Clinical Practice Guideline Medulloblastoma - Alberta Health Services
Clinical Practice Guideline Medulloblastoma - Alberta Health Services
Clinical Practice Guideline Medulloblastoma - Alberta Health Services
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
MEDULLOBLASTOMA<br />
Date Developed: August, 2010<br />
CLINICAL PRACTICE GUIDELINE CNS-008<br />
The recommendations contained in this guideline are a consensus of the <strong>Alberta</strong> Provincial CNS Tumour Team<br />
synthesis of currently accepted approaches to management, derived from a review of relevant scientific literature.<br />
Clinicians applying these guidelines should, in consultation with the patient, use independent medical judgment in<br />
the context of individual clinical circumstances to direct care.
BACKGROUND<br />
CLINICAL PRACTICE GUIDELINE CNS-008<br />
<strong>Medulloblastoma</strong> is the most common brain tumour in children, accounting for 15 to 30 percent of all<br />
pediatric cancers of the central nervous system (CNS); in adults, however, the tumour is quite rare,<br />
accounting for only one to three percent of all primary brain tumours. 1-3 Because of it’s rarity in the adult<br />
population, most published reports in adults with medulloblastoma involve limited and select populations,<br />
and are retrospective analyses conducted over several decades with varying diagnostic procedures and<br />
treatment protocols. Based on the assumption that adult tumours have the same properties as those in<br />
children, adult patients with medulloblastoma are often given treatment protocols according to therapies<br />
developed for children with similarly staged disease at diagnosis. 4,5 However, important histologic and<br />
phenotypic differences have been identified between pediatric and adult medulloblastoma patients. In<br />
addition, radiologic differences have also been identified: adult tumours involve the lateral cerebellar<br />
hemispheres, while pediatric tumours most often occur in the vermis. 6-7 Further, late relapse, which occurs<br />
only rarely in pediatric tumours, occurs more frequently among adult patients with medulloblastoma.<br />
Reported survival rates for adult medulloblastoma vary in the literature. In a recent large, multicentre<br />
study, Padovani et al. retrospectively reviewed the outcomes of 253 adult patients treated for<br />
medulloblastoma between 1975 and 2004, and reported five- and ten-year overall survival rates of 72 and<br />
55 percent, respectively. 6 When low- and high-risk patients were compared, the ten-year overall survival<br />
rates were 62 and 49 percent (p=0.03). 7 Lower five-year survival rates were reported in an unselected,<br />
population-based study published by Roldán et al. 8 In this study, the <strong>Alberta</strong> Cancer Registry database<br />
was used to identify all cases of medulloblastoma occurring in Southern <strong>Alberta</strong> during a 21 year period,<br />
and five-year survival rates were reported to be 44.1 percent for patients over the age of sixteen, and 55.7<br />
percent for those under the age of sixteen. 8 The authors reported that these rates were more in line with<br />
those of other population-based studies. In addition, the survival curves in this analysis did not “level off”,<br />
suggesting that the patients had a lifetime risk of recurrence. 8 A recent analysis of 454 patients in the<br />
Surveillance, Epidemiology, and End Results (SEER) database in the United States reported five- and tenyears<br />
survival rates of 64.9 and 52.1 percent, respectively, for adult patients diagnosed with<br />
medulloblastoma between 1973 and 2004. 9 Multivariate analysis identified that diagnosis after the 1980s,<br />
age of diagnosis before 20 years, gross total resection, and treatment with radiotherapy were all<br />
associated with better survival. 9<br />
The most commonly reported symptoms of medulloblastoma at initial diagnosis are associated with<br />
increased intracranial pressure and cerebellar dysfunction. In the Roldán et al. study, headache (80%),<br />
nausea and vomiting (78%), and ataxia (73%) were most commonly identified; 8 similar symptoms and<br />
rates have been reported in retrospective series from France, India, and the MD Anderson Cancer Center<br />
in the United States. 4,10,11<br />
GUIDELINE QUESTIONS<br />
What is the optimal management strategy for adult patients with medulloblastoma?
