A5V4d
A5V4d A5V4d
Feverish illness in children Other considerations No equalities issue were identified in relation to this question. Recommendations The recommendations covering the predictive value of heart rate are presented at the end of section 5.5. Blood pressure Evidence summary Blood pressure was not identified as an independent risk factor for serious illness in any of the prospective cohort studies and scoring systems. Low blood pressure was identified as one of several risk factors for adverse outcome in children with meningococcal disease. 119 GDG translation The GDG agreed with stakeholder comments that blood pressure should be measured in children with fever who are displaying features of possible serious illness. Blood pressure can be a helpful measurement to monitor children with possible sepsis although low blood pressure is a late feature of septic shock. Other markers such as raised heart rate and prolonged capillary refill time are present earlier and require no special equipment to measure. The GDG concluded that blood pressure should be measured when facilities exist to monitor blood pressure and other markers of inadequate organ perfusion (i.e. shock) are detected. Recommendations The recommendations covering blood pressure are presented at the end of section 5.5. Assessment of dehydration A number of studies have used degree of dehydration as a marker of serious illness. However, the symptoms and signs used in a number of studies have lacked rigour. The GDG looked for evidence for objective symptoms and signs for dehydration. Narrative evidence A recent EL 2+ SR 117 looking at children 1 month to 5 years was found. Although this SR only searched MEDLINE, it was judged to be adequate for inclusion. The authors reviewed 1603 papers, half of which were excluded because of lack of rigour or lack of clarity in outcomes. Of the remainder, only 26 were found to be rigorous enough to meet their criteria. Moreover, in this SR, dehydration was measured using percentage volume lost. They found three studies that evaluated the accuracy of a history of low urine output. A history of low urine output did not increase the likelihood of 5% dehydration (likelihood ratio [LR] 1.3, 95% CI 0.9 to 1.9). The most sensitive signs not requiring particular specialised tests for dehydration were dry mucous membranes, poor overall appearance, and sunken eyes and absent tears (see Table 5.3 for the sensitivities). Prolonged capillary refill time, cool extremities, reduced skin turgor and abnormal respiratory pattern were the most specific individual signs of dehydration. Evidence summary It is difficult to detect dehydration in children with fever. Individual symptoms and parental observations are poor predictors of dehydration. Furthermore, history of low urine output does not increase the risk of dehydration. The results showed that prolonged capillary refill time, reduced skin turgor and abnormal respiratory pattern are the most specific individual signs of dehydration. Table 5.65 Summary characteristics for clinical findings to detect 5% dehydration 117 Clinical feature Sensitivity (95% CI) Specificity (95% CI) Prolonged capillary refill time 0.60 (0.29 to 0.91) 0.85 (0.72 to 0.98) Abnormal skin turgor 0.58 (0.40 to 0.75) 0.76 (0.59 to 0.93) Abnormal respiratory pattern 0.43 (0.31 to 0.55) 0.79 (0.72 to 0.86) 128 2013 Update
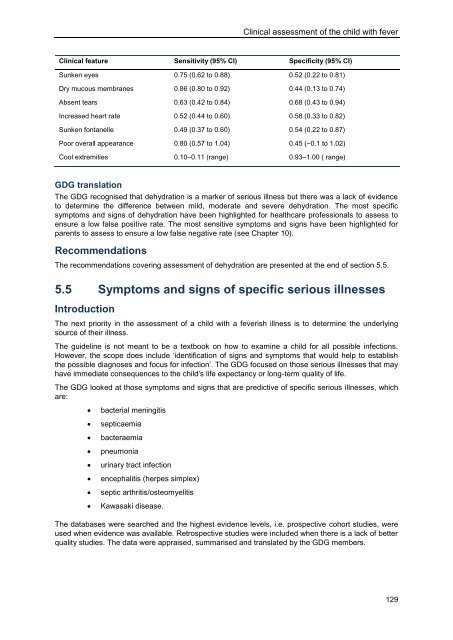
Clinical assessment of the child with fever Clinical feature Sensitivity (95% CI) Specificity (95% CI) Sunken eyes 0.75 (0.62 to 0.88) 0.52 (0.22 to 0.81) Dry mucous membranes 0.86 (0.80 to 0.92) 0.44 (0.13 to 0.74) Absent tears 0.63 (0.42 to 0.84) 0.68 (0.43 to 0.94) Increased heart rate 0.52 (0.44 to 0.60) 0.58 (0.33 to 0.82) Sunken fontanelle 0.49 (0.37 to 0.60) 0.54 (0.22 to 0.87) Poor overall appearance 0.80 (0.57 to 1.04) 0.45 (−0.1 to 1.02) Cool extremities 0.10–0.11 (range) 0.93–1.00 ( range) GDG translation The GDG recognised that dehydration is a marker of serious illness but there was a lack of evidence to determine the difference between mild, moderate and severe dehydration. The most specific symptoms and signs of dehydration have been highlighted for healthcare professionals to assess to ensure a low false positive rate. The most sensitive symptoms and signs have been highlighted for parents to assess to ensure a low false negative rate (see Chapter 10). Recommendations The recommendations covering assessment of dehydration are presented at the end of section 5.5. 5.5 Symptoms and signs of specific serious illnesses Introduction The next priority in the assessment of a child with a feverish illness is to determine the underlying source of their illness. The guideline is not meant to be a textbook on how to examine a child for all possible infections. However, the scope does include ‘identification of signs and symptoms that would help to establish the possible diagnoses and focus for infection’. The GDG focused on those serious illnesses that may have immediate consequences to the child’s life expectancy or long-term quality of life. The GDG looked at those symptoms and signs that are predictive of specific serious illnesses, which are: bacterial meningitis septicaemia bacteraemia pneumonia urinary tract infection encephalitis (herpes simplex) septic arthritis/osteomyelitis Kawasaki disease. The databases were searched and the highest evidence levels, i.e. prospective cohort studies, were used when evidence was available. Retrospective studies were included when there is a lack of better quality studies. The data were appraised, summarised and translated by the GDG members. 129
