A decision aid for women considering hormone therapy after ...
A decision aid for women considering hormone therapy after ...
A decision aid for women considering hormone therapy after ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Patient Education and Counseling 33 (1998) 267–279<br />
A <strong>decision</strong> <strong>aid</strong> <strong>for</strong> <strong>women</strong> <strong>considering</strong> <strong>hormone</strong> <strong>therapy</strong> <strong>after</strong><br />
menopause: <strong>decision</strong> support framework and evaluation<br />
a,b,c, b,c b,c b<br />
Annette M. O’Connor * , Peter Tugwell , George A. Wells , Tom Elmslie ,<br />
b b b a c<br />
Elaine Jolly , Garry Hollingworth , Ruth McPherson , Helen Bunn , Ian Graham ,<br />
a,c<br />
Elizabeth Drake<br />
a University of Ottawa, School of Nursing, Ottawa, Ontario, Canada<br />
b University of Ottawa, Faculty of Medicine, Ottawa, Ontario, Canada<br />
c Clinical Epidemiology Unit, Ottawa Civic Hospital Loeb Research Institute, 1053 Carling Ave, Ottawa, Ontario, K1Y 4E9, Canada<br />
Abstract<br />
Received 30 July 1997; received in revised <strong>for</strong>m 20 October 1997; accepted 10 November 1997<br />
Although postmenopausal <strong>women</strong> are advised to consider their values when deliberating about potential benefits and risks<br />
of <strong>hormone</strong> <strong>therapy</strong> (HRT), feasible, effective methods of <strong>decision</strong> support in primary care have yet to be established. Using<br />
an explicit <strong>decision</strong> support framework, we developed a self-administered HRT <strong>decision</strong> <strong>aid</strong> and evaluated it in a<br />
be<strong>for</strong>e/<strong>after</strong> study of 94 <strong>women</strong> from six family practices. An audiotape guided <strong>women</strong> through an illustrated booklet<br />
including: detailed in<strong>for</strong>mation about HRT benefits and risks tailored to a woman’s clinical risk, and a values clarification<br />
exercise to promote in<strong>for</strong>med <strong>decision</strong> making consistent with personal values. After using the <strong>decision</strong> <strong>aid</strong> participants: had<br />
better general knowledge and more realistic personal expectations of HRT benefits and risks; and, felt more certain,<br />
in<strong>for</strong>med, clear about values, and supported in <strong>decision</strong> making. Women’s values elicited in the clarification exercise were<br />
84% accurate in discriminating between <strong>decision</strong>s. Women with polarized preferences at baseline did not change their minds,<br />
but were better in<strong>for</strong>med. Changes in preferences occurred in the uncertain group, with equal numbers accepting or declining<br />
HRT. Most participants found the <strong>decision</strong> <strong>aid</strong> comprehensible, acceptable in length and pace, and balanced. Decision <strong>aid</strong>s<br />
are useful in preparing <strong>women</strong> <strong>for</strong> <strong>decision</strong> making about this complex, personal issue. © 1998 Elsevier Science Ireland<br />
Ltd.<br />
Keywords: Decision making; Women’s health; Choice behavior; In<strong>for</strong>med consent; Decision support techniques; Patient<br />
education; Patient participation; Health education; Consumer satisfaction; Hormone replacement <strong>therapy</strong> (HRT); Menopause<br />
Practice guidelines [1,2] suggest that post- only <strong>after</strong> learning about the probable benefits and<br />
menopausal <strong>women</strong> consider long-term <strong>hormone</strong> risks and judging their personal value. Implementing<br />
<strong>therapy</strong> (HRT) to protect the heart and bones, but these guidelines is challenging in primary care, given<br />
the complexity of judging the benefits and risks, the<br />
* size of the post-menopausal population, and the<br />
Corresponding author. Tel.: (1-613) 798-5555; fax: (1-613)<br />
761-5492; e-mail: aoconnor@civich.ottawa.on.ca limited resources to support <strong>women</strong>’s <strong>decision</strong> mak-<br />
0738-3991/98/$19.00 © 1998 Elsevier Science Ireland Ltd. All rights reserved.<br />
PII S0738-3991(98)00026-3
268 A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279<br />
ing. General educational materials are limited in stance, diagnosis, or developmental transition; (2)<br />
helping <strong>women</strong> to judge the personal likelihood and require careful deliberation because of the uncertain<br />
personal value of HRT benefits and risks. There<strong>for</strong>e, and/or value-sensitive nature of the benefits and<br />
‘<strong>decision</strong> <strong>aid</strong>s’ are being developed as an adjunct to risks; and (3) need relatively more ef<strong>for</strong>t during the<br />
counseling [3–6]. Decision <strong>aid</strong>s differ from usual deliberation phase than the implementation phase.<br />
patient education materials by: focusing on alter- There<strong>for</strong>e the DSF is less useful <strong>for</strong> <strong>decision</strong>s: (1)<br />
natives, benefits, and risks tailored to a woman’s with no immediate stimulus <strong>for</strong> deliberation; (2)<br />
clinical risk profile; providing detailed descriptions whose key challenge is implementing and maintainof<br />
the benefits and risks in functional terms; using ing the <strong>decision</strong>; or (3) that are rapid, repetitive,<br />
explicit probabilities to describe the likelihood of automatic, impulsive or deferential to authority.<br />
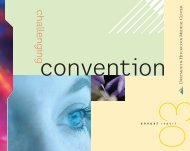
benefits and risks; including values clarification to As shown in Fig. 1, the DSF is organized accordencourage<br />
evaluation of the personal importance of ing to: (1) determinants of <strong>decision</strong>s; (2) <strong>decision</strong><br />
the benefits and risks; and emphasizing choice and support interventions which address the determinants<br />
shared <strong>decision</strong> making [7]. In the case of the HRT to improve the quality of the <strong>decision</strong> making<br />
<strong>decision</strong>, benefits and risks need to be tailored to a process and the <strong>decision</strong>; and (3) evaluation to<br />
woman’s hysterectomy status and risk of coronary ascertain the success of the <strong>decision</strong> support on the<br />
heart disease (CHD), osteoporosis, and breast cancer quality of the <strong>decision</strong> process, <strong>decision</strong>, and out-<br />
[1]. Moreover, a woman needs to consider her values comes of <strong>decision</strong>s. The concepts apply to both the<br />
[1] in balancing the potential benefits of protection client (individual, couple, or group) and the pracfrom<br />
CHD and osteoporosis and relief of menopausal titioner, although the empirical focus in this paper is<br />
symptoms against the endometrial cancer risk, the on the client.<br />
uncertain risk of breast cancer, the side effects of<br />
HRT, and her attitudes toward preventive medication 1.1. Determinants of <strong>decision</strong>s<br />
<strong>for</strong> a natural aging process.<br />
HRT <strong>decision</strong> <strong>aid</strong>s are in the early developmental Essential inputs into <strong>decision</strong>s include the client’s<br />
