In-vitro orthodontic bond strength testing: A systematic ... - share
In-vitro orthodontic bond strength testing: A systematic ... - share
In-vitro orthodontic bond strength testing: A systematic ... - share
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
SYSTEMATIC REVIEW<br />
<strong>In</strong>-<strong>vitro</strong> <strong>orthodontic</strong> <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>:<br />
A <strong>systematic</strong> review and meta-analysis<br />
Katrina J. Finnema, a Mutlu Özcan, b Wendy J. Post, c Yijin Ren, d and Pieter U. Dijkstra e<br />
Groningen, The Netherlands, and Zürich, Switzerland<br />
<strong>In</strong>troduction: The aims of this study were to <strong>systematic</strong>ally review the available literature regarding in-<strong>vitro</strong><br />
<strong>orthodontic</strong> shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> and to analyze the influence of test conditions on <strong>bond</strong> <strong>strength</strong>.<br />
Methods: Our data sources were Embase and Medline. Relevant studies were selected based on predefined<br />
criteria. Study test conditions that might influence in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> were independently assessed by 2<br />
observers. Studies reporting a minimum number of test conditions were included for meta-analysis by<br />
using a multilevel model with 3 levels, with author as the highest level, study as the second level, and<br />
specimens in the study as the lowest level. The primary outcome measure was <strong>bond</strong> <strong>strength</strong>. Results: We<br />
identified 121 relevant studies, of which 24 were included in the meta-analysis. Methodologic drawbacks of<br />
the excluded studies were generally related to inadequate reporting of test conditions and specimen<br />
storage. The meta-analysis demonstrated that 3 experimental conditions significantly affect in-<strong>vitro</strong> <strong>bond</strong><br />
<strong>strength</strong> <strong>testing</strong>. Although water storage decreased <strong>bond</strong> <strong>strength</strong> on average by 10.7 MPa, each second<br />
of photopolymerization time and each millimeter per minute of greater crosshead speed increased <strong>bond</strong><br />
<strong>strength</strong> by 0.077 and 1.3 MPa, respectively. Conclusions: Many studies on in-<strong>vitro</strong> <strong>orthodontic</strong> <strong>bond</strong><br />
<strong>strength</strong> fail to report test conditions that could significantly affect their outcomes. (Am J Orthod<br />
Dentofacial Orthop 2010;137:615-22)<br />
Orthodontic <strong>bond</strong>ing of brackets to teeth is a standard<br />
procedure to align teeth with fixed appliances.<br />
Orthodontic treatment with brackets<br />
generally takes approximately 2 years. Bond failure of<br />
brackets during this period retards treatment and is<br />
costly in terms of time, material, and patient inconvenience.<br />
Bracket de<strong>bond</strong>ing at the end of the treatment<br />
should not damage the enamel. Hypothetically, in-vivo<br />
<strong>testing</strong> in controlled trials is the best way to test the<br />
effectiveness of a <strong>bond</strong>ing system and any detrimental<br />
effects on the enamel. However, clinically, it is almost im-<br />
a Postgraduate student, Department of Orthodontics, University Medical Center<br />
Groningen, University of Groningen, Groningen, The Netherlands.<br />
b Professor, University of Zürich, Dental Materials Unit, Center for Dental and<br />
Oral Medicine, Clinic for Fixed and Removable Prosthodontics and Dental Materials<br />
Science, Zürich, Switzerland.<br />
c Statistician, Department of Epidemiology, University Medical Center<br />
Groningen, University of Groningen, Groningen, The Netherlands.<br />
d Professor and chair, Department of Orthodontics, University Medical Center<br />
Groningen, University of Groningen, Groningen, The Netherlands.<br />
e Professor, Center for Rehabilitation, Department of Oral and Maxillofacial Surgery,<br />
School for Health Research, University Medical Center Groningen, University<br />
of Groningen, Groningen, The Netherlands.<br />
The authors report no commercial, proprietary, or financial interest in the products<br />
or companies described in this article.<br />
Reprint requests to: Katrina J. Finnema, Department of Orthodontics, University<br />
Medical Center Groningen, University of Groningen, Hanzeplein 1, PO Box<br />
30.001, 9700 RB Groningen, The Netherlands; e-mail, k.j.finnema@dmo.<br />
umcg.nl.<br />
Submitted, July 2009; revised and accepted, December 2009.<br />
0889-5406/$36.00<br />
Copyright Ó 2010 by the American Association of Orthodontists.<br />
doi:10.1016/j.ajodo.2009.12.021<br />
possible to distinguish the adhesive potential of a specific<br />
<strong>bond</strong>ing system independent of many other variables<br />
that can influence either the quality or the longevity of<br />
bracket <strong>bond</strong>ing to enamel. 1 <strong>In</strong> addition, the methodologic<br />
quality of in-vivo randomized controlled trials<br />
(RCTs) evaluating de<strong>bond</strong>ing and bracket failure is generally<br />
poor. 2 Consequently, it is difficult to draw conclusions<br />
about the effectiveness of specific <strong>bond</strong>ing systems and<br />
their effects on the enamel from in-vivo studies.<br />
<strong>In</strong>-<strong>vitro</strong> studies possibly allow for more standardized<br />
procedures for <strong>testing</strong> a specific <strong>bond</strong>ing system.<br />
However, the various test conditions that are used hamper<br />
the comparison of their results. 3,4 Test conditions<br />
suggested to influence <strong>bond</strong> <strong>strength</strong> include enamel<br />
origin (ie, bovine vs human), substrate storage (eg,<br />
physiologic saline solution or water), and pretreatment<br />
of the enamel surface (eg, grinding and means of<br />
cleaning). 5-7 <strong>In</strong> addition, <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> might<br />
also be influenced by the specific test mode used (eg,<br />
tensile or shear <strong>testing</strong>). 8 An explanation for the different<br />
outcomes between in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> studies<br />
might therefore be that <strong>bond</strong> <strong>strength</strong> is not being tested<br />
but, rather, an unknown combination of mechanical<br />
properties and factors related to the test surfaces. Lately,<br />
more attention has been given to the various test conditions<br />
and their effects on the results. Recent studies have<br />
evaluated the influence of some of these factors on <strong>bond</strong><br />
<strong>strength</strong>, including force location, 9 tooth type, 10-12<br />
crosshead speed variations, 13,14 and loading mode. 8<br />
615
616 Finnema et al American Journal of Orthodontics and Dentofacial Orthopedics<br />
May 2010<br />
At present, there is no overview on bracket <strong>bond</strong><br />
<strong>strength</strong> from which general conclusions can be drawn.<br />
Because of the lack of standardization, the growing<br />
number of in-<strong>vitro</strong> studies being published can only<br />
be evaluated individually. The aims of this study were<br />
to <strong>systematic</strong>ally review the literature regarding in<strong>vitro</strong><br />
<strong>bond</strong> <strong>strength</strong> and failure mode of the most frequently<br />
used clinical <strong>bond</strong>ing systems and to analyze<br />
by meta-regression the influence of test conditions on<br />
the <strong>bond</strong> <strong>strength</strong> measured.<br />
MATERIAL AND METHODS<br />
Relevant studies were identified in a literature<br />
search and subsequently selected on the basis of inclusion<br />
criteria. Studies fulfilling the inclusion criteria<br />
were assessed for reporting test conditions that could influence<br />
