesions disappear spontaneously in 10-45 days if the ration is corrected.<br />
Ruminants<br />
In the naturally occurring disease in cattle, in severe cases, parakeratosis and alopecia may affect<br />
about 40% of the skin area. The lesions are most marked on the muzzle, vulva, anus, tail-head,<br />
ears, backs of the hindlegs, kneefolds, flank, and neck. Most animals are below average body<br />
condition and are stunted in growth. After treatment with zinc, improvement is apparent in 1 week<br />
and complete in 3 weeks. Experimentally produced cases exhibit the following signs:<br />
•Poor growth<br />
•A stiff gait<br />
283
•Swelling of the coronets, hocks, and knees<br />
•Soft swelling containing fluid on the anterior aspect of the hind fetlocks<br />
•Alopecia<br />
•Wrinkling of the skin of the legs, scrotum and on the neck and head, especially around t<br />
he nostrils<br />
•Hemorrhages around the teeth<br />
•Ulcers on the dental pad.<br />
The experimental disease in cattle is manifested by parakeratotic skin, mainly on the hindl<br />
imbs and udder, and similar lesions on teats, which tend to become eroded during milking.<br />
The fetlocks and pasterns are covered with scabby scales. There is exudation first with<br />
matting of hair, then drying and cracking. The skin becomes thickened and inelastic. Histo<br />
logically, there is parakeratosis. Clinical signs develop about 2 weeks after calves and lam<br />
bs go onto a deficient diet so that there is no evidence of storage of zinc in tissues in th<br />
ese animals. In goats, hair growth, testicular size, and spermatogenesis are reduced, and gr<br />
owth rate is less than normal. Return to a normal diet does not necessarily reverse these-s<br />
igns and the case fatality rate is high. There is a marked delay in wound healing.<br />
Sheep<br />
The natural disease in sheep is characterized by loss of wool and the development of thic<br />
k, wrinkled skin. Wool-eating also occurs in sheep and may be one of the earliest signs n<br />
oticed in lambs after being on a zinc-deficient diet for 4 weeks. Induced cases in lambs h<br />
ave exhibited reduced growth rate, salivation, swollen hocks, wrinkled skin, and open skin<br />
lesions around the hoof and eyes. The experimental disease in goats is similar to that in<br />
lambs.<br />
One of the most striking effects of zinc deficiency in ram lambs is impaired testicular<br />
growth and complete cessation of spermatogenesis. Diets containing 2.44 mg/kg dry matter<br />
(DM) caused poor growth, impaired testicular growth, cessation of spermatogenesis, and o<br />
ther signs of zinc deficiency within 20-24 weeks. A diet containing 17.4 mg/kg DM of zi<br />
nc is adequate for growth, but a content of 32.4 mg/kg DM is necessary for normal testic<br />
ular development and spermatogenesis. On severely deficient experimental diets, other clini<br />
cal signs in young rams are:<br />
284
Drooling copious amounts of saliva when ruminating<br />
•Parakeratosis around eyes, on nose,feet and scrotum<br />
•Shedding of the hooves<br />
•dystrophy and shedding of wool,which showed severe staining<br />
•development of a pungent odor.<br />
In naturally occurring cases in rams the animals stood with their backs arched and feet close<br />
together.<br />
A marginal zinc deficiency in ewes may be characterized by only a reduction in feed intake and<br />
a slightly reduced body weight, and no other external signs of disease. This is important because,<br />
in grazing ruminants, the lack of external signs indicates that zinc deficiency could easily pass<br />
undetected.<br />
Infertility in ewes<br />
Infertility in ewes and a dietary deficiency of zinc have not been officially linked, but a<br />
zinc-responsive infertility has been described in ewes. Again, attention is drawn to the need for<br />
response trials when soil and pasture levels of an element are marginal.<br />
An experimental zinc deficiency in pregnant ewes results in a decrease in the birth weight of<br />
the lambs and a reduced concentration of zinc in the tissues of the lambs; these effects are due to<br />
the reduced feed intake characteristic of zinc deficiency (6). The zinc content of the diet did not<br />
significantly influence the ability of the ewes to become pregnant or maintain pregnancy. The<br />
combination of i pregnancy and zinc deficiency in the ewe leads to highly efficient utilization of<br />
ingested zinc, and the developing fetus will accumulate about 35% of the total dietary intake of<br />
zinc of the ewe during the last trimester of pregnancy. The disease is correctable by the<br />
supplementary feeding of zinc.<br />
Goats<br />
Experimentally induced zinc deficiency in goats results in poor growth, low food intake, testicular<br />
hypoplasia, rough dull coat with loss of hair, and the accumularion of hard, dry, keratinized skin<br />
on the hindlimb scrotum, head and neck. Onthe lower limbs the scabs fissure, crack, and produce<br />
some exudate. In naturally occurring cases in pygmy goats there was extensive alopecia, a<br />
kyphotic stance, extensive areas of parakeratosis, abnormal hoof growth and flaky, painful<br />
coronary bands. A zinc-responsive alopecia and hyperkeratosis in Angora goats has been described.<br />
Affected animals had recurrent pruritus, hyperemia, exfoliation, fleece loss over the hindquarters,<br />
face and ears, and a decline in reproductive performance.<br />
Immediately before parturition in cows there is a precipitate fall in plasma zinc concentration,<br />
which returns to normal slowly after calving. The depression of zinc levels is greater in cows that<br />
experience dystocia. This has led to the hypothesis that dystocia in beef heifers may be caused in<br />
some circumstances by a nutritional deficiency of zinc and that preparturient supplementation of<br />
the diet with zinc may reduce the occurrence of difficult births. This phenomenon does not appear<br />
to occur in sheep. The level of serum zinc increased in cattle during the season of facial eczema<br />
when sporidesmin intoxication causes depiction of liver zinc (7).<br />
CLINICAL PATHOLOGY<br />
Skin scraping<br />
Laboratory examination of skin scrapings yields negative results, but skin biopsy will confirm the<br />
diagnosis of parakeratosis.<br />
Zinc in serum and hair<br />
285
Serum zinc levels may have good diagnostic value. Normal levels are 80- 120 µg/dL<br />
(12.2-18.2µmol/L) in sheep and cattle. Calves and lambs on deficient diets may have levels as low<br />
as 18µg/dL (3.0 µmol/L). Normal serum zinc levels in sheep are above 78 µg/dL (12 µmol/L), and<br />
values below 39 µg/dL (6 µmol/L) or less arc considered as evidence ot deficiency (6). There is a<br />
general relationship between the zinc content of the hair and the level of zinc in the diet, but the<br />
analysis of hair is not considered to be a sufficiently accurate indicator of an animal's zinc status.<br />
In experimental disease in piglets there is a reduction in serum levels of zinc, calcium and alkaline<br />
phosphatase, and it is suggested that the disease could be detected by measuring the serum<br />
alkaline phosphate and serum zinc levels. Levels of zinc in the blood are very labile and simple<br />
estimations of it alone arc-likely to be misleading. For example, other intercurrent diseases<br />
commonly depress serum calcium and copper levels.In addition, zinc levels in plasma fall<br />
precipitately at parturition in cows; they are also depressed by hyperthermal stress. After 1 week<br />
on a highly deficient diet serum zinc levels fall to about 50% of normal, or pretreatment levels.<br />
NECROPSY FINDINGS<br />
Necropsy examinations are not usually performed, but histological examination of skin biopsy<br />
sections reveals a marked increase in thickness of all the elements of the epidermis. Tissue levels<br />
of zinc differ between deficient and normal animals but the differences are statistical rather than<br />
diagnostic.<br />
DIFFERENTIAL DIAGNOSIS<br />
Sarcoptic mange may resemble parakeratosis, but is accompanied by much itching and rubbing.<br />
The parasites may be found in skin scrapings. Treatment with appropriate parasiticides relieves the<br />
condition.<br />
Exudative epidermitis is quite similar in appearance, but occurs chiefly in unweaned pigs. The<br />
lesions have a greasy character that is quite different from the dry, crumbly lesions of<br />
parakeratosis. The mortality rate is higher.<br />
TREATMENT<br />
In outbreaks of parakeratosis in swine, zinc should be added to diet immediately at the rate of 50<br />
mg/kg DM (200 mg of zinc sulfate or carbonate per kg of feed). The calcium level of the diet<br />
should be maintained at between 0.65 and 0.75%. The injection of zinc at a rate of 2-4 mg/kg BW<br />
daily for 10 days is also effective. Zinc oxide suspended in olive oil and given IM at a dose of 200<br />
mg of zinc for adult sheep and 50 mg of zinc for lambs will result in a clinical cure within 2<br />
months. The oral administration of zinc at the rate of 250 mg zinc sulfate daily for 4 weeks<br />
resulted in a clinical cure of zinc deficiency in goats in 12-14 weeks.<br />
CONTROL<br />
Swine<br />
The calcium content of diets for growing pigs should be restricted to 0.5-0.6%. However, rations<br />
containing as little as 0.5% calcium and with normal zinc content (30 mg/kg DM) may produce<br />
the disease. Supplementation with zinc (to 50 mg/kg DM) as sulfate or carbonate has been found<br />
to be highly effective as a preventive and there appears to be a wide margin of safety in its use,<br />
diets containing 1000mg/kg DM added zinc having no apparent toxic effect. The standard<br />
recommendation is to add 200 g of zinc carbonate or sulfate to each tonne of feed. Weight gains in<br />
affected groups arc appreciably increased by the addition of zinc to the diet. The addition of oils<br />
containing unsaturated fatty acids is also an effective preventive. Access to green pasture,<br />
reduction in food intake, and the deletion of growth stimulants from rations will lessen the<br />
286
incidence of the disease but arc not usually practicable.<br />
Ruminants<br />
For cattle, the feeding of zinc sulfate (2-4 g daily) is recommended as an emergency measure<br />
followed by the application of a zinc-containing fertilizer. As an alternative to dietary<br />
supplementation for ruminants, an intraruminal pellet has been demonstrated in sheep. It was<br />
effective for 7 weeks only and would not be satisfactory for long-term use. The creation of<br />
subcutaneous depots of zinc by the injection of zinc oxide or zinc metal dust has been<br />
demonstrated. The zinc dust offered a greater delayed effect.<br />
REVIEW LITERATURE<br />
Lamand, M. (1984) Zinc deficiency in<br />
ruminants. Irish Vet.)., 38, 40-47. Luccke, R. W. (1984) Domestic animals in theelucidation of<br />
zinc's role in nutrition. Fed.<br />
Proc, 43, 2823-2828.<br />
REFERENCES<br />
(1)Luecke, R. W. (1984) Fed. Proc, 43, 2823.<br />
(2)Forbes. R. M. (1984) Fed. Proc, 43, 2835.<br />
(3)Lamand, M. (1984) Irish Vel.J., 38, 40.<br />
(4)Kalinowski.J. & Chavez, E. R. (1986) Can. J.Anim. Sci., 66,201, 217.<br />
(5)Machen, M. el al. (1996)/. Vet. Diagn. Invest., 2, 219.<br />
