Boletin.96.1 Ene-Feb. - Asociacion Medica de Puerto Rico
Boletin.96.1 Ene-Feb. - Asociacion Medica de Puerto Rico
Boletin.96.1 Ene-Feb. - Asociacion Medica de Puerto Rico
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
BOLETÍN<br />
ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
2 JUNTA DE DIRECTORES / JUNTA EDITORA<br />
• MENSAJE DEL PRESIDENTE Y PORTADA<br />
3 DR. RAMÓN EMETERIO BETANCES<br />
Por: Eduardo Rodríguez Vázquez, MD;<br />
7 EDITORIAL<br />
• ARTÍCULOS ORIGINALES • ORIGINAL ARTICLES<br />
8 PUERTO RICO EXPERIENCE WITH PLUGS IN<br />
THE TREATMENT OF ANAL FISTULAS<br />
By: Ignacio Echenique, MD; Juan R. Mella, MS; Francisco Rosado, MD;<br />
Ignacio A. Echenique, MS, Maria T. Mella, MS. and Gerardo Quevedo, MD.<br />
13 EXPERIENCE WITH HAND ASSISTED<br />
LAPAROSCOPIC SURGERY OF THE COLON<br />
By: Ramón K. Sotomayor, MD. and Bolivar Arboleda, MD.<br />
20 COMPARISON BETWEEN OPEN AND LAPAROSCOPIC<br />
APPENDECTOMY IN NON-COMPLICATED APPENDICITIS<br />
By: Aura F. Delgado Cifuentes, BS and Ramón K. Sotomayor, MD.<br />
27 MINIMALLY INVASIVE PARATHYROIDECTOMY<br />
AS TREATMENT FOR PRIMARY HYPERPARATHYROIDISM<br />
By: By: Laureano A. Giral<strong>de</strong>z-Rodriguez, MD.<br />
and Laureano J. Giral<strong>de</strong>z-Casasnovas, MD.<br />
34 PARATHYROID SURGERY WITHOUT INSTANT PTH<br />
OR RADIOGUIDED SESTAMIBI SCAN<br />
By: E. Vázquez-Quintana, MD. FACS. and D.E. Vázquez-Torres, MD.<br />
39 SURVEY OF CARDIAC RHYTHM MANAGEMENT<br />
AND DEVICE IMPLANT PATTERNS IN PUERTO RICO:<br />
ANALYSIS OF 13,854 CARDIAC IMPLANTS<br />
By: Juan M. Aranda, MD; FACC; Miguel Girod, MS; Eng; Fernando Ochoa,<br />
Miguel Abreu, MD; FACC; José J. Rivera, MD; FACC; Juan C. Sotomonte, MD;<br />
Angel Rodríguez, MD; Daniel Arzola, M.D; Raúl Jiménez, MD; FACC.<br />
and Juan M. Aranda Jr; MD; FACC.<br />
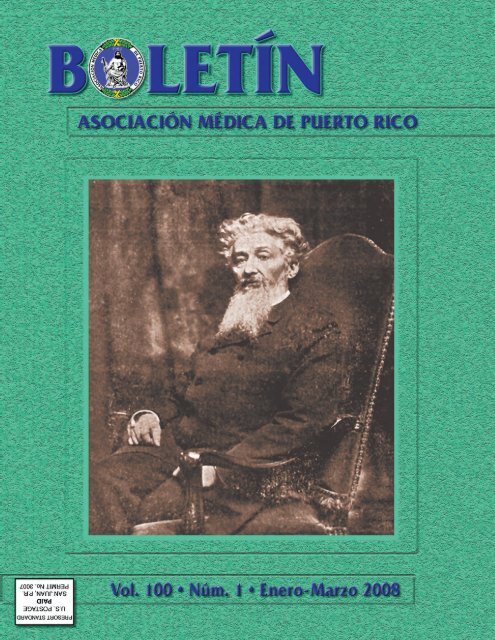
PORTADA<br />
Dr. Ramón Emeterio Betances<br />
Página 3<br />
CONTENIDO<br />
• ARTÍCULO DE REPASO • REVIEW ARTICLE<br />
50 HISTORY OF PARATHYROID SURGERY IN PUERTO RICO<br />
By: Enrique Vázquez-Quintana, MD.<br />
61 28TH F.L. RAFFUCCI RESEARCH FORUM ABSTRACTS<br />
66 CME CREDITS<br />
• INFORME DE CASOS • CASE REPORTS<br />
70 DISTAL FRAGMENTED PORT CATHETER:<br />
CASE REPORT AND REVIEW OF LITERATURE<br />
By: Norman E. Colón-Casasnovas and Humberto Lugo-Vicente<br />
76 HERMANSKY PUDLAK SYNDROME:<br />
AN UNUSUAL FORM OF PROCTO-COLITIS<br />
By: Ignacio Echenique, MD; José M. García González, MD;<br />
Ignacio A. Echenique, MS; Natalio J. Izquierdo, MD; Juan R. Mella, MA;<br />
Eligio Barasorda, MD; María T. Mella, MS. and Siegfried Figueroa-Boilo, MD.<br />
81 LAPAROSCOPIC NEPHRECTOMY WITH LAPAROSCOPICALLY<br />
ASSISTED TRANSVAGINAL EXTRACTION OF INTACT KIDNEY<br />
By: Alfonso Serrano-Ysern, MD; Alvin López, MD; Freddie Mén<strong>de</strong>z, MD;<br />
Lianette Perez, MD. and Jaime Acosta, MD.<br />
86 CALENDARIO DE ACTIVIDADES MÉDICAS<br />
87 SOLICITUD PRELIMINAR DE MEMBRESÍA AMPR<br />
EL IMPRESO DE ESTA EDICIÓN DEL BOLETÍN<br />
HA SIDO POSIBLE POR<br />
UN AUSPICIO EDUCATIVO DE:<br />
TRIPLE S, PUERTO RICO<br />
BOLETÍN • Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
Ave. Fernán<strong>de</strong>z Juncos Núm. 1305<br />
PO Box 9387 • San Juan, <strong>Puerto</strong> <strong>Rico</strong> 00908-9387<br />
Tel.: 787-721-6969 • Fax: 787-724-5208<br />
e-mail: asocmed@coqui.net<br />
web page: asociacionmedicapr.com<br />
Catalogado en Cumulative In<strong>de</strong>x e In<strong>de</strong>x Medicus.<br />
Listed in Cumulative In<strong>de</strong>x and In<strong>de</strong>x Medicus. No. ISSN - 0004-4849<br />
Diseño Gráfico y Emplanaje por:<br />
PubliArt • 787-273-0160<br />
e-mail: publiart@prtc.net<br />
Impreso en Colombia por: D’vinni<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
2<br />
JUNTA DE DIRECTORES<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
ASOCIACIÓN MÉDICA DE PUERTO RICO • 2008<br />
Eduardo Rodríguez Vázquez, MD<br />
Presi<strong>de</strong>nte<br />
Ricardo Marrero Santiago, MD<br />
Presi<strong>de</strong>nte Saliente<br />
Verónica Rodríguez, MD<br />
Secretaria<br />
Raúl Castellanos Bran, MD<br />
Tesorero<br />
Hilda Ocasio Maldonado, MD<br />
Vicepresi<strong>de</strong>nte AMPR<br />
Rolance Chavier Roper, MD<br />
Vicepresi<strong>de</strong>nte AMPR<br />
Raúl A. Yordán Rivera, MD<br />
Vicepresi<strong>de</strong>nte AMPR<br />
Arturo Arché Matta, MD<br />
Pres. Cámara <strong>de</strong> Delegados<br />
José I. Iglesias, MD<br />
Vicepresi<strong>de</strong>nte Cámara Delegados<br />
Rafael Fernán<strong>de</strong>z Feliberti<br />
Delegado Alterno AMA<br />
Eladio Santos Aponte, MD<br />
Delegado Aterno AMA<br />
Wanda Vélez Andujar, MD<br />
Delegado Alterno AMA<br />
José Gerena Díaz<br />
Presi<strong>de</strong>nte Distrito Este<br />
Gustavo Ce<strong>de</strong>ño Quintero MD<br />
Presi<strong>de</strong>nte Distrito Noreste<br />
Wanda Velez Andujar<br />
Presi<strong>de</strong>nta Distrito Sur<br />
Mildred Arché Matta<br />
Presi<strong>de</strong>nta Distrito Central<br />
Verónica Rodriguez MD<br />
Presi<strong>de</strong>nta Consejo <strong>de</strong> Educación Médica Continuada<br />
Ismael Toro Grajales MD<br />
Presi<strong>de</strong>nte Consejo Etico-Judicial<br />
Alejandro Medina Vilar<br />
Presi<strong>de</strong>nte Consejo Relaciones Públicas y Servicios Públicos<br />
Jorge Velez Soto MD<br />
Presi<strong>de</strong>nte Consejo Servicios Médicos<br />
Eladio Santos Aponte MD<br />
Presi<strong>de</strong>nte Consejo Salud Pública y Bienestar Social<br />
Natalio Debs Elias MD<br />
Presi<strong>de</strong>nte Consejo Politica Pública y Legislación<br />
Emilio Arce Ortíz, MD<br />
Presi<strong>de</strong>nte Comité Asesor Presi<strong>de</strong>nte<br />
Ilia E. Zayas Ortíz, MD<br />
Presi<strong>de</strong>nta Instituto Educación Médica<br />
PRESIDENTES<br />
SECCI0NES DE ESPECIALIDAD<br />
ANESTESIOLOGÍA<br />
Carlos Estrada Gutiérrez, MD<br />
CIRUGÍA GENERAL<br />
José García Troncoso, MD<br />
CIRUGÍA ORTOPÉDICA<br />
Kenneth Cintrón, MD<br />
CIRUGÍA ESTÉTICA Y RECONSTRUCTIVA<br />
Natalio Debs Elías, MD<br />
CIRUGÍA TORACICA Y CARDIOVASCULAR<br />
José O’neill Rivera, MD<br />
CIRUGÍA DE LA MANO<br />
José Santiago Figueroa, MD<br />
DERMATOLOGÍA<br />
Luis J. Ortíz Espinosa, MD<br />
ENDOCRINOLOGÍA<br />
Eladio Santos Aponte, MD<br />
MEDICINA DE FAMILIA<br />
Marina Almenas, MD<br />
MEDICINA FÍSICA Y REHABILITACIÓN<br />
Miguel Berrios, MD<br />
MEDICINA INTERNA<br />
Ramón A. Suárez Villamil<br />
MEDICINA PREVENTIVA Y SALUD PÚBLICA<br />
Roberto Rosso Quevedo, MD<br />
OFTALMOLOGÍA<br />
Emilio Arce López, MD<br />
OTORRINOLARINGOLOGÍA<br />
Charles Juarbe<br />
SIQUIATRÍA<br />
Pedro Colberg, MD<br />
NEUROCIRUGÍA<br />
Edwin Lugo Piazza, MD<br />
UROLOGÍA<br />
Pedro Piquer Merino, MD<br />
MEDICINA DE EMERGENCIA<br />
Pablo Laureano Martí, MD<br />
JUNTA EDITORA<br />
Humberto Lugo Vicente, MD<br />
Presi<strong>de</strong>nte<br />
Luis Izquierdo Mora, MD<br />
Melvin Bonilla Félix, MD<br />
Carlos González Oppenheimer, MD<br />
Eduardo Santiago Delpin, MD<br />
Francisco Joglar Pesquera, MD<br />
Yocasta Brugal, MD<br />
Juan Aranda Ramírez, MD<br />
Francisco J. Muñiz Vázquez, MD<br />
Walter Frontera, MD<br />
Mario R. García Palmieri, MD<br />
Raúl Armstrong Mayoral, MD<br />
José Ginel Rodríguez, MD<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Este número <strong>de</strong>l Boletín por primera vez<br />
en los 105 años <strong>de</strong> historia <strong>de</strong>l mismo, le llegará<br />
al universo <strong>de</strong> los médicos <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong>. Esto<br />
es: a todos los médicos con licencia, a todos los<br />
estudiantes <strong>de</strong> medicina <strong>de</strong> nuestras cuatro escuelas<br />
y a todos los Internos y Resi<strong>de</strong>ntes, total una tirada<br />
<strong>de</strong> 12,000 ejemplares.<br />
Es por esto que hoy, quien mejor que el Dr.<br />
Ramón Emeterio Betances para engalanar la<br />
portada <strong>de</strong> nuestro Boletín. El Dr. Betances ha<br />
permanecido en el olvido colectivo por muchos<br />
años y como bien expresó el Dr. Francisco<br />
Manrique Cabrera, “aún se percibe el silencio<br />
oficial con que siempre se acoge a Betances”. Sin<br />
embargo es necesario traerlo a nuestra vida como<br />
ejemplo <strong>de</strong> un ser excepcional, en todas las fases<br />
<strong>de</strong> su existir. Hay que hacer excepción <strong>de</strong> algunos<br />
estudiosos que han trabajado para revivir a<br />
Betances a fin <strong>de</strong> dar a conocer toda su obra en<br />
<strong>Puerto</strong> <strong>Rico</strong> y otros países. Entre éstos hay que<br />
mencionar a:<br />
1. Luis Bonafoux, escritor y periodista, quien<br />
recopiló mucha información sobre<br />
Betances, fue su amigo y se <strong>de</strong>stacó en el<br />
extranjero, especialmente en España y<br />
Francia.<br />
2. Dra. Ada Suárez Díaz, ya fallecida<br />
catedrática universitaria, quien <strong>de</strong>dicó su<br />
vida a investigar y publicar las obras <strong>de</strong>l<br />
prócer y a quien su hijo y mi amigo, el<br />
Licenciado Gilberto Concepción Suárez,<br />
suele llamar “la eterna novia <strong>de</strong> Betances”.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
Mensaje <strong>de</strong>l Presi<strong>de</strong>nte y Portada<br />
Message from the Presi<strong>de</strong>nt and Cover<br />
DR. RAMÓN EMETERIO BETANCES<br />
3<br />
Por: Eduardo Rodríguez Vázquez, MD<br />
Presi<strong>de</strong>nte, Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
3. Los Doctores Félix Ojeda Reyes<br />
puertorriqueño, Paul Estra<strong>de</strong> (Francés)<br />
profesor Emérito <strong>de</strong> la Universidad <strong>de</strong> París,<br />
quienes han <strong>de</strong>dicado años a recopilar,<br />
<strong>de</strong>stacar y publicar la vida y obra <strong>de</strong> Betances.<br />
Su interés les ha llevado a varios países:<br />
Cuba, Santo Domingo, Francia, España,<br />
Estado Unidos y otros en la búsqueda <strong>de</strong><br />
información documental sobre nuestro<br />
patriota. Han continuado la labor titánica <strong>de</strong><br />
mantener viva su figura revisando archivos,<br />
bibliotecas y rescatando documentos,<br />
manuscritos, epistolarios y fotografías a fin<br />
<strong>de</strong> darlas a conocer.<br />
Estos esfuerzos han culminado en la<br />
publicación <strong>de</strong> una serie <strong>de</strong> libros, los cuales<br />
cubren toda la vida <strong>de</strong> Betances, <strong>de</strong>s<strong>de</strong> diferentes<br />
ópticas: familia, estudios, profesión, trabajo, labor<br />
política, profesional y muchos otros aspectos.<br />
Entre estos: La Manigua en París, El Anciano<br />
Maravilloso, El Desterrado <strong>de</strong> París. Ya se han<br />
empezado a publicar las obras completas <strong>de</strong><br />
Betances, siendo el primer volumen su labor<br />
como médico y científico, el cual me honro en<br />
prologar. Todos estos esfuerzos han llevado a<br />
Betances más allá <strong>de</strong> nuestros mares,<br />
eslabonándolo a figuras <strong>de</strong> la talla <strong>de</strong> José Marti,<br />
Simón Bolívar, San Martín y otros gigantes <strong>de</strong><br />
nuestra América. Sus gestiones pronto verán el<br />
fruto en una estatua <strong>de</strong> Betances en Nueva York,<br />
Central Park South y avenida las Américas entre<br />
las estatuas <strong>de</strong> Bolívar y Martí.
4<br />
El Dr. Ramón Emeterio Betances fue uno <strong>de</strong><br />
esos pocos hombres que pudieron combinar en<br />
su vida la excelencia como, estudiante, médico,<br />
patriota, amigo, benefactor, lí<strong>de</strong>r, creador,<br />
abolicionista, valiente ante la adversidad, pujante<br />
ante la injusticia, <strong>de</strong>sobediente ante las<br />
imposiciones <strong>de</strong> crueldad; no dobló nunca la<br />
cabeza, ni se amilanó.<br />
Lucho abiertamente <strong>de</strong> frente contra la tiranía<br />
<strong>de</strong> los que ostentaban el po<strong>de</strong>r y a pesar <strong>de</strong> toda<br />
su acción, nunca abandonó su profesión <strong>de</strong><br />
médico, la cual llevó hasta los menesterosos. En<br />
esas activida<strong>de</strong>s altruistas <strong>de</strong>sarrolló su existir.<br />
Betances viene a la vida en un momento histórico<br />
trascen<strong>de</strong>ntal, el siglo XIX, cuando Europa y la<br />
América Latina convulsionaban buscando avenidas<br />
<strong>de</strong> libertad personal y universal. La rebelión <strong>de</strong> las<br />
colonias norteamericanas contra Inglaterra y la<br />
revolución Francesa <strong>de</strong> 1789 fueron provocadas<br />
por esta ansia <strong>de</strong> libertad personal y comunitaria.<br />
Toda esta rebelión <strong>de</strong> los sojuzgados provocó la<br />
liberación <strong>de</strong> las colonias españolas en América y<br />
la libertad que gesta Bolívar, <strong>de</strong> cinco naciones:<br />
Chile, Colombia, Venezuela, Perú y Bolivia.<br />
En <strong>Puerto</strong> <strong>Rico</strong>, la situación colonial a<br />
principios <strong>de</strong>l siglo XIX, era insostenible ante la<br />
amenaza <strong>de</strong> las guerras <strong>de</strong> In<strong>de</strong>pen<strong>de</strong>ncia en<br />
América, España emite la Real Cédula <strong>de</strong> Gracias<br />
<strong>de</strong>l 1815, a fin <strong>de</strong> aumentar la población blanca<br />
con extranjeros monárquicos y leales a la corona<br />
Española, <strong>de</strong>bían a<strong>de</strong>más, profesar la fé católica.<br />
Llegaron a <strong>Puerto</strong> <strong>Rico</strong>, corsos, franceses,<br />
italianos, alemanes, eslavos y <strong>de</strong> otros países. A<br />
la par que emite esta disposición, impone otra real<br />
or<strong>de</strong>n para impedir que los estudiantes<br />
puertorriqueños y cubanos asistan a universida<strong>de</strong>s<br />
europeas, no españolas y a universida<strong>de</strong>s<br />
norteamericanas. Esta prohibición, que dura<br />
hasta la década <strong>de</strong>l 1830, logra su propósito y<br />
no es hasta 1835 que el primer puertorriqueño,<br />
el Dr. Pedro Gerónimo Goyco y Sabanetas, se<br />
graduó <strong>de</strong> la Facultad <strong>de</strong> Medicina en la<br />
Universidad <strong>de</strong> París.<br />
A partir <strong>de</strong> este momento, hay un movimiento<br />
sostenido <strong>de</strong> <strong>de</strong>cenas <strong>de</strong> jóvenes puertorriqueños<br />
que acu<strong>de</strong>n a Europa especialmente Francia y<br />
Alemania, a iniciar sus estudios universitarios. En-<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
tre estos, se encuentran los Hermanos José Marcial<br />
y Francisco Mariano Quiñónes, Santiago Porrata<br />
Doria, José Maria Arroyo y Juan Secchi (graduados<br />
<strong>de</strong> medicina en París), Gabriel Adolfo Ruiz <strong>de</strong><br />
Hei<strong>de</strong>lberg (1850), Agustín Stahl <strong>de</strong> Wurzburgo<br />
(1864) y otros. Entre ellos va el joven Betances.<br />
Betances llega a Tolosa a la edad <strong>de</strong> diez años,<br />
habiendo muerto su madre, su padre Don Felipe,<br />
lo envía bajo la tutela <strong>de</strong> Jacques Prevost, un<br />
farmacéutico francés, quien casó con una<br />
caborrojeña. Al llegar Prevost a <strong>Puerto</strong> <strong>Rico</strong>, la sub<strong>de</strong>legación<br />
<strong>de</strong> farmacia no convalidó su título, por<br />
lo que tuvo que regresar a su país. Siendo gran<br />
amigo <strong>de</strong> Don Felipe, éste <strong>de</strong>lega en Prevost, la<br />
educación <strong>de</strong> su hijo. Betances se gradúa con dos<br />
bachilleratos, uno en letras y otro en ciencias,<br />
requisitos indispensables para entrar a la facultad<br />
<strong>de</strong> medicina. Obtiene luego su Doctorado en<br />
Medicina y cirugía <strong>de</strong> la Universidad <strong>de</strong> París (1855).<br />
En esta universidad se relaciona con condiscípulos<br />
<strong>de</strong>stacados <strong>de</strong> la talla <strong>de</strong> Charcot, Labbe y Lorain.<br />
Tiene a<strong>de</strong>más una facultad extraordinaria <strong>de</strong><br />
profesores sobresalientes, reconocidos en la<br />
profesión <strong>de</strong> medicina, <strong>de</strong>ntro y fuera <strong>de</strong> Francia<br />
como: Trosseau, Nelaton, Brocca y Cruveilhier. Uno<br />
<strong>de</strong> sus profesores en Oftalmología, viéndolo operar<br />
una catarata comentó: “No hay nadie como los<br />
americanos <strong>de</strong>l sur que tengan esa habilidad innata”.<br />
Betances regresa a <strong>Puerto</strong> <strong>Rico</strong> en el 1856<br />
trayendo los aires <strong>de</strong> libertad que incorporó en<br />
Francia. Enfrenta un régimen absolutista, opresor,<br />
que promulga la sujeción y la esclavitud humana.<br />
Es entonces cuando se rebela y se torna en un adalid<br />
por la libertad <strong>de</strong> su patria en un <strong>de</strong>fensor <strong>de</strong> las<br />
injusticias y en “el Abolicionista”. No Abandona<br />
nunca su carrera <strong>de</strong> médico, prestó sus servicios al<br />
pueblo <strong>de</strong> Mayagüez, quien lo bautizó como “el<br />
Médico <strong>de</strong> los Pobres”, durante la epi<strong>de</strong>mia <strong>de</strong><br />
cólera. Su interés en las enfermeda<strong>de</strong>s fue tal que<br />
“modificó con éxito el tratamiento para la dispepsia,<br />
disentería, fiebre tifoi<strong>de</strong>a y tétano”. Fundó la Clínica<br />
San Antonio en Mayagüez, don<strong>de</strong> realizaba trabajos<br />
clínicos y <strong>de</strong> investigación a la par que atendía a<br />
sus pacientes fuera <strong>de</strong> ésta, aún a los indigentes en<br />
los hogares. En 1860 adoptó el tratamiento para<br />
la pulmonía, el que <strong>de</strong>spués fue utilizado, luego <strong>de</strong><br />
los <strong>de</strong>scubrimientos <strong>de</strong> Pasteur.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Su trabajo sobre la osqueotomía, para tratar la<br />
elefantiasis, fue presentado ante la Aca<strong>de</strong>mia <strong>de</strong><br />
Cirugía <strong>de</strong> París y estimado como uno <strong>de</strong> los más<br />
sobresalientes <strong>de</strong> su época. A<strong>de</strong>más <strong>de</strong> esto, no<br />
abandonó su lucha por la in<strong>de</strong>pen<strong>de</strong>ncia <strong>de</strong> <strong>Puerto</strong><br />
<strong>Rico</strong> y por la liberación <strong>de</strong> los esclavos. Fue<br />
<strong>de</strong>portado en varias ocasiones; en 1870 se instala<br />
en París <strong>de</strong>finitivamente hasta su muerte en 1898.<br />
Por su participación <strong>de</strong>stacada en la diplomacia<br />
antillana fue con<strong>de</strong>corado por el Gobierno Francés<br />
con la cruz <strong>de</strong> Gran Caballero <strong>de</strong> la Legión <strong>de</strong><br />
Honor.<br />
La evaluación <strong>de</strong> la actividad médica y científica<br />
<strong>de</strong> Betances pue<strong>de</strong> dividirse en tres períodos, a<br />
partir <strong>de</strong>l 1855, cuando presenta su tesis doctoral<br />
sobre el aborto.<br />
1. El primer periodo, 1855-64 se <strong>de</strong>staca por<br />
la escasez <strong>de</strong> sus publicaciones <strong>de</strong>bido a la<br />
censura gubernamental <strong>de</strong>l pensamiento<br />
escrito en <strong>Puerto</strong> <strong>Rico</strong> y por la ausencia <strong>de</strong><br />
facilida<strong>de</strong>s para ello. Durante este período<br />
Betances se envuelve <strong>de</strong> lleno en la práctica<br />
<strong>de</strong> la medicina y se inicia en sus luchas<br />
patrióticas y en la Abolición <strong>de</strong> la esclavitud<br />
que culmina en 1873.<br />
2. 1864-1887 Betances publica un solo artículo<br />
sobre osqueotomía ante la sociedad <strong>de</strong> cirugía<br />
<strong>de</strong> París <strong>de</strong>sborda toda su energía en<br />
activida<strong>de</strong>s políticas relacionadas con el Grito<br />
<strong>de</strong> Lares la abolición <strong>de</strong> la esclavitud y la<br />
in<strong>de</strong>pen<strong>de</strong>ncia en <strong>Puerto</strong> <strong>Rico</strong>. En el 1869,<br />
se va al exilio <strong>de</strong>finitivamente. Hemos<br />
encontrado un solo artículo sobre<br />
oftalmología en 1873. Participa <strong>de</strong> lleno en<br />
las luchas patrióticas y se <strong>de</strong>dica a la practica<br />
<strong>de</strong> la medicina en París.<br />
3. 1887-1898 en a<strong>de</strong>lante. Comienza a<br />
publicar activamente numerosos artículos<br />
sobre temas <strong>de</strong> medicina y científicos en<br />
Francia, España, Santo Domingo y <strong>Puerto</strong><br />
<strong>Rico</strong> hasta su muerte en 1898.<br />
El Dr. Betances publicó trabajos sobre:<br />
Oftalmología, Parasitología, Salud Pública, Viruelas,<br />
Vacunas, Medicina Preventiva, Trabajos sobre la<br />
leche, Ginecología, Urología, Técnicas Quirúrgicas,<br />
El cólera, entre otras. Esta visión multidisciplinaria<br />
<strong>de</strong> la vida <strong>de</strong> Betances es lo que hemos perdido a<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
través <strong>de</strong> los años. Hoy el médico es solo médico,<br />
el <strong>de</strong>ntista es <strong>de</strong>ntista, el enfermero es enfermero,<br />
el maestro es maestro. El profesional practica “eso<br />
que sabe”. Así, el cuadro general <strong>de</strong> la profesión se<br />
convierte en lo específico. Betances y su siglo nos<br />
dio una cátedra distinta, fueron los hombres <strong>de</strong>l siglo<br />
XIX, los que acu<strong>de</strong>n a Europa a estudiar, ciencias<br />
naturales, los que transformaron a <strong>Puerto</strong> <strong>Rico</strong>,<br />
añadiendo el elemento <strong>de</strong> estas ciencias, cambiaron<br />
nuestro <strong>de</strong>stino. Román Baldioroty <strong>de</strong> Castro y José<br />
Julián Acosta se licenciaron en física y matemáticas<br />
en España y Francia. Al regresar a <strong>Puerto</strong> <strong>Rico</strong>,<br />
Baldorioty enseño <strong>de</strong>s<strong>de</strong> Historia Natural hasta<br />
Náutica y Acosta, Agricultura hasta su muerte.<br />
La i<strong>de</strong>a <strong>de</strong> la educación en nuestros días es a<br />
veces, una enseñanza simplista <strong>de</strong> estudios culturales<br />
que “<strong>de</strong>sarrollan la sensibilidad y la espiritualidad<br />
<strong>de</strong>l alumno”. Debemos estudiar todo aquello que<br />
pertenece al intelecto abstracto, al estudio <strong>de</strong> las<br />
corrientes <strong>de</strong>l pensamiento que han regido al<br />
universo, a la difusión <strong>de</strong> la cultura clásica y la <strong>de</strong><br />
personas bien preparadas que posean un<br />
conocimiento amplio <strong>de</strong> los múltiples estudios <strong>de</strong>l<br />
ser humano. Muchos <strong>de</strong> los próceres <strong>de</strong> ese siglo<br />
Betances, Agustín Stahl, Pedro Gerónimo Goyco,<br />
Salvador Carbonell, José Francisco Basora, José<br />
Gualberto Padilla, Manuel Alonso, Manuel Zeno<br />
Gandía, Cayetano Coll y Toste, Martín Corchado y<br />
muchos otros, fueron a Europa a estudiar medicina<br />
y no otra profesión.<br />
La formación <strong>de</strong> nuestros principales<br />
abolicionistas, Betances, Basora, Acosta, Quiñónes<br />
era científica, exceptuando a Segundo Ruiz Belvis.<br />
Todos estuvieron influenciados por la Francia <strong>de</strong><br />
los altos principios revolucionarios. La historia que<br />
se nos ha enseñado ha omitido la verda<strong>de</strong>ra historia<br />
<strong>de</strong> las ciencias en nuestra cultura. Se nos ha limitado<br />
solo a apren<strong>de</strong>r una historia política, económica y<br />
social.<br />
Nuestra educación actual es cómoda, discursiva,<br />
a base <strong>de</strong> conferencias y <strong>de</strong> lecturas. Se nos habla<br />
mucho <strong>de</strong> lo que pensaron o dijeron otros, antes<br />
que nosotros. Y no es que esto esté mal, pero<br />
<strong>de</strong>bemos contribuir con nuestro pensamiento y<br />
análisis, a fin <strong>de</strong> lograr una crítica positiva a lo que<br />
se hace, contribuyendo con “lo que po<strong>de</strong>mos<br />
hacer”. ¿ Dón<strong>de</strong> están los nuevos Betances, los<br />
5
6<br />
Stahl, los Acosta, los Baldorioty <strong>de</strong> Castro que<br />
contribuirán al conocimiento general y específico?<br />
Y más aún ¿los que protestarán y combatirán los<br />
estatutos injustos y las malas <strong>de</strong>cisiones?<br />
Ellos fueron los que se apartaron <strong>de</strong> los<br />
aplausos <strong>de</strong>l momento, para <strong>de</strong>scifrar los misterios<br />
<strong>de</strong> la naturaleza, las enfermeda<strong>de</strong>s y los problemas<br />
<strong>de</strong> la sociedad. El hombre <strong>de</strong> ciencias, el médico,<br />
el maestro y otros proponían soluciones para<br />
beneficio <strong>de</strong> sus congéneres. La producción <strong>de</strong>l<br />
hombre <strong>de</strong> ciencias era constante y sin interés<br />
monetario alguno. Se vivía para saber y ayudar.<br />
Ese siglo XIX continuador <strong>de</strong> “La Ilustración”<br />
<strong>de</strong>spertó un gran estímulo, para innovar, inventar,<br />
para vivir una vida intensa, ayudando a su mundo<br />
a ser uno mejor. Existió entonces una intensidad<br />
<strong>de</strong>l esfuerzo humano para modificar lo que estaba<br />
mal y buscar nuevas soluciones. El hombre <strong>de</strong> ese<br />
siglo actuaba con <strong>de</strong>voción, para servir a su país.<br />
Era un hombre culto, que entendía la necesidad<br />
<strong>de</strong> proveer medios a<strong>de</strong>cuados para realizar los<br />
trabajos <strong>de</strong> investigación necesarios, para dotar a<br />
los estudiantes. Fueron hombres <strong>de</strong> una clara<br />
visión, quienes convencidos <strong>de</strong> la necesidad <strong>de</strong><br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
nuevos horizontes <strong>de</strong>jaron sentir sus opiniones, en<br />
momentos <strong>de</strong> rebeldía hacia lo impuesto y así<br />
lograron cambios en muchísimas esferas <strong>de</strong> las vidas<br />
<strong>de</strong> las gentes.<br />
Son estos hombres un reto para nosotros. En<br />
un país tan lleno <strong>de</strong> todo tipo <strong>de</strong> problemas como<br />
el nuestro ¿Qué hacemos? ¿Qué po<strong>de</strong>mos hacer<br />
a<strong>de</strong>más <strong>de</strong> ejercer nuestro trabajo en las horas<br />
impuestas? ¿Qué es lo que po<strong>de</strong>mos añadir en<br />
nuestra vida cotidiana para ayudar a resolver los<br />
problemas que cada día se tornan peor, por nuestra<br />
indiferencia a participar en la vida <strong>de</strong> nuestro <strong>Puerto</strong><br />
<strong>Rico</strong>? Por tanto, yo les exhorto a que se involucren<br />
con mayor intensidad en los grupos, socieda<strong>de</strong>s y<br />
asociaciones que intentan mejorar nuestro entorno.<br />
Que contribuyan con sus conocimientos y<br />
activida<strong>de</strong>s a inventar nuevas avenidas y proyectos<br />
que redun<strong>de</strong>n en el bienestar <strong>de</strong> nuestro pueblo. Si<br />
todos damos <strong>de</strong> nuestro tiempo, en corregir todo<br />
aquello que pue<strong>de</strong> mejorarse, nuestro <strong>Puerto</strong> <strong>Rico</strong><br />
podría atenuar o resolver los múltiples problemas<br />
que nos avasallan.<br />
Solo así podríamos disfrutar <strong>de</strong>l bienestar y la<br />
paz que tanto necesitamos.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Almost 105 years has passed since a group of<br />
renowned physicians foun<strong>de</strong>d a <strong>Medica</strong>l Scientific<br />
Journal in <strong>Puerto</strong> <strong>Rico</strong> un<strong>de</strong>r the shelter of the <strong>Puerto</strong><br />
<strong>Rico</strong> <strong>Medica</strong>l Association. This same Journal now<br />
known as ‘Boletin’ surpassed the tutelage of the<br />
National Library of Medicine in 1966 and became<br />
our first Medline source in <strong>Puerto</strong> <strong>Rico</strong>. Since then<br />
the struggles of time has placed our heritage in<br />
danger on several occasions. Thanks to the<br />
abnegated and unselfish work of a group of<br />
publishing board members, some who actually still<br />
prevails in their position, the ‘Boletin’ has continued<br />
to survive as one of the two Medline source of <strong>Puerto</strong><br />
<strong>Rico</strong> for our research writers. We are honored to<br />
push the gol<strong>de</strong>n pages of time a little longer.<br />
This first 2008 issue <strong>de</strong>als with clinical research<br />
work originating from our recent 58 th Annual Meeting<br />
of the American College of Surgeons - <strong>Puerto</strong><br />
<strong>Rico</strong> Chapter celebrated in <strong>Feb</strong>ruary 2008 at La<br />
Concha Hotel, San Juan, <strong>Puerto</strong> <strong>Rico</strong>. The original<br />
and case reports published encompass resi<strong>de</strong>nts<br />
and young surgeons writing their experience and<br />
results with the new technological advances of<br />
minimal invasive surgical procedures.<br />
The <strong>Puerto</strong> <strong>Rico</strong> <strong>Medica</strong>l Association and his<br />
presi<strong>de</strong>nt, Dr. Eduardo Rodriguez, have ma<strong>de</strong> an<br />
enormous effort to bring, free of charge, the<br />
Internal Medicine Resi<strong>de</strong>ncy, Damas Hospital – Ponce School of Medicine Teaching Consortium, Ponce, <strong>Puerto</strong> <strong>Rico</strong>.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
7<br />
EDITORIAL<br />
Humberto Lugo-Vicente MD, FACS, FAAP<br />
Editor-in-Chief, “Boletin” Asociación <strong>Medica</strong> <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
‘Boletin’ to all of our physician medical community,<br />
medical stu<strong>de</strong>nts and resi<strong>de</strong>nts to encourage them<br />
to see themselves publishing the new trends of our<br />
future medicine.<br />
We are also very happy to inclu<strong>de</strong> a very<br />
important review article on the history of parathyroid<br />
surgery in <strong>Puerto</strong> <strong>Rico</strong>, vis a vis the worldwi<strong>de</strong><br />
history, from our renowned professor and endocrine<br />
surgeon, Dr. Enrique Vázquez-Quintana. A lecture<br />
inclu<strong>de</strong>d as the main speaker of the 28 th Raffucci<br />
Surgical Research Forum.<br />
Finally, the abstracts presented during the 28 th<br />
Raffucci Forum are inclu<strong>de</strong>d also in this issue as a<br />
token of appreciation to the many hours of research<br />
each and every stu<strong>de</strong>nt, resi<strong>de</strong>nt and surgeon has<br />
<strong>de</strong>voted to their presentation.<br />
CME credits can be obtained after studying the<br />
three articles on parathyroid surgery inclu<strong>de</strong>d in this<br />
issue.<br />
Sincerely,<br />
Humberto Lugo-Vicente MD, FACS, FAAP
8<br />
Artículos Originales • Original Articles<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
PUERTO RICO EXPERIENCE WITH PLUGS IN THE<br />
TREATMENT OF ANAL FISTULAS<br />
By: Ignacio Echenique MD.*, Juan R. Mella MS**, Francisco Rosado MD.*, Ignacio A. Echenique MS §,<br />
Maria T. Mella MS § and Gerardo Quevedo MD. ¥<br />
ABSTRACT<br />
Background: Anorectal fistula is a common<br />
problem that affects quality of life. Main objective<br />
of therapy has been to eradicate the fistula tract<br />
while preserving fecal continence. Latest good results<br />
for anal fistula treatment have been an anal<br />
fistula plug. This study was un<strong>de</strong>rtaken to <strong>de</strong>termine<br />
if these results could be reproduced in <strong>Puerto</strong> <strong>Rico</strong>.<br />
Method: From January 2003 to January 2008,<br />
two experienced colorectal surgeons performed this<br />
new operation in 23 consecutive patients. A multivariable<br />
analysis was un<strong>de</strong>rtaken including age, sex,<br />
location of the fistula, previous surgeries, Seton<br />
placement before the insertion of the plug, continence<br />
pre and post operation, as well as close follow<br />
up. No patient with inflammatory bowel disease<br />
was inclu<strong>de</strong>d.<br />
Results: We had a good result or healing of the<br />
fistula in 14 of 23 patients for a success rate of 60%.<br />
We had a subgroup of patients who did slightly better<br />
and had a healing rate of 66% compared to the 60%<br />
of the whole group. It appears to be a trend in favor of<br />
the Seton group but is not statically significant. We<br />
had 9 failures of 23 patients or 39%. Suppuration<br />
was noticed in three patients and all three had failures<br />
of the plug with recurrences.<br />
Conclusions: This new operation is another<br />
alternative to add to our armamentarium but we<br />
need to search for an operation that <strong>de</strong>creases the<br />
inci<strong>de</strong>nce of recurrences we had in our study while<br />
maintaining function of the sphincters.<br />
Key words: plug, fistula-in-ano, surgery<br />
Anorectal fistulas are a common problem that<br />
results in a reduced quality of life as well as physical<br />
and emotional grief. They usually present with<br />
chronic drainage and a pustule-like lesion in the<br />
perianal region that can lead to pain during <strong>de</strong>fecation.<br />
The main objective of surgical therapy is to<br />
eradicate the fistula tract while preserving fecal continence.<br />
Depending on the location and type of fistula,<br />
management of anal fistulas can be quite challenging<br />
<strong>de</strong>spite several treatment options. Those<br />
with low transsphincteric or superficial fistulas can<br />
be treated by primary fistulotomy with low risk of<br />
incontinence. However, this procedure cannot be<br />
performed without risk in the case of mid or high<br />
fistulas. Subsequently, other options have been <strong>de</strong>veloped<br />
since the advent of the primary fistulotomy,<br />
albeit without much success, high recurrence rates,<br />
and/or relatively high complication rates.<br />
Advancement flap procedures have been rela-<br />
From the * Department of Surgery, Auxilio Mutuo Hospital, Rio Piedras, PR, ** Boston University, <strong>Medica</strong>l School, Boston, MA, § Jefferson’s<br />
<strong>Medica</strong>l School Phila<strong>de</strong>lphia, PA, and ¥ Department of Surgery HIMA-San Pablo, Bayamon, PR.<br />
Address reprints to: Ignacio Echenique MD - Office 218, Torre Auxilio Mutuo, 715 Ave. Ponce <strong>de</strong> Leon, Rio Piedras, PR, 00918. E-mail<br />
Poster presented during the 58 th Annual Meeting American College of Surgeons, <strong>Puerto</strong> <strong>Rico</strong> Chapter, <strong>Feb</strong>ruary 22, 2008,<br />
La Concha Hotel, San Juan, PR.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
tively successful in treating anal fistulas with closure<br />
rates as high as 75% (1). This procedure is<br />
technically difficult but has an incontinence rate<br />
between zero and 12.5% (2). The use of a Seton<br />
(Latin seta, a bristle) is a temporizing measure, as it<br />
is inten<strong>de</strong>d to drain and promote fibrosis while is<br />
not curative. The use of fibrin glue has a success<br />
between 50-70% (3). A major disadvantage of the<br />
use of glue in management of anal fistulas is the<br />
ten<strong>de</strong>ncy to become dislodged and eventually extru<strong>de</strong>d<br />
from the secondary opening of fistula tract,<br />
thus resulting in failure of the tract closure. A more<br />
recent therapeutic measure is an anal fistula plug<br />
ma<strong>de</strong> of lyophilized porcine intestinal submucosa.<br />
Recent studies using this plug have been promising.<br />
Champagne et al. have achieved a success rate<br />
of 83% using this new anal fistula plug (3, 4).<br />
Essentially, the fistula plug is an extracellular<br />
matrix that is harvested from porcine small intestinal<br />
submucosa (5, 6). This biomaterial provi<strong>de</strong>s a<br />
scaffold for which it allows a<strong>de</strong>quate strength for<br />
tissue support and permits host cells to reconstruct<br />
related tissues. It acts as a “substitute <strong>de</strong>rmis” that<br />
already possesses several of the factors required for<br />
wound healing and may result in improvement of a<br />
healing injury as in the case of a fistulous tract (7).<br />
Given the high success rate <strong>de</strong>scribed in the literature<br />
for treatment of anal fistula using the anal fistula<br />
plug, this clinical study was un<strong>de</strong>rtaken to <strong>de</strong>termine if<br />
these results could be reproduced in <strong>Puerto</strong> <strong>Rico</strong>.<br />
METHOD<br />
A retrospective analysis based on the personal<br />
experience of two colorectal surgeons using a new<br />
operation for anal fistulas between 2006 and 2008<br />
encompass this study. Results and complications<br />
from this surgical procedure for management of anal<br />
fistulas using an anal fistula plug (Surgisis, Cook<br />
Surgical, Inc.) were evaluated (see Figure 1).<br />
A total of 23 patients were operated during<br />
this period. Factors examined were age, sex, previous<br />
surgery and continence. Other factors studied<br />
such as presence of a complex fistula, multiple<br />
external openings, complications, recurrences<br />
and if re-operation was necessary were<br />
also evaluated. Length of the fistula was <strong>de</strong>fined<br />
as short, mid or long fistulas according to<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
Figure 1: Anal fistula plug<br />
Godsall’s rule. All patients enrolled had mo<strong>de</strong>rate<br />
or <strong>de</strong>ep transsphincteric fistula. Complex fistulas<br />
were not exclu<strong>de</strong>d. Preoperative evaluation<br />
consisted of exclusion of Crohn’s disease,<br />
Endorectal Sonogram and MRI when indicated.<br />
No infections were apparent at the time of anal<br />
fistula plug treatment. In patients that presented<br />
with an abscess we waited three months after the<br />
placement of a Seton and placement of the fistula<br />
plug.<br />
Patients un<strong>de</strong>rwent preoperative mechanical<br />
bowel preparation and prophylactic antibiotics were<br />
given. Spinal anesthesia was used and patients<br />
placed were in jackknife position. We used the standard<br />
technique (6), irrigating the fistula with hydrogen<br />
peroxi<strong>de</strong>, without enlarging the internal opening<br />
or curettage of the track. I<strong>de</strong>ntification of the<br />
internal opening was done after gentle probing<br />
when a Seton was not present. Placement of the<br />
plug, snug in the track and suturing of the plug to<br />
the internal sphincter with a figure of eight absorbable<br />
suture, with closure of the internal opening<br />
and coverage of the plug was performed. Externally,<br />
excess plug was excised and a simple absorbable<br />
suture was used to fix the plug to the skin ensuring<br />
that the skin would remain open for a<strong>de</strong>quate<br />
drainage. Stool softeners, rest and <strong>de</strong>creased physical<br />
activity, prevention of constipation or straining<br />
were encouraged in the postoperative period.<br />
9
10<br />
Figure 2: Fistula plug results<br />
RESULTS<br />
We reviewed the data obtained from the medical<br />
records of patients since the first operation three years<br />
ago with a mean follow up of ten months; the shortest<br />
follow up was five months. The condition was more<br />
common in men than women; 62% compared with<br />
38% respectively. The left anterior area was the most<br />
common location, two long fistulas, two complexes<br />
and 1 horseshoe fistula.<br />
Continence was not affected in any of our patients.<br />
In one case the plug had dissolved and in another, the<br />
plug was dislodged. There were no reported cases of<br />
bleeding, allergic reactions or medical complications.<br />
A total of 23 patients were operated. Eighteen of<br />
23 had a Seton in place before plug surgery was done.<br />
The most common operation before the plug was<br />
drainage of abscess and Seton placement. Other operations<br />
inclu<strong>de</strong>d two procedures for hemorrhoids.<br />
Three patients had no surgery prior to the <strong>de</strong>velopment<br />
of the anal fistula.<br />
Good results: We had good result or healing<br />
of the fistula in 14 of 23 patients for a success rate<br />
of 60% (see Figure 2). Of the 23 total patients, 18<br />
had drainage of an abscesses and placement of<br />
Seton with at least three months between the Seton<br />
placement and the insertion of the plug. Of<br />
the18 patients that had a Seton, 12 (66%) healed.<br />
This was not statistically significant (p = 0.26). Of<br />
the 14 patients with healing of the fistula, 12 (86%)<br />
of the patients had a Seton in place before the placement<br />
of the plug. Secretions of the external opening<br />
were not a factor in predicting who would heal<br />
or fail. However, it may take some time before a<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 3: Total healing group<br />
final outcome can be <strong>de</strong>termined.<br />
Failures: We had 9 failures of 23 patients or<br />
39%. Of these five patients had no Seton placed<br />
before the placement of the fistula plug and 3 of<br />
them failed (60%) and required a re-operation due<br />
to abscess formation. Suppuration was noticed in<br />
3 patients and all three had failures of the plug with<br />
recurrences (see Figure 3).<br />
DISCUSSION<br />
Challenges of treating anal fistulas are prevention<br />
of recurrence and preservation of anal sphincter function.<br />
Since medieval times treatment of anal fistulas<br />
has been a challenge. Surgical techniques have improved<br />
significantly but still many times we must perform<br />
drainage, what John of Ar<strong>de</strong>rne did in London<br />
in 1307 (8). Herman and Desfosses recognized the<br />
presence of glands in the submucosa and the internal<br />
sphincter in 1880, commonly believed to be the origin<br />
of the infections causing abscesses that <strong>de</strong>veloped<br />
into fistulas (9).<br />
Closure of the primary opening with an absorbable<br />
suture plus the use of a biologic anal fistula plug is<br />
another alternative for treating anorectal fistulas with<br />
little risk of incontinence.<br />
A review of the literature available <strong>de</strong>scribed a<br />
success rate between 60 to 80% (5, 6, 7). Our experience<br />
with the 23 patients is 60% but we noted a subgroup<br />
of patients who did slightly better when a previous<br />
Seton was in place and a long fistulous tract (> 3<br />
cm) was not found .<br />
There were complications from this procedure.<br />
Three patients required re-operation and placement<br />
of a Seton for treatment of abscesses. Leaving the<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
external opening for drainage is an important factor<br />
as we noticed accumulation of secretions in this<br />
area that were resolved by wi<strong>de</strong>ning of the external<br />
opening and oral antibiotics. An abscess <strong>de</strong>veloped<br />
exclusively in case of <strong>de</strong>finite failures. Secretions<br />
alone did not correlate with recurrence of the fistulas.<br />
It is important to prevent premature closure of<br />
the external opening as this could lead to formation<br />
of an abscess with failure of the plug and recurrence.<br />
It is also important not to have significant<br />
purulent drainage during at least three months<br />
between drainage of an abscess with Seton placement<br />
before the insertion of the plug.<br />
Basic principles of surgery such as “Do No Harm”<br />
and “Simpler is Better” should be in our minds when<br />
we go into the operative room. If we can obtain a low<br />
recurrence rate with preservation of the sphincter function,<br />
then we have achieved these important principles.<br />
We continue to explore different alternatives and in<br />
the process add new surgical techniques. All surgical<br />
techniques mentioned have a role but we must still<br />
search for a way to <strong>de</strong>crease the inci<strong>de</strong>nce of recurrences<br />
we had in our study.<br />
This new operation is not risk free and it appears<br />
that there may be a benefit to having previous placement<br />
of a Seton before the insertion of the fistula plug.<br />
In this study a subgroup of patients who did slightly<br />
better and had a healing rate of 66% compared to the<br />
60% of the whole group. It appears to be a trend in<br />
favor of the Seton group but is not statically significant<br />
(p = 0.28 NS). This group had a Seton in place<br />
before placement of the fistula plug. This small benefit<br />
could be due to a better-<strong>de</strong>fined fistula track and less<br />
purulent material. The non-seton group in our study<br />
was too small to conclu<strong>de</strong> that all patients should have<br />
a Seton before the insertion of a plug. Further studies<br />
should address this issue. Secretions of the external<br />
opening occurred in some cases and did not correlate<br />
with recurrences. Abscess formation, a fistula with long<br />
track (> 3cm) and dislodging of the plug, were important<br />
factors in the recurrence group. This new technique<br />
with the use of a fistula plug is here to stay and<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
11<br />
we must continue to evaluate the results obtained so<br />
we can do better patients selection of those that could<br />
benefit from this new operation.<br />
RESUMEN<br />
Las fístulas anales son una condición muy frecuente<br />
que afecta la calidad <strong>de</strong> vida <strong>de</strong> los que la pa<strong>de</strong>cen. El<br />
objetivo principal <strong>de</strong>l tratamiento <strong>de</strong> las fístulas anorectales<br />
ha sido el erradicar el tracto fistuloso y a la<br />
misma vez preservar la continencia fecal. Recientemente<br />
se han reportado buenos resultados en el tratamiento<br />
<strong>de</strong> fístulas anales con el uso <strong>de</strong> un tapón para<br />
fístulas (‘anal fistula plug’). Este estudio se llevó a cabo<br />
para <strong>de</strong>terminar si estos buenos resultados se podían<br />
reproducir en <strong>Puerto</strong> <strong>Rico</strong>.<br />
Des<strong>de</strong> enero 2003 a enero 2008, dos cirujanos<br />
colorectales llevaron a cabo esta nueva operación<br />
en 23 pacientes consecutivos. Se hizo un análisis<br />
multifactorial incluyendo sexo, edad, localización<br />
<strong>de</strong> la fístula, cirugías previas, presencia <strong>de</strong><br />
Seton previo a la inserción <strong>de</strong>l tapón, continencia<br />
antes y <strong>de</strong>spués <strong>de</strong> la operación y un seguimiento<br />
bien cercano. Ningún paciente con enfermedad<br />
inflamatoria <strong>de</strong>l intestino fue incluido.<br />
Se obtuvo un buen resultado o cicatrización <strong>de</strong> la<br />
fístula en 14 <strong>de</strong> 23 pacientes para un resultado satisfactorio<br />
<strong>de</strong> 60%. Tuvimos un subgrupo <strong>de</strong> pacientes<br />
con un Seton previo que les fue levemente mejor con<br />
cicatrización <strong>de</strong> la fístula en un 66% comparado con<br />
60% <strong>de</strong>l grupo total. Este beneficio leve no fue<br />
estadísticamente significativo pero sugiere una ten<strong>de</strong>ncia<br />
a ser favorecido el tener un Seton previamente a la<br />
inserción <strong>de</strong>l “Plug”. La operación no funcionó en 9<br />
<strong>de</strong> 23 pacientes o 39%. Supuración se notó en tres<br />
pacientes y los tres fallaron en cerrar la fístula con el<br />
“Plug” con recurrencias.<br />
Esta nueva operación es otra alternativa para sumarse<br />
a las alternativas quirúrgicas pero aun tenemos<br />
que encontrar una operación que disminuya la inci<strong>de</strong>ncia<br />
<strong>de</strong> recurrencias que encontramos en nuestro estudio<br />
y a la misma vez mantenga la función <strong>de</strong>l esfínter.