stages. There is little evidence of their efficacy. and practitioner’s: demographic, clinical, and prac-<br />
Some lack an explicit conceptual framework and tice characteristics; perceptions of the <strong>decision</strong>;<br />
some are unsuitable <strong>for</strong> administration in primary perceptions of important others involved in the<br />
care settings with limited personnel, time, space, or <strong>decision</strong>; and personal and external resources to<br />
technology. Our study objective was to develop and make and implement a choice. These are defined in<br />
evaluate a portable, self-administered <strong>decision</strong> <strong>aid</strong>, Table 1. According to the theories underlying the<br />
based on an explicit framework of <strong>decision</strong> support, DSF, the selection of one alternative over another<br />
which a <strong>women</strong> could use at home to prepare her <strong>for</strong> depends not only on the client and practitioner<br />
structured counseling with her practitioner. We de- characteristics, but also on whether they are knowveloped<br />
a <strong>decision</strong> <strong>aid</strong> delivered via a take-home ledgeable about the issues, expect the alternative will<br />
booklet and audiotape and then evaluated it in a likely lead to outcomes they most value; are reasonbe<strong>for</strong>e/<strong>after</strong><br />
study in 6 family practices. This paper ably certain this is the best alternative; perceive that<br />
presents the <strong>decision</strong> support framework we used to important others agree with and are supportive of<br />
develop the <strong>decision</strong> <strong>aid</strong> and the results of this the alternative; and have the necessary personal and<br />
preliminary evaluation. external resources to make and implement the<br />
choice.<br />
1. Decision support framework 1.2. Decision support<br />
Our <strong>decision</strong> support framework (DSF) is based Decision support involves preparing the client and<br />
on expectancy value, <strong>decision</strong>al conflict, and social the practitioner <strong>for</strong> <strong>decision</strong> making and structuring<br />
support theories [8–15]. It was developed <strong>for</strong> health follow-up counseling. The goal is to improve the<br />
<strong>decision</strong>s that: (1) are stimulated by a new circum- quality of <strong>decision</strong> making by addressing the modifi-
A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279 269<br />
Fig. 1. Decision Support Framework (DSF).<br />
able determinants of <strong>decision</strong>s that are suboptimal: likelihood of benefits and risks. Decision <strong>aid</strong>s may<br />
inadequate knowledge; unrealistic expectations; un- also clarify personal values by either implicitly or<br />
clear values; unclear norms; unwanted pressure; explicitly asking individuals to consider the personal<br />
inadequate support; and inadequate personal and importance they place on each benefit and risk and to<br />
external resources to make the <strong>decision</strong>. Since these identify the tradeoffs they will need to make in<br />
factors also contribute to <strong>decision</strong>al conflict [16], choosing one alternative. As a consequence, there<br />
high <strong>decision</strong>al conflict or uncertainty which results may be better congruence between a person’s values<br />
in <strong>decision</strong> delay can also be addressed. Decision and their choice.<br />
support includes providing tailored in<strong>for</strong>mation, Another potential mechanism <strong>for</strong> creating realistic<br />
clarifying values, and augmenting self-help skills in expectations and clarifying values lies in the detailed<br />
<strong>decision</strong> making and implementation. The mecha- descriptions of benefits and risks depicting their<br />
nisms whereby each of these interventions addresses impact on physical, emotional, and social function.<br />
the suboptimal determinants [16,7] are described Decision makers tend to judge the likelihood of an<br />
below. outcome [14] in accordance with: (a) the ease with<br />
Decision <strong>aid</strong>s include in<strong>for</strong>mation about the prob- which they can imagine it (availability heuristic); and<br />
lem, alternatives, and benefits and risks to improve (b) their belief that they represent the type of person<br />
knowledge of the <strong>decision</strong>. Probabilities tailored to who would normally experience the outcome (reprethe<br />
client’s clinical risk are included to create more sentativeness heuristic). They are also better able to<br />
realistic expectations or subjective judgements of the <strong>for</strong>m an opinion about the value of an outcome when
270 A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279<br />
Table 1<br />
Definitions of determinants of <strong>decision</strong>s in the <strong>decision</strong> support framework<br />
(1) Client’s and practitioner’s sociodemographic and clinical characteristics<br />
Client: age, gender, education, ethnicity, occupation, locale, diagnosis and duration of condition, health status (physical, emotional,<br />
cognitive, social)<br />
Practitioner: age, gender, ethnicity, clinical education and specialty, practice locale, years of experience<br />
(2) Client’s and practitioner’s perceptions of the <strong>decision</strong><br />
Knowledge Cognizance of the clinical problem, alternatives and rationale, consequences (benefits, risks)<br />
Expectations Perceived likelihood or probability of benefits and risks<br />
Values Desirability or personal importance of benefits and risks; under conditions of uncertainty, utilities become<br />
values which incorporate not only desirability but also attitude toward risk<br />
Decisional conflict Uncertainty about course of action to take arising from factors inherent in the <strong>decision</strong> (uncertainty of outcomes,<br />
or the need to make value tradeoffs between benefits and risks) and modifiable factors (inadequate knowledge,<br />
unrealistic expectations, unclear values and norms, unwanted social pressure, inadequate social support, lack of<br />
other resources).<br />
(3) Client’s and practitioner’s perceptions of important others regarding the <strong>decision</strong><br />
Norms Perceptions of what important others think is the appropriate choice. For the client, important others may<br />
include their spouse, family, peers, and practitioner(s). For the practitioners, it may include the client,<br />
professional peers, and personal network.<br />
Pressure Perception of persuasion, influence, coercion from important others to select one alternative<br />
Support In<strong>for</strong>mational, emotional, and tangible help from important others to bolster and sustain <strong>decision</strong> making<br />
Decision participation Actual practice and preferences <strong>for</strong> participation in <strong>decision</strong> making (client controlled, shared with practitioner,<br />
roles practitioner controlled, other controlled)<br />
(4) Client’s and practitioner’s resources to make the <strong>decision</strong><br />
Personal resources<br />
Experience Previous exposure to the clinical problem, alternatives, consequences, <strong>decision</strong> making process<br />
Self-efficacy Confidence in one’s abilities in <strong>decision</strong> making, including shared <strong>decision</strong> making<br />
