SATS 2009 Final Program - Scandinavian Association for Thoracic ...
SATS 2009 Final Program - Scandinavian Association for Thoracic ...
SATS 2009 Final Program - Scandinavian Association for Thoracic ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
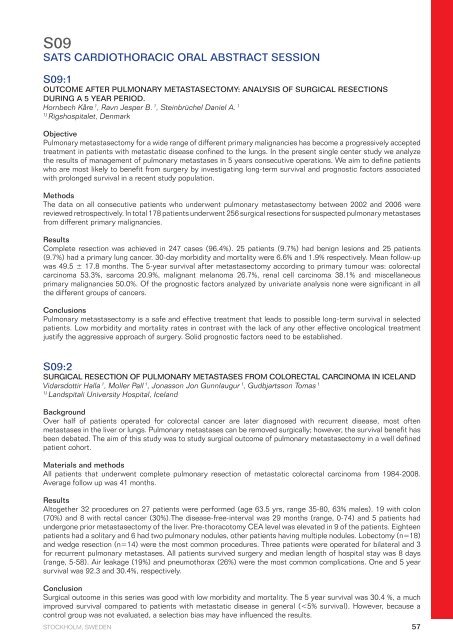
S09<br />
<strong>SATS</strong> CARDIOTHORACIC ORAL ABSTRACT SESSION<br />
S09:1<br />
OUTCOME AFTER PULMONARY METASTASECTOMY: ANALYSIS OF SURGICAL RESECTIONS<br />
DURING A 5 YEAR PERIOD.<br />
Hornbech Kåre 1 , Ravn Jesper B. 1 , Steinbrüchel Daniel A. 1<br />
1) Rigshospitalet, Denmark<br />
Objective<br />
Pulmonary metastasectomy <strong>for</strong> a wide range of different primary malignancies has become a progressively accepted<br />
treatment in patients with metastatic disease confined to the lungs. In the present single center study we analyze<br />
the results of management of pulmonary metastases in 5 years consecutive operations. We aim to define patients<br />
who are most likely to benefit from surgery by investigating long-term survival and prognostic factors associated<br />
with prolonged survival in a recent study population.<br />
Methods<br />
The data on all consecutive patients who underwent pulmonary metastasectomy between 2002 and 2006 were<br />
reviewed retrospectively. In total 178 patients underwent 256 surgical resections <strong>for</strong> suspected pulmonary metastases<br />
from different primary malignancies.<br />
Results<br />
Complete resection was achieved in 247 cases (96.4%). 25 patients (9.7%) had benign lesions and 25 patients<br />
(9.7%) had a primary lung cancer. 30-day morbidity and mortality were 6.6% and 1.9% respectively. Mean follow-up<br />
was 49.5 ± 17.8 months. The 5-year survival after metastasectomy according to primary tumour was: colorectal<br />
carcinoma 53.3%, sarcoma 20.9%, malignant melanoma 26.7%, renal cell carcinoma 38.1% and miscellaneous<br />
primary malignancies 50.0%. Of the prognostic factors analyzed by univariate analysis none were significant in all<br />
the different groups of cancers.<br />
Conclusions<br />
Pulmonary metastasectomy is a safe and effective treatment that leads to possible long-term survival in selected<br />
patients. Low morbidity and mortality rates in contrast with the lack of any other effective oncological treatment<br />
justify the aggressive approach of surgery. Solid prognostic factors need to be established.<br />
S09:2<br />
SURGICAL RESECTION OF PULMONARY METASTASES FROM COLORECTAL CARCINOMA IN ICELAND<br />
Vidarsdottir Halla 1 , Moller Pall 1 , Jonasson Jon Gunnlaugur 1 , Gudbjartsson Tomas 1<br />
1) Landspitali University Hospital, Iceland<br />
Background<br />
Over half of patients operated <strong>for</strong> colorectal cancer are later diagnosed with recurrent disease, most often<br />
metastases in the liver or lungs. Pulmonary metastases can be removed surgically; however, the survival benefit has<br />
been debated. The aim of this study was to study surgical outcome of pulmonary metastasectomy in a well defined<br />
patient cohort.<br />
Materials and methods<br />
All patients that underwent complete pulmonary resection of metastatic colorectal carcinoma from 1984-2008.<br />
Average follow up was 41 months.<br />
Results<br />
Altogether 32 procedures on 27 patients were per<strong>for</strong>med (age 63.5 yrs, range 35-80, 63% males). 19 with colon<br />
(70%) and 8 with rectal cancer (30%).The disease-free-interval was 29 months (range, 0-74) and 5 patients had<br />
undergone prior metastasectomy of the liver. Pre-thoracotomy CEA level was elevated in 9 of the patients. Eighteen<br />
patients had a solitary and 6 had two pulmonary nodules, other patients having multiple nodules. Lobectomy (n=18)<br />
and wedge resection (n=14) were the most common procedures. Three patients were operated <strong>for</strong> bilateral and 3<br />
<strong>for</strong> recurrent pulmonary metastases. All patients survived surgery and median length of hospital stay was 8 days<br />
(range, 5-58). Air leakage (19%) and pneumothorax (26%) were the most common complications. One and 5 year<br />
survival was 92.3 and 30.4%, respectively.<br />
Conclusion<br />
Surgical outcome in this series was good with low morbidity and mortality. The 5 year survival was 30.4 %, a much<br />
improved survival compared to patients with metastatic disease in general (