Sudden Cardiac Death - University of Mississippi Medical Center
Sudden Cardiac Death - University of Mississippi Medical Center
Sudden Cardiac Death - University of Mississippi Medical Center
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
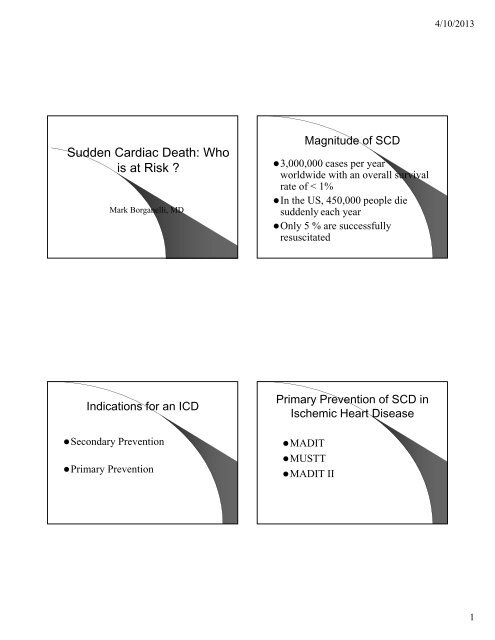
<strong>Sudden</strong> <strong>Cardiac</strong> <strong>Death</strong>: Who<br />
is at Risk ?<br />
Mark Borganelli, MD<br />
Indications for an ICD<br />
Secondary Prevention<br />
Primary Prevention<br />
Magnitude <strong>of</strong> SCD<br />
3,000,000 cases per year<br />
worldwide with an overall survival<br />
rate <strong>of</strong> < 1%<br />
In the US, 450,000 people die<br />
suddenly each year<br />
Only 5 % are successfully<br />
resuscitated<br />
Primary Prevention <strong>of</strong> SCD in<br />
Ischemic Heart Disease<br />
MADIT<br />
MUSTT<br />
MADIT II<br />
4/10/2013<br />
1
1232 patients<br />
Prior MI (> 4 weeks)<br />
EF
SCD-HeFT Protocol<br />
Inclusion criteria<br />
Placebo n=847 Amiodarone n=845<br />
ICD implant n=829<br />
40 months average follow- up<br />
• Optimize: B, ACE-I, Diuretics<br />
Bardy GH. Chapter Excerpt from Arrhythmia Treatment and Therapy. Woosley RL, Singh SN, editors. Marcel Dekker, 1 st edition. 2000;323-42.<br />
SCD-HeFT Investigators Meeting, August 2001, data from most recent follow-up<br />
4/10/2013<br />
3
Causes <strong>of</strong> SCD in Young People<br />
Congenital coronary<br />
anomalies<br />
(19%)<br />
HCM<br />
(36%)<br />
Maron BJ et al. Circulation. 1996;94:850-56.<br />
Mildly increased cardiac mass<br />
(10%)<br />
Ruptured aorta 5%<br />
Tunnelled LAD 5%<br />
Aortic stenosis 4%<br />
Myocarditis 3%<br />
Dilated cardiomyopathy<br />
3%<br />
ARVC 3%<br />
MVP 2%<br />
CAD 2%<br />
Other 6%<br />
Hank Gathers and HCM<br />
(hypertrophic cardiomyopathy)<br />
The first sign <strong>of</strong> trouble came December 9, 1989, in Santa Barbara, California. Six minutes into the second half, Hank Gathers, the All-<br />
American forward for Loyola Marymount, drove to the basket and was fouled. When he went to the foul line, he felt an unusual<br />
sensation. His heart was pounding faster than he had ever noticed. He bounced the ball then launched a shot. He missed. Then, he<br />
collapsed. Coaches and the school's medical personnel immediately rushed to Gathers' side. Within seconds, he rose to his feet and<br />
walked <strong>of</strong>f the court. Yet something was wrong. Drastically wrong.<br />
He was later diagnosed as having an abnormal heartbeat and treated with Inderal, one <strong>of</strong> a class <strong>of</strong> beta blocker drugs that inhibits the<br />
effects <strong>of</strong> adrenaline and smoothes the hearts rhythms. But Gathers detested the drug. He agonized over having to take it. The drug<br />
made him sluggish, moody. His game suffered. He was unable to run the court without getting tired. His shot was <strong>of</strong>f. He'd get woozy<br />
at times. He'd sleep longer.Gathers continually complained to his coaches and doctors about the drug, that the dosage had to be<br />
reduced. They said no. So gradually, Gathers began cutting down on the dosage, and began feeling much better. He also began<br />
skipping some <strong>of</strong> the required testing. He was playing a risky game.<br />
On the morning <strong>of</strong> March 4, 1990, Gathers awakes with excitement. LMU is on its way to the West Coast Conference tournament<br />
championship and a NCAA tournament berth. On the court with his best friend, Bo Kimble, LMU's other brilliant player, Gathers<br />
