January 2006 HCPCS Special Bulletin, No. 193 - TMHP.com
January 2006 HCPCS Special Bulletin, No. 193 - TMHP.com January 2006 HCPCS Special Bulletin, No. 193 - TMHP.com
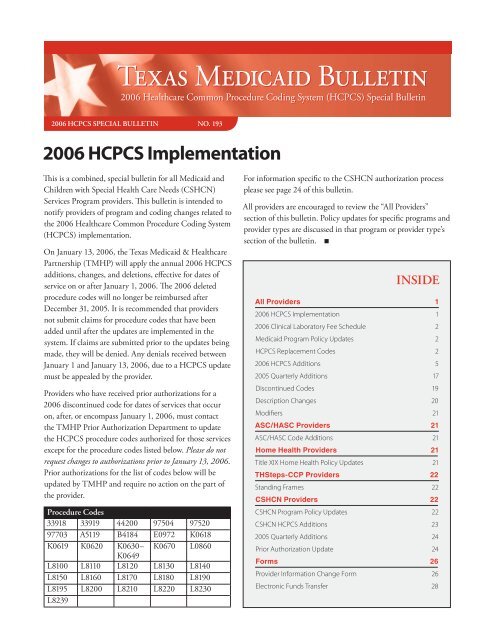
T EXAS MEDICAID BULLETIN 2006 Healthcare Common Procedure Coding System (HCPCS) Special Bulletin 2006 HCPCS SPECIAL BULLETIN NO. 193 2006 HCPCS Implementation This is a combined, special bulletin for all Medicaid and Children with Special Health Care Needs (CSHCN) Services Program providers. This bulletin is intended to notify providers of program and coding changes related to the 2006 Healthcare Common Procedure Coding System (HCPCS) implementation. On January 13, 2006, the Texas Medicaid & Healthcare Partnership (TMHP) will apply the annual 2006 HCPCS additions, changes, and deletions, effective for dates of service on or after January 1, 2006. The 2006 deleted procedure codes will no longer be reimbursed after December 31, 2005. It is recommended that providers not submit claims for procedure codes that have been added until after the updates are implemented in the system. If claims are submitted prior to the updates being made, they will be denied. Any denials received between January 1 and January 13, 2006, due to a HCPCS update must be appealed by the provider. Providers who have received prior authorizations for a 2006 discontinued code for dates of services that occur on, after, or encompass January 1, 2006, must contact the TMHP Prior Authorization Department to update the HCPCS procedure codes authorized for those services except for the procedure codes listed below. Please do not request changes to authorizations prior to January 13, 2006. Prior authorizations for the list of codes below will be updated by TMHP and require no action on the part of the provider. Procedure Codes 33918 33919 44200 97504 97520 97703 A5119 B4184 E0972 K0618 K0619 K0620 K0630– K0670 L0860 K0649 L8100 L8110 L8120 L8130 L8140 L8150 L8160 L8170 L8180 L8190 L8195 L8200 L8210 L8220 L8230 L8239 For information specific to the CSHCN authorization process please see page 24 of this bulletin. All providers are encouraged to review the “All Providers” section of this bulletin. Policy updates for specific programs and provider types are discussed in that program or provider type’s section of the bulletin. INSIDE All Providers 1 2006 HCPCS Implementation 1 2006 Clinical Laboratory Fee Schedule 2 Medicaid Program Policy Updates 2 HCPCS Replacement Codes 2 2006 HCPCS Additions 5 2005 Quarterly Additions 17 Discontinued Codes 19 Description Changes 20 Modifiers 21 ASC/HASC Providers 21 ASC/HASC Code Additions 21 Home Health Providers 21 Title XIX Home Health Policy Updates 21 THSteps-CCP Providers 22 Standing Frames 22 CSHCN Providers 22 CSHCN Program Policy Updates 22 CSHCN HCPCS Additions 23 2005 Quarterly Additions 24 Prior Authorization Update 24 Forms 26 Provider Information Change Form 26 Electronic Funds Transfer 28
- Page 2 and 3: All Providers 2006 Clinical Laborat
- Page 4 and 5: All Providers Discontinued Replacem
- Page 6 and 7: All Providers Procedure Code TOS /
- Page 8 and 9: All Providers Procedure Code TOS /
- Page 10 and 11: All Providers Procedure Code TOS /
- Page 12 and 13: All Providers Procedure Code TOS /
- Page 14 and 15: All Providers Procedure Code TOS /
- Page 16 and 17: All Providers Procedure Code TOS /
- Page 18 and 19: All Providers Procedure Code TOS /
- Page 20 and 21: All Providers Discontinued Procedur
- Page 22 and 23: THSteps-CCP Providers / CSHCN Provi
- Page 24 and 25: CSHCN Providers Procedure Code TOS
- Page 26 and 27: Forms Provider Information Change F
- Page 28 and 29: Forms Electronic Funds Transfer (EF
- Page 30 and 31: Notes Texas Medicaid Bulletin, No.
- Page 32: Current Procedural Terminology (CPT
T EXAS MEDICAID BULLETIN<br />
<strong>2006</strong> Healthcare Common Procedure Coding System (<strong>HCPCS</strong>) <strong>Special</strong> <strong>Bulletin</strong><br />
<strong>2006</strong> <strong>HCPCS</strong> SPECIAL BULLETIN NO. <strong>193</strong><br />
<strong>2006</strong> <strong>HCPCS</strong> Implementation<br />
This is a <strong>com</strong>bined, special bulletin for all Medicaid and<br />
Children with <strong>Special</strong> Health Care Needs (CSHCN)<br />
Services Program providers. This bulletin is intended to<br />
notify providers of program and coding changes related to<br />
the <strong>2006</strong> Healthcare Common Procedure Coding System<br />
(<strong>HCPCS</strong>) implementation.<br />
On <strong>January</strong> 13, <strong>2006</strong>, the Texas Medicaid & Healthcare<br />
Partnership (<strong>TMHP</strong>) will apply the annual <strong>2006</strong> <strong>HCPCS</strong><br />
additions, changes, and deletions, effective for dates of<br />
service on or after <strong>January</strong> 1, <strong>2006</strong>. The <strong>2006</strong> deleted<br />
procedure codes will no longer be reimbursed after<br />
December 31, 2005. It is re<strong>com</strong>mended that providers<br />
not submit claims for procedure codes that have been<br />
added until after the updates are implemented in the<br />
system. If claims are submitted prior to the updates being<br />
made, they will be denied. Any denials received between<br />
<strong>January</strong> 1 and <strong>January</strong> 13, <strong>2006</strong>, due to a <strong>HCPCS</strong> update<br />
must be appealed by the provider.<br />
Providers who have received prior authorizations for a<br />
<strong>2006</strong> discontinued code for dates of services that occur<br />
on, after, or en<strong>com</strong>pass <strong>January</strong> 1, <strong>2006</strong>, must contact<br />
the <strong>TMHP</strong> Prior Authorization Department to update<br />
the <strong>HCPCS</strong> procedure codes authorized for those services<br />
except for the procedure codes listed below. Please do not<br />
request changes to authorizations prior to <strong>January</strong> 13, <strong>2006</strong>.<br />
Prior authorizations for the list of codes below will be<br />
updated by <strong>TMHP</strong> and require no action on the part of<br />
the provider.<br />
Procedure Codes<br />
33918 33919 44200 97504 97520<br />
97703 A5119 B4184 E0972 K0618<br />
K0619 K0620 K0630– K0670 L0860<br />
K0649<br />
L8100 L8110 L8120 L8130 L8140<br />
L8150 L8160 L8170 L8180 L8190<br />
L8195 L8200 L8210 L8220 L8230<br />
L8239<br />
For information specific to the CSHCN authorization process<br />
please see page 24 of this bulletin.<br />
All providers are encouraged to review the “All Providers”<br />
section of this bulletin. Policy updates for specific programs and<br />
provider types are discussed in that program or provider type’s<br />
section of the bulletin.<br />
INSIDE<br />
All Providers 1<br />
<strong>2006</strong> <strong>HCPCS</strong> Implementation 1<br />
<strong>2006</strong> Clinical Laboratory Fee Schedule 2<br />
Medicaid Program Policy Updates 2<br />
<strong>HCPCS</strong> Replacement Codes 2<br />
<strong>2006</strong> <strong>HCPCS</strong> Additions 5<br />
2005 Quarterly Additions 17<br />
Discontinued Codes 19<br />
Description Changes 20<br />
Modifiers 21<br />
ASC/HASC Providers 21<br />
ASC/HASC Code Additions 21<br />
Home Health Providers 21<br />
Title XIX Home Health Policy Updates 21<br />
THSteps-CCP Providers 22<br />
Standing Frames 22<br />
CSHCN Providers 22<br />
CSHCN Program Policy Updates 22<br />
CSHCN <strong>HCPCS</strong> Additions 23<br />
2005 Quarterly Additions 24<br />
Prior Authorization Update 24<br />
Forms 26<br />
Provider Information Change Form 26<br />
Electronic Funds Transfer 28
All Providers<br />
<strong>2006</strong> Clinical Laboratory<br />
Fee Schedule<br />
The National Limitation Amount<br />
(NLA) calculation for <strong>2006</strong> remains<br />
at 74 percent of the median of<br />
the local fees for tests for which<br />
NLAs were established before<br />
<strong>January</strong> 1, 2001. In accordance with<br />
Section 1833(h)(4)(B)(viii) of the<br />
Social Security Act (amended by Section 531 of the Benefits<br />
Improvement and Protection Act [BIPA] of 2000), the NLA<br />
calculation for <strong>2006</strong> is 100 percent of the median of the<br />
local fees for tests for which NLAs are established on or<br />
after <strong>January</strong> 1, 2001. In accordance with Section 4553 of<br />
the Balanced Budget Act of 1997 (which amended Section<br />
1833[h][4][B] of the Social Security Act), there is no annual<br />
update (economic index) to the local laboratory fees for<br />
<strong>2006</strong>.<br />
Medicaid Program Policy Updates<br />
The following Medicaid Program policy updates have<br />
been made to support the <strong>2006</strong> <strong>HCPCS</strong> implementation.<br />
Lipids<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure code 9-B4185 is a benefit of the Texas<br />
Medicaid Program when submitted with documentation<br />
<strong>HCPCS</strong> Replacement Codes<br />
of medical necessity and prior authorized. Procedure code<br />
9-B4185 is reimbursed on a daily basis, but will be denied<br />
as part of another service if hyperalimentation/total<br />
parenteral nutrition is also prior authorized.<br />
