Ground glass opacity on CT scanning of the chest: What does it mean?
Ground glass opacity on CT scanning of the chest: What does it mean?
Ground glass opacity on CT scanning of the chest: What does it mean?
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
G round<br />
<str<strong>on</strong>g>Ground</str<strong>on</strong>g> <str<strong>on</strong>g>glass</str<strong>on</strong>g> <str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> <strong>on</strong><br />
<strong>CT</strong> <strong>scanning</strong> <strong>of</strong> <strong>the</strong> <strong>chest</strong>:<br />
<strong>What</strong> <strong>does</strong> <strong>it</strong> <strong>mean</strong>?<br />
<str<strong>on</strong>g>glass</str<strong>on</strong>g> <str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> (GGO) is<br />
described as a “hazy increased<br />
attenuati<strong>on</strong> <strong>of</strong> lung, w<strong>it</strong>h preservati<strong>on</strong><br />
<strong>of</strong> br<strong>on</strong>chial and vascular margins;<br />
<strong>it</strong> is caused by partial filling <strong>of</strong> air<br />
spaces, interst<strong>it</strong>ial thickening, partial<br />
collapse <strong>of</strong> alveoli, normal expirati<strong>on</strong>, or<br />
increased capillary blood volume.” 1<br />
GGO is a n<strong>on</strong>specific finding, and <strong>the</strong><br />
differential diagnosis <strong>of</strong> <strong>the</strong> many<br />
causes <strong>of</strong> GGO can be lengthy. An<br />
“ABCs” approach and a “pattern”<br />
approach to <strong>the</strong> interpretati<strong>on</strong> <strong>of</strong> GGO<br />
<strong>on</strong> HR<strong>CT</strong> <strong>scanning</strong> <strong>of</strong> <strong>the</strong> lungs have<br />
previously been described. 2,3 This paper<br />
provides an abbreviated review <strong>of</strong> <strong>the</strong><br />
physiologic correlates <strong>of</strong> <strong>the</strong> HR<strong>CT</strong> scan<br />
findings <strong>of</strong> GGO, focusing <strong>on</strong> infiltrative<br />
processes and <strong>the</strong>ir different GGO<br />
patterns <strong>of</strong> presentati<strong>on</strong>.<br />
GGO can be patchy, resulting in a<br />
mosaic pattern <strong>of</strong> lung attenuati<strong>on</strong>.<br />
Such a pattern can be seen in infiltrative<br />
lung disease, airway abnormal<strong>it</strong>ies<br />
(e.g., asthma, br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans),<br />
and chr<strong>on</strong>ic pulm<strong>on</strong>ary vascular disease<br />
(e.g., chr<strong>on</strong>ic thromboembolic disease).<br />
4 The distincti<strong>on</strong> between <strong>the</strong>se<br />
three ent<strong>it</strong>ies can be made by observing<br />
<strong>the</strong> size <strong>of</strong> <strong>the</strong> pulm<strong>on</strong>ary vessels in <strong>the</strong><br />
area <strong>of</strong> increased lung attenuati<strong>on</strong><br />
(increased in both airway disease and<br />
vascular disease, but not in infiltrative<br />
disease), and by examining air trapping<br />
<strong>on</strong> expiratory scans (indicating airway<br />
disease) (figure 1).<br />
Dr. Collins is in <strong>the</strong> Department <strong>of</strong> Radiology<br />
at <strong>the</strong> Univers<strong>it</strong>y <strong>of</strong> Wisc<strong>on</strong>sin Hosp<strong>it</strong>al<br />
and Clinics, in Madis<strong>on</strong>, WI. Dr.<br />
Stern is in <strong>the</strong> Department <strong>of</strong> Radiology<br />
at Harborview Medical Center, Univers<strong>it</strong>y<br />
<strong>of</strong> Washingt<strong>on</strong> in Seattle, WA.<br />
APPLIED RADIOLOGY, December 1998<br />
Jannette Collins, MD and Eric J. Stern, MD<br />
P<strong>it</strong>falls in <strong>the</strong> interpretati<strong>on</strong> <strong>of</strong> GGO <strong>on</strong><br />
<strong>CT</strong> <strong>scanning</strong><br />
As recogn<strong>it</strong>i<strong>on</strong> <strong>of</strong> GGO is based <strong>on</strong> a<br />
subjective assessment <strong>of</strong> lung attenuati<strong>on</strong>,<br />
<strong>it</strong> is important to understand <strong>the</strong><br />
parameters that can interfere w<strong>it</strong>h lung<br />
dens<strong>it</strong>y and make attenuati<strong>on</strong> measurements<br />
unreliable. 5,6 Window widths and<br />
levels that are too narrow can err<strong>on</strong>eously<br />
create <strong>the</strong> appearance <strong>of</strong> GGO<br />
by artificially “blooming” small structures.<br />
In evaluating for GGO, collimati<strong>on</strong><br />
ideally should be 1.0 to 1.5 mm.<br />
True GGO can not always be visualized<br />
w<strong>it</strong>h a thicker collimati<strong>on</strong> because <strong>of</strong><br />
volume averaging, and a thicker collimati<strong>on</strong><br />
sometimes results in a pseudo-GGO<br />
pattern. GGO is <strong>the</strong>refore best imaged<br />
w<strong>it</strong>h high-resoluti<strong>on</strong> <strong>CT</strong> (HR<strong>CT</strong>).<br />
Lung attenuati<strong>on</strong> normally increases<br />
homogeneously w<strong>it</strong>h expirati<strong>on</strong>. This<br />
increased attenuati<strong>on</strong> can obscure<br />
underlying pathologic GGO. Fur<strong>the</strong>rmore,<br />
if <strong>the</strong> expiratory nature <strong>of</strong> <strong>the</strong><br />
A B<br />
examinati<strong>on</strong> is not recognized, an err<strong>on</strong>eous<br />
interpretati<strong>on</strong> <strong>of</strong> pathologic GGO<br />
can be made.<br />
Cardiac and respiratory moti<strong>on</strong> also<br />
can create pseudo-GGO, which can be<br />
distinguished from pathologic GGO by<br />
recognizing <strong>the</strong> blurring and double<br />
images <strong>of</strong> vessels and fissures. GGO in<br />
<strong>the</strong> grav<strong>it</strong>y dependent porti<strong>on</strong>s <strong>of</strong> <strong>the</strong><br />
lungs is <strong>of</strong>ten seen as a result <strong>of</strong> microatelectasis,<br />
which can be differentiated<br />
from pathologic GGO by re-<strong>scanning</strong><br />
<strong>the</strong> area <strong>of</strong> questi<strong>on</strong> w<strong>it</strong>h <strong>the</strong> patient in<br />
<strong>the</strong> pr<strong>on</strong>e pos<strong>it</strong>i<strong>on</strong>.<br />
Infiltrative processes resulting in GGO<br />
Many patterns <strong>of</strong> distributi<strong>on</strong> <strong>of</strong><br />