12<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
REFERENCES<br />
1. Lewis P, Bartolo DC. Treatment of trans-sphincteric fistulae by full thickness anorectal advancement flaps. Br J Surg 1990; 77: 1187–9.<br />
2. Williams, J. G., Farrands, P. A., Williams, A. B., Taylor, B. A., Lunniss, P. J., Sagar, P. M., Varma, J. S. & George, B. D.The Treatment<br />
of Anal Fistula: ACPGBI Position Statement.Colorectal Disease 9 (s4), 18-50.<br />
3. Eric K. Johnson, Janette U. Gaw, David N. Armstrong,Efficacy of Anal Fistula Plug vs. Fibrin Glue in Closure of Anorectal Fistulas, DCR:<br />
vol 49,no. 3 March,2006.<br />
4. Champagne, Bradley J. (2006) Efficacy of Anal Fistula Plug in Closure of Cryptoglandular Fistulas: Long-Term Follow-Up. Diseases of the<br />
Colon & Rectum<br />
5. Maluf-Filho F, Ishioka S, Moura E, Berti L, Sakai P, Garrido A, Gama-Rodrigues J. Fistulae with an acellular matrix. Abstract presented at<br />
the Digestive Disease Week® 2004.<br />
6. Robb BW, Nussbaum MN, Vogler SA, Sklow B. Early experience using porcine small intestinal submucosa to repair fistulas-in-ano. 2004<br />
Annual Meeting of the American Society of Colon & Rectal Surgeons.<br />
7. (2007) The surgisis® AFP anal fistula plug: report of a consensus conference. Colorectal Disease 0(0)<br />
8. John of Ar<strong>de</strong>rne, GLASGOW UNIVERSITY LIBRARY SPECIAL COLLECTIONS DEPARTMENT, England http://special.lib.gla.ac.uk<br />
9. Hermann G, Desfosses L. Sur la muquese <strong>de</strong> la region cloacale du rectum. Comptes end Acad <strong>de</strong>s Sci 1880; 90: 1301–2.<br />
ANUNCIO PÚBLICO • AMPR<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
ABSTRACT<br />
Background: Hand assisted laparoscopic<br />
colectomy (HALS) has been shown to have the advantages<br />
of laparoscopic colectomy in terms of pain,<br />
recovery and length of hospital stay. Studies have<br />
shown similar outcomes in laparoscopic colectomy<br />
as in open surgery. There is a learning curve to<br />
HALS, the operative time is longer, and it is more<br />
difficult than open surgery and requires specialized<br />
equipment. In this report we present our initial<br />
experience over a 2.5 year period using HALS for<br />
colon surgery for diverticulosis, polyps and colon<br />
cancer.<br />
Methods: A retrospective review of office and<br />
hospital charts of patients un<strong>de</strong>rgoing HALS colectomy<br />
from June 2005 to January 2008 was performed<br />
at HIMA-San Pablo Hospital. Demographics,<br />
outcomes data including operative time, conversion<br />
rate to open surgery, reasons for conversion,<br />
time to start feedings, and length of stay were<br />
collected as well as staging and number of no<strong>de</strong>s<br />
for cancer patients. Complications are discussed<br />
along with comments pertinent to the experience<br />
of two surgeons going through the learning curves<br />
of LC and HALS colectomy.<br />
Results: A total of 65 patients un<strong>de</strong>rwent attempted<br />
hand assisted laparoscopic colon resection.<br />
There were 33 males and 32 females between the<br />
ages of 26 and 87. Thirty-one patients un<strong>de</strong>rwent<br />
surgery for diverticulosis; 8 for pre-malignant le-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
13<br />
Artículos Originales • Original Articles<br />
EXPERIENCE WITH HAND ASSISTED<br />
LAPAROSCOPIC SURGERY OF THE COLON<br />
By: Ramón K. Sotomayor, MD.* and Bolivar Arboleda, MD.*<br />
sions (large polyps or polyps with high gra<strong>de</strong> dysplasia),<br />
and 26 for colon cancer. Mean operative<br />
time was 195 minutes (120 to 300); mean length<br />
of stay was six days (range 4-14 days). Conversion<br />
rate was (13.8 %) overall; 21 % during the first year<br />
and 10.8 % after the first year. 5 (7.5 %) of the<br />
patients in which HALS colon resection was completed<br />
had complications with prolonged length of<br />
stay. Patients without complication had an average<br />
length of stay of 4.5 days. The average number of<br />
lymph no<strong>de</strong>s was 14.8 (range 7-24); average length<br />
of specimens for diverticulosis was 17cm. Complications<br />
inclu<strong>de</strong>d postoperative bleeding in three<br />
patients who required early reoperation, prolonged<br />
ileus and small bowel obstruction in two patients.<br />
One patient <strong>de</strong>veloped a pelvic collection requiring<br />
a drain, and one patient had a wound infection requiring<br />
re-admission and antibiotics. No patient required<br />
colostomy due to a complication. There were<br />
no operative <strong>de</strong>aths.<br />
Conclusion: HALS colectomy is a safe and<br />
feasible alternative to open colectomy in a<br />
community hospital setting with proper expertise<br />
and equipment. Patients will benefit from faster<br />
recovery time and <strong>de</strong>creased length of stay in the<br />
hospital. Oncologic results are similar to open<br />
surgery. Operative times are longer than with<br />
open surgery and the operations are difficult to<br />
learn and master.<br />
* From the Department of Surgery Hospital Interamericano <strong>de</strong> Medicina Avanzada, Caguas, <strong>Puerto</strong> <strong>Rico</strong>. Address reprint requests to: Ramon K.<br />
Sotomayor, MD - 300 La Sierra Ave. Aptdo. 61 San Juan, PR 00926. E-mail: ksotomayor@msn.com. Poster Presented at the 58th Annual<br />
Meeting of the <strong>Puerto</strong> <strong>Rico</strong> Chapter of the American College of Surgeons <strong>Feb</strong> 21, 2008, La Concha Hotel, San Juan, <strong>Puerto</strong> <strong>Rico</strong>.
14<br />
Key words: hand assisted, laparoscopy,<br />
colon, surgery<br />
In June 2005 the first cases of Hand Assisted<br />
Laparoscopic colon resections were performed. The<br />
two surgeons participating in this work were experienced<br />
with basic and advanced laparoscopic procedures<br />
namely cholecystectomies, appen<strong>de</strong>ctomies,<br />
Nissen fundoplications and ventral hernias. In this presentation<br />
we were able to review 65 hospital charts of<br />
patients who un<strong>de</strong>rwent hand assisted laparoscopic<br />
surgery. The results and outcomes are discussed in<br />
the following tables; operative time, length of stay,<br />
conversion rate to open surgery, and complications.<br />
We also looked at the stage of the patients, the number<br />
of lymph no<strong>de</strong>s obtained in the specimens and the<br />
length of the specimens in patients who had colon<br />
resection for diverticular disease.<br />
In general, hand assisted laparoscopic resections<br />
were performed using one of the commercially available<br />
hand assist <strong>de</strong>vices Lap Disc (Ethicon) or Gelport<br />
(Applied <strong>Medica</strong>l), are extremely useful as they allow<br />
use as a “hand port” or as a working port by supporting<br />
a trocar by which the camera or instruments can<br />
be passed. Hand assist <strong>de</strong>vices allow the use of tactile<br />
sensation during laparoscopic surgery, and allow easier<br />
atraumatic retraction of the bowel (1, 2). Colon resections<br />
are more difficult than other laparoscopic procedures,<br />
as the surgeon needs access to more than one<br />
quadrant of the abdomen. By facilitating exposure,<br />
hand <strong>de</strong>vices make laparoscopic colon surgery easier<br />
(3). The hand assist <strong>de</strong>vice also protects the wound<br />
during the retrieval of the specimen and for construction<br />
of extracorporeal anastomosis. Disadvantages of<br />
hand assisted surgery inclu<strong>de</strong> the hand getting in the<br />
way in initial cases and the fact that the hand is a<br />
rather large “instrument”. Hand fatigue is also an issue,<br />
but hand assist <strong>de</strong>vices are very useful because<br />
they may be used as a trocar to pass instruments and<br />
perform a fully laparoscopic operation and have been<br />
found to preserve the features of minimally invasive<br />
rugby procedures in terms of postoperative pain, recovery<br />
and oncologic outcome (4).<br />
In this presentation we intend to document what<br />
we have learned in our initial cases and the problems<br />
and pitfalls associated to starting a minimally<br />
invasive colon surgery program.<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Technique for Hand Assisted Laparoscopic<br />
Colon Resections<br />
The technique for hand assisted laparoscopic<br />
colon resections according to the center, but most<br />
authorities agree on proper positioning of the patient,<br />
and careful planning of the trocar positions<br />
and the hand port, in or<strong>de</strong>r to maximize its benefits<br />
in facilitating the operations (1, 2, 3).<br />
We performed segmental resections following<br />
what we found has worked in our center. All cases<br />
were electively admitted. In general, standard bowel<br />
preparation, antibiotic and <strong>de</strong>ep venous thrombosis<br />
with pneumatic compression <strong>de</strong>vices or low<br />
molecular weight heparin was utilized. Small cancers<br />
and polyps were marked prior to surgery. General<br />
endotracheal anesthesia was used. Five and 12<br />
mm trocars, 0 <strong>de</strong>gree and 30 <strong>de</strong>gree, 5 and 10mm<br />
lenses and two monitors were routinely used. For<br />
division of vessels, monopolar cautery, harmonic<br />
scalpel (Ethicon) or LigaSure (Covi<strong>de</strong>n), endoscopic<br />
staplers and endoloops were used.<br />
For left colon cases, the patients were placed<br />
in the semi-lithotomy position, lighted ureteral catheters<br />
were placed and the hand assist <strong>de</strong>vice was<br />
usually placed in the left lower quadrant. Routine<br />
mobilization of the splenic flexure was performed,<br />
anastomosis was intracorporeal with a circular stapling<br />
<strong>de</strong>vice and sigmoidoscopy and insufflation test<br />
was done on all cases.<br />
Right colon resections were done in the supine<br />
position with the hand assist <strong>de</strong>vice in the right lower<br />
quadrant, vessels were divi<strong>de</strong>d intracorporeally and<br />
the anastomosis extracorporeal. Patients were usually<br />
monitored in the intermediate unit overnight.<br />
Nasogastric tubes were used on discretion of the<br />
surgeon. Diet was started when passing flatus, and<br />
discharge after regular bowel movement.<br />
RESULTS<br />
Table 1 shows the <strong>de</strong>mographics of the patients<br />
un<strong>de</strong>rgoing hand assisted laparoscopic colon<br />
resection. Ages ranged from 27 to 87 years old.<br />
48 % un<strong>de</strong>rwent surgery for diverticular disease,<br />
40 % for colon cancer and 12 % for polyps or high<br />
gra<strong>de</strong> dysplasia. 24 patients (37%) had segmental<br />
resections of the right colon with ileo-transverse<br />
colon anastomosis, 38 patients (58%) had segmental<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 1- Demographic data of patients un<strong>de</strong>rgoing hand<br />
assisted laparoscopic colectomy*<br />
total patients<br />
no. patients<br />
65<br />
Gen<strong>de</strong>r 33 females/32 males<br />
Ages<br />
Diagnosis<br />
26 years to 87 years mean- 63years<br />
- diverticulosis 31 (48 %)<br />
-colon cancer 26 (40 %)<br />
-polyps/dysplasia<br />
Procedures<br />
8 (12 %)<br />
- HALS right colectomy 24 (37 %) 2 pt-lap chol w hals rt col<br />
-HALS left colectomy 38(58 %) 5 pt lapp appy w hals lt colon<br />
-HALS transverse colon<br />
-other<br />
3( 5 % )<br />
*all patients in which laparoscopic resection was attempted or started<br />
are inclu<strong>de</strong>d.<br />
resection of the left colon with an intracorporeal<br />
low pelvic anastomosis. Two patients had<br />
laparoscopic cholecystectomies during colon<br />
resection and five patients appen<strong>de</strong>ctomies.<br />
Mean operative time was 195 minutes, ranging<br />
from 120 to 300 minutes (Table 2). Overall,<br />
nine patients (13.8%) required conversion to open<br />
surgery. Diet was started on average of three days<br />
(Range 2 to 7 days). Five patients (7.6%) had complications<br />
requiring prolonged length of stay; overall<br />
length of stay was six days. In patients without a<br />
complication, length of stay was 4.5 days. Three<br />
patients required re-operation in the post-operative<br />
period (4.6 %), and six patients required readmissions<br />
for other reasons.<br />
Table 3 shows the rates and reasons for conversion<br />
to open surgery. During the first year, 21 % of<br />
the patients required conversion to open surgery, while<br />
during the second year only five out of 46 patients<br />
(10.8 %), required conversion. Right colon resections<br />
had an 8.3 % rate of conversion while left colon resections<br />
had an 18.3% rate of conversion to open<br />
surgery. Reasons for conversion were bleeding, large<br />
tumor, one splenic laceration and severe adhesions<br />
from diverticular disease.<br />
Complications are listed on Table 4. Three patients<br />
were reoperated during the first 24 hours;<br />
two due to intraabdominal bleeding, and one due<br />
to anastomotic bleeding. Two patients were found<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
Table 2- Immediate outcome of HALS colon resection<br />
Operative time ( minutes)<br />
mean 195 range 120-300<br />
Conversion to open 4/26<br />
days to start diet (days) 3.36 2-7days<br />
complications with prolonged los 5<br />
length of stay (total) 6 days 4-14 days<br />
length of stay (w out compication) 4.5 days 4-7days<br />
reoperation 2<br />
15<br />
with symptomatic anemia in the post op period,<br />
and were transfused without need for surgery. Two<br />
patients had prolonged ileus; one had documented<br />
small bowel obstruction which resolved with<br />
nasogastric suction. One patient had fever and a<br />
pelvic collection which was drained in the<br />
interventional radiology suite. There were two superficial<br />
wound infections and one <strong>de</strong>ep wound infection<br />
which required re admission, drainage and<br />
antibiotics, which was quite difficult to treat due to<br />
infection running between the planes of the flank<br />
musculature. One patient required admission to the<br />
intensive care unit due to acute respiratory insufficiency<br />
and resolved in 48 hours. There was no need<br />
for diverting stomas as a complication and no<br />
perioperative <strong>de</strong>aths.<br />
Pathological data is listed in Table 5. The colon<br />
cancer specimens had an average of 14.8 no<strong>de</strong>s, and<br />
ranged from 7 to 34. The length of the diverticulosis<br />
cases averaged 17cm, range from 12 to 28cm.<br />
DISCUSSION<br />
Our patients were evenly distributed in terms<br />
of diagnosis with 47% diverticular disease, 38%<br />
for cancer and 12% for polyps or dysplasia.<br />
Operative times in this series ranged from 2 to 4<br />
hours, with an average of three hours in most<br />
cases. We found left colons usually took longer,<br />
namely because of inflammatory conditions<br />
related to past episo<strong>de</strong>s of inflammation. This is<br />
usually the case in most series (3).<br />
The conversion rate to open surgery is an<br />
important issue in laparoscopic surgery. HALS<br />
colon surgery has been found to have a lower<br />
conversion rate than “pure” laparoscopic<br />
approach; and in fact some critics have pointed<br />
out that HALS is really open surgery. The fact is
16<br />
Table 3- Rates and Reasons for Conversion to Open Surgery<br />
no. of patients ( %) comments<br />
Total conversions 9 / 61 (14 %)<br />
during 1st year 4 / 19 (21 %)<br />
After 1st year<br />
HALS Right<br />
5/46 (10.8 %)<br />
Hemicolectomy<br />
HALS Left<br />
2/24 (8.3 %) 1 intraop bleeding<br />
1 large tumor<br />
ureter position unclear<br />
Colectomy w Low 7/38 ( 18.4 %) 1 splenic<br />
Pelvic Anastomosis laceration-splenorraphy<br />
1 inability to mobilize splenic flexure<br />
5 severe adhesions<br />
due to diverticular disease<br />
HALS Transverse<br />
colectomy 0/3<br />
that hand assist <strong>de</strong>vices allow either combination<br />
of pure laparoscopic surgery or the surgeon can<br />
switch to a hand assisted technique as is<br />
necessary (4). Sometimes in our initial cases we<br />
felt that the hand would obstruct the field of view,<br />
and hand fatigue was an issue which we have<br />
learned to <strong>de</strong>al with. At the present time we<br />
approach most cases laparoscopically and use<br />
hand assistance freely for certain difficult parts<br />
of the operation.<br />
The conversion rate was 13.8% overall; but<br />
we broke this down to the conversions in the first<br />
year which were 21% and 10.8% after one year<br />
performing the procedures.<br />
We take this as an expected welcome event, as<br />
it shows progress in <strong>de</strong>veloping new techniques.<br />
One conversion was due to a splenic capsule tear,<br />
one due to a very large tumor invading the abdominal<br />
wall, one due to bleeding, and the remain<strong>de</strong>r<br />
due to inflammatory adhesions. We expect our<br />
conversion rate to further <strong>de</strong>crease with time. One<br />
interesting observation regarding conversions was<br />
the difference in conversion rates between right colon<br />
(8.3 %) and left hemicolectomy (18.4 %). We<br />
attribute this to the difficulty in <strong>de</strong>aling with<br />
inflammatory adhesions and the need to mobilize<br />
the splenic flexure for proper tension free anastomosis.<br />
In the initial experience we have found this<br />
part of the operation to be particularly difficult.<br />
Major complications were the need to re –<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 4- Complications of HALS Colon Resections<br />
no. comments/ outcome<br />
reoperation due to bleeding 3<br />
drop in hgb requiring<br />
2 mesentery, 1 anastomosis<br />
transfusion without surgery 2<br />
outcome<br />
two U PRBC transfused, no adverse<br />
prolonged ileus<br />
suction<br />
2 <strong>de</strong>layed gastric emtpying-nasogastric<br />
small bowel obstruction<br />
Infections<br />
1 nasogastric suction<br />
intraabdominal/ pelvic 1 pelvic drain, CT gui<strong>de</strong>d, antibiotics<br />
urinary 1 re- admission, antibiotics<br />
wound 3 1 re-admit, drain, antibiotics<br />
pulmonary<br />
need for diverting stomas<br />
1 icu stay 48 hr<br />
Carciac, thromboembolic 0<br />
Deaths 0<br />
Table 5- Number of lymph no<strong>de</strong>s and length of specimens<br />
mean range<br />
Colon cancer specimens *<br />
number of lymph no<strong>de</strong>s<br />
Diverticulosis<br />
14.8 7 to 34<br />
length of specimen** 17cm 12 to 28 cm<br />
* inclu<strong>de</strong>s patients with polyps and high gra<strong>de</strong> dysplasia<br />
** specimen length measured by pathology lab<br />
operate on three patients due to bleeding. Two<br />
were due to bleeding from the mesentery of the<br />
colon; and one had an anastomotic bleed which<br />
required re- suturing of the anastomosis 24 hours<br />
after initial surgery. Although this is a pertinent<br />
risk in open surgery, we have learned to divi<strong>de</strong><br />
large vessels intracorporeally with electrosurgical<br />
instruments and staplers this has <strong>de</strong>creased. One<br />
important technical point is to release the tension<br />
on the tissues when dividing the vessels.<br />
We had two patients in which the hemoglobin<br />
level dropped in the post op period, due to<br />
symptomatic anemia, both were transfused and<br />
observed and none required surgery. This is a<br />
complication which again relates to the level of<br />
familiarity with the instruments and the technique<br />
and should <strong>de</strong>crease with experience.<br />
The time to start diet was relatively short as well<br />
as the length of stay, although we have been extremely<br />
conservative in starting diet and discharging patients.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Patients without complications usually started diet on<br />
the 3 rd postop day, and could be discharged on day<br />
four. Several patients had prolonged ileus, small bowel<br />
obstruction and one had a leak which required a drain<br />
and a prolonged stay. Other complications were relatively<br />
minor; two superficial wound infections. There<br />
was one rather difficult wound infection in the lap disc<br />
incision, which we attributed to misplacement of the<br />
lap disc with some enteric spillage into the wound.<br />
The wound was drained and treated and resolved, but<br />
this shows that proper positioning of the lap disc is<br />
essential to avoid this complication (3).<br />
There was one pulmonary complication requiring<br />
a 48 hour stay in the ICU, no cardiac complications,<br />
no <strong>de</strong>aths and no need for diverting stomas<br />
as a complication of surgery.<br />
In terms of oncologic outcome we looked at<br />
the number of lymph no<strong>de</strong>s in the specimen. It is<br />
recommen<strong>de</strong>d by SAGES and the Society of<br />
Colorectal Surgeons (SCRS) to perform at least<br />
twenty cases of benign disease or non curable colon<br />
cancer before performing surgery for colon cancer.<br />
We have tried to follow these gui<strong>de</strong>lines as much<br />
as possible as there is still many unanswered questions<br />
regarding oncologic outcome (5,6). Lymph<br />
no<strong>de</strong> count averaged 14.8 no<strong>de</strong>s; ranging from 7<br />
to 34. In general, most of the cases had more than<br />
12 no<strong>de</strong>s but we did observe that earlier cases<br />
ten<strong>de</strong>d to have less than 12. Again, we feel that<br />
this in an issue that has to do with experience and<br />
familiarity with the procedure and the instruments<br />
and <strong>de</strong>finitely recommend that hospitals and<br />
cre<strong>de</strong>ntialing committees follow these gui<strong>de</strong>lines, in<br />
or<strong>de</strong>r to have safe, high quality surgery.<br />
CONCLUSIONS<br />
We have found hand assisted laparoscopic colon<br />
surgery to be a viable, safe alternative to traditional<br />
open surgery in a community hospital setting<br />
with the procedure having an excellent patient<br />
acceptance. Time to start oral feedings and length<br />
of stay in the hospital is shortened. HALS procedures<br />
can be performed with an a<strong>de</strong>quate level of<br />
safety with a low level of complications. Conversions<br />
to open surgery are to be expected in the<br />
initial experience and left colon cases due to past<br />
episo<strong>de</strong>s of diverticulitis appear more difficult than<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
17<br />
right colon resections, but it is expected that as surgeons<br />
progress and expertise improves, conversions<br />
to open surgery and complications due to bleeding<br />
should <strong>de</strong>crease. Cancer resections can be performed<br />
using HALS techniques, but surgeons need<br />
to have experience with benign disease in or<strong>de</strong>r to<br />
have a<strong>de</strong>quate outcomes in colon cancer surgery.<br />
Due to the difficulties and the time nee<strong>de</strong>d to learning<br />
laparoscopic surgery, it is not clear to us whether HALS<br />
can be applied and utilized by the majority of surgeons.<br />
RESUMEN<br />
Introducción: La cirugía <strong>de</strong> colon<br />
laparoscópica asistida con la mano (CLAM) ha<br />
<strong>de</strong>mostrado tener la ventajas <strong>de</strong> la colectomía<br />
laparoscópica (CL) en términos <strong>de</strong> dolor, recuperación<br />
y estadía en el hospital. Estudios han<br />
<strong>de</strong>mostrado resultados similares en cirugía<br />
laparoscópica que en cirugía abierta para<br />
resecciones <strong>de</strong>l colon. La cirugía laparoscópica<br />
asistida con la mano tiene su curva <strong>de</strong> aprendizaje,<br />
el tiempo <strong>de</strong> cirugía es mayor, es más difícil<br />
que la cirugía abierta y requiere equipo especializado.<br />
En este informe presentamos nuestra<br />
experiencia inicial durante un periodo <strong>de</strong> 2.5<br />
años utilizando CLAM <strong>de</strong>l colon para<br />
diverticulosis, pólipos y carcinoma <strong>de</strong>l colon.<br />
Materiales y Métodos: Se revisaron los<br />
expedientes <strong>de</strong> clínica y hospital <strong>de</strong> todos los<br />
pacientes al que se les practicó CLAM <strong>de</strong>l colon<br />
durante los periodos <strong>de</strong> Junio <strong>de</strong>l 2005 a enero<br />
<strong>de</strong>l 2008 en el Hospital HIMA San Pablo-<br />
Caguas. Se obtuvo información <strong>de</strong>mográfica,<br />
resultados incluyendo tiempo <strong>de</strong> operación, tasas<br />
<strong>de</strong> conversión a cirugía abierta, razones para<br />
conversión, tiempo para comenzar alimentación,<br />
estadía en el hospital, al igual que información<br />
<strong>de</strong> estadio <strong>de</strong> cáncer y el número <strong>de</strong> nódulos<br />
linfáticos obtenidos en los especimenes. Se discuten<br />
las complicaciones con comentarios pertinentes<br />
a la experiencia <strong>de</strong> dos cirujanos con las<br />
técnicas <strong>de</strong> CL y CLAM.<br />
Resultados: Se comenzaron 65 resecciones<br />
<strong>de</strong>l colon utilizando CLAM. Hubo 33 hombres y<br />
32 mujeres entre las eda<strong>de</strong>s <strong>de</strong> 26 y 87 años.<br />
Hubo 31 casos <strong>de</strong> diverticulosis; 8 por condiciones<br />
pre-malignas(pólipos gran<strong>de</strong>s o pólipos
18<br />
con displasia <strong>de</strong> alto grado) y 26 para carcinoma<br />
<strong>de</strong>l colon. El tiempo promedio <strong>de</strong> cirugía fue <strong>de</strong><br />
195 minutos(120 a 300 min.); estadía promedio<br />
fue <strong>de</strong> 6 días (4 a 14 días). La tasa <strong>de</strong> conversión<br />
para todos los casos fue <strong>de</strong> 13.8 %. 21<br />
% durante el primer año y 10.8 % durante el<br />
segundo año. 5 pacientes (7.5 %) tuvieron complicaciones<br />
requiriendo una estadía prolongada.<br />
Los pacientes sin complicaciones tuvieron una<br />
estadía promedio <strong>de</strong> 4.5 días. El número promedio<br />
<strong>de</strong> nódulos linfáticos fue 14.8 (7 a 24; el<br />
tamaño promedio <strong>de</strong> especimenes en<br />
diverticulosis fue <strong>de</strong> 17cm. Complicaciones fueron<br />
sangrado en tres pacientes que requirieron<br />
re-intervención, íleo prolongado y obstrucción<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
intestinal en dos pacientes. Una paciente tuvo<br />
una colección pélvica que requirió drenaje, y uno<br />
tuvo una infección <strong>de</strong> herida requiriendo admisión,<br />
drenaje y antibióticos. Ningún paciente requirió<br />
una ostomía por una complicación y no<br />
hubo muertes perioperatorias.<br />
Conclusión: La cirugía <strong>de</strong> colon<br />
laparoscópica asistida con la mano es una alternativa<br />
segura y viable a cirugía abierta en un<br />
hospital con el equipo y la experiencia apropiada.<br />
Los pacientes se benefician <strong>de</strong> tiempo <strong>de</strong><br />
recuperación más rápido y con corta estadía en<br />
el hospital. Los resultados oncológicos son similares<br />
a cirugía abierta. El tiempo <strong>de</strong> cirugía es<br />
mayor y son operaciones difíciles <strong>de</strong> apren<strong>de</strong>r.<br />
REFERENCES<br />
1. Ballanthyne, GH, et al, Hand Assisted Colectomy: Evolution to a Clinically useful Technique. Dis Colon<br />
Rectum 2004: 47: 753-765<br />
2. Loungnarath, R, Fleshman, J. Hand Assisted Laparoscopic Colectomy Techniques. Seminars in Laparoscopic<br />
Surgery, Volume 8, 2001. pp 220-229.<br />
3. Darzi, A. Hand Assisted Laparoscopic Colorectal Surgery . Seminars in Laparoscopic Surgery, Volume 8,<br />
Number 2(june)2001:pp 153-150<br />
4. Targarona, EM et al. Prospective Trial comparIng conventional Laparoscopic Colectomy with Hand Assisted<br />
Colectomy Surg Endos (2002) 16:234-239<br />
5. A Comparison of Open and Laparoscopically Assisted and Open Colectomy for Colon Cancer. N Eng J Med<br />
2004; 350:2050-92069<br />
6. Position Statement of the Society of Colon and Rectal Surgeons (ASCRS) on Laparoscopic Colectomy for<br />
Curable Colon Cancer. Endorsed by the Society of American Gastrointestinal Endoscopic Surgeons(SAGES)<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
20<br />
Artículos Originales • Original Articles<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
COMPARISON BETWEEN OPEN AND LAPAROSCOPIC<br />
APPENDECTOMY IN NON-COMPLICATED APPENDICITIS<br />
By: Aura F. Delgado Cifuentes, BS* and Ramón K. Sotomayor, MD.**<br />
ABSTRACT<br />
Background/Objective: An extensive web<br />
search failed to provi<strong>de</strong> studies from <strong>Puerto</strong> <strong>Rico</strong><br />
regarding whether open (OA) or laparoscopic<br />
appen<strong>de</strong>ctomy (LA) should be performed for noncomplicated<br />
appendicitis. Our goal is to compare<br />
these techniques in terms of time at operating<br />
room (OR), length of surgery, hospital stay, pain<br />
medication requirements, in-hospital<br />
complications and readmissions.<br />
Methods: 126 patients (64 OA; 62 LA) with<br />
non-complicated appendicitis were studied<br />
retrospectively. Data obtained: <strong>de</strong>mographics,<br />
CT-Scan use, surgery and operating room time,<br />
days in hospital, complications, diet<br />
commencement, pain medications doses,<br />
pathology and readmission.<br />
Results: Difference was found in total time<br />
at OR (80.1± 29 minutes OA; 105.7± 22.6 LA)<br />
and in surgery length (41± 28 OA; 48± 16 LA),<br />
but not in hospital stay (2.1 days OA; 2.2 LA)<br />
nor in in-hospital complication rate. Negative<br />
appen<strong>de</strong>ctomy rate was 24% LA vs. 3% OA.<br />
Readmission rate was higher in OA with 5%<br />
wound infection rate.<br />
Conclusion: Techniques are similar in mean<br />
hospital stay, in-hospital complications, and pain<br />
medication requirements. LA had a higher<br />
negative appen<strong>de</strong>ctomy rate but of these patients<br />
five had surgical diagnosis of acute appendicitis<br />
and after appen<strong>de</strong>ctomy, signs and symptoms<br />
resolved; and two patients had interval<br />
appen<strong>de</strong>ctomies. As these patients were cured,<br />
the real negative appen<strong>de</strong>ctomy rate is 13%, similar<br />
to the historically accepted 16%. The other<br />
eight patients had an a<strong>de</strong>quate diagnosis. We are<br />
concerned OA negative appen<strong>de</strong>ctomy rate is<br />
only 3%; we won<strong>de</strong>r if surgeons are waiting too<br />
long to operate patients. Readmission was higher<br />
in OA (wound infection rate of 5%). Although it<br />
takes more time in the OR, LA is as safe as OA,<br />
has a low rate of complications and lower<br />
readmission rate.<br />
Key words: appen<strong>de</strong>ctomy, acute<br />
appendicitis, laparoscopy<br />
Appen<strong>de</strong>ctomy is the most common abdominal<br />
surgery performed on an emergency basis 2 .<br />
Since its introduction in the 1980’s, there has<br />
been the controversy of whether the practice of<br />
laparoscopic appen<strong>de</strong>ctomy (LA) compares or is<br />
better than open appen<strong>de</strong>ctomy (OA). Contrary<br />
to laparoscopic cholecystectomy which is<br />
accepted as the standard of care to remove the<br />
* From Universidad Central <strong>de</strong>l Caribe, Bayamón, <strong>Puerto</strong> <strong>Rico</strong>, and ** Department of Surgery, HIMA-San Pablo Group, Caguas, PR. Address<br />
reprints: Ramón K. Sotomayor, MD - 300 Avenida La Sierra, Apartado 61, San Juan, PR 00926. E-mail: . Presented at<br />
the 58 th ACS Meeting <strong>Puerto</strong> <strong>Rico</strong> Chapter: <strong>Feb</strong>ruary 21-23, 2008.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
gallblad<strong>de</strong>r, LA is not wi<strong>de</strong>ly accepted by most<br />
surgeons who remain skeptical of replacing the<br />
relatively straightforward OA 3 . This is because<br />
no <strong>de</strong>finitive data shows the superiority of<br />
laparoscopy for treating appendicitis and the<br />
existence of contradictory evi<strong>de</strong>nce regarding this<br />
issue.<br />
Several studies report advantages of<br />
laparoscopic over open appen<strong>de</strong>ctomy; others<br />
claim there is no difference between the two, and<br />
other state OA is better. In the past, randomized<br />
trials were performed in or<strong>de</strong>r to <strong>de</strong>termine if<br />
there was an advantage to LA when compared<br />
to OA. Frazee, et al. (1994) conclu<strong>de</strong>d that<br />
patients who un<strong>de</strong>rwent LA had a shorter<br />
duration of analgesic use and returned to full<br />
activities sooner, reason they stated the<br />
procedure of choice should be LA 4 .<br />
On the other hand, in another randomized<br />
study in 1995, Martin and his colleagues 5 found<br />
LA was comparable to OA in terms of<br />
complications, hospital stay, cost, return to normal<br />
activities and work, but there was a greater<br />
operative time. They conclu<strong>de</strong>d LA does not<br />
confer any significant benefit over the OA for<br />
routine appen<strong>de</strong>ctomies. A prospective<br />
randomized double blind study 6 on 2005<br />
conclu<strong>de</strong>d LA does not confer significant<br />
advantage over OA outcomes, except for quality<br />
of life scores, reason they recommend the choice<br />
of the procedure should be based on surgeon’s<br />
or patient’s preference.<br />
One of the largest studies available, a meta<br />
analysis performed in 2004 using a database of<br />
43,757 patients who un<strong>de</strong>rwent appen<strong>de</strong>ctomy<br />
for acute appendicitis, showed LA was associated<br />
with shorter median length of hospital stay, lower<br />
rate of infection, fewer gastrointestinal and<br />
overall complications, and a higher rate of routine<br />
discharge. 7 They conclu<strong>de</strong>d that laparoscopic<br />
appen<strong>de</strong>ctomy had several advantages over open<br />
appen<strong>de</strong>ctomy and should be performed.<br />
Several studies have been performed but no<br />
general consensus has been reached. An<br />
extensive web search failed to provi<strong>de</strong> published<br />
studies that used data regarding the comparison<br />
of these two approaches from hospitals in Puer-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
21<br />
to <strong>Rico</strong>. The goal of this study is to <strong>de</strong>termine if<br />
any of the two approaches, OA or LA, is more<br />
beneficial for patients or if they are similar in<br />
terms of total time in the operating room (OR),<br />
length of surgery and of hospital stay, starting<br />
diet, requirement of pain medications, in-hospital<br />
complications and readmission rate.<br />
MATERIAL & METHODS<br />
A retrospective chart review of 126 patients<br />
was performed of patients who un<strong>de</strong>rwent noncomplicated<br />
appen<strong>de</strong>ctomies during <strong>Feb</strong>ruary<br />
2005 to June 2007 at HIMA San Pablo Group,<br />
an acute care tertiary hospital in Caguas, PR.<br />
Data was gathered from 64 cases of OA and 62<br />
cases of LA. Exclusion criteria inclu<strong>de</strong>d patients<br />
with perforation at the time of the procedure<br />
confirmed by pathologic findings. Data obtained<br />
inclu<strong>de</strong>d age of patient, sex, height, weight,<br />
previous abdominal surgeries, CT-Scan used and<br />
interpretation, time of surgery, number of days<br />
in hospital, starting diet, use of pain medications,<br />
in-hospital complications, final pathologic<br />
findings and readmission to hospital.<br />
OA was usually performed through a musclesplitting<br />
incision in the right lower quadrant. LA<br />
general steps inclu<strong>de</strong>d: preparing the patient with<br />
general endo-tracheal anesthesia, placement of<br />
foley catheter and nasogastric tube, then<br />
placement of three ports (usually one 10mm port<br />
and two 5mm ports). After full dissection of<br />
appendix its base was ligated using PDS Endoloops<br />
or stapler. It was divi<strong>de</strong>d, resected and then<br />
retrieved using an Endo-bag.<br />
Length of hospital stay was <strong>de</strong>fined as the<br />
difference in days since surgery day to discharge<br />
home day. Total time at OR was <strong>de</strong>fined as the<br />
total time since patient entered the OR until<br />
patient left the room. Total time of surgery was<br />
<strong>de</strong>fined as the total time from the first incision<br />
to full closing of wound. The amount of pain<br />
medications was <strong>de</strong>scribed as the doses of pain<br />
medications received after discharged from<br />
recovery room until the discharge from hospital.<br />
We used SPSS version 10.0 to perform our<br />
statistical analysis that inclu<strong>de</strong>d Chi-square and<br />
t-tests. A p < 0.05 was statistically significant.
