- Page 1 and 2:
IDSA GUIDELINES Primary Care Guidel
- Page 3 and 4:
Table 1. Guidelines from Various So
- Page 5 and 6:
Hispanic persons. Among men, these
- Page 7 and 8:
tion, those exhibiting symptoms or
- Page 9 and 10:
Table 4. Examples of Screening Stra
- Page 11 and 12:
of the vulva and perineum for evide
- Page 13 and 14:
CORECEPTOR TROPISM ASSAY Recommenda
- Page 15 and 16:
Guérin may result in a positive TS
- Page 17 and 18:
tic of neurosyphilis may also be at
- Page 19 and 20:
Table 6. Routine Health Care Mainte
- Page 21 and 22:
Table 9. Routine Immunizations in H
- Page 23 and 24:
women, the benefits may outweigh th
- Page 25 and 26:
are at increased risk of premature
- Page 27 and 28:
hibitor (NRTI) therapy is recommend
- Page 29 and 30:
sons living with HIV infection. The
- Page 31 and 32:
56. ACOG practice bulletin. Breast
- Page 33:
AIDSinfo aidsinfo.nih.gov 800-HIV-0
- Page 37 and 38:
Patient Selection 7. How will patie
- Page 39 and 40:
Adverse Effects of Antiretroviral D
- Page 41 and 42:
Adverse Effects of Antiretroviral D
- Page 43 and 44:
Clinical Manual for Management of t
- Page 45 and 46:
Table of Contents Clinical Manual f
- Page 47 and 48:
Clinical Manual for Management of t
- Page 49 and 50:
Preface—About this Manual | Clini
- Page 51:
Previous Editions Atlanta Contribut
- Page 54 and 55:
♦ ♦ ♦ ♦ ♦ | Clinical Manu
- Page 56 and 57:
1-2 | Clinical Manual for Managemen
- Page 58 and 59:
1-4 | Clinical Manual for Managemen
- Page 60 and 61:
1-6 | Clinical Manual for Managemen
- Page 62 and 63:
1-8 | Clinical Manual for Managemen
- Page 65 and 66:
Initial Physical Examination Backgr
- Page 67 and 68:
Genitals/Rectum • Inspect the gen
- Page 69 and 70:
Initial and Interim Laboratory and
- Page 71 and 72:
Section 1—Testing and Assessment
- Page 73:
Patient Education ♦ ♦ ♦ ♦ D
- Page 76 and 77:
1-22 | Clinical Manual for Manageme
- Page 78 and 79:
1-24 | Clinical Manual for Manageme
- Page 80 and 81:
1-26 | Clinical Manual for Manageme
- Page 82 and 83:
1-28 | Clinical Manual for Manageme
- Page 84 and 85:
1-30 | Clinical Manual for Manageme
- Page 86 and 87:
1-32 | Clinical Manual for Manageme
- Page 88 and 89:
1-34 | Clinical Manual for Manageme
- Page 90 and 91:
1-36 | Clinical Manual for Manageme
- Page 93 and 94:
Section 2—Health Maintenance and
- Page 95:
References ♦ ♦ ♦ ♦ ♦ ♦
- Page 98 and 99:
2-6 | Clinical Manual for Managemen
- Page 100 and 101:
2-8 | Clinical Manual for Managemen
- Page 102 and 103:
2-10 | Clinical Manual for Manageme
- Page 104 and 105:
2-12 | Clinical Manual for Manageme
- Page 106 and 107:
2-14 | Clinical Manual for Manageme
- Page 109 and 110:
Occupational Postexposure Prophylax
- Page 111 and 112:
P: Plan Laboratory Testing Provide
- Page 113 and 114:
For hepatitis C, no recommended pro
- Page 115 and 116:
Section 2—Health Maintenance and
- Page 117 and 118:
as hepatitis C or another sexually
- Page 119 and 120:
for treatment is appropriate, and b
- Page 121 and 122:
Section 2—Health Maintenance and
- Page 123 and 124:
contact with the patient. Patients
- Page 125 and 126:
tablet daily of trimethoprim-sulfam
- Page 127 and 128:
Opportunistic Infection Prophylaxis
- Page 129 and 130:
Discontinuing Primary Prophylaxis P
- Page 131 and 132:
Latent Tuberculosis Background Late
