Medication Prior Authorization
Medication Prior Authorization
Medication Prior Authorization
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
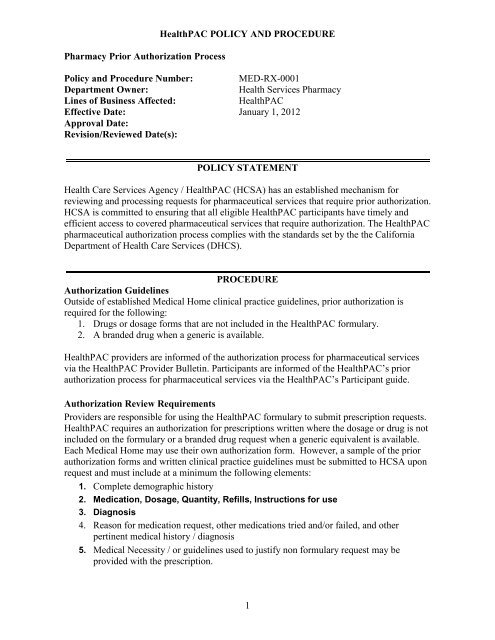
Pharmacy <strong>Prior</strong> <strong>Authorization</strong> Process<br />
HealthPAC POLICY AND PROCEDURE<br />
Policy and Procedure Number: MED-RX-0001<br />
Department Owner: Health Services Pharmacy<br />
Lines of Business Affected: HealthPAC<br />
Effective Date: January 1, 2012<br />
Approval Date:<br />
Revision/Reviewed Date(s):<br />
POLICY STATEMENT<br />
Health Care Services Agency / HealthPAC (HCSA) has an established mechanism for<br />
reviewing and processing requests for pharmaceutical services that require prior authorization.<br />
HCSA is committed to ensuring that all eligible HealthPAC participants have timely and<br />
efficient access to covered pharmaceutical services that require authorization. The HealthPAC<br />
pharmaceutical authorization process complies with the standards set by the the California<br />
Department of Health Care Services (DHCS).<br />
PROCEDURE<br />
<strong>Authorization</strong> Guidelines<br />
Outside of established Medical Home clinical practice guidelines, prior authorization is<br />
required for the following:<br />
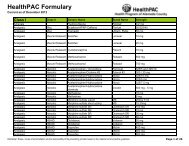
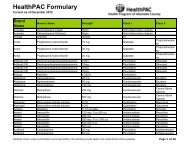
1. Drugs or dosage forms that are not included in the HealthPAC formulary.<br />
2. A branded drug when a generic is available.<br />
HealthPAC providers are informed of the authorization process for pharmaceutical services<br />
via the HealthPAC Provider Bulletin. Participants are informed of the HealthPAC’s prior<br />
authorization process for pharmaceutical services via the HealthPAC’s Participant guide.<br />
<strong>Authorization</strong> Review Requirements<br />
Providers are responsible for using the HealthPAC formulary to submit prescription requests.<br />
HealthPAC requires an authorization for prescriptions written where the dosage or drug is not<br />
included on the formulary or a branded drug request when a generic equivalent is available.<br />
Each Medical Home may use their own authorization form. However, a sample of the prior<br />
authorization forms and written clinical practice guidelines must be submitted to HCSA upon<br />
request and must include at a minimum the following elements:<br />
1. Complete demographic history<br />
2. <strong>Medication</strong>, Dosage, Quantity, Refills, Instructions for use<br />
3. Diagnosis<br />
4. Reason for medication request, other medications tried and/or failed, and other<br />
pertinent medical history / diagnosis<br />
5. Medical Necessity / or guidelines used to justify non formulary request may be<br />
provided with the prescription.<br />
1
The HealthPAC medical home Medical Director / pharmacist / or qualified designee utilizes<br />
criteria that have been approved by the Medical Home / Clinics Pharmacy and Therapeutics<br />
Committee (P&T Committee). The criteria are based on evidenced based guidelines and<br />
current literatures.<br />
1. Initial review is completed by qualified staff Medical Director / pharmacist / or<br />
qualified designee at the Medical Home.<br />
2. If the Medical Home cannot arrive at a decision the request is forwarded to the<br />
Medical Director of the Medical Home for final decision.<br />
All decisions can be rendered by the Medical Home’s Medical Director / pharmacist / or<br />
qualified designee under the auspices and pursuant to criteria established by plan's medical<br />
director in collaboration with the P&T committee.<br />
1. Reasons for denial decisions are clearly documented<br />
<strong>Authorization</strong> Processing Timeframes<br />
The Medical Home processes prior authorization requests for pharmaceutical services within<br />
the following timeframes:<br />
Decision Notification Timeframes<br />
The Medical Home provides notification of the decision within the following timeframes:<br />
Approvals<br />
1. Notifications of approvals of prospective requests are made within five (5) business<br />
days of the receipt of the requests.<br />
2. Pharmacy Services Unit notifies the requesting Providers and pharmacy, if known, of<br />
the approval decisions.<br />
Denials and Modications<br />
1. Notification of denied and modified requests include clear and concise explanations of<br />
the reasons for the denial and a description of the criteria or guidelines used is<br />
provided to the physician and participant within 5 business days.<br />
2. For HealthPAC MCE (Medi-Cal Expantion) Participants: The participant’s right to,<br />
and method of obtaining, a fair hearing to contest the denial, deferral, or modification<br />
action and the decision the Medical Home has made including timeframes for<br />
requesting a hearing / filing a grievence or appeal.<br />
2
Pharmacy Services<br />
DEFINITIONS<br />
AFFECTED DEPARTMENTS/PARTIES<br />
RELATED POLICIES AND PROCEDURES AND OTHER RELATED DOCUMENTS<br />
1. DHCS Contract<br />
REVISION HISTORY<br />
REFERENCES<br />
MONITORING<br />
The HCSA provides oversight of its Medical Homes through an annual audit of the<br />
authorization review process. If opportunities are identified, improvement efforts are<br />
implemented.<br />
3