wins the game's opening tip and LMU is <strong>of</strong>f and running, building a huge lead over outmatched Portland State.<br />
There is 13:34 left in the first half and LMU leads 25-13. <strong>Sudden</strong>ly, Gathers falls to the court. The crowd gasps. He tries to get up, but<br />
slumps back to the floor, unable to muster enough strength. Portland's Josh Lowery, standing over Gathers, extends his hand,<br />
attempting to help him up. But Gathers can't acknowledge it. LMU trainer Chip Schaefer flies <strong>of</strong>f the bench. When he arrives, Gathers'<br />
body starts to go into convulsions. Team physicians rush to his side. He has a pulse, but he is unable to comprehend what is<br />
happening. He is removed from the court on a stretcher, and as soon as the medical staff gets outside the gym door, they hook him up<br />
to the school's defibrillator, which was purchased a few months earlier specifically for Gathers, a device that is actually supposed to be<br />
courtside in case he collapses. Taken <strong>of</strong>f court, an external automatic external defibrillator is used to shock the fibrillating heart<br />
Rescue Ambulance 5 <strong>of</strong> the Los<br />
Angeles Fire Dept. arrives only<br />
seven minutes after Gathers first<br />
collapsed. The rescue vehicle<br />
speeds <strong>of</strong>f to Daniel Freeman<br />
Marina Hospital, two miles away.<br />
Gathers arrives at the hospital<br />
only 24 minutes after he first<br />
collapsed. Emergency personnel<br />
work frantically on him for more<br />
than an hour. Finally, two doctors<br />
emerge from the emergency<br />
Hank suffered from hypertrophic<br />
room. They stonily walk toward<br />
If used < 3 min<br />
Gathers' family and friends.<br />
cardiomyopathy (HCM), a genetic<br />
An AED can<br />
condition where the heart muscle is<br />
They stop. The situation is clear. save over 80%<br />
thickened and is the most common<br />
<strong>Sudden</strong>ly, a woman's shriek <strong>of</strong> SCA victims<br />
cause <strong>of</strong> cardiac arrest in the young<br />
pierces the air. "Oh my God.<br />
He's gone. He's gone."<br />
Hypertrophic Cardiomyopathy<br />
Prevalence 1:300 to 1:600<br />
More common in African Americans<br />
More than 100 gene mutations identified<br />
LV outflow obstruction in 30%<br />
<strong>Sudden</strong> death from ventricular arrhythmia<br />
Most common cause <strong>of</strong> athlete cardiac sudden<br />
death (under age 35)<br />
4/10/2013<br />
4
Etiology<br />
Genetic disease with Autosomal-Dominant<br />
inheritance<br />
Familial (inherited) versus Sporadic (de novo<br />
mutation)<br />
Parents transmit the gene to 50% <strong>of</strong> <strong>of</strong>fspring<br />
Gene mutations code for a sarcomere protein<br />
(most <strong>of</strong>ten beta-myosin heavy chain gene,<br />
myosin binding protein C gene, or troponin T<br />
gene).<br />
Synonyms for Hypertrophic Cardiomyopathy<br />
Asymmetrical hypertrophic cardiomyopathy<br />
Asymmetrical hypertrophy <strong>of</strong> the heart<br />
Asymmetrical septal hypertrophy<br />
Brock's disease<br />
Diffuse muscular subaortic stenosis<br />
Diffuse subvalvular aortic stenosis<br />
Dynamic hypertrophic subaortic stenosis<br />
Dynamic muscular subaortic stenosis<br />
Familial hypertrophic cardiomyopathy<br />
Familial hypertrophic subaortic stenosis<br />
Familial muscular subaortic stenosis<br />
Familial myocardial disease<br />
Functional aortic stenosis<br />
Functional hypertrophic subaortic stenosis<br />
Functional obstructive cardiomyopathy<br />
Functional obstruction <strong>of</strong> the left ventricle<br />