Antihemophilic Factors<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
1-Q0187 and 1-Q2022 are no longer benefits of the Texas<br />
Medicaid Program.<br />
Procedure codes 1-J7188 and 1-J7189 are benefits of Texas<br />
Medicaid. Procedure code 1-J7188 is limited to diagnosis<br />
code 2864, and procedure code 1-J7189 is limited to<br />
diagnosis codes 2860 and 2861.<br />
Nursing Facility Services<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure code 1-99318 is a benefit of the Texas<br />
Medicaid Program and is limited to once per year.<br />
Incidental Services<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
the following procedure codes are benefits of the Texas<br />
Medicaid Program:<br />
Procedure Codes<br />
1-90760 1-90761 1-90765 1-90766 1-90767<br />
1-90768 1-96521 1-96522 1-96523<br />
The above procedure codes will be denied as part of<br />
another service if billed in conjunction with a surgical or<br />
anesthesia procedure.<br />
The following is a list of discontinued procedure codes and the corresponding new replacement <strong>HCPCS</strong> codes. All<br />
providers are encouraged to review this table and the tables on the following pages in addition to the sections of this<br />
bulletin applicable to their provider type.<br />
Discontinued Replacement TOS /<br />
Procedure Code Procedure Code Allowable<br />
90780 90760 1 = 1.67 RVUs<br />
90780 90765 1 = 2.04 RVUs<br />
90780 90766 1 = 0.68 RVUs<br />
90782 90772 1 = 0.49 RVUs<br />
Medicaid / Managed<br />
Care Comments<br />
CSHCN<br />
Comments<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 2 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Discontinued Replacement TOS /<br />
Medicaid / Managed CSHCN<br />
Procedure Code Procedure Code Allowable<br />
Care Comments<br />
Comments<br />
90783 90773 1 = $12.00<br />
90784 90774 1 = 1.52 RVUs<br />
96100 96101 1 = $71.69 (SHARS)<br />
96117 96118 1 = 1.88 RVUs<br />
96400 96401 1 = 1.75 RVUs<br />
96400 96402 1 = 0.94 RVUs<br />
96408 96409 1 = 0.93 RVUs<br />
96410 96413 1 = 1.43 RVUs<br />
96412 96415 NC<br />
96520 96521 1 = 0.96 RVUs<br />
96530 96522 1 = 1.13 RVUs<br />
99052 99053 NC<br />
99054 99051 NC<br />
99301-99303;<br />
99311-99313<br />
99304 1 = 1.43 RVUs<br />
99301-99303;<br />
99311-99313<br />
99305 1 = 1.71 RVUs<br />
99301-99303;<br />
99311-99313<br />
99306 1 = 2.32 RVUs<br />
99301-99303;<br />
99311-99313<br />
99307 1 = 0.89 RVUs<br />
99301-99303;<br />
99311-99313<br />
99308 1 = 1.18 RVUs<br />
99301-99303;<br />
99311-99313<br />
99309 1 = 1.60 RVUs<br />
99301-99303;<br />
99311-99313<br />
99310 1 = 1.60 RVUs<br />
99301-99303;<br />
99311-99313<br />
99318 1 = 1.43 RVUs<br />
A5119 A5120 9 = $0.18<br />
A9523 A9543 9 = MR<br />
A9534 A9545 NC<br />
C9129 J9027 1 = $114.75<br />
J1563 J1566 1 = $35.07<br />
J1563 J1567 1 = $41.31<br />
J1750 J1751 1 = $16.02<br />
J1750 J1752 1 = $16.02<br />
K0618 L0491 9** = $621.58 PA A<br />
K0619 L0492 9** = $402.85 PA A<br />
K0630 L0621 9** = $75.19 PA A<br />
K0631 L0622 9** = $194.97 PA A<br />
K0632 L0623 9** = MR PA A<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
3<br />
All Providers<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Discontinued Replacement TOS /<br />
Medicaid / Managed CSHCN<br />
Procedure Code Procedure Code Allowable<br />
Care Comments<br />
Comments<br />
K0633 L0624 9** = MR PA A<br />
K0634 L0625 9** = $44.59 PA A<br />
K0635 L0626 9** = $63.09 PA A<br />
K0636 L0627 9** = $332.68 PA A<br />
K0637 L0628 9** = $67.89 PA A<br />
K0638 L0629 9** = $170.13 PA A<br />
K0639 L0630 9** = $131.06 PA A<br />
K0640 L0631 9** = $830.85 PA A<br />
K0641 L0632 9** = MR PA A<br />
K0642 L0633 9** = $232.08 PA A<br />
K0643 L0634 9** = MR PA A<br />
K0644 L0635 9** = $800.80 PA A<br />
K0645 L0636 9** = $1,085.59 PA A<br />
K0646 L0637 9** = $844.89 PA A<br />
K0647 L0638 9** = $1,067.44 PA A<br />
K0648 L0639 9** = $648.94 PA A<br />
K0649 L0640 9** = $846.86 PA A<br />
L0860 L0859 9** = $1,138.35 PA A<br />
L8120 A6532 9 = $60.96 PA A<br />
L8130 A6533 9 = $45.10 PA A<br />
L8140 A6534 9 = $49.98 PA A<br />
L8150 A6535 9 = $70.41 PA A<br />
L8160 A6536 9 = $51.66 PA A<br />
L8170 A6537 9 = $74.99 PA A<br />
L8180 A6538 9 = $77.90 PA A<br />
L8190 A6539 9 = $74.60 PA A<br />
L8195 A6540 9 = $75.84 PA A<br />
L8200 A6541 9 = $98.40 PA A<br />
L8210 A6542 9 = $177.94 PA A<br />
L8220 A6543 9 = $45.69 PA A<br />
L8230 A6544 9 = $34.03 PA A<br />
L8239 A6549 9 = MR PA A<br />
Q0136 J0885 1 = $11.44<br />
Q0137 J0881 1 = $4.24<br />
Q2019 J0480 1 = $1,445.31<br />
Q4054 J0882 1 = $4.24<br />
Q4055 J0886 1 = $11.44<br />
S0071 J0133 1 = $0.20<br />
For more information, call the <strong>TMHP</strong> Contact Center at 1-800-925-9126 or the <strong>TMHP</strong>-CSHCN Contact Center at<br />
1-800-568-2413.<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 4 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
<strong>2006</strong> <strong>HCPCS</strong> Additions<br />
The following is a list of new <strong>HCPCS</strong> procedure codes<br />
that do not replace existing codes.<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
01965 7 = 4 units<br />
01966 7 = 4 units<br />
15040 2 = 3.37 RVUs<br />
8 = NC<br />
F = Group 2<br />
15110 2 = 17.83 RVUs<br />
8 = NC<br />
F = Group 2<br />
15111 2 = 2.90 RVUs<br />
8 = NC<br />
F = Group 1<br />
15115 2 = 18.33 RVUs<br />
8 = NC<br />
F = Group 2<br />
15116 2 = 3.95 RVUs<br />
8 = NC<br />
F = Group 1<br />
15130 2 = 14.21 RVUs<br />
8 = NC<br />
F = Group 2<br />
15131 2 = 2.35 RVUs<br />
8 = NC<br />
F = Group 1<br />
15135 2 = 17.00 RVUs<br />
8 = NC<br />
F = Group 2<br />
15136 2 = 2.37 RVUs<br />
8 = NC<br />
F = Group 1<br />
15150 2 = 14.36 RVUs<br />
8 = NC<br />
F = Group 2<br />
15151 2 = 2.48 RVUs<br />
8 = NC<br />
F = Group 1<br />
15152 2 = 3.91 RVUs<br />
8 = NC<br />
F = Group 1<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
CSHCN<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
15155 2 = 17.03 RVUs<br />
8 = NC<br />
F = Group 2<br />
15156 2 = 4.35 RVUs<br />
8 = NC<br />
F = Group 1<br />
15157 2 = 4.74 RVUs<br />
8 = NC<br />
F = Group 1<br />
15170 2 = 7.92 RVUs<br />
8 = NC<br />
F = Group 2<br />
15171 2 = 2.36 RVUs<br />
8 = NC<br />
F = Group 1<br />
15175 2 = 11.83 RVUs<br />
8 = NC<br />
F = Group 2<br />
15176 2 = 2.48 RVUs<br />
8 = NC<br />
F = Group 1<br />
15300 2 = 6.72 RVUs<br />
8 = NC<br />
F = Group 2<br />
15301 2 = 1.54 RVUs<br />
8 = NC<br />
F = Group 1<br />
15320 2 = 7.82 RVUs<br />
8 = NC<br />
F = Group 2<br />
15321 2 = 2.30 RVUs<br />
8 = NC<br />
F = Group 1<br />
15330 2 = 6.71 RVUs<br />
8 = NC<br />
F = Group 2<br />
15331 2 = 1.54 RVUs<br />
8 = NC<br />
F = Group 1<br />
15335 2 = 7.50 RVUs<br />
8 = NC<br />
F = Group 2<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
5<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
All Providers<br />
CSHCN<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
15336 2 = 2.20 RVUs<br />
8 = NC<br />
F = Group 1<br />
15340 2 = 6.89 RVUs<br />
8 = NC<br />
F = Group 2<br />
15341 2 = 0.76 RVUs<br />
8 = NC<br />
F = Group 1<br />
15360 2 = 7.39 RVUs<br />
8 = NC<br />
F = Group 2<br />
15361 2 = 1.75 RVUs<br />
8 = NC<br />
F = Group 1<br />
15365 2 = 7.81 RVUs<br />
8 = NC<br />
F = Group 2<br />
15366 2 = 2.20 RVUs<br />
8 = NC<br />
F = Group 1<br />
15420 2 = 8.82 RVUs<br />
8 = NC<br />
F = Group 2<br />
15421 2 = 2.33 RVUs<br />
8 = NC<br />
F = Group 1<br />
15430 2 = 13.04 RVUs<br />
8 = NC<br />
F = Group 2<br />
15431 2 = 0.62 RVUs<br />
8 = NC<br />
F = Group 1<br />
22010 2 = 9.87 RVUs<br />
8 = NC<br />
F = Group 3<br />
22015 2 = 9.87 RVUs<br />
8 = NC<br />
F = Group 3<br />
22523 2 = 16.29 RVUs<br />
8 = 2.61 RVUs<br />
F = Group 2<br />
22524 2 = 15.61 RVUs<br />
8 = 2.50 RVUs<br />
F = Group 2<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
CSHCN<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
22525 2 = 7.47 RVUs<br />
8 = 1.20 RVUs<br />
F = Group 2<br />
28890 NC<br />
32503 2 = 46.39 RVUs<br />
8 = 7.42 RVUs<br />
F = NC<br />
32504 2 = 50.60 RVUs<br />
8 = 8.10 RVUs<br />
F = NC<br />
33507 2 = 47.73 RVUs<br />
8 = 7.64 RVUs<br />
F = NC<br />
33548 2 = 62.83<br />
8 = 10.05<br />
F = NC<br />
33768 2 = 11.98 RVUs<br />
8 = 1.92 RVUs<br />
F = NC<br />
33880 2 = 35.27 RVUs<br />
8 = 5.64 RVUs<br />
F = NC<br />
33881 2 = 35.27 RVUs<br />
8 = 5.64 RVUs<br />
F = NC<br />
33883 2 = 19.09 RVUs<br />
8 = 3.05 RVUs<br />
F = NC<br />
33884 2 = 6.07 RVUs<br />
8 = 0.97 RVUs<br />
F = NC<br />
33886 2 = 6.07 RVUs<br />
8 = 0.97 RVUs<br />
F = NC<br />
33889 2 = 23.28 RVUs<br />
8 = 3.72 RVUs<br />
F = NC<br />
33891 2 = 29.70 RVUs<br />
8 = 4.75 RVUs<br />
F = NC<br />
33925 2 = 36.82 RVUs<br />
8 = 5.89 RVUs<br />
F = NC<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 6 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
F = A
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
33926 2 = 41.82 RVUs<br />
8 = 6.69 RVUs<br />
F = NC<br />
36598 2 = 1.40 RVUs<br />
8 = NC<br />
F = Group 1<br />
37184 2 = 12.57 RVUs<br />
8 = 2.01 RVUs<br />
F = Group 2<br />
37185 2 = 4.60 RVUs<br />
8 = 0.74 RVUs<br />
F = Group 1<br />