(6)Underwood, E.J. (1981) The Mineral Nutrition of Livestock, 2nd edn. Farnham Royal,<br />
Commonwealth Agricultural Bureaux.<br />
(7)Dewes, H. F. & Lowe, M. D. (1987) NZ Vet.J., 35, 16.<br />
五、锰缺乏症(Manganess Deficiency)<br />
因饲料中缺乏锰或因钙、磷等干扰成分含量过高,引起原发性和继发性动物锰缺乏症。<br />
临床上表现繁殖机能障碍、不育、不孕和骨骼短粗、腱滑脱等现象。可以是因母畜(禽)缺<br />
锰引起幼畜先天性缺乏锰所致。也可以是出生后,饲料中缺锰,引起后天性锰营养缺乏所致。<br />
动物中以家禽最易产生锰缺乏症,鸡、鸭、火鸡、珍珠鸡、鹅,甚至野生禽如鹰、松鸡、<br />
鸸鹋等也有缺锰症报道。其次是幼猪、犊牛、羔羊、绵羊、山羊、实验动物等。<br />
【病因】 原发性锰缺乏症,呈地方流行性。石灰岩风化的土壤中锰含量较少,土壤中<br />
Mn6.3 以上,Mn 4+ 倾<br />
向于氧化为Mn 2+ 。土壤中有机质过多,可与Mn 2+ 形成不溶性复合物,而影响植物吸收利用。<br />
土壤中铁含量过多,亦可减少植物对锰的吸收。钴亦可减少锰的有效性;在反复施钴肥防止<br />
动物地方性消瘦时,易降低植物中锰含量。<br />
锰是植物的必需微量元素。燕麦缺锰可发生灰斑病,叶脉、叶身变黄褐色。甜菜黄斑病,<br />
豆类湿斑病等都与缺锰有关。各种植物中锰含量相差很大,白羽扇豆是高度锰富集植物,其<br />
中锰含量可达 817~3397mg/kg;大多数植物在 100~800mg/Kg之间,如小麦、燕麦、麸皮、<br />
米糠等应能满足动物生长需要。但是,玉米(8mg/kg)、白面(5mg/kg)、豆荚(16mg<br />
287
kg)中锰含量很低,以玉米、豆饼为主食的鸡、猪容易产生锰缺乏症。饲料中胆碱、烟酸、<br />
生物素及VB2、VB12、VD等不足,机体对锰的需要量增多。<br />
动物饲料中钙、磷、镁含量过高,可降低锰在骨骼灰分中含量。常量元素对微量元素的<br />
干扰作用应引起高度重视。此外饲料中铁、钴含量多,亦可干扰锰的吸收。<br />
【病理】 锰是体内多种酶的活性中心。如精氨酸酶,丙酮酸羧化酶、醛缩酶等,与三<br />
羧酸循环关系密切。锰还是超氧化物歧化酶活性中心,与体内自由基清除关系密切。缺锰后<br />
可引起能量代谢紊乱,固醇类物质的合成障碍;锰是多糖聚合酶、半乳糖转移酶活性中心,<br />
缺锰可影响已糖胺、聚糖和硫酸软骨素的合成,并影响软骨生长、骨骼生成和矿化作用,骨<br />
骼形态改变和耳前庭内软骨发育,可致终身平衡失调,尤其是急烈运动时可就地翻转。<br />
锰缺乏可影响固醇类物质合成。性激素是固醇类物质的衍生物。缺锰时,雌激素、睾丸<br />
酮含量减少,引起动物繁殖机能障碍。由此可见锰与脂代谢关系密切。事实上当饲料中胆碱<br />
缺乏时,不仅可影响锰的吸收,而且可助长锰缺乏症。<br />
锰与凝血酶元合成、VK的活性及锰在促进胎儿体内造血过程中作用也不可忽视。<br />
【临床表现】 动物锰缺乏有许多共同的表现。如骨骼短、粗,骨重量正常。腱容易从<br />
骨沟内滑脱,形成“滑腱症”;动物缺锰常引起繁殖机能障碍,母畜不发情,不排卵;公畜<br />
精子密度下降,精子活力减退。母鸡产蛋量减少,鸡胚易死亡等特征。各种动物的临床表现<br />
有:<br />
禽缺锰:小鸡表现软骨生成缺限,关节肥大。主要是胫跗关节肥大,胫骨拧曲或弯曲,<br />
长骨增厚、变短、变粗。小鸡懒于运动。强迫运动时,呈跗关节着地,并很快死亡。有些鸡<br />
胫骨、翅骨短粗,下颌骨缩短,呈鹦鹉喙,球形头。关节肿大和畸形的发病率达 30%~40%。<br />
有的添加过量维生素A和D者,发病率达 80%以上。两肢患病者,站立时腿呈:“O”形或“X”<br />
形,一肢患病者,病肢短,悬垂,健肢着地。刚出壳鸡还显神经症状,如共济失调,呈观星<br />
姿势,按骨软症或VB12缺乏症治疗不但无效,甚至使病情恶化。<br />
小鸭缺锰时,8~20 日龄鸭最易出现临床症状。可有胫跗关节肿大,胫骨远端和跖骨近<br />
端扭转或弯曲,患鸭跛行,最后腓肠肌腱从踝部脱落,患肢完全残废,最后终因采食困难而<br />
死。小火鸡、野鸡雏、松鸡、鹌鹑等均发生。<br />
重型鸡比轻型鸡更易患锰缺乏症。轻度缺锰鸡呈现典型的短腿、短翅、短身躯。<br />
成年母鸡缺锰,可有产蛋减少,蛋受精率下降,鸡胚常于孵化至第 20、21 天死亡,死<br />
胚呈现软骨发育不良,腿短粗,翅、喙短小,头圆,肚大。75%鸡胚出现水肿,鸡蛋中锰较<br />
正常时低得多。中雏有时受惊吓时,可表现神经症状。如惊厥、头向下、向上、甚至扭转向<br />
背部或勾入腹下,它们可以正常生长至成熟,但运动不稳,很难克服。不可逆的步伐紊乱,<br />
与前庭平衡系统受损及耳石生成有关。<br />
蛋壳易碎也是成年鸡缺锰特点之一。有人用含 6.5mg/kg 和 100mg/kgMn 的不同饲料<br />
喂鸡,前者产的蛋,其蛋壳破碎力为 6.6 磅,后者为 9.3 磅,而且蛋壳灰分中 Mn 增加,蛋<br />
壳不光滑。<br />
牛缺锰,引起不孕症犊牛的骨、关节先天性变形。犊牛表现生长不良,被毛干燥,褪色,<br />
钩爪,关节扩大,腿拧曲。羔羊长骨变短,虚弱,关节疼痛,不愿移动,瘫痪。母羊。母牛<br />
繁殖性能下降,常有发情延迟,不能受孕,一侧或两侧性卵巢缩小。<br />
山羊缺锰,发情不明显,妊娠期延长,流产、难产比例增多,常要多次配种或多次人工<br />
授精。约有 1/4 的羊在妊娠 3~5 个月时流产,新生羔雄性比例增多。<br />
猪实验性锰缺乏,引起骨生长减慢,肌肉虚弱,肥胖,发情减少,无规律性,甚至不发<br />
情、胎儿吸收或无乳可授或生后不久死亡。腿虚弱,前肢弯曲,缩短。<br />
临床病理学变化是:犊牛血锰可从 0.18~0.19mg/L,降至很低,肝锰可从 12mg/kg 降<br />
至 8mg/kg 以下。毛锰虽变化较大,一般从 12mg/kg 降为 8mg/kg。但正常母牛于分娩<br />
288
前夕毛发中锰可低至 4.5mg/kg,卵巢中锰可从 2mg/kg 降为 0.6~0.85mg/kg。骨骼灰分<br />
及骨锰含量无明显下降。<br />
【诊断】 本病诊断主要根据临床表现。如母畜繁殖机能下降,不孕,不发情,或屡配<br />
不孕。骨骼变形,短粗有滑腱表现。但骨骼灰分重量不变,新生仔畜常有关节扩大,骨骼变<br />
形等特点。有时有平衡失凋,受到突然刺激时,不平衡现象更为严重。<br />
饲料中锰测定值常低于 40mg/kg。但钙、磷、铁的含量亦应同时考虑。土壤中锰测定<br />
的同时,应注意土壤的 pH 的影响,血液、毛发中锰测定,仅可作为诊断参考。<br />
【防治】 禽患锰缺乏症,多把锰盐或锰的氧化物掺入到矿物质补充剂中,或掺入粉碎<br />
的日粮内。所补充的锰很易进入鸡蛋,改善鸡胚的发育和增加出壳率。如同时添加适量的胆<br />
碱、生物素及多维素,效果更好。锰的氧化物、过氧化物、氯化物、碳酸盐、硫酸盐等似乎<br />
有同样的补锰效果。日粮锰的最后浓度至少为 40~50mg/kg。罗绪刚(1991)等试验认为,<br />
100~120mg/kg 之间,饲料报酬高,腿病发病率最低(仅 2.5%~10%),雏鸡可用 1.0g 高锰<br />
酸钾溶于 20 升常水,每天二次饮用,连用 2 日。间隔 2 日,再饮 l~2 天,可防治雏后天性<br />
缺锰。<br />
猪日粮中锰含量一般能满足其需要,不再补充锰。牛羊在低锰草地放牧时,小母牛每天<br />
给 2g,大牛每天给 4g 硫酸锰,可防止牛的锰缺乏症。每公顷草地用 7.5kg 硫酸锰,与其它<br />
肥料混施,可有效地防止锰缺乏症。<br />
【锰中毒】 (Mangness Poisoning) 相对而言,锰是无毒元素,对禽、畜比较安全。<br />
各种动物对日粮锰的耐受量是:猪 500mg/kg 以下,犊牛 820mg/kg,羔羊 400mg/kg,鸡<br />
1000mg/kg,大鼠甚至可耐受 5000~10000mg/kg。<br />
但锰过多可影响反刍动物瘤胃微生物生长繁殖,锰过多还可干扰铁、钴的吸收和利用。<br />
因此,羊的钴缺乏症,有时饲料中钴并不太低,但因锰太多,一样可产生钴缺乏的典型表现。<br />
锰对铁的干扰作用,还可引起仔猪和兔的缺铁性贫血发病增多,也可引起犊牛生长迟缓和贫<br />
血。一旦调整饲料中锰的浓度,以上现象可迅速克服。<br />
MANGANESE DEFICIENCY<br />
A dietary deficiency of manganese may cause infertility and skeletal deformities both congenitally<br />
and after birth.<br />
ETIOLOGY<br />
A primary deficiency occurs endemically in some areas because of a geological defiency in the<br />
local rock formations (1). Apart from a primary dietary deficiency of manganese, the existence of<br />
factors depressing the availability of ingested manganese is suspected. An excess of calcium<br />
and/or phosphorus in the diet is known to increase the requirements of manganese in the diet of<br />
calves (5), and is considered to reduce the availability of dietary manganese to cattle<br />
generally.Congential chondrodystrophy in calves has been associated with a manganese deficiency<br />
(2), and an outbreak of congenital skeletal defects in Holstein calves due to manganese deficiency<br />
has been reported (3).<br />
EPIDEMIOLOGY<br />
Soils containing less than 3 mg/kg of manganese are unlikely to be able to support normal fertility<br />
in cattle. In areas where manganese-responsive infertility occurs, soils on farms with infertility<br />
problems have contained less than 3 mg/kg of manganese, whereas soils on neighboring farms<br />
with no infertility problems have had levels of more than 9 mg/kg. A secondary soil deficiency is<br />
thought to occur and one of the factors suspected of reducing the availability of manganese in the<br />
soil to plants is high alkalinity. Thus, heavy liming is associated with manganese-responsive<br />
infertility. There are three main soil types on which the disease occurs:<br />
289
•Soils low in manganese have low out put even when pH is less than 5.5<br />
•Sandy soils where availability starts to fall<br />
•Heavy soils where availability starts to fall at pH of 7.0.<br />
Many other factors are suggested as reducing the availability of soil manganese but the<br />
evidence is not conclusive. For example, heavy liming of soils to neutralize sulfur dioxide<br />
emissions from a neighboring smelter is thought to have reduced the manganese intake of grazing<br />
animals.<br />
Herbage on low manganese soils, or on marginal soils where availability is decreased (possibly<br />
even soils with normal manganese content), is low in manganese. A number of figures are given<br />
for critical levels. It is suggested that pasture containing less than 80 mg/kg of manganese is<br />
incapable of supporting normal bovine fertility, and that herbage containing less than 50 mg/kg is<br />
often associated with infertility and anestrus. The Agricultural Research Council feels that,<br />
although definite figures are not available, levels of 40 mg/kg dry matter (DM) in the diet should<br />
be adequate. Other authors state that rations containing less than 20 mg/kg DM may cause<br />
anestrus and reduction in conception rates in cows and the production of poor quality semen by<br />
bulls. Most pasture contains 50-100 mg/kg DM. Skeletal deformities in calves occur when the<br />
deficiency is much greater than the above for example, a diet containing more than 200 mg/kg<br />
DM is considered to be sufficient to prevent them.<br />
Rations fed to pigs usually contain more than 20 mg/kg DM of manganese, and deficiency is<br />
unlikely unless there is interference with manganese metabolism by other substances.<br />
There are important variations in the manganese content of seeds, an important matter in<br />
poultry nutrition (1). Maize and barley have the lowest content. Wheat or oats have three to five<br />
times as much, and bran and pollard are the richest natural sources with 10-20 times the content of<br />
maize or wheat. Cows' milk is exceptionally low in manganese.<br />
PATHOGENESIS<br />
Manganese plays an active role in bone matrix formation, and in the synthesis of chondroitin<br />
sulfate, responsible for maintaining the rigidity of connective tissue. In manganese deficiency<br />
these are affected deleteriously and skeletal abnormalities result. Only 1% of manganese is<br />
absorbed from the diet and the liver removes most of it, leaving very low blood levels of the<br />
element (2).<br />
CLINICAL FINDINGS<br />
In cattle, the common syndromes are infertility, calves with congenital limb deformities and calves<br />
with manifest poor growth, dry coat, and loss of coat color. The deformities include knuckling<br />
over at the fetlocks, enlarged joints and, possibly, twisting of the legs. The bones of affected lambs<br />
are shorter and weaker than normal and there are signs of joint pain, hopping gait, and reluctance<br />
to move.<br />
A severe congenital chondrodystrophy in Charolais calves occurred on one farm (2). The limbs<br />
were shortened and the joints enlarged. The pregnant cows were fed on apple pulp and corn silage<br />
both of which were low in manganese.<br />
290
An outbreak of congenital skeletal malformations in Holstein calves was characterized<br />
clinically by small birth weights (average 15 kg). Abnormalities included joint laxity, doming of<br />
the foreheads, superior brachynathia, and a dwarflike appearance due to the short long bones. The<br />
features of the head were similar to those of the wildebeest. The majority of affected calves were<br />
dyspneic at birth, and snorting and grunting respratory sounds were common. Affected calves<br />
failed to thrive and most were culled due to poor performance.<br />
A manganese-responsive infertility has been described in ewes and is well known in cattle. In<br />
cattle it is manifested by slowness to exhibit estrus, and failure to conceive, often accompanied by<br />
subnormal size of one or both ovaries. Subestrus and weak estrus have also been observed.<br />
Functional infertility' was once thought to occur in cattle on diets with calcium to phosphorus<br />
ratios outside the range of 1:2 to 2:1. This was not upheld on investigation but may have been<br />
correct if high calcium to phosphorus intakesdirectly reduced manganese (or copper or iodine)<br />
availability in diets marginally deficient in one or other of these elements.<br />
In pigs,experimental diets low in manganese cause reduction in skeletal growth, muscle<br />
weakness, obesity, irregular, diminished or absent estrus, agalactia, and resorption of fetuses or the<br />
birth of stillborn pigs. Leg weakness, bowing of the front legs, and shortening of bones also occur.<br />
CLINICAL PATHOLOGY<br />
Thebloodofnormalcattlecontains18-19 µg/dL (3.3-3.5 µmol/L) of manganese, although<br />
considerably lower levels are sometimes quoted.The livers of normalcattlecontain12 mg/kg(0.21<br />
mmol/kg) of manganese anddownto 8mg/kg(0.15 mmol/kg)innewborn calves, which also have a<br />
lower content in hair.Themanganesecontentofhairvaries with intake.The normal level is<br />
about12mg/kg(0.21 mmol/kg)and infertility is observed in association with levelsoflessthan8<br />
mg/kg(0.15 mmol/kg). In normal cows,the manganese content of hair falls during pregnancy from<br />
normal levels of 12 mg/kg (0.21 mmol/kg)in the first month of pregnancy to 4.5 mg/kg (0.08<br />
mmol/kg) at calving.Allof these figures require much more critical evaluation than they have had,<br />
291
efore they can be used as diagnostic tests.<br />
Although tissue manganese levels in normal animals have been described as being between 2<br />
and 4 mg/kg (0.04 and 0.07 mmol/kg), in most tissue (1) there appears to be more variation<br />
between tissues than this. However, tissue levels of manganese do not appear to be depressed in<br />