the results of in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>. The<br />
studies reporting a minimal number of test conditions<br />
were included for meta-analysis.<br />
To identify studies related to in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong>,<br />
a search was performed in the databases of Medline<br />
(1967 to December 2007) and Embase (1950 to December<br />
2007) (Table I). References of identified studies and<br />
relevant review articles were searched for additional<br />
studies missed in the initial search. English was the language<br />
restriction.<br />
<strong>In</strong>itially, the titles and abstracts of the studies identified<br />
in the literature search were prescreened (by<br />
K.J.F.) for relevance to the topic of this study (in-<strong>vitro</strong><br />
<strong>orthodontic</strong> shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>). The full text<br />
of each possibly relevant study was retrieved and assessed<br />
by 2 reviewers (M.Ö., K.J.F.) for inclusion and<br />
detailed assessment of the experimental conditions.<br />
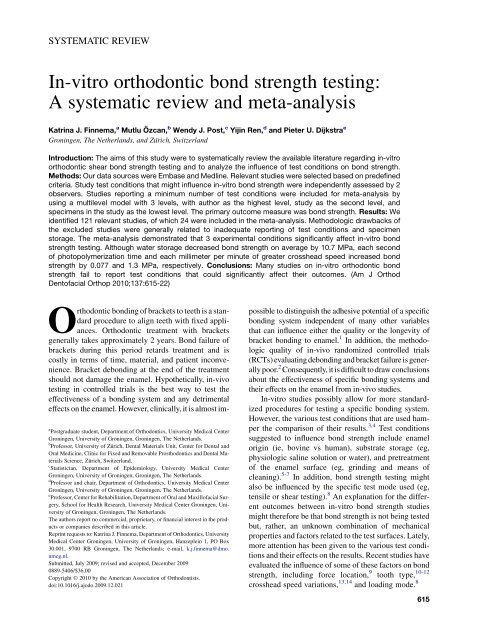
The Figure outlines the algorithm of the study selection<br />
procedure.<br />
Studies regarding <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> were selected<br />
for detailed assessment of the experimental conditions<br />
if they met the following criteria: in-<strong>vitro</strong><br />
investigation, with the shear <strong>bond</strong> <strong>strength</strong>s of metal<br />
brackets evaluated and expressed in megapascals<br />
(MPa), and the sound buccal enamel of human premolars<br />
used. Case reports, abstracts, letters, and narrative<br />
reviews were excluded.<br />
A list of 27 items was used to assess the experimental<br />
conditions, each reflecting an experimental condition<br />
that influences the results of in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> <strong>testing</strong><br />
(Table II). 3,4 Before the assessment of the studies, 2<br />
observers (M.Ö. and K.J.F.) discussed all 27<br />
experimental conditions to reach consensus about<br />
their content. They independently assessed whether<br />
the experimental conditions were reported in the<br />
study. After the assessment, the observers agreed on<br />
Table I. Search strategy in Medline and Embase<br />
Search Literature search strategy<br />
1 Explode "<strong>orthodontic</strong>-brackets"/MeSH<br />
all subheadings<br />
2 Bracket*<br />
3 Fixed applian*<br />
4 #1or#2or#3<br />
5 Explode "dental-<strong>bond</strong>ing"/MeSH all subheadings<br />
6 Bond*<br />
7 #5 or #6<br />
8 #4 and #7<br />
9 Explode "composite-resins"/MeSH all subheadings<br />
10 Explode "compomers"/MeSH all subheadings<br />
11 Explode "glass-ionomer-cements"/MeSH<br />
all subheadings<br />
12 Composite resin<br />
13 Glass ionomer<br />
14 Compomer<br />
15 #8 and (#9 or #12)<br />
16 #8 and (#10 or #14)<br />
17 #8 and (#11 or #13)<br />
18 #8 and <strong>bond</strong> <strong>strength</strong><br />
19 Search Medline/Embase: #15 or #16 or #17 or #18<br />
#, Search; MeSH, medical subjects heading (a thesaurus word); *, truncation<br />
of a text word.<br />
the reporting of the 27 experimental conditions of<br />
each study in a consensus meeting.<br />
Studies included in the meta-analysis<br />
The 2 observers independently determined the most<br />
relevant experimental conditions for in-<strong>vitro</strong> <strong>bond</strong><br />
<strong>strength</strong> studies based on the results from previous studies.<br />
<strong>In</strong> a consensus meeting, agreement was reached on<br />
these required experimental conditions. Studies were<br />
included in the meta-analysis if at least all of the following<br />
experimental conditions were reported: storage<br />
solution of teeth, 15 cleaning of enamel, 16 bracket<br />
type, 17-19 etchant type, 20 etching time, 21 adhesive<br />
type, photopolymerization device, 22 total photopolymerization<br />
time, 23 specimen storage time, 24 crosshead<br />
speed, 9,14 force location on bracket, 13 and blade design<br />
of the jig of the universal <strong>testing</strong> machine. 25<br />
The 2 observers independently extracted the data.<br />
Consensus was reached after discussion in case of disagreement.<br />
First, for each of the 27 experimental conditions, the<br />
number and percentage of included studies describing<br />
this specific item were calculated (Table II). Subsequently,<br />
for each study included in the meta-analysis,<br />
the following data were presented: thymol storage<br />
solution (yes/no), fluor-free cleaning (yes/no), mesh<br />
brackets (yes/no), phosphoric acid etching (yes/no), etching<br />
time (\30 seconds/$30 seconds), photopolymerization<br />
time (seconds), photopolymerized composite (yes/
American Journal of Orthodontics and Dentofacial Orthopedics Finnema et al 617<br />
Volume 137, Number 5<br />
Potentially relevant studies<br />
identified and screened for<br />
retrieval (n = 918)<br />
Studies retrieved for more<br />
detailed evaluation (n = 166)<br />
Potentially appropriate studies<br />
to be included in the<br />
meta-analysis (n = 121)<br />
Studies included in metaanalysis<br />
(n = 28)<br />
Studies with usable<br />
information, by outcome<br />
(n = 24)<br />
Studies excluded, with<br />
reasons (n = 752)<br />
- not relevant for topic<br />
Studies excluded, with<br />
reasons (n = 45)<br />
- did not meet with<br />
inclusion criteria<br />
Studies excluded, with<br />
reasons (n = 93)<br />
- did not meet threshold<br />
Studies withdrawn, by<br />
outcome, with reasons<br />
(n = 4)<br />
- overlapping data<br />
or missing data<br />
Fig. Algorithm of study selection procedure.<br />
no), halogen light (yes/no), water storage (yes/no), storage<br />
time (hours), thermocycling (yes/no), crosshead<br />
speed (millimeters per minute), force location on the<br />
tooth-bracket interface (yes/no), and shearing blade<br />
(yes/no). Of the latter data, the influence on the main outcome<br />
variable (<strong>bond</strong> <strong>strength</strong> in megapascals) was evaluated<br />
in the meta-analysis. Failure mode reported with the<br />
adhesive remnant index (ARI) was also scored when<br />
reported and is presented as the percentage of specimens<br />
with all adhesive left on the enamel. 26<br />
Statistical analysis<br />
Statistical analyses were performed by using the<br />
Statistical Package for the Social Sciences (version<br />
16.0, SPSS, Chicago, Ill). The interobserver agreement<br />
with respect to the reporting of experimental conditions<br />
of the included studies before the consensus meeting<br />
was expressed as the Cohen kappa. For descriptive<br />
statistics, means (standard deviations or medians) and<br />
interquartile ranges in skewed distributions are reported.<br />
<strong>In</strong> MLwin (version 2.02, Centre for Multilevel<br />
Modelling, Bristol, United Kingdom), a 3-level analysis<br />
(random-effects model) was performed. This is a metaregression<br />
analysis. The lowest level corresponded to<br />
the specimen level (specimens in studies), the middle<br />
level with the study, and the highest level corresponded<br />
Table II. Experimental conditions assessed in the 121<br />
articles<br />
Experimental condition<br />
Number (%) of studies<br />
adequately reporting<br />
experimental<br />
condition<br />
1. Substrate origin* 121 (100)<br />
2. Type of teeth* 121 (100)<br />
3. Storage time before <strong>bond</strong>ing 38 (31)<br />
4. Storage temperature before <strong>bond</strong>ing 38 (31)<br />
5. Storage solution before <strong>bond</strong>ing† 108 (89)<br />
6. Cleaning of specimens† 113 (93)<br />
7. Bracket material* 121 (100)<br />
8. Type of bracket† 94 (78)<br />
9. Type of etchant† 111 (92)<br />
10. Time of etching† 109 (90)<br />
11. Adhesive type† 119 (98)<br />
12. Amount of force at bracket placement 18 (15)<br />
13. Light device type† 75 (62)<br />