22<br />
RESULTS<br />
A total of 126 patients, 64 OA and 62 LA,<br />
were studied. Demographics were similar for both<br />
groups (Table 1). Mean age for OA was 28±15 years<br />
(range 2-68) and 30± 15 years (range 6-67) for LA.<br />
Male to female ratio was similar for both groups<br />
and within groups (1:0.68OA; 1:1.1LA). Mean<br />
basal metabolic in<strong>de</strong>x (BMI) was also similar as OA<br />
patients had an average BMI of 26± 7 and LA had<br />
28± 6. There was no difference in previous abdominal<br />
surgeries inci<strong>de</strong>nce as 22% of the patients in<br />
the OA group had previous abdominal surgeries vs.<br />
18% of LA patients. No difference was found<br />
(p=0.14) in the frequency of CT scan use (70%OA<br />
vs. 57%LA).<br />
Difference was found in total time at OR<br />
(p=0.008). OA had an average length of surgery of<br />
80.1± 29 min. vs.105.7± 22.6 min. in LA. This is<br />
an average 25 minute difference between the procedures.<br />
Also we found a significant difference<br />
(p=0.001) of 7 minutes in length of surgery as the<br />
OA group had an average of 41± 28 vs. 48± 16 in<br />
the LA group (Graph 1).<br />
There was no difference (p=0.5) in mean hospital<br />
stay (days). OA had an average of 2.14± 1.4<br />
days of hospital stay vs. 2.19± 1 days in LA. Most<br />
patients in both groups were discharged home<br />
in the first 2 days after surgery. There was also<br />
no difference in pain medication requirements<br />
(p=0.3) and most patients required 1 or 2 doses<br />
of pain medications after leaving recovery room.<br />
Most patients in OA group started on clear liquids<br />
diet (63%) while most patients in LA started<br />
on full liquids diet (58%), but this seem to be related<br />
to surgeon’s preference.<br />
Total in-hospital complication rate was similar<br />
(p=0.5) for both groups being fever the most com-<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
mon (17/21 OA and 18/21 LA). Other complications<br />
in the OA group inclu<strong>de</strong>d one patient with<br />
coffee ground vomiting and severe hiccups, one with<br />
diarrhea, and one with persistent pain after eating.<br />
On the other hand, in the LA group there was<br />
one patient with blood loss anemia who was discharged<br />
with no events, one with urinary retention<br />
and one with diarrhea.<br />
There were 15 cases (24%) of negative pathologies<br />
in the LA group vs. 2 cases (3%) in the OA<br />
group (Table 2). Historically this rate should be<br />
around 16% 1 . Consi<strong>de</strong>ring that there four patients<br />
had surgical diagnosis of acute appendicitis, two<br />
with interval appen<strong>de</strong>ctomies, and one with appendiceal<br />
adhesions with fecalith, the real negative<br />
appen<strong>de</strong>ctomy rate for the LA group is 13% (N=8)<br />
that is similar to the expected rate.<br />
Readmission rate was higher in OA with 71.4%<br />
of all readmissions (5/7) with 2 cases of intestinal<br />
obstruction and 3 cases of wound infection (5% of<br />
patients) (Graph 2). One of the patients with intestinal<br />
obstruction in the OA group was treated conservatively<br />
with naso-gastric suction and IV fluids<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
but the other one required exploratory laparotomy<br />
with enterolysis and enterorraphy. One of the readmissions<br />
for the LA group inclu<strong>de</strong>d one patient<br />
with abdominal swelling who was treated conservatively<br />
and was discharged with no events and one<br />
patient who presented one week after surgery with<br />
intestinal obstruction and required re-exploration<br />
with enterectomy and was discharged with no long<br />
term adverse events.<br />
DISCUSSION<br />
There was difference in total time in the OR<br />
and time of Surgery as we found an average OR<br />
time of 80.1 min. OA vs. 105.7 min. in the LA<br />
group. This is an average of 25 additional minutes<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
23<br />
for the LA group that can be expected as there is<br />
more instrumentation and preparation for<br />
laparoscopic procedures. On the other hand, we<br />
question the clinical relevance of the difference in<br />
surgery time as we found an average of 48 minutes<br />
OA vs. 41 minutes LA, and there’s an average difference<br />
of only 7 minutes between the procedures.<br />
Open and laparoscopic appen<strong>de</strong>ctomies are<br />
similar in terms of mean hospital stay, in-hospital<br />
complications, and pain medication requirements.<br />
Contrary to other series that have reported up to<br />
one day less of hospital stay 1, 7, 8, 9 , we did not found<br />
such a difference between both techniques. We had<br />
one LA patient with blood loss anemia as a complication.<br />
This was a patient with a difficult retrocecal<br />
appendix with final pathology of acute gangrenous<br />
appendicitis. He was found to have hemoglobin<br />
of 8g/dl the second post operative day. Patient<br />
was discharged home with a hospital stay of<br />
six days without need of blood transfusions or any<br />
negative outcomes.<br />
Negative appen<strong>de</strong>ctomy rate was higher in the<br />
LA group and it was higher than the rate published<br />
in other series as we had 24%. But we have to consi<strong>de</strong>r<br />
that we had five patients with surgical diagnosis<br />
of acute appendicitis who after appen<strong>de</strong>ctomy<br />
the leukocytosis, abdominal pain, and other symptoms<br />
resolved completely suggesting diagnosis could<br />
have been early acute appendicitis or mesenteric<br />
a<strong>de</strong>nitis. Other two patients had interval appen<strong>de</strong>ctomies<br />
and were discharged with no events. Taking
24<br />
into account that these 7 patients had excellent recovery<br />
after the appen<strong>de</strong>ctomy, the real negative<br />
appen<strong>de</strong>ctomy rate is 13% (N=8) that is similar to<br />
the historically accepted rate of 16% 1 . The other<br />
eight patients with pre-op diagnosis of acute appendicitis<br />
left OR with an a<strong>de</strong>quate diagnosis as<br />
laparoscopy allow an a<strong>de</strong>quate exploration of the<br />
abdominal cavity. The negative appen<strong>de</strong>ctomy rate<br />
for the OA group was 3%. Published series quote<br />
ranges between 0% to 35.5% with an average of<br />
16% of negative appen<strong>de</strong>c-tomies 1 . Flum (2001,<br />
2002) 10, 11 states that classically, this rate of negative<br />
appen<strong>de</strong>ctomies has been accepted by the clinical<br />
community because the frequency of appendiceal<br />
perforation is consi<strong>de</strong>red by many to be inversely<br />
linked to the rate of negative appen<strong>de</strong>ctomies and<br />
it has been suggested that a higher than zero (10%-<br />
15%) rate of unnecessary appen<strong>de</strong>ctomy must be<br />
tolerated to assure a low threshold for operation,<br />
such that diagnostic <strong>de</strong>lays that might result in perforation<br />
are avoi<strong>de</strong>d. Frazee (1994) 4 states that as<br />
the diagnostic accuracy increases so does the risk<br />
of perforation. Another issue could be that surgeons<br />
want to make sure diagnosis is accurate before submitting<br />
the patient to an open procedure which is<br />
usually ma<strong>de</strong> through a small Rocky-Davis incision<br />
that makes difficult to explore other organs. Sometimes<br />
when a surgeon encounters a negative appendix,<br />
extension of the incision is necessary.<br />
Other series have reported up to a 7% of intraabdominal<br />
abscess rate after LA 1, 7 . In contrast to<br />
this, no intra-abdominal abscesses were reported<br />
in this series. We attribute this to the management<br />
of appendiceal stump. Appendiceal stump was almost<br />
routinely managed with polydioxanone endoloops,<br />
two at the base and one distally. In several<br />
cases of thickened base of appendix it was divi<strong>de</strong>d<br />
flush with the cecum using the endoscopic stapler.<br />
Leakage after this was negative in our patients and<br />
is reflected in the negative intra-abdominal abscess<br />
rate. In addition to that, no patients were admitted<br />
with stump appendicitis. Also, we did not found<br />
patients who had to convert to open procedure.<br />
The readmission rate was lower in the LA<br />
group. The wound infection rate for the OA was<br />
higher than that of the LA group as 5% of OA patients<br />
had a wound infection (3/64) that required<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
readmission vs. 0% in LA group. This is because<br />
no contamination of incision is ma<strong>de</strong> while retrieving<br />
the specimen from the abdomen in the LA procedure<br />
vs. the contamination that occurs with OA.<br />
These three patients were drained at the emergency<br />
room or bedsi<strong>de</strong> and treated with intravenous antibiotics.<br />
One complication after LA inclu<strong>de</strong>s the case<br />
of a patient with multiple previous abdominal surgeries<br />
who <strong>de</strong>velop bowel obstruction one week<br />
after surgery for which readmission with re-exploration<br />
and enterectomy was necessary. Patient was<br />
discharged with no adverse long term outcomes.<br />
Two patients had bowel obstruction after OA and<br />
were readmitted. One was treated with nasogastric<br />
tube suction and IV fluids while the other one required<br />
exploratory laparotomy with enterolysis and<br />
enterorraphy. Both were discharged with no long<br />
term negative outcomes.<br />
Study limitations inclu<strong>de</strong> the fact that most of<br />
the appen<strong>de</strong>ctomies were performed using the open<br />
approach making it necessary to gather records<br />
dated from 2005. Another limitation is the sample<br />
size, as a small sample will yield a greater statistical<br />
error. Also a retrospective study <strong>de</strong>pends on the<br />
accuracy of medical record information and how<br />
well documented it is. In addition to that, most<br />
wound infections are seen in the private office and<br />
are not documented in the same medical record.<br />
Another limitation is the fact that we could not evaluate<br />
other aspects after surgery such as quality of<br />
life in terms of time required to return to normal<br />
daily activities or to work.<br />
Although it takes more time in the operating<br />
room, LA is equally as safe as OA; it also has a low<br />
rate of complications and has a significantly lower<br />
readmission rate. LA is still un<strong>de</strong>rrepresented (e.g.<br />
11% of all appen<strong>de</strong>ctomies in 2005) and more cases<br />
are required in or<strong>de</strong>r to compare both techniques<br />
with more precision. There are other parameters<br />
not measured in this study such as time required by<br />
patients to return to normal activities and work or<br />
complications treated as outpatients that could help<br />
differentiate the outcomes of these procedures.<br />
Further studies including these data and a greater<br />
sample are nee<strong>de</strong>d in or<strong>de</strong>r to <strong>de</strong>termine which<br />
procedure favors patients the most.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Acknowledgements:<br />
The authors thank Professor Iris Parrilla for<br />
contribution in statistical analysis and HIMA hospital<br />
record room personal for their help.<br />
Resumen<br />
Introducción/Objetivo: Una bús-queda<br />
extensa en Internet <strong>de</strong>mostró que no existen<br />
estudios <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong> comparando apen<strong>de</strong>ctomía<br />
abierta (AA) y apen<strong>de</strong>ctomía laparoscópica para el<br />
tratamiento <strong>de</strong> apendicitis aguda. Nuestra meta es<br />
comparar estas dos técnicas en términos <strong>de</strong> tiempo<br />
en la sala <strong>de</strong> operaciones, tiempo <strong>de</strong> cirugía, estadía<br />
en el hospital, requerimientos <strong>de</strong> analgésicos,<br />
compli-caciones y re- admisiones al hospital.<br />
Métodos: Se revisaron expedientes <strong>de</strong> 126<br />
pacientes con diagnóstico <strong>de</strong> apendicitis aguda. Se<br />
recopiló información <strong>de</strong>mográfica, uso <strong>de</strong><br />
tomografía com-putarizada (CT), tiempo <strong>de</strong> cirugía,<br />
tiempo total en la sala <strong>de</strong> operaciones, tiempo para<br />
empezar dieta, uso <strong>de</strong> analgésicos, patología y tasas<br />
<strong>de</strong> re admisión.<br />
Resultados: Se encontró una diferencia en el<br />
tiempo total en sala <strong>de</strong> operaciones (80.1 ± 29<br />
minutos AA; 105.7 ± 22.6 AL) y en el tiempo <strong>de</strong><br />
cirugía (41 ± 28 minutos AA; 48 ± 16 min. AL),<br />
pero no en el tiempo <strong>de</strong> estadía en el hospital (2.1<br />
días AA; 2.2 AL), ni hubo diferencia en la tasa <strong>de</strong><br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
25<br />
complicaciones durante la estadía en el hospital.<br />
La tasa <strong>de</strong> apen<strong>de</strong>ctomía negativa fue <strong>de</strong> 24 % en<br />
apen<strong>de</strong>ctomía laparoscópica vs. 3% en<br />
apen<strong>de</strong>ctomía abierta. Las readmisiones fueron<br />
mayores en apen<strong>de</strong>ctomía abierta que en casos<br />
laparoscópicos al igual que la tasa <strong>de</strong> infecciones<br />
<strong>de</strong> herida.<br />
Conclusiones: Las técnicas son similares en<br />
términos <strong>de</strong> estadía en el hospital, complicaciones<br />
y requerimientos <strong>de</strong> analgésicos. AL tuvo una tasa<br />
más alta <strong>de</strong> apen<strong>de</strong>ctomías negativas pero cinco <strong>de</strong><br />
estos pacientes tuvieron un diagnóstico quirúrgico<br />
<strong>de</strong> apendicitis y sus síntomas y signos resolvieron<br />
luego <strong>de</strong> apen<strong>de</strong>ctomías. Excluyendo estos cinco<br />
casos, la tasa real <strong>de</strong> apéndices negativas es <strong>de</strong> 13<br />
%, similar la tasa histórica <strong>de</strong> alre<strong>de</strong>dor <strong>de</strong> 16 %.<br />
En los <strong>de</strong>más pacientes <strong>de</strong> apen<strong>de</strong>ctomías<br />
laparoscópicas que resultaron negativas (8) se<br />
obtuvo un diagnóstico certero y a<strong>de</strong>cuado durante<br />
la cirugía. Es preocupante la tasa <strong>de</strong> apen<strong>de</strong>ctomías<br />
negativas en apen<strong>de</strong>ctomías abiertas <strong>de</strong> solo 3 %;<br />
lo cual trae la pregunta <strong>de</strong> si se está esperando<br />
<strong>de</strong>masiado tiempo para operar. Las readmisiones e<br />
infecciones <strong>de</strong> herida fueron más altas en<br />
apen<strong>de</strong>ctomías abiertas. Aunque el tiempo <strong>de</strong><br />
cirugía es más largo en cirugía laparoscópica, AL<br />
es una operación segura con baja probabilidad <strong>de</strong><br />
complicaciones y re admisión al hospital.<br />
REFERENCES<br />
1. Hung, S. Appen<strong>de</strong>ctomy. In Souba, W., Fink, M. ACS Surgery. 2005 Ed., New York, WebMD, 2005:656-664.<br />
2. Paulson, Erik, Kalady, M., Pappas, T.: “Suspected Appendicitis”. New England Journal of Medicine. 2003; 348; 3:236-243.<br />
3. Aziz, O., Athanasiou, T., Tekkis, P., et al.: “Laparoscopic versus Open Appen<strong>de</strong>ctomy in Children, a meta-analysis”. Annals of Surgery.<br />
2006; 243:17-27.<br />
4. Frazee, R., Roberts, J., Symmonds, R., et al.: “A Prospective Randomized Trial Comparing Open versus Laparoscopic Appen<strong>de</strong>ctomy”.<br />
Annals of Surgery. 1994; 219:725-731.<br />
5. Martin, L., Puente, I., Sosa, J., et al.: “Open versus Laparoscopic Appen<strong>de</strong>ctomy”. Annals of Surgery. 1995; 222:256-262.<br />
6. Katkhouda, N., Mason, R., Towfigh, S., et al.: “Laparoscopic versus Open Appen<strong>de</strong>ctomy, a prospective randomized double-blind<br />
study”. Annals of Surgery. 2005; 242:439-450.<br />
7. Guller, U., Hervey, S., Purves, H., et al.: “Laparoscopic Versus Open Appen<strong>de</strong>ctomy, Outcomes Comparison Based on a Large<br />
Administrative database”. Annals of Surgery. 2004; 239:43-52.<br />
8. Long, K., Bannon, M., Zietlow, S., et al.: “A prospective randomized comparison of laparoscopic appen<strong>de</strong>ctomy with open appen<strong>de</strong>ctomy”.<br />
Surgery. 2001; 129:390-400.<br />
9. Nguyen, NT, Zainabadi, K., Mavandadi, S., et al.: “Trends in utilization and outcomes of laparoscopic versus open appen<strong>de</strong>ctomy”.<br />
American Journal of Surgery. 2004; 188(6):813-820.<br />
10. Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwi<strong>de</strong> analysis. Arch Surg.2002; 137 :799<br />
–804.<br />
11. Flum DR, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of appendicitis <strong>de</strong>creased over time? A population-based analysis.<br />
JAMA.2001; 286 :1748 –1753.
26<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
ANUNCIO PÚBLICO • AMPR<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
27<br />
Artículos Originales • Original Articles<br />
MINIMALLY INVASIVE PARATHYROIDECTOMY AS<br />
TREATMENT FOR PRIMARY HYPERPARATHYROIDISM<br />
ABSTRACT<br />
Background: Current techniques for<br />
management of primary hyperpara-thyroidism<br />
(pHPT) rely on preoperative localization studies in<br />
or<strong>de</strong>r to perform a direct exploration of the neck.<br />
This case series reports the results of minimally<br />
invasive parathyroi<strong>de</strong>ctomy (MIP) performed in<br />
twenty-two consecutive pHPT patients with<br />
suspected parathyroid a<strong>de</strong>noma.<br />
Methods: All patients with symptomatic pHPT<br />
and or aberrant biochemical markers un<strong>de</strong>rwent preoperative<br />
evaluation including calcium and<br />
parathyroid hormone (PTH) serum levels, and a Tc-<br />
99 Sestamibi (MIBI) scintigraphy scan. The day of<br />
surgery Tc-99 MIBI was administered intravenously<br />
to localize diseased parathyroid glands. Within the<br />
next two hours after administration of IV contrast a<br />
gamma radiation <strong>de</strong>tection <strong>de</strong>vice was applied over<br />
the neck to <strong>de</strong>tect areas of prominent radiation<br />
gradient that served as landmarks during surgery.<br />
All removed tissue was again tested with the gamma<br />
radiation probe and sent for frozen sections to<br />
confirm parathyroid gland tissue. Serum calcium<br />
levels were measured immediately after surgery, 24<br />
hours, and 3 days later at an outpatient visit.<br />
Results: Twenty-two patients with symptomatic<br />
hypercalcemia (6 M, 16 F), mean age of 63 years<br />
(Range 35 to 87), completed pre-operative<br />
Sestamibi scintigraphy and follow up evaluations.<br />
Mean pre-operative calcium and PTH levels were<br />
By: Laureano A. Giral<strong>de</strong>z-Rodriguez, MD.* and Laureano J. Giral<strong>de</strong>z-Casasnovas, MD.**<br />
11.3 mg/dL and 194.2 pg/mL, respectively. Preoperative<br />
Sestamibi scintigraphy were negative in<br />
four (18%) and positive in 18 (82%) patients.<br />
Parathyroid a<strong>de</strong>noma was confirmed by frozen sections<br />
in all patients. The mean operative time was<br />
approximately 32 minutes except in 3 cases which<br />
required combined surgical procedures. There were<br />
no intra-operative complications while minor wound<br />
swelling was the only postoperative complication<br />
reported. All patients exhibited <strong>de</strong>creased serum<br />
calcium levels with resolution of symptoms within a<br />
week, and resumed a normal lifestyle.<br />
Conclusions: MIP using preoperative Tc-99<br />
MIBI scan is an excellent and safe treatment for<br />
patients in pHPT patients with a suspected<br />
parathyroid a<strong>de</strong>noma. In our experience this<br />
technique avoids the potential complications of<br />
extensive neck exploration, reduces operative time,<br />
and has a high patient acceptance.<br />
Key words: minimally, invasive, parathyroi<strong>de</strong>ctomy,<br />
primary hyperpara-thyroidism<br />
The standard treatment for patients with hypercalcemia<br />
due to primary hyperpara-thyroidism<br />
(pHPT) is surgical removal through bilateral exploration<br />
of the neck. Current techniques for surgical<br />
manage-ment of primary pHPT rely on preoperative<br />
localization studies in or<strong>de</strong>r to perform a direct<br />
*PGY-1 Resi<strong>de</strong>nt, Department of Otolaryngology & Head and Neck Surgery, University of <strong>Puerto</strong> <strong>Rico</strong> School of Medicine; Rio Piedras, <strong>Puerto</strong><br />
<strong>Rico</strong>, and ** Head and Neck Surgeon, Hospital Auxilio Mutuo, San Juan, <strong>Puerto</strong> <strong>Rico</strong>. Address Reprints to: Laureano A. Giral<strong>de</strong>z Rodriguez, MD,<br />
B5 Calle Tabonuco, Ste 216 PMB 299 Guaynabo, PR 00968. Email:laureano_giral<strong>de</strong>z@hotmail.com. Poster presented at the 58th Annual Meeting<br />
of the American College of Surgeons, <strong>Puerto</strong> <strong>Rico</strong> Chapter, <strong>Feb</strong>ruary 22, 2008, La Concha Hotel, San Juan, <strong>Puerto</strong> <strong>Rico</strong>.
28<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 1: Transverse Neck Incision showing the<br />
parathyroid a<strong>de</strong>noma Figure 2: Gamma Radiation <strong>de</strong>tection <strong>de</strong>vice.<br />
exploration of the neck. This case series reports<br />
the results of minimally invasive parathyroi<strong>de</strong>ctomy<br />
(MIP) performed in twenty-two consecutive pHPT<br />
patients with suspected parathyroid a<strong>de</strong>noma using a<br />
gamma radiation <strong>de</strong>tection <strong>de</strong>vice (see Fig. 1).<br />
MATERIAL AND METHODS<br />
Twenty-two patients were operated between 2005<br />
and 2007 using the minimally invasive technique. The<br />
pre-operative work up inclu<strong>de</strong>d calcium and<br />
parathyroid hormone (PTH) levels, as well as Sestamibi<br />
scintigraphy scan on all patients. The day of surgery<br />
the patient was first sent to the nuclear medicine<br />
<strong>de</strong>partment were a dose of preoperative Technetium-<br />
99m Sestamibi 30 millicurie injection was administered<br />
intravenously. The patient was then operated within<br />
two hours of the injection.<br />
All patients were given general anesthesia<br />
except for one patient who was given intravenous<br />
sedation and the area of the a<strong>de</strong>noma was explored<br />
using local anesthesia.<br />
A pg/mL (gamma probe) was applied directly<br />
to the neck before surgery to <strong>de</strong>tect the exact area<br />
where the radiation gradient was more prominent.<br />
This i<strong>de</strong>ntified the approximate location of the<br />
a<strong>de</strong>noma. A 2 to 2.5 cm incision was ma<strong>de</strong> at the<br />
midline in the anterior lower neck (Image 2). The<br />
sub-platysmal plane was <strong>de</strong>veloped and a midline<br />
dissection approach was used to reach the thyroid<br />
isthmus. The thyroid isthmus and the gland were<br />
i<strong>de</strong>ntified. The gamma probe was inserted through<br />
the neck incision and the area of highest radiation<br />
gradient was sought again. The exploration for the<br />
parathyroid a<strong>de</strong>noma was done until i<strong>de</strong>ntification<br />
was obtained with visual confirmation. In the<br />
process, the recurrent laryngeal nerve was i<strong>de</strong>ntified.<br />
The vascular pedicle of the a<strong>de</strong>noma was controlled<br />
with Surgi-Clips and the diseased gland removed.<br />
The gamma probe was applied to the removed glandular<br />
tissue on the operating room instrument table<br />
to confirm the high radiation gradient. A frozen<br />
section was performed on all removed glands and<br />
it was confirmed to be parathyroid tissue. The<br />
surgical wound was closed in layers in the usual<br />
manner. Post-operative calcium levels were taken<br />
at the recovery room and twice thereafter in a<br />
twenty four-hour period. Calcium levels were<br />
repeated at the first post-operative outpatient visit<br />
three days later in all patients. Our reported value<br />
of post-operative calcium corresponds to the first<br />
serum calcium sample taken after surgery.<br />
RESULTS<br />
Twenty-two patients were chosen for the case<br />
series based on the minimally invasive surgical technique<br />
chosen. Six were male (27%) and 16 were<br />
female (83%). The mean age for the patients was<br />
62.3 years and the range was 35 to 87 years. Mean<br />
age for males was 61.5 years old and for females<br />
was 62.6 years old. Mean laboratory values were<br />
the following: pre-operative serum calcium levels<br />
were 11.3 mg/dL (Normal value 8.5 mg/dL – 10.3<br />
mg/dL); pre-operative serum PTH 194.2 (Normal<br />
value: 10-60 pg/ml); post-operative serum calcium<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
levels 8.68 mg/dL (Normal value: 8.5 mg/dL – 10.3<br />
mg/dL). (Table 1)<br />
The most common presenting symptom for all<br />
patients was hypertension, followed by musculoskeletal<br />
pain, nephrolithiasis and osteoporosis.<br />
The twenty-two patients were submitted to the<br />
same procedure. Pre-operative Sestamibi Tc-99<br />
scintigraphy was done in 100% of the patients. The<br />
scan was negative in 4 patients (18%) and positive<br />
in 18 patients (82%).<br />
In the present series all patients were operated<br />
un<strong>de</strong>r general anesthesia, except one who was operated<br />
un<strong>de</strong>r IV sedation and local anesthesia. The<br />
average operating time was 32 minutes, with operative<br />
length ranging from 16 to 60 minutes. Intra-operative<br />
usage of the Sestamibi Technetium-<br />
99 gamma probe was used in all patients for localization<br />
of the parathyroid a<strong>de</strong>noma with success. A<br />
more than double increase from the baseline of the<br />
gradient shown in the probe monitor was used as<br />
the standard to imply the presence of the a<strong>de</strong>noma<br />
at that site. Frozen section pathology revealed the<br />
presence of parathyroid tissue in all 22 patients.<br />
Table 1: General Patient Data<br />
Serum Post-Op Surgery<br />
Sestamibi PTH Pre-Op Ca (24hr) Time<br />
Sex Age Scan (pg/mL) Ca (mg/dl) (mg/dL) (min)<br />
M 42 Positive 629 13.2 8.4 45<br />
M 58 Negative 347 12.2 9.2 20<br />
M 87 Positive 102 11.7 8.7 45<br />
F 78 Positive 527 12.5 8.4 20<br />
M 35 Negative 112 12.5 8.5 25<br />
F 66 Positive 275 10 9 25<br />
M 71 Positive 150 10.2 7.7 40<br />
F 38 Positive 128 10.7 8.5 20<br />
F 75 Positive 142 10.8 7.5 40<br />
F 67 Positive 109 10.8 9 23<br />
F 40 Positive 85 12 9.3 40<br />
F 72 Negative 99 10.7 9.8 60<br />
F 50 Negative 110 11 8.2 17<br />
F 73 Positive 191 10.5 7.6 22<br />
F 54 Positive 284 13 9.2 27<br />
M 76 Positive 158 11.1 9.4 60<br />
F 88 Positive 88 11.1 9.5 20<br />
F 72 Positive 151 10.4 8.6 25<br />
F 43 Positive 82 11.3 8.6 25<br />
F 67 Positive 156 11.2 7.6 60<br />
F 61 Positive 174 10.7 8.9 20<br />
F 58 Positive 174 11.3 9.5 16<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
29<br />
There were three cases of concomitant surgery. The<br />
first was combined with a hemi-thyroi<strong>de</strong>ctomy; the<br />
second was combined with a thyroi<strong>de</strong>ctomy as well<br />
due to the fact that the a<strong>de</strong>noma was found embed<strong>de</strong>d<br />
insi<strong>de</strong> the thyroid tissue. The third patient also<br />
had a Zenker diverticulum’s that was excised. In this<br />
particular patient the incision had to be exten<strong>de</strong>d<br />
to encompass the resection of the other pathology.<br />
Multiglandular disease was encountered in two out<br />
of twenty two patients (9%). The procedure inclu<strong>de</strong>d<br />
the other si<strong>de</strong> of the neck in both of these patients.<br />
The presence of multi-glandular disease had been<br />
confirmed on the Sestamibi scintigraphy done preoperatively<br />
in both cases. All the patients in the<br />
study returned to normal serum calcium levels in<br />
the first twenty-four hours after surgery. There were<br />
some sporadic cases of symptomatic hypo-calcemia<br />
that were managed immediately. These episo<strong>de</strong>s<br />
were most common on the second to third postoperative<br />
day when the patient was discharged from<br />
the hospital. The most common symptoms of postoperative<br />
hypocalcemia were perioral, peripheral<br />
extremity paresthesias and dizziness. All patients<br />
were observed in the hospital for a period of twentyfour<br />
hours and were discharged home the next day.<br />
There was one exception, the patient operated<br />
un<strong>de</strong>r IV sedation and local anesthesia was sent<br />
home the same day of surgery after being observed<br />
in the recovery ward for two hours. Average hospital<br />
stay was one day. Symptoms and signs of hypercalcemia<br />
improved immediately and to the last<br />
follow-up visit there have been no patients with recurrence<br />
of hypercalcemia.<br />
DISCUSSION<br />
Twenty-two patients un<strong>de</strong>rwent parathyroi<strong>de</strong>ctomy<br />
because it was indicated based on their symptoms<br />
or due to aberrant biochemical parameters.<br />
The 2002 NIH Consensus Conference on Hyperparathyroidism<br />
Recommendations for Surgery established<br />
the following indications for parathyroi<strong>de</strong>ctomy:<br />
1) Typical bone, renal, gastrointestinal, or<br />
neuromuscular symptom; life-threatening hypercalcemia.<br />
2) Calcium level > 11.2-12.0 mg/dL (> 2.9-<br />
3.0 mmol/L). 3) Urine calcium level > 400 mg/d<br />
(10 mmol/d); renal stones. 4) BMD 2 SD’s
30<br />
nine clearance > 30%. 6) Age < 50 years old. 7)<br />
Patient request. 8) Calcium level > 1 mg/dL (0.25<br />
mol/L) above normal for each laboratory. 9) Bone Mass<br />
Density T score < 2.5 at any sites (This last corresponds<br />
to the WHO <strong>de</strong>finition of osteoporosis.) (1)<br />
The standard treatment for patients with<br />
primary hypercalcemia due to parathyroid<br />
a<strong>de</strong>nomas is surgical removal through bilateral<br />
exploration of the neck. In the past seventeen years<br />
of this single surgeon experience the approach for<br />
removal of parathyroid a<strong>de</strong>nomas has significantly<br />
evolved. The success of bilateral neck exploration<br />
without the aid of localizing techniques has been<br />
well documented in the literature with rate of almost<br />
95% cure since the early eighties in some series (2,<br />
3). This was the standard procedure used for many<br />
years since the beginning of this practice. Yet, we<br />
sought to find ways to ren<strong>de</strong>r the procedure less<br />
morbid in light of the fact that surgical intrusion of<br />
the whole neck is utilized for finding a single<br />
a<strong>de</strong>noma in the majority of cases. Hence, a less<br />
invasive procedure had to be <strong>de</strong>veloped for the<br />
benefit of the patient. Set asi<strong>de</strong>, the inci<strong>de</strong>nce of<br />
multiglandular disease documented in the literature<br />
and in various case series is around 10 to 20% (4,<br />
5). In our experience the presence of multiglandular<br />
disease (9%) was comparable to what has been<br />
reported before.<br />
The advent of intraoperative methylene blue<br />
injection to aid in the direct visualization of<br />
parathyroid a<strong>de</strong>nomas changed our perspectives on<br />
the necessity of bilateral neck explorations. The<br />
procedure consisted on injecting a discrete dose of<br />
methylene blue (amount) prior to operation. Unilateral<br />
neck exploration would be done and the<br />
presence of a<strong>de</strong>noma was confirmed when the<br />
a<strong>de</strong>noma was directly visualized by its bluish<br />
appearance. We began using this method during<br />
the mid to late 1990’s. Nonetheless, intraoperative<br />
usage of methylene blue <strong>de</strong>creased the oxygen<br />
saturation of the patient intraoperatively. Although,<br />
this effect was known to be false –methylene blue<br />
absorbs light at 666 nm, whereas the pulse oximeter<br />
sensor absorbs light at 660 nm to 910 nm, causing<br />
an interference with the sensor and it appears the<br />
patient is <strong>de</strong>saturating- it still was a controversial<br />
practice from our point of view (6). We ceased usage<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
of methylene blue in 2001 and began seeking<br />
alternatives for intraoperative localization that would<br />
be cost effective for the patient and at the same<br />
time would minimize intraoperative and<br />
postoperative risks.<br />
Between 2001 and late 2004 this group<br />
mainly relied on Sestamibi scintigraphy for the<br />
localization of suspected parathyroid a<strong>de</strong>nomas.<br />
If a scintigraphy was positive then the surgeon<br />
procee<strong>de</strong>d to operate in the area where the hot<br />
spot was evi<strong>de</strong>nt on the film. Bilateral neck explorations<br />
were solely indicated for patients<br />
whose scintigraphy was inconclusive or negative,<br />
but the patient still had signs and symptoms of<br />
primary hyperparathyroidism and abnormal laboratory<br />
parameters (hyper-calcemia, hypophosphatemia<br />
and elevated serum PTH levels).<br />
We introduced the use of the gamma probe<br />
combined with Sestamibi scintigraphy to our<br />
practice in the beginning of the year 2005. This<br />
technique, which was documented in the literature<br />
since 1995, had various advantages. It reduced the<br />
surgical incision of the anterior neck by 50%. Before<br />
this we would use a five to 7 cm incision for bilateral<br />
and unilateral neck explorations, because there<br />
was always a question of what the extent of the<br />
surgery would be. The next benefit it ad<strong>de</strong>d was<br />
the <strong>de</strong>crease in operating time for this type of<br />
surgery, which meant less time un<strong>de</strong>r anesthesia.<br />
Likewise, there was a reduction in the morbidity of<br />
the surgery. Access to the diseased gland was<br />
directed to a specific point in the presence of uniglandular<br />
or multiglandular disease. All these variables<br />
led inevitably to <strong>de</strong>creased length of hospital<br />
stay that in turn translates to greater costeffectiveness<br />
for the patient and the hospital. These<br />
factors are stressed in various documented series<br />
(8, 9). The cure rate for our method has been 100%<br />
using this technique comparable to other series that<br />
have reported 98%, 97.8% and 96%, and that have<br />
a significantly higher number of patients (5, 10, 11).<br />
The only docu-mented adverse effect of Sestamibi<br />
in the literature is the <strong>de</strong>velopment of erythema<br />
multiforme in one patient (12).<br />
The introduction of this method also set the stage<br />
for the usage of local anesthesia and IV sedation in<br />
the excision of a neck a<strong>de</strong>noma. This method for<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
anesthesia has gained wi<strong>de</strong> acceptance in the United<br />
States since the late 1990’s. The Mayo Clinic group,<br />
for example, reported 263 patients between 1998 and<br />
2004 who un<strong>de</strong>rwent parathyroi<strong>de</strong>ctomy with IV<br />
sedation and local anesthesia (1). In early 2008 we<br />
performed the first case of parathy-roi<strong>de</strong>ctomy with<br />
IV sedation and local anesthesia in <strong>Puerto</strong> <strong>Rico</strong>. The<br />
patient was discharged home on the same day of<br />
surgery after being monitored for two hours in the<br />
recovery room.<br />
There are two current trends in the effective<br />
localization and removal of parathyroid a<strong>de</strong>nomas. The<br />
first one is the technique we use with our patients,<br />
which involves radio-gui<strong>de</strong>d localization of the diseased<br />
gland. Yet, there is a new movement towards the use<br />
of intraoperative parathyroid hormone measurements.<br />
This technique consists of doing the same<br />
preoperative workup as for the patients mentioned<br />
above, targeting the a<strong>de</strong>noma with preoperative<br />
imaging, removing the diseased gland and obtaining<br />
an intraoperative serum intact PTH measurement<br />
(iPTH). A <strong>de</strong>crease of 50% from the initial serum<br />
PTH concentration means the success of the<br />
surgery. Therefore, there is objective confirmation<br />
during the surgery that the parathyroid gland has<br />
been removed. There is current controversy as to<br />
whether one procedure is more effective than the<br />
other. Although, we already have the necessary tools<br />
for intraoperative PTH measurement during surgery<br />
we have not used them. There are two primary<br />
reasons for this. In view of our success rate with<br />
the gamma probe, even in the presence of multiglandular<br />
disease, we do not believe that the patient<br />
will necessarily benefit from intraoperative PTH<br />
monitoring. Second, there is the problem of the<br />
ad<strong>de</strong>d cost of intraoperative intact PTH testing to<br />
our patients. In one series using the gamma probe<br />
method translated in an average savings of $4,000<br />
US dollars compared to other procedures (9).<br />
Minimally invasive parathyroi<strong>de</strong>ctomy using the<br />
gamma probe is an excellent and safe treatment<br />
for patients with primary hyperparathyroidism and<br />
suspected a<strong>de</strong>noma. This technique avoids the<br />
morbidity of bilateral neck exploration, reduces<br />
operative time, and has a high patient acceptance.<br />
The initial success that we have had has led us to<br />
use it as a standard for parathyroi<strong>de</strong>ctomies.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
31<br />
RESUMEN<br />
Las técnicas <strong>de</strong> manejo actual para el manejo<br />
<strong>de</strong> hiperparatiroidismo primario <strong>de</strong>pen<strong>de</strong>n <strong>de</strong><br />
estudios <strong>de</strong> localización preoperatorio para llevar<br />
a cabo una cirugía exploratoria <strong>de</strong>l cuello.<br />
Esta serie <strong>de</strong> casos informa los resultados <strong>de</strong><br />
paratiroi<strong>de</strong>ctomia minimamente invasiva utilizada<br />
en veintidós pacientes con hiperparatiroidismo<br />
primario y sospecha <strong>de</strong> a<strong>de</strong>noma.<br />
Todos los pacientes con hiperpara-tiroidismo<br />
sintomático o laboratorios en sangre alterados se<br />
les practicaron una evaluación preoperatorio que<br />
incluía niveles <strong>de</strong> calcio, hormona paratiroi<strong>de</strong>a y<br />
una cintigrafía <strong>de</strong> Tc-99 Sestamibi. El día <strong>de</strong> la cirugía<br />
se administro una cantidad <strong>de</strong>l contraste Tc-<br />
99 Sestamibi para localizar la glándula enferma<br />
intra-operatoriamente. En el periodo inmediato <strong>de</strong><br />
la inyección un aparato para <strong>de</strong>tectar radiación<br />
gamma se aplicó al cuello anterior para <strong>de</strong>terminar<br />
el área <strong>de</strong> radiación más prominente hacia don<strong>de</strong><br />
seria dirigida la cirugía. Todo tejido removido durante<br />
la cirugía seria probado nuevamente con el<br />
<strong>de</strong>tector a ver si este tejido resultaba en un gradiente<br />
mayor que aquello <strong>de</strong>tectado en el cuello. A todos<br />
los pacientes se les hizo histología congelada inmediata<br />
para confirmar que el tejido removido fuera<br />
glandular. Los niveles <strong>de</strong> calcio en suero fueron<br />
medidos a las 24 horas y tres días <strong>de</strong>spués en una<br />
visita a la oficina.<br />
Veintidós pacientes con hipercalcemia<br />
sintomática con una edad media <strong>de</strong> 63 años (entre<br />
las eda<strong>de</strong>s <strong>de</strong> 35 a 87 años) se sometieron a<br />
cintigrafía preoperatoria y laboratorios. El calcio<br />
y la PTH promedio antes <strong>de</strong> operarse fueron<br />
<strong>de</strong> 11.3 mg/dL y 194.2 pg/mL respectivamente.<br />
En cuatro pacientes (18%) la cintigrafía fue<br />
negativa y en dieciocho pacientes fue (82%) fue<br />
positiva. El a<strong>de</strong>noma <strong>de</strong> paratiroi<strong>de</strong>s fue confirmado<br />
con histología inmediata en todos los pacientes.<br />
El tiempo operatorio promedio fue <strong>de</strong><br />
32 minutos excepto en tres pacientes en los que<br />
se llevo a cabo otro procedimiento simultáneamente<br />
(hemitiroi-<strong>de</strong>ctomia, etc.). No hubo complicaciones<br />
intra-operatorias. Todos los pacientes<br />
exhibieron una disminución <strong>de</strong> los niveles <strong>de</strong><br />
calcio inmediatamente al igual que resolución <strong>de</strong><br />
los síntomas asociados al a<strong>de</strong>noma.