deficient animals, except for ovaries in which levels of 0.6 mg/kg (0.01 mmol/kg) and 0.85 mg/kg<br />
(0.02 mmol/kg) are recorded in contrast to a normal level of 2 mg/kg (0.04 mmol/kg).<br />
There is then no simple, single diagnostic test permitting detection of manganese deficiency in<br />
animals. Reproductive functions, male and female, are most sensitive to manganese deficiency<br />
and are affected before possible biochemical criteria, e.g. blood and bone alkaline phosphatase,<br />
and liver arginase levels, are significantly changed. The only certain way of detecting moderate<br />
deficiency states is by measuring response to supplementation. Clinical findings in response to<br />
treatment which may provide contributory evidence of manganese deficiency are set out below.<br />
NECROPSY FINDINGS<br />
In congenital chondrodystrophy in calves, the limbs are shortened and all the joints are enlarged.<br />
Histologically, there is poor cartilage maturation with excessive amounts of rarefied cartilage<br />
matrix. There are degenerative changes in the chondrocytes and severe reduction in the<br />
mucopolysaccharide content of all body hyaline cartilage (2, 3).<br />
TREATMENT AND CONTROL<br />
Young cattle have shown a general response in fertility to 2 g MnSO4 daily, but the general<br />
recommendation is daily supplementation with 4 g manganese sulfate providing 980 mg elemental<br />
manganese. This level of feeding is estimated to raise the dietary intake by 75 mg/kg DM<br />
(estimated on a daily intake of 12 kg DM by a 450 kg cow). In some herds a full response was<br />
obtained only after doubling this rate of feeding. Although the feeding of 15 g of manganese<br />
sulfate daily is reported to cause no signs of toxicity, manganese is known to interfere with the<br />
utilization of cobalt and zinc in ruminants. Very large levels of intake to calves can reduce growth<br />
rate and hemoglobin levels. The recommended procedure is to feed the supplement for 9 weeks<br />
commencing 3 weeks before the first service.<br />
Excessive supplementation, up to 5000 mg/kg, of the diet with manganese for periods of up to 3<br />
months appeared to cause only a reduction in appetite and weight gain.<br />
For pigs, the recommended dietary intakes are 24-57 mg manganese per 45 kg BW. Expressed<br />
as a proportion of food intake the recommended dietary level is 40 mg/kg DM in feed.<br />
REFERENCES<br />
(1)Underwood, E.J. (1981) The Mineral Nutrition of Livestock, 2nd edn. Famhain Royal,<br />
Commonwealth Agricultural Bureaux.<br />
(2)Valero, G. et al. (1990) NZ Vet.]., 38, 161.<br />
(3)Stalcy, G. P. et al. (1994)/ South African Vet. Assoc., 65, 73.<br />
六、钴缺乏症(Cobalt Deficiency)<br />
因饲料或饮水中缺乏钴,引起厌食、极度消瘦和贫血的现象称为钴缺乏症。钴缺乏症仅<br />
发生于牛、羊等反刍动物,而杂食动物和食肉动物不发生。同样是食草动物的马和其它非反<br />
刍动物,即使限制在缺钴草场放牧,仍表现健康,生长正常。<br />
【病因】 地区性缺乏钴。世界上有许多地方未经改造时,似乎不适宜发展反刍动物。<br />
如风沙堆积性草场、沙质土、碎石或花岗岩风化的土地,灰化土或是火山灰烬覆盖的地方,<br />
都严重缺乏钴。在土壤中钴含量低于 0.11mg/kg时,牧草中钴含量很低,易引起钴缺乏症。<br />
但土壤中钙含量升高,可减少植物中钴含量。土壤中pH和其它元素如铁、锰含量过高,可<br />
292
减少植物中钴含量。土壤pH升高,植物钴吸收减少,此外,耕作方法、灌溉及植物品种等<br />
都可影响植物中钴含量。有试验表明,当植物中钴含量低于 0.01mg/kg,可发生严重的急<br />
性钴缺乏。牛、羊体况迅速下降,死亡率很高。钴含量为 0.01~0.04mg/kg,羊可表现急性<br />
钴缺乏,牛表现为消瘦病;含量为 0.04~0.07mg/kg,羊可表现钴缺乏症,牛仅有全身体况<br />
下降;含量>0.07mg/kg,牛羊外观似乎健康,羊体况稍差;含量>0.1~0.3mg/kg,牛、羊<br />
健康,繁殖能力良好。同一植株中,叶子含钴量占 56%,种子中仅占 24%,茎、杆、根中<br />
占 18%,而皮壳中钴含量仅占l%~2%。因此,在缺乏钴地区,用干草和谷物饲喂,又未补<br />
充钴,容易产生钴缺乏症。豆科植物中钴含量较高,棉籽饼中钴含量可达 2.0~2.1mg/kg,<br />
普通牧草中钴含量仅 0.03~0.2mg/kg。在加里弗尼亚,牛吃了球茎鬲草后,可患晕倒症,<br />
补充钴可预防,补充VB12无效。<br />
【病理】 钴是动物必需微量元素,尤其是反刍动物。钴在体内贮存量有限,只有在反<br />
刍动物的瘤胃中,钴才能发挥其生物学作用。这是因反刍动物瘤胃中细菌生长、繁殖需要钴,<br />
其中一部分细菌可利用钴合成VB12。有资料证明,细菌在 30~40min内可把瘤胃液中 80%~85<br />
%的钴固定到体内,利用率很高。瘤胃中有 50 亿~80 亿个/g细菌,所合成的VB12是反刍动<br />
物必需的维生素,不仅可保证瘤胃原生动物生长、繁衍,而且也使纤维素的消化正常进行。<br />
如缺乏钴,则因VB12合成不足,可直接影响细菌及原生动物的生长、繁殖,也影响纤维素等<br />
的消化。<br />
反刍动物能量来源与非反刍动物不同,它主要由在瘤胃中产生的丙酸,通过糖异生的途<br />
径合成体内的葡萄糖,并供给能量。在由丙酸转为葡萄糖的过程中,需要甲基丙二酰辅酶A<br />
变位酶参予。VB12是该酶的辅酶,如缺乏它,则可产生反刍动物能量代谢障碍,引起消瘦、<br />
虚弱。<br />
钴可加速体内贮存铁的动员,使之容易进入骨髓。钴还可抑制许多呼吸酶活性,引起细<br />
胞缺氧,刺激红细胞生成素的合成,代偿性促进造血功能。VB12在由N´5-甲基四氢叶酸转为<br />
有活性的四氢叶酸的过程中,有重要作用,因而参予了胸腺嘧啶核苷酸的合成。当缺乏VB12<br />
时,胸腺嘧啶合成受阻,细胞分裂中止,导致巨细胞性贫血。<br />
此外,钴还可改善锌的吸收,锌与味觉素合成密切相关,缺钴情况下,可引起食欲下降,<br />
甚至异食癖。<br />
由此可见,反刍动物缺乏钴,不仅可直接对动物产生不利的影响,而且可影响到细菌、<br />
纤毛虫等生物活性,减少VB12的体内合成,并由此而产生能量代谢障碍和造血功能降低。<br />
至于动物因采食球茎鬲草等引起脑灰质软化症,在新西兰发现因缺钴产生的白肝病,致<br />
肝机能损伤,光过敏现象,用钴制剂预防,可获满意效果,但VB12效果不理想,其机制尚不<br />
清楚。<br />
【临床表现】 绵羊、牛、山羊在低钴草场放牧数周或数月内,外表仍显健康,但继续<br />
下去,畜群中有些动物渐进性食欲减少,被毛由黑变为棕黄色,贫血,可视黏膜淡白,血红<br />
蛋白浓度降为 60g/L,流泪,体重减轻,最终消瘦和虚弱。即使在嫩绿草地放牧的羊、牛<br />
亦如此。牛常可出现异食癖,可视黏膜淡白,易疲劳,生长迟缓。羊毛、奶产量下降,毛脆<br />
而易断,易脱落,动物痒感明显,后期可有繁殖功能下降、拉稀、流泪,特别是绵羊,因流<br />
泪而使面部被毛潮湿,这是严重钴缺乏症的最明显特点。当牛、羊在缺钴草地放牧 6 个月内,<br />
这些症状日趋明显,症状出现后 3~12 个月内可出现死亡。分娩或流产等应激作用下,可使<br />
病畜被迫淘汰。<br />
用活组织穿刺或扑杀,采集肝脏样品(谨防沾污),测定肝脏中VB12含量,可从正常时<br />
的 0.2~0.3mg/kg降为 0.11~0.07mg/kg以下,血液中VB12可从 2.3ng/ml降低至 0.47ng/ml,<br />
瘤胃中钴的浓度可从 1.3±0.9mg/kg降低至 0.09±0.06mg/kg。<br />
尿液中甲基丙二酸(MMA)和亚胺甲基谷氨酸(FIGLU)含量升高。健康动物尿液中<br />
293
这两种物质含量甚微,但当钴缺乏时,FIGLU浓度可从 0.08mmol/L升高到 0.2mmol/L。<br />
MMA浓度可达 15mmol/L以上。尿液需静置 24h以上测定,应预先作酸化处理,以防MMA<br />
降解。补充钴或VB12以后,尿液中几乎检测不出FIGLU。测定FIGIU似乎比MMA更敏感。<br />
钴缺乏动物常显贫血,但血红蛋白和红细胞数常在正常范围内,成正红细胞性或正染色<br />
性贫血。缺钴动物骨髓中红细胞数减少,用VB12或非消化道补充钴,难以纠正这种贫血现象。<br />
此外,钴缺乏动物常可出现低糖血症(
COBALT DEFICIENCY<br />
Cobalt deficiency is a disease of ruminants ingesting a diet deficient in cobalt, which is required<br />
for the synthesis of vitamin B12. The disease is characterized clinically by inappetence and loss of<br />
body weight. Some effects on reproductive performance in sheep have been reported.<br />
Synopsis<br />
Etiology. Dietary deficiency of cobalt resulting in a deficiency of vitamin Bl2.<br />
Epidemiology. Occurs primarily in cattle and sheep unsupplemented with cobalt worldwide<br />
where soils are deficient in cobalt. Associated with ovine white liver disease.<br />
Signs. Inappetence, gradual loss of body weight, pica, marked pallor of the mucous membranes.<br />
Wool and milk production decreased. Decreased lambing percentage.<br />
Clinical pathology. Cobalt, or vitamin B12. concentration of liver. Cobalt concentrations.<br />
Methylmalonic acid in plasma and urine. Formiminoglutamic acid in urine. Anemia.<br />
Lesions. Emaciation, hemosiderosis of spleen.<br />
Diagnostic confirmation. Vitamin B12 and cobalt of liver.<br />
Differential diagnosis list:<br />
Common causes of ill-thrift in ruminants:<br />
•Copper deficiency<br />
•General nutritional deficiency (protein<br />
and energy)<br />
•Johne's disease<br />
•Intestinal helminthiasis.<br />
Treatment. Oral dosing with cobalt or parenteral injections of vitamin B12.<br />
Control. Dietary supplementation with<br />
cobalt. Cobalt-heavy pellets.<br />
ETIOLOGY<br />
The disease is caused by a deficiency of cobalt in the diet which results in a deficiency of vitamin<br />
B12.<br />
EPIDEMIOLOGY<br />
Occurrence<br />
Cobalt deficiency occurs in Australia, New Zealand, the United Kingdom and North America, and<br />
probably occurs in mainy other parts of the world (1). Where the deficiency is extreme, large<br />
tracts of land are unsuitable for the raising of ruminants, and in certain areas suboptima] growth<br />
and production may be limiting factors in the husbandry of sheep and cattle. The concentration of<br />
cobalt in the soil can vary widely as, for example, in Irish cattle farms where the soil cobalt<br />
content varied between 0.2 and 18 mg/kg dry matter (DM), the forage had marginal to normal<br />
cobalt content, and low or very low blood vitamin B12 status was found in 55% of herds sampled<br />
(2). However, the significance of the cobalt deficiency clinically is uncertain (3).<br />
Cattle and sheep are similarly affected and the signs are similar in both species. Cattle are<br />
slightly less susceptible than sheep, and lambs and calves are more seriously affected than adults.<br />
Frank deficiency is unlikely to occur in pigs, or in other omnivores or carnivores, because vitamin<br />
B12 is present in meat and other animal tissues, but there are some reports of improved weight<br />
gains following supplementation of the ration with cobalt. Horses appear to be unaffected.<br />
Although the disease occurs most commonly in ruminants at pasture in severely deficient areas,<br />
sporadic cases occurin marginal areas, especially after long periods of stable feeding. Bulls, rams,<br />
295
and calves are the groups most commonly affected, although dairy cows kept under the same<br />
conditions may develop a high incidence of ketosis.<br />
Risk factors<br />
Dietary and environmental factors<br />
Pastures containing less than 0.07 and 0.04 mg/kg DM result in clinical disease in sheep and cattle,<br />
respectively. The daily requirement for sheep at pasture is 0.08 mg/kg DM of cobalt; for growing<br />
lambs the need is somewhat greater and at pasture levels of less than 0.10 mg/kg DM inefficient<br />
rates of gain are likely. For growing cattle, an intake of 0.04 mg/kg DM in the feed is just below<br />
requirement levels (4). Variations in the cobalt content of pasture occur with seasonal variations in<br />
pasture growth and with drainage conditions. The increased incidence of the disease, which has<br />
been observed in the spring, may be related to domination of the pasture by rapidly growing<br />
grasses, which have a lower cobalt content than legumes. There is also a great deal of variation<br />
between years in the severity of the losses encountered due to variations in the cobalt status of the<br />
animals. Forage grown on well-drained soils has a greater cobalt content than that grown on<br />
poorly drained soils of the same cobalt status. Plant growth is not visibly affected by a low cobalt<br />
content of the soil, but the addition of excessive quantities may retard growth.<br />
Cobalt is also protective against the liver damage in sheep exposed to annual ryegrass (5).<br />
Primary cobalt deficiency occurs only on soils which are deficient in cobalt. Such soils do<br />
not appear to have any geological similarity,varying from<br />
296
windblown shell sands to soils derived from pumice and granite. Japanese soils composed largely of<br />
volcanic ash are seriously deficient. A survey in New Brunswick, Canada, revealed the average value for grass<br />
samples was 0.028 mg/kg DM, and for legume samples, 0.088 mg/kg DM, which justifies supplementation of<br />
ruminant diets with cobalt. The soils in New Brunswick are naturally acidic and with the heavy annual rainfall of<br />
120 cm the cobalt content of the soil is decreased by leaching. Outbreaks of cobalt deficiency have occurred in<br />
cattle grazing on pastures on the granite-derived northern tablelands of New South Wales in Australia, and in sheep<br />
grazing pasture on soils derived from weathered rhyolite and ignimbrite, the former being inherently-low in cobalt.<br />
Cobalt deficiency is now-occurring in areas where it has never before been diagnosed, and in seasons of lush<br />
spring and summer pasture growth, cobalt deficiency should be suspected as a cause of unthriftiness. Lambs<br />
grazing cobalt-deficient pastures of the Northern Netherlands are 6.7 times more likely to die if unsupplemented<br />
with cobalt than supplemented lambs (6).<br />
297
