IgG4-related meningeal disease: clinico-pathological ... - Pathology
IgG4-related meningeal disease: clinico-pathological ... - Pathology
IgG4-related meningeal disease: clinico-pathological ... - Pathology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Acta Neuropathol<br />
DOI 10.1007/s00401-010-0746-2<br />
ORIGINAL PAPER<br />
<strong>IgG4</strong>-<strong>related</strong> <strong>meningeal</strong> <strong>disease</strong>: <strong>clinico</strong>-<strong>pathological</strong> features<br />
and proposal for diagnostic criteria<br />
Katherine M. Lindstrom • John B. Cousar •<br />
M. Beatriz S. Lopes<br />
Received: 25 June 2010 / Revised: 3 September 2010 / Accepted: 4 September 2010<br />
Ó Springer-Verlag 2010<br />
Abstract <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> has evolved from originally<br />
being recognized as a form of pancreatitis to<br />
encompass <strong>disease</strong>s of numerous organs including the<br />
hypophysis and one reported case of dural involvement. A<br />
search of the University of Virginia, Division of Neuropathology<br />
files for 10 years identified ten cases of<br />
unexplained lymphoplasmacytic <strong>meningeal</strong> inflammation<br />
that we then evaluated using immunohistochemical stains<br />
for <strong>IgG4</strong> and IgG. Ten control cases including sarcoidosis<br />
(4), tuberculosis (1), bacterial abscess (2), Langerhans cell<br />
histiocytosis (2), and foreign body reaction (1) were also<br />
examined. The number of <strong>IgG4</strong>-positive plasma cells was<br />
counted in five high power fields (HPFs) and an average<br />
per HPF was calculated. Cases that contained greater than<br />
ten <strong>IgG4</strong>-positive cells/HPF were considered to be <strong>IgG4</strong><strong>related</strong>.<br />
Five of the study cases met these criteria, including<br />
one case of lepto<strong>meningeal</strong> inflammation. All cases<br />
exhibited the typical histological features of <strong>IgG4</strong>-<strong>related</strong><br />
<strong>disease</strong> including lymphoplasmacytic inflammation, fibrosis,<br />
and phlebitis. The dural-based lesions appear to<br />
represent a subset of the cases historically diagnosed as<br />
idiopathic hypertrophic pachymeningitis. While the lepto<strong>meningeal</strong><br />
process most closely resembles non-vasculitic<br />
autoimmune inflammatory meningoencephalitis. Given<br />
these findings, <strong>IgG4</strong>-<strong>related</strong> meningitis should be<br />
K. M. Lindstrom M. B. S. Lopes (&)<br />
Division of Neuropathology, Department of <strong>Pathology</strong>,<br />
University of Virginia School of Medicine, PO Box 800214,<br />
1215 Lee St., Charlottesville, VA 22908-0214, USA<br />
e-mail: msl2e@virginia.edu<br />
J. B. Cousar<br />
Division of Hematopathology, Department of <strong>Pathology</strong>,<br />
University of Virginia School of Medicine, PO Box 800214,<br />
1215 Lee St., Charlottesville, VA 22908-0214, USA<br />
considered in the differential diagnosis of <strong>meningeal</strong><br />
inflammatory lesions after stringent clinical and histologic<br />
criteria are used to rule out other possible diagnoses.<br />
Keywords <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong><br />
<strong>IgG4</strong>-<strong>related</strong> pachymeningitis<br />
Non-vasculitic autoimmune inflammatory<br />
meningoencephalitis<br />
Idiopathic hypertrophic pachymeningitis<br />
Central nervous system<br />
Introduction<br />
Recently, there have been numerous reports about what is<br />
currently termed ‘‘<strong>IgG4</strong>-<strong>related</strong> autoimmune/sclerosing<br />
<strong>disease</strong>s.’’ <strong>IgG4</strong> was first recognized as being associated<br />
with sclerosing <strong>disease</strong>s in 2001 when Hamano et al. [23]<br />
reported that patients with autoimmune pancreatitis (AIP)<br />
had elevated serum levels of <strong>IgG4</strong> in comparison to<br />
patients with other causes of chronic pancreatitis. Soon<br />
after this, examination of pancreatectomy specimens from<br />
patients with AIP revealed that the pancreas, as well as the<br />
surrounding tissues, was infiltrated by increased numbers<br />
of <strong>IgG4</strong>-positive plasma cells [28]. Over the years, cases of<br />
pancreatitis have been described in association with<br />
Sjögren syndrome, sclerosing cholangitis, primary biliary<br />
cirrhosis, and multifocal fibrosclerosis [16, 21, 35, 47], and<br />
it did not take long before it was demonstrated that tissues<br />
from these other organs also showed infiltration by <strong>IgG4</strong>positive<br />
plasma cells [24]. Kamisawa et al. [26] proposed<br />
the concept of an <strong>IgG4</strong>-<strong>related</strong> autoimmune/sclerosing<br />
<strong>disease</strong> that encompassed these conditions [27]. Since then,<br />
<strong>IgG4</strong> has been recognized to be associated with <strong>disease</strong>s<br />
involving numerous organs (Table 1), and these <strong>disease</strong>s<br />
123
Table 1 <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong>s<br />
Organ Disease<br />
Salivary gland Sclerosing sialadenitis [37], Mikulicz’s <strong>disease</strong><br />
[45, 61]<br />
Lung Interstitial pneumonia [55, 73], inflammatory<br />
pseudotumor [54, 69]<br />
Kidney Tubulointerstitial nephritis [57, 64]<br />
Liver Inflammatory pseudotumor [32, 67, 72],<br />
sclerosing cholangitis [67]<br />
Lacrimal gland Sclerosing dacryoadenitis [13]<br />
Retroperitoneum Retroperitoneal fibrosis [24, 63, 74]<br />
Cardiovascular Inflammatory aortic aneurysm [33]<br />
Prostate Prostatitis [65]<br />
Breast Inflammatory pseudotumor [68]<br />
Thyroid Thyroiditis [40, 42]<br />
Pituitary Autoimmune hypophysitis [53, 59, 62]<br />
Lymph nodes Lymphadenopathy [14]<br />
may occur in isolation, in various combinations, and in the<br />
absence of AIP.<br />
<strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s occur predominantly in men and<br />
are more common in the fifth to sixth decade. The patients<br />
often have hypergammaglobulinemia, elevated serum IgG<br />
[34], elevated serum <strong>IgG4</strong> [36], and the presence of autoantibodies<br />
[56]. Histologic examination of involved tissue<br />
reveals characteristic features that include lymphoplasmacytic<br />
inflammation, fibrosis, obliterative phlebitis, and<br />
increased numbers of <strong>IgG4</strong>-positive plasma cells. Other<br />
less commonly seen features are lymphoid follicles and<br />
eosinophilic infiltrates. Clinically, <strong>IgG4</strong>-<strong>related</strong> sclerosing<br />
<strong>disease</strong>s often present as a mass-like lesion that can be<br />
confused with malignancy. However, these <strong>disease</strong>s, which<br />
are believed to be autoimmune in nature, respond well to<br />
corticosteroid therapy. It is important to recognize <strong>IgG4</strong><strong>related</strong><br />
conditions so that patients do not undergo unnecessary<br />
surgical procedures.<br />
In the central nervous system, <strong>IgG4</strong> has been described<br />
in several cases of hypophysitis [53], and it has been<br />
recently reported in a case of pachymeningitis. The report<br />
by Chan et al. [10] proposes that a proportion of idiopathic<br />
hypertrophic pachymeningitis (IHP) cases may be a part of<br />
the <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> spectrum.<br />
Intraspinal IHP was first described by Charcot and<br />
Joffroy [11] and intracranial <strong>disease</strong> was described by<br />