14. Total polymerization time† 84 (69)<br />
15. Light directions 65 (54)<br />
16. Sample storage time† 109 (90)<br />
17. Sample storage solution 103 (85)<br />
18. Sample storage temperature 97 (80)<br />
19. Thermocycling 26 (22)<br />
20. Testing machine 119 (98)<br />
21. Shear <strong>testing</strong> as test method 121 (100)<br />
22. Crosshead speed† 117 (97)<br />
23. Force location on bracket† 83 (69)<br />
24. Blade design† 73 (60)<br />
25. ARI 93 (77)<br />
26. Magnification used in determining ARI 70 (58)<br />
27. Bond <strong>strength</strong> in MPa* 121 (100)<br />
*Studies reporting experimental conditions numbers 1, 2, 7 and 27<br />
were included in the <strong>systematic</strong> review. †Studies reporting experimental<br />
conditions numbers 5, 6, 8, 9, 10, 11, 13, 14, 16, 22, 23 and 24,<br />
together with those conditions marked *, were selected for metaanalysis.<br />
with the author. <strong>In</strong> this way, the correlation within authors<br />
between studies was taken into account. Residual<br />
variance was entered in the multilevel model by using<br />
the within-study variance published in each study.<br />
Different models were compared by using the<br />
change in deviance (–2 log likelihood), a likelihood ratio<br />
test (chi-square distributed). <strong>In</strong> this way, it was also<br />
possible to test the statistical heterogeneity between<br />
authors and between articles by making different assumptions<br />
about (models for) the covariance structure.<br />
Effects with P values smaller than 0.05 were considered<br />
significant.<br />
RESULTS<br />
The searches of Medline and Embase yielded 918<br />
publications. After the first assessment, 166 studies<br />
were judged to be relevant for this <strong>systematic</strong> review.<br />
We found no additional studies by checking the
618 Finnema et al American Journal of Orthodontics and Dentofacial Orthopedics<br />
May 2010<br />
references of the included studies and relevant review<br />
articles. After we used the specified criteria, 121 of<br />
the 166 studies regarding <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> were included<br />
for detailed assessment of the experimental conditions<br />
(Fig). <strong>In</strong>terobserver agreement (Cohen kappa)<br />
for reporting the 27 experimental conditions of the included<br />
studies was 0.86. Disagreements were generally<br />
caused by differences in language interpretation and<br />
were resolved in the consensus meeting.<br />
On average, the 121 included studies reported<br />
a mean of 20.4 (SD, 2.8) experimental conditions with<br />
a minimum of 12 27 and a maximum of 26. 28,29 The<br />
most poorly reported item was the experimental<br />
condition of amount of force at bracket placement.<br />
This was reported in 18 (15%) of the 121 studies. The<br />
most relevant experimental conditions for in-<strong>vitro</strong><br />
<strong>bond</strong> <strong>strength</strong> were reported in the following percentage<br />
of studies: adhesive type, 98%; crosshead speed, 97%;<br />
cleaning of enamel, 93%; etchant type, 92%; etching<br />
time, 90%; specimen storage time, 90%; storage solution<br />
of teeth before <strong>bond</strong>ing, 89%; bracket type, 78%;<br />
total polymerization time, 69%; force location on<br />
bracket, 69%; photopolymerization device, 62%; and<br />
blade design, 60% (Table II).<br />
Studies included for meta-analysis<br />
By using the threshold value, 28 studies were included<br />
in the meta-analysis. <strong>In</strong> 3 of the 9 studies from<br />
the same authors, overlapping study data were reported.<br />
30-32 These duplicated data were not entered in<br />
the meta-analysis. One other study was excluded from<br />
the meta-analysis because the standard deviation of<br />
the main outcome measure (<strong>bond</strong> <strong>strength</strong> in megapascals)<br />
was not reported. 33 As a result, 24 studies were included<br />
in the meta-analysis (Appendix). 28,34-56 From<br />
these studies, data regarding experimental groups with<br />
a photopolymerized adhesive and nonself-ligating<br />
metal brackets were extracted for further analyses.<br />
This yielded 65 experimental groups that tested <strong>bond</strong><br />
<strong>strength</strong> in specimen groups ranging from 5 to 40 premolars<br />
(mean, 14.1; SD, 7.4) (Appendix). Extracted<br />
teeth were stored in distilled water with thymol in 30 experimental<br />
groups. Fluor-free cleaning was explicitly<br />
reported in 32 groups. <strong>In</strong> 58 groups, a metal bracket<br />
with a mesh base was used. Phosphoric acid etching<br />
was used in 47 groups; in 48 experimental groups, the<br />
etching time was $30 seconds. The total polymerization<br />
times in the 65 groups varied from 2 to 60 seconds<br />
(mean, 25.3; SD, 14.8).<br />
A photopolymerized composite was used in 59<br />
groups, and a halogen polymerization device was used<br />
to cure the adhesives in 48 groups. Water storage was re-<br />
Table III. Multilevel meta-analysis with <strong>bond</strong> <strong>strength</strong><br />
(MPa) as the dependent variable<br />
<strong>In</strong>dependent variable Beta (SE)<br />
Lower<br />
95% CI<br />
Upper<br />
95% CI<br />
Water storage<br />
(no, 0; yes,1)<br />
–10.648 (3.541) –17.730 –3.566<br />
Polymerization time<br />
(per second)<br />
0.077 (0.030) 0.017 0.137<br />
Crosshead speed<br />
(mm/min)<br />
1.302 (0.599) 0.104 2.500<br />
Constant 20.014 (3.452) 13.110 26.918<br />
ported in 57 groups; in 8 experimental groups, artificial<br />
saliva was used for storing the test specimens. 28 The<br />
storage times of the specimens ranged from 0 to 672<br />
hours (median, 24; interquartile range, 0-48). Thermocycling<br />
was explicitly reported in 15 of the 65 groups.<br />
The crosshead speeds when removing the bracket varied<br />
from 0.1 to 5.0 mm per minute (median, 0.5; interquartile<br />
range, 0.5-1.0). <strong>In</strong> 23 studies, the force location was<br />
at the bracket-enamel interface. <strong>In</strong> 50 groups, a shearing<br />
blade was used for de<strong>bond</strong>ing the brackets. <strong>In</strong> the remaining<br />
15 groups, a wire loop was used for the same<br />
purpose. Based on the diversity in reported test conditions,<br />
we concluded that there was considerable clinical<br />
heterogeneity in these studies. Bond <strong>strength</strong>s ranged<br />
from 3.5 to 27.8 MPa (mean, 13.4; SD, 5.7). ARI scores<br />
were reported in 57 experimental groups. Specimens<br />
with all adhesive left on the enamel after <strong>bond</strong> <strong>strength</strong><br />
<strong>testing</strong> varied from 0% to 90%.<br />
Meta-analysis<br />
Table III summarizes the results of the metaanalysis.<br />
Heterogeneity between authors and studies<br />
was still significant after entering the predictor variables<br />
(P \0.05). The results of <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> were<br />
negatively influenced when the teeth were stored in water.<br />
Water storage on average decreased <strong>bond</strong> <strong>strength</strong><br />
by 10.7 MPa, assuming that the other predictors remain<br />
constant. Analogously, each second of photopolymerization<br />
time increased the <strong>bond</strong> <strong>strength</strong> by 0.077 MPa;<br />
when crosshead speed increased by 1 mm per minute,<br />
<strong>bond</strong> <strong>strength</strong> increased by 1.3 MPa.<br />
DISCUSSION<br />
There was great diversity in the experimental conditions<br />
of studies reporting <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> in <strong>orthodontic</strong>s.<br />
The results from the meta-analysis in this<br />
<strong>systematic</strong> review indicate that the experimental conditions<br />
of water storage, photopolymerization time, and<br />
crosshead speed significantly influenced the results of<br />
in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>.
