Upper Airway Obstruction
Upper Airway Obstruction
Upper Airway Obstruction
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Ch37 7/10/08 9:47 AM Page 388<br />
37<br />
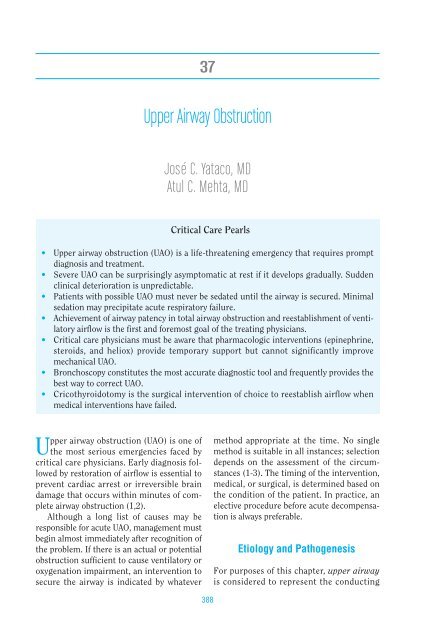
<strong>Upper</strong> <strong>Airway</strong> <strong>Obstruction</strong><br />
José C. Yataco, MD<br />
Atul C. Mehta, MD<br />
Critical Care Pearls<br />
• <strong>Upper</strong> airway obstruction (UAO) is a life-threatening emergency that requires prompt<br />
diagnosis and treatment.<br />
• Severe UAO can be surprisingly asymptomatic at rest if it develops gradually. Sudden<br />
clinical deterioration is unpredictable.<br />
• Patients with possible UAO must never be sedated until the airway is secured. Minimal<br />
sedation may precipitate acute respiratory failure.<br />
• Achievement of airway patency in total airway obstruction and reestablishment of ventilatory<br />
airflow is the first and foremost goal of the treating physicians.<br />
• Critical care physicians must be aware that pharmacologic interventions (epinephrine,<br />
steroids, and heliox) provide temporary support but cannot significantly improve<br />
mechanical UAO.<br />
• Bronchoscopy constitutes the most accurate diagnostic tool and frequently provides the<br />
best way to correct UAO.<br />
• Cricothyroidotomy is the surgical intervention of choice to reestablish airflow when<br />
medical interventions have failed.<br />
<strong>Upper</strong> airway obstruction (UAO) is one of<br />
the most serious emergencies faced by<br />
critical care physicians. Early diagnosis followed<br />
by restoration of airflow is essential to<br />
prevent cardiac arrest or irreversible brain<br />
damage that occurs within minutes of complete<br />
airway obstruction (1,2).<br />
Although a long list of causes may be<br />
responsible for acute UAO, management must<br />
begin almost immediately after recognition of<br />
the problem. If there is an actual or potential<br />
obstruction sufficient to cause ventilatory or<br />
oxygenation impairment, an intervention to<br />
secure the airway is indicated by whatever<br />
388<br />
method appropriate at the time. No single<br />
method is suitable in all instances; selection<br />
depends on the assessment of the circumstances<br />
(1-3). The timing of the intervention,<br />
medical, or surgical, is determined based on<br />
the condition of the patient. In practice, an<br />
elective procedure before acute decompensation<br />
is always preferable.<br />
Etiology and Pathogenesis<br />
For purposes of this chapter, upper airway<br />
is considered to represent the conducting
Ch37 7/10/08 9:47 AM Page 389<br />
passages extending from the nose or mouth<br />
to the main carina (Figure 37-1).<br />
UAO may be functional or anatomic and<br />
may develop acutely or subacutely. Relapsing<br />
polychondritis constitutes a good example of<br />
functional UAO caused by lack of a firm cartilaginous<br />
structure to support the tracheal<br />
wall. Squamous cell carcinoma of the larynx<br />
represents an anatomic example of UAO.<br />
Narrowing of the upper respiratory tract<br />
has an exponential effect on airflow because<br />
Palatine tonsil<br />
Tongue<br />
Oral pharynx<br />
Retropharyngeal space<br />
Root of tongue<br />
Geniohyoid muscle<br />
Mylohyoid muscle<br />
Submandibular<br />
space<br />
Vallecula<br />
Epiglottis<br />
Hypophyarynx<br />
Vocal cord<br />
Thyroid cartilage<br />
Larynx<br />
Cricoid cartilage<br />
Trachea<br />
Sternum<br />
<strong>Upper</strong> <strong>Airway</strong> <strong>Obstruction</strong> 389<br />
linear airflow is a function of the fourth<br />
power of the radius (2-4). Although UAO<br />
occurs at any level of the upper respiratory<br />
tract, laryngeal obstruction has a particular<br />
importance because the larynx is the narrowest<br />
portion of the upper airway. The narrowest<br />
portion of the larynx is at the glottis in<br />
adults and the subglottis in infants (5).<br />
Some infections such as parapharyngeal<br />
or retropharyngeal abscesses and Ludwig<br />
angina (mixed infection of floor of the<br />
Figure 37-1 Anatomy of the upper airway. (Adapted from Aboussouan L, Stoller JK. Diagnosis<br />
and management of upper airway obstruction. Clin Chest Med. 1994;15:35-53; with permission.)
