color pdf
color pdf
color pdf
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
BIMM118<br />
“One of the features which is thought to<br />
distinguish man from other animals is his<br />
desire to take medicines”<br />
(Sir William Osler, 1849-1919)
BIMM118<br />
Definitions<br />
• Pharmacology is the science of the interaction of chemicals with living<br />
systems at all levels<br />
• Pharmacokinetics investigates the effects of the biological system on drugs<br />
(absorption, distribution, elimination…)<br />
• Pharmacodynamics describes the fundamental action of a drug on a<br />
physiological, biochemical or molecular level<br />
• Pharmacogenetics examines the effects of genetic factors to variations in the<br />
drug response<br />
• Toxicology studies the undesirable effects of chemicals on living systems<br />
(includes poisons, antidotes and unwanted side effects of drugs)<br />
• Pharmacy is the art of preparing, compounding and dispensing chemicals for<br />
medicinal use
BIMM118<br />
Definitions<br />
• Prophylactic refers to a drug or procedure aimed to prevent disease<br />
• Palliative refers to a drug or procedure aimed to relieve symptoms<br />
• Therapeutic refers to a drug or procedure aimed to cure disease<br />
• Tolerance is the increased resistance to the usual effects of an established<br />
dose of a particular drug<br />
• Effective dose (ED50) is the concentration at which 50% of the subject show<br />
a predefined response<br />
• Efficacy refers to the inherent capability of a drug to produce a desired effect<br />
• Potency compares the relative effectiveness of drugs to produce a desired effect<br />
e.g. Drug A requires fewer milligrams than Drug B to achieve the same pharmacological response<br />
--> Drug A has the higher potency, yet, both drugs have the same efficacy.
BIMM118<br />
History of Pharmacology<br />
• Initially most medicines were of<br />
botanical or zoological origin<br />
• Since 1950’s, large increase in<br />
synthetic organic chemicals<br />
• Recent introduction of recombinant<br />
DNA technology has extended<br />
synthesis to molecules of human origin
BIMM118<br />
History of Pharmacology<br />
• Early agents were naturally occurring inorganic salts and plant<br />
alkaloids<br />
– Opium<br />
– Foxglove<br />
– Mercury, arsenic or lead compounds<br />
• Most ineffective or actually dangerous<br />
• Standardization of dose very difficult<br />
– Narrow therapeutic index with foxglove
BIMM118<br />
Homeopathy<br />
• 1790-96: Dr. Samuel Hahnemann:<br />
To discover the true mode of action by which cinchona bark cured<br />
malaria, he ingested cinchona juice twice daily for a few days. To his<br />
great astonishment, he very soon developed symptoms very similar<br />
to malarial fever.<br />
– Postulated a new principle of treatment: “Likes cure likes”<br />
– Drug is called the remedy, obtained through serial dilutions of the<br />
chemical<br />
The remedy is mainly extracted from the plants, animals and minerals. The medicinal extract is diluted and<br />
potentiated to such an extent that not even an atom of the mother material can be detected in the remedy by the<br />
time it reaches the 12th potency. Dilutions are done in steps. For example: In the centi scale, one drop of mother<br />
tincture is mixed with 99 drops of alcohol and shaken rigorously using pre-determined strokes. This is termed as<br />
1c. From this, one drop is mixed with 99 drops of alcohol and is termed as 2c and so on. The higher the dilution,<br />
the more powerful the remedy. It was proposed recently that the magnetic aura of the remedy increases with<br />
potency (supposedly, this had been proven with Kirlian photography).<br />
Since the remedies are used after diluting several times, it cannot have chemical effects on the body to create a<br />
long standing side effect.
BIMM118<br />
History of Pharmacology<br />
• Major advance in safe use of naturally derived agents<br />
was the isolation, purification and chemical<br />
characterization of the active compound:<br />
– Allowed administration of a controlled dose<br />
– Allowed administration of the active component of herbal<br />
mixtures to be given alone<br />
– Identification and characterization of active component<br />
allowed definition of mechanism of action, leading to<br />
synthesis of improved agents with greater selectivity,<br />
potency, altered duration of action, etc.
BIMM118<br />
• Aspirin® - first synthetic drug<br />
History of Pharmacology<br />
– Hippocrates: pain relief treatments with powder made from the bark and leaves of<br />
the willow tree (Salix sp.)<br />
– Johann Buchner (1829): isolated Salicin as the<br />
active ingredient in Meadowsweet (Spiraea ulmaria)<br />
(hydrolyzed into glucose and Salicyl-aldehyde -><br />
oxidyzed to Salicylic Acid)<br />
Salicylic Acid is very tough on the stomach-><br />
– Felix Hoffman (1898-9): Chemist at Bayer<br />
synthezised Acetyl-Salicylic Acid,<br />
(process discovered originally by Charles Gerhardt in 1853)<br />
and tested it on his arthritis-suffering father!<br />
– March 6, 1899: Bayer receives patent for Aspirin®<br />
– Sales today exceed 50 billion pills per year
BIMM118<br />
History of Pharmacology<br />
• 20 th Century: Dramatic change in antimicrobial therapy<br />
– Survival of patients with severe infections with historically high<br />
mortality<br />
– Introduction of sulfonamides (Gelmo 1908: Sulfanilamide) and<br />
arsenic compounds (Ehrlich 1908/10: arsephenamine= Salvarsan)<br />
and subsequently penicillins (Fleming 1928/29)
BIMM118<br />
New Drug Discovery<br />
• Analogues to existing drugs<br />
– Usually shows only minor changes in potency, absorption,<br />
duration of action<br />
• New applications for existing drugs<br />
– Occasionally unexpected additional properties may become<br />
evident when the compounds are tested in humans<br />
• Sulfanilamide --> thiazide diuretics<br />
• Sulfanilamide --> sulfonylurea hypoglycemics<br />
• Aspirin® --> Anti-aggregatory --> Cardioprotective
BIMM118<br />
New Drug Discovery<br />
• Synthesis and screening of new chemical entities<br />
• Subject new chemicals to a battery of tests designed to detect<br />
a particular type of biological activity (“Drug screening”)<br />
• Chemicals produced by direct synthesis, or isolation from<br />
biological sources (or combination of both: semi-synthetic)<br />
• Apparently not an efficient method since huge numbers of<br />
chemicals may need to be screened, however, new robotic<br />
instruments are now screening millions of compounds against<br />
defined receptors or enzymes
BIMM118<br />
New Drug Discovery<br />
• Design of compounds for a specific biological function<br />
(“Rational drug design”)<br />
– Synthesis of naturally occurring compounds or structural analogues<br />
• Examples:<br />
– Levodopa, H2 receptor antagonists, omeprazole<br />
– Use of structural information (receptor, enzyme) to develop<br />
interacting compounds<br />
• Examples:<br />
– STI571 (Glevec®): Bcr-Abl specific inhibitor, but high pK =><br />
2 nd generation Bcr-Abl inhibitors are being designed based on the<br />
structure of the Bcr-Abl/STI571 complex<br />
– Cloning of genes to produce large biologically active peptides<br />
• Examples:<br />
– Rec. hormones, cytokines; soluble receptor; antibodies
BIMM118<br />
New Drug Discovery<br />
• Extremely high cost of new drug development in general restricts<br />
it to the province of large pharmaceutical companies<br />
• Cost of new drug development is in the $100 to $500 million<br />
range<br />
• Cost of initial marketing is also very high<br />
• Incentives are very high with important new drugs having greater<br />
than $1 Billion in yearly sales
BIMM118<br />
Patent Protection of new Drugs<br />
• Patent life in the US is 20 years<br />
• Drug is frequently patented five years or more before<br />
marketing begins<br />
• After patents expire, other manufacturers may<br />
produce and sell bioequivalent “generic” products<br />
(usually much cheaper, as these companies had very little “development” cost)
BIMM118<br />
Orphan Drugs<br />
• Drugs for conditions affecting less than 200,000<br />
individuals in the US<br />
• Orphan Drug Act of 1983 provides incentives for the<br />
development of drugs for this small market segment<br />
(tax breaks, exclusive marketing rights, grant funding)<br />
• 890 Orphan drugs in the US for the treatment of 6.5<br />
million people
BIMM118<br />
• Brand Name<br />
Drug Nomenclature<br />
– Prevacid®, Zoton® (New Zealand), Keval® (Mexico), Lanzor® (France), etc.<br />
• Generic Name<br />
– Lansoprazole<br />
• Chemical Name<br />
– 2-[[[3-methyl-4-(2,2,2-trifluroethoxy)-2-pyridyl]methyl]sulfinyl]benzimidazole
BIMM118<br />
Drug Approval<br />
Historically, manufacturers or sellers had no responsibility<br />
--> Regulatory systems have arisen to protect patients from toxicity and<br />
more recently to ensure benefit (efficacy)<br />
1938 - Federal Food, Drug and Cosmetic Act
BIMM118<br />
• Safety<br />
Drug Approval<br />
– Introduction of new drugs has sometimes been bought at the price of<br />
significant toxicity<br />
• 1937: >100 deaths due to diethylene glycol in Sulfanilamide elixir<br />
• 1960’s: Thalidomide (Contergan®) disaster:<br />
– developed by the company Grünenthal as a sleep-inducing drug and to<br />
combat symptoms associated with morning sickness of pregnant women
BIMM118<br />
• Safety<br />
Drug Approval<br />
– Bacterial, isolated cellular, and intact animal toxicity testing<br />
– Testing for toxicities including<br />
• Teratogenicity<br />
• Mutagenicity<br />
• Reproductive toxicity
BIMM118<br />
• Regulatory bodies (FDA)<br />
Drug Quality<br />
– ensure quality of prescribed drugs<br />
• Defined criteria for:<br />
– Purity<br />
– Stability and sterility<br />
– Limits of potentially toxic impurities<br />
– Defined, approved amount of drug, released at a specified rate (United<br />
States Pharmacopoeia, British Pharmacopoeia, European Pharmacopoeia)
BIMM118<br />
Drug Efficacy<br />
• Efficacy must be established in patients for whom the<br />
medicine is intended<br />
• All medicines, except dietary supplements, must<br />
have evidence of efficacy for their licensed<br />
indications.
BIMM118<br />
Drug Efficacy - Dietary Supplements?<br />
• Leptoprin® (30 pills = $153):<br />
– Calcium (amino acid chelate) 264mg<br />
– Vitamin B6 25mg<br />
– Acetylsalicylic acid 324mg<br />
– Caffeine 200mg<br />
– Green Tea Extract (no amount listed)<br />
– L-Tyrosine (no amount listed)<br />
– Kelp 100mg<br />
– Ephedrine 20mg<br />
– Cayenne (no amount listed)<br />
The FDA had previously issued a policy that ephedrine products must be<br />
labeled with possible adverse effects, contain no more than 8 milligrams of<br />
ephedrine per serving, and be used for no longer than seven days, because of<br />
the significant dangers associated with ephedra or ephedrine use.<br />
Since April 2004, ephedrine has been banned in dietary supplements!<br />
Conclusion: The only ingredient in Leptoprin that might assist in weight loss<br />
is calcium. If you do not get enough calcium in your diet, you can buy cheap<br />
supplements at any drugstore.
BIMM118<br />
Drug Efficacy - Dietary Supplements?<br />
• CortiSlim® (30 pills = $78):<br />
– “Dr”. Greg Cynaumon?<br />
Ph.D. from “Sierra University” in Psychology - School was shut down by<br />
the State of California!<br />
– September 2004 : Greg Cynaumon forced to admit that he is not a<br />
psychologist or a marriage and family therapist.The California Board of<br />
Psychology issues a citation and fines Greg Cynaumon $1,500 for<br />
continuing to impersonate a psychologist.<br />
– The California Board of Behavioral Sciences issued a citation and fined<br />
Greg Cynaumon $1,000 for continuing to impersonate a<br />
marriage/family therapist.<br />
– “FTC Targets Products Claiming to Affect the Stress Hormone Cortisol”<br />
Agency Alleges That Marketers of CortiSlim and CortiStress Made<br />
False or Unsubstantiated Claims
BIMM118<br />
Establishing Safety and Efficacy<br />
• Preclinical studies<br />
• Phase I clinical studies<br />
• Phase II clinical studies<br />
• Phase III clinical studies<br />
• Phase IV post-marketing<br />
surveillance
BIMM118<br />
Preclinical Studies<br />
• Pharmacological effects or pharmacological profile<br />
– In-vitro effects using isolated cells/organs<br />
– Receptor-binding characteristics<br />
– in-vivo effects in animals/animal models of human disease<br />
• Drugs are lacking where a good animal model of a human<br />
disease does not exist<br />
– Prediction of potential therapeutic use
BIMM118<br />
• Pharmacokinetics<br />
Preclinical Studies<br />
– Identification of metabolites (since these may be the active<br />
form of the compound)<br />
– Evidence of bioavailability (to assist in design of clinical trials<br />
and assess toxicity)<br />
– Establishment of principal route of administration and rate of<br />
elimination
BIMM118<br />
• Toxicological effects<br />
Preclinical Studies<br />
– In vitro and in vivo batteries of tests to identify toxic<br />
compounds and metabolites prior to extensive exposure of<br />
animals and subsequently humans<br />
– Toxicity testing has two primary goals:<br />
• Recognition of hazards<br />
• Prediction of that hazard occurring in humans at therapeutic<br />
doses<br />
– A wide range of doses is tested<br />
» High doses to detect toxicity<br />
» Low doses to predict risk at therapeutic doses
BIMM118<br />
Toxicity Testing<br />
• Mutagenicity<br />
• A variety of in vitro tests using bacteria and mammalian cell<br />
lines are employed at an early stage to define any potential<br />
effect on DNA that may be linked to carcinogenicity or<br />
teratogenicity<br />
• Carcinogenicity<br />
• Repeated doses given throughout lifetime of an animal (usually<br />
two year rodent assay)<br />
• Especially important in drugs intended for chronic<br />
administration (greater than one year)<br />
• Reproductive toxicity<br />
• Repeated doses given prior to mating and throughout gestation<br />
• Assesses effect on fertility, implantation, fetal growth,<br />
production of fetal abnormalities and neonatal growth
BIMM118<br />
• Acute Toxicity<br />
Toxicity Testing<br />
• Animal model - single dose given by proposed route for<br />
humans<br />
• Defines dose range associated with toxicity<br />
• Defines dose range for initial human trials<br />
• Subacute Toxicity<br />
• Repeated doses given for 14 or 28 days<br />
• Reveals target for toxic effects<br />
• Comparison with single-dose studies indicate potential for<br />
accumulation<br />
• Chronic Toxicity<br />
• Repeated doses given up to six months<br />
• Reveals target(s) for toxicity (except cancer)<br />
• Aim is to define doses associated with adverse effects and “no<br />
observed adverse effect level” associated with “safe” dose
BIMM118<br />
• Animal Studies:<br />
Toxicity Testing<br />
– Remain an important part of toxicological testing<br />
– Essential to investigate both interference with integrative<br />
function and complex homeostatic mechanisms<br />
– Necessary to prevent extensive toxicity in subsequent<br />
human trials<br />
– Extensive research underway to reduce the need for animal<br />
studies by using in vitro methodology
BIMM118<br />
• Animal Studies:<br />
Toxicity Testing<br />
– Methodology is not perfect, but animal studies do provide an<br />
effective predictive screen<br />
– Not all hazards detected at very high doses in experimental<br />
animals are relevant to human health<br />
– FDA has to judge if there is clinical relevance of data in<br />
animals at doses that may be two orders of magnitude<br />
above those intended for human use
BIMM118<br />
Premarketing Clinical Studies: Phase I-III Trials<br />
• Notice of Claimed Investigational New Drug (IND) is<br />
filed with the FDA<br />
– Information on composition and source of drug<br />
– Manufacturing information<br />
– Data from animal studies<br />
– Clinical plans and protocols<br />
– Names and credentials of physicians conducting the trials
BIMM118<br />
Phase I Studies<br />
• Studies carried out in healthy volunteers<br />
• Carried out by pharmaceutical companies or major hospitals<br />
• In some cases patients with the disease in question may be<br />
enrolled (cancer chemotherapy)<br />
• Initially small doses (as little as one fiftieth of intended dose)<br />
• Toxicity evaluated with routine hematology and biochemical<br />
monitoring of liver and renal function<br />
• Dose is escalated until pharmacologic effect is observed or<br />
toxicity occurs
BIMM118<br />
Phase I Studies<br />
• Used to study the disposition, metabolism and main pathways of<br />
elimination of the new drug in humans<br />
• Identify the most suitable dose and route of administration for<br />
further clinical studies<br />
• Use of isotope-labeled (usually beta-emitting) compounds to<br />
investigate pharmacokinetics and metabolism
BIMM118<br />
Phase II Studies<br />
• Pharmacology of the new drug is determined in patients with the<br />
intended clinical condition<br />
• Principal aim is to define relationship between dose and<br />
pharmacological and/or therapeutic response in humans<br />
• During phase II some evidence of beneficial effect may emerge<br />
• Adress subjective element in human illness (placebo effect)<br />
• Additional studies:<br />
• Special populations (elderly, etc.)<br />
• Tests for potential interactions with other drugs<br />
• Optimum dosage established for use in phase III trials
BIMM118<br />
• Main clinical trial<br />
Phase III Studies<br />
– Drug is compared to placebo, or if this would be unethical (effective<br />
treatment for the disease in question already exists), an established<br />
drug in use for this disease<br />
– Comparison to other established treatments<br />
– Addition to established treatment with placebo control
BIMM118<br />
Phase III Studies<br />
• Random placebo-controlled studies<br />
– Randomization of patient population<br />
– Sometimes there is double-blinding of the study<br />
– Between patient population studies<br />
• Separate patient population arms<br />
• With or without crossover<br />
• Require greater number of patients<br />
– Within patient population studies (crossover)<br />
• Alternate treatment with new drug and standard therapy or<br />
placebo<br />
• Takes longer
BIMM118<br />
Phase III Studies<br />
• Measurements of adverse effects and possible<br />
benefit made at regular intervals<br />
• Attention to detecting likely occuring side effects<br />
(type A reactions), and unpredictable, rarer<br />
complications (type B reactions)<br />
– Majority of type B reactions may not be seen until post<br />
marketing because during the Phase III trial usually only 2-<br />
3000 people will take the drug, usually for short periods<br />
– Type B reactions typically occur in one in 1000 to 10,000<br />
patients
BIMM118<br />
Phase IV studies:<br />
• Postmarketing Surveillance<br />
– Ongoing monitoring of drug safety under actual conditions of use in<br />
large numbers of patients. (Pharmacovigilance)<br />
– Physician and pharmacist reporting of adverse drug events<br />
– No fixed duration<br />
– Picks up adverse events occurring in less than one in 1000<br />
subjects
BIMM118<br />
Adverse Reactions to Drugs<br />
• Severe adverse effects:<br />
– Uncommon, but explainable extensions of known<br />
pharmacologic effects<br />
– Unexpected, may not be recognized until a drug has been<br />
marketed for years, sometimes unexplainable (Thalidomide)<br />
• Often represent immunological reactions<br />
– Urticaria, angioedema,<br />
– Lupus-like, serum sickness, cell mediated allergies<br />
– Severest form --> Anaphylactic shock!
BIMM118<br />
The Four Cornerstones of Pharmacokinetics<br />
• Absorption<br />
• Distribution<br />
• Metabolism<br />
• Elimination<br />
Absorption and distribution are influenced by the formulation:<br />
Medicinal Agent --> Formulation --> Medication<br />
Galenic = Science of pharmaceutical formulation<br />
(Galenos of Pergamon, 129-199 AD)
BIMM118<br />
Drug Administration and Absorption<br />
Routes of Drug Administration:<br />
• Oral<br />
• Topical (Percutaneous)<br />
• Rectal or Vaginal<br />
• Pulmonal<br />
• Parenteral
BIMM118<br />
Oral Drug Administration<br />
• Pills<br />
– Antiquated single-dose unit; round, produced by mixing<br />
drug powder with syrup and rolling into shape<br />
• Tablets<br />
– Oblong or disk-like shape, produced through mechanical<br />
pressure; filler<br />
material provides mass; starch or carbonates facilitate<br />
disintegration
BIMM118<br />
Oral Drug Administration<br />
• Coated Tablets<br />
– Tablet covered by a “shell” (wax, highly specialized polymers =<br />
Eudragit®) to facilitate swallowing, cover bad taste or protect<br />
active ingredient from stomach acid
BIMM118<br />
Oral Drug Administration<br />
• Matrix Tablets<br />
– Drug is embedded in inert “carrier” meshwork --><br />
extended or targeted (intestinal) release<br />
• Capsules<br />
– Oblong casing (Gelatin); contains drug in liquid,<br />
powder or granulated form<br />
• Troches or Lozenges; Sublingual Tablets<br />
– Intended to be held in the mouth until dissolved
BIMM118<br />
Oral Drug Administration
BIMM118<br />
Oral Drug Administration<br />
• Aequous Solutions (with Sugar=Syrup)<br />
– Mostly for pediatric use<br />
– 20 drops=1g<br />
• Alcoholic Solutions (=Tinctures)<br />
– Often plant extracts<br />
– 40 drops=1g<br />
• Suspensions<br />
– Insoluble drug particles in aequous or lipophilic media
BIMM118<br />
Percutaneous Drug Administration<br />
Specific formulation determined by physician/dermatologist:<br />
• based on skin type:<br />
– Dry vs. Oily<br />
– Young vs. Old<br />
– Intact vs. Injured<br />
• based on drug properties:<br />
– Hydrophilic vs. Lipophilic<br />
– Soluble vs. Insoluble
BIMM118<br />
Percutaneous Drug Administration
BIMM118<br />
Percutaneous Drug Administration<br />
• Ointment and Lipophilic Cream<br />
– Either pure lipophilic base (lanolin=wool fat; paraffin oil; petrolium jelly) or<br />
“water-in-oil” emulsions<br />
• Paste<br />
– Ointment with >10% pulverized solids (e.g. Zinc- or Titanium-Oxide)<br />
• Lotion and Hydrophilic Cream<br />
– “oil-in-water” emulsions<br />
• Gels<br />
– Either alcohol or aequous solution based (Ethanol gels --> Cooling effect)<br />
– Increased consistency due to gel-forming agents
BIMM118<br />
Percutaneous Drug Administration<br />
•Transdermal Drug Delivery Systems =“Patches” (Nicotin, Isosorbid-Nitrate)<br />
– Single Layer<br />
• Inclusion of the drug directly within the skincontacting<br />
adhesive. In this transdermal<br />
system design, the adhesive not only serves<br />
to affix the system to the skin, but also<br />
serves as the formulation foundation<br />
– Multi-Layer<br />
• Similar to Single-layer, however, the multilayer<br />
encompasses either the addition of a<br />
membrane between two distinct drug-inadhesive<br />
layers or the addition of multiple<br />
drug-in-adhesive layers under a single<br />
backing film<br />
– Reservoir<br />
• Inclusion of a liquid compartment containing<br />
a drug solution or suspension separated from<br />
the release liner by a semi-permeable<br />
membrane and adhesive.
BIMM118<br />
•Eye Drops<br />
•Sterile; Isotonic; pH-neutral<br />
•Nose Drops/Nasal Sprays<br />
•Viscous Solutions<br />
Other Topical Drug Administration<br />
•Pulmonary Formulations<br />
•Inhalation anesthetics (Hospital use only)<br />
•Nebulizers (mostly propellant operated)<br />
•dispense defined amount of Aerosol<br />
(= dispersion of liquid or or solid particles in a gas)<br />
•Size of aerosol particles determines depth of penetration into the<br />
respiratory tract:<br />
>100 µm: Nasopharynx<br />
10-100 µm: Trachea, bronchii<br />
BIMM118<br />
Other Topical Drug Administration<br />
•Suppositories<br />
•Drug incorporated into a fat with a melting point ~35ºC<br />
•Rectal: Absorption mostly intended into systemic circulation (e.g. analgesics)<br />
•Vaginal: Effects intended to be confined to site of application (e.g. candidiasis)
BIMM118<br />
Parenteral Drug Administration<br />
Sterile; iso-osmolar; pyrogen-free; pH=7.4<br />
• Ampules<br />
– Single use (mostly with fracture ring)<br />
• Single and Multi-dose Vials<br />
– 10-100 ml; contain preservatives<br />
• Cartridge ampules<br />
• Infusions<br />
– Solution administered over an extended period of time
BIMM118<br />
• Advantages:<br />
– 100% “Absorption”<br />
Parenteral Drug Administration<br />
– Drug enters general circulation without hepatic passage --><br />
No first-pass hepatic elimination<br />
– Better bioavailability of hydrophilic drugs<br />
• Bioavailability/Speed of Absorption<br />
– Intravenous (i.v.): Fastest (infusions; cardio-vascular drugs)<br />
– Intramuscular (i.m.): Medium (anti-inflammatory; antibiotics)<br />
– Subcutaneous (s.c.): Slowest (vaccines; insulin; depot contraceptives)
BIMM118<br />
Drug Distribution
BIMM118<br />
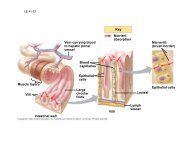
Drug Distribution<br />
• To be absorbed and distributed, drugs must cross barriers (membranes) to<br />
enter and leave the blood stream.<br />
• Body contains two type of barriers which are made up of epithelial or<br />
endothelial cells:<br />
– External (Absorption Barriers): Keratinized epithelium (skin), ciliated epithelium<br />
(lung), epithelium with microvilli (intestine), etc.<br />
These epithelial cells are connected via zonulae occludens (tight junctions) to create<br />
an unbroken phospholipid bilayer. Therefore, drugs MUST cross the lipophilic<br />
membrane to enter the body (except parenteral).
BIMM118<br />
Drug Distribution<br />
– Internal (Blood-Tissue Barriers): Drug permeation occurs mostly in the capillary bed,<br />
which is made up of endothelial cells joined via zonulae occludens.<br />
Blood-Tissue Barrier is developed differently in various capillary beds:<br />
• Cardiac muscle: high endo- and transcytotic activity-> drug transport via vesicles<br />
• Endocrine glands, gut: Fenestrations of endothelial cells (= pores closed by diaphragms)<br />
allow for the passage of small molecules.<br />
• Liver: Large fenestration (100 nm) without diaphragms-> drugs exchange freely between<br />
blood and interstitium<br />
• CNS, placenta: Endothelia lack pores and possess only little trans-cytotic activity-> drugs<br />
must diffuse transcellularly, which requires specific physicochemical properties -> Barriers<br />
are very restrictive, permeable only to certain types of drugs.
BIMM118<br />
• Membrane Permeation:<br />
– Passive Diffusion:<br />
Drug Distribution<br />
• Requires some degree of lipid solubility, which is in part determined by the charge of the<br />
molecule<br />
• For weak acids or bases (which account for the vast majority of drugs), the charge of the<br />
molecule in dependence of the pH of the medium is determined by the<br />
Henderson-Hasselbalch Equation:<br />
Log ([H + Drug] / [Drug]) = pK a - pH<br />
– Active Transport: Drugs “highjack” cellular transporter (e.g. L-DOPA uptake via L-amino acid<br />
carrier)<br />
– Receptor-mediated Endocytosis: Clathrin-coated pits form endosomal vesicles; receptor gets<br />
“recycled” to the cell surface
BIMM118<br />
Drug Distribution<br />
Drug concentration is a<br />
function of absorbtion<br />
AND elimination:<br />
Typical plasma drug<br />
concentration as function<br />
of time after a single oral<br />
dose<br />
AUC = Area Under Curve
BIMM118<br />
Drug Distribution<br />
Bioavailability (F):<br />
the AUC of the (orally)<br />
administered drug divided<br />
by the AUC of the<br />
intravenously<br />
administered drug
BIMM118<br />
Bioavailability:<br />
Drug Distribution<br />
• Intravenous 100% by definition<br />
• Intramuscular 75 to
BIMM118<br />
Drug Distribution<br />
Volume of Distribution (V d ) [ml or l]:<br />
= Amount of drug in the body [mg] / drug concentration plasma [mg/ml]<br />
• V d is an apparent volume (volume that the drug must be distributed<br />
in to produce measured plasma concentration<br />
• Drug with near complete restriction to plasma compartment would<br />
have V d = plasma volume (.04 L/kg) = 2.8 L/70 kg patient<br />
• But: Many drugs are highly tissue bound => large V d<br />
e.g. Chloroquine: V d = 13,000 L
BIMM118<br />
Drug Distribution<br />
Rate of Elimination:<br />
Drug elimination via kidney occurs by filtration => with falling blood<br />
concentration the amount of drug filtered per time unit diminishes<br />
Drug elimination via liver occurs by metabolism, where most enzymes<br />
operate in the quasi-linear range of their concentration-activity curve =><br />
with falling blood concentration the amount of drug metabolized per time<br />
unit diminishes<br />
==>Vast majority of drugs follows first-order kinetics (= rate is proportional to drug<br />
concentration)<br />
Only three drugs follow linear, zero-order (=concentration-independent)<br />
elimination characteristic: Ethanol, Aspirin and Phenytoin
BIMM118<br />
Clearance (CL) [ml/min]:<br />
Drug Distribution<br />
= Rate of Elimination [mg/min] / Drug concentration plasma (C P ) [mg/ml] where<br />
Rate of Elimination [mg/min] = k [1/min] x C P [mg/ml] x V d [ml] and<br />
Elimination rate constant (k) [1/min] = ln 2 / t 1/2 (=half-life)<br />
(ln 2 = 0.693)<br />
=> CL [ml/min] = Elimination rate constant (k) [1/min] x V d [ml] = ln 2 x V d / t 1/2<br />
• It is the sum of all separate organ clearances:<br />
CL = CL renal + CL liver + CL other<br />
• Clearance is the volume of plasma cleared of all drug per unit of time (a<br />
constant for any given drug [ml/min])<br />
• The actual quantity of drug [mg] removed per time unit [min] depends on both<br />
the clearance [ml/min] and the concentration [mg/ml].