Functional obstructive subvalvular aortic stenosis<br />
Functional subaortic stenosis<br />
Hereditary cardiovascular dysplasia<br />
Hypertrophic cardiomyopathy<br />
Hypertrophic constrictive cardiomyopathy<br />
Hypertrophic hyperkinetic cardiomyopathy<br />
Hypertrophic infundibular aortic stenosis<br />
Hypertrophic nonobstructive cardiomyopathy<br />
Hypertrophic obstructive cardiomyopathy<br />
Hypertrophic stenosing cardiomyopathy<br />
Hypertrophic subaortic stenosis<br />
Idiopathic hypertrophic cardiomyopathy<br />
Idiopathic hypertrophic obstructive cardiomyopathy<br />
Idiopathic hypertrophic subaortic stenosis<br />
Idiopathic hypertrophic subvalvular stenosis<br />
Idiopathic muscular hypertrophic subaortic stenosis<br />
Idiopathic muscular stenosis <strong>of</strong> the left ventricle<br />
Idiopathic myocardial hypertrophy<br />
Idiopathic ventricular septal hypertrophy<br />
Irregular hypertrophic cardiomyopathy<br />
Left ventricle muscular stenosis<br />
Low subvalvular aortic stenosis<br />
Muscular aortic stenosis<br />
Muscular hypertrophic stenosis <strong>of</strong> the left ventricle<br />
Muscular stenosis <strong>of</strong> the left ventricle<br />
Muscular subaortic stenosis<br />
Muscular subvalvular aortic stenosis<br />
Non-dilated cardiomyopathy<br />
Nonobstructive hypertrophic cardiomyopathy<br />
Obstructive cardiomyopathy<br />
Obstructive hypertrophic aortic stenosis<br />
Obstructive hypertrophic cardiomyopathy<br />
Obstructive hypertrophic myocardiopathy<br />
Obstructive myocardiopathy<br />
Pseudoaortic stenosis<br />
Stenosing hypertrophy <strong>of</strong> the left ventricle<br />
Stenosis <strong>of</strong> the ejection chamber <strong>of</strong> the left ventricle<br />
Subaortic hypertrophic stenosis<br />
Subaortic idiopathic stenosis<br />
Subaortic muscular stenosis<br />
Subvalvular aortic stenosis <strong>of</strong> the muscular type<br />
Teare's disease<br />
Pathophysiology<br />
Change in sarcomere structure leads to change<br />
in function<br />
Release <strong>of</strong> growth factors that result in<br />
hypertrophy and fibroblast proliferation<br />
(interstitial fibrosis).<br />
Electrically unstable substrate<br />
- disorganized myocardial architecture (disarray)<br />
- ischemia-related replacement scarring<br />
4/10/2013<br />
5
Hypertrophic Cardiomyopathy<br />
4/10/2013<br />
6
ICD-HCM Trial:<br />
Arrhythmias Triggering ICD Interventions<br />
VTVF<br />
14%<br />
VT and VF<br />
9%<br />
VT 48%<br />
Bradyarrhythmias = 0<br />
Maron BJ, et al. N Engl J Med. 2000;342:365-373.<br />
Maron BJ, Bonow RO, Cannon RO III, Leon MB, Epstein SE. Hypertrophic cardiomyopathy:<br />
interrelations<br />
<strong>of</strong> clinical manifestations, pathophysiology, and therapy. N Engl J Med. 1987;316:780-9, 844-<br />
52.<br />
4/10/2013<br />
7
The implantable defibrillator<br />
titanium casing<br />
capacitor(s)<br />
battery<br />
lead(s)<br />
circuitry<br />
header<br />
Hypertrophic Cardiomyopathy<br />
Secondary prevention<br />
Family history <strong>of</strong> SCD<br />
Unexplained syncope<br />
Age younger than 40<br />
Abnormal BP response to exercise<br />
Severe LVH (particularly if wall > 30mm)<br />
A<br />
B<br />
C<br />
D<br />
Case Presentation<br />
• 22 y/o AAM superstar basketball<br />
player drafted by the Celtics<br />
• Took Bird’s place as the superstar<br />
averaging over 20 points a game<br />
• Had 6 bad dizzy spells over a 4<br />
month period<br />
• Collapsed in a play<strong>of</strong>f game in 1993<br />
• Team doctor allowed him to<br />