- Page 133 and 134:
INH may cause liver toxicity and it
- Page 135:
Patient Education ♦ ♦ ♦ ♦
- Page 138 and 139:
2-46 | Clinical Manual for Manageme
- Page 140 and 141:
3-2 | Clinical Manual for Managemen
- Page 142 and 143:
3-4 | Clinical Manual for Managemen
- Page 144 and 145:
3-6 | Clinical Manual for Managemen
- Page 146 and 147:
3-8 | Clinical Manual for Managemen
- Page 148 and 149:
3-10 | Clinical Manual for Manageme
- Page 150 and 151:
3-12 | Clinical Manual for Manageme
- Page 152 and 153:
3-14 | Clinical Manual for Manageme
- Page 154 and 155:
3-16 | Clinical Manual for Manageme
- Page 156 and 157:
3-18 | Clinical Manual for Manageme
- Page 159 and 160:
Reducing Maternal-Infant HIV Transm
- Page 161 and 162:
Some states require written informe
- Page 163 and 164:
contraindicated during pregnancy be
- Page 165 and 166:
Section 3—Antiretroviral Therapy
- Page 167 and 168:
Nelfinavir (Viracept) Adequate drug
- Page 169 and 170:
Section 3—Antiretroviral Therapy
- Page 171 and 172:
Section 3—Antiretroviral Therapy
- Page 173 and 174:
Patient Education ♦ ♦ ♦ ♦
- Page 175:
♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦
- Page 178 and 179:
3-40 | Clinical Manual for Manageme
- Page 180 and 181:
3-42 | Clinical Manual for Manageme
- Page 182 and 183:
3-44 | Clinical Manual for Manageme
- Page 184 and 185:
3-46 | Clinical Manual for Manageme
- Page 186 and 187:
3-48 | Clinical Manual for Manageme
- Page 188 and 189:
3-50 | Clinical Manual for Manageme
- Page 190 and 191:
3-52 | Clinical Manual for Manageme
- Page 192 and 193:
4-2 | Clinical Manual for Managemen
- Page 194 and 195:
4-4 | Clinical Manual for Managemen
- Page 196 and 197:
4-6 | Clinical Manual for Managemen
- Page 198 and 199:
4-8 | Clinical Manual for Managemen
- Page 200 and 201:
4-10 | Clinical Manual for Manageme
- Page 202 and 203:
4-12 | Clinical Manual for Manageme
- Page 204 and 205:
4-14 | Clinical Manual for Manageme
- Page 207 and 208:
Section 4—Complications of Antire
- Page 209 and 210:
♦ ♦ ♦ Toronto General Hospita
- Page 211 and 212:
Adverse Reactions to HIV Medication
- Page 213 and 214:
♦ ♦ ♦ ♦ ♦ Vital signs: No
- Page 215 and 216:
egimen, symptoms of fatigue could i
- Page 217 and 218:
Recreational Drugs and Antiretrovir
- Page 219 and 220:
Section 4—Complications of Antire
- Page 221 and 222:
LSD, Mescaline, Psilocin, and Methy
- Page 223 and 224:
Immune Reconstitution Syndrome Back
- Page 225 and 226:
A: Assessment In the appropriate cl
- Page 227 and 228:
♦ ♦ ♦ ♦ ♦ Navas E, Martin
- Page 229 and 230:
5-2 | Clinical Manual for Managemen
- Page 231 and 232:
5-4 | Clinical Manual for Managemen
- Page 233 and 234:
5-6 | Clinical Manual for Managemen
- Page 235 and 236:
5-8 | Clinical Manual for Managemen
- Page 237 and 238:
5-10 | Clinical Manual for Manageme
- Page 239 and 240:
5-12 | Clinical Manual for Manageme
- Page 241 and 242:
5-14 | Clinical Manual for Manageme
- Page 244 and 245:
Eye Problems Background The immunos
- Page 246:
of
- Page 249 and 250:
5-22 | Clinical Manual for Manageme
- Page 252 and 253:
Fever Background Although fever may
- Page 254 and 255:
Headache Background Headache may ha
- Page 256 and 257:
Lymphadenopathy Background Lymphade
- Page 258:
Treatment Treatment will depend on