Naffzinger [48]. This rare <strong>disease</strong> typically presents clinically<br />
with pain or symptoms of compression of the spinal<br />
cord, spinal nerves, and/or cranial nerves. On MRI, it is<br />
characterized by a marked thickening of the dura that<br />
enhances along its edges [44]. In the spine, the cervical and<br />
thoracic cord are involved most commonly [5], and intracranial<br />
<strong>disease</strong> is typically seen along the base of the<br />
brain, although it less commonly involves the cerebral<br />
123<br />
convexities [17]. In general, the differential diagnosis of dural<br />
lesions includes infections, systemic autoimmune/vasculitic<br />
<strong>disease</strong>s, and neoplasms. These etiologies must be ruled out<br />
before the diagnosis of IHP can be made. It has been previously<br />
postulated that these unexplained cases of hypertrophic<br />
pachymeningitis may be part of a systemic disorder [2, 7].<br />
Clinically and histologically IHP shares many similarities<br />
with <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s. It predominantly affects older<br />
men [41], and the thickened dura exhibits inflammatory<br />
infiltrates composed of lymphocytes and plasma cells, with<br />
occasional histiocytes, neutrophils, and eosinophils [52].<br />
In this study, we retrospectively analyzed cases with<br />
unexplained <strong>meningeal</strong> inflammation in order to (1)<br />
identify additional cases exhibiting involvement by <strong>IgG4</strong>positive<br />
plasma cells, (2) determine whether or not <strong>IgG4</strong><strong>related</strong><br />
<strong>disease</strong> represents a distinct subtype of IHP, and (3)<br />
determine the usefulness of <strong>IgG4</strong> immunostaining in distinguishing<br />
<strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> from other etiologies.<br />
Materials and methods<br />
Case selection<br />
Nine cases with dural inflammation and one case with lepto<strong>meningeal</strong><br />
inflammation were selected from the archives<br />
of the Division of Neuropathology at the University of Virginia<br />
from the period between 1999 and 2009. Study cases<br />
were identified by eliminating any specimens that contained<br />
granulomas, had positive cultures, had a prior history of<br />
neurosurgery in the area, or had any other specific CNS<br />
pathology. All study cases were originally given descriptive<br />
diagnoses after it was determined that there was no evidence<br />
of malignancy, infection, or a specific autoimmune <strong>disease</strong>.<br />
The cases consist of two resections and nine biopsies. One<br />
case without sufficient tissue was left out of the study.<br />
Ten additional cases were used as controls. These<br />
included cases of sarcoidosis (4), tuberculosis (1), bacterial<br />
abscess (2), Langerhans cell histiocytosis (2), and foreign<br />
body reaction (1).<br />
All available material from the ten study cases was<br />
reviewed. Medical records were evaluated to establish<br />
clinical presentation, laboratory and neuroimaging data,<br />
treatment, and clinical follow-up. The University of<br />
Virginia Institutional Review Board approved the study.<br />
Immunohistochemistry<br />
Acta Neuropathol<br />
Immunostains were performed using an autostainer (Dako<br />
Cytomation; Carpinteria, CA) per the manufacturer’s<br />
instructions. Antibodies used were a mouse monoclonal<br />
<strong>IgG4</strong> antibody (clone HP6025; 1:4,000 dilution; Invitrogen,<br />
Carlsbad, CA) and a rabbit polyclonal IgG antibody
Acta Neuropathol<br />
(dilution 1:3,200; Dako, Carpinteria, CA). Sections stained<br />
with <strong>IgG4</strong> were pretreated with antigen retrieval. Appropriate<br />
positive and negative controls were used. The <strong>IgG4</strong>positive<br />
control was an <strong>IgG4</strong>-rich peri-aortic lymph node<br />
associated with an abdominal aortic aneurysm.<br />
The number of <strong>IgG4</strong>-positive and IgG-positive plasma<br />
cells was counted in five high power fields (HPFs) (109<br />
eyepiece, 409 lens) containing the highest concentration of<br />
inflammation. An average number of positive cells per HPF<br />
was calculated. Cases that contained greater ten <strong>IgG4</strong>positive<br />
plasma cells/HPF were considered to be <strong>IgG4</strong><strong>related</strong><br />
according to consensus criteria that have been<br />
established for diagnosing AIP [12, 51].<br />
Tissue artifact made the IgG stain uninterpretable in one<br />
study case (case 5) and one control case (case D). A second<br />
control case (case H) did not have sufficient remaining tissue<br />
to perform IgG staining. The percentage of <strong>IgG4</strong>-positive<br />
cells to IgG-positive cells was calculated in the other cases.<br />
In situ hybridization<br />
In situ hybridization of j- and k-light chains was previously<br />
performed on three of the study cases (cases 1, 2, 3)<br />
during the initial workup of the specimens. Stains were<br />
carried out using an autostainer (BenchMark XT, Ventana<br />
Medical Systems, Tucson, AZ), as per the manufacturer’s<br />
instructions. Specific probes for j- and k-light chains were<br />
obtained from Ventana Medical Systems.<br />
PCR<br />
Three of the study cases (cases 2, 3, 6) were also previously<br />
evaluated for immunoglobulin heavy chain clonality using<br />
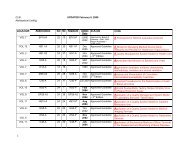
Table 2 Study cases: pathologic features<br />
Case # Lymphoplasmacytic infiltration a<br />
Fibrosis a<br />
IgH receptor DNA that was extracted from the formalinfixed<br />
paraffin-embedded tissue using a modified version<br />
of the QIAGEN QIAamp DNA purification protocol.<br />
InVivoScribe Technologies developed the primer sets<br />
utilized for PCR of the immunoglobulin heavy chain. The<br />
performance of these primers in the detection of clonal<br />
lymphoid proliferations was validated by the BIOMED-2<br />
Concerted Action Group [58]. After PCR, amplicon analysis<br />
was by capillary electrophoresis on the ABI 310<br />
instrument. Validation of this method in the molecular<br />
diagnostics laboratory at the University of Virginia has<br />
confirmed the technical performance of the assay with a<br />
detection rate from formalin-fixed paraffin-embedded tissues<br />
of 94% for B cell lymphomas. The assay is also able<br />
to detect a 1% clonal population in a polyclonal background<br />
under ideal conditions.<br />
Statistical analysis<br />
Statistical analysis was performed using the t test. A<br />
probability of P \ 0.05 was considered statistically<br />
significant.<br />
Results<br />
Five of the ten study cases (cases 1–5; Table 2), including<br />
the case of lepto<strong>meningeal</strong> inflammation, demonstrated<br />
elevated levels of <strong>IgG4</strong>-positive plasma cells (Table 2;<br />
Fig. 1). The mean number of <strong>IgG4</strong>-positive cells/HPF<br />
in these cases was 36.2 (11.8–54.2). The five non-<strong>IgG4</strong><strong>related</strong><br />
cases (cases 6–10; Table 2) had an average of<br />
0.6 <strong>IgG4</strong>-positive cells/HPF (0–2.2). The percentage of<br />
<strong>IgG4</strong>/IgG-positive plasma cells was calculated in the cases<br />
Phebitis a<br />
<strong>IgG4</strong>? cells/HPF <strong>IgG4</strong>?/IgG? Molecular profile<br />
1 Severe; giant cells present Minimal Moderate 54.2 54% j/k ISH: polytypic<br />
2 Severe Severe Severe 46.6 60% j/k ISH: polytypic<br />
IgH PCR: polyclonal B<br />
3 Severe Severe Moderate 41.6 24% j/k ISH: polytypic<br />
IgH PCR: polyclonal B<br />