continue to play in the second half<br />
• Taken to a hospital in Boston<br />
afterwards<br />
4/10/2013<br />
8
• Noted to have NSVT on monitor<br />
• Thallium, MR, and cath done<br />
• Cath revealed normal coronaries but there was<br />
clear large apical WMA and perfusion<br />
abnormality<br />
• A panel <strong>of</strong> 14 cardiologists and EPs met and<br />
recommended to the team that he not play<br />
and consider having an ICD implanted but<br />
they did not talk directly to the patient or the<br />
family<br />
• Team ownership took a neutral position<br />
after originally taking the side <strong>of</strong> the second<br />
group <strong>of</strong> doctors<br />
• Two months later while shooting baskets at<br />
Brandeis <strong>University</strong> he collapsed and died<br />
• Autopsy was performed<br />
• Family was furious and had him transferred<br />
to another local hospital<br />
• MDs there downplayed the abnormalities and<br />
a tilt table test was done and he received the<br />
diagnosis <strong>of</strong> vasodepressor syncope<br />
• They recommend that he take beta-blockers<br />
and do little activity but at a press conference<br />
the doctors said he could play again<br />
• Sought a third opinion from an EP in<br />
California without clear resolution<br />
4/10/2013<br />
9
Greatness<br />
Reggie “the Jet” Lewis was<br />
drafted by the powerhouse<br />
Boston Celtics in the first<br />
round in 1987.<br />
He averaged over 20 points<br />
a game.<br />
Selected as the Celtic’s team<br />
captain after the retirement<br />
<strong>of</strong> Larry Bird.<br />
Lewis suffered six dizzy<br />
spells in 4 months before<br />
collapsing during a play<strong>of</strong>f<br />
game against the Charlotte<br />
Hornets on April 29, 1993.<br />
After he was examined by<br />
the team doctor, he was<br />
allowed to continue to play in<br />
the second half.<br />
Reggie Lewis and Myocarditis<br />
A sad story<br />
Physicians at PBBH developed a<br />
close relationship with Lewis and<br />
his family.<br />
Lewis was prescribed beta<br />
blockers and instructed to do very<br />
little physical activity; however at a<br />
press conference, they stated<br />
Lewis could play again.<br />
Lewis sought a third opinion in<br />
California, but without clear<br />
resolution.<br />
The team ownership took a<br />
neutral position after initially<br />
endorsing the PBBH diagnosis<br />
The family felt abandoned by<br />
the team and all the other<br />
doctors except for the PBBH<br />
group.<br />
Two months later, Lewis<br />
suffered a fatal cardiac arrest<br />
while shooting baskets at<br />
Brandeis on July 27, 1993<br />
His autopsy revealed<br />
extensive scarring <strong>of</strong> the heart<br />
muscle, consistent with the<br />
original diagnosis.<br />
A sad story<br />
He was hospitalized at Baptist Hospital in<br />
Boston where runs <strong>of</strong> NSVT were noted.<br />
Work-up included a thallium scan, MR<br />
imaging, and cardiac catheterization.<br />
He was found to have a large apical<br />
perfusion defect but normal coronary<br />
arteries.<br />
A panel <strong>of</strong> 14 electrophysiologists and<br />
cardiologists reviewed the data in a special<br />
two hour session.<br />
They advised the team not allow Lewis to<br />
play and to consider an ICD, but none <strong>of</strong> the<br />
panel directly met with Lewis or his family.<br />
A sadder ending:<br />
A sad story<br />
Very upset, the family had Lewis transferred to<br />
Peter Bent Brigham Hospital at midnight by van<br />
Physicians there reviewed but minimized the<br />
