michigan hypertension core curriculum - State of Michigan
michigan hypertension core curriculum - State of Michigan
michigan hypertension core curriculum - State of Michigan
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
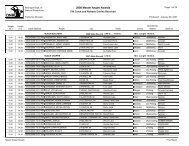
The higher the level <strong>of</strong> BP, the more likely pressure-related target-organs will sustain<br />
injury. Injury to pressure-sensitive target organs is occurs via multiple mechanisms as displayed in<br />
table 4. Endothelial dysfunction, vascular remodeling causing target-organ ischemia, accelerated<br />
atherosclerosis, cardiac remodeling/left ventricular hypertrophy and vascular rarefaction are<br />
examples <strong>of</strong> chronic pressure-related injury. An arterial tear as seen in aortic dissection or rupture<br />
<strong>of</strong> an aneurysm are very dramatic manifestations <strong>of</strong> pressure-related target-organ injury. Table 4.<br />
Mechanisms <strong>of</strong> Blood Pressure-Related Target Organ Injury<br />
7. Mechanisms <strong>of</strong> Pressure-Related Hemodynamically-Mediated Renal Injury<br />
Hypertension has been linked both to chronic kidney disease as well as end-stage renal<br />
disease (ESRD). In fact, <strong>hypertension</strong> is the second leading cause <strong>of</strong> ESRD behind diabetes<br />
mellitus. The distinction between <strong>hypertension</strong> and diabetes mellitus is not entirely distinct. About<br />
70 - 80% <strong>of</strong> persons with diabetes mellitus have <strong>hypertension</strong> (BP > 130/80 mm Hg and/or taking<br />
antihypertensive medications), and obesity augments the risk for both <strong>hypertension</strong> and diabetes<br />
mellitus.<br />
Transmission <strong>of</strong> systemic arterial pressure into the glomerulus, the functional unit <strong>of</strong> the<br />
kidney, is a major cause <strong>of</strong> renal injury. Under normal conditions the glomerulus protects itself from<br />
inordinate transmission <strong>of</strong> arterial pressure into the glomerular capillary loop. The mechanism<br />
by which systemic arterial transmission to the glomerulus is dampened is called autoregulation<br />
<strong>of</strong> renal GFR and blood flow. The afferent arteriole brings blood flow into the glomerulus from<br />
the renal artery where blood is filtered, urine is formed, and blood leaves the glomerulus via the<br />
efferent arteriole. Blood subsequently flows from this glomerular capillary network into another<br />
one, the peritubular capillaries. That is, the efferent arteriole branches into a peritubular capillary<br />
network that surrounds the tubules.<br />
Autoregulation <strong>of</strong> GFR and renal blood flow are accomplished via several mechanisms.<br />
Increases in afferent arteriolar luminal pressure cause constriction <strong>of</strong> this vessel; decreases in<br />
luminal pressure cause dilation <strong>of</strong> this vessel. These afferent luminal caliber changes in response<br />
to changes in pressure are accomplished via the myogenic reflex. Tubuloglomerular feedback<br />
(TGF) is another mechanism through which afferent arteriolar tone can be affected. This<br />
mechanism changes afferent arteriolar tone according to changes in sodium chloride delivery<br />
to the macula densa in the distal nephron. Increased NaCl delivery leads to increased afferent<br />
arteriolar tone while decreased delivery causes afferent arteriolar dilation. Finally, local activation<br />
<strong>of</strong> the RAS system as typically occurs in the setting <strong>of</strong> reduced renal mass (↓ nephron number)<br />
leads to Ang II -mediated efferent >> than afferent arteriole constriction that raises intraglomerular<br />
pressure.<br />
NKFM & MDCH 31