32<br />
La paratiro<strong>de</strong>ctomia minimamente invasiva usando<br />
el aparato <strong>de</strong> captación <strong>de</strong> radiación para localizar<br />
la glándula es una alternativa excelente y segura en el<br />
tratamiento quirúrgico <strong>de</strong> hiperparatiroidismo prima-<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
rio. En nuestra experiencia esta técnica evita la necesidad<br />
<strong>de</strong> tener que explorar el cuello para localizar un<br />
a<strong>de</strong>noma, disminuye el tiempo intraoperatorio y tiene<br />
muy buena aceptación por el paciente.<br />
REFERENCES<br />
1. Grant CS, Thompson G. Primary hyperparathyroidism surgical management since the introduction of the minimally invasive<br />
parathyroi<strong>de</strong>ctomy. Mayo Clinic Experience Arch. Surg. 2005; 140: 472-479<br />
2. Van Heer<strong>de</strong>n JA, Grant CS Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg. 1991; 15:<br />
688-692<br />
3. Kaplan EL, Yashiro T Salti G. Primary Hyperparathyroidism in the 1990s Ann Surg. 1992; 215:300-317<br />
4. Nussbaum SR, Thompson AR, Hutcheson KA, et al. Intraoperative measurement of parathyroid hormone in the surgical management of<br />
hyperparathyroidism. Surgery 1988; 104:1121-1127<br />
5. Gil-Car<strong>de</strong>nas A, Gamino R, et al. Is intraoperative parathyroid hormone assay mandatory for the success of targeted parathyroi<strong>de</strong>comty?<br />
J Am Coll Surg Vol. 204, No.2, <strong>Feb</strong>ruary 2007<br />
6. Pinero A, Illana J, Effect of Oximetry on Dyes Used for Sentinel Lymph No<strong>de</strong> Biopsy Arch Surg. 2004; 139:1204-1207<br />
7. Martinez DA, King DR, et al. Intraoperative i<strong>de</strong>ntification of parathyroid gland pathology: a new approach. J Pediatr Surg. 1995;<br />
30(9):1306-9.<br />
8. Goldstein RE, Blevins L, et al. Effect of minimally invasive radiogui<strong>de</strong>d parathyroi<strong>de</strong>ctomy on efficacy, length-of-stay, and costs in the<br />
management of primary hyperparathyroidism. Ann Surg. 2000; 231(5):732-42<br />
9. Hutchinson JR, Yan<strong>de</strong>ll DW, et al. Three-year financial analysis of radio-gui<strong>de</strong>d parathyroi<strong>de</strong>ctomy. Am Surg. 2004; 70(12):1112-5.<br />
10. Caudle AS, Brier SE, et al. Experienced radio-gui<strong>de</strong>d surgery teams can successfully perform minimally invasive radio-gui<strong>de</strong>d<br />
parathyroi<strong>de</strong>ctomy without intraoperative parathyroid hormone assays. Am Surg. 2006; 72(9): 785-9.<br />
11. Shabtai M, Benhaim M, et al. 140 consecutive cases of minimally invasive, radio-gui<strong>de</strong>d parathyroi<strong>de</strong>ctomy, lessons learned and longterm<br />
results. Surg Endosc. 2003; 17(5):688-91.<br />
12. Thomson LE, Allman KC Eryhtema multiforme reaction to sestamibi. J Nucl Med 2001; 42(3): 534<br />
Hazte socio <strong>de</strong><br />
la Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
Ayudanos a mejorar el escenario<br />
médico hospitalario en <strong>Puerto</strong> <strong>Rico</strong><br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
34<br />
Artículos Originales • Original Articles<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
PARATHYROID SURGERY WITHOUT INSTANT PTH<br />
OR RADIOGUIDED SESTAMIBI SCAN<br />
By: E. Vázquez-Quintana, MD; FACS. and D.E. Vázquez-Torres, MD*<br />
Abstract<br />
Background: Radiogui<strong>de</strong>d Sestamibi scan and<br />
instant PTH (iPTH) are being used in minimally<br />
invasive parathyroid surgery (MIP). Experienced<br />
surgeons cure over 90-95% of the patients with<br />
primary hyperparathyroidism.<br />
Purpose/Method: To study the surgical results<br />
in treating hyperparathyroidism in a for profit<br />
community hospital lacking both iPTH and<br />
radiogui<strong>de</strong>d Sestamibi scan, we reviewed the<br />
patients operated from November 1, 2005 to<br />
October 31, 2006.<br />
Results: The study comprised 56 patients: 52<br />
with primary hyper-parathyroidism, three with<br />
secondary hyperparathyroidism and one with<br />
tertiary hyperparathyroidism. The only localizing<br />
test utilized pre-operatively was the Sestamibi Scan.<br />
PTH was measured immediately before and after<br />
surgery but the results was received seven to ten<br />
days later. The affected glands were removed in all<br />
patients. Fifty of 52 (96%) of the patients with<br />
primary hyperparathyroidism, the three patients<br />
with secondary hyper-parathyroidism and the<br />
patient with tertiary hyperparathyroidism are<br />
normocalcemic with normal PTH levels. Two<br />
patients have persistent mild hypercalcemia.<br />
Associated conditions were three papillary carcinoma<br />
of the thyroid, three multinodular goiter, four<br />
had a single thyroid nodule, one had an adrenal<br />
tumor and three were reoperations.<br />
Conclusion: Parathyroid surgery can be done<br />
safely and effectively in community hospitals without<br />
the utilization of radiogui<strong>de</strong>d Sestamibi scan and<br />
iPTH measurement.<br />
Key words: parathyroid, surgery, instant PTH,<br />
Sestamibi scan<br />
Historically, it has been known that experienced<br />
head and neck surgeons cure 90-95% of patients<br />
with primary hyperparathyroidism at the time of<br />
initial operation. Initially, there were no localizing<br />
tests to aid the surgeon to i<strong>de</strong>ntify the diseased<br />
glands. The patients were referred by the endocrinologist<br />
who ma<strong>de</strong> the diagnosis by excluding other<br />
diseases producing hypercalcemia. The PTH test<br />
was not available and all four parathyroid glands<br />
had to be i<strong>de</strong>ntified intraoperatively. Eventually,<br />
sonography, CT scan, MRI and thallium-technetium<br />
substraction scans were introduced. None of these<br />
studies were found to be superior to the results already<br />
obtained surgically. The best localizing test,<br />
the Sestamibi parathyroid scan, was introduced in<br />
1992. 1 SPECT (Single Proton Emission Computerized<br />
Tomography), a variant of the Sestamibi scan,<br />
has also been used.<br />
In recent years, the use of radiogui<strong>de</strong>d Sestamibi<br />
scan during the operation and instant PTH (iPTH)<br />
sampling have been utilized for Minimally Invasive<br />
* From the Department of Surgery, Pavia Hospital, San Juan, PR. Address Reprints: E. Vazquez Quintana, MD - Pavía Street, Suite 301, San Juan,<br />
P. R. 00909. E-mail <br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 1: Types of Hyperparathyroidism<br />
Total number of patients 56<br />
Primary hyperparathyroidism 52<br />
Single A<strong>de</strong>noma 51<br />
Two A<strong>de</strong>nomas 1<br />
Secondary hyperparathyroidism 3<br />
Tertiary hyperparathyroidism 1<br />
Parathyroid (MIP) surgery. 2 The radiogui<strong>de</strong>d<br />
Sestamibi Scan is recommen<strong>de</strong>d to localize the affected<br />
parathyroid gland and the iPTH is used to<br />
reassure the surgeon that the operation is already<br />
completed and no additional exploration is nee<strong>de</strong>d.<br />
Some authors claim that the use of iPTH improves<br />
the success rate of surgery in hyperparathyroidism.<br />
3,4 Other groups have questioned the use<br />
of iPTH measure-ments in the <strong>de</strong>cision making process<br />
during the operation. 5,6 But the availability of<br />
these two latter techniques is not ubiquitous in all<br />
hospitals. Challenging the need to use these two<br />
modalities we conducted the present study.<br />
METHODS<br />
All patients operated for hyperpara-thyroidism<br />
from November 1, 2005 to October 31, 2006 in a<br />
private for profit community hospital comprise the<br />
study group. A total of 56 patients had surgery<br />
during that period of time. Frozen section was used<br />
in all patients to confirm the removal of parathyroid<br />
tissue. Samples for calcium, phosphorus and PTHintact<br />
were drawn immediately before surgery and<br />
30 minutes after completion of the operation. It<br />
took from seven to ten days to get the PTH intact<br />
measurements, so the results had no influence on<br />
the <strong>de</strong>cision by the operative surgeon. The only<br />
localizing test utilized preoperatively was the<br />
Sestamibi parathyroid scan.<br />
RESULTS<br />
General anesthesia was used in all patients. A<br />
small 2-3 cm. collar incision was utilized and the<br />
diseased gland was approached. A total of 52<br />
patients had primary hyperparathyroidism, 51 had<br />
a single a<strong>de</strong>noma, and one had two a<strong>de</strong>nomas. No<br />
patient had parathyroid hyperplasia or carcinoma.<br />
There were three patients with secondary<br />
hyperparathyroidism and one had tertiary<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
Table 2: Associated conditions:<br />
Papillary carcinoma of thyroid 3<br />
Multinodular goiter 3<br />
Single thyroid nodule 4<br />
Adrenal tumor 1<br />
Re-operations 3<br />
35<br />
hyperparathyroidism. (See table 1). Another 11<br />
patients had associated conditions; three had<br />
papillary carcinoma of the thyroid, three had<br />
multinodular goiter, four had a single thyroid nodule,<br />
one had an adrenal tumor and three were<br />
reoperations. (See table 2). The average operative<br />
time for the initial operation in patients with primary<br />
hyperpara-thyroidism was 30 minutes. After<br />
removal of the affected gland or glands the PTHintact<br />
<strong>de</strong>creased to less that 50% of the preoperative<br />
levels in all except four patients. In those patients<br />
the PTH levels ranged from 88 to181 pg/ml.<br />
Nonetheless, the calcium has remained normal in<br />
two. One patient continued with hypercalcemia<br />
although review of the pathology confirmed that<br />
an a<strong>de</strong>noma of the parathyroid had been removed.<br />
The other patient with a positive Sestamibi scan<br />
removal of the affected gland was interpreted as<br />
normal parathyroid tissue.<br />
All patients with primary hyperparathyroidism,<br />
except three, were discharged on the following day.<br />
Three patients <strong>de</strong>veloped hypocalcemia requiring<br />
intravenous calcium replacement. Two of these<br />
patients had severe hyperparathyroidism with<br />
osteopenia and large a<strong>de</strong>nomas, the other also had<br />
a total thyroi<strong>de</strong>ctomy for multinodular goiter. The<br />
secondary and tertiary hyperparathyroidism patients<br />
remained hospitalized until the calcium stabilized.<br />
Two patients with primary and one with<br />
secondary hyperparathyroidism were reoperations.<br />
One of these patients had a retrosternal mediastinal<br />
a<strong>de</strong>noma. The latter was missed by the former<br />
surgeon although it was seen on a Sestamibi<br />
parathyroid scan. (See figure 1).<br />
DISCUSSION<br />
Since the 1960’s, the senior author has gone<br />
through all the stages in the history of parathyroid<br />
surgery. Initially, there were no tests to help in<br />
localizing the parathyroid glands, therefore,
36<br />
Figure 1: Sestamibi scan showing a<br />
Retrosternal parathyroid a<strong>de</strong>noma<br />
exploration and visual i<strong>de</strong>ntification of all the glands<br />
was required. In an article, “Localization of<br />
Parathyroid Lesions: Blind Study for Surgeons”<br />
published in 1989, 7 the experience of the surgeon<br />
was tested against the use of CT and thallium-<br />
Figure 2: SPECT scan with a marker at the<br />
sternal notch showing the exact location of the<br />
ectopic parathyroid a<strong>de</strong>noma.<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 3: Sestamibi parathyroid scan<br />
Positive 35<br />
Negative 8<br />
Equivocal 9<br />
technetium substraction scans. The senior author<br />
was able to localize the abnormal parathyroid gland<br />
in all 15 hyperparathyroid patients. The CT scan<br />
failed to i<strong>de</strong>ntify the a<strong>de</strong>noma in 73% of the cases.<br />
The thallium-technetium substraction scan missed<br />
almost 50% of the diseased glands.<br />
The sensitivity and specificity of the localizing<br />
tests is variable. The best reported results with<br />
Sestamibi parathyroid scans show a sensitivity and<br />
specificity of over 95%. But that is not the<br />
experience in other centers. The test <strong>de</strong>pends on<br />
the number of oxyphil cells of the parathyroid<br />
a<strong>de</strong>nomas. Patients with negative Sestamibi scans<br />
have lower cure rates. 8<br />
The Sestamibi parathyroid scan, the only<br />
localizing test done preoperatively in the present<br />
series, was correct in localizing the affected gland<br />
in 35 of the 52 patients (67.3%). It was completely<br />
negative in eight and equivocal in nine patients (See<br />
Table 3). A SPECT was used with a marker to <strong>de</strong>termine<br />
how low in the retrosternal region the<br />
a<strong>de</strong>noma was in a patient with persistent<br />
hyperparathyroidism (See figure 2). This gland was<br />
retrieved through the neck incision. Of a total of<br />
52 patients with primary hyperparathyroidism the<br />
affected glands were i<strong>de</strong>ntified and removed in all<br />
patients at the initial operation, only two patients<br />
remained hypercalcemic, for a success rate of 96%<br />
without the use of radiogui<strong>de</strong>d Sestamibi scan or<br />
iPTH measurements.<br />
In <strong>Puerto</strong> <strong>Rico</strong>, none of our 52 hospitals have<br />
laboratories capable of doing iPTH. Only a single<br />
institution is using radiogui<strong>de</strong>d Sestamibi scans. In<br />
the United States of a total of 5,759 hospitals only<br />
around 92 utilize iPTH testing during parathyroid<br />
operations. 9, 10 The ten<strong>de</strong>ncy has been to do<br />
specialized tests in a central laboratory.<br />
Quan-Yang Dhu 6 questioned the use of instant<br />
PTH testing to predict cure in Minimally Invasive<br />
Parathyroi<strong>de</strong>ctomy. PTH monitoring is less accurate<br />
in multiple glandular disease (double a<strong>de</strong>nomas or<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
hyperplasia). The failure rate for PTH testing is from<br />
2-5%. The test works best when it is less nee<strong>de</strong>d.<br />
Peter Stalberg et al 5 have also tested<br />
intraoperative parathyroid hormone measurement<br />
in the <strong>de</strong>cision-making process during minimally<br />
invasive parathyroi<strong>de</strong>ctomy. One hundred patients<br />
with positive Sestamibi scans un<strong>de</strong>rwent MIP.<br />
Ninety-eight patients were cured by MIP, two<br />
remained hypercalcemic. Nine patients failed to<br />
show a drop in iPTH and they would have been<br />
subjected to a more extensive neck exploration<br />
unnecessarily based on a false negative result.<br />
We have documented that parathyroid surgery can<br />
be done effectively with excellent results in a small for<br />
profit community hospital lacking both iPTH testing<br />
and radiogui<strong>de</strong>d Sestamibi parathyroid scans.<br />
RESUMEN<br />
Cintigrafía intraoperatoria radio-guiada por<br />
Sestamibi más el uso instantáneo <strong>de</strong> niveles <strong>de</strong><br />
parathormona (iPTH) se utilizan en el manejo <strong>de</strong><br />
cirugía <strong>de</strong> paratiroi<strong>de</strong>s minimamente invasiva. Cirujanos<br />
con experiencia curan 90 a 95% <strong>de</strong> los<br />
pacientes con hiperparatiroidismo primario.<br />
El propósito <strong>de</strong> este estudio es reconocer los<br />
resultados quirúrgicos en el manejo <strong>de</strong><br />
hiperparatiroidsmo primario en un hospital <strong>de</strong> co-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
37<br />
munidad que carece <strong>de</strong> ambos Cintigrafía por<br />
Sestamibi y iPTH revisando los pacientes operados<br />
<strong>de</strong>s<strong>de</strong> Noviembre 1ero <strong>de</strong> 2005 a Octubre 31, 2006.<br />
El estudio comprendió 56 pacientes: 52 con<br />
hiperparatiroidismo primario, tres con<br />
hiperparatiroidismo secundario y uno con<br />
hiperparatiroidismo terciario. El único estudio<br />
localizante usado preoperatoria-mente fue una<br />
Cintigrafía con Sestamibi. Niveles <strong>de</strong> parathormona<br />
se midieron inmediatamente antes y <strong>de</strong>spués <strong>de</strong> la<br />
cirugía, pero los resultados se recibieron siete a diez<br />
días <strong>de</strong>spués. La glándula afectada se removió en<br />
todos los pacientes. Cincuenta <strong>de</strong> 52 (96%) <strong>de</strong> los<br />
pacientes con hiperparatiroidismo primario, los tres<br />
pacientes <strong>de</strong> hiperparatiroidismo secundario y el<br />
único paciente con hiperparatiroidsmo terciario<br />
están normocalcemicos con niveles normales <strong>de</strong><br />
parathormona (PTH). Dos pacientes persisten con<br />
hipercalcemia leve. Condiciones asociadas incluyen<br />
tres carcinomas papilares <strong>de</strong>l tiroi<strong>de</strong>s. Tres bocios<br />
multinodulares, cuatro nódulos sencillos <strong>de</strong>l tiroi<strong>de</strong>s,<br />
un tumor adrenal y tres re-operaciones.<br />
Cirugía <strong>de</strong> las paratiroi<strong>de</strong>s se pue<strong>de</strong> hacer <strong>de</strong><br />
forma segura y efectiva en hospitales <strong>de</strong> comunidad<br />
sin la utilización intraoperatoria <strong>de</strong> Cintigrafía con<br />
Sestamibi o mediciones instantáneas <strong>de</strong> PTH.<br />
REFERENCES<br />
1. Taillefer R, Boucher Y. Potvin C, Lambert R. Detection and localization of parathyroid a<strong>de</strong>nomas in patients with hyperparathyroidism<br />
using a single radionucli<strong>de</strong> imaging procedure with technetium-99m-sestamibi (Double-phase study). J Nucl Med 1992;33:1801-1807<br />
2. Chen H, Sokol LJ, U<strong>de</strong>lsman R. Outpatient minimally invasive parathyroi<strong>de</strong>ctomy: a combination of sestamibi-SPECT localization,<br />
cervical anesthesia, and intraoperative parathyroid hormone assay. Surgery 1999;126:1016-1021<br />
3. Irvin Gl, Solorzano CC, Carneiro DM. Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited parathyroi<strong>de</strong>ctomy,<br />
improve success rate, and predict outcome. World J Surg. 2004; 28:1287-1292<br />
4. Chen H, Pruhs Z, Starling JR, Mack E. Intraoperative parathyroid hormone testing improves cure rates in patients un<strong>de</strong>rgoing minimally<br />
invasive parathyroi<strong>de</strong>ctomy. Surgery 2005; 138:583-587<br />
5. Stalberg P, Sidhu S, Sywak M, Robinson B, Wildinson M, Delbridge L. Intraoperative Parathyroid Hormone Measurement During<br />
Minimally Invasive Parathyroi<strong>de</strong>ctomy: Does it “Value Add” to Decision Making? J Am Coll Surg 2006: 203:1-6<br />
6. Duh QY. What’s new in general surgery: endocrine surgery. J Am Coll Surg 2005;201:746-753<br />
7. Vázquez-Quintana E, Quintana C, Aguiló F, Pagán-Sáez H, Silva F. Localization of Parathyroid Lesions: Blind Study for Surgeons. Bol.<br />
Asoc. Med <strong>Puerto</strong> <strong>Rico</strong> 1989: 81:342-344<br />
8. Allendorf J, Kim L, Chabot J, DiGiorgi M, Spanknebel K, LoGerfo P. The Impact of Sestamibi Scanning on the Outcome of Parathyroid<br />
Surgery. J Clin Endo & Met 2003; 88:3015-3018<br />
9. American Hospital Association Statistics-Health Forum Data 2006 edition<br />
10. Hortin GL, Carter AB. Intraoperative Parathyroid Hormone Testing: survey of testing program characteristics. Arch Pathol Lab Med<br />
2002: 126; 1045-9
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
39<br />
Artículos Originales • Original Articles<br />
SURVEY OF CARDIAC RHYTHM MANAGEMENT AND<br />
DEVICE IMPLANT PATTERNS IN PUERTO RICO:<br />
ANALYSIS OF 13,854 CARDIAC IMPLANTS<br />
ABSTRACT<br />
Background: Surveys of cardiac pacing and<br />
implantable cardiovertor <strong>de</strong>fibrillators (ICD) have<br />
been reported since 1969 and 1993 respectively.<br />
Increasing costs of medical technology, budget<br />
constraints and emergent new clinical indications<br />
prompted our committee to conduct the first survey<br />
of cardiac rhythm management and <strong>de</strong>vice implant<br />
patterns in <strong>Puerto</strong> <strong>Rico</strong>.<br />
Method: Clinical and <strong>de</strong>mographic data were<br />
obtained for all cardiac <strong>de</strong>vices sold and implanted<br />
from 2000 to 2006, through a joint agreement with<br />
official representatives of the 2 largest<br />
manufacturers and distributors of cardiac<br />
pacemakers and ICD in <strong>Puerto</strong> <strong>Rico</strong>.<br />
Results: 13,854 cardiac <strong>de</strong>vices were<br />
implanted from 2000 to 2006. The number of<br />
permanent pacemakers (PP) implanted per million<br />
population has varied from 430 in the year 2000<br />
to 482 in the year 2006. A significant greater<br />
number of males received PP than females (P < .05).<br />
Yearly increases in implant rates for cardiac<br />
resynchronization therapy (CRT) and ICD were<br />
observed, mainly due to new emergent clinical<br />
indications, appropriate insurance coverage and<br />
availability of implanting electrophysiologists.<br />
By: Juan M. Aranda, M.D., F.A.C.C. ‡, Miguel Girod, M.S ‡, Eng., Fernando Ochoa ‡,<br />
Miguel Abreu, M.D.*, F.A.C.C., José J. Rivera, M.D., F.A.C.C.** ‡, Juan C. Sotomonte, M.D.** ‡,<br />
Angel Rodríguez, M.D.**, Daniel Arzola, M.D.**, Raúl Jiménez, M.D., F.A.C.C.** ‡,<br />
and Juan M. Aranda, Jr., M.D., F.A.C.C. £<br />
Conclusions: Sales figures from PP and ICD<br />
manufacturers are a reliable system to calculate and<br />
analyze changes in cardiac <strong>de</strong>vice implant patterns.<br />
The rate of 482 PP per million population positions<br />
<strong>Puerto</strong> <strong>Rico</strong> as the third largest implant market in<br />
North and South America. This finding should be<br />
useful to insurance health provi<strong>de</strong>rs since 76% of<br />
the implants are performed in patients over 65 years<br />
old. In the year 2006, <strong>Puerto</strong> <strong>Rico</strong> was the 10 th<br />
largest implant market in the world with 67 CRT<br />
implanted per million population. A significant<br />
greater number of CRT and ICD were implanted in<br />
males than females. This gen<strong>de</strong>r difference has<br />
increased in spite of strict requirements to inclu<strong>de</strong><br />
more females in clinical trials and intensive,<br />
educational and awareness efforts conducted among<br />
physicians and patients. A summary of the current<br />
gui<strong>de</strong>lines and clinical indications is provi<strong>de</strong>d to<br />
assist the physician in the selection of patients<br />
referred for cardiac rhythm management and<br />
implant procedures.<br />
Key words: cardiac, rhythm, <strong>de</strong>vice,<br />
implant, heart<br />
* From the Department of Medicine, University of <strong>Puerto</strong> <strong>Rico</strong>, School of Medicine, ** Cardiovascular Center of <strong>Puerto</strong> <strong>Rico</strong>, ‡ the Caribbean,<br />
Pavía Heart and Lung Institute in San Juan, PR, and £ University of Florida College of Medicine, Gainesville, Florida. Request reprints to: Juan M.<br />
Aranda, MD, FACC, Hostos # 411, Hato Rey, P.R. 00918.
40<br />
INTRODUCTON<br />
Surveys of permanent cardiac pacing modalities<br />
in the United States have been published every 4 years<br />
since 1969 (1-6). Worldwi<strong>de</strong> information on cardiac<br />
pacemakers and implantable cardiovertor –<br />
<strong>de</strong>fibrillators (ICD) implant patterns have also been<br />
reported since 1973 and 1993 respectively (7-16). The<br />
last world survey presented in the XII World Symposium<br />
of Cardiac Pacing and Electro-physiology in 2003<br />
inclu<strong>de</strong>d Panama and Dominican Republic as the first<br />
countries from Central America and the Caribbean<br />
Region participating in the study (17).<br />
With increasing costs of medical technology and<br />
on going budget constraints, insurance companies,<br />
government health directors, cardiac <strong>de</strong>vice manufacturers<br />
and health provi<strong>de</strong>rs have become increasingly<br />
interested in emergent cardiac <strong>de</strong>vice indications,<br />
changes in implant patterns and timely implant<br />
statistics. These factors prompted us to conduct<br />
the first survey on cardiac rhythm modalities<br />
and <strong>de</strong>vices implant patterns in <strong>Puerto</strong> <strong>Rico</strong>. The<br />
study was conducted from 2000 through 2006.<br />
MATERIAL AND METHODS<br />
A steering committee was formed in 2004 by<br />
all clinical and interventional electro-physiologists<br />
practicing their sub-specialty in <strong>Puerto</strong> <strong>Rico</strong>. As new<br />
electrophysiologists arrived in 2005 and 2006, they<br />
were incorporated in the committee.<br />
The committee <strong>de</strong>veloped the gui<strong>de</strong>lines of the<br />
study and selected all the information and<br />
parameters required to start and successfully complete<br />
the study. The objectives were thoroughly<br />
discussed with authorized representatives of the two<br />
main manufacturers and distributors of cardiac<br />
<strong>de</strong>vices in <strong>Puerto</strong> <strong>Rico</strong>. After adopting a<br />
professional and ethical policy to protect the<br />
patients privileged information and manufacturer<br />
privileged data, Boston Scientific CRM. (St. Paul,<br />
MN) previously Guidant Corp. and Medtronic Inc.,<br />
(Minneapolis, MN) agreed to participate and<br />
contribute to the survey. An agreement was ma<strong>de</strong><br />
not to discuss or present individual company figures<br />
except in a global form after analysis of the data.<br />
The committee estimated that these 2 companies<br />
provi<strong>de</strong>d over 98% of all the implanted <strong>de</strong>vices<br />
during the surveyed period of time.<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
The information requested inclu<strong>de</strong>d the<br />
patient’s age and gen<strong>de</strong>r, indication, type of <strong>de</strong>vice<br />
implanted, initial mo<strong>de</strong> of pacing, hospitals active<br />
in pacemaker and ICD implants, number of <strong>de</strong>vices<br />
sold per year and complications of the procedures.<br />
The manufacturers provi<strong>de</strong>d the information for all<br />
permanent pacemaker systems and ICD <strong>de</strong>vices sold<br />
and implanted in <strong>Puerto</strong> <strong>Rico</strong> since 2000.<br />
The information received was entered in a<br />
computerized data base for processing using<br />
Microsoft Office Excel 2003 SP2 for data analysis<br />
and the Statistical Package for the Social Sciences<br />
for Windows version 11.0.1 (SPSS Inc. Chicago,<br />
Illinois) for statistical calcu-lations. The statistical<br />
analysis consisted of calculating means, marginal<br />
percent and percent for various subcategories. Chi<br />
square and / or Fisher’s tests of association and<br />
two-tailed in<strong>de</strong>pen<strong>de</strong>nt t-tests were used to i<strong>de</strong>ntify<br />
significant differences in patients characteristics,<br />
implants per year and changes in the mo<strong>de</strong> of<br />
pacing. For all tests a p value less than 0.05 was<br />
consi<strong>de</strong>red to be statistically significant.<br />
RESULTS<br />
1- Classification of Cardiac Rhythm Modalities<br />
The worldwi<strong>de</strong> survey of cardiac pacing<br />
published in 2001 (17) classified cardiac rhythm<br />
modalities in three distinct categories:<br />
a-Cardiac Devices (permanent pacemakers)<br />
implanted for therapy of slow symptomatic<br />
rhythms (single and dual chamber pacing).<br />
b-Cardiac Devices (implantable cardiovertor<strong>de</strong>fibrillator<br />
or ICD) implanted for therapy of<br />
malignant ventricular arrhythmias or ventricular<br />
fibrillation (one or two leads ICD system).<br />
c-Cardiac Devices implanted for therapy of<br />
heart failure or cardiac resyn-chronization<br />
therapy (CRT) through atrial and<br />
simultaneous biventricular stimulation. This<br />
modality is subdivi<strong>de</strong>d into CRT-P (pacing<br />
without ICD) and CRT-D (pacing with ICD).<br />
2- Patterns of Cardiac Rhythm Management<br />
Thirteen thousand, eight hundred and fifty<br />
four (13,854) cardiac <strong>de</strong>vices were implanted<br />
from 2000 to 2006 (Table 1). The total<br />
number of implanted <strong>de</strong>vices has significantly<br />
increased throughout the 6 year period (P <<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 1: Total cardiac <strong>de</strong>vices implanted (2000-2006)<br />
*Permanent Pacemaker; **Inclu<strong>de</strong>s CRT–P and CRT-D<br />
.05). This pattern has been due to the yearly<br />
increases in the number of ICD and CRT<br />
implanted. This is supported by the fact that<br />
the percentage of permanent pacemakers of<br />
the total number of <strong>de</strong>vices implanted per<br />
year <strong>de</strong>creased from 98% in 2000 to 80%<br />
in 2006 (P < .05), while the % of ICD and<br />
CRT increased from 2% to 20% in the same<br />
period (P < .05). Table 2 highlights the<br />
number of <strong>de</strong>vices implanted per million<br />
population. This allows us to compare our<br />
implant rates with other countries in Europe,<br />
North and South America (18-19).<br />
Table 3: Largest Implanting Markets of CRT-P and CRT<br />
- D Devices Per Million Population (2004-2006) (19).<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
41<br />
Table 2: Total <strong>de</strong>vices implanted per million population<br />
(2000 - 2006)<br />
* Population in millions<br />
3- Demographics of Implanted Devices<br />
Our pacemaker implant rate per million<br />
population (18) has remained relatively stable<br />
and has varied from 430 to 482 in 2000<br />
and 2006, respectively. This information,<br />
ranked <strong>Puerto</strong> <strong>Rico</strong> in 2006 as the third<br />
largest implanting country in North and<br />
South America, behind United States (950<br />
per million) and Canada (591 per million) and<br />
17th in the world among countries with the<br />
largest implanting rates (19).<br />
The rate of ICD implants has significantly<br />
increased from 8 ICD per million in 2000 to<br />
55 per million in 2006. Our implant rate in<br />
2006 (55 per million) followed the United States<br />
(396 per million) and Canada (56 per million)<br />
and far excee<strong>de</strong>d the implant rates of larger<br />
countries in Central and South America (19).<br />
The CRT implant rate in 2006 (67 per million)<br />
ranked second in North and South America<br />
behind the United States (245 / million) and<br />
11 th among the largest implanting countries in<br />
the world (19) (Table 3). The dramatic changes<br />
observed in implant patterns were due to<br />
improved recognition of traditional indications<br />
and more significantly, to the recent approval<br />
of clinical indications with appropriate medical<br />
coverage sponsored by governmental and<br />
private insurance companies.