BIMM118<br />
Half-life (t 1/2 ) [min]:<br />
Drug Distribution<br />
= ln 2 x V d [ml] / CL [ml/min] (ln 2 = 0.693)<br />
or<br />
= ln 2 / Elimination rate constant (k) [1/min]<br />
• Half-life is the time required for the concentration of a drug to<br />
fall by 50%<br />
• The half-life is constant and related to (k) for drugs that<br />
follow first-order kinetics
BIMM118<br />
Drug Distribution<br />
Dosage Regimens:<br />
With multiple dosing or continuous infusion, a drug will accumulate until<br />
the amount administered per time unit equals the amount eliminated per<br />
time unit. The plasma concentration at this point is called the steady-state<br />
concentration (C SS ) [mg/ml]:<br />
C SS = Infusion rate [mg/min] /<br />
Clearance [ml/min]<br />
Typically, 90% of the C SS is<br />
reached after 3.3 half-lifes;<br />
~100% after 5 half-lifes
BIMM118<br />
Loading Dose:<br />
Drug Distribution<br />
For drugs with long t 1/2 , 3-5 half-lifes is to long to wait for C SS<br />
=> loading dose is used.<br />
Loading dose must ‘fill’ the V d to achieve the target C P :<br />
Maintenance Dose:<br />
Loading dose [mg] = V d [ml] x C P [mg/ml]<br />
Must replace the drug that is being eliminated over time:<br />
C SS [mg/ml] = Infusion rate [mg/min] / Clearance [ml/min] =><br />
Infusion rate [mg/min] = Clearance [ml/min] x C SS [mg/ml] =><br />
Infusion rate [mg/min] = ln 2 x V d [ml] / t 1/2 [min] x C SS [mg/ml]
BIMM118<br />
Drug Distribution<br />
• Drug Binding to Plasma Proteins:<br />
• Primarily albumin (4.6g/100ml), also β-globulins and acidic glycoproteins<br />
• Other specialized plasma proteins (transcortin; thyroxin-binding globulin; etc.)<br />
Binding to plasma proteins is instantaneous and reversible.<br />
• Of great importance, as the free (=effective) drug concentration determines<br />
intensity of response<br />
Drug-protein binding also influences biotransformation and elimination =><br />
Binding to plasma proteins is equivalent to depot formulations<br />
– Possible site for drug interactions:<br />
If two drugs bind to the same site on e.g. the albumin molecule, then drug B has<br />
the potential of displacing drug A from its binding site --> effective concentration<br />
of drug A is increased --> Toxic concentration or increased elimination<br />
– Impaired liver function:<br />
can lead to altered pharmacokinetics of drugs that bind to albumin at high rates<br />
due to decreased albumin concentrations in the blood
BIMM118<br />
BLOOD LEVEL<br />
TOXIC<br />
LEVELS<br />
Margin of safety<br />
Margin of safety<br />
THERAPEUTIC<br />
RANGE<br />
Therapeutic Range<br />
TIME<br />
In this example the<br />
treatment would not be<br />
effective as a therapeutic<br />
concentration in the blood<br />
is not maintained
BIMM118<br />
BLOOD LEVEL<br />
TOXIC<br />
LEVELS<br />
Margin of safety<br />
Margin of safety<br />
THERAPEUTIC<br />
RANGE<br />
Therapeutic Range<br />
TIME<br />
In this example severe<br />
toxicity would occur as the<br />
therapeutic concentration<br />
in the blood is exceeded<br />
due to accumulation of the<br />
drug
BIMM118<br />
BLOOD LEVEL<br />
TOXIC<br />
LEVELS<br />
Margin of safety<br />
Margin of safety<br />
THERAPEUTIC<br />
RANGE<br />
Therapeutic Range<br />
TIME<br />
In this example the<br />
treatment would be<br />
effective as the therapeutic<br />
concentration in the blood<br />
is maintained without<br />
approaching toxic levels
BIMM118<br />
• Therapeutic Index:<br />
Therapeutic Range<br />
= Maximum non-toxic dose / Minimum effective dose<br />
Problem:<br />
Does not take into account variability between individuals<br />
=> “Improved formula”:<br />
= LD 50 / ED 50<br />
Problems:<br />
• LD 50 reflects only death, but no other toxic side effects (e.g. Ototoxicity of aminoglycosides)<br />
• ED 50 depends on condition treated (e.g. Aspirin: Headache vs. rheumatism)<br />
• LD 50 depends on patients overall condition (e.g. Aspirin: dangerous to asthmatic patients)<br />
==><br />
Therapeutic Index is not particularly useful to describe the clinical usefulness of a drug!
BIMM118<br />
Drug Metabolism and Elimination<br />
• Elimination of drugs occurs primarily through renal mechanism<br />
– Secretion into bile also possible, but allows for re-absorption in the intestine<br />
• Secretion into the urine requires ionized or hydrophilic molecules, but:<br />
– Most drugs are not small molecules that are highly ionized at body pH<br />
– Most drugs are poorly ionized and lipophilic<br />
=> This decreases renal excretion and facilitates renal tubular reabsorption<br />
– Many drugs are highly protein bound, and therefore not efficiently filtered in the kidney<br />
– Most drugs would have a long duration of action if termination of their effects<br />
depended only on renal excretion<br />
Solution: Drug Metabolism
BIMM118<br />
Drug Metabolism<br />
• Most metabolic products are less pharmacologically active<br />
Important exceptions:<br />
• Where the metabolite is more active<br />
(Prodrugs, e.g. Erythromycin-succinate (less irritation of GI) --> Erythromycin)<br />
• Where the metabolite is toxic (acetaminophen)<br />
• Where the metabolite is carcinogenic<br />
• Close relationship between the biotransformation of drugs and normal biochemical<br />
processes occurring in the body:<br />
– Metabolism of drugs involves many pathways associated with the synthesis of endogenous<br />
substrates such as steroid hormones, cholesterol and bile acids<br />
– Many of the enzymes involved in drug metabolism are principally designed for the metabolism<br />
of endogenous compounds<br />
– These enzymes metabolize drugs only because the drugs resemble the natural compound
BIMM118<br />
• Phase I Reactions<br />
Phases of Drug Metabolism<br />
– Convert parent compound into a more polar (=hydrophilic) metabolite by adding or<br />
unmasking functional groups (-OH, -SH, -NH2, -COOH, etc.)<br />
– Often these metabolites are inactive<br />
– May be sufficiently polar to be excreted readily<br />
• Phase II Reactions<br />
– Conjugation with endogenous substrate to further increase aqueous solubility<br />
– Conjugation with glucoronide, sulfate, acetate, amino acid<br />
– Phase I usually precede phase II reactions<br />
Liver is principal site of drug metabolism:<br />
– Other sites include the gut, lungs, skin and kidneys<br />
– For orally administered compounds, there is the<br />
“First Pass Effect”<br />
• Intestinal metabolism<br />
• Liver metabolism<br />
• Enterohepatic recycling<br />
• Gut microorganisms - glucuronidases
BIMM118<br />
Drug Metabolism
BIMM118<br />
Drug Metabolism - Phase I<br />
• Phase I Reactions<br />
– Oxidation<br />
– Reduction<br />
– Hydrolytic cleavage<br />
– Alkylation (Methylation)<br />
– Dealkylation<br />
– Ring cyclization<br />
– N-carboxylation<br />
– Dimerization<br />
– Transamidation<br />
– Isomerization<br />
– Decarboxylation
BIMM118<br />
Drug Metabolism - Oxidation<br />
Two types of oxidation reactions:<br />
– Oxygen is incorporated into the drug molecule (e.g. hydroxylation)<br />
– Oxidation causes the loss of part of the drug molecule<br />
(e.g. oxidative deimination, dealkylation)<br />
Microsomal Mixed Function Oxidases (MFOs)<br />
• “Microsomes”<br />
form in vitro after cell homogenization and fractionation of ER<br />
– Rough microsomes are primarily associated with protein synthesis<br />
– Smooth microsomes contain a class of oxidative enzymes called<br />
• “Mixed Function Oxidases” or “Monooxygenases”<br />
– These enzymes require a reducing agent (NADPH) and molecular oxygen<br />
(one oxygen atom appearing in the product and the other in the form of water)
BIMM118<br />
Drug Metabolism - Oxidation<br />
• MFO consists of two enzymes:<br />
– Flavoprotein, NADPH-cytochrome c reductase<br />
• One mole of this enzyme contains one mole each of flavin<br />
mononucleotide (FMN) and flavin adenine dinucleotide (FAD)<br />
• Enzyme is also called NADPH-cytochrome P450 reductase<br />
– Cytochrome P450<br />
• named based on its light absorption at 450 nm when complexed<br />
with carbon monoxide<br />
• is a hemoprotein containing an iron atom which can alternate<br />
between the ferrous (Fe ++ ) and ferric (Fe +++ ) states<br />
• Electron acceptor<br />
• Serves as terminal oxidase<br />
• its relative abundance compared to NADPH-cytochrome P450<br />
reductase makes it the rate-limiting step in the oxidation reactions
BIMM118<br />
Drug Metabolism - Oxidation<br />
• Humans have 18 families of cytochrome P450 genes and 43 subfamilies:<br />
– CYP1 drug metabolism (3 subfamilies, 3 genes, 1 pseudogene)<br />
– CYP2 drug and steroid metabolism (13 subfamilies, 16 genes, 16 pseudogenes)<br />
– CYP3 drug metabolism (1 subfamily, 4 genes, 2 pseudogenes)<br />
– CYP4 arachidonic acid or fatty acid metabolism (5 subfamilies, 11 genes, 10 pseudogenes)<br />
– CYP5 Thromboxane A2 synthase (1 subfamily, 1 gene)<br />
– CYP7A bile acid biosynthesis 7-alpha hydroxylase of steroid nucleus (1 subfamily member)<br />
– CYP7B brain specific form of 7-alpha hydroxylase (1 subfamily member)<br />
– CYP8A prostacyclin synthase (1 subfamily member)<br />
– CYP8B bile acid biosynthesis (1 subfamily member)<br />
– CYP11 steroid biosynthesis (2 subfamilies, 3 genes)<br />
– CYP17 steroid biosynthesis (1 subfamily, 1 gene) 17-alpha hydroxylase<br />
– CYP19 steroid biosynthesis (1 subfamily, 1 gene) aromatase forms estrogen<br />
– CYP20 Unknown function (1 subfamily, 1 gene)<br />
– CYP21 steroid biosynthesis (1 subfamily, 1 gene, 1 pseudogene)<br />
– CYP24 vitamin D degradation (1 subfamily, 1 gene)<br />
– CYP26A retinoic acid hydroxylase important in development (1 subfamily member)<br />
– CYP26B probable retinoic acid hydroxylase (1 subfamily member)<br />
– CYP26C probabvle retinoic acid hydroxylase (1 subfamily member)<br />
– CYP27A bile acid biosynthesis (1 subfamily member)<br />
– CYP27B Vitamin D3 1-alpha hydroxylase activates vitamin D3 (1 subfamily member)<br />
– CYP27C Unknown function (1 subfamily member)<br />
– CYP39 7 alpha hydroxylation of 24 hydroxy cholesterol (1 subfamily member)<br />
– CYP46 cholesterol 24-hydroxylase (1 subfamily member)<br />
– CYP51 cholesterol biosynthesis (1 subfamily, 1 gene, 3 pseudogenes) lanosterol 14-alpha demethylase
BIMM118<br />
Drug Metabolism - Oxidation<br />
• Induction of P450 enzymes:<br />
– PPAR (peroxisome proliferator activated receptor) ligands<br />
(e.g.clofibrate)<br />
– CYP1 family are induced by aromatic hydrocarbons<br />
(cigarette smoke; charred food)<br />
– CYP2E enzymes induced by ethanol<br />
– CYP2B enzymes induced 40-50 fold by barbiturates<br />
• Polymorphisms cause differences in drug metabolism:<br />
– CYP2C19 has a polymorphism that changes the enzyme's ability to metabolize mephenytoin (a<br />
marker drug). In Caucasians, the polymorphism for the poor metabolizer phenotype is only seen<br />
in 3% of the population. However, it is seen in 20% of the asian population.<br />
=> It is important to be aware of a person's race when drugs are given that are<br />
metabolized differently by different populations<br />
• P450s and drug interactions:<br />
– Barbiturates induce CYP2B => increased metabolism of other drugs<br />
– Antifungals (e.g. ketoconazole) inhibit fungal CYP51 and unintentionally also human CYP3A4<br />
=> reduced metabolism of other drugs<br />
– Grapefruit juice contains a CYP3A4 inhibitor =>12 fold increase in some drug concentrations<br />
CYP3A4 Substrates: • Acetominophen (Tylenol) • Codeine (narcotic) • Cyclosporin A (immunosuppressant),<br />
• Diazepam (Valium) • Erythromycin (Antibiotic) • Lidocaine (local anaesthetic), • Lovastatin (HMGCoA<br />
reductase inhibitor), • Taxol (cancer drug), • Warfarin (anticoagulant).
BIMM118<br />
• Drug oxidation requires:<br />
– Cytochrome P450<br />
– Cytochrome P450 reductase<br />
– NADPH<br />
– Molecular oxygen<br />
• The cycle involves four steps:<br />
Drug Metabolism - Oxidation<br />
1. Oxidized (Fe3+) cytochrome P-450 combines with a drug substrate to form a binary complex.<br />
2. NADPH donates an electron to the cytochrome P-450 reductase, which in turn reduces the<br />
oxidized cytochrome P-450-drug complex.<br />
3. A second electron is introduced from NADPH via the same cytochrome P-450 reductase, which<br />
serves to reduce molecular oxygen and form an "activated oxygen"-cytochrome P-450-substrate<br />
complex.<br />
4. This complex in turn transfers "activated" oxygen to the drug substrate to form the oxidized<br />
product. The potent oxidizing properties of this activated oxygen permit oxidation of a large number<br />
of substrates.
BIMM118<br />
Aromatic hydroxylation:<br />
Aliphatic hydroxylation:<br />
Drug Metabolism - Oxidation
BIMM118<br />
Epoxidation:<br />
Dealkylation:<br />
Drug Metabolism - Oxidation
BIMM118<br />
Drug Metabolism - Oxidation<br />
O-demethylation: S-demethylation:<br />
N-oxidation: N-hydroxylation:
BIMM118<br />
Drug Metabolism - Oxidation<br />
Oxidation reactions NOT catalyzed by Cytochrome P450:<br />
Flavin containing monoxygenase system<br />
– Present mainly in liver but some is expressed in gut and lung<br />
– Located in smooth endoplasmic reticulum<br />
– Oxidizes compounds containing sulfur and nitrogen<br />
– Uses NADH and NADPH as cofactors<br />
• Alcohol dehydrogenase (cytosol)<br />
• Aldehyde oxidation (cytosol)<br />
• Xanthine oxidase<br />
• Amine oxidases<br />
– Monoamine oxidase (nerve terminals, mitochondria)<br />
– Diamine oxidase found in liver microsomes<br />
• Primarily endogenous metabolism
BIMM118<br />
Monoamine Oxidases (MAO):<br />
Drug Metabolism - Oxidation<br />
• Catalyze oxidative deamination of endogenous catecholamines (epinephrine)<br />
• Located in nerve terminals and peripheral tissues<br />
• Substrates for catecholamine metabolism found in foods (tyramine) can<br />
cause a drug/food interaction<br />
• Inhibited by class of antidepressants called MAO inhibitors<br />
(Inhibition of MAO isoforms in the CNS also effects levels of serotonin - Tranylcypromine)<br />
These drugs can cause severe or fatal drug/drug interactions with drugs that<br />
increase release of catecholamines or inhibit their reuptake in nerve terminals<br />
(Meperidine, pentazocine, dextromethorphan, SSRI antidepressants)
BIMM118<br />
Azo-reduction:<br />
Nitro-reduction:<br />
Dehalogenation:<br />
Drug Metabolism - Reduction
BIMM118<br />
Hydrolysis reactions<br />
Ester hydrolysis:<br />
Drug Metabolism - Reduction<br />
Amide hydrolysis:
BIMM118<br />
Drug Metabolism - Phase I<br />
• Almost any drug can undergo modifications by drug-metabolizing<br />
enzyme systems<br />
• Drugs can be subject to several Phase I pathways<br />
• These reactions create functional groups that place the drugs in a<br />
correct chemical state to be acted upon by Phase II conjugative<br />
mechanisms<br />
• Main function of phase I reactions is to prepare chemicals for phase II<br />
metabolism and subsequent excretion<br />
• Phase II is the true “detoxification” step in the metabolism process.
BIMM118<br />
Drug Metabolism - Phase II<br />
• Conjugation reactions<br />
– Glucuronidation by UDP-Glucuronosyltransferase:<br />
(on -OH, -COOH, -NH2, -SH groups)<br />
– Sulfation by Sulfotransferase:<br />
(on -NH2, -SO2NH2, -OH groups)<br />
– Acetylation by acetyltransferase:<br />
(on -NH2, -SO2NH2, -OH groups)<br />
– Amino acid conjugation<br />
(on -COOH groups)<br />
– Glutathione conjugation by Glutathione-S-transferase:<br />
(to epoxides or organic halides)<br />
– Fatty acid conjugation<br />
(on -OH groups)<br />
– Condensation reactions
BIMM118<br />
Drug Metabolism - Glucuronidation<br />
• Glucuronidation ( = conjugation to α-d-glucuronic acid)<br />
– Quantitatively the most important phase II pathway for drugs and endogenous<br />
compounds<br />
– Products are often excreted in the bile.<br />
– Enterohepatic recycling may occur due to gut glucuronidases<br />
– Requires enzyme UDP-glucuronosyltransferase (UGT):<br />
• Genetic family of enzymes<br />
– Metabolizes a broad range of structurally diverse endogenous and exogenous compounds<br />
– Structurally related family with approximately 16 isoforms in man
BIMM118<br />
Drug Metabolism - Glucuronidation<br />
• Glucuronidation – requires creation of high energy intermediate:<br />
UDP-Glucuronic Acid:
BIMM118<br />
Drug Metabolism - Glucuronidation<br />
• Glucuronidation Pathway and Enterohepatic Recirculation
BIMM118<br />
Drug Metabolism - Glucuronidation<br />
• N-glucuronidation:<br />
– Occurs with amines (mainly aromatic )<br />
– Occurs with amides and sulfonamides
BIMM118<br />
Drug Metabolism - Glucuronidation<br />
• O-glucuronidation:<br />
– Occurs by ester linkages with carboxylic acids<br />
– Occurs by ether linkages with phenols and alcohols
BIMM118<br />
Sulfation:<br />
Drug Metabolism - Sulfation<br />
• Major pathway for phenols but also occurs for alcohols, amines and thiols<br />
• Energy rich donor required:<br />
PAPS (3’-Phosphoadenosine-5’-phosphosulfate)<br />
• Sulfation and glucuronidation are competing pathways:<br />
– Sulfation predominates at low substrate concentrations<br />
– Glucuronidation predominates at higher concentrations<br />
– There is relatively less PAPS in cell cytosol compared to UDPGA<br />
• Sulfotransferases (=SULTs) catalyze transfer of sulfate to substrates:<br />
– Phenol, alcohol and arylamine sulfotransferases are fairly non-specific<br />
– Steroid sulfotransferases are very specific
BIMM118<br />
Acetylation:<br />
Drug Metabolism - Acylation<br />
• Common reaction for aromatic amines and sulfonamides<br />
• Requires co-factor acetyl-CoA<br />
• Responsible enzyme is N-acetyltransferase<br />
• Takes place mainly in the liver<br />
• Important in sulfonamide metabolism because acetyl-sulfonamides are less<br />
soluble than the parent compound and may cause renal toxicity due to<br />
precipitation in the kidney<br />
Fatty Acid Conjugation:<br />
• Stearic and palmitic acids are conjugated to drug by esterification reaction<br />
• Occurs in liver microsomal fraction<br />
(Cannabiols are excreted in this fashion => long half-life)
BIMM118<br />
Drug Metabolism - Other conjugations<br />
Amino Acid Conjugation:<br />
• ATP-dependent acid:CoA ligase forms active CoA-amino acid conjugates which then<br />
react with drugs by N-Acetylation:<br />
– Usual amino acids involved are:<br />
• Glycine. Glutamine, Ornithine, Arginine<br />
Glutathione Conjugation:<br />
• Tripeptide Gly-Cys-Glu; conjugated by glutathione-S-transferase (GST)<br />
• Glutathione is a protective factor for removal of potentially toxic compounds<br />
• Conjugated compounds can subsequently be attacked by<br />
γ-glutamyltranspeptidase and a peptidase to yield the cysteine conjugate =><br />
product can be further acetylated to N-acetylcysteine conjugate
BIMM118<br />
Drug Metabolism - Phase I & II<br />
Phase I and II - Summary:<br />
• Products are generally more water soluble<br />
• These reactions products are ready for (renal) excretion<br />
• There are many complementary, sequential and competing<br />
pathways<br />
• Phase I and Phase II metabolism are a coupled interactive<br />
system interfacing with endogenous metabolic pathways
BIMM118<br />
Drug Action: Receptor Theory<br />
Many drugs act by binding to receptors (see Lecture 4) where they either provoke<br />
or inhibit a biological response.<br />
Agonists:<br />
• Can be drugs or endogenous ligands for the receptor<br />
• Increasing concentrations of the agonist will produce an increase in the<br />
biological response:<br />
– Full Agonist: Evokes 100% of the maximum possible effect<br />
– Partial Agonist: Produces the same type of biological response, but cannot<br />
achieve 100% even at very high doses
BIMM118<br />
Antagonists:<br />
Drug Action: Receptor Theory<br />
• Block or reverse the effects of agonists. They have no effects on their own<br />
– Competitive Antagonists: Compete with agonist for receptor binding => Agonist<br />
appears less potent, but can still achieve 100% effect (but at higher<br />
concentrations)<br />
– Non-competitive Antagonists: Bind to receptor at different site and either prevent<br />
agonist binding or the agonist effect => maximal achievable response reduced<br />
– Inverse Agonists: Not the same as antagonists! Inverse agonists trigger a<br />
negative response (= reduce baseline) (e.g. diazepam = full agonist =<br />
anticonvulsant BUT inverse agonists of benzodiazepin receptor are convulsants)
BIMM118<br />
Four major drug targets:<br />
Drug Targets<br />
Exceptions: Colchicin (acts on tubulin), Cyclosporin (acts via immunophillins), etc.
BIMM118<br />
Drug Targets
BIMM118<br />
Drug Targets
BIMM118<br />
Drug Targets: Receptors<br />
Responses to the extracellular environment involve cell membrane or<br />
intracellular receptors whose engagement modulates cellular components<br />
that generate, amplify, coordinate and terminate postreceptor signaling via<br />
(cytoplasmic) second messengers.<br />
Transmembrane signaling is accomplished by only a few mechanisms:<br />
– Transmembrane ion channels: open or close upon binding of a ligand or upon<br />
membrane depolarization<br />
– G-protein-coupled receptors: Transmembrane receptor protein that stimulates<br />
a GTP-binding signal transducer protein (G-protein) which in turn generates an<br />
intracellular second messenger<br />
– Nuclear receptors: Lipid soluble ligand that crosses the cell membrane and acts<br />
on an intracellular receptor<br />
– Kinase-linked receptors: Transmembrane receptor proteins with intrinsic or<br />
associated kinase activity which is allosterically regulated by a ligand that binds to<br />
the receptor’s extracellular domain
BIMM118<br />
Drug Targets: Receptors
BIMM118<br />
Receptors<br />
• Rapidly acting (milliseconds) transmembrane ion channels: Multi-unit complexes<br />
with central aqueous channel. Upon binding of a ligand, channel opening allows a<br />
specific ion travel down its concentration gradient ==><br />
Transient cell membrane depolarization (post synaptic potential)<br />
• Example: Nicotinic acetylcholine receptor: Pentameric structure (two alpha chains, one each<br />
beta, gamma, and delta chain). Activation occurs by binding of two molecules ACh to the alpha<br />
subunits, triggering the opening of the channel for Na + and K + ions.<br />
Myasthenia gravis: Autoimmune disease caused by inactivating antibodies against NAchR
BIMM118<br />
Receptors<br />
Many other types of transmembrane ion channels ==><br />
Ion channels are common drug targets!<br />
• Voltage-gated channels:<br />
• Gating: controlled by membrane polarization/depolarization<br />
• Selectivity: Na + , K + or Ca + ions<br />
• Intracellular ligand-gated channels:<br />
• Ca + controlled K + channel<br />
• ATP-sensitive K + channel<br />
• IP 3 -operated Ca + channel (in the ER membrane)
BIMM118<br />
Calcium as Second Messenger<br />
Ca ++ ==> very important in regulating cellular and physiological responses<br />
– Extracellular concentrations are 2 mM (EM, blood), and levels in cytoplasmic vesicles and the<br />
ER can reach up to 10mM.<br />
– Baseline cytosolic Ca 2+ concentration is around 100 nM in resting cells.<br />
Conc in mM ECF ICF<br />
K+ 4.5 160<br />
Na+ 144 7<br />
Cl- 114 7<br />
Ca++ 2.2 0.0001<br />
– High gradient makes this a very fast and sensitive signaling system: only slight changes in<br />
membrane permeability will result in dramatic changes in the concentration of [Ca 2+ ] i .<br />
– Low level of [Ca 2+ ] i is also necessary to facilitate a phosphate oriented cellular metabolism<br />
(high calcium and high phosphate concentrations are incompatible!!)<br />
==> Evolutionary challenge: Maintain calcium gradient !!!<br />
– Evolvement of proteins that bind Ca 2+ with high affinity, but reject magnesium!<br />
– Two classes of Ca-binding proteins:<br />
• membrane-integrated (unlimited capacity --> transporter systems: Ca-channels, calcium pumps)<br />
• non-membranous (limited capacity --> not only buffering, but processing of signal through<br />
conformational changes that enable interaction with target proteins: Calmodulin, Troponin C ...)
BIMM118<br />
Sources of Ca ++ :<br />
Calcium as Second Messenger<br />
• Extracellular compartment: (predominantly in nerve, cardiac and smooth muscle cells)<br />
Three types of plasma-membrane localized calcium channels:<br />
– Voltage operated calcium channels:<br />
Action potental depolarizes plasma membrane, which results in the opening of “voltage”<br />
dependent calcium channels (channels can be opened by increase in extracellular K + ).<br />
Each channel protein has four homologous domains, each containing six membrane spanning<br />
α-helices (the fourth one functions as the “voltage” sensor.
BIMM118<br />
Three types:<br />
Type<br />
L<br />
N<br />
T<br />
Calcium as Second Messenger<br />
Properties<br />
High activation threshold;<br />
slow inactivation<br />
Low activation threshold;<br />
slow inactivation<br />
Low activation threshold;<br />
fast inactivation<br />
– Ligand gated calcium channels:<br />
Calcium channels opened after ligand binding to the receptor (e.g. glutamate/NMDA receptor;<br />
ATP receptor; nicotinic ACh receptors ( muscarinic ACh receptors signal through G-Proteins<br />
--> slower), prostaglandin receptors<br />
– Store operated calcium channels:<br />
Location/Function<br />
Plasma membrane of many cells;<br />
main Ca ++ source for contraction in<br />
smooth and cardiac muscle<br />
Main Ca ++ source for transmitter<br />
release by nerve terminals<br />
Widely distributed; important in<br />
cardiac pacemaker and Purkinje<br />
cells<br />
Activated by emptying of intracellular stores, exact mechanism unknown<br />
Blockers<br />
Dihydropyridines;<br />
verapamil; diltiazem<br />
ω-Conotoxin<br />
(snail venom)<br />
Mibefradil; (verapamil;<br />
diltiazem)
BIMM118<br />
Calcium as Second Messenger<br />
Intracellular compartment: (predominantly in muscle cells)<br />
– Calcium stored in mM concentrations in endo/sarcoplasmatic reticulum bound to Calsequestrin .<br />
(Previously mitochondria were thought to play an important role as Ca ++ -stores, but the uptake rate<br />
is 10x lower than that of the ER/SR -> not useful)<br />
Calcium release from the ER/SR is regulated by two receptors in the ER/SR membrane:<br />
– Ryanodine receptors (RyR):<br />
• Named after sensitivity to Ryanodine: plant alkaloid, irreversible inhibitor<br />
• Very important in skeletal muscle: direct coupling of RyRs with the dihydropyridine receptors of the T-tubules<br />
(dihydropyridine receptors are closely related to the L-type Ca ++ channels) (see Ca ++ effects)<br />
• Activity of RyRs in non-muscle cell lacking T-tubules regulated by cyclic ADP ribose<br />
• Caffeine: reversible activator of RYRs<br />
– IP 3 - Receptors (IP 3 R):<br />
• Inositol-1,4,5-triphosphate is produced through the<br />
activity of receptor activated phospholipases C --><br />
diffuses through cytoplasm and binds IP 3 R
BIMM118<br />
Removal of Ca ++ :<br />
• Ca ++ - pumps:<br />
Calcium as Second Messenger<br />
Activity of these pumps is induced by increases in cytosolic calcium.<br />
– Plasma membrane Na + /Ca 2+ exchanger (mainly in excitable cells, e.g. cardiac cells)<br />
three Na + - ions are exchanged for one Ca ++ -ion<br />
Digitalis alkaloids: Na + / K + -ATPase inhibitors => intracellular Na + raises => Na + /Ca 2+ exchange less efficient =><br />
Ca 2+ intracellular increases => stronger contractions<br />
– Plasma membrane Ca 2+ -ATPase (PMCA)<br />
two Ca ++ - ions are transported per ATP molecule hydrolyzed; regulated by CaM, PKA or PKC<br />
– SR/ER Ca ++ -ATPase (SERCA):<br />
80% (!) of integral membrane protein of SR<br />
target of thapsigargin ( => Ca ++ -release from intracellular stores)<br />
• Ca ++ - buffers:<br />
Low affinity (!) but high capacity (50-100 Ca ++ -ions/molecule)<br />
– Calsequestrin (very acidic, 37% of amino acids are aspartic and glutamic acid),<br />
– Calreticulin, Parvalbumin
BIMM118<br />
Ca ++ Sensors:<br />
• Annexins:<br />
Calcium as Second Messenger<br />
Family of proteins w/ common feature that they interact w/ membranes in a Ca ++ - dependent manner.<br />
Low affinity for Ca ++ -ions restricts action to membrane proximity (high local Ca ++ conc.!);<br />
implicated in the regulation of PLA2, cytoskeletal (re)organization and vesicle movement<br />
• EF-hand proteins:<br />
named after the shape created by the E and F α-helices of the Ca ++ -binding domain; high affinity
BIMM118<br />
Calcium as Second Messenger<br />
– Calmodulin:<br />
ubiquitous expression; binds 4 Ca ++ -ions; acts through stimulation of either protein kinases<br />
(CaMKs)<br />
or protein phosphatases (Calcineurin); also activates cAMP phosphodiesterase<br />
– Troponin C:<br />
restricted expression, regulates contraction of skeletal and heart muscle
BIMM118<br />
Calcium as Second Messenger
BIMM118<br />
Calcium as Second Messenger<br />
Function of cytoplasmic free Ca ++ :<br />
• Muscle contraction:<br />
– Skeletal and cardiac muscle:<br />
• Contraction (=actin-myosin interaction) controlled by proteins on actin filaments (tropomyosin w/ troponin)<br />
• Troponin I inhibits formation of cross-bridges between actin and myosin => muscle relaxed.<br />
• Troponin C combines with Ca 2+ -ions and blocks the action of Troponin I => muscle contracted
BIMM118<br />
– Smooth muscle:<br />
Calcium as Second Messenger<br />
Contraction controlled by proteins acting either on actin....<br />
• NO Troponin=>regulation occurs through the CaM binding Caldesmon :<br />
Low [Ca ++ ]: Caldesmon forms complex with actin and tropomyosin => access of myosin to actin restricted<br />
=>muscle relaxed.<br />
… or on myosin<br />
• Myosin light chains inhibit actin-myosin interaction:<br />
phosphorylation of myosin light chain (MLC) by MLC kinase (MLCK) relieves this inhibition =><br />
phosphorylated myosin is able to interact w/ actin => contraction
BIMM118<br />
Calcium as Second Messenger<br />
• Neuronal excitibility and secretion:<br />
– Increase of [Ca ++ ] induces fusion of the synaptic vesicles with the plasma mambrane =><br />
this causes exocytosis of neuro-transmitters into the synaptic cleft.