Although soils containing less than 0.25 mg/kg cobalt are likely to produce pastures containing insufficient<br />
cobalt, the relationship between levels of cobalt in soil and pasture is not always constant. The factors governing<br />
the relationship have not been determined, although heavy liming is known to reduce the availability of cobalt in<br />
the soil. Manganese appears to have a similar action, but the agricultural significance of the relationship is<br />
unknown.<br />
Ovine white liver disease<br />
A specific hepatic dysfunction of sheep has been described in New Zealand, Australia, the United Kingdom (7),<br />
and Norway (8). It has been called 'white liver disease' because of the grayish color of the liver. Clinically, it is<br />
manifestedby pho-tosensitization when the disease is acute, and anemia and emaciation when the disease is<br />
chronic. It seems likely that the disease is a toxic hepatopathy against which adequate levels of dietary cobalt are<br />
protective (9).<br />
PATHOGENESIS<br />
Cobalt is unique as an essential trace element m ruminant nutrition because it is stored in the body in limited<br />
amounts only and not in all tissues. In the adult ruminant, its only known function is in the rumen and it must,<br />
therefore, be present continuously in the feed.<br />
The effect of cobalt in the rumen is to participate in the production of vitamin Bl2 (cyanocobalamin), and<br />
compared to other species the requirement for vitamin B]2 is very much higher in ruminants. In sheep, the<br />
requirement is of the order of 11ug/day, and probably 500 ug/day arc-produced in the rumen, most being lost in the<br />
process. Animals in the advanced stages of cobalt deficiency are cured by the oral administration of cobalt or by<br />
the parenteral administration of vitamin B12. On cobalt-deficient diets the appearance of signs is accompanied by<br />
a fall of as much as 90% in the vitamin 13,, content of the feces, and on oral dosing with cobalt the signs disappear<br />
and vitamin B12 levels in the feces return to normal. Parenteral administration of cobalt is without appreciable<br />
clinical effect, although some cobalt does enter the alimentary tract in the bile and leads to the formation of a small<br />
amount of cobalamin.<br />
The essential defect in cobalt deficiency in ruminants is an inability to metabolize propionic acid, which is<br />
accompanied by a failure of appetite and death from inanition. The efficiency of cobalt m preventing staggers m<br />
sheep grazing pasture dominated by (Phalaris tuberosa) and possibly by canary grass {Phalaris minor) or rhompa<br />
grass, a hybrid Phalaris spp., is also unexplained. A suggestion that a dietary deficiency of cobalt can lead to the<br />
development of polio-ence phalomalacia appears not to be valid.<br />
The pathogenesis of ovine white liver disease is unclear. It is unknown if the disease is a simple cobalt deficiency,<br />
or a hepatotoxic disease in cobalt/vitamin B12-deficient lambs. Marginal to deficient cobalt-deficient grass is<br />
essential for the development of the disease (8). Cobalt fertilization of deficient pastures results in an increase in<br />
vitamin BP in lambs (9). Hepatic dysfunction occurs in affected sheep (10). Affected lambs generally have higher<br />
serum levels of copper than in cobalt/vitamin B12-supplemented lambs grazing the same pastures (11). Dosing<br />
affected lambs with copper oxide needles resulted in toxic levels of liver copper (12). It is suggested that the<br />
disease is a manifestation of Bl2 deficiency made worse by factors triggering early hepatic fatty change, resulting<br />
in more severe liver damage and loss of intracellular homeo-stasis, rendering the hepatocytes more vulnerable to<br />
other elements such as copper (13). The amount of fructan in the pasture may be an important factor in the<br />
pathogenesis of the lesion (4). One hypothesis suggests that the high level of fructan may initiate hepatic<br />
lipodystrophy, leading to hepatic insufficiency, growth reduction and ovine white liver disease (4). Vitamin B12 is<br />
therapeutic (14).<br />
CLINICAL FINDINGS<br />
No specific signs arc characteristic of cobalt deficiency. A gradual decrease in appetite is the only obvious clinical<br />
sign. It is accompanied by loss of body weight, emaciation and weakness, and these are often observed in the<br />
298
presence of abundant green feed. Pica is likely to occur, especially in cattle. There is marked pallor of the mucous<br />
membranes and affected animals are easily fatigued. Growth, lactation, and wool production are severely retarded,<br />
and the wool may be tender or broken. In sheep, severe lacrimation with profuse outpouring of fluid sufficient to<br />
mat the wool of the face is one of the most important signs in advanced cases. Signs usually become apparent<br />
when animals have been on affected areas for about 6 months and death occurs in 3-12 months after the first<br />
appearance of illness, although severe wasting may be precipitated by the stress of parturition or abortion.<br />
Cobalt deficiency in pregnant ewes can result m decreased lambing percentage, increased percentage of stillbirths,<br />
and increased neonatal mortality (15). Lambs from deficient ewes are slower to start sucking, have reduced<br />
concentrations of serum colostra] immunoglobulins, and have lower serum vitamin BI2 and higher methylmalonic<br />
acid concentrations than lambs from cobalt-adequate dams. CLINICAL PATHOLOGY<br />
Estimation of the cobalt or vitamin B12 content of the liver, as described under necropsy findings, is the most<br />
valuable diagnostic test available. All tests suffer from the disadvantage that tissue cobalt levels will reflect the<br />
cobalt intake for a considerable time prior to the estimation, and animals suffering from acute cobalt deficiency<br />
may be observed to have normal tissue levels of the clement. Estimations of the cobalt content of soils and pasture<br />
have limited value because of the seasonal variations that occur.<br />
299
windblown shell sands to soils derived from pumice and granite. Japanese soils composed largely<br />
of volcanic ash are seriously deficient. A survey in New Brunswick, Canada, revealed the average<br />
value for grass samples was 0.028 mg/kg DM, and for legume samples, 0.088 mg/kg DM, which<br />
300
justifies supplementation of ruminant diets with cobalt. The soils in New Brunswick are naturally<br />
acidic and with the heavy annual rainfall of 120 cm the cobalt content of the soil is decreased by<br />
leaching. Outbreaks of cobalt deficiency have occurred in cattle grazing on pastures on the<br />
granite-derived northern tablelands of New South Wales in Australia, and in sheep grazing pasture<br />
on soils derived from weathered rhyolite and ignimbrite, the former being inherently-low in cobalt.<br />
Cobalt deficiency is now-occurring in areas where it has never before been diagnosed, and in<br />
seasons of lush spring and summer pasture growth, cobalt deficiency should be suspected as a<br />
cause of unthriftiness. Lambs grazing cobalt-deficient pastures of the Northern Netherlands are 6.7<br />
times more likely to die if unsupplemented with cobalt than supplemented lambs (6).<br />
Although soils containing less than 0.25 mg/kg cobalt are likely to produce pastures containing<br />
insufficient cobalt, the relationship between levels of cobalt in soil and pasture is not always<br />
constant. The factors governing the relationship have not been determined, although heavy liming<br />
is known to reduce the availability of cobalt in the soil. Manganese appears to have a similar<br />
action, but the agricultural significance of the relationship is unknown.<br />
Ovine white liver disease<br />
A specific hepatic dysfunction of sheep has been described in New Zealand, Australia, the United<br />
Kingdom (7), and Norway (8). It has been called 'white liver disease' because of the grayish color<br />
of the liver. Clinically, it is manifestedby pho-tosensitization when the disease is acute, and<br />
anemia and emaciation when the disease is chronic. It seems likely that the disease is a toxic<br />
hepatopathy against which adequate levels of dietary cobalt are protective (9).<br />
PATHOGENESIS<br />
Cobalt is unique as an essential trace element m ruminant nutrition because it is stored in the body<br />
in limited amounts only and not in all tissues. In the adult ruminant, its only known function is in<br />
the rumen and it must, therefore, be present continuously in the feed.<br />
The effect of cobalt in the rumen is to participate in the production of vitamin Bl2<br />
(cyanocobalamin), and compared to other species the requirement for vitamin B]2 is very much<br />
higher in ruminants. In sheep, the requirement is of the order of 11ug/day, and probably 500<br />
ug/day arc-produced in the rumen, most being lost in the process. Animals in the advanced stages<br />
of cobalt deficiency are cured by the oral administration of cobalt or by the parenteral<br />
administration of vitamin B12. On cobalt-deficient diets the appearance of signs is accompanied by<br />
a fall of as much as 90% in the vitamin 13,, content of the feces, and on oral dosing with cobalt the<br />
signs disappear and vitamin B12 levels in the feces return to normal. Parenteral administration of<br />
cobalt is without appreciable clinical effect, although some cobalt does enter the alimentary tract<br />
in the bile and leads to the formation of a small amount of cobalamin.<br />
The essential defect in cobalt deficiency in ruminants is an inability to metabolize propionic acid,<br />
which is accompanied by a failure of appetite and death from inanition. The efficiency of cobalt m<br />
preventing staggers m sheep grazing pasture dominated by (Phalaris tuberosa) and possibly by<br />
canary grass {Phalaris minor) or rhompa grass, a hybrid Phalaris spp., is also unexplained. A<br />
suggestion that a dietary deficiency of cobalt can lead to the development of polio-ence<br />
phalomalacia appears not to be valid.<br />
The pathogenesis of ovine white liver disease is unclear. It is unknown if the disease is a simple<br />
cobalt deficiency, or a hepatotoxic disease in cobalt/vitamin B12-deficient lambs. Marginal to<br />
deficient cobalt-deficient grass is essential for the development of the disease (8). Cobalt<br />
fertilization of deficient pastures results in an increase in vitamin BP in lambs (9). Hepatic<br />
301
dysfunction occurs in affected sheep (10). Affected lambs generally have higher serum levels of<br />
copper than in cobalt/vitamin B12-supplemented lambs grazing the same pastures (11). Dosing<br />
affected lambs with copper oxide needles resulted in toxic levels of liver copper (12). It is<br />
suggested that the disease is a manifestation of Bl2 deficiency made worse by factors triggering<br />
early hepatic fatty change, resulting in more severe liver damage and loss of intracellular<br />
homeo-stasis, rendering the hepatocytes more vulnerable to other elements such as copper (13).<br />
The amount of fructan in the pasture may be an important factor in the pathogenesis of the lesion<br />
(4). One hypothesis suggests that the high level of fructan may initiate hepatic lipodystrophy,<br />