abnormalities.<br />
A tilt table test was positive and the diagnosis<br />
was changed to vasodepressor syncope.<br />
Myocarditis<br />
Myocarditis can be produced by a variety <strong>of</strong><br />
different disorders, most <strong>of</strong> them infectious.<br />
Many case are not detected because there are<br />
not significant symptoms, but fatigue and<br />
decreased exercise tolerance can be early<br />
signs.<br />
Chest pains, sudden death, and abnormal<br />
heart beats can be seen as well.<br />
Sometimes obtaining a piece <strong>of</strong> heart muscle<br />
by way <strong>of</strong> a biopsy can be helpful in making a<br />
definitive diagnosis.<br />
Myocarditis should be suspected when a<br />
patient, especially a young male, presents with<br />
otherwise unexplained cardiac abnormalities <strong>of</strong><br />
new onset. Some may describe recent upper<br />
respiratory infection or recent diarrhea.<br />
Case Presentation<br />
• 20 year old white female basketball<br />
player at the <strong>University</strong> <strong>of</strong><br />
Washington<br />
• Leading scorer for the team<br />
• Rare episodes <strong>of</strong> dizziness<br />
• Collapsed in her room in late<br />
December 2002 and awakened from<br />
a coma Jan 1 2003 with no sequelae<br />
after being resuscitated with an<br />
external defibrillator<br />
Case Presentation was Kayla Burt Long QT syndrome<br />
4/10/2013<br />
10
LQT1<br />
LQT2<br />
LQT3<br />
Gender + QT +<br />
disease gene<br />
Priori et al 2003<br />
decreasing risk<br />
Torsade de pointes<br />
Rate 200 - 250 bpm<br />
Rhythm Irregular<br />
Recognition Continuously changing QRS morphology<br />
Management <strong>of</strong> LQTS<br />
β-blockers, exercise restriction in all (controversial in<br />
LQT3)<br />
Sodium channel blocker (mexiletine, ranolazine) in<br />
LQT3 (?)<br />
ICDs in “high-risk” subgroups<br />
Resuscitated from cardiac arrest while compliant<br />
with an effective β-blocker regimen<br />
Resuscitated from cardiac arrest<br />
Age 500?)<br />
Males with LQT3<br />
Family history <strong>of</strong> SCD is not a marker <strong>of</strong> high risk<br />
4/10/2013<br />
11
Case Presentation<br />
• 24 year old white male with no prior known<br />
significant medical history<br />
• Developed flu-like illness and high spiking<br />
fevers<br />
• Had dizziness during one <strong>of</strong> the fever spikes<br />
• Had frank syncope sitting at a desk checking<br />
his e-mail during another fever spike<br />
• ECG revealed classic Type I Brugada<br />
pattern with fever<br />
• Brugada pattern was not seen when fever<br />
was not present<br />
Brugada Syndrome<br />
The Brugada Syndrome<br />
<strong>Sudden</strong> death (due to VF) <strong>of</strong>ten at night; may be especially common in young<br />
SE Asian men (SUDS)<br />
J point elevation in V1-V3 and “RBBB” not always present; exacerbated by Na +<br />
channel block, -blockers; improved by isoproterenol. Syncope/SCD may be<br />
provoked by fever.<br />
Provocation by sodium channel blockers implicated SCN5A.<br />
SCN5A mutations causing loss <strong>of</strong> I Na function– through multiple mechanisms –<br />
now identified in ~20% <strong>of</strong> affected subjects. GPD1L mutations identified in a<br />
large kindred.<br />
4/10/2013<br />
12
Brugada Syndrome Mechanisms<br />
Benito Progr Cardiovasc Dis 2008; 51:1-22<br />
ECG in Brugada Syndrome<br />
Brugada Syndrome Management<br />
Benito et al. Progr Cardiovasc Dis 2008;51:1-22.<br />
4/10/2013<br />
13
Catecholaminergic Polymorphic VT<br />