BIMM118<br />
• Immune response:<br />
Calcium as Second Messenger<br />
– TCR stimulation => [Ca ++ ] increases => activates Calcineurin => dephosphorylates NFATc on<br />
ser/thr => NFATc translocates to nucleus where it combines with NFATn and induces transcription<br />
of IL-2 gene => T cell proliferation<br />
Calcineurin: target of immunesuppressive drugs FK506 and ciclosporin, which form a complex with<br />
immunophillins and compete with Ca ++ /CaM for binding to calcineurin => no NFATc activation
BIMM118<br />
G-Protein-coupled Receptors<br />
GPCR: Large family of receptors with a probable common evolutionary precursor. Transmembrane protein<br />
that is serpentine in shape, crossing the lipid bilayer seven times.<br />
G-Proteins:<br />
– Guanine nucleotide binding proteins:<br />
participate in reversible, GTP-mediated interactions.<br />
– Common features:<br />
• bind GDP and GTP with high affinity, but adopt different structure depending on the bound nucleotide.<br />
• GTP-bound complex has high affinity for other proteins (“acceptor’), affecting their enzymatic activity<br />
• possess intrinsic GTPase activity that is usually activated by interaction with regulatory proteins (e.g. GAPs)<br />
• covalent attachment of various lipids (myristoylation, palmitoylation,...) is responsible for membrane targeting<br />
– Additional control exerted through:<br />
• GTPase Activating Proteins (GAPs): function on small GTP binding proteins<br />
• Guanine-nucleotide Exchange Factors (GEFs): promote GDP release<br />
• Regulators of G-protein Signaling (RGSs): similar to GAPs, but act on heterotrimeric G-Proteins
BIMM118<br />
G-Proteins:<br />
Two major groups:<br />
G-Protein-coupled Receptors<br />
• “Small GTP binding proteins” (act downstream of receptor: ras, rac etc.) => see growth factor<br />
receptor signaling<br />
• “Heterotrimeric G-proteins” (directly coupled to receptor and enzyme):<br />
• Coupled to 7 transmembrane spanning receptors: (β-adrenergic R, PG-R)<br />
• All members are heterotrimeric, consisting of α, β and γ subunits
BIMM118<br />
G-Protein-coupled Receptors<br />
α, β and γ subunits:<br />
α-subunit (23 isoforms): contains the GTP/GDP binding site, is responsible for identity<br />
β (5 isoforms) and γ (12 isoforms) subunits: are identical or very similar; interchangeable in vitro;<br />
most of them are ubiquitiously expressed; membrane anchored through prenylation of G β<br />
– G q and<br />
– G olf (expressed only in olfactory cells) are coupled to PLCβ<br />
– G T (=Transducin) is coupled to a cGMP phosphodiesterase and is expressed only in the rod cells of the<br />
retina (these cells are INactivated by light!). Photons hit Rhodopsin => activated opsin is generated =><br />
facilitates GTP loading of G T => activates cGMP phosphodiesterase => cGMP (keeps Na + and Ca 2+<br />
channels open to cause membrane depolarization => neuro-transmitter release) converted to 5’GMP<br />
(inactive => channels closed) => membrane polarization => NO neurotransmitter release)
BIMM118<br />
Main targets:<br />
Phospholipase Cβ:<br />
G-Protein-coupled Receptors<br />
see Lipid and Inositol Signaling<br />
Adenylate cyclase:<br />
• Two repeats of six transmembrane α-helices and two catalytic domains that convert ATP into cAMP<br />
• Activated or inhibited by G-proteins (a brain specific isoform is also activated through activated CaM):<br />
GTP-bound G αs activates AC, GTP-bound G αi inhibits activity (Forskolin: direct activator of AC => cAMP⇑)
BIMM118<br />
G-Protein-coupled Receptors<br />
Cholera-toxin: causes ADP-ribosylation of G sα => release of GTP inhibited => G sα trapped in active form. cAMP<br />
regulates secretion of fluid into the intestinum => enormous loss of liquid and electrolytes => death!<br />
Pertussis-toxin: causes ADP-ribosylation of G iα , release of GDP inhibited => G iα locked in its INactive form => can not<br />
inhibit AC!
BIMM118<br />
Targets of cAMP:<br />
Protein Kinase A (PKA):<br />
– Consists of four subunits: two regulatory<br />
and two catalytic subunits => after cAMP<br />
binding to the regulatory subunits the<br />
catalytic subunits dissociate and<br />
translocate to the target substrates.<br />
Cyclic Nucleotides<br />
– First identified process regulated by PKA<br />
was glycogenolysis (PKA phosphorylates<br />
glycogen phosphorylase kinase which in<br />
turn activates glycogen phosphorylase.<br />
PKA also phosphorylates and inactivates<br />
glycogen synthase => release of glucose)
BIMM118<br />
Cyclic Nucleotides<br />
– PKA also phosphorylates transcription factors: CREB<br />
• CRE (cAMP response element) in the promoter of cAMP responsive genes<br />
• CREB becomes phosphorylated by PKA that translocated to the nucleus
BIMM118<br />
Cyclic Nucleotides<br />
• Guanylate Cyclase:<br />
– Yields cyclic GMP<br />
– Second messenger in only a few cell types (intestinal mucosa, vascular smooth<br />
muscle)<br />
– cGMP stimulates cGMP-dependent protein kinases<br />
– Action terminated by hydrolysis of cGMP and dephosphorylation of protein kinase<br />
substrates<br />
– Nitric Oxide activates cytoplasmic guanylyl cyclase:
BIMM118<br />
Phosphodiesterases:<br />
Cyclic Nucleotides<br />
• Attenuate G-protein/AC coupled-receptor derived signals by converting cAMP to 5’AMP,<br />
or cGMP to 5’GMP<br />
• several families; activation creates feed-back loops<br />
• Phosphodiesterase inhibitors:<br />
Methylxanthines:<br />
Caffeine, theophylline =><br />
enhance and prolong the signals<br />
originating from adrenergic receptors<br />
Sildenafil (Viagra®):<br />
Specific PDE V inhibitor
BIMM118<br />
Regulation of Receptors<br />
• Receptors not only initiate regulation of physiological and<br />
biochemical function but are themselves subject to many regulatory<br />
and homeostatic controls.<br />
• Controls include regulation of synthesis and degradation of the<br />
receptor by multiple mechanisms; covalent modification,<br />
association with other regulatory proteins, and/or relocalization<br />
within the cell.<br />
• Modulating inputs may come from other receptors, directly or<br />
indirectly.<br />
• Receptors are always subject to feedback regulation by their own<br />
signaling outputs.
BIMM118<br />
Regulation of Receptors<br />
• Heterologous desensitization:<br />
– Four residues in the cytosolic domain of the β-adrenergic receptor<br />
can be phosphorylated by PKA<br />
– Activity of all Gs protein – coupled receptors, not just the βadrenergic<br />
receptor, is reduced<br />
• Homologous desensitization:<br />
– Other residues in the cytosolic domain of the β-adrenergic<br />
receptor are phosphorylated by the receptor-specific β-adrenergic<br />
receptor kinase (BARK)<br />
– BARK only phosphorylates the β-adrenergic receptor which<br />
facilitates β-arrestin binding to the phosphorylated receptor
BIMM118<br />
Receptor Desensitization
BIMM118<br />
Receptor Down-Regulation<br />
• Slower onset (hours to days), more prolonged effect<br />
• Decreased synthesis of receptor proteins<br />
• Increase in receptor internalization and degradation<br />
• Internalization involves endocytosis of receptor: the endocytic vesicle<br />
may ultimately return the receptor to the cell surface, or alternatively<br />
may deliver the receptor to a lysosome for destruction.<br />
• Endocytic vesicles are associated with phosphatases which can clear<br />
phosphate from a receptor and ready it for reuse before returning it to<br />
the plasma membrane.
BIMM118<br />
Nuclear Receptors<br />
• Lipid soluble ligands that penetrate cell membrane (corticosteroids,<br />
mineralocorticoids, sex steroids, Vitamin D, thyroid hormone)<br />
• Receptors contain DNA-binding domains and act as ligand-regulated<br />
transcriptional activators or suppressors(=> characteristic lag period of 30<br />
minutes to several hours):<br />
Ligand binding of the receptors triggers the formation of a dimeric complex that can interact with<br />
specific DNA sequences (=“Response Elements”) to induce transcription. The resulting protein<br />
products possess half-lifes that are significantly longer than those of other signaling<br />
intermediates => Effects of nuclear receptor agonists can persist for hours or days after plasma<br />
concentration is zero.
BIMM118<br />
• Examples:<br />
Nuclear Receptors<br />
– Glucocorticoids: Inhibit transcription of COX-2; induce transcription of Lipocortin<br />
– Mineralcorticoids: Regulate expression of proteins involved in renal function<br />
– Retinoids (Vit A derivatives): Control embryonic development of limbs and<br />
organs; affect epidermal differentiation => dermatological use (Acne)<br />
– PPARs (Peroxisome Proliferation-Activated Receptors): control metabolic<br />
processes:<br />
• PPARα: Target of Fibrates (cholesterol lowering drugs: stimulate βoxidation<br />
of fatty acids)<br />
• PPARγ: Target of Glitazones (anti-diabetic drugs: induce expression of<br />
proteins involved in insulin signaling => improved glucose uptake)
BIMM118<br />
Phospholipids, Phosphoinositols & Eicosanoids
BIMM118<br />
Phospholipids, Phosphoinositols & Eicosanoids<br />
Common types of<br />
Phospholipids:
BIMM118<br />
Phospholipids, Phosphoinositols & Eicosanoids<br />
Second messenger<br />
– released through hydrolysis by phospholipases and/or<br />
– generated through the actions of lipid kinases<br />
Phospholipases: Phosphatidylinositol-kinases:
BIMM118<br />
Phospholipids, Phosphoinositols & Eicosanoids<br />
Phospholipases:<br />
• PLA2:<br />
– Cytoplasmic form (90 kDa) is regulated through nM Ca ++ (Annexins) and<br />
phosphorylation; AA specific => signaling function<br />
– Secreted form (pancreas, 14 kDa) is also Ca ++ dependent (mM range)=><br />
digestive function<br />
• PLC: coupled to a variety of (growth factor) receptors:<br />
– PLCβ is activated through GPCRs (G qα ) => binding enhances its catalytic<br />
activity and in return the GTPase activity of G qα (similar to GAP function in ras<br />
signaling)<br />
– PLCγ couples with its SH2 domains directly to growth factor receptors (EGFR,<br />
PDGFR) or the TCR, where it is activated through tyrosine phosphorylation
BIMM118<br />
Phospholipids, Phosphoinositols & Eicosanoids<br />
Both phospholipases yield finally arachidonic acid (see below), in addition, PLC activity also produces<br />
DAG and IP 3 :<br />
• DAG: remains membrane bound; diacylglycerol kinase phosphorylates DAG to generate<br />
phosphatidic acid which functions as a substrate for PLA 2 .<br />
Phosphatidyl-serine (PS), Ca ++ and DAG activate PKC on the plasma membrane<br />
• IP 3 : see Ca ++ signaling!!<br />
– Glucocorticoids: inhibit PLA2 by transcriptionally inducing Lipocortin, a protein<br />
which binds to PLA2 and blocks its activity.<br />
– Phorbol esters: strongest known tumor promotors; mimic DAG => bind PKC and<br />
activate it. Also potent activator of Ca 2+ influx, MAPK pathway etc.
BIMM118<br />
Phospholipids, Phosphoinositols & Eicosanoids<br />
Lipid kinases:<br />
• PI 3 -kinase:<br />
– binds to and becomes tyrosine phosphorylated in response to activation of<br />
growth factor receptors or immune receptors<br />
– 85 kDa regulatory subunit (pY) and a 110 kDa catalytic subunit<br />
– regulatory subunit contains SH2 and SH3 domains<br />
– PIP 3 -phosphates can bind to the pleckstrin homology (PH) domain of Akt<br />
=> Akt activation => phosphorylation of BAD, which dissociates from the<br />
antiapoptotic protein bcl-2 => inhibition of apoptosis<br />
• Wortmannin: fungal metabolite, potent, irreversible inhibitor of PI3Kinase<br />
• Ly290004: synthetic compound, blocks ATP binding site of PI3Kinase
BIMM118<br />
• Eicosanoids:<br />
Arachidonic Acid Metabolism<br />
collective name for derivatives of arachidonic acid (=5,8,11,14 - eicosatetraenic acid)<br />
– AA is mainly generated through the action of PLA 2 and DAG-lipase.<br />
– Rapidly metabolized by cyclooxygenase and lipoxygenase into<br />
prostaglandins and leukotrienes:
BIMM118<br />
• Prostaglandins:<br />
Arachidonic Acid Metabolism<br />
– First observed in seminal fluid => name<br />
– Structure of cyclopentane ring defines letter<br />
– Double bonds in side chains account for number<br />
– Greek letter refers to the spatial position of the OH-group at C-9<br />
Initial step in PG synthesis<br />
catalyzed by PGH-synthase<br />
which has dual enzymatic<br />
activity:<br />
cyclooxygenase (closes ring<br />
=>PGG2)<br />
and<br />
peroxidase (=> 15-OH)
BIMM118<br />
Arachidonic Acid Metabolism<br />
Biological functions of PGs:<br />
• Vascular tone Relaxation: PGs E 1 , E 2 , F 2α and I 2<br />
Constriction: PGs F 2α , TxA 2<br />
• Platelet aggregation Increase: PGs E 1 , TxA 2<br />
Decrease: PGs E 2 , I 2<br />
• Uterus tone Increase: PGs E 1 , E 2 , F 1α<br />
• Bronchial muscle Constriction: PGFs<br />
Relaxation: PGEs<br />
• Gastric secretion Inhibition: PGs E 1 , E 2 , I 2<br />
• Temperature and pain Increase: PGEs
BIMM118<br />
• Leukotrienes:<br />
Arachidonic Acid Metabolism<br />
– First found in leucocytes; contain 3 conjugated double bonds<br />
– Lipoxygenase generates Hydroperoxyeicosatetraenoic acid (HPETE)<br />
– LTC 4 , D 4 and E 4 mediate allergic reaction: Slow Reacting Substance of Anaphylaxis (SRS-A)<br />
=> mediates anaphylactic shock 10,000 fold more potent than histamine!!! => constricts<br />
bronchi, dilate blood vessels<br />
– LTB 4 is a very strong chemoattractant for macrophages
BIMM118<br />
Growth Factor Receptors<br />
• Many growth factors (EGF, PDGF, IGF-1, CSF-1, ...) signal through receptors with intrinsic<br />
tyrosine kinase activity<br />
• Common features:<br />
– Large, glycosylated ligand binding domain<br />
– Single hydrophobic transmembrane domain<br />
– Activation occurs through ligand mediated oligomerization<br />
– Undergo ligand induced downregulation by internalization<br />
– Cytoplasmic tyrosine kinase domain:<br />
• most highly conserved region<br />
• GlyXGlyXXGlyX(15-20)Lys<br />
Lys is critical for ATP binding - mutation renders receptor kinase inactive, which<br />
abrogates all cellular responses => signaling depends on tyrosine phosphorylation<br />
of receptor and cytoplasmic substrates<br />
• Tyrosine kinase receptors also bind and activate cytoplasmic tyrosine kinases<br />
– Autophosphorylation sites:<br />
• conserved in the C-term of each receptor class<br />
• autophosphorylation does not effect K m of receptor kinase activity<br />
• provide docking sites for SH2 domain containg signaling proteins
BIMM118<br />
Growth Factor Receptors<br />
• Three subclasses:<br />
– Class I: two Cys-rich region in the EC, monomeric ligand<br />
EGF-R, erbB2, erbB3, erbB4 (heregulin receptors)<br />
– Class II: heterotetrameric: 2 α and 2 β chains stabilized through S-S bonds: monomeric ligand<br />
Insulin-R, IGF-1-R<br />
– Class III: Repeats of mmunoglobulin-like structure, dimeric ligand<br />
FGF-R, NGF-R, PDGF-R, CSF-1-R, c-kit
BIMM118<br />
Signaling through Adapter proteins:<br />
Growth Factor Receptors<br />
• grb2: adapter with one SH2 domain which binds PY<br />
residue on RTK, and two SH3 domains which bind to<br />
• Sos: “Son of Sevenless” (mutation in drosophila<br />
prevents development of the R7 photoreceptor cell).<br />
Functions as a GEF to facilitate GTP loading of<br />
• ras: GTP binding protein, farnesylated; protooncogene,<br />
provides a docking site on the plasma membrane for raf.<br />
• ras-GAP: negative regulator of groth factor signaling:<br />
promotes GTP hydrolysis through the GTPase activity of<br />
ras.
BIMM118<br />
Signaling through Adapter proteins:<br />
Growth Factor Receptors<br />
• raf: ser/thr kinase of the MAPKKK/MEKK family (MEKK<br />
does normally NOT phosphorylate MEK, but rather<br />
MKK4/7 => Stress pathway); requires context of plasma<br />
membrane for activation (mixing GTP-ras and raf in a<br />
test tube fails to activate raf) => raf likely to be<br />
phosphorylated at the plasma membrane. Activated raf<br />
phosphorylates...<br />
• MEK: Dual specificity kinase (in case of Stress pathway:<br />
SEK) phosphorylates ERKs or MAPKs on tyr and thr -><br />
• ERKs: migrate to the nucleus where they phosphorylate<br />
transcription factors such as fos and jun; also feedback<br />
loop to other signaling molecules
BIMM118<br />
Growth Factor Receptors
BIMM118<br />
• “Classical” hormones:<br />
Cytokine Receptors<br />
– produced by cells organized into endocrine organs,<br />
– often referred to as “endocrine signal molecules”<br />
– target cells usually distant from the site of synthesis<br />
– hormone carried by blood stream from producing gland to target cells<br />
– signal through receptors coupled to G-proteins (e.g. epinephrine receptor), ion-channels<br />
– (e.g. acetylcholine receptor) or receptors with intrinsic enzymatic activity<br />
• Cytokines:<br />
– single producing and effector cell<br />
– only affect target cells in close proximity (autocrine or paracrine)<br />
– almost exclusively involved in regulating immunological processes<br />
– sometimes subdivided into different groups based on their origin (lymphokines, monokines,<br />
interleukines)<br />
– often carry several (old) names based on their multiple biological functions: e.g. Lymphocyte<br />
Activating Factor (LAF) = Mitogenic Protein (MP) = T Cell Replacing Factor III (TRF-III) = B<br />
Cell Activating Factor (BAF) = B cell Differentiation Factor (BDF) = INTERLEUKIN 1
BIMM118<br />
Cytokine Receptors<br />
• Basic characteristics:<br />
– only one copy of encoding gene per haploid cell (~20 different IFNα’s, but each<br />
encoded by a distinct gene)<br />
– genes segmented into 4 or 5 exons (exceptions are IFNα and IFNβ: no introns)<br />
– mature protein usually between 8 and 25 kDa<br />
– barely any structural resemblances<br />
– often N-glycosylated<br />
– often form oligomers<br />
– some carry signal sequence in precursor<br />
– expression is tightly regulated on a transcriptional level<br />
– generally pleiotropic<br />
– usually highly species specific (up and down)<br />
• Multiple (old) classifications:<br />
– Based on origin (Lymphokines, Monokines..)<br />
– Based on action (inhibitory, stimulating, antiviral, chemotactic...)<br />
– Based on composition of receptor (single-chain vs. multi-chain)
BIMM118<br />
Cytokine Receptors<br />
• Current nomenclature based on structure of receptors:<br />
– Type I cytokine receptors = hematopoietin receptor family:<br />
receptors contain W-S-X-W-S motif in the C-terminus<br />
• IL-2 R, IL-3 R, IL-4 R, IL-5 R, IL-6 R (has also Ig-like domain), IL-7 R, IL-9 R, IL-11 R<br />
IL-13 R, IL-15 R, GM-CSF R, EPO R, G-CSF R (has also Ig-like domain)<br />
– Type II cytokine receptors = Interferon receptor family:<br />
receptors contain IRH1 (200aa extracellular) and IRH2 (50 aa cytoplasmic) domain<br />
• IFNα/β R, IFNγ R<br />
– Type III cytokine receptors = TNF receptor family:<br />
receptors contain 4 Cys rich regions in extracellular domain<br />
• TNFα R, TNFβ=LT R, NGF R (trk), fas, CD40<br />
– Type IV cytokine receptors = Immunoglobulin family:<br />
receptors contain an Ig like repeat in the extracellular domain<br />
• IL-1 R, M-CSF R (c-fms), SCF R = steel factor R (kit) (tyrosine kinase activity), (IL-6 R) (has<br />
also W-S-X-W-S motif), (G-CSF R)<br />
– (Chemokine receptors):<br />
• C-X-C subgroup (α-family): IL-8, PF4, βTG<br />
• C-C subgroup (β-family): RANTES, MCAF, MIP-1β
BIMM118<br />
Signal Transduction:<br />
Cytokine Receptors<br />
Receptors lack intrinsic catalytic activity but associate w/ cytosolic enzymes<br />
STAT: Signal transducer and activator of transcription<br />
– contain SH2 domains<br />
– become tyrosine phosphorylated after stimulation<br />
– 6 family members<br />
– homo or heterodimerize<br />
– translocate to nucleus and bind enhancers<br />
JAK: Janus kinase<br />
– large cytoplasmic tyrosine kinases (130-140 kDa)<br />
– NO SH2 or SH3 domains<br />
– kinase-like domain
BIMM118<br />
Ser/Thr-kinase Receptors<br />
Transforming Growth Factors = TGFs:<br />
– Murine sarcoma virus infected cells can not bind EGF => cells produce a growth factor that<br />
competes for EGF binding (=sarcoma growth factor, SGF).<br />
– SGF promoted anchorage independent growth (reversible) => first evidence that transformed<br />
cells produce their own growth factor!<br />
– SGF was found to consist of two subunits:<br />
TGFα: EGF competitor, binds and signals through the EGF receptor,<br />
potent mitogen, but does not support anchorage-independent growth<br />
overexpressed in epithelium of psoriasis patients (=> hyperproliferation of keratinocytes)<br />
– TGFβ: acts through distinct receptor, it also is a potent mitogen, but it also does not support<br />
anchorage-independent growth (only combination does!)<br />
TGFβ- receptors I and II:<br />
– external ligand binding domain and cytosolic serine/threonine kinase activity.<br />
– betaglycan: proteoglycan required for TGFβ binding
BIMM118<br />
Signal Transduction:<br />
SMADs:<br />
Ser/Thr-kinase Receptors<br />
– 8 members - conserved MH1 and MH2 domain<br />
– rapidly phosphorylated in response to TGFβ (2,3) or<br />
BMP (1,5,8)<br />
– Smads function in heteromeric complexes<br />
– “common” Smad = Smad-4 (Smad-4 required for all<br />
Smad signaling)<br />
– translocate to the nucleus<br />
– phosphorylated by the receptor itself<br />
– phosphorylation motif: SSXS<br />
– Smad1 potentially also activated by MAPK<br />
– Mutations of Smads and /or TGFβR are found in 90%<br />
of colon cancers
BIMM118<br />
NFκB<br />
– originally identified as a transcription factor binding an<br />
enhancer (κB)in the κ-light chain immunoglobulin gene<br />
– Activated by a variety of (proinflammatory) signals<br />
(IL-1, TNF, Phorbol esters...)<br />
– Homo-or heterodimer composed of p50 and/or p65<br />
subunits<br />
– retained in its inactive form in the cytoplasm by the<br />
inhibitory protein IκB<br />
– dissociation of NFκB from IκB activates NFκB’s DNA<br />
binding capabilities<br />
– NFκB/ IκB association is regulated by serine<br />
phosphorylation of IκB!<br />
– Phosphorylated IκB does not dissociate from NFκB,<br />
rather is marked for degradation (NFκB activation can<br />
be inhibited by protease inhibitors!)<br />
– Phosphorylation of IκB through IκB-kinase (complex<br />
>600 kDa)<br />
– IKK: two kinase subunits: IKKα and IKKβ, homo- or<br />
heterodimers IKKγ (NEMO): no kinase activity,<br />
required for complex assembly = regulatory subunit
BIMM118<br />
Autonomic Nervous System
BIMM118<br />
Autonomic Nervous System
BIMM118<br />
• Ganglia close to the<br />
innervated organs<br />
• Myelinated axons<br />
• Note:<br />
Somatic nervous<br />
system has no<br />
ganglia!<br />
Autonomic Nervous System<br />
• Ganglia close to the<br />
spinal column<br />
• Preganglionic axons<br />
are myelinated;<br />
postganglionic axons<br />
are unmyelinated
BIMM118<br />
Transmitters:<br />
• Acetylcholine:<br />
Autonomic Nervous System<br />
– ALL preganglionic neurons<br />
– ALL parasympathetic postganglionic neurons<br />
• Norepinephrine (= Noradrenalin):<br />
– MOST sympathetic postganglionic neurons<br />
– Exceptions: Sweat glands (Acetylcholine);<br />
Renal arteries (Dopamine)<br />
• Epinephrine (= Adrenalin):<br />
– Adrenal medulla upon sympathetic impulses<br />
(no ganglion!)
BIMM118<br />
Receptors:<br />
• Cholinergic Receptors:<br />
Autonomic Nervous System<br />
– Muscarinic (M): at the target organ<br />
named after activation by Muscarine<br />
(poison of Amanita muscaria)<br />
– Nicotinic (N):<br />
ganglia, motor endplate, medulla<br />
named after activation by Nicotine<br />
• Adrenergic Receptors:<br />
– α, β − receptors
BIMM118<br />
Cholinergic receptors:<br />
• Muscarinic receptors:<br />
Hetrotrimeric G protein-coupled<br />
– CNS, gastric mucosa: M1<br />
– Cardiac: M2<br />
– Glandular/Smooth muscle: M3<br />
• Nicotinic receptors:<br />
Ion channel-coupled<br />
– Muscle type (motor endplate)<br />
– Ganglion type<br />
– CNS type<br />
Cholinergic System<br />
Acetylcholine is rapidly hydrolyzed by a membrane-associated<br />
Acetylcholinesterase in the synaptic cleft
BIMM118<br />
Cholinergic System - Agonists<br />
= Cholinomimetics = Parasympathomimetics<br />
Two main classes:<br />
• Direct Parasympathomimetics:<br />
– Have affinity for M (and/or N receptors) => mimic AcCholine<br />
– Act mostly on the M type receptors (not subtype selective)<br />
Exception: Nicotine, (Muscle N type only: Tubocurarine,<br />
Succinylcholine)<br />
• Indirect Parasympathomimetics :<br />
– Inhibit the activity of Acetylcholinesterase => [AcCholine] increased
BIMM118<br />
Cholinergic System - Agonists<br />
Muscarinic Parasympathomimetics<br />
The extremely short half-life of AcCholine<br />
makes it therapeutically useless =><br />
• Carbachol:<br />
– Not hydrolyzed by AcCholinesterase<br />
– Also activates N receptors<br />
• Bethanechol:<br />
– Not hydrolyzed by AcCholinesterase<br />
– Does not activate N receptors<br />
– Lacks cardiovascular effects<br />
– Treatment of urinary retention<br />
Bethanechol
BIMM118<br />
Cholinergic System - Agonists<br />
Muscarinic<br />
Parasympathomimetics<br />
Pilocarpine:<br />
– Chief alkaloid in Pilocarpus jaborandi<br />
– Does not activate N receptors<br />
– Used to treat glaucoma<br />
Ciliary muscle contraction=>increased outflow<br />
of aqueous humor => reduction in intraocular<br />
pressure<br />
• Muscarine:<br />
– Chief alkaloid in Amanita muscaria<br />
– No therapeutic application
BIMM118<br />
Cholinergic System - Agonists<br />
Acetylcholinesterase Inhibitors<br />
=> Extend half-life of AcCholine => trigger activation of both M and N receptors
BIMM118<br />
Cholinergic System - Agonists<br />
Acetylcholinesterase Inhibitors<br />
Reversible Inhibitors:<br />
Used to treat Glaucoma (topical) and<br />
Myasthenia Gravis (systemic)<br />
• Carbamates:<br />
– Physostigmine (only topical)<br />
from Physostigma venenosum<br />
(= Calabar bean; West Africa)<br />
– Neostigmine<br />
• Quarternary alcohols:<br />
– Edrophonium<br />
Used to diagnose Myasthenia Gravis<br />
(very short half-life)
BIMM118<br />
Cholinergic System - Agonists<br />
Acetylcholinesterase Inhibitors<br />
• “Horny goat weed”<br />
– Epimedium sagittatum<br />
– Acts as AcCh-esterase inhibitor (active ingredient unknown)<br />
– Indirect stimulation of vascular M3 receptors triggers NO production => vasodilation<br />
(action similar to Sildenafil (Viagra®), which potentiates NO effects)
BIMM118<br />
Cholinergic System - Agonists<br />
Acetylcholinesterase Inhibitors<br />
Irreversible Inhibitors:<br />
No medical application!<br />
• Organophosphates:<br />
– Insecticides<br />
• Malathion<br />
• Parathion<br />
– Nerve gases<br />
• Sarin<br />
• Tabun<br />
• Soman
BIMM118<br />
Cholinergic System - Antagonists<br />
= Cholinolytics = Parasympatholytics<br />
• Muscarinic receptor blockers:<br />
– Competitive antagonists<br />
– Widespread medical applications:<br />
• Inhibition of bronchial and gastric secretion<br />
• Relaxation of smooth muscles (Bronchii, pupillary sphincter…)<br />
• Cardioacceleration<br />
• CNS-altering effects<br />
• Nicotinic receptor blockers:<br />
– Ganglion-specific blockers: no clinical applications<br />
– Neuromuscular blockers: Muscle relaxants
BIMM118<br />
Cholinergic System - Antagonists<br />
Muscarinic Parasympatholytics<br />
Atropine<br />
Chief alkaloid in Atropa belladonna: CNS-stimulant (leaves were used as “asthma cigarettes”)<br />
Hyoscine (=Scopolamine)<br />
Chief alkaloid in Datura stramonium: CNS-depressant => antiemetic (motion sickness)
BIMM118<br />
Cholinergic System - Antagonists<br />
Muscarinic Parasympatholytics<br />
Clinical applications:<br />
• Atropine:<br />
– before anesthesia: prevent hypersecretion of bronchial mucus<br />
– Bradycardy<br />
– Acetylcholinesterase-inhibitor and mushroom poisoning<br />
– Ophtalmology (eye exams)<br />
• Scopolamine:<br />
– Motion sickness (as patches)<br />
• Ipratropium:<br />
– Inhalation for asthma and bronchitis<br />
• Pirenzepine:<br />
– Peptic ulcers: selectively inhibits M1 receptors (gastric mucosa) =><br />
reduced gastric acid production<br />
• N-Butyl-scopolamine:<br />
– Spasmolytic (intestinal or menstrual cramps)
BIMM118<br />
Cholinergic System - Antagonists<br />
Nicotinic Parasympatholytics<br />
Two classes (both act as neuromuscular blockers => muscle relaxants):<br />
• Competitive antagonists = Nondepolarizing blockers<br />
– Act by competing with AcCh for binding to the N receptors<br />
– Prevent depolarization of the endplate<br />
– Action can be reversed by increasing AcCh concentrations (e.g. via AcCh-esterase inhibitors)<br />
• Agonists = Depolarizing blockers<br />
– AcCh mimetics that are not hydrolyzed by AcCh-esterase (but hydrolyzed by plasma esterases)<br />
– Act by triggering a sustained depolarization of the neuromuscular endplate<br />
– No new action potential can be generated<br />
– Can NOT be reversed increasing AcCh concentrations (would cause further depolarization)
BIMM118<br />
Cholinergic System - Antagonists<br />
Nicotinic Parasympatholytics<br />
Nondepolarizing blockers<br />
• Curare:<br />
– Plant derived arrow poison in S-America<br />
– Active ingredient is d-Tubocurarine<br />
– Death occurs through respiratory paralysis<br />
– Tubocurarine is not absorbed orally => no risk eating the prey<br />
– Tubocurarine was used clinically as muscle relaxant during surgery<br />
but: Tubocurarine triggers histamine release => blood pressure drops
BIMM118<br />
Cholinergic System - Antagonists<br />
Nicotinic Parasympatholytics<br />
Nondepolarizing blockers<br />
Synthetic quarternary ammonium compounds<br />
– Replaced tubocurarine as muscle relaxants<br />
– No or little histamine release<br />
• Pancuronium long-lasting action (1-2h)<br />
Used in lethal injection (together with barbiturate + KCl)<br />
• Vecuronium intermediate-lasting action (
BIMM118<br />
Cholinergic System - Antagonists<br />
Nicotinic Parasympatholytics<br />
Depolarizing blockers<br />
• Succinylcholine = Suxamethonium<br />
– “dimeric” Acetylcholine<br />
– Acts agonistic like AcCh<br />
– NOT hydrolyzed by AcCh-esterase (only by plasmaesterases)<br />
– Initial depolarization triggers muscle twitching<br />
– Followed by persistant depolarization (~10min)<br />
– Used for brief procedures (e.g. intubation; shock therapy)
BIMM118<br />
Cholinergic System<br />
Parasympathetic Drugs - Summary
BIMM118<br />
Autonomic Nervous System
BIMM118<br />
• Ganglia close to the<br />
innervated organs<br />
• Myelinated axons<br />
• Note:<br />
Somatic nervous<br />
system has no<br />
ganglia!<br />
Autonomic Nervous System<br />
• Ganglia close to the<br />
spinal column<br />
• Preganglionic axons<br />
are myelinated;<br />
postganglionic axons<br />
are unmyelinated
BIMM118<br />
Transmitters:<br />
• Acetylcholine:<br />
Autonomic Nervous System<br />
– ALL preganglionic neurons<br />
– ALL parasympathetic postganglionic neurons<br />
• Norepinephrine (= Noradrenalin):<br />
– MOST sympathetic postganglionic neurons<br />
– Exceptions: Sweat glands (Acetylcholine);<br />
Renal arteries (Dopamine)<br />
• Epinephrine (= Adrenalin):<br />
– Adrenal medulla upon sympathetic impulses<br />
(no ganglion!)