American Journal of Orthodontics and Dentofacial Orthopedics Finnema et al 619<br />
Volume 137, Number 5<br />
As previously shown in 2 other reviews evaluating<br />
<strong>orthodontic</strong> <strong>bond</strong> <strong>strength</strong> studies, there is still great diversity<br />
in test protocols and quality of these studies. 3,4<br />
The observed heterogeneity between the studies in<br />
this meta-analysis was clinically and statistically large.<br />
Not one study described all 27 experimental conditions.<br />
This finding might relate to the fact that some experimental<br />
conditions—eg, the ARI and thermocycling—<br />
were not used in all studies. However, when evaluating<br />
the 121 studies for the most relevant experimental conditions,<br />
only 28 fulfilled the threshold value. This finding<br />
indicates that most of these in-<strong>vitro</strong> studies did not<br />
properly report important confounding factors that affect<br />
<strong>bond</strong> <strong>strength</strong> outcomes. When we finally included<br />
24 of these 28 studies in a meta-analysis, water storage<br />
of the <strong>bond</strong>ed specimens, photopolymerization time,<br />
and crosshead speed were shown to be the variables<br />
that primarily affected the <strong>bond</strong> <strong>strength</strong> outcomes.<br />
Water storage decreased <strong>bond</strong> <strong>strength</strong> on average<br />
by 10.7 MPa. Although this was the most pronounced<br />
effect of an experimental condition on in-<strong>vitro</strong> <strong>bond</strong><br />
<strong>strength</strong> outcomes, this finding was mainly influenced<br />
by 1 relatively large study sample in which artificial saliva<br />
was used as a storage medium for specimens. 28<br />
Most in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> studies used distilled water<br />
for storing the specimens, but 11% of the studies did not<br />
report the storage medium. It was previously reported<br />
that specimen storage in artificial saliva reduces <strong>bond</strong><br />
<strong>strength</strong> similarly to the effect of water degradation. 57<br />
Although our study indicates that distilled water has<br />
a different effect on <strong>bond</strong> <strong>strength</strong> than artificial saliva,<br />
future research on the effects of different storage media<br />
on <strong>bond</strong> <strong>strength</strong> is needed.<br />
The second experimental condition that we found to<br />
significantly affect in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> was photopolymerization<br />
time. Each additional second of photopolymerization<br />
increased <strong>bond</strong> <strong>strength</strong> by 0.077 MPa. It was<br />
previously suggested that photopolymerization time has<br />
a greater influence on in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> than the<br />
type of photopolymerization device. 23,58 The studies in<br />
this meta-analysis showed considerable variations in<br />
photopolymerization time: from 2 to 50 seconds. Moreover,<br />
31% of the included studies did not even report<br />
polymerization time (Appendix). Most remaining studies<br />
used 40 seconds for polymerizing the adhesive; this<br />
corresponds to the routine clinical standard. The fact<br />
that the majority of these studies used a halogen device<br />
for polymerizing the adhesive most likely explains<br />
why this polymerization time was used. The results<br />
from our meta-analysis, however, suggest that a longer<br />
polymerization time yields higher <strong>bond</strong> <strong>strength</strong>s,<br />
although the most optimal time for polymerizing the<br />
adhesive cannot be deduced from our results.<br />
The third experimental condition shown to significantly<br />
affect outcomes of <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> was<br />
crosshead speed. An increase in crosshead speed of 1<br />
mm per minute yielded an increase in average <strong>bond</strong><br />
<strong>strength</strong> of 1.3 MPa. The opposite effect was demonstrated<br />
in 2 previous studies in which increases in crosshead<br />
speed from 0.5 to 5.0 mm per minute and from 1 to<br />
200 mm per minute, respectively, were associated with<br />
significant decreases of in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong>. 14,59 This<br />
phenomenon was suggested to relate to the induction of<br />
a stiff body response and the elimination of the<br />
viscoelastic properties of the adhesive. 59 <strong>In</strong> another<br />
study, no effect was observed on <strong>bond</strong> <strong>strength</strong> with<br />
crosshead speed variations between 0.1 and 5 mm per<br />
minute. 9 <strong>In</strong> the studies included in this meta-analysis,<br />
crosshead speeds ranged from 0.1 to 5 mm per minute<br />
with most using a speed of 0.5 mm per minute<br />
(Appendix). We have no obvious explanation for the<br />
discrepancy of our results with those of previous studies;<br />
unknown confounders might be responsible.<br />
Bond <strong>strength</strong> values reported in the 24 studies in<br />
this meta-analysis ranged from 3.5 to 27.8 MPa. Clinical<br />
implications of in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> values are<br />
generally based on the recommendation in a review article<br />
from 1975 60 ; a ‘‘clinically acceptable’’ value was<br />
defined as an in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> of 6 to 8 MPa. According<br />
to this criterion, 53 of the 65 experimental<br />
groups from our meta-analysis should be considered<br />
to have clinically acceptable <strong>bond</strong> <strong>strength</strong> values. Because<br />
it has never actually been tested whether 6 to 8<br />
MPa is a sufficient in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> for clinical<br />
use, the use of this reference value has been criticized<br />
before. 4,61 Since the publication of this reference<br />
value, various materials have been used, and the<br />
effects of various test conditions (eg, pH and<br />
temperature variations) have been implicated in the<br />
aging of composite resins. 61 This implies that interpretation<br />
of <strong>bond</strong> <strong>strength</strong> data should be limited to the relative<br />
effectiveness of the adhesives used in a study.<br />
Extrapolation of absolute values and comparing them<br />
with a supposedly ‘‘clinically acceptable’’ reference<br />
value should be avoided. 62<br />
Since shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> is the most commonly<br />
used method for de<strong>bond</strong>ing brackets, only studies<br />
that used this method were included in our review.<br />
With respect to shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>, there are<br />
also some variations in blade design. Most studies<br />
used a shearing blade for de<strong>bond</strong>ing the brackets,<br />
whereas in some studies a wire loop was used. 40-43,45-47<br />
De<strong>bond</strong>ing brackets with a wire loop is not a true<br />
form of shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>, since it also<br />
incorporates a component of tensile stress. Although<br />
blade design could not be identified as an
620 Finnema et al American Journal of Orthodontics and Dentofacial Orthopedics<br />
May 2010<br />
experimental condition that significantly affected in<strong>vitro</strong><br />
<strong>bond</strong> <strong>strength</strong> results in this meta-analysis, different<br />
shearing blades could have an effect. This should be<br />
substantiated by additional studies.<br />
Theoretically, in-<strong>vitro</strong> studies determine the true<br />
<strong>strength</strong> of a given <strong>bond</strong>ing system to the enamel substrate.<br />
Unfortunately, in-<strong>vitro</strong> studies have not been successful<br />
in predicting in-vivo effectiveness. 63,64 An<br />
accurate simulation of the clinical situation seems<br />
necessary to obtain clinically relevant results from in<strong>vitro</strong><br />
experiments. 4 However, because of the many conditions<br />
involved in the in-vivo situation, an accurate<br />
simulation is at present an unrealistic goal. Although<br />
in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> <strong>testing</strong> is valuable for initial<br />
screening and selection of materials, it cannot be regarded<br />