ground <str<strong>on</strong>g>glass</str<strong>on</strong>g> <str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> can be seen <strong>on</strong><br />
HR<strong>CT</strong> <strong>of</strong> <strong>the</strong> lungs. It is important to<br />
emphasize that most such disease<br />
processes can and do result in more than<br />
<strong>on</strong>e pattern, <strong>of</strong>ten simultaneously; <strong>the</strong><br />
patterns change depending up<strong>on</strong> <strong>the</strong><br />
acu<strong>it</strong>y or chr<strong>on</strong>ic<strong>it</strong>y <strong>of</strong> <strong>the</strong> disease<br />
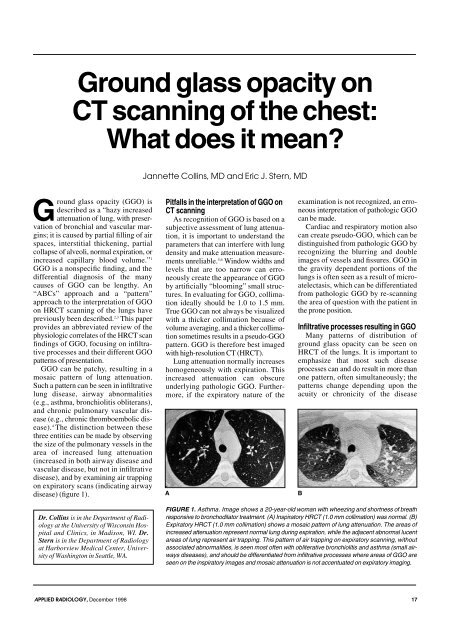
FIGURE 1. Asthma. Image shows a 20-year-old woman w<strong>it</strong>h wheezing and shortness <strong>of</strong> breath<br />
resp<strong>on</strong>sive to br<strong>on</strong>chodilator treatment. (A) Inspiratory HR<strong>CT</strong> (1.0 mm collimati<strong>on</strong>) was normal. (B)<br />
Expiratory HR<strong>CT</strong> (1.0 mm collimati<strong>on</strong>) shows a mosaic pattern <strong>of</strong> lung attenuati<strong>on</strong>. The areas <strong>of</strong><br />
increased attenuati<strong>on</strong> represent normal lung during expirati<strong>on</strong>, while <strong>the</strong> adjacent abnormal lucent<br />
areas <strong>of</strong> lung represent air trapping. This pattern <strong>of</strong> air trapping <strong>on</strong> expiratory <strong>scanning</strong>, w<strong>it</strong>hout<br />
associated abnormal<strong>it</strong>ies, is seen most <strong>of</strong>ten w<strong>it</strong>h obl<strong>it</strong>erative br<strong>on</strong>chiol<strong>it</strong>is and asthma (small airways<br />
diseases), and should be differentiated from infiltrative processes where areas <strong>of</strong> GGO are<br />
seen <strong>on</strong> <strong>the</strong> inspiratory images and mosaic attenuati<strong>on</strong> is not accentuated <strong>on</strong> expiratory imaging.<br />
17
Causes <strong>of</strong> a diffuse pattern <strong>of</strong><br />
GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong><br />
• Acute rejecti<strong>on</strong> <strong>of</strong> lung<br />
transplantati<strong>on</strong><br />
• Adult respiratory distress syndrome<br />
• Edema<br />
• Extrinsic allergic alveol<strong>it</strong>is<br />
• Hemorrhage<br />
• Infectious pneum<strong>on</strong>ia<br />
Table 1 FIGURE 2. Acute rejecti<strong>on</strong> <strong>of</strong> lung transplantati<strong>on</strong>.<br />
A 38-year-old man presents w<strong>it</strong>h increasing<br />
shortness <strong>of</strong> breath 3 weeks after<br />
process. We have categorized <strong>the</strong> etiologies<br />
<strong>of</strong> GGO according to <strong>the</strong> most comm<strong>on</strong>ly<br />
seen patterns <strong>of</strong> distributi<strong>on</strong>:<br />
Diffuse pattern <strong>of</strong> GGO—Disease<br />
processes comm<strong>on</strong>ly resulting in a diffuse<br />
pattern <strong>of</strong> GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong><br />
are listed in table 1. Acute rejecti<strong>on</strong> is<br />
comm<strong>on</strong> after lung transplantati<strong>on</strong>.<br />
However, differentiating between<br />
reperfusi<strong>on</strong> edema, infecti<strong>on</strong>, and rejecti<strong>on</strong><br />
can be difficult both clinically and<br />
radiographically. HR<strong>CT</strong> is reported to<br />
be 65% sens<strong>it</strong>ive and 85% specific in<br />
making <strong>the</strong> diagnosis <strong>of</strong> acute rejecti<strong>on</strong><br />
in <strong>the</strong> lung transplant populati<strong>on</strong>. 7 The<br />
<strong>on</strong>ly significant HR<strong>CT</strong> finding in acute<br />
rejecti<strong>on</strong> (seen in 65% <strong>of</strong> <strong>the</strong>se patients)<br />
is GGO, which is patchy and localized<br />
in mild rejecti<strong>on</strong> and widespread in<br />
severe rejecti<strong>on</strong> (figure 2). The main<br />
differential diagnosis in this group <strong>of</strong><br />
patients is cytomegalovirus pneum<strong>on</strong>ia,<br />
which can have an identical radiographic<br />
appearance.<br />
Adult respiratory distress syndrome<br />
(ARDS) is a form <strong>of</strong> n<strong>on</strong>hydrostatic pulm<strong>on</strong>ary<br />
edema, characterized by leaky<br />
capillary membranes. These leaks lead<br />
to extravasati<strong>on</strong> <strong>of</strong> protein-rich fluid into<br />
<strong>the</strong> interst<strong>it</strong>ial and alveolar spaces <strong>of</strong> <strong>the</strong><br />
lung. Am<strong>on</strong>g <strong>the</strong> comm<strong>on</strong> causes <strong>of</strong><br />
ARDS are aspirati<strong>on</strong>, c<strong>on</strong>tusi<strong>on</strong>, smoke<br />
inhalati<strong>on</strong>, and sepsis. <strong>CT</strong> scan findings<br />
<strong>of</strong> ARDS include bilateral and grav<strong>it</strong>ydependent<br />
lung opac<strong>it</strong>ies. 8 Early in <strong>the</strong><br />
course <strong>of</strong> ARDS, all patients dem<strong>on</strong>strate<br />
GGO <strong>on</strong> <strong>CT</strong>, which persists <strong>on</strong> follow-up<br />
<strong>CT</strong> in 50% <strong>of</strong> patients (figure 3). 9<br />
Both cardiogenic and n<strong>on</strong>-cardiogenic<br />
edema occurs when <strong>the</strong> capac<strong>it</strong>y<br />
<strong>of</strong> <strong>the</strong> lung lymphatics to drain capillary<br />
transudate is exceeded. Etiologies<br />
include venous and lymphatic obstructi<strong>on</strong>,<br />
increased capillary permeabil<strong>it</strong>y,<br />
and hypoproteinemia. 5 HR<strong>CT</strong> scan find-<br />
bilateral lung transplantati<strong>on</strong>. HR<strong>CT</strong> (1.0 mm<br />
collimati<strong>on</strong>) shows diffuse bilateral GGO, correlating<br />
w<strong>it</strong>h a pathologic diagnosis <strong>of</strong> severe<br />
acute rejecti<strong>on</strong>.<br />
FiGURE 3. Early adult respiratory distress<br />
syndrome (ARDS). A 12-year-old boy w<strong>it</strong>h<br />
acute shortness <strong>of</strong> breath and hypoxemia,<br />
requiring intubati<strong>on</strong> and mechanical ventilati<strong>on</strong><br />
after receiving chemo<strong>the</strong>rapy for lymphoma.<br />
HR<strong>CT</strong> (1.0 mm collimati<strong>on</strong>) shows<br />
diffuse bilateral GGO. Pulm<strong>on</strong>ary artery<br />
wedge pressure was normal, and transbr<strong>on</strong>chial<br />
lung biopsy and br<strong>on</strong>choalveolar<br />
lavage showed no evidence <strong>of</strong> infecti<strong>on</strong>.<br />