42<br />
Figure 1 shows the gen<strong>de</strong>r differences in<br />
recipients of permanent pacemakers, CRT’s<br />
and ICD’s in <strong>Puerto</strong> <strong>Rico</strong>. Note that a significant<br />
greater number of males received PP<br />
than females (p < .05). 557 pacemakers per<br />
million males were implanted in 2006 as<br />
compared to 386 per million females (Figure<br />
2), even though the population of females<br />
in <strong>Puerto</strong> <strong>Rico</strong> has been greater than males<br />
since 2000 (p < .05) (18). This gen<strong>de</strong>r difference<br />
has remained relatively constant in<br />
the last 7 years. Our data also shows that in<br />
<strong>Puerto</strong> <strong>Rico</strong> four times as many men as<br />
women received an ICD to prevent sud<strong>de</strong>n<br />
cardiac <strong>de</strong>ath (Figure 3). Almost twice as<br />
many males as females received CRT to treat<br />
heart failure in spite of the fact that women<br />
account for the majority of <strong>de</strong>aths from heart<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
failure (20). This has occurred in spite of<br />
significant efforts to increase female participants<br />
in clinical studies which have shown similar<br />
benefits in the female as compared to the male<br />
gen<strong>de</strong>r (20). In the last 4 years, this gen<strong>de</strong>r disparity<br />
has become more significant in our patient<br />
population as newer indications have been<br />
implemented in clinical practice (21).<br />
The patients that received resynchronization<br />
therapy, ICD or both appear to<br />
be younger than the patients with PP implants.<br />
Figure 4 shows that approximately<br />
66% of PP recipients were > 70 years as<br />
compared to 37% of CRT and ICD recipients<br />
(p < .05). Only 17% of PP were implanted<br />
in patients < 60 years as compared<br />
to 32% for CRT and ICD recipients. In <strong>Puerto</strong><br />
<strong>Rico</strong>, similar to European and North Ameri-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
can Countries, 32% of all PP implanted since<br />
2000 were in patients > 80 years of age, a<br />
characteristic of countries with a comprehensive<br />
health care system (22).<br />
4- Indications and Clinical Features of Device<br />
Recipients<br />
a- Permanent Pacemaker Recipients<br />
The indications for initial PP implant were<br />
clearly i<strong>de</strong>ntified in 4,518 patients (Figure<br />
5). Sick sinus syndrome (43%) and advanced<br />
atrio-ventricular conduction disturbances<br />
(48%), either complete A-V block or Mobitz<br />
II A-V block, were the most frequent indications<br />
for implant. These observations are very<br />
similar to the data reported in the world survey<br />
for calendar year 2001 (23). In 2001, a<br />
permanent pacemaker was first implanted in<br />
<strong>Puerto</strong> <strong>Rico</strong> for post ablation A-V block.<br />
Since then, 14 other patients have received<br />
PP implants for this complication of<br />
radiofrequency ablation for supraventri-cular<br />
tachycardia. None were reported in 2005<br />
and 2006, a reflection of the local expertise<br />
gained in the earlier years of ablation.<br />
There has been a progressive and significant<br />
increase in the use of dual chamber pacing<br />
systems (DDD) as shown in Figure 6. This<br />
trend became statistically significant in 2004<br />
(p < .05). It increased from 50% in 2000 to<br />
70% in 2006. Correspondingly the single chamber<br />
pacing implants (VVI) <strong>de</strong>creased to 30% in<br />
2006. It has been selected mostly for recipients<br />
whose un<strong>de</strong>rling rhythm was atrial fibrilla-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
43<br />
tion with high gra<strong>de</strong> A-V block.<br />
b- CRT and ICD Recipients<br />
The first ICD was implanted in <strong>Puerto</strong> <strong>Rico</strong><br />
in 1993 by Colón, Jiménez et a. (24). About 5<br />
per year were implanted through 1998. Since<br />
2000, there has been a significant increase in<br />
ICD implants in <strong>Puerto</strong> <strong>Rico</strong> (30). Thirty (2% of<br />
total cardiac <strong>de</strong>vices) were implanted in 2000<br />
as compared to 216 (9% of total cardiac <strong>de</strong>vices)<br />
in 2006 (Table 2). As new indications for<br />
the <strong>de</strong>vice were approved for patients with congestive<br />
heart failure, the potential target population<br />
expan<strong>de</strong>d as well (25-29).<br />
Table 4 shows the total number of CRT and<br />
ICD recipients in whom the indications for the <strong>de</strong>vices<br />
were i<strong>de</strong>ntified (1,585 of 1,594 implants).<br />
63% of the ICD <strong>de</strong>vices were implanted in patients<br />
with ischemic or non ischemic cardiomiopathy, EF<br />
< 35%, congestive heart failure Class I – II – III<br />
New York Heart Association and a QRS complex<br />
less than 120 msec (25). This group inclu<strong>de</strong>d asymptomatic<br />
survivors of an acute myocardial infarction<br />
(>40 days) and a EF < 30%. It has been<br />
shown that ICD implants in these groups of patients<br />
<strong>de</strong>creased sud<strong>de</strong>n <strong>de</strong>ath by 23% (25-30). The ICD’s<br />
were implanted in the other group (37%) either<br />
because they had spontaneous or induced, hemodynamically<br />
unstable ventricular tachycardia or ventricular<br />
fibrillation. When the QRS complex was over<br />
120 msec, the patients met the criteria for cardiac<br />
resynchroni-zation therapy (CRT), except<br />
those that were asymptomatic (Class I) (26-29).<br />
Table 4 also shows that all CRT – P <strong>de</strong>vices
44<br />
implanted in <strong>Puerto</strong> <strong>Rico</strong> since 2000 were implanted<br />
in patients with EF < 35%, CHF, Class<br />
II, III and IV and QRS duration > 120 msec. CRT<br />
in addition to a<strong>de</strong>quate medical therapy reduces<br />
mortality, hospitalizations and improves cardiac<br />
function, structure, symptoms and quality of life<br />
(26-29). A <strong>de</strong>fibrillator was ad<strong>de</strong>d to CRT therapy<br />
in 2002 after it was <strong>de</strong>monstrated that prophylactic<br />
single lead ICD implantation in patients<br />
with CHF II, III, who received CRT, <strong>de</strong>creased sud<strong>de</strong>n<br />
<strong>de</strong>ath by 30% (27). 274 CRT-D implants in<br />
<strong>Puerto</strong> <strong>Rico</strong> were performed in this group of patients,<br />
34% of them had spontaneous or induced<br />
ventricular tachycardia or ventricular fibrillation.<br />
An interesting observation was ma<strong>de</strong> in a subgroup<br />
analysis of 2,123 patients with permanent<br />
pacemakers and 232 with CRT and ICD <strong>de</strong>vices<br />
implanted in 2005. The implant procedures for PP<br />
were evenly divi<strong>de</strong>d between private hospitals<br />
throughout the island (49%) and primary aca<strong>de</strong>mic<br />
medical centers including the VA Hospital (51%).<br />
On the other hand, most of the CRT / ICD implants<br />
(88%) were performed in the aca<strong>de</strong>mic centers<br />
as compared to 12% implanted in private hospitals<br />
(p < .05). Several factors were i<strong>de</strong>ntified to<br />
explain these differences; availability of trained implanting<br />
electrophysiologists, appropriate medical<br />
implant facilities and hospital reimbursement for the<br />
procedure by private or government medical insurance<br />
companies.<br />
In the year 2006, the average hospital reimbursement<br />
for implanting a CRT-D in the United<br />
States was $44,000 as compared to $31,000 the<br />
highest reimbursement to a medical school affiliated<br />
hospital in <strong>Puerto</strong> <strong>Rico</strong> and $24,000.00 if the<br />
procedure was performed in a private institution<br />
(31). The lower reimbursement to private hospitals<br />
is probably the most important factor that explains<br />
the low number of CRT and ICD implanted in these<br />
institutions (Figure 7).<br />
DISCUSSION<br />
This study conducted by clinical and<br />
interventional electrophysiologists in <strong>Puerto</strong> <strong>Rico</strong><br />
together with the main manufacturers and distributors<br />
of cardiac <strong>de</strong>vices, inclu<strong>de</strong>d over 98% of all<br />
<strong>de</strong>vices implanted from 2000 – 2006. In the ab-<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 4: Clinical Indications for CRT and ICD<br />
Implants in <strong>Puerto</strong> <strong>Rico</strong> 2000-2006<br />
sence of an on going pacemaker and ICD registry<br />
or a <strong>de</strong>dicated coordinator to conduct hospital surveys<br />
of cardiac implants, using sales figures form<br />
pacemakers and ICD manufacturers has been shown<br />
to be a practical and reliable system to calculate<br />
implant rates and <strong>de</strong>lineate trends in the market<br />
(32).<br />
The major drawback of this method has been<br />
the limited clinical information that is obtained from<br />
sales figures (14). A specific example in our study,<br />
has been the absence of data related to procedural<br />
complications and outcomes of ICD implants in<br />
survivors of sud<strong>de</strong>n cardiac <strong>de</strong>ath. Nonetheless,<br />
the committee believes that the numbers used to<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
calculate implants per year are very reliable and represent<br />
current trends in <strong>Puerto</strong> <strong>Rico</strong>. Similar data<br />
collection has been used to calculate annual implant<br />
rates in the United States (14).<br />
The classification of implantable cardiac <strong>de</strong>vices<br />
into <strong>de</strong>vices for bradycardia therapy, <strong>de</strong>vices for<br />
tachycardia therapy (malignant ventricular<br />
arrhythmias) and <strong>de</strong>vices for heart failure (cardiac<br />
resynchronization therapy) is useful specially for the<br />
non implanting cardiologist and non cardio-vascular<br />
physician since it allows them to i<strong>de</strong>ntify specific<br />
cardiac <strong>de</strong>vices with specific clinical indications.<br />
With increasing costs of sophisticated medical technology<br />
and <strong>de</strong>creased reimbursement for specialized<br />
hospital procedures, our findings should be of significant<br />
interest to insurance companies, <strong>de</strong>vice manufactures,<br />
health directors and medical provi<strong>de</strong>rs. Our<br />
rate of permanent pacemaker implants per million<br />
population has remained relatively stable from 2000<br />
through 2006 with a greater number implanted in<br />
males than females even-though the number of females<br />
has been greater than males through the 7 year period<br />
(18). The rate of 482 pacemakers implanted per<br />
million population in 2006, positions <strong>Puerto</strong> <strong>Rico</strong> as<br />
the third largest implanting market in our hemisphere<br />
and 17 th in the world among countries with the largest<br />
implanting rates (19). It does not appear that this rate<br />
will increase significantly over the next five years. Our<br />
study was not <strong>de</strong>signed to address this issue since we<br />
expected that the data would have shown significant<br />
yearly increases per million in PP implant rates.<br />
Geographic and Regional Variations in Pacemakers<br />
and ICD Implantation Rates<br />
Geographic variations in annual implant rates have<br />
been substantial within the United States and variations<br />
have been reported among states and regions<br />
(33, 34). Several factors interact with each other to<br />
<strong>de</strong>termine each country annual rate (14, 17, 22).<br />
• Economic Indices<br />
The Gross National Product and per capita<br />
annual health expenditure are directly but<br />
not always related to PP and ICD implant<br />
rates (22-23). The correlation is mo<strong>de</strong>st<br />
since some countries with similar economic<br />
indices have different implant rates, (22)<br />
which may be influenced by medical health<br />
coverage, procedural reimbursement and<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
45<br />
the age distribution of their population.<br />
• Insurance Coverage and Procedure Reimbursement<br />
<strong>Medica</strong>l insurance coverage and procedural<br />
reimbursement for hospitals is another <strong>de</strong>terminant<br />
factor. The DRG (Diagnosis Related<br />
Group) may inclu<strong>de</strong> cost of the <strong>de</strong>vice<br />
and hospitalization, even if prolonged. The<br />
type of institution where the <strong>de</strong>vice is implanted<br />
also influences hospital reimbursement,<br />
as a result hospital administrators scrutinize<br />
each implant, specially if the procedure<br />
is performed in a private institution. This<br />
is clearly the situation in <strong>Puerto</strong> <strong>Rico</strong> as previously<br />
discussed.<br />
• Cost of the Device<br />
The lower the cost of the <strong>de</strong>vice the higher<br />
the implant rate. The goal of all payors and<br />
administrators is to obtain the lowest price<br />
for the best <strong>de</strong>vice available in the market<br />
(33). Whether the <strong>de</strong>vice is imported or<br />
manufactured locally is another influential<br />
factor. The price of imported <strong>de</strong>vices is usually<br />
higher and <strong>de</strong>pends on multiple factors<br />
such as local taxation, reimbursement, medical<br />
coverage and where is the <strong>de</strong>vice manufactured<br />
or assembled (32-34).<br />
• Implanting Physicians<br />
Available trained implanting cardiologists or<br />
electrophysiologists significantly increased<br />
the CRT and ICD implants observed in our<br />
study. The number of implanting physicians<br />
increased in <strong>Puerto</strong> <strong>Rico</strong> after 2000 with the<br />
arrival of several trained implanting electrophysiologists<br />
that implemented very well the<br />
emergent newly approved clinical indications.<br />
• Aging Population<br />
The age distribution of the population varies<br />
significantly among different geographical areas<br />
(22, 34). 82% of the pacemakers in <strong>Puerto</strong> <strong>Rico</strong><br />
were implanted in patients over 60 years old, 80%<br />
were ol<strong>de</strong>r than 65 years. Our data agrees with<br />
the information reported in the literature (22).<br />
Therefore the number of potential candidates for<br />
permanent pacing is directly proportional to the %<br />
of the population over 65 years. It is then reasonable<br />
and more significant to compare rates among
46<br />
different countries calculating the rate of implants<br />
for each age group, specifically the rate per million<br />
population over 65 years. Subgroup analysis of our<br />
data shows the following pertinent observations;<br />
In 2002, the implant rate in <strong>Puerto</strong> <strong>Rico</strong> per<br />
million population over 65 years (3,308) was very<br />
similar to the rate per million over 65 reported in<br />
the United States (3,560)(22). Even though the<br />
overall rate per million in the United States in 2002<br />
(840 / million) was almost twice the overall implant<br />
rate in <strong>Puerto</strong> <strong>Rico</strong> (475 / million) in the same year.<br />
The rate in <strong>Puerto</strong> <strong>Rico</strong> per million over 65 was<br />
significantly greater than any of the other larger<br />
implanting countries in 2002 (22). We believe that<br />
the explanation to this paradox is the availability of<br />
medical insurance to all patients over 65 that qualify<br />
to receive <strong>Medica</strong>re Parts A and B. This type of<br />
medical coverage might not be available in many of<br />
the other larger implanting countries.<br />
This information (implant rate per million population<br />
>65 years) is useful to all medical health provi<strong>de</strong>rs<br />
since it allows the plan administrator to estimate<br />
the number of patients enrolled in their network<br />
that may require implantable cardiac <strong>de</strong>vices.<br />
This will enable the health plan to i<strong>de</strong>ntify and assign<br />
the economic resources required to fund these<br />
life saving clinical services.<br />
World Wi<strong>de</strong> Increases in CRT and ICD<br />
Implants<br />
Figure 8 summarizes the progressive yearly increases<br />
in CRT and ICD implanted in <strong>Puerto</strong> <strong>Rico</strong><br />
since 2000 and the published studies that documented<br />
the clinical indications and improved medical<br />
outcomes after the <strong>de</strong>vices were implanted.<br />
Miracle study (28) published in 2001 was instrumental<br />
in providing objective evi<strong>de</strong>nce which<br />
lead the Food and Drug Administration to approve<br />
the biventricular pacing system as <strong>de</strong>finite therapy<br />
for Class III – IV patients with congestive heart failure<br />
in spite of optimal medical therapy. The same<br />
investigators reported in 2003 (Miracle CRT-D) that<br />
combined CRT with an implantable cardiovertor<br />
<strong>de</strong>fibrillation in advanced congestive heart failure,<br />
diminished cardiac mortality (27). This report together<br />
with the approval of prophylactic ICD implant<br />
in patients with a previous myocardial infarc-<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
* 80% of PP were implanted in patients 65 years or ol<strong>de</strong>r<br />
tion (MADIT II) and an ejection fraction < 30% explains<br />
the significant increases in ICD implants from<br />
2002 through 2004 (30).<br />
In the years 2003 and 2004 the reports published<br />
in SCD – HeFT (25) and Companion Trials<br />
(29) further expan<strong>de</strong>d the indications for ICD implants.<br />
SCD – HEFT (Sud<strong>de</strong>n Cardiac Death in<br />
Heart Failure) showed that in patients with NYHA<br />
Class II, III CHF and an EF < 35%, a single lead<br />
ICD implant reduced overall mortality by 23% irrespective<br />
of the QRS duration. Companion Trial<br />
<strong>de</strong>monstrated that in patients with CHF and optimal<br />
medical therapy, the addition of an ICD to cardiac<br />
resynchronization therapy <strong>de</strong>creased mortality<br />
30% (29). As a result of these studies, CRT – D<br />
implants in <strong>Puerto</strong> <strong>Rico</strong> increased 100% yearly from<br />
2003 to 2005.<br />
Although, all cause mortality with cardiac<br />
resynchronization alone <strong>de</strong>creased as compared to<br />
optimal medical therapy, it was not significant and<br />
the results of CRT on the risks and complications<br />
of the implanting procedure remained unclear. The<br />
Care-Heart Failure Study published in 2005 (26)<br />
clearly showed that in patients with echocardio-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
graphic criteria of ventricular dyssynchrony, cardiac<br />
resynchronization improved symptoms, quality of<br />
life, reduced compli-cations and risk of <strong>de</strong>ath by<br />
36% in addition to the benefits affor<strong>de</strong>d by optimal<br />
medical therapy. The addition of a <strong>de</strong>fibrillator might<br />
further reduce the risk of sud<strong>de</strong>n <strong>de</strong>ath by 7% (29).<br />
As of August, 2006, the following are the approved<br />
clinical indications for an implantable<br />
cardiovertor – <strong>de</strong>fibrillator (ICD) and cardiac<br />
resynchronization therapy (CRT) with or without a<br />
<strong>de</strong>fibrillator (25-30). The committee realizes that<br />
individual assessment of each candidate and an explanation<br />
of the risk and benefits of the procedure<br />
are the clinical approaches to follow, however it<br />
hopes that the following summary helps in the selection<br />
and referral of candidates for implantation<br />
of CRT and ICD <strong>de</strong>vices.<br />
Indications FOR ICD<br />
A-Patients with Ischemic Cardiomiopathy<br />
• EF < 30%<br />
Previous myocardial infarction,<br />
more than 40 days (30)<br />
• EF < 35%<br />
Previous myocardial infarction<br />
more than 40 days<br />
Spontaneous or induced sustained<br />
ventricular tachycardia or ventricular<br />
fibrillation, not related to an acute<br />
infarction or reversible causes (29).<br />
• EF < 35%<br />
Congestive Heart Failure Class II –<br />
III, after optimal medical therapy (25).<br />
B-Patients with Non Ischemic Cardio-myopathy<br />
• EF < 35%<br />
Cardiomyopathy of more than 9<br />
months duration<br />
Congestive Heart Failure Class II or<br />
III after a<strong>de</strong>quate medical therapy (27).<br />
If the duration of the QRS complex<br />
is more than 120 msec seconds and<br />
the patient presents CHF Class II -<br />
IV, he / she meets the criteria for<br />
cardiac resynchronization therapy.<br />
Others<br />
C-Patients with Genetic Cardiac, Hereditary<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
47<br />
Diseases (6).<br />
• Prolonged (congenital) QT syndrome<br />
• Hypertrophic Cardiomyopathy<br />
• Brugada Syndrome<br />
• Idiopathic Ventricular Fibrillation or<br />
Ventricular Tachycardia (hemodinamically<br />
unstable)<br />
As more clinical indications emerge and are<br />
approved for patient selection, it is imperative that<br />
each country performs on going evaluations of cardiac<br />
rhythm management and <strong>de</strong>vice implant patterns<br />
in or<strong>de</strong>r to <strong>de</strong>termine the most cost effective<br />
way to allocate the clinical and economic resources<br />
that are available. The permanent data base <strong>de</strong>veloped<br />
during this study provi<strong>de</strong>s the fundamental tool<br />
to achieve this objective in <strong>Puerto</strong> <strong>Rico</strong>.<br />
ACKNOWLEDGEMENT<br />
We acknowledge the cooperation of Carlos<br />
Girod, MD, FACC for the <strong>de</strong>tailed revision of the<br />
manuscript and Ms. Luz M. González for her expertise<br />
in word processing used for the preparation<br />
of this article.<br />
RESUMEN<br />
Evaluaciones <strong>de</strong> patrones <strong>de</strong> estimulación cardiaca<br />
e implantes <strong>de</strong> cardiovertores – <strong>de</strong>sfibriladores<br />
se han reportado <strong>de</strong>s<strong>de</strong> 1969 y 1993<br />
respectivamente. Aumentos en costos <strong>de</strong><br />
tecnología médica, limitaciones presupuestarias y<br />
nuevas indicaciones clínicas, motivó a nuestro grupo<br />
<strong>de</strong> trabajo a llevar a cabo la primera recopilación y<br />
evaluación <strong>de</strong> manejo <strong>de</strong> ritmo cardiaco y patrones<br />
<strong>de</strong> implantes en <strong>Puerto</strong> <strong>Rico</strong>.<br />
Información clínica y <strong>de</strong>mográfica se obtuvo <strong>de</strong><br />
todos los dispositivos cardiacos vendidos e<br />
implantados <strong>de</strong>s<strong>de</strong> el año 2000 – 2006, a través<br />
<strong>de</strong> acuerdos pre-establecidos con representantes <strong>de</strong><br />
las 2 compañías <strong>de</strong> distribución y manufactura <strong>de</strong><br />
marcapasos cardiacos y <strong>de</strong>sfibriladores implantables<br />
en <strong>Puerto</strong> <strong>Rico</strong>.<br />
Se implantaron 13,854 dispositivos durante el<br />
periodo <strong>de</strong> estudio (enero, 2000 – diciembre, 2006).<br />
No hubo aumentos en el número <strong>de</strong> implantes <strong>de</strong><br />
marcapasos permanentes por millón <strong>de</strong> habitantes;<br />
la tasa varió <strong>de</strong> 430 en el año 2000 a 482 en el<br />
año 2006. Los marcapasos se implantaron
48<br />
significativa-mente mas en hombres que en mujeres<br />
(p
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
26- Cleland J.G., Daubert J.C., Erdmann E. et al; The effect of cardiac resynchronization or morbity and mortality in heart failure N. Engl J.<br />
Med. April 14, 2005. 352: 1539-1549.<br />
27- Bristow M.R., Saxon L.A., Boehmer J., et al; Effect of Cardiac Resynchronization Therapy with and without an Implantable Defibrillator<br />
in Morbity and Mortality in Advanced CHF. N. Eng. J. Med March, 2004 350: 1245-1256.<br />
28- Abraham W., Fisher W, Smith A., et al, Cardiac Resynchronization in Chronic Heart Failure N Engl J. Med 2002, 364; - 1845-1853.<br />
(Miracle CRT-P)<br />
29- Young J.B., Abraham W.T., Smith A.L., et al, Combined Cardiac Resynchronization and Implantable Cardioversion Defibrillation in<br />
advanced chronic heart failure: the Miracle ICD Trial JAMA 2003: 289: 2685-94 (Miracle CRT-D).<br />
30- Moss A.J., Zareba W., Hall W.J., et al, Prophylactic Implantation of a Defibrillator in Patients with Myocardial Infarction and Reduced<br />
Ejection Fraction N Engl J. Med 2002; 346: 877-883. (MADIT II).<br />
31- Centers for <strong>Medica</strong>re and <strong>Medica</strong>id Services, www.cms.hhs.gov. November 24, 2006.<br />
32- Mond H.G.; The World Survey of Cardiac Pacing and Cardiovertor Defibrillator; Lesson Learnt J. Inter Card Electrophysiol (2006) 17:<br />
211-214.<br />
33- Ector H., Rickards A.F., Lin<strong>de</strong> C., et al, Demographic data on First Pacemaker implantation in Europe. Europace 2001, 2: B 132.<br />
34- Wennberg J.E., Un<strong>de</strong>rstanding Geographic Variations in Health Care Delivery (editorial ) N Engl J Med. 1999; 340: 52-53.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
49
50<br />
Artículos <strong>de</strong> Repaso • Review Articles<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
HISTORY OF PARATHYROID SURGERY IN PUERTO RICO<br />
By: Enrique Vázquez-Quintana, MD*<br />
ABSTRACT<br />
Review article that inclu<strong>de</strong>s the worldwi<strong>de</strong> history,<br />
as a reference for the rea<strong>de</strong>rs, and the local<br />
history of hyperparathyroidism in <strong>Puerto</strong> <strong>Rico</strong>.<br />
WORLDWIDE HISTORY<br />
Few things in the history of medicine are more<br />
fascinating than the history of parathyroid disease.<br />
It is interesting to know how many medical stu<strong>de</strong>nts<br />
have participated in endocrine surgery making significant<br />
discoveries.<br />
The ol<strong>de</strong>st example of what is believed to be<br />
the first case of hyperparathyroidism dates to the<br />
Early Neolithic period, around 7000 years ago. The<br />
examination of a skeleton revealed osteopenia, osteodystrophia<br />
fibrosa cystica and salt-and-pepper<br />
appearance of the cranium.<br />
Sir Richard Owen, an anatomist of the Natural<br />
History Museum of London, in 1850, was the first<br />
to <strong>de</strong>scribe the parathyroid glands in a rhinoceros<br />
autopsy, as a small compact yellow glandular body<br />
attached to the thyroid gland. No credit was given<br />
to his observations since he never performed a histological<br />
confirmation.<br />
Robert Remak, a microanatomist and embryologist,<br />
in 1855, <strong>de</strong>scribed a small gland in association<br />
with the thymus, which was clearly not a<br />
lymph no<strong>de</strong> (1).<br />
Rudolph Virchow, in 1862, also <strong>de</strong>scribed in a<br />
single specimen, a gland that was not an accessory<br />
thyroid gland, lymph no<strong>de</strong> or any other neck structure<br />
familiar to him as pathologist.<br />
In 1887, Ivar Victor Sandstrom, a Swedish<br />
medical stu<strong>de</strong>nt, <strong>de</strong>scribed the number, location,<br />
color and blood supply of the parathyroids in animals<br />
and 50 human autopsies. He wrote a manuscript<br />
entitled “On a new gland in man and fellow<br />
animals”. He suggested the name “glandulae<br />
parathyroidae”. The manuscript was rejected by<br />
German editors because of its length. Years later it<br />
was published in the Uppsala <strong>Medica</strong>l Journal. His<br />
contribution was not recognized as <strong>de</strong>served and<br />
he committed suici<strong>de</strong> a few years later.<br />
Eugene Cley, French physiologist, in 1891,<br />
observed the relationship between tetany and the<br />
parathyroid glands.<br />
In 1891, Fre<strong>de</strong>rich von Recklinghausen, a pathology<br />
professor at Strasbourg, <strong>de</strong>scribed seven<br />
patients with bone disease, multiple neurofibromas<br />
and cafe au-lait spots.<br />
The first attempt to transplant the parathyroid<br />
glands was performed by Anton von Eiselberg, a<br />
disciple of Theodor Billroth in 1892.<br />
Neovascularization of the transplanted glands was<br />
observed in experimental animals.<br />
M. Askanazy, in 1903, <strong>de</strong>scribed a patient<br />
with bone disease associated with a large parathyroid<br />
mass, speculating that it might be a parathyroid<br />
tumor.<br />
* From the Department of Surgery, Pavia Hospital, San Juan, PR. Address Reprints: E. Vazquez Quintana, MD - Pavía Street, Suite 301, San Juan,<br />
P. R. 00909. E-mail evazquezmd@gmail.com Main Lecture of the 28 th Raffucci Surgical Forum given on <strong>Feb</strong>ruary 21,2008 at Hotel La Concha,<br />
San Juan, <strong>Puerto</strong> <strong>Rico</strong><br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Tetany, after total thyroi<strong>de</strong>ctomy, led to important<br />
discoveries regarding parathyroid function.<br />
Pathologist William J. MacCallum, at the John<br />
Hopkins Hospital, in 1903, <strong>de</strong>scribed tumors of the<br />
parathyroid gland and the relief of tetany with parathyroid<br />
extract in experimental animals. Both<br />
MacCallum and Carl Voegtlin <strong>de</strong>monstrated that<br />
tetany could be corrected by parathyroid extract or<br />
by giving calcium intravenously.<br />
Pfeiffer and Mayer, in 1907, were the first to<br />
achieve clinical success with autotransplanted parathyroid<br />
tissue.<br />
In 1907, William Stewart Halsted, at John<br />
Hopkins University used parathyroid transplantation<br />
in dogs. He used calcium gluconate to treat<br />
tetany in experimental animals and patients after<br />
thyroi<strong>de</strong>ctomy. He emphasized the preservation of<br />
the parathyroids during thyroid surgery.<br />
Jacob Erdheim, a pathologist from the University<br />
of Vienna, reported in 1907 the association of bone<br />
disease with abnormalities of the parathyroid gland.<br />
But he believed that the bone changes were primary<br />
and not related to an excess of parathyroid hormone.<br />
Freidrich Schkagenhaufer a physician from<br />
Vienna was the first to suggest that parathyroid tumor<br />
was the primary disease and the bone effects<br />
as secondary. He recommen<strong>de</strong>d surgery to remove<br />
the enlarged glands to cure the bone condition.<br />
In 1907, William Halsted and Herbert M. Evans,<br />
a medical stu<strong>de</strong>nt at Hopkins <strong>de</strong>fined the blood supply<br />
of the parathyroid glands using vascular cast injections.<br />
They found that the inferior thyroid artery was the<br />
principal blood supply to both inferior and superior<br />
parathyroid glands in over 90% of the cases.<br />
In 1923, Adolf M. Hanson, a medical stu<strong>de</strong>nt<br />
working in the pharmacology laboratory at the<br />
University of Minnesota, prepared a bovine parathyroid<br />
extract that could be used to treat tetany in<br />
dogs. He observed that the parathyroid extract<br />
causes osteoporosis in animals if used for a long<br />
period of time.<br />
James P. Collip, a biochemist from the University<br />
of Alberta, Canada, also in<strong>de</strong>pen<strong>de</strong>ntly <strong>de</strong>veloped<br />
an extract i<strong>de</strong>ntical to that of Hanson. He was<br />
the first to induce experimental hypercalcemia and<br />
to <strong>de</strong>scribe the effects of severe hypercalcemia.<br />
Clinically, the three most famous patients with<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
51<br />
hyperparathyroidism are Albert Gahne, Charles<br />
Martell and Elva Dawkings (2).<br />
In April 1925, O. Hirsch, a Viennese<br />
otorhinolaryngologist, explored the neck of a patient<br />
who had cystic lesions in both maxillae and mandible<br />
in which he suspected Von Recklinghausen’s disease.<br />
He was looking for a parathyroid tumor but the exploration<br />
was negative.<br />
Albert Gahne was a 34 year street car conductor<br />
in Vienna. His symptoms started in 1919. For<br />
five additional years he <strong>de</strong>veloped bony pains. Decalcification<br />
of the bones was documented by x-rays<br />
and cystic fibrosis of the pelvis and both femurs<br />
observed. He was treated with parathyroid extract<br />
and in July 2, 1995, four fresh human parathyroids<br />
were transplanted. Because no improvement<br />
was observed, Felix Mandl, chairman of surgery at<br />
the University of Vienna, on July 30, 1925, explored<br />
his neck. The operation was done un<strong>de</strong>r local<br />
anesthesia. A large left lower parathyroid tumor<br />
was i<strong>de</strong>ntified close to the inferior thyroid artery.<br />
The lesion was removed, and three other normal<br />
parathyroids were i<strong>de</strong>ntified and preserved. The<br />
pathology revealed no rim of normal parathyroid<br />
tissue to suggest an a<strong>de</strong>noma. The conclusion was<br />
that it was an atypical a<strong>de</strong>noma which may have<br />
malignant <strong>de</strong>generation. He had an excellent recovery.<br />
No symptoms of tetany occurred. He improved<br />
and was discharged on August 7, 1925.<br />
Bone healing and bone <strong>de</strong>nsity improved.<br />
He was readmitted in <strong>Feb</strong>ruary 1926 because of<br />
kidney stones and nephrocalcinosis. His renal problems<br />
and bone pains continued to improve. By May of<br />
1926 he was able to walk with canes. After six years<br />
of clinical improvement, he was again readmitted on<br />
March 23, 1933, with kidney stones and unable to<br />
walk. On October 18, 1933, his neck was re-explored,<br />
no recurrence or additional tumor was found. A portion<br />
of the thyroid was removed, two additional parathyroids<br />
were found, one insi<strong>de</strong> the thyroid. He had<br />
no improvement, continued with hypercalcemia and<br />
died from uremia on <strong>Feb</strong>ruary 26, 1936, almost eleven<br />
years after his first operation.<br />
The autopsy showed extensive cystic fibrosis of<br />
the bones, brown tumors in both femurs and clavicle<br />
and <strong>de</strong>calcification of the spinal column. He had bilateral<br />
kidney stones with hydronephrosis and nephro-
52<br />
Figure 1: Photo of Charles Martell before and<br />
after his disease.<br />
calcinosis. No abnormal parathyroid tissue was found<br />
in the neck, mediastinum or retroperitoneum.<br />
The histologic diagnosis of the tumor removed<br />
from this patient is not clear. An ectopic tumor was<br />
consi<strong>de</strong>red by Mandl but it was not proven at autopsy.<br />
The possibility of parathyroid carcinoma has been<br />
entertained by some authors, but again no proof of<br />
recurrence or metastasis was <strong>de</strong>tected postmortem.<br />
The first parathyroid operation for a parathyroid<br />
tumor in the United States was performed by<br />
EJ Lewis at Cook County Hospital in Chicago, on<br />
June 6, 1926. The patient was a 29 year old woman<br />
with parathyroid carcinoma. The operation was<br />
done six months after Felix Mandl’s operation in<br />
Vienna and 4 months before the Charles Martell’s<br />
first operation in Boston. Multiple no<strong>de</strong>s were found<br />
in the neck. She <strong>de</strong>veloped recurrence of the tumor<br />
requiring excision.<br />
In July 20, 1927, two years after Mandl’s operation,<br />
E. Gold, another Viennese surgeon explored<br />
the neck of a 54 year old female with von<br />
Recklinghausen’s disease. A bilateral neck exploration<br />
was done assisted by his chief, A. Eiselsberg,<br />
and un<strong>de</strong>r the supervision of Felix Mandl. He removed<br />
a parathyroid a<strong>de</strong>noma from the right up-<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
per gland measuring 2.5 X 2.6 cm. Gold was the<br />
first to use the term hyperparathyroidism for the<br />
elevated parathyroid metabolism.<br />
After analyzing 55 other cases, Mandl conclu<strong>de</strong>d<br />
that surgery was the only way to cure hyperparathyroidism.<br />
He advised bilateral neck exploration<br />
to i<strong>de</strong>ntify the normal and abnormal parathyroid<br />
glands. He established the gold standard in the treatment<br />
of hyperparathyroidism.<br />
The most famous patient with hyperparathyroidism<br />
is Charles Martell (see Figure 1). He is probably<br />
the most extensively studied patient with this<br />
disease in the annals of medicine. Charles Martell<br />
was a healthy sea marine captain who was 30 years<br />
old when the diagnosis of hyperparathyroidism was<br />
ma<strong>de</strong> in January 1926 by Eugene F. Dubois at the<br />
Belleveu Hospital in New York City. Extensive calcium<br />
metabolism studies were done and he was<br />
transferred to Massachusetts General Hospital on<br />
April 1927. In May, 1927, he had two neck operations.<br />
During the first, only the right neck was explored<br />
and a normal parathyroid was removed. The<br />
second operation was limited to the left si<strong>de</strong> and<br />
again only one normal parathyroid was removed.<br />
In 1929 he un<strong>de</strong>rwent a third neck operation in<br />
New York City by Russell Patterson with negative<br />
results. In May, 1932, he was readmitted to MGH,<br />
more studies were done un<strong>de</strong>r Fuller Albright and<br />
Benjamin Castleman. Oliver Cope performed three<br />
negative cervical explorations on this patient.<br />
Martell himself insisted on a mediastinal exploration<br />
for an elusive gland. The seventh and last operation<br />
was done by Edward D. Churchill and Cope<br />
and they removed a 3 X 3cm mediastinal parathyroid<br />
a<strong>de</strong>noma. Although a remnant of tissue was<br />
left in the sternal notch region, on the third postoperative<br />
day he <strong>de</strong>veloped tetany. Six weeks later<br />
while un<strong>de</strong>rgoing the removal of an obstructing ureteral<br />
stone he <strong>de</strong>veloped laryngospasm and died.<br />
The third of the most famous patients is Elva<br />
Dawkings. She was a 56 year old woman who was<br />
admitted to Barnes Hospital at Washington University.<br />
She was complaining of muscle weakness, bone<br />
fractures and bilateral renal stones. A fourth year medical<br />
stu<strong>de</strong>nt, Henry A. Dixon, was intrigued by her symptoms.<br />
He documented a serum calcium of 17 mgs/dl<br />
and serum phosphorus of 1.4 mgs/dl. Isaac Y. Olch<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 2: Photo of Dr. Manuel Paniagua<br />
Cámara Courtesy of his daughter,<br />
Dr. Carmen T. Paniagua<br />
explored the neck of this patient on August 1, 1928,<br />
and removed a left lower parathyroid a<strong>de</strong>noma measuring<br />
3 X 3 cms. Her calcium dropped to 4.5 mgs/<br />
dl and she was given the Collip’s parathyroid extract<br />
and calcium intravenously and orally.<br />
James Walton of London, in 1931, recommen<strong>de</strong>d<br />
a wi<strong>de</strong> exposure during surgery, not only<br />
to explore all the parathyroid glands, but also to<br />
search behind the trachea and the mediastinum.<br />
G. Gordan is quoted as saying “The historical<br />
diagnosis of hyperparathyroidism has gone from<br />
bone to stone, to an epigastric moan to none”.<br />
HISTORY IN PUERTO RICO<br />
“In God we trust, all others must bring their<br />
data” By Clau<strong>de</strong> H. Organ, M.D.<br />
The first three <strong>Puerto</strong> Rican endo-crinologists<br />
trained in the United States were Doctors Manuel<br />
Paniagua Cámara, Agustín Martínez <strong>de</strong> Andino and<br />
Lillian Haddock Suárez.<br />
Dr. Paniagua Cámara was the first endocrinologist<br />
in <strong>Puerto</strong> <strong>Rico</strong> (see Figure 2). Was born in San<br />
Juan, <strong>Puerto</strong> <strong>Rico</strong> in 1914 and died in 1983. He obtained<br />
his medical <strong>de</strong>gree in Madrid, Spain and completed<br />
his internal medicine training at the Bayamón<br />
District Hospital. Then obtained his endocrinology<br />
subspecialty at the Thomas Jefferson University in<br />
Phila<strong>de</strong>lphia. He served as captain of the U.S. Army<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
53<br />
Figure 3: Photo of Dr. Agustín Martínez <strong>de</strong> Andino<br />
Courtesy of his son Dr. Richard <strong>de</strong> Andino<br />
during the Second World War. In 1977, he was a founding<br />
member of the Sociedad <strong>Puerto</strong>rriqueña <strong>de</strong><br />
Endocrinología y Diabetes (SPED). He was the medical<br />
director of the Rio Piedras Municipal Hospital as<br />
well as Director of the Endocrinology and Diabetes<br />
Section of the San Juan City Hospital in the <strong>Puerto</strong><br />
<strong>Rico</strong> <strong>Medica</strong>l Center until his retirement in 1982. Dr.<br />
Paniagua published 20 medical articles, none of them<br />
on hyperparathyroidism.<br />
Dr. Agustín Martínez <strong>de</strong> Andino completed his<br />
medical education at the Jefferson <strong>Medica</strong>l College in<br />
Phila<strong>de</strong>lphia in 1944 (see Figure 3). Then he did his<br />
internship and resi<strong>de</strong>ncy in internal medicine and fellowship<br />
in endocrinology at the same institution. He<br />
returned to <strong>Puerto</strong> <strong>Rico</strong> in 1952. He was a founding<br />
member and second presi<strong>de</strong>nt of the Sociedad<br />
<strong>Puerto</strong>rriqueña <strong>de</strong> Endocrinología y Diabetes. He was<br />
chief of the Endocrine and Diabetes Section of the<br />
Department of Medicine at the San Juan City Hospital<br />
in Santurce since August, 1952, to June 30, 1968.<br />
Dr. Martínez <strong>de</strong> Andino was attending in the Metabolic<br />
Disease Ward at the San Patricio Veterans Administration<br />
Hospital from 1952 to 1964. He published<br />
29 articles, none of them about hyperparathyroidism.<br />
Dr Juan E. Rizek was the first physician trained<br />
in endocrinology in <strong>Puerto</strong> <strong>Rico</strong> at the San Juan City<br />
Hospital from 1958-60. The Chairman of Medicine<br />
was Dr. Rurico Díaz Rivera and the Director of Endocrinology<br />
was Dr. Agustín Martínez <strong>de</strong> Andino.