37186 2 = 6.90 RVUs<br />
8 = 1.10 RVUs<br />
F = Group 2<br />
37187 2 = 11.69 RVUs<br />
8 = 1.87 RVUs<br />
F = Group 2<br />
37188 2 = 8.45 RVUs<br />
8 = 1.35 RVUs<br />
F = Group 2<br />
37718 2 = 10.97 RVUs<br />
8 = 1.76 RVUs<br />
F = Group 3<br />
37722 2 = 13.07 RVUs<br />
8 = 2.09 RVUs<br />
F = Group 3<br />
43770 NC<br />
43771 NC<br />
43772 NC<br />
43773 NC<br />
43774 NC<br />
43886 NC<br />
43887 NC<br />
43888 NC<br />
44180 2 = 22.52 RVUs<br />
8 = 3.60 RVUs<br />
F = Group 3<br />
44186 2 = 15.84 RVUs<br />
8 = 2.53 RVUs<br />
F = Group 2<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
CSHCN<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
44187 2 = 26.17 RVUs<br />
8 = 4.19 RVUs<br />
F = Group 4<br />
44188 2 = 18.44 RVUs<br />
8 = 2.95 RVUs<br />
F = Group 3<br />
44213 2 = 3.67 RVUs<br />
8 = 0.59 RVUs<br />
F = NC<br />
44227 2 = 40.52 RVUs<br />
8 = 6.48 RVUs<br />
F = Group 4<br />
45395 2 = 47.83 RVUs<br />
8 = 7.65 RVUs<br />
F = NC<br />
45397 2 = 51.98 RVUs<br />
8 = 8.32 RVUs<br />
F = Group 4<br />
45400 2 = 25.25 RVUs<br />
8 = 4.04 RVUs<br />
F = Group 3<br />
45402 2 = 27.72 RVUs<br />
8 = 4.44 RVUs<br />
F = Group 3<br />
45499 2 = MR<br />
8 = MR<br />
F = MR<br />
45990 2 = 1.39 RVUs<br />
8 = NC<br />
F = Group 2<br />
46505 2 = 4.97 RVUs<br />
8 = NC<br />
F = Group 1<br />
46710 2 = 25.15 RVUs<br />
8 = 4.02 RVUs<br />
F = NC<br />
46712 2 = 33.62 RVUs<br />
8 = 5.38 RVUs<br />
F = NC<br />
50250 2 = 30.54 RVUs<br />
8 = 4.89 RVUs<br />
F = Group 3<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
7<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
All Providers<br />
CSHCN<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
50382 2 = 7.71 RVUs<br />
8 = NC<br />
F = Group 1<br />
50384 2 = 7.02 RVUs<br />
8 = NC<br />
F = Group 1<br />
50387 2 = 2.79 RVUs<br />
8 = NC<br />
F = Group 1<br />
50389 2 = 1.54 RVUs<br />
8 = NC<br />
F = Group 1<br />
50592 2 = 10.17 RVUs<br />
8 = NC<br />
F = Group 2<br />
51999 2 = MR<br />
8 = MR<br />
F = MR<br />
57295 2 = 12.80 RVUs<br />
8 = 2.05 RVUs<br />
F = Group 2<br />
58110 2 = 1.17 RVUs<br />
8 = NC<br />
F = Group 1<br />
61630 NC<br />
61635 NC<br />
61640 NC<br />
61641 NC<br />
61642 NC<br />
64650 2 = 1.06 RVUs<br />
8 = NC<br />
F = Group 1<br />
64653 2 = 1.34 RVUs<br />
8 = NC<br />
F = Group 1<br />
75956 NC<br />
75957 NC<br />
75958 NC<br />
75959 NC<br />
76376 4 = 3.8 RUVs<br />
I = 0.29 RVUs<br />
T = 3.51 RVUs<br />
Medicaid /<br />
Managed Care<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
PA (Managed<br />
Care Only)<br />
CSHCN<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
F = A<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
76377 4 = 4.01 RVUs<br />
I = 0.24 RVUs<br />
T = 3.77 RVUs<br />
77421 4 = 4.00 RVUs<br />
I = 0.54 RVUs<br />
T = 3.46 RVUs<br />
77422 6 = NC<br />
I = NC<br />
T = 1.89 RVUs<br />
77423 6 = NC<br />
I = NC<br />
T = 1.89 RVUs<br />
80195 5 = $18.97<br />
82271 5 = $4.49<br />
82272 5 = $4.49<br />
83037 5 = $27.42<br />
83631 5 = $27.42<br />
83695 5 = $18.09<br />
83700 5 = $15.56<br />
83701 5 = $34.30<br />
83704 5 = $34.30<br />
83900 5 = $14.07<br />
83907 5 = $14.07<br />
83908 5 = $14.07<br />
83909 5 = $14.07<br />
83914 5 = $14.07<br />
86200 5 = $16.70<br />
86355 5 = $52.13<br />
86357 5 = $52.13<br />
86367 5 = $52.13<br />
86480 5 = $52.13<br />
I = NC<br />
T = NC<br />
86923 5 = $13.39<br />
I = NC<br />
T = NC<br />
86960 5 = $16.73<br />
I = NC<br />
T = NC<br />
87209 5 = $12.09<br />
Medicaid /<br />
Managed Care<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 8 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
87900 5 = $182.11<br />
88333 NC<br />
88334 NC<br />
88384 5 = $31.44<br />
88385 5 = 2.21 RVUs<br />
I = NC<br />
T = NC<br />
88386 5 = 2.78 RVUs<br />
I = NC<br />
T = NC<br />
89049 5 = 5.02 RVUs<br />
I = NC<br />
T = NC<br />
90649 NC<br />
90714 1 = Informational<br />
Only<br />
90736 NC<br />
90761 1 = 0.53 RVUs<br />
90767 1 = 1.12 RVUs<br />
90768 1 = 0.65 RVUs<br />
90775 1 = 0.71 RVUs<br />
90779 1 = MR<br />
91022 NC<br />
92626 1 = 0.61 RVUs<br />
92627 1 = 0.15 RVUs<br />
92630 1 = 3.01 RVUs<br />
92633 1 = 3.01 RVUs<br />
95251 NC<br />
95865 5 = 3.13 RVUs<br />
I = 2.42 RVUs<br />
T = 0.71 RVUs<br />
95866 5 = 2.11 RVUs<br />
I = 1.88 RVUs<br />
T = 0.23 RVUs<br />
95873 1 = 0.77 RVUs<br />
95874 1 = 0.78 RVUs<br />
96101 5 = 1.88 RVUs<br />
I = NC<br />
T = NC<br />
96102 NC<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
Medicaid /<br />
Managed Care<br />
96103 NC<br />
96116 NC<br />
96118 1 = 1.88 RVUs<br />
96119 NC<br />
96120 NC<br />
96411 1 = 0.93 RVUs<br />
96416 NC<br />
96417 NC<br />
96523 1 = 0.74 RVUs<br />
97760 1 = $35.00 A<br />
97761 1 = $35.00<br />
C = NC<br />
A<br />
97762 1 = $35.00 A<br />
98960 NC<br />
98961 NC<br />
98962 NC<br />
99060 1 = $12.69<br />
99143 NC<br />
99144 NC<br />
99145 NC<br />
99148 NC<br />
99149 NC<br />
99150 NC<br />
99300 1 = 3.58 RVUs<br />
99324 1 = 1.16 RVUs<br />
99325 1 = 1.67 RVUs<br />
99326 1 = 2.20 RVUs<br />
99327 1 = 2.20 RVUs<br />
99328 1 = 2.20 RVUs<br />
99334 1 = 1.20 RVUs<br />
99335 1 = 1.83 RVUs<br />
99336 1 = 2.68 RVUs<br />
99337 1 = 2.68 RVUs<br />
99339 NC<br />
99340 NC<br />
0089T NC<br />
0090T NC<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
9<br />
All Providers<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
0091T NC<br />
0092T NC<br />
0093T NC<br />
0094T NC<br />
0095T NC<br />
0096T NC<br />
0097T NC<br />
0098T NC<br />
0099T NC<br />
0100T NC<br />
0101T NC<br />
0102T NC<br />
0103T NC<br />
0104T NC<br />
0105T NC<br />
0106T NC<br />
0107T NC<br />
0108T NC<br />
0109T NC<br />
0110T NC<br />
0111T NC<br />
0115T NC<br />
0116T NC<br />
0117T NC<br />
0120T NC<br />
0123T NC<br />
0124T NC<br />
0126T NC<br />
0130T NC<br />
0133T NC<br />
0135T NC<br />
0137T NC<br />
0140T NC<br />
0141T NC<br />
0142T NC<br />
0143T NC<br />
0144T NC<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
Medicaid /<br />
Managed Care<br />
0145T NC<br />
0146T NC<br />
0147T NC<br />
0148T NC<br />
0149T NC<br />
0150T NC<br />
0151T NC<br />
0152T NC<br />
0153T NC<br />
0154T NC<br />
1003F NC<br />
1004F NC<br />
1005F NC<br />
1006F NC<br />
1007F NC<br />
1008F NC<br />
2001F NC<br />
2002F NC<br />
2003F NC<br />
2004F NC<br />
3000F NC<br />
3002F NC<br />
4003F NC<br />
4012F NC<br />
4014F NC<br />
4015F NC<br />
4016F NC<br />
4017F NC<br />
4018F NC<br />
A0998 NC<br />
A4218 NC, Bill<br />
Vendor Drug<br />
Program<br />
A4233 9 = $6.55 A<br />
A4234 9 = $6.55 A<br />
A4235 9 = $6.55 A<br />
A4236 9 = $6.55 A<br />
A4363 9 = $1.58<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 10 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
Medicaid /<br />
Managed Care<br />
A4411 9 = $3.72<br />
A4412 9 = $5.50<br />
A4604 NC<br />
A5512 NC<br />
A5513 NC<br />
A6457 9 = $1.14 PA A<br />
A6513 9 = MR PA A<br />
A6530 9 = $36.35 PA A<br />
A6531 9 = $43.27 PA A<br />
A6550 9 = $51.97 PA<br />
A9275 9 = $30.74 PA<br />
A9281 NC<br />
A9282 NC<br />
A9535 NC<br />
A9536 NC<br />
A9537 NC<br />
A9538 NC<br />
A9539 NC<br />
A9540 NC<br />
A9541 NC<br />
A9542 NC<br />
A9544 NC<br />
A9546 NC<br />
A9547 NC<br />
A9548 NC<br />
A9549 NC<br />
A9550 NC<br />
A9551 NC<br />
A9552 NC<br />
A9553 NC<br />
A9554 NC<br />
A9555 NC<br />
A9556 NC<br />
A9557 NC<br />
A9558 NC<br />
A9559 NC<br />
A9560 NC<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
Medicaid /<br />
Managed Care<br />
A9561 NC<br />
A9562 NC<br />
A9563 9 = $69.39<br />
A9564 9 = $155.47<br />
A9565 NC<br />
A9566 NC<br />
A9567 NC<br />
A9698 NC<br />
B4185 9 = $87.60 PA A<br />
E0170 NC<br />
E0171 NC<br />
E0172 NC<br />
E0485 NC<br />
E0486 NC<br />
E0641 9 = NC<br />
J = $853.57<br />
L = NC<br />
PA A<br />
E0642 9 = NC<br />
J** = MR<br />
L = NC<br />
PA A<br />
E0705 9 = NC<br />
J = $37.91<br />
L = NC<br />
PA A<br />
E0762 NC<br />
E0764 NC<br />
E0911 9 = NC<br />
J = $211.64<br />
L = $18.13<br />
PA A<br />
E0912 9 = NC<br />
J = $311.72<br />
L = $28.40<br />
PA A<br />
E1392 NC<br />
E1812 9 = NC<br />
J** = $1,935.20<br />
L = NC<br />
PA<br />
E2207 9 = NC<br />
J = $43.35<br />
L = $4.34<br />
PA A<br />
E2208 9 = NC<br />
J = $118.78<br />
L = $11.87<br />
PA A<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
11<br />
All Providers<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
E2209 9 = NC<br />
J = $107.16<br />
L = $10.74<br />
E2210 9 = NC<br />
J = $6.55<br />
L = NC<br />
E2211 9 = NC<br />
J = $29.24<br />
L = NC<br />
E2212 9 = NC<br />
J = $5.88<br />
L = NC<br />
E2213 9 = NC<br />
J = $29.24<br />
L = NC<br />
E2214 9 = NC<br />
J = $30.60<br />
L = NC<br />
E2215 9 = NC<br />
J = $9.60<br />
L = NC<br />
E2216 9 = NC<br />
J = $29.24<br />
L = NC<br />
E2217 9 = NC<br />
J = $32.88<br />
L = NC<br />
E2218 9 = NC<br />
J = $29.24<br />
L = NC<br />
E2219 9 = NC<br />
J = $32.88<br />
L = NC<br />
E2220 9 = NC<br />
J = $24.24<br />
L = NC<br />
E2221 9 = NC<br />
J = $25.55<br />
L = NC<br />
E2222 9 = NC<br />
J = $32.88<br />
L = NC<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
E2223 9 = NC<br />
J = MR<br />
L = NC<br />
E2224 9 = NC<br />