The patient went <strong>on</strong> to develop severe<br />
ARDS w<strong>it</strong>h complicati<strong>on</strong>s <strong>of</strong> barotrauma.<br />
ings in patients w<strong>it</strong>h hydrostatic pulm<strong>on</strong>ary<br />
edema include areas <strong>of</strong> GGO,<br />
interlobular septal thickening, peribr<strong>on</strong>chovascular<br />
interst<strong>it</strong>ial thickening,<br />
increased vascular caliber, pleural effusi<strong>on</strong>,<br />
and thickening <strong>of</strong> fissures. 10<br />
Extrinsic allergic alveol<strong>it</strong>is, also<br />
called hypersens<strong>it</strong>iv<strong>it</strong>y pneum<strong>on</strong><strong>it</strong>is, is<br />
a complex immunologic reacti<strong>on</strong> by<br />
<strong>the</strong> lung, primarily to inhaled organic<br />
antigens. The clinical presentati<strong>on</strong> may<br />
be acute, subacute, or chr<strong>on</strong>ic. HR<strong>CT</strong><br />
scan findings will vary w<strong>it</strong>h <strong>the</strong> stage<br />
<strong>of</strong> disease. In <strong>the</strong> acute and subacute<br />
phases, findings include GGO (in<br />
82%), small nodules (55%), a reticular<br />
pattern (36%), and air trapping. 11 GGO<br />
FIGURE 4. Extrinsic allergic alveol<strong>it</strong>is.<br />
Imaging <strong>of</strong> a 50-year-old farmer w<strong>it</strong>h an<br />
acute <strong>on</strong>set <strong>of</strong> increasing shortness <strong>of</strong><br />
breath. HR<strong>CT</strong> (1.0 mm collimati<strong>on</strong>) shows<br />
diffuse bilateral GGO, correlating w<strong>it</strong>h <strong>the</strong><br />
clinical diagnosis <strong>of</strong> acute farmer’s lung.<br />
FIGURE 5. Diffuse alveolar hemorrhage. A<br />
45-year-old man presents w<strong>it</strong>h increasing<br />
shortness <strong>of</strong> breath 2 m<strong>on</strong>ths after b<strong>on</strong>e marrow<br />
transplantati<strong>on</strong>. Helical <strong>CT</strong> scan (10 mm<br />
collimati<strong>on</strong>) shows diffuse bilateral GGO.<br />
correlates histologically w<strong>it</strong>h m<strong>on</strong><strong>on</strong>uclear<br />
cell infiltrati<strong>on</strong> <strong>of</strong> <strong>the</strong> alveolar<br />
walls. 11 The distributi<strong>on</strong> <strong>of</strong> GGO can be<br />
diffuse, patchy, or centrilobular (figure<br />
4) in this c<strong>on</strong>d<strong>it</strong>i<strong>on</strong>.<br />
Pulm<strong>on</strong>ary hemorrhage can be diffuse,<br />
patchy, or focal, depending <strong>on</strong> <strong>the</strong> underlying<br />
cause, <strong>of</strong> which <strong>the</strong>re are many. 12 In<br />
<strong>the</strong> acute phase, <strong>CT</strong> scans show c<strong>on</strong>solidati<strong>on</strong><br />
or GGO (figure 5). In <strong>the</strong> subacute<br />
phase, <strong>CT</strong> shows 1- to 3-mm nodules that<br />
are distributed in a uniform fashi<strong>on</strong>, comm<strong>on</strong>ly<br />
accompanied by GGO and interlobular<br />
septal thickening. 13<br />
Infectious pneum<strong>on</strong>ia <strong>of</strong> any cause<br />
(e.g., bacterial, viral, mycobacterial, fungal,<br />
and paras<strong>it</strong>ic) can cause GGO to<br />
appear <strong>on</strong> HR<strong>CT</strong> scans. A diffuse pattern<br />
<strong>of</strong> GGO in <strong>the</strong> absence <strong>of</strong> associated <strong>CT</strong><br />
scan findings is a characteristic presentati<strong>on</strong><br />
for cytomegalovirus pneum<strong>on</strong>ia<br />
(CMV) and Pneumocystis carinii pneum<strong>on</strong>ia<br />
(PCP). CMV is <strong>the</strong> most comm<strong>on</strong><br />
viral pathogen to cause substantial mor-<br />
18 APPLIED RADIOLOGY, December 1998
Causes <strong>of</strong> a patchy pattern <strong>of</strong><br />
GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong><br />
• Acute rejecti<strong>on</strong> <strong>of</strong> lung<br />
transplantati<strong>on</strong><br />
• Adult respiratory distress syndrome<br />
• Br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans organizing<br />
pneum<strong>on</strong>ia (BOOP)<br />
• Br<strong>on</strong>chioloalveolar cell carcinoma<br />
• Extrinsic allergic alveol<strong>it</strong>is<br />
• Hemorrhage<br />
• Infectious pneum<strong>on</strong>ia<br />
• Pulm<strong>on</strong>ary alveolar proteinosis<br />
Table 2<br />
bid<strong>it</strong>y and mortal<strong>it</strong>y in patients w<strong>it</strong>h<br />
AIDS, 14 and is a relatively comm<strong>on</strong> complicati<strong>on</strong><br />
in organ transplant recipients. In<br />
patients w<strong>it</strong>h AIDS and CMV pneum<strong>on</strong>ia,<br />
<strong>CT</strong> <strong>scanning</strong> will show GGO, dense<br />
c<strong>on</strong>solidati<strong>on</strong>, br<strong>on</strong>chial wall thickening<br />
or br<strong>on</strong>chiectasis, and interst<strong>it</strong>ial reticulati<strong>on</strong><br />
w<strong>it</strong>hout air-space disease (although<br />
GGO may occur in isolati<strong>on</strong>). 15 In organ<br />
transplant recipients w<strong>it</strong>h CMV pneum<strong>on</strong>ia,<br />
<strong>CT</strong> <strong>scanning</strong> shows small nodules,<br />
c<strong>on</strong>solidati<strong>on</strong>, GGO, and irregular lines<br />
(figure 6). The presence <strong>of</strong> an isolated<br />
ground <str<strong>on</strong>g>glass</str<strong>on</strong>g> infiltrate w<strong>it</strong>hout add<strong>it</strong>i<strong>on</strong>al<br />
findings in patients w<strong>it</strong>h AIDS is highly<br />
suggestive <strong>of</strong> PCP(figure 7). 16<br />
Patchy GGO patterns—Many <strong>of</strong> <strong>the</strong><br />
causes <strong>of</strong> a patchy distributi<strong>on</strong> <strong>of</strong> GGO<br />
<strong>on</strong> HR<strong>CT</strong> <strong>scanning</strong>, listed in table 2,<br />
may also result in a diffuse pattern <strong>of</strong><br />
GGO. Pulm<strong>on</strong>ary alveolar proteinosis is<br />
a disease <strong>of</strong> <strong>the</strong> lung that results in filling<br />
in <strong>of</strong> <strong>the</strong> alveoli by a periodic acid-<br />
Schiff-pos<strong>it</strong>ive proteinaceous material<br />
that is rich in lipid. 17,18 HR<strong>CT</strong> <strong>scanning</strong><br />
<strong>of</strong> this disorder shows GGO, w<strong>it</strong>h an<br />
overlying branching pattern <strong>of</strong> wh<strong>it</strong>e<br />
linear structures forming geometric<br />