as a substitute for in-vivo <strong>testing</strong>. Orthodontic<br />
materials that perform well in in-<strong>vitro</strong> experiments<br />
should always be tested with in-vivo RCTs.<br />
Although we <strong>systematic</strong>ally reviewed the current<br />
literature on in-<strong>vitro</strong> shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>, our<br />
study has some possible limitations. Selection bias<br />
could have resulted in inappropriate inclusion or exclusion<br />
of studies based on factors other than the inclusion<br />
criteria. This chance was minimized by having 2 observers<br />
independently assess the articles. Another shortcoming<br />
might have been our language restriction.<br />
Moreover, only 2 databases were searched. Some relevant<br />
studies might have been missed by doing so. However,<br />
we believe that our conclusion of poor descriptions<br />
of test conditions in most in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> studies<br />
would not be altered by studies that were possibly<br />
missed because of language and database restrictions.<br />
This is substantiated, since 93 (77%) of the 121 potentially<br />
appropriate studies were excluded from the<br />
meta-analysis because test conditions were not adequately<br />
reported. Finally, this is a <strong>systematic</strong> review<br />
concerning in-<strong>vitro</strong> observational studies. Conclusions<br />
in <strong>systematic</strong> reviews and meta-analyses are preferably<br />
based on results from RCTs. No RCTs were available<br />
for the topic of this <strong>systematic</strong> review and metaanalysis.<br />
Selection bias, information bias, and unknown<br />
confounders threatened the validity of each study that<br />
we evaluated. <strong>In</strong> future in-<strong>vitro</strong> studies, bracket de<strong>bond</strong>ing<br />
should be evaluated more carefully by considering<br />
the items studied in this review. With this approach,<br />
the most dominant factor affecting bracket adhesion in<br />
<strong>vitro</strong> might also be identified and correlated with the<br />
clinical situation.<br />
CONCLUSIONS<br />
<strong>In</strong> this <strong>systematic</strong> review and meta-analysis, a summary<br />
of factors is given that can affect the in-<strong>vitro</strong> <strong>bond</strong><br />
<strong>strength</strong> of <strong>orthodontic</strong> brackets. Experimental conditions<br />
that significantly influence in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong><br />
are water storage of the <strong>bond</strong>ed specimens, photopolymerization<br />
time, and crosshead speed. Based on the results<br />
from this <strong>systematic</strong> review, we concluded that<br />
many studies did not properly report test conditions<br />
that could have significantly affected the outcomes. Because<br />
of developments in adhesive dentistry and the increasing<br />
numbers of <strong>bond</strong> <strong>strength</strong> studies, uniform<br />
guidelines for standardization of the experimental conditions<br />
of in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> research is clearly<br />
indicated.<br />
REFERENCES<br />
1. Leloup G, D’Hoore W, Bouter D, Degrange M, Vreven J. Metaanalytical<br />
review of factors involved in dentin adherence. J Dent<br />
Res 2000;80:1605-14.<br />
2. Mandall NA, Millett DT, Mattick CR, Hickman J,<br />
Worthington HV, Macfarlane TV. Orthodontic adhesives: a <strong>systematic</strong><br />
review. J Orthod 2002;29:205-10.<br />
3. Fox NA, McCabe JF, Buckley JG. A critique of <strong>bond</strong> <strong>strength</strong> <strong>testing</strong><br />
in <strong>orthodontic</strong>s. Br J Orthod 1994;21:33-3.<br />
4. Eliades T, Brantley WA. The inappropriateness of conventional<br />
<strong>orthodontic</strong> <strong>bond</strong> <strong>strength</strong> assessment protocols. Eur J Orthod<br />
2000;22:13-23.<br />
5. Oesterle LJ, Shellhart WC, Belanger GK. The use of bovine<br />
enamel in <strong>bond</strong>ing studies. Am J Orthod Dentofacial Orthop<br />
1998;114:514-9.<br />
6. Mühleman HR. Storage medium and enamel hardness. Helvetica<br />
Odontologica Acta 1964;8:112-7.<br />
7. Eliades T, Viazis AD, Eliades G. Bonding of ceramic brackets to<br />
enamel: morphologic and structural considerations. Am J Orthod<br />
Dentofacial Orthop 1991;99:369-75.<br />
8. Katona TR, Long RW. Effect of loading mode on <strong>bond</strong> <strong>strength</strong> of<br />
<strong>orthodontic</strong> brackets <strong>bond</strong>ed with 2 systems. Am J Orthod Dentofacial<br />
Orthop 2006;129:60-4.<br />
9. Klocke A, Kahl-Nieke B. <strong>In</strong>fluence of crosshead speed in <strong>orthodontic</strong><br />
<strong>bond</strong> <strong>strength</strong> <strong>testing</strong>. Dent Mater 2005;21:139-44.<br />
10. Oztürk B, Malkoç S, Koyutürk AE, Catalbas B, Ozer F. <strong>In</strong>fluence<br />
of different tooth types on the <strong>bond</strong> <strong>strength</strong> of two <strong>orthodontic</strong><br />
adhesive systems. Eur J Orthod 2008;30:407-12.<br />
11. Hobson RS, McCabe JF, Hogg SD. Bond <strong>strength</strong> to surface<br />
enamel for different tooth types. Dent Mater 2001;17:184-9.<br />
12. Linklater RA, Gordon PH. An ex vivo study to investigate <strong>bond</strong><br />
<strong>strength</strong>s of different tooth types. J Orthod 2001;28:59-65.<br />
13. Klocke A, Kahl-Nieke B. <strong>In</strong>fluence of force location in <strong>orthodontic</strong><br />
shear <strong>bond</strong> <strong>strength</strong> <strong>testing</strong>. Dent Mater 2005;21:391-6.<br />
14. Bishara SE, Soliman M, Laffoon J, Warren JJ. Effect of changing<br />
a test parameter on the shear <strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong><br />
brackets. Angle Orthod 2005;75:832-5.<br />
15. Titley K, Caldwell R, Kulkarni G. Factors that affect the shear<br />
<strong>bond</strong> <strong>strength</strong> of multiple component and single bottle adhesives<br />
to dentin. Am J Dent 2003;16:120-4.<br />
16. Lindauer SJ, Browning H, Shroff B, Marshall F, Anderson RH,<br />
Moon PC. Effect of pumice prophylaxis on the <strong>bond</strong> <strong>strength</strong> of<br />
<strong>orthodontic</strong> brackets. Am J Orthod Dentofacial Orthop 1997;<br />
111:599-605.<br />
17. Bishara SE, Soliman MM, Oonsombat C, Laffoon JF, Ajlouni R.<br />
The effect of variation in mesh-base design on the shear <strong>bond</strong><br />
<strong>strength</strong> of <strong>orthodontic</strong> brackets. Angle Orthod 2004;74:400-4.
American Journal of Orthodontics and Dentofacial Orthopedics Finnema et al 621<br />
Volume 137, Number 5<br />
18. Sharma-Sayal SK, Rossouw PE, Kulkarni GV, Titley KC. The influence<br />
of <strong>orthodontic</strong> bracket base design on shear <strong>bond</strong> <strong>strength</strong>.<br />
Am J Orthod Dentofacial Orthop 2003;124:74-82.<br />
19. Knox J, Hubsch P, Jones ML, Middleton J. The influence of<br />
bracket base design on the <strong>strength</strong> of the bracket-cement interface.<br />
J Orthod 2000;27:249-54.<br />
20. De Munck J, Van Landuyt K, Peumans M, Poitevin A,<br />
Lambrechts P, Braem M, et al. A critical review of the durability<br />
of adhesion to tooth tissue: methods and results. J Dent Res 2005;<br />
84:118-32.<br />
21. Gardner A, Hobson R. Variations in acid-etch patterns with different<br />
acids and etch times. Am J Orthod Dentofacial Orthop 2001;<br />
120:64-7.<br />
22. Niepraschk M, Rahiotis C, Bradley TG, Eliades T, Eliades G. Effect<br />
of various curing lights on the degree of cure of <strong>orthodontic</strong><br />
adhesives. Am J Orthod Dentofacial Orthop 2007;132:382-4.<br />
23. Eliades T. Orthodontic materials research and applications: part 1.<br />
Current status and projected future developments in <strong>bond</strong>ing and<br />
adhesives. Am J Orthod Dentofacial Orthop 2006;130:445-51.<br />
24. Yamamoto A, Yoshida T, Tsubota K, Takamizawa T,<br />
Kurokawa H, Miyazaki M. Orthodontic bracket <strong>bond</strong>ing: enamel<br />
<strong>bond</strong> <strong>strength</strong> vs time. Am J Orthod Dentofacial Orthop 2006;130:<br />
435. e1-6.<br />
25. Mojtahedzadeh F, Akhoundi MS, Noroozi H. Comparison of wire<br />
loop and shear blade as the 2 most common methods for <strong>testing</strong><br />