J = $45.02<br />
L = NC<br />
E2225 9 = NC<br />
J = $32.88<br />
L = NC<br />
E2226 9 = NC<br />
J = $45.88<br />
L = NC<br />
E2371 9 = NC<br />
J = $186.00<br />
L = NC<br />
E2372 NC<br />
G0235 NC<br />
G0332 NC<br />
G0333 NC<br />
G0372 NC<br />
G0375 NC<br />
G0376 NC<br />
G0378 NC<br />
G0379 NC<br />
G8006 NC<br />
G8007 NC<br />
G8008 NC<br />
G8009 NC<br />
G8010 NC<br />
G8011 NC<br />
G8012 NC<br />
G8013 NC<br />
G8014 NC<br />
G8015 NC<br />
G8016 NC<br />
G8017 NC<br />
G8018 NC<br />
G8019 NC<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
PA A<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 12 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
G8020 NC<br />
G8021 NC<br />
G8022 NC<br />
G8023 NC<br />
G8024 NC<br />
G8025 NC<br />
G8026 NC<br />
G8027 NC<br />
G8028 NC<br />
G8029 NC<br />
G8030 NC<br />
G8031 NC<br />
G8032 NC<br />
G8033 NC<br />
G8034 NC<br />
G8035 NC<br />
G8036 NC<br />
G8037 NC<br />
G8038 NC<br />
G8039 NC<br />
G8040 NC<br />
G8041 NC<br />
G8051 NC<br />
G8052 NC<br />
G8053 NC<br />
G8054 NC<br />
G8055 NC<br />
G8056 NC<br />
G8057 NC<br />
G8058 NC<br />
G8059 NC<br />
G8060 NC<br />
G8061 NC<br />
G8062 NC<br />
G8075 NC<br />
G8076 NC<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
G8077 NC<br />
G8078 NC<br />
G8079 NC<br />
G8080 NC<br />
G8081 NC<br />
G8082 NC<br />
G8093 NC<br />
G8094 NC<br />
G8099 NC<br />
G8100 NC<br />
G8103 NC<br />
G8104 NC<br />
G8106 NC<br />
G8107 NC<br />
G8108 NC<br />
G8109 NC<br />
G8110 NC<br />
G8111 NC<br />
G8112 NC<br />
G8113 NC<br />
G8114 NC<br />
G8115 NC<br />
G8116 NC<br />
G8117 NC<br />
G8126 NC<br />
G8127 NC<br />
G8128 NC<br />
G8129 NC<br />
G8130 NC<br />
G8131 NC<br />
G8152 NC<br />
G8153 NC<br />
G8154 NC<br />
G8155 NC<br />
G8156 NC<br />
G8157 NC<br />
Medicaid /<br />
Managed Care<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
13<br />
All Providers<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
G8158 NC<br />
G8159 NC<br />
G8160 NC<br />
G8161 NC<br />
G8162 NC<br />
G8163 NC<br />
G8164 NC<br />
G8165 NC<br />
G8166 NC<br />
G8167 NC<br />
G8170 NC<br />
G8171 NC<br />
G8172 NC<br />
G8182 NC<br />
G8183 NC<br />
G8184 NC<br />
G8185 NC<br />
G8186 NC<br />
G9033 NC<br />
G9041 NC<br />
G9042 NC<br />
G9043 NC<br />
G9044 NC<br />
G9050 NC<br />
G9051 NC<br />
G9052 NC<br />
G9053 NC<br />
G9054 NC<br />
G9055 NC<br />
G9056 NC<br />
G9057 NC<br />
G9058 NC<br />
G9059 NC<br />
G9060 NC<br />
G9061 NC<br />
G9062 NC<br />
G9063 NC<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
G9064 NC<br />
G9065 NC<br />
G9066 NC<br />
G9067 NC<br />
G9068 NC<br />
G9069 NC<br />
G9070 NC<br />
G9071 NC<br />
G9072 NC<br />
G9073 NC<br />
G9074 NC<br />
G9075 NC<br />
G9076 NC<br />
G9077 NC<br />
G9078 NC<br />
G9079 NC<br />
G9080 NC<br />
G9081 NC<br />
G9082 NC<br />
G9083 NC<br />
G9084 NC<br />
G9085 NC<br />
G9086 NC<br />
G9087 NC<br />
G9088 NC<br />
G9089 NC<br />
G9090 NC<br />
G9091 NC<br />
G9092 NC<br />
G9093 NC<br />
G9094 NC<br />
G9095 NC<br />
G9096 NC<br />
G9097 NC<br />
G9098 NC<br />
G9099 NC<br />
G9100 NC<br />
Medicaid /<br />
Managed Care<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 14 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
G9101 NC<br />
G9102 NC<br />
G9103 NC<br />
G9104 NC<br />
G9105 NC<br />
G9106 NC<br />
G9107 NC<br />
G9108 NC<br />
G9109 NC<br />
G9110 NC<br />
G9111 NC<br />
G9112 NC<br />
G9113 NC<br />
G9114 NC<br />
G9115 NC<br />
G9116 NC<br />
G9117 NC<br />
G9118 NC<br />
G9119 NC<br />
G9120 NC<br />
G9121 NC<br />
G9122 NC<br />
G9123 NC<br />
G9124 NC<br />
G9125 NC<br />
G9126 NC<br />
G9127 NC<br />
G9128 NC<br />
G9129 NC<br />
G9130 NC<br />
J0132 1 = $1.92<br />
J0278 1 = $1.33<br />
J0365 NC<br />
J0795 1 = $4.39<br />
J1162 1 = $510.00<br />
J1265 1 = $0.58<br />
J1430 1 = $70.98<br />
Medicaid /<br />
Managed Care<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
J1451 1 = $11.29<br />
J1640 NC<br />
J1675 NC<br />
J1945 1 = $147.29<br />
J2278 1 = $6.21<br />
J2325 1 = $30.03<br />
J2425 1 = $11.22<br />
J2503 1 = $101.49<br />
J2504 1 = $166.60<br />
J2513 1 = $12.98<br />
J2805 NC<br />
J2850 NC<br />
J3285 1 = $58.18<br />
J3355 NC<br />
J3471 1 = $0.13<br />
J3472 1 = $130.00<br />
J7188 1 = $0.85<br />
J7189 1 = $1.26<br />
J7306 NC<br />
J7341 1 = $26.32<br />
J7620 1 = $0.80<br />
J7627 NC<br />
J7640 NC<br />
J8498 NC, Bill<br />
Vendor Drug<br />
Program<br />
J8515 NC, Bill<br />
Vendor Drug<br />
Program<br />
J8540 NC, Bill<br />
Vendor Drug<br />
Program<br />
J8597 NC, Bill<br />
Vendor Drug<br />
Program<br />
J9025 1 = $4.05<br />
J9175 NC<br />
J9225 1 = $5,100.00<br />
J9264 1 = $8.46<br />
Medicaid /<br />
Managed Care<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
15<br />
All Providers<br />
CSHCN<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
Medicaid /<br />
Managed Care<br />
L2034 9** = $625.40 PA A<br />
L2387 9** = $87.90 PA A<br />
L3671 9** = $48.48 PA A<br />
L3672 9** = $580.17 PA A<br />
L3673 9** = $580.17 PA A<br />
L3702 9** = $79.12 PA A<br />
L3763 9** = $79.12 PA A<br />
L3764 9** = $364.35 PA A<br />
L3765 9** = $79.12 PA A<br />
L3766 9** = $833.68 PA A<br />
L3905 9** = $833.68 PA A<br />
L3913 9** = $184.18 PA A<br />
L3919 9** = $184.18 PA A<br />
L3921 9** = $184.18 PA A<br />
L3933 9** = $37.71 PA A<br />
L3935 9** = $37.71 PA A<br />
L3961 9** = $580.17 PA A<br />
L3967 9** = $417.08 PA A<br />
L3971 9** = $959.63 PA A<br />
L3973 9** = $959.63 PA A<br />
L3975 9** = $417.08 PA A<br />
L3976 9** = $580.17 PA A<br />
L3977 9** = $959.63 PA A<br />
L3978 9** = $959.63 PA A<br />
L5703 9** = $1,988.95 PA A<br />
L5858 9** = $1,453.47 PA A<br />
L5971 9** = $667.39 PA A<br />
L6621 9** = $212.21 PA A<br />
L6677 9** = $83.66 PA A<br />
L6883 9** = MR PA A<br />
L6884 9** = MR PA A<br />
L6885 9** = MR PA A<br />
L7400 9** = MR PA A<br />
L7401 9** = MR PA A<br />
L7402 9** = MR PA A<br />
L7403 9** = MR PA A<br />
L7404 9** = MR PA A<br />
CSHCN<br />
Procedure<br />
Code<br />
TOS /<br />
Allowable<br />
Medicaid /<br />
Managed Care<br />
L7405 9** = MR PA A<br />
L7600 9** = MR PA A<br />
L8609 NC<br />
L8623 9** = $52.45 PA A<br />
L8624 9** = $52.45 PA A<br />
L8680 NC<br />
L8681 NC<br />
L8682 NC<br />
L8683 NC<br />
L8684 NC<br />
L8685 NC<br />
L8686 NC<br />
L8687 NC<br />
L8688 NC<br />
L8689 NC<br />
Q0510 NC<br />
Q0511 NC<br />
Q0512 NC<br />
Q0513 NC<br />
Q0514 NC<br />
Q0515 NC, Bill<br />
Vendor Drug<br />
Program<br />
S2068 NC<br />
S2078 NC<br />
S2079 2 = 19.18 RVUs PA (Managed<br />
8 = NC<br />
F = Group 6<br />
Care Only)<br />
S3854 NC<br />
V2788 NC<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
CSHCN<br />
For more information, call the <strong>TMHP</strong> Contact Center at<br />
1-800-925-9126 or the <strong>TMHP</strong>-CSHCN Contact Center<br />
at 1-800-568-2413.<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 16 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
2005 Quarterly Additions<br />
The Centers for Medicare & Medicaid Services (CMS)<br />
updated <strong>HCPCS</strong> codes on a quarterly basis in 2005. The<br />
following is a <strong>com</strong>plete list of <strong>HCPCS</strong> codes implemented<br />
throughout 2005. These codes are valid for <strong>2006</strong> (effective<br />
date shown).<br />
Procedure Code TOS / Allowable Effective Date<br />
C1713 NC 8/10/2005<br />
C1714 NC 8/10/2005<br />
C1715 NC 8/10/2005<br />
C1717 NC 8/10/2005<br />
C1721 NC 8/10/2005<br />
C1722 NC 8/10/2005<br />
C1724 NC 8/10/2005<br />
C1725 NC 8/10/2005<br />
C1726 NC 8/10/2005<br />
C1727 NC 8/10/2005<br />
C1728 NC 8/10/2005<br />
C1729 NC 8/10/2005<br />
C1730 NC 8/10/2005<br />
C1731 NC 8/10/2005<br />
C1732 NC 8/10/2005<br />
C1733 NC 8/10/2005<br />
C1750 NC 8/10/2005<br />
C1751 NC 8/10/2005<br />
C1752 NC 8/10/2005<br />
C1753 NC 8/10/2005<br />
C1754 NC 8/10/2005<br />
C1755 NC 8/10/2005<br />
C1756 NC 8/10/2005<br />
C1757 NC 8/10/2005<br />
C1758 NC 8/10/2005<br />
C1759 NC 8/10/2005<br />
C1760 NC 8/10/2005<br />
C1762 NC 8/10/2005<br />
C1763 NC 8/10/2005<br />
C1764 NC 8/10/2005<br />
C1766 NC 8/10/2005<br />
C1767 NC 8/10/2005<br />
C1768 NC 8/10/2005<br />
C1769 NC 8/10/2005<br />
C1770 NC 8/10/2005<br />
Procedure Code TOS / Allowable Effective Date<br />
C1771 NC 8/10/2005<br />
C1772 NC 8/10/2005<br />
C1773 NC 8/10/2005<br />
C1776 NC 8/10/2005<br />
C1777 NC 8/10/2005<br />
C1778 NC 8/10/2005<br />
C1779 NC 8/10/2005<br />
C1780 NC 8/10/2005<br />
C1781 NC 8/10/2005<br />
C1782 NC 8/10/2005<br />
C1784 NC 8/10/2005<br />
C1785 NC 8/10/2005<br />
C1786 NC 8/10/2005<br />
C1787 9 = NC<br />
J = MR<br />
8/10/2005<br />
L = NC<br />
C1788 NC 8/10/2005<br />
C1789 NC 8/10/2005<br />
C1813 NC 8/10/2005<br />
C1815 NC 8/10/2005<br />
C1816 9 = NC<br />
J = MR<br />
8/10/2005<br />
L = NC<br />
C1817 NC 8/10/2005<br />
C1819 NC 8/10/2005<br />
C1874 NC 8/10/2005<br />
C1875 NC 8/10/2005<br />
C1876 NC 8/10/2005<br />
C1877 NC 8/10/2005<br />
C1878 NC 8/10/2005<br />
C1879 NC 8/10/2005<br />
C1880 NC 8/10/2005<br />
C1881 NC 8/10/2005<br />
C1882 NC 8/10/2005<br />
C1883 NC 8/10/2005<br />
C1885 NC 8/10/2005<br />
C1887 NC 8/10/2005<br />
C1891 NC 8/10/2005<br />