shapes and outlining polyg<strong>on</strong>al, triangular,<br />
and square forms. 19,20 This pattern is<br />
<strong>of</strong>ten referred to as “crazy paving,” and<br />
is characteristic, but not pathognom<strong>on</strong>ic,<br />
<strong>of</strong> <strong>the</strong> diagnosis <strong>of</strong> alveolar proteinosis<br />
(figure 8). 21 O<strong>the</strong>r processes that<br />
can show a crazy paving pattern at<br />
HR<strong>CT</strong> <strong>scanning</strong> include ARDS, lipoid<br />
pneum<strong>on</strong>ia, and PCP.<br />
Focal GGO patterns—There is overlap<br />
between causes <strong>of</strong> diffuse, patchy,<br />
and focal distributi<strong>on</strong>s <strong>of</strong> GGO (table 3)<br />
w<strong>it</strong>h <strong>chest</strong> <strong>CT</strong> <strong>scanning</strong>. When pulm<strong>on</strong>ary<br />
hemorrhage is due to focal neo-<br />
APPLIED RADIOLOGY, December 1998<br />
FIGURE 6. Cytomegalovirus pneum<strong>on</strong>ia.<br />
Imaging <strong>of</strong> a 42-year-old man w<strong>it</strong>h acute<br />
respiratory symptoms 3 m<strong>on</strong>ths after b<strong>on</strong>e<br />
marrow transplantati<strong>on</strong>. Helical <strong>CT</strong> scan<br />
(10 mm collimati<strong>on</strong>) shows diffuse bilateral<br />
GGO, areas <strong>of</strong> septal thickening (straight<br />
arrows), and ill-defined small nodular opac<strong>it</strong>ies<br />
(curved arrows). Small bilateral pleural<br />
effusi<strong>on</strong>s are present.<br />
FIGURE 7. Pneumocystis carinii pneum<strong>on</strong>ia<br />
in a 39-year-old man w<strong>it</strong>h AIDS. HR<strong>CT</strong><br />
(1.5 mm collimati<strong>on</strong>) shows patchy bilateral<br />
areas <strong>of</strong> GGO and a small cystic lesi<strong>on</strong> in<br />
<strong>the</strong> left upper lobe (arrows).<br />
plasm, trauma, or pulm<strong>on</strong>ary infarcti<strong>on</strong>,<br />
a focal pattern <strong>of</strong> <str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> results. Certain<br />
infecti<strong>on</strong>s, such as lobar pneum<strong>on</strong>ia, also<br />
may result in a focal pattern <strong>of</strong> GGO.<br />
Br<strong>on</strong>choalveolar lavage is a procedure<br />
used to diagnose pulm<strong>on</strong>ary diseases and<br />
to identify predictors <strong>of</strong> prognosis. The<br />
technique involves injecti<strong>on</strong> <strong>of</strong> normal<br />
saline through a br<strong>on</strong>choscope that is<br />
generally wedged into <strong>the</strong> lingular or<br />
middle lobe br<strong>on</strong>chus. Most, but not all<br />
<strong>of</strong> <strong>the</strong> fluid is aspirated back into <strong>the</strong><br />
scope and examined for inflammatory<br />
and immune mediator cells and specific<br />
proteins. 22 The residual fluid dem<strong>on</strong>strates<br />
a segmental or lobar distributi<strong>on</strong><br />
<strong>of</strong> GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong>, which should<br />
suggest <strong>the</strong> possibil<strong>it</strong>y <strong>of</strong> recent br<strong>on</strong>choalveolar<br />
lavage, especially if <strong>the</strong><br />
GGO is observed in <strong>the</strong> right middle lobe<br />
or lingula. 5<br />
The “halo” pattern <strong>of</strong> GGO—A<br />
“halo” <strong>of</strong> GGO occasi<strong>on</strong>ally can be seen<br />
around a nodule or focal area <strong>of</strong> lung<br />
FIGURE 8. Lipoid pneum<strong>on</strong>ia. Image is <strong>of</strong> a<br />
46-year-old man w<strong>it</strong>h a 6-m<strong>on</strong>th history <strong>of</strong><br />
mild dyspnea and chr<strong>on</strong>ic rhin<strong>it</strong>is, treated<br />
w<strong>it</strong>h oily nose drops. HR<strong>CT</strong> (1.0 mm collimati<strong>on</strong>)<br />
shows bilateral patchy areas <strong>of</strong><br />
GGO w<strong>it</strong>h a background <strong>of</strong> intralobular and<br />
interlobular septal thickening, producing <strong>the</strong><br />
“crazy paving” pattern first described w<strong>it</strong>h<br />
alveolar proteinosis. (Figure courtesy <strong>of</strong><br />
Tomas Franquet, MD, Barcel<strong>on</strong>a, Spain.)<br />
FIGURE 9. Invasive aspergillosis. Image is <strong>of</strong> a<br />
49-year-old man w<strong>it</strong>h acute myelogenous<br />
leukemia and fever. Helical <strong>CT</strong> scan (7.0 mm<br />
collimati<strong>on</strong>) shows a triangular area <strong>of</strong> c<strong>on</strong>solidati<strong>on</strong><br />
abutting <strong>the</strong> peripheral right lung and<br />
involving both <strong>the</strong> right middle and lower lobes.<br />
This distributi<strong>on</strong> and shape is characteristic <strong>of</strong><br />
hemorrhagic infarcti<strong>on</strong> caused by <strong>the</strong> angioinvasive<br />
fungal agent aspergillosis. The surrounding<br />
GGO, creating <strong>the</strong> “halo sign”,<br />
represents hemorrhage and is highly specific for<br />
early invasive aspergillosis in leukemic patients.<br />
c<strong>on</strong>solidati<strong>on</strong>. Table 4 lists <strong>the</strong> processes<br />
known to produce <strong>the</strong> halo sign. It was<br />
first reported as a sign <strong>of</strong> early invasive<br />
pulm<strong>on</strong>ary aspergillosis in patients w<strong>it</strong>h<br />
leukemia. 23 The GGO represents a<br />
Causes <strong>of</strong> a focal pattern <strong>of</strong> GGO<br />
<strong>on</strong> <strong>CT</strong> <strong>scanning</strong><br />
• Br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans organizing<br />
pneum<strong>on</strong>ia (BOOP)<br />
• Br<strong>on</strong>choalveolar lavage<br />
• Br<strong>on</strong>chioloalveolar cell carcinoma<br />
• Hemorrhage<br />
• Pulm<strong>on</strong>ary infecti<strong>on</strong><br />
Table 3<br />
19
FIGURE 10. Br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans organizing<br />
pneum<strong>on</strong>ia. Image is <strong>of</strong> a 50-year-old<br />
man w<strong>it</strong>h increasing shortness <strong>of</strong> breath after<br />
bilateral lung transplantati<strong>on</strong>. HR<strong>CT</strong> (1.0 mm<br />
collimati<strong>on</strong>) shows bilateral patchy areas <strong>of</strong><br />
GGO in both a br<strong>on</strong>chovascular and peripheral<br />
distributi<strong>on</strong>.<br />
FIGURE 11. C<strong>on</strong>tusi<strong>on</strong>s. Image is <strong>of</strong> a 22year-old<br />
man involved in a motor vehicle accident.<br />