Motivation Readiness and interest in <strong>decision</strong> making, including shared <strong>decision</strong> making<br />
Skills Abilities in making and implementing a <strong>decision</strong><br />
Other Instrumental and financial capabilities to implement choices<br />
External resources (assets from others that are required to make and implement the <strong>decision</strong>)<br />
Type Access to in<strong>for</strong>mation, advice, emotional support, instrumental help, financial assistance, and health and social<br />
services<br />
Source Social networks, professional networks, support groups, voluntary agencies, and the <strong>for</strong>mal health care,<br />
education, and social sectors<br />
it is familiar, simple, and directly experienced [15]. menting <strong>decision</strong>s and managing their consequences.<br />
The detailed scenarios in <strong>decision</strong> <strong>aid</strong>s may translate The acquisition or re-en<strong>for</strong>cement of self-help skills<br />
an outcome into familiar, vivid functional descrip- may reduce <strong>decision</strong> delay and improve implementations<br />
with which clients can identify and may tion of <strong>decision</strong>s.<br />
provide vicarious experience from which to better Other mechanisms of <strong>decision</strong> support may imjudge<br />
the likelihood and value of each benefit and prove the quality of <strong>decision</strong> making. Helping inrisk<br />
<strong>for</strong> them. dividuals to actively consider a <strong>decision</strong> in the<br />
To address the problem of unclear norms, a context of their own clinical risks and values may<br />
<strong>decision</strong> <strong>aid</strong> may provide in<strong>for</strong>mation on experts’ enhance a person’s: perceived relevance of the<br />
and other clients’ opinions and practices and the issues; engagement in the process; self-efficacy, and<br />
underlying rationale <strong>for</strong> diverging opinions. Deci- sense of mastery and control [17]. These in turn may<br />
sions <strong>aid</strong>s or follow-up counseling may also address increase satisfaction with the <strong>decision</strong> process, the<br />
unwanted pressure, inadequate support and resources <strong>decision</strong>, and increase implementation of the deciby<br />
enhancing self-help skills in handling pressure, sion.<br />
seeking social support and external resources, imple- Decision support should also address other deter-
A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279 271<br />
minants in the DSF (practitioner and client charac- the objectives, content, and <strong>decision</strong> support methteristics,<br />
preferences <strong>for</strong> <strong>decision</strong> participation). For ods.<br />
example, a woman’s <strong>decision</strong> <strong>aid</strong> needs to be gender We structured the content of the <strong>decision</strong> <strong>aid</strong><br />
sensitive and appropriate <strong>for</strong> the age, education, and according to the ACP counseling guidelines [1] and<br />
ethnicity of the population. It needs to be flexible to delivered it using a self-administered, self-paced<br />
clients’ preferences <strong>for</strong> participation in <strong>decision</strong> booklet and audiotape. It was designed to be used by<br />
making. Shared <strong>decision</strong> making is preferred more a woman at home in preparation <strong>for</strong> a follow-up visit<br />
frequently among female, younger, and better edu- to discuss the issue with her practitioner. The 40 min<br />
cated clients [18,19], but the <strong>aid</strong> should accommo- audiotape guided a woman through a 32-page illusdate<br />
all <strong>women</strong>’s preferences. Women perceive risks trated booklet including:<br />
differently from men [20]; there<strong>for</strong>e the method of<br />
presenting risk in<strong>for</strong>mation should be acceptable to 2.1. General in<strong>for</strong>mation<br />
them.<br />
1. CHD, osteoporosis, endometrial cancer, and<br />
1.3. Evaluating <strong>decision</strong> support breast cancer including definition, incidence, median<br />
age of onset, mortality rates, and the phys-<br />
The DSF distinguishes between quality <strong>decision</strong> ical, emotional and social impact of these dismaking<br />
and quality outcomes, because good deci- eases; and major risk factors;<br />
sions can still result in bad outcomes, due to the 2. prevention and early detection strategies;<br />
stochastic nature of clinical events. Since <strong>decision</strong>s 3. HRT regimens; benefits and risks including efthat<br />
depend on client’s values cannot be judged as fects on CHD, osteoporosis, menopausal sympright<br />
or wrong, the DSF defines a high quality toms, endometrial cancer, breast cancer, side<br />
<strong>decision</strong> as in<strong>for</strong>med, consistent with personal val- effects, contraindications, and other concerns<br />
ues, and acted upon, and in which <strong>decision</strong> makers <strong>women</strong> express about taking HRT;<br />
express satisfaction with the <strong>decision</strong> making process 4. probabilities of disease with and without HRT<br />
and the <strong>decision</strong> [6,16]. Indicators of quality <strong>decision</strong> according to risk of disease and hysterectomy<br />
making may include: adequate knowledge; realistic status;<br />
expectations; clear values, congruence between values<br />
and one’s choice; low <strong>decision</strong>al conflict; deci- 2.2. Steps in weighing her own benefits and risks<br />
sion implementation, and satisfaction with the <strong>decision</strong><br />
and <strong>decision</strong> making process [6,16]. Improving Guidance was provided in completing a Personal<br />
the quality of <strong>decision</strong> making may impact favourab- Worksheet to:<br />
ly on clients’ outcomes such as: (a) persistence with<br />
the <strong>decision</strong> [21]; (b) health related quality of life, 1. identify her personal lifetime benefits and risks of<br />
which is derived, in part, from values; (c) reduced HRT tailored to her hysterectomy status, and risk<br />
distress from consequences [22,23]; (d) reduced of CHD, osteoporosis and breast cancer; review<br />
regret; (e) appropriate and efficient use of resources; her menopausal symptoms status and menstrual<br />
and (f) long-term satisfaction with care. history; and consider other issues important in the<br />
<strong>decision</strong>;<br />
2. clarify her values using a ‘weigh scale’ to rate her<br />
2. The HRT <strong>decision</strong> <strong>aid</strong> perceived importance of each benefit and risk;<br />
3. identify her current health practices in promoting<br />
The early prototypes of the HRT <strong>decision</strong> <strong>aid</strong> were healthy bones, heart, and breasts;<br />
developed using an iterative process with the re- 4. list her questions;<br />
search team and panels of clients, medical and 5. identify her preference <strong>for</strong> participation in decinursing<br />
practitioners, and educators. These groups sion making; and<br />
guided its development using criteria such as need, 6. indicate her predisposition or ‘leaning’ toward<br />
feasibility, and appropriateness and acceptability of taking HRT.