- Page 261 and 262:
5-34 | Clinical Manual for Manageme
- Page 264 and 265:
Neurologic Symptoms Background The
- Page 266 and 267:
♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦
- Page 268 and 269:
Pulmonary Symptoms Background Short
- Page 270:
Treatment Once the diagnosis is mad
- Page 273 and 274:
5-46 | Clinical Manual for Manageme
- Page 275 and 276:
5-48 | Clinical Manual for Manageme
- Page 277 and 278:
6-2 | Clinical Manual for Managemen
- Page 280 and 281:
Candidiasis, Oral and Esophageal Ba
- Page 282:
Maintenance therapy Use caution whe
- Page 285 and 286:
6-10 | Clinical Manual for Manageme
- Page 288 and 289:
Cervical Dysplasia Background Cervi
- Page 290:
Patient Education ♦ ♦ ♦ ♦ P
- Page 293 and 294:
6-18 | Clinical Manual for Manageme
- Page 296 and 297:
Cryptosporidiosis Background Crypto
- Page 298:
Patient Education ♦ ♦ ♦ ♦
- Page 301 and 302:
6-26 | Clinical Manual for Manageme
- Page 303 and 304:
6-28 | Clinical Manual for Manageme
- Page 305 and 306:
6-30 | Clinical Manual for Manageme
- Page 308 and 309:
Gonorrhea and Chlamydia Background
- Page 310 and 311:
Treatment of Gonorrhea Treatment op
- Page 312 and 313:
Hepatitis B Infection Background He
- Page 314 and 315:
♦ ♦ ♦ ♦ ♦ Some patients t
- Page 316 and 317: Hepatitis C Infection Background He
- Page 318 and 319: pregnancy. Ribavirin is teratogenic
- Page 320 and 321: Herpes Simplex, Mucocutaneous Backg
- Page 322: References ♦ ♦ ♦ ♦ ♦ Cent
- Page 325 and 326: 6-50 | Clinical Manual for Manageme
- Page 327 and 328: 6-52 | Clinical Manual for Manageme
- Page 330 and 331: Kaposi Sarcoma Background Kaposi sa
- Page 332 and 333: Treatment Treatment of KS is not co
- Page 334 and 335: Molluscum Contagiosum Background Mo
- Page 336 and 337: Mycobacterium avium Complex Backgro
- Page 338 and 339: Table 1. Interactions between Rifab
- Page 340 and 341: Mycobacterium tuberculosis: Treatme
- Page 342 and 343: P: Plan Diagnostic Evaluation Durin
- Page 344 and 345: Table 1. Regimens for Treatment of
- Page 346 and 347: Rifabutin may be substituted for ri
- Page 348: Patient Education ♦ ♦ ♦ ♦
- Page 351 and 352: 6-76 | Clinical Manual for Manageme
- Page 353 and 354: 6-78 | Clinical Manual for Manageme
- Page 356 and 357: Non-Hodgkin Lymphoma Background Non
- Page 358: Patient Education ♦ ♦ ♦ ♦ S
- Page 361 and 362: 6-86 | Clinical Manual for Manageme
- Page 363 and 364: 6-88 | Clinical Manual for Manageme
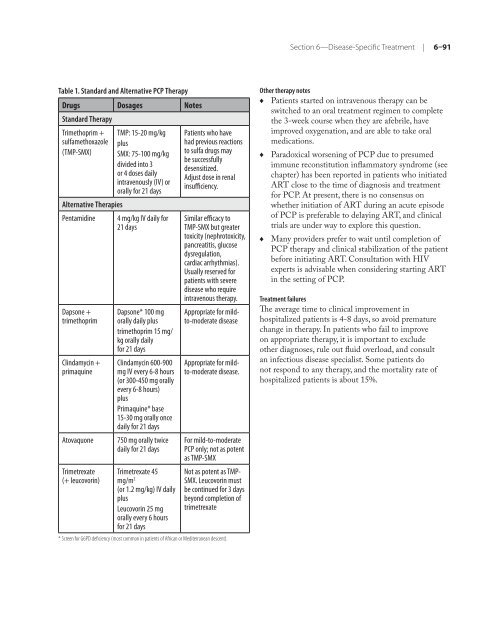
- Page 365: 6-90 | Clinical Manual for Manageme
- Page 369 and 370: 6-94 | Clinical Manual for Manageme
- Page 371 and 372: 6-96 | Clinical Manual for Manageme
- Page 373 and 374: 6-98 | Clinical Manual for Manageme
- Page 375 and 376: 6-100| Clinical Manual for Manageme
- Page 377 and 378: 6-102| Clinical Manual for Manageme
- Page 380 and 381: Toxoplasmosis Background Toxoplasma
- Page 382 and 383: ♦ Atovaquone 1,500 mg orally twic
- Page 384 and 385: Linear Gingival Erythema Background
- Page 386 and 387: Background Necrotizing ulcerating p
- Page 388 and 389: Oral Health Background Examination
- Page 390 and 391: Maxillary Tori; Mandibular Tori S:
- Page 392 and 393: Periodontal Disease Background The
- Page 394 and 395: Oral Hairy Leukoplakia Background O
- Page 396 and 397: Oral Ulceration Background Oral ulc