C1892 NC 8/10/2005<br />
C1893 NC 8/10/2005<br />
C1894 NC 8/10/2005<br />
C1895 NC 8/10/2005<br />
C1896 NC 8/10/2005<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
17<br />
All Providers<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Procedure Code TOS / Allowable Effective Date<br />
C1897 NC 8/10/2005<br />
C1898 NC 8/10/2005<br />
C1899 NC 8/10/2005<br />
C2615 NC 8/10/2005<br />
C2617 NC 8/10/2005<br />
C2619 NC 8/10/2005<br />
C2620 NC 8/10/2005<br />
C2621 NC 8/10/2005<br />
C2622 NC 8/10/2005<br />
C2625 NC 8/10/2005<br />
C2626 NC 8/10/2005<br />
C2627 NC 8/10/2005<br />
C2628 NC 8/10/2005<br />
C2629 NC 8/10/2005<br />
C2630 NC 8/10/2005<br />
C2631 NC 8/10/2005<br />
C2633 NC 8/10/2005<br />
C2634 NC 5/1/2005<br />
C2635 NC 5/1/2005<br />
C2636 NC 5/1/2005<br />
C2637 NC 11/16/2005<br />
C9220 1 = $186.16 5/1/2005<br />
C9221 NC 5/1/2005<br />
C9222 NC 5/1/2005<br />
C9224 NC 11/16/2005<br />
C9225 NC 11/16/2005<br />
C9725 NC 11/16/2005<br />
G0328 NC 8/10/2005<br />
G9034 NC 5/1/2005<br />
G9035 NC 5/1/2005<br />
G9036 NC 5/1/2005<br />
K0730 NC 8/10/2005<br />
Q0480 NC 11/16/2005<br />
Q0481 NC 11/16/2005<br />
Q0482 NC 11/16/2005<br />
Q0483 NC 11/16/2005<br />
Q0484 NC 11/16/2005<br />
Q0485 NC 11/16/2005<br />
Q0486 NC 11/16/2005<br />
Q0487 NC 11/16/2005<br />
Q0488 NC 11/16/2005<br />
Procedure Code TOS / Allowable Effective Date<br />
Q0489 NC 11/16/2005<br />
Q0490 NC 11/16/2005<br />
Q0491 NC 11/16/2005<br />
Q0492 NC 11/16/2005<br />
Q0493 NC 11/16/2005<br />
Q0494 NC 11/16/2005<br />
Q0495 NC 11/16/2005<br />
Q0496 NC 11/16/2005<br />
Q0497 NC 11/16/2005<br />
Q0498 NC 11/16/2005<br />
Q0499 NC 11/16/2005<br />
Q0500 NC 11/16/2005<br />
Q0501 NC 11/16/2005<br />
Q0502 NC 11/16/2005<br />
Q0503 NC 11/16/2005<br />
Q0504 NC 11/16/2005<br />
Q0505 NC 11/16/2005<br />
Q4079 NC 8/10/2005<br />
Q4080 NC 11/16/2005<br />
Q9958 NC 8/10/2005<br />
Q9959 NC 8/10/2005<br />
Q9960 NC 8/10/2005<br />
Q9961 NC 8/10/2005<br />
Q9962 NC 8/10/2005<br />
Q9963 NC 8/10/2005<br />
Q9964 NC 8/10/2005<br />
S0109 NC 5/1/2005<br />
S0133 1 = $5,700.00 8/10/2005<br />
S0145 1 = $343.60 8/10/2005<br />
S0146 1 = $60.24 8/10/2005<br />
S0166 NC 5/1/2005<br />
S0167 NC 5/1/2005<br />
S0168 NC 5/1/2005<br />
S0198 1 = $1,054.70 8/10/2005<br />
S0265 NC 8/10/2005<br />
S0515 NC 5/1/2005<br />
S0613 NC 8/10/2005<br />
S2075 2 = 18.19 RVUs<br />
8 = NC<br />
8/10/2005<br />
F = Group 4<br />
S2076 2 = 10.89 RVUs<br />
8 = NC<br />
F = Group 9<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
8/10/2005<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 18 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Procedure Code TOS / Allowable Effective Date<br />
S2077 2 = 7.19 RVUs<br />
8 = NC<br />
F = Group 7<br />
8/10/2005<br />
S2114 2 = 27.96 RVUs<br />
8 = NC<br />
F = Group 3<br />
11/16/2005<br />
S2117 2 = 21.68 RVUs<br />
8 = NC<br />
F = Group 4<br />
11/16/2005<br />
S2900 NC 8/10/2005<br />
S3626 5 = $94.37<br />
I = NC<br />
T = NC<br />
11/16/2005<br />
S3820 G = $1785.00 5/1/2005<br />
S3822 G = $210.00 5/1/2005<br />
S3823 G = $249.00 5/1/2005<br />
S3828 G = $420.00 5/1/2005<br />
S3829 G = $420.00 5/1/2005<br />
S3833 G = $540.00 5/1/2005<br />
S3834 G = $171.00 5/1/2005<br />
S3840 G = $256.80 5/1/2005<br />
S3841 G = $816.00 5/1/2005<br />
S3842 G = $477.00 5/1/2005<br />
S3843 G = $90.00 5/1/2005<br />
S3844 G = $258.00 5/1/2005<br />
S3845 G = $355.25 5/1/2005<br />
S3846 G = $355.25 5/1/2005<br />
S3847 G = $138.00 5/1/2005<br />
S3848 G = $138.00 5/1/2005<br />
S3849 G = $138.00 5/1/2005<br />
S3850 G = $253.75 5/1/2005<br />
S3851 G = $117.00 5/1/2005<br />
S3853 G = $253.75 5/1/2005<br />
S8093 4 = 11.45 RVUs<br />
I = 2.07 RVUs<br />
T = 9.38 RVUs<br />
5/1/2005<br />
S8270 9 = NC<br />
J = MR<br />
L = NC<br />
8/10/2005<br />
S9097 NC 5/1/2005<br />
For more information, call the <strong>TMHP</strong> Contact Center at<br />
1-800-925-9126 or the <strong>TMHP</strong>-CSHCN Contact Center at<br />
1-800-568-2413.<br />
Discontinued Codes<br />
The following is a list of procedure codes that have been<br />
discontinued by CMS and have no replacements. For a<br />
list of discontinued codes and their replacements and<br />
allowable amounts, see page 2.<br />
Discontinued Procedure Codes<br />
01964 15342 15343 15350 15351<br />
15810 15811 16010 16015 21493<br />
21494 31585 31586 32520 32522<br />
32525 33918 33919 37720 37730<br />
42325 42326 43638 43639 44200<br />
44201 44239 69410 76375 78160<br />
78162 78170 78172 78455 82273<br />
83715 83716 86064 86379 86585<br />
86587 90781 90788 90799 90871<br />
90939 92330 92335 92390 92391<br />
92392 92393 92395 92396 92510<br />
95858 96115 96408 96414 96545<br />
97020 97504 97520 97703 99141<br />
99142 99261 99262 99263 99271<br />
99272 99273 99274 99275 99321<br />
99322 99323 99331 99332 99333<br />
0023T 0033T 0034T 0035T 0036T<br />
0037T 0038T 0039T 0040T A4254<br />
A4260 A4643 A4644 A4645 A4646<br />
A4647 A4656 A5509 A5511 A6551<br />
A9511 A9513 A9514 A9515 A9519<br />
A9520 A9522 A9525 A9533 B4184<br />
B4186 C1080 C1081 C1082 C1083<br />
C1093 C1775 C9123 C9127 C9128<br />
C9202 C9203 C9205 C9206 C9211<br />
C9212 C9218 C9223 C9400 C9401<br />
C9402 C9403 C9404 C9405 C9410<br />
C9411 C9413 C9414 C9415 C9417<br />
C9418 C9419 C9420 C9421 C9422<br />
C9423 C9424 C9425 C9426 C9427<br />
C9428 C9429 C9430 C9431 C9432<br />
C9433 C9435 C9436 C9437 C9438<br />
C9439 C9440 C9704 C9713 C9718<br />
C9719 C9720 C9721 C9722 E0169<br />
E0590 E0752 E0754 E0756 E0757<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
19<br />
All Providers<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
All Providers<br />
Discontinued Procedure Codes<br />
E0758 E0759 E0953 E0954 E0972<br />
E0996 E1000 E1001 E1019 E1021<br />
E1025 E1026 E1027 E1210 E1211<br />
E1212 E1213 G0030 G0031 G0032<br />
G0033 G0034 G0035 G0036 G0037<br />
G0038 G0039 G0040 G0041 G0042<br />
G0043 G0044 G0045 G0046 G0047<br />
G0110 G0111 G0112 G0113 G0114<br />
G0115 G0116 G0125 G0210 G0211<br />
G0212 G0213 G0214 G0215 G0216<br />
G0217 G0218 G0220 G0221 G0222<br />
G0223 G0224 G0225 G0226 G0227<br />
G0228 G0229 G0230 G0231 G0232<br />
G0233 G0234 G0242 G0244 G0253<br />
G0254 G0258 G0263 G0264 G0279<br />
G0280 G0296 G0336 G0338 G0345<br />
G0346 G0347 G0348 G0349 G0350<br />
G0351 G0353 G0354 G0355 G0356<br />
G0357 G0358 G0359 G0360 G0361<br />
G0362 G0363 G0369 G0370 G0371<br />
G0374 G9021 G9022 G9023 G9024<br />
G9025 G9026 G9027 G9028 G9029<br />
G9030 G9031 G9032 J0880 J2324<br />
J7051 J7616 J7617 K0064 K0066<br />
K0067 K0068 K0074 K0075 K0076<br />
K0078 K0102 K0104 K0106 K0415<br />
K0416 K0452 K0600 K0620 K0628<br />
K0629 K0670 K0671 K0731 K0732<br />
L0860 L1750 L2039 L3963 L8100<br />
L8110 L8620 Q0187 Q1001 Q1002<br />
Q2001 Q2002 Q2003 Q2005 Q<strong>2006</strong><br />
Q2007 Q2008 Q2011 Q2012 Q2013<br />
Q2014 Q2018 Q2020 Q2021 Q2022<br />
Q3000 Q3002 Q3003 Q3004 Q3005<br />
Q3006 Q3007 Q3008 Q3009 Q3010<br />
Q3011 Q3012 Q4075 Q4076 Q4077<br />
Q9941 Q9942 Q9943 Q9944 S0114<br />
S0118 S0168 S2082 S2090 S2091<br />
S2215 S8434 T<strong>2006</strong><br />
For more information, call the <strong>TMHP</strong> Contact Center at<br />
1-800-925-9126 or the <strong>TMHP</strong>-CSHCN Contact Center<br />
at 1-800-568-2413.<br />
Description Changes<br />
The following procedure code descriptions have changed.<br />
Please contact the appropriate copyright holder to obtain<br />
procedure code descriptions.<br />
Description Changes<br />
0001F 0005F 0078T 15000<br />
15001 15100 15101 15120<br />
15121 15200 15201 15220<br />
15240 15260 15400 15401<br />
16020 16025 16030 2000F<br />
30130 30140 30801 30930<br />
31520 31525 31526 31530<br />
31531 31535 31536 31540<br />
31541 31560 31561 31570<br />
31571 33502 34833 34834<br />
36415 37209 4011F 43848<br />
44202 44310 44320 45119<br />
45540 45550 50688 52647<br />
52648 57421 61864 64613<br />
67901 67902 75900 76012<br />
77412 82270 83036 83898<br />
83901 84238 86920 86921<br />
86922 87904 88175 90657<br />
90658 90680 90713 90715<br />
90870 90940 91020 92506<br />
92507 92520 92568 92569<br />
95250 96405 96406 96420<br />
96422 96423 97024 97542<br />
97811 97813 97814 99050<br />
99056 99058 99298 A4215<br />
A4216 A4409 A4410 A4414<br />
A4415 A4554 A4630 A4632<br />
A4641 A4642 A6025 A6550<br />
A7032 A7033 A9500 A9502<br />
A9503 A9504 A9505 A9507<br />
A9508 A9510 A9512 A9516<br />
A9517 A9521 A9524 A9526<br />
A9528 A9529 A9530 A9531<br />
A9532 A9600 A9605 A9699<br />
B4100 B4149 C2634 C2635<br />
E0116 E0203 E0637 E0638<br />
E0761 E0935 E0971 E1038<br />
E1039 J7340 J7342 J7343<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 20 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Description Changes<br />
J7344 J7350 J7626 K0669<br />
L1832 L1843 L1844 L1845<br />
L1846 L2036 L2037 L2038<br />
L2405 L3170 L3215 L3216<br />
L3217 L3219 L3221 L3222<br />
L3230 L3906 L3923<br />
For more information, call the <strong>TMHP</strong> Contact Center at<br />
1-800-925-9126 or the <strong>TMHP</strong>-CSHCN Contact Center<br />
at 1-800-568-2413.<br />
Modifiers<br />
The modifiers QB, QQ, and QU have been discontinued<br />
by CMS.<br />