Helical <strong>CT</strong> scan (10 mm collimati<strong>on</strong>)<br />
shows bilateral areas <strong>of</strong> GGO and c<strong>on</strong>solidati<strong>on</strong><br />
in a typical peripheral n<strong>on</strong>-segmental distributi<strong>on</strong>.<br />
There are both posterior and anterior<br />
rib fractures adjacent to <strong>the</strong> s<strong>it</strong>es <strong>of</strong> c<strong>on</strong>tusi<strong>on</strong>.<br />
peripheral ring <strong>of</strong> hemorrhage or hemorrhagic<br />
infarcti<strong>on</strong> surrounding target<br />
lesi<strong>on</strong>s <strong>of</strong> pulm<strong>on</strong>ary aspergillosis (figure<br />
9). Several infectious and n<strong>on</strong>infectious<br />
causes <strong>of</strong> <strong>the</strong> <strong>CT</strong> halo sign have<br />
since been reported. 24 In most patients,<br />
hemorrhagic nodules can be distinguished<br />
from n<strong>on</strong>hemorrhagic nodules<br />
by <strong>the</strong> presence <strong>of</strong> a halo <strong>of</strong> GGO.<br />
Ano<strong>the</strong>r cause <strong>of</strong> focal GGO, or a<br />
nodule w<strong>it</strong>h a surrounding halo <strong>of</strong> GGO,<br />
is <strong>the</strong> post-biopsy pseudo nodule. These<br />
pseudo nodules have been described in<br />
Causes <strong>of</strong> a “halo” pattern <strong>of</strong><br />
GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong><br />
• Invasive pulm<strong>on</strong>ary aspergillosis<br />
• Neoplasm, hemorrhagic<br />
• Post-biopsy pseudo nodule<br />
Table 4<br />
FIGURE 12. Desquamative interst<strong>it</strong>ial pneum<strong>on</strong><strong>it</strong>is.<br />
Image is <strong>of</strong> a 77-year-old man w<strong>it</strong>h a<br />
3-m<strong>on</strong>th history <strong>of</strong> increasing shortness <strong>of</strong><br />
breath. HR<strong>CT</strong> (1.5 mm collimati<strong>on</strong>) shows<br />
bilateral areas <strong>of</strong> GGO and c<strong>on</strong>solidati<strong>on</strong> in a<br />
peripheral distributi<strong>on</strong> w<strong>it</strong>hout evidence <strong>of</strong><br />
h<strong>on</strong>eycombing or tracti<strong>on</strong> br<strong>on</strong>chiectasis.<br />
patients who have underg<strong>on</strong>e lung transplantati<strong>on</strong><br />
and transbr<strong>on</strong>chial lung<br />
biopsy, 25 but <strong>the</strong>y may be seen in any<br />
patient after lung biopsy.<br />
A peripheral pattern <strong>of</strong> GGO—<br />
Processes that are known to result in a<br />
peripheral lung distributi<strong>on</strong> <strong>of</strong> GGO<br />
w<strong>it</strong>h HR<strong>CT</strong> <strong>scanning</strong> are listed in table<br />
5. This particular distributi<strong>on</strong> pattern<br />
can be very helpful in narrowing <strong>the</strong> differential<br />
diagnosis, especially when<br />
combined w<strong>it</strong>h o<strong>the</strong>r clinical data and<br />
associated <strong>CT</strong> scan findings.<br />
Br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans organizing<br />
pneum<strong>on</strong>ia (BOOP) is a disease characterized<br />
histologically by <strong>the</strong> presence <strong>of</strong><br />
granulati<strong>on</strong> tissue plugs w<strong>it</strong>hin respiratory<br />
br<strong>on</strong>chioles and alveolar ducts, and<br />
organizing pneum<strong>on</strong>ia extending into<br />
<strong>the</strong> surrounding alveoli. 26 <strong>CT</strong> scans<br />
show patchy GGO (in 8 to 75% <strong>of</strong><br />
patients), nodules, or areas <strong>of</strong> c<strong>on</strong>solidati<strong>on</strong><br />
w<strong>it</strong>h a predominantly peripheral<br />
(50% <strong>of</strong> patients), bilateral, and n<strong>on</strong>segmental<br />
distributi<strong>on</strong> (figure 10). 27-29<br />
Collagen vascular diseases are multisystem<br />
disorders characterized by<br />
vascular changes, fibrosis, and inflammati<strong>on</strong><br />
<strong>of</strong> c<strong>on</strong>nective tissue. Specific<br />
diseases include progressive systemic<br />
sclerosis (scleroderma), systemic lupus<br />
ery<strong>the</strong>matosus, polymyos<strong>it</strong>is/dermatomyos<strong>it</strong>is,<br />
rheumatoid arthr<strong>it</strong>is, and Sjogren’s<br />
syndrome. GGO is seen <strong>on</strong> <strong>CT</strong><br />
<strong>scanning</strong> in 63 to 100% <strong>of</strong> <strong>the</strong>se<br />
patients, 30 and is a sign <strong>of</strong> active inflammati<strong>on</strong><br />
in <strong>the</strong> absence <strong>of</strong> significant h<strong>on</strong>eycombing,<br />
br<strong>on</strong>chiectasis, or o<strong>the</strong>r<br />
signs <strong>of</strong> lung fibrosis. 31<br />
Pulm<strong>on</strong>ary c<strong>on</strong>tusi<strong>on</strong> results from<br />
trauma to <strong>the</strong> <strong>chest</strong> wall and lung, w<strong>it</strong>h<br />
Causes <strong>of</strong> a peripheral pattern <strong>of</strong><br />
GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong><br />
• Br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans organizing<br />
pneum<strong>on</strong>ia (BOOP)<br />
• Collagen vascular disease<br />
• C<strong>on</strong>tusi<strong>on</strong><br />
• Desquamative interst<strong>it</strong>ial<br />
pneum<strong>on</strong><strong>it</strong>is<br />
• Drug toxic<strong>it</strong>y<br />
• Eosinophilic pneum<strong>on</strong>ia<br />
• Fibrosis<br />
• Sarcoidosis<br />
Table 5<br />
bleeding into <strong>the</strong> air spaces and lung<br />
interst<strong>it</strong>ium. Generally, <strong>the</strong> cause is a<br />
compressi<strong>on</strong> injury w<strong>it</strong>h significant<br />
kinetic energy absorpti<strong>on</strong> adjacent to <strong>the</strong><br />
s<strong>it</strong>e <strong>of</strong> <strong>chest</strong> wall injury. The <strong>CT</strong> scan<br />
appearance <strong>of</strong> lung c<strong>on</strong>tusi<strong>on</strong> is that <strong>of</strong><br />
ill-defined areas <strong>of</strong> GGO, c<strong>on</strong>solidati<strong>on</strong>,<br />
or both, usually w<strong>it</strong>h a peripheral, n<strong>on</strong>anatomic<br />
distributi<strong>on</strong> (figure 11). 32,33<br />
Desquamative interst<strong>it</strong>ial pneum<strong>on</strong><strong>it</strong>is<br />
is characterized by alveolar filling w<strong>it</strong>h<br />
macrophages. The HR<strong>CT</strong> scan findings<br />
c<strong>on</strong>sist <strong>of</strong> GGO w<strong>it</strong>h a lower lung z<strong>on</strong>e<br />