DEVELOPMENT<br />
CLINICAL PRACTICE GUIDELINE CNS-008<br />
This guideline was reviewed and endorsed by the <strong>Alberta</strong> Provincial CNS Tumour Team. Members of the<br />
<strong>Alberta</strong> Provincial CNS Tumour Team include medical oncologists, radiation oncologists, surgical<br />
oncologists, neurosurgeons, nurses, neuropathologists, and pharmacists. Evidence was selected and<br />
reviewed by a working group comprised of members from the <strong>Alberta</strong> Provincial CNS Tumour Team and a<br />
Knowledge Management Specialist from the <strong>Guideline</strong> Utilization Resource Unit. A detailed description of<br />
the methodology followed during the guideline development process can be found in the <strong>Guideline</strong><br />
Utilization Resource Unit Handbook.<br />
SEARCH STRATEGY<br />
Medical journal articles were searched using the Medline (1950 to March Week 4, 2010), EMBASE (1980<br />
to March Week 4, 2010), Cochrane Database of Systematic Reviews (1 st Quarter, 2010), and PubMed<br />
electronic databases; the references and bibliographies of articles identified through these searches were<br />
scanned for additional sources. The MeSH heading <strong>Medulloblastoma</strong> was combined with the search terms<br />
“Surgery”, “Radiotherapy”, “Drug Therapy”, “Therapy”, and “Follow-up Studies”. The results were limited to<br />
adults, practice guidelines, systematic reviews, meta-analyses, comparative studies, multicentre studies,<br />
randomized controlled trials, and clinical trials. Articles were excluded from the review if they: addressed<br />
medulloblastoma in pediatric or adolescent patients, had a non-English abstract, were not available<br />
through the library system, or were case studies involving less than 5 patients. A review of the relevant<br />
existing practice guidelines for medulloblastoma was also conducted by accessing the practice guidelines<br />
on the websites of the British Columbia Cancer Agency (BCCA) and the National Cancer Institute (NCI).<br />
TARGET POPULATION<br />
The recommendations outlined in this guideline apply to adults over the age of 18 years diagnosed with<br />
medulloblastoma. Different principles may apply to pediatric patients.<br />
RECOMMENDATIONS<br />
Evaluation and Workup:<br />
1. Evaluation and management of adult patients with medulloblastoma should be discussed and planned<br />
within a multidisciplinary tumour team. Whenever possible, participation in a clinical trial is<br />
encouraged.<br />
2. The initial workup should include cerebrospinal fluid (CSF) cytology if safe, and an MRI of the brain<br />
and total spine, given the risk of seeding throughout the craniospinal axis.<br />
Treatment:<br />
3. Maximal safe surgical resection followed by postoperative radiotherapy and possibly adjuvant<br />
chemotherapy is the recommended treatment algorithm for adult patients with medulloblastoma. An<br />
attempt should be made to excise as much as possible of the grossly visible tumour.<br />
4. Postoperative radiotherapy to the entire craniospinal axis to a dose of 36-40Gy, followed by a posterior<br />
fossa boost to 54-55.8Gy should be administered. Sites of gross disease elsewhere in the craniospinal<br />
axis should be boosted to at least 40Gy. Concurrent chemotherapy may allow for use of lower<br />
craniospinal radiation doses of 23.4Gy.