<strong>orthodontic</strong> shear <strong>bond</strong> <strong>strength</strong>. Am J Orthod Dentofacial Orthop<br />
2006;130:385-7.<br />
26. A˚ rtun J, Bergland S. Clinical trials with crystal growth conditioning<br />
as an alternative to acid-etch enamel pretreatment. Am J Orthod<br />
1984;85:333-40.<br />
27. Sehgal V, Shetty VS, Mogra S, Bhat G, Eipe M, Jacob S, et al.<br />
Evaluation of antimicrobial and physical properties of <strong>orthodontic</strong><br />
composite resin modified by addition of antimicrobial agents—an<br />
in-<strong>vitro</strong> study. Am J Orthod Dentofacial Orthop 2007;131:525-9.<br />
28. Chang WG, Lim BS, Yoon TH, Lee YK, Kim CW. Effects of<br />
salicylic-lactic acid conditioner on the shear <strong>bond</strong> <strong>strength</strong> of<br />
brackets and enamel surfaces. J Oral Rehabil 2005;32:287-95.<br />
29. Tecco S, Traini T, Caputi S, Festa F, de Luca V, D’Attilio M. A<br />
new one-step dental flowable composite for <strong>orthodontic</strong> use: an<br />
in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> study. Angle Orthod 2005;75:672-7.<br />
30. Vicente A, Bravo LA, Romero M, Ortız AJ, Canteras M. Bond<br />
<strong>strength</strong> of brackets <strong>bond</strong>ed with an adhesion promoter. Br Dent<br />
J 2004;196:482-5.<br />
31. Vicente A, Bravo LA, Romero M, Ortız AJ, Canteras M. Effects<br />
of 3 adhesion promoters on the shear <strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong><br />
brackets: an in-<strong>vitro</strong> study. Am J Orthod Dentofacial Orthop 2006;<br />
129:390-5.<br />
32. Vicente A, Bravo LA, Romero M. Self-etching primer and a nonrinse<br />
conditioner versus phosphoric acid: alternative methods for<br />
<strong>bond</strong>ing brackets. Eur J Orthod 2006;28:173-8.<br />
33. Aljubouri YD, Millett DT, Gilmour WH. Laboratory evaluation of<br />
a self-etching primer for <strong>orthodontic</strong> <strong>bond</strong>ing. Eur J Orthod 2003;<br />
25:411-5.<br />
34. Buyukyilmaz T, Usumez S, Karaman AI. Effect of self-etching<br />
primers on <strong>bond</strong> <strong>strength</strong>—are they reliable? Angle Orthod<br />
2003;73:64-70.<br />
35. Kim MJ, Lim BS, Chang WG, Lee YK, Rhee SH, Yang HC. Phosphoric<br />
acid incorporated with acidulated phosphate fluoride gel<br />
etchant effects on bracket <strong>bond</strong>ing. Angle Orthod 2005;75:<br />
678-84.<br />
36. Klocke A, Korbmacher HM, Huck LG, Kahl-Nieke B. Plasma arc<br />
curing lights for <strong>orthodontic</strong> <strong>bond</strong>ing. Am J Orthod Dentofacial<br />
Orthop 2002;122:643-8.<br />
37. Martin S, Garcia-Godoy F. Shear <strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong><br />
brackets cemented with a zinc oxide-polyvinyl cement. Am J Orthod<br />
Dentofacial Orthop 1994;106:615-20.<br />
38. McCourt JW, Cooley RL, Barnwell S. Bond <strong>strength</strong> of light-cure<br />
fluoride-releasing base-liners as <strong>orthodontic</strong> bracket adhesives.<br />
Am J Orthod Dentofacial Orthop 1991;100:47-52.<br />
39. Northrup RG, Berzins DW, Bradley TG, Schuckit W. Shear <strong>bond</strong><br />
<strong>strength</strong> comparison between two <strong>orthodontic</strong> adhesives and<br />
self-ligating and conventional brackets. Angle Orthod 2007;77:<br />
701-6.<br />
40. Romano FL, Tavares SW, Nouer DF, Consani S, Borges de Araújo<br />
Magnani MB. Shear <strong>bond</strong> <strong>strength</strong> of metallic <strong>orthodontic</strong><br />
brackets <strong>bond</strong>ed to enamel prepared with self-etching primer. Angle<br />
Orthod 2005;75:849-53.<br />
41. Sayinsu K, Isik F, Sezen S, Aydemir B. New protective polish effects<br />
on shear <strong>bond</strong> <strong>strength</strong> of brackets. Angle Orthod 2006;76:<br />
306-9.<br />
42. Sayinsu K, Isik F, Sezen S, Aydemir B. Light curing the primer—<br />
beneficial when working in problem areas? Angle Orthod 2006;<br />
76:310-3.<br />
43. Schaneveldt S, Foley TF. Bond <strong>strength</strong> comparison of moistureinsensitive<br />
primers. Am J Orthod Dentofacial Orthop 2002;122:<br />
267-73.<br />
44. Scougall Vilchis RJ, Yamamoto S, Kitai N, Hotta M,<br />
Yamamoto K. Shear <strong>bond</strong> <strong>strength</strong> of a new fluoride-releasing <strong>orthodontic</strong><br />
adhesive. Dent Mater J 2007;26:45-51.<br />
45. Signorelli MD, Kao E, Ngan PW, Gladwin MA. Comparison of<br />
<strong>bond</strong> <strong>strength</strong> between <strong>orthodontic</strong> brackets <strong>bond</strong>ed with halogen<br />
and plasma arc curing lights: an in-<strong>vitro</strong> and in-vivo study. Am<br />
J Orthod Dentofacial Orthop 2006;129:277-82.<br />
46. Sunna S, Rock WP. An ex vivo investigation into the <strong>bond</strong><br />
<strong>strength</strong> of <strong>orthodontic</strong> brackets and adhesive systems. Br J Orthod<br />
1999;26:47-50.<br />
47. Tecco S, Traini T, Caputi S, Festa F, de Luca V, D’Attilio M. A<br />
new one-step dental flowable composite for <strong>orthodontic</strong> use: an<br />
in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> study. Angle Orthod 2005;75:672-7.<br />
48. Usxümez S, Büyükyilmaz T, Karaman AI. Effect of light-emitting<br />
diode on <strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong> brackets. Angle Orthod<br />
2004;74:259-63.<br />
49. Uysal T, Basciftci FA, Usxümez S, Sari Z, Buyukerkmen A. Can<br />
previously bleached teeth be <strong>bond</strong>ed safely? Am J Orthod Dentofacial<br />
Orthop 2003;123:628-32.<br />
50. Vicente A, Bravo LA, Romero M, Ortiz AJ, Canteras M. Adhesion<br />
promoters: effects on the <strong>bond</strong> <strong>strength</strong> of brackets. Am<br />
J Dent 2005;18:323-6.<br />
51. Vicente A, Bravo LA, Romero M, Ortız AJ, Canteras M. Shear<br />
<strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong> brackets <strong>bond</strong>ed with self-etching<br />
primers. Am J Dent 2005;18:256-60.<br />
52. Vicente A, Bravo LA, Romero M. <strong>In</strong>fluence of a nonrinse conditioner<br />
on the <strong>bond</strong> <strong>strength</strong> of brackets <strong>bond</strong>ed with a resin adhesive<br />
system. Angle Orthod 2005;75:400-5.<br />
53. Vicente A, Bravo LA, Romero M, Ortiz AJ, Canteras M. A<br />
comparison of the shear <strong>bond</strong> <strong>strength</strong> of a resin cement and<br />
two <strong>orthodontic</strong> resin adhesive systems. Angle Orthod 2005;<br />
75:109-13.<br />
54. Vicente A, Navarro R, Mena A, Bravo LA. Effect of surface treatments<br />
on the <strong>bond</strong> <strong>strength</strong> of brackets <strong>bond</strong>ed with a compomer.<br />
Am J Dent 2006;19:271-4.<br />
55. Vicente A, Bravo LA. Direct <strong>bond</strong>ing with precoated brackets and<br />
self-etching primers. Am J Dent 2006;19:241-4.<br />
56. Wendl B, Droschl H. A comparative in-<strong>vitro</strong> study of the <strong>strength</strong><br />
of directly <strong>bond</strong>ed brackets using different curing techniques. Eur<br />
J Orthod 2004;26:535-44.
622 Finnema et al American Journal of Orthodontics and Dentofacial Orthopedics<br />
May 2010<br />
57. Kitasako Y, Burrow MF, Nikaido T, Tagami J. The influence of<br />
storage solution on dentin <strong>bond</strong> durability of resin cement. Dent<br />
Mater 2000;16:1-6.<br />
58. Ilie N, Hickel R. Correlation between ceramics translucency and<br />
polymerization efficiency through ceramics. Dent Mater 2008;24:<br />
908-14.<br />
59. Eliades T, Katsavrias E, Zinelis S, Eliades G. Effect of loading<br />
rate on <strong>bond</strong> <strong>strength</strong>. J Orofac Orthop 2004;65:336-42.<br />
60. Reynolds IR. A review of direct <strong>orthodontic</strong> <strong>bond</strong>ing. Br J Orthod<br />
1975;2:171-8.<br />
61. Eliades T. Comparing <strong>bond</strong> <strong>strength</strong>s. Am J Orthod Dentofacial<br />
Orthop 2002;122(6):13-15A.<br />
62. Eliades T, Bourauel C. <strong>In</strong>traoral aging of <strong>orthodontic</strong> materials:<br />
the picture we miss and its clinical relevance. Am J Orthod Dentofacial<br />
Orthop 2005;127:403-12.<br />
63. Murray SD, Hobson RS. Comparison of in-vivo and in-<strong>vitro</strong><br />
shear <strong>bond</strong> <strong>strength</strong>. Am J Orthod Dentofacial Orthop 2003;123:2-9.<br />
64. Sunna S, Rock WP. Clinical performance of <strong>orthodontic</strong> brackets<br />
and adhesive systems: a randomized clinical trial. Br J Orthod<br />
1998;25:283-7.