(73%) and a peripheral (59%) predominant<br />
distributi<strong>on</strong> (figure 12). Usual interst<strong>it</strong>ial<br />
pneum<strong>on</strong><strong>it</strong>is, or idiopathic<br />
pulm<strong>on</strong>ary fibrosis, results in a similar<br />
distributi<strong>on</strong> <strong>of</strong> GGO <strong>on</strong> <strong>CT</strong> <strong>scanning</strong> but<br />
typically w<strong>it</strong>h more areas <strong>of</strong> h<strong>on</strong>eycombing<br />
and tracti<strong>on</strong> br<strong>on</strong>chiectasis<br />
(figure 13).<br />
Pulm<strong>on</strong>ary toxic<strong>it</strong>y has been associated<br />
w<strong>it</strong>h numerous drugs and a variety<br />
<strong>of</strong> radiographic and <strong>CT</strong> patterns. <strong>CT</strong><br />
<strong>scanning</strong> shows nodular areas <strong>of</strong> GGO<br />
and c<strong>on</strong>solidati<strong>on</strong>, <strong>of</strong>ten w<strong>it</strong>h a peripheral<br />
distributi<strong>on</strong>. 35,36<br />
Pulm<strong>on</strong>ary eosinophilia occurs w<strong>it</strong>h a<br />
variety <strong>of</strong> c<strong>on</strong>d<strong>it</strong>i<strong>on</strong>s or diseases, or can<br />
be idiopathic. Chr<strong>on</strong>ic idiopathic<br />
eosinophilic pneum<strong>on</strong>ia is characterized<br />
by multiple dense areas <strong>of</strong> <str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> <strong>on</strong><br />
<strong>chest</strong> radiographs and <strong>CT</strong> scans. In <strong>on</strong>e<br />
study <strong>of</strong> patients w<strong>it</strong>h chr<strong>on</strong>ic<br />
eosinophilic pneum<strong>on</strong>ia, <strong>the</strong> most comm<strong>on</strong><br />
HR<strong>CT</strong> finding was GGO, usually<br />
adjacent to areas <strong>of</strong> c<strong>on</strong>solidati<strong>on</strong>, w<strong>it</strong>h<br />
a peripheral distributi<strong>on</strong>. 37 Acute idiopathic<br />
eosinophilic pneum<strong>on</strong>ia is characterized<br />
by diffuse GGO and<br />
micr<strong>on</strong>odules <strong>on</strong> <strong>chest</strong> radiographs and<br />
<strong>CT</strong> scans, <strong>of</strong>ten in a br<strong>on</strong>chovascular<br />
distributi<strong>on</strong>. 38<br />
20 APPLIED RADIOLOGY, December 1998
FIGURE 13. Usual interst<strong>it</strong>ial pneum<strong>on</strong><strong>it</strong>is.<br />
Image is <strong>of</strong> a 78-year-old man w<strong>it</strong>h chr<strong>on</strong>ic<br />
progressive shortness <strong>of</strong> breath. HR<strong>CT</strong> (1.5<br />
mm collimati<strong>on</strong>) shows GGO associated w<strong>it</strong>h<br />
h<strong>on</strong>eycombing and tracti<strong>on</strong> br<strong>on</strong>chiectasis in<br />
a peripheral and bibasilar distributi<strong>on</strong>. In this<br />
case, <strong>the</strong> GGO likely reflects micr<strong>of</strong>ibrosis.<br />
Sarcoidosis is a multisystemic disorder<br />
<strong>of</strong> unknown cause characterized by<br />
<strong>the</strong> presence <strong>of</strong> n<strong>on</strong>caseating granulomatous<br />
inflammati<strong>on</strong> affecting various<br />
s<strong>it</strong>es <strong>of</strong> <strong>the</strong> body, w<strong>it</strong>h a propens<strong>it</strong>y to<br />
involve <strong>the</strong> respiratory tract. The most<br />
comm<strong>on</strong> HR<strong>CT</strong> scan findings <strong>of</strong> pulm<strong>on</strong>ary<br />
sarcoidosis are irregularly thickened<br />
br<strong>on</strong>chovascular bundles (88%)<br />
and small nodules al<strong>on</strong>g vessels (50%). 39<br />
GGO is present in 75% <strong>of</strong> patients w<strong>it</strong>h<br />
sarcoidosis, which corresp<strong>on</strong>ds histologically<br />
w<strong>it</strong>h many granulomatous lesi<strong>on</strong>s,<br />
w<strong>it</strong>h or w<strong>it</strong>hout perigranulomatous<br />
fibrosis, in <strong>the</strong> interst<strong>it</strong>ium and alveolar<br />
septa around small vessels. Sarcoidosis<br />
can result in a predominantly peripheral<br />
distributi<strong>on</strong> <strong>of</strong> GGO and/or c<strong>on</strong>solidati<strong>on</strong>,<br />
or a diffuse or patchy pattern <strong>of</strong><br />
<strong>on</strong>ly GGO (figures 14 and 15).<br />
Br<strong>on</strong>chovascular and centrilobular<br />
patterns <strong>of</strong> GGO—Processes that can<br />
result in GGO in a predominantly br<strong>on</strong>chovascular<br />
distributi<strong>on</strong> include eosinophilic<br />
pneum<strong>on</strong>ia and sarcoidosis. A<br />
predominantly centrilobular distributi<strong>on</strong><br />
<strong>of</strong> GGO has been described w<strong>it</strong>h both<br />
extrinsic allergic alveol<strong>it</strong>is and respiratory<br />
br<strong>on</strong>chiol<strong>it</strong>is. All reported cases <strong>of</strong><br />
respiratory br<strong>on</strong>chiol<strong>it</strong>is have occurred in<br />
cigarette smokers. 40-42 In <strong>the</strong> major<strong>it</strong>y <strong>of</strong><br />
<strong>the</strong>se patients, HR<strong>CT</strong> shows GGO,<br />
which is <strong>of</strong>ten extensive, as <strong>the</strong> predominant<br />
finding. 43 Pigmented macrophages<br />
w<strong>it</strong>hin respiratory br<strong>on</strong>chioles and adjacent<br />
alveolar ducts and alveoli lead to <strong>the</strong><br />
br<strong>on</strong>chovascular distributi<strong>on</strong> <strong>of</strong> GGO.<br />
C<strong>on</strong>clusi<strong>on</strong><br />
GGO from infiltrative lung disease is<br />
a n<strong>on</strong>specific finding <strong>on</strong> HR<strong>CT</strong> scans<br />
APPLIED RADIOLOGY, December 1998<br />
FIGURE 14. Sarcoidosis. Image is <strong>of</strong> a 33year-old<br />
asymptomatic woman. HR<strong>CT</strong> (1.0<br />
mm collimati<strong>on</strong>) shows bilateral patchy areas<br />
<strong>of</strong> GGO. There were no enlarged lymph<br />
nodes or parenchymal nodules.<br />
FIGURE 15. Sarcoidosis. Image is <strong>of</strong> a 25year-old<br />
asymptomatic man. HR<strong>CT</strong> (1.0 mm<br />
collimati<strong>on</strong>) shows bilateral patchy areas <strong>of</strong><br />
GGO in a br<strong>on</strong>chovascular distributi<strong>on</strong>, some<br />
showing air br<strong>on</strong>chograms (arrows).<br />
<strong>of</strong> <strong>the</strong> <strong>chest</strong>, correlating histologically<br />