4 Severe Moderate Minimal 11.8 30% ND<br />
5 Severe; lymphoid follicles; giant cells present Severe Moderate 26.8 – ND<br />
6 Moderate None None 0.4 1% IgH PCR: polyclonal B<br />
7 Minimal Severe None 0 0 ND<br />
8 Minimal Severe None 0 0 ND<br />
9 Moderate; lymphoid follicles Moderate None 2.2 8% ND<br />
10 Moderate None None 0.2 1% ND<br />
j/k ISH j- and k-light chains in situ hybridization, IgH PCR PCR for immunoglobulin heavy chain clonality<br />
a Intensity: severe, moderate, minimal<br />
123
Fig. 1 Immunohistochemistry<br />
demonstrates an increased<br />
percentage of <strong>IgG4</strong>-positive<br />
plasma cells. The inflammation<br />
is often focal, predominantly in<br />
a perivascular location. a IgG-<br />
IHC 4009, b <strong>IgG4</strong>-IHC 4009,<br />
c <strong>IgG4</strong>-IHC 2009<br />
that had interpretable immunostaining for IgG. The average<br />
percentage in the <strong>IgG4</strong>-<strong>related</strong> cases was 42% (24–60%),<br />
and it was 3% (1–8%) in the non-<strong>IgG4</strong> cases. Statistical<br />
analysis showed a significant difference between these two<br />
sets of cases (Table 3) by both mean <strong>IgG4</strong> cells/HPF and<br />
<strong>IgG4</strong>/IgG ratio.<br />
Histologic review of the <strong>IgG4</strong>-<strong>related</strong> pachymeningitis<br />
cases revealed lymphoplasmacytic inflammation infiltrating<br />
the dense connective tissue of the dura with varying<br />
amounts of sclerosis (Fig. 2). The one case with lepto<strong>meningeal</strong><br />
inflammation had a similar lymphoplasmacytic<br />
inflammatory infiltrate but less prominent sclerosis<br />
(Fig. 3). The inflammation tended to be perivascular in<br />
location, and phlebitis was present. However, obliterative<br />
phlebitis was not seen. Infiltrating macrophages were<br />
present in most cases, and rare giant cells were seen in two<br />
Table 3 Comparison of <strong>IgG4</strong>-<strong>related</strong> and non-<strong>IgG4</strong>-<strong>related</strong> cases<br />
Acta Neuropathol<br />
cases (cases 1, 5). There were occasional granulocytes in<br />
the majority of cases. One of the larger resection specimens<br />
contained several lymphoid follicles (case 5). The sample<br />
size was limited in all but two of the cases (cases 2, 5) as<br />
small biopsies were taken for diagnostic purposes only.<br />
Crush artifact distorted several of the cases and limited the<br />
evaluation of IgG in one study case.<br />
Overall, the <strong>IgG4</strong>-<strong>related</strong> cases had a higher degree of<br />
lymphoplasmacytic infiltration (Table 2). The degree of<br />
fibrosis was comparable between <strong>IgG4</strong>-<strong>related</strong> and non-<br />
<strong>IgG4</strong> cases, in particular in the cases of dural involvement.<br />
The only histological feature that appears to be predominantly<br />
seen in the <strong>IgG4</strong>-<strong>related</strong> cases was phlebitis. In none<br />
of the non-<strong>IgG4</strong> cases was phlebitis observed (Table 2).<br />
In situ hybridization of j- and k-light chains revealed a<br />
polyclonal population of plasma cells in the three studied<br />
<strong>IgG4</strong>-<strong>related</strong> (n = 5) Non-<strong>IgG4</strong>-<strong>related</strong> (n = 5) P<br />
IgG-positive plasma cells/HPF 97.3 (39.8–71.4) 17.6 (0–40.2) 0.001<br />
<strong>IgG4</strong>-positive plasma cells/HPF 36.2 (11.8–54.2) 0.6 (0–2.2) 0.02<br />
<strong>IgG4</strong>/IgG-positive plasma cell ratio (%) 42 (24–60) 3 (0–8) 0.01<br />
123
Acta Neuropathol<br />
Fig. 2 The five <strong>IgG4</strong>-<strong>related</strong><br />
cases all showed similar<br />
histological features including<br />
fibrosis with lymphoplasmacytic<br />
inflammation (a, b) and<br />
phlebitis (c). One case involving<br />
the spine had extension of the<br />
inflammation into the<br />
surrounding soft tissue (d).<br />
H&E 409, 2009, 1009, 2009<br />
cases. The three cases analyzed by PCR revealed no evidence<br />
of a clonal IgH-receptor gene rearrangement.<br />
A summary of the clinical data of the ten study cases is<br />
shown in Table 4. The cases with increased levels of <strong>IgG4</strong><br />
(cases 1–5) included two women and three men with ages<br />
ranging from 53 to 74 years. The non-<strong>IgG4</strong> cases (cases<br />
6–10) included four women and one man with an age range<br />
31–57 years. None of the patients have had the diagnosis<br />
of systemic or localized <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong><br />
(Table 1). The majority of the ten patients presented with<br />
clinical signs and symptoms due to either cord compression<br />
or pain. There were no significant differences between<br />
<strong>IgG4</strong>-<strong>related</strong> cases and non-<strong>IgG4</strong>-<strong>related</strong> cases regarding<br />
previous or concomitant systemic immunologic <strong>disease</strong>s.<br />
In fact, other than two patients (cases 1, 6) with a history of<br />
rheumatoid arthritis and one patient (case 4) with history of<br />
Chron’s <strong>disease</strong>, the majority of the patients had no contributory<br />
previous <strong>disease</strong>s.<br />
Laboratory data was remarkable for CSF abnormalities<br />
in five out of ten patients with a variable increase of protein<br />
levels and pleocytosis. However, there was no distinction<br />
between <strong>IgG4</strong>-<strong>related</strong> cases (cases 1, 2) and non-<strong>IgG4</strong><strong>related</strong><br />
cases (cases 6, 8, 10). Since the diagnosis of an<br />
<strong>IgG4</strong>-<strong>related</strong> disorder was not contemplated at the time of<br />
presentation, none of the patients had serum or CSF <strong>IgG4</strong><br />
levels performed.<br />
Other than one patient (case 4) in which clinical followup<br />
was lost immediately after surgery, all patients have<br />
been followed by a median of 16 months (10–115 months).<br />
These nine patients were treated with steroids after surgery,<br />
and two out of four <strong>IgG4</strong>-<strong>related</strong> cases were still receiving<br />
steroids at their last clinical visit. One patient (case 2) has<br />
stopped steroids since receiving radiation therapy for his<br />
spinal cord lesion for <strong>disease</strong> control.<br />
Two of the control cases had elevated numbers of<br />
<strong>IgG4</strong>-positive cells (Table 5; Fig. 4). One case consisted<br />
of tuberculous meningitis with positive cultures for<br />
M. tuberculosis, and the second was a lumbar abscess that<br />
was culture positive for S. aureus.<br />
Discussion<br />
In this study we identified five cases of meningitis (four<br />
dural, one lepto<strong>meningeal</strong>) that demonstrated increased<br />
numbers of <strong>IgG4</strong>-positive plasma cells. All of these cases<br />
exhibited the characteristic lymphoplasmacytic inflammation<br />
and fibrosis of <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong>s.<br />
However, obliterative phlebitis was not appreciated. This is<br />
likely <strong>related</strong> to the limited sampling size of the specimens.<br />
Previous studies of AIP and retroperitoneal fibrosis also<br />
had difficulty finding evidence of obliterative phlebitis in<br />
biopsy specimens [66, 70, 74]. A slight male predominance<br />
(M:F 3:2) and older age (mean 61 years) was seen in the<br />
<strong>IgG4</strong>-<strong>related</strong> group in comparison to the non-<strong>IgG4</strong> cases<br />
(1:4, 46 years). This is typical of <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s<br />