- Page 398 and 399: Oral Warts Background Oral warts ar
- Page 400 and 401: 7-2 | Clinical Manual for Managemen
- Page 402 and 403: 7-4 | Clinical Manual for Managemen
- Page 404 and 405: 7-6 | Clinical Manual for Managemen
- Page 406 and 407: 7-8 | Clinical Manual for Managemen
- Page 408 and 409: 7-10 | Clinical Manual for Manageme
- Page 411 and 412: Anxiety Disorders Background Anxiet
- Page 413: Patient Education ♦ ♦ Behaviora
- Page 416 and 417:
8-6 | Clinical Manual for Managemen
- Page 418 and 419:
8-8 | Clinical Manual for Managemen
- Page 420 and 421:
8-10 | Clinical Manual for Manageme
- Page 423 and 424:
Insomnia Background Insomnia is a c
- Page 425 and 426:
Suicidal Ideation Background Transi
- Page 427 and 428:
Section 8—Neuropsychiatric Disord
- Page 429 and 430:
P: Plan ♦ ♦ ♦ ♦ ♦ Check t
- Page 431 and 432:
Correctional Settings Background Ca
- Page 433 and 434:
Adherence Adherence is one of the m
- Page 435:
Karnofsky Performance Scale Backgro
- Page 438 and 439:
10-4 | Clinical Manual for Manageme
- Page 440 and 441:
10-6 | Clinical Manual for Manageme
- Page 442 and 443:
10-8 | Clinical Manual for Manageme
- Page 444 and 445:
FDA Approved Antiretrovirals for th
- Page 446 and 447:
Updated March 2008 Entry Inhibitors
- Page 448 and 449:
Drug Name Pill Dose Adverse Effects
- Page 450 and 451:
2 Recreational Drugs and HIV Antire
- Page 452 and 453:
GENERAL PHARMACOKINETICS AMYL NITRI
- Page 454 and 455:
GENERAL Erectile Dysfunction Agents
- Page 456 and 457:
KETAMINE (K, Special K) Paranoia, a
- Page 458 and 459:
10 PATIENT INFORMATION TO REDUCE HA
- Page 460 and 461:
12 FOR FURTHER INFORMATION, PLEASE
- Page 462 and 463:
THIS SECTIONTO BE COMPLETED BY PROV
- Page 464 and 465:
What’s New in the Guidelines? Jan
- Page 466 and 467:
Table of Contents GUIDELINES PANEL
- Page 468 and 469:
Table 15b. Drug Interactions betwee
- Page 470 and 471:
January 10, 2011 Guidelines Panel M
- Page 472 and 473:
Table 1. Outline of the Guidelines
- Page 474 and 475:
Baseline Evaluation (Updated Januar
- Page 476 and 477:
Table 3. Laboratory Monitoring Sche
- Page 478 and 479:
January 10, 2011 6. Casseb J, Posad
- Page 480 and 481:
January 10, 2011 7. Gatanaga H, Tsu
- Page 482 and 483:
January 10, 2011 Clinicians are thu
- Page 484 and 485:
using virus does not exclude the po
- Page 486 and 487:
Table 4. Recommendations for Using
- Page 488 and 489:
January 10, 2011 29. Smith DM, Wong
- Page 490 and 491:
January 10, 2011 4. Phillips EJ, Su
- Page 492 and 493:
Genotypic Assays January 10, 2011 G
- Page 494 and 495:
Treatment Goals (Updated January 10
- Page 496 and 497:
January 10, 2011 21. Yamashita TE,
- Page 498 and 499:
January 10, 2011 The other 50% of t
- Page 500 and 501:
January 10, 2011 • Untreated HIV
- Page 502 and 503:
January 10, 2011 morbidity and mort
- Page 504 and 505:
RECOMMENDATIONS January 10, 2011 Ba
- Page 506 and 507:
THE NEED FOR EARLY DIAGNOSIS OF HIV
- Page 508 and 509:
January 10, 2011 46. El-Sadr WM, Lu
- Page 510 and 511:
January 10, 2011 107. Simoni JM, Ku
- Page 512 and 513:
January 10, 2011 Lastly, the Panel
- Page 514 and 515:
Table 5b. Acceptable Antiretroviral
- Page 516 and 517:
January 10, 2011 NVP may be used as
- Page 518 and 519:
January 10, 2011 boosted PI regimen