- Page 84 and 85: Feverish illness in children Table
- Page 86 and 87: Feverish illness in children Table
- Page 88 and 89: Feverish illness in children Table
- Page 90 and 91: Feverish illness in children Number
- Page 92 and 93: Feverish illness in children Table
- Page 94 and 95: Feverish illness in children Table
- Page 96 and 97: Feverish illness in children Number
- Page 98 and 99: Feverish illness in children The fo
- Page 100 and 101: Feverish illness in children Nasal
- Page 102 and 103: Feverish illness in children Neck s
- Page 104 and 105: Feverish illness in children the YO
- Page 106 and 107: Feverish illness in children The ev
- Page 108 and 109: Feverish illness in children Based
- Page 110 and 111: Feverish illness in children Howeve
- Page 112 and 113: Feverish illness in children Non-bl
- Page 114 and 115: Feverish illness in children also h
- Page 116 and 117: Feverish illness in children strong
- Page 118 and 119: Feverish illness in children Qualit
- Page 120 and 121: Feverish illness in children The fi
- Page 122 and 123: Feverish illness in children for sp
- Page 124 and 125: Feverish illness in children Number
- Page 126 and 127: Feverish illness in children Figure
- Page 128 and 129: Feverish illness in children Table
- Page 130 and 131: Feverish illness in children report
- Page 132 and 133: Feverish illness in children Figure
- Page 136 and 137: Feverish illness in children Review
- Page 138 and 139: Feverish illness in children A thir
- Page 140 and 141: Feverish illness in children The AH
- Page 142 and 143: Feverish illness in children 136 gr
- Page 144 and 145: Feverish illness in children Table
- Page 146 and 147: Feverish illness in children Resear
- Page 148 and 149: Feverish illness in children risk o
- Page 150 and 151: Feverish illness in children 36 Chi
- Page 152 and 153: Feverish illness in children The GD
- Page 154 and 155: Feverish illness in children 42 Chi
- Page 156 and 157: Feverish illness in children childr
- Page 158 and 159: Feverish illness in children The GD
- Page 160 and 161: Feverish illness in children The in
- Page 162 and 163: Feverish illness in children to cha
- Page 164 and 165: Feverish illness in children Few st
- Page 166 and 167: Feverish illness in children Number
- Page 168 and 169: Feverish illness in children Number
- Page 170 and 171: Feverish illness in children Number
- Page 172 and 173: Feverish illness in children Number
- Page 174 and 175: Feverish illness in children Table
- Page 176 and 177: Sensitivity Feverish illness in chi
- Page 178 and 179: Feverish illness in children One st
- Page 180 and 181: Feverish illness in children Recomm
- Page 182 and 183: Feverish illness in children Observ
Clinical assessment of the child with fever<br />
Clinical feature Sensitivity (95% CI) Specificity (95% CI)<br />
Sunken eyes 0.75 (0.62 to 0.88) 0.52 (0.22 to 0.81)<br />
Dry mucous membranes 0.86 (0.80 to 0.92) 0.44 (0.13 to 0.74)<br />
Absent tears 0.63 (0.42 to 0.84) 0.68 (0.43 to 0.94)<br />
Increased heart rate 0.52 (0.44 to 0.60) 0.58 (0.33 to 0.82)<br />
Sunken fontanelle 0.49 (0.37 to 0.60) 0.54 (0.22 to 0.87)<br />
Poor overall appearance 0.80 (0.57 to 1.04) 0.45 (−0.1 to 1.02)<br />
Cool extremities 0.10–0.11 (range) 0.93–1.00 ( range)<br />
GDG translation<br />
The GDG recognised that dehydration is a marker of serious illness but there was a lack of evidence<br />
to determine the difference between mild, moderate and severe dehydration. The most specific<br />
symptoms and signs of dehydration have been highlighted for healthcare professionals to assess to<br />
ensure a low false positive rate. The most sensitive symptoms and signs have been highlighted for<br />
parents to assess to ensure a low false negative rate (see Chapter 10).<br />
Recommendations<br />
The recommendations covering assessment of dehydration are presented at the end of section 5.5.<br />
5.5 Symptoms and signs of specific serious illnesses<br />
Introduction<br />
The next priority in the assessment of a child with a feverish illness is to determine the underlying<br />
source of their illness.<br />
The guideline is not meant to be a textbook on how to examine a child for all possible infections.<br />
However, the scope does include ‘identification of signs and symptoms that would help to establish<br />
the possible diagnoses and focus for infection’. The GDG focused on those serious illnesses that may<br />
have immediate consequences to the child’s life expectancy or long-term quality of life.<br />
The GDG looked at those symptoms and signs that are predictive of specific serious illnesses, which<br />
are:<br />
bacterial meningitis<br />
septicaemia<br />
bacteraemia<br />
pneumonia<br />
urinary tract infection<br />
encephalitis (herpes simplex)<br />
septic arthritis/osteomyelitis<br />
Kawasaki disease.<br />
The databases were searched and the highest evidence levels, i.e. prospective cohort studies, were<br />
used when evidence was available. Retrospective studies were included when there is a lack of better<br />
quality studies. The data were appraised, summarised and translated by the GDG members.<br />
129