Notice: This CMS-approved document has been submitted - Philips ...
Notice: This CMS-approved document has been submitted - Philips ... Notice: This CMS-approved document has been submitted - Philips ...
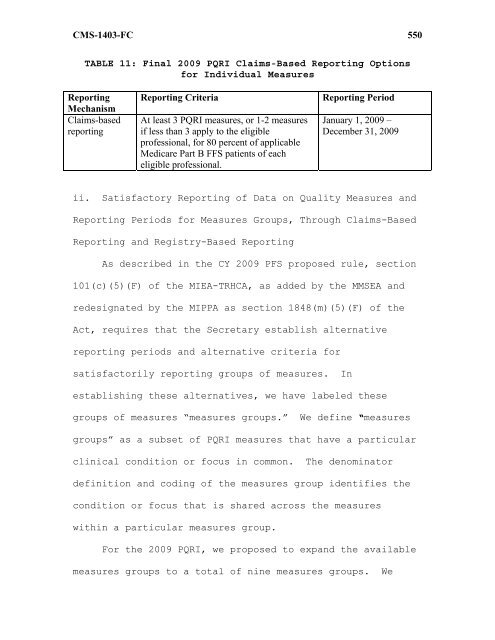
CMS-1403-FC TABLE 11: Final 2009 PQRI Claims-Based Reporting Options for Individual Measures Reporting Mechanism Claims-based reporting Reporting Criteria Reporting Period At least 3 PQRI measures, or 1-2 measures if less than 3 apply to the eligible professional, for 80 percent of applicable Medicare Part B FFS patients of each eligible professional. January 1, 2009 – December 31, 2009 ii. Satisfactory Reporting of Data on Quality Measures and Reporting Periods for Measures Groups, Through Claims-Based Reporting and Registry-Based Reporting As described in the CY 2009 PFS proposed rule, section 101(c)(5)(F) of the MIEA-TRHCA, as added by the MMSEA and redesignated by the MIPPA as section 1848(m)(5)(F) of the Act, requires that the Secretary establish alternative reporting periods and alternative criteria for satisfactorily reporting groups of measures. In establishing these alternatives, we have labeled these groups of measures “measures groups.” We define “measures groups” as a subset of PQRI measures that have a particular clinical condition or focus in common. The denominator definition and coding of the measures group identifies the condition or focus that is shared across the measures within a particular measures group. For the 2009 PQRI, we proposed to expand the available measures groups to a total of nine measures groups. We 550
CMS-1403-FC proposed to carry forward three of the four 2008 measures groups for the 2009 PQRI: (1) Diabetes Mellitus; (2) Chronic Kidney Disease (CKD); and (3) Preventive Care. In addition, we proposed to add six new measures groups for the 2009 PQRI: (1) Coronary Artery Bypass Graft (CABG) Surgery; (2) Coronary Artery Disease (CAD) (3) Rheumatoid Arthritis; (4) Human Immunodeficiency Virus(HIV)/Acquired Immune Deficiency Syndrome (AIDS); (5) Perioperative Care; and (6) Back Pain. We proposed to allow measures groups to be reported through claims-based or registry-based submission for the 2009 PQRI. We proposed that the form and manner of quality data submission for 2009 measures groups would be posted on the PQRI section of the CMS Web site at http://www.cms.hhs.gov/pqri no later than December 31, 2008, and will detail specifications and specific instructions for reporting measures groups via claims and registry-based reporting. The final 2009 PQRI measures groups and the measures selected for inclusion in each of the 2009 measures groups 551
- Page 499 and 500: CMS-1403-FC group could recover onl
- Page 501 and 502: CMS-1403-FC incurred, thereby compe
- Page 503 and 504: CMS-1403-FC needed to provide the t
- Page 505 and 506: CMS-1403-FC performing supplier for
- Page 507 and 508: CMS-1403-FC providers, the services
- Page 509 and 510: CMS-1403-FC commenter also expresse
- Page 511 and 512: CMS-1403-FC overutilization of in-o
- Page 513 and 514: CMS-1403-FC provisions for single-s
- Page 515 and 516: CMS-1403-FC we did not propose such
- Page 517 and 518: CMS-1403-FC and PCs supervised or p
- Page 519 and 520: CMS-1403-FC provisions will not app
- Page 521 and 522: CMS-1403-FC (Pub. L. 110-173) (MMSE
- Page 523 and 524: CMS-1403-FC reporting data on quali
- Page 525 and 526: CMS-1403-FC PQRI and a more detaile
- Page 527 and 528: CMS-1403-FC and our responses to th