CLINICAL PRACTICE GUIDELINE CNS-008<br />
5. In contrast to childhood medulloblastoma, the role of chemotherapy in adult patients with<br />
medulloblastoma is less clear. Based on extrapolation from the pediatric literature, however, adjuvant<br />
chemotherapy may be considered for adults with high-risk disease, and also for the treatment of<br />
recurrence. There is currently no strong evidence to support a specific chemotherapy regimen in<br />
adults.<br />
Follow-up:<br />
6. Long term follow-up (5 to 10 years) is recommended following completion of therapy, due to the<br />
potential for late recurrence, as well as neurocognitive, neuroendocrine, thyroid, pulmonary, cardiac,<br />
gastrointestinal, renal, and reproductive late effects.<br />
DISCUSSION<br />
Evaluation and Workup<br />
Combined modality therapy, including surgery, radiotherapy, and possibly chemotherapy is the standard of<br />
care for both children and adult patients with medulloblastoma. Therefore, evaluation and management<br />
should be discussed and planned with a multidisciplinary team of clinicians. Whenever possible, patient<br />
participation in a clinical trial is encouraged (recommendation #1).<br />
Prior to initiating therapy, an MRI of the brain and total spine is recommended, as this is an important tool<br />
for accurate staging of the tumour, particularly when the tumour extends beyond the posterior fossa and<br />
into the spinal spaces. 12,13 Postoperative neuro-imaging with MRI will help to quantify residual disease,<br />
and is recommended within 72 hours to two weeks following surgical resection. 12-14 <strong>Medulloblastoma</strong><br />
tumours in adult patients are associated with a high likelihood for craniospinal seeding and spread through<br />
the cerebrospinal fluid (CSF). Therefore, when safe to do so, the workup of adult patients should include<br />
CSF cytology (recommendation #2). 15<br />
Staging and Classification<br />
Historically, medulloblastoma has been clinically staged according to the Chang staging definitions for<br />
tumour and metastases parameters, described in Table 1. 16<br />
Table 1. Chang Staging System for <strong>Medulloblastoma</strong> 16<br />
Tumour Classification Description<br />
T1 greatest tumour dimension 3cm<br />
T3a greatest tumour dimension >3cm with spread into the aqueduct of Sylvius and/or foramen of<br />
Luschka, cerebral subarachnoid space, third or lateral ventricles<br />
T3b greatest tumour dimension >3cm with unequivocal spread into the brainstem; for T3b, surgical<br />
staging may be used in the absence of involvement at imaging<br />
T4 greatest tumour dimension >3cm with spread beyond the aqueduct of Sylvius and/or the foramen<br />
magnum<br />
Metastasis Classification Description<br />
M0 no evidence of gross subarachnoid or hematogenous metastasis<br />
M1 microscopic tumour cells in cerebrospinal fluid<br />
M2 gross nodular seeding in cerebellum<br />
M3 gross nodular seeding in spinal subarachnoid space<br />
M4 metastasis beyond cerebrospinal axis
CLINICAL PRACTICE GUIDELINE CNS-008<br />
More recently, low- and high-risk classification has been identified to be an important factor in treatment<br />
decisions as well as a prognostic indicator in several studies. 5,6,17 Low-risk patients are those that have T1,<br />
T2, T3a and M0 disease, and have totally or near totally resected disease (< 1.5 cm 2 ) following surgery. In<br />
contrast, high-risk patients are those that have T3b or T4 and M1 to M3 disease, and do have<br />
postoperative residual tumours. 5<br />
Histology<br />
<strong>Medulloblastoma</strong> is described as malignant and invasive, and is classified by the World <strong>Health</strong><br />
Organization (WHO) as a grade IV tumour. 18 In addition to the classic type of medulloblastoma, four<br />
histologic subtypes have also been identified (desmoplastic/nodular type, medulloblastoma with extensive<br />
nodularity, anaplastic medulloblastoma, large-cell medulloblastoma), and recent publications stress the<br />
importance of these histologic subtypes in the prognosis of medulloblastoma. 18 In general, the large-cell<br />
and anaplastic subtypes appear to be associated with the worst prognosis. 19<br />
Standard histologic reporting for medulloblastoma includes documentation of tumour necrosis, mitoses,<br />
apoptosis, cell size, nuclear wrapping, nodularity, and large cell and anaplastic distribution.<br />
Immunohistochemical tests, such as those for expression or mutation of p53, INI 1, Her2/neu, and βcatenin,<br />
may also be required for determining prognosis and ruling out medulloblastoma mimics. 19,20 Other<br />
specialized molecular tests, including those for MYC-C and MYC-N amplification, and loss of chromosome<br />
17p, may allow a more accurate prediction of disease prognosis, 19-22 but are not considered standard tests<br />
in <strong>Alberta</strong> at the present time.<br />
Treatment<br />
Surgery. Maximal safe surgical resection followed by postoperative radiotherapy and possibly adjuvant<br />
