michigan hypertension core curriculum - State of Michigan
michigan hypertension core curriculum - State of Michigan
michigan hypertension core curriculum - State of Michigan
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Clinical Implications: In the setting <strong>of</strong> chronic, poorly controlled <strong>hypertension</strong> rapid reductions in<br />
BP can lead to cerebral ischemia attributable to reductions in cerebral blood flow at BP levels that<br />
are within the hypertensive range.<br />
A. Reductions in MAP below the Lower Limit <strong>of</strong> CBF Autoregulation<br />
As systemic perfusion pressure falls below the lower limits <strong>of</strong> CBF autoregulation, cerebral<br />
resistance vessels have dilated maximally but are no longer able to maintain cerebral blood flow.<br />
As CBF falls, cerebral oxidative metabolism is supported by augmentation <strong>of</strong> oxygen extraction<br />
from the declining cerebral blood flow. At this point symptoms <strong>of</strong> cerebral hypoperfusion such as<br />
lethargy, confusion, somnolence, etc. can appear. When CBF falls below ~10 ml/100g/min, the<br />
ionic gradient across neuronal cell membranes becomes disrupted leading to calcium influx and<br />
potassium efflux and neuronal cell injury/death occur. Unlike the heart where oxygen extraction<br />
is maximal at rest, the brain can extract greater amounts <strong>of</strong> oxygen from blood traversing it<br />
when cerebral blood flow falls. This provides at least some measure <strong>of</strong> cushion against cerebral<br />
ischemia.<br />
B. Increases in MAP above the Upper Limit <strong>of</strong> CBF Autoregulation<br />
As systemic perfusion pressure rises cerebral resistance vessels normally constrict.<br />
When systemic perfusion pressure rises above the upper limits <strong>of</strong> CBF autoregulation then CBF<br />
increases dramatically and there is increased permeability <strong>of</strong> the cerebral vasculature leading<br />
to cerebral edema and increased intracranial pressure. Raised intracranial pressure has two<br />
important physiological effects. First, systemic BP increases further. Secondly CBF may fall<br />
though this tendency is counterbalanced by the reflex rise in systemic perfusion pressure.<br />
Symptoms <strong>of</strong> CNS dysfunction again can occur such as seizures, lethargy, stupor, coma, etc.<br />
The clinical term for this life-threatening clinical situation is hypertensive encephalopathy. Table<br />
6 displays clinical symptoms that characterize hypertensive encephalopathy.<br />
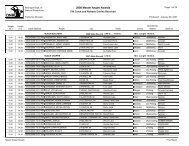
Table 6<br />
9. Blood Pressure and Cerebral Blood Flow Regulation during Acute Brain Ischemia<br />
Hypertension is the major risk factor for stroke. Approximately 80% <strong>of</strong> patients with acute<br />
stroke have elevated BP at the time <strong>of</strong> hospital admission. The observation <strong>of</strong> elevated BP at the<br />
time <strong>of</strong> admission has also been made in persons without antecedent <strong>hypertension</strong>.<br />
Blood pressure reflexively rises during acute cerebral ischemia and brain trauma. During<br />
acute cerebral ischemia, cerebral blood flow autoregulation is disrupted in the ischemic areas<br />
<strong>of</strong> the brain surrounding the already infarcted area. Disruption <strong>of</strong> CBF autoregulation is greater<br />
for brainstem ischemic lesions than for hemispheric lesions; severe hemispheric lesions cause<br />
greater disruption <strong>of</strong> autoregulation than minor hemispheric lesions; and subcoritcal lesions<br />
NKFM & MDCH 35