Part 3 Chest x rays made easy abnormalities
Part 3 Chest x rays made easy abnormalities
Part 3 Chest x rays made easy abnormalities
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Education<br />
<strong>Chest</strong> x <strong>rays</strong> <strong>made</strong> <strong>easy</strong><br />
In the third of a five part series, Elizabeth Dick looks at <strong>abnormalities</strong> of the lung fields<br />
The basics of looking at a chest x ray (recap):<br />
● First look at the mediastinal contours—run<br />
your eye down the left side of the patient<br />
and then up the right.<br />
● The trachea should be central. The aortic<br />
arch is the first structure on the left,<br />
followed by the left pulmonary artery;<br />
notice how you can trace the pulmonary<br />
artery branches fanning out through the<br />
lung (see figure 1).<br />
● Two thirds of the heart lies on the left side<br />
of the chest, with one third on the right.<br />
The heart should take up no more than<br />
half of the thoracic cavity. The left border<br />
of the heart is <strong>made</strong> up by the left atrium<br />
and left ventricle.<br />
● The right border is <strong>made</strong> up by the right<br />
atrium alone. Above the right heart border<br />
lies the edge of the superior vena cava.<br />
● The pulmonary arteries and main bronchi<br />
arise at the left and right hila. Enlarged<br />
lymph nodes can also occur here, as can<br />
primary tumours. These make the hilum<br />
seem bulky—note the normal size of the<br />
hila on this film.<br />
● Now look at the lungs. Apart from the<br />
pulmonary vessels (arteries and veins), they<br />
should be black (because they are full of<br />
air). Scan both lungs, starting at the apices<br />
and working down, comparing left with<br />
right at the same level, just as you would<br />
when listening to the chest with your<br />
stethoscope. The lungs extend behind the<br />
heart, so look here too. Force your eye to<br />
look at the periphery of the lungs—you<br />
should not see many lung markings here; if<br />
you do then there may be disease of the air<br />
spaces or interstitium. Don’t forget to look<br />
for a pneumothorax.<br />
● Make sure you can see the surface of the<br />
hemidiaphragms curving downwards, and<br />
that the costophrenic and cardiophrenic<br />
angles are not blunted—suggesting an<br />
effusion. Check there is no free air under<br />
the hemidiaphragm.<br />
● Finally, look at the soft tissues and bones.<br />
Are both breast shadows present? Is there<br />
a rib fracture? This would make you look<br />
even harder for a pneumothorax. Are the<br />
bones destroyed or sclerotic?<br />
Pneumothorax<br />
It is important to view around the periphery<br />
of the lungs to look for a pneumothorax<br />
(air in the pleural space with associated<br />
collapsed lung). It is very <strong>easy</strong> to miss<br />
a pneumothorax. Watch out for the<br />
following signs:<br />
408<br />
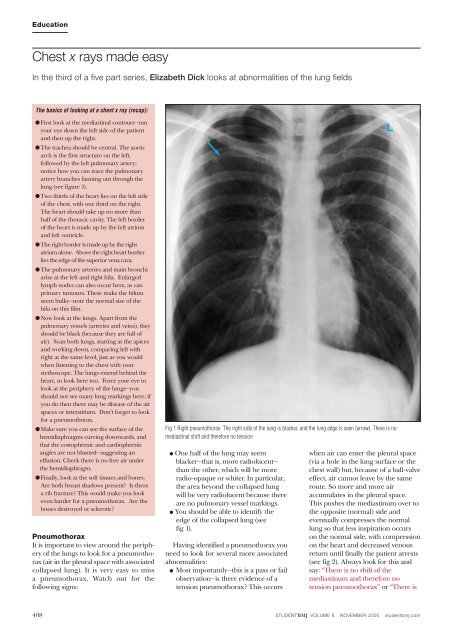
Fig 1 Right pneumothorax. The right side of the lung is blacker, and the lung edge is seen (arrow). There is no<br />
mediastinal shift and therefore no tension<br />
● One half of the lung may seem<br />
blacker—that is, more radiolucent—<br />
than the other, which will be more<br />
radio-opaque or whiter. In particular,<br />
the area beyond the collapsed lung<br />
will be very radiolucent because there<br />
are no pulmonary vessel markings.<br />
● You should be able to identify the<br />
edge of the collapsed lung (see<br />
fig 1).<br />
Having identified a pneumothorax you<br />
need to look for several more associated<br />
<strong>abnormalities</strong>:<br />
● Most importantly—this is a pass or fail<br />
observation—is there evidence of a<br />
tension pneumothorax? This occurs<br />
L<br />
when air can enter the pleural space<br />
(via a hole in the lung surface or the<br />
chest wall) but, because of a ball-valve<br />
effect, air cannot leave by the same<br />
route. So more and more air<br />
accumulates in the pleural space.<br />
This pushes the mediastinum over to<br />
the opposite (normal) side and<br />
eventually compresses the normal<br />
lung so that less inspiration occurs<br />
on the normal side, with compression<br />
on the heart and decreased venous<br />
return until finally the patient arrests<br />
(see fig 2). Always look for this and<br />
say: “There is no shift of the<br />
mediastinum and therefore no<br />
tension pneumothorax” or “There is<br />
STUDENTBMJ VOLUME 8 NOVEMBER 2000 studentbmj.com
shift of the mediastinum away from<br />
the side of the pneumothorax<br />
indicating a (right/left) tension<br />
pneumothorax. This is a medical<br />
emergency which I would treat<br />
immediately by inserting a large bore<br />
cannula into the (right/left) pleural<br />
space.”<br />
● The cause of the pneumothorax may<br />
be apparent—for example, fracture of<br />
the ribs.<br />
● There may be associated surgical<br />
emphysema—that is, air in the soft<br />
tissues—and air in the mediastinum<br />
(see fig 3).<br />
There is extra shadowing in<br />