54<br />
Dr. Lillian Haddock Suárez finished her medical<br />
<strong>de</strong>gree at Temple University School of Medicine in<br />
1954 (see Figure 4). She did her internship at the<br />
Bayamón District Hospital and Resi<strong>de</strong>ncy in Internal<br />
Medicine at the San Juan City Hospital in Santurce,<br />
P. R. She then completed a fellowship in Endocrinology<br />
and Metabolism at John Hopkins Hospital from<br />
1957 to 1959. She was a member of the Endocrine<br />
Section at the San Juan City Hospital from 1959-<br />
1960. When the University of <strong>Puerto</strong> <strong>Rico</strong> School of<br />
Medicine moved to the University Hospital at the<br />
<strong>Puerto</strong> <strong>Rico</strong> <strong>Medica</strong>l Center she was <strong>de</strong>signated by Dr.<br />
Mario R. García Palmieri as Director of the Endocrine<br />
Section in 1960. She held that position until 1976.<br />
In 1998 she ma<strong>de</strong> Professor Emeritus of the University<br />
of <strong>Puerto</strong> <strong>Rico</strong>.<br />
Dr. Elena Villavicencio obtained her medical <strong>de</strong>gree<br />
at the University of <strong>Puerto</strong> <strong>Rico</strong> School of Medicine in<br />
1957 (see Figure 5). She completed her internship and<br />
resi<strong>de</strong>ncy in Internal Medicine at the San Juan City<br />
Hospital from 1957 to 1960. She was the first fellow<br />
trained in endocrinology at the University Hospital from<br />
1960-1961. She then obtained a Fellowship in Diabetes<br />
at the University of Minnesota from 1961-1963.<br />
She joined the faculty of the Department of Medicine at<br />
the University Hospital in Rio Piedras in 1963, position<br />
she held until 1967 when she moved to San Antonio,<br />
Texas. In 1968, she started as Clinical Professor of Medicine<br />
at the University of South Texas <strong>Medica</strong>l School.<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 4: Photo of Dr. Lillian Haddock Suárez Figure 5: Photo of Dr. Elena Villavicencio<br />
(Courtesy of her daughter Francesca Cuello)<br />
When I started my resi<strong>de</strong>ncy in General Surgery at<br />
the University Hospital in Rio Piedras, the Chairman of<br />
Surgery was Dr. Francisco L. Raffucci and the Program<br />
Director in Surgery was Dr. Leo Cuello Mainardi (see<br />
Figure 6). Dr. Cuello married Dr. Elena Villavicencio.<br />
Dr. Francisco L. Raffucci was a pioneer in cardiovascular<br />
surgery in <strong>Puerto</strong> <strong>Rico</strong>. He was also involved<br />
in treating patients with portal hyper-tension, liver failure<br />
and pancreatic diseases. At the end of this article<br />
you will become aware of other areas in which he actively<br />
participated.<br />
Dr. Leo Cuello Mainardi was born in Santiago <strong>de</strong><br />
los Caballeros in the Dominican Republic. His parents<br />
moved to <strong>Puerto</strong> <strong>Rico</strong> while he was an infant. He completed<br />
his Bachelor in Biology at the Mayaguez College<br />
of the University of <strong>Puerto</strong> <strong>Rico</strong>. Then he obtained<br />
his medical <strong>de</strong>gree at the University of Paris.<br />
He completed his resi<strong>de</strong>ncy in General Surgery at the<br />
University Hospital in Rio Piedras and a Master in<br />
Science and subspecialty in Thoracic and Cardiovascular<br />
Surgery at the University of Minnesota. From<br />
1963 to 1967, he was an Associate Professor in Surgery<br />
at the University Hospital. In 1967, he and Dr.<br />
Villavicencio moved to San Antonio, Texas. He has<br />
been professor of surgery at the University of Texas<br />
<strong>Medica</strong>l School since 1973.<br />
My interest in parathyroid surgery started in<br />
1964 when Dr. Cuello Mainardi assigned me to dis-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 6: Photos of Dr. Francisco L. Raffucci<br />
and Dr. Leo Cuello Mainardi<br />
cuss the topic of hypercalcemia. I prepared a seminar<br />
on the differential diagnosis of hypercalcemia<br />
that inclu<strong>de</strong>s: sarcoidosis, milk-alkali syndrome,<br />
multiple myeloma, hypernephroma, metastatic bone<br />
disease and hyperparathyroidism.<br />
G. Gordan in 1958 stated: “The historical diagnosis<br />
of hyperparathyroidism has gone from bone<br />
to stone, to an epigastric moan to none”.<br />
The first article on hyperparathyroidism was<br />
published in 1970. It was entitled, “The Clinical,<br />
biochemical, operative and pathological analysis of<br />
14 cases of primary hyperparathyroidism”, by Lillian<br />
Haddock, Julián Vázquez Plard, Franciso Aguiló,<br />
María <strong>de</strong>l C. Vázquez, Francisco L. Raffucci and<br />
Juan Velázquez (3). They reported 14 patients, 8<br />
males and 6 females. Their age ranged from 16 to<br />
67 years. The pathology revealed 12 a<strong>de</strong>nomas,<br />
one carcinoma and one mediastinal lesion. The latter<br />
patient died from bilateral pneumothorax. For<br />
such a small series it was rare to have one carcinoma<br />
and one mediastinal lesion, both of which<br />
have very low in inci<strong>de</strong>nce.<br />
I did my first operation for hyperpara-thyroidism<br />
in September 1970. The patient was a 41 year old<br />
female with bone pains, repeated urinary infections,<br />
burning sensation on the eyes and constipation. The<br />
x-rays revealed nephrocalcinosis and a pelvic bone<br />
cyst. The neck was explored on September 21,<br />
1970. No neck lesions were found. A large lower<br />
neck and mediastinal mass was found that required<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
Figure 7: Photo of the Lebsche sternal chisel<br />
55<br />
a median sternotomy for its removal. A large 12 x<br />
5 x 3 mass, weighing 113.3 grams, was removed.<br />
It is the second largest parathyroid a<strong>de</strong>noma ever<br />
reported in the medical literature. The following<br />
table shows the parathyroid a<strong>de</strong>nomas weighing<br />
over 50 grams reported in the medical literature.<br />
This is the instrument used to do the sternotomy<br />
on this patient (see Figure 7). At that time we<br />
did not have the electric saw used nowadays for<br />
median sternotomies.<br />
The patient is alive after 36 years; she is now<br />
77 years old. Her calcium is 10-10.3 mgs/dl, PTH<br />
72.8 pg/ml. Her serum creatinine is elevated, 1.8<br />
mgs/dl and her creatinine clearance is low, 24.93<br />
ml/min. She has no kidney stones and continues<br />
to work (see Figure 8).
56<br />
More cases of hyperparathyroidism were diagnosed<br />
following the <strong>de</strong>termination of serum calcium<br />
levels in the SMA23 test, now known as Comprehensive<br />
Metabolic Profile, PTH measurements introduced<br />
in the 1970’s and the utilization of localization<br />
tests to aid the surgeon during the operative<br />
procedure.<br />
The localization tests utilized at different times<br />
during the history of this disease are:<br />
Toluidine blue<br />
Thyroid lymphography<br />
Seleno-methionine<br />
PTH <strong>de</strong>termination with massage<br />
Barium swallow<br />
Thallium-technetium substraction saca<br />
Ultrasonography<br />
CT scanning<br />
Nuclear magnetic resonance<br />
Arteriography<br />
Selective cannulation of neck veins for<br />
PTH levels<br />
Sestamibi parathyroid scan<br />
Parathyroid scan with SPECT<br />
Some of these tests are no longer used.<br />
Since the first article published in 1970, the<br />
following articles have been published:<br />
1. Localization of Parathyroid Lesions: Blind<br />
study for Surgeons in 1989 (4). Fifteen<br />
consecutive patients with hyperparathyroidism<br />
were studied by the Endocrine Section<br />
of the University Hospital in Rio<br />
Piedras, P.R. The results were unknown<br />
to the surgeon and the resi<strong>de</strong>nt. The endocrinology<br />
fellow was present at the operating<br />
room with the localization studies<br />
results. In all 15 patients an a<strong>de</strong>noma was<br />
i<strong>de</strong>ntified and removed. Only four parathyroid<br />
a<strong>de</strong>nomas were i<strong>de</strong>ntified by CT scan.<br />
The Thallium-technetium substraction scan<br />
i<strong>de</strong>ntified 7 of the 15 affected glands. It<br />
was conclu<strong>de</strong>d that the utilization of those<br />
two localizing tests were not indicated at<br />
the initial parathyroid gland surgery.<br />
2. Unusual Cases of Hyperparathyroidism (5)<br />
published in September, 1995. This publication<br />
<strong>de</strong>scribes patients with parathyroid<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 8: Photo of AVC and her surgeon -<br />
<strong>Feb</strong>ruary 2008.<br />
carcinoma, a large mediastinal a<strong>de</strong>noma,<br />
reoperation for hyperplasia 20 years after<br />
the first operation, advanced bone disease<br />
and tertiary hyperparathyroidism secondary<br />
to hypophosphatemic rickets.<br />
3. Surgical Management of Hyperparathyroidism:<br />
a 24 Year Experience, (6) published in<br />
September, 1995. A total of 130 patients<br />
from 1971-1994 were inclu<strong>de</strong>d. Females<br />
predominated. The average age was 56.7<br />
years ranging from 18-83 years. Renal lithiasis<br />
and bone changes were seen in 66.6%<br />
of the patients and 28.1% were asymptomatic.<br />
A<strong>de</strong>nomas were seen in 93.1%, hyperplasia,<br />
5.4%, one carcinoma and 9.2% had<br />
associated thyroid lesions. No patient died<br />
as the result of the operations.<br />
4. Radiologic Manifestations of Hyperparathyroidism<br />
(7) published in September, 1995.<br />
5. Parathyroid Carcinoma: Diagnosis and Management<br />
(8) published in November 1997.<br />
The criteria for malignancy are: invasion of<br />
surrounding tissues, capsular invasion, <strong>de</strong>nse<br />
fibrous septa, vascular or lymphatic metastasis,<br />
presence of mitotic figures and visceral<br />
metastasis (see Figure 9).<br />
6. Clinical Profile of 128 Subjects Operated for<br />
Primary Hyperparathyroidism (9) published<br />
in 1998.<br />
7. A total of 128 patients are inclu<strong>de</strong>d, females<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 9: Sli<strong>de</strong> of Barium swallow, gross pathology, microscopic examination.<br />
predominate. Only 7% were asymptomatic.<br />
Single a<strong>de</strong>nomas were seen in 73.8%, 14.2<br />
hyperplasia, four multiple a<strong>de</strong>nomas, two carcinomas<br />
and two mediastinal a<strong>de</strong>nomas. The<br />
cure rate was 93%. There were two <strong>de</strong>aths,<br />
one from bilateral pneumothorax and one<br />
from respiratory failure.<br />
8. Parathyroid Surgery without Instant PTH or<br />
Radiogui<strong>de</strong>d Sestamibi Scan (10) presented<br />
at Poster Section of the Southeastern Surgical<br />
Congress in <strong>Feb</strong>ruary 2007. Fifty two<br />
patients with primary hyperparathyroidism,<br />
50 are normocalcemic and with normal PTH,<br />
for a success rate of 96%. Eleven patients<br />
had associated thyroid conditions, including<br />
three papillary carcinomas.<br />
9. Dr. William Mén<strong>de</strong>z-Latalladi presented a paper<br />
at the Western Surgical Association meeting<br />
in 2007. The paper was entitled Long<br />
Term Outcome of Patients with Elevated PTH<br />
following Intraoperative Parathormone<br />
Gui<strong>de</strong>d Parathyroi<strong>de</strong>c-tomy (11). Five hundred<br />
twenty two patients operated at the<br />
University Of Miami School Of Medicine<br />
were followed for 43 months. They had a<br />
97% success rate and 505 patients remained<br />
with normal calcium and PTH levels. Thirty<br />
three percent (107) <strong>de</strong>veloped elevated PTH<br />
levels and of these 7% had recurrent hyper-<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
57<br />
parathyroidism warranting reoperation.<br />
In <strong>Puerto</strong> <strong>Rico</strong>, no hospital has the<br />
capability of doing instant PTH measurements<br />
and in only two hospitals the Sestamibi<br />
radioactive gui<strong>de</strong>d probe is utilized.<br />
Since 1970 to early 2008, I have<br />
operated 583 patients with hyperparathyroidism.<br />
The following are some<br />
Sestamibi Scans showing few mediastinal<br />
lesions among this group of patients (see<br />
next page, Figure 10).<br />
The NIH Consensus Conference in 1990 established<br />
the indications for surgery in hyperparathyroidism<br />
as follows:<br />
1. Serum calcium above 1-1.5 mgs/dl above<br />
the normal values.<br />
2. Urinary calcium above 400 mgs/24hours.<br />
3. Creatinine Clearance reduced by 30%.<br />
4. Bone <strong>de</strong>nsity below 2 standard <strong>de</strong>viations<br />
of normal.<br />
5. Patients un<strong>de</strong>r 50 years of age.<br />
6. <strong>Medica</strong>l Surveillance not possible.<br />
These indications were revised in another meeting<br />
in April 2002 to inclu<strong>de</strong> asymptomatic patients<br />
and only minor changes were ma<strong>de</strong>.<br />
The surgeon who performed the first parathyroid<br />
operation in <strong>Puerto</strong> <strong>Rico</strong> was Dr. Francisco L.<br />
Raffucci. This is the pathology report of the lesion
58<br />
Figure 10: Sestamibi scans.<br />
removed from a 65 year old female on May 17,<br />
1960 (see Figure 11). The pathology was interpreted<br />
by Dr. Enrique Koppisch.<br />
The first of the initial group of patients operated<br />
at the <strong>Puerto</strong> <strong>Rico</strong> <strong>Medica</strong>l Center was a<br />
60 year old male patient whose serum calcium<br />
fluctuated between 12.9-15mgs/dl. A left lower<br />
parathyroid a<strong>de</strong>noma was removed somewhere<br />
after June 1960, measuring 4x3cm and weighing<br />
12 grams. He <strong>de</strong>veloped tetany postoperatively<br />
but was treated and recovered. The pathology<br />
revealed a chief cell a<strong>de</strong>noma. He was also<br />
operated by Dr. Raffucci.<br />
Two of the authors of the first publication on<br />
hyperparathyroidism suffered the disease and un<strong>de</strong>rwent<br />
surgery in March and September 2004.<br />
Hyperparathyroidism is an enigmatic or perplexing<br />
disease. Generally, we have four parathyroid<br />
glands, an unknown external stimulus makes<br />
one of the glands to produce an excess parathyroid<br />
hormone. Single a<strong>de</strong>noma is the most frequent<br />
pathological finding, double a<strong>de</strong>nomas are<br />
very rare and recurrent disease is also rare.<br />
Normocalcemic hyperparathyroidism has been<br />
reported as well as patients with non-functioning<br />
parathyroid a<strong>de</strong>nomas. Why the external<br />
stimulus does not repeat itself more frequently<br />
in the remaining three glands to produce recurrent<br />
hyperparathyroidism in a higher percent of<br />
cases? What is the stimulus for hyperplasia when<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
all the four glands are affected? Is the stimulus<br />
different from that producing an a<strong>de</strong>noma?<br />
Humbleness:<br />
We surgeons ought to have:<br />
Intellectual and technical ability<br />
Correct diagnosis<br />
Surgical assistance<br />
Peace of mind<br />
Altruism<br />
Empathy<br />
Spirituality<br />
And remember, there is always someone who<br />
knows more than you do: another surgeon or…The<br />
Chief of the <strong>Medica</strong>l Staff (see Figure 12).<br />
I leave you with a quotation by the late Dr.<br />
Gumersindo Blanco: “In life there is only chance,<br />
change and <strong>de</strong>ath”.<br />
ACKNOWLEDGMENTS:<br />
Dr. Sylvia Barceló, Director of the Outpatient<br />
Clinics at the <strong>Puerto</strong> <strong>Rico</strong> <strong>Medica</strong>l Center, and<br />
Mrs. Lisandra Brenes Torres, Manager of the<br />
Health Information Division of the <strong>Medica</strong>l Center,<br />
who <strong>de</strong>voted their time and effort in trying<br />
to retrieve the old records of the first patients<br />
who suffered this disease.<br />
RESUMEN<br />
Se presenta la historia <strong>de</strong>l <strong>de</strong>scu-brimiento<br />
<strong>de</strong> las glándulas paratiroi<strong>de</strong>s y <strong>de</strong> la enfermedad<br />
<strong>de</strong> hiperparatiroidismo a nivel mundial. Se<br />
<strong>de</strong>scriben los síntomas, la operación y los<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 11: Raffucci operative report.<br />
Figure 12: Chief of medical staff.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
59<br />
hallazgos patológicos <strong>de</strong>l primer paciente<br />
operado <strong>de</strong> hiper-paratiroidismo en Viena, Austria<br />
en el 1925. Luego se mencionan los otros<br />
dos pacientes más famosos que tuvieron<br />
hiperparatiroidismo en Estados Unidos. A lo<br />
largo <strong>de</strong>l artículo se indica la participación <strong>de</strong><br />
varios estudiantes <strong>de</strong> medicina que aportaron<br />
gran<strong>de</strong>s conocimientos a esta enfermedad.<br />
Luego a nivel local se indica quién fue el cirujano<br />
que operó el primer paciente con<br />
hiperparatiroidismo primario en <strong>Puerto</strong> <strong>Rico</strong> en<br />
el 1960. Se señalan las indicaciones para operar<br />
a estos pacientes, al igual que las pruebas<br />
utilizadas para i<strong>de</strong>ntificar las glándulas afectadas.<br />
Se discuten los síntomas <strong>de</strong>l primer paciente<br />
operado por el autor en el 1970. Se resumen<br />
las publicaciones sobre este tema en <strong>Puerto</strong> <strong>Rico</strong><br />
y la experiencia <strong>de</strong>l autor <strong>de</strong>s<strong>de</strong> el 1970 tratando<br />
pacientes con hiperparatiroidismo. Finalmente,<br />
se plantean unas aseveraciones sobre lo<br />
enigmático <strong>de</strong> esta enfermedad.
60<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
REFERENCES<br />
1. DuBose J., Ragsdale T., Morvant J. “Bodies So Tiny”: The History of Parathyroid Surgery, Current Surgery Vol 62/Number 1 January/<br />
<strong>Feb</strong>ruary 2005 Pag. 91-95<br />
2. Organ, C.H. The History of Parathyroid Surgery J Am Coll Surg 191:284-299<br />
3. Haddock L., Vázquez Plard J., Aguiló F., Vázquez María <strong>de</strong>l C., Raffucci FJ., Velázquez J. The Clinical, Biochemical, Operative and<br />
Pathological Análisis of 14 Cases with Primary Hyperparathyroidism Bol. Asoc. Med PR Vol 62 Number 3, Pages 76085, March 1970.<br />
4. Vázquez-Quintana, E., Quintana, C., Aguiló F., Pagán Sáez H., Silva F., Localization of Parathyroid Lesions: Blind Study for Surgeons<br />
Bol. Asoc. Med PR Vol. 81:343-344 Sept. 1989<br />
5. Vázquez-Quintana, E., Haddock, L., Aguiló, F., Sotomayor, R., Ramírez, M., Vázquez-Plard, J., Rabell, V., Pagán-Sáez, H. Unusual<br />
Cases of Hyperparathyroidism <strong>Puerto</strong> <strong>Rico</strong> Health Sciences Journal Vol. 14, No.3, September 1995<br />
6. Vázquez-Quintana, E. Surgical Management of Hyperparathyroidism: a 24 Year Experience Bol Asoc. Med PR Vol. 87, No. 7-8-9 July-<br />
September 1995<br />
7. Vázquez-Quintana, E., Pagán Sáez, H.,Bayrón Vélez, F., <strong>de</strong> Jesús, M. Radiologic Manifestations of Hyperparathyroidism Bol. Asoc. Med.<br />
PR Vol. 87 July- Sept. 1995<br />
8. Vázquez-Quintana, D. Parathyroid Carcinoma: Diagnosis and Management- The American Surgeon Vol. 63, No.11. Pag .954-957,<br />
November 1996.<br />
9. Haddock, L., Aguiló, F., Vázquez-Quintana, E., Vázquez, María <strong>de</strong>l C., Rabell, V., Allen<strong>de</strong>, M. Clinical Profile of 128 Subjects Operated<br />
for Primary Hyperparathyroidism <strong>Puerto</strong> <strong>Rico</strong> Health Sciences Journal Vol.17, No. 4, Pag. 309-316 Dec. 1998<br />
10. Vázquez-Quintana, E., Vázquez-Torres, DE., Parathyroid Surgery Without Instant PTH or Radiogui<strong>de</strong>d Sestamici Scan Submitted for publication<br />
11. Mén<strong>de</strong>z-Latalladi, W., et al. Long Term Outcome of Patients with Elevated PTH following Intraoperative Parathyroid Hormone Gui<strong>de</strong>d<br />
Parathyroi<strong>de</strong>ctomy Submitted for publication.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
61<br />
Artículos <strong>de</strong> Repaso • Review Articles<br />
28 TH F.L. RAFFUCCI RESEARCH FORUM ABSTRACTS<br />
<strong>Feb</strong>ruary 21, 2008, La Concha Hotel, San Juan, <strong>Puerto</strong> <strong>Rico</strong><br />
1. Results of the Malpractice Survey in<br />
San Juan<br />
By: Norma I. Cruz, M.D., <strong>Puerto</strong> <strong>Rico</strong> College of Physicians<br />
and Surgeons, District of San Juan<br />
Introduction: The current medical liability insurance<br />
crisis has changed the way medicine and<br />
surgery are practiced. To evaluate the extent of<br />
these changes and the frequency of malpractice<br />
claims in our community, the District of San Juan<br />
of the <strong>Puerto</strong> <strong>Rico</strong> College of Physicians and Surgeons<br />
performed a survey.<br />
Method: A questionnaire, consisting of 15<br />
items which evaluated medical liability, was mailed<br />
to all physicians in the San Juan District. The questionnaire<br />
requested information on basic <strong>de</strong>mographics,<br />
medical specialty, insurance company<br />
used, annual premium paid, umbrella coverage,<br />
changes ma<strong>de</strong> in their medical practices to <strong>de</strong>crease<br />
medical liability risk, malpractice claims received<br />
during the last ten years, and if awards exceeding<br />
insurance coverage were paid. Physicians were<br />
requested to return the completed questionnaires<br />
by FAX or mail to the main office of the <strong>Puerto</strong><br />
<strong>Rico</strong> College of Physicians and Surgeons. The questionnaires<br />
were mailed in October 2006 and replies<br />
were received up to the end of January 2007 (a three<br />
month period). All information received was analyzed<br />
using the computerized statistical program SPSS (Statistical<br />
Package for the Social Sciences).<br />
Results: A total of 432 completed questionnaires<br />
were returned. Since the region has 3,558<br />
physicians on the mailing list, 12% of the group<br />
participated in the survey. The mean age of the<br />
respon<strong>de</strong>rs was 51± 13 and 72% were males. The<br />
mean time in practice was 21 years and 86% were<br />
specialists. The main professional liability insurance<br />
carrier was SIMED (82%) followed by Triple S<br />
(12%). Umbrella coverage, in addition to basic liability<br />
insurance, was carried by only 11% of the<br />
respon<strong>de</strong>rs. Changes in their medical practices to<br />
<strong>de</strong>crease medical liability risk had been ma<strong>de</strong> by<br />
76% of the physicians. Currently, 59% of physicians<br />
do not accept emergency cases and 72% do<br />
not accept high risk patients. If we add the respon<strong>de</strong>rs<br />
that indicated that they plan to “close their<br />
office”, “leave <strong>Puerto</strong> <strong>Rico</strong>”, or “retire” it appears<br />
that <strong>Puerto</strong> <strong>Rico</strong> would lose 63% of its medical<br />
manpower. Malpractice claims were received at<br />
least once in the previous ten years by 44% of the<br />
physicians. The awards requested by these claims excee<strong>de</strong>d<br />
the insurance coverage 79% of the time. However,<br />
after the final court <strong>de</strong>cision was reached, only 28%<br />
of the payments excee<strong>de</strong>d the insurance coverage.<br />
Conclusion: The medical liability crisis has<br />
affected the majority of physicians in San Juan, leading<br />
76% of them to make changes in their practices<br />
to <strong>de</strong>crease the risk. As a result of these<br />
changes, the number of physicians willing to care<br />
for high risk and emergency patients has <strong>de</strong>creased<br />
significantly. The problem is compoun<strong>de</strong>d by malpractice<br />
awards that exceed a physician’s insurance<br />
coverage 28% of the time.
62<br />
2. Role of Surgeon-Performed Ultrasound<br />
in Predicting Malignancy in Patients with<br />
In<strong>de</strong>terminate Thyroid Nodules<br />
By: William Mén<strong>de</strong>z-Latalladi, M.D., John I. Lew, M.D.,<br />
Steven Rodgers, M.D., George I. Irvin, M.D. and Carmen C.<br />
Solorzano, M.D., Dept of Surgery, Med. School, UPR, Div. of<br />
Endocrine Surgery, Dept. of Surgery, Univ. of Miami-Miller<br />
School of Medicine, Miami, Fl<br />
Introduction: Certain ultrasound features can<br />
predict malignancy in patients with thyroid nodules.<br />
The purpose of this study was to <strong>de</strong>termine the value<br />
of office based surgeon-performed ultrasound (SUS)<br />
in predicting thyroid nodule malignancy in patients with<br />
in<strong>de</strong>terminate fine needle aspiration (FNA) cytology.<br />
Method: From 2002 to 2007, 477 consecutive<br />
patients un<strong>de</strong>rwent FNA of dominant thyroid nodules.<br />
Of these patients 180/477 (38%) were judged to have<br />
in<strong>de</strong>terminate FNA: follicular neoplasm (FN, n=108),<br />
Hurthle cell neoplasm (HN, n=29) and “suspicious<br />
papillary thyroid cancer” (SPTC, n=43). SUS-characteristics<br />
for thyroid nodules were recor<strong>de</strong>d prior to thyroi<strong>de</strong>ctomy<br />
and entered into a prospective database.<br />
Data points analyzed inclu<strong>de</strong>d patient’s age and sex,<br />
nodule size, shape, echogenicity, consistency (solid/<br />
cystic), bor<strong>de</strong>rs, multiplicity/multi-centricity and presence<br />
of microcalcifications. Features of thyroid nodules<br />
were compared to final pathology. Univariate and<br />
multivariate analyses were performed. The accuracy<br />
of individual SUS features as well as the presence of 2<br />
or more adverse features in predicting malignancy was<br />
also examined.<br />
Results: There were 144 females and 36<br />
males. The mean age was 52 years (17-87). The<br />
mean tumor size was 2.7cm (0.65-6.6). Overall,<br />
final pathology revealed cancer in 91/180 (50%)<br />
patients. Malignancy was present in 40/108 (37%)<br />
FN, 11/29 (38%) HN, and 40/43 (93%) SPTC.<br />
On univariate analysis, the presence of<br />
microcalcifications correlated highly with malignancy<br />
with a specificity, positive predictive value<br />
(PPV), and accuracy of 81%, 75%, and 70%, respectively.<br />
On multivariate analysis, solid nodules,<br />
shape (taller>wi<strong>de</strong>r), hypoechogenicity and presence<br />
of microcalcifications were significantly associated<br />
with malignancy (p
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
cancer in this population. When compared by HI,<br />
diabetes increases the occurrence of breast cancer<br />
5.7 times in the public compared to 2.9 in the private<br />
HI. These findings suggest that diabetes is associated<br />
with breast cancer, especially in the public<br />
HI population.<br />
Conclusion: Diabetes increases the occurrence<br />
of breast cancer 4.5 times in the <strong>Puerto</strong> Rican population<br />
evaluated. Further studies will analyze clinical<br />
and economic factors that might contribute to<br />
this difference.<br />
4. The Role of Non-Invasive Imaging<br />
Studies in the Diagnosis of Right Blunt<br />
Diaphragmatic Rupture: A Case Series and<br />
Review of Literature<br />
By: Suhein D. Galloza, M.D., Pablo Rodriguez, M.D., Quirico<br />
Canario, M.D., Emmanuel Agosto, B.SE, Gori Ballester, M.D.,<br />
Wilma Rodríguez, M.D. and Fernando Joglar, M.D., <strong>Puerto</strong><br />
<strong>Rico</strong> Trauma Center and Dept. of Surgery, UPR<br />
Introduction: Diaphragmatic injuries represent<br />
approximately 0.8-5% of blunt chest and abdominal<br />
trauma. The diagnosis is frequently missed or<br />
<strong>de</strong>layed in the acute phase because they present<br />
with variable clinical and radiological signs. A misdiagnosis<br />
represents a risk for complications (e.g.<br />
organ herniation), consequently increasing morbidity<br />
and mortality. A high in<strong>de</strong>x of suspicion and<br />
an aggressive search should continue in patients<br />
at risk, especially those that have failed to<br />
progress clinically.<br />
Objective: To evaluate current diagnostic modalities<br />
for the diagnosis of right diaphragmatic rupture<br />
in blunt trauma patients in an effort to improve<br />
early i<strong>de</strong>ntification of this injury.<br />
Method: A retrospective chart review of all the<br />
cases of right traumatic diaphragmatic rupture admitted<br />
to the <strong>Puerto</strong> <strong>Rico</strong> Trauma Center between<br />
November 2006 and July 2007 was performed. In<br />
this study a retrospective analysis of the chest radiograph<br />
(CXR), ultrasound, and computed tomography<br />
(CT scan) were performed to evaluate the<br />
possibility of unnoticed injuries, and to note any sign<br />
that might be helpful in the assessment of future<br />
cases. The images were reviewed by a trauma attending<br />
and a senior level radiology resi<strong>de</strong>nt for signs<br />
that were suggestive of right diaphragmatic rupture.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
63<br />
Results: During the study period a total of<br />
1,185 patients were admitted to the <strong>Puerto</strong> <strong>Rico</strong><br />
Trauma Center. From this population of patients<br />
873 (73.9%) were admitted due to blunt injuries,<br />
and 252 (21.3%) due to penetrating injuries. Blunt<br />
diaphragmatic rupture was diagnosed in 8 patients<br />
(0.92%). Right traumatic diaphragmatic rupture<br />
secondary to severe blunt trauma resulting from<br />
motor vehicle acci<strong>de</strong>nts was i<strong>de</strong>ntified in two females<br />
and one male ranging in age from 46-62,<br />
representing 0.3 % of the admissions during the<br />
study period.<br />
Retrospective review of the initial CXRs and<br />
CT scans failed to <strong>de</strong>monstrate signs suggestive<br />
of diaphragmatic rupture. The right upper quadrant<br />
view of the Focused Abdominal Sonography<br />
for Trauma (FAST) showed a diaphragmatic discontinuity<br />
that was suggestive of a rupture of the<br />
right hemidiaphragm during the initial assessment<br />
of one case. All of the cases presented with refractory<br />
hemothorax and pleural effusions <strong>de</strong>spite<br />
chest tube drainage. Initial studies did not i<strong>de</strong>ntify<br />
the diaphragmatic injuries and a vi<strong>de</strong>o-assisted<br />
thoracoscopy failed to i<strong>de</strong>ntify the injury<br />
in one of the cases. In terms of follow-up imaging<br />
studies after the admission, the CXR of case<br />
1 showed elevation of the right hemidiaphragm;<br />
the CT scan of case 3 <strong>de</strong>monstrated the liver<br />
herniating into the right thoracic cavity, and an<br />
ultrasound confirmed discontinuity of the right<br />
hemidiaphragm. Fluoroscopy was used for case<br />
2 preoperatively, <strong>de</strong>monstrating abnormal diaphragmatic<br />
motion.<br />
Conclusion: The use of the ultrasound can be<br />
a valuable tool for the evaluation of the diaphragm<br />
in addition to the CXR and CT scan. The diaphragmatic<br />
discontinuity observed by ultrasound was the<br />
key sign that raised the suspicion of a right diaphragmatic<br />
rupture. Neither the CXR nor the CT<br />
scans were suggestive of a right diaphragmatic rupture<br />
at the initial evaluation. The fluoroscopy was<br />
a helpful alternative that suggested a diaphragmatic<br />
rupture; however, this is not always a feasible test.<br />
Sequential films and additional studies were nee<strong>de</strong>d<br />
in or<strong>de</strong>r to diagnose the diaphragmatic rupture.<br />
Further prospective studies are nee<strong>de</strong>d to provi<strong>de</strong><br />
a concrete conclusion.
64<br />
5. Carotid Endarterectomy Un<strong>de</strong>r Regional<br />
Anesthesia: Our Experience at the <strong>Puerto</strong><br />
<strong>Rico</strong> Veterans’ Administration Hospital<br />
By: Luis Rodriguez-Escolá, M.D., Gustavo De Jesús-Gómez, M.D.,<br />
Carlos Calimano-Guardiola, M.D., Norma Santiago-Rivera, M.D.<br />
and Ernesto Rivé-Mora, M.D., Vascular Surgery, VA.<br />
Introduction: Endarterectomy is the standard<br />
treatment for symptomatic and critical carotid artery<br />
stenotic lesions. Controversies persist on many technical<br />
issues, one of which is general versus regional<br />
anesthesia. We present our experience with Carotid<br />
Endarterectomy (CAE) un<strong>de</strong>r regional anesthesia.<br />
Method: This is a <strong>de</strong>scriptive study on a retrospective<br />
analysis of all patients who un<strong>de</strong>rwent CAE<br />
in the <strong>Puerto</strong> <strong>Rico</strong> Veterans’ Administration <strong>Medica</strong>l<br />
Center from 2005-2007. All pertinent data was recovered<br />
from the Computerized Patient Record System<br />
(CPRS electronic patient record system).<br />
Results: The patient population for the study<br />
period consists of a total of 50 subjects. Demographic<br />
information did not vary significantly among studied<br />
individuals. A significant amount of comorbid conditions<br />
were encountered, among which hypertension<br />
and diabetes were most common. The mean age for<br />
our study population was 70 years with an age range<br />
between 65 and 95 years. The indication for endarterectomy<br />
was evenly distributed among symptomatic<br />
and asymptomatic lesions. All procedures were completed<br />
un<strong>de</strong>r regional / local anesthesia. All procedures<br />
were performed by the same Vascular Surgeon<br />
and a General Surgery senior resi<strong>de</strong>nt. Average operative<br />
time was 135 minutes, ranging from 75 min<br />
to 150 min. Mean length of stay was 2 days. All<br />
patients were followed-up at clinics for a minimum of<br />
2 weeks post surgery. So far, during this time period,<br />
we have not encountered any complications.<br />
Conclusions: We hope to provi<strong>de</strong> additional evi<strong>de</strong>nce<br />
that Carotid Endarterectomy un<strong>de</strong>r Regional<br />
Anesthesia is safe and appealing. This investigation is<br />
ongoing, final results are not yet available.<br />
6. Pediatric Brain Tumors in <strong>Puerto</strong> <strong>Rico</strong><br />
By: Manuel F Saavedra M.D., Juan Vigo Prieto, M.D., Iván<br />
Sosa, M.D., Lincoln Jiménez, M.D. and Indira De Jesús Alvelo,<br />
M.D., Division of Neurosurgery, Pediatric Hospital PRMC, UPR<br />
Introduction: Brain tumors are the second<br />
most common malignancy among children and<br />
the most common form of solid tumor. We have<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
studied the inci<strong>de</strong>nce and important characteristics<br />
of pediatric brain tumors in our population.<br />
Data was collected from the Pediatric Hospital<br />
at the <strong>Puerto</strong> <strong>Rico</strong> <strong>Medica</strong>l Center which is the<br />
only full time Neurosurgical Pediatric Center in<br />
the Island and provi<strong>de</strong>s this service for our current<br />
population.<br />
Method: We collected data retrospectively,<br />
during 5 and _ year period from January 2002 to<br />
July 2007. The information was reviewed from the<br />
Neurosurgical Procedures Data Base and the <strong>Medica</strong>l<br />
Records of the University Pediatric Hospital of<br />
<strong>Puerto</strong> <strong>Rico</strong> <strong>Medica</strong>l Center. We inclu<strong>de</strong>d all pediatric<br />
neurosurgical procedures for brain tumors and<br />
exclu<strong>de</strong>d recurrent tumors, spinal tumors and other<br />
scalp and skull tumors. Data was analyzed and compared<br />
with current literature.<br />
Results: The inci<strong>de</strong>nce rate for pediatric brain<br />
tumors was 1.99/100,000 child per year. Patients<br />
most commonly involved were between the ages of<br />
9 to 19 years old, male more affected than female<br />
and the Supratentorial region the most common<br />
affected area. By far the most common single tumor<br />
was the Pilocytic Astrocytoma WHO I representing<br />
30% of the total cases.<br />
Conclusion: The inci<strong>de</strong>nce rates for pediatric<br />
brain tumors in <strong>Puerto</strong> <strong>Rico</strong> are somehow different<br />
from current literature, supratentorial tumors were<br />
more common in this population. The variable of<br />
Hispanic Population may have a role on this issue.<br />
Further studies need to be conducted.<br />
7. Surgical Inci<strong>de</strong>nce of Central Nervous<br />
System Tumors in <strong>Puerto</strong> <strong>Rico</strong><br />
By: Gisela Murray, M.D. Lincoln Jimenez, M.D., Frankie Báez,<br />
M.D., Liliam Colón, M.D, and Ricardo H. Brau, M.D., Section<br />
of Neurosurgery and Dept. of Pathology, Med. School, UPR<br />
Introduction: Published studies regarding the<br />
inci<strong>de</strong>nce of central nervous system (CNS) tumors in<br />
<strong>Puerto</strong> <strong>Rico</strong> are exceedingly rare. The general un<strong>de</strong>rstanding<br />
is that the inci<strong>de</strong>nce of these tumors in <strong>Puerto</strong><br />
<strong>Rico</strong> is similar to the one found in the United States.<br />
The objective of this study is to <strong>de</strong>scribe the specific<br />
profile of all the CNS tumors that are surgically intervened<br />
in <strong>Puerto</strong> <strong>Rico</strong>. To the best of our knowledge,<br />
this is the first study of its kind in <strong>Puerto</strong> <strong>Rico</strong>.<br />
Method: A retrospective analysis of all the surgical<br />
procedures from January 1, 2002 to May 31, 2006<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
for adult CNS tumors in <strong>Puerto</strong> <strong>Rico</strong> was performed.<br />
Each case was evaluated for <strong>de</strong>mographic information,<br />
operative procedure, lesion <strong>de</strong>scription and official<br />
pathological report. Recurrent lesions were exclu<strong>de</strong>d.<br />
The information was organized to form a database<br />
of all the CNS neoplasms.<br />
Results: A total of 1,018 procedures for CNS<br />
tumors were performed on 1,005 patients. The<br />
inci<strong>de</strong>nce rate of CNS tumors in <strong>Puerto</strong> <strong>Rico</strong> is 6.7<br />
per 100,000 people. The most common histological<br />
type found was Meningioma WHO I (24%), followed<br />
by pituitary a<strong>de</strong>nomas (16%), and Glioblastoma<br />
Multiforme (14%). Among the spinal cord tumors,<br />
Schwannomas were the most frequent (20%).<br />
Conclusion: Our results reflect a unique histopathological<br />
distribution of CNS tumors in <strong>Puerto</strong> <strong>Rico</strong>.<br />
In our series, primary tumors are more common than<br />
metastatic tumors. Benign histological tumors were<br />
more frequent than more malignant variants. Although<br />
this study reflects only the histologically diagnosed tumors,<br />
it is headway towards diagnosing the exact inci<strong>de</strong>nce<br />
of CNS tumors in <strong>Puerto</strong> <strong>Rico</strong>.<br />
8. Distal Fragmented Port Catheter: Case<br />
Report and Review of Literature<br />
By: Norman E. Colón-Casasnovas, MS3 and Humberto Lugo-<br />
Vicente, M.D., Section of Pediatric Surgery, Dept. of Surgery,<br />
Med. School, UPR<br />
Introduction: Insertion of long-term central<br />
venous catheters (CVC) plays a vital role in providing<br />
continuous venous access for therapy in children.<br />
CVC line fractures are most commonly seen<br />
after long-term periods of therapy during removal.<br />
Usual place of rupture is proximal, at the point of<br />
entrance of the catheter into the vein, when the<br />
subclavian approach is utilized. We discuss a case<br />
that shows that CVC can also fracture in places<br />
different than the most common location and is<br />
possible not to <strong>de</strong>tect that a fracture has occurred<br />
if a substantial portion of catheter is removed.<br />
Method: We report a two-year-old child that<br />
was inci<strong>de</strong>ntally found to have a distal fragmented<br />
piece of CVC left after previous “successful” removal<br />
on simple chest films. At time of removal the catheter<br />
length was <strong>de</strong>emed properly. A CT Scan confirmed<br />
the suspected diagnosis. Fragment of catheter<br />
was successfully removed via femoral percutaneous<br />
endovascular technique.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
65<br />
Results: CVC fractures can be suspected when<br />
there is resistance during removal or the length retrieved<br />
is too short. In this case the ease of retrieval<br />
and unusual site of rupture was the cause of not<br />
noticing that a part of catheter remained fixed to<br />
the vessel wall. Different potential mechanisms of<br />
CVC rupture inclu<strong>de</strong> mechanical trauma, manufacturing<br />
<strong>de</strong>fect or material <strong>de</strong>gradation. Ruptures<br />
should be <strong>de</strong>tected early to prevent complications<br />
such as sepsis, endocarditis, thrombosis, embolization,<br />
vessel stenosis and dysrhythmia. Best method<br />
to remove the fragmented catheter is via percutaneous<br />
endovascular retrieval method. After catheter<br />
removal a hyper<strong>de</strong>nsity silhouette on a CXR<br />
can mimic the fragmented portion of a catheter<br />
known as a calcified cast or “ghost”. To differentiate<br />
a “ghost” from an actual fragmented portion of<br />
catheter a CT Scan is nee<strong>de</strong>d.<br />
Conclusion: Most important single step in preventing<br />
such complication is to keep record of the<br />
patient length of catheter that was inserted to be able<br />
to measure it after removal confirming it still has the<br />
same length. Fragmented CVC should be removed<br />
using percutaneous endovascular techniques.<br />
9. Tracheostomy Decannulation: A<br />
Retrospective Chart Review<br />
By: Fernando Joglar, M.D., Pablo Rodríguez, M.D., Quirico<br />
Canario, M.D., Guillermo Rivera, MS4, Laura Santos, M.D.,<br />
Marian Báez, M.D., Suhein D. Galloza, M.D. and Ada Lebron,<br />
M.S., Trauma Section, Dept. of Surgery, Med. School, UPR<br />
Introduction: The benefits of tracheostomy in<br />
patients on prolonged mechanical ventilation have<br />
been well <strong>de</strong>scribed. Studies have shown that early<br />
tracheostomy <strong>de</strong>creases the length of stay in the<br />
trauma intensive care unit, vocal cord ulceration and<br />
subglottic inflammation. Of notice is that the majority<br />
of these studies have focused on the timing of<br />
tracheostomy placement, but little has been written<br />
about the <strong>de</strong>cannulation process and the outcomes<br />
of patients after <strong>de</strong>cannulation. We evaluated<br />
the long-term outcomes of tracheostomized<br />
trauma patients after in-hospital <strong>de</strong>cannulation.<br />
Method: A retrospective <strong>de</strong>scriptive chart review<br />
of 160 patients admitted to the Trauma Intensive<br />
Care Unit at the <strong>Puerto</strong> <strong>Rico</strong> Trauma Hospital<br />
over a 28 month period (September 2003-December<br />
2005) who un<strong>de</strong>rwent tracheostomy was con-
66<br />
ducted. Information about <strong>de</strong>mographics, admission,<br />
diagnoses, duration of mechanical ventilation,<br />
cannulation times, complications, and outcomes was<br />
gathered. Follow-up information was obtained from<br />
the speech pathology <strong>de</strong>cannulation protocol registry<br />
of our Trauma Hospital. Chi-square and stu<strong>de</strong>nt<br />
t-test analyses were used to compare and <strong>de</strong>scribe<br />
the groups that <strong>de</strong>veloped complications as<br />
well as the groups that were <strong>de</strong>cannulated early (25 days).<br />
Results: Of the 160 charts reviewed, 26 patients<br />
died and 29 patients were lost to followup.<br />
There were 105 patients inclu<strong>de</strong>d in the<br />
analysis, 92 males and 13 females, with a mean<br />
age of 37 ± 17 years. The mean cannulation time<br />
was 42 ± 61 days (median = 25 days). The majority<br />
of patients were successfully <strong>de</strong>cannulated<br />
during the first 50 days after tracheostomy (82%).<br />
The complications i<strong>de</strong>ntified were swallowing<br />
difficulties (10.5%), hoarseness (9.5%), tracheal<br />
stenosis (1.9%) and granulomas (1.9%). Patients<br />
who <strong>de</strong>veloped swallowing problems had significantly<br />
longer cannulation times compared to the<br />
group that had no complications (p
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
ing. In the United States the estimated age of retirement<br />
for general surgeons is currently higher<br />
than in the past and the number of resi<strong>de</strong>nts that<br />
enter into the general surgery workforce has remained<br />
constant. The potential effect of this trend<br />
might result in a future crisis in the general surgery<br />
workforce. To project the number of general surgeons<br />
that will be active for the next five, ten and<br />
fifteen years and to analyze the potential impact on<br />
the general surgery workforce in <strong>Puerto</strong> <strong>Rico</strong>.<br />
Method: A survey formulary was distributed<br />
among the general surgeons in <strong>Puerto</strong> <strong>Rico</strong>. They<br />
were asked to provi<strong>de</strong> information such as their<br />
expected age of retirement, years in practice, location<br />
of practice, membership in surgical associations,<br />
and availability for emergency <strong>de</strong>partment<br />
calls. They were also asked to classify the types of<br />
surgical procedures done as endocrine,<br />
hepatobiliary, trauma, hernia, transplant,<br />
laparoscopic procedures, vascular, bariatric, burns,<br />
colorectal and oncologic. Statistical analysis was<br />
done on the projected number of general surgeons<br />
that will be active in five, ten and fifteen years. In<br />
addition, the listing of graduates from the University<br />
of <strong>Puerto</strong> <strong>Rico</strong> School of Medicine General<br />
Surgery Resi<strong>de</strong>ncy program for the last eleven years<br />
was reviewed.<br />
Results: A total of 85 surgeons completed and<br />
returned the survey formulary. Seventy-eight (91.8<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
67<br />
%) out of these surgeons have an active practice<br />
status, seven (8.2%) are currently retired. The mean<br />
age of active surgeons is 52.5 (range: 33- 78) years<br />
old. Thirty-four out of the 76 surgeons range from<br />
51- 60 years old, representing 44.7% of the work<br />
force. The average years of practice of active surgeons<br />
is 21.2 (2- 54) years and the average expected<br />
age of retirement is at 64.9 (50- 80) years<br />
old. In five years 10.5% of surgeons will be retired.<br />
Similarly, projections suggest that 31.6% and<br />
56.6% of active surgeons will be retired in 10 and<br />
15 years respectively. Conversely, only 40.4 % (19)<br />
of the 47 general surgeons who graduated from the<br />
University of <strong>Puerto</strong> <strong>Rico</strong> General Surgery Resi<strong>de</strong>ncy<br />
during the last 11 years are actively practicing as general<br />
surgeons, while 51.1 % (24) continued training in<br />
a surgical subspecialty. In addition, 8.5 % (4) of general<br />
surgery graduates have relocated to practice general<br />
surgery in the United States.<br />
Conclusion: The diversion of general surgeons<br />
into subspecialties is creating a potential <strong>de</strong>ficit on the<br />
general surgery workforce in <strong>Puerto</strong> <strong>Rico</strong>. The patient<br />
population is growing and the number of new general<br />
surgeons is <strong>de</strong>creasing. Although the mean age of retirement<br />
has increased for general surgeons, indicating<br />
that surgeons remain in practice longer, this is only<br />
a short term answer to a long term problem. If these<br />
trends continue we will face a worsening crisis of access<br />
to general surgical care.