- Page 520 and 521:
January 10, 2011 RTV-Boosted SQV (S
- Page 522 and 523:
January 10, 2011 TDF plus either FT
- Page 524 and 525:
January 10, 2011 threshold of nonin
- Page 526 and 527:
Table 6. Advantages and Disadvantag
- Page 528 and 529:
Table 7. Antiretroviral Components
- Page 530 and 531:
January 10, 2011 presented at: 5th
- Page 532 and 533:
January 10, 2011 83. Post FA, Moyle
- Page 534 and 535:
January 10, 2011 Efavirenz (EFV) in
- Page 536 and 537:
References January 10, 2011 1. Pane
- Page 538 and 539:
Management of the Treatment-Experie
- Page 540 and 541:
simplify the regimen if possible (e
- Page 542 and 543:
January 10, 2011 • Repeated detec
- Page 544 and 545:
References January 10, 2011 1. d'Ar
- Page 546 and 547:
January 10, 2011 58. Hammer S, Bass
- Page 548 and 549:
Types of Treatment Simplification J
- Page 550 and 551:
January 10, 2011 15. Loutfy M, Ribe
- Page 552 and 553:
Exposure-Response Relationships and
- Page 554 and 555:
January 10, 2011 Table 9b. Trough C
- Page 556 and 557:
January 10, 2011 • In patients wh
- Page 558 and 559:
January 10, 2011 17. Cressey TR, Jo
- Page 560 and 561:
January 10, 2011 (ARCHITECT), recen
- Page 562 and 563:
January 10, 2011 Table 10. Identify
- Page 564 and 565:
HIV-INFECTED ADOLESCENTS AND YOUNG
- Page 566 and 567:
Special Considerations in Adolescen
- Page 568 and 569:
HIV AND ILLICIT DRUG USERS (IDUs) (
- Page 570 and 571:
January 10, 2011 history of drug us
- Page 572 and 573:
References January 10, 2011 1. Colf
- Page 574 and 575:
Women of Childbearing Potential Jan
- Page 576 and 577:
Discontinuation of Antiretroviral T
- Page 578 and 579:
HIV-2 INFECTION (Updated January 10
- Page 580 and 581:
January 10, 2011 Considerations for
- Page 582 and 583:
References January 10, 2011 1. Spra
- Page 584 and 585:
January 10, 2011 absence of signs a
- Page 586 and 587:
MYCOBACTERIUM TUBERCULOSIS DISEASE
- Page 588 and 589:
January 10, 2011 inhibitors (NNRTIs
- Page 590 and 591:
January 10, 2011 4. Kaplan JE, Bens
- Page 592 and 593:
Interventions to Improve Adherence
- Page 594 and 595:
References January 10, 2011 1. Ches
- Page 596 and 597:
Table 13. Antiretroviral Therapy-As
- Page 598 and 599:
Table 13. Antiretroviral Therapy-As
- Page 600 and 601:
DRUG INTERACTIONS (Updated January
- Page 602 and 603:
January 10, 2011 11. Hoggard PG, Ke
- Page 604 and 605:
Table 15a. Drug Interactions betwee
- Page 606 and 607:
Table 15a. Drug Interactions betwee
- Page 608 and 609:
Table 15a. Drug Interactions betwee
- Page 610 and 611:
Table 15a. Drug Interactions betwee
- Page 612 and 613:
January 10, 2011 Table 15b. Drug In
- Page 614 and 615:
Table 15b. Drug Interactions betwee
- Page 616 and 617:
January 10, 2011 Table 15d. Drug In
- Page 618 and 619:
ATV Table 16b. Interactions between
- Page 620 and 621:
Preventing Secondary Transmission o
- Page 622 and 623:
Conclusion January 10, 2011 The Pan
- Page 624 and 625:
DXA dual-energy x-ray absorptiometr
- Page 626 and 627:
T-20 enfuvirtide TAM thymidine anal
- Page 628 and 629:
Appendix B, Table 1. Characteristic
- Page 630 and 631:
Appendix B, Table 3. Characteristic
- Page 632 and 633:
Appendix B, Table 3. Characteristic
- Page 634 and 635:
January 10, 2011 Appendix B, Table
- Page 636:
Appendix B, Table 7. Antiretroviral