Common Behavioural Disorders in Children
Common Behavioural Disorders in Children
Common Behavioural Disorders in Children
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
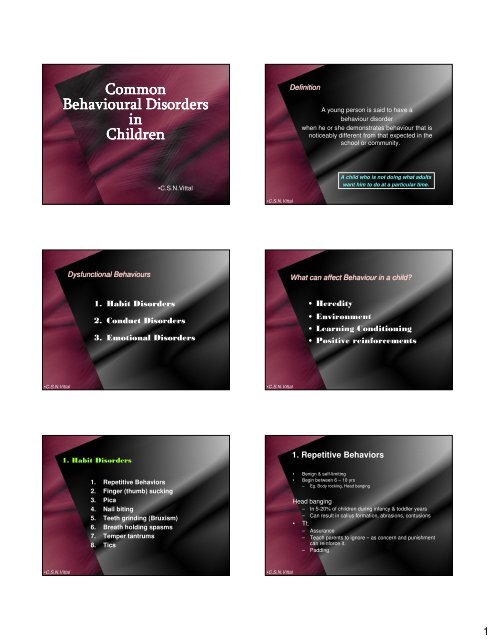
<strong>Common</strong><br />
<strong>Common</strong><br />
<strong>Behavioural</strong> <strong>Behavioural</strong> <strong>Disorders</strong><br />
<strong>Disorders</strong><br />
<strong>in</strong><br />
<strong>Children</strong><br />
<strong>Children</strong><br />
Dysfunctional Behaviours<br />
1. Habit <strong>Disorders</strong><br />
•C.S.N.Vittal<br />
2. Conduct <strong>Disorders</strong><br />
3. Emotional <strong>Disorders</strong><br />
1. Habit <strong>Disorders</strong><br />
1. Repetitive Behaviors<br />
2. F<strong>in</strong>ger (thumb) suck<strong>in</strong>g<br />
3. Pica<br />
4. Nail bit<strong>in</strong>g<br />
5. Teeth gr<strong>in</strong>d<strong>in</strong>g (Bruxism)<br />
6. Breath hold<strong>in</strong>g spasms<br />
7. Temper tantrums<br />
8. Tics<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
Def<strong>in</strong>ition<br />
A young person is said to have a<br />
behaviour disorder<br />
when he or she demonstrates behaviour that is<br />
noticeably different from that expected <strong>in</strong> the<br />
school or community.<br />
A child who is not do<strong>in</strong>g what adults<br />
want him to do at a particular time.<br />
What can affect Behaviour <strong>in</strong> a child?<br />
• Heredity<br />
• Environment<br />
• Learn<strong>in</strong>g Condition<strong>in</strong>g<br />
• Positive re<strong>in</strong>forcements<br />
1. Repetitive Behaviors<br />
• Benign & self-limit<strong>in</strong>g<br />
• Beg<strong>in</strong> between 6 – 10 yrs<br />
– Eg. Body rock<strong>in</strong>g, Head bang<strong>in</strong>g<br />
Head bang<strong>in</strong>g<br />
– In 5-20% of children dur<strong>in</strong>g <strong>in</strong>fancy & toddler years<br />
– Can result <strong>in</strong> callus formation, abrasions, contusions<br />
• Tt.<br />
– Assurance<br />
– Teach parents to ignore – as concern and punishment<br />
can re<strong>in</strong>force it.<br />
– Padd<strong>in</strong>g<br />
1
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
2.F<strong>in</strong>ger (Thumb) suck<strong>in</strong>g & Nail Bit<strong>in</strong>g<br />
• Sensory solace for child<br />
(“<strong>in</strong>ternal strok<strong>in</strong>g”) to<br />
cope with stressful<br />
situation <strong>in</strong> <strong>in</strong>fants and<br />
toddlers.<br />
• Re<strong>in</strong>forced by attention<br />
from parents.<br />
• Predispos<strong>in</strong>g factors:<br />
Developmental delay<br />
Neglect<br />
2.F<strong>in</strong>ger (Thumb) suck<strong>in</strong>g & Nail Bit<strong>in</strong>g<br />
Management<br />
• Reassure parents that it’s transient.<br />
• Improve parental attention / nurtur<strong>in</strong>g.<br />
• Teach parent to ignore; and give more<br />
attention to positive aspects of child’s<br />
behavior.<br />
• Provide child praise / reward for substitute<br />
behaviors.<br />
• Bitter salves, thumb spl<strong>in</strong>ts, gloves may be<br />
used to reduce thumb suck<strong>in</strong>g.<br />
3.Temper Tantrums<br />
Precipitationg factors<br />
• Hunger<br />
• Fatigue<br />
• Lack of sleep<br />
• Innate personality of child<br />
• Ineffective parental skills<br />
• Over pamper<strong>in</strong>g<br />
• Dysfunctional family / Family violence<br />
• School aversion<br />
•C.S.N.Vittal<br />
2.F<strong>in</strong>ger (Thumb) suck<strong>in</strong>g & Nail Bit<strong>in</strong>g<br />
• Most give up by 2 yrs<br />
• If cont<strong>in</strong>ued beyond 4 yrs –<br />
number of squelae<br />
• If resumed at 7 – 8 yrs : sign of<br />
Stress<br />
• Adverse Effects<br />
– Malocclusion – open bite<br />
– Mastication difficulty<br />
– Speech difficulty (D and T)<br />
– Lisp<strong>in</strong>g<br />
3.Temper Tantrums<br />
– Paronychia and digital<br />