w<strong>it</strong>h partial filling <strong>of</strong> air spaces,<br />
inflammatory or fibrotic interst<strong>it</strong>ial<br />
thickening, or increased capillary<br />
blood volume. GGO also can represent<br />
mosaic perfusi<strong>on</strong> sec<strong>on</strong>dary to chr<strong>on</strong>ic<br />
vascular disease, or air trapping from<br />
small airways disease. It is important to<br />
correlate <strong>the</strong> HR<strong>CT</strong> pattern <strong>of</strong> GGO<br />
w<strong>it</strong>h clinical history and associated<br />
HR<strong>CT</strong> scan findings in developing a<br />
differential diagnosis. AR<br />
REFERENCES<br />
1. Austin JHM, Müller NL, Friedman PJ, et al:<br />
Glossary <strong>of</strong> terms for <strong>CT</strong> <strong>of</strong> <strong>the</strong> lungs: Recommendati<strong>on</strong>s<br />
<strong>of</strong> <strong>the</strong> Nomenclature Comm<strong>it</strong>tee <strong>of</strong> <strong>the</strong><br />
Fleischner Society. Radiology 200:327-331, 1996.<br />
2. Collins J, Stern EJ: <str<strong>on</strong>g>Ground</str<strong>on</strong>g>-<str<strong>on</strong>g>glass</str<strong>on</strong>g> <str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> at<br />
<strong>CT</strong>: The ABCs. AJR 169:355-367, 1997.<br />
3. Collins J, Stern EJ: Patterns <strong>of</strong> ground <str<strong>on</strong>g>glass</str<strong>on</strong>g><br />
<str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g> <strong>on</strong> <strong>CT</strong> <strong>scanning</strong> <strong>of</strong> <strong>the</strong> <strong>chest</strong>. Postgraduate<br />
Radiology. In press.<br />
4. Stern EJ, Swensen SJ, Hartman TE, Frank<br />
MS: <strong>CT</strong> mosaic pattern <strong>of</strong> lung attenuati<strong>on</strong>: Distinguishing<br />
different causes. AJR 165:813-816, 1995.<br />
5. Remy-Jardin M, Remy J, Giraud F, et al: Computed<br />
tomography assessment <strong>of</strong> ground-<str<strong>on</strong>g>glass</str<strong>on</strong>g><br />
<str<strong>on</strong>g>opac<strong>it</strong>y</str<strong>on</strong>g>: Semiology and significance. J Thorac<br />
Imaging 8:249-264, 1993.<br />
6. Primack SL, Remy-Jardin M, Remy J, Müller<br />
NL: High-resoluti<strong>on</strong> <strong>CT</strong> <strong>of</strong> <strong>the</strong> lung: P<strong>it</strong>falls in <strong>the</strong><br />
diagnosis <strong>of</strong> infiltrative lung disease. AJR 167:413-<br />
418, 1996.<br />
7. Loubeyre P, Revel D, Delignette A, et al: Highresoluti<strong>on</strong><br />
computed tomographic findings associated<br />
w<strong>it</strong>h histologically diagnosed acute lung<br />
rejecti<strong>on</strong> in heart/lung transplant recipients. Chest<br />
107:132-138, 1995.<br />
8. Tagliabue M, Casella TC, Zinc<strong>on</strong>e GE, et al:<br />
<strong>CT</strong> and <strong>chest</strong> radiography in <strong>the</strong> evaluati<strong>on</strong> <strong>of</strong> adult<br />
respiratory distress syndrome. Acta Radiol 35:230-<br />
234, 1994.<br />
9. Owens CM, Evans TW, Keogh BF, Hansell<br />
DM: Computed tomography in established adult<br />
respiratory distress syndrome: Correlati<strong>on</strong> w<strong>it</strong>h<br />
lung injury score. Chest 106:1815-1821, 1994.<br />
10. Storto ML, Kee ST, Golden JA, Webb WR:<br />
Hydrostatic pulm<strong>on</strong>ary edema: High-resoluti<strong>on</strong> <strong>CT</strong><br />
findings. AJR 165:817-820, 1995.<br />
11. Hansell DM, Wells AU, Padley SPG, Müller<br />
NL: Hypersens<strong>it</strong>iv<strong>it</strong>y pneum<strong>on</strong><strong>it</strong>is: Correlati<strong>on</strong> <strong>of</strong><br />
individual <strong>CT</strong> patterns w<strong>it</strong>h functi<strong>on</strong>al abnormal<strong>it</strong>ies.<br />
Radiology 199:123-128, 1996.<br />
12. Albelda SM, Gefter WB, Epstein DM, Miller<br />
WT: Diffuse pulm<strong>on</strong>ary hemorrhage: A review and<br />
classificati<strong>on</strong>. Radiology 154:289-297, 1985.<br />
13. Cheah FK, Sheppard MN, Hansell DM: Computed<br />
tomography <strong>of</strong> diffuse pulm<strong>on</strong>ary hemorrhage<br />
w<strong>it</strong>h pathological correlati<strong>on</strong>. Clin Radiol<br />
48:89-93, 1993.<br />
14. Wallace MJ, Hannah J: Cytomegalovirus<br />
pneum<strong>on</strong><strong>it</strong>is in patients w<strong>it</strong>h AIDS: Findings in an<br />
autopsy series. Chest 92:198-203, 1987.<br />
15. McGuinness G, Scholes JV, Garay SM, et al:<br />
Cytomegalovirus pneum<strong>on</strong><strong>it</strong>is: Spectrum <strong>of</strong><br />
parenchymal <strong>CT</strong> findings w<strong>it</strong>h pathologic correlati<strong>on</strong><br />
in 21 AIDS patients. Radiology 192:451-459,<br />
1994.<br />
16. Sider L, Gabriel H, Curry DR, Pham MS: Pattern<br />
recogn<strong>it</strong>i<strong>on</strong> <strong>of</strong> <strong>the</strong> pulm<strong>on</strong>ary manifestati<strong>on</strong>s <strong>of</strong> AIDS<br />
<strong>on</strong> <strong>CT</strong> scans. Radiographics 13:771-784, 1993.<br />
17. Rosen SH, Castleman B, Liebow AA: Pulm<strong>on</strong>ary<br />
alveolar proteinosis. N Engl J Med 258:<br />
1123-1144, 1958.<br />
18. Nhieu JTV, Vojtek AM, Bernaudin JF, et al:<br />
Pulm<strong>on</strong>ary alveolar proteinosis associated w<strong>it</strong>h<br />
Pneumocystis carinii: Ultrastructural identificati<strong>on</strong><br />
in br<strong>on</strong>choalveolar lavage in AIDS and immunocompromised<br />
n<strong>on</strong>-AIDS patients. Chest 98:801-<br />
805, 1990.<br />
19. Godwin JD, Müller NL, Takasugi JE: Pulm<strong>on</strong>ary<br />
alveolar proteinosis: <strong>CT</strong> findings. Radiology<br />
169:609-613, 1988.<br />
20. Murch CR, Carr DH: Computed tomography<br />
appearances <strong>of</strong> pulm<strong>on</strong>ary alveolar proteinosis.<br />
Clin Radiol 40:240-243, 1989.<br />
21. Franquet T, Giménez A, Bordes R, et al: The<br />
crazy-paving pattern in exogenous lipoid pneum<strong>on</strong>ia:<br />
<strong>CT</strong>-pathologic correlati<strong>on</strong>. AJR 170:315,<br />
1998.<br />
22. Fraser RS, Pare JAP, Fraser RG, Pare PD,<br />
(eds): Methods <strong>of</strong> clinical, laboratory, and functi<strong>on</strong>al<br />
investigati<strong>on</strong>. In: Synopsis <strong>of</strong> diseases <strong>of</strong> <strong>the</strong><br />
<strong>chest</strong>, ed 2, pp 141-164. Philadelphia, WB Saunders,<br />
1994.<br />
23. Kuhlman JE, Fishman EK, Siegelman SS:<br />
Invasive pulm<strong>on</strong>ary aspergillosis in acute<br />