American Journal of Orthodontics and Dentofacial Orthopedics Finnema et al 622.e1<br />
Volume 137, Number 5<br />
APPENDIX REFERENCES<br />
1. Buyukyilmaz T, Usumez S, Karaman AI. Effect of self-etching<br />
primers on <strong>bond</strong> <strong>strength</strong>—are they reliable? Angle Orthod<br />
2003;73:64-70.<br />
2. Chang WG, Lim BS, Yoon TH, Lee YK, Kim CW. Effects of<br />
salicylic-lactic acid conditioner on the shear <strong>bond</strong> <strong>strength</strong> of<br />
brackets and enamel surfaces. J Oral Rehabil 2005;32:287-95.<br />
3. Kim MJ, Lim BS, Chang WG, Lee YK, Rhee SH, Yang HC. Phosphoric<br />
acid incorporated with acidulated phosphate fluoride gel<br />
etchant effects on bracket <strong>bond</strong>ing. Angle Orthod 2005;75:678-84.<br />
4. Klocke A, Korbmacher HM, Huck LG, Kahl-Nieke B. Plasma arc<br />
curing lights for <strong>orthodontic</strong> <strong>bond</strong>ing. Am J Orthod Dentofacial<br />
Orthop 2002;122:643-8.<br />
5. Martin S, Garcia-Godoy F. Shear <strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong><br />
brackets cemented with a zinc oxide-polyvinyl cement. Am<br />
J Orthod Dentofacial Orthop 1994;106:615-20.<br />
6. McCourt JW, Cooley RL, Barnwell S. Bond <strong>strength</strong> of light-cure<br />
fluoride-releasing base-liners as <strong>orthodontic</strong> bracket adhesives.<br />
Am J Orthod Dentofacial Orthop 1991;100:47-52.<br />
7. Northrup RG, Berzins DW, Bradley TG, Schuckit W. Shear <strong>bond</strong><br />
<strong>strength</strong> comparison between two <strong>orthodontic</strong> adhesives and selfligating<br />
and conventional brackets. Angle Orthod 2007;77:701-6.<br />
8. Romano FL, Tavares SW, Nouer DF, Consani S, Borges de Araújo<br />
Magnani MB. Shear <strong>bond</strong> <strong>strength</strong> of metallic <strong>orthodontic</strong><br />
brackets <strong>bond</strong>ed to enamel prepared with self-etching primer.<br />
Angle Orthod 2005;75:849-53.<br />
9. Sayinsu K, Isik F, Sezen S, Aydemir B. New protective polish effects<br />
on shear <strong>bond</strong> <strong>strength</strong> of brackets. Angle Orthod 2006;76:306-9.<br />
10. Sayinsu K, Isik F, Sezen S, Aydemir B. Light curing the primer–<br />
beneficial when working in problem areas? Angle Orthod 2006;<br />
76:310-3.<br />
11. Schaneveldt S, Foley TF. Bond <strong>strength</strong> comparison of moistureinsensitive<br />
primers. Am J Orthod Dentofacial Orthop 2002;122:<br />
267-73.<br />
12. Scougall Vilchis RJ, Yamamoto S, Kitai N, Hotta M,<br />
Yamamoto K. Shear <strong>bond</strong> <strong>strength</strong> of a new fluoride-releasing<br />
<strong>orthodontic</strong> adhesive. Dent Mater J 2007;26:45-51.<br />
13. Signorelli MD, Kao E, Ngan PW, Gladwin MA. Comparison of<br />
<strong>bond</strong> <strong>strength</strong> between <strong>orthodontic</strong> brackets <strong>bond</strong>ed with halogen<br />
and plasma arc curing lights: an in-<strong>vitro</strong> and in-vivo study. Am<br />
J Orthod Dentofacial Orthop 2006;129:277-82.<br />
14. Sunna S, Rock WP. An ex vivo investigation into the <strong>bond</strong><br />
<strong>strength</strong> of <strong>orthodontic</strong> brackets and adhesive systems. Br J Orthod<br />
1999;26:47-50.<br />
15. Tecco S, Traini T, Caputi S, Festa F, de Luca V, D’Attilio M. A<br />
new one-step dental flowable composite for <strong>orthodontic</strong> use: an<br />
in-<strong>vitro</strong> <strong>bond</strong> <strong>strength</strong> study. Angle Orthod 2005;75:672-7.<br />
16. Usxümez S, Büyükyilmaz T, Karaman AI. Effect of light-emitting<br />
diode on <strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong> brackets. Angle Orthod<br />
2004;74:259-63.<br />
17. Uysal T, Basciftci FA, Usxümez S, Sari Z, Buyukerkmen A. Can<br />
previously bleached teeth be <strong>bond</strong>ed safely? Am J Orthod Dentofacial<br />
Orthop 2003;123:628-32.<br />
18. Vicente A, Bravo LA, Romero M, Ortiz AJ, Canteras M.<br />
Adhesion promoters: effects on the <strong>bond</strong> <strong>strength</strong> of brackets.<br />
Am J Dent 2005;18:323-6.<br />
19. Vicente A, Bravo LA, Romero M, Ortız AJ, Canteras M. Shear<br />
<strong>bond</strong> <strong>strength</strong> of <strong>orthodontic</strong> brackets <strong>bond</strong>ed with self-etching<br />
primers. Am J Dent 2005;18:256-60.<br />
20. Vicente A, Bravo LA, Romero M. <strong>In</strong>fluence of a nonrinse conditioner<br />
on the <strong>bond</strong> <strong>strength</strong> of brackets <strong>bond</strong>ed with a resin<br />
adhesive system. Angle Orthod 2005;75:400-5.<br />
21. Vicente A, Bravo LA, Romero M, Ortiz AJ, Canteras M.<br />
A comparison of the shear <strong>bond</strong> <strong>strength</strong> of a resin cement<br />
and two <strong>orthodontic</strong> resin adhesive systems. Angle Orthod<br />
2005;75:109-13.<br />
22. Vicente A, Navarro R, Mena A, Bravo LA. Effect of surface treatments<br />
on the <strong>bond</strong> <strong>strength</strong> of brackets <strong>bond</strong>ed with a compomer.<br />
Am J Dent 2006;19:271-4.<br />
23. Vicente A, Bravo LA. Direct <strong>bond</strong>ing with precoated brackets and<br />
self-etching primers. Am J Dent 2006;19:241-4.<br />
24. Wendl B, Droschl H. A comparative in-<strong>vitro</strong> study of the <strong>strength</strong><br />
of directly <strong>bond</strong>ed brackets using different curing techniques.<br />
Eur J Orthod 2004;26:535-44.