272 A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279<br />
2.3. Suggested steps <strong>for</strong> a follow-up visit with her questionnaire. The timing of our post-<strong>decision</strong> <strong>aid</strong><br />
practitioner assessment was planned to capture <strong>women</strong>’s knowledge<br />
and perceptions at what would normally be<br />
The completed Personal Worksheet provided a considered the time of <strong>decision</strong> making. However,<br />
focus <strong>for</strong> discussion <strong>for</strong> the woman to: <strong>for</strong> the current evaluation, there was no planned<br />
follow-up to discuss the issue with the woman’s<br />
1. review possible benefits and risks with her prac- family physician.<br />
titioner to verify and fill in gaps;<br />
2. discuss personal values by showing the prac- 3.2. Sample<br />
titioner her weigh scale;<br />
3. make a <strong>decision</strong> <strong>considering</strong> benefits, risks, per- We recruited 94 <strong>women</strong> including never users,<br />
sonal values, and preference <strong>for</strong> <strong>decision</strong> partici- <strong>for</strong>mer users, and current users of HRT. Inclusion<br />
pation; and criteria were: age 50–60 years; at least 2 years<br />
4. plan the next steps. postmenopausal; and, able to read English. Exclusion<br />
criteria were: HRT use less than 2 years; previous<br />
The booklet included illustrative icons to represent discontinuation of HRT due to intolerable side<br />
each concept. The text was adjusted to a Grade 8 effects; osteoporosis-associated fractures; and absoreading<br />
level, but was comprehensible to those with lute contra-indications to HRT [2]. Our inclusion and<br />
less than Grade 8 reading because of the accompany- exclusion criteria were designed to reflect the usual<br />
ing audiotape and illustrations. The data describing group of <strong>women</strong> deciding about HRT: current users<br />
lifetime risks and benefits were those used in the to determine how long they want to take it; <strong>for</strong>mer<br />
ACP guidelines from the overview of Grady et al. users <strong>for</strong> menopausal symptom relief who may not<br />
[24]. A woman used the <strong>aid</strong> in a self-paced, active want to consider it <strong>for</strong> preventive purposes, and<br />
way, responding to checklists and writing in her never users who may wish to consider it <strong>for</strong> prevenopinions.<br />
In order to familiarize herself with the tive purposes.<br />
steps in weighing the benefits and risks, she was The study received approval from the local ethics<br />
shown how four other <strong>women</strong> completed the steps review committee.<br />
be<strong>for</strong>e being asked to complete her own assessment.<br />
The four different cases also rein<strong>for</strong>ced the notion 3.3. Measures<br />
that <strong>decision</strong> making is variable and can be individualized<br />
according to a woman’s health history, Our sources of data included: a recruitment<br />
values, current health practices, and preferences <strong>for</strong> screening questionnaire; baseline and post-<strong>decision</strong><br />
<strong>decision</strong> participation. <strong>aid</strong> questionnaires; and, responses completed by<br />
participants in the <strong>decision</strong> <strong>aid</strong> group. The following<br />
client variables from the DSF were elicited: socio-<br />
3. Evaluation methods demographic and clinical variables; perceptions of<br />
the <strong>decision</strong> (knowledge, expectations, values, deci-<br />
3.1. Be<strong>for</strong>e/<strong>after</strong> study design sional conflict); and perceptions of others (pressure,<br />
support, and <strong>decision</strong> participation preferences). Ac-<br />
Participants were screened and recruited over six ceptability of the intervention was also elicited in the<br />
months from 6 family practices in downtown Ot- post-<strong>decision</strong> <strong>aid</strong> questionnaire.<br />
tawa, Canada. Following a routine office visit, the Client characteristics included age, education,<br />
participants completed a baseline questionnaire menstrual and hormonal history, hysterectomy status<br />
eliciting their knowledge, personal expectations and and clinical risks <strong>for</strong> CHD, osteoporosis, and breast<br />
importance ratings of HRT benefits and risks, current cancer.<br />
leaning toward taking HRT, and <strong>decision</strong>al conflict. Knowledge of HRT benefits, risks and side effects<br />
At the next office visit, be<strong>for</strong>e seeing their physician, as described in the <strong>decision</strong> <strong>aid</strong> was determined with<br />
participants completed the <strong>decision</strong> <strong>aid</strong> and another a 21-item questionnaire using a true/false/unsure
A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279 273<br />
response <strong>for</strong>mat. Expectations of HRT benefits and tic if they were in the appropriate quartile of<br />
risks were elicited as perceived lifetime probabilities probability (excluding the extremes of 0% or 100%)<br />
of CHD, hip fracture, and breast cancer with and as described in the <strong>decision</strong> <strong>aid</strong>.<br />
without HRT. Expectations were classified as realis- Values or importance ratings of HRT benefits and<br />
Fig. 2. Relationship between <strong>women</strong>’s values and their <strong>decision</strong>s to take HRT.
