The Venipuncture From an Arm Vein
The Venipuncture From an Arm Vein
The Venipuncture From an Arm Vein
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
So You’re Going to Collect a Blood Specimen: An Introduction to Phlebotomy 21<br />
<strong>The</strong> <strong>Venipuncture</strong> <strong>From</strong> <strong>an</strong> <strong>Arm</strong> <strong>Vein</strong> J<br />
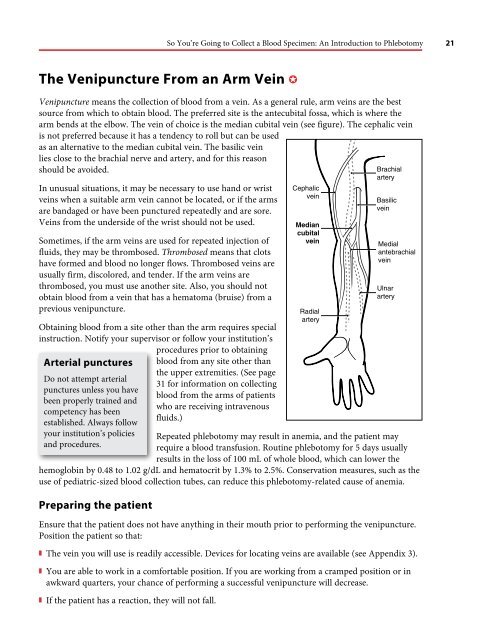
<strong>Venipuncture</strong> me<strong>an</strong>s the collection of blood from a vein. As a general rule, arm veins are the best<br />
source from which to obtain blood. <strong>The</strong> preferred site is the <strong>an</strong>tecubital fossa, which is where the<br />
arm bends at the elbow. <strong>The</strong> vein of choice is the medi<strong>an</strong> cubital vein (see figure). <strong>The</strong> cephalic vein<br />
is not preferred because it has a tendency to roll but c<strong>an</strong> be used<br />
as <strong>an</strong> alternative to the medi<strong>an</strong> cubital vein. <strong>The</strong> basilic vein<br />
lies close to the brachial nerve <strong>an</strong>d artery, <strong>an</strong>d for this reason<br />
should be avoided.<br />
Brachial<br />
In unusual situations, it may be necessary to use h<strong>an</strong>d or wrist<br />
veins when a suitable arm vein c<strong>an</strong>not be located, or if the arms<br />
are b<strong>an</strong>daged or have been punctured repeatedly <strong>an</strong>d are sore.<br />
<strong>Vein</strong>s from the underside of the wrist should not be used.<br />
Sometimes, if the arm veins are used for repeated injection of<br />
fluids, they may be thrombosed. Thrombosed me<strong>an</strong>s that clots<br />
have formed <strong>an</strong>d blood no longer flows. Thrombosed veins are<br />
usually firm, discolored, <strong>an</strong>d tender. If the arm veins are<br />
thrombosed, you must use <strong>an</strong>other site. Also, you should not<br />
obtain blood from a vein that has a hematoma (bruise) from a<br />
previous venipuncture.<br />
Obtaining blood from a site other th<strong>an</strong> the arm requires special<br />
instruction. Notify your supervisor or follow your institution’s<br />
procedures prior to obtaining<br />
Arterial punctures<br />
Do not attempt arterial<br />
punctures unless you have<br />
been properly trained <strong>an</strong>d<br />
competency has been<br />
established. Always follow<br />
your institution’s policies<br />
<strong>an</strong>d procedures.<br />
blood from <strong>an</strong>y site other th<strong>an</strong><br />
the upper extremities. (See page<br />
31 for information on collecting<br />
blood from the arms of patients<br />
who are receiving intravenous<br />
fluids.)<br />
Repeated phlebotomy may result in <strong>an</strong>emia, <strong>an</strong>d the patient may<br />
require a blood tr<strong>an</strong>sfusion. Routine phlebotomy for 5 days usually<br />
results in the loss of 100 mL of whole blood, which c<strong>an</strong> lower the<br />
hemoglobin by 0.48 to 1.02 g/dL <strong>an</strong>d hematocrit by 1.3% to 2.5%. Conservation measures, such as the<br />
use of pediatric-sized blood collection tubes, c<strong>an</strong> reduce this phlebotomy-related cause of <strong>an</strong>emia.<br />
Preparing the patient<br />
Ensure that the patient does not have <strong>an</strong>ything in their mouth prior to performing the venipuncture.<br />
Position the patient so that:<br />
z <strong>The</strong> vein you will use is readily accessible. Devices for locating veins are available (see Appendix 3).<br />
z You are able to work in a comfortable position. If you are working from a cramped position or in<br />
awkward quarters, your ch<strong>an</strong>ce of performing a successful venipuncture will decrease.<br />