Ch37 7/10/08 9:47 AM Page 390<br />
390 Systemic Disorders<br />
mouth) can be associated with severe soft tissue<br />
swelling causing UAO.<br />
The differential diagnosis of UAO is wide<br />
and varies by age group and by clinical setting.<br />
Table 37-1 summarizes the most common<br />
causes of airway obstruction. Figures<br />
37-2 and 37-3 show examples of benign and<br />
malignant causes of UAO.<br />
Clinical Signs and Symptoms<br />
In a conscious patient, signs and symptoms of<br />
UAO include marked respiratory distress,<br />
altered voice, dysphagia, odynophagia, the<br />
hand-to-the-throat choking sign, stridor, facial<br />
swelling, prominence of neck veins, absence of<br />
air entry into the chest, and tachycardia. In an<br />
Table 37-1 Differential Diagnosis of <strong>Upper</strong><br />
<strong>Airway</strong> <strong>Obstruction</strong> According to Etiology<br />
Traumatic causes<br />
• Laryngeal stenosis<br />
• <strong>Airway</strong> burn<br />
• Acute laryngeal injury<br />
• Facial trauma (mandibular or maxillary fractures)<br />
• Hemorrhage<br />
Infections<br />
• Suppurative parotitis<br />
• Retropharyngeal abscess<br />
• Tonsillar hypertrophy<br />
• Ludwig’s angina<br />
• Epiglottitis<br />
• Laryngitis<br />
• Laryngotracheobronchitis (croup)<br />
• Diphtheria<br />
Iatrogenic causes<br />
• Tracheal stenosis post-tracheostomy<br />
• Tracheal stenosis post-intubation<br />
• Mucous ball from transtracheal catheter<br />
Foreign bodies<br />
Vocal cord paralysis<br />
Tumors<br />
• Laryngeal tumors (benign or malignant)<br />
• Laryngeal papillomatosis<br />
• Tracheal stenosis (caused by intrinsic or<br />
extrinsic tumors)<br />
Angioedema<br />
• Anaphylactic reactions<br />
• C1 inhibitor deficiency<br />
• Angiotensin-converting enzyme inhibitors<br />
Figure 37-2 Tracheal amyloidosis causing<br />
narrowing of the distal trachea.<br />
Figure 37-3 Extrinsic compression of the<br />
trachea caused by intrathoracic malignancy.<br />
unconscious or sedated patient, the first sign of<br />
airway obstruction may be inability to ventilate<br />
with a bag-valve mask after an attempt to open<br />
the airway with a jaw-thrust maneuver. After a<br />
few minutes of complete airway obstruction,<br />
asphyxiation progresses to cyanosis, bradycardia,<br />
hypotension, and irreversible cardiovascular<br />
collapse (1-3).<br />
Occasionally, UAO can develop slowly and is<br />
confused with reactive airway disease. However,
Ch37 7/10/08 9:47 AM Page 391<br />
the obstructive noise or stridor is thought to be<br />
a specific for UAO. Stridor is heard during the<br />
entire respiratory cycle but typically intensifies<br />
during inspiration and is usually more prominent<br />
above the neck. The presence of stridor<br />
indicates severe airway obstruction (airway passage<br />
Ch37 7/10/08 9:47 AM Page 392<br />
392 Systemic Disorders<br />
Airflow, L/S<br />
A<br />
Airflow, L/S<br />
C<br />
10<br />
5<br />
5<br />
10<br />
10<br />
5<br />
5<br />
10<br />
Expiration<br />
Inspiration<br />
100 0<br />
Lung volume, % VC<br />
Expiration<br />
Inspiration<br />
100 0<br />
Lung volume, % VC<br />
Airflow, L/S<br />
B<br />
Airflow, L/S<br />
D<br />
10<br />
5<br />
5<br />
10<br />
10<br />
5<br />
5<br />
10<br />
Expiration<br />
Inspiration<br />
100 0<br />
Lung volume, % VC<br />
Expiration<br />
Inspiration<br />
100 0<br />
Lung volume, % VC<br />
Figure 37-4 Flow-volume curves in upper airway obstruction. (A) indicates the normal contour of<br />
the inspiratory and expiratory curves; (B) With variable intrathoracic obstruction (e.g.,<br />
tracheomalacia within the thorax), obstruction is marked during exhalation with marked truncation<br />