The following is a <strong>com</strong>plete list of new modifiers:<br />
Modifiers<br />
AQ FB J1 P1 P4 QR<br />
BL GR J2 P2 P5 27<br />
CR GS J3 P3 P6 63<br />
For more information, call the <strong>TMHP</strong> Contact Center at<br />
1-800-925-9126 or the <strong>TMHP</strong>-CSHCN Contact Center<br />
at 1-800-568-2413.<br />
ASC/HASC PROVIDERS<br />
ASC/HASC Code Additions<br />
Additions for ambulatory surgical center/hospital<br />
ambulatory surgical center (ASC/HASC) facilities<br />
are effective for dates of service on or after<br />
<strong>January</strong> 1, <strong>2006</strong>, and are listed with appropriate<br />
group payments in the <strong>2006</strong> <strong>HCPCS</strong> replacement<br />
and additions tables beginning on page 2. For more<br />
information, call the <strong>TMHP</strong> Contact Center at<br />
1-800-925-9126.<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
All Providers / ASC/HASC Providers / Home Health Providers<br />
21<br />
HOME HEALTH PROVIDERS<br />
Title XIX Home Health<br />
Policy Updates<br />
The following policy updates have been made to support<br />
the <strong>2006</strong> <strong>HCPCS</strong> implementation.<br />
Trapeze Bars<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure codes J/L-E0911 and J/L-E0912 are benefits<br />
of Title XIX Home Health Services when submitted with<br />
documentation of medical necessity and prior authorized.<br />
Purchase is limited to one per five years, and rental is<br />
limited to once per month.<br />
Standing Frames and Wheelchair Accessories<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
the following procedure codes are benefits of Title XIX<br />
Home Health Services when submitted with documentation<br />
of medical necessity and prior authorized.<br />
Procedure Codes<br />
J-E0641 J-E0705 J-E2207 J-E2208<br />
J-E2209 J-E2210 J-E2211 J-E2212<br />
J-E2213 J-E2214 J-E2215 J-E2216<br />
J-E2217 J-E2218 J-E2219 J-E2220<br />
J-E2221 J-E2222 J-E2223 J-E2224<br />
J-E2225 J-E2226 J-E2371 J-E2372<br />
Purchase of the above procedure codes is limited to one<br />
per five years.<br />
Powered Wheelchairs<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure codes J-E1019, J-E1021, J-E1210, J-E1211,<br />
J-E1212, and J-E1213 are no longer benefits of the Texas<br />
Medicaid Program.<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure codes J/L-K0010, J/L-K0011, and J/L-K0012<br />
are benefits of Title XIX Home Health Services with prior<br />
authorization.<br />
The codes in the following table will deny as part of<br />
another service if billed with procedure codes J/L-K0010,<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
THSteps-CCP Providers / CSHCN Providers<br />
J/L-K0011, or J/L-K0012, which are considered for reimbursement<br />
only when billed as replacement parts.<br />
Procedure Codes<br />
J-E0970 J-E0971 J-E0973 J-E0981<br />
J-E0982 J-E0990 J-E0994 J-E0995<br />
J-E0996 J-E0997 J-E0998 J-E0999<br />
J-E1000 J-E1001 J-E2210 J-E2366<br />
J-E2368 J-E2369 J-E2370<br />
For more information, call the <strong>TMHP</strong> Contact Center<br />
at 1-800-925-9126.<br />
THSTEPS-CCP PROVIDERS<br />
Standing Frames<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure code J-E0642 is a benefit of the Texas Health<br />
Steps-Comprehensive Care Program (THSteps-CCP) for<br />
clients under 21 years of age when submitted with documentation<br />
of medical necessity and prior authorized.<br />
For more information, please call the <strong>TMHP</strong> Contact<br />
Center at 1-800-925-9126.<br />
CSHCN PROVIDERS<br />
CSHCN Program Policy Updates<br />
The following Children with <strong>Special</strong> Health Care Needs<br />
(CSHCN) Services Program policy changes have been<br />
made to support the 2005 <strong>HCPCS</strong> implementation.<br />
Powered Wheelchairs<br />
Due to the deletion of <strong>HCPCS</strong> procedure codes J-E1019,<br />
J-E1210, J-E1211, J-E1212, and J-E1213, effective for<br />
dates of service on or after <strong>January</strong> 1, <strong>2006</strong>, procedure<br />
codes J/L-K0010, J/L-K0011, and J/L-K0012 are<br />
benefits of the CSHCN Services Program with prior<br />
authorization.<br />
The codes in the following table will deny as part of<br />
another service if billed with procedure codes J/L-K0010,<br />
J/L-K0011, or J/L-K0012, which are considered for<br />
reimbursement only when billed as replacement parts.<br />
Procedure Codes<br />
J-E0970 J-E0971 J-E0973 J-E0981<br />
J-E0982 J-E0990 J-E0994 J-E0995<br />
J-E0996 J-E0997 J-E0998 J-E0999<br />
J-E1000 J-E1001 J-E2210 J-E2366<br />
J-E2368 J-E2369 J-E2370<br />
Antihemophilic Factors<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
1-Q0187 and 1-Q2022 are no longer benefits of the<br />
CSHCN Services Program.<br />
Procedure codes 1-J7188 and 1-J7189 are benefits of the<br />
CSHCN Services Program. Procedure code 1-J7188 is<br />
limited to diagnosis code 286.4, and procedure code<br />
1-J7189 is limited to diagnosis codes 286.0 and 286.1.<br />
Lipids<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure code 9-B4185 is a benefit of the CSHCN<br />
Services Program for diagnosis codes 042, 140.0–208.9,<br />
277.0–277.09, or 555.0–555.9. Procedure code 9-B4185<br />
must be authorized if requested for diagnoses other<br />
than 042, 140.0–208.9, 277.0–277.09, or 555.0–555.9.<br />
Procedure code 9-B4185 is reimbursed on a daily basis,<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 22 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
ut will be denied as part of another service if hyperalimentation/total<br />
parenteral nutrition is billed on the same<br />
date of service.<br />
Trapeze Bars<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
procedure codes J/L-E0911 and J/L-E0912 are benefits<br />
of the CSHCN Services Program when submitted with<br />
documentation of medical necessity and authorized.<br />
Purchase is limited to one per five years and rental is<br />
limited to once per month.<br />
Standing Frames and Wheelchair Accessories<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
the following procedure codes are benefits of the CSHCN<br />
Services Program when submitted with documentation of<br />
medical necessity and authorized.<br />
Procedure Codes<br />
J-E0641 J-E0705 J-E2207 J-E2208<br />
J-E2209 J-E2210 J-E2211 J-E2212<br />
J-E2213 J-E2214 J-E2215 J-E2216<br />
J-E2217 J-E2218 J-E2219 J-E2220<br />
J-E2221 J-E2222 J-E2223 J-E2224<br />
J-E2225 J-E2226 J-E2371 J-E2372<br />
Purchase of the above procedure codes is limited to one<br />
per five years.<br />
Incidental Services<br />
Effective for dates of service on or after <strong>January</strong> 1, <strong>2006</strong>,<br />
the following procedure codes are benefits of the CSHCN<br />
Services Program:<br />
Procedure Codes<br />
1-90760 1-90761 1-90765 1-90766 1-90767<br />
1-90768 1-96521 1-96522 1-96523<br />
The above procedure codes will be denied as part of<br />
another service if billed in conjunction with a surgical or<br />
anesthesia procedure.<br />
For more information, call the <strong>TMHP</strong>-CSHCN Contact<br />
Center at 1-800-568-2413.<br />
CSHCN <strong>HCPCS</strong> Additions<br />
New <strong>HCPCS</strong> codes, applicable rates, and related requirements<br />
for the CSHCN Services Program can be found in<br />
the <strong>HCPCS</strong> replacement and additions tables beginning<br />
on page 2. CSHCN follows Medicaid covered services<br />
and allowable amounts with the following exceptions:<br />
Procedure Code TOS / Allowable<br />
01965 NC<br />
01966 NC<br />
88333 5 = 2.36 RVUs<br />
I = 1.77 RVUs<br />
T = 0.59 RVUs<br />
88334 5 = 1.23 RVUs<br />
I = 0.87 RVUs<br />
T = 0.36 RVUs<br />
90714 1 = $17.85<br />
96101 NC<br />
96415 1 = 1.03 RVUs<br />
96417 1 = 1.07 RVUs<br />
97761 1 = $35.00<br />
C= NC<br />
99304 NC<br />
99305 NC<br />
99306 NC<br />
99307 NC<br />
99308 NC<br />
99309 NC<br />
99310 NC<br />
99318 NC<br />
99324 NC<br />
99325 NC<br />
99326 NC<br />
99327 NC<br />
99328 NC<br />
99334 NC<br />
99335 NC<br />
99336 NC<br />
99337 NC<br />
99340 NC<br />
J1640 1 = $6.51<br />
J7188 1 = MR<br />
J7189 1 = MR<br />
28890 NC<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
23<br />
CSHCN Providers<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
CSHCN Providers<br />
Procedure Code TOS / Allowable<br />
43770 NC<br />
43771 NC<br />
43772 NC<br />
43773 NC<br />
43774 NC<br />
E0170 9 = NC<br />
J = MR<br />
L = NC<br />
E0171 9 = NC<br />
J = MR<br />
L = NC<br />
E0172 9 = NC<br />
J = MR<br />
L = NC<br />
S3626 NC<br />
For more inforamtion, call the <strong>TMHP</strong>-CSHCN Contact<br />
Center at 1-800-568-2413.<br />
2005 Quarterly Additions<br />
The Centers for Medicare & Medicaid Services (CMS)<br />
updated <strong>HCPCS</strong> codes on a quarterly basis in 2005. A<br />
<strong>com</strong>plete list of <strong>HCPCS</strong> codes implemented throughout<br />
2005 can be found in the “2005 Quarterly Additions”<br />
table on page 17. The following exceptions to the codes<br />
found in that table exist for the CSHCN Services<br />
Program:<br />