[31].<br />
Clinically, the four patients with <strong>IgG4</strong>-<strong>related</strong> pachymeningitis<br />
presented with pain or compressive symptoms,<br />
which lead to the identification of an enhancing mass or<br />
123
Fig. 3 The case with lepto<strong>meningeal</strong> <strong>disease</strong> showed similar histological<br />
features with infiltration of <strong>IgG4</strong>-positive plasma cells into the<br />
cortex and the Virchow-Robin spaces. a H&E 1009, b <strong>IgG4</strong>-IHC<br />
2009<br />
dural thickening. Two of the cases were intracranial and<br />
two were intraspinal. The intracranial cases were biopsied<br />
for diagnosis and the intraspinal cases were resected due to<br />
spinal cord compression. Clinically, all of these cases fit<br />
the diagnosis of IHP. IHP has always been a diagnosis of<br />
exclusion. Before making this diagnosis infection, neoplasia,<br />
and autoimmune/vasculitic <strong>disease</strong>s must be ruled<br />
out. Surgical resection was historically recommended as<br />
the only means of treatment for IHP [5, 22], but some cases<br />
have been shown to respond to immunosuppression [41,<br />
52]. Current treatment recommendations are for biopsy<br />
followed by high dose corticosteroid therapy and decompressive<br />
surgery if emergently required [20]. Response to<br />
corticosteroid therapy is generally variable [20, 41, 52],<br />
and <strong>IgG4</strong>-<strong>related</strong> cases may represent part of the steroidresponsive<br />
subset of this <strong>disease</strong>.<br />
We are also reporting one case of <strong>IgG4</strong>-<strong>related</strong> leptomeningitis,<br />
a manifestation that has not been previously<br />
described. The patient (case 1) presented with cognitive<br />
decline and gait instability and was found to have<br />
123<br />
Acta Neuropathol<br />
lepto<strong>meningeal</strong> enhancement. Dural, <strong>meningeal</strong>, and cortical<br />
biopsies showed lymphoplasmacytic inflammation<br />
involving the leptomeninges and Virchow–Robin spaces<br />
(Fig. 3). There was no dural inflammation, no evidence of<br />
infection, and no vasculitis identified. Similar presentations<br />
and pathologic findings have been described in patients<br />
with autoimmune <strong>disease</strong>s such as Hashimoto’s thyroiditis<br />
[9] and Sjögren syndrome [3], and in patients described as<br />
having non-vasculitic autoimmune inflammatory meningoencephalitis<br />
(NAIM) [8]. It is important to recognize<br />
patients with encephalopathy caused by autoimmune <strong>disease</strong>s<br />
because the dementia is often reversible with steroid<br />
treatment [43]. Our study indicates that it may be important<br />
to recognize <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> as a cause of reversible<br />
dementia.<br />
In the present study, cases that were considered <strong>IgG4</strong><strong>related</strong><br />
demonstrated an increased number of <strong>IgG4</strong>-positive<br />
cells ranging from 11.8 to 54.2 cells/HPF. AIP is the first<br />
and probably the best studied of the <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s.<br />
Early studies evaluating AIP tended to consider <strong>IgG4</strong>positive<br />
cell counts ranging from [10 cells/HPF to [30<br />
cells/HPF to be sufficient for diagnosis [18, 30, 39, 75]. By<br />
the current Asian diagnostic criteria [51] and the Mayo<br />
Clinic’s histology, imaging, serology, other organ<br />
involvement and response to therapy (HISORt) criteria<br />
[12], finding C10 <strong>IgG4</strong>-positive plasma cells/HPF in the<br />
setting of a characteristic histopathology is considered<br />
sufficient to support the diagnosis of AIP. However, additional<br />
clinical and radiologic evidence is required to<br />
definitively make the diagnosis.<br />
No consensus criteria have been established thus far for<br />
extra-pancreatic <strong>disease</strong>. Some studies in organs such as<br />
lung, lymph nodes, and salivary glands advocate using the<br />
ratio of <strong>IgG4</strong>/IgG-positive cells to establish diagnostic<br />
cutoff levels [14, 37, 45, 73]. Ratios ranging from 30 to<br />
50% have been applied for diagnosing cases of extrapancreatic<br />
<strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>; however, there are no<br />
established international criteria and most of the diagnostic<br />
breakpoints are established by internal controls in a given<br />
series [14, 45, 73, 74]. For example, in a large series of<br />
<strong>IgG4</strong>-<strong>related</strong> lymphadenopathy, the <strong>IgG4</strong>/IgG cutoff ratio<br />
of 40% was used because the control reactive lymphadenitis<br />
cases had levels up to 30%. As demonstrated in<br />
Table 3, the mean <strong>IgG4</strong>/IgG-positive plasma cell ratio in<br />
our cases shows a statistically significant difference<br />
between our <strong>IgG4</strong>-<strong>related</strong> and non-<strong>IgG4</strong>-<strong>related</strong> cases.<br />
It seems that either <strong>IgG4</strong>-positive cell numbers or <strong>IgG4</strong>/<br />
IgG-positive cell ratios could potentially be used in practice<br />
for diagnosis. However, based on the literature<br />
experience, we favor the use of the cutoff of C10 <strong>IgG4</strong>positive<br />
cells/HPF recommended by the Asian and Mayo<br />
Clinic’s guidelines for AIP due to the recognized evidence<br />
basis of these criteria [12, 51]. Moreover, our study cases
Acta Neuropathol<br />
Table 4 Study cases: clinical data and follow-up<br />
Case Age Sex Clinical presentation Laboratorial data Previous clinical history Treatment Follow-up<br />
and neuroimaging<br />
Rheum<br />
Serum CSF <strong>IgG4</strong><br />
panel<br />
Steroids 10 months; doing well<br />
(on steroids)<br />
ND recently Normal Mild increased protein ND Juvenile RA since age 12<br />
(treatment with steroids,<br />
methrotrexate, and TNF-blocker<br />
on/off for several years)<br />
Stage I non-small Ca lung<br />
lobectomy followed by sepsis<br />
1 74 F Mild cognitive decline<br />
Lepto<strong>meningeal</strong><br />
enhancement<br />
(2 years prior presentation)<br />
15 months; doing well<br />
(out of steroids)<br />
Steroids<br />
Radiation therapy<br />
ND Asthma<br />
COPD<br />
Normal Oligoclonal bands Elevated protein;<br />
17 WBC (51%<br />
lymphocytes); IgG<br />
index: 34.30<br />
2 55 M Cord compression<br />
C3–C7 mass<br />
(0.5–6.1 mg/dL)<br />
17 months; doing well<br />
(on steroids and<br />
TNF-blocker)<br />
ND ND Unremarkable Steroids and<br />
TNF-blocker<br />
Normal IgG: 1,860.0 (nl:<br />
694–1,618 mg/dL)<br />
SPEP: c-globulins: 1.78<br />
3 60 F Bilateral optic<br />
neuropathy<br />
Dural thickening<br />
(0.65–1.25 g/dL)<br />
ND ND ND ND Diverticulitis<br />
Unknown Lost follow-up after<br />
Crohn’s <strong>disease</strong><br />
surgery<br />
Type II Diabetes Mellitus<br />
SPEP normal ND ND Unremarkable Steroids 115 months; doing well<br />
(out of steroids)<br />
4 63 M Bilateral hand<br />
numbness<br />
C2–C3 mass<br />
ANA ?<br />
(speckled;<br />
1:80)<br />
5 53 M Chronic lower neck<br />
headaches<br />
Posterior fossa tumor<br />
Steroids 15 months; doing well<br />
(on steroids)<br />
ND RA since age 51 (treatment with<br />
steroids and TNF-blocker)<br />
Streptococcal meningitis during<br />
ND recently Normal Elevated protein;<br />
18 WBC (71%<br />
lymphocytes)<br />
6 57 F Occasional seizures<br />
Dural enhancement<br />
RA treatment<br />
14 months; doing well<br />
(out of steroids)<br />