leading to hepatic insufficiency, growth reduction and ovine white liver disease (4). Vitamin B12 is<br />
therapeutic (14).<br />
CLINICAL FINDINGS<br />
No specific signs arc characteristic of cobalt deficiency. A gradual decrease in appetite is the only<br />
obvious clinical sign. It is accompanied by loss of body weight, emaciation and weakness, and<br />
these are often observedin the presence of abundant green feed. Pica is likely to occur, especially<br />
in cattle. There is marked pallor of the mucous membranes and affected animals are easily<br />
fatigued. Growth, lactation, and wool production are severely retarded, and the wool may be<br />
tender or broken. In sheep, severe lacrimation with profuse outpouring of fluid sufficient to mat<br />
the wool of the face is one of the most important signs in advanced cases. Signs usually become<br />
apparent when animals have been on affected areas for about 6 months and death occurs in 3-12<br />
months after the first appearance of illness, although severe wasting may be precipitated by the<br />
stress of parturition or abortion.<br />
Cobalt deficiency in pregnant ewes can result m decreased lambing percentage, increased<br />
percentage of stillbirths, and increased neonatal mortality (15). Lambs from deficient ewes are<br />
slower to start sucking, have reduced concentrations of serum colostra] immunoglobulins, and<br />
have lower serum vitamin BI2 and higher methylmalonic acid concentrations than lambs from<br />
cobalt-adequate dams.<br />
CLINICAL PATHOLOGY<br />
Estimation of the cobalt or vitamin B12 content of the liver, as described under necropsy findings,<br />
is the most valuable diagnostic test available. All tests suffer from the disadvantage that tissue<br />
cobalt levels will reflect the cobalt intake for a considerable time prior to the estimation, and<br />
animals suffering from acute cobalt deficiency may be observed to have normal tissue levels of<br />
the clement. Estimations of the cobalt content of soils and pasture have limited value because of<br />
the seasonal variations that occur.<br />
Cobalt concentrations<br />
Cobalt concentrations in the plasma of normal sheep are of the order of 1-3 ug/dL (0.17-0.51<br />
umol/L), and in deficient animals these are reduced to 0.03-0.41 umol/L. Clinical signs of cobalt<br />
deficiency in sheep are associated with serum vitamin B12 levels of less than 0.20 mg/mL, and<br />
serum vitamin B12 levels are used as a laboratory test of cobalt status in animals. Levels of<br />
0.2-0.25 ug/L are indicative of cobalt deficiency. These rise rapidly to 0.5-1.0 ug/L on treatment.<br />
The value of serum vitamin B12 assay as a diagnostic tool is in some doubt, but correctly<br />
interpreted they appear to be worthwhile. Radioassay methods for measuring serum and liver<br />
vitamin B12 in cattle and sheep have now replaced the microbiological assays. Serum vitamin B12<br />
values greater than 0.2 ug/L are indicative of a normal vitamin Bl2 status in cattle. Deprivation of<br />
feed from sheep for 24 hours results in a marked increase in serum vitamin B12. The serum<br />
302
vitamin B12 levels of sheep at pasture are unreliable indicators of liver vitamin B12.<br />
Methylmalonic acid<br />
Because of some of the difficulties with the interpretation of serum vitamin B12 levels, other<br />
biochemical tests, especially methylmalonic acid (MMA) in plasma and urine as diagnostic and<br />
prognostic indicators and formiminoglutamic acid (FIGLU) tests are now used (16). The<br />
determination of MMA has the potential to distinguish between subchmically and clinically<br />
affected animals, which serum vitamin B12, cannot do. Methylmalonic acid is ordinarily<br />
metabolized in ruminants by a vitamin B12 enzyme system. An elevated plasma concentration of<br />
MMA is a comparatively early indicator of functional vitamin B12 deficiency (17). It is<br />
recommended that 10 umol/L be an upper limit of normality for plasma MMA in barley-fed<br />
animals, and 5 umol/L be the upper limit for grass-fed animals (17). A comparison of serum<br />
vitamin Bl2 and serum MMA as diagnostic measures of cobalt status in cattle indicates that =2<br />
umol/L is normal, 2-4 umol/L represents subclinical deficiency, and =4 umol/L reprcsents<br />
deficiency (18). In a cobalt-deficient animal the methylmalonic content of urine is abnormally<br />
high and this has some merit as a test for the presence of the deficiency (9). Cobalt-adequate<br />
lambs have plasma MMA levels of less than 5 umol/L, urinary MMA less than 120 umol/L and<br />
urinary MMA/creatinine values of less than 0.022 umol MMA/mmol of urinary creatinine. An<br />
unequivocal result for methylmalonic acid is a concentration of greater than 30 ug/mL for ten<br />
animals selected randomly from a flock. If the urine is kept for more than 24 hours it should be<br />
acidified to avoid degradation of the methylmalonic acid. Commercial kits are now available for<br />
assay of vitamin B12in ruminant blood.<br />
Formiminoglutamic acid<br />
The concentration of formiminoglutamic acid in urine is a reliable indicator of the cobalt status of<br />
lambs. Levels of 0.08-20 umol/mL in the urine of affected lambs return to zero rapidly after<br />
treatment. However, the concentration of formiminoglutamic acid increases in the urine of lambs<br />
only in the later stages of cobalt deficiency when there is weight loss and ill-thrift. Animals with<br />
subclinical cobalt deficiency do not produce urinary formiminoglutamic acid at levels that would<br />
be useful diagnostically. Neither MMA nor formiminoglutamic acid is a normal constituent of<br />
urine and their presence in urine, without the need for a quantitative measurement, is probably a<br />
positive indication of cobalt deficiency.<br />
Hematology<br />
Affected animals are anemic, but their hemoglobin and erythrocyte levels are often within the<br />
normal range because of an accompanying hemoconcentration. The anemia is normocytic and<br />
normochromic. There is also a decrease in cellularity of the bone marrow in cobalt-deficient sheep.<br />
It is not repaired by the administration of vitamin B12 or by the parenteral administration of cobalt.<br />
Affected animals are also hypoglycemic (less than 60 mg glucose per dL of plasma) and have low<br />
serum alkaline phosphatase levels (less than 20 U/L). The response to cobalt administration is<br />
matched by a very rapid return to normal of these levels. Unfortunately, there are too many other<br />
factors affecting their concentration for them to be of much value in diagnostic work.<br />
NECROPSY FINDINGS<br />
At necropsy, emaciation is extreme. The livers of sheep affected with white liver disease are pale<br />
and fatty. In most cases of cobalt deficiency the spleen is dark due to the accumulation of<br />
hemosiderin. The microscopic changes of ovine white liver disease include hepatocellular<br />
dissociation and intracytoplasmic accumulations of lipid and ceroid-lipofuscin within hepatocytes.<br />
303
The ultrastructural changes of experimentally-induced ovine white liver disease have also been<br />
documented (19).<br />
Biochemical assays reveal very high iron levels in the liver and spleen, and low cobalt levels in<br />
the liver. In normal sheep, cobalt levels in the liver are usually above 0.20 mg/kg DM, but m<br />
affected sheep are typically less than 0.05 mg/kg DM. Liver cobalt levels in cattle fed excessive<br />
amounts of cobalt and thought to be affected by cobalt poisoning can be as high as 69 mg/kg DM.<br />
Normal levels of the vitamin of cattle in New Zealand are 0.70-1.98 mg/kg of liver. After oral<br />
dosing with cobalt, "the level of the element in the liver rises, but returns to the pretreatment level<br />
in 10-30 days. Since serum B]2 levels reflect cobalt status, it is often useful to submit sera from<br />
surviving herdmates when attempting to confirm the diagnosis.<br />
Samples for confirmation of diagnosis<br />
•Toxicology-50 gliver(ASSAY(Co)), 2 mL serum (ASSAY (B12)).<br />
•Histology - formalin-fixed liver (LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
Cobalt deficiency must be differentiated from other causes of ‘ill-thrift' or ‘enzootic marasmus'.<br />
Ill-thrift<br />
In young animals, in which this situation is most often encountered, nutritional deficiencies of<br />
copper, selenium and vitamin D are possible causes of ill-thrift. Lack of total digestible nutrients<br />
is the commonest cause of thin animals, but owners are usually aware of the shortage and do not<br />
present their animals for diagnosis. However, it does happen, especially with urban people who<br />
become farmers and are unaware of the actual<br />
needs of animals. So it is best to check the feed supply and also to check whether or not the<br />
animals have any teeth. These circumstances are seen so commonly in today's era of hobby farms<br />
that a new disease category 'hobby farm malnutrition' is warranted.<br />
304
Internal parasitism<br />
Careful necropsy or fecal examination will determine the degree of helminth infestation, but<br />
cobalt-deficient animals are more susceptible to parasitism and the presence of a heavy parasite<br />
load should not rule out the diagnosis of primary cobalt deficiency. It is also common for parasitic<br />
disease and cobalt deficiency to occur together in the one animal. It is then necessary to make two<br />
diagnoses and conduct two control programs. In sheep, special care is needed to differentiate the<br />
disease from Johne's disease. The differential diagnosis of anemia has been discussed elsewhere<br />
(pp. 416, 1295).<br />
Dietary supplementation response<br />
The most conclusive method of determining if animal production is being affected by the<br />
deficiency of a trace mineral is to measure the response of a production parameter, such as weight<br />
gain, milk production, wool production, or reproductive performance following supplementation<br />
of animals with the element under consideration (20). However, if the degree of response can be<br />
related to a tissue level of the element, or its metabolites, then tissue analyses can replace the need<br />
for field trials, which require considerable expertise and resources and can take several months to<br />
monitor the results and obtain a quantitative outcome.<br />
Growth response curve to supplementation A new approach to defining mineral deficiencies is<br />
based on constructing response curves for any specified level of serum vitamin B12 that can be<br />
used to determine liveweight response to supplementation and the probability of obtaining a<br />
response (20). The technique closely relates the tissue mineral or biochemical indicator with the<br />
degree of production response to treatment. The advantages of this method over the traditional<br />
method have been described (20). The results from published and unpublished cobalt/vitamin B12<br />
weight response trials in young sheep grazing pasture in New Zealand have been reviewed (20).<br />
No significant weight gain responses occurred to vitamin B,? or cobalt treatment in trials with<br />
serum vitamin B12 levels above 500 pmol/L or liver vitamin B12<br />
levels greater than 500 nmol/kg. The fitted response curve approached 0 g/day at 500 pmol/L for<br />