Procedure Code TOS / Allowable Effective Date<br />
C9224 1 = $1,621.74 11/16/2005<br />
C9225 1 = $19,600.50 11/16/2005<br />
Q4080 1 = $31.52 11/16/2005<br />
S3625 NC 5/1/2005<br />
S3626 NC 11/16/2005<br />
S3820 NC 5/1/2005<br />
S3822 NC 5/1/2005<br />
S3823 NC 5/1/2005<br />
S3828 NC 5/1/2005<br />
S3829 NC 5/1/2005<br />
S3833 NC 5/1/2005<br />
S3834 NC 5/1/2005<br />
S3840 NC 5/1/2005<br />
S3841 NC 5/1/2005<br />
Procedure Code TOS / Allowable Effective Date<br />
S3842 NC 5/1/2005<br />
S3843 NC 5/1/2005<br />
S3844 NC 5/1/2005<br />
S3845 NC 5/1/2005<br />
S3846 NC 5/1/2005<br />
S3847 NC 5/1/2005<br />
S3848 NC 5/1/2005<br />
S3849 NC 5/1/2005<br />
S3850 NC 5/1/2005<br />
S3851 NC 5/1/2005<br />
S3853 NC 5/1/2005<br />
For more information, call the <strong>TMHP</strong>-CSHCN Contact<br />
Center at 1-800-568-2413.<br />
Prior Authorization Update<br />
Effective <strong>January</strong> 1, <strong>2006</strong>, the <strong>2006</strong> <strong>HCPCS</strong> deleted<br />
procedure codes are no longer reimbursed by the<br />
CSHCN Services Program. Providers who have received<br />
authorizations for dates of service that occur on or after<br />
<strong>January</strong> 1, <strong>2006</strong>, will need to submit a written request on<br />
the appropriate, <strong>com</strong>pleted CSHCN authorization request<br />
form in order to update the <strong>HCPCS</strong> procedure code(s)<br />
authorized for those services, except for the procedure<br />
codes listed below. Authorizations for the codes below will<br />
be updated by <strong>TMHP</strong> and require no action on the part<br />
of the provider.<br />
Procedure Codes<br />
33918 33919 44200 97504<br />
97520 97703 A5119 K0618<br />
K0619 K0620 K0630 - K0649 L0860<br />
L8100 L8110 L8120 L8130<br />
L8140 L8150 L8160 L8170<br />
L8180 L8190 L8195 L8200<br />
L8210 L8220 L8230 L8239<br />
Important: Please do not request changes to authorizations<br />
prior to <strong>January</strong> 13, <strong>2006</strong> (see “<strong>2006</strong> <strong>HCPCS</strong><br />
Implementation” on page 1).<br />
Background<br />
Authorization is a condition for reimbursement. It is not<br />
a guarantee of payment. Each provider must be enrolled<br />
A = Authorization Required; MR = Manually Reviewed; NC = <strong>No</strong>n-Covered Service; PA = Prior Authorization Required;<br />
RVU = Relative Value Unit; ** = CSHCN and Comprehensive Care Program (CCP) Only<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 24 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
and eligible, and must verify client eligibility. Any services<br />
provided while the client is not eligible, or services<br />
provided beyond the limitation of the CSHCN Services<br />
Program, are not reimbursed.<br />
<strong>TMHP</strong> sends notification to the client when an authorization<br />
approval, denial, or reduction in requested services<br />
letter is sent to his or her provider. Refer to the specific<br />
provider sections of the <strong>2006</strong> CSHCN Provider Manual—<br />
Part I for more details on the services that require authorization<br />
or prior authorization. Fax transmittal confirmations<br />
and postal registered mail receipts are not accepted<br />
as proof of timely authorization submission.<br />
An authorization is a request submitted to the program<br />
to provide a service the program may consider for<br />
reimbursement. The request must be submitted on a<br />
program-approved form and must contain all information<br />
necessary for the program to make a determination<br />
regarding coverage. The request may be submitted before<br />
the service is provided, but must not be received by the<br />
program more than 90 days following the date the service<br />
was provided. If the service was already provided, the<br />
authorization form may be attached to the claim, as long<br />
as it is received within the authorization (90-day) deadline.<br />
Only <strong>com</strong>plete authorization requests may be accepted<br />
by the program. <strong>No</strong> extensions beyond the 90-day initial<br />
deadline are given for providers to correct in<strong>com</strong>plete<br />
authorization requests. This 90-day deadline applies to all<br />
services requiring authorization (not prior authorization,<br />
including extensions and emergency situations).<br />
In<strong>com</strong>plete authorization requests, or claims for services<br />
requiring authorization but submitted without an attached<br />
authorization form or all required documentation, are<br />
denied and are reconsidered only when resubmitted and<br />
received by the program within the initial 90-day authorization<br />
deadline. Requests to extend the deadline beyond<br />
90-days from the date of service are not considered.<br />
A prior authorization is a request submitted to the<br />
program to provide a service the program may consider<br />
for reimbursement. The request must be submitted on a<br />
program-approved form and must contain all information<br />
necessary for the program to make a determination<br />
regarding coverage. Prior authorization must be obtained<br />
before the delivery of the service. However, when the<br />
service is provided after hours or on a <strong>TMHP</strong>-recognized<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
25<br />
CSHCN Providers<br />
holiday or weekend, services may be prior authorized<br />
when authorization is requested on the next working<br />
day. A <strong>com</strong>plete form must be received according to these<br />
deadlines for prior authorization to be considered. The<br />
program does not grant extensions to these deadlines to<br />
allow providers to correct and resubmit in<strong>com</strong>plete prior<br />
authorization requests.<br />
In<strong>com</strong>plete prior authorization requests are denied and<br />
are reconsidered only when <strong>com</strong>pleted and received by the<br />
program before the service is provided. The prior authorization<br />
requirement may be waived if the clients eligibility<br />
had not been determined when the request was received<br />
by <strong>TMHP</strong>. Claims for these services must be received<br />
within 95 days of the eligibility add date.<br />
All inpatient admission/stays or inpatient rehabilitation<br />
admissions, including extensions of any previously<br />
authorized inpatient stays, must be prior authorized. The<br />
request may be submitted by the hospital, provided that<br />
all required information indicating inpatient admission is<br />
on the request form. Both the facility and the physician/<br />
supplier must be enrolled in the CSHCN Services<br />
Program for either inpatient or outpatient claims to be<br />
considered for reimbursement.<br />
Providers must mail or fax written authorization requests,<br />
along with all other applicable documentation, to the<br />
following address:<br />
Texas Medicaid & Healthcare Partnership<br />
ATTN: CSHCN Authorizations, MC-A11<br />
12357-B Riata Trace Parkway<br />
Austin, TX 78727<br />
Fax: 1-512-514-4222<br />
Providers must mail or fax written prior authorization<br />
requests, along with all other applicable documentation,<br />
to the following address:<br />
Texas Medicaid & Healthcare Partnership<br />
ATTN: CSHCN Authorizations, MC-<strong>193</strong>8<br />
12357-B Riata Trace Parkway<br />
Austin, TX 78727<br />
Fax: 1-512-514-4222<br />
For more information call the <strong>TMHP</strong>-CSHCN Contact<br />
Center at 1-800-568-2413.<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
Forms<br />
Provider Information Change Form<br />
Traditional Medicaid, Children with <strong>Special</strong> Health Care Needs (CSHCN), and Primary Care Case Management (PCCM)<br />
providers can <strong>com</strong>plete and submit this form to update their provider enrollment file. Print or type all of the information on<br />
this form. Mail or fax the <strong>com</strong>pleted form and any additional documentation to the address at the bottom of the page.<br />
Check the box to indicate a PCCM Provider Date:<br />
9-digit Texas Provider Identifier (TPI): Provider Name:<br />
List any additional TPIs that use the same provider information:<br />
TPI:______________________ TPI:______________________ TPI:______________________<br />
TPI:______________________ TPI:______________________ TPI:______________________<br />
Physical Address* Accounting/Mailing Address** Secondary Address<br />
City: City: City:<br />
State: ZIP: State: ZIP: State: ZIP:<br />
Phone:<br />
( )<br />
Phone:<br />
( )<br />
Fax: Fax: Fax:<br />
Phone:<br />
Email: Email: Email:<br />
Type of Change: (Check the appropriate box below.)<br />
Change of physical address, telephone, and/or fax number<br />
Change of billing/mailing address, telephone, and/or fax number<br />
Change/Add secondary address, telephone, and/or fax number<br />
Change of provider status (e.g., termination from plan, moved out of area, specialist)<br />
Explain in the Comments field<br />
Other (e.g., panel closing, capacity changes, and age acceptance)<br />
Comments:<br />