Normal Normal ND ND Unremarkable Antibiotics; steroids<br />
(short course)<br />
7 54 F Right retro orbital pain,<br />
headache, middle<br />
ear effusion on the<br />
right side<br />
Petrous apex dural<br />
thickening/mass<br />
Steroids 21 months; doing well<br />
(out of steroids)<br />
ND Skin biopsy positive for<br />
granulomatous <strong>disease</strong><br />
Normal Normal Mild elevated protein<br />
and pleocytosis;<br />
TB negative<br />
16 months; doing well<br />
(out of steroids)<br />
ND Normal ND ND Lyme <strong>disease</strong> Steroids (replacement<br />
only)<br />
102 months; doing well<br />
(out of steroids)<br />
Steroids (short course);<br />
chronic pain killers<br />
ND Acute leg pain<br />
s/p epidural steroid injection<br />
IgG index: 32.20<br />
(0.5–6.1 mg/dL)<br />
Normal Elevated IgA<br />
SPEP normal<br />
8 36 M Progressive cognitive<br />
decline 2–3 years<br />
Meningeal<br />
enhancement<br />
9 51 F Persistent headaches<br />
Sellar mass<br />
10 31 F Cord compression<br />
L4–L5 mass<br />
Rheum panel (one or more of the following tests): RF rheumatoid factor, ANA anti-nuclear antibody, anti-DS DNA anti-double stranded DNA, CRP C-reactive protein, anti-RPN anti-ribonuclear protein, anti-neutrophil<br />
cytoplasm, anti-Smith antigen<br />
RA rheumatoid arthritis, CSF cerebral spinal fluid, SPEP serum protein electrophoresis, UPEP urine protein electrophoresis, COPD chronic obstructive pulmonary <strong>disease</strong>, TNF-blocker tumor necrosis factor blocker,<br />
ND not done<br />
123
Table 5 Control cases: clinical data and immunohistochemistry<br />
Control # Age Sex <strong>IgG4</strong>? cells/HPF <strong>IgG4</strong>?/IgG? Diagnosis<br />
A 36 M 10.4 19% Miliary tuberculosis<br />
B 48 M 0 0% Sarcoidosis<br />
C 34 F 11.2 33% Lumbar S. aureus abscess<br />
D 60 F 3.4 – Post-surgical abscess<br />
E 32 M 4.8 4% Foreign body reaction<br />
F 48 F 0 0% Sarcoidosis<br />
G 56 F 2.4 14% Langerhans cell histiocytosis<br />
H 10 F 2.6 – Langerhans cell histiocytosis<br />
I 27 M 0.2 3% Sarcoidosis<br />
J 18 F 0 0% Sarcoidosis<br />
demonstrate a distinct and significant breakpoint between<br />
the cases with <strong>IgG4</strong>-positive cells and those without.<br />
Yet, the total number of plasma cells in our cases is<br />
much lower than what has been reported in many of the<br />
studies of <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s involving extra-pancreatic<br />
tissues [14, 37, 45]. We postulate that the relatively low<br />
numbers of plasma cells in our specimens may be due to<br />
the relatively hypocellular, dense collagenous nature of the<br />
dura mater in comparison to tissues like lung, lymph nodes,<br />
and salivary gland. Studies of other normally hypocellular,<br />
fibrotic tissues, such as the retroperitoneum, have also<br />
shown lower cell counts in comparison to other organs<br />
examined in the same studies [60, 63]. Additionally, most<br />
of our cases were diagnosed by biopsy alone and had relatively<br />
small sample sizes. <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s have been<br />
shown to be heterogeneous processes with variable cellularity.<br />
Inflammation is often concentrated around ducts and<br />
vessels and may be scarce in highly sclerotic areas [38, 66,<br />
75]. This could create difficulties when trying to diagnose<br />
the <strong>disease</strong> with a biopsy alone. In fact, studies have typically<br />
shown lower numbers of <strong>IgG4</strong>-positive cells in<br />
biopsies when compared to resections [18, 69, 75].<br />
Therefore, we believe that the higher cutoff values used by<br />
some researchers may not be entirely appropriate in the<br />
setting of <strong>meningeal</strong> <strong>disease</strong>, and perhaps different criteria<br />
need to be applied in different organs and in biopsies<br />
versus resections.<br />
Two of the control cases in this study showed increased<br />
numbers of <strong>IgG4</strong>-positive cells close to or above our cutoff<br />
value. However, these cases could easily be distinguished<br />
from <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> based on the histology alone<br />
(Fig. 4). One case (case A) was culture positive for<br />
M. tuberculosis and contained necrotizing granulomatous<br />
inflammation. The second case (case C) that met the<br />
diagnostic criteria was a lumbar abscess that was culture<br />
positive for S. aureus. The biopsy exhibited abundant acute<br />
inflammation and necrosis. <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> would not<br />
have entered into the histologic differential in either of<br />
123<br />
Acta Neuropathol<br />
Fig. 4 Two control cases exhibited elevated levels of <strong>IgG4</strong>-positive<br />
plasma cells but did not have the histology of <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>.<br />
One was a case of M. Tuberculosis (a) and the other was an S. aureus<br />
abscess (b). H&E 1009, 2009<br />
these cases, and they would likely not have been immunostained<br />
during the course of a normal diagnostic workup.<br />
Overlap of <strong>IgG4</strong> staining and serum levels with non-<strong>IgG4</strong><strong>related</strong><br />
<strong>disease</strong>s, such as pancreatic cancer and Rosai–<br />
Dorfman <strong>disease</strong>, has been well documented [29, 54].
Acta Neuropathol<br />
As the criteria established for AIP suggest, the diagnosis<br />
of an <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> should not be made solely on the<br />
basis of <strong>IgG4</strong> immunostains. In addition to the histopathology,<br />
the clinical picture, including <strong>IgG4</strong> serum studies<br />
and radiology, should be considered, and a combination of<br />
findings should be used to make the diagnosis. Some cases,<br />
that fit the histologic and clinical criteria of an <strong>IgG4</strong>-<strong>related</strong><br />
<strong>disease</strong>, can have borderline numbers of <strong>IgG4</strong>-positive<br />
plasma cells in tissue, particularly in biopsies [18, 75].<br />
Similarly, patients that meet diagnostic criteria in tissue<br />
may have normal serum <strong>IgG4</strong> levels [12]. Since our study<br />
was a retrospective analysis, many of the important clinical<br />
data on the patient population could not be obtained.<br />
Comparison of the two groups of <strong>IgG4</strong>-<strong>related</strong> and non-<br />
<strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> did not reveal substantial differences<br />
in terms of clinical presentation and laboratory data. This<br />
makes future prospective studies of autoimmune meningitis<br />
invaluable in validating the concept of <strong>IgG4</strong>-<strong>related</strong><br />
<strong>meningeal</strong> <strong>disease</strong>.<br />
It is still not entirely understood how <strong>IgG4</strong> is <strong>related</strong> to<br />
the pathogenesis of sclerosing <strong>disease</strong>s. <strong>IgG4</strong> is the least<br />
common subclass of IgG, representing \5% of IgG in<br />
serum. High serum levels are found in a limited number of<br />
conditions including atopic dermatitis, parasitic <strong>disease</strong>s,<br />
asthma, and pemphigus [1, 23]. Unlike the other forms of<br />
IgG, <strong>IgG4</strong> does not fix complement. It also consists of<br />
effectively monovalent antibodies that have reduced pathologic<br />
potential and primarily function by interfering with<br />
immune-mediated inflammation. Given this, it has been<br />
suggested that the elevated levels of <strong>IgG4</strong> in sclerosing<br />