68<br />
QUESTIONS<br />
1- The best localizing test for patients with hyperparathyroidism<br />
consist of:<br />
a) MRI<br />
b) CT-Scan<br />
c) barium swallow<br />
d) Sestamibi Scan<br />
e) thallium-technetium substraction scans<br />
2- The accuracy of the Sestamibi scan <strong>de</strong>pends on:<br />
a) the concentration of iodine in the thyroid gland<br />
b) the amount of radioactive material injected<br />
c) number of oxyphil cells of the a<strong>de</strong>noma<br />
d) number of follicular cells of the a<strong>de</strong>noma<br />
e) none of the above<br />
3- Hyperparathyroidism causes:<br />
a) hypocalcemia and hyperphospathemia<br />
b) hypernatremia and hypochloremia<br />
c) hypercalcemia and hyperphosphatemia<br />
d) hypercalcemia and hypophosphatemia<br />
e) hyperkalemia and hyponatremia<br />
4- Recommendation for surgery in hyperparathyroidism<br />
inclu<strong>de</strong>s all of the above,<br />
EXCEPT:<br />
a) bone, renal, gastrointestinal, or neuromuscular<br />
symptom<br />
b) calcium level > 11.2-12.0 mg/dL<br />
CME Credits<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Instructions: Answer the questions below, fill in your personal information, cut and send with a check<br />
for $20.00 payable to: <strong>Asociacion</strong> <strong>Medica</strong> <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong>.<br />
To obtain CME four (4) credits AMA 1, you should read the three articles on Parathyroid surgery and be<br />
able to answer four of six questions correctly.<br />
Fill in the following information:<br />
c) renal stones with urine calcium level > 400 mg/d<br />
d) Bone Mass Density T score < 2.5 at any sites<br />
e) normal creatinine clearance<br />
5- The most common pathological hystology<br />
found in hyperparathyroidism is:<br />
a) a<strong>de</strong>noma<br />
b) hyperplasia<br />
c) carcinoma<br />
d) follicular<br />
e) papillary<br />
6) The surgeon that performed the first parathyroid<br />
operation in <strong>Puerto</strong> <strong>Rico</strong> was:<br />
a) Enrique Vázquez Quintana<br />
b) Gumersindo Blanco<br />
c) Enrique Márquez<br />
d) Francisco Raffucci<br />
e) Fernando Noya<br />
ANSWERS<br />
1- (A) (B) (C) (D) (E)<br />
2- (A) (B) (C) (D) (E)<br />
3- (A) (B) (C) (D) (E)<br />
4- (A) (B) (C) (D) (E)<br />
5- (A) (B) (C) (D) (E)<br />
6- (A) (B) (C) (D) (E)<br />
Name _________________________________ License No. ________________<br />
Postal Address ____________________________________________________<br />
Telephone _______________________ Fax ______________________________<br />
Cut along the dotted line and send answers with check to:<br />
Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
PO Box 9387<br />
San Juan, PR 00908-9387<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
70<br />
Informe <strong>de</strong> Casos • Case Reports<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
DISTAL FRAGMENTED PORT CATHETER:<br />
CASE REPORT AND REVIEW OF LITERATURE<br />
By: Norman E. Colón-Casasnovas* and Humberto Lugo-Vicente**<br />
ABSTRACT<br />
Background: Insertion of long-term central<br />
venous catheters (CVC) plays a vital role in providing<br />
continuous venous access for therapy in children.<br />
CVC line fractures are most commonly seen<br />
after long-term periods of therapy during removal.<br />
Usual place of rupture is proximal, at the point of<br />
entrance of the catheter into the vein, when the<br />
subclavian approach is utilized. We discuss a case<br />
that shows that CVC can also fracture in places<br />
different than the most common location and is<br />
possible not to <strong>de</strong>tect that a fracture has occurred<br />
if a substantial portion of catheter is removed.<br />
Method: We report a two-year-old child that<br />
was inci<strong>de</strong>ntally found to have a distal fragmented<br />
piece of CVC left after previous “successful” removal<br />
on simple chest films. At time of removal the catheter<br />
length was <strong>de</strong>emed properly. A CT Scan confirmed<br />
the suspected diagnosis. Fragment of catheter<br />
was successfully removed via femoral percutaneous<br />
endovascular technique.<br />
Results: CVC fractures can be suspected when<br />
there is resistance during removal or the length retrieved<br />
is too short. In this case the ease of retrieval<br />
and unusual site of rupture was the cause of not<br />
noticing that a part of catheter remained fixed to<br />
the vessel wall. Different potential mechanisms of<br />
CVC rupture inclu<strong>de</strong> mechanical trauma, manufac-<br />
turing <strong>de</strong>fect or material <strong>de</strong>gradation. Ruptures<br />
should be <strong>de</strong>tected early to prevent complications<br />
such as sepsis, endocarditis, thrombosis, embolization,<br />
vessel stenosis and dysrhythmia. Best method<br />
to remove the fragmented catheter is via percutaneous<br />
endovascular retrieval method. After catheter<br />
removal a hyper<strong>de</strong>nsity silhouette on a CXR<br />
can mimic the fragmented portion of a catheter<br />
known as a calcified cast or “ghost”. To differentiate<br />
a “ghost” from an actual fragmented portion of<br />
catheter a CT Scan or echocardiogram is nee<strong>de</strong>d.<br />
Conclusion: Most important single step in preventing<br />
such complication is to keep record of the<br />
patient length of catheter that was inserted to be able<br />
to measure it after removal confirming it still has the<br />
same length. Fragmented CVC should be removed<br />
using percutaneous endovascular techniques.<br />
Key words: hemoport, fragmentation,<br />
chemotherapy, complication, distal<br />
INTRODUCTION<br />
Insertion of long-term central venous catheters<br />
plays a vital role in providing continuous venous<br />
access for such therapy as parenteral nutrition, longterm<br />
antibiotics, dialysis and cancer chemo-therapy<br />
in children and adults. 1 Central venous catheter<br />
From the * U.P.R. School of Medicine, and ** Section of Pediatric Surgery, Department of Surgery, U.P.R. School of Medicine. Address reprints:<br />
Humberto Lugo-Vicente MD, PO Box 10426, Caparra Heights Station, San Juan, PR 00922 . Poster presented at the 28 th<br />
Annual Meeting Raffucci Surgical Forum, <strong>Feb</strong>ruary 21, 2008, La Concha Hotel, San Juan, <strong>Puerto</strong> <strong>Rico</strong>.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
(CVC) line fractures are most commonly seen after<br />
long-term periods of therapy during removal of the<br />
indwelling catheter. The usual place of rupture is<br />
proximal, at the point of entrance of the catheter<br />
into the vein, when the subclavian approach is utilized.<br />
This is a well known complication recognized<br />
as the pinch-off syndrome, which is a mechanical<br />
occlusion of the catheter due to a narrowing of the<br />
catheter that occurs as the catheter is compressed<br />
between the first rib and the clavicle. 2 We present a<br />
unique case since the site of fragmentation and rupture<br />
of the catheter occurred at a significantly distal<br />
site making less obvious that a fracture has occurred<br />
since a substantial part of the catheter was properly<br />
removed. The purpose of this case report is to<br />
share our experience and suggest a comprehensive<br />
step by step management plan on how to properly<br />
<strong>de</strong>tect and prevent such situation.<br />
CASE HISTORY<br />
A two-year-old male child with previously diagnosed<br />
acute lymphoblastic leukemia since one year<br />
prior to admission comes to the emergency room<br />
of our institution with fever of one day duration.<br />
Since the patient had been receiving peripheral<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
71<br />
chemotherapy with his last dose applied three days<br />
before the onset of fever, it raised suspicion of a<br />
pneumonic process related to immune suppression.<br />
A simple chest film (CXR) was or<strong>de</strong>red and it showed<br />
a hyper<strong>de</strong>nsity silhouette on superior vena cava and<br />
right atrium suggesting the presence of a fragment<br />
of a previously removed MedPort catheter four<br />
months ago (Figure 1). At that time the catheter,<br />
placed through the left external jugular vein, was<br />
removed because the port had rotated and upon<br />
flushing to see if the lumen was patent no blood<br />
came out. The patient tolerated the procedure well<br />
and the catheter length removed with the port was<br />
<strong>de</strong>emed properly. Patient had this catheter for one<br />
year when chemotherapy was started upon discovery<br />
of his leukemic condition.<br />
In addition, to rule out systemic infections a<br />
urinalysis and blood tests were also or<strong>de</strong>red (WBC<br />
= 6.30 [N 5.0-13.5], HGB = 11.8 [N 10.5-14.5<br />
g/dL], MCV = 77.3 [N 80-96], NEU% = 82.2 [N<br />
16.0-70 %], LYM% = 10.6 [N 20.0-70.0 %]). Urinalysis<br />
showed no evi<strong>de</strong>nce of urinary tract infection<br />
or blood in urine.<br />
After evaluating the CXR the suspicion of a fragment<br />
of a catheter or calcified cast (“ghost”) insi<strong>de</strong><br />
the superior vena cava and right atrium lead us to<br />
or<strong>de</strong>r further imaging tests. A CT scan of the thorax<br />
without contrast (see Figure 2) showed that the<br />
catheter tip was within the most superior aspect of<br />
the right atrium insi<strong>de</strong> a calcified cast, minimal cardiomegaly,<br />
clear lung fields, normal anatomy within
72<br />
the pulmonary, hilar, mediastinal and thoracic wall<br />
components. No mass or gross lympha<strong>de</strong>nopathy<br />
was found. Lung perfusion scan showed no evi<strong>de</strong>nce<br />
or probability of emboli. A cardiac report was or<strong>de</strong>red<br />
and it showed that the heart had normal segmental<br />
anatomy, normal dimensions, a trivial tricuspid<br />
regurgitation but otherwise normal flows,<br />
normal function, no vegetations and a catheter-like<br />
structure with <strong>de</strong>finite lumen seen from innominate<br />
vein into superior vena cava with tip in right atrium.<br />
Blood cultures did not show growth after 24h, 2<br />
days and 3 days.<br />
Patient was started on broad spectrum antibiotics<br />
and was transferred to the Cardiovascular<br />
Hospital for further examination and removal of the<br />
catheter fragment via femoral percutaneous<br />
endovascular technique. The catheter fragmented<br />
further during the retrieval procedure embolizing<br />
each fragment to the right and left pulmonary artery<br />
but both segments with a total length of two<br />
centimeters were able to be removed satisfactorily<br />
without complications. The child was discharged<br />
from the hospital two days later.<br />
DISCUSSION<br />
As previously mentioned, insertion of long-term<br />
central line catheters plays a vital role in providing<br />
continuous central venous access for therapy such<br />
as parenteral nutrition, long-term antibiotics and<br />
cancer chemotherapy in children and adults. Even<br />
though many complications with long-term application<br />
of indwelling catheters have been previously<br />
reported, to our knowledge, no report exists showing<br />
the probability of a distal fracture in a central<br />
line on the pediatric child and a plan of management<br />
on how to prevent it. To correctly position a<br />
CVC the tip of the hemoport catheter should lie<br />
within the superior vena cava or right atrial junction.<br />
Placement can be done through the external<br />
or internal jugular vein or using the subclavian vein<br />
approach with the port usually lying infraclavicularly<br />
in the anterior chest area. Very rarely (inci<strong>de</strong>nce of<br />
0-2.1%) proximal fragmentation with or without<br />
embolization of the port catheter can occur spe-<br />
3, 4<br />
cially during removal of the port.<br />
A distal fracture of a CVC can be suspected if<br />
the catheter offers resistance to removal and/or the<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
length removed is too short. In our case the catheter<br />
fracture occurred without resistance and at an<br />
unusually distal site, when a substantial part of the<br />
catheter was properly removed. Since the external<br />
jugular approach was utilized the catheter length<br />
was longer than a similar subclavian site approach.<br />
The ease of retrieval, <strong>de</strong>ceiving length and unusual<br />
site of rupture was the cause of not noticing that the<br />
distal part of the catheter was fixed to the vessel wall.<br />
There are several types of catheters currently<br />
on the market. The most commonly used materials<br />
for long term therapy are polyurethane and silicone.<br />
Different potential mechanisms of rupture of a catheter<br />
inclu<strong>de</strong> manufacturing <strong>de</strong>fect, mechanical<br />
trauma, the angle formed at the point of entry of<br />
the catheter into the vein (the catheter being a rigid<br />
structure), excessive hydrostatic pressure when flushing<br />
or infusing (Polyurethane catheters ruptured at<br />
flow rates between 4 and 15.4 mL/sec, with one<br />
catheter not rupturing at the maximal flow rate [17<br />
mL/sec], while silicone catheters ruptured at flow<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
rates between 0.5 to 3.5 mL/sec) 5 , material <strong>de</strong>gradation,<br />
stress due to constant motion (the constant<br />
movement of the vein as the adjacent artery<br />
moves as the heart beats, movement during pulmonary<br />
inspiration/expiration, external manipulation<br />
of the catheter), <strong>de</strong>position of fibrin, clot or<br />
calcium within the catheter, or the pinch-off sign<br />
effect (a narrowing of the catheter that occurs as<br />
the catheter is compressed between the first rib and<br />
the clavicle).<br />
There is much controversy in the literature regarding<br />
which material is better in preventing complications.<br />
For example, Gieneva et al, reported that<br />
in 200 cases of catheter fixation to the vessel wall<br />
194 were ma<strong>de</strong> of polyurethane and conclu<strong>de</strong>d that<br />
silicone catheters do not become as adherent to their<br />
fibrous sheet and vessel wall as with catheters ma<strong>de</strong><br />
of polyurethane. 6 Hla Thei et al, reported a case in<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
73<br />
which a catheter ma<strong>de</strong> of silicon was extensively<br />
adhered to the vessel wall. 7 Overall, catheter rupture<br />
is probably a combination between its material<br />
and ongoing situations to which this specific material<br />
is susceptible to fracture. Further specific studies<br />
remains to be performed to be able to <strong>de</strong>termine<br />
which of both materials is best in preventing<br />
complications.<br />
It is important to <strong>de</strong>tect catheter fractures as<br />
early as possible to provi<strong>de</strong> prompt treatment and<br />
prevent complications that are associated with intravascular<br />
catheter remnants after removal. These<br />
complications are well documented in the literature<br />
and inclu<strong>de</strong>: sepsis, endocarditis, thrombosis with<br />
catheter fixation to the vessel wall, pulmonary abscess<br />
from catheter embolization, vessel stenosis and<br />
dysrhythmia with or without sud<strong>de</strong>n <strong>de</strong>ath.<br />
There are different possible approaches to remove<br />
the remaining portion of a fractured catheter. Thoracotomy<br />
and sternotomy have been used with great success<br />
in removal but the morbidity associated with these<br />
procedures is high in the pediatric population. We<br />
preferred the percutaneous endovascular retrieval<br />
method by an invasive cardiologist or radiologist due<br />
to <strong>de</strong>creased morbidity and high success rate if per-<br />
8, 9<br />
formed by a skilled physician.<br />
Sometimes the physician may think that a portion<br />
of a catheter remains insi<strong>de</strong> the patient after<br />
removal because of hyper<strong>de</strong>nsity or hyperechoic<br />
silhouette found on a CXR or sonogram that mimics<br />
a catheter portion. 10 This shadows is caused by<br />
a fibrin sheath or thrombosis that forms around the<br />
catheter and then calcifies (it is called a calcified<br />
cast or “ghost”). 11 They suggest that the best way<br />
of differentiating a calcified cast or ghost from a<br />
portion of fractured catheter, if still uncertain after<br />
extensive sonographic evaluation, is to perform a<br />
CT scan. 10 Basically the difference is established<br />
looking closely at the margins of the silhouette, if it<br />
has uniform margins and a <strong>de</strong>finite lumen it is a<br />
catheter fragment, if not it is probably a “ghost”.<br />
We prefer a CT over a sonogram since it is not<br />
operator <strong>de</strong>pen<strong>de</strong>nt. Also the ribs and clavicles can<br />
make sonographic examination difficult.<br />
The best way to diagnose a distal catheter rupture<br />
is having a previous measurement of the length<br />
of the catheter before it is inserted so the physician
74<br />
is able to measure it after removal. Since distal fracture<br />
of a catheter is a rare event, not many perform<br />
this crucial step in <strong>de</strong>tecting catheter rupture<br />
complications. As in our case, sometimes this is an<br />
inci<strong>de</strong>ntal finding on a CXR film that was done looking<br />
for respiratory infections, but it can also be an<br />
inci<strong>de</strong>ntal finding using sonography for other reasons.<br />
In these situations a physician should suspect the possibility<br />
of a remaining fragment of a fractured catheter<br />
and should rule out the possibility of a calcified cast by<br />
performing a CT scan or doing an extensive<br />
sonographic analysis of the margins of the silhouette.<br />
In terms of insertion and removal of central lines<br />
we propose two algorithms. On algorithm 1 our<br />
preference in selecting the insertion site of the catheter<br />
is based primarily on accessibility, risk of complications<br />
and caliber of the vein. The pediatric<br />
population has a smaller vessel caliber compared<br />
to the adult population. The prevention of future<br />
complications caused by possible stenosis in the<br />
present pediatric population and risks during the<br />
procedure are forces that gui<strong>de</strong>d us in choosing this<br />
particular or<strong>de</strong>r. It has been well established in the<br />
literature that in as fast as two weeks a central line<br />
catheter causes stenosis of the subclavian vein. 12<br />
The external jugular vein is our first choice because<br />
it’s the most accessible compared to internal jugular<br />
vein and the subclavian vein and has the lowest<br />
risk of complications. Our second choice is the internal<br />
jugular vein which is <strong>de</strong>eper and has more<br />
risk of complications compared to the external jugular.<br />
13 Compared to the subclavian vein it has a larger<br />
caliber and a lowest risk of complications. Our third<br />
choice would be the subclavian vein because compared<br />
to the other two has a higher risk of complications<br />
such as pneumothorax, hemothorax, arrhythmia<br />
and stenosis. There is no need for performing<br />
chest films after successful insertion of catheter<br />
if it is done un<strong>de</strong>r fluoroscopy. 14<br />
As <strong>de</strong>picted in algorithm 2, during catheter removal<br />
the most important step is to measure the<br />
length of the catheter after each successful removal.<br />
If the catheter measures less than during insertion<br />
a distal fracture has occurred during retrieval and a<br />
chest film should be taken. With a retained fragment<br />
we suggest to place the patient in broad spectrum<br />
antibiotics to prevent infections, or<strong>de</strong>r a chest<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
CT scan without contrast for exact localization of<br />
fragment and surgery procedure planning, and consult<br />
interventional radiology or cardiology for<br />
15, 16<br />
endovascular percutaneous retrieval.<br />
RESUMEN<br />
La inserción <strong>de</strong> catéteres venosos centrales<br />
(CVC) juega un rol vital en proveer terapia <strong>de</strong> acceso<br />
venoso a niños. Fractura <strong>de</strong> estos catéteres suele<br />
verse luego <strong>de</strong> su uso prolongado al tratar <strong>de</strong><br />
removerlos. El sitio usual <strong>de</strong> ruptura es proximal<br />
don<strong>de</strong> el catéter entra en la vena cuando se usa el<br />
abordaje <strong>de</strong> la subclavia. En este reporte discutimos<br />
un caso don<strong>de</strong> el CVC se fracturó en su parte mas<br />
distal y no se <strong>de</strong>tectó que una fractura había ocurrido<br />
cuando se removió el catéter.<br />
Este es un niño <strong>de</strong> dos años que se encontró<br />
inci<strong>de</strong>ntalmente que tenía un pedazo <strong>de</strong> CVC distal<br />
fragmentado en una placa <strong>de</strong> pecho. Cuando el catéter<br />
se removió se daba por hecho que había salido<br />
completo. Un CT-Scan confirmó el diagnostico y el<br />
catéter se removió satisfactoriamente usando la técnica<br />
percutanea endovascular.<br />
Fracturas <strong>de</strong> CVC se <strong>de</strong>ben sospechar cuando<br />
hay resistencia al removerlo o si el largo que se<br />
remueve es muy corto. Existen diferentes<br />
mecanismos potenciales para la ruptura <strong>de</strong> estos<br />
CVC que incluyen trauma mecánico, <strong>de</strong>fecto <strong>de</strong><br />
manufactura o <strong>de</strong>gradación <strong>de</strong>l material <strong>de</strong> que están<br />
hechos. La ruptura se <strong>de</strong>be <strong>de</strong>tectar temprano parta<br />
evitar complicaciones como sepsis, endocarditis,<br />
trombosis, embolización, estenosis <strong>de</strong>l vaso<br />
sanguíneo o arritmias. El mejor método para remover<br />
el catéter fragmentado es usando la técnica<br />
endoscópica percutanea. Luego <strong>de</strong> remover un<br />
catéter una silueta hiper<strong>de</strong>nsa que se ve en placa<br />
sencilla <strong>de</strong> pecho pue<strong>de</strong> representar un tracto<br />
calcificado o ‘fantasma’. Para diferenciar este tracto<br />
o ‘fantasma’ <strong>de</strong> un pedazo <strong>de</strong> catéter se <strong>de</strong>be hacer<br />
un CT-Scan o ecocardiograma.<br />
El paso mas importante en prevenir tal<br />
complicación <strong>de</strong>scrita es mantener en el expediente<br />
medico <strong>de</strong>l paciente el largo <strong>de</strong>l catéter que se puso<br />
originalmente y medir el largo al removerlo para<br />
<strong>de</strong>terminar si el catéter salió completo o no.<br />
Catéteres fragmentados se <strong>de</strong>ben remover usando<br />
la técnica percutanea endovascular.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
REFERENCES<br />
1- Courtney M. Townsend Jr., et al: (2004) Sabiston Textbook of Surgery. 17th Ed. Phila<strong>de</strong>lphia: Elsevier Inc pp. 2081<br />
2- DA Andris, EA Krzywda, et al: Pinch-off syndrome: a rare etiology for central venous catheter occlusion. J Parenter Enteral Nutr. 18(6):531-<br />
3. 1994<br />
3- Klotz HP, Schopke W, et al: Catheter fracture: a rare complication of totally implantable subclavian venous access <strong>de</strong>vices. J Surg Oncol.<br />
62(3):222-5, 1996<br />
4- Jones SA, Giacomantonio M: A complication associated with central line removal in the pediatric population. J Pediatr Surg. 38(4):594-<br />
6, 2003<br />
5- Salis AI, Eclavea A, et al: Maximal flow rates possible during power injection through currently available PICCs: an in vitro study. J Vasc<br />
Interv Radiol. 15(3):275-81, 2004<br />
6- Wilson GJ, van Noesel MM, et al: The catheter is stuck: complications experienced during removal of a totally implantable venous access<br />
<strong>de</strong>vice. A single-center study in 200 children. J Pediatr Surg. 41(10):1694-8, 2006<br />
7- Thein H, Ratanjee SK: Tethered hemodialysis catheter with retained portions in central vein and right atrium on attempted removal. Am J<br />
Kidney Dis. 46(3):e35-9, 2005<br />
8- Roye GD, Breazeale EE, et al: Management of catheter emboli. South Med J. 89(7):714-7, 1996<br />
9- Chen CC, Liang CD, et al: Percutaneous removal of a peripherally inserted central catheter remnant using cardiac catheterization. Pediatr<br />
Int. 48(4):430-2, 2006<br />
10- Konen O, Daneman A, et al: Intravascular linear thrombus after catheter removal: sonographic appearance mimicking retained catheter<br />
fragment. Pediatr Radiol. 34(2):125-9, 2004<br />
11- Hughes DB, Ullery BW, Spigland N: Formation of a calcified “cast” in a long-term indwelling central venous catheter: a case report. J<br />
Pediatr Surg. 41(11):1927-9, 2006<br />
12- Courtney M. Townsend Jr., et al: (2004) Sabiston Textbook of Surgery. 17th Ed. Phila<strong>de</strong>lphia: Elsevier Inc pp. 2082<br />
13- Belani KG, Buckley JJ, et al: Percutaneous cervical central venous line placement: a comparison of the internal and external jugular vein<br />
routes. Anesth Analg. 59(1):40-4 1980<br />
14- Janik JE, Cothren CC, et al: Is a routine chest x-ray necessary for children after fluoroscopically assisted central venous access? J Pediatr<br />
Surg. 38(8):1199-202, 2003<br />
15- Fuenfer MM, Georgeson KE, Cain WS, Colvin EV, Johnson WH Jr, Pearce FB, McMahon WS: Etiology and retrieval of retained central<br />
venous catheter fragments within the heart and great vessels of infants and children. J Pediatr Surg. 33(3):454-6, 1998<br />
16- Giretti R, Caruselli M, Zannini R, <strong>de</strong> Vivo E, Piattellini G, Bechi P, Catani F, Amici M, Santelli F, Pagni R: Dislocation of central venous<br />
catheters in paediatric patients. J Vasc Access. 7(3):132-5, 2006<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
75
76<br />
Informe <strong>de</strong> Casos • Case Reports<br />
HERMANSKY PUDLAK SYNDROME:<br />
AN UNUSUAL FORM OF PROCTO-COLITIS<br />
By: Ignacio Echenique MD.*, José M. García González MD.**, Ignacio A. Echenique MS. §,<br />
Natalio J. Izquierdo MD.**, Juan R. Mella MA.£, Eligio Barasorda MD.*, Maria T. Mella MS. §<br />
and Siegfried Figueroa-Boilo MD. ¥<br />
ABSTRACT<br />
Hermansky-Pudlak syndrome (HPS) is a rare autosomal<br />
recessive disor<strong>de</strong>r consisting of oculocutaneous<br />
albinism, platelet dysfunction and systemic complications<br />
associated with lipofuscin <strong>de</strong>position in the reticuloendothelial<br />
system. HPS has been associated with a<br />
granulomatous enterocolitis with pathologic features<br />
suggestive of Crohn’s disease. It remains uncertain if<br />
HPS represents a truly distinct form of granulomatous<br />
enterocolitis. We report a series of two patients with<br />
HPS treated in <strong>Puerto</strong> <strong>Rico</strong>, and the results from medical<br />
and surgical intervention for gastrointestinal disease.<br />
Our experience with HPS patients has shown<br />
the difficult management of perineal disease similar<br />
in the management of Crohn’s. However, complications<br />
from the bleeding diathesis necessitate<br />
caution during surgery and potential anesthesia<br />
complications. Furthermore, avoidance of a perineal<br />
wound is preferred, and when possible, ileostomies<br />
have fewer complications than colostomies as they<br />
do not involve the small bowel.<br />
Key words: Hermansky Pudlak, syndrome,<br />
proctocolitis<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
The first <strong>de</strong>scription by Hermansky Pudlak syndrome<br />
(HPS) was ma<strong>de</strong> in Prague in 1959. They <strong>de</strong>scribed<br />
two unrelated patients with oculocutaneous<br />
albinism who had pseudohemophilia, peculiar pigmented<br />
reticular cells in the bone marrow and pulmonary<br />
fibrosis. HPS is also frequently associated with<br />
pulmonary fibrosis and granulomatous colitis (1). In<br />
the northwestern coast of <strong>Puerto</strong> <strong>Rico</strong> (PR) there is a<br />
prevalence of 1 in 1800 while 1 in 22 are carriers,<br />
making the island one of the places with the highest<br />
inci<strong>de</strong>nce of HPS in the world. In PR, 5 out of 6 albinos<br />
have the HPS gene (2). The first <strong>de</strong>scription of<br />
an HPS patient with perineal disease presentation<br />
was in 1989 (3). Since then until 2006 more cases<br />
have been <strong>de</strong>scribed (4, 5). Several genes have been<br />
associated with the syndrome; (6, 7); however, only<br />
HPS type 1 and HPS type 3 have been reported in<br />
<strong>Puerto</strong> <strong>Rico</strong> (8).<br />
In this study we present two patients with HPS<br />
who had complicated perineal disease and granulomatous<br />
colitis as part of the syndrome. The severe<br />
perineal disease and recto-vaginal fistulas were the<br />
cause for their referral to surgery.<br />
From the *Department of Surgery, Auxilio Mutuo Hospital, Rio Piedras, P.R., § Jefferson’s <strong>Medica</strong>l School Phila<strong>de</strong>lphia, PA, ** Department of<br />
Ophthalmology, UPR School of Medicine, £ Boston University, <strong>Medica</strong>l School, Boston, MA, and ¥ Department of Surgery, Hospital HIMA-San<br />
Pablo, Bayamon, PR. Address reprints to: Ignacio Echenique, MD - Office 218, Torre Auxilio Mutuo, 715 Ave. Ponce <strong>de</strong> Leon, Rio Piedras, PR,<br />
00918. E-mail . Poster presented at the 58 th Annual Meeting American College of Surgeons, <strong>Puerto</strong> <strong>Rico</strong> Chapter, <strong>Feb</strong>ruary<br />
22, 2008, La Concha Hotel, San Juan, PR.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 1: Ceroid <strong>de</strong>posits; mucosal sparing;<br />
skip lesions; predominately submucosal<br />
inflammation and ulceration; and noncaseating<br />
granulomas<br />
CASE HISTORY 1<br />
In 1991, we treated an 11 year-old girl from<br />
the central region of PR with a history of HPS who<br />
had severe rectal stricture, rectovaginal & perineal<br />
fistulas, and severe distal colitis with lower gastrointestinal<br />
bleeding. She failed aggressive medical<br />
therapy and was referred for a diverting stoma.<br />
In this operation she had significant bleeding. She<br />
<strong>de</strong>veloped Pyo<strong>de</strong>rma-Gangrenosa at the colostomy<br />
site and required extensive enterostomal therapy and<br />
wound care. A year after her fecal diversion, with<br />
failure to improve her perineal symptoms after the<br />
colostomy, she un<strong>de</strong>rwent a total proctocolectomy<br />
with intersphincteric resection and end ileostomy.<br />
She <strong>de</strong>veloped a persistent perineal wound sinus.<br />
Her multiple fistulas continue to drain and eventually,<br />
improved but still remained with a perineal sinus.<br />
Histopathology showed: ceroid <strong>de</strong>posits; mucosal<br />
sparing; skip lesions; predominately submucosal inflammation<br />
and ulceration with non-caseating granulomas<br />
(Figure 1). She had no pulmonary fibrosis.<br />
CASE HISTORY 2<br />
In 1983, a 15 year-old girl from <strong>Puerto</strong> <strong>Rico</strong><br />
presented HPS and severe perianal and perineal<br />
fistulas, recto-vaginal fistula and diffused colonic<br />
disease. After failure of treatment of her perineal<br />
disease she un<strong>de</strong>rwent a total proctocolectomy and<br />
terminal ileostomy. Postoperatively she <strong>de</strong>veloped<br />
a persistent perineal sinus needing a gracilis flap,<br />
but the perineal fistulas recurred months later. She<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
77<br />
had multiple re-admissions and required multiple<br />
interventions for small bowel obstructions and ileostomy<br />
complications. She also <strong>de</strong>veloped very symptomatic<br />
fistulization at the ileostomy site and required<br />
resection of more than 40 cm of small bowel.<br />
A white-grayish, wax-like material was found retroperitoneally<br />
associated with a severe inflammatory<br />
tissue reaction and causing obstructive uropathy.<br />
She eventually died from complications of her disease.<br />
She had no pulmonary fibrosis.<br />
DISCUSSION<br />
Shinella and co-workers first <strong>de</strong>scribed a patient<br />
with HPS who had granulomatous colitis and a patient<br />
with the syndrome who had small bowel involvement.<br />
They <strong>de</strong>scribed a patient who had gastrointestinal<br />
complications and presented an acute abdomen<br />
(9). Witkop and co-workers <strong>de</strong>scribed in their study<br />
that ceroid lesions in HPS are associated with pulmonary<br />
fibrosis and granulomatous gastrointestinal disease<br />
and are the most frequent accounting for the<br />
majority cause of <strong>de</strong>aths (2). Gastrointestinal complications<br />
occurred in 10.6% of patients and a mortality<br />
rate of 9% among <strong>de</strong>ceased patients with the syndrome<br />
(10). The accumulation of ceroid-like pigment in the<br />
macrophages lysosomes is believed to cause their rupture<br />
with release of lysosomal hydrolases, causing tissue<br />
damage in lungs and colon. (2, 10) Patients with<br />
HP syndrome may have a confusing clinical presentation<br />
that may mimic Crohn’s disease. In our cases,<br />
both patients had severe perineal disease and a very<br />
symptomatic recto-vaginal fistula as part of the initial<br />
presentation. They both required a total<br />
proctocolectomy with end Ileostomy. They both had<br />
persistent perineal sinus, one partially resolved with<br />
gracilis flap. One patient <strong>de</strong>veloped terminal ileum disease<br />
that required several surgical interventions. This<br />
ileal involvement has been <strong>de</strong>scribed in the literature<br />
(13). This presentation could be easily confused with<br />
Crohn’s Disease. The GI complications of HPS are<br />
not the <strong>de</strong>velopment of classical Crohn’s as has been<br />
suggested in the literature (5). The histological difference<br />
between Crohn’s and HPS granulomatous colitis<br />
are the tissue ceroid <strong>de</strong>posits in HPS (10). These ceroid<br />
<strong>de</strong>posits are not present in the granulomas of Crohn’s<br />
Disease. It is very important to distinguish both conditions,<br />
as the treatment for the bleeding disor<strong>de</strong>r in HPS
78<br />
requires specialized care. Patients with HPS, as part<br />
of the syndrome, also have a bleeding diathesis due to<br />
absence or <strong>de</strong>creased number of platelets <strong>de</strong>nse bodies<br />
(9, 10). This absence leads to abnormal platelet function,<br />
<strong>de</strong>spite the normal number of platelets. For this<br />
reason up to 75% of patients with the syndrome have<br />
abnormal bleeding times. Recently, Infliximab has been<br />
reported to obtain some remission in HPS patients as in<br />
Crohn’s and presents a possible therapy for treatment<br />
of HPS granulomatous proctocolitis (11, 12).<br />
Surgical management for perineal disease in<br />
patients with the syndrome should be similar to the<br />
one recommen<strong>de</strong>d for patients from the general<br />
population with Crohn’s disease. If possible, a<br />
perineal wound should be avoi<strong>de</strong>d. Ileostomies do<br />
better than colostomies but rarely small bowel involvement<br />
has been <strong>de</strong>scribed without colitis (13).<br />
Due to bleeding diathesis and potential anesthesia<br />
complications, elective surgery or tissue biopsies<br />
should be done with caution in patients with<br />
the syndrome.<br />
Patients with oculocutaneous albinism, or relatives<br />
of a patient with the condition who are either<br />
<strong>Puerto</strong> Ricans or <strong>Puerto</strong> Rican <strong>de</strong>scendants living<br />
in the continental U.S., must be screened to rule<br />
out HPS. Genetic linkage analysis is available for<br />
this purpose (8). Pre and postoperative management<br />
between surgeon, hematologist and<br />
pneumologist is advisable in patients with HPS, or<br />
patients with OCA who are <strong>Puerto</strong> Rican or <strong>Puerto</strong><br />
Rican <strong>de</strong>scendants living in continental U.S. (4, 14).<br />
Hermansky Pudlak syndrome presents a well known<br />
hereditary condition that shares many characteristics<br />
with Crohn’s disease and presents a medicosurgical<br />
challenge that requires both diseases to be<br />
evaluated for similarities that may help in future<br />
management of both.<br />
A study is been conducted (2007) evaluating medical<br />
treatments in colitis sponsored by the National Institute<br />
of Allergy and Infectious Diseases (15). Recommendations<br />
from this study are inclu<strong>de</strong>d in Table 1.<br />
RESUMEN<br />
El Síndrome Hermansky-Pudlak (SHP) es una<br />
condición rara autosómica recesiva que consiste <strong>de</strong><br />
albinismo oculocutáneo, disfunción plaquetaria y<br />
complicaciones sistémicas asociadas con el <strong>de</strong>pósito<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Table 1: Recommendations for <strong>Medica</strong>l<br />
Treatment of Colitis<br />
• Complete History and physical exam<br />
• Hematology consultation<br />
• Watch for partial oculocutaneous<br />
albinism if positive family history of<br />
albinism in a patient of Hispanic<br />
origin, particularly from <strong>Puerto</strong> <strong>Rico</strong><br />
• Endoscopic biopsies may not reveal the<br />
ceroid pigment<br />
• Skin Biopsies<br />
• Imaging studies<br />
• Pulmonary evaluation<br />
• Genetic counseling<br />
• Avoid drugs affecting platelet function<br />
• Avoid elective surgery or tissue biopsies<br />
• Same management for perineal<br />
disease as in Crohn’s<br />
• High rate of bleeding of dysfunctional bowel<br />
• Low Hartman’s pouch – avoid<br />
perineal wound if possible<br />
Ileostomies better than colostomies<br />
<strong>de</strong> lipofusina en el sistema reticuloendoteliar. SHP<br />
ha sido asociado con enterocolitis granulomatosa<br />
con características patológicas sugestivas <strong>de</strong> la<br />
enfermadad <strong>de</strong> Crohns. Sin embargo, algunos<br />
autores aún no están seguros <strong>de</strong> que SHP represente<br />
realmente una forma distinta <strong>de</strong> en-terocolitis<br />
granulomatosa. El síndrome es casi exclusivamente<br />
encontrado en pacientes <strong>de</strong> <strong>de</strong>scen<strong>de</strong>ncia<br />
puertorriqueña, particularmente en las regiones<br />
central y nor-oeste <strong>de</strong> la isla.<br />
Se reporta una serie <strong>de</strong> dos pacientes con SHP<br />
tratados en San Juan, <strong>Puerto</strong> <strong>Rico</strong>, y los resultados<br />
<strong>de</strong> los tratamientos médicos y quirúrgicos <strong>de</strong> las<br />
manifestaciones gastrointestinales.<br />
Nuestra experiencia con pacientes con SHP<br />
nos ha <strong>de</strong>mostrado la dificultad en el manejo cuando<br />
la presentación es perineal y similar a las<br />
presentaciones <strong>de</strong> Crohns. Sin embargo,<br />
complicaciones por los <strong>de</strong>sor<strong>de</strong>nes <strong>de</strong> coagulación<br />
nos obliga a tener cautela en operaciones y posibles<br />
complicaciones durante anestesia. Aún más, es<br />
preferible el tratar <strong>de</strong> evitar una herida en el perineo<br />
y cuando sea necesario una ostomía, la ileostomías<br />
si el íleo no esta afectado, pues tienen menos<br />
complica-ciones que las colostomías.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
REFERENCES<br />
1. Hermansky F, Pudlak P: Albinism associated with hemorrhagic diathesis and unusual pigmented reticular cells in<br />
the bone marrow: report of two cases with histochemical studies. Blood 1959, 14: 162-169<br />
2. Witkop CJ, Nuñez BM, Rao GH, Gaudier F, Summers CG, Shanahan F, Harmon KR, Townsend D, Sedano HO, King<br />
RA: Albinism and Hermansky-Pudlak Syndrome in <strong>Puerto</strong> <strong>Rico</strong>. Bol Asoc. Med PR 1990, 82: 333-339.<br />
3. Sherman A, Genuth L, Hazzi CG, Balthazar EJ, Schinella RA., Perirectal abscess in the Hermansky-Pudlak<br />
syndrome. [Am J Gastroenterol. 1989<br />
4 Echenique I, Hermansky Pudlack Syndrome, An Unusual form of Colitis, Eastern Colorectal Surgical Congress, Podium<br />
Presentation, Palm Beach, Fl. 2001<br />
5 Hazzan D, Seward S, Stock H, Zisman S, Gabriel K, Harpaz N, et al., Crohn’s-like colitis, enterocolitis and perianal<br />
disease in Hermansky-Pudlak syndrome. Colorectal Dis. †Sep†2006; 8(7): 539-43<br />
6 Spritz RA. Molecular Genetics of the Hermansky-Pudlak and Chediak-Higashi syndromes. Platelets. 1998, 9(1): 21-9.<br />
7 Spritz RA. Molecular genetics of oculocutaneous albinism. Semin Dermatol. 1993 Sep; 12(3): 167-72.<br />
8 Santiago Borrero PJ, Rodriguez-Perez Y, Renta JY, Izquierdo NJ, Del Fiero L, Muñoz D, Molina NL, Ramírez S, Pagan-<br />
Mercado G, Ortiz I, Rivera-Caragol E, Spritz RA, Cadilla CL., Genetic Testing for oculocutaneous albinism type 1 and 2<br />
and Hermansky-Pudlack syndrome type 1 and 3 mutations in <strong>Puerto</strong> <strong>Rico</strong>, J Invest Dermatol.2006 Jan;126(1):85-90<br />
9 Schinella RA, Greco MA, Cobert BL, Denmark LW, Cox RP. Hermansky-Pudlak Syndrome with granulomatous colitis.<br />
Ann Intern Med 1980, 92: 20-3.<br />
10 Witkop CJ, Townsed D, Bitterman PB, Harmon K. The role of cerunoid in lung and gastrointestinal disease in Hermansky-<br />
Pudlak syndrome. Adv Exp Med Biol 1989, 266: 283-296.<br />
11 Grucela, Patel, Goldstein, Ron Palmon, Sachar, DR. Steinhagen, Granulomatous enterocolitis Associated with Hermansky-<br />
Pudlack Syndrome. AMJ Gastroenterology 2006; 101:2090-2095<br />
12 Erzin Y, Cosgun S, Dobrucali A, Tasyurekli M, Erdamar S, Tuncer M. Complicated granulomatous colitis in a<br />
patient with Hermansky-Pudlak Syndrome successfully treated with Infliximab. Acta Gastroenterol Belg. 2006<br />
Apr-Jun; 69(2): 213-6.<br />
13 De Leusse A, Dupuy E, Huizing M, Danel C, Jian R Marteau P. Ileal Crohns Disease in a women with Hermansky<br />
Pudlack Syndrome, Gastroenrol Clin Biol 2006,Apr;30(4):621-4<br />
14 Izquierdo NJ, Townsend W, Hussels IE. Ocular findings in the Hermansky-Pudlak Syndrome.Trans Am Ophthalmol<br />
Soc. 1995; 93:191-200; discussion 200-2.<br />
15 National Institute of Allergy and Infectious Diseases (NIAID) <strong>Medica</strong>l Treatment of Colitis in Patients With Hermansky-<br />
Pudlak Syndrome http://clinicaltrials.gov/ct2/show/NCT00514982?cond=%22Hermanski-Pudlak+<br />
Syndrome%22&rank=1.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
79
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
81<br />
Informe <strong>de</strong> Casos • Case Reports<br />
LAPAROSCOPIC NEPHRECTOMY WITH<br />
LAPAROSCOPICALLY ASSISTED TRANSVAGINAL<br />
EXTRACTION OF INTACT KIDNEY<br />
ABSTRACT<br />
Purpose: Describe the first laparoscopic<br />
transperitoneal nephroureterectomy followed by<br />
laparoscopically assisted transvaginal extraction of<br />
the intact kidney performed in <strong>Puerto</strong> <strong>Rico</strong>.<br />
Case History/Results: A 39 year-old female<br />
patient consulted her urologist regarding chronic<br />
urinary tract infection. A diagnosis of a non-functioning<br />
left kidney was ma<strong>de</strong>, secondary to long<br />
standing obstruction due to a distal ureteral stone.<br />
Laparoscopic nephroureterectomy procedure was<br />
performed and the intact specimen was removed<br />
through a transverse posterior colpotomy. Patient<br />
was discharged home the next day without intraoperative<br />
or post-operative complications.<br />
Conclusions: Laparoscopic nephrec-tomy with<br />
transvaginal extraction of the intact specimen provi<strong>de</strong>s<br />
a surgical option as a minimally invasive technique<br />
with very few functional and cosmetic compromises<br />
and with low post-operative morbidity<br />
when performed in appropriate female patients.<br />
Key words: laparoscopy, nephrectomy,<br />
transvaginal<br />
INTRODUCTION<br />
The combination of laparoscopic nephrectomy<br />
with vaginal <strong>de</strong>livery of the intact kidney has been<br />
By: Alfonso Serrano-Ysern MD.*, Alvin Lopez MD.**, Freddie Men<strong>de</strong>z MD.**,<br />
Lianette Perez MD.* and Jaime Acosta MD.<br />
previously <strong>de</strong>scribed in the urologic literature (1-4).<br />
Many abdominal procedures which once required<br />
large skin incisions can now be performed<br />
through smaller incisions with the associated advantages<br />
of less morbidity and improved cosmesis.<br />
Usually, to remove the intact specimen after<br />
laparoscopic nephrectomy a 4–8 centimeters incision<br />
is nee<strong>de</strong>d (5).<br />
The laparoscopic nephrectomy is a procedure<br />
which uses minimally invasive surgical techniques,<br />
with low post-operative morbidity. This procedure<br />
can be done transperitoneally or retroperitoneally<br />
and used for both, benign and malignant diseases<br />
(6-11).<br />
Controversy exists between intact extractions<br />
of the specimen versus morcellation. With the morcellation<br />
technique for extraction of renal tumors,<br />
the specimen can be evaluated for histology but not<br />
for pathological staging (5,12).<br />
Colpotomy is an old technique with minimal<br />
morbidity, used by the gynecologist for diagnostic<br />
and therapeutic purposes in selected patients (13).<br />
This technique provi<strong>de</strong>s an excellent route for cases<br />
where a voluminous specimen extraction is nee<strong>de</strong>d.<br />
In addition it has the advantage of leaving a small<br />
hid<strong>de</strong>n scar from an esthetic point of view.<br />
* From the Department of Obstetrics and Gynecology, and ** Department of Urology, Hospital Interamericano <strong>de</strong> Medicina Avanzada (HIMA),<br />
Caguas, <strong>Puerto</strong> <strong>Rico</strong>. Address reprints: Alfonso Serrano-Ysern MD, P.O. Box 4980, Caguas, <strong>Puerto</strong> <strong>Rico</strong> 00726-4980. E-mail:<br />
. Poster presented at the 58 th Annual Meeting of the American College of Surgeons, <strong>Puerto</strong> <strong>Rico</strong> Chapter, <strong>Feb</strong>ruary 22, 2008,<br />
La Concha Hotel, San Juan, <strong>Puerto</strong> <strong>Rico</strong>.