chemotherapy is the recommended treatment strategy for adult patients with medulloblastoma<br />
(recommendation #3). An attempt should be made to excise as much as possible of grossly visible<br />
tumour, as several studies have correlated outcome with the extent of resection and the amount of<br />
residual tumour. 3,6,8,9,23,24 In a retrospective review of 32 adult patients with medulloblastoma confined to<br />
the craniospinal axis, Chan et al. reported that the five year disease-free survival rate was significantly<br />
better for patients who underwent complete total resection versus a less than complete resection (89% vs.<br />
27%; RR=10.9, 95% CI 2.73-80.8; p
CLINICAL PRACTICE GUIDELINE CNS-008<br />
The authors also reported a trend to longer event-free survival for doses higher than 50Gy to the posterior<br />
fossa (p=0.09). In the series reported by Padovani et al., a spinal radiation dose greater than 30Gy and a<br />
posterior fossa radiation dose greater than 50Gy both correlated significantly with overall survival<br />
(p=0.0054 and p
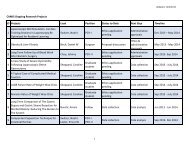
Study N Median<br />
Age (yrs)<br />
Abacioglu et<br />
al., 2002 39<br />
30 27 N=10 high-risk patients: varying combinations<br />
of procarbazine + CCNU + vincristine<br />
Greenberg et<br />
al., 2001 40<br />
Kunschner et<br />
al., 2001 4<br />
Chan et al.,<br />
2000 23<br />
Le et al.,<br />
1997 25<br />
Prados et al.,<br />
1995 17<br />
Carrie et al.,<br />
1994 3<br />
Chemotherapy Regimen(s) Outcomes<br />
17 23 N=10: weekly vincristine followed by cisplatin<br />
+ CCNU + vincristine (Packer protocol)<br />
N=7: cisplatin/etoposide alternating with<br />
vincristine/ cyclophosphamide (POG protocol)<br />
28 30.5 N=1: thioguanine + procarbazine +<br />
dibromodulcitol + CCNU + vincristine<br />
N=4: cyclophosphamide + etoposide +<br />
cisplatin<br />
N=1: methotrexate + nitrogen mustard +<br />
vincristine + prednisone + procarbazine<br />
32 25.5 N=16: cisplatin + vincristine<br />
N=4: cisplatin + vincristine +<br />
cyclophosphamide + etoposide<br />
N=1: cisplatin + vincristine +<br />
cyclophosphamide<br />
N=1: cisplatin + vincristine + etoposide<br />
N=1: vincristine + CCNU<br />
34 23 N=12: procarbazine + hydroxyurea<br />
N=5: cisplatin + CCNU + vincristine<br />
N=2: CCNU + vincristine + procarbazine +<br />
hydroxyurea<br />
N=2: thioguanine + procarbazine +<br />
dibromodulcitol + CCNU + vincristine<br />
N=1: CCNU + hydroxyurea<br />
N=1: cytarabine<br />
47 28 N=11 low-risk patients: procarbazine +<br />
hydroxyurea (+ CCNU in one patient)<br />
N=21 high-risk patients: nitrosourea-based<br />
combination chemotherapy<br />
156 28 N=31: vincristine + BCNU + procarbazine +<br />
hydroxyurea + cisplatin + cytarabine +<br />
methotrexate<br />
N=29: vincristine + CCNU or BCNU<br />
N=9: ifosfamide + cisplatin + vincristine<br />
N=6: other protocols<br />
CLINICAL PRACTICE GUIDELINE CNS-008<br />
5-year OS rate = 65%; 8-year OS rate = 51%<br />
5-year DFS rate = 69% CT versus 60% no<br />
CT (p=not significant)<br />
Median OS = 36 months Packer protocol<br />
versus 57 months POG protocol (p=0.058)<br />
Toxicity during Packer protocol treatment was<br />
moderately severe<br />
No significant difference in OS demonstrated<br />
between the patients treated with CT versus<br />
no CT<br />
5-year OS rate = 83%; 8-year OS rate = 45%<br />
The use of CT was adversely associated with<br />
rate of posterior fossa control (p=0.03)<br />
Patients who received CT presented with<br />
more advanced M-stage than patients treated<br />
with RT alone<br />
5-year OS rate = 58%<br />
No effect of CT on survival or posterior fossa<br />
control<br />
5-year OS rates = 81% low-risk patients<br />
versus 54% high-risk patients (p=0.03)<br />
Treatment with adjuvant CT associated with<br />
longer survival (p=0.03)<br />
Lack of adjuvant CT associated with shorter<br />
time to tumour progression (p=0.05)<br />
5-year OS rate = 66% CT versus 57% no CT<br />
(p=not significant)<br />
10-year OS rate = 52% CT versus 43% no<br />
CT (p=not significant)<br />
No significant difference in survival between<br />
different CT regimens<br />
CT appeared to be much more toxic in this<br />
adult series than in children<br />
Abbreviations: CCNU=lomustine, OS=overall survival, CT=chemotherapy, RT=radiotherapy, RR=relative risk, CI=confidence interval, DFS=disease-free<br />
survival, POG=Pediatric Oncology Group, BCNU=carmustine.<br />
Prospective randomized studies are required to more definitively address whether primary adjuvant<br />
chemotherapy is effective in the treatment of adults with medulloblastoma. At the present time, it seems<br />
reasonable to treat high-risk adult patients with the chemotherapy protocols which have been shown to be<br />
effective through randomized clinical trials in the pediatric population. Decisions should be made on an<br />
individual basis for each patient, and should be discussed and planned at multidisciplinary tumour board<br />
meetings.