<strong>disease</strong>s may actually be a consequence of the <strong>disease</strong><br />
rather than a cause [1].<br />
Studies of sclerosing <strong>disease</strong>s have suggested that they<br />
are autoimmune in nature based on their strong association<br />
with other autoimmune <strong>disease</strong>s, the presence of antinuclear<br />
antibodies, and their steroid sensitivity. Thus far a<br />
definitive autoantibody has not been identified, but immune<br />
complexes have been documented in the kidney and pancreas<br />
of AIP patients, and serum studies have suggested the<br />
presence of <strong>IgG4</strong> autoantibodies [4, 19]. The lymphoplasmacytic<br />
infiltrates are composed mostly of a mixture of<br />
CD4- and CD8-positive T cells, and different studies have<br />
demonstrated a predominantly Th1-type reaction in the<br />
peripheral blood and a predominantly Th2-type reaction in<br />
the tissues of AIP patients [27, 50, 71]. A recent study of<br />
the peripheral blood of patients with AIP revealed an<br />
increase in CD25-high-expressing regulatory T cells and a<br />
decrease in naïve regulatory T cells [46]. Based on these<br />
studies, it has been suggested that the pathogenesis of the<br />
sclerosing <strong>disease</strong>s may be a two phase process that has<br />
both Th1 and Th2 responses. An initial Th1 response may<br />
be a result of a reaction to a self-antigen in the presence of<br />
a decreased number of naïve regulatory T cells. This initial<br />
response could then switch to a Th2 response as <strong>disease</strong><br />
progresses. The Th2 response subsequently drives the differentiation<br />
of B cells into <strong>IgG4</strong> plasma cells [6, 46].<br />
Nevertheless, <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>s in all locations<br />
respond well to corticosteroid therapy. There is a decrease<br />
in the serum <strong>IgG4</strong> level following treatment and imaging<br />
has shown a reduction in the size of mass lesions [23, 69].<br />
Histologic resolution of the inflammatory infiltrates has<br />
even been demonstrated in cases of <strong>IgG4</strong>-<strong>related</strong> tubulointerstitial<br />
nephritis and retroperitoneal fibrosis [49, 57].<br />
Initial responses are often good, but relapses may occur<br />
after cessation of steroids. Alternative immunosuppressive<br />
agents may be used in those requiring long-term therapy<br />
[15]. One case with long-term follow-up exhibited a<br />
relapsing–remitting course with development of <strong>IgG4</strong><strong>related</strong><br />
<strong>disease</strong>s in four organs over a 14-year time period<br />
[25]. Four of the <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong> patients in our series<br />
needed long-term corticosteroid treatment for control of the<br />
<strong>disease</strong>. One patient has had radiation therapy as well for<br />
control of the <strong>disease</strong>. This highlights the need to recognize<br />
these <strong>disease</strong>s, as patients are prone to requiring longstanding<br />
treatment and may develop <strong>disease</strong> in multiple<br />
locations.<br />
In conclusion, this study presents four additional cases<br />
of <strong>IgG4</strong>-<strong>related</strong> pachymeningitis and one likely case of<br />
<strong>IgG4</strong>-<strong>related</strong> leptomeningitis. It is important to consider<br />
these entities in the differential diagnosis of <strong>meningeal</strong><br />
thickening and/or enhancement as they are medically<br />
treatable conditions. Due to the lack of international standards<br />
for the histological diagnosis of extra-pancreatic<br />
<strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>, we recommend the use of the consensus<br />
criteria for AIP of C10 <strong>IgG4</strong>-positive cells/HPF as<br />
minimum criteria for the diagnosis [12, 51]. We should<br />
emphasize, however, that clinical and laboratorial data are<br />
essential in making the definitive diagnosis of <strong>IgG4</strong>-<strong>related</strong><br />
<strong>meningeal</strong> <strong>disease</strong>. Biopsy can be used to rule out other<br />
conditions and confirm the diagnosis, so that corticosteroid<br />
therapy can be initiated.<br />
Acknowledgments We would like to thank Michael W. Cruise,<br />
M.D., Ph.D. for working up the <strong>IgG4</strong> antibody in our laboratory.<br />
References<br />
1. Aalberse RC, Stapel SO, Schuurman J, Rispens T (2009)<br />
Immunoglobulin G4: an odd antibody. Clin Exp Allergy<br />
39:469–477. doi:10.1111/j.1365-2222.2009.03207.x<br />
2. Adler JR, Sheridan W, Kosek J, Linder S (1991) Pachymeningitis<br />
associated with a pulmonary nodule. Neurosurgery 29:283–287<br />
3. Alexander GE, Provost TT, Stevens MB, Alexander EL (1981)<br />
Sjogren syndrome: central nervous system manifestations.<br />
Neurology 31:1391–1396<br />
4. Aoki S, Nakazawa T, Ohara H, Sano H, Nakao H, Joh T et al<br />
(2005) Immunohistochemical study of autoimmune pancreatitis<br />
123
using anti-<strong>IgG4</strong> antibody and patients’ sera. Histopathology<br />
47:147–158. doi:10.1111/j.1365-2559.2005.02204.x<br />
5. Ashkenazi E, Constantini S, Pappo O, Gomori M, Averbuch-<br />
Heller L, Umansky F (1991) Hypertrophic spinal pachymeningitis:<br />
report of two cases and review of the literature.<br />
Neurosurgery 28:730–732<br />
6. Bateman AC, Deheragoda MG (2009) <strong>IgG4</strong>-<strong>related</strong> systemic<br />
sclerosing <strong>disease</strong>—an emerging and under-diagnosed condition.<br />
Histopathology 55:373–383. doi:10.1111/j.1365-2559.2008.03217.x<br />
7. Berger JR, Snodgrass S, Glaser J, Post MJ, Norenberg M,<br />
Benedetto P (1989) Multifocal fibrosclerosis with hypertrophic<br />
intracranial pachymeningitis. Neurology 39:1345–1349<br />
8. Caselli RJ, Boeve BF, Scheithauer BW, O’Duffy JD, Hunder GG<br />
(1999) Nonvasculitic autoimmune inflammatory meningoencephalitis<br />
(NAIM): a reversible form of encephalopathy.<br />
Neurology 53:1579–1581<br />
9. Castillo P, Woodruff B, Caselli R, Vernino S, Lucchinetti C,<br />
Swanson J et al (2006) Steroid-responsive encephalopathy associated<br />
with autoimmune thyroiditis. Arch Neurol 63:197–202.<br />
doi:10.1001/archneur.63.2.197<br />
10. Chan SK, Cheuk W, Chan KT, Chan JK (2009) <strong>IgG4</strong>-<strong>related</strong><br />
sclerosing pachymeningitis: a previously unrecognized form of<br />
central nervous system involvement in <strong>IgG4</strong>-<strong>related</strong> sclerosing<br />
<strong>disease</strong>. Am J Surg Pathol 33:1249–1252. doi:10.1097/PAS.<br />
0b013e3181abdfc2<br />
11. Charcot JM, Joffroy A (1869) Deux cas d’atrophie musculaire<br />
progressive avec lesions de las substance grise et des faisceaux<br />
anterolateraux de la moelle epiniere. Arch Physiol Norm Pathol<br />
2:354–367; 629–649, 744–769<br />
12. Chari ST, Smyrk TC, Levy MJ, Topazian MD, Takahashi N,<br />
Zhang L et al (2006) Diagnosis of autoimmune pancreatitis: the<br />
Mayo Clinic experience. Clin Gastroenterol Hepatol<br />
4:1010–1016. doi:10.1016/j.cgh.2006.05.017; quiz 934<br />
13. Cheuk W, Yuen HK, Chan JK (2007) Chronic sclerosing dacryoadenitis:<br />
part of the spectrum of <strong>IgG4</strong>-<strong>related</strong> Sclerosing<br />
<strong>disease</strong>? Am J Surg Pathol 31:643–645. doi:10.1097/01.pas.<br />
0000213445.08902.11<br />
14. Cheuk W, Yuen HK, Chu SY, Chiu EK, Lam LK, Chan JK<br />
(2008) Lymphadenopathy of <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong>. Am<br />