of the expiratory curve; (C) With variable extrathoracic obstruction (e.g., collapse of tracheal cartilage<br />
in the neck following trauma), obstruction is more marked during inspiration; (D) Finally, with<br />
fixed obstructions (e.g., tracheal stenosis), both the inspiratory and expiratory curves are markedly<br />
truncated. (Adapted from Hall JB, Schmidt GA, Wood LD, eds. Principles of Critical Care. New York:<br />
McGraw-Hill; 1992; with permission.)<br />
subdiaphragmatic abdominal thrust can force<br />
air from the lungs; this may be sufficient to<br />
create an artificial cough and expel a foreign<br />
body from the airway. Repeat abdominal<br />
thrusts may be needed to clear the airway.<br />
Several medical and surgical approaches<br />
are available in the management of UAO<br />
including oropharyngeal airways, endotra-<br />
cheal intubation (transnasally or orally),<br />
tracheotomy, cricothyroidotomy, fiberoptic<br />
intubation, racemic epinephrine, corticosteroids,<br />
helium–oxygen mixtures, laser therapy,<br />
bronchoscopic dilation, and airway<br />
stenting (Table 37-2). The selection of the<br />
intervention will depend on the cause of UAO<br />
and the urgency to obtain a secure airway.
Ch37 7/10/08 9:47 AM Page 393<br />
Table 37-2 Interventions in <strong>Upper</strong> <strong>Airway</strong><br />
<strong>Obstruction</strong><br />
Medical Interventions<br />
Heimlich maneuver (suspected foreign body<br />
aspiration)<br />
Oropharyngeal airways<br />
Endotracheal intubation (transnasally or orally)<br />
Racemic epinephrine<br />
Corticosteroids<br />
Helium–oxygen mixture<br />
Surgical or Bronchoscopic Interventions<br />
Fiberoptic intubation<br />
Cricothyroidotomy<br />
Tracheostomy<br />
Laser/electrocautery/balloon dilation<br />
<strong>Airway</strong> stenting<br />
Racemic Epinephrine<br />
Racemic epinephrine is usually used in circumstances<br />
when the patient with a partial<br />
UAO is still conscious and able to ventilate,<br />
and vasoconstriction is desired to decrease<br />
mucosal edema.<br />
Racemic epinephrine administered by<br />
means of a nebulizer has been proven to be<br />
effective in treating croup (laryngotracheobronchitis)<br />
in the pediatric population<br />
decreasing morbidity, mortality, and hospital<br />
stay (6). Conversely, racemic epinephrine is<br />
not effective in the treatment of epiglottitis<br />
and may be deleterious (7).<br />
Racemic epinephrine also is used to treat<br />
postextubation laryngeal edema, which has<br />
been reported to occur from 2.3% to 6.9% (8).<br />
The typical case is that of a patient, breathing<br />
easily for the first two or three hours, followed<br />
by the gradual progression of dyspnea,<br />
inspiratory stridor, and increased work of<br />
breathing. In this situation repeat racemic<br />
epinephrine treatments can be used as a temporary<br />
measure until the acute swelling and<br />
inflammation subsides. These patients should<br />
remain in the intensive care unit under careful<br />
observation until it is confirmed that the<br />
UAO has resolved or greatly improved.<br />
Corticosteroids<br />
Corticosteroids have been used to treat UAO<br />
because of their potential beneficial effect in<br />
<strong>Upper</strong> <strong>Airway</strong> <strong>Obstruction</strong> 393<br />
reducing airway edema. Randomized trials<br />
have confirmed the usefulness of corticosteroids<br />
in the treatment of croup with<br />
decreases in the need for intubation and<br />
hospital stay (9). However the treatment of<br />
epiglottitis with steroids is controversial and<br />
often contraindicated (5).<br />