CLINICAL PRACTICE GUIDELINE CNS-008<br />
Future directions. Several recent studies have shown that salvage therapy with combination<br />
chemotherapy may be of benefit in adults with recurrent medulloblastoma. 4,10 The use of temozolomide as<br />
an alternative to some of the older chemotherapy regimens has also recently shown favourable results<br />
with improved efficacy and reduced adverse effects in adult patients with both newly diagnosed and<br />
recurrent medulloblastoma. 41-43 Another approach is combination chemotherapy after radiotherapy with a<br />
reduced craniospinal axis dose (23.4Gy), or radiotherapy plus concurrent vincristine. 26,44<br />
Follow-up<br />
In their population-based review of adult patients with medulloblastoma in <strong>Alberta</strong>, Roldán et al. reported a<br />
50 percent survival rate at five years, and noted that the estimated survival curves did not level off,<br />
suggesting that these patients have a lifetime risk of tumour recurrence, and should not be considered<br />
“cured”. 8 Late relapses in adult patients with medulloblastoma have also been documented in several<br />
other studies. Chan et al. reported that 59 percent of all recurrences in their series occurred more than two<br />
years after completion of treatment, and 29 percent occurred more than five years after the completion of<br />
treatment. 23 Riffaud et al. reported a recurrences rate of 41 percent, with a median time to first recurrence<br />
of 4.2 years (range 0.7–18 years). 10 Similarly, in the only prospective study published to date, Brandes et<br />
al. reported that the risk of recurrence increased markedly after seven years of follow-up for low-risk adult<br />
patients, and after ten years for high-risk adult patients. 5<br />
Due to the potential for late recurrences, the <strong>Alberta</strong> CNS Tumour Team members recommend a minimum<br />
of five to ten years of follow-up for adult patients with medulloblastoma (recommendation #6). In particular,<br />
monitoring and surveillance should be focused on neurocognitive, neuroendocrine, thyroid, pulmonary,<br />
cardiac, gastrointestinal, renal, and reproductive system late effects. 14 An MRI of the brain and full spine<br />
with gadolinium enhancement should be obtained every three to six months for the first two years of<br />
follow-up, and every year thereafter. The final discharge of the patient to their family physician will be at<br />
the discretion of the treating oncologist.<br />
GLOSSARY OF ABBREVIATIONS<br />
Acronym Description<br />
BCNU carmustine<br />
CCNU lomustine<br />
CI confidence interval<br />
CNS central nervous system<br />
CSF cerebrospinal fluid<br />
CT chemotherapy<br />
DFS disease-free survival<br />
Gy gray<br />
MRI magnetic resonance imaging<br />
OS overall survival<br />
POG Pediatric Oncology Group<br />
RR relative risk<br />
RT radiotherapy<br />
SEER Surveillance, Epidemiology, and End Results database<br />
WHO World <strong>Health</strong> Organization
DISSEMINATION<br />
CLINICAL PRACTICE GUIDELINE CNS-008<br />
Present and review the guideline at the local and provincial tumour team meetings and weekly rounds.<br />
Post the guideline on the <strong>Alberta</strong> <strong>Health</strong> <strong>Services</strong> website.<br />
Send an electronic notification of the new guideline to all members of <strong>Alberta</strong> <strong>Health</strong> <strong>Services</strong>, Cancer<br />
Care.<br />
MAINTENANCE<br />
A formal review of the guideline will be conducted at the next Annual Provincial Meeting in October 2011.<br />
If critical new evidence is brought forward before that time, however, the guideline working group<br />