J Surg Pathol 32:671–681. doi:10.1097/PAS.0b013e318157c068<br />
15. Church NI, Pereira SP, Deheragoda MG, Sandanayake N, Amin<br />
Z, Lees WR et al (2007) Autoimmune pancreatitis: clinical and<br />
radiological features and objective response to steroid therapy in<br />
a UK series. Am J Gastroenterol 102:2417–2425. doi:10.1111/j.<br />
1572-0241.2007.01531.x<br />
16. Clark A, Zeman RK, Choyke PL, White EM, Burrell MI, Grant<br />
EG et al (1988) Pancreatic pseudotumors associated with multifocal<br />
idiopathic fibrosclerosis. Gastrointest Radiol 13:30–32. doi:<br />
10.1007/BF01889019<br />
17. D’Andrea G, Trillo G, Celli P, Roperto R, Crispo F, Ferrante L<br />
(2004) Idiopathic intracranial hypertrophic pachymeningitis: two<br />
case reports and review of the literature. Neurosurg Rev<br />
27:199–204. doi:10.1007/s10143-004-0321-1<br />
18. Deheragoda MG, Church NI, Rodriguez-Justo M, Munson P,<br />
Sandanayake N, Seward EW et al (2007) The use of immunoglobulin<br />
g4 immunostaining in diagnosing pancreatic and<br />
extrapancreatic involvement in autoimmune pancreatitis. Clin<br />
Gastroenterol Hepatol 5:1229–1234. doi:10.1016/j.cgh.2007.<br />
04.023<br />
19. Deshpande V, Chicano S, Finkelberg D, Selig MK, Mino-<br />
Kenudson M, Brugge WR et al (2006) Autoimmune pancreatitis:<br />
a systemic immune complex mediated <strong>disease</strong>. Am J Surg Pathol<br />
30:1537–1545. doi:10.1097/01.pas.0000213331.09864.2c<br />
20. Dumont AS, Clark AW, Sevick RJ, Myles ST (2000) Idiopathic<br />
hypertrophic pachymeningitis: a report of two patients and review<br />
of the literature. Can J Neurol Sci 27:333–340<br />
123<br />
Acta Neuropathol<br />
21. Epstein O, Chapman RW, Lake-Bakaar G, Foo AY, Rosalki SB,<br />
Sherlock S (1982) The pancreas in primary biliary cirrhosis and<br />
primary sclerosing cholangitis. Gastroenterology 83:1177–1182<br />
22. Guidetti B, La Torre E (1967) Hypertrophic spinal pachymeningitis.<br />
J Neurosurg 26:496–503. doi:10.3171/jns.1967.26.5.0496<br />
23. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T<br />
et al (2001) High serum <strong>IgG4</strong> concentrations in patients with<br />
sclerosing pancreatitis. N Engl J Med 344:732–738<br />
24. Hamano H, Kawa S, Ochi Y, Unno H, Shiba N, Wajiki M et al<br />
(2002) Hydronephrosis associated with retroperitoneal fibrosis<br />
and sclerosing pancreatitis. Lancet 359:1403–1404<br />
25. Hori M, Makita N, Andoh T, Takiyama H, Yajima Y, Sakatani T<br />
et al (2010) Long-term clinical course of <strong>IgG4</strong>-<strong>related</strong> systemic<br />
<strong>disease</strong> accompanied by hypophysitis. Endocr J 57(6):485–492<br />
26. Kamisawa T, Egawa N, Nakajima H (2003) Autoimmune pancreatitis<br />
is a systemic autoimmune <strong>disease</strong>. Am J Gastroenterol<br />
98:2811–2812. doi:10.1111/j.1572-0241.2003.08758.x<br />
27. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K<br />
et al (2003) A new <strong>clinico</strong><strong>pathological</strong> entity of <strong>IgG4</strong>-<strong>related</strong><br />
autoimmune <strong>disease</strong>. J Gastroenterol 38:982–984. doi:10.1007/<br />
s00535-003-1175-y<br />
28. Kamisawa T, Funata N, Hayashi Y, Tsuruta K, Okamoto A, Amemiya<br />
K et al (2003) Close relationship between autoimmune<br />
pancreatitis and multifocal fibrosclerosis. Gut 52:683–687<br />
29. Kamisawa T, Chen PY, Tu Y, Nakajima H, Egawa N, Tsuruta K<br />
et al (2006) Pancreatic cancer with a high serum <strong>IgG4</strong> concentration.<br />
World J Gastroenterol 12:6225–6228<br />
30. Kamisawa T, Okamoto A (2006) Autoimmune pancreatitis:<br />
proposal of <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong>. J Gastroenterol<br />
41:613–625. doi:10.1007/s00535-006-1862-6<br />
31. Kamisawa T, Okamoto A (2008) <strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong>.<br />
World J Gastroenterol 14:3948–3955<br />
32. Kanno A, Satoh K, Kimura K, Masamune A, Asakura T, Unno M<br />
et al (2005) Autoimmune pancreatitis with hepatic inflammatory<br />
pseudotumor. Pancreas 31:420–423<br />
33. Kasashima S, Zen Y, Kawashima A, Endo M, Matsumoto Y,<br />
Kasashima F (2009) A new <strong>clinico</strong><strong>pathological</strong> entity of <strong>IgG4</strong><strong>related</strong><br />
inflammatory abdominal aortic aneurysm. J Vasc Surg<br />
49:1264–1271. doi:10.1016/j.jvs.2008.11.072 (discussion 1271)<br />
34. Kawa S, Hamano H (2003) Autoimmune pancreatitis and bile<br />
duct lesions. J Gastroenterol 38:1201–1203. doi:10.1007/<br />
s00535-003-1213-9<br />
35. Kawaguchi K, Koike M, Tsuruta K, Okamoto A, Tabata I, Fujita<br />
N (1991) Lymphoplasmacytic sclerosing pancreatitis with cholangitis:<br />
a variant of primary sclerosing cholangitis extensively<br />
involving pancreas. Hum Pathol 22:387–395<br />
36. Kim KP, Kim MH, Song MH, Lee SS, Seo DW, Lee SK (2004)<br />
Autoimmune chronic pancreatitis. Am J Gastroenterol<br />
99:1605–1616. doi:10.1111/j.1572-0241.2004.30336.x<br />
37. Kitagawa S, Zen Y, Harada K, Sasaki M, Sato Y, Minato H et al<br />
(2005) Abundant <strong>IgG4</strong>-positive plasma cell infiltration characterizes<br />
chronic sclerosing sialadenitis (Kuttner’s tumor). Am J<br />
Surg Pathol 29:783–791<br />
38. Kloppel G, Luttges J, Lohr M, Zamboni G, Longnecker D (2003)<br />
Autoimmune pancreatitis: <strong>pathological</strong>, clinical, and immunological<br />
features. Pancreas 27:14–19<br />
39. Kojima M, Sipos B, Klapper W, Frahm O, Knuth HC, Yanagisawa<br />
A et al (2007) Autoimmune pancreatitis: frequency, <strong>IgG4</strong><br />
expression, and clonality of T and B cells. Am J Surg Pathol<br />
31:521–528. doi:10.1097/01.pas.0000213390.55536.47<br />
40. Komatsu K, Hamano H, Ochi Y, Takayama M, Muraki T,<br />
Yoshizawa K et al (2005) High prevalence of hypothyroidism in<br />
patients with autoimmune pancreatitis. Dig Dis Sci 50:<br />
1052–1057<br />
41. Kupersmith MJ, Martin V, Heller G, Shah A, Mitnick HJ (2004)<br />
Idiopathic hypertrophic pachymeningitis. Neurology 62:686–694
Acta Neuropathol<br />
42. Li Y, Bai Y, Liu Z, Ozaki T, Taniguchi E, Mori I et al (2009)<br />
Immunohistochemistry of <strong>IgG4</strong> can help subclassify Hashimoto’s<br />
autoimmune thyroiditis. Pathol Int 59:636–641. doi:10.1111/j.<br />
1440-1827.2009.02419.x<br />
43. Lyons MK, Caselli RJ, Parisi JE (2008) Nonvasculitic autoimmune<br />
inflammatory meningoencephalitis as a cause of potentially<br />
reversible dementia: report of 4 cases. J Neurosurg 108:<br />
1024–1027. doi:10.3171/JNS/2008/108/5/1024<br />
44. Mamelak AN, Kelly WM, Davis RL, Rosenblum ML (1993)<br />
Idiopathic hypertrophic cranial pachymeningitis report of three<br />
cases. J Neurosurg 79:270–276. doi:10.3171/jns.1993.79.2.0270<br />
45. Masaki Y, Dong L, Kurose N, Kitagawa K, Morikawa Y,<br />
Yamamoto M et al (2009) Proposal for a new clinical entity,<br />
<strong>IgG4</strong>-positive multiorgan lymphoproliferative syndrome: analysis<br />
of 64 cases of <strong>IgG4</strong>-<strong>related</strong> disorders. Ann Rheum Dis<br />
68:1310–1315. doi:10.1136/ard.2008.089169<br />
46. Miyoshi H, Uchida K, Taniguchi T, Yazumi S, Matsushita M,<br />
Takaoka M et al (2008) Circulating naive and CD4 ? CD25 high<br />
regulatory T cells in patients with autoimmune pancreatitis.<br />
Pancreas 36:133–140. doi:10.1097/MPA.0b013e3181577553<br />
47. Montefusco PP, Geiss AC, Bronzo RL, Randall S, Kahn E,<br />
McKinley MJ (1984) Sclerosing cholangitis, chronic pancreatitis,<br />
and Sjogren’s syndrome: a syndrome complex. Am J Surg<br />
147:822–826<br />
48. Naffzinger HC, Stern WE (1949) Chronic pachymeningitis;<br />