BIMM118<br />
Adrenergic System<br />
Termination of (nor)epinephrine action:<br />
• Reuptake into presynaptic nerve ending<br />
– Predominant mechanism<br />
– active transport; inhibited by Cocaine<br />
• Catechol-O-methyltransferase (COMT)<br />
– In the cytoplasm of post-junctional cells<br />
• Monoamino-oxidase (MAO)<br />
– In mitochondria of nerve and post-junctional cells<br />
• Presynaptic α2-receptors<br />
– Negative feedback that inhibits norepinephrine<br />
release
BIMM118<br />
Adrenergic receptors:<br />
• alpha 1<br />
– most vascular smooth muscles<br />
– Activate PLCβ => Ca ++ => Contraction<br />
• alpha 2<br />
– mostly presynaptic<br />
– Inhibit adenylate cyclase (Gα i )<br />
• beta 1<br />
– mostly heart<br />
– Activate adenylate cyclase<br />
• beta 2<br />
– respiratory and uterine smooth muscle<br />
– Activate adenylate cyclase<br />
• beta 3<br />
– mostly adipocytes<br />
– Activate adenylate cyclase => lipolysis<br />
• (Dopamine)<br />
Adrenergic System
BIMM118<br />
Sympathomimetics<br />
Adrenergic System - Agonists<br />
Indirect Sympathicomimetics:<br />
MAO - Inhibitors:<br />
– Inhibition of MAO causes increase in free Norepinephrine<br />
– In the CNS, MAO also metabolizes dopamine and serotonin => MAO inhibitors trigger<br />
increase in these “happy hormones” => uses as antidepressants<br />
– Irreversible inhibition of MAO => long-lasting effect (weeks!)<br />
• Tranylcypromine<br />
• Moclobemide<br />
Possibility of severe adverse interactions of MAO inhibitors with numerous other drugs<br />
=> fatal hypertension
BIMM118<br />
Sympathomimetics<br />
Adrenergic System - Agonists<br />
Indirect Sympathicomimetics :<br />
• Ephedrine<br />
– Chief alkaloid in Ephedra, no clinical use<br />
– Displace norepinephrine in storage vesicle => forced norepinephrine release<br />
– Found in many dietary supplements: “Energy-Boosters”, Diet pills (Metabolife®) etc.<br />
– Ingredient in many herbal preperations: Ephedra, Ma Huang<br />
Epinephrine Ephedrine<br />
The FDA has received more than 800 reports of adverse effects associated with use of products<br />
containing ephedrine alkaloid since 1994. These serious adverse effects, include hypertension (elevated<br />
blood pressure), palpitations (rapid heart rate), neurophathy (nerve damage), myopathy (muscle injury),<br />
psychosis, stroke, memory loss, heart rate irregularities, insomnia, nervousness, tremors, seizures, heart<br />
attacks, and death.<br />
In Feb ‘04, the agency has banned the marketing of dietary supplements containing<br />
ephedrine alkaloids (ban challenged by court order in April ‘05).
BIMM118<br />
Sympathomimetics<br />
Indirect Sympathicomimetics :<br />
Amphetamines<br />
Adrenergic System - Agonists<br />
– Displace norepinephrine in storage vesicle => forced epinephrine release<br />
– Also inhibit norepinephrine re-uptake and degradation by MAO (“triple action”)<br />
• Methylphenidate (Ritalin®)<br />
– Treatment of ADD<br />
• Fenfluramine<br />
– Appetite suppressant (now banned in US)<br />
(combined with Phentermine = “FenPhen”)<br />
• Metamphetamine/MDMA<br />
– Effectiveness disappears due to catecholamine depletion<br />
of vesicles => post-use depression<br />
=> urge for re-administration!<br />
Ephedrine
BIMM118<br />
Sympathomimetics<br />
Non-selective agonists:<br />
• Epinephrine (Adrenaline)<br />
Adrenergic System - Agonists<br />
– Activates both α and β receptors;<br />
– Blood pressure increase, but effect on systolic pressure dominant<br />
– Dilates bronchii<br />
– Potent vasopressor => Clinical uses limited<br />
– Used for:<br />
symptomatic treatment of anaphylactic shock (Epi-Pen®)<br />
adjuvant in local anesthetics (increases duration, reduces bleeding)<br />
• Norepinephrine (Noradrenaline)<br />
– Activates mostly α receptors => systolic and diastolic blood pressure increase<br />
– Very potent vasopressor => Clinical uses limited to severe shock treatment
BIMM118<br />
Sympathomimetics<br />
α 1 - selective agonists<br />
Clinical applications:<br />
• Methoxamine<br />
Adrenergic System - Agonists<br />
– Treatment of hypotensive state<br />
• Phenylephrine<br />
– (Local) vasoconstrictor<br />
nasal decongestant<br />
Epinephrine Phenylephrine
BIMM118<br />
Sympathomimetics<br />
α 1 - selective agonists (cont’d)<br />
Clinical applications:<br />
Adrenergic System - Agonists<br />
Nasal decongestants (mostly OTC):<br />
• Naphazoline (Privine®, Rhinon®)<br />
• Oxymetazoline (Afrin®, etc.)<br />
• Xylometazoline (Privin®)<br />
Should be used less than 10 days, otherwise reactive hyperemia (“rhinitis medicamentosa”) develops!<br />
Continued used can result in local hypoxia => atrophic damage of the nasal mucosa
BIMM118<br />
Sympathomimetics<br />
α 2 - selective agonists<br />
Adrenergic System - Agonists<br />
Phenotypically produce sympatholytic effects!<br />
Activate presynaptic α 2 receptors in the cardiovascular control center in the CNS<br />
=> reduced sympathetic nervous system activity => blood pressure decrease<br />
Clinical applications:<br />
Hypertension<br />
• Clonidine<br />
• Guanfacine
BIMM118<br />
β 1 - receptors<br />
• Mostly in heart<br />
Adrenergic System - Agonists<br />
• Increase contractility = “positive inotrope”<br />
• Increase heart rate = “positive chronotrope”<br />
β 2 - receptors<br />
• Respiratory system – located in bronchial smooth muscle<br />
• Produce bronchial dilation
BIMM118<br />
Sympathomimetics<br />
β 1 - selective agonists<br />
Clinical applications:<br />
• Dobutamine<br />
Adrenergic System - Agonists<br />
– Strong inotropic effect with little chronotropic effect =><br />
increase in cardiac output without significant increase in heart rate<br />
– Short-term treatment of impaired cardiac function after cardiac surgery, MI etc.<br />
– Also used in “Dobutamine Stress Test” = Heart sonogram: Dobutamine mimics exercise<br />
Epinephrine Dobutamine
BIMM118<br />
Sympathomimetics<br />
β 2 - selective agonists<br />
Clinical applications:<br />
Asthma:<br />
Adrenergic System - Agonists<br />
• Non-selective sympathomimetics => strong cardiac side effects<br />
• β 2 - selective agonists target predominantly the respiratory system<br />
• Drugs differ in speed of onset and in duration of action => acute vs. long-term treatment<br />
• Additionally, preferential activation of pulmonary receptors due to application as aerosols<br />
• Metaproterenol (Alupent®)<br />
• Albuterol = Salbutamol (Ventolin®)<br />
• Formoterol (Foradil®)<br />
• Etc…
BIMM118<br />
Sympatholytics<br />
α - selective antagonists<br />
Adrenergic System - Antagonists<br />
Promote vasodilation => decreased peripheral resistance => blood pressure <br />
(Side effects: reflex tachycardia and postural hypotension)<br />
Relaxation of the smooth muscles in the bladder neck<br />
Clinical applications:<br />
Hypertension; Urinary retention<br />
Non-selective α-antagonist:<br />
• Phentolamine (for pheochromocytoma)<br />
• Ergot alkaloids see 5HT receptor<br />
α 1 -selective antagonists:<br />
• Prazosin (Minipress®)<br />
first α 1 - selective antagonist<br />
• Terazosin longer half-life<br />
• Doxazosin longer half-life
BIMM118<br />
Sympatholytics<br />
α 2 - selective antagonists<br />
• Yohimbine<br />
Adrenergic System - Antagonists<br />
– Chief active compound in Pausinystalia yohimbine (bark)<br />
– Effects opposite of Clonidine<br />
– Enters CNS => increased sympathetic output => increased heart rate, blood<br />
pressure, can cause severe tremors<br />
– Ingredient in many weight loss products<br />
– Extensive (past) use in treatment of male sexual dysfunction
BIMM118<br />
Sympatholytics<br />
Adrenergic System - Antagonists<br />
β - selective antagonists (”β - blockers”)<br />
β 2 - selective antagonists would trigger bronchial constriction => no clinical use<br />
β 2 - antagonism is mostly an “undesired side effect” of β-selective antagonists<br />
(goal is to antagonize β 1 - receptors)<br />
Non-cardiac effects: CNS - anxiolytic; skeletal muscle - reduction of tremor<br />
Clinical applications:<br />
• Angina pectoris<br />
• Hypertension<br />
• Cardiac dysrhythmias<br />
• MI<br />
• Heart failure<br />
• Familial tremor<br />
• “Stage fright”
BIMM118<br />
Sympatholytics<br />
β - selective antagonists<br />
Adrenergic System - Antagonists<br />
• First-generation β-receptor antagonists blocked β 1 and β 2 -receptors =<br />
noncardioselective (β-receptors in the heart are β 1 - receptors).<br />
• Many β-receptor antagonists posses intrinsic agonist activity<br />
• Basic conserved structure: Norepinephrine side chain linked to aromatic structure by<br />
a methylene-oxygen bridge.<br />
Prototype:<br />
• Propranolol<br />
Epinephrine
BIMM118<br />
Sympatholytics<br />
Adrenergic System - Antagonists<br />
β - selective, noncardioselective antagonists (cont’d):<br />
• Nadolol<br />
• Pindolol<br />
• Timolol<br />
• Labetalol - also antagonistic on α 1 - receptors => potent antihypertonic drug<br />
β 1 - specific “cardioselective” antagonists:<br />
• Metoprolol<br />
• Atenolol<br />
• Esmolol - quick onset / short duration => used in urgent settings
BIMM118<br />
β-Sympatholytics<br />
Epinephrine<br />
Adrenergic System - Antagonists
BIMM118<br />
Cardiovascular Pharmacology<br />
• Hypertension<br />
• Angina pectoris<br />
• Cardiac Arrhythmias<br />
• Heart Failure
BIMM118<br />
Cardiovascular Pharmacology<br />
• Cardiovascular (=Circulatory) system – heart and blood vessels<br />
• Arteries – transport blood to tissues<br />
• Capillaries – sites of exchange, fluid O2, CO2, nutrients etc.<br />
• Venules – collect blood from capillaries<br />
• Veins – transport blood back to heart<br />
• Blood moves within vessels – higher pressure to lower pressure<br />
Resistance to flow depends on vessel diameter, length and<br />
viscosity of blood
BIMM118<br />
Cardiac blood flow<br />
Cardiovascular Pharmacology<br />
• The mammalian heart is a double pump in which the right side<br />
operates as a low-pressure system delivering de-oxygenated blood<br />
to the lungs, while the left side is a high pressure system delivering<br />
oxygenated blood to the rest of the body.<br />
• The walls of the right ventricle are much thinner than those of the<br />
left, because the work load is lower for the right side of the heart.<br />
• The ventricular muscle is relatively stiff, and it would take some time<br />
to fill with venous blood during diastole. The thin, flexible atria serve<br />
to buffer the incoming venous supply, and their initial contraction at<br />
the begining of each cardiac cycle fills the ventricles efficiently in a<br />
short space of time.
BIMM118<br />
Cardiovascular Pharmacology
BIMM118<br />
Cardiovascular Pharmacology<br />
Regulation of cardiac output<br />
~ 5L /minute; dependent on:<br />
• Heart rate<br />
• Stroke volume<br />
• Preload<br />
• Afterload<br />
Starling’s Law<br />
Ventricular contraction is proportional to muscle fiber stretch<br />
Aortic output pressure rises as the venous filling pressure is increased<br />
Increased venous return – increase cardiac output – up to a point!
BIMM118<br />
Cardiovascular Pharmacology<br />
Cardiac electrical activity<br />
• Cardiac muscle does not require any nervous stimulation to contract.<br />
• Each beat is initiated by the spontaneous depolarisation of pacemaker<br />
cells in the sino-atrial (SA) node. These cells trigger the neighbouring atrial<br />
cells by direct electrical contacts and a wave of depolarisation spreads out<br />
over the atria, eventually exciting the atrio-ventricular (AV) node.<br />
• Contraction of the atria precedes that of the ventricles, forcing extra blood<br />
into the ventricles and eliciting the Starling response.<br />
• The electrical signal from the AV node is carried to the ventricles by a<br />
specialised bundle of conducting tissue (the bundle of His)<br />
• The conducting tissues are derived from modified<br />
cardiac muscle cells, the Purkinje fibers.<br />
The conducting bundles divide repeatedly through<br />
the myocardium to coordinate electrical and<br />
contractile activity across the heart.<br />
• Although each cardiac muscle cell is in electrical<br />
contact with most of its neighbours, the message<br />
normally arrives first via the Purkinje system.
BIMM118<br />
Venous return<br />
Cardiovascular Pharmacology<br />
• Systemic filling pressure<br />
• Auxiliary muscle pump<br />
• Resistance to flow between peripheral vessels and right atrium<br />
• Right atrial pressure - elevation<br />
Regulation of Arterial Pressure<br />
• Arterial pressure = cardiac output + peripheral resistance<br />
• Arterial pressure affected by:<br />
– the autonomic nervous system (fast)<br />
– the renin-angiotensin system (hours or days)<br />
– the kidneys (days or weeks)
BIMM118<br />
Potential drug targets:<br />
Antihypertensive Drugs<br />
Hypertension:<br />
• Usually symptom-free<br />
• Consequences: Heart failure, kidney damage,<br />
stroke, blindness …<br />
• CNS, ANS: decrease sympathetic tone<br />
• Heart: decrease cardiac output<br />
• Veins: dilate => decrease preload<br />
• Arterioles: dilate => decrease afterload<br />
• Kidneys: increase diuresis; inhibit RAA system
BIMM118<br />
Antihypertensive Drugs<br />
Four major drug categories<br />
• Sympathetic nervous system suppressors:<br />
– α 1 and β 1 antagonists<br />
– α 2 agonists<br />
• Direct vasodilators:<br />
– Calcium channel antagonists<br />
– Potassium channel agonists<br />
• Renin-angiotensin system targeting drugs:<br />
– ACE inhibitors<br />
– Angiotensin II receptor antagonists<br />
• Diuretics:<br />
– Thiazides<br />
– Loop diuretics<br />
– K + - sparing diuretics
BIMM118<br />
Antihypertensive Drugs:Vasodilators<br />
Calcium channel blockers (= Calcium antagonists):<br />
– Inhibit calcium entry into cells of the arteries<br />
=> decreased afterload<br />
Dihydropyridines:<br />
– Target specifically L-type channels on vascular smooth muscle cells<br />
– No cardiac effects (“Vasoselective Ca ++ antagonists”)<br />
– Can cause peripheral edema<br />
• Nifedipine<br />
– Prototype<br />
• Nicardipine<br />
• Nimodipine<br />
• Nisoldipine<br />
• Amlodipine
BIMM118<br />
Antihypertensive Drugs: Vasodilators<br />
Potassium channel agonists:<br />
• Minoxidil<br />
– Increases outward K + current => membrane hyperpolarization, which<br />
inhibits Ca ++ channel activity<br />
– Used only for severe, treatment-resistant hypertension<br />
– Major side effect: Hirsutism => used topically to treat baldness (Rogaine®)
BIMM118<br />
Antihypertensive Drugs: Vasodilators<br />
• Nitroprusside<br />
– Very unstable (only iv)<br />
– Metabolized by blood vessels into NO<br />
=> activates cGMP production => vasodilation<br />
– Rapid action (30 sec !), short duration (effect ends after 3 min) => blood<br />
pressure “titration”<br />
– Used only to treat hypertensive emergencies
BIMM118<br />
Antihypertensive Drugs: RAAS-targeting drugs<br />
Renin-angiotensin system<br />
• Important role in regulating blood volume, arterial<br />
pressure, and cardiac and vascular function.<br />
• Most important site for renin release is the kidney:<br />
sympathetic stimulation (acting via β1-<br />
adrenoceptors), renal artery hypotension (e.g.<br />
stenosis), and decreased sodium delivery to the<br />
distal tubules stimulate the release of renin by the<br />
kidney.<br />
• Renin acts upon a circulating substrate,<br />
angiotensinogen (produced mainly by the liver)<br />
which undergoes proteolytic cleavage to form the<br />
decapeptide angiotensin I (AT I).<br />
• Vascular endothelium, particularly in the lungs,<br />
contains angiotensin converting enzyme (ACE),<br />
which cleaves off two amino acids to form the<br />
octapeptide, angiotensin II (AT II).
BIMM118<br />
Antihypertensive Drugs: RAAS-targeting drugs<br />
Renin-angiotensin system<br />
Angiotensin II<br />
• Constricts vessels thereby increasing vascular<br />
resistance and arterial pressure<br />
• Stimulates the adrenal cortex to release<br />
aldosterone, which acts upon the kidneys to<br />
increase sodium and fluid retention<br />
• Stimulates the release of vasopressin (antidiuretic<br />
hormone, ADH) from the pituitary which acts upon<br />
the kidneys to increase fluid retention<br />
• Facilitates norepinephrine release and inhibits re-<br />
uptake from nerve endings, thereby enhancing<br />
sympathetic adrenergic function<br />
• Stimulates cardiac and vascular hypertrophy
BIMM118<br />
Antihypertensive Drugs: RAAS-targeting drugs<br />
ACE - Inhibitors<br />
• Captopril<br />
– First ACE inhibitor<br />
– Given po<br />
– Frequent side effect: cough (reduced inactivation of kinins)<br />
• Enalapril<br />
• Benazepril<br />
• Ramipril<br />
• Lisinopril<br />
• Etc…
BIMM118<br />
Antihypertensive Drugs: RAAS-targeting drugs<br />
AT II Receptor Antagonists<br />
Do not interfer with kinin processing => no cough<br />
• Losartan<br />
• Candesartan<br />
• Eprosartan<br />
• Valsartan<br />
• Irbesartan<br />
• Etc…
BIMM118<br />
Angina pectoris<br />
• Medical term for chest pain or discomfort due to coronary heart<br />
disease. Typical angina pectoris (=“tight heart” is uncomfortable<br />
pressure, fullness, squeezing or pain in the center of the chest<br />
• Angina is a symptom of myocardial ischemia, which occurs when the<br />
myocardium does not receive sufficient oxygen.<br />
• People with stable angina have episodes of chest discomfort that are<br />
usually predictable, such as on exertion or under stress (Treatment:<br />
Nitrates, β-blockers).<br />
• In people with unstable angina, the chest pain is unexpected and usually<br />
occurs while at rest. The discomfort may be more severe and prolonged<br />
than typical angina (Treatment: Nitrates).<br />
• Variant angina is also called Prinzmetal's angina. Unlike typical angina, it<br />
nearly always occurs when a person is at rest, and does not follow<br />
physical exertion or emotional stress. Variant angina is due to coronary<br />
artery spasm (Treatment: Ca ++ channel blockers).
BIMM118<br />
• Nitroglycerin<br />
– Organic nitrate<br />
Angina pectoris - Nitrates<br />
– Acts on vascular smooth muscle to promote vasodilation<br />
– Primarily works on veins, only modest dilation of arterioles<br />
– Decreases oxygen demand by decreasing venous return =><br />
use in stable angina<br />
It was originally believed that nitrates and nitrites dilated coronary blood vessels,<br />
thereby increasing blood flow to the heart. It is now believed that atherosclerosis<br />
limits coronary dilation and that the benefits of nitrates and nitrites are due to<br />
dilation of arterioles and veins in the periphery. The resultant reduction in preload,<br />
and to a lesser extent in afterload, decreases the workload of the heart and lowers<br />
myocardial oxygen demand.<br />
– Oral, sublingual, IV, buccal and transdermal administration<br />
– Adverse effects – headache, tachycardia, hypotension<br />
– Never to be combined with other drugs causing<br />
vasodilation (Viagra®) or hypotension
BIMM118<br />
Angina pectoris - Nitrates<br />
• Isosorbide-dinitrate (ISDN)<br />
– More stable than nitroglycerol<br />
– Longer lasting effect<br />
– Tolerance can occur – give lowest dose possible<br />
• Nitroprusside
BIMM118<br />
Arrhythmias:<br />
Cardiac Arrhythmia<br />
Abnormal rhythms of the heart that cause the heart to pump less effectively<br />
Arrhythmia occurs:<br />
– when the heart’s natural pacemaker develops an abnormal rate or rhythm<br />
– when the normal conduction path is interrupted<br />
– when another part of the heart takes over as pacemaker<br />
Types of arrhythmia:<br />
– Tachycardia: unusually fast heartbeat<br />
– Bradycardia: unusually slow heartbeat<br />
– Atrial fibrillation: the atria quiver rather than contract normally because of rapid and irregular<br />
electrical signals in the heart. Beside the abnormal heart beat, there is also a risk that blood<br />
will pool in the atria, possibly causing the formation of blood clots.<br />
– Ventricular fibrillation: life threatening condition in which the heart ceases to beat regularly<br />
and instead “quivers” or fibrillates very rapidly – sometimes at 350 beats per minute or more<br />
(causes 350,000 death/year in the US - “sudden cardiac arrest”)
BIMM118<br />
Arrhythmias:<br />
Drug Classes:<br />
• Class I: Sodium channel blockers<br />
• Class II: β-blockers<br />
Cardiac Arrhythmia<br />
• Class III: Potassium channel blockers<br />
• Class IV: Calcium channel blockers<br />
• Other arrhythmic drugs
BIMM118<br />
Arrhythmias:<br />
Cardiac Arrhythmia<br />
Class I - Sodium channel blockers:<br />
Block Na + entry during depolarization phase<br />
For atrial and ventricular arrhythmias (“all-purpose”)<br />
• Procainamide<br />
• Quinidine<br />
For acute treatment of ventricular arrhythmias<br />
• Lidocaine<br />
For chronic treatment of ventricular arrhythmias<br />
• Flecainide<br />
• Propofenone
BIMM118<br />
Arrhythmias:<br />
Class II - β-blockers:<br />
For tachycardia<br />
• Propranolol<br />
Cardiac Arrhythmia<br />
Class III - Potassium channel blockers:<br />
Prolong repolarization phase by blocking outward potassium flux<br />
For treatment of intractable ventricular arrhythmias<br />
• Bretylium<br />
• Amiodarone<br />
Class IV - Calcium channel blockers:<br />
Prolong repolarization phase by blocking inward calcium current<br />
Predominantly for treatment of atrial arrhythmias<br />
• Verapamil
BIMM118<br />
Arrhythmias:<br />
Other antiarrhythmics:<br />
• Adenosine<br />
Cardiac Arrhythmia<br />
For paroxysmal supraventricular tachycardia<br />
• Digoxin<br />
iv only, extremely short half-life<br />
used to terminate arrhythmias (blocks reentrant pathway)<br />
For atrial fibrillation<br />
• Epinephrine, Isoproterenol<br />
For bradycardia<br />
(Paroxysmal = an arrhythmia that suddenly begins and ends)
BIMM118<br />
Congestive heart failure:<br />
Congestive Heart Failure<br />
• characterised by inadequate contractility, so that the ventricles have<br />
difficulty in expelling sufficient blood => rise in venous blood pressures<br />
• Raised venous pressures impair fluid drainage from the tissues and<br />
produce a variety of serious clinical effects:<br />
– Right sided heart failure causes lower limb oedema. Blood pooling in the lower<br />
extremities is associated with intravascular clotting and thromboembolism<br />
– Left sided heart failure produces pulmonary oedema and respiratory distress<br />
– Causes: Blocked coronary arteries; viral infections; hypertension; MI; leaky heart valves
BIMM118<br />
Congestive Heart Failure<br />
Classification of severity<br />
• I – no limitation of physical activity<br />
• II – slight limitation<br />
• III – marked limitation<br />
• IV – symptoms occur at rest
BIMM118<br />
Congestive Heart Failure<br />
Treatment options:<br />
• Diuretics<br />
– Loop diuretics<br />
– Thiazides<br />
– Spironolactone<br />
• ACE inhibitors & AT II antagonists<br />
• Vasodilators<br />
– Nitrates<br />
• Cardiac Glycosides
BIMM118<br />
Cardiac Glycosides:<br />
Congestive Heart Failure<br />
• Chief active ingredient in several plant families and animals:
BIMM118<br />
Cardiac Glycosides:<br />
• Two main categories:<br />
Congestive Heart Failure<br />
– Cardenolides (Digitalis, Convallaria, Oleandra)<br />
– Bufadienolides (Helleborus, Poison Arrow Frog)
BIMM118<br />
Cardiac Glycosides:<br />
Congestive Heart Failure<br />
• Cardiac glycosides slow the heart rate and increase the force of<br />
contraction<br />
• Extracts of D. purpurea have been used clinically for over 200 years to<br />
treat heart failure and edema (“dropsy”)<br />
• The cardiac glycosides inhibit the Na + /K + -ATPase pump, which causes an<br />
increase in intracellular Na + => slowing of the Na + /Ca ++ -exchanger =><br />
increase in intracellular Ca ++ .<br />
• Low therapeutic index => Associated with an appreciable risk of toxicity<br />
• Digoxin is the most widely used preparation of digitalis (half-life = 1-2<br />
days), although digitoxin (half-life = 7 days) is used in situations where<br />
long half-life may be an advantage.<br />
• Digitalis is the drug of choice for heart failure associated with atrial<br />
fibrillation
BIMM118<br />
Cardiac Glycosides:<br />
Congestive Heart Failure<br />
• Improve cardiac performance (=positive inotrope)<br />
• Increases cardiac output<br />
• Decreased sympathetic tone<br />
• Increase urine output<br />
• Decreased renin release<br />
• Does not prolong life (only symptom relief)<br />
Toxicity:<br />
• Overdose; drug interaction; accidental ingestion of plants (children!)<br />
• Potassium competes with cardiac glycoside for binding to Na + /K + -ATPase<br />
pump => potassium is an “antidot” for cardiac glycoside poisoning<br />
• Injection of anti-cardiac glycoside antibodies
BIMM118<br />
Renal Pharmacology<br />
Diuretics:<br />
• Carbonic Anhydrase Inhibitors<br />
• Thiazides<br />
• Loop Diuretics<br />
• Potassium-sparing Diuretics
BIMM118<br />
Kidneys:<br />
Renal Pharmacology<br />
• Represent 0.5% of total body weight,<br />
but receive ~25% of the total arterial<br />
blood pumped by the heart<br />
• Each contains from one to two million<br />
nephrons:<br />
– The glomerulus<br />
– The proximal convoluted tubule<br />
– The loop of Henle<br />
– The distal convoluted tubule
BIMM118<br />
Functions<br />
Renal Pharmacology<br />
• Clean extracellular fluid and maintain ECF volume<br />
and composition<br />
• Acid-base balance<br />
• Excretion of wastes and toxic substances<br />
• Renal processes<br />
• Filtration - glomerulus<br />
• Reabsorption<br />
• Tubular secretion<br />
In 24 hours the kidneys reclaim:<br />
– ~ 1,300 g of NaCl<br />
– ~ 400 g NaHCO 3<br />
– ~ 180 g glucose<br />
– almost all of the 180 L of water that entered the tubules
BIMM118<br />
Renal Pharmacology<br />
• Blood enters the glomerulus under pressure<br />
• This causes water, small molecules (but not<br />
macromolecules like proteins) and ions to filter<br />
through the capillary walls into the Bowman's capsule<br />
• This fluid is called nephric filtrate<br />
– Not much different from interstitial fluid<br />
• Nephric filtrate collects within the Bowman's capsule<br />
and flows into the proximal tubule:<br />
• Here all of the glucose and amino acids, >90% of the<br />
uric acid, and ~60% of inorganic salts are reabsorbed by active transport<br />
– The active transport of Na + out of the proximal tubule is controlled by angiotensin II.<br />
– The active transport of phosphate (PO 4 ) 3- is regulated (suppressed by) the parathyroid hormone.<br />
• As these solutes are removed from the nephric filtrate, a large volume of the<br />
water follows them by osmosis:<br />
– 80–85% of the 180 liters deposited in the Bowman's capsules in 24 hours<br />
• As the fluid flows into the descending segment of the loop of Henle, water<br />
continues to leave by osmosis because the interstitial fluid is very hypertonic:<br />
– This is caused by the active transport of Na + out of the tubular fluid as it moves up the ascending<br />
segment of the loop of Henle<br />
• In the distal tubules, more sodium is reclaimed by active transport, and still more<br />
water follows by osmosis.
BIMM118<br />
Diuretics:<br />
• Increase output of urine<br />
Renal Pharmacology<br />
• Primary indications are hypertension and mobilization of<br />
edematous fluid (e.g. kidney problems, heart failure,<br />
cirrhosis,…)<br />
Basic mechanism:<br />
• Block reabsorption of sodium and chloride => water will<br />
also stay in the nephron<br />
• Diuretics that work on the earlier nephron have greatest<br />
effect, since they are able to block more sodium and<br />
chloride reabsorption
BIMM118<br />
Diuretics:<br />
Renal Pharmacology<br />
Carbonic anhydrase inhibitors:<br />
• Azetazolamide<br />
– Can trigger metabolic acidosis<br />
– Not in use as diuretic anymore<br />
– Primary indications is glaucoma<br />
(prevents production of aequous humor)<br />
• Dorzolamide<br />
CA-inhibitors are sulfonamides =><br />
cross-allergenic with antibiotics etc.