Experimental studies in animals have<br />
shown that corticosteroids given at the time<br />
of extubation decrease capillary dilatation<br />
and permeability as well as edema formation<br />
and inflammatory cells infiltration. The preventive<br />
use of steroids for postextubation<br />
laryngeal edema is until now widely accepted.<br />
However, a placebo controlled, double-blind,<br />
multicenter study showed that dexamethasone<br />
does not prevent laryngeal edema after<br />
tracheal extubation, regardless of intubation<br />
duration (8-10).<br />
Heliox<br />
Heliox, a helium–oxygen gas mixture, is<br />
effective in reducing the work of breathing by<br />
decreasing airway resistance to turbulent<br />
flow in the density-dependent pressure drop<br />
across the airway obstruction. Heliox has<br />
been used in several conditions including<br />
postextubation laryngeal edema, tracheal<br />
stenosis or extrinsic compression, status<br />
asthmaticus, and angioedema (11,12).<br />
To be effective, the helium–oxygen ratio<br />
must be at least 70:30. Unfortunately, most<br />
patients with UAO also have lung disease with<br />
varying degrees of hypoxemia preventing the<br />
use of heliox at effective concentrations.<br />
Although the work of breathing and dyspnea<br />
improves to some degree with the use of<br />
heliox, the mechanical obstruction is still in<br />
place. The use of heliox in patients with<br />
severe UAO should only be used to provide<br />
temporary support pending definitive diagnosis<br />
and management.<br />
Endotracheal Intubation<br />
In most cases of UAO, the patency of the<br />
upper airway can be reestablished with endotracheal<br />
intubation after rapid assessment of<br />
the patient’s airway anatomy. Evaluation of
Ch37 7/10/08 9:47 AM Page 394<br />
394 Systemic Disorders<br />
mouth opening (>40 mm), dentition, cervical<br />
spine mobility (flexion-extension), thyromental<br />
distance (normal is >3 finger breadths)<br />
and the function of the temporomandibular<br />
joints are key to subsequent success and<br />
avoidance of complications (13,14).<br />
Orotracheal intubation under direct visualization<br />
with a laryngoscope is the most<br />
commonly used route for emergency intubations.<br />
In patients with distorted airway<br />
anatomy or suspected cervical spine injury,<br />
fiberoptic bronchoscopy can be used to guide<br />
the intubation. The endotracheal tube is positioned<br />
over a bronchoscope; the operator<br />
introduces the fiberoptic bronchoscope into<br />
the patient’s mouth or nose and advances it<br />
through the vocal cords into the trachea. The<br />
endotracheal tube is then advanced over the<br />
bronchoscope.<br />
A prompt and successful intubation in a<br />
patient with UAO allows restoration of adequate<br />
ventilation and oxygenation and the<br />
performance of further diagnostic and therapeutic<br />
procedures.<br />
Surgical Interventions<br />
Overall, emergency laryngotracheal intubation<br />
is effective in approximately 97% of<br />
cases (13). Thus, a surgical airway is needed<br />
in only 3% of such emergencies. The need for<br />
an immediate surgical airway must be evaluated<br />
considering the potential difficulties<br />
associated with emergency intubation. In<br />
cases of UAO the surgical airway is considered<br />
emergently in cases of laryngotracheal<br />
trauma, foreign body lodged in the pharyngolaryngeal<br />
area, or severe anatomic deformity<br />
caused by trauma.<br />
When surgical airway management is<br />
required, cricothyroidotomy is the procedure<br />
of choice in the emergency setting; it is faster<br />
