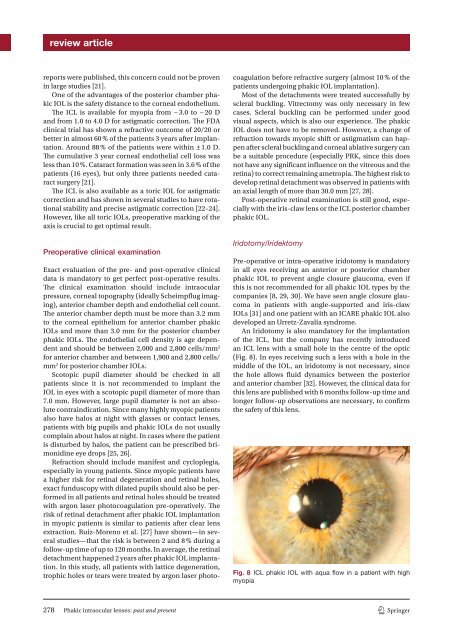
eview articlereports were published, this concern could not be provenin large studies [ 21 ].One of the advantages of the posterior chamber phakicIOL is the safety distance to the corneal endothelium.The ICL is available for myopia from − 3.0 to − 20 Dand from 1.0 to 4.0 D for astigmatic correction. The FDAclinical trial has shown a refractive outcome of 20/20 orbetter in almost 60 % of the patients 3 years after implantation.Around 88 % of the patients were within ± 1.0 D.The cumulative 3 year corneal endothelial cell loss wasless than 10 %. Cataract formation was seen in 3.6 % of thepatients (16 eyes), but only three patients needed cataractsurgery [21 ].The ICL is also available as a toric IOL for astigmaticcorrection and has shown in several studies to have rotationalstability and precise astigmatic correction [22 –24 ].However, like all toric IOLs, preoperative marking of theaxis is crucial to get optimal result.Preoperative clinical examinationExact evaluation of the pre- and post-operative clinicaldata is mandatory to get perfect post-operative results.The clinical examination should include intraocularpressure, corneal topography (ideally Scheimpflug imaging),anterior chamber depth and endothelial cell count.The anterior chamber depth must be more than 3.2 mmto the corneal epithelium for anterior chamber phakicIOLs and more than 3.0 mm for the posterior chamberphakic IOLs. The endothelial cell density is age dependentand should be between 2,000 and 2,800 cells/mm 2for anterior chamber and between 1,900 and 2,800 cells/mm 2 for posterior chamber IOLs.Scotopic pupil diameter should be checked in allpatients since it is not recommended to implant theIOL in eyes with a scotopic pupil diameter of more than7.0 mm. However, large pupil diameter is not an absolutecontraindication. Since many highly myopic patientsalso have halos at night with glasses or contact lenses,patients with big pupils and phakic IOLs do not usuallycomplain about halos at night. In cases where the patientis disturbed by halos, the patient can be prescribed brimonidineeye drops [ 25 , 26 ].Refraction should include manifest and cycloplegia,especially in young patients. Since myopic patients havea higher risk for retinal degeneration and retinal holes,exact funduscopy with dilated pupils should also be performedin all patients and retinal holes should be treatedwith argon laser photocoagulation pre-operatively. Therisk of retinal detachment after phakic IOL implantationin myopic patients is similar to patients after clear lensextraction. Ruiz-Moreno et al. [ 27 ] have shown—in severalstudies—that the risk is between 2 and 8 % during afollow-up time of up to 120 months. In average, the retinaldetachment happened 2 years after phakic IOL implantation.In this study, all patients with lattice degeneration,trophic holes or tears were treated by argon laser photo-coagulation before refractive surgery (almost 10 % of thepatients un<strong>der</strong>going phakic IOL implantation).Most of the detachments were treated successfully byscleral buckling. Vitrectomy was only necessary in fewcases. Scleral buckling can be performed un<strong>der</strong> goodvisual aspects, which is also our experience. The phakicIOL does not have to be removed. However, a change ofrefraction towards myopic shift or astigmatism can happenafter scleral buckling and corneal ablative surgery canbe a suitable procedure (especially PRK, since this doesnot have any significant influence on the vitreous and theretina) to correct remaining ametropia. The highest risk todevelop retinal detachment was