274 A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279<br />
risks were assessed: (1) using a scale anchored by 0 <strong>decision</strong>al conflict scores were found, we planned<br />
(not at all important to me) and 10 (extremely post hoc analysis of the subscales. To improve the<br />
important to me); and from the values clarification clinical interpretation of changes in scores of the<br />
exercise (Fig. 2) in which <strong>women</strong> shaded a portion expectations and <strong>decision</strong>al conflict measures, we<br />
of each benefit and risk box on the weigh scale to described each item in the scale. For each item in the<br />
indicate how important it was to them (no shading 5 <strong>decision</strong>al conflict scale, we described the percentage<br />
not at all important to me; completely shaded 5 of respondents whose score fell within the norm of<br />
extremely important to me). Values were quantified groups who make <strong>decision</strong>s (2.0 or less 5<br />
as the proportion of the height of the box that was agreement/strong agreement with positively worded<br />
shaded; the measurements were stable on retest items or disagreement/strong disagreement with<br />
(Pearson r 5 0.70–0.89) and were 95% accurate in negatively worded items).<br />
discriminating between those who accepted or de- The sample size of 94 participants was selected to<br />
clined HRT [5]. Value congruence with the <strong>decision</strong> detect an effect size of at least 0.40 on the DCS with<br />
was calculated as: the multiple correlation between Type I error of 0.05 and Type II error of 0.20. This<br />
<strong>women</strong>’s values and their <strong>decision</strong>; and the accuracy effect size was judged clinically important because<br />
of the values in discriminating between those who effect sizes observed between those who make and<br />
made different <strong>decision</strong>s. delay <strong>decision</strong>s have ranged between 0.43 and 0.82<br />
Decisional conflict or uncertainty was measured [16,25].<br />
with a Decisional Conflict Scale (DCS) which<br />
elicits: uncertainty about choosing among alterna- 3.5. Limitations<br />
tives; modifiable factors contributing to uncertainty<br />
such as feeling unin<strong>for</strong>med, unclear about values and The lack of a control group precluded controlling<br />
unsupported in <strong>decision</strong> making; and perceived <strong>for</strong> repeated measurement and co-interventions. Reeffective<br />
<strong>decision</strong> making. The scale has satisfactory sults are generalizable to <strong>women</strong> with comparable<br />
reliability and discriminates between those who characteristics including an interest in HRT and<br />
make and delay <strong>decision</strong>s [16,25]. willingness to participate in a study. We measured<br />
Two items in the DCS were also used to elicit only a subset of variables in the DSF; the impact on<br />
perceived pressure and support from others. Accep- the remaining variables especially <strong>decision</strong> imtability<br />
of the <strong>decision</strong> <strong>aid</strong> was assessed in terms of: plementation, long-term persistence, and satisfaction<br />
(1) comprehensibility of each component of the with the <strong>decision</strong> cannot be ascertained. The inter<strong>decision</strong><br />
<strong>aid</strong> on a 100 mm visual analogue scale vention did not include follow-up with a practitioner;<br />
anchored by ‘poor’ to ‘excellent’; and (2) the length, there<strong>for</strong>e, some participants may have only been<br />
pace, amount of in<strong>for</strong>mation, and balance using making a hypothetical <strong>decision</strong>.<br />
structured response categories. Decisions were assessed:<br />
(1) as a ‘leaning’ toward taking HRT on a<br />
15-point scale anchored by ‘yes <strong>hormone</strong>s’ and ‘no 4. Results<br />
<strong>hormone</strong>s’ with ‘unsure’ at the mid-point; and (2) as<br />
a choice (yes, no, unsure). The test–retest Pearson r Demographic and clinical characteristics (summacoefficients<br />
<strong>for</strong> each approach were 0.95 and 0.91, rized in Table 2) show that participants were approxrespectively<br />
[5]. imately equally distributed in terms of their age<br />
group, current use of HRT, and hysterectomy status.<br />
3.4. Analysis plan and sample size The majority of participants: had at least some post<br />
secondary education; preferred to share <strong>decision</strong><br />
After describing the characteristics of our sample making with their practitioner; had at least one risk<br />
and their <strong>decision</strong> participation preferences, we factor <strong>for</strong> CHD; and did not report having low bone<br />
evaluated the expected changes in the following DSF density or a first degree relative with breast cancer.<br />
variables using paired t-tests: <strong>decision</strong>al conflict, The characteristics of the sample were comparable to<br />
knowledge; and, expectations. If changes in the total regional census and survey data except <strong>for</strong> propor-
A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279 275<br />
Table 2<br />
Demographic and clinical characteristics of the participants<br />
Variable Study participants n 5 94<br />
a<br />
Regional data<br />
% (95% Confidence Interval) % (95% Confidence Interval)<br />
Age<br />
50–55 51 (41,61) 50<br />
56–60<br />
Highest education level<br />
49 (41,61) 50<br />
, High school diploma 20 (13,29) 25<br />
High school diploma 17 (10,26) 18<br />
Some post-secondary 32 (23,41) 40<br />
University degree<br />
HRT use<br />
31 (22,41) 17<br />
Current use 47 (37,60) 35 (29,41)<br />
Previous use 16 (10,24) 15 (11,20)<br />
Never use<br />
HRT <strong>decision</strong> participation preferences<br />
37 (28,47) 50 (44,56)<br />
Woman decides <strong>after</strong> opinion from practitioner 21<br />
Shared 63<br />
Practitioner decides 5<br />
Unsure 11<br />
Hysterectomy<br />
CHD (Coronary Heart Disease) risk factors<br />
46<br />
Early family history 39<br />
Hypertension 25<br />
Smokers 17<br />
High cholesterol 14<br />
