Surgery and Healing in the Developing World - Dartmouth-Hitchcock
Surgery and Healing in the Developing World - Dartmouth-Hitchcock Surgery and Healing in the Developing World - Dartmouth-Hitchcock
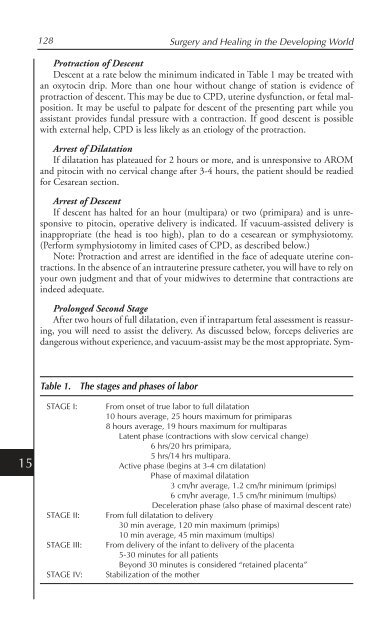
15 128 Surgery and Healing in the Developing World Protraction of Descent Descent at a rate below the minimum indicated in Table 1 may be treated with an oxytocin drip. More than one hour without change of station is evidence of protraction of descent. This may be due to CPD, uterine dysfunction, or fetal malposition. It may be useful to palpate for descent of the presenting part while you assistant provides fundal pressure with a contraction. If good descent is possible with external help, CPD is less likely as an etiology of the protraction. Arrest of Dilatation If dilatation has plateaued for 2 hours or more, and is unresponsive to AROM and pitocin with no cervical change after 3-4 hours, the patient should be readied for Cesarean section. Arrest of Descent If descent has halted for an hour (multipara) or two (primipara) and is unresponsive to pitocin, operative delivery is indicated. If vacuum-assisted delivery is inappropriate (the head is too high), plan to do a cesearean or symphysiotomy. (Perform symphysiotomy in limited cases of CPD, as described below.) Note: Protraction and arrest are identified in the face of adequate uterine contractions. In the absence of an intrauterine pressure catheter, you will have to rely on your own judgment and that of your midwives to determine that contractions are indeed adequate. Prolonged Second Stage After two hours of full dilatation, even if intrapartum fetal assessment is reassuring, you will need to assist the delivery. As discussed below, forceps deliveries are dangerous without experience, and vacuum-assist may be the most appropriate. Sym- Table 1. The stages and phases of labor STAGE I: From onset of true labor to full dilatation 10 hours average, 25 hours maximum for primiparas 8 hours average, 19 hours maximum for multiparas Latent phase (contractions with slow cervical change) 6 hrs/20 hrs primipara, 5 hrs/14 hrs multipara. Active phase (begins at 3-4 cm dilatation) Phase of maximal dilatation 3 cm/hr average, 1.2 cm/hr minimum (primips) 6 cm/hr average, 1.5 cm/hr minimum (multips) Deceleration phase (also phase of maximal descent rate) STAGE II: From full dilatation to delivery 30 min average, 120 min maximum (primips) 10 min average, 45 min maximum (multips) STAGE III: From delivery of the infant to delivery of the placenta 5-30 minutes for all patients Beyond 30 minutes is considered “retained placenta” STAGE IV: Stabilization of the mother
Basic Obstetrics and Obstetric Surgery in a Mission Setting 129 physiotomy may be appropriate if the cause is clearly mild CPD. In the face of failed vacuum-assist or severe CPD, you must go to Cesarean section. Shoulder Dystocia By definition, shoulder dystocia is the failure of the shoulders to deliver spontaneously after delivery of the head. This is a true obstetric emergency. It may occur in from 1-5% of deliveries and is very unpredictable. Anticipate dystocia in cases of known fetal macrosomia or maternal diabetes. Begin to suspect a developing dystocia in cases of prolonged second stage labor. In all cases, your patient should begin her delivery with an empty bladder. Recognize dystocia when the head is delivered (with or without difficulty) and the ring of vulvar tissue then appears to form a snug collar around the neck of the fetus. The head appears to be held tightly against the vulva and/or appears to retract (the “turtle sign”). The usual amount of gentle downward traction will not disimpact the anterior shoulder, which is stuck behind the pubic symphysis. You or your assistant should begin to count time upon delivery of the head. If you encounter the “turtle sign” or encounter difficulty delivering the anterior shoulder within the first 30 seconds, declare a dystocia. Do this without conveying a sense of panic to your patient. Your assistants should have been drilled in the responses that you will now direct. Your next actions will depend upon whether or not you anticipated the dystocia (in cases of fetal macrosomia and/or maternal diabetes), and upon whether or not the patient has received epidural anesthesia. A suggested sequence would be as follows: 1. At 30 seconds, if the shoulders are not delivered with ease or a “turtle sign” is encountered, inform your assistants that you are managing a dystocia. DO NOT employ fundal pressure, DO NOT increase your traction on the head and neck of the fetus. 