(average 30 sec), simpler, and more likely to<br />
be successful than tracheotomy. Intraluminal<br />
diameter of the trachea is narrowest at the<br />
level of the cricoid; there is concern that prolonged<br />
use of a cricothyroidotomy may cause<br />
subglottic injury and lead to subglottic narrowing.<br />
It is recommended that cricothy-<br />
roidotomy be converted to formal tracheotomy<br />
if longer than 72 hours of use is<br />
anticipated.<br />
Tracheostomy is probably the last option<br />
available to establish an airway in acute UAO.<br />
Laryngeal trauma is a relative contraindication<br />
to cricothyroidotomy and laryngotracheal<br />
intubation; it is the only indication for<br />
emergency tracheostomy. This procedure is<br />
time-consuming and requires expertize and<br />
attention to detail. Comparison of emergent<br />
versus elective tracheotomy reveals a twofold<br />
complication rate in the former because of<br />
the time spent on isolating the trachea as a<br />
result of commonly occurring bleeding (13,15).<br />
Cricothyroidotomy has a higher success<br />
rate than tracheostomy; it also has better<br />
patient neurologic outcome based primarily<br />
on less time required for the procedure (11).<br />
Overall, patients requiring an emergency<br />
surgical airway have a relatively high mortality<br />
(15).<br />
Laser Therapy<br />
Carbon dioxide or neodymium:yttrium-aluminum-garnet<br />
(Nd:YAG) laser therapy can be<br />
used to treat intraluminal tracheobronchial<br />
lesions once the UAO has been stabilized with<br />
a secure airway. Although the onset of airway<br />
compromise is usually gradual, some patients<br />
remain asymptomatic despite airways that<br />
are only two to three millimeter in diameter.<br />
These patients only develop dyspnea on exercise<br />
or when complete blockage results from<br />
mucus, bleeding, or inflammation with<br />
swelling. Laser therapy can be used to excise<br />
tracheal webs, to treat benign obstructive<br />
lesions, or as palliative therapy for malignant<br />
tracheobronchial lesions.<br />
Tracheal Stenting<br />
Tracheal stents placed using either rigid or<br />
flexible bronchoscopy can be helpful to maintain<br />
a patent airway in patients with tracheal<br />
obstruction caused by benign or malignant<br />
conditions. <strong>Airway</strong> resection and reconstruction<br />
provide the definitive correction, but
Ch37 7/10/08 9:47 AM Page 395<br />
many patients have unresectable disease. For<br />
these patients, therapeutic bronchoscopy<br />
provides rapid palliation that can be lifesaving<br />
and improve quality of life. Benign<br />
lesions can be managed with dilation, with or<br />
without laser resection. Malignant lesions<br />
often require core out of the tumor with a<br />
rigid bronchoscope followed by laser, photodynamic<br />
therapy, brachytherapy, cryotherapy,<br />
or electrocautery. <strong>Airway</strong> stents are a valuable<br />
adjunct to these techniques and can provide<br />
prolonged palliation from an unresectable<br />
recalcitrant benign stenosis or rapidly recurrent<br />
endoluminal tumor.<br />
Neither silicone nor the available metal<br />
stents conform to all the ideal characteristics<br />
desired for an endobronchial stent. The silicone<br />
stent has the advantages of being easily<br />
repositioned or removed, causing minimal<br />
granulation, and being inexpensive. Its disadvantages<br />
are the need for rigid bronchoscopy<br />
and general anesthesia, reduced inner diameter,<br />
and the potential for being dislodged or<br />
distorted (16,17). The expandable metal stent<br />
has the advantages of being easily delivered<br />