abnormalities<br />
• In 18 months to 3 yr olds due to<br />
development of sense of autonomy.<br />
• Child displays defiance, negativism /<br />
oppositionalism by hav<strong>in</strong>g temper tantrums.<br />
• Normal part of child development.<br />
• Gets re<strong>in</strong>forced when parents respond to it<br />
by punitive anger.<br />
• Child wrongly learns that temper tantrums<br />
are a reasonable response to frustration.<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
3.Temper Tantrums –<br />
Management<br />
• In general, parents advised to:<br />
Set a good example to child<br />
Pay attention to child<br />
Spend quality time<br />
Have open communication with child<br />
Have consistency <strong>in</strong> behavior<br />
• Dur<strong>in</strong>g temper tantrum:<br />
Parents to ignore child and once child is calm, tell child<br />
that such behavior is not acceptable<br />
Verbal reprimand should not be abusive<br />
Never beat or threaten child<br />
Impose “Time Out” - if temper tantrum is disruptive, out<br />
of control and occurr<strong>in</strong>g <strong>in</strong> public place.<br />
2
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
4.Even<strong>in</strong>g Colic<br />
• Intermittent episodes of abdom<strong>in</strong>al pa<strong>in</strong> and<br />
severe cry<strong>in</strong>g <strong>in</strong> normal <strong>in</strong>fants<br />
• Beg<strong>in</strong>s at 1-2 wks age and persists till 3-4 mo.<br />
• Cry<strong>in</strong>g usually <strong>in</strong> late afternoon or even<strong>in</strong>g<br />
• Diagnosis :<br />
“ Infant cries for > 3 hrs per day for > 3 day<br />
per week for > 3 weeks”<br />
4.Even<strong>in</strong>g Colic<br />
Attack<br />
• Beg<strong>in</strong>s suddenly with a loud cry<br />
• Cry<strong>in</strong>g cont<strong>in</strong>uous – lasts for several<br />
hours – mostly <strong>in</strong> the late afternoon or<br />
even<strong>in</strong>gs<br />
• Face becomes red and legs drawn up<br />
on the abdomen<br />
• Abdomen becomes tense<br />
• Attack term<strong>in</strong>ates after exhaustion or<br />
after passage of flatus or feces<br />
5.Stranger Reaction / Anxiety<br />
By 6-7 months age <strong>in</strong>fant can differentiate from<br />
primary care givers and others<br />
At this age they develop fear of others.<br />
This may last for a few months to peak around<br />
13-15 months<br />
If <strong>in</strong>fant on approach of stranger behaves with<br />
more <strong>in</strong>tense discomfort – such as<br />
cont<strong>in</strong>uous cry<strong>in</strong>g, vomit<strong>in</strong>g, refusal to<br />
socialize : Stranger anxiety.<br />
It might be an <strong>in</strong>dication for later development of<br />
behavioural problem as separation anxiety.<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
4.Even<strong>in</strong>g Colic<br />
Cause<br />
• Not known<br />
• More likely if the child is over active and<br />
parents are over anxious<br />
• Could be a manifestation of<br />
• hunger,<br />
• aerophagia,<br />
• cow’s milk <strong>in</strong>tolerance,<br />
• immaturity of <strong>in</strong>test<strong>in</strong>e,<br />
• overfeed<strong>in</strong>g,<br />
• <strong>in</strong>take of food with high CHO content<br />
4.Even<strong>in</strong>g Colic<br />
Management<br />
Dur<strong>in</strong>g Episode<br />
– Hold the child erect or prone<br />
– Avoid drugs<br />
– No much role to antispasmodics, carm<strong>in</strong>atives,<br />
simethicone, suppositories or enemas<br />
Counsel<strong>in</strong>g - Cop<strong>in</strong>g with the parents<br />
– Reassure the parents that <strong>in</strong>fant is not sick<br />
– They need to soothe more with repetitive sound<br />
and stimulate less with decrease <strong>in</strong> pick<strong>in</strong>g up and<br />
feed<strong>in</strong>g with every cry<br />
5.Stranger Reaction / Anxiety<br />
Management<br />
• Teach relaxation technique such as<br />