members will revise and update the document accordingly.<br />
CONFLICT OF INTEREST<br />
Participation of members of the <strong>Alberta</strong> Provincial CNS Tumour Team in the development of this guideline<br />
has been voluntary and the authors have not been remunerated for their contributions. There was no<br />
direct industry involvement in the development or dissemination of this guideline. <strong>Alberta</strong> <strong>Health</strong> <strong>Services</strong><br />
– Cancer Care recognizes that although industry support of research, education and other areas is<br />
necessary in order to advance patient care, such support may lead to potential conflicts of interest. Some<br />
members of the <strong>Alberta</strong> Provincial CNS Tumour Team are involved in research funded by industry or have<br />
other such potential conflicts of interest. However the developers of this guideline are satisfied it was<br />
developed in an unbiased manner.<br />
REFERENCES<br />
1. Brandes AA, Paris MK. Review of the prognostic factors in medulloblastoma of children and adults. Crit Rev Oncol Hematol<br />
2004;5:121-8.<br />
2. Bloom HJG, Bessel EM. <strong>Medulloblastoma</strong> in adults: a review of 47 patients treated between 1952 and 1981. Int J Radiat<br />
Oncol Biol Phys 1990 Apr;18(4):763-72.<br />
3. Carrie C, Lasset C, Alapetite C, Haie-Meder C, Hoffstetter S, Demaille MC, et al. Multivariate analysis of prognostic factors in<br />
adult patients with medulloblastoma: retrospective study of 156 patients. Cancer 1994 Oct;74(8):2352-60.<br />
4. Kunschner LJ, Kuttesch J, Hess K, Yung WKA. Survival and recurrence factors in adult medulloblastoma: the MD Anderson<br />
Cancer Center experience from 1978 to 1998. Neuro Oncol 2001 Jul;3(3):167-73.<br />
5. Brandes AA, Franceschi E, Tosoni A, Blatt V, Ermani M. Long-term results of a prospective study on the treatment of<br />
medulloblastoma in adults. Cancer 2007 Nov;110(9):2035-41.<br />
6. Padovani L, Sunyach MP, Perol D, Mercier C, Alapetite C, Haie-Meder C, et al. Common strategy for adult and pediatric<br />
medulloblastoma: a multicenter series of 253 adults. Int J Radiat Oncol Biol Phys 2007 Jun;68(2):433-40.<br />
7. Giordana MT, Cavalla P, Dutto A, Borsotti L, Chiò A, Schiffer D. Is medulloblastoma the same tumor in children and adults? J<br />
Neurooncol 1997 Nov;35(2):169-76.<br />
8. Roldán G, Brasher P, Vecil G, Senger D, Rewcastle B, Cairncross G, et al. Population-based study of medulloblastoma:<br />
outcomes in <strong>Alberta</strong> from 1975 to 1996. Can J Neurol Sci 2008 May;35(2):210-5.<br />
9. Lai R. Survival of patients with adult medulloblastoma. A population-based study. Cancer 2008 Apr;112(7):1568-74.<br />
10. Riffaud L, Saikali S, Leray E, Hamlat A, Haegelen C, Vauleon E, et al. Survival and prognostic factors in a series of adults<br />
with medulloblastomas. J Neurosurg 2009 Sep;111(3):478-87.<br />
11. Lal P, Nagar YS, Kumar S, Singh S, Das KJM, Narayan SL, et al. <strong>Medulloblastoma</strong>s: clinical profile, treatment techniques and<br />
outcome – an institutional experience. Indian J Cancer 2002 Jul-Sept;39(3):97-105.<br />
12. Brandes AA, Palmisano V, Monfardini S. <strong>Medulloblastoma</strong> in adults: clinical characteristics and treatment. Cancer Treat Rev<br />
1999 Feb;25(1):3-12.<br />
13. Eisenstat DD. <strong>Clinical</strong> management of medulloblastoma in adults. Expert Rev Anticancer Ther 2004;4(5):795-802.<br />
14. Merchant TE, Pollack IF, Loeffler JS. Brain tumors across the age spectrum: biology, therapy, and late effects. Semin Radiat<br />
Oncol 2010 Jan;20(1):58-66.