Mutations in genes controlling intracellular calcium<br />
• Autosomal dominant (CPVT1):<br />
Mutations in the ryanodine release channel<br />
(RYR2) Sarcoplasmic Reticulum (SR) Ca 2+<br />
“leak”<br />
Exercise-related PVT<br />
-blockers effective; Ca 2+ channel blockers<br />
are not<br />
• Autosomal recessive (CPVT2)<br />
One large Bedouin kindred<br />
Mutations in calsequestrin (an SR Ca 2+<br />
buffering protein)<br />
Bidirectional VT and Ventricular Fibrillation in CPVT<br />
Human CPVT<br />
RyR2<br />
Knockout<br />
Mouse<br />
Priori, S. G. et al. J. Clin. Invest. 2005;115:2033-2038<br />
CPVT – Exercise Test<br />
Catecholaminergic Polymorphic VT<br />
Take Home Points<br />
1. ECG is essentially normal at rest<br />
2. Exercise induced PVCs with bigeminy –Think CPVT<br />
3. Patients should be restricted from competitive athletics<br />
4. If symptomatic and normal QTc –Think CPVT instead <strong>of</strong><br />
“concealed LQT1”<br />
5. RyR2 CPVT (CPVT1) ~ 50 –65% <strong>of</strong> CPVT<br />
6. 15% SUD/12% SIDS – RyR2 positive<br />
7. CPVT1 is more severe and less responsive to beta blocker<br />
therapy than LQT1<br />
From Ackerman MJ, HRS 2007.<br />
4/10/2013<br />
14
Case Presentation<br />
• 34 y/o former athlete and now<br />
<strong>of</strong>fshore worker<br />
• Presented while running as he runs<br />
3 to 5 miles per day four times per<br />
week<br />
• Severe dizziness and near syncope<br />
• Flagged down car who took him<br />
HOME<br />
• Wife insisted he go to hospital<br />
12-lead ECG Induction <strong>of</strong> VT<br />
4/10/2013<br />
15
RV Gram: <strong>Cardiac</strong> MR:<br />
Axial T1-weighted black blood spin-echo images<br />
Transmural fatty replacement <strong>of</strong> the right ventricular myocardium (RV) and the<br />
right ventricular outflow tract (RVOT)<br />
4/10/2013<br />
16
Anatomy:<br />
Localized or general dilatation <strong>of</strong> the RV myocardium<br />
associated with thinning <strong>of</strong> the affected regions<br />
The myocardium is progressively replaced with transmural<br />
fibrous and fatty tissue with scattered residual myocardium<br />
It can also affect the LV<br />
Triangle <strong>of</strong> dysplasia: Diaphragmatic RV, Infundibulum and<br />
apex.<br />
Recommendations:<br />
Patients with ARVC should NOT participate in<br />
competitive sports<br />
ICD for secondary prevention<br />
ICD for primary prevention if ARVD w/ high risk*<br />
features<br />
Anti-arrhythmics for pts who don’t want or can’t<br />
have an ICD<br />
Pts w/ ARVD + ICD who still have arrhythmias<br />
consider anti-arrhythmic<br />
ARVD Pts + ICD + antiarrhythmics, consider RFA<br />
If anti-arrhythmics to be used consider sotalol or<br />
amiodarone<br />
*Extensive dz, LV involvement, FHx <strong>of</strong> SCD, unexplained syncope<br />
Transmural fatty<br />
infiltration<br />
Anatomy:<br />
Triangle <strong>of</strong> dysplasia<br />
Arrhythmogenic Right<br />
Ventricular Dysplasia<br />
<strong>Cardiac</strong> Arrest<br />
Sustained VT<br />
Unequivocal Syncope<br />
Extensive Myocardial Disease<br />
Frequent NSVT<br />
Family history <strong>of</strong> SCD<br />
4/10/2013<br />
17
Congenital coronary anomalies<br />
• Anomalous origin <strong>of</strong> the left main or left anterior<br />
descending coronary artery from the right sinus <strong>of</strong><br />
Valsalva is most common<br />
• <strong>Cardiac</strong> arrest may be the first manifestation<br />
Normal Anomalous<br />
from Cheitlin MD, Circ 1974<br />
Normal Coronary Anatomy<br />
Pete Maravich and Single Coronary<br />