serum vitamin B12 and 375 nmol/kg for liver vitamin B12. The minimum vitamin B12 at which an<br />
economic response to treatment (=10 g/day BW gain) is not likely is 336 pmol/L for serum and<br />
282 nmol/kg for liver (20). Variable responses to cobalt or vitamin B12 include age, breed, sex,<br />
energy intake, concurrent disease, and length of pasture. Higher soil contamination on short<br />
pastures may result in increased cobalt intake and reduced response to vitamin B12 or cobalt.<br />
Serum vitamin B12 levels may also increase following prolonged yarding, and within 24-48 hours<br />
after changes in dietary cobalt.<br />
TREATMENT<br />
Cobalt and vitamin B12<br />
Affected animals respond satisfactorily to oral dosing with cobalt or the IM injection of vitamin<br />
B12. Oral dosing with vitamin B12 is effective, but much larger doses are required. Oral dosing<br />
with cobalt sulfate is usually at the rate of about 1 mg cobalt/day in sheep and can be given in<br />
accumulated doses at the end of each week. Intervals of 2 weeks between dosing are inadequate<br />
for the best possible response. On the other hand, the monthly dosing of lambs with oral doses of<br />
300 mg of cobalt is sufficient greatly to reduce deaths and permit some growth at suboptimal<br />
levels. The response to dosing is very quick, significant elevation of serum vitamin B12 levels<br />
being evident within 24 hours. When large doses of cobalt are administered to some sheep, other<br />
undosed sheep on the same pasture may find sufficient additional cobalt on the pasture from the<br />
305
feces of their Hock-mates to meet their needs. No exact data are available on dose rates for cattle<br />
but ten times the prophylactic rate should be effective. Vitamin B12 should be given in 100-300 ug<br />
doses for lambs and sheep at weekly intervals. Vitamin B12,, therapy is not likely to be used<br />
generally because of the high cost and the comparable effect of oral cobalt administration.<br />
However, vitamin B12 (hydroxycobalainin) may be a suitable therapeutic agent. One injection of 1<br />
mg provides protection to lambs for 14 weeks, and for weaners protection for up to 40 weeks.<br />
Treatment of lambs with ovine white liver disease with hydroxycobalamin results in an immediate<br />
beneficial response and treatment is repeated 10 days later (7).<br />
Cobalt toxicity<br />
Overdosing with cobalt compo inds is unlikely, but toxic signs of loss of weight, rough hair coat,<br />
listlessness, anorexia, and muscular incoordination appear in calves at dose rates of about 40-45<br />
mg of elemental cobalt per 50 kg BW per day. Sheep appear to be much more resistant to the toxic<br />
effects of cobalt than are cattle. Pigs have tolerated up to 200 mg cobalt/kg of diet. At intakes of<br />
400 and 600 mg/kg there is growth depression, anorexia, stiff legs, incoordination, and muscle<br />
tremors. Supplementation of the diet with methionine, or with additional iron, manganese, and<br />
zinc alleviates the toxic effects.<br />
CONTROL<br />
The recommended safe level of cobalt in the diet for sheep and cattle is 0.11 mg cobalt kg/DM<br />
diet. If this is not available, supplementation of the diet with cobalt is necessary. Calves reared on<br />
cobalt-deficient pastures require cobalt or vitamin B12, supplementation prior to weaning. Cobalt<br />
deficiency in grazing animals can be prevented most easily by the top-dressing of affected pasture<br />
with cobalt salts. The amount of top-dressing required will vary with the degree of deficiency.<br />
Recommendations include 400-600 g/ hectare cobalt sulfate annually or 1.2-1.5 kg/hectare every 3<br />
-4 years. The response to pasture treatment is slow, requiring some weeks to complete. Affected<br />
animals should be treated orally or by injection of vitamin B12 to obtain a quick, interim response.<br />
In New Zealand, the requirement for cobalt of ruminants grazing on the pumice soils of the<br />
Central Plateau was established in the 1930s and top-dressing to increase the cobalt intake was<br />
widely practiced for many years. An on-farm survey conducted in 1978-1979 indicated that cobalt<br />
inputs could be halved because adequate reserves of soil cobalt had accumulated. However, the<br />
economic downturn in agriculture resulted in less use of cobalt, and follow-up surveys indicated a<br />
general overall decline in soil and pasture cobalt levels, which was pronounced in areas with a<br />
poor history of cobalt top-dressing. There is now a need to increase the soil level of cobalt to<br />
prevent cobalt<br />
deficiency in grazing ruminants. A regular cobalt input is required to build up reserves. This input<br />
requirement is about 350 g cobalt sulfate/hectare for 7-10 years on the most deficient areas.<br />
Individual farm to farm variation exists within an area and it is necessary to monitor their soil,<br />
pasture, and animal cobalt status. To achieve a level of cobalt of 0.08 mg/kg DM in pasture (the<br />
critical level for sheep) a soil cobalt level of 1.7 and 2.2 mg/kg DM is required for the<br />
yellow-brown pumice soils and yellow-brown loams, respectively (21).<br />
Supplementation of the diet with 0.1 mg cobalt/day for sheep and 0.3-1.0 mg/day for cattle is<br />
required, and can be accomplished by inclusion of the cobalt in salt or a mineral mixture. Cobalt<br />
can also be supplied to cattle in their drinking water supply.<br />
Cobalt-heavy pellet<br />
The use of'heavy pellets' containing 90% cobalt oxide is an alternative means of overcoming the<br />
306
difficulty of maintaining .\n adequate cobalt intake in a deficient area. I he pellet is m the form of<br />
a bolus (5 g for sheep, 20 g for cattle) which, when given by mouth, lodges in the reticulum and<br />
gives off cobalt continuously m very small but adequate amounts. Reports on their use in sheep<br />
and cattle indicate that they are effective. Adminisation of the pellets to lambs and calves less than<br />
2 months old is likely to be ineffective because of failure to retain them in the undeveloped<br />
reticulum. The problem of cobalt deficiency in sucking animals can be overcome in part if the<br />
dams are treated because of the increased vitamin B12 content of their milk, but the daily intake of<br />
the lambs will still be much below the minimal requirement. In about 5% of animals the pellets do<br />
not lodge in the reticulum and approximately 20% are rejected during the year after administration.<br />
If no response occurs, retreatment is advisable. A further possible cause of failure is where pellets<br />
become coated with calcareous material, particularly if the drinking water is highly mineralized or<br />
it pasture top-dressing is heavy. The effects of pellet coating can be overcome by simultaneous<br />
dosing with an abrasive metal pellet. The cost is relatively high and, where top-dressing of<br />
pastures is practiced, addition of cobalt to the fertilizer is the cheaper form of<br />
administration.Pellets are preferred in extensive range-grazing where top-dressing is impracticable<br />
and animals are seen only at infrequent intervals.<br />
Controlled release glass boluses of cobalt<br />
Boluses of controlled release glass containing cobalt are available for oral administration to cattle<br />
and sheep. The boluses are retained in the forestomachs for up to several months and slowly<br />
release cobalt.<br />
Combine cobalt with administration of anthelmintics<br />
Anthelmintics are convenient and efficient vehicles for supplementing the diet with selenium and<br />
cobalt on a regular basis, because both the selenium and cobalt status of lambs decline as they<br />
become dependent on forage, with its adherent nematode larvae, for their nutrients. As a result, the<br />
periods of highest incidence of cobalt and selenium deficiency and helminthiasis coincide. In one<br />
trial, there were lasting responses to selenium but transient, though significant, responses to the<br />
cobalt in the form of increases in plasma vitamin B12, In some trials, the administration of a<br />
monthly bolus of 250 mg cobalt was more effective than the cobalt in the anthelmintic. The<br />
optimum level of cobalt supplementation of an anthelmintic ranges from 20 to 100 mg cobalt per<br />
treatment. When the anthelmintic is given at 3-weekly intervals there may be a cumulative effect.<br />
A comparison of giving 500 ug cyanocobalamin subcutaneously to one group of lambs, with 2.5<br />
mg cobalt orally in an anthelmintic to another group, revealed that even the lowest dose of cobalt<br />
in anthelmintics will be of some nutritional benefit (22).<br />
REFERENCES<br />
(1)McDonald, I. W. (1993) Aust.J. AXr. Res.,44, 347.<br />
(2)Mcc.J. F. & Rogers. P. A. M. (1996) IrishVet.J., 49, 160.<br />
(3)Mee.J. F. & Rogers, P. A. M. (1996) IrishVet.J., 49, 529.<br />
(4)Uvlund, M. J. & Pestalozzi, M. (1990) AdaVet. Scand., 31, 373.<br />
(5) Davits, S. C. ct al. (1993) Ami. Vet.J., 70, 1866.<br />
(6)Vellema, P. ct al. (1997) Vet. Quart., 19,1.<br />
(7)Dannatt, L. & Porter, T. A. (1996) Vet.Rec., 7.!9, 371.<br />
(8)Uvlund. M.J. & Pestaloxzzi, M. (1990)<br />
Acta Vet. Scand., 31. 257.<br />
(9) Uvlund, M.J. (1990) Ada Vet. Scand., 31, 267.<br />
307
(10)Uvlund, M.J. (1990) Acta Vet. Scand., 31,277.<br />
(11)Uvlund, M.J. (1990) Acta Vet. Scand., 31,297.<br />
(12)Uvlund, M.J. (1990) Acta Vet. Scand., 31,287.<br />
(13)Uvlund, M.J. (1990) Ada Vet. Scand., 31,309.<br />
(14)Uvlund, M.J. (1990) Ada Vet. Scand., 31,369.<br />
(15)Fisher, G. E. ik MacPherson, A. (1991)Res. Vet. Set., 50, 319.<br />
(16)McGhie.T. K. (1991)J. Chmmatograph.Biomed. Appi, 566, 215.<br />
(17)O'Harte, F. R M. ct al. (1989) Br.J. Nutr.,62, 729.<br />
(18)Paterson.J. E. & MacPherson, A. (1990)Vet. Rec, 126, 329.<br />
(19)Kennedy, S. et al. (1997) Vet. Hatlwl., 34,575.<br />
(20)Clark, R. Ci. et al. (1989) NZ Vct.J., 37,7.<br />
(21)Hawke, M. F. et al. (1994) Proc. NZGrassland Assoc, 56, 249.<br />
(22)Suttle, N. F. et al. (1990) Vet. Rec, 126,192.<br />
七、碘缺乏症(Iodine Deficiency)<br />
动物缺乏碘,可引起甲状腺肿大,新生畜死亡,脱毛等临床特征。多因饲料中缺乏碘或<br />
因碘的拮抗成分太多引起。碘缺乏症可发生于各种家畜、家禽和人。<br />
【病因】 原发性缺碘,是因饲料中碘含量不足,继发性缺碘,是因饲料中含有拮抗碘<br />
吸收和利用的物质。<br />
世界上许多内陆地区,新生纪大陆,远离海洋,雨水稀少的地区,或虽近海,但雨水太<br />
多,表土流失的地区,可产生碘缺乏症。我国西南、西北、四川、东北大兴安岭、湖北、安<br />
徽某些地区,患地方性甲状腺肿的人数很多。雨水过多的斯里兰卡、印尼、海南岛,也有许<br />
多区域性缺碘。土壤中碘含量不仅和内陆降水量有关,与人群密度关系密切。在人烟稀少的<br />
地区,土壤中缺碘现象明显,动物缺碘现象亦严重。<br />
碘是植物的必需微量元素。碘缺少地区,植物中碘含量减少。不同品种的植物,碘含量<br />
308
不一样。海带中碘含量达 4000~6000mg/kg,普通牧草碘含量仅 0.06~0.5mg/kg,除了沿<br />
海并经常用海藻作为饲料来源的地区外,许多地区如不补充碘则可酿成地区性缺碘。<br />
有些植物中含有碘的拮抗剂,可干扰碘的吸收、利用,称为致甲状腺肿原食物。如硫氰<br />
酸盐,葡萄糖异硫氰酸盐,糖苷花生廿四烯苷,及含氰糖苷等。苞菜、白菜、甘蓝、油菜、<br />
菜籽饼、菜籽粉、花生粉甚至豆粉、芝麻饼、豌豆及白三叶草等,其中甲状腺肿原性物质甲<br />
硫咪唑,甲硫脲含量较高,饲料中上述成分含量较多,容易引起碘缺乏。此称为条件性碘缺<br />
乏症。妊娠母牛饲料中供给含 20%的菜籽粉,新生幼畜死亡率明显增加。<br />
多年生的草地被翻耕后,腐植质中所结合的碘大量流失,降解,使本来已处于临界碘缺<br />
乏的地区,更易产生临床碘缺乏症。酸性土壤,用石灰改造后的土壤,饲料植物中钾离子含<br />
量太高等,可促进碘排泄。促进临床碘缺乏症的发生。<br />
【病理】 碘是动物必需微量元素,身体内的碘 70%~80%集中在甲状腺中。甲状腺中<br />
碘主要用于合成甲状腺素,又称为四碘甲状腺原氨酸和三碘甲状腺原氨酸,是具有生物学活<br />
性的碘化酪氨酸。甲状腺内还有一碘和二碘甲状腺原氨酸及无机碘化物,它们缺乏生物学活<br />
性。甲状腺素的排放是复杂的生物学过程,受下丘脑分泌的促甲状腺释放因子(TRF)和垂<br />
体分泌的促甲状腺素控制。甲状腺释放甲状腺素入血,并分布全身。在缺乏碘的情况下,由<br />
于甲状腺素分泌不足,因而促甲状腺素分泌增多,甲状腺泡增生,目的在于加速甲状腺对碘<br />
的摄取、甲状腺素合成及排放。但因缺乏碘,甲状腺即使增生,仍不能满足动物的需要,因<br />