CLINICAL PRACTICE GUIDELINE CNS-008<br />
15. Gajjar A, Fouladi M, Walter AW, Thompson SJ, Reardon DA, Merchant TE, et al. Comparison of lumbar and shunt<br />
cerebrospinal fluid specimens for cytologic detection of leptomeningeal disease in pediatric patients with brain tumors. J Clin<br />
Oncol 1999 Jun;17(6):1825-8.<br />
16. Chang CH, Housepian EM, Herbert C Jr. An operative staging system and a megavoltage radiotherapeutic technic for<br />
cerebellar medulloblastomas. Radiology 1969 Dec;93(6):1351-9.<br />
17. Prados MD, Warnick RE, Wara WM, Larson DA, Lamborn K, Wilson CB. <strong>Medulloblastoma</strong> in adults. Int J Radiat Oncol Biol<br />
Phys 1995 Jul;32(4):1145-52.<br />
18. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the<br />
central nervous system. Acta Neuropathol 2007 Aug;114(2):97-109.<br />
19. Gulino A, Arcella A, Giangaspero F. Pathological and molecular heterogeneity of medulloblastoma. Curr Opin Oncol 2008<br />
Nov;20(6):668-75.<br />
20. Pizer BL, Clifford SC. The potential impact of tumour biology on improved clinical practice for medulloblastoma: progress<br />
towards biologically driven clinical trials. Br J Neurosurg 2009 Aug;23(4):364-75.<br />
21. Korshunov A, Remke M, Werft W, Benner A, Ryzhova M, Witt H, et al. Adult and pediatric medulloblastomas are genetically<br />
distinct and require different algorithms for molecular risk stratification. J Clin Oncol 2010 Jun;28(18):3054-60.<br />
22. Lamont JM, McManamy CS, Pearson AD, Clifford SC, Ellison DW. Combined histopathological and molecular cytogenetic<br />
stratification of medulloblastoma patients. Clin Cancer Res 2004 Aug;10(16):5482-93.<br />
23. Chan AW, Tarbell NJ, Black PM, Louis DN, Frosch MP, Ancukiewicz M, et al. Adult medulloblastoma: prognostic factors and<br />
patterns of relapse. Neurosurgery 2000 Sep;47(3):623-31.<br />
24. del Charco JO, Bolek TW, McCollough WM, Maria BL, Kedar A, Braylan RC, et al. <strong>Medulloblastoma</strong>: time-dose relationship<br />
based on a 30-year review. Int J Radiat Oncol Biol Phys. 1998 Aug;42(1):147-54.<br />
25. Le QT, Weil MD, Wara WM, Lamborn KR, Prados MD, Edwards MS, et al. Adult medulloblastoma: an analysis of survival and<br />
prognostic factors. Cancer J Sci Am 1997 Jul-Aug;3(4):238-45.<br />
26. Douglas JG, Barker JL, Ellenbogen RG, Geyer JR. Concurrent chemotherapy and reduced-dose cranial spinal irradiation<br />
followed by conformal posterior fossa tumor bed boost for average-risk medulloblastoma: efficacy and patterns of failure. Int J<br />
Radiat Oncol Biol Phys 2004 Mar;58(4):1161-4.<br />
27. Duetsch M, Thomas PRM, Krischer J, Boyett JM, Albright L, Aronin P, et al. Results of a prospective randomized trial<br />
comparing standard dose neuraxis irradiation (36,000 cGy/20) with reduced neuraxis irradiation (2,340 cGy/13) in patients<br />
with low-stage medulloblastoma. A Combined Children's Cancer Group-Pediatric Oncology Group Study. Pediatr Neurosurg<br />
1996;24(4):167-77.<br />
28. Spiegler BJ, Bouffet E, Greenberg ML, Rutka JT, Mabbott DJ. Change in neurocognitive functioning after treatment with<br />
cranial irradiation in childhood. J Clin Oncol 2004 Feb;22(4):706-13.<br />
29. Merchant TE, Kun LE, Krasin MJ, Jones-Wallace D, Chintagumpala MM, Woo SY, et al. A multi-institution prospective trial of<br />
reduced-dose craniospinal irradiation (23.4 Gy) followed by conformal posterior fossa (36 Gy) and primary-site irradiation<br />