“Pistol” Pete Maravich:<br />
shattering records<br />
•Pete Maravich had a style <strong>of</strong><br />
play that was twenty years<br />
ahead <strong>of</strong> his time<br />
•This gift enabled him to<br />
currently hold every major<br />
NCAA scoring record<br />
•NCAA career record for<br />
most points (3,667 points in<br />
83 games)<br />
•NCAA record for highest per<br />
game average (44.5 ppg)<br />
•NCAA record for most<br />
games over 50 points (28)<br />
Playing guard with<br />
LSU, his father<br />
Maravich was head<br />
coach<br />
“Pistol” Pete Maravich:<br />
the original showtime<br />
•He had a brilliant career with three NBA teams<br />
•NBA All-Rookie Team<br />
•All NBA First Team (‘76, ’77)<br />
•Five-time NBA All-Star ((’73, ’74, ’77, ’78, ’79)<br />
•Led NBA in scoring in 1977 (31.1 ppg)<br />
•Scored 15,948 points (24.2 ppg) in 658 games<br />
•NBA 50th Anniversary All-Time Team (1996)<br />
•NBA Hall <strong>of</strong> Fame (1987)<br />
•Voted one <strong>of</strong> the 50 greatest players <strong>of</strong> all time<br />
•He played for 10<br />
consecutive seasons in<br />
the NBA, but in the end he<br />
collapsed and died at age<br />
40 playing a pickup game<br />
•He was found to have<br />
only one coronary artery<br />
instead <strong>of</strong> the normal two<br />
•It is suspected that he<br />
died <strong>of</strong> a terminal<br />
arrhythmia due to this<br />
undiagnosed congenital<br />
heart defect<br />
Patient killer :Congenital Anomaly<br />
•Maravich was born with one coronary artery causing<br />
hypertrophy <strong>of</strong> the myocardium that was likely the source<br />
<strong>of</strong> his arrhythmia.<br />
•His defect is reported to occur in less than .1% <strong>of</strong> the<br />
human population.<br />
•Normal coronary anatomy versus Maravich’s heart<br />
(above).<br />
4/10/2013<br />
18
Case Presentation<br />
• 18 y/o Ole Miss football player<br />
becomes weak and lightheaded at<br />
football practice<br />
• Something is different this time !!<br />
• Difficulty standing up due to weakness<br />
and chest hurts<br />
• Coaches take him immediately to<br />
student health center<br />
• Collapses and full arrest as ECG leads<br />
are being attached<br />
• Immediate defibrillation<br />
Wolff-Parkinson-White Syndrome<br />
SVT<br />
4/10/2013<br />
19
Wolff-Parkinson-White Syndrome Normal AV Conduction<br />
Accessory Pathway in Sinus Rhythm (WPW) AV Reentry Tachycardia<br />
4/10/2013<br />
20
Pre-Excitation Syndromes (WPW)<br />
Surface EKG<br />
P wave<br />
R wave<br />
T wave<br />
Morady F. NEJM 1999<br />
Intracardiac EGM Enlarged View <strong>of</strong> AV Groove<br />
RF Catheter Site for Left Sided Accessory<br />
Pathway<br />
Atrial Fibrillation with WPW<br />
4/10/2013<br />
21
WPW: Atrial Fibrillation Degenerating to Ventricular<br />
Fibrillation<br />
Elimination <strong>of</strong> Accessory Pathway Function<br />
and Cure <strong>of</strong> WPW Syndrome<br />
4/10/2013<br />
22
Nonischemic Dilated CM<br />
SCD/HFT Data Unexplained Syncope<br />
If Class II-III CHF &<br />
EF < =35%, then<br />
ICD<br />
IHD EF < 40,>35<br />
Syncope or NSVT<br />
YES<br />
EPS<br />
VT Induced<br />
ICD<br />
Long QT or Brugada<br />
Syncope Asymptomatic<br />
ICD<br />
<strong>Medical</strong> Individual<br />
And/or ICD Approach<br />
SCD survivor or spontaneous<br />
VT/VF not due to a transient<br />
or reversible cause and cannot<br />
be successfully ablated<br />
IHD EF
Animation – Ventricular<br />
Dysynchrony<br />
Click to Start/Stop<br />
Miracle Trial Conclusions<br />
