michigan hypertension core curriculum - State of Michigan
michigan hypertension core curriculum - State of Michigan
michigan hypertension core curriculum - State of Michigan
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
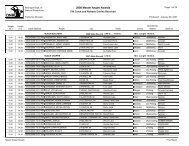
Compelling Indications for Specific Antihypertensive Medication Classes<br />
182 Hypertension Core Curriculum<br />
Khaled Ismail, MD<br />
Learning Objectives:<br />
1. Learn the various coexisting conditions for which specific classes <strong>of</strong> antihypertensive drugs are<br />
indicated.<br />
2. Understand the evidence supporting the use <strong>of</strong> different antihypertensive drug classes in<br />
patients with these comorbidities.<br />
Pretest:<br />
1. A 38 year-old male with a history <strong>of</strong> type 2 diabetes presents to your <strong>of</strong>fice for a routine<br />
checkup. His BP is 155/95 mmHg and his last hemoglobin A1C was 8.9%. His BP on a previous visit 6<br />
weeks ago was 150/90 mmHg. He currently takes only insulin. Which medication is the best choice for<br />
initial antihypertensive therapy?<br />
a. hydrochlorothiazide 25mg<br />
b. losartan 50 mg/d plus chlorthalidone 25 mg/d (correct answer)<br />
c. metoprolol 25 mg bid<br />
d. amlodipine 5 mg/d<br />
e. clonidine 0.1mg bid<br />
The JNC 7 guidelines published in 2003 identified several “compelling indications” for<br />
prescribing certain antihypertensive medication classes. 1 These indications include congestive heart<br />
failure (CHF), a history myocardial infarction or stroke, chronic kidney disease, diabetes and an overall<br />
elevated risk for coronary artery disease.<br />
Large, randomized controlled trials (RCT) have shown survival benefits independent <strong>of</strong> BP<br />
control when treating HF (specifically systolic dysfunction) when beta blockers, angiotensin converting<br />
enzyme (ACE) inhibitors and angiotensin receptor blockers are administered. The investigators<br />
found a 31% relative risk reduction in all-cause mortality at one year in patients with American Heart<br />
Association class 4 heart failure patients treated with enalapril. 2 The ARB valsartan was found to<br />
reduce hospitalization due to CHF in patients with class 2 or greater heart failure. 3 Beta-blockers<br />
such as extended-release metoprolol have been shown in RCT to significantly reduce mortality. 4,5 The<br />
administration <strong>of</strong> the aldosterone antagonist, spironolactone to patients with classes 3 and 4 heart<br />
failure has also been associated with a 30% reduction in mortality. 6 Following myocardial infarction,<br />
beta-blockers, ACE inhibitors and aldosterone antagonists have each been associated with significant<br />
reductions in mortality (23%, 19%, and 15% respectively). 5,7,8 Thus, in hypertensive patients with<br />
systolic heart failure, it is imperative that these drug classes be preferentially used in the prescribed<br />
antihypertensive regimens.<br />
Numerous prospective studies in animals and humans have shown the renoprotective effects<br />
<strong>of</strong> RAS antagonists in patients with CKD. Thus, these agents are definitely indicated in patients with<br />
diabetic and non-diabetic nephropathy. 9,10 It is a mistake, however, to believe that BP control, in most<br />
instances, will be obtained without additional antihypertensive agents – most notably diuretics and/or<br />
calcium antagonists.<br />
Diabetic patients should be treated with RAS antagonists – either an ACE inhibitor or an ARB.