(55.8 Gy) and dose-intensive chemotherapy for average-risk medulloblastoma. Int J Radiat Oncol Biol Phys 2003;57(2 Suppl<br />
1):S194-5.<br />
30. Smee RI, Williams JR. <strong>Medulloblastoma</strong>s – primitive neuroectodermal tumours in the adult population. J Med Imag Radiat<br />
Oncol 2008 Feb;52(1):72-6.<br />
31. Evans AE, Jenkin RD, Sposto R, Ortega JA, Wilson CB, Wara W, et al. The treatment of medulloblastoma. Results of a<br />
prospective randomized trial of radiation therapy with and without CCNU, vincristine, and prednisone. J Neurosurg 1990<br />
Apr;72(4):572-82.<br />
32. Tait DM, Thornton-Jones H, Bloom HJ, Lemerle J, Morris-Jones P. Adjuvant chemotherapy for medulloblastoma: the first<br />
multi-centre control trial of the International Society of Paediatric Oncology (SIOP I). Eur J Cancer 1990 Apr;26(4):464-9.<br />
33. Packer RJ, Sutton LN, Elterman R, Lange B, Goldwein J, Nicholson HS, et al. Outcome for children with medulloblastoma<br />
treated with radiation and cisplatin, CCNU, and vincristine chemotherapy. J Neurosurg 1994 Nov;81(5):690-8.<br />
34. Zeltzer PM, Boyett JM, Finlay JL, Albright AL, Rorke LB, Milstein JM, et al. Metastasis stage, adjuvant treatment, and residual<br />
tumor are prognostic factors for medulloblastoma in children: conclusions from the Children's Cancer Group 921 randomized<br />
phase III study. J Clin Oncol 1999 Mar;17(3):832-45.<br />
35. Packer RJ, Gajjar A, Vezina G, Rorke-Adams L, Burger PC, Robertson PL, et al. Phase III study of craniospinal radiation<br />
therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol 2006<br />
Sep;24(25):4202-8.<br />
36. Ang C, Hauerstock D, Guiot MC, Kasymjanova G, Roberge D, Kavan P, et al. Characteristics and outcomes of<br />
medulloblastoma in adults. Pediatr Blood Cancer 2008 Nov;51(5):603-7.<br />
37. Ertas G, Ucer AR, Altundag MB, Durmus S, Calikoglu T, Ozbagi K, et al. <strong>Medulloblastoma</strong>/primitive neuroectodermal tumor in<br />
adults: prognostic factors and treatment results: a single-center experience from Turkey. Med Oncol. 2008;25(1):69-72.<br />
38. Herrlinger U, Steinbrecher A, Rieger J, Hau P, Kortmann RD, Meyermann R, et al. Adult medulloblastoma: prognostic factors<br />
and response to therapy at diagnosis and at relapse. J Neurol 2005 Mar;252(3):291-9.
CLINICAL PRACTICE GUIDELINE CNS-008<br />
39. Abacioglu U, Uzel O, Sengoz M, Turkan S, Ober A. <strong>Medulloblastoma</strong> in adults: treatment results and prognostic factors. Int J<br />
Radiat Oncol Biol Phys 2002 Nov;54(3):855-60.<br />
40. Greenberg HS, Chamberlain MC, Glantz MJ, Wang S. Adult medulloblastoma: multiagent chemotherapy. Neuro Oncol 2001<br />
Jan;3(1):29-34.<br />
41. Nicholson HS, Kretschmar CS, Krailo M, Bernstein M, Kadota R, Fort D, et al. Phase 2 study of temozolomide in children and<br />
adolescents with recurrent central nervous system tumors: a report from the Children's Oncology Group. Cancer 2007<br />
Oct;110(7):1542-50.<br />
42. Durando X, Thivat E, Gilliot O, Irthum B, Verrelle P, Vincent C, et al. Temozolomide treatment of an adult with a relapsing<br />
medulloblastoma. Cancer Investigation 2007 Sept;25(6):470-5.<br />
43. Hongeng S, Visudtibhan A, Dhanachai M, Laothamatus J, Chiamchanya S. Treatment of leptomeningeal relapse of<br />
medulloblastoma with temozolomide. J Pediatr Hematol Oncol 2002 Oct;24(7):591-3.<br />
44. Nieder C, Mehta MP, Jalali R. Combined radio- and chemotherapy of brain tumours in adult patients. Clin Oncol (R Coll<br />
Radiol) 2009 Sep;21(7):515-24.