Diabetes 11<br />
At least 1 risk factor 54<br />
Low bone density 7<br />
Mother or sister has breast cancer 14<br />
a Education data is from the regional census. Clinical data is from regional surveys.<br />
tion with university degrees, which was higher in the using the <strong>decision</strong> <strong>aid</strong> are summarized in Table 4.<br />
study sample. There were statistically significant improvements in<br />
Changes in Decisional Conflict <strong>after</strong> using the knowledge ( p 5 0.001) with respondents having<br />
<strong>decision</strong> <strong>aid</strong> are summarized in Table 3. There was a approximately half of the test items correct be<strong>for</strong>e<br />
statistically significant decline in total <strong>decision</strong>al the <strong>decision</strong> <strong>aid</strong> and three quarters correct <strong>after</strong> the<br />
conflict scores ( p 5 0.001). When each subscale was <strong>decision</strong> <strong>aid</strong>. Expectation scores also improved ( p 5<br />
examined, the 95% confidence limits of the differ- 0.001) with respondents having approximately a<br />
ences between group means had no overlap with zero third of their expectations realistic be<strong>for</strong>e the deci<strong>for</strong><br />
the subscales of feeling uncertain, unin<strong>for</strong>med, sion <strong>aid</strong> and slightly over half <strong>after</strong> the <strong>decision</strong> <strong>aid</strong>.<br />
unclear about values, and unsupported in <strong>decision</strong> There were improvements in all expectations, most<br />
making. There was overlap with zero <strong>for</strong> the sub- notably in <strong>women</strong>’s expectations of outcomes with<br />
scale of perceiving one has made an ineffective HRT (32% to 46%). When unrealistic expectations<br />
<strong>decision</strong>. When individual scale items were ex- were classified as high or low <strong>for</strong> each outcome,<br />
amined, there were improvements in all but one scale (data not shown), we found that participants with<br />
item, with improvements ranging from 2% to 36%. unrealistic expectations of outcomes without any<br />
Changes in Knowledge and Expectations <strong>after</strong> HRT consistently underestimated their risk of CHD
276 A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279<br />
Table 3<br />
Post-<strong>decision</strong> <strong>aid</strong> changes in <strong>decision</strong>al conflict (n 5 94)<br />
Be<strong>for</strong>e <strong>aid</strong> After <strong>aid</strong><br />
Mean (S.D.) Mean (S.D.) t statistic p value<br />
a<br />
(1) Total DCS score 2.5 (0.7) 2.2 (0.5) 3.9 0.001<br />
(2) Subscore Mean (S.D.) Mean (S.D.) Difference 95% CL<br />
(a) Uncertainty 2.9 (1.2) 2.5 (1.1) 0.1 (0.5,0.1)<br />
(b) Unin<strong>for</strong>med 2.5 (1.0) 1.9 (0.6) 0.2 (0.5, 0.8)<br />
(c) Unclear values 2.6 (0.8) 2.2 (0.6) 0.3 (0.6, 0.2)<br />
(d) Unsupported 2.8 (0.7) 2.6 (0.7) 0.2 (0.4, 0.07)<br />
(e) Ineffective choice 2.2 (0.6) 2.1 (0.6) 0.2 (0.3,-0.05)<br />
b<br />
(3) Percentage expressing no problems with each DCS item (score 2 or less )<br />
% % Difference<br />
(a)<br />
55 1E2asy choice 43<br />
Sure what to do 43 68 25<br />
Clear best choice<br />
(b)<br />
57 65 8<br />
89 1K8 now alternatives 71<br />
Know HRT benefits 54 85 31<br />
Know HRT risks<br />
(c)<br />
47 83 36<br />
Aware importance of ben-<br />
89 1efi6ts 73<br />
Aware importance of risks 72 92 20<br />
Sure which more important<br />
(d)<br />
30 49 19<br />
Feel no pressure from<br />
83 o0thers 83<br />
Have enough support 48 50 2<br />
Have enough advice<br />
(e)<br />
13 34 21<br />
78 1I2n<strong>for</strong>med choice 66<br />
Reflects values 83 87 4<br />
Will stick with 68 70 2<br />
Satisfied with 74 78 4<br />
a<br />
DCS scores are calculated by summing each item (ranging from 1 to 5) and dividing by the number of items. Scores theoretically range<br />
from 1 (low <strong>decision</strong>al conflict) to 5 (high <strong>decision</strong>al conflict). According to the scale norms, groups who delay choices have average<br />
<strong>decision</strong>al conflict scores above 2.5; those who make choices have average scores of 2 or less.<br />
b<br />
To score 2 or less on one single item, a respondent agrees or strongly agrees with a positively worded item or disagrees/strongly disagrees<br />
with a negatively worded item.<br />
S.D. 5 standard deviation.<br />
and overestimated their risk of breast cancer. Virtual- importance ratings, the multiple correlation coeffily<br />
all of the <strong>women</strong>’s unrealistic expectations with cients were 0.40 be<strong>for</strong>e the <strong>decision</strong> <strong>aid</strong> and 0.56<br />
HRT were in the direction of overestimating the <strong>after</strong> the <strong>decision</strong> <strong>aid</strong>. When we used discriminant<br />
positive effects on CHD and osteoporosis and also function analysis to examine congruence between<br />
overestimating the negative effect on breast cancer. <strong>decision</strong>s <strong>after</strong> using the <strong>aid</strong> and importance ratings<br />
When change in value congruence with the deci- from the weigh scale in the <strong>decision</strong> <strong>aid</strong>, <strong>women</strong>’s<br />
sion was assessed by examining the multiple correla- values were 84% accurate in discriminating between<br />
tion coefficients between leaning toward HRT and choices. As shown in Fig. 2, those choosing HRT
A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279 277<br />
Table 4<br />
Post-<strong>decision</strong> <strong>aid</strong> changes in knowledge and realistic expectations (n 5 94)<br />
Be<strong>for</strong>e <strong>aid</strong> After <strong>aid</strong><br />
a<br />
(1) Knowledge score Mean (S.D.) Mean (S.D.) Mean diff. (S.D.) p value<br />
54 (19) 75 (21) 21 (20) 0.001<br />
b<br />
(2) Realistic expectations score Mean (S.D.) Mean (S.D.) Mean diff. (S.D.) p value<br />
32 (19) 55 (28) 23 (22) 0.001<br />
(3) Percentage realistic expectations % % Difference<br />
CHD without HRT 29% 39% 10%<br />
Hip fracture without HRT 34% 44% 10%<br />