BIMM118<br />
Diuretics:<br />
Renal Pharmacology<br />
Loop diuretics (= high ceiling diuretics):<br />
– Strong, but brief diuresis (within 1 hr, lasts ~ 4hrs)<br />
– Used for moderate to severe fluid retention and hypertension<br />
– Most potent diuretics available<br />
– Act by inhibiting the Na + /K + /2Cl - symporter in the ascending limb in the loop of Henle<br />
– Major side effects: loss of K + (and Ca ++ and Mg ++ )<br />
• Furosemide<br />
• Bumetanide<br />
• Torasemide
BIMM118<br />
Diuretics:<br />
Thiazide diuretics:<br />
Renal Pharmacology<br />
– Used for mild to moderate hypertension, mild heart failure,<br />
– Medium potency diuretics<br />
– Act by inhibiting the Na + /Cl - symporter in the distal convoluted tube<br />
– Major side effects: loss of K + (and Mg ++ , but not Ca ++ )<br />
• Hydrochlorothiazide<br />
• Benzthiazide<br />
• Cyclothiazide …
BIMM118<br />
Renal Pharmacology<br />
Major side effects of these diuretics:<br />
• Hypokalemia, hyponatremia, hypochloremia<br />
• Hypotension and dehydration<br />
• Interaction with Cardiac Glycosides<br />
=> Potassium can be given orally or IV<br />
or<br />
Potassium-sparing diuretics:<br />
• Often used in combination with high-ceiling diuretics or<br />
thiazides due to potassium-sparing effects<br />
• Produce little diuresis on their own
BIMM118<br />
Diuretics:<br />
Potassium-sparing diuretics:<br />
Renal Pharmacology<br />
– Act on the distal portion of the distal tube (where Na + is exchanged for K + )<br />
– Aldosterone promotes reabsorption of Na + in exchange for K +<br />
(transcriptionally upregulates the Na + /K + pump and sodium channels)<br />
• Spironolactone<br />
– Aldosterone receptor antagonist<br />
– Onset of action requires several days<br />
• Amiloride; Trimterene<br />
– Block sodium channels<br />
– Quick onset<br />
Aldosterone Spironolactone
BIMM118<br />
Diuretics:<br />
Osmotic diuretics:<br />
Renal Pharmacology<br />
– Small, non-reabsorbable molecules that inhibit passive reabsorption of water<br />
– Predominantly increase water excretion without significantly increasing Na +<br />
excretion => limited use<br />
– Used to prevent renal failure, reduction of intracranial pressure<br />
(does not cross blood-brain barrier => water is pulled out of the brain into the blood)<br />
• Mannitol<br />
– Only given IV – can crystallize (=> given with filter needle or in-line filter)
BIMM118<br />
Renal Pharmacology
BIMM118<br />
Renal Pharmacology<br />
Uric acid<br />
• only slightly soluble in water and easily precipitates out of solution forming needlelike<br />
crystals of sodium urate<br />
– sodium urate crystals contribute to the formation of kidney stones and<br />
– produce the excruciating pain of gout when deposited in the joints.<br />
• Curiously, our kidneys reclaim most of the uric acid filtered at the glomeruli. Why, if it<br />
can cause problems?<br />
– Uric acid is a potent antioxidant and thus can protect cells from damage by reactive oxygen<br />
species (ROS).<br />
– The concentration of uric acid is 100-times greater in the cytosol than in the extracellular<br />
fluid. So when lethally-damaged cells release their contents, crystals of uric acid form in the<br />
vicinity. These enhance the ability of nearby dendritic cells to "present" any antigens<br />
released at the same time to T cells leading to a stronger immune response.<br />
=> risk of kidney stones and gout may be the price we pay for these protections.<br />
• Most mammals have an enzyme — uricase — for breaking down uric acid into a<br />
soluble product. However, during the evolution of great apes and humans, the gene<br />
encoding uricase became inactive.<br />
– Uric acid is the chief nitrogenous waste of insects, lizards, snakes and birds<br />
(the whitish material that birds leave on statues)
BIMM118<br />
Uricosuric agents:<br />
Renal Pharmacology<br />
– At therapeutic doses promote excretion and inhibit reabsorption of uric acid<br />
(normally, only 8-12% of the initially filtered urates are eliminated)<br />
– At low, subtherapeutic doses, both excretion and reabsorption are inhibited<br />
=> possibility of an increase in uric acid concentration<br />
• Probenicid<br />
– Inhibits reabsorption of urates in the proximal convoluted tubule<br />
– Strong inhibitory effect on penicillin excretion<br />
• Sulfinpyrazone
BIMM118<br />
Gastrointestinal Pharmacology<br />
• Antacids<br />
– Peptic ulcer therapy<br />
• Antiemetics<br />
• Laxatives<br />
• Antidiarrheal drugs
BIMM118<br />
Acid production:<br />
• 2.5 L per day<br />
• Isotonic HCl solution<br />
• pH < 1<br />
Gastrointestinal Pharmacology<br />
• Produced by parietal cells<br />
Mucus production:<br />
• Produced by mucus-secreting cells<br />
• Also produce bicarbonate, which becomes<br />
trapped in the mucus layer => pH gradient<br />
across the mucus layer (can become<br />
destroyed by alcohol)
BIMM118<br />
Antacids:<br />
Gastrointestinal Pharmacology<br />
Weak bases:<br />
• Aluminum hydroxide<br />
– Cause constipation<br />
• Magnesium hydroxide<br />
– Cause diarrhea<br />
=> often combined<br />
Usally taken 5-7 times per day
BIMM118<br />
Antacids:<br />
Gastrointestinal Pharmacology<br />
• Histamine stimulates acid production by parietal cells<br />
• Mast cells produce a steady basal level of histamine,<br />
which increases in response to gastrin or acetylcholine<br />
• Parietal cells express histamine H 2 receptors =><br />
H 2 receptor blockers:<br />
• Cimetidine (Tagamet®)<br />
– First H 2 -blocker available<br />
– Inhibits P450 => Drug interaction<br />
• Ranitidine (Zantac®)<br />
– Does not inhibit P450 => fewer side effects<br />
• Nizatidine (Axid®)<br />
• Famotidine (Pepcid®)
BIMM118<br />
Antacids:<br />
Gastrointestinal Pharmacology<br />
Proton pump inhibitors:<br />
– Irreversibly inhibit the H + /K + - ATPase in gastric parietal cells<br />
– Drugs are inactive at neutral pH, but since they are weak bases,<br />
are activated in the acidic stomach milieu => restricted activity<br />
– Acid production abliterated for 24-48 hours<br />
• Omeprazole (Prilosec®)<br />
• Lansoprazole (Prevacid®)<br />
• Esomeprazole (Nexium®)<br />
• Rabeprazole
BIMM118<br />
Gastrointestinal Pharmacology<br />
Gastroesophageal reflux disease (GERD):<br />
– Backflow of stomach acid into the esophagus<br />
– Esophagus is not equipped to handle stomach acid => scaring<br />
– Usual symptom is heartburn, an uncomfortable burning sensation behind the<br />
breastbone (MI often mistaken for GERD !)<br />
– More severe symptoms: difficulty swallowing, chest pain<br />
– Reflux into the throat can cause sore throat<br />
– Complications include esophageal erosions, esophageal ulcer and narrowing of<br />
the esophagus (esophageal stricture)<br />
– In some patients, the normal esophageal lining or epithelium may be replaced<br />
with abnormal (Barrett's) epithelium. This condition<br />
(Barrett's esophagus) has been linked to cancer of<br />
the esophagus.<br />
– Primary treatment option are proton pump inhibitors
BIMM118<br />
Gastrointestinal Pharmacology<br />
Mucosal protective agents:<br />
• Misoprostol<br />
– Prostaglandin E 1 analog (PG stimulate mucus and bicarbonate production)<br />
– Used when treatment with NSAIDs inhibits<br />
endogenous PG synthesis<br />
• Sucralfate<br />
– Complex of aluminum hydroxide and sulfated sucrose<br />
– Forms complex gels with mucus => mucus stabilized => diffusion of H + impaired<br />
– Not absorbed => essentially free of side effects<br />
– Must be taken every 6 hours
BIMM118<br />
Gastrointestinal Pharmacology<br />
Peptic Ulcer Disease<br />
Imbalance between defenses and aggressive factors<br />
• Defensive factors:<br />
Prevent the stomach and duodenum from self-digestion<br />
– Mucus: continually secreted, protective effect<br />
– Bicarbonate: secreted from endothelial cells<br />
– Blood flow: good blood flow maintains mucosal integrity<br />
– Prostaglandins: stimulate secretion of bicarbonate and mucus, promote blood flow,<br />
suppress secretion of gastric acid<br />
• Aggressive factors:<br />
– Helicobacter pylori: gram negative bacteria, can live in stomach and duodenum,<br />
may breakdown mucus layer => inflammatory response to presence of the bacteria also<br />
produces urease – forms CO 2 and ammonia which are toxic to mucosa<br />
– Gastric Acid: needs to be present for ulcer to form => activates pepsin and injures<br />
mucosa<br />
– Decreased blood flow: causes decrease in mucus production and bicarbonate synthesis,<br />
promote gastric acid secretion<br />
– NSAIDS: inhibit the production of prostaglandins<br />
– Smoking: nicotine stimulates gastric acid production
BIMM118<br />
Gastrointestinal Pharmacology<br />
Peptic Ulcer Disease<br />
(~25 mill. Americans will have an ulcer in their life)<br />
Most common cause (> 85%): Helicobacter pylorii<br />
(not stress or hot sauce!)<br />
Treatment options:<br />
• Antibiotics<br />
• Antisecretory agents<br />
• Mucosal protectants<br />
• Antisecretory agents that enhance mucosal defenses<br />
• Antacids
BIMM118<br />
Gastrointestinal Pharmacology<br />
Antibiotic ulcer therapy:<br />
Combinations must be used:<br />
• Bismuth (PeptoBismol®) – disrupts cell wall of H. pylori<br />
• Clarithromycin – inhibits protein synthesis<br />
• Amoxicillin – disrupts cell wall<br />
• Tetracyclin – inhibits protein synthesis<br />
• Metronidazole – used often due to bacterial resistance to<br />
amoxicillin and tetracyclin, or due to intolerance by the patient<br />
Standard treatment regimen for peptic ulcer:<br />
Omeprazole + amoxicillin + metronidazole
BIMM118<br />
Gastrointestinal Pharmacology<br />
Antiemetic drugs:<br />
Vomiting:<br />
– Infection, pregnancy, motion sickness, adverse drug effects,…<br />
– Triggered by the “vomiting center” or “chemoreceptor trigger zone (CTZ)” in<br />
the medulla (CTZ is on the ‘blood side’ of the blood-brain barrier).<br />
Treatment options:<br />
– H 1 antagonists: Meclizine, promethazine, dimenhydramine…<br />
– Muscarinic receptor antagonists: Scopolamine (motion sickness)<br />
– Benzodiazepines: Lorazepam (during chemotherapy)<br />
– D 2 antagonists: have also peripheral prokinetic effects => increase motility of<br />
the GI tract => increases the rate of gastric emptying.<br />
Caution in patients with Parkinson’s disease!<br />
Metoclopramide<br />
Domperidone<br />
– Cannabinoids:<br />
Marihuana ?<br />
Synthetic cannabinoids: during chemotherapy<br />
Nabilone<br />
Dronabinol
BIMM118<br />
Laxatives:<br />
Gastrointestinal Pharmacology<br />
• Laxative – production of a soft formed stool over a period of 1 or more days<br />
• Catharsis – prompt, fluid evacuation of the bowel, more intense<br />
Indications for laxative use:<br />
• Pain associated with bowel movements<br />
• To decrease amount of strain under certain conditions<br />
• Evacuate bowel prior to procedures or examinations<br />
• Remove poisons<br />
• To relieve constipation caused by pregnancy or drugs<br />
Contraindications:<br />
• Inflammatory bowel diseases<br />
• Acute surgical abdomen<br />
• Chronic use and abuse
BIMM118<br />
Gastrointestinal Pharmacology<br />
Laxatives:<br />
• Stimulate peristalsis<br />
• Soften bowel content<br />
Classification:<br />
• Bulk laxatives<br />
– Non-absorbable carbohydrates<br />
– Osmotically active laxatives<br />
• Irritant laxatives = purgatives<br />
– Small bowel irritants<br />
– Large bowel irritants<br />
• Lubricant laxatives<br />
– Paraffin<br />
– Glycerol
BIMM118<br />
Gastrointestinal Pharmacology<br />
Laxatives:<br />
Bulk laxatives:<br />
Increase in bowel content volume triggers stretch receptors in the intestinal wall<br />
=> causes reflex contraction (peristalsis) that propels the bowel content forward<br />
Carbohydrate-based laxatives<br />
– Insoluble and non-absorbable<br />
– Non digestable; take several days for effect<br />
– Expand upon taking up water in the bowel<br />
– Must be taken with lots of water<br />
• Vegetable fibers (e.g. Psyllium, lineseed)<br />
• Bran (husks = milling waste product)<br />
Osmotically active laxatives<br />
– Partially soluble, but not absorbable<br />
– Saline-based (mostly sulfates)<br />
– Effect in 1-3 hrs => used to purge intestine (e.g. surgery, poisoning)<br />
• MgSO 4 (= Epsom salt)<br />
• Na 2 SO 4 (= Glauber’s salt)
BIMM118<br />
Gastrointestinal Pharmacology<br />
Laxatives:<br />
Irritant laxatives:<br />
Cause irriatation of the enteric mucosa => more water is secreted than absorbed<br />
=> softer bowel content and increased peristaltic due to increase volume<br />
Small bowel irritants<br />
• Ricinoleic acid (Castor oil)<br />
– Active ingredient of Ricinus communis<br />
– The oil (triglyceride) is inactive<br />
– Ricinoleic acid released from oil through lipase activity<br />
Ricin:<br />
– Lectin from the beans of R.communis<br />
– Potent toxin: inhibits protein synthesis<br />
– Potential bioterrorism agent (LD ~100µg)<br />
In 1978, ricin was used to assassinate Georgi Markov,<br />
a Bulgarian journalist who spoke out against the<br />
Bulgarian government. He was stabbed with the point<br />
of an umbrella while waiting at a bus stop near Waterloo<br />
Station in London. They found a perforated metallic<br />
pellet embedded in his leg that had presumably<br />
contained the ricin toxin.
BIMM118<br />
Gastrointestinal Pharmacology<br />
Laxatives:<br />
Irritant laxatives:<br />
Large bowel irritants<br />
Anthraquinones<br />
Active ingredient of Senna sp. (Folia and fructus sennae),<br />
Rhamnus frangulae (cortex frangulae) and Rheum sp. (rhizoma rhei):<br />
contain inactive glycosides => active anthraquinones released in colon<br />
take 6-10 hours to act
BIMM118<br />
Gastrointestinal Pharmacology<br />
Laxatives:<br />
Irritant laxatives:<br />
Large bowel irritants<br />
Diphenolmethanes<br />
– Derivatives of phenolphtalein<br />
• Bisacodyl<br />
– Oral administration: effect in 6-8 hrs<br />
– Rectal administration: effect in 1 hr<br />
– Often used to prepare for intestinal surgery<br />
• Sodium picosulfate
BIMM118<br />
Gastrointestinal Pharmacology<br />
Laxative abuse:<br />
Most common cause of constipation!<br />
– Longer interval needed to refill<br />
colon is misinterpreted as<br />
constipation => repeated use<br />
– Enteral loss of water and salts<br />
causes release of aldosterone<br />
=> stimulates reabsorption in<br />
intestine, but increases renal<br />
excretion of K + => double loss of<br />
K + causes hypokalemia, which<br />
in turn reduces peristalsis. This<br />
is then often misinterpreted as<br />
constipation => repeated use
BIMM118<br />
Gastrointestinal Pharmacology<br />
Antidiarrheal drugs: treat only symptoms!<br />
– Diarrhea is usually caused by infection (Salmonella, shigella, campylobacter,<br />
clostridium, E. coli), toxins, anxiety, drugs…<br />
– In healthy adults mostly discomfort and inconvenience<br />
– In children (particularly mal-nourished) a principal cause of death due to<br />
excessive loss of water and minerals.<br />
Antimotility agents:<br />
– Muscarinic receptor antagonists (not useful due to side effects) and opiates:<br />
• Morphine<br />
• Codeine<br />
• Diphenoxylate<br />
– All have CNS effects - NOT useful for diarrhea treatment<br />
• Loperamide<br />
– Selective action on the GI tract<br />
– Does not produce CNS effects<br />
– First choice antidiarrheal opoid<br />
– Combined with Dimethicone<br />
(Silicon-based gas-absorbent)
BIMM118<br />
Drugs for Metabolic Disorders<br />
• Diabetes mellitus<br />
• Hyperlipidemia
BIMM118<br />
Diabetes mellitus<br />
Pancreas:<br />
• Islets of Langerhans: site of hormone production<br />
– A (alpha) cells – produce Glucagon<br />
– B (beta) cells – produce Insulin<br />
– D (delta) cells – produce Somatostatin<br />
Insulin and Glucagon are the major regulators of blood glucose
BIMM118<br />
Diabetes mellitus<br />
Blood glucose levels are tightly regulated:
BIMM118<br />
Diabetes mellitus
BIMM118<br />
Diabetes mellitus<br />
Insulin:<br />
• First protein whose sequence was identified (1955)<br />
• 51 amino acids; synthesized as proinsulin (84 aa)<br />
• 6-10 mg stored in the pancreas<br />
• ~ 2 mg released per day<br />
• Liver, brain and red blood cells do not require Insulin for glucose uptake<br />
(only muscle and fat cells depend on insulin)<br />
• Main release stimulus: elevated blood sugar<br />
• Main effect: promote storage of glucose (increase in glucose uptake<br />
(GLUT4) and glycogen synthesis)<br />
• Also inhibits lipolysis, and promotes lipogenesis and amino acid uptake<br />
Glucagon:<br />
• 29 amino acids<br />
• Main release stimulus: hunger (= low blood sugar)
BIMM118<br />
Diabetis mellitus:<br />
Diabetes mellitus<br />
• Group of metabolic diseases characterized by high blood sugar<br />
• Elevated levels of blood glucose (hyperglycemia) lead to spillage of<br />
glucose into the urine (diabetes mellitus means “sweet urine”)<br />
Two distinct clinical forms:<br />
• Type I (= insulin-dependent diabetes = juvenile onset diabetes)<br />
– Caused by destruction of the B cells<br />
– Generally appears in childhood<br />
– Absolutely dependent on insulin replacement<br />
• Type II (= insulin-independent diabetes = adult onset diabetes)<br />
– Caused by target cell resistance to insulin (InsR decreased, signaling defect)<br />
– Mostly obese patients (likely genetic predisposition)<br />
– Obesity appears to reduce the number of insulin receptors<br />
– Can be treated with oral hypoglycemic drugs
BIMM118<br />
Complications:<br />
• Short-term<br />
– Hyperglycemia, (hypoglycemia)<br />
– Ketoacidosis<br />
Diabetes mellitus<br />
• Long-term<br />
– Disruptions in blood flow => Cardiovascular complications => Amputations<br />
Microvascular disease: blood flow to microvasculature lowered (kidney, eye)<br />
– Retinopathy – blindness<br />
– Nephropathy – primary cause of morbidity and mortality<br />
– Neuropathy – nerve damage<br />
– Erectile dysfunction
BIMM118<br />
Insulin:<br />
Diabetes mellitus<br />
Therapeutic insulin used to be purified from porcine or bovine pancreas =><br />
functionally active, but many patients developed an immune response<br />
Today, human insulin is produced by recombinant DNA technology<br />
Main side effect: Hypoglycemia (requires immediate attention!)<br />
“Natural” insulin and four modified insulins are used clinically:<br />
• Regular (Natural) Insulin<br />
– Unmodified human insulin<br />
– rapid acting with short duration (half-life 9 min)<br />
– Only one that can be given IV (infusions, since injections are too brief acting)<br />
– Useful for emergencies (hyperglycemic coma)<br />
• Insulin Lispro (Humalog®)<br />
– reversal of the order of the 28 th and 29 th amino acids of the Beta-chain<br />
– Mutation prevents dimer formation<br />
– more rapid acting – effects 5-15 minutes<br />
– Usually given right before meals
BIMM118<br />
Insulin:<br />
Diabetes mellitus<br />
Main problem with using natural and rapid acting insulin: wide fluctuations in concentration<br />
=> Longer lasting formulations:<br />
• Insulin Lente<br />
– mixed with zinc => forms micro-precipitates =><br />
takes longer to absorb => longer acting<br />
– Only for s.c. administration<br />
– Ultra-lente: longest acting<br />
• NPH Insulin<br />
– regular insulin mixed with protamine (large positively charged protein)<br />
=> delayed absorption<br />
– NPH = neutral protamine Hagedorn<br />
– Long acting
BIMM118<br />
Insulin:<br />
• Insulin Glargine (Lantus®)<br />
Diabetes mellitus<br />
– amino acid asparagine at position A21 is replaced by glycine and two arginines<br />
are added to the C-terminus of the B-chain<br />
– low aqueous solubility at neutral pH, but it is completely soluble at pH 4 (as in the<br />
LANTUS injection solution). After injection into the subcutaneous tissue, the acidic<br />
solution is neutralized, leading to formation of microprecipitates from which small<br />
amounts of insulin glargine are slowly released, resulting in a relatively constant<br />
concentration/time profile over 24 hours with no pronounced peak.
BIMM118<br />
Insulin administration:<br />
Diabetes mellitus<br />
• Subcutaneously (oral application impossible due to degradation)<br />
• Only Regular Insulin can be given IV if needed<br />
• Jet injectors<br />
• Pen injectors<br />
• Implantable insulin pumps<br />
• Intranasal insulin - mucosal atrophy (abandoned)<br />
• Pulmonary insulin (inhalation) - in clinical trial
BIMM118<br />
Diabetes mellitus<br />
Oral hypoglycemic agents:<br />
Useful only in Type II diabetes!<br />
Sulfonylureas<br />
Stimulate insulin release (increase sensitivity of B cell towards glucose: block ATPgated<br />
K + channel => membrane depolarization => Ca ++ increase => insulin secretion),<br />
reduce serum glucagon levels, increase insulin binding on target cells<br />
First generation sulfonylureas:<br />
• Tolbutamide (t 1/2 = 6-12h)<br />
• Chlorpropamide (not used anymore)<br />
• Tolazamide<br />
• Acetohexamide<br />
Second generation sulfonylureas:<br />
• Glimepiride (t 1/2 = 18-24h), 100x more<br />
potent than Tolbutamide<br />
• Glipizide<br />
• Glyburide
BIMM118<br />
Diabetes mellitus<br />
Oral hypoglycemic agents:<br />
-glitazones (Thiozolidinediones)<br />
Increase insulin sensitivity of target cells:<br />
function as PPARγ agonists => promote transcription of insulin receptor signaling<br />
components and of glucose transporters<br />
Main side effect: hypoglycemia<br />
• Troglitazone<br />
– First of its class<br />
– Hepatotoxic!<br />
– No longer in use<br />
• Rosiglitazone<br />
• Pioglitazone<br />
– Half-life ~ 7hrs<br />
– Half-life of active metabolites up to 150 hrs !
BIMM118<br />
Diabetes mellitus<br />
Oral hypoglycemic agents:<br />
Biguanides<br />
• Metformine<br />
– Only drug in this class in use<br />
– Increase glucose uptake and inhibit gluconeogenesis in the liver<br />
– Mechanism unclear<br />
– Also lowers LDL and VLDL<br />
– Adverse side effects: Diarrhea, nausea<br />
– Benefitial side effect: appetite suppressant!<br />
– Does not cause hypoglycemia<br />
– Not for patients with liver or kidney<br />
disease (predisposition to lactic acidosis)
BIMM118<br />
Novel concepts:<br />
Alpha-Glucosidases:<br />
Diabetes mellitus<br />
– Intestinal enzymes in the small intestine<br />
– Break down complex carbohydrates (Starch, Glygogen)<br />
Alpha-Glucosidase Inhibitors:<br />
– Inhibit carbohydrate breakdown => less monosaccherides available for absorption<br />
– Saccharides that act as competitive enzyme inhibitors<br />
– DO NOT increase insulin levels !!<br />
– Maybe useful in Type I diabetes as well?<br />
• Acarbose<br />
– Also inhibits alpha-amylases<br />
– No significant absorption => no systemic side effects<br />
– Used to prevent postprandial hyperglycemia<br />
– Side effects: Diarrhea, flatulence (intestinal bacteria digest the carbohydrates!)<br />
• Miglitol<br />
– Systemically absorbed<br />
– No effect on alpha-amylases
BIMM118<br />
Novel concepts (cont’d):<br />
Incretins:<br />
Diabetes mellitus<br />
– Gastrointestinal hormones: Glucagon-Like Peptide 1 (GLP1)<br />
Gastric Inhibitory Peptide (GIP)<br />
– Both are inactivated by Dipeptidyl Peptidase 4 (DPP4)<br />
– Insulin released before glucose levels become elevated<br />
– Reduce gastric emptying => slower carbohydrate absorption<br />
– Inhibit Glucagon release<br />
– Reduce food intake<br />
Incretin mimetic:<br />
• Exenatide<br />
– Originally identified in the saliver of the Gila Monster (“Lizard spit”)<br />
– No effect if glucose levels are normal => no risk of hypoglycemic shock<br />
– Long-term weight loss<br />
– Only for s.c.injection<br />
DPP4-Inhibitors:<br />
No effect if glucose levels are normal => no risk of hypoglycemic shock<br />
Oral administration!<br />
• Sitagliptin<br />
• Vildagliptin
BIMM118<br />
Novel concepts (cont’d):<br />
Diabetes mellitus<br />
Amylin:<br />
– Pancreatic hormone (also from β-Islet cells)<br />
– Reduces gastric emptying<br />
– Inhibit Glucagon release<br />
– Promotes satiety (=> decreased food intake)<br />
Amylin mimetics:<br />
• Pramlintide<br />
– Only drug other than insulin approved for Type I Diabetes !!<br />
– Used in combination with insulin
BIMM118<br />
Artherosclerosis:<br />
Hyperlipidemia
BIMM118<br />
Artherosclerosis:<br />
Hyperlipidemia
BIMM118<br />
Artherosclerosis:<br />
Hyperlipidemia<br />
Initiating mechanism:<br />
– Endothelial cells (EC) bind LDL<br />
– When activated (e.g. injury), EC and attached macrophages produce ROS<br />
– ROS oxidize LDL, which results in lipid peroxidation<br />
– This leads to the destruction of the LDL receptors which normally clear LDL<br />
– Oxidized LDL is phagocytosed by macrophages via “scavenger receptors”<br />
– Upon ingestion of oxidized LDL, macrophages become foam cells<br />
– One species of LDL, lipoprotein(a) contains apoprotein(a) which is structually<br />
similar to plasminogen. Plasminogen activator on EC processes plasminogen into<br />
the fibrinolytic enzyme plasmin.<br />
– LDL displaces plasminogen on EC => plasmin reduced => thrombosis promoted
BIMM118<br />
Lipoprotein metabolism:<br />
– Absorbed lipids released by enterocytes<br />
in form of chylomicrones<br />
– Chylomicrones bypass the liver, enter the<br />
circulation via lymph and are hydrolyzed<br />
in target tissues by lipoprotein lipases<br />
– 60-70% of the cholesterol in the liver<br />
stems from de novo synthesis<br />
– Liver requires cholesterol to produce<br />
VLDL particles, which are released into<br />
the blood stream<br />
– VLDL particles provide target tissues<br />
with fatty acids => become LDL particles<br />
– HDL particles transfer cholesterol from<br />
tissues to LDL particles<br />
Hyperlipidemia
BIMM118<br />
Cholesterol:<br />
– 60-70% (=1000 mg) synthesized (not from<br />
Hyperlipidemia<br />
food!): Liver, intestines, reproductive organs…<br />
– Rate-limiting enzyme: HMG-CoA reductase<br />
(3-hydroxy-3-methyl-glutaryl-CoA reductase)<br />
< 200mg/dl: no risk<br />
200-240 mg/dl: moderate risk<br />
> 240 mg/dl: high risk
BIMM118<br />
Lipid-lowering drugs:<br />
Hyperlipidemia<br />
HMG-CoA reductase inhibitors (Statins):<br />
– Bear structural resemblance to HMG-CoA<br />
– Reversible competitive inhibitors of HMG-CoA reductase<br />
– Isolated from Aspergillus sp.<br />
– Side effects: Hepatotoxicity, GI disturbances, myopathy<br />
• Simvastatin (Zocor®)<br />
• Lovastatin (Mevacor®)<br />
– Both drugs are precursors =><br />
activated in the liver<br />
– Lactone ring is hydrolyzed<br />
Lovastatin
BIMM118<br />
Lipid-lowering drugs:<br />
Hyperlipidemia<br />
HMG-CoA reductase inhibitors (Statins):<br />
• Fluvastatin (Lescol®)<br />
• Pravastatin (Pravachol®)<br />
– Both drugs are already in active form<br />
• Atorvastatin (Lipitor®)<br />
– Long-lasting inhibition if HMGR<br />
Atorvastatin<br />
Fluvastatin<br />
Pravastatin
BIMM118<br />
Hyperlipidemia<br />
Lipid-lowering drugs:<br />
HMG-CoA reductase inhibitors (Statins):<br />
• Statins accumulate in the liver (usually an undesired drug effect)<br />
• Cholesterol synthesis is predominantly effected in the liver =><br />
hepatocytes must meet their cholesterol requirements through<br />
different mechanisms =><br />
• Hepatic upregulation of the LDL-receptors => increase in LDL<br />
uptake => decrease in circulating LDL
BIMM118<br />
Lipid-lowering drugs:<br />
Hyperlipidemia<br />
Fibrates:<br />
– Fibric acid derivates<br />
– PPARα agonists: stimulate β-oxidation of fatty acids<br />
– Also stimulate lipoprotein lipase activity<br />
– Reduce hepatic VLDL production<br />
– Affect predominantly VLDL levels (little effect on LDL)<br />
– Increase in HDL !<br />
– Side effects: Myositis (unusual, but severe)<br />
• Clofibrate<br />
• Bezafibrate (Cedur®)<br />
• Fenofibrate (Tricor®)<br />
• Ciprofibrate<br />
• Gemfibrozil (Lopid®)
BIMM118<br />
Lipid-lowering drugs:<br />
Bile acid binding resins:<br />
– Anion exchange resins<br />
Hyperlipidemia<br />
– Prevent reabsorption and enterohepatic recirculation of bile acids<br />
=> increase in hepatic LDL receptors => increase in hepatic LDL uptake<br />
=> Reduced LDL in the plasma<br />
– Side effects: resins are not absorbed => no systemic side effects<br />
mostly bloating, constipation, diarrhea<br />
– Interfer with absorption of drugs (e.g. digoxin) and fat-soluble vitamins<br />
– Not particularly appetizing<br />
• Cholestyramine<br />
• Colestipol
BIMM118<br />
Hyperlipidemia
BIMM118<br />
Steroid-based Drugs<br />
• Adrenocortical<br />
Hormones
BIMM118<br />
Adrenal gland:<br />
• Medulla:<br />
Adrenocortical Hormones<br />
– produces Epinephrine<br />
(stimulated by sympathetic impulse)<br />
• Cortex:<br />
– Zona glomerulosa – produces Aldosterone<br />
(stimulated by Angiotensin II and ACTH)<br />
– Zona fasciculata – produces Glucocorticoids<br />
(stimulated by ACTH = Corticotropin)<br />
– Zona reticularis – produces Androgens<br />
(physiological role unclear)
BIMM118<br />
Steroid hormone synthesis:<br />
Adrenocortical Hormones<br />
• Pregnenolone synthesis is rate-limiting step<br />
• C21 hydroxylase:<br />
– Prevents hydroxylation of C17 (-> c)<br />
=> Only mineralocorticoids<br />
• C17 hydroxylase:<br />
– Hydroxylation of C17 (-> f, g) can be followed<br />
by hydroxylation of C11 and C21 (-> h, j, k)<br />
=> Sex hormones and glucocorticoids<br />
• P450 C17α hydroxylase:<br />
– Produces 17-Keto-steroids (-> l)<br />
=> Sex hormones
BIMM118<br />
Adrenocortical Hormones<br />
Steroid hormone classification:<br />
• Progesterone:<br />
– C21<br />
– C 3: =O<br />
– C17: -OH or =O<br />
• Mineralocorticoids:<br />
– C21<br />
– C21: -OH<br />
– C3: =O<br />
• Glucocorticoids :<br />
– C21<br />
– C21, C17: -OH<br />
– C 3: =O<br />
– C11: -OH or =O<br />
• Estrogens :<br />
– C18<br />
– C17: -OH or =O<br />
– C 3: -OH<br />
• Androgens :<br />
– C19<br />
– C17: -OH<br />