2. Evaluate the need for an episiotomy, which may be helpful if there is a component of perineal resistance as well. Try to accomplish delivery with the next uterine contraction using the following maneuvers. 3. McRobert’s maneuver: Your assistants should immediately see that the patient’s hips are sharply flexed into an exaggerated lithotomy position - help her to grasp her legs and pull her knees towards her chest. Maintain your grasp of the baby’s head and watch and feel for any signs of spontaneous restitution. 4. Suprapubic pressure: Simultaneous with the maneuver above, the assistant standing on that side of the patient where the fetal spine is thought to lie should deliver suprapubic pressure in an oblique and cephalad direction, attempting to disengage the impacted shoulder from the symphysis pubis while you continue to apply gentle downward traction on the head and neck. 5. If unable to deliver with McRobert’s maneuver and suprapubic pressure, turn the patient from the supine lithotomy position to assume a hands-and-knees position (Gaskin’s maneuver). In this case, DO NOT allow her hips to flex sharply. Redirect your traction appropriately to lift the anterior shoulder away from the symphysis and deliver the fetus. (It would also be reasonable to employ Gaskin’s maneuver as your first intervention, especially in cases where you have anticipated a dystocia, rather than discovered one intrapartum.) 15
- Page 94 and 95: 10 78 Surgery and Healing in the De
- Page 96 and 97: 10 80 Surgery and Healing in the De
- Page 98 and 99: 10 82 Surgery and Healing in the De
- Page 100 and 101: 10 84 Surgery and Healing in the De
- Page 102 and 103: 10 86 Surgery and Healing in the De
- Page 104 and 105: 11 88 Surgery and Healing in the De
- Page 106 and 107: 11 90 Surgery and Healing in the De
- Page 108 and 109: CHAPTER 12 Communication in the Thi
- Page 110 and 111: 12 94 Surgery and Healing in the De
- Page 112 and 113: 12 96 Surgery and Healing in the De
- Page 114 and 115: CHAPTER 13 Anesthesia in the Third
- Page 116 and 117: 13 100 Surgery and Healing in the D
- Page 118 and 119: 13 102 Surgery and Healing in the D
- Page 120 and 121: 13 104 Surgery and Healing in the D
- Page 122 and 123: 13 106 Surgery and Healing in the D
- Page 124 and 125: 13 108 Surgery and Healing in the D
- Page 126 and 127: 14 110 Surgery and Healing in the D
- Page 128 and 129: 14 112 Surgery and Healing in the D
- Page 130 and 131: 14 114 Surgery and Healing in the D
- Page 132 and 133: 14 116 Surgery and Healing in the D
- Page 134 and 135: CHAPTER 15 Basic Obstetrics and Obs
- Page 136 and 137: 15 120 Surgery and Healing in the D
- Page 138 and 139: 15 122 Surgery and Healing in the D
- Page 140 and 141: 15 124 Surgery and Healing in the D
- Page 142 and 143: 15 126 Surgery and Healing in the D
- Page 146 and 147: 15 130 Surgery and Healing in the D
- Page 148 and 149: 15 132 Surgery and Healing in the D
- Page 150 and 151: 15 134 Surgery and Healing in the D
- Page 152 and 153: 15 136 Surgery and Healing in the D
- Page 154 and 155: 15 138 Surgery and Healing in the D
- Page 156 and 157: 15 140 Surgery and Healing in the D
- Page 158 and 159: 15 142 Surgery and Healing in the D
- Page 160 and 161: CHAPTER 16 Pointers for American Su
- Page 162 and 163: 16 146 Surgery and Healing in the D
- Page 164 and 165: 16 148 Surgery and Healing in the D
- Page 166 and 167: 16 150 Surgery and Healing in the D
- Page 168 and 169: 16 152 Surgery and Healing in the D
- Page 170 and 171: 17 154 Surgery and Healing in the D
- Page 172 and 173: 17 156 Surgery and Healing in the D
- Page 174 and 175: 17 158 Surgery and Healing in the D
- Page 176 and 177: 17 160 Surgery and Healing in the D