report of a case and review of the literature. Arch Neurol Psychiatry<br />
62:383–411<br />
49. Neild GH, Rodriguez-Justo M, Wall C, Connolly JO (2006)<br />
Hyper-<strong>IgG4</strong> <strong>disease</strong>: report and characterisation of a new <strong>disease</strong>.<br />
BMC Med 4:23. doi:10.1186/1741-7015-4-23<br />
50. Okazaki K, Uchida K, Ohana M, Nakase H, Uose S, Inai M et al<br />
(2000) Autoimmune-<strong>related</strong> pancreatitis is associated with autoantibodies<br />
and a Th1/Th2-type cellular immune response.<br />
Gastroenterology 118:573–581<br />
51. Otsuki M, Chung JB, Okazaki K, Kim MH, Kamisawa T, Kawa S<br />
et al (2008) Asian diagnostic criteria for autoimmune pancreatitis:<br />
consensus of the Japan-Korea symposium on autoimmune<br />
pancreatitis. J Gastroenterol 43:403–408. doi:10.1007/s00535-<br />
008-2205-6<br />
52. Riku S, Kato S (2003) Idiopathic hypertrophic pachymeningitis.<br />
Neuropathology 23:335–344<br />
53. Shimatsu A, Oki Y, Fujisawa I, Sano T (2009) Pituitary and stalk<br />
lesions (infundibulo-hypophysitis) associated with immunoglobulin<br />
G4-<strong>related</strong> systemic <strong>disease</strong>: an emerging clinical entity.<br />
Endocr J 56:1033–1041<br />
54. Shrestha B, Sekiguchi H, Colby TV, Graziano P, Aubry MC,<br />
Smyrk TC et al (2009) Distinctive pulmonary histopathology<br />
with increased <strong>IgG4</strong>-positive plasma cells in patients with autoimmune<br />
pancreatitis: report of 6 and 12 cases with similar<br />
histopathology. Am J Surg Pathol 33:1450–1462. doi:<br />
10.1097/PAS.0b013e3181ac43b6<br />
55. Taniguchi T, Ko M, Seko S, Nishida O, Inoue F, Kobayashi H<br />
et al (2004) Interstitial pneumonia associated with autoimmune<br />
pancreatitis. Gut 53:770 (author reply 770–771)<br />
56. Uchida K, Okazaki K, Asada M, Yazumi S, Ohana M, Chiba T<br />
et al (2003) Case of chronic pancreatitis involving an autoimmune<br />
mechanism that extended to retroperitoneal fibrosis.<br />
Pancreas 26:92–94<br />
57. Uchiyama-Tanaka Y, Mori Y, Kimura T, Sonomura K, Umemura<br />
S, Kishimoto N et al (2004) Acute tubulointerstitial nephritis<br />
associated with autoimmune-<strong>related</strong> pancreatitis. Am J Kidney<br />
Dis 43:e18–e25<br />
58. van Dongen JJ, Langerak AW, Bruggemann M, Evans PA,<br />
Hummel M, Lavender FL et al (2003) Design and standardization<br />
of PCR primers and protocols for detection of clonal immunoglobulin<br />
and T-cell receptor gene recombinations in suspect<br />
lymphoproliferations: report of the BIOMED-2 Concerted Action<br />
BMH4-CT98–3936. Leukemia 17:2257–2317. doi:10.1038/sj.<br />
leu.2403202<br />
59. Wong S, Lam WY, Wong WK, Lee KC (2007) Hypophysitis<br />
presented as inflammatory pseudotumor in immunoglobulin<br />
G4-<strong>related</strong> systemic <strong>disease</strong>. Hum Pathol 38:1720–1723. doi:<br />
10.1016/j.humpath.2007.06.011<br />
60. Yamamoto H, Yamaguchi H, Aishima S, Oda Y, Kohashi K,<br />
Oshiro Y et al (2009) Inflammatory myofibroblastic tumor versus<br />
<strong>IgG4</strong>-<strong>related</strong> sclerosing <strong>disease</strong> and inflammatory pseudotumor: a<br />
comparative <strong>clinico</strong>pathologic study. Am J Surg Pathol<br />
33:1330–1340<br />
61. Yamamoto M, Takahashi H, Sugai S, Imai K (2005) Clinical and<br />
<strong>pathological</strong> characteristics of Mikulicz’s <strong>disease</strong> (<strong>IgG4</strong>-<strong>related</strong><br />
plasmacytic exocrinopathy). Autoimmun Rev 4:195–200. doi:<br />
10.1016/j.autrev.2004.10.005<br />
62. Yamamoto M, Takahashi H, Ohara M, Suzuki C, Naishiro Y,<br />
Yamamoto H et al (2006) A case of Mikulicz’s <strong>disease</strong> (<strong>IgG4</strong><strong>related</strong><br />
plasmacytic <strong>disease</strong>) complicated by autoimmune<br />
hypophysitis. Scand J Rheumatol 35:410–411. doi:10.1080/03<br />
009740600758110<br />
63. Yamashita K, Haga H, Mikami Y, Kanematsu A, Nakashima Y,<br />
Kotani H et al (2008) Degree of <strong>IgG4</strong>? plasma cell infiltration in<br />
retroperitoneal fibrosis with or without multifocal fibrosclerosis.<br />
Histopathology 52:404–409. doi:10.1111/j.1365-2559.2007.<br />
02959.x<br />
64. Yoneda K, Murata K, Katayama K, Ishikawa E, Fuke H,<br />
Yamamoto N et al (2007) Tubulointerstitial nephritis associated<br />
with <strong>IgG4</strong>-<strong>related</strong> autoimmune <strong>disease</strong>. Am J Kidney Dis<br />
50:455–462. doi:10.1053/j.ajkd.2007.05.018<br />
65. Yoshimura Y, Takeda S, Ieki Y, Takazakura E, Koizumi H,<br />
Takagawa K (2006) <strong>IgG4</strong>-associated prostatitis complicating<br />
autoimmune pancreatitis. Intern Med 45:897–901<br />
66. Zamboni G, Luttges J, Capelli P, Frulloni L, Cavallini G, Pederzoli<br />
P et al (2004) Histo<strong>pathological</strong> features of diagnostic and<br />
clinical relevance in autoimmune pancreatitis: a study on 53<br />
resection specimens and 9 biopsy specimens. Virchows Arch<br />
445:552–563. doi:10.1007/s00428-004-1140-z<br />
67. Zen Y, Harada K, Sasaki M, Sato Y, Tsuneyama K, Haratake J<br />
et al (2004) <strong>IgG4</strong>-<strong>related</strong> sclerosing cholangitis with and without<br />
hepatic inflammatory pseudotumor, and sclerosing pancreatitisassociated<br />
sclerosing cholangitis: do they belong to a spectrum of<br />
sclerosing pancreatitis? Am J Surg Pathol 28:1193–1203<br />
68. Zen Y, Kasahara Y, Horita K, Miyayama S, Miura S, Kitagawa S<br />
et al (2005) Inflammatory pseudotumor of the breast in a patient<br />
with a high serum <strong>IgG4</strong> level: histologic similarity to sclerosing<br />
pancreatitis. Am J Surg Pathol 29:275–278<br />
69. Zen Y, Kitagawa S, Minato H, Kurumaya H, Katayanagi K,<br />
Masuda S et al (2005) <strong>IgG4</strong>-positive plasma cells in inflammatory<br />
pseudotumor (plasma cell granuloma) of the lung. Hum Pathol<br />
36:710–717. doi:10.1016/j.humpath.2005.05.011<br />
70. Zen Y, Sawazaki A, Miyayama S, Notsumata K, Tanaka N,<br />
Nakanuma Y (2006) A case of retroperitoneal and mediastinal<br />
fibrosis exhibiting elevated levels of <strong>IgG4</strong> in the absence of<br />
sclerosing pancreatitis (autoimmune pancreatitis). Hum Pathol<br />
37:239–243. doi:10.1016/j.humpath.2005.11.001<br />
71. Zen Y, Fujii T, Harada K, Kawano M, Yamada K, Takahira M<br />
et al (2007) Th2 and regulatory immune reactions are increased in<br />
immunoglobin G4-<strong>related</strong> sclerosing pancreatitis and cholangitis.<br />
Hepatology 45:1538–1546. doi:10.1002/hep.21697<br />
72. Zen Y, Fujii T, Sato Y, Masuda S, Nakanuma Y (2007) Pathological<br />
classification of hepatic inflammatory pseudotumor with<br />
respect to <strong>IgG4</strong>-<strong>related</strong> <strong>disease</strong>. Mod Pathol 20:884–894. doi:<br />
10.1038/modpathol.3800836<br />
73. Zen Y, Inoue D, Kitao A, Onodera M, Abo H, Miyayama S et al<br />
(2009) <strong>IgG4</strong>-<strong>related</strong> lung and pleural <strong>disease</strong>: a <strong>clinico</strong>pathologic<br />
123
study of 21 cases. Am J Surg Pathol 33:1886–1893. doi:<br />
10.1097/PAS.0b013e3181bd535b<br />
74. Zen Y, Onodera M, Inoue D, Kitao A, Matsui O, Nohara T et al<br />
(2009) Retroperitoneal fibrosis: a <strong>clinico</strong>pathologic study with<br />
respect to immunoglobulin G4. Am J Surg Pathol 33:1833–1839<br />
123<br />
Acta Neuropathol<br />
75. Zhang L, Notohara K, Levy MJ, Chari ST, Smyrk TC (2007)<br />
<strong>IgG4</strong>-positive plasma cell infiltration in the diagnosis of autoimmune<br />
pancreatitis. Mod Pathol 20:23–28. doi:10.1038/<br />
modpathol.3800689