with flexible bronchoscopy, having minimal<br />
migration, and conforming well to the<br />
anatomy of the airway. The major disadvantage<br />
is that it is permanent and can cause significant<br />
granulation tissue within the stent<br />
(17). Because of the intrinsic problems associated<br />
with airway stents, regardless of type,<br />
it is important to remember that these<br />
patients require lifelong management and<br />
are at risk for development of stent obstruction<br />
or migration. In one series, 41% of<br />
patients required additional endoscopic<br />
interventions to maintain airway patency. In<br />
patients with benign disease and normal life<br />
expectancy (e.g., relapsing polychondritis) a<br />
much higher percentage of patients require<br />
further interventions (16,17).<br />
Complications<br />
Pulmonary Edema<br />
Postobstructive pulmonary edema is the sudden<br />
onset of edema following UAO without<br />
evidence of any other underlying cardiopul-<br />
<strong>Upper</strong> <strong>Airway</strong> <strong>Obstruction</strong> 395<br />
monary condition (18-20). There are two<br />
types of postobstructive pulmonary edema.<br />
Type I follows a sudden, severe airway<br />
obstruction such as postextubation laryngospasm,<br />
epiglottitis, croup, strangulation,<br />
choking, and hanging. Type I is associated<br />
with any cause of acute UAO. Type II pulmonary<br />
edema develops after surgical relief<br />
of long-term UAO. Reported causes include<br />
tonsillectomy and removal of upper airway<br />
tumors. Postobstructive pulmonary edema<br />
usually occurs within one hour of a precipitating<br />
event but it has reported to occur up to<br />
six hours later. The exact pathogenesis is<br />
unclear but the current theory is that young<br />
patients are able to generate extremely high<br />
negative intrathoracic pressure, which<br />
increases venous return, decreases cardiac<br />
output, and causes fluid transudation into<br />
the alveolar space. The cause of type II postobstructive<br />
pulmonary edema is less clear,<br />
but it appears that the obstructing lesion<br />
produces a modest level of positive endexpiratory<br />
pressure (PEEP) and increases<br />
end-expiratory lung volume. The sudden<br />
removal of this PEEP may then lead to interstitial<br />
fluid transudation and pulmonary<br />
edema (20).<br />
The treatment of postobstructive pulmonary<br />
edema is supportive with supplemental<br />
oxygen, intubation, and application of low<br />
levels of PEEP (5 cm H 2 O). The role of diuretics<br />
in this setting is unclear. Most patients<br />
respond promptly to appropriate treatment<br />
and have full recovery.<br />
Summary<br />
<strong>Upper</strong> airway obstruction is a potentially fatal<br />
emergency faced by critical care physicians. It<br />
can be caused by myriad conditions that will<br />
require a particular treatment after appropriate<br />
diagnosis. Regardless of the specific cause,<br />
the patient with UAO must be carefully monitored<br />
in the ICU for impending respiratory<br />
failure. A secure and patent airway should be<br />
established if clinical deterioration is seen.<br />
Pharmacologic interventions have limited
Ch37 7/10/08 9:47 AM Page 396<br />
396 Systemic Disorders<br />
usefulness in the setting of acute mechanical<br />
UAO. The critical care physician must be competent<br />
in the full range of airway access procedures.<br />
Overall, patients requiring an<br />
emergency surgical airway have a poor neurological<br />
outcome and higher mortality. Figure<br />
37-5 gives an algorithmic approach to management<br />
of UAO.<br />
REFERENCES<br />
Impending respiratory failure<br />