– C 3: =O
BIMM118<br />
Glucocorticoids (GC):<br />
Adrenocortical Hormones<br />
• Inhibit all phases of inflammatory reaction<br />
• Promote fetal development (lungs)<br />
• Inhibit NFκB nuclear translocation => transcription of proinflammatory<br />
mediators is prevented<br />
• Upregulate lipocortin => inhibits PLA 2 => no PG and LT synthesis<br />
• Undesirable effects of increased GC:<br />
– Immune suppression<br />
– Increased glucose release (=> “steroid diabetes”)<br />
– Glucose coverted to fat => adiposity<br />
– Increased protein catabolism => muscle atrophy<br />
– Salt and water retention (increased GC lead to reduction in ACTH => decreases<br />
levels of aldosterone) => hypertension<br />
– Osteoporosis
BIMM118<br />
Glucocorticoids (GC):<br />
Adrenocortical Hormones<br />
• Adrenal cortex failure (= Addison’s disease)<br />
Lack of GC production:<br />
– Chronic fatigue and muscle weakness.<br />
– Loss of appetite, inability to digest food, and weight loss.<br />
– Low blood pressure (hypotension)<br />
– Blotchy, dark tanning and freckling of the skin<br />
(feedback missing => increased corticotropin)<br />
– Blood sugar abnormalities<br />
– Inability to cope with stress<br />
• Adrenal cortex tumors (= Cushing Syndrome)<br />
GC overproduction<br />
– Upper body obesity<br />
– “Buffalo hump”<br />
– Red, round face<br />
– Hypertension<br />
– Water retention<br />
– Thin skin and bruising<br />
– Poor wound healing
BIMM118<br />
Adrenocortical Hormones<br />
Glucocorticoids (GC):<br />
Clinical uses:<br />
• Allergic Rhinitis<br />
• Rheumatoid Arthritis<br />
• Asthma<br />
• Multiple Sclerosis<br />
• Carpal Tunnel Syndrome<br />
• Dermatitis<br />
• COPD<br />
• Osteoarthritis<br />
• Gout<br />
• Psoriasis<br />
• Inflammatory Bowel Disease<br />
• Sinusitis<br />
• Lupus Erythematosus<br />
• Many conditions flare up if GC therapy is discontinued due<br />
to adreno-corticol atrophy
BIMM118<br />
Glucocorticoids (GC):<br />
• Hydrocortison (= Cortisol)<br />
– Main glucocortocoid in humans<br />
Adrenocortical Hormones<br />
– Also binds mineralocorticoid receptor<br />
(Cortison does NOT)<br />
– Used for replacement therapy (Addison’s Disease)<br />
– Otherwise mostly topical application due to<br />
sodium-retaining effects
BIMM118<br />
Glucocorticoids (GC):<br />
• Prednisone<br />
– Inactive until converted to<br />
• Prednisolone<br />
Adrenocortical Hormones<br />
– Drug of choice for systemic application<br />
– Lower sodium-retaining effects<br />
O<br />
Prednisolone<br />
HO<br />
CH 3<br />
O<br />
CH 3<br />
OH<br />
OH<br />
O<br />
Prednisone<br />
O<br />
CH 3<br />
O<br />
CH 3<br />
OH<br />
OH
BIMM118<br />
Glucocorticoids (GC):<br />
• Triamcinoline<br />
Adrenocortical Hormones<br />
– Stronger anti-inflammatory (5x) than cortisol<br />
– No sodium-retaining effect<br />
Halogenated GC<br />
• Betamethasone<br />
• Dexamethasone<br />
– 30x more potent than cortisol<br />
– No water and sodium retaining effects<br />
O<br />
O<br />
O<br />
HO<br />
CH 3<br />
HO<br />
HO<br />
CH 3<br />
F<br />
CH 3<br />
F<br />
O<br />
CH 3<br />
O<br />
CH 3<br />
O<br />
CH 3<br />
OH<br />
O<br />
O<br />
OH<br />
OH<br />
OH<br />
CH 3<br />
OH<br />
CH 3
BIMM118<br />
Glucocorticoids (GC):<br />
• Administration<br />
– Oral<br />
– Nasal<br />
– Cutaneous<br />
– IV<br />
– Inhalation<br />
Adrenocortical Hormones
BIMM118<br />
Steroid-based Drugs<br />
• Sex Steroids
BIMM118<br />
Sex Steroids<br />
• Female reproductive cycle<br />
– Gonadotropin Releasing Hormone<br />
(GnRH) = Gonadoliberin<br />
stimulates release of<br />
– Follicle stimulating hormone<br />
(FSH) = Follitropin<br />
and<br />
– Luteinising Hormone<br />
(LH) = Lutropin<br />
which trigger production of<br />
– Estrogens (E) and Gestagens (G)<br />
which in turn negatively regulate<br />
– Pituitary (E+G) and Hypothalamus (G)<br />
hormone production
BIMM118<br />
Sex Steroids<br />
• Female reproductive cycle<br />
– Cycle length varies from 21-35 days<br />
• Menstruation 3-6 days<br />
– First (= Proliferative) phase:<br />
• Variable (7-21 days)<br />
• FSH and LH promote follicle development<br />
• One follicle becomes the Graafian follicle<br />
(the rest degenerate)<br />
• Graaffian Follicle:<br />
– Consists of thecal and granulosa cells<br />
which surround the ovum<br />
• FSH-stimulated granulosa cells produce<br />
estrogens from androgen precursors<br />
generated by LH-stimulated thecal cells<br />
• Estrogens are responsible for the<br />
proliferative phase: increase in thickness<br />
and vascularity of endometrium; secretion<br />
of protein+ carbo-rich mucus<br />
• Constant low estrogen inhibits LH/FSH production BUT high estrogen cause<br />
surge of LH production => swellign and rupture of Graafian follicle = Ovulation
BIMM118<br />
Sex Steroids<br />
• Female reproductive cycle<br />
– Second (= Secretory) phase:<br />
• Secretory phase constant (~ 14 days)<br />
• LH-stimulated ruptured follicle develops<br />
into Corpus luteum which secrets<br />
Progesterone<br />
• Progesterone (Pg) is responsible for the<br />
secretory phase: endometrium becomes<br />
suitable for implantation; mucus thickens<br />
• Thermogenic effects of Pg =><br />
body temperature increase 0.5º C<br />
• Without implantation: Pg secretion stops<br />
=> menstuation is triggered<br />
• With implantation: continued Pg production<br />
which (via inhibition of LH and FSH prod.)<br />
blocks further ovulation<br />
• Chorion (“precursor” of placenta) secretes<br />
human chorionic gonadotropin (HCG) which<br />
maintains endometrium lining throughout<br />
pregnancy (HCG -> see pregnancy test)
BIMM118<br />
Sex Steroids<br />
• Female reproductive cycle
BIMM118<br />
Sex Steroids<br />
Estrogens<br />
All produced from androgen precursors<br />
Three main endogenous estrogens:<br />
• Estradiol<br />
– Primary estrogen in humans<br />
– Breast development<br />
– Improving bone density<br />
– Growth of the uterus<br />
– Accelerating bone maturation and epiphyses closure<br />
– Development of the endometrium to support pregnancy<br />
– Promoting vaginal mucosal thickness and secretions<br />
– Increase HDL<br />
• Estrone<br />
• Estriol<br />
– only during pregnancy (made by fetus)
BIMM118<br />
Sex Steroids<br />
Estrogens<br />
– Estrogens induce expression of progesterone receptors<br />
– Progesterone inhibits expression of estrogen receptors<br />
– Two types of estrogen receptors => potential for selective drugs<br />
• Estradiol<br />
– Not suitable for oral administration (rapid hepatic elimination)<br />
=> stable derivatives:<br />
• Ethinylestradiol<br />
• Diethyl-Stilbestrol<br />
– Stilbene derivative
BIMM118<br />
Estrogens<br />
• Mestranol<br />
Sex Steroids<br />
– Used in oral contraceptives<br />
– Inactive => Cleavage of C3-methoxy group<br />
yields ethinylestradiol<br />
• Raloxifene<br />
– Selective estrogen receptor modifier (=SERM)<br />
– Antiestrogenic effects on breast and endometrium<br />
– Estrogenic effects on bone and lipid metabolism<br />
=> use in postmenopausal osteoporosis<br />
Clinical uses of estrogens:<br />
– Replacement therapy (Turner syndrome; menopause)<br />
– Contraception<br />
– Cancer therapy
BIMM118<br />
Anti-Estrogens<br />
• Tamoxifen<br />
Sex Steroids<br />
– Antiestrogenic effects on mammary tissue<br />
– Weak estrogenic effects on bone and lipid metabolism<br />
• Clomiphene<br />
– Inhibits estrogen binding in the pituitary<br />
=> prevention of negative feedback=> ovulation<br />
Clinical uses of anti-estrogens:<br />
– Breast cancer therapy (Tamoxifen)<br />
– Infertility (Clomiphen)
BIMM118<br />
Progesterons<br />
• Progesterone<br />
Sex Steroids<br />
– Inhibits rhythmic contractions of the myometrium<br />
– Not suitable for oral administration<br />
(rapid hepatic elimination) => stable derivatives:<br />
• Hydroxyprogesterone<br />
• Medroxyprogesterone
BIMM118<br />
Progesterons<br />
Sex Steroids<br />
Testosterone derivatives with progesterone activity:<br />
• Norethindrone<br />
• Norgestrel<br />
• Desogestrel
BIMM118<br />
Anti-Progesterons<br />
• Mifepristone (RU486)<br />
Sex Steroids<br />
– developed during the early 1980s by the French company Roussel Uclaf<br />
– while investigating glucocorticoid receptor antagonists, they discovered compounds<br />
that blocked the similarly shaped progesterone receptor. Further refinement led to the<br />
production of RU 486<br />
– Clinical testing of mifepristone as a means of inducing medical abortion began in<br />
France in 1982. Results from these trials showed that when used as a single agent,<br />
mifepristone induced a complete abortion in up to 80% of women up to 49 days’<br />
gestation.<br />
– Addition of small doses of a prostaglandin analogue (=> see misoprostol) a few days<br />
later to stimulate uterine contractions, a complete medical abortion is achieved in<br />
nearly 100 percent of women<br />
– approved in the US in 2000 for the termination of<br />
early pregnancy (defined as 49 days or less)
BIMM118<br />
Sex Steroids<br />
• Male reproductive system<br />
– Gonadotropin Releasing Hormone<br />
(GnRH) = Gonadoliberin<br />
stimulates release of<br />
– Follicle stimulating hormone (FSH)<br />
(Stimulates Sertoli cells =><br />
promotes gametogenesis)<br />
and<br />
– Luteinising Hormone (LH) =<br />
Interstitial Cell Stimulating Hormone (ICSH)<br />
which triggers production of<br />
– Testosterone (T) (by Leydig cells)<br />
which in turn negatively regulates<br />
– Pituitary and Hypothalamus hormone production
BIMM118<br />
Androgens<br />
Sex Steroids<br />
• Testosterone<br />
– Primary androgen in humans<br />
– Possesses androgenic and anabolic effects:<br />
Androgenic effects:<br />
• Growth and development of male sex organs<br />
• Important for (male) sex drive and performance<br />
• Development of secondary sexual characteristics<br />
• Important role in spermatogenesis<br />
Anabolic effects:<br />
• Development of muscle mass<br />
• Reverse catabolic or tissue-depleting processes<br />
• Dihydro-Testosterone<br />
– Active metabolite<br />
– Mediates most of testosterone actions<br />
O<br />
O<br />
CH 3<br />
CH 3<br />
H<br />
CH 3<br />
CH 3<br />
OH<br />
OH
BIMM118<br />
Androgens<br />
Sex Steroids<br />
• Testosterone<br />
– Hepatic elimination after oral administration<br />
– Also short half-life after injection => ester derivatives:<br />
Proprionate, enanthate, cypionate…<br />
• Fluoxymesterone<br />
– Hepatic elimination after oral administration<br />
O<br />
O<br />
HO<br />
CH 3<br />
CH 3<br />
F<br />
CH 3<br />
CH 3<br />
OH<br />
OHR<br />
CH 3
BIMM118<br />
Anabolic Androgens<br />
Sex Steroids<br />
Testosterone derivatives: anabolic effects dominant<br />
• Nandrolone<br />
– Injection<br />
• Stanozolol<br />
– oral administration<br />
HN<br />
N<br />
O<br />
CH 3<br />
H<br />
H<br />
CH 3<br />
OH<br />
CH OH<br />
3<br />
CH3<br />
O<br />
CH 3<br />
CH 3<br />
OH
BIMM118<br />
Anabolic Androgens<br />
• Dehydroepiandrosterone (DHEA)<br />
Sex Steroids<br />
– Popular item in health food stores: DHEA was prescription only until<br />
recently when changes in federal law labeled it as a nutritional<br />
supplement (DHEA sales now equal that of melatonin)<br />
– Is actually a testosterone precursor<br />
– Supposedly by maintaining youthful DHEA levels one can improve mood,<br />
memory, energy and libido, while preserving lean body mass and counteracting<br />
the effects of stress hormones.<br />
– DHEA may have serious side effects:<br />
• If it abnormally increases testosterone, then testosterone side effects may be<br />
expected, including acne, testicular atrophy and increased risk of prostate cancer.<br />
• Women taking excessive doses of DHEA have reported acne and facial hair.<br />
– DHEA can also be converted into estrogen, so high levels of DHEA can lead to<br />
estrogen side effects as well, including gynaecomasty and increased risk of<br />
breast cancer.<br />
– DHEA is often marketed as an anabolic steroid: This is misleading since as an<br />
androgen precursor its metabolism will produce testosterone which has anabolic<br />
properties
BIMM118<br />
Anti-Androgens<br />
• Flutamide<br />
– Non-steroidal receptor antagonist<br />
– Used in prostate cancer treatment<br />
Sex Steroids<br />
• Finasteride<br />
– Inhibits 5α-reductase => prevent conversion of<br />
testosterone into the more potent dihydrotestosterone (DHT)<br />
– Used to treat prostate gland enlargement and hair loss<br />
(bald man have higher average levels of DHT)<br />
O<br />
N<br />
H<br />
CH 3<br />
H<br />
CH 3<br />
O<br />
N<br />
H<br />
CH 3<br />
CH 3<br />
CH 3<br />
CF 3<br />
HN<br />
O<br />
NO 2<br />
CH 3<br />
CH 3
BIMM118<br />
GnRH analogs/modifiers<br />
Sex Steroids<br />
• Danazol<br />
– Inhibits GnRH release => no FSH/LH production<br />
=> no steroid production<br />
– Used to treat endometriosis<br />
(growth of endometrial tissue outside of the uterus)<br />
• Synthetic GnRH (Gonadorelin, Buserelin, Leuprorelin…)<br />
– Up to 200x more potent than GnRH<br />
– If given in pulses (s.c.) stimulate gonadotropin release => induce ovulation<br />
– If given continously they desensitize the GnRH receptors => gonadal<br />
suppression (“medical castration”)<br />
– Used in sex hormone-dependent conditions (prostate, breast cancer;<br />
endometriosis; uterine fibroids…)<br />
– Side effects: menopausal symptoms<br />
N<br />
O<br />
CH 3<br />
CH 3 OH<br />
CH
BIMM118<br />
Oral Contraceptives<br />
• History<br />
Sex Steroids<br />
– 1937: Investigators demonstrated that the female<br />
hormone progesterone could halt ovulation in rabbits<br />
– 1949: Scientists at the University of Pennsylvania<br />
achieved the production of synthetic progestins<br />
– 1953: Margaret Sanger, Katherine McCormick and Gregory Pincus team up to<br />
develop a reliable contraceptive<br />
– 1950s: Large scale testing of “the pill” was successful<br />
– 1960: FDA approves first oral contraceptive<br />
(Early pill formulations contained up to 150 micrograms (mcg) of estrogen!)<br />
– 1982/84: Introduction of the bi- and tri-stage formulation<br />
– 1988: FDA recognized several severe long-term side effects (high estrogen!)<br />
– Currently used by 16 mill. women in the US (40% of women between 18 and 24
BIMM118<br />
Oral Contraceptives<br />
Sex Steroids<br />
Either combination estrogen/progesterone of progesterone alone<br />
• Combination pills:<br />
– Highly effective<br />
– Estrogen component is mostly ethinylestradiol, sometimes mestranol<br />
– Progesterone component varies<br />
– 21 day cycle with 7 day break (causes withdrawal bleeding)<br />
– Can be mono- or biphasic<br />
Mechanism:<br />
– Estrogen inhibits FSH secretion (neg. feedback loop!)<br />
=> suppression of follicle development<br />
– Progesterone inhibits LH secretion (neg. feedback loop!)<br />
=> inhibition of ovulation; also increases mucus viscosity<br />
– Both steroids alter endometrium => prevent implantation
BIMM118<br />
Oral Contraceptives<br />
Sex Steroids<br />
Estrogen<br />
Progesterone
BIMM118<br />
Contraceptives<br />
Sex Steroids<br />
• “Mini Pill”:<br />
– Contains only a progesterone (Levonorgestrel, Ethynodiol…)<br />
– Used when estrogen in contraindicated (e.g. thrombosis)<br />
– Taken daily without interruption<br />
– Acts mainly by increasing viscosity of mucus<br />
(Mucolytica in cough medicine can cause failure)<br />
– Less reliable than combination pill<br />
• Postcoital contraceptives (“Morning after pill”)<br />
– High dose of progesterone (Levonorgestrel)<br />
– Must be taken within 72 hrs<br />
– Nausea and vomiting are common side effects<br />
• Depot and patch formulations<br />
– Injection of oily depot formulations every 3 month<br />
– Transdermal delivery systems
BIMM118<br />
Oral Contraceptives<br />
Side effects:<br />
– Thrombosis<br />
– Hypertension<br />
– Intermittant bleeding<br />
– Weight gain<br />
– Depression<br />
– Nausea<br />
– Loss of libido<br />
Sex Steroids<br />
Drug interactions:<br />
– Steroids are metabolized by P450 enzymes<br />
– Minimal dose of steroid is used to prevent risk of thrombosis<br />
– Any increase in clearance by P450-inducing drugs can result in contraception failure<br />
– Frequent cause of OC failure is diarrhea (diminished time for absorption)
BIMM118<br />
Drugs against Allergies<br />
• Antihistamines<br />
• Leukotriene Modulators<br />
• Glucocorticoids<br />
• Epinephrine
BIMM118<br />
Allergy<br />
Allergy:<br />
represents a sensitivity to a specific substance, called an<br />
allergen, that is contacted through the skin, inhaled into the<br />
lungs, swallowed, or injected.<br />
Anaphylaxis:<br />
is a severe whole-body allergic reaction that occurs within minutes of<br />
exposure, progresses rapidly and can lead to anaphylactic shock and death.
BIMM118<br />
Allergy - Symptoms
BIMM118<br />
Allergy - Pathophysiology
BIMM118<br />
Allergy - Food<br />
• Allergic reactions to foods almost always occur immediately<br />
• The majority of reactions are not fatal<br />
• In general, reactions worsen with age
Allergy - Latex<br />
BIMM118 Latex: milky sap from the rubber tree hevea brasiliensis
BIMM118<br />
Latex has cross-reactive epitopes<br />
with foods: banana, avocado,<br />
chestnut<br />
Allergy - Latex
BIMM118<br />
Allergy - Hymenoptera stings<br />
Hymenoptera (hymen=membrane; ptera=wings): ants, bees, wasps<br />
Bee<br />
Wasp<br />
Bumble Bee<br />
Yellow jacket
BIMM118<br />
Allergy - Drugs<br />
Predominantly against beta-lactam antibiotics and NSAIDs:
BIMM118<br />
Allergy - Diagnosis
BIMM118<br />
Allergy - Mediators
BIMM118<br />
Allergy - Histamine<br />
Receptors:<br />
part of the super family of G-protein coupled receptors<br />
•H1-Receptor<br />
–Gq coupled to Phospholipase C<br />
–CNS, smooth muscle cells of airways, GI tract, cardiovascular system, endothelial<br />
cells and lymphocytes => Vasodilation, bronchoconstriction, seperation of<br />
endothelial cells, pain and itching, allergic rhinitis, motion sickness.<br />
•H2-Receptor<br />
–Gs coupled to Adenylyl Cyclase<br />
–Parietal cells; vascular smooth muscle cells => mediate histamine induced gastric<br />
acid secretion; vasodilation<br />
•H3-Receptor<br />
–Gi/o coupled to AC, also to N-type voltage gated Ca channels and reduce Ca influx<br />
–CNS => Presynaptic, feedback inhibition of histamine synthesis and release; also<br />
controls release of other neurotransmitters<br />
•H4-Receptor<br />
–coupled to Gi/o in mast cells, can trigger calcium mobilization<br />
–found primarily in bone marrow and immune cells => mast cell chemotaxis
BIMM118<br />
Allergy - Histamine<br />
Histamine:<br />
Endogenous bioactive amine: synthesized, stored and released in<br />
–mast cells, which are abundant in the skin, GI, and the respiratory tract<br />
–basophils in the blood<br />
–neurons in the CNS and peripheral NS<br />
•Physiological actions<br />
–Primary stimulant for gastric acid and pepsin secretion<br />
(acid secretion is further enhanced by gastrin and vagal stimulation)<br />
–Neurotransmitter (both in the CNS and peripheral sites)<br />
•Pathophysiological actions<br />
–Mediator of immediate hypersensitivity reactions and acute inflammatory responses<br />
–Anaphylaxis<br />
–Duodenal ulcers
BIMM118<br />
Allergy - Histamine Effects<br />
Actions of Histamine:<br />
Vascular:<br />
H 1 - vasodilation mediated by NO and PGs (via endothelial cells)<br />
H 2 - vasodilation mediated by cAMP (vascular smooth muscle cells)<br />
H 1 - coronary vasoconstriction<br />
H 1 - increased permeability of post capillary venules => edema<br />
Heart:<br />
H 1 - decreased AV conduction<br />
H 2 - increased chronotropy<br />
H 2 - increased inotropy<br />
Lung:<br />
H 1 - bronchoconstriction<br />
H 1 - increased mucus viscosity<br />
H 1 - stimulation of vagal sensory nerve endings: cough and bronchospasm<br />
Gastrointestinal System:<br />
H 2 - acid, fluid and pepsin secretion<br />
H 1 - increased intestinal motility and secretions<br />
Cutaneous Nerve Endings:<br />
H 1 - pain and itching<br />
Symptoms range from mild allergic symptoms to anaphylactic shock:<br />
• mild/cutaneous: erythema, urticaria, and/or itching<br />
• moderate: skin reactions, tachycardia, dysrhythmias, moderate<br />
hypotension, mild respiratory distress<br />
• severe/anaphylactic: severe hypotension, ventricular fibrillations, cardiac arrest,<br />
bronchospasm, respiratory arrest
BIMM118<br />
Allergy - Drugs Targeting Histamine<br />
• H1 Receptor Antagonists<br />
Actually inverse agonists (H-receptors display baseline activity!)<br />
– 1 st Generation (Sedating):<br />
• Ethylenediamines: 1st antihistamines => obsolete<br />
• Ethanolamines: Diphenhydramine, Doxylamine, Clemastine<br />
• Alkylamines: Chlorpheniramine<br />
• Piperazines: Meclizine, Hydroxyzine<br />
– 2 nd Generation (Non-sedating):<br />
• Piperazines: Cetirizine<br />
• Piperidines: Loratadine, Fexofenadine<br />
• (H2 Receptor Antagonists => GI drugs)<br />
• (H3 Receptor Agonist and Antagonists: potential new drugs being developed)<br />
• Mast Cell Stabilizers
BIMM118<br />
H1-Antagonists (“Antihistamines”)<br />
First generation drugs:<br />
• Applications:<br />
– Adjunctive in anaphylaxis (H 2 antagonists and epinephrine also used)<br />
– Antiallergy (allergic rhinitis, allergic dermatoses, contact dermatitis)<br />
– Sedative/sleep aid<br />
– Prevention of motion sickness<br />
• Adverse effects:<br />
– Sedation (Paradoxical Excitation in children)<br />
– Dizziness, Fatigue<br />
– Peripheral anti-muscarinic effects: (also block muscarinic Ach receptors)<br />
• Dry Mouth<br />
• Blurred Vision<br />
• Constipation<br />
• Urinary Retention<br />
• Drug interactions:<br />
– Additive with classical muscarinic Ach receptor antagonists<br />
– Potentiate CNS depressants<br />
• opioids<br />
• sedatives<br />
• general and narcotic analgesics<br />
• alcohol
BIMM118<br />
H1-Antagonists (“Antihistamines”)<br />
First generation drugs:<br />
• Diphenhydramine (Benadryl®):<br />
– Allergic rhinitis (=seasonal allergies);<br />
skin allergies (=contact dermatitis); cough relief<br />
– Penetrates blood/brain barrier => Sedative/sleep aid<br />
• Dimenhydrinate (Dramamine®):<br />
– 1:1 ratio Diphenhydramine : 8-Cl-Theophylline => Slower action<br />
– Anti H1 and anti-muscarinic activity => good antiemetic<br />
– Used to treat nausea, motion sickness
BIMM118<br />
H1-Antagonists (“Antihistamines”)<br />
First generation drugs:<br />
• Doxylamine (Unisom®, Nyquil®):<br />
– Antiallergy: as good as diphenhydramine<br />
– Most potent OTC sedative/sleep aid (better than barbiturates!)<br />
• Clemastine (Tavist®):
BIMM118<br />
H1-Antagonists (“Antihistamines”)<br />
First generation drugs:<br />
• Chlorpheniramine (Chlor-Trimeton®):<br />
– Also anti-depressant (inhibits serotonin re-uptake)<br />
• Meclizine (Dramamine II®):<br />
– Antiemetic: Less drowsiness than original Dramamine<br />
• Hydroxyzine (Atarax®):<br />
– Antihistamine action due to metabolite: Cetirizine<br />
Second generation drugs:<br />
• Cetirizine (Zyrtec®):
BIMM118<br />
H1-Antagonists (“Antihistamines”)<br />
Second generation drugs:<br />
• Loratadine (Claritin®):<br />
– Does not enter CNS => NO drowsiness!<br />
– t1/2=8h => Active metabolite: Desloratadine (t1/2=28h)<br />
• Desloratadine (Clarinex®):<br />
• Fexofenadine (Allegra®):<br />
– Highly selective for H1-Receptor<br />
– $ 2B in sales/year !!
BIMM118<br />
Mast Cell Stabilizers<br />
• Cromolyn=Cromoglycate (Intal®, Nasalcrom®):<br />
– Only prevents asthma, but can NOT stop an attack in progress<br />
– Acts by preventing mediator release from mast cells (likely by<br />
preventing Ca++ influx)<br />
– Usually applied via inhalation or as eye drops<br />
• Nedocromil (Tilade®):
BIMM118<br />
Allergy - Leukotrienes<br />
Leukotrienes:<br />
Generated by 5-Lipoxygenase:<br />
Converts AA into 5-HPETE, which in turn is converted into<br />
– LTB4: potent mediator of inflammation<br />
and<br />
– Cysteinyl-LTs (LTC4, LTD4, LTE4 = SRS-A): mediate asthmatic responses<br />
• Physiological actions:<br />
– LTB4:<br />
• Mediated by specific LTB4 receptor<br />
• Adherence, chemotaxis and activation of macrophages<br />
• Stimulates cytokine and chemokine production<br />
• Present in inflammatory exsudates (RA, ulcerative colititis, psoriasis)<br />
– Cys-LTs:<br />
• Mediated by shared receptor for LTC4, LTD4 and LTE4<br />
• Contraction of bronchial muscles (longer lasting than histamine)<br />
• Peripheral vasodilation, coronary vasoconstriction<br />
• Found in sputum of chronic bronchitis, asthmatic lung; lavage of allergic rhinitis
BIMM118<br />
Allergy - Leukotrienes<br />
Cys-LTs-R antagonists:<br />
Used as add-on therapy for mild to moderate asthma:<br />
• Prevent exercise and aspirin-induced asthma<br />
• Decrease response to allergens<br />
• Montelukast (Singulair®):<br />
– Oral application<br />
– t1/2=5h<br />
• Zafirlukast (Accolate®):<br />
– Oral application<br />
– t1/2=10h<br />
LTB4
BIMM118<br />
5-Lipoxygenase inhibitor:<br />
• Zileuton (Zyflo®):<br />
– Only approved LO inhibitor<br />
– Prevents production of all LTs<br />
– Not useful for treatment of attacks<br />
Allergy - Leukotrienes
BIMM118<br />
Drugs Targeting the CNS<br />
• Hypnotics/Anxiolytics<br />
• Antidepressants<br />
• Neuroleptics<br />
• Parkinson<br />
• Epilepsy
BIMM118<br />
Neurotransmitters in the CNS<br />
• Norepinephrine:<br />
– Excitory or inhibitory<br />
Drugs Targeting the CNS<br />
– Targeted by: MAO inhibitors (); tricyclic antidepressant (); amphetamines ()<br />
• Acetylcholine:<br />
– Excitory (M1; N) or inhibitory (M2)<br />
– Targeted by: M inhibitors (); Acetylcholine-esterase inhibitors ()<br />
• Glutamate:<br />
– Excitory<br />
– Targeted by: antiepileptics, ketamine, phencyclidine ()<br />
• GABA (γ-amino-butyric acid):<br />
– Inhibitory (increases g Cl - and g K +, but not g Na + => hyperpolarization (higher threshold for<br />
activation<br />
– Targeted by: hypnotics, sedative, anti-epileptics ()<br />
• Dopamine:<br />
– Inhibitory<br />
– Targeted by: older neuroleptics (); anti-parkinson drugs, amphetamines ()<br />
• Serotonin:<br />
– Excitory or inhibitory<br />
– Targeted by: MAO inhibitors, SSRIs, Tricyclic antidepressants, hallucinogens ()
BIMM118<br />
Drugs Targeting the CNS<br />
Glutamate<br />
• Excitatory amino acid:<br />
– Uniformly distributed throughout the brain<br />
– Mainly derived from glutamine or glucose<br />
– Stored in synaptic vesicles<br />
– Four distinct receptors exist -<br />
(NMDA receptor subtype most significant for drug action: needs to be<br />
“co-occupied” by glycine to become activated)<br />
– Termination mainly by re-uptake into nerve terminal and astrocytes<br />
– Astrocytes convert it to glutamine (lack activity) and return it to nerve cells
BIMM118<br />
Drugs Targeting the CNS<br />
GABA (γ-amino-butyric acid)<br />
• Inhibitory amino acid:<br />
– Only found in the brain<br />
– Mainly derived from glutamate via glutamic acid decarboxylase (GAD)<br />
– Stored in synaptic vesicles<br />
– Two distinct receptors exist - GABA A and GABA B<br />
(GABA A receptor subtype most significant for drug action: mostly post-synaptic:<br />
Cl - - influx hyperpolarizes the cell => inhibitory)<br />
– Termination mainly by deamination (GABA transaminase)
BIMM118<br />
Dopamine<br />
• Inhibitory amino acid:<br />
– Precursor to (nor)epinephrine<br />
Drugs Targeting the CNS<br />
– Termination mainly by reuptake (dopamine transporter - inhibited by Cocaine)<br />
and metabolism via MAO B and COMT<br />
– Two distinct receptor groups exist (coupled to heterotrimeric G proteins):<br />
D 1 -group (D 1 ,D 5 : stimulate Adenylate cyclase: CNS, renal arteries)<br />
D 2 -group (D 2 ,D 3, D 4 : inhibit Adenylate cyclase: CNS)<br />
– Three main dopaminergic pathways:<br />
• Nigrostriatal (substantia nigra): motor control (Parkinson’s disease)<br />
• Mesolimbic/mesocortical: emotion and reward system<br />
• Tuberohypophysal: from hypothalamus to pituitary<br />
• (Medulla oblongata: Vomiting center: D2 receptors)<br />
– Schizophrenia: increased dopamine levels and<br />
D 2 receptors
BIMM118<br />
Drugs Targeting the CNS<br />
5-Hydroxytryptamine (5-HT = Serotonin)<br />
• Excitatory or Inhibitory amino acid:<br />
– Generated from tryptophane<br />
– Termination mainly by reuptake and MAO B<br />
– Seven distinct receptor types exist (7-TM):<br />
5-HT 1 group (CNS, blood vessels) (cAMP)<br />
5-HT 2 group (CNS, blood vessels) (IP 3 /DAG)<br />
5-HT 3 group (peripheral nervous system)<br />
5-HT 4 group (enteric nervous system)<br />
– Main functions:<br />
• Intestine: increases motility<br />
• Blood vessel: constriction (large vessels)<br />
dilation (arterioles)<br />
• Nerve ending: triggers nociceptive receptors<br />
5-HT injection causes pain<br />
(5-HT found in nettle stings)<br />
• Neurons: excites some neurons, inhibits others<br />
inhibition mostly presynaptic (inhibit transmitter release)<br />
LSD = agonist of 5-HT 2A receptor
BIMM118<br />
Drugs Targeting the CNS<br />
Sites of drug action in the CNS:
BIMM118<br />
Anxiety:<br />
Drugs Targeting the CNS<br />
Panic disorder (panic attacks) - rapid-onet attacks of extreme fear and feelings of heart<br />
palpitations, choking and shortness of breath.<br />
Phobic anxiety is triggered by a particular object, for example; spiders,<br />
snakes, heights, or open spaces.<br />
Obsessive-compulsive disorder - uncontrollable recurring anxiety-producing thoughts and<br />
uncontrollable impulses (compulsive hand-washing, checking that doors are locked: “Monk”)<br />
Generalized anxiety disorder - extreme feeling of anxiety in the absence<br />
of any clear cause<br />
Post-traumatic stress disorder (PTSD) - recurrent recollections of a<br />
traumatic event of unusual clarity which produce intense psychological distress.