Tax Information—Tax Identification (ID) Number and Name for the Internal Revenue Service (IRS)<br />
Tax ID Number: Effective Date:<br />
Exact name reported to the IRS for this Tax ID:<br />
The signature and date are required or the form will not be processed.<br />
Provider Signature: Date:<br />
Mail or fax the<br />
<strong>com</strong>pleted form to:<br />
Texas Medicaid & Healthcare Partnership (<strong>TMHP</strong>)<br />
Provider Enrollment MC-B05<br />
PO Box 200795<br />
Austin, TX 78720-0795<br />
( )<br />
Fax: 1-512-514-4214<br />
* The physical address cannot be a PO Box. Traditional Medicaid providers who change their ZIP code must submit a copy of the Medicare<br />
letter along with this form.<br />
** All providers who make changes to the Accounting/Mailing address must submit a copy of the W-9 Form along with this form.<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 26 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Instructions for Completing the<br />
Provider Information Change Form<br />
Signatures:<br />
The provider’s signature is required on the Provider Information Change Form for any and all<br />
changes requested for individual provider numbers.<br />
A signature by the authorized representative of a group or facility is acceptable for requested<br />
changes to group or facility provider numbers.<br />
Address:<br />
Performing providers (physicians performing services within a group) may not change<br />
accounting information.<br />
For Traditional Medicaid, changes to the accounting or mailing address require a copy of the<br />
W9 form.<br />
For Traditional Medicaid, a change in ZIP code requires copy of the Medicare letter.<br />
Tax Identification Number (TIN):<br />
TIN changes for individual practitioner provider numbers can only be made by the individual to<br />
whom the number is assigned.<br />
Performing providers cannot change the TIN.<br />
General:<br />
Forms will be returned unprocessed if the nine-digit provider number is not indicated on the<br />
Provider Information Change Form.<br />
The W-9 form is required for all name and TIN changes.<br />
Mail or fax the <strong>com</strong>pleted form to:<br />
Texas Medicaid & Healthcare Partnership (<strong>TMHP</strong>)<br />
Provider Enrollment MC-B05<br />
PO Box 200795<br />
Austin, TX 78720-0795<br />
Fax: 1-512-514-4214<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
27<br />
Forms<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
Forms<br />
Electronic Funds Transfer (EFT) Information<br />
Electronic Funds Transfer (EFT) is a payment method to deposit funds for claims<br />
approved for payment directly into a provider’s bank account. These funds can be<br />
credited to either checking or savings accounts, provided the bank selected accepts<br />
Automated Clearinghouse (ACH) transactions. EFT also avoids the risks associated<br />
with mailing and handling paper checks, ensuring funds are directly deposited into a<br />
specified account.<br />
The following items are specific to EFT:<br />
Applications are processed within five workdays of receipt.<br />
Pre–notification to your bank takes place on the cycle following the application<br />
processing.<br />
Future deposits are received electronically after pre–notification.<br />
The Remittance and Status (R&S) report furnishes the details of individual credits<br />
made to the provider’s account during the weekly cycle.<br />
Specific deposits and associated R&S reports are cross–referenced by both<br />
Texas Provider Identifier (TPI) and R&S number.<br />
EFT funds are released by <strong>TMHP</strong> to depository financial institutions each Friday.<br />
The availability of R&S reports is unaffected by EFT and they continue to arrive<br />
in the same manner and time frame as currently received.<br />
<strong>TMHP</strong> must provide the following notification according to ACH guidelines:<br />
Most receiving depository financial institutions receive credit entries on the day<br />
before the effective date, and these funds are routinely made available to their<br />
depositors as of the opening of business on the effective date. Please contact<br />
your financial institution regarding posting time if funds are not available on the<br />
release date.<br />
However, due to geographic factors, some receiving depository financial<br />
institutions do not receive their credit entries until the morning of the effective day<br />
and the internal records of these financial institutions will not be updated. As a<br />
result, tellers, bookkeepers, or automated teller machines (ATMs) may not be<br />
aware of the deposit and the customer’s withdrawal request may be refused.<br />
When this occurs, the customer or <strong>com</strong>pany should discuss the situation with the<br />
ACH coordinator of their institution who, in turn should work out the best way to<br />
serve their customer’s needs.<br />
In all cases, credits received should be posted to the customer’s account on the<br />
effective date and thus be made available to cover checks or debits that are<br />
presented for payment on the effective date.<br />
To enroll in the EFT program, <strong>com</strong>plete the attached Electronic Funds Transfer<br />
Authorization Agreement. You must return a voided check or deposit slip with the<br />
agreement to the <strong>TMHP</strong> address indicated on the form.<br />
Contact <strong>TMHP</strong> Customer Service at 1–800–925–9126 if you need assistance.<br />
Page 1 of 2 EFTAG11.17.2003_v1.0<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 28 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
Electronic Funds Transfer (EFT) Authorization Agreement<br />
Enter ONE Texas Provider Identifier (TPI) per Form<br />
NOTE: Complete all sections below and attach a voided check or a photocopy of your<br />
deposit slip.<br />
Type of Authorization: NEW CHANGE<br />
Provider Name Nine–Character Billing TPI<br />
Provider Accounting Address Provider Phone Number<br />
Street Address or PO Box City State Zip<br />
Bank Name ABA/Transit Number<br />
Bank Phone Number Account Number<br />
Bank Address Type Account (check one)<br />
Street Address or PO Box City State Zip<br />
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
Page 2 of 2 EFTAG11.17.2003_v1.0<br />
29<br />
ext.<br />
Checking Savings<br />
I (we) hereby authorize Texas Medicaid & Healthcare Partnership (<strong>TMHP</strong>) to present credit entries into<br />
the bank account referenced above and the depository named above to credit the same to such account.<br />
I (we) understand that I (we) am responsible for the validity of the information on this form. If the <strong>com</strong>pany<br />
erroneously deposits funds into my (our) account, I (we) authorize the <strong>com</strong>pany to initiate the necessary<br />
debit entries, not to exceed the total of the original amount credited for the current pay period.<br />
I (we) agree to <strong>com</strong>ply with all certification requirements of the applicable program regulations, rules,<br />
handbooks, bulletins, standards, and guidelines published by the Texas Health and Human Services<br />
Commission (HHSC) or its health insuring contractor. I (we) understand that payment of claims will be<br />
from federal and state funds, and that any falsification or concealment of a material fact may be<br />
prosecuted under federal and state laws.<br />
I (we) will continue to maintain the confidentiality of records and other information relating to clients in<br />
accordance with applicable state and federal laws, rules, and regulations.<br />
Authorized Signature<br />
Date<br />
Title Email Address (if applicable)<br />
Contact Name Phone<br />
DO NOT WRITE IN THIS AREA — For Office Use<br />
Return this form to:<br />
Texas Medicaid & Healthcare Partnership<br />
ATTN: Provider Enrollment<br />
PO Box 200795<br />
Austin TX 78720–0795<br />
Input By: Input Date:<br />
Forms<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
<strong>No</strong>tes<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong> 30 <strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong>
<strong>2006</strong> <strong>HCPCS</strong> <strong>Special</strong> <strong>Bulletin</strong><br />
31<br />
<strong>No</strong>tes<br />
Texas Medicaid <strong>Bulletin</strong>, <strong>No</strong>. <strong>193</strong>
Current Procedural Terminology (CPT) is copyright <strong>2006</strong> American Medical Association (AMA), and Current Dental Terminology (CDT) is copyright <strong>2006</strong> American Dental Association (ADA).<br />
All Rights Reserved. <strong>No</strong> fee schedules, basic units, relative values, or related listings are included in CPT or CDT. The AMA and the ADA assume no liability for the data contained herein.<br />
Applicable Federal Acquisition Regulation System/Department of Defense Regulation System (FARS/DFARS) restrictions apply to government use.<br />
PLACE POSTAGE<br />
HERE<br />
ATTENTION: BUSINESS OFFICE<br />
<strong>No</strong>. <strong>193</strong><br />
Texas Medicaid<br />
<strong>2006</strong> Healthcare Common Procedure Coding System (<strong>HCPCS</strong>) <strong>Special</strong> <strong>Bulletin</strong>