z If the patient has a reaction, they will not fall.<br />
Cephalic<br />
Cephalic vein<br />
vein<br />
Medi<strong>an</strong> cubital Medi<strong>an</strong> vein<br />
cubital<br />
vein<br />
Radial<br />
Radial artery<br />
artery<br />
Brachial artery<br />
artery<br />
Basilic<br />
Basilic vein<br />
vein<br />
Medial<br />
Medial <strong>an</strong>tebrachial vein<br />
<strong>an</strong>tebrachial<br />
vein<br />
Ulnar<br />
Ulnar artery<br />
artery
22 So You’re Going to Collect a Blood Specimen: An Introduction to Phlebotomy<br />
Hospitalized patient not in bed<br />
Have the patient sit at a small table where the elbow c<strong>an</strong><br />
be placed on a hard surface, or in a position in which the<br />
arm c<strong>an</strong> be placed across the bed. If necessary, put a small<br />
pillow or a roll of towels under the extended arm to<br />
support it.<br />
Outpatient/ambulatory patient<br />
Ask the patient to sit in a chair designed for phlebotomy<br />
or at a small table where the elbow is placed across a hard<br />
surface. This will ensure that there is sufficient support<br />
for the arm. This support will help prevent the patient<br />
from pulling the arm back when the needle is inserted<br />
into a vein. For inf<strong>an</strong>ts or small children, have a second<br />
individual, such as a parent, hold the arm of the child<br />
firmly so that the arm will not jerk suddenly when the<br />
needle is inserted into the vein.<br />
Home visits<br />
Tourniquet<br />
Pillow<br />
Follow the same principles outlined above. Do not place<br />
your equipment on or near food. Ensure patient safety<br />
since there may not be <strong>an</strong>y help available if the patient<br />
faints (see pages 36–37).<br />
Some patients may have fragile bones<br />
or restrictions to phlebotomy sites due<br />
to recent surgeries. Make certain to<br />
obey <strong>an</strong>y signage that warns the<br />
phlebotomist against potential injuries<br />
to the patient from phlebotomy.<br />
Hospitalized patient in bed<br />
Make sure the patient is in a position<br />
where the arm is easy to access for<br />
venipuncture. Place the blood<br />
collection tray where it is readily<br />
available but is not in d<strong>an</strong>ger of being<br />
upset by the patient. Never put your<br />
equipment on the patient’s bed.<br />
Never label tubes prior to collection.<br />
Never leave <strong>an</strong>y equipment in the<br />
room.<br />
Before phlebotomy, always ask<br />
patients if they are taking<br />
<strong>an</strong>ticoagul<strong>an</strong>ts or if they have <strong>an</strong><br />
inherited blood clotting problem.<br />
Patients who are taking medicine to<br />
prevent their blood from clotting<br />
(ie, <strong>an</strong>ticoagul<strong>an</strong>ts such as coumadin,<br />
heparin, or aspirin) or patients who<br />
have inherited a blood clotting<br />
abnormality (eg, hemophilia) may<br />
continue to bleed from the punctured<br />
vein. If this bleeding is not stopped,<br />
blood may accumulate within the tissues<br />
of the arm, specifically in the enclosed<br />
area of the arm that surrounds the<br />
muscle. This bleeding c<strong>an</strong> lead to<br />
compartment syndrome, a condition<br />
in which the blood accumulates in a<br />
contained space within the arm such<br />
that the pressure produced c<strong>an</strong> interfere<br />
with blood flow <strong>an</strong>d may injure the<br />
muscle. This is a rare but very serious<br />
complication <strong>an</strong>d requires <strong>an</strong><br />
emergency surgical procedure to open<br />
the compartment, relieve the pressure,<br />
<strong>an</strong>d stop the bleeding.