Breast cancer without HRT 41% 51% 10%<br />
CHD with HRT 22% 57% 35%<br />
Hip fracture with HRT 14% 57% 46%<br />
Breast cancer with HRT 43% 75% 32%<br />
a Knowledge score calculated as the percentage items correct.<br />
b Realistic defined as a response within the correct quartile on a probability scale ranging from 0% to 100%, excluding the extremes of 100%<br />
and 0%. Total score calculated as the percentage of expectations measured that were realistic.<br />
S.D. 5 standard deviation.<br />
Table 5<br />
Change in <strong>women</strong>’s predisposition to take HRT <strong>after</strong> exposure to a <strong>decision</strong> <strong>aid</strong> (n 5 94)<br />
Be<strong>for</strong>e <strong>decision</strong> <strong>aid</strong> After <strong>decision</strong> <strong>aid</strong><br />
Leaning ‘Yes’ Unsure Leaning ‘No’<br />
(n 5 52) (n 5 19) (n 5 23)<br />
Leaning ‘Yes’ (n 5 47) 44 3 0<br />
Unsure (n 5 28) 7 15 6<br />
Leaning ‘No’ (n 5 19) 1 1 17<br />
placed more importance on the benefits compared to 5. Discussion<br />
the risks; those declining HRT placed more importance<br />
on the risks. For those who were unsure, the This be<strong>for</strong>e/<strong>after</strong> study demonstrated that the<br />
importance they placed on the benefits was compar- <strong>decision</strong> <strong>aid</strong> per<strong>for</strong>med according to the predictions<br />
able to those placed on the risks. Moreover, the of the DSF: reducing uncertainty, increasing knowlbenefit<br />
side of the scale was similar to those choos- edge, creating realistic expectations, clarifying valing<br />
HRT; on the risk side, it was similar to those ues, and supporting <strong>decision</strong> making. It is promising<br />
declining HRT. that over half of the <strong>women</strong> exposed to a <strong>decision</strong><br />
Changes in the participants’ predisposition to <strong>aid</strong> had good general knowledge and realistic extaking<br />
HRT are presented in Table 5. There was little pectations, and felt they had enough advice to make<br />
change in the groups whose baseline predispositions a <strong>decision</strong>. Considering the large numbers of <strong>women</strong><br />
were strongly polarized either toward choosing or who will reach menopausal age over the next decade,<br />
toward declining HRT. Most of the change took the self-administered <strong>decision</strong> <strong>aid</strong> has the potential to<br />
place in the group who were unsure at baseline, with streamline follow-up counseling with their practitionroughly<br />
equal numbers of the unsure group choosing ers. It provides the clinician with a summary of the<br />
to accept or decline HRT <strong>after</strong> using the <strong>decision</strong> <strong>aid</strong>. woman’s benefit/risk profile, values, questions and
278 A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279<br />
predispositions, and may facilitate triaging according practitioners <strong>for</strong> shared <strong>decision</strong> making, the <strong>decision</strong><br />
to the type and level of counseling required. <strong>aid</strong>’s impact on the client–practitioner interaction;<br />
One of the clear benefits of <strong>decision</strong> <strong>aid</strong>s is to and long-term efficacy and efficiency. Are <strong>decision</strong><br />
create more realistic expectations of benefits and <strong>aid</strong>s superior to usual approaches in primary care?<br />
risks by providing detailed probabilistic in<strong>for</strong>mation What else is needed besides the <strong>women</strong>’s <strong>decision</strong><br />
according to the woman’s clinical risk profile. With- <strong>aid</strong> to prepare practitioners <strong>for</strong> shared <strong>decision</strong><br />
out this in<strong>for</strong>mation, <strong>women</strong> underestimate their risk making? What are the effects of the <strong>decision</strong> <strong>aid</strong><br />
of heart disease, overestimate their risk of breast <strong>after</strong> <strong>women</strong> discuss HRT with their practitioners at<br />
cancer, and overestimate the potential benefits and follow-up visits? Does the <strong>aid</strong> streamline the process,<br />
risks from HRT. It remains to be seen if the re- improve <strong>women</strong>’s and practitioners’ satisfaction with<br />
alignment of expectations will have positive effects their interaction, reduce remaining <strong>decision</strong>al conon<br />
outcomes such as fear, regret, and <strong>decision</strong> flict, and improve satisfaction with the choice that is<br />
persistence. eventually made? What are the effects of the deci-<br />
The improved clarity of values from using the sion <strong>aid</strong> on long-term persistence with the <strong>decision</strong>,<br />
<strong>decision</strong> <strong>aid</strong> may have been due to the weigh scale distress from HRT side effects, and post-<strong>decision</strong>al<br />
exercise. By leading <strong>women</strong> through a series of regret? Such questions are currently being evaluated<br />
different examples of how other <strong>women</strong> have judged in our randomized controlled trial which includes<br />
the personal importance of the benefits and risks, preparatory materials <strong>for</strong> practitioners as well as<br />
they learned how values contribute to a <strong>decision</strong> and <strong>women</strong>, analysis of client–practitioner interactions,<br />
were prepared to per<strong>for</strong>m the exercise <strong>for</strong> them- and longer-term follow-up.<br />
selves. A second explanation is that respondents In conclusion, our <strong>decision</strong> <strong>aid</strong> prepared <strong>women</strong><br />
were better able to <strong>for</strong>m an opinion about the value <strong>for</strong> <strong>decision</strong> making about HRT. By individualizing<br />
of an outcome [15] because of the detailed descrip- the <strong>decision</strong> according to their clinical risk profiles<br />
tions of how CHD, osteoporosis, and breast cancer and values, <strong>women</strong> had less uncertainty, better<br />