BIMM118<br />
Hypnotics / Anxiolytics<br />
Barbiturates<br />
– Derivatives of barbituric acid<br />
– Hypnotic/anxiolytic effect discovered in the early 20th century (Veronal®, 1903)<br />
– Until the 60s the largest group of hypnotics (more hypnotic than anxiolytic)<br />
– Act by both enhancing GABA responses and mimicking GABA (open Cl-channels<br />
in the absence of GABA) => increased inhibition of the CNS (also block<br />
glutamate receptors)<br />
– High risk of dependence (severe withdrawal symptoms)<br />
– Strong depressent activity on the CNS => anesthesia<br />
– At higher doses respiratory (inhibit hypoxic and CO 2 response of<br />
chemoreceptors) and cardiovascular depression =><br />
very little use today as hypnotics (only for epilepsy and anesthesia)<br />
– Potent inducers of the P450 system in the liver => high risk of drug interactions<br />
(oral contraceptives)
BIMM118<br />
Hypnotics / Anxiolytics<br />
Barbiturates<br />
Different barbiturates vary mostly in their duration of action<br />
• Phenobarbital<br />
– Long-acting: used for anticonvulsive therapy<br />
• Thiopental<br />
– Very short acting (very lipophilic => redistributed from the brain into the fat tissue<br />
=> CNS concentration falls below effective levels: used for i.v. anesthesia<br />
• Amobarbital<br />
• Pentobarbital<br />
• Secobarbital
BIMM118<br />
Hypnotics / Anxiolytics<br />
Benzodiazepines<br />
– Derivatives of Benzodiazepin<br />
– Valium (diazepam) in 1962<br />
– Characteristic seven-membered ring fused to aromatic ring<br />
– Selectively activates GABA receptor operated<br />
chloride channels (bind to the benzodiazepin<br />
receptor which is part of the GABA-receptor/<br />
chloride channel complex)<br />
– Increase the affinity of GABA for its receptor<br />
– Used to treat anxieties of all kinds (phobias,<br />
preoperative anxiety, myocardial infarction<br />
(prevent cardiac stress due to anxiety…)<br />
– Significantly fewer side effects than barbiturates<br />
=> much safer => more widespread use<br />
– Cause anterograde amnesia (useful<br />
for minor surgeries)
BIMM118<br />
Benzodiazepines<br />
Hypnotics / Anxiolytics<br />
Different benzodiazepines vary mostly in their duration of action<br />
• Chlordiazepoxide (Librium®)<br />
– introduced in 1960, first benzodiazepine<br />
• Diazepam (Valium®), Clonazepam,<br />
– Strongly anticonvulsive => therapy of status epilepticus<br />
• Lorazepam<br />
• Flunitrazepam (Rohypnol®)<br />
– Known as “date-rape drug”, “roofie”<br />
– Color- and tasteless,<br />
– Disinhibiting effect (particularly with EtOH), amnesia !<br />
– Death unlikely, but high risk of dependence<br />
• Alprazolam<br />
– Has also antidepressive properties<br />
• Triazolam<br />
– Causes paradoxical irritability (=> withdrawn in the UK)<br />
Alprazolam
BIMM118<br />
Antidepressants<br />
Clinical Depression<br />
Characterized by feelings of misery, guilt, low self-esteem without cause<br />
Lack of motivation, missing drive to act<br />
Mania: opposite symptoms<br />
Unipolar depression: Depressive phase only<br />
Bipolar disorder: Depression alternates with mania<br />
“Amine hypothesis of depression”:<br />
States that a functional decrease in brain norepinephrine and/or serotonin is<br />
responsible for the disorder (maybe over-simplified, BUT =><br />
Most anti-depressive drugs facilitate the activity of these brain amines<br />
• Several drug classes<br />
– MAO inhibitors<br />
– Tricyclic antidepressants (TCAs)<br />
– Selective Serotonine Reuptake Inhibitors (SSRIs)<br />
– Misc. Heterocyclic antidepressants<br />
– Lithium (bipolar disorder only)
BIMM118<br />
MAO Inhibitors:<br />
Antidepressants<br />
– Increase levels of norepinephrine, serotonin and dopamine by preventing their<br />
metabolism<br />
– Use is declining due to side effects (can cause fatal hypertensive crisis) =><br />
Last choice of treatment today (only if other drugs fail)<br />
– Possibility of severe food-drug interaction (“cheese reaction”: Tyramine is usually<br />
metabolized and inactivated in the gut by MAOs. MAO-inhibition allows for<br />
uptake of tyramine, which displaces norepinephrine in the storage vesicles =><br />
NE released => hypertension and cardiac arrhythmias.<br />
• Tranylcypromine<br />
• Phenelzine
BIMM118<br />
Tricyclic antidepressants:<br />
Antidepressants<br />
– Increase levels of norepinephrine and serotonin by preventing their neuronal<br />
reuptake => extended duration of post-synaptic effects<br />
– Strong interaction with alcohol<br />
– Side effect: Sedation (H1-block)<br />
• Imipramine<br />
• Desipramine<br />
• Clomipramine<br />
• Amitriptyline<br />
• Nortriptyline
BIMM118<br />
Antidepressants<br />
Selective Serotonin Reuptake Inhibitors (SSRIs):<br />
– Increase levels of serotonin specifically by preventing their neuronal reuptake =><br />
extended duration of post-synaptic effects<br />
– Same efficacy as TCAs, but fewer side effects<br />
– Main side effect: inhibition of sexual climax<br />
– Rare, but severe side effect: aggression, violence<br />
• Fluoxetine (Prozac®)<br />
Most widely prescribed antidepressant<br />
Sales exceed 1 bill. $ / year<br />
• Paroxetine (Paxil®)<br />
• Sertraline (Zoloft®)<br />
• Clotalopram (Celexa®)
BIMM118<br />
Schizophrenia<br />
Endogenous psychosis characterized by:<br />
Neuroleptics<br />
Positive symptoms: thought disorder (illogical, incoherent, garbled sentences),<br />
mood inappropriation, paranoia (persecution mania) and hallucinations (voices)<br />
and<br />
Negative symptoms: withdrawal from society, flattened emotional responses, defect<br />
in selective attention (can’t distinguish between important and insignificant)<br />
Affects up to 1% of population, high suicide rate (10%)<br />
Amphetamines promote dopamine release => mimic schizophrenia<br />
“Dopamine hypothesis of schizophrenia”:<br />
States that a functional increase in brain dopamine is responsible for the disorder.<br />
In addition, 5-HT might play a role, possibly by modulating dopamine responses.<br />
Anti-psychotic drugs act as dopamine D2 (and 5-HT) receptor blockers<br />
• Several drug classes<br />
– Typical (older, pre-1980s) neuroleptics: phenothiazines, butyrophenones<br />
relieve mostly positive symptoms<br />
– Atypical (newer) neuroleptics: fewer extrapyramidal side effects<br />
relieve both positive and negative symptoms
BIMM118<br />
Classical neuroleptics:<br />
Phenothiazines<br />
• Chlorpromazine<br />
• Triflupromazine<br />
• Fluphenazine…<br />
Butyrophenones<br />
• Haloperidol<br />
• Trifluperidol<br />
• Spiroperidol<br />
Neuroleptics
BIMM118<br />
Classical neuroleptics:<br />
Adverse effects:<br />
Neuroleptics<br />
– Mostly extensions of dopamine-receptor antagonism (extrapyramidal effects due<br />
to dopamine blockage in the striatum):<br />
• Acute dystonia: Motor impairment, involuntary movements of face, tongue, neck..<br />
(reversible; develops immediately after start of treatment)<br />
• Akathesia (Pseudo-Parkinsonism): motor restlessness, rigidity, tremor<br />
(reversible; develops days to month after start of treatment)<br />
• Tardive Dyskinesia: involuntary movements of most body parts (head, lips, limbs..)<br />
– Sedation (results from H1-receptor blockage)<br />
(irreversible; develops after extended treatment in 20-40% of<br />
patients) - main problem of classical neuroleptic therapy<br />
– Also block muscarinic cholinergic and α-adrenergic receptors (=> dry mouth,<br />
constipation, urinary retention)<br />
– Lactation (dopamine suppresses prolactin release)<br />
– Strong interaction with alcohol
BIMM118<br />
Atypical neuroleptics:<br />
– Inhibit 5-HT and D2 receptors<br />
Neuroleptics<br />
– Act predominantly in the limbic system, but not in the striatum => fewer<br />
extrapyramidal side effects (might also be due to adrenergic receptor blockage)<br />
• Clozapine<br />
– Can cause agranulocytosis<br />
(=> strict monitoring required)<br />
• Olanzapine<br />
– Same efficacy as Clozapine, but no agranulocytosis<br />
• Risperidone<br />
• Olanzapine
BIMM118<br />
Pathology:<br />
Parkinson’s Disease<br />
• Loss of dopaminergic neurons in the Pars compacta of the Substantia nigra<br />
• The excitatory influence of ACh becomes unopposed => movement disorders<br />
(tremor, muscle stiffness, slow movements, and difficulty walking)<br />
• Symptoms: stooped and rigid posture, shuffling gait, tremor, a masklike facial<br />
appearance, and "pill rolling"
BIMM118<br />
Pathology:<br />
Parkinson’s Disease<br />
• Loss of dopaminergic suppression of the cholinergic neurons in the striatum =><br />
increased GABA output to the thalamus => suppression of stimulating input into the<br />
motor cortex => movement disorder<br />
• Treatment strategies: Dopamine replacement<br />
Dopamine agonists<br />
Cholinergic antagonists (Atropine - see Lecture 6)
BIMM118<br />
Dopamine replacement:<br />
Parkinson’s Disease<br />
Dopamine does not cross blood-brain barrier => use of<br />
• Levodopa (L-Dopa)<br />
– Metabolic precursor of dopamine<br />
– High concentrations required, as most of L-Dopa is decarboxylated in the<br />
periphery => high concentration of peripheral dopamine => side effects!<br />
– L-Dopa combined with<br />
• Carbidopa<br />
– L-Dopa decarboxylase - inhibitor<br />
– Does not cross blood-brain barrier =><br />
only peripheral effect => increases the amount<br />
of L-Dopa that reaches the brain
BIMM118<br />
Dopamine agonists:<br />
Parkinson’s Disease<br />
Actions and side effects similar to L-Dopa<br />
• Bromocriptine<br />
– Derived from ergot alkaloids<br />
– Potent D2 agonist<br />
– Initially used to treat galactorrhoea (inhibit Prl release)<br />
• Pergolide<br />
• Pramipexole<br />
Indirect dopamine agonists:<br />
• Selegiline<br />
– Inhibitor of MAO B (mostly in the CNS => few peripheral side effects, e.g. cheese<br />
reaction etc.)<br />
– Extends half-life of dopamine
BIMM118<br />
Pathology:<br />
Epilepsy<br />
– Group of disorders characterized by excessive excitability of neurons within the<br />
central nervous system (CNS)<br />
– Characteristic syptom is seizure<br />
– ~0.5% of population is affected<br />
Classification:<br />
– Simple (patient remains conscious, often involves brain lesions) or complex<br />
(patient looses consciousness)<br />
– Partial (only localized brain region is affected) or generalized<br />
Generalized seizures are devided into:<br />
• Tonic clonic seizures (grand mal): strong contraction of entire musculature<br />
=> rigid spasm, often accompanied by salivation, defaecation and<br />
respiratory arrest. Tonic phase is followed by series of violent jerks, which<br />
slowly die out in a few minutes<br />
• Absence seizures (petite mal): often in children. Less dramatic, but more<br />
frequent (several seizures/day): patient stops abruptly what (s)he was doing<br />
and “spaces out”
BIMM118<br />
Epilepsy<br />
Treatment strategies:<br />
Enhancement of GABA action<br />
Mostly for partial and generalized convulsive seizures (not effective in absence seizures)<br />
• Carbamazepine<br />
– Benzodiazepine => increases Cl - -influx in response to GABA => counteracts<br />
depolarization<br />
• Tiagabin<br />
– Prevents GABA re-uptake<br />
Inhibition of sodium channels<br />
• Phenytoin<br />
– Blocks voltage-gated Na + -channels in the inactivated (refractory) state => preferential<br />
inhibition of high-frequency discharges<br />
(very limited effect on normal frequency excitation<br />
= “use-dependent inhibition”)<br />
– Eliminated following zero-order kinetics<br />
– Used for convulsive seizures (not effective in<br />
absence seizures)<br />
– gingival hyperplasia (fairly high percentage)
BIMM118<br />
Treatment strategies:<br />
Inhibition of calcium channels<br />
• Ethosuximide<br />
– Blocks T-type channels<br />
– Drug of choice for absence seizures<br />
• Valproate<br />
Epilepsy<br />
– Exact mechanism unclear (causes GABA increase in the brain)<br />
– Useful for convulsive and absence seizures<br />
– Teratogenic<br />
– Hepatotoxic (elevated liver enzymes, even fatal hepatic failure)
BIMM118<br />
Glycine receptor antagonist<br />
Glycine:<br />
– Non-essential amino acid<br />
Strychnine<br />
– Major inhibitory neurotransmitter (similar to GABA)<br />
– Binds NMDA receptor (not strychnine sensitive)<br />
– Glycine receptor (Cl - ion channel) - binding is Strychnine sensitive<br />
Strychnine:<br />
– Main alkaloid in Strychnos nux-vomica seeds<br />
– Among the most bitter substances known<br />
– Poisoning causes most severe muscle spasm (“arching”):<br />
Convulsions progress to death by asphyxiation (LD 50 =10mg)<br />
(Considered one of the most painful deaths: horrific seizures without losing consciousness)<br />
– Popular use as a rodent pesticide<br />
– Antidotes: Anticonvulsants (Diazepines)<br />
Muscle relexants
BIMM118<br />
Ethanol<br />
Most widely consumed “drug”:<br />
1 drink = ~ 8-12g ethanol (= 0.17-0.26 mole) =><br />
not unusual to consume >1mole/session<br />
(equivalent to ~ 0.5 kg of most other drugs)<br />
• Biological effects<br />
Resembles actions of general, volatile anesthetics<br />
Acts on many different levels:<br />
– Low concentrations:<br />
• enhancement of excitatory effects of N-ACh and 5-HT 3 receptors =><br />
agitation<br />
– Higher concentrations:<br />
• Inhibition of neurotransmitter release by blocking Na + and Ca 2+ channels<br />
• Inhibition of NMDA receptor function<br />
• Enhancement of GABA-mediated inhibition (similar to benzodiazepines)<br />
Peripheral effects:<br />
• Cutaneous vasodilation (heat loss!!)<br />
• Increased salvary and gastric secretion (=> hunger)<br />
• Increased glucocorticoid release<br />
• Inhibition of anti-diuretic hormone (ADH) secretion => diuresis<br />
• Inhibition of Oxytocin release (=> delay of labor induction)
BIMM118<br />
• Alcoholism<br />
– Long-term effect:<br />
Ethanol - Alcoholism<br />
– Liver damage: increased fat accumulation due to increased “stress” => increased release of<br />
fatty acids from fat tissue, and impaired fatty acid oxidation due to “metabolic competition”<br />
– Chronic malnutrition (ethanol satisfies the<br />
– Addiction:<br />
“caloric requirement”, but no vitamins etc.)<br />
– Alcohol use linked to endorphine system (AA Wistar rats more sensitive to endorphine<br />
release after alcohol consumption => proned to alcoholism)<br />
– Endorphines are part of the bodies “reward system” =>re-inforced behavior<br />
– Withdrawal:<br />
– Long-term alcohol use leads to reduced GABA levels<br />
– Abrupt stop of alcohol consumption => lack of GABA input =><br />
Seizures, halluzinations, tremor, convulsions, “Delirium tremens”<br />
– More than 15 mill. Americans are considered Alcoholics !!!
BIMM118<br />
Treatment strategies:<br />
• Disulfiram (Antabuse®)<br />
– Blocks Aldehyde-dehydrogenase =><br />
Ethanol - Alcoholism<br />
accumulation of Acetaldehyde after alcohol consumption:<br />
nausea, vomiting,”hang-over”<br />
– Also inhibits dopamine-hydroxylase =><br />
blocks dopamine->NE conversion =><br />
rise in dopamine: schizophrenic symptoms<br />
• Naltrexone (“Sinclair Method”)<br />
– Opioid receptor antagonist<br />
– Prevents the “reward response”<br />
– Patient is allowed to consume alcohol in usual setting =><br />
BUT: urge to drink diminishes over time<br />
– Very simple and successful (~80%) regimen
BIMM118<br />
Drugs against Pain<br />
• Anesthesia<br />
• Narcotic Analgetics<br />
• Local Anesthetics<br />
• NSAIDs
BIMM118<br />
General Anesthetics<br />
State of drug-induced absence of perception of all sensations:<br />
Unconciousness, analgesia, amnesia and muscle relaxation<br />
General anesthesia is usually induced with intravenous anesthetics,<br />
and maintained with inhalation anesthetics<br />
1846 - first surgery under ether-anethesia; 1847 - introduction of chloroform<br />
Originally, anesthesia was achieved with a single agent (e.g ether, nitrous oxide).<br />
However, to satisfy all four anesthesia requirements with one agent necessitates<br />
high dosage => increased risk of suppression of vital functions.
BIMM118<br />
General Anesthetics<br />
Inhalation anesthetics:<br />
• Very diverse drugs: ether, nitrous oxide, halogenated hydrocarbons<br />
• Mechanism of action largely unknown (probably inhibition of glutamate receptors and<br />
increased activity of GABA receptors)<br />
• Actions are affected by cardiac output and ventilation rate<br />
• Elimination predominantly through exhalation of the unchanged gas<br />
Potency and speed of induction/recovery depend on two properties of the anesthetic:<br />
• Solubility in blood (blood:gas partition coefficient)<br />
– Speed of onset is inversely correlated with the solubility in blood (more soluble => slower<br />
onset): blood acts as a reservoir that “needs to be filled”<br />
• Solubility in lipid (oil:gas partition coefficient)<br />
– Determines the potency of the anesthetic<br />
– Minimal alveolar concentration (MAC)<br />
= alveolar concentration at 1 atm that produces immobility<br />
in 50% of the patients exposed to a painful stimulus<br />
(usually expressed in Vol%)<br />
– More lipophilic anesthetics have higher potency<br />
– Lipophilic anesthetics gradually accumulate in body fat<br />
=> prolonged “hang-over”
BIMM118<br />
General Anesthetics<br />
Inhalation anesthetics:<br />
• Ether<br />
– Obsolete (except in underdeveloped regions)<br />
– Slow onset and recovery<br />
– Post-operative nausea, vomiting<br />
– Highly explosive<br />
• Nitrous oxide<br />
– Low potency (must be combined with other agents)<br />
– Rapid induction and recovery<br />
– Good analgesic properties<br />
• Halothane<br />
– Widely used agent<br />
– Potent, non-explosive and non-irretant<br />
– 30% metabolized in liver<br />
=> repeated use can cause liver damage<br />
– No analgetic properties<br />
– Causes hypotension (vasodilation, cardio-suppression)
BIMM118<br />
General Anesthetics<br />
Inhalation anesthetics:<br />
• Enflurane<br />
– Similar to halothane<br />
– Less metabolized => smaller risk of liver damage<br />
• Isoflurane<br />
• Desflurane<br />
• Sevoflurane
BIMM118<br />
General Anesthetics<br />
Intravenous anesthetics:<br />
• Thiopental<br />
– Barbiturate with very high lipid solubility<br />
– Rapid action, but accumulates in fat with extended use<br />
– No analgesic effect<br />
– Narrow therapeutic range<br />
• Propofol<br />
– Rapidly metabolized => quick recovery<br />
– Drug of choice for day-case surgery<br />
– Used as continuous infusion<br />
• Ketamine<br />
– Phencyclidine analogue<br />
– Good analgesia and amnesia<br />
– High incidence of hallucinations during recovery<br />
• Midazolame<br />
– Benzodiazepine
BIMM118<br />
General Anesthetics<br />
Modern anesthesia:<br />
Employs a combination of drugs to achieve the goals of a “balanced anesthesia”:<br />
– Anxiolytic premedication (Diazepines)<br />
– Autonomic stabilization (Atropin: prevents visceral reflexes)<br />
– Analgetics (Opioids: Fentanyl)<br />
– Muscle relaxant (Pancuronium)
BIMM118<br />
Opioid Analgesics<br />
Opiates:<br />
– Alkaloids derives from Papaver somniferum<br />
– Already used 4000 B.C. (opius greek: “little juice”)<br />
– 1805: Morphine isolated (morpheus: Greek god of dreams)<br />
– 1874: synthesis of heroin (introduced in 1898 by Bayer as a cough medicine)<br />
– Opium tincture heavily used during civil war<br />
– Opiates freely available in the US until 1914<br />
– 1914: Harrison Act<br />
Prevented physicians from maintaining addiction
BIMM118<br />
Opioid Analgesics<br />
Opiates:<br />
– Act through receptors (7TM, coupled to Gα i or ion-channels) for endogenous opioids:<br />
Enkephalins, endorphines,…<br />
– Reduce cAMP, but countereffect: upregulation of adenylate cyclase => tolerance<br />
Endorphine Morphin<br />
– Three receptor subtypes:<br />
• mu (µ): account for most of the morphin effects<br />
• delta (δ): mediate reduced GI motility and respiratory suppression (in addition to µ)<br />
• kappa (κ): mediate dysphoria and contribute to sedation, weak analgesic effect<br />
– Most opiods are full agonists for all receptors<br />
(exception: Pentazocine, buprenorphine, which are mixed a(nta)gonists based on receptor type)
BIMM118<br />
Opiates:<br />
Mechanism of analgesic action:<br />
Opioid Analgesics<br />
– Spinal analgesia:<br />
Activation of presynaptic opioid receptors => decreased Ca ++ flux => decreased<br />
neurotransmitter (Substance P) release => decreased transmission of pain signal from<br />
nocireceptors<br />
– Supraspinal analgesia:<br />
Activation of postsynaptic opioid receptors in the medulla and midbrain => increased K +<br />
flux => hyperpolarization => inhibition of neurons in the pain pathway<br />
– Oral opioids are subject to first-pass<br />
elimination => low oral bioavailability<br />
– Morphine is metabolized and eliminated<br />
via glucuronidation<br />
– Heroin, Fentanyl: very lipophilic =><br />
rapid accumulation in the CNS
BIMM118<br />
Opiates:<br />
Morphine:<br />
– CNS:<br />
– Eyes:<br />
• Sedation and drowsiness<br />
Opioid Analgesics<br />
• Nausea (direct stimulation of the chemoreceptor trigger zone)<br />
• Cough suppressant (suppressive effect on medulla; independent of analgesic effect)<br />
• Pupillary constriction (stimulate parasympathetic portion of the oculomotor nucleus)<br />
– Respiratory system:<br />
• Strongly suppressive on all phases (frequency; volume)<br />
• Also depression of hypoxic drive<br />
– GI:<br />
• Increases resting tone of the smooth muscle of the entire GI tract => segmentation<br />
• Decreased peristaltic movements, increased sphincter tonus => constipation<br />
– Urinary tract:<br />
• Increased smooth muscle cell tone => urinary retention<br />
Withdrawal symptoms:<br />
– Mostly autonomic hyperactivity: diarrhea, vomiting, chills, cramps, pain…
BIMM118<br />
Codeine (3-methoxy-morphine):<br />
Opioid Analgesics<br />
– Better oral absorption than morphine<br />
– Only 20% of analgesic effect of morphine<br />
(does not increase significanly by increasing the dose)<br />
– Prodrug: Converted into morphine by demethylation via CYP2D6<br />
(mutated in ~10% of the population => resistance to the analgesic effect)<br />
– CYP2D6 inhibitors (e.g. Fluoxetine) reduce efficacy of Codeine<br />
– Little euphoria => rarely addictive<br />
– GI and respiratory effects similar to morphine<br />
(=> codeine and dihydrocodeine are widely used as antitussiva)<br />
Dextromethorphane (DXM):<br />
– Synthetic morphine derivative<br />
– Equally antitussive as codeine<br />
– Does not act through opioid receptors<br />
– No analgesic or GI effects
BIMM118<br />
Heroin (diamorphine):<br />
– Diacetylated morphine<br />
Opioid Analgesics<br />
– Greater lipophilicity => crosses blood/brain barrier better<br />
=> greater “rush”<br />
– Used in UK as analgesic<br />
(~2x more potent than morphine)<br />
Hydrocodone (Vicodin®):<br />
– Often combined with NSAIDs<br />
– Contained in over 200 preparations in the US<br />
Oxycodone (OxyContin®):<br />
– Used in slow-release formulation to treat chronic pain<br />
– People seeking an alternative to heroin often try OxyContin.<br />
They chew the time-release tablets for a quicker high. Some crush the tablet<br />
to snort or inject it. Prescriptions are often obtained fraudulently, and in many<br />
robberies of pharmacies, only Oxycontin is stolen.
BIMM118<br />
Meperidine (Pethidine):<br />
– Actions similar to morphine<br />
Opioid Analgesics<br />
– Much shorter duration => used during labour<br />
Methadone:<br />
– Actions similar to morphine<br />
– Significantly longer duration (t 1/2 = >24 h) => less psychological dependence<br />
– Used to treat morphine and heroin addiction<br />
Etorphine:<br />
– 1000x more potent than morphine, but similar efficacy<br />
– No clinical advantage<br />
– Used to immobilize wild animals (high potency permits small volumes in darts)<br />
Fentanyl:<br />
– High potency (allows use in transdermal delivery systems)<br />
– Short lasting: used in anesthesia and in patient-controlled infusion systems
BIMM118<br />
Opiate antagonists:<br />
• Naloxone:<br />
– Short acting<br />
Opioid Analgesics<br />
– Rapidly reversed opoid-induced analgesia and<br />
respiratory suppression<br />
– No effect if no opioids are present<br />
– Used to treat opiate overdoses and to improve breathing<br />
in newborns whose mothers received opioids<br />
– Induces severe withdrawal symptoms in opioid addicts<br />
• Naltrexone:<br />
– Similar to naloxone, but much longer duration of action<br />
– Used to “protect” detoxified addicts by preventing any<br />
opioid effect if the patient relapses
BIMM118<br />
Mode of action:<br />
Local Anesthetics<br />
– Block generation of action potential by reversibly inhibiting Na + -influx<br />
– Are weak bases (pK=8-9) => mainly ionized at physiological pH<br />
– Act in their ionized form, but penetrate the cell membrane in the non-ionized form<br />
– Preferentially block activated Na + -channels = “Use dependence”<br />
(higher affinity for open/inactivated channel; easier access to open channel)
BIMM118<br />
Mode of action:<br />
Local Anesthetics<br />
• Different nerve fibers show differential sensitivity towards LA:<br />
– High sensitivity:<br />
thin, non-myelinated nerve fibers (sensory roots): Pain, touch,<br />
temperature<br />
– Medium sensitivity:<br />
thin->medium, myelinated nerve fibers (sympathetic nerves): vasomotor,<br />
visceromotor function<br />
– Low sensitivity:<br />
Thick, myelinated nerve fibers (somatic nervous system): motor function
BIMM118<br />
Classification:<br />
Local Anesthetics<br />
• Aromatic part linked by ester or amide bond to basic side chain:<br />
• Esters:<br />
– Inactivated quickly by non-specific esterases in the plasma and tissue<br />
• Amides:<br />
– More stable, longer plasma half-lifes
BIMM118<br />
Classification:<br />
• Cocaine<br />
– First local anesthetic<br />
– Isolated in 1860 from Coca<br />
(Indians, who chewed Coca<br />
leaves for their psychotropic<br />
effects, knew about the numbing<br />
effect they produced on the mouth<br />
and tongue)<br />
• Procaine<br />
– First synthetic local anesthetic<br />
• Many more …caines today<br />
Local Anesthetics
BIMM118<br />
Clinical use and<br />
Administration:<br />
– LA often combined<br />
with vasoconstrictors<br />
to extend duration of<br />
action (also to<br />
minimize bleeding)<br />
Local Anesthetics
BIMM118<br />
NSAIDs<br />
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):<br />
• Act by inhibiting CycloOXygenases (COX) => no PG production<br />
– COX-1: Constitutively expressed => house-keeping function<br />
– COX-2: Induced by pro-inflammatory factors (TNFα, IL-1)<br />
– COX-3: Just recently discovered<br />
• PGs do not cause pain, but sensitize nocireceptors to stimulation<br />
(e.g. by 5-HT, Bradykinine, capsaicin, …)<br />
• IL-1 release from activated macrophages (bacteria, etc.) induces COX-2 in<br />
the brain => PG E produced => affects thermoregulation => fever<br />
=> NSAIDs have anti-pyretic effects<br />
• Classical NSAIDs: inhibit both COX-1 and COX-2 (inhibition is reversible,<br />
with the exception of Aspirin) => housekeeping PGs reduced => side<br />
effects (gastrointestinal, bronchospasms,…)<br />
• 2nd generation NSAIDs: COX-2 specific => only the inflammatory response<br />
is inhibited => fewer side effects
BIMM118<br />
NSAIDs<br />
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):<br />
• Aspirin (= Acetyl-Salicylic Acid = ASA)<br />
– Oldest NSAID<br />
– Irreversible, non-selective COX inhibitor<br />
(causes acetylation of COX)<br />
– Can cause Reye’s Syndrome in children:<br />
(Combined encephalopacy and liver disorder - 20-40% lethality!!)<br />
=> Avoid Aspirin in children<br />
– Anti-rheumatic activity requires high doses =><br />
CNS effects possible (tinnitus, nausea, etc.) =><br />
other NSAIDs have been developed
BIMM118<br />
NSAIDs<br />
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):<br />
• Acetaminophen = Paracetamol (Tylenol®)<br />
– Most commonly used analgesic/antipyretic<br />
– Weak anti-inflammatory activity<br />
– Mechanism still debated (COX-3 inhibitor ??)<br />
– Overdose can produce fatal hepatotoxicity:<br />
at high doses (2-3x max. therapeutic dose), a toxic metabolite is produced that is<br />
conjugated to glutathione in the liver. If glutathione is depleted, metabolites<br />
accumulate => liver necrosis : more than 100 deaths/year in the US !