622.e2 Finnema et al American Journal of Orthodontics and Dentofacial Orthopedics<br />
May 2010<br />
Appendix table. Overview of the experimental conditions and outcomes of the studies in the meta-analysis<br />
Reference<br />
number of<br />
study<br />
Number<br />
per<br />
group<br />
Thymol<br />
storage<br />
Fluor-free<br />
cleaning<br />
Mesh<br />
base<br />
Phosphoric<br />
acid<br />
etch<br />
Etch<br />
time<br />
$30 s<br />
Polymerization<br />
time (s)<br />
1 20 N N Y Y Y 40 Y<br />
1 20 N N Y N N 40 Y<br />
1 20 N N Y N N 40 Y<br />
1 20 N N Y N Y 40 Y<br />
2 9 Y Y Y Y N 30 Y<br />
2 9 Y Y Y Y N 4 Y<br />
2 9 Y Y Y Y N 50 Y<br />
2 9 Y Y Y Y N 4 Y<br />
2 9 Y Y Y N Y 30 Y<br />
2 9 Y Y Y N Y 4 Y<br />
2 9 Y Y Y N Y 50 Y<br />
2 9 Y Y Y N Y 4 Y<br />
3 10 Y Y Y Y Y 40 Y<br />
3 10 Y Y Y Y Y 40 Y<br />
3 10 Y Y Y Y Y 40 Y<br />
4 15 N N Y Y Y 6 Y<br />
4 15 N N Y Y Y 2 Y<br />
4 15 N N Y Y Y 6 Y<br />
4 15 N N Y Y Y 2 Y<br />
4 15 N N Y Y Y 20 Y<br />
5 10 N N Y Y N 60 Y<br />
6 10 N N Y Y Y 20 Y<br />
6 10 N N Y Y Y 20 Y<br />
6 10 N N Y Y Y 20 N<br />
6 10 N N Y Y Y 20 N<br />
7 20 N N Y Y N 20 Y<br />
8 10 Y Y N Y Y 40 Y<br />
8 10 Y Y N N N 40 Y<br />
8 10 Y Y N N N 40 Y<br />
9 20 N N N Y Y 40 Y<br />
10 15 N N N Y Y 40 Y<br />
10 15 N N N Y Y 40 Y<br />
11 40 Y Y Y Y Y 40 Y<br />
12 35 Y Y Y Y Y 30 Y<br />
12 35 Y Y Y N Y 30 Y<br />
13 15 Y N Y Y Y 20 Y<br />
13 15 Y N Y Y Y 20 Y<br />
13 15 Y N Y Y Y 6 Y<br />
13 15 Y N Y Y Y 6 Y<br />
14 10 N N Y Y Y 20 Y<br />
14 10 N N N Y Y 20 Y<br />
14 10 N N Y Y Y 20 Y<br />
15 15 Y Y Y Y Y 40 Y<br />
16 20 N Y Y Y Y 40 Y<br />
16 20 N Y Y Y Y 10 Y<br />
16 20 N Y Y Y Y 20 Y<br />
16 20 N Y Y Y Y 40 Y<br />
17 20 N Y Y Y Y 20 Y<br />
18 25 Y N Y Y Y 20 Y<br />
19 25 Y N Y N N 20 Y<br />
20 15 Y N Y N N 20 Y<br />
21 25 Y N Y Y Y 30 Y<br />
22 15 Y N Y Y Y 40 Y<br />
22 15 Y N Y N N 40 Y<br />
23 15 Y N Y Y Y 20 Y<br />
23 15 Y N Y N N 20 Y<br />
24 5 N Y Y Y Y 40 Y<br />
24 5 N Y Y Y Y 10 Y<br />
24 5 N Y Y Y Y 2 Y<br />
24 5 N Y Y Y Y 3 Y<br />
24 5 N Y Y Y Y 24 Y<br />
24 5 N Y Y N N 40 N<br />
24 5 N Y Y N N 10 N<br />
24 5 N Y Y N N 6 N<br />
24 5 N Y Y N N 24 N<br />
Light-cured<br />
composite<br />
*On bracket-adhesive interface; †all adhesive remained on enamel; Y, yes; N, no; ?, only mean ARI value given; NR, not reported; SEM, standard<br />
error of the mean.
American Journal of Orthodontics and Dentofacial Orthopedics Finnema et al 622.e3<br />
Volume 137, Number 5<br />
Appendix table. (Continued)<br />
Halogen<br />
light<br />
Water<br />
storage<br />
Storage<br />
time (h) Thermocycling<br />
Crosshead speed<br />
(mm/min)<br />
Force<br />
location*<br />
Shear<br />
blade<br />
ARI†<br />
(%)<br />
Bond <strong>strength</strong><br />
(MPa) SEM<br />
Y Y 24 N 0.5 Y Y 85 13.10 0.69<br />
Y Y 24 N 0.5 Y Y 75 16.00 1.01<br />
Y Y 24 N 0.5 Y Y 0 11.50 0.74<br />
Y Y 24 N 0.5 Y Y 0 9.90 0.89<br />
Y N 72 Y 0.5 Y Y 11 24.40 1.84<br />
N N 72 Y 0.5 Y Y 11 18.21 1.34<br />
Y N 72 Y 0.5 Y Y 11 27.76 1.03<br />
N N 72 Y 0.5 Y Y 11 25.09 1.24<br />
Y N 72 Y 0.5 Y Y 0 23.44 1.94<br />
N N 72 Y 0.5 Y Y 0 21.23 1.37<br />
Y N 72 Y 0.5 Y Y 0 22.89 1.19<br />
N N 72 Y 0.5 Y Y 0 16.24 1.05<br />
Y Y 1 N 1.0 Y Y 22 14.05 1.03<br />
Y Y 24 N 1.0 Y Y 30 20.94 0.79<br />
Y Y 0 Y 1.0 Y Y 10 18.03 0.84<br />
N Y 48 N 1.0 N Y 0 12.09 0.89<br />
N Y 48 N 1.0 N Y 0 7.66 0.41<br />
Y Y 48 N 1.0 N Y 7 11.24 0.92<br />
Y Y 48 N 1.0 N Y 0 6.41 0.57<br />
Y Y 48 N 1.0 N Y 7 11.85 1.13<br />
Y Y 24 Y 0.5 Y Y NR 19.60 3.04<br />
Y Y 24 N 0.5 N Y NR 11.35 0.93<br />
Y Y 672 N 0.5 N Y NR 9.19 1.20<br />
Y Y 24 N 0.5 N Y NR 11.58 0.95<br />
Y Y 672 N 0.5 N Y NR 5.39 0.75<br />
N Y 40 N 0.1 N Y 90 15.20 1.01<br />
Y Y 24 N 0.5 N N 80 6.43 0.59<br />
Y Y 24 N 0.5 N N 50 4.61 0.28<br />
Y Y 24 N 0.5 N N 0 4.74 0.4<br />
Y Y 72 N 3.0 N N NR 13.03 0.54<br />
Y Y 72 N 3.0 N N NR 14.45 0.61<br />
Y Y 72 N 3.0 N N NR 14.17 0.54<br />
Y Y 72 Y 2.0 N N 17.5 14.82 0.41<br />
Y Y 360 Y 5.0 Y Y 29 18.10 0.93<br />
Y Y 360 Y 5.0 Y Y 29 12.70 0.56<br />
Y Y 0.5 N 1.0 N N ? 13.6 0.98<br />
Y Y 1 Y 1.0 N N ? 16.1 0.93<br />
N Y 0.5 N 1.0 N N ? 14.2 1.19<br />
N Y 1 Y 1.0 N N ? 18.2 1.19<br />
Y Y 24 N 5.0 N N 0 21.56 1.05<br />
Y Y 24 N 5.0 N N 0 22.32 0.51<br />
Y Y 24 N 5.0 N N 0 17.82 0.5<br />
Y Y 72 N 1.0 N N 65 23.23 1.34<br />
Y Y 24 N 0.5 Y Y 85 13.10 0.69<br />
N Y 24 N 0.5 Y Y 50 9.10 0.69<br />
N Y 24 N 0.5 Y Y 55 13.90 1.07<br />
N Y 24 N 0.5 Y Y 55 12.70 1.16<br />
Y Y 24 N 0.5 Y Y 80 12.90 0.76<br />
Y Y 24 N 1.0 N Y 0 12.27 1.00<br />
Y Y 24 N 1.0 N Y 0 12.20 0.85<br />
Y Y 24 N 1.0 N Y 0 10.45 1.06<br />
Y Y 24 N 1.0 N Y 0 14.93 0.95<br />
Y Y 24 N 1.0 N Y 0 7.19 0.73<br />
Y Y 24 N 1.0 N Y 0 8.34 0.51<br />
Y Y 24 N 1.0 N Y 0 14.13 2.27<br />
Y Y 24 N 1.0 N Y 0 14.28 2.74<br />
Y Y 1 N 0.5 N Y 0 9.50 0.72<br />
Y Y 1 N 0.5 N Y 0 5.80 0.58<br />
N Y 1 N 0.5 N Y 0 3.50 0.49<br />
N Y 1 N 0.5 N Y 0 5.20 0.31<br />
N Y 1 N 0.5 N Y 0 5.80 0.72<br />
Y Y 1 N 0.5 N Y 0 8.20 0.80<br />
Y Y 1 N 0.5 N Y 0 7.50 0.63<br />
N Y 1 N 0.5 N Y 0 9.40 0.85<br />
N Y 1 N 0.5 N Y 0 8.00 0.67