而促甲状腺素进一步分泌,甲状腺进一步增生的恶性循环,最终致甲状腺肥大。体表触诊即<br />
可感知到肿大的甲状腺,严重时局部听诊可听到“嗡嗡声”的呼吸性杂音。<br />
低浓度的硫氰酸盐,可抑制甲状腺上皮代谢活性,限制腺体对碘的摄取。有些牧草、饲<br />
料性植物,如三叶草、油菜、甘蓝等,其中硫氰酸糖苷含量较高,甲状腺素的合成可受明显<br />
的影响。某些硫氧嘧啶类药物,由于对碘化酶、过氧化酶和脱碘酶有抑制作用,可干扰碘的<br />
代谢,最终导致甲状腺肥大。家畜中除了马驹和其它幼畜有甲状腺增生和肥大现象外,更多<br />
的则是表现生长发育停滞,繁殖机能减退,新生幼畜生命力下降,死亡,幼畜全身脱毛现象。<br />
这些与碘参与体内 100 多种酶的生物学活性有关。<br />
【临床表现】 母马缺碘时,所产驹体质弱,生后不久死亡的比例很高,幼驹被毛生长<br />
正常,生后 3 周左右局部触诊时,甲状腺稍肿大。多数情况下不能独自站立,甚至不能吮乳,<br />
前肢下部过度曲屈,后肢下部过度伸展,中央及第三跗骨钙化缺陷,造成跛行和跗关节变形。<br />
在严重缺碘地区,成年马甲状腺可明显增生,肥大,尤其是纯血品种和轻型马更敏感。<br />
牛缺碘时,成年动物甲状腺肥大现象极少见,主要是新生幼畜甲状腺增生,躯体瘦小,<br />
体质虚弱,如人工辅助其吮乳,几天后可自行恢复,但在恶劣气候条件下出生时。死亡率较<br />
高。有时甲状腺肿大,以至产生呼吸困难,少数犊牛伴有全身或部分脱毛。公牛性欲下降,<br />
母牛乳产量降低,发情现象不明显。流产率、死胎和生后不久死亡发生率增加。<br />
成年羊生活在缺碘地区,甲状腺肿大现象发生率较高,但其它症状不明显;新生羔羊表<br />
现虚弱,广泛脱毛,不能吮乳,呼吸困难。触诊可见甲状腺增大,皮下轻度水肿,四肢弯曲,<br />
站立困难,以至不能站立。山羊症状与绵羊类似,但山羊羔甲状腺肿大和脱毛更明显,脱毛<br />
可分为完全脱落,周身被毛纤化,或外观基本正常三种类型。<br />
猪缺碘所下仔猪全身少毛、无毛,预产期推迟,体质极弱,生后 1~3 天内死亡,并伴有<br />
颈以至全身皮肤粘液水肿,发亮。脱毛现象在四肢最明显,常于生后几小时内死亡。甲状腺<br />
呈暗紫红色肿大现象可能存在,但引起呼吸困难现象者极少。幸存猪生长不良,步样强拘和<br />
腿虚弱。<br />
狗缺碘引起甲状腺分泌不足,症状发展缓慢,开始时动物显得易疲劳,不愿在户外活动,<br />
警犬执行任务时,显得紧张,不能适应长远追捕任务。有的狗奔跑较慢,步样强拘,被毛的<br />
皮肤干燥,污秽,生长缓慢,掉毛,皮肤增厚,特别是眼睛上方额骨处皮肤增厚,上眼睑低<br />
309
垂,面部臃肿。母狗发情不明显,情期甚短,甚至不发情;公狗睾丸缩小,精子缺失。大约<br />
有半数病狗有高胆固醇血症,偶尔可有肌酸磷酸激酶(CPK)活性升高,这可能与胆固醇或<br />
CPK 在体内周转慢有关,血液中甘油脂和脂蛋白含量增加。<br />
鸡缺碘时,羽毛失去光泽,公鸡睾丸缩小,精子缺失。鸡冠缩小,性欲下降;母鸡实验<br />
性切除甲状腺后,产蛋量减少。母鸡对缺碘似乎较能耐受,给予低碘饲料在相当长时间内没<br />
有产蛋减少和孵化率下降现象。有人用低碘饲料饲喂 35 周,而未影响孵化率和胚胎重。<br />
缺碘动物血液中蛋白结合碘常低于 24~40ng/ml 以下,但各品种动物间有明显差异,<br />
乳汁中碘浓度低于 8ng/ml 以下。<br />
剖检可见甲状腺增生、掉毛及颈部粘液性水肿。健康犊牛甲状腺平均重 6.5g,羔羊 2.0g<br />
以下。其中碘含量应占 0.03%以上(约为干重的 0.1%)。镜检可见甲状腺组织增生,皮肤生<br />
毛泡萎缩,骨组织钙化延迟。<br />
【诊断】 临床型甲状腺肿易于诊断。但如仅有新生畜死亡增多,无甲状腺肿胀者易误<br />
诊。主要应根据血液和乳汁中蛋白结合碘(PBI)含量而定,如血液中 PBI 浓度明显低于 24ng<br />
/ml,牛乳中 PBI 低于 8ng/ml,羊乳中低于 80ng/ml,则意味着缺碘。此外缺碘母畜妊<br />
娠期延长,胎儿大多有掉毛现象。这些为诊断碘缺乏症提供了可靠的依据。<br />
测定已死亡的新生畜甲状腺重量有诊断意义,羔羊新鲜甲状腺重在 1.3g 以下为正常,<br />
1.3~2.8g 间为可疑,2.8g 以上为甲状腺肿。腺体中碘的含量在 0.1%以下(干重)者为缺碘。<br />
血清甲状腺素的浓度不太可靠,不仅因甲状腺素浓度有季节性变化,而且受动物年龄、生理<br />
状态及肠道寄生虫等因素的影响。<br />
区别。<br />
诊断中还应与传染性流产、遗传性甲状腺增生和小马的无腺体增生性甲状腺腺区肿大相<br />
【防治】 用含碘的盐砖让动物自由舔食,或者饲料中掺入海藻、海草之类物质,或把<br />
碘掺入矿物质补充剂中,通常将碘化钾或碘酸钾与硬脂酸混合后,掺入饲料或盐砖内,以防<br />
止碘挥发,浓度达 0.01%,有良好的预防碘缺乏的作用。<br />
草原上为提高牧草中碘含量,可在化肥中掺入适量的碘。可用碘酸钠代替碘化钠,但此<br />
法效果并不理想,因为植物对碘的吸收是有限的。用含碘盐砖自由舔食,各个个体之间相差<br />
很多,牧民大多愿意定期喂服碘,即在生后四周,一次给予碘化钾 280mg或 360mg碘酸钾<br />
(KIO3),另一次在妊娠 4 月龄或产羔前 2~3 周时,以同样剂量给母羊一次口服,可较好地<br />
预防新生羔羊死亡。母羊还可在产羔前一次性注射 1ml碘化樱粟花油(含碘 40%)。亦可有<br />
效地防止甲状腺肿和新生羔死亡。亦有人主张在母畜怀孕后期,于饮水中加入 1~2 滴碘酊,<br />
产羔后用 3%碘酊涂擦乳头,让仔畜吮乳时吃进碘,亦有较好的预防作用。<br />
妊娠、泌乳牛饲料中应含 0.8~1.0mg/kg(干重计)碘,空怀牛,犊牛饲料中应含 0.1~0.3mg<br />
/kg 碘,或在肚皮、四肢间,每周一次涂擦碘酊(牛 4ml,猪、羊 2ml),都有较好的防止<br />
缺碘的作用。<br />
通常情况下,动物对碘的需要量是:产乳牛(奶产量在 18kg/日以上)需 400~800µg/日,<br />
干乳期非产乳牛,100~400µg/日,绵羊 50~100µg/日,猪 80~160µg/日,鸡(2~2.5kg)<br />
5~9µg/日。<br />
碘用量过大,亦可引起中毒,张素芳等报道,有用 0.2%碘化钾饮水防止霉菌病而引起<br />
雏鹑急性死亡。多于饮后 10h 出现吃食减少,萎顿、闭目、缩颈、打盹、步态不稳,口腔粘<br />
液增多,拉稀,呼吸困难,阵发性角弓反张。剖检可见,肺水肿,瘀血,气管粘液增多,十<br />
二指肠出血,肝、肾肿大充血。回、盲肠积液,脑轻度水肿。<br />
IODINE DEFICIENCY<br />
Synopsis<br />
310
Etiology. Primary dietary deficiency ofiodine or secondary toconditioning factors such as calcium,<br />
Brassica plants, or bacterial pollution of water. Epidemiology. In all species, most common in<br />
continental land masses. Neonatal animals. Diets of dams deficient in iodine or containing<br />
conditioning factors such as certain plants.<br />
Signs. Goiter as palpable enlargement of thyroid gland. Neonatal mortality due to stillbirths, weak<br />
neonates may not be able to suck and die in few days, alopecia at birth, myxedema. Clinical<br />
pathology. Blood iodine levels.<br />
Lesions. Thyroid enlargement, alopecia, myxedema. Diagnostic confirmation. Goiter and iodine<br />
deficiency.<br />
Differential diagnosis list:<br />
•Weak calf syndrome<br />
•Abortion<br />
•Congenital defects (Chapter 34).<br />
Treatment. Not usually undertaken.<br />
Control. Insure dietatry intake of iodine in pregnant animals<br />
ETIOLOGY<br />
Iodine deficiency may be due to deficient iodine intake or secondarily conditioned by a high<br />
intake of calcium, diets consisting largely of Brasska spp., or gross bacteial pollution of feedstuffs<br />
or drinking water. A continued intake of a low level of cyanogenetic glycosides, e.g. in white<br />
clover, is commonly associated with a high incidence of goitrous offspring. Lmamann, a glycoside<br />
in linseed meal, is the agent producing goiter in newborn lambs born from ewes fed the meal<br />
during pregnancy. A continued intake of the grass Cynodon aethiopicus with low iodine and high<br />
cyanogenetic glucoside contents may cause goiter in lambs. Rapeseed and rapeseed meal are also<br />
goitrogenic.<br />
EPIDEMIOlOGY<br />
311
Occurrence<br />
Goiter caused by iodine deficiency occurs in all of the continental land masses. It is not ot major<br />
economic importance because of the ease of recognition and correction, but if neglected may<br />
cause heavy mortalities in newborn animals. The most common cause of iodine deficiency in<br />
farm animals is the failure to provide iodine in the diet. The sporadic occurrence of the disease<br />
in marginal areas attracts most attention. An epi-demiological survey in Germany found up to<br />
10% of cattle and sheep farms, and 15% of swine herds were affected with iodine deficiency,<br />
which were both primary and secondary due to the presence of nitrates, thiocyanates or<br />
glucosinolates in the diet (1).<br />
The importance of subclinical iodine deficiency as a cause of neonatal mortality could be much<br />
greater than clinical disease. For example, in southern Australia ewes supplemented with iodine<br />
by the single injection of iodine in oil, have had less mortality in the lambs, have grown larger<br />
lambs, or performed the same as controls.<br />
Young animals are more likely to bear goitrous offspring than older ones and this may account<br />
for the apparent breed susceptibility of Dorset Horn sheep, which mate at an earlier age than other<br />
breeds.<br />
A simple deficiency of iodine in the diet and drinking water may occur and is related to<br />
geographical circumstances. Areas where the soil iodine is not replenished by cyclical accessions<br />
of oceanic iodine include large continental land masses and coastal areas where prevailing winds<br />
are offshore. In such areas, iodine deficiency is most likely to occur where rainfall is heavy and<br />
soil iodine is continually depleted by leaching. Soil formations rich in calcium or lacking in humus<br />
are also likely to be relatively deficient in iodine. The ability of soil to retain iodine under<br />
conditions of heavy rainfall is directly related to their humus content, and limestone soils arc, in<br />
general, low in organic matter. A high dietary intake of calcium also decreases intestinal<br />
absorption of iodine, and in some areas heavy applications of lime to pasture are followed by the<br />
development of goiter in lambs. This factor may also be important in areas where drinking water<br />
is heavily mineralized.<br />
Risk factors<br />
Dietary and environmental factors<br />
There are several situations in which the relationship between iodine intake and the occurrence of<br />
goiter is not readily apparent. Goiter may occur on pasture containing adequate iodine; it is then<br />
usually ascribed to a secondary or conditioned iodine deficiency. A diet rich in plants of the<br />
Brassica spp., including cabbages and brussels sprouts, may cause simple goiter and<br />
hypothyroidism in rabbits, which is preventable by administered iodine. Hypothyroidism has also<br />
been produced in rats by feeding rape-seed, and in mice by feeding rapeseed oil meal, heeding<br />
large quantities of kale to pregnant ewes causes a high incidence of goiter and hypothyroidism,<br />
also pre¬ventable by administering iodine in the newborn lambs. The goitrogenic substance in<br />
these plants is probably a glu-cosinolate capable of producing thiocyanate in the rumen. The<br />
thio-cyanate content, or potential content, varies between varieties of kale, being much less in<br />
rape-kale, which also does not show the two-fold increase in thiocyanate content other varieties<br />
show in autumn. Small young leaves contain up to five times as much thiocyanate as large, fully<br />
formed leaves. Some of these plants are excellent sources of feed, and in some areas it is probably<br />
economical to continue feeding them, provided suitable measures are taken to prevent goiter in the<br />
newborn. Although kale also causes mild goiter in weaned lambs this does not appear to reduce<br />
312
their rate of gain.<br />
A diet high in linseed meal (20% of ration) given to pregnant ewes may result in a high<br />
incidence of goitrous lambs, which is preventable with iodine or thyroxine. Under experimental<br />
conditions, groundnuts are goitrogenic for rats, the goitrogenic substance being a<br />
glyco-side-arachidoside. The goitrogenic effect is inhibited by supplementation of the diet with<br />
small amounts of iodine. Soybean byproducts are also considered to be goitrogenic. Gross<br />
bacterial contamination of drinking water by sewage is a cause of goiter in humans in countries<br />
where hygiene is poor. There is a record of a severe outbreak of goitrous calves from cattle<br />
running on pasture heavily dressed with crude sewage. Prophylactic dosing of the cows with<br />
potassium iodide prevented further cases. Feeding sewage sludge is also linked to the occurrence<br />
of goiter.<br />
Goiter in lambs may occur when permanent pasture is plowed and resown. This may be due to<br />
the sudden loss of decomposition and leaching of iodine-binding humus in soils of marginal iodine<br />
content. In subsequent years the disease may not appear. There may be some relation between this<br />
occurrence of goiter and the known variation in the iodine content of particular plant species,<br />
especially if new pasture species are sown when the pasture is plowed. The maximum iodine<br />
content of some plants is controlled by a strongly inherited factor and is independent of soil type<br />
or season. Thus, in the same pasture, perennial rye grass may contain 146 µg iodine per 100 g dry<br />
matter (DM) and Yorkshire for grass only 7µg/100 g DM. Because goiter has occurred in lambs<br />
when the ewes are on a diet containing less than 30 µg iodine per 100 g DM, the importance of<br />
particular plant species becomes apparent. A high incidence of goiter associated with heavy<br />
mortality has been observed in the new¬born lambs of ewes grazing on pasture dominated by<br />
white clover and by subterranean clover and perennial ryegrass.<br />
Congenital goiter has been observed in foals born to mares on low iodine intake, but also to<br />
mares fed an excessive amount of iodine during pregnancy.<br />
313
PATHOGENESIS<br />
Iodine deficiency results in a decreased production of thyroxine and stimulation of the secretion of<br />
thyrotropic hormone by the pituitary gland. This commonly results in hypcrplasia of thyroid tissue<br />
and a considerable enlargement of the gland. Most cases of goiter of the newborn are of this type.<br />
The primary deficiency of thyroxine is responsible for the severe weakness and hair abnormality<br />