BIMM118<br />
NSAIDs<br />
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):<br />
• Ibuprofen (Advil®, Motrin®)<br />
• Naproxen (Aleve®)<br />
• Diclofenac (Voltaren®)<br />
• Indomethacine (Indocid®)
BIMM118<br />
COX-2 specific NSAIDs:<br />
• Rofecoxib (Vioxx®)<br />
– Launched in 1999<br />
NSAIDs<br />
– Marketed in 86 countries: 2.5 bill.$ /year<br />
– Recent trial to test Rofecoxib for efficacy in <strong>color</strong>ectal polyps treatment revealed<br />
an increased risk of heart disease (+ 50%) after 18 month continuous use<br />
– Sept. 2004: Merck voluntarily withdrew Vioxx® from the market pending further<br />
investigation.<br />
• Celecoxib (Celebrex®)<br />
– April 2005: FDA required Pfizer to include a “boxed warning” indicating a<br />
potential risk of cardiovascular side effects<br />
• Valdecoxib (Bextra®)<br />
– April 2005: FDA required Pfizer to withdraw Bextra® from the market due to<br />
unfavorable risk vs. benefit profile (mostly already known adverse skin reactions)
BIMM118<br />
Chemotherapeutic Agents<br />
• Antibiotics<br />
• Antifungals<br />
• Antivirals<br />
• Antiprotozoal<br />
• Antihelmintics<br />
• Anticancer drugs
BIMM118<br />
General Aspects:<br />
Antibiotics<br />
• Principle:<br />
inhibit growth of bacteria without harming the host<br />
– Drug must penetrate body tissue to reach bacteria (exception: GI infection)<br />
(unique targets: cell wall, protein synthesis, metabolic pathways…)<br />
– Bacteria targeted must be within the spectrum of the AB<br />
– Drug can be bactericidal or bacteriostatic<br />
– Different agents can be combined for synergistic effect<br />
(Note: not all combinations are useful, e.g. cell wall synthesis inhibitors loose effectiveness<br />
when combined with bacteriostatic drugs)<br />
– Identification of the invasive microorganism necessary for optimal treatment<br />
• General side effect:<br />
Alteration in normal body flora<br />
– GI tract harbors symbiotic bacteria which are killed by AB =><br />
resistant bacteria repopulate the niche = secondary or superinfection<br />
(most common: overgrowth of Clostridium difficile)
BIMM118<br />
Antibiotics<br />
• Resistance:<br />
loss of efficacy of a given AB against a particular strain<br />
– Frequently: Staphylococcus aureus, pseudomonas aeruginosa, mycobacterium<br />
tuberculosii<br />
Acquisition:<br />
– Spontaneous mutation<br />
– Adaption: drug metabolism (β-lactamase); alternative metabolic pathways<br />
– Gene transfer: plasmids (via conjugation and transduction); transposons<br />
Manifestation:<br />
– Microbes may increase manufacture of drug-metabolizing enzymes (penicillins)<br />
– Microbes may cease active uptake of certain drugs (tetracyclines)<br />
– Changes in receptors which decrease antibiotic binding and action<br />
– Microbes may synthesize compounds that antagonize drug actions<br />
– Antibiotic use promotes the emergence of drug-resistant microbes<br />
(especially the use of broad-spectrum antibiotics)<br />
!!! The more ABs are used, the greater the chance of resistance !!!
BIMM118<br />
• Resistance avoided/delayed by:<br />
Antibiotics<br />
– Using AB only when absolutely needed and indicated:<br />
AB often abused for viral infections (diarrhea, flu-symptoms, etc.)<br />
– Starting with narrow-spectrum drugs<br />
– Limiting use of newer drugs<br />
– (Minimizing giving antibiotics to livestock)<br />
– Identifying the infecting organism<br />
– Defining the drug sensitivity of the infecting organism<br />
– Considering all host factors:<br />
site of infection, inability of drug of choice to penetrate the site of infection, etc.<br />
– Using AB combinations only when indicated:<br />
Severe or mixed infections, prevention of resistance (tuberculosis)<br />
Worldwide more than 500 metric tons antibiotics are used anually !!!
BIMM118<br />
Classification:<br />
• Cell wall synthesis inhibitors<br />
Antibiotics<br />
– Beta-lactams (penicillins, cephalosporins, aztreonam, imipenem)<br />
– Poly-peptides (bacitracin, vancomycin)<br />
• Protein synthesis inhibitors<br />
– Aminoglycosides<br />
– Tetracyclins<br />
– Macrolides<br />
– Chloramphenicol<br />
– Clindamycin<br />
• Folate antagonists<br />
– Sulfonamides<br />
– Trimethoprim<br />
• Quinolones
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Bacterial cell wall:<br />
Three types:<br />
• Gram-negative (e.g. E.coli, Salmonella)<br />
– Few peptidoglycan layers<br />
(Lipopolysaccheride)<br />
• Gram-positive (e.g. Staphylococci, Listeria)<br />
– Many peptidoglycan layers<br />
(Lipoteichoic acid)<br />
– Stains w/ crystal-violet/iodine<br />
• Acid-fast positive (Mycobacteria)<br />
– Cell wall contains waxy substance<br />
(Mycolic acid)<br />
– Stain w/ acid fast test (heating required)
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Beta-lactam antibiotics:<br />
1928 - Alexander Fleming observes the antibacterial effects of Penicillin<br />
1940 - Florey and Chain extract Penicillin<br />
Classification:<br />
• Penicillins<br />
– Narrow spectrum – penicillinase sensitive<br />
– Narrow spectrum – penicillinase resistant<br />
– Broad spectrum penicillins<br />
– Extended-spectrum penicillins<br />
• Cephalosporines<br />
• Carbapenems<br />
• Monobactams<br />
• Vancomycin, Bacitracin
BIMM118<br />
Penicillins<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Inhibit transpeptidase required for cross-linking peptidoglycan chains<br />
Also inactivate an inhibitor of an autolytic bacterial enzyme => lysis<br />
Narrow spectrum – penicillinase (= β-lactamase) sensitive<br />
• Benzylpenicillin<br />
– Naturally occuring<br />
– Poor oral availability (sensitive to stomach acid)<br />
=> given by injection<br />
– Active against gram-positive bacteria<br />
• Phenoxymethylpenicillin<br />
– Better oral availability (acid resistant)
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Narrow spectrum – penicillinase (= β-lactamase) resistant<br />
• Methicillin<br />
– Semisynthetic<br />
– Poor oral availability (only parenteral)<br />
– Active against gram-pos bacteria<br />
– Mostly used for Staphylococcus aureus<br />
• Oxacillin<br />
– Good oral availability<br />
• Cloxacillin<br />
• Dicloxacillin
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Broad spectrum – penicillinase (= β-lactamase) sensitive<br />
(= Aminopenicillins)<br />
• Ampicillin<br />
– Semisynthetic<br />
– Good oral availability<br />
– Active against gram-pos and gram-neg bacteria<br />
– Active against enterobacteria<br />
• Amoxicillin<br />
– Excellent oral availability
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Extended spectrum – penicillinase (= β-lactamase) sensitive<br />
(= Carboxypenicillins)<br />
• Carbenicillin<br />
– Semisynthetic<br />
– Poor oral availability<br />
– Active against gram-pos and gram-neg bacteria<br />
– Active against Pseudomonas aeruginosa, Klebsiella<br />
• Ticarcillin<br />
• Mezlocillin<br />
• Pipercillin
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Cephalosporines<br />
Derived from Cephalosporium sp. (same antibiotic mechanism as penicillins)<br />
Cross-allergies with penicillins are common<br />
Some CSs antagonize Vitamin K => bleeding<br />
Some CSs block alcohol oxidation => disulfiram effect<br />
Classified into generations:<br />
• 1-4<br />
• Increasing activity against gram-negative bacterial and anaerobes<br />
• Increasing resistance to destruction by beta-lactamases<br />
• Increasing ability to reach cerebrospinal fluid
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
First generation – β-lactamase sensitive<br />
• Cefazolin<br />
– Naturally occuring<br />
– Active against gram-positive bacteria<br />
• Cephalexin<br />
Second generation – β-lactamase sensitive<br />
• Cefaclor<br />
– Some activity against gram-neg bacteria<br />
• Cefamandole<br />
• Cefoxitin
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Third generation – mostly β-lactamase resistant<br />
• Cefotaxime<br />
– Active against gram-negative bacteria<br />
– Active against Pseudomonas aeruginosa<br />
– Active against enterobacteria, gonococcus<br />
– Penetrates the CNS => used for meningitis<br />
• Ceftriaxone<br />
Fourth generation – mostly β-lactamase restistant<br />
• Cefepime<br />
– Broadest antimicrobial spectrum of any drug<br />
– Used for MDR bacteria and mixed<br />
infections<br />
• Cefpirome
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Beta-lactamase inhibitors<br />
• Clavulanic acid<br />
– Irreversible inhibitor of β-lactamase<br />
– Good oral absorption<br />
– Combined with amoxicillin or ticarcillin<br />
• Sulbactam
BIMM118<br />
Antibiotics - Cell wall synthesis inhibitors<br />
Vancomycin<br />
• Only effective against gram-positive bacteria<br />
• Poor oral absorption => used for GI infections<br />
• Used to be the “Magic bullet” for methicillin-resistant<br />
staphylococci, but now staph are becoming V-resistant.<br />
• Dose-related ototoxocity:<br />
Tinnitus, high-tone deafness; can progress to total deafness<br />
Bacitracin<br />
• Mixture of polypeptides<br />
• Serious nephrotoxicity => only topical use
BIMM118<br />
Antibiotics - Protein synthesis inhibitors<br />
Protein synthesis inhibitors:<br />
Inhibit either the 30s or 50s ribosomal subunit<br />
(bacterial ribosomal subunits differ from<br />
mammalian ones => drugs are selective<br />
for bacterial protein synthesis)<br />
Class based on chemical structure<br />
of the compounds<br />
Drugs need to enter bacteria =><br />
entry inhibition is a point of drug resistance<br />
• Classification:<br />
– Aminoglycosides (bactericidal)<br />
– Tetracyclins<br />
– Macrolides<br />
– Chloramphenicol<br />
– Clindamycin
BIMM118<br />
Antibiotics - Protein synthesis inhibitors<br />
Aminoglycosides<br />
– Broad spectrum antibiotics (bactericidal)<br />
– Penetration into cell requires an oxygen-dependent transport => anaerobes are<br />
resistant<br />
(Chloramphenicol blocks this transport => inhibits AG uptake into bacteria;<br />
Penicillins weaken the cell wall => promote AG uptake)<br />
– Poor oral absorption (very polar) => parenteral administration<br />
– Narrow therapeutic range - severe side effects:<br />
Ototoxicity: destruction of outer hair cells in organ of Corti<br />
Nephrotoxicity: killing of proximal tubular cells<br />
Neuromuscular toxicity: blockage of presynaptic ACh release => respiratory suppression<br />
– Elimination almost completely by glomerular filtration<br />
(impaired kidney function => concentration of AG increases => toxicity)
BIMM118<br />
Antibiotics - Protein synthesis inhibitors<br />
Aminoglycosides<br />
• Gentamicin<br />
• Tobramycin<br />
• Streptomycin<br />
• Neomycin<br />
• Kanamycin<br />
• Amikacin
BIMM118<br />
Antibiotics - Protein synthesis inhibitors<br />
Tetracyclines<br />
Penetration into cell requires an energy-dependent transport not present in mammals<br />
Oral absorption impaired by food (insoluble chelates with Ca, Mg => caution w/ antacids)<br />
Side effects:<br />
Incorporation into teeth and bone => staining of teeth; retardation of bone growth<br />
(not used in children and during pregnancy)<br />
Photosensitivity<br />
Broad spectrum antibiotics (bacteriostatic)<br />
Also useful for treating rickettsial diseases (Rocky mountain spotted fever), Spirochetes<br />
(Lyme disease), Mycoplasma (pneumonia)
BIMM118<br />
Antibiotics - Protein synthesis inhibitors<br />
Tetracyclines<br />
• Tetracycline<br />
– From Streptomyces sp.<br />
• Oxytetracycline<br />
• Minocycline<br />
• Doxycycline<br />
– Used to treat rosacea and prevent rhinophyma<br />
– No food interaction
BIMM118<br />
Macrolides<br />
Antibiotics - Protein synthesis inhibitors<br />
Narrow spectrum antibiotics similar to penicillin (bacteriostatic or bactericidal)<br />
=> good alternative for patients w/ penicillin allergy<br />
Few side effects (GI disturbances), similar food interaction as tetracyclines<br />
Also used for treating Mycoplasma (pneumonia) and Legionella (Legionnaire’s disease)<br />
• Erythromycin<br />
– From Streptomyces erythreus<br />
• Azithromycin<br />
– Very long half-life (>24 h)<br />
– Convient use (Z-Pak®, Zithromax®) - 6 pill regimen<br />
• Clarithromycin<br />
– Used for H. pylori infection
BIMM118<br />
Antibiotics - Protein synthesis inhibitors<br />
Chloramphenicol<br />
Very broad spectrum (almost all bacteria except Pseudomonas aeruginosa)<br />
Very severe side effects<br />
– Bone marrow depression => fatal aplastic anemia<br />
Reserved for life-threatening, otherwise treatment-resistant infections<br />
Clindamycin<br />
Medium broad spectrum (gram-positive organisms, anaerobes)<br />
Used for treatment of penicillin-resistant cocci<br />
Side effects: Colitis (triggered by toxin from clindamycin-resistant Clostridium difficile =><br />
combined w/ vancomycin to kill C. difficile)
BIMM118<br />
Folate antagonists<br />
Antibiotics - Folate Antagonsits<br />
Bacteria can not absorb folic acid => synthesis from p-amino-benzoic acid (PABA)<br />
required (Folic acid is a vitamin for humans => synthesis pathway is restricted to<br />
bacteria => selective drug target)<br />
Folate antagonsists block folate synthesis => inhibition of nucleotide synthesis =><br />
bacteriostatic effect<br />
(pus provides alternative source for nucleotides => drugs are inactive in the presence<br />
of pus or necrotic tissue)
BIMM118<br />
Sulfonamides<br />
Antibiotics - Folate Antagonists<br />
Structural analogues of PABA => compete with PABA for Dihydropteroate-synthase<br />
Used for infected burns, STDs, toxoplasmosis…<br />
Note:<br />
Many local anesthetics are PABA-esters => they antagonize folate antagonists<br />
• Sulfadiazine<br />
• Sulfadimidine<br />
• Sulfamethoxazole
BIMM118<br />
Trimethoprim<br />
Antibiotics - Folate Antagonists<br />
Resembles pteridine moiety of folates => compete with folates for Dihydrofolatereductase<br />
Use similar to sulfonamides<br />
Combined with Sulfomethoxazole (synergistic effect) = Co-trimoxazole (Bactrim®)<br />
Used for urinary tract infections
BIMM118<br />
Quinolones<br />
Antibiotics - Quinolones<br />
Synthetic inhibitors of DNA-Gyrase (= Topoisomerase II), a bacterial enzyme that<br />
winds and unwinds DNA (required for supercoiling the bacterial genome) =><br />
inhibition of DNA synthesis and transcription<br />
Very broad spectrum, bactericidal - well tolerated<br />
Al and Mg interfer with absorption (antacids!)<br />
Mostly fluorinated = Fluoroquinolones (except nalidixic acid = first quinolone)
BIMM118<br />
Quinolones<br />
• Nalidixic acid<br />
– Oldest quinolone<br />
Antibiotics - Quinolones<br />
– Only used for urinary tract infections<br />
– Improvement through structure-activity relationship:<br />
• Ciprofloxacin<br />
• Adding fluorine at position 6 will significantly increase activity<br />
• Substitution of piperazinyl-ring at position-7 will give the drug antipseudomonal activity<br />
– Most commonly used quinolone (Cipro®)<br />
– Very broad spectrum => used for emergencies<br />
(B. anthracis attacks in 2001)<br />
• Levofloxacin<br />
• Ofloxacin<br />
• Norfloxacin<br />
• Travofloxacin …
BIMM118<br />
Antibiotics - Summary
BIMM118<br />
Chemotherapeutic Agents<br />
• Antibiotics<br />
• Antifungals<br />
• Antivirals<br />
• Antihelmintics<br />
• Antiprotozoal<br />
• Anticancer drugs
BIMM118<br />
Fungal Growth Patterns<br />
• Yeasts<br />
– Unicellular fungi, reproduce by budding<br />
– Moist mucoid or waxy colonies that resemble bacteria<br />
• Molds (=Filamentous Fungi)<br />
– Multicellular filamentous, “fluffy” colonies consisting of branching tubular structures<br />
called hyphae<br />
– Collection of intertwined hyphae called mycelium<br />
– Vegetative hyphae act like roots, penetrating the supporting medium and absorbing<br />
nutrients<br />
– Aerial hyphae project above the surface of the mycelium and bear the reproductive<br />
structures of the mold (often spread through the air)<br />
Aspergillus<br />
Candida albicans
BIMM118<br />
Fungal Growth Patterns<br />
• Dimorphic Fungi<br />
– Grow as molds at ambient environmental<br />
temperatures (e.g. 25˚ C) where they form<br />
reproductive spore structures.<br />
– Spores are aerosolized and infectious<br />
– Inhaled spores grow as yeasts at body<br />
temperature (37˚ C) in the host<br />
Yeast form Mold form<br />
Coccidioides immitis
BIMM118<br />
Fungal Habitats<br />
• Most clinically relevant fungi reside in the soil, in bird feces, on<br />
vegetation, or on the skin and mucous membranes of mammals.<br />
• Some have distinctive ecologic and geographical niches.
BIMM118<br />
Mycosis<br />
• Fungal infections (= mycosis)<br />
– spread generally from the environment to people (or animals) with limited<br />
person-to-person spread.<br />
– Skin and lungs are prominent entry site for many fungi<br />
– Patients with impaired cell-mediated immunity (e.g. AIDS, organ transplant)<br />
at heightened risk for severe disease.<br />
• Types of fungal infections<br />
– Superficial: Outer skin layer - no immune response<br />
caused mostly by yeasts (Dandruff)<br />
– Cutenous: Epidermal layers - evoke immune response<br />
Tinea (Ringworm, Athlete’s foot, jock itch)<br />
caused by Dermatophytes:<br />
– Subcutenous: Chronic infection of subdermal tissues<br />
may require surgical intervention<br />
– Systemic: Mostly originating in the lung<br />
caused by virulent dimorphic fungi<br />
– Opportunistic: In immunocompromised conditions<br />
(AIDS; altered mucosal flora due to antibiotics):<br />
mostly Candidiasis and Aspergillosis (often cause of epidemic death in birds)
BIMM118<br />
Superficial Mycoses<br />
• Tinea versi<strong>color</strong> (= Pityriasis versi<strong>color</strong>)<br />
– Caused by a lipophilic yeast, Malassezia furfur<br />
– Normal flora of skin and scalp<br />
– Growth on media markedly enhanced by adding fat<br />
(Clinical mycology labs routinely stock olive oil!)<br />
• Dandruff (= Scurf = Pityriasis capitis)<br />
– Caused by a lipophilic yeast, Malassezia globosa<br />
– Accellerated shedding of skin cells
BIMM118<br />
Cutaneous Mycosis<br />
– Also known as “ringworm” and tinea (latin “worm”) because of round shape<br />
of lesions<br />
– Infections confined to skin,hair and nails<br />
– Caused by Dermatophyte molds (Trychophytum; Microsporum)<br />
Clinical classification based on location:<br />
• Tinea capitis<br />
– Ringworm of scalp and hair<br />
• Tinea barbae<br />
– Ringworm of beard region
BIMM118<br />
• Tinea corporis<br />
Cutaneous Mycosis<br />
– Ringworm of the smooth skin of the body<br />
• Tinea cruris<br />
– Starts in groin area (“Jock itch”)<br />
– Causes by Trychophytum rubrum
BIMM118<br />
• Tinea pedis<br />
– Classically interdigital (”Athlete’s foot”)<br />
Cutaneous Mycosis<br />
– key risk factor for invasive bacterial<br />
infections in diabetics through disruption<br />
of normal skin barriers<br />
• Tinea unguium<br />
– Infection of finger and toe nails<br />
– Often associated with T. pedis
BIMM118<br />
• Sporotrichosis<br />
Subcutaneous Mycoses<br />
– Sporothrix schenckii - Dimorphic fungus<br />
– Found on vegetation, especially rose bushes<br />
– Introduced into skin by trauma (gardening!)<br />
– Initial ulcer develops into granulomatous nodule
BIMM118<br />
Systemic Mycosis<br />
– Infections are rare (high natural immunity)<br />
– Usually requires large inoculum<br />
– Often endemic to specific aereas<br />
Mostly associated with four fungi:<br />
• Coccidioides immitis -> Coccidioidomycosis<br />
– Soil fungus (dry, dusty soil => inhalation of spores)<br />
– SW USA (Arizona and Central Valley of CA) and Mexico<br />
(“Valley fever”)<br />
– Epidemic after (Northridge) earthquake or sandstorms<br />
– Considered most virulent fungus<br />
(select agent: BSL-3)<br />
– Starts with flu-like symptoms, meningitis<br />
– Striking racial/ethnic differences in rate of dissemination:<br />
Filipinos>African Americans>Hispanics>Asians>Caucasians<br />
(Kern County, Filipinos 0.23% of population but 22% of cases)<br />
Likely due to genetic differences in blood group/ HLA
BIMM118<br />
Systemic Mycosis<br />
• Histoplasma capsulatum -> Histoplasmosis (“Cave disease”)<br />
– Soil fungus (soil containing guano (bird, bat droppings)! => spores inhaled)<br />
(In 1890 European starlings were introduced into Central Park, NYC in an effort to bring all of<br />
the birds mentioned by Shakespeare to the US => Now there are 200M-1B starlings in N.<br />
America, whose droppings are a major route of transmission for histoplasma)<br />
– S-SE USA (Ohio and Mississippi Valley)<br />
– Starts with flu-like symptoms, meningitis<br />
– Fungus lives intracellular in macrophages =><br />
immune-evasion<br />
– 95% of infected individuals asymptomatic<br />
(chronic infection can lead to lung fibrosis)<br />
– In immunecompromised patients systemic infection develops =><br />
multiorgan failure, sepsis
BIMM118<br />
Systemic Mycosis<br />
• Blastomyces dermatitides -> Blastomycosis<br />
– Soil fungus (=> spores inhaled)<br />
– S-SE USA<br />
– Predominantly in lung and skin<br />
• Paracoccidioides brasiliensis<br />
– Soil fungus (=> spores inhaled)<br />
– Central and South America (Brazil—death rate up to 1.5/1000)
BIMM118<br />
Opportunistic Mycosis<br />
– Some fungi are commensal (mucosal flora of mouth, gut, vagina etc.)<br />
– Usually growth balanced by microorganisms (lactobacilli)<br />
– Only a problem in situations of compromised immune responses<br />
(AIDS, antibiotics, chemotherapy, radiation, alcoholism, etc.)<br />
• Candida albicans -> Candidiasis<br />
– Dimorphic fungus BUT also mold at 37˚ C<br />
– Also other Candida species<br />
– Cutanous candidiasis: mostly in moist skin folds (obese patients):
BIMM118<br />
Opportunistic Mycosis<br />
• Candida albicans -> Candidiasis (cont.)<br />
– Oral candidiasis (“Thrush”)<br />
• Babies; denture users<br />
• Can progress into<br />
Candida esophagitis<br />
– Vaginal candidiasis (“Yeast infection”)<br />
• Does NOT require immune dysfunction<br />
• Severe itching/burning<br />
• Commonly associated with antibiotica use<br />
• Bacterial infection often falsly self-diagnosed as candidiasis<br />
(2/3 of self-diagnosed “yeast infections” actually bacterial!)
BIMM118<br />
Opportunistic Mycosis<br />
• Candida albicans -> Candidiasis (cont.)<br />
– Systemic candidiasis<br />
• Mucocutaneous barriers breached in patients after surgery, burns<br />
• Dissemination to kidneys, skin, eye, heart, bone, liver, etc.<br />
• Often fatal !
BIMM118<br />
Opportunistic Mycosis<br />
• Cryptococcus neoformans -> Cryptococcosis<br />
– Ubiquitous, but especially abundant in pigeon droppings<br />
– Cryptococcal meningitis most common manifestation<br />
– Complication in AIDS patients<br />
• Aspergillus sp. -> Aspergillosis<br />
– Mostly pulmonary infections<br />
– Allergenic<br />
(Allergic sinusitis and allergic bronchopulmonary aspergillosis)<br />
– Infections common in birds
BIMM118<br />
Differences between fungi and mammalian cells<br />
ANIMALS FUNGI<br />
Cell structure Eukaryotic Eukaryotic<br />
DNA Diploid Haploid<br />
Ribosomes 80S 80S<br />
Cell wall No chitin, mannans, glucans<br />
Cell membrane Predominantly cholesterol Predominantly ergosterol<br />
Microtubule affinity for griseofulvin No Yes<br />
Cytosine deaminase No Yes<br />
Squalene epoxidase No Yes
BIMM118<br />
Polyenes (Amphotericin, Nystatin)<br />
Azoles (Ketoconazole, Miconazole,<br />
Fluconazole, Itraconazole,<br />
Voriconazole, Posaconazole)<br />
5-Flucytosine<br />
Griseofulvin<br />
Echinocandins (Caspofungin,<br />
Micafungin, Anidulofungin)<br />
Allylamines (Terbinafine)<br />
Overview of Antifungal Drugs<br />
MECHANISM OF ACTION<br />
Selectively bind to ergosterol in fungal cell membrane,<br />
altering membrane fluidity and producing pores and<br />
osmotic cell death. Much less binding to cholesterol.<br />
Selectively block ergosterol synthesis by inhibiting<br />
demethylation of lanosterol. Fungal P450 enzyme much<br />
more sensitive than mammalian counterpart.<br />
Converted by fungal cytosine deaminase into 5-fluorouracil;<br />
inhibits DNA synthesis. Mammalian cells lack cytosine<br />
deaminase.<br />
Inhibit fungal growth by binding to microtubules, disrupting<br />
mitotic spindles. Mammalian microtubules less sensitive.<br />
Inhibit fungal Beta glucan synthesis, disrupting cell wall<br />
integrity. Mammalian cells have no cell walls.<br />
Selectively blocks ergosterol synthesis by inhibiting<br />
squalene epoxidase (not found in animals)
BIMM118<br />
Antifungal Drugs - Polyenes<br />
Polyenes<br />
– bind to fungal membrane sterols (ergosterol)<br />
– alter selectively permeability to K + (and Mg 2+ ) => Fungicidal<br />
– Resistance due to altered sterols<br />
• Amphotericin B<br />
– Isolated from Streptomyces nodosus<br />
– Given iv, it (poor oral absorption) and topical<br />
– Active against most systemic fungi<br />
– iv not well tolerated (chills, headaches, nausea)<br />
– Pronounced renal toxicity =><br />
Encapsulated into liposomes<br />
(less drug reaches the kidneys?)<br />
• Nystatin<br />
– Only for topical application<br />
(Canidida, dermatophytes)
BIMM118<br />
Antifungal Drugs - Azoles<br />
Azoles<br />
– inhibit the synthesis of ergosterol<br />
(block demethylation of lanosterol by inhibiting fungal CYP3A<br />
= 14-demethylase)<br />
– Fungistatic<br />
– Active against systemic fungi and dermatophytes<br />
– Resistance due to altered 14-demethylase<br />
• Two groups<br />
– Imidazoles<br />
– Triazoles
BIMM118<br />
Imidazoles<br />
• Clotrimazole<br />
– Only used topical<br />
– Candidiasis, tinea<br />
Antifungal Drugs - Azoles<br />
• Ketoconazole<br />
– Tinea, candidiasis, blastomycosis, coccidioidomycosis<br />
– Also for dandruff (Nizoral®)<br />
– First oral -azole (mostly replaced by fluconazole and itraconazole)<br />
– Absorption best at low pH (antacids interfer !)<br />
– Does not enter CNS well
BIMM118<br />
Imidazoles<br />
• Miconazole<br />
– Used topical and p.o.<br />
(intestinal fungal infections)<br />
– Also used in E6 slide film processing<br />
• Tioconazole<br />
Antifungal Drugs - Azoles
BIMM118<br />
Antifungal Drugs - Azoles<br />
Triazoles<br />
Newer, less toxic, more effective!<br />
• Fluconazole (Diflucan®)<br />
– Used i.v. and p.o.<br />
– Reaches high CSF concentrations<br />
– 90% excreted unchanged<br />
– t1/2 = 25 hrs<br />
– Used against Candidiasis, Coccoidosis (meningitis)<br />
– Well tolerated<br />
• Itraconazole (Sporanox ®)<br />
– Used i.v. and p.o.(p.o. poor absorption)<br />
– Absorption increased by acids (Orange juice, Coke!)<br />
– Absorption decreased by antacids<br />
– Does not reach CSF<br />
– Highly lipophilic => fatty tissue accumulation<br />
– Very broad spectrum<br />
• Voriconazole (Vfend ®)<br />
– Used for severe systemic infections and emerging fungi (very broad spectrum)<br />
• Posaconazole (Noxafil ®)<br />
– Very broad spectrum (tested against >18,000 fungi!)
BIMM118<br />
Antifungal Drugs - Antimetabolites<br />
5’-Flucytosine (Ancobon ®)<br />
– Only available antimetabolite drug<br />
– Activated by deamination within the fungal cells to 5-fluorouracil<br />
– 5-fluorouracil inhibits thymidylate synthetase<br />
– Also inhibits fungal protein synthesis by replacing uracil with<br />
5-flurouracil in fungal RNA<br />
– Resistance common (=> used in combination with other<br />
antifungals)<br />
– Broad range (only in the treatment of serious infections caused by<br />
susceptible strains of Candida and/or Cryptococcus)<br />
– Well orally absorbed
BIMM118<br />
Antifungal Drugs - Antimetabolites<br />
Griseofulvin (Grisactin®, Fulvicin®)<br />
– Inhibit fungal growth by binding to microtubules =><br />
disruption of mitotic spindles => fungistatic<br />
(mammalian microtubules less sensitive)<br />
– Mainly effective against dermatophytes (tinea)<br />
(incorporates into keratin => requires several weeks of therapy)<br />
– Oral administration (use declining due to better drugs - e.g. Triazoles)<br />
– Side effects: Nausea, hepato- and renal toxicity, photosensitivity,…<br />
– Veterinary use common
BIMM118<br />
Antifungal Drugs - Echinocandins<br />
– Inhibit synthesis of glucan in the fungal cell wall<br />
(likely block 1,3-beta glucan synthase)<br />
– Newest antifungals<br />
– Well tolerated<br />
• Caspofungin<br />
– Used i.v.<br />
– Active against Candida and Aspergillus<br />
– Approved 2001<br />
– Approved 2005 for invasive Aspergillosis<br />
• Anidulafungin<br />
– Used i.v.<br />
– Active against Candida and Aspergillus<br />
– Approved 2006 for invasive Aspergillosis<br />
• Micafungin
BIMM118<br />
Antifungal Drugs - Allylamines<br />
Allylamines<br />
– inhibit fungal sterol synthesis (ergosterol) by<br />
inhibiting squalene epoxidase<br />
• Terbinafine (Lamasil®)<br />
– Synthetic antifungal<br />
(mostly topical; p.o. for tinea unguium)<br />
– Lipophilic: accumulates in fat, skin and nails<br />
– Active against most dermatophytes (tinea, ringworm)<br />
• Butenafine (Lotrimin® Ultra)<br />
– Also anti-inflammatory activity<br />
– Superior antifungal activity over Terbinafine<br />
• Naftifine (Naftin®)<br />
• Amorolfine (Loceryl®)
BIMM118<br />
Antifungals - Summary