- Page 178 and 179: 17 162 Surgery and Healing in the D
- Page 180 and 181: 17 164 Surgery and Healing in the D
- Page 182 and 183: 17 166 Surgery and Healing in the D
- Page 184 and 185: 18 168 Surgery and Healing in the D
- Page 186 and 187: 18 170 Surgery and Healing in the D
- Page 188 and 189: 18 172 Surgery and Healing in the D
- Page 190 and 191: 18 174 Surgery and Healing in the D
- Page 192 and 193: 18 176 Surgery and Healing in the D
15<br />
128 <strong>Surgery</strong> <strong>and</strong> <strong>Heal<strong>in</strong>g</strong> <strong>in</strong> <strong>the</strong> Develop<strong>in</strong>g <strong>World</strong><br />
Protraction of Descent<br />
Descent at a rate below <strong>the</strong> m<strong>in</strong>imum <strong>in</strong>dicated <strong>in</strong> Table 1 may be treated with<br />
an oxytoc<strong>in</strong> drip. More than one hour without change of station is evidence of<br />
protraction of descent. This may be due to CPD, uter<strong>in</strong>e dysfunction, or fetal malposition.<br />
It may be useful to palpate for descent of <strong>the</strong> present<strong>in</strong>g part while you<br />
assistant provides fundal pressure with a contraction. If good descent is possible<br />
with external help, CPD is less likely as an etiology of <strong>the</strong> protraction.<br />
Arrest of Dilatation<br />
If dilatation has plateaued for 2 hours or more, <strong>and</strong> is unresponsive to AROM<br />
<strong>and</strong> pitoc<strong>in</strong> with no cervical change after 3-4 hours, <strong>the</strong> patient should be readied<br />
for Cesarean section.<br />
Arrest of Descent<br />
If descent has halted for an hour (multipara) or two (primipara) <strong>and</strong> is unresponsive<br />
to pitoc<strong>in</strong>, operative delivery is <strong>in</strong>dicated. If vacuum-assisted delivery is<br />
<strong>in</strong>appropriate (<strong>the</strong> head is too high), plan to do a cesearean or symphysiotomy.<br />
(Perform symphysiotomy <strong>in</strong> limited cases of CPD, as described below.)<br />
Note: Protraction <strong>and</strong> arrest are identified <strong>in</strong> <strong>the</strong> face of adequate uter<strong>in</strong>e contractions.<br />
In <strong>the</strong> absence of an <strong>in</strong>trauter<strong>in</strong>e pressure ca<strong>the</strong>ter, you will have to rely on<br />
your own judgment <strong>and</strong> that of your midwives to determ<strong>in</strong>e that contractions are<br />
<strong>in</strong>deed adequate.<br />
Prolonged Second Stage<br />
After two hours of full dilatation, even if <strong>in</strong>trapartum fetal assessment is reassur<strong>in</strong>g,<br />
you will need to assist <strong>the</strong> delivery. As discussed below, forceps deliveries are<br />
dangerous without experience, <strong>and</strong> vacuum-assist may be <strong>the</strong> most appropriate. Sym-<br />
Table 1. The stages <strong>and</strong> phases of labor<br />
STAGE I: From onset of true labor to full dilatation<br />
10 hours average, 25 hours maximum for primiparas<br />
8 hours average, 19 hours maximum for multiparas<br />
Latent phase (contractions with slow cervical change)<br />
6 hrs/20 hrs primipara,<br />
5 hrs/14 hrs multipara.<br />
Active phase (beg<strong>in</strong>s at 3-4 cm dilatation)<br />
Phase of maximal dilatation<br />
3 cm/hr average, 1.2 cm/hr m<strong>in</strong>imum (primips)<br />
6 cm/hr average, 1.5 cm/hr m<strong>in</strong>imum (multips)<br />
Deceleration phase (also phase of maximal descent rate)<br />
STAGE II: From full dilatation to delivery<br />
30 m<strong>in</strong> average, 120 m<strong>in</strong> maximum (primips)<br />
10 m<strong>in</strong> average, 45 m<strong>in</strong> maximum (multips)<br />
STAGE III: From delivery of <strong>the</strong> <strong>in</strong>fant to delivery of <strong>the</strong> placenta<br />
5-30 m<strong>in</strong>utes for all patients<br />
Beyond 30 m<strong>in</strong>utes is considered “reta<strong>in</strong>ed placenta”<br />
STAGE IV: Stabilization of <strong>the</strong> mo<strong>the</strong>r