leukemia: Characteristic findings <strong>on</strong> <strong>CT</strong>, <strong>the</strong> <strong>CT</strong><br />
halo sign, and <strong>the</strong> role <strong>of</strong> <strong>CT</strong> in early diagnosis.<br />
Radiology 157:611-614, 1985.<br />
23
24. Primack SL, Hartman TE, Lee KS, Müller NL:<br />
Pulm<strong>on</strong>ary nodules and <strong>the</strong> <strong>CT</strong> halo sign. Radiology<br />
190:513-515, 1994.<br />
25. Kazero<strong>on</strong>i EA, Cascade PN, Gross BH:<br />
Transplanted lungs: Nodules following transbr<strong>on</strong>chial<br />
biopsy. Radiology 194:209-212, 1995.<br />
26. Epler GR, Colby TV: The spectrum <strong>of</strong> br<strong>on</strong>chiol<strong>it</strong>is<br />
obl<strong>it</strong>erans. Chest 83:161-162, 1983.<br />
27. Müller NL, Miller RR: State <strong>of</strong> <strong>the</strong> art: Computed<br />
tomography <strong>of</strong> chr<strong>on</strong>ic diffuse infiltrative lung<br />
disease, part 2. Am Rev Respir Dis 142:1440-1448,<br />
1990.<br />
28. Corcoran HL, Renner WR, Milstein MJ:<br />
Review <strong>of</strong> high-resoluti<strong>on</strong> <strong>CT</strong> <strong>of</strong> <strong>the</strong> lung. Radiographics<br />
12:917-939, 1992.<br />
29. Bouchardy LM, Kuhlman JE, Ball WC, et al:<br />
<strong>CT</strong> findings in br<strong>on</strong>chiol<strong>it</strong>is obl<strong>it</strong>erans organizing<br />
pneum<strong>on</strong>ia (BOOP) w<strong>it</strong>h radiographic, clinical, and<br />
histologic correlati<strong>on</strong>. J Comput Assist Tomogr<br />
17:352-357, 1993.<br />
30. Johkoh T, Ikezoe J, Kohno N, et al: High-resoluti<strong>on</strong><br />
<strong>CT</strong> and pulm<strong>on</strong>ary functi<strong>on</strong> tests in collagen<br />
vascular disease: Comparis<strong>on</strong> w<strong>it</strong>h idiopathic<br />
pulm<strong>on</strong>ary fibrosis. Eur J Radiol 18:113-121, 1994.<br />
31. Remy-Jardin M, Remy J, Cortet B, et al: Lung<br />
changes in rheumatoid arthr<strong>it</strong>is: <strong>CT</strong> findings. Radiology<br />
193:375-382, 1994.<br />
32. Wagner RB, Crawford WO, Schimpf PP:<br />
Classificati<strong>on</strong> <strong>of</strong> parenchymal injuries <strong>of</strong> <strong>the</strong> lung.<br />
Radiology 167:77-82, 1988.<br />
33. Schnyder P, Gamsu G, Essinger A, Duvoisin<br />
B: Trauma. In: Moss AA, Gamsu G, Genant HK (eds):<br />
Computed tomography <strong>of</strong> <strong>the</strong> body, pp 311-323.<br />
Philadelphia, WB Saunders, 1992.<br />
34. Hartman TE, Primack SL, Swensen SJ, et al:<br />
Desquamative interst<strong>it</strong>ial pneum<strong>on</strong>ia: Thin-secti<strong>on</strong><br />
<strong>CT</strong> findings in 22 patients. Radiology 187:787-790,<br />
1993.<br />
35. Ar<strong>on</strong>chick JM, Gefter WB: Drug-induced pulm<strong>on</strong>ary<br />
disorders. Semin Roentgenol 30:18-34, 1995.<br />
36. Patz EF, Peters WP, Goodman PC: Pulm<strong>on</strong>ary<br />
drug toxic<strong>it</strong>y following high-dose chemo<strong>the</strong>rapy<br />
w<strong>it</strong>h autologous b<strong>on</strong>e marrow transplantati<strong>on</strong>: <strong>CT</strong><br />
findings in 20 cases. J Thorac Imaging 9:129-134,<br />
1994.<br />
37. Ebara H, Ikezoe J, Johkoh T, et al: Chr<strong>on</strong>ic<br />
eosinophilic pneum<strong>on</strong>ia: Evoluti<strong>on</strong> <strong>of</strong> <strong>chest</strong> radiograms<br />
and <strong>CT</strong> features. J Comput Assist Tomogr<br />
18:737-744, 1994.<br />
38. Tsunemi K, Kanayama I, K<strong>on</strong>do T, et al:<br />
Acute eosinophilic pneum<strong>on</strong>ia evaluated w<strong>it</strong>h highresoluti<strong>on</strong><br />
computed tomography. Intern Med<br />
32:891-894, 1993.<br />
39. Nishimura K, Itoh H, K<strong>it</strong>aichi M, et al: Pulm<strong>on</strong>ary<br />
sarcoidosis: Correlati<strong>on</strong> <strong>of</strong> <strong>CT</strong> and<br />
histopathologic findings. Radiology 189:105-109,<br />
1993.<br />
40. Myers JL, Veal CFJ, Shin MS, Katzenstein A-<br />
LA: Respiratory br<strong>on</strong>chiol<strong>it</strong>is causing interst<strong>it</strong>ial<br />
lung disease: A clinicopathologic study <strong>of</strong> six<br />
cases. Am Rev Respir Dis 135:880-884, 1987.<br />
41. Yousem SA, Colby TV, Gaensler EA: Respiratory<br />
br<strong>on</strong>chiol<strong>it</strong>is-associated interst<strong>it</strong>ial lung disease<br />
and <strong>it</strong>s relati<strong>on</strong>ship to desquamative<br />
interst<strong>it</strong>ial pneum<strong>on</strong>ia. Mayo Clin Proc 64:1373-<br />
1380, 1989.<br />
42. Myers J: Respiratory br<strong>on</strong>chiol<strong>it</strong>is w<strong>it</strong>h interst<strong>it</strong>ial<br />
lung disease. Semin Respir Med 13:134-139,<br />
1992.<br />
43. Holt RM, Schmidt RA, Godwin JD, Raghu G:<br />
High resoluti<strong>on</strong> <strong>CT</strong> in respiratory br<strong>on</strong>chiol<strong>it</strong>is-associated<br />
interst<strong>it</strong>ial lung disease. J Comput Assist<br />
Tomogr 17:46-50, 1993.<br />
REPRINT INFORMATION<br />
Articles found in Applied Radiology and Supplements are available as custom reprints for a<br />
modest charge. If you have wr<strong>it</strong>ten, or been featured in an article, or if you simply find <strong>on</strong>e<br />
<strong>of</strong> our topics appropriate for use in a promoti<strong>on</strong>al or educati<strong>on</strong>al applicati<strong>on</strong>, we will<br />
arrange for reprints for you. Some <strong>of</strong> our readers have found reprints valuable communicati<strong>on</strong><br />
pieces for:<br />
◆ Seminars, c<strong>on</strong>ferences and speaking presentati<strong>on</strong>s ◆ Staff educati<strong>on</strong> and training<br />
◆ Patient educati<strong>on</strong> ◆ Reference and research compilati<strong>on</strong> ◆ Keeping abreast <strong>of</strong> new<br />
technologies ◆ M<strong>on</strong><strong>it</strong>oring imaging trends ◆ Networking and sharing w<strong>it</strong>h colleagues<br />
◆ Resume and curriculum v<strong>it</strong>ae enhancement<br />
For more informati<strong>on</strong> c<strong>on</strong>tact:<br />
Maura Brennan, Anders<strong>on</strong> Publishing Ltd., 1301 West Park Avenue, Ocean, NJ 07712<br />
PHONE: 732-695-0600 ◆ FAX: 732-695-9501 ◆ EMAIL: Anders<strong>on</strong>Pub@compuserve.com<br />
pickup Pediatric AIDS<br />
ad from page 31 <strong>of</strong> <strong>the</strong><br />
September issue<br />
24 APPLIED RADIOLOGY, December 1998