- Page 529 and 530: CMS-1403-FC provisions of the Priva
- Page 531 and 532: CMS-1403-FC reducing eligible profe
- Page 533 and 534: CMS-1403-FC administrative or judic
- Page 535 and 536: CMS-1403-FC professionals who did n
- Page 537 and 538: CMS-1403-FC base the incentive paym
- Page 539 and 540: CMS-1403-FC A few commenters noted
- Page 541 and 542: CMS-1403-FC administrative burden t
- Page 543 and 544: CMS-1403-FC requested that more det
- Page 545 and 546: CMS-1403-FC incentive payments for
- Page 547 and 548: CMS-1403-FC December 31, 2009 and J
- Page 549: CMS-1403-FC the reporting period fo
- Page 553 and 554: CMS-1403-FC measures group is appli
- Page 555 and 556: CMS-1403-FC measures results and nu
- Page 557 and 558: CMS-1403-FC (Delmarva Foundation fo
- Page 559 and 560: CMS-1403-FC registries to report on
- Page 561 and 562: CMS-1403-FC reporting options for r
- Page 563 and 564: CMS-1403-FC incentive payment for P
- Page 565 and 566: CMS-1403-FC to report 2009 PQRI qua
- Page 567 and 568: CMS-1403-FC Comment: We received nu
- Page 569 and 570: CMS-1403-FC Comment: One comment su
- Page 571 and 572: CMS-1403-FC quality measures result
- Page 573 and 574: CMS-1403-FC requirements listed on
- Page 575 and 576: CMS-1403-FC a data submission vendo
- Page 577 and 578: CMS-1403-FC As we stated in the CY
- Page 579 and 580: CMS-1403-FC whether eligible profes
- Page 581 and 582: CMS-1403-FC ● Agree that the regi
- Page 583 and 584: CMS-1403-FC soon thereafter as is t
- Page 585 and 586: CMS-1403-FC Comment: We received ma
- Page 587 and 588: CMS-1403-FC Comment: One commenter
- Page 589 and 590: CMS-1403-FC additional 2.0 percent
- Page 591 and 592: CMS-1403-FC EHRs in 2009. The measu
- Page 593 and 594: CMS-1403-FC i. Overview and Summary
- Page 595 and 596: CMS-1403-FC voluntary consensus sta
- Page 597 and 598: CMS-1403-FC Comment: Several commen
- Page 599 and 600: CMS-1403-FC the AMA-PCPI should be
<strong>CMS</strong>-1403-FC<br />
TABLE 11: Final 2009 PQRI Claims-Based Reporting Options<br />
for Individual Measures<br />
Reporting<br />
Mechanism<br />
Claims-based<br />
reporting<br />
Reporting Criteria Reporting Period<br />
At least 3 PQRI measures, or 1-2 measures<br />
if less than 3 apply to the eligible<br />
professional, for 80 percent of applicable<br />
Medicare Part B FFS patients of each<br />
eligible professional.<br />
January 1, 2009 –<br />
December 31, 2009<br />
ii. Satisfactory Reporting of Data on Quality Measures and<br />
Reporting Periods for Measures Groups, Through Claims-Based<br />
Reporting and Registry-Based Reporting<br />
As described in the CY 2009 PFS proposed rule, section<br />
101(c)(5)(F) of the MIEA-TRHCA, as added by the MMSEA and<br />
redesignated by the MIPPA as section 1848(m)(5)(F) of the<br />
Act, requires that the Secretary establish alternative<br />
reporting periods and alternative criteria for<br />
satisfactorily reporting groups of measures. In<br />
establishing these alternatives, we have labeled these<br />
groups of measures “measures groups.” We define “measures<br />
groups” as a subset of PQRI measures that have a particular<br />
clinical condition or focus in common. The denominator<br />
definition and coding of the measures group identifies the<br />
condition or focus that is shared across the measures<br />
within a particular measures group.<br />
For the 2009 PQRI, we proposed to expand the available<br />
measures groups to a total of nine measures groups. We<br />
550