the lungs<br />
It may be difficult to work out what is causing<br />
extra shadowing in the lungs, especially<br />
near the mediastinum where normal<br />
structures may overlay the extra shadowing.<br />
It is useful to look at the periphery of<br />
the lungs because normally the outermost<br />
edge of the lungs should be fairly black<br />
with a few tapering blood vessels. If you do<br />
see more shadowing in the periphery then<br />
there may be either interstitial or air space<br />
disease. As examiners often show films<br />
with one of these two types of shadowing,<br />
understanding the difference between<br />
these two is worth while because it will help<br />
you to interpret what you see and lead you<br />
to the correct differential diagnosis.<br />
The lung is <strong>made</strong> up of bronchi, which<br />
branch, at the end of which are alveoli. The<br />
interstitial space (or potential space) surrounds<br />
the alveoli. The whole of the lung<br />
Fig 3 Surgical emphysema (arrow) and pneumomediastinum (arrowhead)<br />
Fig 2 Left tension pneumothorax with shift of the mediastinum to the right. The lung edge is arrowed<br />
Education<br />
from bronchi to alveoli is the air space—<br />
that is, it normally contains air. But the<br />
air spaces can fill up—with fluid (such as in<br />
severe pulmonary oedema), with pus (as<br />
in infection), with blood (as in rare diseases<br />
such as Goodpasture’s syndrome, associated<br />
with renal failure), or with tumour<br />
cells (alveolar carcinoma).<br />
Fluid and pus are more common than<br />
the second two. When the air spaces fill up,<br />
the alveoli fill first, with the bronchi being<br />
relatively spared. Therefore the bronchi,<br />
which are still air filled, stand out against<br />
the alveoli, which are filled with pus or<br />
fluid. This is called an air bronchogram<br />
and is simply a sign that there is air space<br />
disease. Consolidation is another term for<br />
air space shadowing (see figs 4 and 5). If<br />
there is air space disease then you need to<br />
work out which part of the lungs it is affecting.<br />
A quick way is to use the word “zone”<br />
to describe which part of the lung is affected.<br />
Say something like “There is shadowing<br />
in the air spaces of the right mid and<br />
lower zone.” You can then take your time<br />
to work out which lobe is affected. You can<br />
STUDENTBMJ VOLUME 8 NOVEMBER 2000 studentbmj.com 409<br />
L<br />
L
Education<br />
Fig 4 Left and right lower lobe air space shadowing in an ITU patient<br />
Fig 6 Recticular-nodular shadowing caused by lung fibrosis (circled). Note how the heart has lost its normal smooth<br />
outline and seems “shaggy”<br />
Features of air space and interstitial lung disease<br />
410<br />
Air space disease Interstitial lung disease<br />
Zones Any Any<br />
Appearances Confluent shadowing Linear/reticular/nodular<br />
Air bronchograms shadowing<br />
Causes Fluid (pulmonary oedema, Fluid (pulmonary oedema/<br />
(differential adult respiratory distress lymphangitis<br />
diagnoses) syndrome) carcinomatosa)<br />
Pus (infection/consolidation) Inflammation leading to<br />
fibrosis (industrial lung<br />
Blood disease, inflammatory<br />
(Goodpasture’s syndrome) arthritides, inflammation of<br />
unknown cause, sarcoid)<br />
Tumour cells<br />
(alveolar cell carcinoma)<br />
L<br />
L<br />
find out more about lobar anatomy in the<br />
later section on collapse and consolidation.<br />
Let’s turn to the interstitial space. This<br />
surrounds bronchi, vessels, and groups of<br />
alveoli. When there is disease in the<br />
interstitium it manifests itself by reticulonodular<br />
shadowing (criss cross lines or<br />
tiny nodules or both). The main two<br />
processes affecting the interstitium are<br />
accumulation of fluid (occurring in pulmonary<br />
oedema or in lymphangitis carcinomatosa)<br />
and inflammation leading to<br />
fibrosis (occurring in industrial lung disease,<br />
inflammatory arthritides such as<br />
rheumatoid arthritis, inflammation of<br />
unknown cause such as cryptogenic fibrosing<br />
alveolitis and sarcoidosis). If you see<br />
criss cross lines or tiny nodules or both say:<br />
“There is reticulo-nodular shadowing within<br />
the lower zones.” (See figure 6.)<br />
Use the table to work out whether the<br />
extra shadowing you can see is air space or<br />
interstitial.<br />
Next month: we will look at collapse,<br />
consolidation, and pleural effusions.<br />
I would like to thank Dr Anju Sahdev,<br />
Dr Brian Holloway, and Dr Robert Dick<br />
for contributing some of the films which<br />
are illustrated.<br />
Elizabeth Dick, specialist registrar in radiology,<br />
North Thames Deanery<br />
Fig 5 Right middle and lower zone consolidation/air<br />
space shadowing. Note air bronchogram (arrow).<br />
There is no loss of volume, which is a key feature of<br />
consolidation<br />
Erratum: see p407.<br />
See Web Extra at<br />
studentbmj.com for our<br />
web-based x ray quiz<br />
STUDENTBMJ VOLUME 8 NOVEMBER 2000 studentbmj.com<br />
L