Never attempt venipuncture on<br />
a st<strong>an</strong>ding patient. Patients<br />
sometimes faint during or after<br />
venipuncture. A st<strong>an</strong>ding patient<br />
might suddenly collapse.<br />
So You’re Going to Collect a Blood Specimen: An Introduction to Phlebotomy 23<br />
Selecting the vein for venipuncture<br />
Whenever possible, a blood specimen should not be obtained<br />
from <strong>an</strong> extremity when <strong>an</strong> IV is running (see page 31) or when<br />
dermatitis (skin inflammation) is present over the vein. If the<br />
patient has had a mastectomy with lymph nodes removed from<br />
the underarm area, a physici<strong>an</strong>’s authorization is required prior<br />
to performing phlebotomy on the involved extremity. <strong>The</strong> patient may offer specific information<br />
about arm preference, <strong>an</strong>d it is import<strong>an</strong>t for you to listen to their specific needs. Follow <strong>an</strong>y special<br />
instructions of the ordering physici<strong>an</strong> or laboratory.<br />
Inspect the preferred arm first. If it appears good, attempt to draw from this arm. You may be able<br />
to see the vein. <strong>Vein</strong>s appear blue <strong>an</strong>d are slightly raised above the skin surface. <strong>Vein</strong>s may be more<br />
difficult to see in obese people.<br />
Gloves c<strong>an</strong> be put on at this point or they c<strong>an</strong> be put on just before the venipuncture. Consult your<br />
institution’s policy/procedure <strong>an</strong>d follow the established guidelines. Always wash your h<strong>an</strong>ds or use<br />
<strong>an</strong> alcohol-based h<strong>an</strong>d rub before you glove, <strong>an</strong>d wear new, properly fitting gloves. Never tear or<br />
remove the tip of the finger of the glove for <strong>an</strong>y reason.<br />
Attach <strong>an</strong> unused sterile needle to the needle holder <strong>an</strong>d assemble the necessary blood collection<br />
tubes. Always have extra evacuated tubes close at h<strong>an</strong>d in case problems are encountered with the<br />
original tubes.<br />
Apply the tourniquet about 3 inches above the elbow, or midway between the elbow <strong>an</strong>d shoulder.<br />
z <strong>The</strong> tourniquet must be applied with enough tension to compress the vein, but not the artery. (An<br />
artery carries blood into the area, <strong>an</strong>d if the tourniquet is too tight, blood flow will slow or stop.)<br />
z If appropriate, have the patient form a fist to make the veins more prominent, thus aiding in<br />
identification of the vein. <strong>The</strong>re must not be <strong>an</strong>y h<strong>an</strong>d “pumping,” which c<strong>an</strong> alter some <strong>an</strong>alyte<br />
concentrations. Asking the patient to clench their fist repeatedly has been reported to be a common<br />
error in phlebotomy practice.<br />
z Have the patient keep their h<strong>an</strong>d closed until blood is flowing freely into the tube, <strong>an</strong>d then ask the<br />
patient to open their h<strong>an</strong>d.<br />
z Some special tests may require that blood be collected without a tourniquet. Consult your<br />
phlebotomy m<strong>an</strong>ual or ask your supervisor for information.<br />
z Do not leave the tourniquet on for more th<strong>an</strong> 1 minute while you search for a vein. If more th<strong>an</strong><br />
1 minute passes, release the tourniquet for at least 3 minutes. <strong>The</strong>n, reapply the tourniquet.<br />
Inspect <strong>an</strong>d palpate the area to find a vein. Prolonged obstruction of blood flow by the tourniquet<br />
(ie, tourniquet in place for longer th<strong>an</strong> 2 to 3 minutes) ch<strong>an</strong>ges some test results.<br />
Always palpate or feel for the vein, even when the vein is seen. This procedure gives you practice in<br />
finding deeper, unseen veins. <strong>The</strong> vein will feel like <strong>an</strong> elastic tube that “gives” under the pressure of<br />
your finger. Arteries pulsate, so make certain the structure you feel is not pulsating.