observed in patients withan axial length of more than 30.0 mm [ 27 , 28 ].Post-operative retinal examination is still good, especiallywith the iris-claw lens or the ICL posterior chamberphakic IOL.Iridotomy/IridektomyPre-operative or intra-operative iridotomy is mandatoryin all eyes receiving an anterior or posterior chamberphakic IOL to prevent angle closure glaucoma, even ifthis is not recommended for all phakic IOL types by thecompanies [ 8 , 29 , 30 ]. We have seen angle closure glaucomain patients with angle-supported and iris-clawIOLs [ 31 ] and one patient with an ICARE phakic IOL alsodeveloped an Urretz-Zavalia syndrome .An Iridotomy is also mandatory for the implantationof the ICL, but the company has recently introducedan ICL lens with a small hole in the centre of the optic(Fig. 8 ). In eyes receiving such a lens with a hole in themiddle of the IOL, an iridotomy is not necessary, sincethe hole allows fluid dynamics between the posteriorand anterior chamber [ 32 ]. However, the clinical data forthis lens are published with 6 months follow-up time andlonger follow-up observations are necessary, to confirmthe safety of this lens.Fig. 8 ICL phakic IOL with aqua flow in a patient with highmyopia278 Phakic intraocular lenses: past and present 1 3
eview articlePost-operative clinical examinationPost-operative clinical examination should inclu<strong>der</strong>efraction, routine slitlamp examination with measurementof intraocular pressure and funduscopy with dilatedpupils, measurement of the endothelial cell count,and Scheimpflug imaging. Since the anterior chamberchanges with age, Scheimpflug imaging should be performedevery year to document the position of the IOLin the eye and also the anterior chamber depth. This isespecially important in hyperopic patients. As describedabove, significant loss of corneal endothelium is a seriouscomplication after phakic IOL implantation and theIOL should be removed [ 7 ].ConclusionThere has been a great progress in designs and materialsof phakic IOLs within the last 20 years. Two differentkinds of phakic IOLs are FDA approved at the momentand have shown excellent results within the last 10–15years. The iris-claw lens originally invented by Fechnerand Worst and the posterior chamber phakic IOL named‘ICL’. However, FDA approval is only for the treatment ofmyopic patients at the moment. Clinical trials for FDAapproval with toric IOLs are ongoing. The lenses are notyet approved for the implantation in hyperopic patients.Almost all angle supported phakic IOLs have beenabandoned from the market few years after introduction,so far. Alcon has recently introduced a new foldableangle supported phakic IOL made of hydrophobic acrylicmaterial (Cachet, Alcon, USA). Since the maximumfollow-up time with this IOL is only 3 years, refractivesurgeons should be cautious with this IOL, until longerfollow-up periods are published. Many angle-supportedphakic IOLs have shown good results within the first 3years after implantation and had to be abandoned afterwardsdue to serious complications [ 4 ].Financial disclosureThe authors have no financial interest in any techniqueor product mentioned in this manuscript.Conflict of interestTh e authors declare that there are no actual or potentialconflicts of interest in relation to this article.References1. Fujitani A, Hayasaka S, Fukuyama J, Noda S, Setogawa T.Retrocorneal ridges after anterior posterior radial keratotomy(Sato’s operation) in a patient with retinitis pigmentosa.Ann Ophthalmol. 