affects <strong>women</strong>’s lives. knowledge, more realistic expectations, clearer val-<br />
Although the <strong>decision</strong> <strong>aid</strong> had a favourable impact ues, and felt more supported in their <strong>decision</strong>. Future<br />
on <strong>women</strong>’s com<strong>for</strong>t with the process used to arrive evaluations are required to examine their effects<br />
at their choice, it had little impact on their <strong>decision</strong> relative to usual care and on practitioner–client<br />
per se. However, these results were confounded by<br />
two factors: (1) <strong>women</strong>’s previous experience with<br />
<strong>decision</strong> making about HRT, which may have en-<br />
interactions and long-term behaviour.<br />
trenched their views; and (2) the rather hypothetical<br />
nature of the <strong>decision</strong> making which did not involve<br />
Acknowledgements<br />
planned follow-up with their physicians. Future<br />
evaluations should focus on <strong>women</strong> who are actually<br />
<strong>considering</strong> the issue <strong>for</strong> the first time with their<br />
This project was supported by the Institute of<br />
Clinical Evaluative Sciences in Ontario, Toronto,<br />
Ontario, Canada and the Medical Research Council<br />
practitioners and changes should be monitored <strong>after</strong><br />
of Canada.<br />
reviewing the <strong>decision</strong> <strong>aid</strong> and <strong>after</strong> counseling by<br />
their practitioners.<br />
The lack of difference in the DCS effective<br />
<strong>decision</strong> making subscale is intriguing. The scale References<br />
may not be sensitive to change. Alternatively, it may<br />
only be useful when <strong>women</strong> are asked to reflect on a [1] American College of Physicians. Guidelines <strong>for</strong> counselling<br />
<strong>decision</strong> they are actually about to make.<br />
postmenopausal <strong>women</strong> about preventive <strong>hormone</strong> <strong>therapy</strong>.<br />
Ann Intern Med 1992;117(12):1038–41.<br />
Although we are encouraged by the generally<br />
[2] Society of Obstetricians and Gynaecologists of Canada,<br />
favourable effects of the <strong>decision</strong> <strong>aid</strong>, there are Canadian Menopause Consensus Conf. JSOGC 1994;16:4–<br />
outstanding questions about: the relative efficacy of 40.<br />
the <strong>aid</strong> compared to usual care; the preparation of [3] Kroll JC, Rothert ML, Rovner D et al. Decision support
A.M. O’Connor et al. / Patient Education and Counseling 33 (1998) 267 –279 279<br />
interventions: More is not necessarily better. Med Dec [15] Fischhoff B, Slovic P, Lichtenstein, S. Knowing what you<br />
Making 1994;14(4):440 (Abstract). want: Measuring labile values. In: Wallsten TS, ed. Cogni-<br />
[4] Mort EA. Clinical <strong>decision</strong> making in the face of uncertainty: tive processes in choice and <strong>decision</strong> behavior. Hillsdale, NJ:<br />
Hormone replacement <strong>therapy</strong> as an example. J Family Lawrence Erlbaum, 1980.<br />
Practice 1996;42:147–51. [16] O’Connor AM. Validation of a <strong>decision</strong>al conflict scale. Med<br />
[5] O’Connor A, Tugwell P, Wells G. Testing a portable, self- Dec Making 1995;15(1):25–30.<br />
administered <strong>decision</strong> <strong>aid</strong> <strong>for</strong> post-menopausal <strong>women</strong> con- [17] Bandura A. Self-efficacy mechanism in human agency.<br />
sidering long-term <strong>hormone</strong> replacement <strong>therapy</strong> to prevent American Psychologist 1982;37:122–47.<br />
osteoporosis and heart disease. Med Dec Making [18] Degner LF, Russell C. Preferences <strong>for</strong> treatment control<br />
1994;14(4):438 (Abstract). among adults with cancer. Res Nursing Health 1988;11:367–<br />
[6] Hayward R, pers. comm., McMaster University. 74.<br />
[7] O’Connor A, Llewellyn-Thomas H, Sawka C et al. Physi- [19] Blanchard CG, Labreque MS, Ruckdeschel JC et al. Incians’<br />
opinions about <strong>decision</strong> <strong>aid</strong>s <strong>for</strong> patients <strong>considering</strong> <strong>for</strong>mation and <strong>decision</strong> making preferences of hospitalized<br />
systemic adjuvant <strong>therapy</strong> <strong>for</strong> axillary-node negative breast adult patients. Soc Sci Med 1988;27:1139–45.<br />
cancer. Patient Edu Counsel 1997;30:143–53. [20] Flynn J, Slovic P, Mertz CK. Gender, race, and perception of<br />
[8] Keeney RL, Raiffa H. Decisions with multiple objectives: environmental health risks. Risk Analysis 1994;14:1101–8.<br />
Preferences and value tradeoffs. New York: John Wiley and [21] Haynes R, Taylor D, Sackett D. Compliance in health care.<br />
Sons, 1976. Baltimore: John Hopkins University Press, 1979.<br />
[9] Feather NT. Expectations and actions: Expectancy–value [22] Padilla GV, Grant MM, Rains BL et al. Distress reduction<br />
models in psychology. Hillsdale NJ: Lawrence Erlbaum, and the effects of preparatory teaching films and patient<br />
1982. control. Res Nur Health 1981;4:375–87.<br />
[10] Janis IL, Mann L. Decision making. New York: The Free [23] O’Connor A, Pennie R, Dales R. Framing effects on<br />
Press, 1977. expectations, <strong>decision</strong>s and side effects experienced: The<br />
[11] Orem DE. Nursing: Concepts of practice, 5th ed. Toronto: case of influenza immunization. J Clin Epidemiol<br />
Mosby, 1995. 1996;49(11):1271–6.<br />
[12] Norbeck JS. Social support. Annual Rev Nur Res 1988;6:85– [24] Grady D, Rubin SM, Petitti DB et al. Hormone <strong>therapy</strong> to<br />
109. prevent disease and prolong life in postmenopausal <strong>women</strong>.<br />
[13] Ajzen I, Fishbein M. Understanding attitudes and predicting Ann Intern Med 1992;117(12):1016–37.<br />
social behaviour. Englewood Cliffs: Prentice Hall, 1980. [25] Bunn H, O’Connor AM. Validation of client <strong>decision</strong> making<br />
[14] Tversky A, Kahneman D. The framing of <strong>decision</strong>s and the instruments in the context of psychiatry. Can J Nurs Res<br />
psychology of choice. Science 1981;211:453–8. 1996;28(3):13–27.