Is ET intubation<br />
possible?<br />
Yes<br />
No<br />
Urgent establishment of<br />
patent airway<br />
Direct or fiberoptic<br />
intubation<br />
Crycothyroidotomy vs<br />
Tracheotomy<br />
1. Jacobson S. <strong>Upper</strong> airway obstruction. Emerg<br />
Med Clin North Am. 1989;7:205-17.<br />
2. Khosh MM, Lebovics RS. <strong>Upper</strong> airway obstruction.<br />
In: Parrillo JE, Dellinger RP, eds. Critical<br />
Care Medecine. St. Louis: Mosby; 2001:808-25.<br />
3. King EG, Sheehan GJ, McDonell TJ. <strong>Upper</strong> airway<br />
obstruction. In: Hall JB, Schmidt GA,<br />
Wood LD, eds. Principles of Critical Care. New<br />
York: McGraw-Hill; 1992:1710-8.<br />
4. Aboussouan L, Stoller JK. Diagnosis and management<br />
of upper airway obstruction. Clin<br />
Chest Med. 94119;5:35-53.<br />
Stridor suggestive of<br />
UAO<br />
Quick history and physical<br />
examination<br />
Gradual onset and mild<br />
symptoms<br />
Selection of appropriate ancillary<br />
studies:<br />
• Bronchoscopy<br />
• CT upper airway<br />
• Spirometry<br />
Figure 37-5 Algorithm for management of upper airway obstruction. (CT = computed tomography;<br />
ET = endotracheal; UAO = upper airway obstruction.)<br />
5. Dickison AE. The normal and abnormal pediatric<br />
airway. Recognition and management of<br />
obstruction. Clin Chest Med. 87819;5:83-96.<br />
6. Quan L. Diagnosis and treatment of croup. Am<br />
Fam Physician. 92419;6:747-55.<br />
7. Kissoon N, Mitchell I. Adverse effects of<br />
racemic epinephrine in epiglottitis. Pediatr<br />
Emerg Care. 85119;143-4.<br />
8. Darmon JY, Rauss A, Dreyffus D, et al. Evaluation<br />
of risk factors for laryngeal edema after tracheal<br />
extubation in adults and its prevention by dexamethasone.<br />
Anesthesiology. 1992;77:245-51.<br />
9. Kairys SW, Olmstead EM, O’Connor GT.<br />
Steroid treatment of laryngotracheitis: a metaanalysis<br />
of the evidence from randomized trials.<br />
Pediatrics. 1989;83:683-93.<br />
10. McCulloch TM, Bishop MJ. Complications of<br />
translaryngeal intubation. Clin Chest Med.<br />
1991;12:507-21.<br />
11. Boorstein JM, Boorstein SM, Humphries GN,<br />
et al. Using helium–oxygen mixtures in the<br />
emergency management of acute upper airway<br />
obstruction. Ann Emerg Med. 1989;18:688-90.<br />
12. Curtis JL, Mahlmeister M, Fink JB, et al.<br />
Helium–oxygen gas therapy. Chest. 1986;90:<br />
455-7.
Ch37 7/10/08 9:47 AM Page 397<br />
13. Feller-Kopman D. Acute complications of artificial<br />
airways. Clin Chest Med. 2003;24:445-55.<br />
14. Steinert R, Lullwitz E. Failed intubation with<br />
case reports. HNO. 1987;35:439-42.<br />
15. Goldberg J, Levy PS, Morkovin V, Goldberg JB.<br />
Mortality from traumatic injuries: a casecontrol<br />
study using data from the national<br />
hospital discharge survey. Med Care. 1983;21:<br />
692-704.<br />
16. Wood DE, Liu YH, Vallieres E, et al. <strong>Airway</strong><br />
stenting for malignant and benign tracheobronchial<br />
stenosis. Ann Thorac Surg. 2003;76:<br />
167-74.<br />
<strong>Upper</strong> <strong>Airway</strong> <strong>Obstruction</strong> 397<br />
17. Saad CP, Murthy S, Krizmanich G, Mehta AC.<br />
Self-expandable metallic airway stents and<br />
flexible bronchoscopy: long term outcome<br />
analysis. Chest. 2003;124:1993-9.<br />
18. Kanter RK, Waichko I. Pulmonary edema<br />
associated with upper airway obstruction. Am<br />
J Dis Child. 1984;138:356.<br />
19. Wilms D, Shure D. Pulmonary edema due to<br />
upper airway obstruction in adults. Chest.<br />
88919;4:1090-2.<br />
20. Van Kooy MA, Gargiulo RF. Postobstructive<br />
pulmonary edema. Am Fam Physician.2000;<br />
62:401-4.