slowly expos<strong>in</strong>g them to stranger,<br />
– <strong>in</strong>itially from a distance<br />
– Ask<strong>in</strong>g them to greet and slowly<br />
advance<br />
• Reassure the parents that the<br />
behaviour gradually decl<strong>in</strong>es<br />
– But if persists, refer to child psychiatrist<br />
3
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
6.Pica<br />
Repeated or chronic <strong>in</strong>gestion of<br />
non-nutritive substances.<br />
– Examples: mud, pa<strong>in</strong>t, clay, plaster,<br />
charcoal, soil.<br />
• It’s an eat<strong>in</strong>g disorder.<br />
• Normal <strong>in</strong> <strong>in</strong>fants and toddlers.<br />
• Pass<strong>in</strong>g phase.<br />
6.Pica<br />
Pica after 2nd yr of life needs <strong>in</strong>vestigation<br />
• Predispos<strong>in</strong>g factors :<br />
Parental neglect<br />
Poor supervision<br />
Mental retardation<br />
Lack of affection Psychological neglect,<br />
orphans)<br />
Family disorganization<br />
Lower socioeconomic class<br />
Autism<br />
7.Breath Hold<strong>in</strong>g Spasms<br />
• Behavioral problem <strong>in</strong> <strong>in</strong>fants and<br />
toddlers.<br />
• Child cries and then holds breath<br />
until limp.<br />
• Cyanosis may occur.<br />
• Sometimes, loss of consciousness,<br />
or even seizure can occur.<br />
• It is child’s attempt to control<br />
environment: parents /caregivers.<br />
• Benign condition: no risk of epilepsy<br />
develop<strong>in</strong>g <strong>in</strong> later life.<br />
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
6.Pica<br />
Geophagia<br />
Pagophagia<br />
Hyalophagia<br />
Amylophagia<br />
Xylophagia<br />
Trichophagia<br />
Urophagia<br />
Coprophagia<br />
6.Pica<br />
•C.S.N.Vittal<br />
Eat<strong>in</strong>g of mud, soil, clay, chalk, etc.<br />
Consumption of ice<br />
Consumption of glass<br />
Consumption of starch<br />
Consumption of wood<br />
Consumption of hair<br />
Consumption of ur<strong>in</strong>e<br />
Consumption of feces<br />
• Screen<strong>in</strong>g <strong>in</strong>dicated for:<br />
Iron deficiency anemia<br />
Worm <strong>in</strong>festations<br />
Lead poison<strong>in</strong>g<br />
Family dysfunction<br />
• Treat cause accord<strong>in</strong>gly.<br />
• Usually remits <strong>in</strong> childhood but can<br />
cont<strong>in</strong>ue <strong>in</strong>to adolescence<br />
7.Breath Hold<strong>in</strong>g Spasms<br />
Management<br />
• Referral to Child Guidance Cl<strong>in</strong>ic:<br />
• Referral to Child Psychologist<br />
– If BHS accompanied with head<br />
bang<strong>in</strong>g or highly aggressive<br />
behavior<br />
4
•C.S.N.Vittal<br />
•C.S.N.Vittal<br />
8.Stutter<strong>in</strong>g / Stammer<strong>in</strong>g<br />
• Defect speech<br />
• Stumbl<strong>in</strong>g and spasmodic<br />
repetition of some syllables with<br />
pauses<br />
• Difficulty <strong>in</strong> pronounc<strong>in</strong>g<br />
consonants<br />
• Caused by spasm of l<strong>in</strong>gual and<br />
palatal muscles<br />
8.Stutter<strong>in</strong>g / Stammer<strong>in</strong>g<br />
Management<br />
• Parents should be reassured<br />
• They should not show undue concern<br />
and accept his speech without<br />
pressuriz<strong>in</strong>g him to repeat<br />
• <strong>Children</strong> should be given emotional<br />
support<br />
• Older children with secondary<br />
stutter<strong>in</strong>g should be referred to speech<br />
therapist<br />
•C.S.N.Vittal<br />
8.Stutter<strong>in</strong>g / Stammer<strong>in</strong>g<br />
• Usually beg<strong>in</strong>s between 2 – 5 yrs<br />
• Rem<strong>in</strong>d<strong>in</strong>g and ridicul<strong>in</strong>g<br />
aggravate<br />
• Child loses self confidence and<br />
become more hesitant<br />
• They can often s<strong>in</strong>g or recite<br />
poems without stutter<strong>in</strong>g<br />
Thank Thank Thank Thank QQ<br />
QQ<br />
• CSN Vittal<br />
5