82<br />
Figure 1: KUB, left kidney with multiple calculi<br />
(see arrows) and left distal ureteral calculi.<br />
Figure 3: Renal diuretic scan using 99mTc-MAG3 with<br />
non-visualization of the left kidney throughout the<br />
study which suggested a non-functioning left renal unit.<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Figure 2: (CT) scan showed left renal atrophy,<br />
multiple calculi (see arrow),<br />
hydroureteronephrosis secondary to a left distal<br />
ureteral calculi and perinephric fatty stranding<br />
We <strong>de</strong>scribe the first laparoscopic transperitoneal<br />
nephroureterectomy followed by laparoscopically assisted<br />
transvaginal extraction of the intact kidney performed<br />
in <strong>Puerto</strong> <strong>Rico</strong> (March, 2005).<br />
CASE HISTORY<br />
A 39 year-old woman was seen in a urologic<br />
consult for evaluation due to chronic urinary tract<br />
infections. Workup inclu<strong>de</strong>d a computed tomography<br />
(CT) scan which showed left renal atrophy with<br />
multiple calculi including hydroureterone-phrosis<br />
secondary to a left distal ureteral calculi and perinephric<br />
fatty stranding. A renal diuretic scan using<br />
99mTc-MAG3 revealed non- visualization of the left<br />
kidney throughout the study which suggested a nonfunctioning<br />
left renal unit. (Fig. 1,2,3)<br />
A gynecologic consultation was obtained in this<br />
patient (gravida 3, para 3, abort 0) with 3 previous<br />
cesarean sections. She was asymptomatic, the<br />
physical examination including the gynecologic examination<br />
was unremarkable (weight: 68 Kgs.,<br />
height: 152 Cms.). Informed consent was obtained<br />
for laparoscopic nephroureterectomy and transvaginal<br />
extraction of the specimen.<br />
During surgery, the patient was placed in the<br />
modified lateral <strong>de</strong>cubitus position, left si<strong>de</strong> up with<br />
legs in stirrups. The urology team performed a<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
laparoscopic transperitoneal nephroureterectomy<br />
using 4 ports. Operative time was 250 minutes.<br />
After completion of the primary laparoscopic procedure<br />
the specimen was placed into a retrieval bag.<br />
(LapSac® 8x10” / Cook®)*<br />
The operating table was positioned to the si<strong>de</strong> so<br />
that the patient rested in the lithotomy and<br />
Tren<strong>de</strong>lenburg positions. There was no need to place<br />
a new port and only previous trocars were used. The<br />
pelvis was visualized and adhesions were lysed. The<br />
laparoscope was pushed behind the uterus into the<br />
cul-<strong>de</strong>-sac so that the surgeon making the vaginal incision<br />
could use the light through the vagina.<br />
A transverse posterior colpotomy (13) was<br />
done. The in<strong>de</strong>x finger was used to displace the<br />
rectum and the peritoneum was opened without<br />
danger of injury to the bowel. The vaginal incision<br />
was exten<strong>de</strong>d sharply by stretching to approximately<br />
5-6 centimeters. The retrieval bag (LapSac®) drawstring<br />
was pushed through the vaginal incision; and<br />
while exerting a downward pressure the surgeon<br />
pulled the drawstring and removed the intact kidney<br />
in the retrieval bag.<br />
The posterior colpotomy incision was repaired<br />
with interrupted mattress absorbable sutures, including<br />
all layers. Operative time for the vaginal extraction<br />
procedure was 45 minutes. Blood loss was<br />
minimal and the specimen weighed 238 grams. No<br />
intra-operative complications occurred.<br />
The postoperative course was uneventful.<br />
There was no vaginal spotting and the patient was<br />
discharged home the next day.<br />
The pathologic examination revealed a left kidney<br />
surroun<strong>de</strong>d by perirenal fat. Also attached to<br />
the kidney was the ureter, and at the distal margin<br />
of the resection the obstructing calculus was i<strong>de</strong>ntified.<br />
Pathologic diagnosis was: Ureterolithiasis,<br />
hydronephrosis, chronic pyelonephritis and chronic<br />
glomerulonephritis consistent with the clinical diagnosis<br />
of non-functional kidney. (Fig.4)<br />
DISCUSSION<br />
The first laparoscopy on a human was performed<br />
in 1910 by the Swedish Doctor H.C.<br />
Jacobeus (14). In 1911, Doctor Bertram M.<br />
Bernheim (15) of Johns Hopkins University was the<br />
first to perform laparoscopic surgery in the United<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
83<br />
Figure 4: Specimen weighed 238 grams. Kidney<br />
surroun<strong>de</strong>d by perirenal fat, attached was the ureter,<br />
and at the distal margin of the resection the<br />
obstructing calculus was i<strong>de</strong>ntified (see arrow).<br />
States. The technique of posterior colpotomy was<br />
<strong>de</strong>scribed by Bradbury (13) in 1952.<br />
Laparoscopy and colpotomy have long been used<br />
by gynecologists for diagnosis and treatment of pelvic<br />
pathology. In the early 1970s, therapeutic laparoscopy<br />
was introduced by gynecologists. Rapid technical advances<br />
in miniaturized surgical tools, fiber optics, and<br />
vi<strong>de</strong>o systems enabled new <strong>de</strong>velopments in minimally<br />
invasive surgical techniques and the substitution of laparotomy.<br />
These methods greatly reduced post-operative<br />
complications (15).<br />
The first laparoscopic nephrectomy was <strong>de</strong>scribed<br />
by Clayman et al (16) in 1991. The laparoscopic nephrectomy<br />
procedure is now well established with consi<strong>de</strong>rable<br />
advantages such as <strong>de</strong>creased post-operative<br />
morbidity, <strong>de</strong>creased analgesic requirements, improved<br />
cosmesis with a shorter hospital stay and convalescence<br />
(6-9,12,11,17).<br />
The combination of laparoscopic nephrectomy<br />
and vaginal extraction of the intact specimen was
84<br />
reported in 1993. Breda et al (1) reported the extraction<br />
of a non cancerous kidney and Dauleh (2)<br />
reported the extraction of two kidneys, one using a<br />
retrieval bag and the other removed intact but not<br />
protected by a bag. Gill et al (3) <strong>de</strong>scribed in 2002<br />
ten cases of vaginal extraction of kidney after<br />
laparoscopic nephrectomy using a retrieval bag and<br />
Sunoo et al (4) reported one case of laparoscopic<br />
radical nephrectomy with vaginal <strong>de</strong>livery and retrieval<br />
bag in 2005.<br />
Contraindication for this type of surgical intervention<br />
inclu<strong>de</strong>s such systemic conditions as chronic obstructive<br />
pulmonary disease with hypercarbia, ascites,<br />
bleeding diatheses, bowel obstruction and acute or<br />
chronic vaginal pathology. Previous history of renal,<br />
abdominal or pelvic surgery is a relative contraindication.<br />
This procedure should be individualized, based<br />
on the surgeons experience (8,13).<br />
Hand assisted laparoscopic donor nephrectomy<br />
has gained acceptance. This technique is likely to become<br />
the “gold standard” in the near future (18). In<br />
this particular setting it is necessary to obtain the intact<br />
specimen with minimal trauma and the posterior<br />
colpotomy would need further investigation to consi<strong>de</strong>r<br />
it a surgical option in donor females.<br />
CONCLUSION<br />
This report <strong>de</strong>scribes the first transperitoneal<br />
nephroureterectomy for benign disease with transvaginal<br />
extraction of the intact kidney, using<br />
laparoscopically assisted posterior colpotomy, performed<br />
in <strong>Puerto</strong> <strong>Rico</strong>.<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
Transvaginal extraction of the intact specimen<br />
provi<strong>de</strong>s a surgical option for both benign and malignant<br />
disease processes, as a minimally invasive<br />
technique with very few functional and cosmetic<br />
compromises and with low morbidity when performed<br />
in appropriate female patients.<br />
RESUMEN<br />
Propósito: Describir la primera Nefroureterectomia<br />
Transperitoneal Laparoscopica seguida por extracción<br />
<strong>de</strong>l riñón intacto, por vía transvaginal con ayuda <strong>de</strong>l<br />
laparoscopio, realizada en <strong>Puerto</strong> <strong>Rico</strong>.<br />
Caso / Resultados: Paciente femenina <strong>de</strong> 39<br />
años <strong>de</strong> edad, que consulto a su urólogo por<br />
infecciones crónicas <strong>de</strong>l tracto urinario. Se realizó<br />
un diagnóstico <strong>de</strong> un riñón izquierdo no funcionante,<br />
secundario a una obstrucción crónica, por un cálculo<br />
distal <strong>de</strong>l uréter izquierdo.<br />
Se realizó una Nefroureterectomia<br />
Transperitoneal Laparoscopica, luego el espécimen<br />
intacto, fue removido através <strong>de</strong> una colpotomía<br />
posterior transversa. La paciente fue egresada al<br />
día siguiente, sin complicaciones intra-operatorias<br />
o post-operatorias.<br />
Conclusiones: La Nefroureterectomia<br />
Transperitoneal Laparoscopica con extracción <strong>de</strong>l<br />
espécimen intacto, provee una opción quirúrgica,<br />
con una técnica mínimamente invasiva, poco<br />
compromiso funcional y cosmético, con una baja<br />
morbilidad post-operatoria, cuando se realiza en los<br />
pacientes femeninos apropiados.<br />
REFERENCES<br />
1.- Breda, G. Silvestre, P. Giunta, A. et al. Laparoscopic nephrectomy with vaginal <strong>de</strong>livery of the intact kidney. Eur Urol 24(1): 116-7,<br />
1993.<br />
2.- Dauleh, MI. Townell, NH. Laparoscopic nephroureterectomy for malignancy: vaginal route for retrieval of intact specimen. Br J Urol<br />
72(5 Pt 1): 667-8, Nov. 1993.<br />
3.- Gill, I.S. Cherullo EE. Meraney, AM. et al. Vaginal extraction of the intact specimen following laparoscopic radical nephrectomy. J Urol<br />
167(1): 238-41, Jan. 2002<br />
4.- Sunoo, Ch. Aaberg, RA. Nakamura, J.K. Laparoscopically assisted vaginal extraction of the kidney after laparoscopic radical nephrectomy.<br />
The permanente J. 9(1): 1-5, 2005<br />
5.- Varkarakis, I. Rha, K. Hernan<strong>de</strong>z, F. Kavoussi, LR. Jarret, TW. Laparoscopic specimen extraction: Morcellation. BJU International.<br />
95(2):27. 2005<br />
6.- Rassweiler, J. Fre<strong>de</strong>, T. Henkel, TO. et al. Nephrectomy: A comparative study between the transperitoneal and retroperitoneal<br />
laparoscopic versus the open approach. Eur Urol 33:489-496, 1998<br />
7.- Kerbl, K. Clayman, RV. McDougall, EM. Gill, IS. Et al. Transperitoneal nephrectomy for benign disease of the kidney: Comparison of<br />
laparoscopic and open surgical techniques. J Urol 43(5):607-13. 1994<br />
8.- Harmon, WJ. Bishoff, JT. Transperitoneal laparoscopic radical nephrectomy. (emedicine® web site) July 25, 2001. Available at: http:/<br />
/www.emedicine.com Accessed March 12, 2005<br />
9.- Rassweiler, JJ. Stock, C. Fre<strong>de</strong>, T. et al. Transperitoneal and retroperitoneal laparoscopic nephrectomy in comparison with conventional<br />
nephrectomy. Urologe A. 35(3):215-22. 1996<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
10.- Rassweiler, JJ. Henkel, TO. Potempa, DM. et al. Transperitoneal laparoscopic neprectomy: Training , technique,and results. J Urol.<br />
7(6):505-15. 1993<br />
11.- Eraky, I. Kappany, H. Shamaa, MA. Laparoscopic nephrectomy: an established routine procedure. J Endourol. 8(4):275-8. 1994<br />
12.- Kaouk, JH. Gill, IS. Laparoscopic radical nephrectomy: Morcellate or leave intact? Leave intact. Rev Urol 4(1): 38-42. 2002<br />
13.- Bradbury, WC. West J Surg Obstet Gynecol. 60(8): 377–86, Aug. 1952.<br />
14.- Jacobaeus, HC. Ueber die möglich keit die zystoskopie bei untersuchung seröser höhlungen anzuwe<strong>de</strong>n. Munch Med Wochenschr. 57:<br />
2090-2, 1910.<br />
15.- Stellato, TA. History of laparoscopic surgery. Surgical Clinics of North America. Vol. 72: 5, Oct. 1992.<br />
16.- Clayman, RV. Kavoussi, LR. Soper, NJ. et al. Laparoscopic nephrectomy : initial case report. J Urol 146(2) : 278-82, Aug. 1991.<br />
17.- Gill, IS. Kavousi, LR. Clayman RV. et al. Complications of laparoscopic nephrectomy in185 patients: A multi-institutional review. J<br />
Urol 154(2):479-483. 1995<br />
18.- Handchin, AE. Weber, M. Demartines, N. Clavien, PA. Laparoscopic donor nephrectomy. Br. J Surg. 90(11):1323-32. 2003.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
85
86<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
CALENDARIO DE ACTIVIDADES MÉDICAS<br />
18-21 <strong>de</strong> julio XV Congreso <strong>Puerto</strong>rriqueño <strong>de</strong> Cardiología<br />
auspiciado por la Sociedad <strong>Puerto</strong>rriqueña <strong>de</strong> Cardiología,<br />
Westin Río Mar, para información 787-620-2228<br />
23-25 <strong>de</strong> mayo American College of Cardiology P.R. Chapter<br />
The Ritz Carlton San Juan Hotel, Isla Ver<strong>de</strong><br />
23-26 <strong>de</strong> mayo Congreso Sociedad Radiológica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
Río Mar Beach Resort<br />
31 <strong>de</strong> mayo Activa tu salud, camina con nosotros<br />
Paseo Lineal <strong>de</strong> Bayamón 2:00pm<br />
6-8 <strong>de</strong> junio Clinica Multifásica Distrito Este, Vieques<br />
Municipio Vieques<br />
7 <strong>de</strong> junio Clinica Multifásica <strong>de</strong> la AMPR, en la Se<strong>de</strong><br />
AMPR, Santurce<br />
21 <strong>de</strong> junio Jornada Científica AMPR, en la Se<strong>de</strong><br />
AMPR, Santurce<br />
27 <strong>de</strong> junio Concierto Lírico AMPR, en la Se<strong>de</strong><br />
AMPR, Santurce<br />
29 <strong>de</strong> junio Asamblea Extraordinaria <strong>de</strong> la AMPR<br />
Club <strong>de</strong> Leones, Bayamón<br />
OFICINAS ADMINISTRATIVAS SUBSCRIPCIONES Y ANUNCIOS<br />
Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
• Ave. Fernán<strong>de</strong>z juncos Núm. 1305 • PO Box 9387 • San Juan, <strong>Puerto</strong> <strong>Rico</strong> 00908-9387<br />
• Tel 787-721-6969 • Fax: 787- 724-5208 • Email: asocmed@coqui.net<br />
Publicación mensual - $40.00 anuales.<br />
El “Boletín” se distribuye a todos los socios <strong>de</strong> la<br />
Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong> como parte<br />
<strong>de</strong> su cuota anual.<br />
Todo anuncio que se publique en el Boletín <strong>de</strong> la<br />
Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong> <strong>de</strong>berá cumplir con<br />
las normas establecidas por la Asociación Médica <strong>de</strong><br />
<strong>Puerto</strong> <strong>Rico</strong> y la Asociación Médica Americana.<br />
La Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong> no se hace<br />
responsable por los productos o servicios anunciados.<br />
La publicación <strong>de</strong> los mismos no necesariamente<br />
implica el endoso <strong>de</strong> la Asociación Médica <strong>de</strong> <strong>Puerto</strong><br />
<strong>Rico</strong>.<br />
Todo anuncio para ser publicado <strong>de</strong>be reunir las<br />
normas establecidas por la publicación. Todo<br />
material <strong>de</strong>be entregarse listo para la imprenta y<br />
con sesenta días <strong>de</strong> anterioridad a su publicación.<br />
La AMPR no se hará responsable por material y/o<br />
artículos que no cumplan con estos requisitos.<br />
Todo artículo recibido y/o publicado está sujeto a<br />
las normas y reglamentos <strong>de</strong> la Asociación Médica<br />
<strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong>. Ningún artículo que haya sido<br />
previamente publicado será aceptado para esta<br />
publicación. La Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
no se hace responsable por las opiniones expresadas<br />
o puntos <strong>de</strong> vista vertidos por los autores, a menos<br />
que esta opinión esté claramente expresada y/o<br />
<strong>de</strong>finida <strong>de</strong>ntro <strong>de</strong>l contexto <strong>de</strong>l artículo.<br />
Todos los <strong>de</strong>rechos reservados. El Boletín está<br />
totalmente protegido por la ley <strong>de</strong> <strong>de</strong>rechos <strong>de</strong>l autor<br />
y ninguna persona o entidad pue<strong>de</strong> reproducir total<br />
o parcialmente el material que aparezca publicado<br />
sin el permiso escrito <strong>de</strong> los autores.<br />
“Boletín / Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong>”<br />
is published monthly for $40.00 per year by:<br />
Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
PO. Box 9387 San Juan, <strong>Puerto</strong> <strong>Rico</strong> 00908-9387<br />
1305 Fernán<strong>de</strong>z Juncos Ave.<br />
Email: asocmed@coqui.net<br />
"POSTMASTER"<br />
Send address changes to:<br />
Boletín / Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong><br />
1305 Fernán<strong>de</strong>z Juncos Ave. P.O. Box 9387<br />
San Juan, <strong>Puerto</strong> <strong>Rico</strong> 00908-9387<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
• Ave. Fernán<strong>de</strong>z Juncos Núm. 1305 •<br />
• PO Box 9387 • San Juan, <strong>Puerto</strong> <strong>Rico</strong> 00908-9387 •<br />
• Tel 787-721-6969 • Fax: 787- 722-1191 •<br />
• email: asocmed@coqui.net •<br />
A la Junta <strong>de</strong> Directores:<br />
Por la presente solicito ser admitido como socio <strong>de</strong> la Asociación Médica <strong>de</strong> <strong>Puerto</strong> <strong>Rico</strong>,<br />
para lo cual someto la siguiente información preliminar: (Use Letra <strong>de</strong> Mol<strong>de</strong>)<br />
Nombre<br />
Socio:<br />
CUOTA:<br />
Dirección Postal:<br />
Activo Activo no Resi<strong>de</strong>nte Interno-Resi<strong>de</strong>nte<br />
$150.00 $100.00 $60.00<br />
Afiliado Estudiante<br />
$60.00 No paga cuota<br />
Pueblo: ZIP Co<strong>de</strong>: Teléfono Resi<strong>de</strong>ncial:<br />
Dirección Oficina:<br />
Teléfono Oficina: Fax: No. Beeper:<br />
Número Seguro Social: Estado Civil:<br />
Fecha <strong>de</strong> Nacimiento: Ciudad y País: Ciudadanía:<br />
Nornibre dél Padre: Nombre <strong>de</strong> la Madre: Nombre <strong>de</strong>l Cónyuge:<br />
Escuela <strong>de</strong> Medicina: Número <strong>de</strong> Licencia:<br />
Especialidad: Año <strong>de</strong> Graduación:<br />
INTERNO RESIDENTE (Llenar):<br />
Fecha <strong>de</strong> Comienzo: • Término <strong>de</strong> Entrenamiento<br />
AFILIADO (Llenar):<br />
Fecha- Cominzo • Término <strong>de</strong> Entrenamiento<br />
ESTUDIANTE (Llenar):<br />
— SOLICITUD PRELIMINAR DE INGRESO COMO SOCIO—<br />
Fecha <strong>de</strong> Graduación: • Escuela <strong>de</strong> Medicina<br />
Certifico que la información arriba brindada es cierta y completa.<br />
Firma <strong>de</strong>l Solicitante: Fecha:<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008<br />
NOTA: ES REQUISITO INDISPENSABLE PARA LA.APROBACION DE<br />
LA SOLICITUD EL QUE SE LLENEN TODOS LOS ENCASILLADOS<br />
87
BOLETÍN<br />
88<br />
BOLETÍN • ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
ASOCIACIÓN MÉDICA DE PUERTO RICO<br />
• Instrucciones para los Autores*<br />
El “Boletín” acepta para su publicación artículos relativos a medicina y cirugía<br />
y las ciencias afines. ¡Igualmente acepta artículos especiales y correspon<strong>de</strong>ncia que<br />
pudiera ser <strong>de</strong> interés general para la profesión médica. Se urge a los autores se<br />
esfuercen en perseguir claridad, brevedad, e ir a lo pertinente en sus manuscritos,<br />
no importa el tema o formato <strong>de</strong>l manuscrito.<br />
El artículo, si se aceptara, será con la condición <strong>de</strong> que se publicara únicamente<br />
en la revista. Para facilitar la labor <strong>de</strong> revisión <strong>de</strong> la junta Editora y la <strong>de</strong>l impresor,<br />
se requiere <strong>de</strong> los autores que sigan las siguientes instrucciones:<br />
• Manuscrito<br />
El manuscrito completo, incluyendo las leyendas y referencias <strong>de</strong>berán estar escritos<br />
en maquinilla a doble espacio; por un sólo lado <strong>de</strong> cada página, en TRIPLICADO y con<br />
amplio margen (ARTÍCULO DEBERÁ SER ACOMPAÑADO POR UN “CD”). En<br />
página separada <strong>de</strong>berá incluirse lo siguiente: título, nombre <strong>de</strong> autor(es) y su grado (ej.:<br />
MD, FACP), ciudad don<strong>de</strong> se hizo el trabajo, el hospital o institución académica,<br />
patrocinadores <strong>de</strong>l estudio, y si un artículo ha sido leído en alguna reunión o congreso, así<br />
<strong>de</strong>be hacerse constar como una nota al calce.<br />
El manuscrito <strong>de</strong>be comenzar con una breve introducción en la cual se especifique<br />
el propósito <strong>de</strong>l mismo. Las secciones principales (como por ejemplo: materiales y métodos)<br />
<strong>de</strong>ben i<strong>de</strong>ntificarse con un encabezamiento en letras mayúsculas.<br />
Artículos referentes a resultados <strong>de</strong> estudios clínicos o investigaciones <strong>de</strong> laboratorio<br />
<strong>de</strong>ben organizarse bajo los siguientes encabezamientos: introducción, Materiales y Métodos,<br />
Resultados, Discusión, Resumen (en español e inglés), Reconocimiento y Referencias.<br />
Artículos referentes a estudios <strong>de</strong> casos aislados <strong>de</strong>ben organizarse en la siguiente<br />
forma: Introducción, Materiales y Métodos si es aplicable, Observaciones <strong>de</strong>l Caso,<br />
Discusión, Resumen (en español e inglés), Reconocimientos y Referencias.<br />
• Nomenclatura<br />
Deben usarse los nombres genéricos <strong>de</strong> los medicamentos. Podrán usarse también<br />
los nombres comerciales, entre paréntesis, si así se <strong>de</strong>sea se usará con preferencia el<br />
sistema métrico <strong>de</strong> pesos y medidas.<br />
• Tablas<br />
Las tablas <strong>de</strong>ben aparecer en hojas separadas. Estas <strong>de</strong>ben incluir el título, y el<br />
número <strong>de</strong> la tabla <strong>de</strong>be estar en romano. Los símbolos <strong>de</strong> unida<strong>de</strong>s <strong>de</strong>ben limitarse al<br />
encabezamiento <strong>de</strong> las columnas. Se <strong>de</strong>ben omitir líneas verticales en la tabla. Se usará en<br />
las tablas el mismo idioma en el cual está escrito el artículo. Deben limitarse las tablas a<br />
solo aquellas que contribuyan al mejor entendimiento <strong>de</strong>l manuscrito.<br />
• Ilustraciones<br />
Las fotografías y microfotografías se someterán como copias en papel <strong>de</strong> lustre,<br />
sin montar o en transparencias. En el reverso <strong>de</strong> la figura <strong>de</strong>be aparecer el número <strong>de</strong> la<br />
figura (arábigo) y el autor. Debe indicarse la parte superior <strong>de</strong> la ilustración.<br />
• Resumen<br />
Un abstracto no mayor <strong>de</strong> 150 palabras <strong>de</strong>be acompañar los manuscritos. Debe<br />
incluir los puntos principales que ilustren la substancia <strong>de</strong>l artículo y la exposición <strong>de</strong>l<br />
problema, métodos, resultados y conclusiones.<br />
• Referencias<br />
Las referencias <strong>de</strong>ben ir numeradas sucesivamente <strong>de</strong> acuerdo a su aparición en el<br />
texto. Los números <strong>de</strong>ben aparecer en paréntesis al nivel <strong>de</strong> la línea u oración. Al final <strong>de</strong><br />
cada artículo las referencias <strong>de</strong>ben aparecer en el or<strong>de</strong>n numérico en que se citan en el<br />
texto. Deben utilizarse solamente las abreviaturas para títulos <strong>de</strong> revistas científicas según<br />
indicadas en el “Cumulative In<strong>de</strong>x Medicus" que publica la Asociación Médica Americana.<br />
Las referencias <strong>de</strong>ben seguir el patrón que se <strong>de</strong>scribe a continuación.<br />
1. Para artículos <strong>de</strong> revistas: Apellido(s) e iniciales <strong>de</strong>l nombre <strong>de</strong>l autor(es), título <strong>de</strong>l<br />
artículo, nombre <strong>de</strong> la revista, año, volumen, páginas. Por ejemplo: Villavicencio R:<br />
Soplos inocentes en pediatría, Bol Asoc Méd P <strong>Rico</strong> 198 1; 73: 479-87. Si hay más<br />
<strong>de</strong> 7 autores, incluir los primeros 3 y añadir et al.<br />
2. Para citación <strong>de</strong> libros don<strong>de</strong> el autor(es) <strong>de</strong>l capítulo citado es a su vez el (los) editor(es):<br />
Apellido(s) e iniciales <strong>de</strong>l autor(es), título <strong>de</strong>l libro, número <strong>de</strong> edición, ciudad, casa<br />
editora, año y página. Por ejemplo: Keith JD, Rowe RD, Vlad P: Heart disease in<br />
infancy and childhood, 3d. Ed., New York, MacMillan, 1978: 789<br />
3. Para citación <strong>de</strong> libros don<strong>de</strong> el editor(es) no es el autor(es) <strong>de</strong>l capítulo citado se<br />
aña<strong>de</strong> el autor(es) <strong>de</strong>l capítulo y el título <strong>de</strong>l mismo. Por ejemplo: Olley PM: Cardiac<br />
arrythmias; In: Keith ID, Rowe RD, Vlad P Eds. Heart disease in infancy and childhood,<br />
3d Ed., New York, MacMillan, 1978: 275-301<br />
• Cartas al Editor<br />
Se publicarán a discreción <strong>de</strong> la Junta Editora. Deben estar escritas en maquinilla a<br />
doble espacio, no <strong>de</strong>ben ser mayores <strong>de</strong> 500 palabras, ni incluir más <strong>de</strong> cinco referencias.<br />
(ARTÍCULO DEBERÁ SER ACOMPAÑADO POR UN “CD”)* Estas<br />
“Instrucciones para los Autores` son <strong>de</strong> acuerdo a las normas establecidas por el<br />
Comité Internacional <strong>de</strong> Editores <strong>de</strong> Revistas Médicas en sus `Requisitos Uniformes<br />
para Manuscritos Sometidos a Revistas Bio-Médicas".<br />
• Instructions to Authors*<br />
The “Buletín” will accept for publication contributions relating to the<br />
various areas of medicine, surgery and allied medical sciences. Special articles<br />
and correspon<strong>de</strong>nce on subjects of general interest to physicians will also be<br />
accepted. All material is accepted with the un<strong>de</strong>rstanding that is to be published<br />
solely in this journal.<br />
All authors are urged to seek clarity, brevity, and pertinence in the manuscripts<br />
regardless of subject or format.<br />
In or<strong>de</strong>r to facilitate review of the article by the Editorial Board and the work of the<br />
printer, the authors must conform with the following instructions:<br />
• Manuscripts<br />
The entire manuscript, including legends and references should be<br />
typewritten double spaced in TRIPLICATE with ample margins (ARTICLES<br />
SHOULD BE ACCOMPANIED WITH A ”CD”). A separate title page should<br />
inclu<strong>de</strong> the following: title, authors and their <strong>de</strong>grees (e.g. MD, FACP), city<br />
where the work was done, hospital or aca<strong>de</strong>mic institutions, acknowledgments<br />
of financial sponsors, and if the paper has been at a meeting the place and date<br />
should be given.<br />
The manuscripts should start with a brief introductory paragraph or<br />
paragraphs which should state its purpose. The main sections (for example,<br />
Materials and Methods) should be i<strong>de</strong>ntified by heading in capital letters.<br />
Articles reporting the results of clinical studies or laboratory investigation<br />
should be organized un<strong>de</strong>r the following headings: Introduction, Materials and<br />
Methods, Result if indicated, Discussion, Summary in English and Spanish,<br />
Acknowledgments if any, and References.<br />
• Nomenclature<br />
Generic names of drugs should be used; tra<strong>de</strong> names my also be given in parenthesis,<br />
if <strong>de</strong>sired, metric units of measurement should be used preferentially.<br />
• Tables<br />
These should be typed on separate sheets with the title and table number (Roman)<br />
centered. Symbol for units should be confined lo the column headings. Vertical lines should<br />
be omitted. The language used in the tables must be the same as that of the article. Inclu<strong>de</strong><br />
only those tables which will enhance the un<strong>de</strong>rstanding of the article. They should<br />
supplement, not duplicate the text.<br />
• Illustrations<br />
Photographs and photomicrographs should be submitted as glossy prints<br />
(unmounted) or sli<strong>de</strong>s. They should be labeled in the back with the name of the authors<br />
and figure number (Arabic) and the top should be indicated. Legend to the figures should<br />
be typed on a separate sheet.<br />
• Summary<br />
An abstract not longer than 150 words should accompany all articles. It must inclu<strong>de</strong><br />
the main points that present the core of the article and the exposition of the problem,<br />
method, results, and conclusions.<br />
• References<br />
These should be numbered serially as they appear in the text. The number should<br />
be enclosed in parenthesis on the line or writing and not as superscript, numbers. At the<br />
end of the article references should be listed in the numerical or<strong>de</strong>r in which they are first<br />
cited in the text. The titles of journals should be abbreviated according to the style used in<br />
the "Cumulative In<strong>de</strong>x Medicus" published by the American <strong>Medica</strong>l Association. The<br />
correct forms of references are as given below:<br />
1. For periodicals: Surname and initials of author(s), title of article, name of journal,<br />
year, volume, pages. For example: Villavicencio R.: Soplos inocentes en pediatría.<br />
Bol Asoc Med P <strong>Rico</strong> 198 1; 73: 479 87. If there are more than 7 authors list only<br />
3 and add et al.<br />
2. For books when the authors of the cited chapter is at the same time the editor:<br />
Surname and initials of author(s), title, edition, city, publishing house, ~ear and page.<br />
For example: Keith JD, Rowe RD, Vlad P: Heart disease in infancy and childhood,<br />
3d Ed., New York, MacMillan, 1978: 789<br />
3. For chapter in book when the author of the chapter is not one of the Olley PM:<br />
Cardiac arrythmias: In: Keith JD, Rowe RD, Vlad P. Eds. Heart disease in infancy and<br />
childhood, 3d Ed. New York, MacMillan, 1978, 275-301<br />
• Letters to the Editor<br />
Will be published at the discretion of the Editorial Board. They should be typewritten<br />
double-spaced, should not exceed 500 words nor more than five references.<br />
ARTICLES SHOULD BE ACCOMPANIED WITH A "CD" *The above<br />
'Instructions to Authors" are according to the format required by the international<br />
Committee of <strong>Medica</strong>l Journal Editors in its “Uniform Requirements for Manuscripts<br />
Submitted to Biomedical Journals”.<br />
Vol. 100 • Núm. 1 • <strong>Ene</strong>ro-Marzo 2008