1993;25:392–3.2. Chen LJ, Chang YJ, Kuo JC, Rajagopal R, Azar DT. Metaanalysisof cataract development after phakic intraocular lenssurgery. J Cataract Refract Surg. 2008;34:1181–200.3. Ba i ko ff G. Phakic anterior chamber intraocular lenses. IntOphthalmol Clin. 1991;31:75–86.4. Huang D, Schallhorn SC, Sugar A, et al. Phakic intraocularlens implantation for the correction of myopia: a report bythe American Academy of Ophthalmology. Ophthalmology.2009;116:2244–58.5. Fechner PU, Heijde GL van <strong>der</strong>, Worst JG. Intraocularlens for the correction of myopia of the phakic eye. KlinMonatsbl Augenheilkd. 1988;193:29–34.6. Ba i ko ff G. Refractive phakic IOLs—then and now. Cataract& Refractive Surgery today. 2004:72–4.7. Plainer S, Wenzl E, Saalabian AA, et al. Long-term followupwith I-care phakic IOLs. Br J Ophthalmol. 2011;95:710–4.8. Kohnen T, Knorz MC, Cochener B, et al. AcrySof phakicangle-supported intraocular lens for the correctionof mo<strong>der</strong>ate-to-high myopia: one-year results of a multicenterEuropean study. Ophthalmology. 2009;116:1314–21.9. Javaloy J, Alio JL, Iradier MT, et al. Outcomes of ZB5Mangle-supported anterior chamber phakic intraocularlenses at 12 years. J Refract Surg. 2007;23:147–58.10. Fellner P, Vidic B, Ramkissoon Y, et al. Pupil ovalizationafter phakic intraocular lens implantation is associatedwith sectorial iris hypoperfusion. Arch Ophthalmol.2005;123:1061–5.11. Espandar L, Meyer JJ, Moshirfar M. Phakic intraocularlenses. Curr Opin Ophthalmol. 2008;19:349–56.12. Sourdille P, Baikoff G, Colin J. Safety concers put spotlighton angle-supported phakic IOLs. Eurotimes. 2007 November;8–9.13. Kohnen T, Klaproth OK. Three-year stability of an anglesupportedfoldable hydrophobic acrylic phakic intraocularlens evaluated by Scheimpflug photography. J CataractRefract Surg. 2010;36:1120–6.14. Pechmeja J, Guinguet J, Colin J, Bin<strong>der</strong> PS. Severe endothelialcell loss with anterior chamber phakic intraocularlenses. J Cataract Refract Surg. 2012;38:1288–92.15. Stulting RD, John ME, Maloney RK et al. Three-year resultsof Artisan/Verisyse phakic intraocular lens implantation.Results of the United States Food And Drug Administrationclinical trial. Ophthalmology. 2008;115:464–72 e461.16. Dick HB, Budo C, Malecaze F, et al. Foldable Artiflex phakicintraocular lens for the correction of myopia: two-yearfollow-up results of a prospective European multicenterstudy. Ophthalmology. 2009;116:671–7.17. Koss MJ, Cichocki M, Kohnen T. Posterior synechias followingimplantation of a foldable silicone iris-fixated phakicintraocular lens for the correction of myopia. J CataractRefract Surg. 2007;33:905–9.18. Dick HB, Buchner SE. [Toric phakic intraocular lenses].Ophthalmologe. 2007;104:1032–40.19. Ruckhofer J, Seyeddain O, Dexl AK, Grabner G, Stoiber J.Correction of myopic astigmatism with a foldable iris-clawtoric phakic intraocular lens: short-term follow-up. J CataractRefract Surg. 2012;38:582–8.20. Donoso R, Castillo P. Correction of high myopia with thePRL phakic intraocular lens. Journal of cataract and refractivesurgery. 2006;32:1296–1300.21. San<strong>der</strong>s DR, Doney K, Poco M. United States Food andDrug Administration clinical trial of the implantable collamerlens (ICL) for mo<strong>der</strong>ate to high myopia: three-yearfollow-up. Ophthalmology. 2004;111:1683–92.22. Choi SH, Lee MO, Chung ES, Chung TY. Comparison of thetoric implantable collamer lens and bioptics for myopicastigmatism. J Refract Surg. 2010:1–7.23. Hashem AN, El Danasoury AM, Anwar HM. Axis alignmentand rotational stability after implantation of thetoric implantable collamer lens for myopic astigmatism. JRefract Surg. 2009;25:S939–43.1 3Phakic intraocular lenses: past and present 279