of the affected animals. Although the defect is described as hairlessness, it is truly hypoplasia of<br />
the hairs, with many very slender hairs present and a concurrent absence and diminution in size of<br />
hair follicles. A hyperplastic goiter is highly vascular and the gland can be felt to pulsate with the<br />
arterial pulse and a loud murmur may be audible over the gland. Colloid goiter is less common in<br />
animals and probably represents an involutional stage after primary hyperplasia.<br />
Other factors, particularly the ingestion of low levels of cyanide, exert their effects by inhibiting<br />
the metabolic activity of the thyroid epithelium and restricting the uptake of iodine. Thiocyanates<br />
and sulfocyanates are formed during the process of detoxication of cyanide in the liver and these<br />
substances have a pronounced depressing effect on iodine uptake by the thyroid. Some pasture and<br />
fodder plants, including white clover, rape and kale, are known to have a moderate content of<br />
cyanogenetic glucosides. These goitro-genic substances may appear in the milk and provide a<br />
toxic hazard to both animals and man. The inherited form in cattle is due to the increased activity<br />
of an enzyme that deiodinatesiodotyrosines so rapidly that the formation of thyroxine is inhibited.<br />
Iodine is an essential element for normal fetal brain and physical development in sheep. A<br />
severe iodine deficiency in pregnant ewes causes reduction in fetal brain and body weight from 70<br />
days of gestation to parturition. The effects are mediated by a combination of maternal and fetal<br />
hypothyroidism, the effect of maternal hypothyroidism being earlier than the onset of fetal thyroid<br />
secretion (2). There is also evidence of fetal hypothyroidisms, and absence of wool growth and<br />
delayed skeletal maturation near parturition.<br />
CLINICAL FINDINGS<br />
Although loss of condition, decreased milk production, and weakness might be anticipated these<br />
signs are not usually observed in adults. Loss of libido in the bull, failure to express estrus in the<br />
cow, and a high incidence of aborted, stillborn or weak calves have been suggested as<br />
manifestations of hypothyroidism m cattle, whereas prolonged gestation is reported in mares, ewes,<br />
and sows.<br />
A high incidence of stillbirths and weak, newborn animals is the most common manifestation<br />
of iodine deficiency. Partial or complete alopecia and palpable enlargement of the thyroid gland<br />
are other signs that occur with varying frequency in the different species. Affected foals have a<br />
normal hair coat and little thyroid enlargement, but are very weak at birth. In most cases they are<br />
unable to stand without support and many are too weak to suck. Excessive flexion of the lower<br />
forelegs and extension of lower parts of the hindlegs has also been observed in affected foals.<br />
Defective ossification has also been reported, the manifestation is collapse of the central and third<br />
tarsal bones leading to lameness and deformity of the hock. Enlargement of the thyroid also occurs<br />
commonly in adult horses in affected areas, Thoroughbreds and light horses being more<br />
susceptible than draft animals.<br />
In cattle, the incidence of thyroid enlargement in adults is much lower than in horses and the<br />
cardinal manifestations are gross enlargement of the thyroid gland and weakness in newborn<br />
calves. If they are assisted to suck for a few days, recovery is usual, but if they are born on the<br />
range during inclement weather many will die. In some instances, the thyroid gland is sufficiently<br />
314
large to cause obstruction to respiration. Partial alopecia is a rare accompaniment.<br />
In pigs, the characteristic findings are birth of hairless, stillborn or weak piglets often with<br />
myxedema of the skin of the neck. The hairlessness is most marked on the limbs. Most affected<br />
piglets die within a few hours of birth. Thyroid enlargement may be present but is never<br />
sufficiently great to cause visible swelling in the live pig. Survivors arc-lethargic, do not grow<br />
well, have a waddling gait and leg weaknesses due to weakness of ligaments and joints.<br />
Adult sheep in iodine-deficient areas may show a high incidence of thyroid enlargement but are<br />
clinically normal in other respects. Newborn lambs manifest weakness, extensive alopecia and<br />
palpble, if not visible, enlargement of the thyroid glands. Goats present a similar clinical picture,<br />
except that all abnormalities are more severe than in lambs. Goat kids are goitrous and alopecic.<br />
The degree of alopecia varies from complete absence of hair, through very fine hair, to hair that is<br />
almost normal.<br />
Animals surviving the initial danger period after birth may recover, except for partial<br />
persistence of the goiter. The glands may pulsate with the normal arterial pulse and may extend<br />
down a greater part of the neck and cause some local edema. Auscultation and palpation of the<br />
jugular furrow may reveal the presence of a murmur and thrill, the 'thyroid thrill', due to the<br />
increased arterial blood supply of the glands.<br />
Experimental hypothyroidism produced in horses by surgical excision of the gland results in a<br />
syndrome of poor growth, cold sensitivity, long, dull hair coat, docility, lethargy, edema of<br />
hindlimbs and a coarse, thick appearance of the face. The rectal temperature is depressed and<br />
blood cholesterol levels are high. Administration of thyroprotein reverses the syndrome.<br />
CLINICAL PATHOLOGY<br />
Estimations of iodine levels in the blood and milk are reliable indicators of the thyroxine status of<br />
the animal. Organic or protein-bound iodine is estimated in serum or plasma and used as an index<br />
of circulating thyroid hormone, provided access to exogenous iodine in the diet, or as treatment, is<br />
adequately controlled. There may be between-breed differences in blood iodine levels but levels of<br />
2.4-14 µg of protein-bound iodine per 100 mL of plasma appear to be in the normal range. In ewes,<br />
an iodine concentration in milk of below 8 µg/L indicates a state of iodine deficiency.<br />
Levels of thyroxine in the blood have not been much used to measure thyroid gland sufficiency<br />
in animals. Work in ewes has shown that normal lambs at birth have twice the serum thyroxine<br />
levels of their dams, but goitrous lambs have levels less than those of their dams. However, low<br />
mean thyroxine levels (50 nmol/L is normal) are not a definitive indication of iodine deficiency<br />
because of the variety of factors affecting thyroxine levels. These levels fall rapidly soon after<br />
birth and approximate the dam's levels at 5-6 weeks of age.<br />
Bloodcholesterollevelshavebeen<br />
used as an indicator of thyroid function in humans but are not used in the investigation of goiter in<br />
animals.<br />
In determining the iodine status of an area, iodine levels in soil and pasture should be obtained<br />
but the relationship between these levels, and between them and the status of the grazing animal,<br />
may be complicated by conditioning factors.<br />
315
NECROPSY FINDINGS<br />
Macroscopic thyroid enlargement, alopecia and myxedema may be evident. The weights of<br />
thyroid glands have diagnostic value. In full-term normal calves the average fresh weight is 6.5g,<br />
in lambs 2g is average. The iodine content of the thyroid will also give some indication of the<br />
iodine status of the animal. At birth a level of 0.03% of iodine on a wet weight basis (0.1% on dry<br />
weight) can be considered to be the critical level in cattle and sheep. On histological examination,<br />
hyperplasia of the glandular epithelium may be seen. The hair follicles will be found to be<br />
hypoplastic. Delayed osseous maturation, manifested by absence of centers of ossification, is also<br />
apparent in goitrous newborn lambs.<br />
Samples for confirmation of diagnosis<br />
•Toxicology - 1 thyroid gland (ASSAY(Iodine))<br />
•Histology - skin, thyroid (LM).<br />
DIFFERENTIAL DIAGNOSIS<br />
Iodine deficiency is easily diagnosed if goiter is present but the occurrence of stillbirths without<br />
obvious goiter may be confusing. Abortion due to infectious agents in cattle and sheep must be<br />
considered in these circumstances. In stillbirths due to iodine deficiency, gestation is usually<br />
prolonged beyond the normal period, although this may be difficult to determine in animals bred<br />
at pasture. Inherited defects of thyroid hormone synthesis are listed under the heading of inherited<br />
diseases. Hyperplastic goiter without gland enlargement has been observed in newborn foals in<br />
which rupture of the common digital extensor tendons, forelimb contracture, and mandibular<br />
prognathism also occur. The cause of the combination of defects in unknown.<br />
TREATMENT<br />
316
Treatment of neonates with obvious clinical evidence of iodine deficiency is usually not<br />
undertaken because of the high case fatality rate. When outbreaks of iodine deficiency occur in<br />
neonates, the emphasis is usually on providing additional iodine to the pregnant dams. The<br />
recommendations for control can be adapted to the treatment of affected animals.<br />
CONTROL<br />
The recommended dietary intake of iodine for cattle is 0.8-1.0 mg/kg DM of feed for lactating and<br />
pregnant cows, and 0.1-0.3 mg/kg DM of feed for non-pregnant cows and calves.<br />
Iodine can be provided in salt or a mineral mixture. The loss of iodine from salt blocks may be<br />
appreciable and an iodine preparation that is stable but contains sufficient available iodine is<br />
required. Potassium iodate satisfies these requirements and should be provided as 200 mg of<br />
potassium iodate per kg of salt. Potassium iodide alone is unsuitable, but when mixed with<br />
calcium stearate (8% of the stearate in potassium iodide) it is suitable for addition to salt - 200<br />
mg/kg of salt.<br />
Individual dosing of pregnant ewes, on two occasions during the 4th and 5th months of<br />
pregnancy, with 280 mg potassium iodide or 370 mg potassium iodate has been found to be<br />
effective in the prevention of goiter in lambs when the ewes are on a heavy diet of kale. For<br />
individual animals, weekly application of tincture of iodine (4 mL cattle, 2 mL pig and sheep) to<br />
the inside of the flank is also an effective preventive. The iodine can also be administered as an<br />
injection in poppy seed oil (containing 40% bound iodine): 1 mL given IM 7-9 weeks before<br />
lambing is sufficient to prevent severe goiter and neonatal mortality in the lambs. Control of goiter<br />
can be achieved for up to 2 years. The gestation period is also reduced to normal. A similar<br />
injection 3-5 weeks before lambing is less efficient.<br />
A device to release iodine slowly into the forestomachs, while still retaining its position there,<br />
has given good results in preventing congenital goiter in lambs when fed to ewes during late<br />
pregnancy.<br />
REFERENCES<br />
(1)Korber, R. al. (1985) Mh Vet. Med., 40,220.<br />
(2)Hetzel, B. S. & Mano, M. T. (1989) J. Nutr.,119, 145.<br />
317