In NYHA Class III and IV heart failure<br />
patients with ventricular dysynchrony<br />
and with or without an ICD indication,<br />
CRT significantly improves quality <strong>of</strong><br />
life, NYHA class, and maximal exercise<br />
capacity (peak VO 2, exercise time)<br />
CRT adds incremental benefit to the<br />
treatment <strong>of</strong> heart failure<br />
Clinical Consequences <strong>of</strong><br />
Ventricular Dysynchrony<br />
Abnormal<br />
interventricular septal<br />
wall motion1 Reduced dP/dt3,4 Reduced pulse<br />
pressure4 Click to Start/Stop<br />
1 Grines CL, Bashore TM, Boudoulas H, et al. Circulation 1989;79:845-853.<br />
2 Xiao, HB, Lee CH, Gibson DG. Br Heart J 1991;66:443-447.<br />
3 Xiao HB, Brecker SJD, Gibson DG. Br Heart J 1992;68:403-407.<br />
4 Yu C-M, Chau E, Sanderson JE, et al. Circulation. 2002;105:438-445.<br />
Conclusions<br />
Reduced EF and CO4 Reduced diastolic<br />
filling time1,2,4 Prolonged MR<br />
duration1,2,4 In NYHA Class III and IV heart failure patients with<br />
ventricular dyssynchrony CRT significantly<br />
improves:<br />
– Quality <strong>of</strong> life<br />
– NYHA class<br />
– Maximal exercise capacity (peak VO2, exercise time)<br />
CRT adds incremental benefit to the treatment <strong>of</strong><br />
heart failure<br />
What About MORTALITY?<br />
4/10/2013<br />
24
COMPANION<br />
Comparison <strong>of</strong> <strong>Medical</strong> Therapy, Pacing, and<br />
Defibrillation in Chronic Heart Failure<br />
Published in 2004<br />
Hypothesis: Can CRT decrease morbidity and<br />
mortality in Class III-IV HF patients over drugs<br />
alone?<br />
Patient population: 1,520<br />
Study design: randomized, three arms<br />
– CRT group (no defibrillation)<br />
– CRT-D group<br />
– Conventional therapy group (no device)<br />
Inclusion criteria: NYHA Class III-IV,<br />
LVEF≤35%, QRS ≥ 120 ms<br />
Exclusion criterion: Standard ICD or pacing<br />
indication<br />
COMPANION Conclusions<br />
CRT-D in combination with OPT<br />
reduced the risk <strong>of</strong> all-cause mortality<br />
by 36% when compared to OPT alone<br />
COMPANION RESULTS<br />
Both CRT and CRT-D decreased the risk <strong>of</strong> allcause<br />
mortality or first hospitalization for any<br />
reason by about 20% over conventional therapy<br />
CRT-D reduced mortality (p=0.003) by 36%<br />
CRT-P reduced mortality (p=0.059) by 24%<br />
For death from or hospitalization for a CV cause<br />
– CRT reduced risk 25%<br />
– CRT-D reduced risk 28%<br />
For death from or hospitalization for HF<br />
– CRT reduced risk 34%<br />
– CRT-D reduced risk 40%<br />
Indications for the ICD <strong>Cardiac</strong><br />
Resynchronization Systems<br />
CRT ICD systems are indicated<br />
for the reduction <strong>of</strong> HF<br />
symptoms in patients that meet<br />
the following criteria:<br />
– Standard ICD indication<br />
– Moderate to severe heart failure<br />
(NYHA Class III/IV)<br />
– QRS 120 – 130 ms<br />
– LV ejection fraction 35%<br />
– Symptomatic despite stable,<br />
optimal medical therapy<br />
4/10/2013<br />
25
Implant Procedure<br />
Coronary Sinus Angiograms<br />
AP View LAO View<br />
Click to Start/Stop<br />
Implantation <strong>of</strong> a Biventricular Device<br />
Note visible branches Coronary Sinus Angiograms – Victim <strong>of</strong><br />
Anatomy<br />
Varying Patient Anatomy<br />
4/10/2013<br />
26
Venous Anatomy<br />
Lead in Lateral <strong>Cardiac</strong> Vein<br />
Thank You !!!<br />
AP Position<br />
Lead Placed in Target Vein<br />
LAO View Lateral Coronary Vein Placement<br />
4/10/2013<br />
27